Anthem Network Update: Healthcare Policy & Program Changes
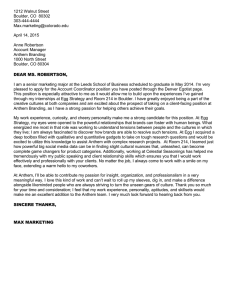
advertisement

December 2015 In this issue Page Announcements – ICD-10 update ICD indicator required on paper claim forms 3 AIM alerts Reminder of the most recent updates to the Cancer Care Quality Program 4 New program highlights affordable choices for Virginia members 5 Enhancements to AIM Clinical Appropriateness Guidelines for Advanced Imaging – effective February 22, 2016 7 New precertification requirements for certain radiation therapy services begins March 1, 2016 9 Coverage and clinical guideline update REMINDER: Specialty pharmacy site-of-service reviews began November 1 11 Business update 1 of 41 New regional vice president and senior clinical officer in Virginia 13 Updates to Blue Physician Recognition Program 13 Incentive opportunity for physicians treating patients with Anthem plans purchased on or off the exchange 14 Misrouted protected health information (PHI) 16 HEDIS® 2015 results are in for our PPO and HealthKeepers lines of business 16 Enhanced Personal Health Care program offers greater value for members and greater financial opportunity for PCPs 19 Enhanced Personal Health Care: Referral providers benefit by improving and controlling costs 20 Improving your patients’ health care experience 21 Survey says… Patients see room for improvement with physician care 21 Respiratory antibiotic use performance 23 We believe in continuous improvement 25 Case Management Program 25 Coordination of care 26 Important information about utilization management 27 Members’ rights and responsibilities 28 anthem.com Important phone numbers VAPENABSNL (12/15) In this issue, continued Page Business update, continued Clinical practice and preventive health guidelines available on the Web GeoBlue: BlueCard provider outreach 28 28 Behavioral health update Documentation and reporting guidelines for applied behavior analysis (ABA) and treatments for Autism Spectrum Disorder 29 Health care reform update (including health insurance exchange) Refer to anthem.com for information about health care reform and the exchange in 2016 29 eBusiness Receive e-mail notifications via our Network eUPDATE Updated contact information for ERA and EFT registration 30 30 Medicaid information Attention Medicaid Providers: ICD-10 coding for diabetic complications Coverage guidelines and Clinical Utilization Management Guidelines update Update: Home and hydration therapy medical necessity reviews Update: Scoliosis and spinal deformity medical necessity reviews Home health and outpatient therapies will require separate authorizations 32 32 32 33 33 Medicare-Medicaid plan update CDC predicts another moderately severe flu season predominated by influenza A (H3N2) ICD-10 coding supports MMP providers in reporting more clinical details for diabetic complications 33 34 Medicare information Avoid denials of Medicare Advantage diagnostic claims by completing item 20 (CMS-1500) correctly – Individual membership only 34 Please include modifiers to help ensure accurate payment 35 Oxygen DME precertifications will be reduced in 2016 35 Anthem to review ER level 5 professional claims 35 Register for imaging site scores by March 1, 2016, to avoid unnecessary line-item denials 36 More $0 copay medications available to Medicare Advantage members with chronic conditions 37 Avastin for ophthalmic use – C9257 can be billed in office setting for network providers 37 Enhanced reimbursement available for certain Part B injectable drugs 37 Anthem place of service claims adjudication mirrors CMS guidelines 38 Anthem individual Medicare Advantage plan names changing for 2016 38 Keep up with Medicare Advantage news at Important Medicare Advantage Updates 38 Pharmacy update CVS/specialty is exclusive in-network specialty pharmacy for Anthem members with medical benefit coverage for specialty medications 39 Searchable Formulary Tool gives providers easier access to formulary/drug list information 40 Pharmacy information available on anthem.com 41 December 2015 2 of 41 Announcements – ICD-10 update ICD indicator required on paper claim forms With the implementation of ICD-10 on October 1, 2015, it may be appropriate to report either ICD-9 or ICD-10 codes depending upon the dates of service. Paper claim forms have an ICD indicator that identifies the ICD code set being reported on the claim. Anthem Blue Cross and Blue Shield is requiring the ICD indicator field be populated on paper claim forms. Claims will be rejected if the ICD indicator field is not populated. This requirement applies to both the UB-04 and CMS-1500 claim forms. UB-04 form (also known as the CMS-1450 form) – The ICD indicator is Field 66. (also known as the Diagnosis and Procedure Code Qualifier) CMS-1500 form version 02/12 – The ICD indicator is Box 21. (Reminder: We only accept the 02/12 form version) Providers must enter the qualifier code that denotes the version of the ICD code set being reported on the claim. Indicator Code Set 9 ICD-9 diagnosis codes and/or procedure codes 0 ICD-10 diagnosis codes and/or procedure codes December 2015 3 of 41 AIM alerts (Information regarding Anthem’s implementation of AIM Specialty Health ® initiatives) Reminder of the most recent updates to the Cancer Care Quality Program Attention Oncologists and Hematologists As a reminder, Anthem Blue Cross and Blue Shield’s Cancer Care Quality Program ("Program"), a quality initiative, provides participating physicians with evidence-based cancer treatment information that allows them to compare planned cancer treatment regimens against evidence-based clinical criteria. The Program also identifies certain evidence-based Cancer Treatment Pathways ("Pathways"). Participating physicians who are in-network for the member's benefit plan are eligible to participate in the Program and for enhanced reimbursement if an appropriate treatment regimen is ordered that is on Pathway. AIM Specialty Health® (AIM), a separate company, administers the Program on behalf of Anthem. Effective December 1, 2015, Anthem added the following cancer treatment Pathways for the Cancer Care Quality Program. New Pathways added to the Program include: Pathways for gastric and esophageal cancers Pathways for head and neck cancers Effective January 1, 2016, the following Pathways are moving from “on” Pathway to “off” Pathway status: Fludarabine+cyclophosphamide+mitoxantrone+rituximab (FCMR) for follicular lymphoma, second and subsequent lines of therapy Rituximab for chronic lymphocytic leukemia (CLL), first line therapy This means that providers will not be eligible for an enhanced reimbursement when these regimens are prescribed. This does not restrict the use of these regimens for members when clinically appropriate, and claims will be adjudicated in accordance with the members’ benefit plans. The Pathways developed for this Program are intended to support quality cancer care. To access the full Pathways document, go online to Ca nce rCare Qu alit yProgram. com, our dedicated provider website. Note: Participating physicians who are in-network for the member's benefit plan are eligible to participate in the Program and for enhanced reimbursement if an appropriate treatment regimen is ordered that is on Pathway. December 2015 4 of 41 New program highlights affordable choices for Virginia members Beginning January 1, 2016, Anthem Blue Cross and Blue Shield in Virginia will launch the Anthem Imaging Shopper, Anthem Sleep Shopper and Anthem Surgical Shopper programs to help members compare facility costs on computed tomography (CT) imaging, magnetic resonance imaging (MRI) and in-lab sleep studies. Administered in partnership with AIM Specialty Health® (AIM), the program will also include many surgical procedures, such as colonoscopy, endoscopy and knee and shoulder arthroscopy. The programs are available to all fully insured members and some self-funded (administrative services only or ASO) groups who have selected the program for their members. The program does not