Visual Fields - Venu Eye Institute
advertisement

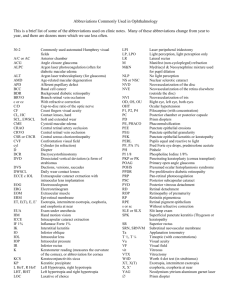
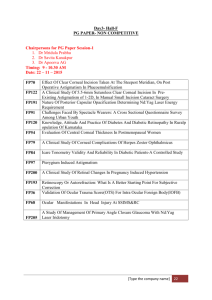
Jo ur nal of the Venu Eye Ins titut e & Resear ch Cent re Volume 6 Issue 1 October to December 2014 Visual Fields Pg. 3 Dry Eye Pg. 6 Penetrating Keratoplasty Pg. 11 Keep an Eye on Child’s Vision Pg. 14 Binocular Single Vision Pg. 16 Glaucoma Screening Pg. 18 Systemic Disease that Affect Our Eyes Pg. 20 From the editors desk “Education is the most powerful weapon which you can use to change the world.” -Nelson Mandela Dear friends Greetings from the Venu family. It gives us immense pleasure to reach to you every time through the medium of our journal 'VERGE'. Your kind patronage has made this publication one of the most sought journal for optometrists & allied cadre. In this issue we have hand picked articles reflecting various aspects of optometry and allied sciences relevant for an optometrist e.g. dry eye, screening of glaucoma and visual field. Being a totally asymptomatic disease most of the time, Glaucoma is rightly said as “sneak thief of sight”. Screening is the only way to detect this disease at an early stage so that patient does not reach a stage of irreversible blindness. Automated Visual field testing is gold standard for diagnosis and follow up of all glaucoma patients. Yet its use is not limited to glaucoma as many neurological, retinal and neuro ophthalmic cases need field testing for their proper assessment. We have tried to cover various methods of field testing and types of possible defects we get on these tests. Dry eye syndrome is a multifactorial disease affecting usually older people but with use of computer and digital gadgets, it is increasingly more common in younger professionals also. Timely diagnosis and its management is of paramount importance to give the patient a comfortable vision and avoid its serious complications. Throughout the developing world, the problem of corneal blindness is overshadowed by the backlog of cataract blindness and most of the resources have been earmarked for the alleviation of cataract blindness. Ignorance and poverty have contributed as much to the cataract blindness as to the corneal blindness. In India, we have an estimated 4.6 million people with corneal blindness that is curable through keratoplasty. We have discussed in detail various indications, contraindications and complications of penetrating keratoplasty. A case of keratoconus with its detailed clinical findings is also given with this chapter to give the readers a glimpse of this condition and various management options available. There is a myth in people's mind that nothing serious can happen in a child's eye. We need to remove this misconception from people's mind. An overview of common pediatric ocular problems and warning clues for them gives a glimpse into this matter. The eye can be affected in a number of systemic diseases. Problems in the eye may be a first presentation of the systemic disease or patients with known systemic problems may need to have their eyes specifically checked for complications. Awareness of these associations is the first step in diagnosis and management of these often complex patients. This is a very broad topic still we have tried to compile a concise article on this matter which can serve as a guide. We would like to conclude by thanking you for your encouragement. We look forward to your valuable feedback. Managing Editor : Ms. Tanuja Joshi Editorial Team : : : : : : : Dr. Wangchuk Doma Dr. Samiksha Chaudhary Dr. O.P. Gupta Dr. Bhumika Sharma Dr. Shashi Sharma Mr. Bhaskar Ghosh Ms. Sheeba Qumar Editorial Support : Mr. Satish Kumar 2 Verge Journal of the Venu Eye Institute & Research Centre Visual Fields Ms. Sukanya, Bsc IIIrd Year Venu Eye Institute & Research Centre The visual field refers to the total area in which objects can be seen in the side (peripheral) vision while we focus our eyes on a central point. In optometry and ophthalmology a visual field test is used to determine whether it is affected by diseases that cause l o c a l scotoma or a more extensive loss of vision or e v e n a reduction in sensitivity (threshold). Normal limits : The normal human visual field extends to approximately 60 degrees nasally (toward the nose, or inward) from the vertical meridian in each eye, to 100 degrees temporalily (away from the nose, or outwards) from the vertical meridian, and approximately 60 degrees above and 75 below the horizontal meridian. The macula corresponds to the central 13 degrees of the visual field; the fovea to the central 3 degrees. Aetiology ? There are many causes of visual field loss. Some more common ones are included here. ? Central field loss occurs with: ? Age-related macular degeneration. ? Optic neuropathy. ? Leber's optic atrophy. ? Macular holes. ? Cone dystrophies. ? A number of rare conditions like Best's disease, Stargardt's disease and achromatopsia. ? Peripheral field loss occurs with: ? Glaucoma (angle-closure glaucoma and open October - December 2014 angle glaucoma). ? Retinal detachment. ? Retinitis pigmentosa. ? Chorioretinitis. History The following needs to be established: ? Was the onset sudden, rapid or slow? ? Where is the field loss? It is often helpful to say to the patient, "If what you see is like a television screen then where is the bit that is missing?" ? Does it affect one eye or both? If the patient says that it affects only one eye, it is worth asking them to close or cover the affected eye and to note again if there is any visual loss. If it is much more marked in one eye than the other, the loss in the less affected eye may be overlooked. ? Does the visual defect look like a black spot, a blur or does the picture look normal? If the lesion is cortical, the patient may fail to notice any defect. If the onset has been insidious, it may also have gone unnoticed. Looking for evidence of 'asymptomatic' visual field loss ? Does the patient tend to bump into people or things? ? Has there been any damage to the car recently? Patients may continue to drive, as they are oblivious of quite significant field loss. This can cause failure to judge parking, failure to negotiate obstacles or notice other vehicles at road junctions. There may be remarkable lack of insight despite numerous claims on the insurance. ? Are there any associated neurological or ophthalmic symptoms? Types of Visual Field Tests Confrontation visual field testing typically is used as a screening visual field test. One eye is Verge Journal of the Venu Eye Institute & Research Centre 3 covered, while the other eye fixates on a target object, such as the doctor's open eye, while the doctor stands or sits directly in front of you. The patient is then are asked to describe what