Visited ER at 03:21 Chief complaints Present illness Past History PE
advertisement

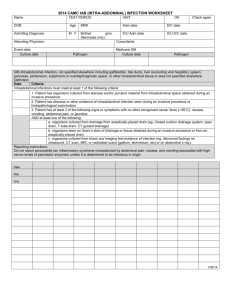
Visited ER at 03:21 A 66 Year-Old Man with abdominal pain • • • • 主述:右腳截肢疼痛,腹痛 Triage III TPR 35.3/89/18 BP 106/54 SpO2 100% E4V5M6 Ying-Lin,Tan, R1 Emergency Department, SKH 2013/01/09 Morning Meeting. Consultant:Vs Yang yu- Jeng Present illness Chief complaints • Abdominal pain for 2 days • Abdominal pain for 2 days Below umbilicus,back pain(+). 大小便解不出來 Past History • Past History ~Poor controlled DM ~Right DM foot s/p BK amputation • No known drug allergy PE • • • • Conscious clear Pale conjunctiva BS clear Soft. Tender over lower abdominen. No knocking pain over CVangle. • Right BK. Wound:clean.no erytheryma • Anal tone:intact. Impression & Management • DDx • Management 1. Abdominal pain,cause? • 03:35 – CBC.DC.PLT 2. R/o Anemia – F/S(121) 3. Right leg pain,r/o – BUN/Cre/AST/NA/K wound pain. – – – – – – Imaging PT/APTT IV N/S 60cc/hr Morphine 4mg IV st KUB,L‐spine Stool OB DRE(Yellow) Management • 04:14 Bedside echo: No GB stone. No AAA. No hydronephrosis. No ascites. Distended bladder. On Foley. U/A,U/C. 04:30 Initial Lab Report 危險值 • K=2.1 Blood • WBC:10.6K,Seg:83.5%,Band: 4.5% • Hb=6.7 gm/dl ( 11/30 9.4) • Ht=19.9% • RDW:17.3% • PLt:100K BUN:60 Cre:1.94.1 Na:135 • Stool OB: (‐) Lab Urine analysis • RBC:>100 • WBC:>100 • Epithelial cell:0‐1 • Bacteria +++ Management 1.Anemia:備輸pRBC 2U 2.Infection,UTI: B/C X II ,Cefmetazole 1g iv st VBG(G3),CRP 3.Acute renal failure 4.Hypokalemia: • KCL 20meq in N/S 100cc IVD run >30 mins • KCL 20meq po st • KCL 20meq in N/S 500cc in run 60cc/hr • Urine Cre,K,Na,osmolarity • On monitor • 排Nephro 住院,待轉EC. 5.Back pain,cause unknown Data • VBG G3: PH:7.439 PCO2:35.9 HCO3:24.3 S02:98% So? • Lower abdominal pain to back pain:? L2 compression fracture可以解釋嗎? CRP:15 EC management. 09:14 Lower back pain • 你想到甚麼DDx? 26~3 PS admission:Pneumonia,Wound infection,E/coli bacteremia 病人訴:3回家後背痛加劇,無法起來 如何DD with Lower back pain? Abdominal CT • T12 prevertebral abscess • L2 oeteomyelitis • Left psoas,illopsoas muscle abscess • Pelvic dirty ascites. Bone fracture? Leukocytosis,CRPinfection Spinal stenosis ? ? Further management • Consult Infection,GU,NS 13:42 NS Dr: Supportive therapy and Abx. Monitor lower limb muscle power 16:30 Uro Dr:Suggest medical therapy at first. 20:00 GU note 1.Antibiotic treatment first and medical treament first. 2.Surgical drainage may be arranged after antibiotic therapy 3.Correct ARF status 00:08 NS note • Muscle Power: Upper limb:Lt/Rt:4/4 Lower limb:Lt/Rt:2/3 ‐>NS:Decreased muscl epowersuggest to arrange emergent L‐spine MRI if no contraindication. 09:49 Infection Clinical Course • May keep Oxacillin 2g iv Q6H and Ceftriaxone 2g iv Q12H • Correct anemia,hypokalemia • May discuss with NS Doctor again due to decreased muscle power. • May discuss with Uro doctor for abscess drainage 23~25 ER EC‐>25 GU28 Seizure+desaturation‐ >DNR ‐>1/2 Expired Lower back pain Discussion 1.Approach to lower back pain 2.Psoas muscle abscess. Uptodate:Approach to acute back pain in adult TIntinallis:Chapeter:neck and back pain Neurologic emergency • Acute:<6weeks • Emergent: Abdominal aortic aneurysm, Epidural compression syndrome Lower back pain 1. Age: 18y/o:tumor,infection 50y/o:AAA,fracture,spinal stenosis,tumor 2. Pain Location and Radiation To buttock& thigh:Sciatica ‐>disc herniation 3. Trauma Minor trauma+Risk factor of osteoporosis ‐>fracture Lower back pain 4. Systemic Complaints •Fever, chills, night sweats, malaise, undesired weight loss •Risk factors: recent bacterial infection, urinary tract infection, or pneumonia; recent GU/ GI procedure; immunocompromised status; injection drug use; alcoholism, renal failure, diabetes. Risk factors for osteoporosis :old aged female sex, steroid use, alcoholism. Lower back pain 5. Pain Features •Benign:improves with rest ,lying •Red flag:night pain,BW loss,unrelenting pain •Worsening by:Valsalva maneuver, sitting ‐>disk herniation. •Neurologic claudication ‐> Spinal stenosis •Neurologic DeficitsBowel or bladder incontinence (overflow incontinence) Back to our case • Age>50 y/o, DM,back pain: 1. Trauma history(‐),X‐ray:osteolytic change in L spine,elevation CRP(ESR?),DM infection(osteomyelitis) Back pain+UTI+poor response ti TxPsoas muscle abscess Osteomyelitisextension to psoas,illopsoas m.Spinal cord involvement(?) 2. 3. Psoas muscle abscess • Primary VS Secondary. Primary abscess Secondary psoas abscess • Hematogenous or lymphatic seeding • Risk factors :diabetes, intravenous drug use, human immunodeficiency virus (HIV) infection, renal failure, and other forms of immunosuppression. Trauma,hematoma formation • Most prevalent in older patients. • In Taiwan, 2 retrospective reviews were carried out, and 20 % were classified as having primary abscesses. • Direct spread of infection to the psoas muscle from an adjacent structure. • Risk factors :trauma ,instrumentation in the inguinal region, lumbar spine, or hip region. Microbiology • Primary :Staphylococcus aureus. • Secondary:monomicrobial or polymicrobialenteric organisms ,Anaerobes • Klebsiella pneumoniae is an important cause of psoas abscess in Taiwan, especially in patients with diabetes. Thank You for your Attention!!!