364
THE NEW ENGLAND JOURNAL OF MEDICINE
Feb. 7, 1991
GLUCOSE-INDUCED EXERTIONAL FATIGUE IN MUSCLE PHOSPHOFRUCTOKINASE
DEFICIENCY
RONALD G. HALLER, M.D.,
AND
STEVEN F. LEWIS, PH.D.
Abstract Background. The exercise capacity of patients with muscle phosphofructokinase deficiency is low
and fluctuates from day to day. The basis of this variable
exercise tolerance is unknown, but our patients with this
disorder report that fatigue of active muscles is more rapid
after a high-carbohydrate meal.
Methods and Results. To determine the effect of carbohydrate on exercise performance, we asked four patients with muscle phosphofructokinase deficiency to
perform cycle exercise under conditions of differing availability of substrate - i.e., after an overnight fast, and during an infusion of glucose or triglyceride (with 10 U of
heparin per kilogram of body weight) after an overnight
fast. As compared with fasting and the infusion of triglyceride with heparin, the glucose infusion lowered plasma levels of free fatty acids and ketones, reduced maximal work
capacity by 60 to 70 percent, and lowered maximal oxygen
consumption by 30 to 40 percent. Glucose also increased
the relative intensity of submaximal exercise, as indicated
by a higher heart rate at a given workload during exercise.
The maximal cardiac output (i.e., oxygen delivery) was not
affected by varying substrate availability, but the maximal
systemic arteriovenous oxygen difference was significantly lower during glucose infusion (mean +SE, 5.5+0.3 ml
per deciliter) than after fasting (7.6+0.4 ml per deciliter,
P<0.05) or during the infusion of triglyceride with heparin
(8.9+1.3 ml per deciliter, P<0.05).
Conclusions. In muscle phosphofructokinase deficiency, the oxidative capacity of muscle and the capacity for
aerobic exercise vary according to the availability of bloodborne fuels. We believe that glucose infusion lowers exercise tolerance by inhibiting lipolysis and thus depriving
muscle of oxidative substrate (plasma free fatty acids and
ketones); this impairs the capacity of working muscle to
extract oxygen and lowers maximal oxygen consumption.
(N Engl J Med 1991; 324:364-9.)
DHOSPHOFRUCTOKINASE catalyzes the rate1 limiting reaction in glycolysis, the phosphorylation of fructose-6-phosphate to fructose-i1,6-diphosphate. An inherited deficiency of the muscle form
of phosphofructokinase (muscle phosphofructokinase
deficiency, or Tarui's disease) results in a complete
block in muscle glycolysis and glycogenolysis, leading
to premature muscle fatigue, cramping, and often injury when the muscles' energy demand is increased by
exercise.' Patients with muscle phosphofructokinase
deficiency, like those with muscle phosphorylase deficiency (McArdle's disease), have premature fatigue
not only during isometric exercise or exercise inducing
ischemia but also during dynamic or isotonic exercise. ', Dynamic exercise relies predominantly on
oxidative metabolism3; studies of normal subjects
in whom muscle glycogen has been depleted4 and
patients with muscle phosphorylase deficiency5 suggest that the severe reduction in the capacity for
dynamic exercise when glycolysis in muscle is impaired is due to the inability to generate pyruvate, the
oxidative fuel required to support normal maximal
aerobic power.4'5 As a result, persons with this condition are dependent on alternative fuels such as
free fatty acids to meet requirements for oxidation in
muscle during exercise. In patients with muscle
phosphorylase deficiency, exercise capacity varies according to the availability of these alternative,
blood-borne oxidative substrates. Epitomizing this
substrate-dependent variation in exercise tolerance is
the "second-wind" phenomenon, in which previously
fatiguing exercise can be performed with relative
ease6; this phenomenon is attributable to the increased
availability of blood-borne oxidative substrates, particularly free fatty acids.7'8 In patients with muscle
phosphorylase deficiency, the infusion of glucose or
the administration of agents that stimulate hepatic
glycogenolysis and raise the blood glucose levels also
improves exercise tolerance by augmenting glucose
oxidation by working muscle,9 and some investigators
have postulated that increased utilization of glucose
by working muscle is crucial for the development of a
second wind.'0"'
Exercise tolerance also fluctuates in patients with
muscle phosphofructokinase deficiency, 1'23 although
some investigators argue that a second wind is unusual in such patientsla"' and suggest that this relates to
the fact that utilization of glucose as well as glycogen
is blocked in this disorder. To identify and determine
the possible basis of variations in exercise capacity in
patients with muscle phosphofructokinase deficiency,
we studied five such patients; in four of them we measured exercise capacity under conditions of varying
substrate availability.
METHODS
From the Departments of Neurology (R.G.H.) and Physiology (S.F.L.), Department of Veterans Affairs Medical Center, Dallas, and the University of Texas
Southwestem Medical Center (R.G.H., S.F. L.), Dallas. Address reprint requests
to Dr. Haller at the Neurology Service (127), VA Medical Center, 4500 S.
