Conventional and natural products against oral infections
advertisement

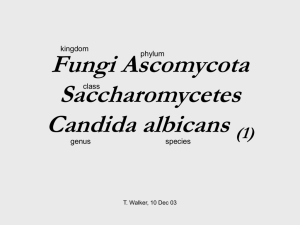
Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ Conventional and natural products against oral infections Flaviana Bombarda de Andrade1, Raquel Zanin Midena1, Cristiane Yumi Koga-Ito2 and Marco Antonio Hungaro Duarte1 1 2 Department of Dentistry, Endodontics and Dental Materials, Bauru Dental School, University of São Paulo, Brazil Department of Oral Bioscience and Diagnosis, Institute of Science and Technology, Universidade Estadual Paulista/UNESP In 1674, the Netherlander Antony van Leeuwenhoek (1632 - 1723), recognized as the discoverer of the microorganisms, created a device composed by plates of metal and lens, like a microscope, where he observed from human saliva, teeth and faeces, little movable objects, invisible through the naked eyes, that he called “animalcule” [1]. The oral cavity is an environment highly infected by commensal microorganisms that, initially, play the role of protection of the mucosa. The “resident” microbiota cohabits in a harmonic relationship with the host, as a beneficial infection and as a local host defense, since it makes difficult the implantation of pathogenic species, strange for this microbiota. This resident microbiota can become pathogenic when the host conditions are changed or the harmonic equilibrium is broken [2]. Due to the existence of teeth and periodontal spaces, the oral cavity shows many different ecological sites with peculiar environmental characteristics. The oral microbiota is the most complex inside the human, with more than 30 different genders of bacteria and more than 700 species. There are approximately 350 bacterial cultivable species and more than 200 species identified only by molecular techniques. The total number of oral microorganisms is similar to the intestinal microbiota besides more complex about the number of species [3, 4, 5]. However, the accumulation of the microbial biofilms can develop some diseases. Beyond the bacteria, other microorganisms such as virus and fungi can also colonize and induce oral diseases. The oral infections own specific characteristics, with a predominantly strict anaerobic and/or facultative microbiota, with propitious surfaces for adhesion and suitable nutrients. These microorganisms organize themselves quickly into biofilms, from initial adhesion to the dental enamel surface, gingival epithelium, tongue and mucosa, once they are flooded by saliva. Saliva contains proteins that can favor the molecular adsorption. Some species possess receptors or produce polysaccharides that can facilitate the adhesion and start the multiplication process. The nutrients come from saliva, accumulated food and gingival fluid [3, 5, 6, 7]. In addition, the oral microorganisms have to compete for sites where the receptors are already occupied by initial colonizers, deal with the positive and negative relationships among other microorganisms, resist to host defenses and possess some virulence factors [2, 8]. At the intrauterine life, the mouth is free of microorganisms. Some hours after the birth, the infection starts, with microorganisms coming from people in a strait contact with the baby, especially the mother, as a vertical infection. The facultative anaerobic bacteria are the most adaptable to the new mucosa, mainly the genus Streptococcus. When the teeth appear, new ecological sites are created and the oral microbiota develops more complex and intensely [3, 9]. The most prevalent species capable to adhere to the teeth surfaces are facultative anaerobic species as S. sanguinis, S. gordonii and S. oralis, in addition to some species of Actinomyces. Interproximal areas, enamel grooves and cracks provide conditions for the development of strict anaerobic bacteria. The gingival groove is a niche with very low content of oxygenation and it is conducive to installation of these anaerobes. The toothed adult man can have until 108 bacterial cells per mL of saliva and 1010 cell per gram of dental biofilm [3, 5]. Bacteria can adhere to the dental surface directly or to other initial colonizers by means of adesins and fimbriae. Some Gram-negative periodontopathogens are not able to adhere to the teeth, however, they have adherence binders toward to the periodontal pocket epithelium and/or to the initial colonizers [4, 8]. Saliva is responsible for the regulation of the supragengival microbiota, since it offers to the adhered microorganisms suitable temperature, pH, and humidity, in addition to some nutrients as proteins, amino acids, carbohydrates, vitamins and inorganic compounds. On the other side, saliva possess antibodies, antimicrobial substances and enzymes as lysozime and lactoferrin, pH stabilization system and a mechanical drag action due to the salivary flux. This salivary flux is increased during the speech and chewing, what is favorable to the removal of bigger accumulation of microorganisms. In spite of, during the sleep, this flux is greatly reduced, promoting the accumulation of biofilms and maintaining the acid pH [2,10]. The gingival fluid also helps to regulate the subgingival microbiota. Since the biofilm accumulation increases, the inflammatory response develops and the gingival exudate increases too. This fluid possesses many host defense factors as cells and the complement, however, is a great source of nutrients for anaerobic bacteria as proteins, hemin, k vitamin and hormones [3, 4]. Other factors that can promote the oral microorganism accumulation are cavities, inadequate restorations, prosthesis, crowding, orthodontic devices, epithelium loss, and in a more effective way, the systemic condition of the host, the diet and the quality of oral hygiene [3, 11]. 