he sees on the far edges or periphery of your field of view. A patient undergoes visual field testing with a Humphrey Field Analyzer (HFA), which uses automated perimetry to measure responses to visual stimuli appearing in central and side vision. If an eye disease is suspected, patient may need to undergo more comprehensive, formal types of visual field testing to evaluate the quality of your central and peripheral vision. Numerous tests for measuring visual field loss exist, and can include: Automated Perimetry: Various forms of automated perimetry tests measure the responses to the presence of objects in different areas of the field of view. doubling is based on an optical illusion produced with vertical bars of contrasting colors (usually black and white) appearing on a screen. These bars appear to double in number when they alternately flicker at higher frequencies, a phenomenon thought to be due to the unique response of specific light-sensitive cells (photoreceptors) in the retina. Inability to see vertical bars at certain frequencies could indicate optic nerve or other types of eye damage with accompanying loss of vision in certain areas of the visual field. Electroretinography: This test measures electrical activity generated by the photoreceptor cells in the retina when the eye is stimulated by a special strobe light or a reversing checkerboard pattern of light. The measurement is captured by an electrode placed on the front surface of the eye (cornea), and a graphic record called an electroretinogram (ERG) is produced. Electroretinography is useful in diagnosing several hereditary and acquired disorders of the retina, including retinitis pigmentosa, a detached retina or functional changes in the retina caused by arteriosclerosis (hardening of the arteries) or diabetes inability to see objects in an appropriate portion of visual field indicates the vision loss in that area. Examination Visual acuity assessment indicates the eye's greatest power of resolution whereas visual field testing measures the peripheral sensitivity. Since the image is projected on to the retina upside down and inverted, a lesion of the top right of the retina or in the pathway beyond will cause a defect in the bottom left of the visual field. Assessing for visual field defects can be via: ? Screening tests (easily carried out in a surgery) which include confrontational visual field testing and use of an Amsler grid. ? Quantitative measurements using manual or automated Frequency Doubling Perimetry: Frequency Terms which may be encountered include: While patient's head is held still, usually with a chin rest inside a large bowl-like instrument, staring at a source of light straight ahead. Random lights of different intensities are flashed in your peripheral field of vision. Patient has to press a button or use other means to indicate the response when he perceives the computer-generated light suddenly appearing in your field of view. 4 Verge Journal of the Venu Eye Institute & Research Centre ? Visual field defect - a portion of the visual field is missing. This may be central (eg, an optic disc or nerve problem) or peripheral (along the visual pathways from the optic chiasm back). ? Scotoma - this is a type of visual field defect. It is a defect surrounded by normal visual field. ? Relative scotoma - an area where objects of low luminance cannot be seen but larger or brighter ones can. ? Absolute scotoma - nothing can be seen at all within that area. ? Hemianopia - a binocular visual defect in each eye's hemifield. ? Bitemporal hemianopia - the two halves lost are on the outside of each eye's peripheral vision, effectively creating a central visual tunnel. ? Homonymous hemianopia - the two halves lost are on the corresponding area of the visual field in both eyes, ie either the left or the right half of the visual field. ? Altitudinal hemianopia - refers to the dividing line between loss and sight being horizontal rather than vertical, with visual loss either above or below the line. ? Quadrantanopia - is an incomplete hemianopia referring to a quarter of the schematic 'pie' of visual field loss. ? Sectoral defect - is also an incomplete hemianopia. Venu as seen with full visual fields October - December 2014 Venu as seen with bitemporal hemianopsia Venu as seen with binasal hemianopsia Venu as seen with left homonymous hemianopsia Venu as seen with right homonymous hemianopsia What Abnormal Results Mean Abnormal results may be due to diseases or central nervous system disorders, such as tumors that damage or press on (compress) the parts of the brain that deal with vision. Other diseases that may affect the visual field of the eye include: ? Diabetes ? Glaucoma ? High blood pressure ? Macular degeneration ? Multiple sclerosis ? Overactive thyroid (hyperthyroidism) ? Pituitary gland disorders ? Retinal detachment ? Stroke ? Temporal arteritis Verge Journal of the Venu Eye Institute & Research Centre 5 DRY EYE Mr. Bhaskar Ghosh, Sr. Optometrist Venu Eye Institute & Research Centre INTRODUCTION Dry eye disease is a very common multifactorial disease of the lacrimal functional unit that results in tear film instability, hyperosmolarity, chronic irritation and inflammation of the ocular surface. Diagnostic tools have been developing rapidly; however, both classic dry eye tests (Schirmer I test, floroscein in staining of the surface epithelium and tear film break-up time) and noninvasive imaging techniques are essential for an exact diagnosis. The management of dry eye syndrome can be either conservative or invasive based on the severity of the disease. The basic aim of treatment is to improve quality of life and reduce subjective complaints and objective ocular surface alterations in dry eye patients. The first line of treatment is tear substitution with artificial tear drops, gels and ointments. In moderate cases preservative-free tear supplementation, topical anti-inflammatory therapy and retinol treatment is recommended. Temporary or permanent punctal plug occlusion, therapeutic contact lenses or moisture chamber constitute other options. In severe cases the application of topical autologous serum, systemic a n t i - i n f l a m m a t o r y t h e r a p y, a n d r o g e n substitution, secretagogues and surgical intervention can be effective. In the future, noninvasive diagnostic tools and instruments such as screening methods are likely to be developed. In addition, causal therapy of the dry eye will play a greater role, including cyclosporine therapy, secretion stimulation, growth factor-containing artificial tears, as well as secratogogues, immunomodulants and androgenic complexes for severe forms of the disease. Dry eye disease (also known as keratoconjunctivitis sicca) is characterized