Enhanced Myogenic Responsiveness of Renal
advertisement

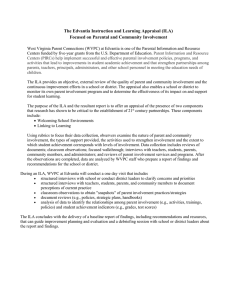
153 Enhanced Myogenic Responsiveness of Renal Interlobular Arteries in Spontaneously Hypertensive Rats Koichi Hayashi, Murray Epstein, and Rodger Loutzenhiser We recently demonstrated that the interlobular artery (ILA) constricts in response to elevating renal arterial pressure (RAP), suggesting that the ILA contributes to renal autoregulation. In the present study, we examined the segmental myogenic responsiveness of the ILA in kidneys from Wistar-Kyoto (WKY) rats and spontaneously hypertensive rats (SHR). The tapered nature of the ILA allowed us to characterize the regional responsiveness, using the basal diameter to define segments as either proximal (greater than 60 fim), intermediate (40-60 pim), or distal (less than 40 pm). At 80 mm Hg, segmental diameters were similar in WKY and SHR arteries (proximal, 76.0±3.1 versus 71.6±3.5 /un; intermediate, 48.2±1.4 versus 48.1±1.7 /im; distal, 30.7±0.9 versus 27.9±13 Aim for WKY and SHR, respectively). In both strains, intermediate and distal segments exhibited graded reductions in diameter as RAP was elevated, whereas proximal segments did not Pressure-induced decrements in the diameters of distal ILA segments were similar in WKY (-24±2%) and SHR (-20±2%;p>0.1). The intermediate ILA of SHR exhibited an augmented myogenic responsiveness, constricting at lower RAP levels and exhibiting greater maximal decrements in diameter at 180 mm Hg (i.e., - 1 9 ±2% and -12±2% for SHR and WKY, respectively; p<0.05). Nifedipine (1.0 fiM) reduced pressureinduced vasoconstriction of intermediate and distal ILA segments by 56 ±11% and 79 ±7%, respectively, in WKY. In contrast, nifedipine completely abolished pressure responses of both segments in SHR kidneys, suggesting a greater involvement of calcium channels in mediating myogenic vasoconstriction of the HA in SHR. In concert, these observations indicate an augmented myogenic reactivity of the intermediate HA segment in SHR and suggest that this adaptation reflects an enhanced activity of calcium channels. (Hypertension 1992; 19:153-160) S ustained hypertension alters the renal excretory response to pressure1 and renal autoregulation.2 We have previously demonstrated that myogenic afferent arteriolar vasoconstriction is reset to higher renal arterial pressure (RAP) levels in spontaneously hypertensive rats (SHR).3 Although the afferent arteriole is primarily responsible for both acute4-5 and chronic6'7 adaptations to elevated RAP, the interlobular artery (ILA) may also contribute to renal autoregulation.8'9 The involvement of the ILA in chronic adaptations of the renal vasculature to hypertension has not been previously examined. From the Nephrology Section and Research Services, Veterans Administration Medical Center, and the Division of Nephrology, University of Miami, School of Medicine, Miami, Fla. Supported by grants from the Department of Veterans Affairs. R.L. is an Established Investigator of the American Heart Association. Address for correspondence: Rodger Loutzenhiser, PhD, Nephrology Section (111C1), Veterans Administration Medical Center, 1201 N.W. 16th Street, Miami, FL 33125. Received January 12, 1990; accepted in revised form October 17, 1991. The diameter of the ILA decreases as the vessel courses from its origin at the arcuate artery to superficial cortical regions. The tapered characteristic of the ILA contributes to a substantial pressure gradient along its length8'9 and may influence its responsiveness to pressure. Luminal pressure measured at the distal, superficial segment is lower than that measured within the aorta8 and is partially, albeit not perfectly, autoregulated.9 Thus, it is possible that the ILA exhibits regional differences in its response to pressure. However, segmental myogenic responses of this vessel have not been previously characterized. Furthermore, the myogenic reactivity of this vessel in normotensive and hypertensive animals has not been compared. In the present study, segmental responses of the ILA to acute elevations in RAP were studied in in vitro perfused hydronephrotic kidneys isolated from normotensive rats (Wistar-Kyoto) and SHR. The effects of the nifedipine on myogenic vasoconstriction of the ILA were also assessed to determine the role of potential dependent calcium channels mediating in this response. 