apply to the following plans: The Blue Cross and Blue Shield Service Benefit Plan (also known as the Federal Employee Program or FEP); plans purchased on or off the Health Insurance Marketplace (also called the exchange); Anthem HealthKeepers Plus (Medicaid); Medicare Advantage, Medicare-Medicaid Duals Demonstration or Medicare Supplement plans. The following programs will be offered, and program highlights are included below: Anthem Imaging Shopper Anthem Sleep Shopper (excludes ASO) Anthem Surgical Shopper Anthem Imaging Shopper The Anthem Imaging Shopper program involves proactive outreach to certain Anthem members who are eligible for the program to provide information about imaging costs to help the members select an imaging provider. While most members go to locations recommended by their physicians, these members may not realize that their out-ofpocket costs may vary, depending on where they receive imaging service(s). In addition, according to feedback we have received, most members are open to receiving cost information if it may help them reduce their cost share. As a result, when we receive precertification requests for certain MRI, magnetic resonance angiography (MRA), CT and/or computed tomography angiography (CTA) services, we will call the members and give them information so they understand the choices available to them. During this outreach, members may have an opportunity to reduce their health care expenses by selecting lower-cost providers or locations. This is a voluntary program. Members will not be denied access to services if they do not choose the lower-cost option. Our goal is simply to give our members information to make informed choices about their health plan benefits. Note: Our member outreach will exclude pediatric and oncology cases. Anthem Sleep Shopper Did you know that a sleep study can cost members as much as $2,500 depending on where they live and where they have services performed? December 2015 5 of 41 While most members go to the sleep study facility or lab recommended by their physicians, our members may not realize that their out-of-pocket costs may vary depending on where they receive the service(s). In addition, feedback from our members indicates that most are open to receiving information that could help them save 10 to 15 percent of their cost share. Anthem’s Sleep Shopper program includes proactive outreach to members with key information on sleep testing facilities when an in-lab (PSG), titration, split-night, multiple sleep latency test (MSLT) or maintenance of wakefulness test (MWT) is requested by their physician. Members may have an opportunity to reduce their health care expenses by selecting a lowercost provider. This is a voluntary program. Members will not be denied access to services if they do not choose a lower-cost option. As before, our goal is simply to provide members with information to make informed choices about their health plan benefits. Note: Our member outreach will exclude pediatric cases. Anthem Surgical Shopper Program This new program highlights affordable choices in surgical procedures. Surgical procedures included are: Colonoscopy- screening, biopsy, and lesion removal Endoscopy – Upper GI with Biopsy Arthroscopic ACL Repair Knee Arthroscopy with Cartilage Repair Shoulder Arthroscopy Shoulder Arthroscopy with Rotator Cuff Repair How the program works: The ordering or servicing provider may contact AIM when your patient requires one of the above surgical procedures. Once AIM is notified, aggregate surgical facility cost information will be shared with you and your eligible patient to help select a lower cost option. The range of approximate cost information is based on Anthem’s historical claims data for contracted providers for the various services in scope. This data is updated twice per year. You may contact AIM in one of two ways: Online through ProviderPortalSM at www.aimspecialtyhealth.com/goweb Via telephone at (800) 554-0580 or by using the number displayed on the back of the member ID card Claims will not be denied for failure to inform AIM of these services. This is a voluntary program. Members will not be denied access to services if they do not choose a lower-cost option. As always, our goal is simply to provide members with information to make informed choices about their health plan benefits. December 2015 6 of 41 In addition to the above services listed under the surgical shopper program, members may call (or go online via the “Estimate Your Cost” tool) to obtain cost information for the following procedures: Cataract removal Carpal tunnel repair CT scans Ultrasounds MRI scans Bariatric surgery Labor and delivery Hysterectomy Registration with Optinet ensures your provider data is accessible for these programs You must register with Optinet to ensure your provider information is accessible for these shopper programs. Online registration is available via AIM’s ProviderPortalSM at www.providerportal.com and AIM Specialty Health site via the Availity Web Portal at www.availity.com. A checklist and interactive tutorial are available in the AIM portal to assist you in completing your registration. Be sure to select “Submit” each time you make an update, or the survey will show as incomplete. For technical assistance in completing your registration, call AIM toll free at 800-252-2021. For general questions about registration process, please reference the AIM FAQs and other materials available on AIM’s ProviderPortalSM at www.providerportal.com and AIM Specialty Health site via the Availity Web Portal at www.availity.com. Should you have any questions about Optinet registration or any of these shopper programs, please contact your Anthem network manager. Enhancements to AIM Clinical Appropriateness Guidelines for Advanced Imaging – effective February 22, 2016 On February 22, 2016, the following changes to the AIM Clinical Appropriateness Guidelines for Radiology, Oncologic Positron Emission Tomography (PET), and Cardiology will become effective. A summary of these changes is provided on the next page. December 2015 7 of 41 Radiology guidelines MRI and CT o Expanded list of “red flag” indications for headache evaluation and added a requirement for conservative therapy in low-risk patients o Developed comprehensive new criteria for venous sinus thrombosis based on risk factors MRI/MRA or CT/CTA o CT Neck (soft tissue) and CT Chest o Developed new criteria for headache evaluation for appropriate simultaneous imaging Added new requirement of short course conservative therapy for low-risk patients with hoarseness CT Chest o Developed new criteria for immunosuppressed patients with persistent pneumonia o Aligned pulmonary nodule criteria with the Fleischner Society guidelines MRI Pelvis o Developed new criteria for sports hernia after sufficient initial evaluation and failed conservative management o Revised criteria for advanced imaging in low risk prostate cancer and in the surveillance of gynecologic malignancy MRI Upper and Lower Extremity o Expanded criteria for suspected occult fractures at high-risk sites following non-diagnostic radiographs Oncologic PET guidelines Clarified language for surveillance PET imaging Clarified PET requirement for breast cancer to include invasive disease Expanded thyroid cancer to include well-differentiated follicular subtype Replaced “not covered” with “not medically necessary” December 2015 8 of 41 Cardiology guidelines Revised cardiac imaging criteria for management of patients with Kawasaki disease to align with published literature. Clarified appropriate frequency of echocardiography in children with established congenital heart disease. For younger children with complex congenital heart disease, evaluation based on symptoms is difficult. Therefore, the guideline has been liberalized to allow more frequent echocardiography in this cohort. Clarified language to reduce variability of guideline interpretation based on user feedback. If you have any questions or comments regarding these enhancements to