by precorneal tear film instability (reduced tear break-up time [TBUT]) and damage of the exposed surface epithelium (fluorescein or Bengal rose staining of the corneal and conjunctival epithelia), which cause chronic 6 Verge Journal of the Venu Eye Institute & Research Centre irritation of the ocular surface. In most cases, dry eye symptoms are associated with decreased lacrimal gland secretion. However, the disease can be related to quantitatively normal lacrimal production and glandular hypersecretion. Reduced tear volume is a common cause of ocular manifestations; nevertheless, lacrimal hyposecretion evaluated by the Schirmer test is not essential in the diagnosis of dry eye disease. ANATOMY The tear film covers the normal ocular surface. It is generally considered to comprise the following 3 intertwined layers: n A superficial thin lipid layer (0.11 µm) – This layer is produced by the meibomian glands, and its principal function is to retard tear evaporation and to assist in uniform tear spreading[2] n A middle thick aqueous layer (7 µm) – This layer is produced by the main lacrimal glands (reflex tearing), as well as by the accessory lacrimal glands of Krause and Wolf ring (basic tearing) n An innermost hydrophilic mucin layer (0.020.05 µm) – This layer is produced by both the conjunctiva goblet cells and the ocular surface epithelium and associates itself with the ocular surface via its loose attachments to the glycocalyx of the microplicae of the epithelium; it is the hydrophilic quality of the mucin that allows the aqueous layer to spread over the corneal epithelium. Classifying dry eye disorders Virtually all dry eye disorders are related to an increase in tear film osmolarity above the normal limit of 311 mOsm/L. Osmolarity increases when water is lost from the tear film without an accompanying decrease in solutes, such as sodium and potassium. Increased osmolarity may result from any condition that decreases tear production or increases tear evaporation. Everyone experiences a gradual decline in tear function with age, usually secondary to an associated decline in corneal sensation and meibomian gland function. However, in most people, physiologic reserve along with some ptosis is adequate to prevent symptoms and disease. WHY DRY EYE In most cases, dry eye problem can be diagnosed on the basis of patient's history. Patients with dry eye disorders complain of chronic sandy-gritty irritation that worsens as the day progresses. The eyelids form a watertight seal over the eyes during sleep, giving the ocular surfaces a chance to recover. However, once the patient opens his eyes in the morning, evaporation begins and tear film's osmolarity increases as the day progresses. Patients with meibomitis (posterior blepharitis) also complain of chronic sandy gritty eye irritation, but in these patients, the symptoms are worse upon awakening. Morning irritation occurs because tear production decreases during sleep, and eye closure brings the inflamed lids against the eye where inflammatory mediators act on the cornea. When these patients awaken, tear flow October - December 2014 increases, the lids pull away from the cornea and symptoms improve. Eventually, chronic meibomian gland inflammation leads to dysfunction. Complaints Depending on the severity of dry eye syndrome (DES), or keratoconjunctivitis sicca (KCS), the following are the most common patient complaints: u Foreign-body sensation and ocular dryness and grittiness u Hyperemia u Mucoid discharge u Ocular irritation u Excessive tearing (secondary to reflex secretion) u Photophobia u Fluctuating or blurry vision Investigations:Invasive Techniques: 1) TBUT 2) Schirmer test 3) Phenol red thread Non-Invasive Techniques: 1) Tearscope 2) Hand-held keratoscope 3) Keratometer Schirmer Test Without Anesthesia (Schirmer1) - Measures Reflex Tear Secretion (dry eye = < 6mm wetting) With Anesthesia (Schirmer2) - Measures Basal Tear Secretion (dry eye =< 3mm wetting) Verge Journal of the Venu Eye Institute & Research Centre 7 Tear break up time (TBUT): Invasive TBUT Stain the tears with fluorescein dye and measure the interval between a complete blink and the appearance of the first randomly distributed dry spot or hole in the pre-corneal tear film.The normal value is more than 10 seconds Dry eyes can also be the result of inflammation in the lacrimal glands. A vicious cycle follows in that the eye irritated by dry eyes, can over stimulate the nerve fibers of the lacrimal glands which causes further lacrimal gland inflammation due to its over stimulation and thus reducing the tear formation. ETIOLOGY An evaporative state An aqueous deficiency state Etiology: Evaporative loss Non-Invasive TBUT Instillation of fluorescein is not required Done with the instrument called “Xeroscope” It consists of a hemispherical bowl with a grid of white lines inscribed onto its inner matte black surface mounted a slit lamp. A ring fluorescent tube attached to the rim of the bowl illuminates the grid. It is viewed on the cornea through the slit lamp Normal – 30 sec AIM &OBJECTIVE Effective treatment of dry eyes requires a careful examination to determine which factor is causing the symptoms. The main aim of the treatment is to keep the eyes moist. The initial treatment is usually the use of lubricating eyedrops. These lubricate the eyes, and relieve the symptoms. Hydroxypropyl methylcellulose is the most commonly used medication followed by Carboxy Methycellulose. Those with severe dry eyes require more aggressive therapy with lacrimal punctual occlusion plugs. Dry eyes due to diseases of the meibomian glands and blepharitis generally respond well to treatment with an antibiotic eye ointment like tetracycline, ciprofloxacin, chloramphenicol. 8 Verge Journal of the Venu Eye Institute & Research Centre Causes of evaporative loss can be further classified as intrinsic or extrinsic. Intrinsic causes Meibomian gland disease (MGD) may involve a reduced number of functioning glands, as in congenital deficiency or acquired MGD, or replacement, as in distichiasis, lymphedema-distichiasis syndrome, or metaplasia. MGD may be divided into 3 sub-types as follows: Hypersecretory - Meibomian seborrhea Hyposecretory - Retinoid therapy Obstructive – This may be simple, primary or secondary to local disease (e.g., anterior blepharitis), systemic disease (e.g., acne rosacea, seborrheic dermatitis, atopy, ichthyosis, or psoriasis), syndromes (e.g., anhidrotic ectodermal dysplasia, ectrodactyly syndrome, or Turner syndrome), or systemic toxicity (e.g. 13-cis retinoic acid or polychlorinated biphenyls); or it may be cicatricial, primary or secondary to local disease (e.g., chemical burns, trachoma, pemphigoid, erythema multiforme, acne rosacea, vernal keratoconjunctivitis [VKC], or atopic keratoconjunctivitis [AKC]) Evaporative loss may result from a low blink rate caused by the following: Physiologic phenomenon, such as may occur during performance of tasks that require concentration (eg. working at a computer or a microscope) Extrapyramidal disorder, such as Parkinson disease (decreasing dopaminergic neuron pool) Evaporative loss may result from the following disorders of eyelid aperture and eyelid-globe congruity: Exposure (e.g. craniostenosis, proptosis, exophthalmos, and high myopia) Lid palsy Ectropion Lid coloboma Extrinsic causes Vitamin A deficiency may cause dry eye as a consequence of the following: Developmental disorder of goblet cells. Lacrimal acinar damage Other extrinsic causes are as follows: Contact lens wear Ocular surface disease (e.g., allergy) Severity October - December 2014 DEFICIENT AQUEOUS PRODUCTION Causes of deficient aqueous production can be further classified as related or unrelated to NonSjögren syndrome Primary lacrimal gland deficiencies that may impair aqueous production include the following: Idiopathic Age-related dry eye Congenital alacrima (eg, Riley-Day syndrome) Familial dysautonomia Secondary lacrimal gland deficiencies that may impair aqueous production include the following: Lacrimal gland infiltration Lymphoma AIDS Graft vs host disease Amyloidosis Hemochromatosis Lacrimal gland infectious diseases HIV diffuse infiltrative lymphadenopathy syndrome Trachoma Systemic vitamin A deficiency (xerophthalmia)Malnutrition, fat-free diets, intestinal malabsorption from inflammatory bowel disease, bowel resection, or chronic alcoholism Lacrimal gland ablation Lacrimal gland denervation Lacrimal obstructive diseases that may impair aqueous production include the following: Ocular cicatricial pemphigoid Erythema multiforme and Stevens-Johnson syndrome Chemical and thermal burns Endocrine imbalance Trachoma Medications that may impair aqueous production include the following: Antihistamines Verge Journal of the Venu Eye Institute & Research Centre 9 Beta blockers Atropine Oral contraceptives Chronic contact lens wear CN VII damage For classification of DES on the basis of severity, the Delphi Panel Report was adopted and modified as a third component of the DEWS (see the Table below) Other conditions that impair aqueous production include the following: Dry Eye Severity level Variable 1 Discomfort (severity and frequency) Mild, episodic; occurs under environmental stress Visual symptoms None or episodic mild fatigue Conjunctival injection Conjunctival staining Corneal staining (severity and location) Corneal and tear signs Lid and meibomian glands Tear breakup time Schirmer value 2 Moderate, episodic or chronic; occurs with or without stress Annoying or activity-limiting, episodic 3 4 (must have signs and symptoms) Severe, frequent or constant; occurs without stress Severe or disabling, constant Annoying, chronic or Constant and possibly constant, activitydisabling limiting None to mild None to mild +/– +/++ None to mild Variable Moderate to marked Marked None to mild Variable Marked central Severe punctate erosions Filamentary keratitis, Filamentary keratitis, mucus clumping, mucus clumping, None to mild increased tear debris, increased tear debris ulceration Trichiasis, MGD variably MGD variably keratinization, MGD frequent present present symblepharon Variable = 10 s =5s Immediate Variable = 10 mm/5 min = 5 mm/5 min = 2 mm/5 min MGD=meibomian gland dysfunction. Mild debris, decreased meniscus Increasing the tear secretion SUMMARY: Immune inhibition therapy Eliminating the etiological factors Re-establish the tear film Tears replacement therapy Other supporting treatment Maintain moisture in the eyes 10 Verge Journal of the Venu Eye Institute & Research Centre Penetrating Keratoplasty Ms. Vamshu Bhat, B.Sc IIIrd Year Venu Eye Institute & Research Centre Penetrating Keratoplasty refers to the replacement of the host cornea with a donor cornea.It is used with success in patients with decreased visual acuity secondary to corneal opacity, in the treatment of corneal thinning or perforation, for the removal of non responding infectious foci and for the relief of pain. ? Pre-existing conditions that limit visual potential, including amblyopia, macular or retinal disease and optic nerve damage ? Multiple graft rejections ? Stromal neovascularization ? Poorly controlled glaucoma ? Eyelid abnormality ? Dry eye Pros and cons of PK Pros: ? Established technique with good long-term data ? Potential for best corrected visual acuity ? Less surgical skill required Cons: ? Greater risk for graft rejection ? Greater post operative astigmatism ? Greater loss of endothelial cells Indications ? Pseudophakic or aphakic corneal edema ? Endothelial dystrophies: Fuchs and posterior polymorphous corneal dystrophy ? Regraft related to allograft rejection ? Regraft unrelated to allograft rejection ? Stromal dystrophies: lattice, granular, avellino, ? Keratoconus and other ectasias ? Viral/postviral keratitis/keratopathy ? Microbial including Fungal and Bacterial keratitis /post microbial keratitis/keratopathy ? Non-infectious ulcerative keratitis or perforation ? Corneal degenerations and dystrophies including Fuchs endothelial dystrophy ? Chemical injuries ? Mechanical trauma, non-surgical ? Congenital opacity ? Iridocorneal endothelial syndrome ? Refractive indications ? Other causes of corneal opacification or distortion, including surgical trauma Surgical Procedure The initial step in Penetrating Keratoplasty should be the preparation of the donor tissue. The use a corneal button 0.250.50mm larger than the diameter of the host corneal o p e n i n g i s recommended as it can help to reduce excessive postoperative corneal flattening, reduce the risk of secondary glaucoma and enhance wound closure. Contraindications ? Active uveitis ? Active keratitis, except when necessary for tectonic support or for removal of infectious material in progressive microbial keratitis ? Severe ocular surface disease The host cornea is trephined, the anterior chamber is filled with viscoelastic and the donor tissue is placed endothellial side down on the recipient's eye. The cornea is then sutured in place with either interrupted or continuous sutures. Interrupted sutures are preferred in October - December 2014 Verge Journal of the Venu Eye Institute & Research Centre 11 vascularized, inflammed or thinned corneas as well as in pediatric cases. Penetrating keratoplasty may be combined with cataract surgery, secondary intraocular lens implantation,glaucoma surgery or retinal surgery. Follow-up care A. Post-operative visit is advised to ensure epithelial healing and control of IOP and inflammation B. Visits are indicated more frequently in