154 Hypertension Vol 19, No 2 February 1992 Methods Animal Preparation Male Wistar-Kyoto (WKY) and stroke-prone SHR (body weight, 120-150 g; Charles River Breeding Laboratories, Wilmington, Mass.) were used as donors of hydronephrotic kidneys. The right ureter was ligated under methoxyflurane (Pitman-Moore, Washington Crossing, N.J.) anesthesia in 6-week-old animals. After 8-10 weeks of chronic unilateral hydronephrosis, when tubular atrophy of the right kidney had progressed to a stage that allowed direct microscopic visualization of the renal microvessels,10 the kidneys were excised and perfused in vitro as described below. On the day of the perfusion study, systolic blood pressures of the conscious donor animals were measured by tail-cuff sphygmomanometry (model KN210-1, Natume, Tokyo). Data were obtained from the mean of at least five measurements. Perfusion of Hydronephrotic Kidneys Donor animals were anesthetized with methoxyflurane. The renal artery of the hydronephrotic kidney was cannulated as described previously.3'11-14 An infusion of warm oxygenated media was initiated during the cannulation procedure. The hydronephrotic kidney was excised and perfused on the stage of an inverted microscope (model K, Nikon, Tokyo) modified to accommodate a heated chamber with a thin glass viewing port on the bottom surface. Kidneys were allowed to equilibrate for at least 30 minutes before initiating the experimental protocols. The kidneys were perfused with a cell-free artificial medium consisting of a Krebs-Ringer bicarbonate buffer containing 5 mM D-glucose, 7.5% bovine serum albumin (Bovuminar, Armour Pharmaceutical Co., Kankakee, 111.), and a complement of amino acids as detailed previously.15 The perfusate was saturated with 95% Oj-5% CO2 and the pH was adjusted to 7.4. The apparatus used to study the hydronephrotic kidneys in vitro is described in detail in previous publications.1113 Kidneys receive media from a pressurized reservoir. The perfusion pressure, monitored at the level of the renal artery, is altered by adjusting a back-pressure-type regulator (model 10BP, Fairchild Industrial Products Co., Winston-Salem, N.C.) controlling the exit of gas from the media reservoir. ILA diameters were measured by computer-assisted image processing as detailed previously.3-11-13-14 Video images of the renal microcirculation were recorded on videocassette and later transmitted to an IBM-AT computer equipped with a video acquisition and display board (model FVG-128, Datacube, Peabody, Mass.). Vessel diameters were estimated from the mean distance between parallel edges of the selected vascular segments. Vessel segments approximately 50 ^,m in length were analyzed. Diameters were measured at 2-4-second intervals for at least 1 DMal: <40fim :40-60ffm Proximal: > 60fnn Arcuata Artery FIGURE 1. Schematic diagram of the interlobular artery (ILA). The ILA is tapered along its length with greatest diameter near the arcuate artery (proximal segment) and the smallest diameter at the terminal portion (distal segment). minute at each RAP. Thus, each diameter was obtained by averaging 15-30 individual measurements. Experimental Protocols Renal microvascular responses were observed as RAP was elevated in 20-mm Hg increments from 80 mm Hg to a maximum of 180 mm Hg. Vessels from 13 WKY and 13 SHR kidneys were studied. To define the regional variations in the responses of the ILA, vessels with diameters in the ranges of 10-30 fim, 30-40 yum, 40-50 nm, 50-60 ^m, 60-80 fim, and greater than 80 fim were grouped for analysis. This analysis indicated that small vessels with basal diameters less than 40 fim responded similarly to pressure. Furthermore, the largest ILA segments (greater than 60 fim) were uniformly unresponsive to elevated pressure (see below). Therefore, to facilitate further analysis, ILAs were classified as either proximal (greater than 60 fim), intermediate (40-60 fim), or distal (less than 40 ^.m) in all subsequent analyses (see Figure 1). The range of basal diameters of the ILAs was similar in WKY (20.7-119.5 fim) and SHR (17.2-93.7 fim). In an additional series of experiments, the ability of nifedipine to inhibit pressure responses of the ILA was examined in both WKY (n=6) and SHR (n = 10) kidneys. Initially, ILA diameters were determined at the RAPs of 80-180 mmHg in the absence of nifedipine. Nifedipine was then administered at a concentration of 1.0 fiM, a dose previously found to completely inhibit myogenic responses of the afferent arteriole.3 After a 10-minute equilibration period, the responses of the same regions of the ILAs were reassessed in the presence of the calcium antagonist. Statistics All data are expressed as the mean±SEM. Data were analyzed by one-way analysis of variance followed when appropriate by application of Student's t test. Changes within experimental groups were subjected to paired analysis. For multiple comparisons within data groups, a value of N*P<0.05 (where TV Hayashi et al Proximal I nt©fTT>0tfflt8 Myogenic