Lancaster, Dallas, TX 75216.
Supported by the Department of Veterans Affairs, by the Muscular Dystrophy
Association, by grants (HL-06296 and MOI-RR-00633) from the National Institutes of Health, and by the Harry S. Moss Heart Center. Dr. Lewis is the recipient
of a Research Career Development Award (HL-01581) from the National Institutes of Health.
Patients
The five patients studied were an 18-year-old man (Patient 1) and
his 22-year-old sister (Patient 2), a 48-year-old man (Patient 3), and
a 17-year-old woman (Patient 4) and her 10-year-old brother (Patient 5). The histories obtained from the four younger patients were
confirmed by their parents. All the patients were of Ashkenazic
Jewish descent, and the four younger patients were members of
families that practiced Orthodox Judaism. Each of the five patients
had a history of lifelong exercise intolerance with premature muscle
fatigue, and each reported occasions on which initially fatiguing
exercise became more easily tolerated, as in the second-wind phenomenon described in patients with muscle phosphorylase deficien-
The New England Journal of Medicine
Downloaded from nejm.org on October 2, 2016. For personal use only. No other uses without permission.
Copyright © 1991 Massachusetts Medical Society. All rights reserved.
Vol. 324 No. 6
EXERTIONAL FATIGUE IN PFK DEFICIENCY
Perhaps more vivid, however, was their experience in which
exercise that had previously been well tolerated seemed more difficult and produced fatigue more rapidly. Reduced exercise capacity
was typically noted after eating, particularly after a meal high in
carbohydrates. An example of an experience common to the four
younger patients was variable exercise tolerance in walking to synagogue: if they had eaten breakfast, they tired far more easily than
if they had fasted. The major symptoms noted after eating were
increased susceptibility to fatigue of active muscles, manifested by
heaviness or weakness of the limbs and the need to rest frequently. The oldest patient (Patient 3) also had noted that eating a
high-carbohydrate meal reduced his exercise tolerance, but he identified increased susceptibility to exertional nausea as his chief
cy.
symptom.
Three of the four older patients had elevated serum creatine
kinase levels. In addition, all the patients had evidence of a partial
defect of phosphofructokinase in red cells, an elevated serum bilirubin concentration (27.4 to 82.1 ,umol per liter) or an elevated reticulocyte count (or both), and normal hemoglobin and hematocrit
values compatible with a compensated hemolytic anemia. The diagnosis of muscle phosphofructokinase deficiency was established biochemically by the demonstration of an absence of phosphofructokinase in biopsy specimens of skeletal muscle (Patient 1)12 or an
absence of the M subunit of phosphofructokinase in red cells (Patients 3, 4, and 5).14 In one patient (Patient 2), the diagnosis was
inferred from the presence of symptoms and laboratory findings
identical to those in her brother (Patient 1), in whom the diagnosis
was confirmed biochemically. Phosphorus-31 nuclear magnetic resonance (31P NMR) spectroscopy performed during maximal forearm exercise9 in the four older patients revealed the accumulation of
a hexose phosphate peak and the absence of a decrease in muscle
pH from resting values
findings compatible with a metabolic
block at the level of muscle phosphofructokinase.'51'7
The four older patients (Patients 1, 2, 3, and 4) were studied at
the Clinical Research Center, Southwestern Medical Center. The
research protocol was approved by the institutional review board,
and informed consent was obtained from the patients or their parents before testing.
Study Protocol
The patients exercised on a pedal-rate-independent cycle ergom(National Aeronautics and Space Administration Skylab ergometer) at submaximal and maximal workloads for 5 to 6 minutes
in an ascending order of intensity, with 15 minutes of rest between
exercise periods. Maximal exercise was regarded as the highest
workload at which cycling could be continued for five minutes. At
rest and during the last minute at each workload, expired air was
collected in Douglas bags and cardiac output was determined. Ventilation, oxygen uptake, and carbon dioxide production were measured with a Tissot spirometer and a mass spectrometer (PerkinElmer 1I OOA). The ratio of ventilation to oxygen uptake and the
respiratory exchange ratio were calculated from data on gas exchange. Cardiac output was measured noninvasively according to
the acetylene-rebreathing technique of Triebwasser et al.'8 as previously described.'9 The systemic arteriovenous oxygen difference
was calculated from the Fick equation
i.e., by dividing the oxygen uptake (in millieter
-
365
HALLER AND LEWIS
emulsion [Liposyn II, Abbott Laboratories; 5 percent safflower oil
and 5 percent soybean oil] infused at a rate of 1 ml per minute,
beginning 30 minutes before exercise and continuing until the completion of the exercise test) after an overnight fast, with heparin
(a total of 10 U per kilogram of body weight given in three intravenous injections at relatively equal intervals during exercise testing), to promote lipolysis and increase plasma levels of free fatty
acids.