the guidelines, please contact AIM via email at aim.guidelines@aimspecialtyhealth.com. Click here to access and download a copy of the current guidelines. New precertification requirements for certain radiation therapy services begins March 1, 2016 On March 1, 2016, Anthem Blue Cross and Blue Shield and affiliate HealthKeepers, Inc. are expanding our Radiation Therapy Program to require precertification of: Image Guided Radiation Therapy (IGRT). Fractions (also referred to as units) for breast and bone metastases for covered individuals getting External Beam Radiation Therapy (EBRT) or Intensity Modulated Radiation Therapy (IMRT). Special treatment procedure and special physics consult (CPT® codes 77470 and 77370) (e.g., total body irradiation, hemibody radiation, or endocavitary irradiation and special medical radiation physics consultation). AIM Specialty Health® (AIM®), a separate company, administers the Radiation Therapy Program on behalf of Anthem and HealthKeepers, Inc. A complete list of CPT codes requiring precertification is available on the Point of Care preauthorization inquiry via the Availity Web Portal or the actual guidelines for the listing. Effective March 1, 2016, the newly added CPT codes under the expanded Radiation Therapy Program include: December 2015 9 of 41 IGRT IMRT EBRT Special Treatment (e.g., total body irradiation, hemibody radiation, per oral, or endocavitary irradiation) Special medical radiation physics consultation CPT Code G6001 G6002 G6017 77387 77014 G6015 or 77385-6 77427 G6003-6 or 77402 G6007-10 or 77407 G6011-14 or 77412 77427 77470 77370 All Anthem local members who currently require precertification for non-emergency outpatient radiation therapy are included in this program. For Anthem in Virginia and HealthKeepers, Inc., these precertification requirements do not apply to the following: Blue Cross and Blue Shield Service Benefit Plan also known as the Federal Employee Program® (FEP). Medicare Advantage and Medicare Supplement plans. Department of Corrections. National Accounts. Anthem HealthKeepers Plus/FAMIS plans (Medicaid). Anthem HealthKeepers Medicare-Medicaid Plan or MMP. [Members are enrolled in both Medicare and Medicaid under the Commonwealth Coordinated Care Plan, also known as the Duals Demonstration (“Demonstration”) Program.] Members with Anthem as secondary coverage. Unicare and HealthLink. Determine if precertification is needed for an Anthem or HealthKeepers, Inc. member by clicking the “Coverage & Clinical UM Guidelines, and Pre-Cert Requirements” link on anthem.com or by calling the precertification phone number printed on the member’s ID card. December 2015 10 of 41 Starting February 22, 2016, ordering physicians may submit a precertification request for these additional requirements to AIM through the AIM ProviderPortalSM (available 24/7 to process orders in real-time), through the Availity Web Portal or by calling the AIM call center toll free at 1-866-789-0158 (weekdays, 8 a.m. to 5 p.m. ET). Note: Retrospective requests received more than two business days after the date of service will not be accepted by AIM for precertification review. Any post-service clinical review will be handled by anthem or HealthKeepkers according to the terms of the applicable health benefit plan and/or provider agreement. Radiation therapy performed as part of an inpatient admission will continue to be reviewed through Anthem’s inpatient precertification process. Members currently undergoing treatment on March 1, 2016, will not be impacted by the new enhancements to this program. However, members starting treatment on or after March 1, 2016 must follow the enhanced Radiation Therapy Program precertification requirements noted above. Thank you for your collaboration and ongoing support of the Radiation Therapy Program. If you have further questions, please contact your local network manager or call the provider customer service area at the phone number on the member’s ID card. Coverage and clinical guideline update REMINDER: Specialty pharmacy site-of-service reviews began November 1 In our August 2015 edition and October 2015 edition of the Network Update, Anthem Blue Cross and Blue Shield and affiliate HealthKeepers, Inc. shared information about a new requirement that the setting for specialty pharmacy infusions will be reviewed for appropriate clinical setting beginning November 1, 2015. In this December edition, we are sharing details about this change again as a reminder and for easy reference. Anthem and HealthKeepers, Inc. recognize that most patients prefer to receive their infusions in their physician’s office, infusion center or at home through home infusion therapy. This is more convenient for the member, results in lower member financial responsibility and, in many cases, is a clinically appropriate setting. For our members who require infusion therapy services, out-of-pocket expenses, the place of infusion service, safety, time and convenience are contributing factors that can impact health care quality, value and member satisfaction. However, there may be other circumstances where a patient’s medical situation requires that he or she receive infusions in a hospital facility. Therefore, beginning November 1, the setting for specialty pharmacy infusions will be reviewed for appropriate clinical setting. Anthem and HealthKeepers, Inc. will review the drug appropriateness for clinical indications and the site of service using a new clinical guideline CG-DRUG-47. During the review process, the nurse reviewer will provide other options if a setting is considered not medically necessary. More information follows below about CG-DRUG-47. December 2015 11 of 41 Our members count on their physicians to provide comprehensive information so the members can make informed decisions about their health care choices. Members may have questions about alternate settings in which they can receive their intravenous infusions and costs associated with other aspects of their intravenous infusion therapy. We encourage you to discuss with our members the options available to get their intravenous infusions safely and conveniently, at a lower, out-ofpocket cost. Level of Care: Specialty Pharmaceuticals (CG-DRUG-47) This new clinical UM guideline provides clinical criteria for use of outpatient infusion therapy service in the hospital outpatient department or hospital outpatient clinical level of care for intravenous (IV) infusion therapy. An outpatient infusion therapy service in the hospital outpatient department or hospital outpatient clinic level of care for the use of an infused pharmacologic or biologic agent is considered medically necessary when all of the following are present: 1. The inherent complexity or risk of the infusion required by an individual is such that it can be performed safely and effectively only by or under the general supervision of skilled nursing personnel; AND 2. The individual's medical status or therapy is such that it requires enhanced monitoring beyond that which would routinely be needed for infusion therapy; AND 3. The potential changes in the individual’s clinical condition are such that immediate access to specific services of a medical center/hospital setting, having emergency resuscitation equipment and personnel, and inpatient admission or intensive care is necessary, for example, the individual is at significant risk of sudden life-threatening changes in medical status based on clinical conditions including but not limited to: a. b. c. Concerns regarding fluid overload status, or History of anaphylaxis to prior infusion therapy with a related pharmacologic or biologic agent, or Acute mental status changes. All other uses of outpatient infusion therapy services in the hospital outpatient department or hospital outpatient clinic level of care for the infusion of pharmacologic and biologic agents are considered not medically necessary. The services addressed in this coverage guideline will require authorization for all of our products offered by