Improvement of motor performance and modulation of cortical
advertisement
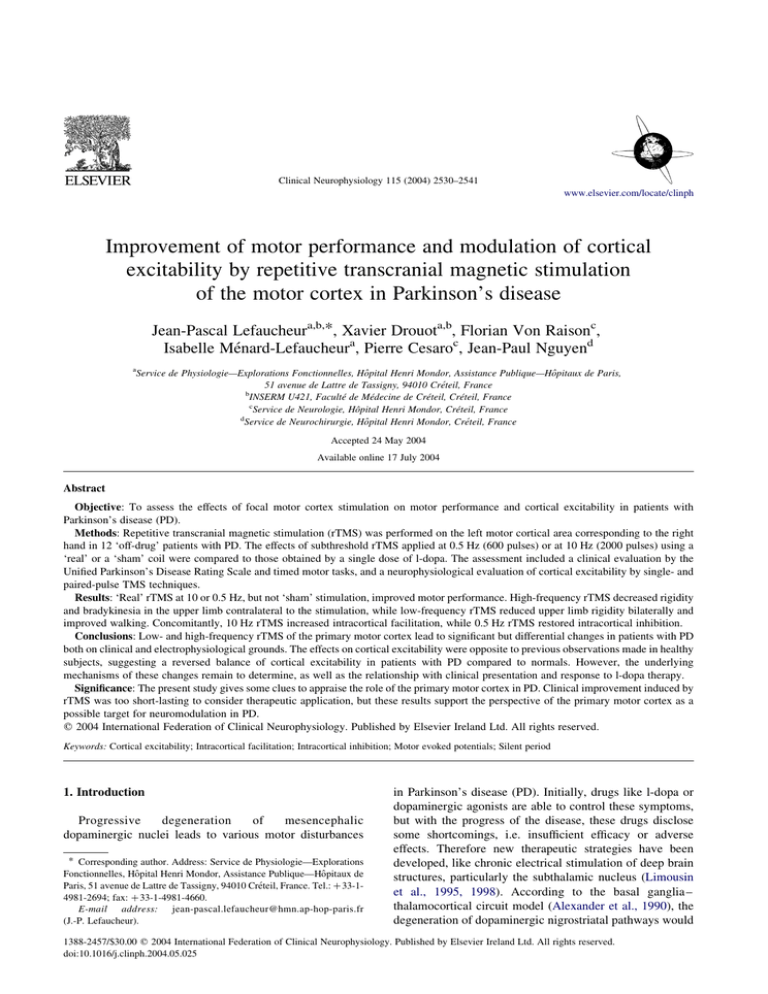
Clinical Neurophysiology 115 (2004) 2530–2541 www.elsevier.com/locate/clinph Improvement of motor performance and modulation of cortical excitability by repetitive transcranial magnetic stimulation of the motor cortex in Parkinson’s disease Jean-Pascal Lefaucheura,b,*, Xavier Drouota,b, Florian Von Raisonc, Isabelle Ménard-Lefaucheura, Pierre Cesaroc, Jean-Paul Nguyend a Service de Physiologie—Explorations Fonctionnelles, Hôpital Henri Mondor, Assistance Publique—Hôpitaux de Paris, 51 avenue de Lattre de Tassigny, 94010 Créteil, France b INSERM U421, Faculté de Médecine de Créteil, Créteil, France c Service de Neurologie, Hôpital Henri Mondor, Créteil, France d Service de Neurochirurgie, Hôpital Henri Mondor, Créteil, France Accepted 24 May 2004 Available online 17 July 2004 Abstract Objective: To assess the effects of focal motor cortex stimulation on motor performance and cortical excitability in patients with Parkinson’s disease (PD). Methods: Repetitive transcranial magnetic stimulation (rTMS) was performed on the left motor cortical area corresponding to the right hand in 12 ‘off-drug’ patients with PD. The effects of subthreshold rTMS applied at 0.5 Hz (600 pulses) or at 10 Hz (2000 pulses) using a ‘real’ or a ‘sham’ coil were compared to those obtained by a single dose of l-dopa. The assessment included a clinical evaluation by the Unified Parkinson’s Disease Rating Scale and timed motor tasks, and a neurophysiological evaluation of cortical excitability by single- and paired-pulse TMS techniques. Results: ‘Real’ rTMS at 10 or 0.5 Hz, but not ‘sham’ stimulation, improved motor performance. High-frequency rTMS decreased rigidity and bradykinesia in the upper limb contralateral to the stimulation, while low-frequency rTMS reduced upper limb rigidity bilaterally and improved walking. Concomitantly, 10 Hz rTMS increased intracortical facilitation, while 0.5 Hz rTMS restored intracortical inhibition. Conclusions: Low- and high-frequency rTMS of the primary motor cortex lead to significant but differential changes in patients with PD both on clinical and electrophysiological grounds. The effects on cortical excitability were opposite to previous observations made in healthy subjects, suggesting a reversed balance of cortical excitability in patients with PD compared to normals. However, the underlying mechanisms of these changes remain to determine, as well as the relationship with clinical presentation and response to l-dopa therapy. Significance: The present study gives some clues to appraise the role of the primary motor cortex in PD. Clinical improvement induced by rTMS was too short-lasting to consider therapeutic application, but these results support the perspective of the primary motor cortex as a possible target for neuromodulation in PD. q 2004 International Federation of Clinical Neurophysiology. Published by Elsevier Ireland Ltd. All rights reserved. Keywords: Cortical excitability; Intracortical facilitation; Intracortical inhibition; Motor evoked potentials; Silent period 1. Introduction Progressive degeneration of mesencephalic dopaminergic nuclei leads to various motor disturbances * Corresponding author. Address: Service de Physiologie—Explorations Fonctionnelles, Hôpital Henri Mondor, Assistance Publique—Hôpitaux de Paris, 51 avenue de Lattre de Tassigny, 94010 Créteil, France. Tel.: þ 33-14981-2694; fax: þ 33-1-4981-4660. E-mail address: jean-pascal.lefaucheur@hmn.ap-hop-paris.fr (J.-P. Lefaucheur). in Parkinson’s disease (PD). Initially, drugs like l-dopa or dopaminergic agonists are able to control these symptoms, but with the progress of the disease, these drugs disclose some shortcomings, i.e. insufficient efficacy or adverse effects. Therefore new therapeutic strategies have been developed, like chronic electrical stimulation of deep brain structures, particularly the subthalamic nucleus (Limousin et al., 1995, 1998). According to the basal ganglia – thalamocortical circuit model (Alexander et al., 1990), the degeneration of dopaminergic nigrostriatal pathways would 1388-2457/$30.00 q 2004 International Federation of Clinical Neurophysiology. Published by Elsevier Ireland Ltd. All rights reserved. doi:10.1016/j.clinph.2004.05.025 J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 result in functional deafferentation of the frontal cortex, including the primary motor cortex, that could contribute to the pathophysiology of motor disturbances in patients with PD. Therefore, the motor cortex is an appealing target for neuromodulation therapy in PD. Cortical activity can be transiently modified by the application of repetitive transcranial magnetic stimulation (rTMS). Shortening of reaction time and movement time during 5 Hz rTMS applied over the motor cortex was first shown in patients with PD in 1994 (Pascual-Leone et al., 1994). Since this first study, several rTMS trials have been reported in PD, based on various experimental designs: (i) focal stimulation using a figure-of-eight coil or non-focal stimulation using a circular coil; (ii) low-frequency stimulation (from 0.2 to 1 Hz) or high-frequency stimulation (5, 10 or 20 Hz); (iii) subthreshold stimulation, i.e. at intensity lower than motor threshold, or suprathreshold stimulation, i.e. at intensity above motor threshold; (iv) clinical assessment by motor task speed measurement or by motor performance scoring, e.g. using the Unified Parkinson’s Disease Rating Scale (UPDRS). Then, the results of all the previous rTMS studies performed in patients with PD are puzzling owing to their methodological differences. Only one study assessed the effects of focal primary motor cortex stimulation on UPDRS score (Siebner et al., 2000b) and showed a significant improvement of the UPDRS score after a 20 min session of subthreshold 5 Hz rTMS. Beside rTMS protocols, single- or paired-pulse TMS paradigms allow to study some excitatory and inhibitory nervous pathways involved in motor control, and provide various parameters of cortical excitability, e.g. motor threshold, silent period, intracortical inhibition or facilitation. Studies of cortical excitability determinants in PD disclosed mainly a reduction of motor inhibitory control, which could be restored following various antiparkinsonian medication or neurosurgical therapies (reviewed in Cantello et al. (2002)), whereas the influence of rTMS remains unknown. In the present series of 12 patients with PD, we have tested the effects of motor cortex rTMS on motor performance assessed by UPDRS scoring and timed motor tasks, and on motor cortex excitability assessed by single- and paired-pulse TMS techniques. Sessions of rTMS were applied at two frequencies, 0.5 and 10 Hz, compared to sham stimulation (negative control) and to l-dopa administration (positive control). 