On the first day, the patients underwent preliminary graded exercise testing followed by a rest period of approximately one hour,
during which the glucose infusion was begun, and continued exercise testing during the infusion. On the following day, the exercise
workloads completed during the glucose infusion were repeated and
maximal work capacity during fasting was determined by means of
graded exercise. After a one-hour rest period, during which the
infusion of triglyceride with heparin was begun, graded exercise
testing was repeated. The patients were not aware that exercise
performance was expected to vary with differing metabolic conditions, but they were aware that different substrates were being infused. The number of exercise periods varied as a function of the
maximal work capacity under differing metabolic conditions, ranging from one or two periods during glucose infusion to three or four
periods during fasting and triglyceride-heparin infusion. Accordingly, the total duration of the exercise sessions (sequential periods
of 5 minutes of exercise and 15 minutes of rest) ranged from 20 to
approximately 80 minutes.
Venous (antecubital) blood samples were collected in the last
minute of each exercise period for the determination of substrate
levels. The samples were placed on ice and centrifuged in the cold
within 15 minutes, and the plasma was stored frozen at - 70°C until
assayed. Plasma free fatty acids were measured with a colorimetric
assay.' Plasma ketone (acetoacetic and 13-hydroxybutyric acids)
and glucose levels were determined enzymatically.2' All plasma
samples from each patient were analyzed at the same time in duplicate. The results are expressed as means ±SEM. The statistical
significance of differences in values during glucose infusion, fasting,
and triglyceride-heparin infusion was determined by repeatedmeasures one-way analysis of variance. A Newman-Keuls multiple-comparisons test was used to test for specific intergroup differences. A P value below 0.05 was considered to indicate statistical
significance.
RESULTS
Glucose infusion approximately doubled plasma
glucose levels as compared with levels during fasting
or triglyceride-heparin infusion and was associated
with the lowest levels of plasma free fatty acids and
ketones (Table 1). Triglyceride-heparin infusion resulted in significantly higher plasma levels of free fatty
acids and ketones than did fasting or glucose infusion.
These variations in substrate availability were associated with substantial differences in the responses to
submaximal and maximal exercise.
liters) by the cardiac output (in deciliters).
The heart rate was monitored continuously
by means of electrocardiographic recordings; the rate recorded during the last min-
Table 1. Substraite Levels after Five to Six Minutes of Maximal Exercise in Four Adult
Patients wi ith Muscle Phosphofructokinase Deficiency, According to Study
ute of exercise was correlated with other re-
CONDMONS
sponses to
Conditions.*
GLUCOSE
exercise.
The patients were tested under three conditions: in the fasting state (after an overnight fast lasting 12 to 14 hours); during an
infusion of glucose (10 percent dextrose infused at a rate of 6 ml per minute, beginning
30 minutes before exercise and continuing
until the completion of the exercise test)
after an overnight fast, to simulate a highcarbohydrate meal; and during an infusion
of triglyceride (a 10 percent triglyceride
FEE FArrY AciDs
,B-HYDRoxYBUTYRIC AcD
pmolliter
mmoUliter
Glucose
infusion
Fasting
TiglyceidI0hSpai1 n
infusion
*Valuesa
set
8.8+1.0
3.9±0.3*
4.5±0.2*
0.23±0.04t
0.67±0.17t
1.89±0.35
24±4t
67±22t
454±61
means( : SE) for single plasma samples obtained from each patient at the end of maximal
of metabolic condiiLons.
tP<O.O5 for decon priwn with dhe value duing triglyceride-heparin infusion.
tPc0.05 for dte con nparison with dte value during glucose infusion.
The New England Journal of Medicine
Downloaded from nejm.org on October 2, 2016. For personal use only. No other uses without permission.
Copyright © 1991 Massachusetts Medical Society. All rights reserved.