1574 © FORMATEX 2013 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ The more frequent oral diseases as caries, periodontal disease, periimplantitis, pulp space infections and candidiasis are called endogenous diseases, since their etiological agents are part of the resident microbiota, also in the healthy condition although in lower numbers. These diseases caused by biofilms are chronic, with a long duration, low clinical immunity and sporadic episodes of acute manifestations [3, 8]. The main biofilms produced in the oral cavity are: the cariogenic, at the dental surfaces, mainly composed by Grampositive, facultative, and saccharolytic bacteria and the periodontal biofilm at the gingival sulcus, mainly composed of Gram-negative, anaerobic and proteolytic bacteria distributed in these areas because of the nutritional and respiratory requirements. Also, there are the supra lingual biofilm with an anaerobic microbiota, most responsible for bad breath and the biofilm over dentures with the predominance of the fungi Candida albicans. The products of the metabolism from the cariogenic biofilm include a lot of acids, which can demineralize the enamel and start the dental decay. This process evolves and when it reaches the dental pulp the microbiota changes to anaerobic and proteolytic ones, due to the availability of proteins from dead pulp tissue. The periodontal biofilm generates protein metabolic products that can stimulate the inflammatory and immunological response of the tissue. Costerton et al. (1987) [12] conceptualize the biofilm as an association of microorganisms attached to a solid surface bathed by a liquid substance and embedded by a polysaccharidic matrix. This organizational form in biofilms gives great resistance to the microorganisms, due to the difficulty of chemical agents and host defense factors to penetrate inside the biofilm mass, besides genetic changes of virulence factors among the microorganisms. According to this idea, the biofilms are only totally removed by physical or mechanical ways. The dental biofilm, called before as “dental plaque” fits perfectly in this concept, since it is adhered to the teeth and mucosa surfaces and it is bathed by saliva. Its removal can be made efficiently by correct oral hygiene, teeth brushing and flossing, besides tongue cleaners [4, 12]. There is a continuing search for the development of effective antiseptics against cariogenic and periodontal biofilms, which may be used as adjuncts in controlling the formation of supragingival biofilm. If the chemical substances can not remove the formed biofilm, at least mouthrinses can impair its new formation (“de-novo” plaque formation). Some circumstances are good to use chemical products as: clean hidden surfaces, clean post surgical areas, for people with problems of coordination and demotivation, people inside hospitals and diminish the generated aerosol from patient mouth under dental treatment to the environment. Several active ingredients were tested in various formulations, especially chlorhexidine, cetylpyridinium chloride, triclosan and essential oils. The chlorhexidine normally is the most effective antimicrobial agent, not aggressive to the host tissue, but it has other adverse effects as teeth and restorations coloration, change of taste and ardency at the mucosa [13,14]. Parwani et al. (2013) [15] explored a alternative (herbal/natural miswak) to gold standard chlorhexidine gluconate mouthwash for the anti-plaque efficacy. They found that 0.2% chlorhexidine gluconate mouthwash remains the best anti-plaque agent. However, when socio-economic factor and/or side-effects of chlorhexidine need consideration, the tested herbal mouthwash may be considered as a good alternative. Haffajee et al. (2009) [16] investigated if antimicrobial mouthrinses with different formulations could affect the composition of the subgingival microbiota (by using checkerboard DNA-DNA hybridization) and clinical parameters of adjacent tissues in 116 periodontal maintenance subjects. The mouthrinses were herbal 1, herbal 2, essential oil, and chlorhexidine. Streptococcus and Capnocytophaga species were reduced most in the herbal rinse groups, while Veillonella parvula was reduced most in the essential oil and chlorhexidine groups. Actinomyces were also markedly reduced in the chlorhexidine group. Mean Plaque (PI) and Gingival Indices (GI) were reduced between baseline and three months in each group, especially for chlorhexidine and herbal rinses. The observed microbial changes were accompanied by improvements in clinical parameters. At the same way, Ferreira et al. (2006) [17] compared the antimicrobial effect of a commercial chlorhexidine, propolis and water mouthwashs over the total number of oral microorganisms, Candida albicans and Streptococcus mutans from saliva of healthy students. They observed that chemical solutions acted more efficiently over the species, chlorhexidine over C. albicans and S. mutans, and propolis over C. albicans. The total number of microorganisms was reduced equally by the three solutions showing the mechanical effect of the mouthwashes. The subgengival biofilms can induce periodontal diseases. The environment inside the gingival sulcus or pockets has a low amount of oxygen, about 1 to 2%, while in the normal air this rate is 21% [3].The nutrients are composed of protein from the gingival fluid, them the proteolytic and strict anaerobic microorganisms can establish in this site. It is a complex microbiota that stimulates the immunological response at the periodontal tissue. The main pathogens of this disease (chronic disease) are Porphyromonas gingivalis (Figure 1), Treponema denticola and Tanerella forsythia, besides many others associated. These three species compose the red complex of Socransky & Haffajee (2002). Recently, Jiao et al. (2013) [18] using molecular techniques, found a new bacterium in periodontal disease which stimulates a cell receptor, which is responsible for the recruitment of clastic cells, increasing the bone resorption. This last one can also be associated with the aggressive periodontitis, which is caused by a facultative Gram-negative bacterium Aggregatibacter actinomycetemcomitans. This microorganism is very persistent and treated with systemic antibiotic therapy. © FORMATEX 2013 1575 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ A 1576 B © FORMATEX 2013 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ genetic profile of the