HealthKeepers, Inc. with the exception of Anthem HealthKeepers Plus (Medicaid). Other exceptions are Medicare Advantage, the MedicareMedicaid Plan (Dual Integration product) and the Blue Cross Blue Shield Service Benefit Plan (also known as the Federal Employee Program or FEP) which will not be reviewed at this time with this guideline. A pre-determination can be requested for our Anthem PPO products. December 2015 12 of 41 Business update New regional vice president and senior clinical officer in Virginia Recently, Anthem Blue Cross and Blue Shield announced that Maureen Dempsey, M.D., joined Anthem in Virginia as regional vice president and senior clinical officer. Dr. Dempsey, a board-certified pediatrician, succeeds Karen Remley, M.D., who accepted the position of chief executive officer with the prestigious American Academy of Pediatrics. In her position as Anthem in Virginia's senior clinical officer, Dr. Dempsey will be responsible for clinical program oversight, medical management and quality of care initiatives. She will also have a leadership role working with our internal provider solutions team to expand and create effective provider collaboration activities such as our Enhanced Personal Health Care program. Most recently, Dr. Dempsey was the regional medical director for Humana's Mid-Atlantic region. She has also worked at the Virginia Department of Health (VDH) where she served as chief deputy commissioner for Public Health. During her last year at VDH, she was the acting commissioner of health. Dr. Dempsey has also served as a physician surveyor for the National Committee on Quality Assurance, and she was the executive director of Health and Dental Care for Kids in St. Louis. With her vast experience and background, Dr. Dempsey is uniquely positioned to engage our provider partners, as we work collaboratively to help ensure Anthem members continue to have access to affordable and quality health care. Updates to Blue Physician Recognition Program Anthem Blue Cross and Blue Shield (Anthem) is committed to providing members with the tools they need to effectively partner with their physicians and make more informed health care choices. As part of that effort, Anthem is pleased to participate in the Blue Cross and Blue Shield Association’s consumer engagement initiative. The Blue Physician Recognition (BPR) Program is designed to reinforce Blue Plans’ commitment to quality by providing more meaningful and consistent information on physician quality improvement and recognition on the Blue National Doctor & Hospital Finder site and on Anthem’s online provider directories. A BPR indicator is used to identify physicians, groups and/or practices who have demonstrated their commitment to delivering quality and patient-centered care by participating in local, national, and/or regional quality improvement programs as determined by the local Blue Plan. Anthem recognizes primary care physicians practicing in the specialties of Family Practice, Internal Medicine and General Practice with a BPR designation if they have achieved recognition from either the National Committee for Quality Assurance (NCQA) or Bridges to Excellence (BTE) based on their successful completion of a care recognition program. Information regarding these recognition programs can be found at http://www.ncqa.org or http://www.hci3.org. December 2015 13 of 41 At a minimum, we will update these recognitions annually to reflect the current status as identified by the Blue Cross and Blue Shield Association’s Quality Recognition Extract. If you have questions regarding the update, please contact your Anthem network contracting representative. Incentive opportunity for physicians treating patients with Anthem plans purchased on or off the exchange In 2014, Anthem Blue Cross and Blue Shield and our affiliate HealthKeepers, Inc. announced that we would engage Inovalon – an independent company that provides secure, clinical documentation services – to conduct outreach efforts for our health care exchange business. Anthem and HealthKeepers, Inc. are working with Inovalon to help ensure that our members, who have purchased health care plans on and off the exchange, get their diagnoses confirmed, corrected, and updated every year, as well as have potential preventive care gaps addressed. To accomplish this goal, Anthem network providers – usually primary care physicians – may receive letters from Inovalon, asking you to perform patient outreach and assessments, followed by submission of a SOAP Note (also called Encounter Facilitation Form). SOAP Note stands for Subjective, Objective, Assessment, and Plan which is the standardized document format of a medical record. If you receive a request from Inovalon, we understand that completing these SOAP Note requests may take time. We would like to offer contracted exchange providers the opportunity to increase your reimbursement. As a reminder, you are eligible to receive $100 in addition to your office visit fee for each properly submitted electronic SOAP Note submitted through Inovalon's ePASS tool. You may also elect to submit your patient assessment data for the members we request using the paper SOAP Note option via Inovalon's secure fax line at 1-866-682-6680. For each paper SOAP Note properly submitted for patient assessments performed, you are eligible to receive $50 in addition to your office visit fee. Submitting a SOAP Note Paper: You have the option to fax in a completed paper SOAP Note to Inovalon at 1-866-682-6680. To ensure that the paper SOAP Note is fully processed, all required fields must be completed and signed by the member's physician. Electronically: You may use ePASS (Electronic Patient Assessment Solution Suite), an electronic tool that retrieves information about your Anthem patients, including potential preventive care gaps, and drops this data into the SOAP Note to document your patients’ conditions. The ePASS® tool may be used for members Inovalon identifies, and the members have purchased individual and small group health plans on and off the exchange. To utilize ePASS®, please sign up online at the following Web address: https://ePASS.inovalon.com Overview of the ePASS® tool If you receive a request from Inovalon to complete a SOAP note and you're interested in an overview of the ePASS® tool, please see below for various webinar dates. We encourage you to register in advance by sending an email to ePASSProviderRelations@Inovalon.com with your name, organization, contact information and date of the webinar you’d like. December 2015 14 of 41 This webinar provides a practical overview of how ePASS can be used to access a supplemental clinical profile and complete a compliant electronic encounter SOAP Note for patients Inovalon identifies on Anthem’s behalf. The webinar typically lasts 30 minutes with time for questions. Tips for joining an ePASS® tool overview webinar: First: Join by calling the toll-free number and enter the access code. Second: click on WebEx Link and enter meeting code. Webinar Date Time December 02, 2015 3:00 - 3:30 p.m. EST December 09, 2015 3:00 - 3:30 p.m. EST December 16, 2015 3:00 - 3:30 p.m. EST January 06, 2016 3:00 - 3:30 p.m. EST January 13, 2016 3:00 - 3:30 p.m. EST January 20, 2016 3:00 - 3:30 p.m. EST January 27, 2016 3:00 - 3:30 p.m. EST The following dial-in information and WebEx link/entry code are the same for all webinar dates. Phone Number/Access Code: 1-888-850-4523. Enter Access Code: 10860 WebEx Link/Meeting Code: Visit:https://inovalon.webex.com. Enter: 745 497 369 For more information on the outreach process or the ePASS tool, please click HERE. Or, go to anthem.com>Providers (select Virginia)>Health Insurance Exchange> “Anthem engages Inovalon to conduct outreach efforts for our ACA individual and small group on and off exchange business – FAQs.” You may also contact Inovalon toll free at 1-877-448-8125. December 2015 15 of 41 Misrouted protected health information (PHI) As a reminder, providers and facilities are required to review all member