ACETOACETIC ACID
l0±It
28±8t
183±37
exercise under each
THE NEW ENGLAND JOURNAL OF MEDICINE
366
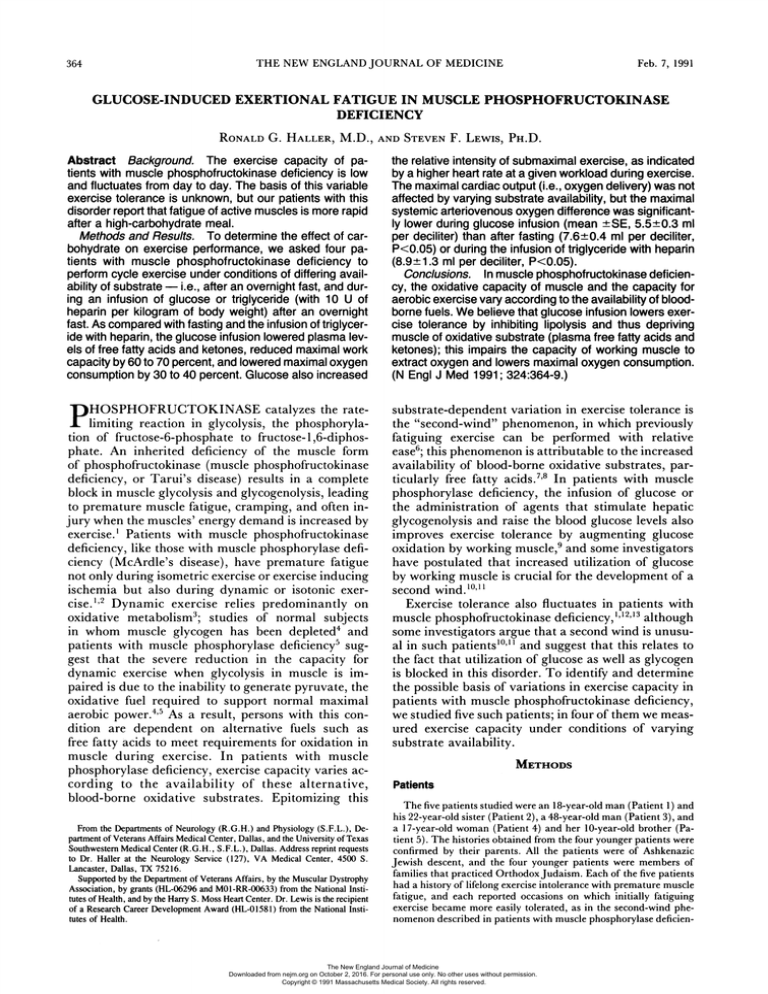
During exercise performed at the same workload
(10 W for Patients 2 and 4, 15 W for Patient 1, and 18
W for Patient 3) and with similar oxygen uptake (Table 2) under each set of study conditions, the mean
heart rate in each patient during glucose infusion
was 16 beats per minute higher than during fasting
(P<0.05) and almost 30 beats higher than during triglyceride-heparin infusion (P<0.05) (Table 2 and
Fig. lA). The mean cardiac output was also significantly higher during glucose infusion than during
fasting (P<0.05) or triglyceride-heparin infusion
(P<0.05) (Table 2). The level of pulmonary ventilation, the ratio of ventilation to oxygen uptake, and the
respiratory exchange ratio were highest during glucose infusion (Fig. lB through 1D). The mean respiratory exchange ratio during glucose infusion, which
was significantly higher than during fasting (P<0.05)
or triglyceride-heparin infusion (P<0.05), paralleled
and was probably caused by the increase in the ratio
of ventilation to oxygen uptake during the glucose
infusion, rather than by an increase in the oxidation of
carbohydrate.
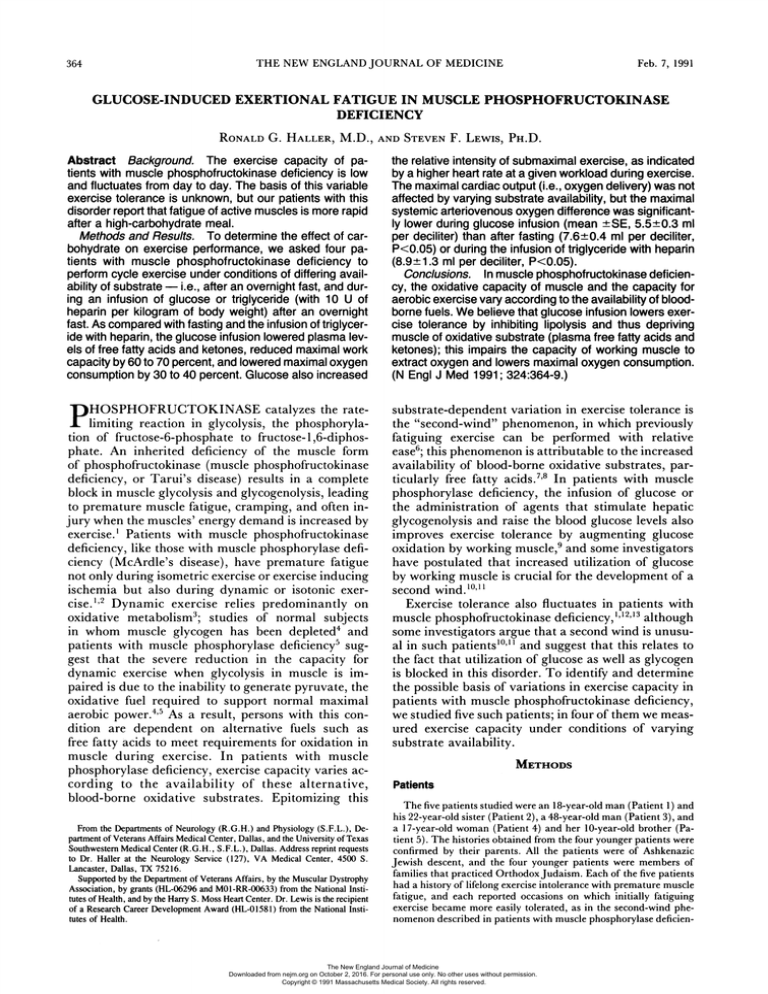
Maximal exercise capacity also was altered significantly by interventions that modified the availability
of substrate. As was consistent with the patients'
histories of decreased exercise tolerance after a highcarbohydrate meal, the maximal work rate and maximal oxygen uptake were lower during glucose infusion (Fig. 2A and 2B). The mean maximal work rate
during glucose infusion (13.3±2.0 W) was less than
half that during fasting (32.5±2.5 W, P<0.05) and
less than one third that during triglyceride-heparin
infusion (41.3±5.9 W, P<0.05). Correspondingly,
the mean maximal oxygen uptake during glucose
infusion (10.5±1.5 ml per kilogram per minute) was
only 70 percent of uptake during fasting (14.6±
2.9 ml per kilogram per minute, P<0.05) and about
60 percent of uptake during triglyceride-heparin infusion (17.0±2.5 ml per kilogram per minute,
P<0.05).