the first 90 days C. Essential components of the post-operative exam include: ? Interval history ? Measurement of visual acuity ? Slit-lamp biomicroscopy ? IOP assessment D. Topical corticosteroid and other ophthalmic medications E. Suture removal Intraoperative Complications ? Damage to the lens or iris ? Damage to the donor tissue ? Vitreous loss ? Retained Descemet membrane ? Poor graft centration ? Irregular trephination and wound leak ? Suturing problems ? Problems reforming the anterior chamber, Vitreous in the anterior chamber? ? Hyphaema ? Choroidal haemorrhage or effusion and supra choroidal haemorrhage ? Post-operative Complications ? Wound leak ? Flat chamber/iris incarceration ? Elevated IOP ? Endophthalmitis ? Glaucoma 12 Verge Journal of the Venu Eye Institute & Research Centre ? Severe inflammation including formation of fibrin ? Microbial or viral keratitis ? Persistent epithelial defect ? Primary endothelial failure ? Recurrence of primary disease ? Suture-related problems ? Post-operative astigmatism ? Allograft rejection ? Anterior or Posterior synechiae ? Pupillary block ? Choroidal detachment ? Corneal vascularisation ? Epithelial ingrowth ? Transmission of donor disease ? Traumatic wound rupture ? Graft failure Corneal Graft Rejection A Symptoms ? Decreased vision ? Pain ? Redness ? Photophobia after corneal transplant B Signs ? Keratic precipitates or a white line on the corneal endothelium ? Stromal edema or infiltrates ? Subepithelial or epithelial edema ? Conjunctival injection ? Anterior chamber cells or flare ? Neovascularization C Differential Diagnosis ? Increased intraocular pressure ? Uveitis ? Suture abscess ? Corneal infection ? Recurrent disease in the graft (Herpetic or corneal dystrophy) D Treatment ? A topical steroid is prescribed immediately, such as prednisolone acetate 1% q 1hr ? Cycloplegic agent ? Systemic steroids (prednisone 40-80 mg daily) should be considered in cases that do not respond to topical steroids and in recurrent rejection episodes Is penetrating keratoplasty for corneal endothelial disorders associated with donor age or not??? Although most of the cases did not show a significant difference in 10-year success rates comparing donor ages 12 to 65 years and 66 to 75 years, there was evidence of donor age effect at the extremes of the age range. Observation of a fairly constant 10-year success rate for donors aged 34 to 71 years, which account for approximately 75% of corneas available for transplant, the Cornea Donor Study results indicate that donor age is not an important factor in most penetrating keratoplasties for endothelial disease. CASE HISTORY: A 22-year-old male with a history of progressive keratoconus Chief Complaint: Diminishing vision and progressive corneal ectasia in a patient with keratoconus. History of Present Disease: A 22-year-old male with keratoconus was referred for progressive corneal ectasia and diminishing visual acuity. Initial management included spectacle correction, but progression of his disease required correction with rigid gas permeable contact lenses. Best corrected visual acuity was 20/100 OD, 20/50 OS and 20/50 OU. The patient was unable to work because of poor vision. Glasses did not provide adequate correction and he was intolerant tocontact lenses, particularly in the right eye in which the lens continued to pop out despite the best possible fit. The patient was referred Past Ocular History: Progressive keratoconus OD > OS as described above. October - December 2014 Medical History: None. Family History: Father has keratoconus. Medications: None Ocular Exam: Visual Acuity - best corrected with contact lenses: ? OD—20/100 ? OS—20/50 Anterior segment examination: ? OD—clear cornea with central thinning (central corneal thickness 419 microns, thinnest 360), Fleischer ring, Vogt's striae, Munson's sign ? OS—clear cornea with central thinning (central corneal thickness 467 microns, thinnest 396) Dilated fundus exam: ? Normal OU Figure1: Slit lamp photo OD showing i r o n deposition in the corneal b a s a l epithelial cells (Fleischer ring). Figure2: Slit lamp photo demonstrating ectasia and protrusion of the cornea. central corneal thickness was 419 microns Treatment: The most common surgical options for keratoconus include Deep Anterior Lamellar Keratoplasty (DALK) and Penetrating Keratoplasty (PK). Verge Journal of the Venu Eye Institute & Research Centre 13 Keep an Eye on Child’s Vision Ms. Garima Raghav, Optometrist Intern Venu Eye Institute & Research Centre In India, we have many prevailing myths regarding vision, the common one's being that a squint is lucky and that hours of TV or video games can cause refractive errors. But there is one more myth that is still prevailing in the Indian minds, that in the worst case scenario their child can get a pair of glasses. But times have changed a lot. And with these advancements our awareness towards the various eye diseases should also increase which urges for a more collaborative approach to combat causes of childhood vision loss. Now a days we have advanced techniques to treat most of the eye problems. But problem arises with the late diagnosis. And in cases of children a late diagnosis can leave an impact on their whole life. So let's have a look at the common eye problems that we see in children: 1. Amblyopia or Lazy Eye If there is a significant difference in the image quality between both the eyes then there is a mental preference to the better eye and suppression of the other one. This suppression gradually becomes permanent which leads to loss of vision in the weak eye if not managed timely. Reason for this could be many like refractive error, squint, cataract etc. In such cases early detection is important as they can be best treated only upto 6 years of age. Amblyopia is one of the major cause of childhood blindness and needs to be detected and managed at an early age. 2. Strabismus More commonly known as squint, it is the misalignment of the visual axis which is commonly seen during childhood. It can be of various types and can have various etiology. Squint can cause amblyopia which needs an effective management plan consisting of glasses, 14 Verge Journal of the Venu Eye Institute & Research Centre patching and surgeries to combat the possible side effects. Their management is critical for maintaining a good visual functioning of the child. 3. Refractive error All infants are born hyperopic but as they grow old their refractive status makes a shift towards myopia to attain the state of emmetropia. But its failure significantly hinders the childs visual performance. In children this condition usually goes un-diagnosed as they interpret this blurred stimulus as the best possible image they can get with their eyes. It not only alters their ability to see but is also capable of degrading their academic performance, generate asthenopic symptoms and might cause some serious effects like bilateral amblyopia. They are quiet common and demands an immediate action. 