mutans strains from mothers and children, to verify the transmission. The dental treatment in mothers could prevent caries in children in the future. In one of these works, Pieralisi et al. (2010) [20] observed by molecular techniques, horizontal transmission (from colleagues each other in schools) besides vertical transmission (from mother to child) of S. mutans. On the other side, the etiology of dental caries has been investigated in order to identify other pathogens, also highly involved in caries process, since they survive in a acid pH, as Bifidobacterium and Actinomyces species [21]. Under normal conditions, the dentin-pulp complex is free of microorganisms and isolated from the oral environment. The coating dental structures (enamel and cementum) act as a barrier against the entry of microorganisms to the pulp cavity. When these structures are lost, either by decay, trauma or periodontal disease, the pulp will be unprotected and can evolve to necrosis, allowing the entry of micro-organisms via dentinal tubules or by exposure of the pulp tissue to the oral cavity. Deficient restorations and anachoresis are other ways for entry of microorganisms to the endodontic space [22, 23]. The bacteria in infected root canals include a restricted group of species [24]. The root canals have specific conditions, the availability of nutrients, low oxygen tension and bacterial interactions are important ecological determinants [25]. The first researcher to observe microorganisms in the root canals was Miller (1894)[26], by means of an optical microscope, finding cocci, bacilli and spirochetes. He suggested that the presence of bacteria inside root canal is the cause of apical periodontitis. Seventy years after this, Kakehashi et al (1965)[27] confirmed their assumptions. They evaluated the response of dental pulps exposed to the oral environment of conventional and germ-free mice. In conventional mice, there were necroses of the pulp tissue and periapical lesions, while germ-free mice showed viable pulp with a minimal inflammatory response and in some cases a dentin barrier, protecting the tissue of the oral cavity. Möller et al (1981) [28] conducted a study that also showed that microorganisms are the main cause of apical periodontitis and the absence of microorganisms leads to healing tissue. The endodontic infection can be classified to primary, secondary (endodontic retreatment) or persistent, when the composition of the microbiota may vary [29]. In the primary, the root canal infections present polymicrobial, predominantly anaerobic bacteria, Gram-negative or Gram-positive, in proportions that vary according to the painful symptomatology. The number of bacterial species in root canals may vary from 1 to 12, and the number of bacterial cells recovered is between less than 102 to more than 108. There is a correlation between the size of the periapical lesion and the number of bacterial species and cells present in the root canal. Thus, teeth with large lesions usually harbor more bacterial species and have a higher density of bacteria [25, 30,31]. The root canal microbiota is dominated by anaerobic bacteria. Facultative anaerobic bacteria such as Streptococcus also play a significant role in the infection, particularly in the coronal portion of the canal in the tooth pulp chamber exposed to the cavity [24]. Studies on the dynamics of root canal infections have shown that the relative proportions of anaerobic microorganisms and bacterial cells increase with time and that the facultatively anaerobic bacteria are outnumbered when the canals have been infected for 3 months or more [32]. Bacterial species commonly found in primary infections belong to the Gram-negative genera of Fusobacterium, Dialistes, Porphyromonas, Prevotlla, Tanerella, Treponema, Campylobacter and Veillonella and Gram-positive Parvimonas, Filifactor, Pseudormibacter, Olsenella, Actinomyces, Peptostreptococcus, Streptococcus, Propionibacterium and Eubacterium. Differences in availability of nutrients and oxygen tension in the apical region compared with the main root canal are important reasons for the dominance of slow growing, obligatory anaerobic bacteria in the apical region. The endodontic treatment aims to eliminate or significantly reduce micro-organisms in the root canal system through irrigating solutions and dressings with antiseptic properties. Moreover, with the step of the filling and subsequent sealing the crown prevent introduction of new microorganisms. However, faults can occur during the treatment and some micro-organisms can resist causing failure and persistence of periapical inflammation, resulting in persistent symptoms and flare-ups. The composition of the microbiota after root canal treatment failure differs from that found in untreated teeth [33,34]. Gram-negative bacteria, which are common members of primary infection, are usually eliminated. Most studies reveled that Gram-positive bacteria are more frequently present [30]. They include streptococci, Parvimonas micra, Actinomyces species, Propionibacterium species, Pseudoramibacter alactolyticus, Lactobacilli, Enterococcus faecalis and Olsenella uli. The number of present species in the secondary or persistent infections is smaller than occurs in primary infections, an average of one to five bacterial species per case, with counts reaching 102 to 105 cells per sample. Enterococcus faecalis is the species most often found in cases of treatment failure [35]. In addition to the bacterial species, fungi can also be found in cases of secondary infection or persistent, as Candida albicans [36]. This species has the ability to colonize and invade the dentin and seems to be resistant to calcium hydroxide dressing [37]. The presence of microorganism in root canals can cause apical periodontitis, which function is act as a barrier to separate the infection of root canal from alveolar bone and other body sites. However, in some cases the microorganisms colonize and break this barrier to the apical area establishing an extra-radicular infection. Persistent extraradicular infection is not affected by the