information received from Anthem Blue Cross and Blue Shield and our affiliate HealthKeepers, Inc. to help ensure no misrouted PHI is included. Misrouted PHI includes information about members that a provider or facility is not currently treating. PHI can be misrouted to providers and facilities by mail, fax or e-mail. Providers and facilities are required to immediately destroy any misrouted PHI or safeguard the PHI for as long as it is retained. In no event are providers or facilities permitted to misuse or re-disclose misrouted PHI. If providers or facilities cannot destroy or safeguard misrouted PHI, providers and facilities must contact Anthem’s provider services area to report receipt of misrouted PHI. HEDIS® 2015 results are in for our PPO and HealthKeepers lines of business Thank you for participating in the annual Healthcare Effectiveness Data and Information Set (HEDIS) data collection project for 2015 impacting our PPO and HealthKeepers (non-Medicaid) lines of business. You play a central role in promoting the health of our members. By documenting services in a consistent manner, it is easy for you to track care that was provided and identify any additional care that is needed to meet the recommended guidelines. Consistent documentation and responding to our medical record requests in a timely manner eliminates follow-up calls to your office and also helps improve HEDIS scores, both by improving care itself and by improving our ability to report validated data regarding the care you provided. Further information regarding documentation guidelines can be found on the HEDIS page of our provider portal. The provider portal can be accessed at www.anthem.com and clicking on “Provider,” followed by “Virginia” then “Health and Wellness,” and “Quality Improvement and Standards.” You will find reference documents entitled “HEDIS 101 for Providers” and the “HEDIS Physician Documentation Guideline” under the HEDIS information section on the Quality Improvement and Standards webpage. The table below shows some of our key measure rates across East Region. The rates in bold in the HEDIS 2015 column reflect an increase from 2014 rates. Yellow boxes indicate rates that are above the national average. Bold indicates improvement in rate over the previous year. Comprehensive Diabetes Care - Poor HbA1c Control (>9): Lower rate is good December 2015 16 of 41 Anthem HealthKeepers/POS Measures HEDIS 2015 Rate (Percent) Adult BMI Assessment Childhood Immunization Status - DTAP 84.58 89.43 Childhood Immunization Status - MMR Childhood Immunization Status - HIB Childhood Immunization Status - VZV Childhood Immunization Status - PCV Childhood Immunization Status – HEP A Childhood Immunization Status - ROTAVIRUS Childhood Immunization Status – TDAP/TD Immunizations for Adolescents – MENINGITIS Weight Assessment/Counseling–Nutritional Counseling - TOTAL Weight Assessment and Counseling – Physical Activity- TOTAL Appropriate Treatment Children w/ URI Spirometry Testing for COPD Well-Child Visits in the first 15 Months of Life (6+ visits) Persistence of Beta-Blocker Treatment after AMI Comprehensive Diabetes Care – Eye Exams Comprehensive Diabetes Care – Nephropathy 93.37 97.54 94.35 92.14 85.26 90.17 89.43 64.80 60.58 55.72 81.16 37.90 84.36 85.22 60.58 86.13 Antidepressant Medication Mgmt – Acute FU Care Children’s ADHD Medication – Initiation *lower rate is better 60.79 37.42 December 2015 17 of 41 PPO Measures HEDIS 2015 Rate (Percent) Adult BMI Assessment Childhood Immunization Status – DTAP Childhood Immunization Status – IPV Childhood Immunization Status – MMR Childhood Immunization Status – HIB Childhood Immunization Status – HEP B Childhood Immunization Status – VZV Childhood Immunization Status – PCV Childhood Immunization Status – ROTAVIRUS Childhood Immunization Status – TDAP/TD Colorectal Cancer Screening Immunizations for Adolescents – MENINGITIS Immunizations for Adolescents – TDAP/TD Weight Assessment and Counseling – BMI TOTAL Weight Assessment and Counseling – Nutrition Counseling TOTAL Weight Assessment and Counseling – Physical Activity TOTAL 81.10 84.18 90.27 87.83 90.27 86.62 89.05 84.43 84.67 81.33 69.47 63.88 81.33 51.82 56.45 Antibiotic Treatment Adults w/ Acute Bronchitis 19.14 Appropriate Testing for Children w/ Pharyngitis Appropriate Treatment Children w/ URI Well-Child Visits in the first 15 Months of Life (6+ visits) 82.61 79.83 80.39 Effectiveness of Care - Cardiovascular Persistence of Beta-Blocker Treatment after AMI 80.87 Effectiveness of Care - Diabetes Comprehensive Diabetes Care – Blood Pressure Control <140/90 65.69 Effectiveness of Care – Behavioral Health Antidepressant Medication Mgmt – Acute 63.69 Antidepressant Medication Mgmt – Continuation 47.53 FU Care Children’s ADHD Medication – Initiation 34.89 FU Care Children’s ADHD Medication - Continuation *lower rate is better 39.50 52.31 In Virginia, many scores for the HealthKeepers/Point of Service line of business improved and exceeded the national average, especially those in Weight Access/Counsel Physical Activity Total, Medication Management for people with asthma with the largest rate increases noted in Weight Access/Counseling Physical Activity. In the PPO line of business, there were December 2015 18 of 41 also many improved scores that exceeded the national average, especially those in Weight Access/Counseling total BMI 7-14 year, Weight Access/Counseling BMI 12-17 years and with the largest rate increases noted in Weight Access/Counseling in BMI and Weight Access/Counseling Physical Activity 12-17 years. Although many rates were above the national average, this year the PPO plan had the greatest number of decrease in rates. There are opportunities for improvement for the measures with the most significant decreases in rates including: Follow-Up Care Children ADHD Med Initiation, Follow Up Care Med Continuation, Persistence of Beta Blocker Treatment after AMI, Well-Child visits in the first 15 months of Life (6+ visits), and Child Immunization Status DTap. Each year, our goal is to improve our process for requesting and obtaining medical records for our HEDIS project. In order to demonstrate the exceptional care that you have provided to our members and in an effort to improve our scores, you and your office staff can help facilitate commercial HEDIS process improvement by: Responding to our requests for medical records within five days if at all possible Providing the appropriate care within the designated timeframes Accurately coding all claims Documenting all care clearly in the patient’s medical record Again, we thank you and your staff for demonstrating teamwork as we work together to improve the health of our members and your patients. We look forward to working with you again next HEDIS season. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). Enhanced Personal Health Care program offers greater value for members and greater financial opportunity for PCPs Anthem Blue Cross and Blue Shield has a long history of offering payment innovation programs to primary care providers (PCPs) and some specialist providers in our networks. Because the health care industry continues to evolve to a more patient-centered approach to care delivery, we are focusing our efforts on our Enhanced Personal Health Care (EPHC) program which offers greater value for our members and greater financial opportunity for PCPs. Enhanced Personal Health Care is the name we give to arrangements between our health plan and participating providers when the arrangements include three things: 1. Value-based payment that rewards high quality and efficiency 2. Exchange of clinical data, and 3. A mutual commitment to ensuring our members receive patient-centered care. December 2015 19 of 41 Enhanced Personal Health Care arrangements are flexible enough to accommodate organizations of all sizes, and run the gamut from agreements with solo primary care physicians to accountable care agreements with large integrated systems. The goal is to have a more effective outreach and