2. Patients and methods 2.1. Patients Twelve patients (5 women and 7 men) aged from 51 to 76 years (mean ^ SEM: 64 ^ 2) were included in this study. All these patients fulfilled the UK Parkinson’s Disease 2531 Brain Bank criteria for idiopathic PD (Gibbs and Lees, 1988) and suffered from a bilateral akinetic-rigid syndrome. Patients with permanent rest tremor were excluded from the study because of their impossibility to maintain a complete relaxation of hand muscles, precluding a reliable determination of the rest motor threshold. Other exclusion criteria were the presence of implanted devices or a past personal history of seizure. All patients gave their written informed consent for the study, which was approved by the ethical committee of Henri Mondor Hospital. The clinical features of the patients are presented in Table 1, including the modified Hoehn and Yahr staging scale and the Schwab and England Activities of Daily Living scale. 2.2. General design Patients were examined 12 h after an overnight withdrawal of anti-parkinsonian medication, i.e. in ‘off-drug’ condition (no patient was treated by long-acting dopaminergic agonists). First, motor performance was assessed clinically and TMS parameters of motor cortex excitability (see below) were measured (‘pre’ condition). Second, one of the 4 interventions, i.e. l-dopa intake, 0.5 Hz rTMS, 10 Hz rTMS or sham rTMS (see below) was performed. Twenty minutes after the end of the rTMS session, both clinical motor evaluation and cortical excitability measurement were checked on again (‘post’ condition). Evaluation after l-dopa intake was performed in the earliest best-on condition according to the patients (usually 30 – 60 min after drug administration). About 30 – 45 min were requested to complete both clinical and electrophysiological evaluations. The order of the 3 rTMS interventions was randomised across patients, and each session were separated Table 1 Clinical data for the 12 patients Patient (n) Age Sex Hoehn (years) and Yahr classification Schwab Disease l-Dopa and duration equivalent England (years) (mg) scale (%) 1 2 3 4 5 6 7 8 9 10 11 12 67 51 66 67 60 76 69 57 58 73 74 51 4 4 4 4 4 3.5 3.5 3 3 2.5 2.5 2.5 60 70 70 70 80 70 50 80 80 80 90 90 22 13 10 10 11 12 18 11 9 7 7 4 3.4^0.2 74^3 11^1 Mean^SEM 64^2 F M M M F M M M F M F F 850 900 900 950 750 900 1000 560 700 750 500 250 701^75 The l-dopa equivalent dose was calculated on the basis of drug correspondences proposed by Lozano et al. (1995). 2532 J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 by at least 3 weeks in order to minimize the effects of practice. 2.3. Clinical motor performance A well-trained neurologist (Dr Florian Von Raison) performed the clinical examination before and after each intervention. This examiner and the patients were blinded for the type of rTMS intervention. First, the patients were rated on the motor section (items 18– 31) of the UPDRS III. Rigidity score for the right and the left upper limbs was the item 22 of the UPDRS motor score. Bradykinesia score for the right and the left upper limbs was calculated as the sum of items 23– 25 of the UPDRS motor score. Second, timed motor tasks were performed, including a ballistic task and a pegboard test. For the ballistic task, the patients were asked to tap with the index finger two targets drawn on a table and fixed 30 cm apart, as fast as possible, the score being the time (in seconds) to achieve 20 go-and-back. For the pegboard test, the patients had to pick the pegs from a well, one by one, using only one hand and to insert consecutively them into the holes. The peg tray consisted in two rows of 30 holes each (Purdue Pegboard). The subjects were instructed to move as fast as possible in attempting to place all pegs. The score was the number of pegs arranged in 30 s. For these both tests, the patients sat comfortably on a chair and they performed the task with the right hand first, then with the left hand. Third, gait performance was analysed using the walking test of the Core Assessment Program for Surgical Interventional Therapies (CAPSIT) in PD (Defer et al., 1999). Briefly, patients were asked to walk as fast as possible 7 m back and forth including turning. The time and the number of steps were recorded. was recorded from the right FDI muscle using surface electrodes in a belly-tendon montage. After amplification and bandpass (20 – 5000 Hz) filtering, raw signals were recorded and stored on floppy disk for off-line analysis (Phasis II, EBNeuro, Florence, Italy). In order to evaluate motor cortex excitability, we measured the motor threshold at rest (RMT), the MEP size at 120% RMT intensity (MEP120), the duration of the cortical silent period (CSP) and both the intracortical inhibition (ICI) and facilitation (ICF). RMT was defined as the minimum intensity of stimulation, which was required in producing MEPs of 50 mV in amplitude at least, in 5 out of 10 trials while the target muscle being relaxed (Rossini et al., 1994). Thereafter, average peak-to-peak MEP size was determined over 5 single trials performed at 120% RMT intensity (MEP120). CSP was obtained by delivering a single TMS pulse at suprathreshold intensity (140% RMT) during a tonic FDI muscle contraction. The shortest CSP duration was measured from the negative peak of the MEP until the first reoccurrence of voluntary electromyographic activity in a series of 5 consecutive trials (Ridding et al., 1995). Paired-pulse paradigm was performed to assess intracortical excitability according to the Kujirai’s procedure (Kujirai et al., 1993), using a BiStim module (Magstim Co., Whitland, Carmarthenshire, Wales) and a figure-of-eight coil. The intensity was set at 80% RMT for the conditioning stimulus and at 120% RMT for the test stimulus. Short interstimuli intervals (ISIs of 2 – 4 ms) were applied to assess ICI, whereas longer ISIs (10 – 15 ms) allowed ICF measurement. Eight trials were recorded for each condition and were averaged. The conditioned test MEP120 amplitude was expressed as percentage of the unconditioned test MEP120 amplitude. For each patient, the maximal ICI and ICF values, whatever ISI, were retained for analysis (Chen et al., 1998). 2.4. Motor cortex excitability 2.5. Interventions Patients sat on a comfortable reclining chair. Magstim 200 magnetic stimulator (Magstim Co., Whitland, Carmarthenshire, Wales) and a figure-of-eight stimulating coil (70 mm Double Coil, 9925-00, Magstim Co., Whitland, Carmarthenshire, Wales) were used to activate the left motor cortical area corresponding to the right first dorsal interosseus (FDI) muscle. The coil was held tangentially to the patients’ head surface over the left motor cortex with the handle of the coil pointing occipitally. Using this orientation, the current induced in the brain flows perpendicular to the line of the central sulcus, which leads to predominately trans-synaptic activation of the corticospinal system (Kaneko et al., 1996). The coil was moved to determine the optimal position for eliciting MEPs of maximal amplitude in the right FDI muscle, i.e. the ‘motor hot spot’. When the motor hot spot was found, the stimulation coil was fixed with a device to maintain the same location throughout the experiment. Electromyogram The 4 