4. Vergence and Accommodative Anamolies As far as numbers are concerned, these conditions are found on massive scale. Though the potential side effects when compared to other conditions are not as severe but the asthenopic symptoms that they are capable of generating are quiet sufficient to cause a significant degradation in academic performance. Most commonly parents of such children report of lack of concentration and which in most of the cases is usually blamed upon the notorious behaviour of the child, leaving the possible cause undiagnosed. There are also some other conditions that are not as common but need an immediate attention when diagnosed, like: Retinoblastoma, an intraocular tumour usually seen in early childhood. It is vision threatening, and needs immediate enucleation (removal of eye ball) as in late stages the tumour can be life threatening also. Congenital/Developmental cataracts are the media opacities seen in the lens during childhood and can cause form deprivation amblyopia which among all types of amblyopia is most dangerous and most difficult to treat. Early surgery is the only key to good vision. In many cases it is usually present with a family history so patient education often plays an important role. There are other eye conditions like keratoconous, congenital glaucoma etc which are often seen with many syndromes and needed to be tackled accordingly. Ophthalmologist are medical doctors who provide comprehensive eye care with medicine and surgery. Peadiatric ophthalmologist are doctors who have additional special training to treat childhood eye problems. Optometrists provide services that may be similar to ophthalmologists, they examine, diagnose, monitor, refer and manage to some extent, but they don't perform surgery. Some optometrists specialize in childhood eye problems. We are talking about keeping an eye on child's vision. But unlike adults a child is not going to come to an optometrist and say "hey I'm not able to see clearly. I need glasses." In children there are certain signs that often indicate a particular condition. Some of them are: ? Constant eye rubbing - From a common allergic conjunctivitis to early keratoconus this feature is common and can be present in various conditions hence it is needed to be taken seriously. ? Extreme light sensitivity ? Poor focusing is often seen in the child having significant accommodatative or vergence anamoly. These deficits adversely affects the child's academic performance. ? Poor visual tracking (following an object) ? Abnormal alignment or movement of the eyes (after 6 months of age). Till six months eyes learn to work in co-ordination. But any ocular misalignment or abnormal eye movement after this age should be viewed with suspicion. ? Chronic redness of the eyes ? Chronic tearing of the eyes ? A white pupillary reflex (leucocoria) instead of black - can be a cataract or in rare cases it can be a retinoblastoma In school going children, other signs to watch for include: ? Being unable to see objects at a distance ? Having trouble reading the blackboard (such children usually squeeze their eyes to see the blackboard or copy from his or her bench mate's notebook) ? Squinting ? Difficulty in reading ? Sitting too close to the television (most common!) Watch your child for signs of poor vision or squinting eyes. If you notice any eye problems, have your child examined right away so that the problem doesn't become permanent. If caught early, eye conditions can often be treated efectively. Now we have a next question standing in front of us. When to take the child to the doctor? In our country, eye check-ups are usually preceded by a referral from a teacher or more rarely from a school screening camp. But the point is a regular eye examination is equally important like a regular health check up. Cont. on Page No. 19 October - December 2014 Verge Journal of the Venu Eye Institute & Research Centre 15 Binocular Single Vision Ms. Radhika, B.Sc IIIrd Year Venu Eye Institute & Research Centre Binocular Single Vision may be defined as the state of simultaneous vision, which is achieved by the coordinated use of both eyes, so that separate and slightly dissimilar images arising in each eye are appreciated as a single image by the process of fusion. Thus binocular vision implies fusion, the blending of sight from the two eyes to form a single percept. Binocular Single Vision can be: 1. Normal – Binocular Single vision can be classified as normal when it is bifoveal and there is no manifest deviation. 2. Anomalous - Binocular Single vision is anomalous when the images of the fixated object are projected on the fovea of one eye and an extrafoveal area of the other eye i.e. when the visual direction of the retinal elements has changed. A small manifest strabismus is therefore always present in anomalous Binocular Single vision. Normal Binocular Single vision requires: 1. Clear Visual Axis leading to a reasonably clear vision in both eyes 2. The ability of the retino-cortical elements to function in association with each other to promote the fusion of two slightly dissimilar images i.e. Sensory fusion. 3. The precise co-ordination of the two eyes for all direction of gazes, so that corresponding retino-cortical element are placed in a position to deal with two images i.e. Motor fusion. The advantages of a Binocular vision are: 1. The first and the foremost advantage of a binocular vision is single vision 2. In addition to single vision it results in stereopsis – the most precise kind of depth perception 3. Enlargement of the field of vision 4. Compensation for blind spot GRADES OF BINOCULAR SINGLE VISION: 16 Verge Journal of the Venu Eye Institute & Research Centre Worth classified binocular single vision to be of three grades? Simultaneous Macular Perception ? Fusion ? Stereopsis Simultaneous Macular Perception Simultaneous perception exists when signals transmitted from the two eyes to the visual cortex are perceived at the same time. It consists of the ability to see two dissimilar objects simultaneously. FUSION Fusion is the cortical unification of visual objects into a single percept that is made possible by the simultaneous stimulation of corresponding retinal areas. Slides for simultaneous macular perception Fusion Slides Sensory Fusion – It is based on the innate orderly topographic relationship between the retina and the visual cortex, whereby corresponding retinal points, project to the same cortical locus, and corresponding adjacent retinal points have