action of antimicrobial agents such irrigants and medicaments using during root © FORMATEX 2013 1577 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ canal treatment. Apical surgery may be the only method for definitive removal of an established extra-radicular infection promoting repair in therapy-resistant cases (Figure 3) [38]. A B Fig. 3 Periapical biofilm of a persistent endodontic lesion, showing presence of a fungus joined to the filling material – guta-percha (A) and a streptococci chain inside this biofilm in the extrarradicular area. Irrigating solutions such as sodium hypochlorite and chlorhexidine have a wide spectrum of action on the microorganisms present in endodontic infections. However, during the treatment they act for a short time and often cannot penetrate inside some parts of the root canal system. Therefore, the use of the dressings is necessary to allow a longer action against microorganisms in root canal and prevent the proliferation of microorganisms, acting as a mechanical barrier to reinfection [39]. The use of calcium hydroxide in clinical situations involving necrotic pulp is advantageous as a result of its antiseptic action on the microorganisms present in the main root canal, its ramifications, in the dentinal tubules, as well as in the apical cementum [40]. The addition of other antiseptic substances to calcium hydroxide has been proposed to enhance its antimicrobial effect [41], like phytotherapics, such as Casearia sylvestris [42]. The use of propolis in Endodontics, a bee hives product, as intracanal dressing, has been shown to be effective against several bacterial species found in endodontic infections, such as E. faecalis and certain anaerobes. Its antimicrobial effect is similar to other drugs used, such as chlorhexidine gel 2%, formocresol, and camphorated paramonochlorophenol, and better than calcium hydroxide. Its biocompatibility is another great advantage [43,44]. A recently study conducted by the Department of Endodontics, Bauru Dental School, São Paulo, Brazil, evaluated the antimicrobial effect of calcium hydroxide pastes associated to propolis inside the root canals. Bovine dentin tubes previously infected with Enterococcus faecalis were used and these pastes remained inside root canals for 15 days. By analysis with Confocal Laser Scanning Microscopy and microbiological culture, the Propolis addition in the calcium hydroxide pastes showed lower cell viability as compared to the calcium hydroxide paste alone. The authors concluded that there are advantages in using Propolis in calcium hydroxide pastes, increasing intratubular penetration which improves the performance against these micro-organisms (Figure 4) [45]. 1578 © FORMATEX 2013 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ A B Fig. 4 Images using a confocal laser scanning microscopy of dentin tubules with Enterococcus faecalis (from Arias, 2013). These fragments were stained with the Life&Dead dye, showing alive green bacteria and dead bacteria stained in red. In first sample the teeth was treated with calcium hydroxide paste, showing some live bacteria (A) and in the second sample, the teeth was treated with calcium hydroxide plus propolis paste, showing most of bacteria dead (B). Photodynamic therapy is a reaction between photosynthetic dyes and light, generating a cytotoxic effect over the microorganisms, usually via oxidative reactions that result in cell death through apoptosis. In Endodontics, photodynamic therapy has shown good results [46, 47], being an interesting tool to obtain better antisepsis in endodontic treatment [48]. Ozonated water can also be applied during the biomechanical preparation in Endodontics, as an auxiliary substance to irrigation, and should be used as end-irrigating [49]. Furthermore, its use significantly reduced the number of Candida albicans and Enterococcus faecalis in root canals of human teeth [50]. The ozone can also be used in the process of intracanal medicament in form of ozonized oil, and has shown satisfactory results when compared to similar calcium hydroxide [51]. Candida spp. are considered opportunistic pathogens as they are both colonizers and have the ability to cause infections in response to alterations in the host’s physiology [52]. The presence of these yeasts in the oral cavity of healthy individuals varies from 35 to 60%. C. albicans is the most prevalent species, totalizing 60 to 70% of the isolates, followed by C. tropicalis and C. glabrata [53,54]. Therefore, the isolation of Candida spp. from oral cavity is not a confirmatory evidence of infection and clinical signs and symptoms must be also considered for the diagnosis of candidiasis [55]. Occurrence of disease is a result of an imbalance between host’s factors (local or systemic predisposing factors) and candidal virulence factors. The most frequently related systemic factors are use of broad-spectrum antibiotics and corticosteroids, diabetes mellitus and immunosuppression [56-59]. Inadequate oral hygiene, use of dentures, orthodontic devices, chronic periodontits, smoking, and xerostomia have been cited as oral local factors [60-63]. Capacity of adherence to mucosa, growth at 37°C, hydrophobicity, yeast-to-hyphae transition, biofilm formation, production of histolytic enzymes (such as aspartyl proteases and phospholipases) have been cited as the main C. albicans virulence factors [64,65]. Oral candidiasis is common among immunocompromised individuals, while systemic infection can be observed in more severe cases of immunosuppression [66]. Although C. albicans is more frequently isolated in cases of oral candidiasis, C. parapsilosis, C. glabrata, C. krusei, C. guilliermondii, C. lipolytica and C. kefyr have been considered as emergent pathogens. Several studies showed that patients with systemic predisposing factors have higher incidence of non-albicans species when compared to healthy controls [67-71]. Oral candidiasis can be observed basically as three different clinical variants: pseudomembranous, erythematous and hyperplastic [72]. Candida albicans has been also cited as a putative endodontic