interventions were: (i) l-dopa intake. Corresponding to 150% of the usual morning dose administered per os; (ii) 0.5 Hz rTMS. A 20 min stimulation applied at 80% RMT intensity and 0.5 Hz frequency (600 stimuli) over the left primary motor cortical area corresponding to the right hand using a real TMS coil; (iii) 10 Hz rTMS. A series of 20 trains of 10 s duration (50 s intertrain intervals) applied at 80% RMT intensity and 10 Hz frequency (2000 stimuli) over the same target using a real TMS coil; (iv) sham rTMS. The same protocol as for 10 Hz rTMS but using a sham 8-shaped coil (Magstim Placebo Coil System 1730-23-00, Magstim Co., Whitland, Carmarthenshire, Wales). A sham rTMS session was not performed at 0.5 Hz to lighten the protocol. The rTMS sessions were applied using the Super-Rapid Magstim magnetic stimulator (Magstim Co., Whitland, Carmarthenshire, Wales) and an 8-shaped coil (70 mm J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 2533 Double Coil, 9925-00, The Magstim Co., Whitland, Carmarthenshire, Wales) held tangentially to the patients’ head surface over the left motor cortical hot spot corresponding to the right FDI muscle with the handle of the coil pointing occipitally. As aforementioned, using this orientation, the induced current leads to trans-synaptic activation of the corticospinal system over the precentral gyrus. The Magstim Placebo Coil System, which was designed not to have a stimulating effect on the cortex, was preferred to the method consisting in holding a real TMS coil angled 458 tangentially to the scalp, which do not meet the criteria for an ideal sham, as previously shown (Loo et al., 2000). Moreover, the patients were informed that the 3 rTMS sessions were different but not that they included a placebo condition. Therefore, even if the sham coil caused no sensorimotor stimulation of trigeminal afferents or scalp muscles, we assumed that the patients could not realize that sham rTMS was ineffective. and the rigidity subscore bilaterally, and improved walking; 10 Hz rTMS decreased the global UPDRS III motor score, reduced rigidity and bradykinesia subscores and improved the ballistic task for the right upper limb, without any effect on gait; sham rTMS did not modify any parameter. 2.6. Statistical analysis 4. Discussion The variations among the conditions were assessed for the clinical scores of motor performance (rigidity and bradykinesia subscores of UPDRS, ballistic task, pegboard test and gait analysis) and for the various parameters of motor cortex excitability (RMT, MEP120 amplitude, CSP duration, ICI and ICF) using non-parametric repeated measures ANOVA (Friedman test). Dunn’s post-tests were applied to compare the results before and after each type of intervention. A P value of less than 0.05 was considered as significant. The present study showed that primary motor cortex stimulation could improve motor performance in patients with PD, concomitantly with cortical excitability changes. The mean reduction of UPDRS motor score resulting from 0.5 or 10 Hz rTMS (2 19.5 or 2 17.1%) was equal to 28 – 32% of the l-dopa effect (2 61.2%). Because it was not ethical to keep patients unmedicated for several days, we were not able to appraise the duration of rTMS effects, as it was reported for patients with writer’s cramp (Siebner et al., 1999a) or neurogenic pain (Lefaucheur et al., 2001). However, a majority of patients indicated that the day after the 10 Hz rTMS session was better than usual. 3.2. Motor cortex excitability A significant variation among the conditions was found for all the electrophysiological parameters (P , 0:05; Friedman test), except for RMT ðP ¼ 0:94Þ: Dunn’s post-tests disclosed various significant changes depending on the type of intervention: MEP120 amplitude was reduced by l-dopa; CSP duration was prolonged by l-dopa, 0.5 Hz and 10 Hz rTMS; ICI was restored by l-dopa and 0.5 Hz rTMS; ICF was improved only by 10 Hz rTMS. No other significant modification was observed, particularly following sham rTMS. 3. Results 4.1. Effects on motor performance No adverse effect of rTMS was observed. The results of the 4 interventions (l-dopa intake, 0.5 Hz rTMS, 10 Hz rTMS or sham rTMS) are shown by Figs. 1 and 2 for clinical scores and by Fig. 3 for motor cortex excitability parameters. Due to the limited number of patients, it was impossible to define subgroups and to determine statistically the influence of the age of the patient, of the stage or the duration of the disease, or of the dose of l-dopa intake on these results. 3.1. Clinical motor performance A significant variation among the conditions was found for all the clinical parameters (P , 0:05; Friedman test in all cases). Dunn’s post-tests disclosed various significant effects for each type of intervention: l-dopa administration decreased the global UPDRS III motor score, reduced rigidity and bradykinesia subscores for both upper limbs, and improved timed motor tasks and gait performance; 0.5 Hz rTMS reduced the global UPDRS III motor score The present study compared the effects induced by highand low-frequency rTMS of the motor cortex in patients with PD: 10 Hz rTMS improved bradykinesia and rigidity subscores of the upper limb controlaterally to the stimulation, while 0.5 Hz rTMS improved upper limb rigidity bilaterally, as well as walking. In fact, the two types of stimulation differed for frequency but also for the number of stimuli. The number of stimuli could act on the duration of the after effects (Touge et al., 2001). In contrast, the way of interhemispheric excitability changes was shown to be associated with rTMS frequency (0.5 versus 5 Hz), independent of pulse number (Gorsler et al., 2003). Therefore we assumed that the differential effects obtained in this study following 0.5 or 10 Hz rTMS sessions were likely to result from the difference in stimulation frequency rather than in pulse number. The various studies including rTMS protocols applied over the primary motor cortex and performed in patients with PD are listed in Table 2. The first trial of 2534 J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 Fig. 1. Total UPDRS III score and subscores for rigidity and bradykinesia of the right (R) and the left (L) upper limb, before (black bars) and after (white bars) each type of intervention (l-dopa intake or rTMS session). Values are presented as means þ s.e.m. Variation among the conditions was significant for all the scores (P # 0:0001 (a –e), Friedman test). Significant differences between before and after intervention are indicated (*: P , 0:05; **: P , 0:01; ***: P , 0:001; Dunn’s post-tests). high-frequency rTMS of the primary motor cortex was characterized by positive effects on reaction time and movement time in patients with PD compared to controls: performance on the pegboard test was significantly improved during subthreshold 5 Hz rTMS (Pascual-Leone et al., 1994). However, this result was not confirmed in a larger replicative study compared to sham stimulation, some patients performing faster during rTMS, others showing the opposite effect (Ghabra et al., 1999). Using a ballistic task, Siebner et al. (1999b) reported that bradykinesia could be reduced in patients with PD beyond the time of magnetic stimulation, i.e. after subthreshold 5 Hz rTMS applied over the cortical area corresponding to the moving arm. In the present study, we confirmed that subthreshold high-frequency rTMS over the left motor cortex was able to improve the performance of the right upper limb in a timed ballistic task, without any significant change in the pegboard score. This discrepancy probably reflects the distinct effect that rTMS exerted on brain networks engaged by the two tests, which disclose different abnormalities of motor control resulting in bradykinesia. J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 2535 Fig. 2. Results for timed motor tasks (ballistic task: hand-arm movement (time in seconds) and pegboard score (number of pegs) for the right (R) and the left (L) upper limb; gait: walking time and number of steps), before (black bars) and after (white bars) each type of intervention (l-dopa intake or rTMS session). Values are presented as means þ SEM. Variation among the conditions was significant for all the parameters (P ¼ 0:0011 (a), 0.0319 (b), 0.0107 (c), 0.0221 (d), 0.0001 (e), 0.0005 (f), Friedman test). Significant differences between before and after intervention are indicated (*: P , 0:05; **: P , 0:01; Dunn’s post-tests). Improvement of UPDRS motor score after motor cortex stimulation was previously reported in only one paper, which tested one session of 5 Hz rTMS compared to midfrontal sham rTMS (Siebner et al., 2000b). The reduction in UPDRS score was mainly due to alleviation of bradykinesia and rigidity in the upper limb contralaterally to the stimulated cortex. Similar results were obtained in the present study following one session of 10 Hz rTMS. Another study assessed clinical motor effects of high-frequency rTMS (5, 10 or 20 Hz) in a series of 7 unmedicated patients with PD, but did not report any significant change in UPDRS score, walking speed or motor reaction time (Tergau et al., 1999). Unfortunately, this latter study was performed with a large circular coil centred over the vertex. The possibility of stimulating various cortical areas other than the primary motor cortex limits considerably the value of non-focal stimulation of frontal areas using a circular coil in PD. For example, stimulation of the motor supplementary area, which is located only 2 –4 cm anterior to the vertex, adjacent to the leg area of the primary motor cortex, was consistently shown to worsen motor performance in patients with PD (Boylan et al., 2001; Cunnington et al., 1996). Positive effects of low-frequency rTMS on motor performance of patients with PD were also previously reported, even by means of repeated sessions (Ikeguchi 2536 J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 Fig. 3. Rest motor threshold, motor evoked potential (MEP) size at 120% suprathreshold intensity, silent period duration to cortical stimulation, intracortical inhibition and intracortical facilitation (expressed as % of conditioned MEP amplitude), before (black bars) and after (white bars) each type of intervention (l-dopa intake or rTMS session). Values are presented as means þ SEM. Variation among the conditions was significant for all the parameters (P ¼ 0:0333 (b), 0.0003 (c), 0.0001 (d), 0.0070 (e), Friedman test), except for the motor threshold (P ¼ 0:9416 (a), Friedman test). Significant differences between before and after intervention are indicated (*: P , 0:05; **: P , 0:01; Dunn’s post-tests). et al., 2003; Mally and Stone, 1999a,b; Shimamoto et al., 2001). However, these results remained controversial (Okabe et al., 2003) and were also obtained with a large circular coil applied to frontal areas, raising the same problems of specificity as discussed above. The present study used a focal coil and showed that bilateral effects on upper limb rigidity could result from unilateral, low-frequency stimulation of the hand motor cortical area. Such a bilateral improvement resulting from unilateral rTMS could be explained at a cortical level, as discussed later. To resume the clinical results of the present study, rTMS at both high and low frequencies improved motor performance, but on different parameters and to a lesser extent than l-dopa. Concomitant changes in cortical excitability could account for these clinical effects, as we will see below. 4.2. Effects on cortical excitability In the present study, various cortical excitability changes were induced by l-dopa intake or by motor cortex rTMS, depending on stimulation frequency. The physiological significance of these excitability parameters is now understood. RMT measures the membrane-related aspects of pyramidal cell excitability (Ziemann et al., 1996), while MEP size reflects global excitability of the corticospinal J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 2537 Table 2 Studies including clinical or electrophysiological assessment of repetitive transcranial magnetic stimulation (rTMS) of the primary motor cortex in patients with Parkinson’s disease Patients (n) Stimulus frequency (Hz) Pulses (n) 8-shaped coil, assessment during rTMS session Pascual-Leone et al. (1994a) 6 5 Ghabra et al. (1999) Gilio et al. (2002)** 5 5 40 10 2000 750 2250 750 11 15 8-shaped coil, assessment after rTMS session The present study 12 Siebner et al. (1999b) Siebner et al. (2000a) Siebner et al. (2000b) 12 10 10 5 5 5 Sommer et al. (2002)** The present study 11 12 1 0.5 900 600 Circular coil, assessment after rTMS session Tergau et al. (1999) 7 20, 10, 5, 1 1000 Mally and Stone (1999a, b) Shimamoto et al. (2001) Ikeguchi et al. (2003) Okabe et al. (2003)* 1 0.2 0.2 0.2 30 £ 2/day, (7–10 days) 30 £ 2/week (2 months) 30 £ 2/2 day (2 weeks) 50 £ 2/week (2 months) 10, 49 9 12 85 Results Shortening of reaction time and movement time No significant effect on movement time Normal increase in CSP duration, absence of rest MEP size increase Increase in CSP duration and intracortical facilitation UPDRS improvement (rigidity and bradykinesia contralaterally to rTMS) Shortening of movement time Increase in CSP duration UPDRS improvement (rigidity and bradykinesia contralaterally to rTMS) Increase in finger tapping frequency Increase in CSP duration and intracortical inhibition UPDRS improvement (rigidity ipsi-and contralaterally to rTMS) No significant effect on UPDRS or reaction time UPDRS, H&Y and ADL improvement UPDRS, H&Y and ADL improvement UPDRS and ADL improvement No significant effect on UPDRS Stimulus intensity was lower than the rest motor threshold in most of the studies, but higher than the active motor threshold in one case (*) or than the rest motor threshold in two cases (**). UPDRS, unified Parkinson’s disease rating scale; H&Y, Hoehn and Yahr score; ADL, activities of daily living score; MEP, motor evoked potential; CSP, cortical silent period. pathway (Devanne et al., 1997). ICF results from highthreshold interneuronal excitatory input to the pyramidal cells (Ilic et al., 2002). ICI