adjacent cortical representation. Motor Fusion - It is the ability to align the eyes in such a manner that sensory fusion can be maintained. The stimulus for these fusional eye movements is retinal disparity outside panum's area and the eyes moving in opposite direction (vergence). Unlike sensory fusion, motor fusion is the exclusive function of the extrafoveal retinal periphery. STEREOPSIS Stereopsis allows subjective ordering of visual objects in depth; or three-dimension. It is the highest form of binocular co-operation and it adds a new quality of vision. Central and Peripheral Suppression ? Images formed on the fovea of the deviating eye are prevented from reaching consciousness in order to avoid confusion. This is called central suppression. ? The image similar to the one falling on the fovea of the fixing eye falls on the peripheral retina of the deviating eye. Suppression of this image is called peripheral suppression. Monocular and Alternate Suppression ? If the image from one eye alone is suppressed, it is called monocular suppression. This leads to amblyopia in that eye. ? If the images from the two eyes are suppressed alternately, it is called alternate suppression. This occurs in alternating squints and usually both eyes have fairly good visual acuity. ANOMALIES OF SMP Confusion When squinting occurs the two fovea view two different objects that are physically separated in objective space, and send two different images to a single cortical perceptual area. This leads to confusion. But, confusion is not common as the cortex immediately settles for one image with its inherent strong cortical or retinal rivalry. Diplopia When squinting occurs an object in space is perceived by the fovea of one eye and some other extra-foveal point of the other eye, which has a different projection or localization value in space. Thus an object would be localized twice in space causing diplopia. Diplopia usually results from an acquired misalignment of the visual axis. Suppression The image formed in one eye is prevented from reaching consciousness. This is called suppression. It occurs when there is strabismic misalignment of the visual axis. It is an adaptation to avoid diplopia and/or confusion. There are various types of suppression: October - December 2014 Facultative and Obligatory Suppression ? Suppression is called facultative when it is present only when the eyes are in the deviated state and absent in all other states. ? Obligatory Suppression is present at all times irrespective of whether the eyes are aligned or misaligned. Retinal Correspondence, Abnormal (ARC) It is type of retinal correspondence in which the fovea of one eye is associated with an extrafoveal area of the other eye to give rise to a perception of a single object. This phenomenon is common in strabismus, but may also occur as a result of a macular lesion. Amblyopia Amblyopia, also called lazy eye, is a disorder of sight. It involves decreased vision in an eye that otherwise appears normal, or out of proportion to associated structural problems of the eye. Verge Journal of the Venu Eye Institute & Research Centre 17 Glaucoma Screening Ms. Arti Gupta, B.Sc IIIrd Year Venu Eye Institute & Research Centre Glaucoma is a condition that causes damage to the optic nerve and gets worse over time. It's often associated with a buildup of pressure inside the eye. Glaucoma tends to be inherited and may not show up until later in life. Normally, this fluid, called aqueous humor, flows out of the eye through a mesh-like channel. If this channel becomes blocked, fluid builds up, causing glaucoma. The direct cause of this blockage is unknown, but it can be inherited. Less common causes of glaucoma include a blunt or chemical injury to the eye, severe eye infection, blockage of blood vessels in the eye, inflammatory conditions of the eye, and occasionally eye surgery to correct another condition. Glaucoma usually occurs in both eyes, but it may involve each eye to a different extent. The increased pressure, called intraocular pressure, can damage the optic nerve, which transmits images to the brain. If damage to the optic nerve from high eye pressure continues, glaucoma will cause permanent loss of vision. Without treatment, glaucoma can cause total permanent blindness within a few years. Because most people with glaucoma have no early symptoms or pain from this increased pressure, it is important to get the eyes checked regularly so that glaucoma can be diagnosed and treated before long-term visual loss occurs. RISK FACTORS:? Age more than 40. ? Family history of glaucoma ? High eye pressure(IOP) ? Farsightedness ? High blood pressure ? Diabetes ? Patients taking corticosteroid medicines ? Eye injury Diagnosis of Glaucoma If patient is over age 40 and have a family history of glaucoma, a complete eye checkup is necessary at least once in a year. Patients with some health problems such as diabetes or a family history of glaucoma or are at risk for other eye diseases. Why Does Pressure Rise in the Eye to Cause Glaucoma? Glaucoma usually occurs when pressure in your eye increases. This can happen when eye fluid isn't circulating normally in the front part of the eye. 18 Verge Journal of the Venu Eye Institute & Research Centre Individuals at high risk for glaucoma should have a dilated pupil eye examination at least every one to two years. Eye doctors use several tests to detect glaucoma; these tests include: ? Tonometry measures the pressure inside the eye ? Field testing measures the entire area seen by the forwardlooking eye to document straighta h e a d (central) and/or side (peripheral) vision. ? A visual acuity test measures sight at various distances. While seated 20 feet from an eye chart, the patient is asked to read standardized visual charts with each eye, with and without corrective lenses. ? Pachymetry uses an ultrasonic wave instrument to help determine the thickness of the cornea and better evaluate eye pressure. ? Ophthalmoscopy allows the doctor to examine the interior of the eye by looking through the pupil with a special instrument. This can help detect damage to the optic n e r v e caused by glaucoma. ? Gonioscopy allows the doctor to view the front part of the eye (anterior chamber) to determine if the iris is closer than normal to the back of the cornea. This test can help diagnose closeda n g l e glaucoma. ? O p t i c n e r v e October - December 2014 imaging helps document optic nerve changes over time. Nerve imaging techniques include stereo optic nerve photographs, scanning laser polarimetry (GDx), confocal scanning laser ophthalmoscopy (Heidelberg Retinal Tomograph or HRT) and optical coherence tomography (OCT). It is very important to have regular eye examination particularly if patient has any