To investigate the physiologic basis for the variation
in maximal oxygen uptake under these conditions of
differing substrate availability, we analyzed the components of oxygen uptake
namely, cardiac output
(representing oxygen delivery) and systemic arteriove-
Feb. 7, 1991
c
c
E
1-
E
r-
0
a:
V
C0
D
I
B
A
ctS
29
a:
cc
70-
1.68
1.2-
0
C.
r_
30
20-
a:
1.0-
0.8
._
10 i
Gloe Fastng Triglydend-
HeparWn
nfusion
Infuslon
Glucose Fasting TriglycerideInfusion
Hepawin
Infusion
D
C
Figure 1. Heart Rate and Respiratory Function during Cycle Exercise in Four Adult Patients with Muscle Phosphofructokinase Deficiency, after Glucose Infusion, Fasting, and TriglycerideHeparin Infusion.
The work intensity for each patient was the same under each set
of metabolic conditions: 10 W for Patient 2 (open squares) and
Patient 4 (solid squares), 15 W for Patient 1 (open circles), and
18 W for Patient 3 (solid circles).
nous oxygen difference (denoting oxygen extraction).
The mean maximal cardiac output was similar under
each set of conditions (glucose infusion, 191+±29 ml
per kilogram per minute; fasting, 193+40; triglyceride-heparin infusion, 196+46), indicating that maximal oxygen delivery was unaltered by glucose or differences in the availability of fatty acids and ketones
(Fig. 2C). In contrast, the mean maximal systemic
arteriovenous oxygen difference was significantly
smaller during glucose infusion than during fasting or
triglyceride-heparin infusion (Fig. 2D). The low
maximal systemic arteriovenous oxygen difference
(5.5 +0.3 ml per deciliter) during glucose infusion suggests that the high carbohydrate load impaired the
capacity of skeletal muscle deficient in phosphofructokinase to extract oxygen from circulating blood. The
mean maximal arteriovenous oxygen difference was
significantly larger during fasting (7.6±0.4 ml per
Table 2. Cardiac and Respiratory Function dunng Constant-Workload Exercise in the Four Adult Patients, According to
Study Conditions.*
CONDMON
WOUoA
W
Glucose infusion
Fasting
Triglyceide-hparin
13.3±t2.0
13.3±2.0
13.3±2.0
OXYGEN
UPfrAKE
m/kg/mnn
10.5±0.6
10.4+0.6
11.0±0.3
CARDIC
OUTPUT
AnTsovEous
VENTILATONI
RoSPRToRY
OXYGEN
OXYGEN
EXCHANGE
HEAR
RATE
DIFFENCE
VENnLATON
liters/min
33±t7
21±2
21±2
literslmin
beatsamin
mildi
11.4+0.6
137±2
5.50±0.15
9.9±0.5t
9.3±O.5t
121±t2t*
109±4t
6.43±0.59
7.15±0.43t
UPTE
RATIO
52±9
1.090. 13
34±2
32±1
0.81±t0.00t
0760t.Olt
ifusion
*Wodcoad was conant over a period of five to six minutes of exercise. Values me nmns (±SE) of single deterinations obtied (as described in the text) during the last minute of exercise in
each padent under each set of measbolic conditions.
VP<0.05 for the comparison widt the value during Iriglyceride-heparin infusion.
tP<0.05 for the compaison with the value during glucose infusion.
The New England Journal of Medicine
Downloaded from nejm.org on October 2, 2016. For personal use only. No other uses without permission.
Copyright © 1991 Massachusetts Medical Society. All rights reserved.
Vol. 324 No. 6
EXERTIONAL FATIGUE IN PFK DEFICIENCY - HALLER AND LEWIS
c
E
r0
c
S
I
oN
A
id
c
0
250-
v-aE 200
150
._.
0
C)
B
8
W
cz
10
E
11
10.
9-
af
100
0
50
0o
0
:s
Glucose Fasig TriglycsdInfusion
Hepan
Infusion
C
GkiMo Fadng Tddglycrd
t
Infusion
t
Heparin
Infusion
D
Figure 2. Maximal Work Intensity, Cardiac Output, and RespiratoFunction dunng Maximal Cycle Exercise under the Three Sets
of Study Conditions.