pathogen. More recently, the capacity of C. albicans to survive and form biofilm for over six months under anaerobic and nutrient-limited conditions was reported [73], corroborating the ability of these yeasts in surviving inside root canals. Conventional therapeutic options for oral candidiasis range from topical polyene antifungals to azole agents. However, the increase in the occurrence of resistance of Candida spp. to conventional antifungals has been related in the last decades. Even though the prevalence of resistant oral isolates seems to be still low, they have been found in particular among patients with predisposing factors [69, 74]. Besides, antifungal drugs show relevant limitations, such as low spectrum, interaction with other drugs, high cost and toxic effects. Markedly, the toxic effects are result of the similarities between yeast and host cells (both eucariotic), are very relevant in clinical context. In particular for © FORMATEX 2013 1579 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ erithematous candidosis, the recurrence of the lesion after treatment with conventional antifungals has been reported especially when associated to poor denture hygiene [75]. Regarding the presence of C. albicans in endodontic infections, the conventional intracanal medications such as 2% chlorhexidine [76,77] and 1% sodium hypochlorite [78] has been considered effective. The combination of calcium hydroxide and 2% chlorhexidine gel showed efficacy against Candida spp. in vivo [79]. Calcium hydroxide alone is less effective against C. albicans [80]. Due to the reported limitations regarding the available therapeutic alternatives, the searching for new options is highly necessary. In this context, alternative protocols and natural products have been widely investigated aiming the finding of new antifungal molecules. The use of ozonated water to the disinfection of dentures infected by C. albicans has been proposed [81] and it showed efficacy in reducing the number of yeasts adhered to acrylic specimens [82]. Additionally, ozonated water reduced counts of C. albicans experimentally inoculated in root canals in vitro at immediate sampling. However, no residual effect was observed since increased values of CFU were detected after 7 days [83]. Vinegar and sodium bicarbonate can be also considered promising alternative substances with efficacy for the disinfection of acrylic resin inoculated with C. albicans, due to their low cost and availability [84,85]. Investigations on the dental applications of propolis for candida infections have been done. The use of propolis ethanolic extract inhibited in vitro growth of C. albicans isolates from oral candidiasis [86]. Moreover, this extract showed similar clinical effectiveness for the treatment of patients with denture-associated candidiasis when compared to miconazole [87]. On the contrary, propolis as intracanal medicament was not able to reduce counts of C. albicans experimentally infected root canals [88]. Plants extracts, essential oils and compounds have been an important source of research for new antifungal options against Candida spp. Effectiveness of Coriandrum sativum L. essential oil on the biofilm formation by C. albicans isolates from patients with periodontal disease was reported [89]. Cybopogon citratus and Syzygium aromaticum essential oils inhibited C. albicans biofilm formation and were more active against pre-formed biofilms when compared to amphotericin B and fluconazole in vitro [90]. Methanol extract of Mentha piperita, Rosmarinus officinalis, Arrabidaea chica, Tabebuia avellanedae, Punica granatum and Syzygium cumini showed antifungal activity on Candida species [91]. Methanol extract of Ficus deltoidea showed in vitro activity on C. albicans [92]. Seed and leaf extracts of Abelmoschus moschatus were tested against C. albicans cells, using microdilution test, and showed similar inhibitory effect when compared to nystatin [93]. A paste containing ethyl acetate fraction (AcOEt) extracted from Arctium lappa inhibited the growth of C. albicans besides of other endodontically related microorganisms [94]. Some studies already evaluate isolated substances or secondary metabolites from plants. The effects of licorice and its isolated compounds (licochalcone A, glabridin and glycyrrhizic acid) on C albicans also show promising results. Glabridin and licochalcone A showed potent antifungal activity and prevented yeast-hyphal transition. Besides, licochalcone Z showed a significant effect on C. albicans biofilm formation [95,96]. The in vitro and in vivo antiCandida activities of pogostone that is isolated from Pogostemon cablin (Blanco) Benth have been also reported. Pogostone was equally effective against fluconazole-resistant C. albicans strains when compared to voriconazole [97]. A-type cranberry proanthocyanidins prevented C. albicans biofilm formation and reduced the adherence to oral epithelial cells and saliva-coated acrylic resin specimen [98]. The compounds 2',6'-dihydroxy-4'geranyloxyacetophenone and 2',6'-dihydroxy-4'-farnesyloxy-acetophenone, extracted from plants belonging to the Rutaceae family, showed high antimicrobial activity on C. albicans [99]. References [1] [2] McGhee JR, Michalek SM, Cassell GH. Dental Microbiology. Harper & Row, Philadelphia, 1982. De Lorenzo JL, Avila-Campos MJ. Relações microbiota-hospedeiro: Infecção e resistência. In: De Lorenzo JL. Microbiologia para o estudante de odontologia. Atheneu, São Paulo, 2004. [3] De Lorenzo JL. O ecossistema bucal. In: De Lorenzo JL. Microbiologia para o estudante de odontologia. Atheneu, São Paulo, 2004. [4] Socransky SS, Haffajee AD. Dental biofilms: difficult therapeutic targets. Periodontology 2000, Vol. 28, 2002, 12–55 [5] Aas JA, Paster BJ, Stokes LN, Olsen I, Dewhirst FE. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol. 2005 Nov;43(11):5721-32. [6] Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986 Dec;50(4):353-80. [7] Kolenbrander PE, London J. Adhere today, here tomorrow: oral bacterial adherence. J Bacteriol. 