care coordination to help close gaps in care for Anthem members who are high risk and/or have chronic health conditions. For large national employer customers, we offer a national network of providers who work under value-based payments. That national network includes Enhanced Personal Health Care within our affiliated health plans’ geographic coverage area, but also includes similar programs hosted by other members of the Blue Cross and Blue Shield Association. This network of patient-centered, value-based payment programs is called Blue Distinction Total Care. Providers who participate in Enhanced Personal Health Care arrangements are part of Blue Distinction Total Care by default. Employers and their employees, your patients, may refer to the program by either name. Our “Find a Doctor” tool may identify you as a participant in Enhanced Personal Health Care or Blue Distinction Total Care. As our fellow Blue Cross and Blue Shield plans grow their own value-based programs, we will increasingly share information between plans, and gain the ability to share more information with participating providers even if the patient is covered by another Blue Cross Blue Shield Association member plan. The design of other plans’ value-based payment programs will not necessarily mirror Enhanced Personal Health Care in every respect or in every case, but BCBS Association member plans share the aim of rewarding high-quality evidence-based efficient care with primary care at the heart of a patientcentered delivery system. Enhanced Personal Health Care: Referral providers benefit by improving quality and controlling costs A key goal of the Enhanced Personal Health Care Program is to improve quality while controlling health care costs. One of the ways this is done is by giving primary care physicians (PCPs) in the Program quality and cost information about the health care providers to which the PCPs refer their attributed members (the referral providers). If a referral provider is higher quality and/or lower cost, this component of the Program should result in their getting more referrals from PCPs. The converse should be true if referral providers are lower quality and/or higher cost. We will share data on which we relied in making these evaluations upon request, and will discuss it with referral providers including any opportunities for improvement. Any such requests should be directed to your Anthem network manager. December 2015 20 of 41 Improving your patients’ health care experience Anthem is committed to working with our network physicians to make our members’ health care experience a positive one. Towards this end we wanted to share with you a document we discovered that was developed by the California Quality Cooperative. This resource outlines some helpful tips you can use to improve your relationship with your patients and provide better care at the same time. Simply log onto our website at www.anthem.com and follow this path: Providers>Select State>Enter>Health & Wellness>Guide to Improving the Patient Experience. "This information is provided by the California Quality Collaborative. A health care improvement organization dedicated to advancing the quality and efficiency of outpatient care in California." Survey says… Patients see room for improvement with physician care Every year, Anthem Virginia sends out the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) survey to our HealthKeepers (HMO)/Point of Service (POS) members. The survey provides Anthem members an opportunity to share their perceptions of the quality of care and services provided by our HMO/POS network physicians. The CAHPS survey is used by all HMO/POS plans that undergo accreditation review by the National Committee for Quality Assurance (NCQA). The following tables compare our results from 2014 with those in 2015. Each column contains the score achieved for each measure along with the box color coded to reflect the NCQA Quality Compass National Percentile achieved by Anthem Virginia. These Quality Compass percentiles are derived from the scores of all other HMO plans across the country that perform the CAHPS survey. Our goal is to achieve the 75th Percentile. When you’re reviewing these results, we encourage you to focus on and address those performance areas of your own practice that may have room for improvement. Addressing those areas will help our members, your patients, have a positive experience that meets their medical needs and their satisfaction with the quality of services provided. December 2015 21 of 41 2015 Anthem Virginia HealthKeepers/POS CAHPS® Adult Member Satisfaction Survey Results and NCQA Quality Compass Percentile Achieved NCQA Quality Compass Percentile Legend 5 10th 25th 50th 75th 90th Trend 2014 vs. 2015 Survey Question 2014 2015 Rating of Physician 1 Rating of Personal Doctor Rating of Specialist Seen Most Often Rating of All Health Care Provided in Past 12 Months 83% 83% 80% 85% 80% 79% Got appointment for urgent care as soon as needed 88% 91% Got appointment for check-up or routine care as soon as needed 89% 82% How often personal doctor explained things understandably to you 96% 97% How often personal doctor listened carefully to you 93% 95% How often personal doctor showed respect for what you had to say 94% 95% How often personal doctor spent enough time with you 90% 93% DNA 89% -- DNA 68% -- DNA 67% -- 74% 81% 73% 76% Getting Care Quickly 2 Got help or advice needed when calling doctor after regular office hours Doctor’s Communication with Patients 2 Shared Decision Making Doctor discussed reasons to take a medicine? 3 Doctor discussed reasons not to take a medicine? Doctor asked what you thought was best for you? 3 4 Continuity of Care and Health Promotion How often did your personal doctor seem informed about care you received from other health providers? 2 Did you and your doctor discuss ways to prevent illness? 4 1 = Percent responding 8, 9 or 10 (0-10, where 0 is the worst and 10 is the best). 2 = Percent responding “Usually” or “Always.” 3 =% responding “A lot” or “Some” 4 = % responding "Yes" 5 = Percentile Definition – A score equal to or greater than 75 percent of all those attained on a survey question is said to be in the 75th percentile. DNA = Data Not Available December 2015 22 of 41 NA = Number of survey respondents too low to be valid. Consumer Assessment of Healthcare Providers and Systems (CAHPS®) is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ). *The source of data contained in this report is Quality Compass ® 2015 and is used with the permission of the National Committee for Quality Assurance (NCQA). Any analysis, interpretation or conclusion based on these data is solely that of the authors, and NCQA specifically disclaims responsibility for any such analysis, interpretation or conclusion. Quality Compass is a registered trademark of NCQA. Respiratory antibiotic use performance Improving antibiotic use improves patient outcomes and saves money. The National Committee for Quality Assurance (NCQA) has identified three Healthcare Effectiveness Data and Information Set (HEDIS) measures around antibiotic use: Children (2 to 18 years) who present with Pharyngitis who are first given a group A streptococcus (strep) test and then appropriately receive an antibiotic. Children (3 months to 18 years) with a diagnosis of Upper Respiratory Infection who are not given an antibiotic prescription. Adults with a diagnosis of Acute Bronchitis who are not given an antibiotic prescription. The ratings for each of these metrics are determined by claims data only. Furthermore, it only takes one time of an antibiotic being inappropriately prescribed (and filled) in the one year measurement period to lower the scores. Local performance for appropriate testing and antibiotic prescribing – Anthem and our affiliate HealthKeepers, Inc. Based on claims data for our Anthem PPO and HealthKeepers lines of business in Virginia, the reported HEDIS rates were as follows: Appropriate testing for Pharyngitis in Children Appropriate treatment for Children with Upper Respiratory Infection Appropriate treatment for Adults with Acute Bronchitis December 2015 Measurement Period Rate Guide HealthKeepers Rates PPO Rates 7/1/2013 to 6/30/2014 7/1/2013 to 6/30/2014 Higher is better. 