The four patients are represented by the same symbols used in
Figure 1.
ry
deciliter) than during glucose infusion (P<0.05); with
the marked elevations in plasma levels of free fatty
acids and ketones during triglyceride-heparin infusion, oxygen extraction was almost twice that during
glucose infusion (8.9± 1.3 ml per deciliter, P<0.05).
The levels of oxygen extraction during fasting, glucose
infusion, and triglyceride-heparin infusion varied in
the direction of the changes in the concentrations of
free fatty acids and ketones, implying that oxidative
metabolism in muscle is linked to the availability of
these oxidizable substrates in patients with muscle
phosphofructokinase deficiency.
DISCUSSION
The low exercise capacity of patients with muscle
phosphofructokinase deficiency correlates with their
low maximal oxygen uptake and is consistent with the
crucial role of oxidative metabolism in supporting energy needs during dynamic exercise. The maximal
oxygen uptake in the patients with this disorder was
similar to that in patients with muscle phosphorylase
deficiency studied in our laboratory, representing one
third to one half the uptake in healthy sedentary subjects (30 to 40 ml per kilogram per minute).22
Maximal oxygen uptake is the product of oxygen
delivery and oxygen extraction during maximal exercise. In the patients with muscle phosphofructokinase
deficiency, maximal cardiac output was similar to that
in healthy sedentary subjects,22 implying that maximal oxygen uptake was not limited by oxygen delivery. In contrast, the maximal systemic arteriovenous
oxygen difference in the patients with muscle phosphofructokinase deficiency was low, as reported previously in patients with muscle phosphorylase deficiency.5 These results are consistent with the view that
muscle glycogenolysis is essential for the expression of
367
normal maximal aerobic power during exercise.4'5
They also suggest that the block in muscle glycogenolysis that is common to both muscle phosphorylase
deficiency and muscle phosphofructokinase deficiency, rather than the impaired glucose metabolism in
skeletal muscle or red cells - an additional feature of
muscle phosphofructokinase deficiency'- is the principal mechanism impairing muscle oxidative metabolism. The cellular basis for attenuated maximal oxygen extraction and low maximal oxygen uptake in
muscle phosphorylase deficiency has been postulated
to be substrate-limited oxidative phosphorylation.23
We propose a similar mechanism to account for the
defect in oxidation in patients with muscle phosphofructokinase deficiency.
The block in oxidation of muscle glycogen increases
patients' dependence on circulating oxidative substrates to meet energy requirements during exercise.
This is illustrated by the marked variation in the capacity for dynamic exercise in patients with muscle
phosphorylase deficiency according to the availability
of blood-borne fuels. Pearson and coworkers used the
term "second wind" to characterize the increase in the
capacity for exercise that occurs spontaneously or in
response to infusions of carbohydrate or lipid in patients with muscle phosphorylase deficiency.6 The
common denominator of a second wind - whether
achieved spontaneously, by substrate infusions, or by
interventions that augment substrate mobilization,7
muscle blood flow,8 or cellular fuel transport24 - is
apparently an increased cellular supply of oxidizable
substrate and hence an augmented rate of adenosine
triphosphate production through oxidative phosphorylation.923 Blood glucose is an important oxidative
fuel in muscle phosphorylase deficiency. Increasing
the availability of glucose increases the maximal oxygen uptake and the maximal systemic arteriovenous
oxygen difference5 and attenuates the decrease in
phosphocreatine and the increase in inorganic phosphate in working muscle, as monitored by 31P NMR9
- a finding consistent with enhanced oxidative phosphorylation.
In muscle phosphofructokinase deficiency, in contrast, the utilization of blood glucose is blocked, and
therefore lipids represent the primary fuel available
for muscular work. The dependence of patients with
muscle phosphofructokinase deficiency on lipids as
fuel is indicated by the improvement in their exercise
performance that accompanied the increase in plasma
levels of free fatty acids and ketones during fasting
or triglyceride-heparin infusion, as well as by the
marked decline in exercise capacity when the levels of
free fatty acids and ketones fell during glucose infusion. This glucose-induced decrease in exercise tolerance confirms our patients' experience of increased
effort and more rapid fatigue during exercise after a
high-carbohydrate meal. Glucose lowered the peak
workload that could be attained, and increased the
relative intensity of a given level of exercise, as indicated by the higher heart rate and higher ratio of
The New England Journal of Medicine
Downloaded from nejm.org on October 2, 2016. For personal use only. No other uses without permission.
Copyright © 1991 Massachusetts Medical Society. All rights reserved.
368
Feb. 7, 1991
THE NEW ENGLAND JOURNAL OF MEDICINE
pulmonary ventilation to oxygen uptake in each patient during glucose infusion. Glucose lowered the
maximal oxygen uptake by decreasing the maximal
systemic arteriovenous oxygen difference without altering maximal cardiac output; this finding is consistent with the hypothesis that glucose impairs exercise
performance in patients with muscle phosphofructokinase deficiency by impairing the capacity of working
muscle for oxidative phosphorylation. We propose the
term "out-of-wind" to characterize this carbohydrateinduced decrease in exercise performance.