is mediated by a low-threshold GABA A receptor-dependent inhibitory pathway (Ilic et al., 2002). CSP and ICI are produced through activation of different cortical GABAergic circuits (Sanger et al., 2001). RMT was found to be similar in patients with PD and in normals (Ridding et al., 1995; Valls-Sole et al., 1994). However, at a given intensity above RMT, MEP size could be larger in patients than in normals (Cantello et al., 1991; Valls-Sole et al., 1994). Then, it was suggested that excitability of the corticospinal motor output was enhanced in PD, at least at rest and during both premovement and post-movement periods (Chen et al., 2001). This excessive tonic corticospinal activity at rest is coupled with a relative failure of volitional recruitment, as shown by the reduction of MEP facilitation during voluntary contraction (Valls-Sole et al., 1994). Regarding ICF, the earliest descriptions did not report any significant differences between patients and controls (Hanajima et al., 1996; Marchese et al., 2000; Ridding et al., 1995). A slight reduction of ICF was first noted in PD by Strafella et al. (2000). The present series disclosed more clearly a defective ICF in patients with PD. However, recruitment bias in patients’ selection and the criterion to retain maximal ICF for analysis may have concurred to find defective ICF, as well as a reduced excitability of the high-threshold circuits responsible for ICF. In summary, excitability changes in PD are characterized by an overactive corticospinal output at rest, coupled with a reduction of the facilitatory inputs involved in ICF or voluntary contraction. To our knowledge, modification of RMT, ICF or MEP size by anti-parkinsonian treatment was not previously reported, except a reduction in MEP size for 5 patients after pallidotomy (Young et al., 1997). The present study disclosed that l-dopa intake did not change RMT or ICF but reduced MEP amplitude. Enhanced MEP size at rest is related to an excessive tonic activity in the whole cortico-motoneuron system (including the spinal level), and seems to be specifically associated with rigidity in PD (Cantello et al., 1991). Therefore, the decrease in MEP size following l-dopa intake could more particularly reflect the decrease in rigidity induced by this drug. 2538 J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 Changes in the excitability of inhibitory drive seem also involved in the pathophysiology of PD and in the mechanisms of action of anti-parkinsonian treatment. CSP duration was found to be shorter and/or ICI to be reduced in patients with PD compared to normals (Cantello et al., 1991; Hanajima et al., 1996; Haug et al., 1992; Marchese et al., 2000; Nakashima et al., 1995; Priori et al., 1994; Ridding et al., 1995; Strafella et al., 2000; Valls-Sole et al., 1994). These results suggested an imbalance of the corticospinal excitability in PD towards a state of disinhibition or a decrease in the excitability of inhibitory circuits. Moreover, CSP duration is normalized and/or ICI is restored by acute or chronic treatment with l-dopa or apomorphine (Manfredi et al., 1998; Marchese et al., 2000; Nakashima et al., 1995; Pierantozzi et al., 2001; Priori et al., 1994; Ridding et al., 1995; Strafella et al., 2000), as well as by pallidotomy (Young et al., 1997) or subthalamic nucleus stimulation (Cunic et al., 2002; Dauper et al., 2002; Pierantozzi et al., 2002). The present results confirmed that l-dopa intake was able to prolong CSP duration and to restore ICI in patients with PD. Regarding rTMS influence, published data were lacking in PD, in contrast to normals. In normals, low-frequency subthreshold rTMS was found to reduce global excitability (MEP size) and/or facilitatory input (ICF) (Gangitano et al., 2002; Maeda et al., 2000; Romero et al., 2002; Touge et al., 2001), but not to increase inhibition (Fitzgerald et al., 2002; Romero et al., 2002). This was evoking a phenomenon of disfacilitation. In the present series of patients with PD, the opposite was observed, since an increase in inhibitory drive (CSP duration and ICI) was observed rather than a decrease in corticospinal output. The present patients were older (mean age 64 years) than most of the healthy volunteers in whom rTMS effects have been previously studied, but age differences should probably not explain opposite results. Moreover, younger patients with focal dystonia (mean age 41 years) presented a pattern of response to low-frequency motor cortex rTMS similar to that observed in the patients of the present study (Siebner et al., 1999a). Effects of high-frequency rTMS on cortical excitability are more complex. In healthy subjects, subthreshold high-frequency stimulation is sufficient to increase MEP size (Gangitano et al., 2002; Maeda et al., 2000) and to reduce ICI (Peinemann et al., 2000), corresponding to a state of disinhibition, while suprathreshold intensity is required to increase ICF (Wu et al., 2000) and prolong CSP duration (Romeo et al., 2000), corresponding to a facilitation of both excitatory and inhibitory drive or to an action on the excitatory mechanisms alone. In the present series, ICF increase and CSP lengthening were observed following subthreshold 10 Hz TMS, without any change in MEP size or ICI. This strongly evoked a reversed balance of cortical excitability in patients with PD compared to normals. A prolonged CSP duration following subthreshold highfrequency rTMS applied over the motor cortex was already reported in 10 patients with PD (Siebner et al., 2000a). The effects on ICF, which were not observed after l-dopa intake, suggested a non-dopaminergic effect induced by high-frequency rTMS for this variable. To resume the cortical excitability changes observed in the present study, motor cortex rTMS could restore inhibitory mechanisms at low frequency and both excitatory and inhibitory mechanisms at high frequency. 4.3. Pathophysiological significance regarding primary motor cortex involvement in PD Thus, the present study showed that the stimulation of the primary motor cortex improved motor performance in patients with PD, concomitantly with well-characterized cortical excitability changes. In particular, a bilateral clinical improvement was observed after low-frequency rTMS. A bilateral modulation of motor cortex activity induced by unilaterally applied low-frequency rTMS was already described in functional brain imaging studies of healthy subjects (Fox et al., 1997; Lee et al., 2003) or on the basis of cortical excitability changes (Plewnia et al., 2003; Wassermann et al., 1998). Specifically, subthreshold rTMS applied unilaterally at a frequency of 0.5 Hz with a figureof-eight coil was shown to modify cortical excitability of the unstimulated primary motor cortex (Gorsler et al., 2003) or to modulate oscillatory activity of the primary sensory cortex (Ogawa et al., 2004). High-frequency motor cortex rTMS was also associated in healthy subjects with bilateral cortical activation persisting beyond the time stimulation (Siebner et al., 2000c), but such effects in patients with