Responses of Interlobular Arteries Distal 155 o Decrease 0 -1 In " 10 -j Diameter -10- -20 (%Ch«n9«) -20—I -30 -I I 200-, 20 1 I 40 60 80 100 Basal Diameter (microns) 3(1501.10050 - FIGURE 2. Representative tracings illustrate segmental differences in myogenic reactivity of an interlobular artery (ILA) from a Wistar-Kyoto kidney. As renal arterial pressure (RAP) was increased, the diameter of the proximal segment did not change (left), whereas the intermediate (middle) and distal (right) ILA segments vasoconstricted markedly. Data are plotted as percent changes from basal diameter (Le., at 80 mmHg). represents the number of comparisons) was considered to indicate statistically significant differences. Results Segmental Heterogeneity of the Response of the Interiobular Artery to Pressure On the day of study, systolic blood pressures of conscious donor animals were 139 ±1 mm Hg («=13) in WKY and 205±5 mmHg (n = 13) in SHR QxO.001). Myogenic responsiveness of the ILA exhibited segmental heterogeneity in both WKY and SHR. Figure 2 illustrates representative tracings obtained from an ILA of WKY. To facilitate a comparison of the responses of the three segments, data are expressed as the percent change from basal diameter (i.e., at 80 mm Hg). As depicted, the larger ILA segment (63.8 pm, proximal) maintained its diameter but did not constrict as RAP was increased. In contrast, elevation of RAP elicited vasoconstriction in the two smaller segments. Increasing RAP to 180 mm Hg decreased the diameters of the intermediate and distal segments by 12% (from 50.2 to 44.0 jtm) and 22% (from 32.1 to 25.2 ^m), respectively. To delineate regional differences in the responses of the ILA to pressure, vessel segments were grouped according to their diameters at 80 mm Hg. The results of this analysis are summarized in Figure 3. The decrement in vessel diameter elicited by raising RAP from 80 to 180 mmHg is expressed as the percent change and is plotted as a function of basal diameter. As illustrated, the response of the ILA to pressure increased as basal diameter decreased, suggesting an increase in myogenic reactivity along the FIGURE 3. Line graph shows segmental responsiveness of the interlobular artery (ILA) to pressure in Wistar-Kyoto (o) and spontaneously hypertensive rats (•). Responses of ILA segments observed when renal arterial pressure is elevated from 80 to 180 mm Hg are presented as mean ± SEM of percent change in vessel diameters. Basal vessel diameters (yjn, mean±SEM) are measured at 80 mm Hg. length of the vessel. In WKY, ILA segments smaller than 40 fj,m exhibited prominent vasoconstriction (10-30 fim, -24.9 + 2.6%, n = 12; 30-40 p.m, -23.0±2.1%, n=19), whereas smaller decreases in vessel diameter were observed in larger caliber segments (40-50 fim, -12.6±3.3%, n = 10; 50-60 pm, -12.6+3.2%, n=7; 60-80 nm, -8.4±3.4%, n=9; greater than 80 ^m, -6.6±4.1%, n=5). In SHR, prominent vasoconstriction was observed in vessels with basal diameters ranging from 10 to 60 ^.m (10-30 tun, -21.1+2.0%, H=14; 30-40 fim, -19.5±3.2%, n=9; 40-50 /xm, -19.5±3.2%, n=9; 50-60 -21.2±3.4%, n=8). Segments greater than 60 in diameter did not constrict in response to pressure elevation (60-80 /xm, -1.4±1.3%, n=8; greater than 80 p-m, -1.7±3.7%, n=3) in SHR. Based on these results, ILA segments were categorized as either proximal (greater than 60 fim), intermediate (40-60 ^m), or distal (less than 40 ^m) in subsequent analyses. Figure 4 summarizes pressure responses of proximal ILA segments in WKY and SHR kidneys. At 80 mm Hg, the proximal ILA diameters in SHR (71.6±3.5 fim, n=6) did not differ significantly from that of WKY (76.0±3.1 pm, n=W,p>05). Increasing RAP to 180 mmHg tended to reduce proximal ILA diameters slightly, however, significant changes in vessel diameters were not attained in either strain (WKY, 71.2+4.5 fim,p>0.05; SHR, 70.7+3.8 fim,p>0A). Pressure responses of intermediate ILA segments are summarized in Figure 5. Responsiveness of the intermediate segment to pressure was enhanced in kidneys from SHR. Basal diameters of the intermediate ILA were identical in WKY (48.2 ±1.4 /im, n = l l ) and SHR (48.1 ±1.7 jun,n = 14,/»0.5). At 180 mm Hg, the diameters of intermediate ILAs from SHR kidneys tended to be smaller than those of WKY kidneys (38.7±1.6 ^m and 42.5±1.2 urn, respectively,/? =0.08). When these data were expressed 156 Hypertension Vol 19, No 2 February 1992 Distal Segment Proximal Segment 80 - i 32 - a c 5 o 27 22 - 1 65 - 1 80 100 120 140 160 180 80 Renal Arterial Pressure (mm Hg) FIGURE 4. Line graph shows effects of elevating renal arterial pressure (RAP) on proximal interiobuiar artery (ILA) diameters in Wistar-Kyoto (o) (n=10) and spontaneously