90.65% 82.61% Reported as an inverted rate. Higher is better. Reported as an inverted rate. Higher is better. 81.16% 79.83% 16.3% 19.14% 1/1/2013 to 6/30/2014 23 of 41 Things that might help you In an effort to help slow the emergence of antibiotic resistant bacteria and prevent the spread of antibiotic resistant infections, please commit to: Avoid prescribing antibiotics inappropriately: Recent studies have shown that displaying poster-sized commitment letters in exam rooms to avoid inappropriate antibiotic prescribing was a simple, low-cost, and effective method for improvement.1 Write a prescription for symptom relief instead of an antibiotic and educate patients on comfort measures that may work without antibiotics. Communicate with patients: Parents indicate that they would be satisfied with their medical visit even if antibiotics are not prescribed, provided that the physician explains the reasons for the decision.2 Discuss realistic expectations for recovery time, explain that antibiotics do not significantly reduce the duration of symptoms, and that unnecessary use of antibiotics may cause adverse effects that lead to antibiotic resistance. Test for bacterial infections: If a child presents with a sore throat, do a strep test and prescribe accordingly. Don’t send a script home with the patient “just in case,” but rather offer to call it in if the test comes back positive. Code claims correctly and accurately: If your patient has comorbidities, bacterial infections, or competing diagnoses, the standard codes for adults with acute bronchitis (AAB) and upper respiratory infection (URI) may not be applicable. Ensure proper documentation is in the medical record and use correct diagnosis and procedure codes on claim/encounter. Here are some resources that might help you and your patients: Anthem one-minute video: www.anthem.com/cold Choosing Wisely—www.choosingwisely.org: 5 Patient Questions to ask Before Taking Antibiotics and Antibiotics: When you Need them and When you Don't in English and Antibiotics: When you Need them and When you Don't in Spanish AWARE program materials-- Physician-Patient Resources in English and Spanish CDC “Get Smart about Antibiotics”-- Patient and Provider Materials and References including Clinical Guidelines SOURCES 1 Meeker, Daniella, et al. “Nudging Guidelines – Concordant Antibiotic Prescribing: A Randomized Clinical Trial.” JAMA Internal Medicine. 2014; 174 (3): p 425-431. 2 Barden, LS, et al. “Current Attitudes regarding use of Antimicrobial Agents: Results from Physicians’ and Parents’ Focus Group Discussions.” Clinical Pediatrics (Phila). Nov 1998; 37(11): p 665-671. December 2015 24 of 41 We believe in continuous improvement Commitment to our members’ health and their satisfaction with the care and services they receive is the basis for the Anthem Blue Cross and Blue Shield Quality Improvement Program. Annually, Anthem prepares a quality program description that outlines the plan’s clinical quality and service initiatives. We strive to support the patient-physician relationship, which ultimately drives all quality improvement. The goal is to maintain a well-integrated system that continuously identifies and acts upon opportunities for improved quality. An annual evaluation is also developed highlighting the outcomes of these initiatives. To see a summary of Anthem’s quality program and most current outcomes, visit us at www.anthem.com. Case Management Program Managing illness can sometimes be a difficult thing to do. Knowing who to contact, what test results mean or how to get needed resources can be a bigger piece of a healthcare puzzle that for some, are frightening and complex issues to handle. Anthem is available to offer assistance in these difficult moments with our Case Management Program. Our case managers are part of an interdisciplinary team of clinicians and other resource professionals that are there to support members, families, primary care physicians and caregivers. The case management process utilizes experience and expertise of the care coordination team whose goal is to educate and empower our members to increase self-management skills, understand their illness, and learn about care choices in order to access quality, efficient health care. Members or caregivers can refer themselves or family members by calling the number located in the grid below. They will be transferred to a team member based on the immediate need. Physicians can also refer by contacting us telephonically or through electronic means. No issue is too big or too small. We can help with transitions across level of care so that patients and caregivers are better prepared and informed about healthcare decisions and goals. Contacting us CM Telephone Number 1-877-332-8193 (Local/Commercial only) National 1-877-447-6481 Federal Employee Program 800-711-2225 December 2015 CM Email Address VA.CM@Anthem.com VANatlAccts-CM@wellpoint.com CM Business Hours Monday – Friday, 8 a.m. to 9 p.m. EST Saturday, 9 a.m. to 5:30 p.m. Monday – Friday, 8 a.m. to 5 p.m. No email Monday – Friday, 8 a.m. to 7 p.m. EST 25 of 41 Coordination of care Coordination of care among providers is a vital aspect of good treatment planning to ensure appropriate diagnosis, treatment and referral. Anthem would like to take this opportunity to stress the importance of communicating with your patient’s other health care practitioners. This includes primary care physicians (PCPs) and medical specialists, as well as behavioral health practitioners. Coordination of care is especially important for patients with high utilization of general medical services and those referred to a behavioral health specialist by another health care practitioner. Anthem urges all of its practitioners to obtain the appropriate permission from these patients to coordinate care between behavioral health and other health care practitioners at the time treatment begins. We expect all health care practitioners to: 1. Discuss with the patient the importance of communicating with other treating practitioners. 2. Obtain a signed release from the patient and file a copy in the medical record. 3. Document in the medical record if the patient refuses to sign a release. 4. Document in the medical record if you request a consultation. 5. If you make a referral, transmit necessary information; and if you are furnishing a referral, report appropriate information back to the referring practitioner. 6. Document evidence of clinical feedback (i.e., consultation report) that includes, but is not limited to: o Diagnosis o Treatment plan o Referrals o Psychopharmacological medication (as applicable) In an effort to facilitate coordination of care, Anthem in Virginia has several tools available on the provider website including a coordination of care template and cover letters for both behavioral health and other health care practitioners.* In addition, there is a provider toolkit on the website with information about alcohol and other drugs which contains brochures, guidelines and patient information.