The effects of glucose infusion in patients with muscle phosphofructokinase deficiency are in direct contrast to the exercise response to the administration of
glucose in patients with muscle phosphorylase deficiency,5- 25 but they are similar to those produced by
the administration of nicotinic acid in patients with
muscle phosphorylase deficiency.8'25'26 Both glucose
and nicotinic acid inhibit triglyceride hydrolysis and
reduce plasma levels of free fatty acids, thus reducing
the level of hepatic ketogenesis and the availability of
lipid fuels for oxidation by working muscle. The antilipolytic effect of glucose in muscle phosphorylase deficiency is apparently countered by an increase in
muscle glucose oxidation, which balances or surpasses
the energy deficit that would otherwise accompany a
decreased availability of lipid fuels. This formulation
is supported by the observation that glucose can produce a second wind in patients with muscle phosphorylase deficiency who are given nicotinic acid.26 In
contrast, in patients with muscle phosphofructokinase
deficiency glucose produces an unopposed decline in
the availability of oxidative substrate and thus a
shortage in the oxidative energy supply relative to demand during exercise.
We propose the scheme outlined in Figure 3 to explain the effect of glucose in muscle phosphofructokinase deficiency. The inability to use glycogen or blood
glucose makes phosphofructokinase-deficient muscle
heavily dependent on fatty acids and ketone bodies as
oxidative fuels. Intravenous glucose or dietary carbohydrate lowers plasma levels of free fatty acids and
reduces hepatic production of ketones, thus depriving
muscle of oxidative substrate. The decline in available
substrate reduces the rate of oxidative phosphorylation and impairs muscle oxygen extraction. Conversely, when free fatty acids and ketones are relatively
plentiful, the rate of oxidative phosphorylation is augmented, muscle oxygen extraction is increased, and
exercise capacity is enhanced. The out-of-wind effect
represents an extreme on the continuum of substrate
availability, opposite to the extreme represented by
the second wind. Both phenomena illustrate that, in
the presence of a complete block in glycogen breakdown due to muscle phosphorylase or muscle phosphofructokinase deficiency, oxidative metabolism in
muscle is paced by access to blood-borne fuels and
thus is subject to peaks and valleys of substrate availability according to dietary and other variables that
condition the mobilization, delivery, or cellular trans-
Figure 3. Postulated Mechanism of the Out-of-Wind Effect Induced by Glucose in Patients with Muscle Phosphofructokinase
Deficiency.
X denotes the site of the metabolic block in skeletal muscle. The
dotted arrows indicate pathways of substrate oxidation that are
blocked as a consequence of phosphofructokinase deficiency.
Oxidative phosphorylation and oxygen uptake (02) by muscle are
largely dependent on the availability of free fatty acids (FFA) and
ketones (produced from FFA in the liver) for the production of
acetyl coenzyme A (acetyl CoA) to support oxidative metabolism.
Glucose lowers (-) FFA levels, thus depriving muscle of substrate and reducing maximal rates of oxidative phosphorylation
and oxygen uptake. ADP denotes adenosine diphosphate, ATP
adenosine triphosphate, and Pi inorganic phosphate.
port of these fuels. Glycogen is thus crucial to normal
muscle oxidative metabolism both because it is needed
to fuel maximal rates of oxidative phosphorylation
and because it is the most readily available of muscle
oxidative substrates and so buffers against normal
fluctuations in the availability of extramuscular fuels
during submaximal exercise.
We are indebted to Dr. Salvatore DiMauro (Department of Neurology, Neurological Institute, Columbia University College of
Physicians and Surgeons, New York) for diagnosis and referral in
the cases of Patients 1 and 2; to Dr. Shobanna Vora (deceased;
Scripps Institute, La Jolla, Calif.) for diagnosis and referral in the
cases of Patients 3, 4, and 5; to Ms. Marguerite Gunder, Ms. Karen
Ayyad, Mr. Paul Gustafson, Mr. Julius Lamar, and Mr. Willie
Moore for expert technical assistance; and to Dr. Gunnar Blomqvist
for invaluable support.
REFERENCES
1. Rowland LT, DiMauro S, Layzer RB. Phosphofructokinase deficiency. In:
Engel AE, Banker BQ, eds. Myology: basic and clinical. New York:
McGraw-Hill, 1986:1603-17.
2. DiMauro S, Bresolin N. Phosphorylase deficiency. In: Engel AE, Banker
BQ, eds. Myology: basic and clinical. New York: McGraw-Hill, 1986:
1585-601.
3. Sahlin K. Metabolic changes limiting muscle performance. In: Saltin B, ed.
Biochemistry of exercise VI. Champaign, Ill.: Human Kinetics, 1986:32343.
4. Gollnick PD. Metabolism of substrates: energy substrate metabolism during
exercise and as modified by training. Fed Proc 1985; 44:353-7.
5. Haller RG, Lewis SF, Cook JD, Blomqvist CG. Myophosphorylase deficiency impairs muscle oxidative metabolism. Ann Neurol 1985; 17:1969.