PD were not supported by the present results. The changes induced by rTMS in the complex patterns of interregional coupling within the motor system may well differ between high- and low-frequency rTMS, as it was shown for the transcallosal cross-talk between the right and left primary motor cortices (Gorsler et al., 2003). In addition, apart from the cortical changes, an influence of cortical stimulation on subcortical structures cannot be ruled out. For instance, primary motor cortex rTMS was shown to increase dopamine release in the nigrostriatal system (Strafella et al., 2003). However, rTMS effects did not overlap the effects of l-dopa (cf. effects of high-frequency rTMS on ICF), and the mechanisms of action of rTMS were supposed to take place, at least partly, at the cortical level in the present study. Thus, these results support the interest of modulating motor cortex activity to act on motor performance in patients with PD. A dysfunction in the primary motor cortex, related to the impaired nigriostriato-thalamic network, could contribute to motor disturbances in patients with PD, as suggested by various neurophysiological or imaging data. For instance, an abnormal synchronization between cortical and subcortical (basal ganglia) oscillatory activities has been demonstrated at the origin of akinesia (Cassidy et al., 2002). In particular, bradykinesia was associated with a J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 movement-related decrease in desynchronization of the mu rhythm over the primary motor cortex (Devos et al., 2004). A bilateral overactivation of the primary motor cortex was observed in imaging studies of patients with PD (using functional magnetic resonance imaging, single-photon or positron emission tomography) (Haslinger et al., 2001; Sabatini et al., 2000; Samuel et al., 1997; Thobois et al., 2000). This hyperactivity, either primary or secondary to the development of compensatory mechanisms (Buhmann et al., 2003), was shown reduced after dopaminergic treatment (Feigin et al., 2001; Haslinger et al., 2001) or deep brain stimulation (Ceballos-Baumann et al., 1999; Limousin et al., 1997; Thobois et al., 2002). However, imaging studies did not allow the distinction between excitatory and inhibitory synaptic changes. Results obtained by TMS techniques in patients with PD suggested an imbalance of the corticospinal excitability towards a state of reduced inhibition at rest, especially in rigid patients, and towards a defective activation when a voluntary output was to be produced, especially in akinetic patients (Cantello et al., 2002). In the present study, low-frequency rTMS increased inhibitory mechanisms and decreased rigidity whereas high-frequency rTMS increased both inhibitory and excitatory mechanisms and improved both rigidity and bradykinesia. Thus, the restoration of inhibitory inputs may relieve rigidity by reducing the excessive corticospinal motor output at rest, whereas the restoration of excitatory inputs may relieve bradykinesia by improving a defective cortical activation during voluntary movement. However, such correlations between excitability changes and the relief of specific parkinsonian symptoms are purely speculative, and future studies, based on larger series of patients, might test these hypotheses properly. 4.4. Clinical perspectives for motor cortex stimulation in PD The present study provided original data that could open perspectives to act on motor performance in patients with PD by stimulating the primary motor cortex. As assessed on UPDRS motor score, the clinical improvement obtained by unilateral motor cortex stimulation in the present study was significant (17 – 19.5% reduction) and not far from the results, which were reported for unilateral subthalamic nucleus stimulation (23% reduction) (Kumar et al., 1999). This improvement was clearly transient, inconsistent with a therapeutic goal, but resulted just from one session of stimulation. By repeating rTMS sessions, the clinical effects could be enhanced or prolonged, as it was shown for the treatment of depression (George et al., 2000). Nevertheless, the best way to stimulate a targeted cortical area remains to implant electrodes. Recently, promising clinical effects were obtained by chronic, unilateral stimulation of the motor cortex using implanted extradural electrodes in patients with PD (Canavero et al., 2002) and 2539 in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)lesioned monkeys, the primate model of PD (Drouot et al., 2002). Even if rTMS effects are not necessarily predictive of a good outcome of an implanted cortical procedure, the present results gave some clues to guide the development of original therapeutic strategies using cortical stimulation to control motor disability in PD. References Alexander GE, Crutcher MD, DeLong MR. Basal ganglia–thalamocortical circuits: parallel substrates for motor, oculomotor, prefrontal and limbic functions. Prog Brain Res 1990;85:119– 46. Boylan LS, Pullman SL, Lisanby SH, Spicknall KE, Sackeim HA. Repetitive transcranial magnetic stimulation to SMA worsens complex movements in Parkinson’s disease. Clin Neurophysiol 2001;112: 259– 64. Buhmann C, Glauche V, Stürenburg HJ, Oechsner M, Weiller C, Büchel C. Pharmacologically modulated fMRI-cortical responsiveness to levodopa in drug-naive hemiparkinsonian patients. Brain 2003;126:451– 61. Canavero S, Paolotti R, Bonicalzi V, Castellano G, Greco-Crasto S, Rizzo L, Davini O, Zenga F, Ragazzi P. Extradural motor cortex stimulation for advanced Parkinson disease. Report of two cases. J Neurosurg 2002; 97:1208–11. Cantello R, Gianelli M, Bettucci D, Civardi C, De Angelis MS, Mutani R. Parkinson’s disease rigidity: magnetic motor evoked potentials in a small hand muscle. Neurology 1991;41:1449 –56. Cantello R, Tarletti R, Civardi C. Transcranial magnetic stimulation and Parkinson’s disease. Brain Res Rev 2002;38:309–27. Cassidy M, Mazzone P, Oliviero A, Insola A, Tonali P, Di Lazzaro V, Brown P. Movement-related changes in synchronization in the human basal ganglia. Brain 2002;125:1235–46. Ceballos-Baumann AO, Boecker H, Bartenstein P, von Falkenhayn I, Riescher H, Conrad B, Moringlane JR, Alesch F. A positron emission tomographic study of subthalamic nucleus stimulation in Parkinson’s disease: enhanced movement-related activity of motor-association cortex and decreased motor cortex resting activity. Arch Neurol 1999;56:997–1003. Chen R, Tam A, Butefisch C, Corwell B, Ziemann U, Rothwell JC, Cohen LG. Intracortical inhibition and facilitation in different representations of the human motor cortex. J Neurophysiol 1998;80:2870– 81. Chen R, Kumar S, Garg RR, Lang AE. Impairment of motor cortex activation and deactivation in Parkinson’s disease. Clin Neurophysiol 2001;112:600–7. Cunic D, Roshan L, Khan FI, Lozano AM, Lang AE, Chen R. Effects of subthalamic nucleus stimulation on motor cortex excitability in Parkinson’s disease. Neurology 2002;58:1665–72. Cunnington R, Iansek R, Thickbroom GW, Laing BA, Mastaglia FL, Bradshaw JL, Phillips JG. Effects of magnetic