1993 Jun;175(11):3247-52. [8] Nolte WA. Interactions between microorganisms and the host. In: ____Oral Microbiology, 4th ed., Mosby, St Louis, 1982. [9] Caufield PW, Cutter GR, Dasanayake AP. Initial acquisition of mutans streptococci by infants: evidence for a discrete window of infectivity. J Dent Res. 1993 Jan;72(1):37-45. [10] Felizardo KR, Gonçalves RB, Schwarcz WD, Poli-Frederico RC, Maciel SM, Andrade FB. An evaluation of the expression profiles of salivary proteins lactoferrin and lysozyme and their association with caries experience and activity. Rev Odonto Ciênc. 2010;25(4):344-349. 1580 © FORMATEX 2013 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ [11] Botelho, MPJ, Maciel, SM, Cerci-Neto, A, Dezan, CC, Fernandes, KBP, Andrade, FB. Cariogenic Microorganisms and Oral Conditions in Asthmatic Children. Caries Research.2011;45:386-392,. [12] Costerton JW, Cheng KJ, Geesey GG, Ladd TI, Nickel C, Dasgupta M, Marrie TJ. Bacterial biofilms in nature and disease. Ann. Rev. Microbiol. 1987. 41:435-64. [13] Feres M, Gursky LC, Faveri M, Tsuzuki CO, Figueiredo LC. Clinical and microbiological benefits of strict supragingival plaque control as part of the active phase of periodontal therapy. J Clin Periodontol. 2009 Oct;36(10):857-67. [14] Feres M, Figueiredo LC, Faveri M, Opperman RV, Greggianin BF, Oliveira SC, Lubiana NF. Controle diário do biofilme com antissépticos – Uma visão atual para a prática clínica. Enxaguatórios no dia a dia do dentista. Rev ABO Nac. 2010 Agosto/setembro; 18(4):3-8. [15] Parwani SR, Parwani RN, Chitnis PJ, Dadlani HP, Prasad SV. Comparative evaluation of anti-plaque efficacy of herbal and 0.2% chlorhexidine gluconate mouthwash in a 4-day plaque re-growth study. J Indian Soc Periodontol. 2013 Jan;17(1):72-7. [16] Haffajee AD, Roberts C, Murray L, Veiga N, Martin L, Teles RP, Letteri M, Socransky SS. Effect of herbal, essential oil, and chlorhexidine mouthrinses on the composition of the subgingival microbiota and clinical periodontal parameters. J Clin Dent. 2009;20(7):211-7. [17] Ferreira FBA, Jacob NC, Luvisotto E, Segura VG, Marcucci MC. Avaliação microbiológica in vivo do efeito de bochechos à base de própolis e de clorexidina. Braz Oral Res, v. 20, Supplement (Proceedings of the 23rd Annual SBPqO Meeting), p 98, 2006. [18] Jiao Y, Darzi Y, Tawaratsumida K, Marchesan JT, Hasegawa M, Moon H, Chen GY, Nunez G, Giannobile WV, Raes J, Inohara N. Induction of Bone Loss by Pathobiont-Mediated Nod1 Signaling in the Oral Cavity. Cell Host & Microbe 13: 595– 601, 2013. [19] Gebara EC, Faria CM, Pannuti C, Chehter L, Mayer MP, Lima LA. Persistence of Helicobacter pylori in the oral cavity after systemic eradication therapy. J Clin Periodontol. 2006 May;33(5):329-3 [20] Pieralisi, FJS, Rodrigues, MR,Segura, VG, Maciel, SM, Ferreira, FBA, Garcia, JE, Poli-Frederico, RC. Genotypic Diversity of Streptococcus mutans in Caries-Free and Caries-Active Preschool Children. International Journal of Dentistry (Print). 2010;16, 2010. [21] Beighton D. The complex oral microflora of high-risk individuals and groups and its role in the caries process. Community Dent Oral Epidemiol. 2005 Aug;33(4):248-55. [22] Grossman LI. Origin of microorganisms in traumatized, pulpless, sound teeth. J Dent Res. 1967 May-Jun;46(3):551-3 [23] Siqueira Jr, Jf. Treatment of Endodontic Infections. 1st ed. São Paulo Quintessence;2011. [24] Sundqvist G. Taxonomy, ecology, and pathogenicity of the root canal flora. Oral Surg Oral Med Oral Pathol. 1994 Oct;78(4):522-30 [25] Sundqvist G. Ecology of the root canal flora. J Endod 1992;18:427–30. [26] Miller WD. An introduction to the study of the bacteriopathology of the dental pulp. Dent Cosmos 1894; 36: 505-528. [27] Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965 Sep;20:340-9 [28] Moller AJR, Fabricius L, Dahlen G, Ohman AE, Heyden G. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res 1981; 89:475-484. [29] Siqueira JF Jr. Endodontic infections: concepts, paradigms, and perspectives. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 Sep;94(3):281-93 [30] Siqueira Jr, JF, Rôças, IN. Update on endodontic microbiology: candidate pathogens and patterns of colonization. ENDO (Lond Engl) 2008;2(1)7-20 [31] Sundqvist G, Figdor D. Life as an endodontic pathogen. Ecological differences between the untreated and root-filled root canals. Endod Topics 2003;6:3–28 [32] Fabricius L, Dahlén G, Öhman AE, Möller AJR. Predominant indigenous oral bacteria isolated from infected root canals after varied times of closure. Scand J Dent Res 1982: 90: 134–144. [33] Sundqvist G, Figdor D, Persson S, Sjögren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jan;85(1):86-93. [34] Pinheiro ET, Gomes BP, Ferraz CC, Teixeira FB, Zaia AA, Souza Filho FJ. Evaluation of root canal microorganisms isolated from teeth with endodontic failure and their antimicrobial susceptibility. Oral Microbiol Immunol. 2003 Apr;18(2):100-3. [35] Gomes BP, Pinheiro ET, Jacinto RC, Zaia AA, Ferraz CC, Souza-Filho FJ. Microbial analysis of canals of root-filled teeth with periapical lesions using polymerase chain reaction. J Endod. 2008 May;34(5):537-40 [36] Siqueira JF Jr, Rôças IN, Lopes HP, Elias CN, de Uzeda M. Fungal infection of the radicular dentin. J Endod. 2002 Nov;28(11):770-3. [37] Sen BH, Safavi KE, Spångberg LS. Colonization of Candida albicans on cleaned human dental hard tissues. Arch Oral Biol. 1997 Jul;42(7):513-20. [38] Ferreira FB, Ferreira AL, Gomes BP, Souza-Filho FJ. Resolution of persistent periapical infection by endodontic surgery. Int Endod J. 2004 Jan;37(1):61-9. [39] Siqueira JF Jr, Uzeda M. Influence of different vehicles on the antibacterial effects of calcium hydroxide. J Endod. 1998 Oct;24(10):663-5 [40] Estrela C, Sydney GB, Bammann LL, Felippe Júnior O. Mechanism of action of calcium and hydroxyl ions of calcium hydroxide on tissue and bacteria. Braz. Dental J. 1995;6:85–90. [41] Evans MD, Baumgartner JC, Khemaleelakul S, Xia T. efficacy of calcium hydroxide: chlorhexidine paste as an intracanal medication in bovine dentin. J Endod 2003;29: 338–9. [42] Duarte MA, Midena RZ, Zeferino MA, Vivan RR, Weckwerth PH, Santos F, Guerreiro-Tanomaru JM, Tanomaru-Filho M. Evaluation of pH and calcium ion release of calcium hydroxide pastes containing different substances. J Endod. 