hypertensive rats ( • ) (n=6). Vessel diameters (mean±SEM) did not change significantly in response to elevated RAP (compared with diameter at 80 mm Hg) in either strain. as the percent changes from the basal diameter, the vasoconstriction of intermediate segments in SHR (-19.3±2.4%) was found to be significantly greater than that of WKY (-11.5+2.4%, p<0.05). Furthermore, the intermediate segment of SHR exhibited a lower threshold response, manifesting significant vasoconstriction at 100 mm Hg (46.7±1.6 fim, p<0.005). In WKY, significant vasoconstriction of Intermediate segment 48 - i 2 E 38 - 1 I 80 i I I I I 100 120 140 160 180 Renal Arterial Pressure (mm Hg) FIGURE 5. Line graph shows effects of elevating renal arterial pressure (RAP) on diameters of intermediate interiobuiar artery (ILA) segments in Wistar-Kyoto (WKY) (n=ll) and spontaneously hypertensive rats (SHR) (n=14). As RAP was elevated, the intermediate ILA diameters decreased progressively in SHR ( • ) and WKY (o> Intermediate ILA segment of SHR manifested an enhanced response when compared with that of WKY. Results are mean±SEM. *p<0.01 vs. diameter at 80 mm Hg. 100 120 140 160 180 Renal Arterial Pressure (mm Hg) FIGURE 6. Line graph shows effects of elevated renal arterial pressure (RAP) on diameters of the distal interiobuiar artery (ILA) segment in Wistar-Kyoto (o) (n=28) and spontaneously hypertensive rats (•) (n=21). Diameters of the distal ILA segment decreased in a similar fashion as RAP was raised. Results are mean±SEM. *p<0.01 vs. diameter at 80 mmHg. the intermediate ILA was not attained until RAP was elevated to 140 mm Hg (44.1 ±1.3 iim,p<Q.0\). Figure 6 summarizes the vasoconstrictor responses to pressure of distal ILA segments in WKY and SHR kidneys. Basal diameters of this segment in SHR (27.9±1.3 /im, n=2l) did not differ from that in WKY (30.7 ±0.9 Aim, n=28,p>0.05). Similarly, at all levels of RAP, the vasoconstrictor responses did not differ between the two strains (p>0.l). Thus, in both WKY and SHR, significant vasoconstriction was observed at 100 mm Hg (WKY, 28.9 ±1.0 fim,p< 0.001; SHR, 26.7±1.2 /xm,/?<0.001), and further increases in RAP elicited pressure-dependent vasoconstriction of this segment. At 180 mm Hg, the diameters of the distal segment were 23.5+1.0 Aim in WKY (/?<0.001) and 22.4±1.1 fim in SHR (p<0.001), corresponding to 23.6±1.8% and 19.9±1.7% decrements from the basal diameter, respectively (p>0.1). Thus, the distal segment of the ILA exhibited identical pressure responsiveness in the two strains. To further facilitate comparison of the segmental myogenic responsiveness of the ILA in WKY and SHR, data from proximal, intermediate, and distal segments in kidneys from each strain are expressed as percent changes from the basal diameter in Figure 7. Distal LLA segments constricted prominently in both strains, whereas proximal LLA segments did not exhibit significant vasoconstriction in either strain. The response of the intermediate segment clearly differed in WKY and SHR kidneys. In WKY, the response of the intermediate ILA segment was significantly less than that of the distal segment (120 mm Hg, -4.5±2.1% versus -13.0±1.4%,p<0.005; 140 mm Hg, -8.1±2.4% versus -17.6 + 1.7%, /?<0.005; 160 mmHg, -10.4±2.7% versus -21.1±1.9%, /?<0.005; 180 mmHg, -11.5±2.4% versus -23.6±1.8%,/7<0.001; intermediate and distal segments, respectively). In Hayashi et al Myogenic Responses of Interlobular Arteries WKY o 157 SHR - Prox Prox ~ -10 a -\ Inter I If'0 35 £ -20 H Dtat -30 - 1 -30 - 1 I I 80 I I I I 1 100 120 140 160 180 I I I I I 80 100 120 140 160 180 Reno) Arterial Pressure (mm Hg) Renal Arterial Pressure (mm Hg) FIGURE 7. Line graphs show comparison of the segmental myogenic responsiveness in Wistar-Kyoto (WKY) (left panel) and spontaneously hypertensive rat (SHR) (right panel) kidneys. In both strains, the distal interlobular artery segment (Dist; A) vasoconstricted markedly, whereas the diameters of the proximal segment (Prox; m) decreased only modestly. In WKY, the responses of the intermediate segment (Inter, o) were less than those of the distal segment (left panel). In SHR, the responses of the intermediate segments were greatly augmented (right panel). Thus, in SHR the magnitude of myogenic vasoconstriction of the intermediate segment was identical to that of the distal segment. Results are mean±SEM. contrast, the responses of the intermediate ILA from SHR kidneys was identical to that of the distal segment at every level of RAP (p>0.l). Effects of Nifedipine on Pressure-Induced Interlobular Artery Vasoconstriction The effects of nifedipine on myogenic responses of intermediate and distal ILA segments were assessed by measuring the responses