6. Pearson CM, Rimer DG, Mommaerts WFHM. A metabolic myopathy due
to absence of muscle phosphorylase. Am J Med 1961; 30:502-17.
The New England Journal of Medicine
Downloaded from nejm.org on October 2, 2016. For personal use only. No other uses without permission.
Copyright © 1991 Massachusetts Medical Society. All rights reserved.
Vol. 324 No. 6
EXERTIONAL FATIGUE IN PFK DEFICIENCY - HALLER AND LEWIS
7. Porte D Jr, Crawford DW, Jennings DB, Aber C, Mcllroy MB. Cardiovascular and metabolic responses to exercise in a patient with McArdle's syndrome. N Engl J Med 1966; 275:406-12.
8. Pemow BB, Havel RI, Jennings DB. The second wind phenomenon in
McArdle's syndrome. Acta Med Scand Suppl 1967; 472:294-307.
9. Lewis SF, Haller RG, Cook JD, Nunnally RL. Muscle fatigue in McArdle's
disease studied by 31P-NMR: effect of glucose infusion. J Appl Physiol
1985; 59:1991-4.
10. Tarui S, Mineo I, Shimizu T, Sumi S, Kono N. Muscle phosphofructokinase deficiency and related disorders. In: Serratrice G, Desnuelle C, Pellissier J, et al., eds. Neuromuscular diseases. New York: Raven Press,
1984:71-7;
11. Mineo I, Kono N, Shimizu T, Sumi S, Nonaka K, Tarui S. A comparative
study of glucagon effect between McArdle disease and Tarui disease. Muscle Nerve 1984; 7:552-9.
12. Layzer RB, Rowland LP, Ranney HM. Muscle phosphofructokinase deficiency. Arch Neurol 1967; 17:512-23.
13. Agamanolis DP, Askari AD, DiMauro S, et al. Muscle phosphofructokinase
deficiency: two cases with unusual polysaccharide accumulation and immunologically active enzyme protein. Muscle Nerve 1980; 3:456-67.
14. Vora S, Davidson M, Seaman C, et al. Heterogeneity of the molecular
lesions in inherited phosphofructokinase deficiency. J Clin Invest 1983;
72:1995-2006.
15. Edwards RHT, Dawson MJ, Wilkie DR, Gordon RE, Shaw D. Clinical use
of nuclear magnetic resonance in the investigation of myopathy. Lancet
1982; 1:725-31.
16. Argov Z, Bank WJ, Maris J, Leigh JS Jr, Chance B. Muscle energy metabolism in human phosphofructokinase deficiency as recorded by 3 1P nuclear
magnetic resonance spectroscopy. Ann Neurol 1987; 22:46-51.
17. Duboc D, Jehenson P, Tran-Dinh S, Marsac C, Syrota A, Fardeau M.
Phosphorus NMR spectroscopy study of muscular enzyme deficiencies involving glycogenolysis and glycolysis. Neurology 1987; 37:663-71.
18. Triebwasser JH, Johnson RU, Burpo RP, Campbell JC, Reardon WC,
Blomqvist CG. Noninvasive determination of cardiac output by a modified
acetylene rebreathing procedure utilizing mass spectrometer. Aviat Space
Environ Med 1977; 48:203-9.
19. Haller RG, Lewis SF, Estabrook RW, DiMauro S, Servidei S, Foster DW.
Exercise intolerance, lactic acidosis, and abnormal cardiopulmonary regulation in exercise associated with adult skeletal muscle cytochrome c oxidase
deficiency. J Clin Invest 1989; 84:155-61.
20. Lauwerys RR. Colorimetric determination of free fatty acids. Anal Biochem
1969; 32:331-3.
21. Williamson DH, Mellanby J, Krebs HA. Enzymatic determination of D(-)3-hydroxybutyric acid and acetoacetic acid in blood. Biochem J 1962;
82:90-6.
22. Lewis SF, Haller RG. Skeletal muscle disorders and associated factors that
limit exercise performance. Exerc Sport Sci Rev 1989; 17:67-113.
23. Idem. The pathophysiology of McArdle's disease: clues to regulation in
exercise and fatigue. J Appl Physiol 1986; 61:391-401.
24. Schmid R, Mahler R. Chronic progressive myopathy with myoglobinuria:
demonstration of a glycogenolytic defect in the muscle. J Clin Invest 1959;
38:2044-58.
25. Haller RG, Lewis SF. Abnormal ventilation during exercise in McArdle's
syndrome: modulation by substrate availability. Neurology 1986; 36:7169.
26. Lewis SF, Haller RG, Cook JD, Blomqvist CG. Metabolic control of cardiac output response to exercise in McArdle's disease. J Appl Physiol 1984;
57:1749-53.
~>I
Old Woa of th Kaa
369
a UgnaDVDHIE,MD
The New England Journal of Medicine
Downloaded from nejm.org on October 2, 2016. For personal use only. No other uses without permission.
Copyright © 1991 Massachusetts Medical Society. All rights reserved.