stimulation over supplementary motor area on movement in Parkinson’s disease. Brain 1996;119:815–22. Dauper J, Peschel T, Schrader C, Kohlmetz C, Joppich G, Nager W, Dengler R, Rollnik JD. Effects of subthalamic nucleus (STN) stimulation on motor cortex excitability. Neurology 2002;59:700–6. Defer GL, Widner H, Marie RM, Remy P, Levivier M. Core assessment program for surgical interventional therapies in Parkinson’s disease (CAPSIT-PD). Mov Disord 1999;14:572–84. Devanne H, Lavoie B, Capaday C. Input–output properties and gain changes in human corticospinal pathway. Exp Brain Res 1997;114: 329– 38. Devos D, Labyt E, Derambure P, Bourriez JL, Cassim F, Reyns N, Blond S, Guieu JD, Destée A, Defebvre L. Subthalamic nucleus stimulation 2540 J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 modulates motor cortex oscillatory activity in Parkinson’s disease. Brain 2004;127:408 –19. Drouot X, Oshino S, Lefaucheur JP, Besret L, Conde F, Keravel Y, Peschanski M, Hantraye P, Palfi S. Electrical neuromodulation of motor cortex facilitates locomotor activity in a primate model of Parkinson’s disease. Proceedings of the Annual Meeting of the Society for Neuroscience, November 2002, Orlando; 2002. Feigin A, Fukuda M, Dhawan V, Przedborski S, Jackson-Lewis V, Mentis MJ, Moeller JR, Eidelberg D. Metabolic correlates of levodopa response in Parkinson’s disease. Neurology 2001;57:2083 –8. Fitzgerald PB, Brown TL, Daskalakis ZJ, Chen R, Kulkarni J. Intensitydependent effects of 1 Hz rTMS on human corticospinal excitability. Clin Neurophysiol 2002;113:1136– 41. Fox P, Ingham R, George MS, Mayberg H, Ingham J, Roby J, Martin C, Jerabek P. Imaging human intra-cerebral connectivity by PET during TMS. NeuroReport 1997;8:2787–91. Gangitano M, Valero-Cabré A, Tormos JM, Mottaghy FM, Romero JR, Pascual-Leone A. Modulation of input–output curves by low and high frequency repetitive transcranial magnetic stimulation of the motor cortex. Clin Neurophysiol 2002;113:1249–57. George MS, Nahas Z, Molloy M, Speer AM, Oliver NC, Li XB, Arana GW, Risch SC, Ballenger JC. A controlled trial of daily left prefrontal cortex TMS for treating depression. Biol Psychiatry 2000;48:962–70. Ghabra MB, Hallett M, Wassermann EM. Simultaneous repetitive transcranial magnetic stimulation does not speed fine movement in PD. Neurology 1999;52:768– 70. Gibbs WR, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 1988;51: 745– 52. Gilio F, Curra A, Inghilleri M, Lorenzano C, Manfredi M, Berardelli A. Repetitive magnetic stimulation of cortical motor areas in Parkinson’s disease: implications for the pathophysiology of cortical function. Mov Disord 2002;17:467 –73. Gorsler A, Baumer T, Weiller C, Munchau A, Liepert J. Interhemispheric effects of high and low frequency rTMS in healthy humans. Clin Neurophysiol 2003;114:1800–7. Hanajima R, Ugawa Y, Terao Y, Ogata K, Kanazawa I. Ipsilateral corticocortical inhibition of the motor cortex in various neurological disorders. J Neurol Sci 1996;140:109–16. Haslinger B, Erhard P, Kämpfe N, Boecker H, Rummeny E, Schwaiger M, Conrad B, Ceballos-Baumann AO. Event-related functional magnetic resonance imaging in Parkinson’s disease before and after levodopa. Brain 2001;124:558 –70. Haug BA, Schonle PW, Knobloch C, Kohne M. Silent period measurement revives as a valuable diagnostic tool with transcranial magnetic stimulation. Electroencephalogr Clin Neurophysiol 1992;85:158 –60. Ikeguchi M, Touge T, Nishiyama Y, Takeuchi H, Kuriyama S, Ohkawa M. Effects of successive repetitive transcranial magnetic stimulation on motor performances and brain perfusion in idiopathic Parkinson’s disease. J Neurol Sci 2003;209:41–6. Ilic TV, Meintzschel F, Cleff U, Ruge D, Kessler KR, Ziemann U. Shortinterval paired-pulse inhibition and facilitation of human motor cortex: the dimension of stimulus intensity. J Physiol (Lond) 2002;545: 153– 67. Kaneko K, Kawaii S, Fuchigami Y, Morita H, Ofuji A. The effect of current direction induced by transcranial magnetic stimulation on the corticospinal excitability in human brain. Electroencephalogr Clin Neurophysiol 1996;101:478 –82. Kujirai T, Caramia MD, Rothwell JC, Day BL, Thompson PD, Ferbert A, Wroe S, Asselman P, Marsden CD. Corticocortical inhibition in human motor cortex. J Physiol (Lond) 1993;471:501–19. Kumar R, Lozano AM, Sime E, Halket E, Lang AE. Comparative effects of unilateral and bilateral subthalamic nucleus deep brain stimulation. Neurology 1999;53:561–6. Lee L, Siebner HR, Rowe JB, Rizzo V, Rothwell JC, Frackowiak RSJ, Friston KJ. Acute remapping within the motor system induced by low- frequency repetitive transcranial magnetic stimulation. J Neurosci 2003;23:5308–18. Lefaucheur JP, Drouot X, Nguyen JP. Interventional neurophysiology for pain control: duration of pain relief following repetitive transcranial magnetic stimulation of the motor cortex. Neurophysiol Clin 2001;31: 247 –52. Limousin P, Pollak P, Benazzouz A, Hoffmann D, Le Bas JF, Broussolle E, Perret JE, Benabid AL. Effect of parkinsonian signs and symptoms of bilateral subthalamic nucleus stimulation. Lancet 1995;345:91– 5. Limousin P, Greene J, Pollak P, Rothwell J, Benabid AL, Frackowiak R. Changes in cerebral activity pattern due to subthalamic nucleus or internal pallidum stimulation in Parkinson’s disease. Ann Neurol 1997; 42:283–91. Limousin P, Krack P, Pollak P, Benazzouz A, Ardouin C, Hoffmann D, Benabid AL. Electrical stimulation of the subthalamic nucleus in advanced Parkinson’s disease. N Engl J Med 1998;339:1105–11. Loo CK, Taylor JL, Gandevia SC, McDarmont BN, Mitchell PB, Sachdev PS. Transcranial magnetic stimulation (TMS) in controlled treatment studies: are some ‘sham’ forms active? Biol Psychiatry 2000;47: 325 –31. Lozano AM, Lang AE, Galvez-Jimenez N, Miyasaki J, Duff J, Hutchinson WD, Dostrovsky JO. Effect of GPi pallidotomy on motor function in Parkinson’s disease. Lancet 1995;346:1383–7. Maeda F, Keenan JP, Tormos JM, Topka H, Pascual-Leone A. Modulation of corticospinal excitability by repetitive transcranial magnetic stimulation. Clin Neurophysiol 2000;111:800 –5. Mally J, Stone TW. Therapeutic and ‘dose-dependent’ effect of repetitive microelectroshock induced by transcranial magnetic stimulation in Parkinson’s disease. J Neurosci Res 1999a;57:935–40. Mally J, Stone TW. Improvement in Parkinsonian symptoms after repetitive transcranial magnetic stimulation. J Neurol Sci 1999b;162: 179 –84. Manfredi L, Garavaglia P, Beretta S, Pellegrini G. Increased cortical inhibition induced by apomorphine in patients with Parkinson’s disease. Neurophysiol Clin 1998;28:31– 8. Marchese R, Trompetto C, Buccolieri A, Abbruzzese G. Abnormalities of motor cortical excitability are not correlated with clinical features in atypical parkinsonism. Mov Disord 2000;15:1210 –4. Nakashima K, Wang Y, Shimoda M, Sakuma K, Takahashi K. Shortened silent period produced by magnetic cortical stimulation in patients with Parkinson’s disease. J Neurol Sci 1995;130:209–14. Ogawa A, Ukai S, Shinosaki K, Yamamoto M, Kawaguchi S, Ishii R, Takeda M. Slow repetitive transcranial magnetic stimulation