before and after adminis- Intermediate Segment WKY Distal Segment SHR WKY So #NHMIplne SHR " N ^ ^ Nifedipine % "S" -10 • II es "S--10 E o) I & -20-I Control 2 5 • Control Q £ O -20-30 J Control 80100120140160180 80100120140160180 Renal Arterial Pressure (mm Hg) FIGURE 8. Line graphs show effects of1.0 tiM nifedipine on the pressure-induced vasoconstriction of the intermediate interlobular artery (ILA) segments in Wistar-Kyoto (WKY) (left panel) and spontaneously hypertensive rat (right panel) kidneys. In WKY, nifedipine greatly attenuated myogenic responses; however, the intermediate ILA vasoconstricted significantly in the presence of the calcium antagonist. In contrast, nifedipine completely abolished myogenic vasoconstriction in SHR. *Points at which diameters differed (p<0.01) compared with basal diameter. fPoints at which responses (percent change) differed between nifedipine and control (p<0.05). Data are mean±SEM of percent change. Open symbols, control; closed symbols, nifedipine. - 3 0 •> 80100120140160180 80100120140160180 Renal Arterial Pressure (mm Hg) FIGURE 9. Line graphs show effects of nifedipine on the pressure-induced vasoconstriction of distal interlobular artery segments in Wistar-Kyoto (WKY) (left panel) and spontaneously hypertensive rats (SHR) (right panel). Administration of 1 fiM nifedipine partially prevented the pressure-induced vasoconstriction of this segment in WKY. In contrast, nifedipine completely inhibited the pressure response in SHR kidneys. *Points at which diameters differed (p<0.01) compared with basal diameter. fPoints at which responses (percent change) differed between nifedipine and control (p<0.05). Data are mean±SEM of percent change. Open symbols, control; closed symbols, nifedipine. 158 Hypertension Vol 19, No 2 February 1992 tration of the calcium antagonist in WKY and SHR kidneys. The results of these studies are summarized in Figures 8 and 9. In WKY, nifedipine only partially inhibited myogenic responses in each segment. Thus, elevating RAP from 80 to 180 mmHg elicited a 14.4 ±2.7% decrement in the intermediate ILA diameter (i.e., from 50.0±1.5 to 43.0±2.2 yon, p<0.001, n=l2, Figure 8, left panel). After 1 fiM nffedipine, this vessel exhibited a partial response, manifesting a 4.6±1.2% decrement in diameter at 180 mm Hg (i.e., from 49.6±1.4 to 47.4±1.6 /xm,p<0.005). This corresponds to a 56±11% inhibition of myogenic vasoconstriction of the intermediate ILA in WKY kidneys. The distal ILA segment constricted by 27.6±2.4% at 180 mmHg (i.e., from 31.2+2.0 to 22.6±1.7 urn, /?<0.001, n=9) in the absence of nifedipine and by 6.0±2.2% in the presence of nifedipine (Figure 9), corresponding to a 79 ±7% inhibition of myogenic responsiveness in this segment. The intermediate ILA segment in SHR exhibited an enhanced response to nifedipine (Figure 8, right panel). In the absence of nifedipine, the intermediate ILA segment manifested a 20.1 ±2.7% decrement in diameter at 180 mmHg (from 45.8±2.0 to 36.6+1.9 jan, /?<0.001, n=l). After nifedipine administration, increasing RAP resulted in a passive distention of this segment, increasing diameter to 120±9% (i.e., from 45.7+2.1 fim at 80 mm Hg to 47.0±2.0 /im at 180 mmHg, p=0.08, n=7). Thus, nifedipine completely inhibited myogenic vasoconstriction of this segment. Myogenic vasoconstriction of the distal ILA segment was also inhibited by nifedipine in kidneys from SHR. In the absence of nifedipine, the distal ILA exhibited a 73.1±2.1% decrease in diameter (i.e., from 30.3+1.9 to 23.1±1.7 ^m,p<0.001, n=8) in kidneys from SHR (Figure 9). After nifedipine administration, the diameter of distal ILA segments did not change in response to elevation of RAP, exhibiting neither a decrease nor a passive distention (Figure 9). Discussion Renal vascular resistance (RVR) is increased in both human and experimental hypertension.6-7'16'17 To the extent that vasodilators reverse the increased RVR associated with hypertension, the increase in resistance may be viewed as reflecting a functional adaptation of the renal circulation.16"18 Afferent arteriolar resistance is a principal determinant of RVR19 and is elevated in hypertensive animals.6'720 The contribution of the ILA to altered renal hemodynamics in hypertension has not been fully defined. The ILA, originating at the arcuate artery near the corticomedullary junction and terminating at the superficial cortex, is anatomically well suited to regulate the arterial pressure gradient within the renal cortex. The ELA is tapered along its length, varying in diameter from more than 90 jim near the arcuate artery to less than 30 fim at the terminal segment. Intraluminal pressure at the proximal portion is directly related to