2009 Sep;35(9):1274-7. © FORMATEX 2013 1581 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ [43] Ferreira FB, Torres SA, Rosa OP, Ferreira CM, Garcia RB, Marcucci MC, Gomes BP. Antimicrobial effect of propolis and other substances against selected endodontic pathogens. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Nov;104(5):709-16. [44] Ferreira FB, Silva E Souza Pde A, do Vale MS, de Moraes IG, Granjeiro JM. Evaluation of pH levels and calcium ion release in various calcium hydroxide endodontic dressings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004 Mar;97(3):38892. [45] Arias MPC. Influência da agitação ultrassônica na ação antimicrobiana de pastas de3 hidróxido de cálcio e própolis. 2013. Dissertation (Master degree in Applied Dental Science), Bauru Dental School, University of São Paulo, Brazil. [46] Nunes MR, Mello I, Franco GC, de Medeiros JM, Dos Santos SS, Habitante SM, Lage-Marques JL, Raldi DP. Effectiveness of photodynamic therapy against Enterococcus faecalis, with and without the use of an intracanal optical fiber: an in vitro study. Photomed Laser Surg. 2011 Dec;29(12):803-8. [47] Silva LA, Novaes AB Jr, de Oliveira RR, Nelson-Filho P, Santamaria M Jr, Silva RA. Antimicrobial photodynamic therapy for the treatment of teeth with apical periodontitis: a histopathological evaluation. J Endod. 2012 Mar;38(3):360-6. [48] Silva Garcez A, Núñez SC, Lage-Marques JL, Jorge AO, Ribeiro MS. Efficiency of NaOCl and laser-assisted photosensitization on the reduction of Enterococcus faecalis in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Oct;102(4):e93-8. [49] Lynch E. Evidence-based efficacy of ozone for root canal irrigation. J Esthet Restor Dent. 2008;20(5):287-93. [50] Cardoso MG, de Oliveira LD, Koga-Ito CY, Jorge AO. Effectiveness of ozonated water on Candida albicans, Enterococcus faecalis, and endotoxins in root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Mar;105(3):e85-91. [51] Silveira AM, Lopes HP, Siqueira JF Jr, Macedo SB, Consolaro A. Periradicular repair after two-visit endodontic treatment using two different intracanal medications compared to single-visit endodontic treatment. Braz Dent J.2007;18(4):299-304. [52] Soll DR. Candida commensalism and virulence: the evolution of phenotypic plasticity. Acta Trop. 2002 Feb;81(2):101-10. [53] Odds FC. Candida and candidosis. London: Baillière Tindall. 1988. [54] Samaranayake LP, MacFarlane MW. Oral candidosis. Cambridge: Universty Press, 1990. [55] Ellepola AN, Samaranayake LP. Oral candidal infections and antimycotics. Crit Rev Oral Biol Med. 2000;11(2):172-98 [56] Jabra-Rizk MA, Ferreira SM, Sabet M, Falkler WA, Merz WG, Meiller TF. Recovery of Candida dubliniensis and other yeasts from human immunodeficiency virus-associated periodontal lesions. J Clin Microbiol. 2001 Dec;39(12):4520-2. [57] Komiyama EY, Ribeiro PM, Junqueira JC, Koga-Ito CY, Jorge AO. Prevalence of yeasts in the oral cavity of children treated with inhaled corticosteroids. Braz Oral Res. 2004 Jul-Sep;18(3):197-201. [58] Belazi M, Velegraki A, Koussidou-Eremondi T, Andreadis D, Hini S, Arsenis G, Eliopoulou C, Destouni E, Antoniades D. Oral Candida isolates in patients undergoing radiotherapy for head and neck cancer: prevalence, azole susceptibility profiles and response to antifungal treatment. Oral Microbiol Immunol. 2004 Dec;19(6):347-51. [59] Belazi M, Velegraki A, Fleva A, Gidarakou I, Papanaum L, Baka D, Daniilidou N, Karamitsos D. Candidal overgrowth in diabetic patients: potential predisposing factors. Mycoses. 2005 May;48(3):192-6 [60] Darwazeh AM, Al-Refai S, Al-Mojaiwel S. Isolation of Candida species from the oral cavity and fingertips of complete denture wearers. J Prosthet Dent. 2001 Oct;86(4):420-3. [61] Grimoud AM, Marty N, Bocquet H, Andrieu S, Lodter JP, Chabanon G. Colonization of the oral cavity by Candida species: risk factors in long-term geriatric care. J Oral Sci. 2003 Mar;45(1):51-5. [62] Hägg U, Kaveewatcharanont P, Samaranayake YH, Samaranayake LP. The effect of fixed orthodontic appliances on the oral carriage of Candida species and Enterobacteriaceae. Eur J Orthod. 2004 Dec;26(6):623-9. [63] Soysa NS, Ellepola AN. The impact of cigarette/tobacco smoking on oral candidosis: an overview. Oral Dis. 2005 Sep;11(5):268-73. [64] Calderone RA, Fonzi WA. Virulence factors of Candida albicans. Trends Microbiol. 2001 Jul;9(7):327-35. [65] Mayer FL, Wilson D, Hube B. Candida albicans pathogenicity mechanisms. Virulence. 2013 Feb 15;4(2):119-28. [66] Hube B. From commensal to pathogen: stage- and tissue-specific gene expression of Candida albicans. Curr Opin Microbiol. 2004 Aug;7(4):336-41 [67] Back-Brito GN, Mota AJ, Vasconcellos TC, Querido SM, Jorge AO, Reis AS, Balducci I, Koga-Ito CY. Frequency of Candida spp. in the oral cavity of Brazilian HIV-positive patients and correlation with CD4 cell counts and viral load. Mycopathologia. 2009 Feb;167(2):81-7 [68] Araújo Navas EA, Inocêncio AC, Almeida JD, Back-Brito GN, Mota AJ, Jorge AO, Querido SM, Balducci I, Koga-Ito CY. Oral distribution of Candida species and presence of oral lesions in Brazilian leprosy patients under multidrug therapy. J Oral Pathol Med. 2009 Nov;38(10):764-7 [69] Bremenkamp RM, Caris AR, Jorge AO, Back-Brito GN, Mota AJ, Balducci I, Brighenti FL, Koga-Ito CY. Prevalence and antifungal resistance profile of Candida spp. oral isolates from patients with type 1 and 2 diabetes mellitus. Arch Oral Biol. 2011 Jun;56(6):549-55 [70] Araújo Navas EA, Sato EI, Pereira DF, Back-Brito GN, Ishikawa JA, Jorge AO, Brighenti FL, Koga-Ito CY. Oral microbial colonization in patients with systemic lupus erythematous: correlation with treatment and disease activity. Lupus. 2012 Aug;21(9):969-77. [71] Back-Brito GN, da Mota AJ, de Souza Bernardes LÂ, Takamune SS, Prado Ede F, Cordás TA, Balducci I, da Nobrega FG, Koga-Ito CY. Effects of eating disorders on oral fungal diversity. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Apr;113(4):512-7 [72] Reichart PA, Samaranayake LP, Philipsen HP. Pathology and clinical correlates in oral candidiasis and its variants: a review. Oral Dis. 2000 Mar;6(2):85-91. [73] Ning Y, Hu X, Ling J, Du Y, Liu J, Liu H, Peng Z. Candida albicans survival and biofilm formation under starvation conditions. Int Endod J. 2013 Jan;46(1):62-70. [74] Koga-Ito CY, Lyon JP, Vidotto V, de Resende MA. Virulence factors and antifungal susceptibility of Candida albicans isolates from oral candidosis patients and control individuals. Mycopathologia. 2006 Apr;161(4):219-23. 1582 © FORMATEX 2013 Microbial pathogens and strategies for combating them: science, technology and education (A. Méndez-Vilas, Ed.) ____________________________________________________________________________________________ [75] Gendreau L, Loewy ZG. Epidemiology and etiology of denture stomatitis. J Prosthodont. 2011 Jun;20(4):251-60 [76] Valera MC, Salvia AC, Maekawa LE, Camargo SE, Carvalho CA, Camargo CH, Koga-Ito CY. Antimicrobial analysis of chlorhexidine gel and intracanal medicaments against microorganisms inoculated in root canals. Minerva Stomatol. 2010 JulAug;59(7-8):415-21. [77] Mohammadi Z, Giardino L, Palazzi F. Evaluation of the antifungal activity of four solutions used as a final rinse in vitro. Aust Endod J. 2013 Apr;39(1):31-4. [78] Valera MC, Silva KC, Maekawa LE, Carvalho CA, Koga-Ito CY, Camargo CH, Lima RS. Antimicrobial activity of sodium hypochlorite associated with intracanal medication for Candida albicans and Enterococcus faecalis inoculated in root canals. J Appl Oral Sci. 2009 Nov-Dec;17(6):555-9. [79] Sinha N, Patil S, Dodwad PK, Patil AC, Singh B. Evaluation of antimicrobial efficacy of calcium hydroxide paste, chlorhexidine gel, and a combination of both as intracanal medicament: An in vivo comparative study. J Conserv Dent. 2013 Jan;16(1):65-70. [80] Mohammadi Z, Shalavi S, Yazdizadeh M. Antimicrobial activity of calcium hydroxide in endodontics: a review. Chonnam Med J. 2012 Dec;48(3):133-40. [81] Oizumi M, Suzuki T, Uchida M, Furuya J, Okamoto Y. In vitro testing of a denture cleaning method using ozone. J Med Dent Sci. 1998 Jun;45(2):135-9. [82] Arita M, Nagayoshi M, Fukuizumi T, Okinaga T, Masumi S, Morikawa M, Kakinoki Y, Nishihara T. Microbicidal efficacy of ozonated water against Candida albicans adhering to acrylic denture plates. Oral Microbiol Immunol. 2005 Aug;20(4):206-10. [83] Cardoso MG, de Oliveira LD, Koga-Ito CY, Jorge AO. Effectiveness of ozonated water on Candida albicans, Enterococcus faecalis, and endotoxins in root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Mar;105(3):e85-91. [84] da Silva FC, Kimpara ET, Mancini MN, Balducci I, Jorge AO, Koga-Ito CY. Effectiveness of six different disinfectants on removing five microbial species and effects on the topographic characteristics of acrylic resin. J Prosthodont. 2008 Dec;17(8):627-33. [85] Sousa FA, Paradella TC, Koga-Ito CY, Jorge AO. Effect of sodium bicarbonate on Candida albicans adherence to thermally activated acrylic resin. Braz Oral Res. 2009 Oct-Dec;23(4):381-5. [86] Martins RS, Péreira ES Jr, Lima SM, Senna MI, Mesquita RA, Santos VR. Effect of commercial ethanol propolis extract on the in vitro growth of Candida albicans collected from HIV-seropositive and HIV-seronegative Brazilian patients with oral candidiasis. J Oral Sci. 2002 Mar;44(1):41-8. [87] Santos VR, Gomes RT, de Mesquita RA, de Moura MD, França EC, de Aguiar EG, Naves MD, Abreu JA, Abreu SR. Efficacy of Brazilian propolis gel for the management of denture stomatitis: a pilot study. Phytother Res. 2008 Nov;22(11):1544-7. [88] Carbajal Mejía JB. Antimicrobial effects of calcium hydroxide, chlorhexidine, and propolis on Enterococcus faecalis and Candida albicans. J Investig Clin Dent. 2013 [Epub ahead of print]. [89] Furletti VF, Teixeira IP, Obando-Pereda G, Mardegan RC, Sartoratto A, Figueira GM, Duarte RM, Rehder VL, Duarte MC, Höfling JF. Action of Coriandrum sativum L. Essential Oil upon Oral Candida albicans Biofilm Formation. Evid Based Complement Alternat Med. 2011;2011:985832. [90] Khan MS, Ahmad I. Biofilm inhibition by Cymbopogon citratus and Syzygium aromaticum essential oils in the strains of Candida albicans. J Ethnopharmacol. 2012 Mar 27;140(2):416-23. [91] Höfling JF, Anibal PC, Obando-Pereda GA, Peixoto IA, Furletti VF, Foglio MA, Gonçalves RB. Antimicrobial potential of some plant extracts against Candida species. Braz J Biol. 2010 Nov;70(4):1065-8. [92] Abdsamah O, Zaidi NT, Sule AB. Antimicrobial activity of Ficus deltoidea Jack (Mas Cotek). Pak J Pharm Sci. 2012 Jul;25(3):675-8. [93] Gul MZ, Bhakshu LM, Ahmad F, Kondapi AK, Qureshi IA, Ghazi IA. Evaluation of Abelmoschus moschatus extracts for antioxidant, free radical scavenging, antimicrobial and antiproliferative activities using in vitro assays. BMC Complement Altern Med. 2011 Aug 17;11:64. [94] Gentil M, Pereira JV, Sousa YT, Pietro R, Neto MD, Vansan LP, de Castro França S. In vitro evaluation of the antibacterial activity of Arctium lappa as a phytotherapeutic agent used in intracanal dressings. Phytother Res. 2006 Mar;20(3):184-6. [95] Messier C, Grenier D. Effect of licorice compounds licochalcone A, glabridin and glycyrrhizic acid on growth and virulence properties of Candida albicans. Mycoses. 2011 Nov;54(6):e801-6 [96] Messier C, Epifano F, Genovese S, Grenier D. Licorice and its potential beneficial effects in common oro-dental diseases. Oral Dis. 2012 Jan;18(1):32-9. [97] Li YC, Liang HC, Chen HM, Tan LR, Yi YY, Qin Z, Zhang WM, Wu DW, Li CW, Lin RF, Su ZR, Lai XP. Anti-Candida albicans activity and pharmacokinetics of pogostone isolated from Pogostemonis Herba. Phytomedicine. 2012 Dec 15;20(1):77-83. [98] Feldman M, Tanabe S, Howell A, Grenier D. Cranberry proanthocyanidins inhibit the adherence properties of Candida albicans and cytokine secretion by oral epithelial cells. BMC Complement Altern Med. 2012 Jan 16;12:6. [99] Bonifait L, Marquis A, Genovese S, Epifano F, Grenier D. Synthesis and antimicrobial activity of geranyloxy- and farnesyloxy-acetophenone derivatives against oral pathogens. Fitoterapia. 2012 Sep;83(6):996-9. © FORMATEX 2013 1583