increases somatosensory high-frequency oscillations in humans. Neurosci Lett 2004;358:193–6. Okabe S, Ugawa Y, Kanazawa I. 0.2-Hz repetitive transcranial magnetic stimulation has no add-on effects as compared to a realistic sham stimulation in Parkinson’s disease. Mov Disord 2003;18:382–8. Pascual-Leone A, Valls-Sole J, Brasil-Neto JP, Cammarota A, Grafman J, Hallett M. Akinesia in Parkinson’s disease. II. Effects of subthreshold repetitive transcranial motor cortex stimulation. Neurology 1994;44: 892 –8. Peinemann A, Lehner C, Mentschel C, Munchau A, Conrad B, Siebner HR. Subthreshold 5-Hz repetitive transcranial magnetic stimulation of the human primary motor cortex reduces intracortical paired-pulse inhibition. Neurosci Lett 2000;296:21 –4. Pierantozzi M, Palmieri MG, Marciani MG, Bernardi G, Giacomini P, Stanzione P. Effect of apomorphine on cortical inhibition in Parkinson’s disease patients: a transcranial magnetic stimulation study. Exp Brain Res 2001;141:52 –62. Pierantozzi M, Palmieri MG, Mazzone P, Marciani MG, Rossini PM, Stefani A, Giacomini P, Peppe A, Stanzione P. Deep brain stimulation of both subthalamic nucleus and internal globus pallidus restores intracortical inhibition in Parkinson’s disease paralleling apomorphine effects: a paired magnetic stimulation study. Clin Neurophysiol 2002; 113:108– 13. J.-P. Lefaucheur et al. / Clinical Neurophysiology 115 (2004) 2530–2541 Plewnia C, Lotze M, Gerloff C. Disinhibition of the contralateral motor cortex by low-frequency rTMS. NeuroReport 2003;14:609–12. Priori A, Berardelli A, Inghilleri M, Accornero N, Manfredi M. Motor cortical inhibition and the dopaminergic system. Pharmacological changes in the silent period after transcranial brain stimulation in normal subjects, patients with Parkinson’s disease and drug-induced parkinsonism. Brain 1994;117:317–23. Ridding MC, Inzelberg R, Rothwell JC. Changes in excitability of motor cortical circuitry in patients with Parkinson’s disease. Ann Neurol 1995; 37:181–8. Romeo S, Gilio F, Pedace F, Ozkaynak S, Inghilleri M, Manfredi M, Berardelli A. Changes in the cortical silent period after repetitive magnetic stimulation of cortical motor areas. Exp Brain Res 2000;135: 504–10. Romero JR, Anschel D, Sparing R, Gangitano M, Pascual-Leone A. Subthreshold low frequency repetitive transcranial magnetic stimulation selectively decreases facilitation in the motor cortex. Clin Neurophysiol 2002;113:101 –7. Rossini PM, Barker AT, Berardelli A, Caramia MD, Caruso G, Cracco RQ, Dimitrijevic MR, Hallett M, Katayama Y, Lücking CH, Maertens de Noordhout AL, Marsden CD, Murray NMF, Rothwell JC, Swash M, Tomberg C. Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 1994;91:79–92. Sabatini U, Boulanouar K, Fabre N, Martin F, Carel C, Colonnese C, Bozzao L, Berry I, Montastruc JL, Chollet F, Rascol O. Cortical motor reorganization in akinetic patients with Parkinson’s disease: a functional MRI study. Brain 2000;123:394–403. Samuel M, Ceballos-Baumann AO, Blin J, Uema T, Boecker H, Passingham RE, Brooks DJ. Evidence for lateral premotor and parietal overactivity in Parkinson’s disease during sequential and bimanual movements: a PET study. Brain 1997;120:963–76. Sanger TD, Garg RR, Chen R. Interactions between two different inhibitory systems in the human motor cortex. J Physiol (Lond) 2001;530:307 –17. Shimamoto H, Takasaki K, Shigemori M, Imaizumi T, Ayabe M, Shoji H. Therapeutic effect and mechanism of repetitive transcranial magnetic stimulation in Parkinson’s disease. J Neurol 2001;248:48–52. Siebner HR, Tormos JM, Ceballos-Baumann AO, Auer C, Catala MD, Conrad B, Pascual-Leone A. Low-frequency repetitive transcranial magnetic stimulation of the motor cortex in writer’s cramp. Neurology 1999a;52:529– 37. Siebner HR, Mentschel C, Auer C, Conrad B. Repetitive transcranial magnetic stimulation has a beneficial effect on bradykinesia in Parkinson’s disease. NeuroReport 1999b;10:589 –94. Siebner HR, Mentschel C, Auer C, Lehner C, Conrad B. Repetitive transcranial magnetic stimulation causes a short-term increase in the duration of the cortical silent period in patients with Parkinson’s disease. Neurosci Lett 2000a;284:147– 50. 2541 Siebner HR, Rossmeier C, Mentschel C, Peinemann A, Conrad B. Short-term motor improvement after sub-threshold 5-Hz repetitive transcranial magnetic stimulation of the primary motor hand area in Parkinson’s disease. J Neurol Sci 2000b;178:91–4. Siebner HR, Peller M, Willoch F, Minoshima S, Boecker H, Auer C, Drzezga A, Conrad B, Bartenstein P. Lasting cortical activation after repetitive TMS of the motor cortex: a glucose metabolic study. Neurology 2000c;54:956–63. Sommer M, Kamm T, Tergau F, Ulm G, Paulus W. Repetitive paired-pulse transcranial magnetic stimulation affects corticospinal excitability and finger tapping in Parkinson’s disease. Clin Neurophysiol 2002;113: 944– 50. Strafella AP, Valzania F, Nassetti SA, Tropeani A, Bisulli A, Santangelo M, Tassinari CA. Effects of chronic levodopa and pergolide treatment on cortical excitability in patients with Parkinson’s disease: a transcranial magnetic stimulation study. Clin Neurophysiol 2000;111: 1198–202. Strafella AP, Paus T, Fraraccio M, Dagher A. Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain 2003;126:2609–15. Tergau F, Wassermann EM, Paulus W, Ziemann U. Lack of clinical improvement in patients with Parkinson’s disease after low and high frequency repetitive transcranial magnetic stimulation. Electroencephalogr Clin Neurophysiol Suppl 1999;51:281–8. Thobois S, Dominey PF, Decety J, Pollak P, Gregoire MC, Le Bars D, Broussolle E. Motor imagery in normal subjects and in asymmetrical Parkinson’s disease: a PET study. Neurology 2000;55:996–1002. Thobois S, Dominey P, Fraix V, Mertens P, Guenot M, Zimmer L, Pollak P, Benabid AL, Broussolle E. Effects of subthalamic nucleus stimulation on actual and imagined movement in Parkinson’s disease: a PET study. J Neurol 2002;249:1689–98. Touge T, Gerschlager W, Brown P, Rothwell JC. Are the after-effects of low-frequency rTMS on motor cortex excitability due to changes in the efficacy of cortical synapses? Clin Neurophysiol 2001;112:2138–45. Valls-Sole J, Pascual-Leone A, Brasil-Neto JP, Cammarota A, McShane L, Hallett M. Abnormal facilitation of the response to transcranial magnetic stimulation in patients with Parkinson’s disease. Neurology 1994;44:735–41. Wassermann EM, Wedegaertner FR, Ziemann U, George MS, Chen R. Crossed reduction of human motor cortex excitability by 1-Hz transcranial magnetic stimulation. Neurosci Lett 1998;250:141–4. Wu T, Sommer M, Tergau F, Paulus W. Lasting influence of repetitive transcranial magnetic stimulation on intracortical excitability in human subjects. Neurosci Lett 2000;287:37 –40. Young MS, Triggs WJ, Bowers D, Greer M, Friedman WA. Stereotactic pallidotomy lengthens the transcranial magnetic cortical stimulation silent period in Parkinson’s disease. Neurology 1997;49:1278 –83. Ziemann U, Rothwell JC, Ridding MC. Interaction between intracortical inhibition and facilitation in human motor cortex. J Physiol 1996;496: 873– 81.