systemic blood pressure,21 whereas that within the distal segment is partially autoregulated.8-9 The seg- mental responsiveness of the ILA to pressure, however, has not been previously examined. Furthermore, the effects of hypertension on the myogenic responsiveness of this vessel have not been investigated. Segmental Differences in Pressure Response of Interiobular Artery in Spontaneously Hypertensive Rats The present study clearly demonstrates that myogenic reactivity of the ILA exhibits a regional heterogeneity, increasing in magnitude from proximal to distal segments (Figure 2). Although we cannot ascertain fully the mechanisms responsible for the variation in myogenic reactivity along the ILA, it is likely that vessel diameter itself is a contributing factor. At increased pressures, myogenic vasoconstriction would be opposed by an increased distending force exerted on the vessel wall. Since wall tension directly relates to vessel diameter (LaPlace: wall tension=pressure x radius), the distending force, countervailing the myogenic constrictor response, would be greater in larger vessels. The role of the HA in maintaining renal autoregulation has not been established. Previous investigators have suggested that this vessel contributes to RVR.8-9-22 T0nder and Aukland8 observed the intraluminal pressure of the ILA in the outer cortex to be substantially less than that of the aorta. Similarly, Kallskog et al9 demonstrated that changes in renal perfusion pressure result in much smaller changes in the pressure within the superficial segment of the ILA. Although the major contribution of the afferent arteriole is clearly acknowledged, these findings indicate that the ILA also contributes importantly to autoregulatory responses. Previous studies have not determined the relative contributions of myogenic responses of proximal versus distal segments of the ILA. Our current findings indicate that the distal and intermediate segments of the ILA contribute more to autoregulation than the proximal portion of this vessel. Altered Pressure Response of the Interiobular Artery in Spontaneously Hypertensive Rats Hypertension is associated with alterations in the renal response to pressure, including a shift in renal autoregulation.2 In previous studies with the isolated perfused hydronephrotic kidney, we demonstrated that pressure-induced afferent arteriolar vasoconstriction is reset to higher pressure levels in SHR.3 In the present study, alterations in the myogenic responsiveness of the intermediate segment of the ILA were observed to occur in this same model. In contrast to the afferent arteriole, however, myogenic responses of intermediate ILA segments were enhanced, exhibiting both a lower threshold pressure (Figure 5) and a greater maxima] response (Figure 7). Thus, the nature of the adaptations of the afferent arteriole and ILA in SHR exhibits opposite characteristics. Furthermore, the adaptive changes in myogenic reactivity of the ILA were restricted to the intermediate segment of this Hayashi et al Myogenic Responses of Interlobular Arteries vessel: distal and proximal ILA segments responded similarly in SHR and WKY. The reasons for the differing adaptive responses of the intermediate ILA and afferent arteriole of SHR cannot be discerned from the present study. An enhanced vasoconstriction of the ILA could conceivably reduce the increment in transmural pressure sensed by downstream afferent arterioles, thereby resulting in a shift in afferent arteriolar responses to higher renal arterial pressures. Although this formulation remains a possibility, we did not observe alterations of pressure-induced afferent arteriolar responses to be restricted to those vessels arising downstream from the intermediate ELA. Furthermore, the response of RVR to pressure was also shifted to higher pressures in SHR, suggesting a correlation with the altered responsiveness of the afferent arteriole.3 Thus, we do not believe that the shift in afferent arteriolar responsiveness is due to increased ILA vasoconstriction. Rather, we suggest that the altered responsiveness of the intermediate ILA and afferent arteriole in SHR reflects different functional adaptations of these two vessel types to hypertension. Our current observations of the actions of nifedipine support the view that differing mechanisms may underlie the adaptations of the ILA and afferent arteriole in SHR. We previously demonstrated that nifedipine has identical effects on myogenic vasoconstriction of afferent arterioles in WKY and SHR, completely abolishing afferent arteriolar responses in both strains at 1.0 jtM and exhibiting an identical IQo.3 In contrast, however, the effects of nifedipine on myogenic