of the risk factors associated with glaucoma. However, if diagnose early glaucoma is treatable. If detected early, disease prognosis can be delayed by monitoring and controlling the eye pressure. C o n t d . f r o m P a g e No.15 Here is a rough guideline for when to get it done: ? Newborns should be checked for general eye health by a pediatrician or family physician in the hospital nursery ? High-risk newborns (including premature infants), those with a family history of eye problems, and those with obvious eye irregularities should be examined by an eye doctor ? In the first year of life, all infants should be routinely screened for eye health during checkups with their pediatrician or family doctor ? Around the age of 3½ years, children should have eye health screenings and visual acuity tests (tests that measure sharpness of vision) with their pediatrician or family doctor. ? Around the age of 5 years, children should have their vision and eye alignment checked by their pediatrician or family doctor. Those who fail either test should be examined by an eye doctor. ? After the age of 5 years, routine screenings should be done at school and the doctor's clinic Verge Journal of the Venu Eye Institute & Research Centre 19 Systemic Disease that affect our Eyes Ms. Neha, B.Sc IIIrd Year Venu Eye Institute & Research Centre Systemic diseases are the diseases that occur in any part of our body. They can happen to any person at any age. Ocular involvement in systemic disorders is quite frequent. It is important for the ophthalmologist as well as general physician to pay necessary attention towards it. Many-a time, the ocular manifestation may be the presenting signs and the ophthalmologist should refer the patient to the related specialist for further treatment & diagnosis. Sometimes, patient suffering from high blood pressure and diabetes does not know that they are suffering from it unless the disease affects their eyes. So, systemic diseases are very important to be considered in case of eyes. HOW EYES ARE RELATED WITH SYSTEMIC DISEASES? The eyes are linked with the other part of body by many means, such as its blood supply, nerve supply & meninges with the brain. So, it is obvious that we can expect that eye would reflect changes within the body, especially vascular changes. COMMON SYSTEMIC DISEASES THAT EFFECT OUR EYES are as follows: ? Ocular disorder due to nutritional deficiencies like XEROPHTHALMIA. ? Ocular problem due to immunological disorder like * RHEUMATOID ARTHIRITIS * SYSTEMIC LUPUS ERYTHEMATOSUS * SARCOIDOSIS * REITER SYNDROME ? Ocular problem related with some haematological disease like- SICKLE CELL ANAEMIA ? Ocular problem related with some infectious 20 Verge Journal of the Venu Eye Institute & Research Centre systemic disorder like AIDS, TUBERCULOSIS ? Ocular disorder due to some endocrine disorder or circulatory disorder like * DIABETES MELLITUS * HYPERTHYROIDISM * HYPERTENSION ? Ocular disorder related to muscular disorder like MYASTHENIA GRAVIS HOW DO SYSTEMIC DISEASE EFFECT OUR EYES ? XEROPHTHALMIA –It is a common nutritional deficiency disorder of eye. It occurs due to dietary deficiency of vitamin A or its defective absorption from gut. It can cause night blindness, conjunctival xerosis, corneal xerosis, corneal ulcer & scar. ? A U T O IMMUNE DISORDERO c u l a r involvement occur as a component of various auto immune disorder, but the eye can also be involved secondarily, due to post inflammatory effect of disease or side effect of medication. common disease like RHEUMATOID ARTHIRITIS, SYSTEMIC L U P U S E RY T H E M AT O S U S , SARCOIDOSIS can cause inflammation in the eye. A common example of hypertensive retinopathy is seen in systemic lupus Scleritis Uveitis limbic keratitis, disc oedema. ? HYPERTENSION- It is the most common systemic disease. Every person of age 40 may be suffering from it. It can cause macular edema, cotton wool spots, retinal detachment,sub conjunctival haemorrhages etc. ? MYASTHENIA GRAVIS - It is a muscular disorder. It can affect the extra ocular muscle of eye. The extra ocular muscle differs from skeletal muscle elsewhere in the body in the nerve to motor end plate ratio and tonicity of the muscle. It can cause ptosis & diplopia. erythematosus. Besides this, dry eye, scleriti, uveitis enlargement of lacrimal glands are also some ocular feature of these disease. ? SICKLE CELL ANAEMIA- It is a haematological disease. The ocular manifestation may be the initial reason for presentation to an ophthalmologist or physician in some cases. It can cause dilated conjunctival vessels, retinal capillary o c c l u s i o n , neovascularization, chorioretinal scar. ? AIDS- It is an infectious disease with the HIV virus, an RNA virus of the human retrovirus family. The disease is characterized by a deficiency of T-helper lymphocytes. Ocular lesion is a common feature of AIDS. The ocular manifestations of HIV infection itself are microangiopathy affecting mainly the conjunctiva and retina and Kaposi sarcoma of the lids & conjunctiva. It can cause HIV retinopathy. Ocular features include cotton wool spots on retina, superficial & deep hemorrhages, microaneurysmes, retinal detachment etc. ? TUBERCULOSIS- is also a bacterial infectious disease. It causes a whole spectrum of involvement from lids to the ocular coats. ? DIABETES MELLITUS – It is a metabolic disorder. Blood sugar is raised due to defective insulin secretion/resistance to its action. In long standing cases of diabetes, ocular complication are found, they may even lead to visual loss. It can cause subconjunctival haemorrhages, refraction changes, premature formation of senile cataract, glaucoma etc. ? HYPERTHYRODISM - It can cause exophthalmos, lid retraction, lid lag, superior Systemic diseases are diseases that can happen to any person. We can't do anything to stop them but we can reduce the effect or treat the disease when it is diagnosed. For this a regular health checkup is advised to every person. A regular eye checkup can reveal any systemic disease at its early stages. So, we can treat them. If the eyes are involved then the ophthalmologist can do the treatment and depending upon the condition of disease, if systemic treatment is needed then the patients is referred to the related specialist for further management. Ocular treatment include therapy, inflammatory drugs, laser therapy, surgery etc. By following all the parameters we can prevent all eye problems related to systemic diseases October - December 2014 Verge Journal of the Venu Eye Institute & Research Centre 21 HOW CAN WE PREVENT THE EFFECT OF SYSTEMIC DISEASES ON BODY? VERGE October-December 2014 Applied for Registered With Registrarof Newspapers of India Regd. No. Pending Volume 17 issue 1 Volume 6 Issue 1