responses of the ILA differed in SHR and WKY. At 1.0 jtM, nifedipine only partially inhibited myogenic vasoconstriction of the ILA in WKY kidneys but completely eliminated the pressure responses in SHR. This finding suggests an alteration in excitation-contraction coupling of the ILA in SHR. Since afferent arteriolar responses to nifedipine were identical in WKY and SHR,3 it follows that differing cellular mechanisms underlie the adaptations of these two vessel types to hypertension. The observation that 1.0 fiM nifedipine inhibited myogenic ILA responses to a greater extent in SHR than WKY suggests an augmented calcium channel activity in the ILA of this strain. Although we have no direct evidence to support this interpretation, it is of interest that Hermsmeyer and Rusch23-24 observed smooth muscle cells cultured from SHR to exhibit a greater ratio of L-type versus T-type calcium channels than cells cultured from WKY, suggesting an alteration in calcium channel expression in vascular smooth muscle of this strain. Studies by Steele and Challoner-Hue25 also suggest that preglomerular resistance vessels of SHR kidneys exhibit alterations in calcium channel activity; they observed that isolated perfused kidneys from SHR manifested an exaggerated response of glomerular filtration rate to administration of verapamil in comparison with kidneys isolated from WKY. These authors suggested that 159 the renal vasculature of the SHR exhibits an enhanced calcium channel activity. The present observations support and extend these interpretations and suggest that the ILA represents a potential site of augmented calcium channel activity in the SHR. Finally, the adaptation of the intermediate ILA segment in SHR kidneys may be relevant to the pattern of pathological findings in kidneys from this hypertensive model. In SHR kidneys, glomerular injury is most prevalent in juxtamedullary nephrons, whereas pathological changes are much less apparent in superficial glomeruli.26-27 In addition, Feld et al26 demonstrated that urinary protein excretion is elevated in SHR, whereas albumin clearance in superficial nephrons appears normal, suggesting that proteinuria derives mainly from juxtamedullary nephrons. Furthermore, the distribution of the glomerular injury in SHR also corresponds to differences in intrarenal hemodynamics. Juxtamedullary glomeruli manifest a higher single nephron glomerular filtration rate in SHR than in WKY,28 presumably due to elevated glomerular capillary pressure. In contrast, in superficial glomeruli both glomerular capillary pressure and single nephron glomerular filtration rate are similar in SHR and WKY,6>7 indicating an increased preglomerular resistance in SHR. Previously, it has been assumed that an increased afferent arteriolar resistance alone prevented an increase in superficial glomerular capillary pressure in SHR kidneys.6-7'20 The results of the present study indicate that the intermediate ILA segment exhibits an augmented myogenic response that may also contribute to the increased preglomerular resistance, especially of superficial glomeruli. It is tempting to speculate that the enhanced vasoconstriction of the intermediate ILA acts in concert with afferent arteriolar vasoconstriction to prevent or attenuate elevated glomerular capillary pressure in superficial nephrons. This postulate concerning the possible pathophysiological consequences of the myogenic response of the ILA is offered with a number of caveats. We have not demonstrated that the augmented ILA vasoconstriction reduces the pressure within downstream vessels nor have we shown that the altered ILA responses occur to a similar extent in nonhydronephrotic kidneys. Gearly, further studies are required to establish the role of the ILA in regulating the arterial pressure gradient within the renal cortex. In conclusion, the present study demonstrates that myogenic reactivity of the ILA to pressure varies along the length of the vessel, with greater responses occurring in the more distal segments. In SHR, the myogenic responsiveness of the intermediate ILA segment is markedly augmented, suggesting an adaptation in this hypertensive model that could differentially influence pressures in superficial and juxtamedullary nephrons. Finally, pressure-induced contractions of the ILA from SHR were inhibited by 1.0 /AM nifedipine to a greater extent than those of WKY rats, suggesting that the enhanced myogenic reactivity of this vessel 160 Hypertension Vol 19, No 2 February 1992 reflects an alteration in calcium channel activity associated with the hypertensive state. Acknowledgment We gratefully acknowledge the contribution of Hayley Forster in the statistical analysis of these data and preparation of the manuscript. References 1. Roman RJ: Altered pressure-natriuresis relationship in young spontaneously hypertensive rats. Hypertension 1987;9(suppl III):III-130-ni-136 2. Iversen BM, Sekse I, Ofctad J: Resetting of renal blood flow autoregulation in spontaneously hypertensive nts.AmJ Physiol 1987;252:F480-F486 3. Hayashi K, Epstein M, Loutzenhiser R: Pressure-induced vasoconstriction of renal microvessels in normotensive and hypertensive rats: Studies in the isolated perfused hydronephrotic kidneys. Ore Res 1989;65:1475-1484 4. Navar LG, Marsh DL, Blantz RC, Hall J, Ploth DW, Nasjletti A; Intrinsic control of renal hemodynamics. Fed Proc 1982;41: 3022-3030 5. 0ien AH: A mathematical analysis of the myogenic hypothesis with special reference to autoregulation of renal blood flow. Ore Res 1983;52:241-252 6. Arendshorst WJ, Beierwaltes WH: Renal and nephron hemodynamics in spontaneously hypertensive rats. Am J Physiol 1979;236:F246-F251 7. Azar S, Johnson MA, Scheinman J, Bruno L, Tobian L: Regulation of glomerular capillary pressure and filtration rate in young Kyoto hypertensive rats. Clin Sci 1979;56:203-209 8. T0nder KJH, Aukland K: Interlobular arterial pressure in the rat kidney. Renal Physiol 1979/80;2:214-221 9. KaUskog 0 , Lindbom LO, Ulfendahl HR, Wolgast M: Hydrostatic pressures within the vascular structures of the rat kidney. Pflugers Arch 1976;363:205-210 10. Steinhausen M, Snoei H, Parekh N, Baker R, Johnson PC: Hydronephrosis: A new method to visualize vas afferens, efferens, and glomerular network. Kidney Int 1983;23:794-806 11. Loutzenhiser R, Hayashi K, Epstein M: Atrial natriuretic peptide reverses afferent arteriolar vasoconstriction and potentiates efferent arteriolar vasoconstriction in the isolated perfused rat kidney. / Pharmacol Exp Ther 1988;246:522-528 12. Loutzenhiser R, Hayashi K, Epstein M: Calcium antagonists augment glomerular filtration rate (GFR) of angiotensin Il-vasoconstricted isolated perfused rat kidneys (IPRK) by dilating afferent but not efferent arterioles (abstract). / Cardiovasc Pharmacol 1988;12(suppl 6):S149 13. Loutzenhiser R, Epstein M, Hayashi K, Horton C: Direct visualization of the effects of endothelin on the renal microvasculature. Am J Physiol 1990;258:F61-F68 14. Loutzenhiser R, Hayashi K, Epstein M: Divergent effects of KQ-induced depolarization on afferent and efferent arterioles. Am J Physiol 1989;257:F561-F564 15. Epstein M, Flamenbaum W, Loutzenhiser R: Characterization of the renin-angiotensin system in the isolated perfused rat kidney. Renal Physiol 1980;2:244-256 16. Yokoyama S, Kaburagi T: Clinical effects of intravenous nifedipine on renal function. / Cardiovasc Pharmacol 1983;5: 67-71 17. Hsu C-H, Slavicek JH, Kurtz TW: Segmental renal vascular resistance in the spontaneously hypertensive rat. Am J Physiol 1982;242:H961-H966 18. Hollenberg NK, Adams DF, Solomon H, Chenitz WR, Burger BM, Abrams HL, Merrill JP: Renal vascular tone in essential and secondary hypertension: Hemodynamic and angiographic responses to vasodilators. Medicine 1975^54:29-44 19. Blantz RC: Segmental renal vascular resistance: Single nephron. Annu Rev Physiol 1980;42:573-588 20. Dilley JR, Stier CT, Arendshorst WJ: Abnormalities in glomerular function in rats developing spontaneous hypertension. Am J Physiol 1984;246:F12-F20 21. Stumpe KO, Lowitz HD, Ochwadt B: Function of juxtamedullary nephrons in normotensive and chronically hypertensive rats. Pflugers Arch 1969;313:43-52 22. Ofstad J, Iversen BM, Merkrid L, Sekse I: Autoregulation of renal blood flow (RBF) with and without participation of afferent arterioles. Acta Physiol Scand 1987;130:25-32 23. Hermsmeyer K, Rusch N: Calcium channel alterations in genetic hypertension. Hypertension 1989;14:453-456 24. Rusch NJ, Hermsmeyer K: Calcium currents are altered in the vascular muscle cell membrane of spontaneously hypertensive rats. Ore Res 1988;63:997-1002 25. Steele TH, Challoner-Hue L: Glomerular response to verapamil by isolated spontaneously hypertensive rat kidney. Am J Physiol 1985;248:F668-F673 26. Feld LG, Van Liew JB, Galaske RG, Boyian JW: Selectivity of renal injury and proteinuria in the spontaneously hypertensive rat. Kidney Int 1977; 12:332-343 27. Olson JL, Wilson SK, Heptinstall RH: Relation of glomerular injury to preglomerular resistance in experimental hypertension. Kidney Int 1986;29:849-857 28. Bank N, Alterman L, Aynedjian HS: Selective deep nephron hyperfutration in uninephrectomized spontaneously hypertensive rats. Kidney Int 1983;24:185-191 KEY WORDS • arteries • vasoconstriction • microcirculation • essential hypertension • calcium channel bloclters • ion channels • spontaneously hypertensive rats