** *Access to the forms and cover letters are available at anthem.com>Providers> Provider Home>Answers@Anthem **Access to the Toolkit is available at anthem.com>Providers>Provider Home> Health and Wellness December 2015 26 of 41 Important information about utilization management Our utilization management (UM) decisions are based on the appropriateness of care and service needed, as well as the member’s coverage according to their health plan. We do not reward providers or other individuals for issuing denials of coverage, service or care. Nor, do we make decisions about hiring, promoting, or terminating these individuals based on the idea or thought that they will deny benefits. In addition, we do not offer financial incentives for UM decision makers to encourage decisions resulting in under-utilization. Anthem’s coverage guidelines are available on Anthem’s website at anthem.com. You can also request a free copy of our UM criteria from our medical management department, and providers may discuss a UM denial decision with a physician reviewer by calling us toll-free at the numbers listed below. UM criteria are also available on the web. Just select “Coverage & Clinical UM Guidelines, and Pre-Cert Requirements” from the Provider home page at anthem.com. We work with providers to answer questions about the utilization management process and the authorization of care. Here’s how the process works: Call us toll free from 8:30 a.m. - 5 p.m. Monday through Friday (except on holidays). More hours may be available in your area. Federal Employee Program hours are 8 a.m. – 7 p.m. Eastern. If you call after normal business hours, you can leave a private message with your contact information. Our staff will return your call on the next business day. Calls received after midnight will be returned the same business day. Our associates will contact you about your UM inquiries during business hours, unless otherwise agreed upon. The following phone lines are for physicians and their staffs. Members should call the customer service number on their health plan ID card. To discuss UM Process and Authorizations 1-800-533-1120 Behavioral Health: 1-800-991-6045 Federal Employee Program Phone 800-860-2156 FAX 800 732-8318 (UM) FAX 877 606-3807 (ABD) To Discuss Peer-to-Peer UM Denials 1-800-533-1120 Prompts 2,5,4,4,1 To Request UM Criteria 1-800-533-1120 Prompts 2,5,4,4,1 Behavioral Health: 1-800-991-6045 Behavioral Health: 1-800-991-6045 Federal Employee Program Phone 800-860-2156 Federal Employee Program Phone 800-860-2156 FAX 800 732-8318 (UM) FAX 877 606-3807 (ABD) TTY/TDD 711 or TTY: 800-828-1120(T) Voice: 800-828-1140(V) For language assistance, members can simply call the Customer Service phone number on the back of their ID card and a representative will be able to assist them. December 2015 27 of 41 Our utilization management associates identify themselves to all callers by first name, title and our company name when making or returning calls. They can inform you about specific utilization management requirements, operational review procedures, and discuss utilization management decisions with you. Members’ rights and responsibilities The delivery of quality health care requires cooperation between patients, their providers and their health care benefit plans. One of the first steps is for patients and providers to understand their rights and responsibilities. Therefore, in line with our commitment to involve the health plan, participating practitioners and members in our system, Anthem Blue Cross and Blue Shield has adopted a Members’ Rights and Responsibilities statement. It can be found on our Web site. To access, go to the "Provider" home page at anthem.com. From there, select “Provider” and Virginia> then Health & Wellness> Quality > Member Rights & Responsibilities. Clinical practice and preventive health guidelines available on the Web As part of our commitment to provide you with the latest clinical information and educational materials, we have adopted nationally recognized medical, behavioral health, and preventive health guidelines, which are available to providers on our website. The guidelines, which are used for our Quality programs, are based on reasonable medical evidence, and are reviewed for content accuracy, current primary sources, the newest technological advances and recent medical research. All guidelines are reviewed annually, and updated as needed. The current guidelines are available on our website. To access the guidelines, go to the "Provider" home page at www.anthem.com. From there, select “Provider” and Virginia> then Health & Wellness> Practice Guidelines. Or, for Anthem HealthKeepers Plus (Medicaid/FAMIS), select this LINK. GeoBlue: BlueCard provider outreach GeoBlue, in partnership with Blue Cross Blue Shield of Michigan, began serving over 3,000 internationally-based General Motors employees effective January 1, 2015. Many of these members will be seeking care in the U.S. and presenting the GeoBlue identification card. These members are enrolled in a Blue Cross Blue Shield product and have full access to the BlueCard provider network. The identification card follows all BlueCard specifications and all BlueCard processes apply. If you have any questions, please contact our Customer Service team at 1-855-282-3517. December 2015 28 of 41 Behavioral health update Documentation and reporting guidelines for applied behavior analysis (ABA) and treatments for Autism Spectrum Disorder Anthem implemented the new ABA CPT codes effective January 1, 2015. Anthem’s new policy is effective December 1, 2015, and outlines the health plan’s documentation and reporting guidelines for ABA and treatments for autism spectrum disorder utilizing this code set. Please refer to the AMA’s CPT codebook and Anthem’s documentation policies to ensure your practice is in compliance with these documentation requirements. The documentation policies can be found at anthem.com. Please review the policy and ensure that all aspects are being addressed. Health care reform (including health insurance exchange) Refer to anthem.com for information about health care reform and the exchange in 2016 With the new year rapidly approaching, we want to share information regarding our plans that members can purchase on or off the Health Insurance Marketplace also called the exchange. We will include the following for 2016: Member ID Card Update for ACA-compliant Health Plans Virginia Individual Plan Guide Virginia Small Group Product Guide We continue to post information on our dedicated Web pages regarding health care reform and the health plans HealthKeepers, Inc. is offering on and off the exchange. Click either of these Web pages Health Care Reform or Health Insurance Exchange for more information, and refer back to these pages often. December 2015 29 of 41 eBusiness Receive e-mail notifications via our Network eUPDATE Our provider newsletter, Network Update, is our primary source for providing important information to health care providers and professionals. Network Update is published bi-monthly and is posted to our website on the Virginia provider section of anthem.com for easy 24/7 access Note that in addition to this newsletter and our website, we also use our e-mail service – Network eUPDATE – to communicate new information. If you are not yet signed up to receive Network eUPDATEs, we encourage you to enroll now so you’ll be sure to receive all information we will be sending about the Health Insurance Marketplace or commonly called exchanges and other pertinent topics. Reminder notifications sent via e-mail When you sign up, you’ll not only receive an e-mail reminder for each newsletter posted online, you’ll also be notified of other late breaking news and important information you’ll need when providing services and filing claims for our members. It’s easy to sign up – just select Virginia and access the provider home page. There, you’ll find a link to register for our Network eUPDATE. Updated contact information for ERA and EFT registration Please note that we have updated the contact information for providers registering for Electronic Remittance Advice (ERA) and Electronic Funds Transfer (EFT). Anthem Blue Cross and Blue Shield in Virginia continues to use EnrollHub™, a CAQH Solution™ for the enrollment of EFT and ERA as noted below, but we have updated the amount of time a provider should wait before contacting Provider Services to resolve any EFT registration issues. December 2015 30 of 41 Electronic Remittance Advice, Electronic Funds Transfer Registration and Contact Information Type of Transaction EFT only EFT and ERA (both) How to Register, Update, or Cancel Use EnrollHub Use the EnrollHub For registration related questions, contact: EnrollHub Help Desk at 1-844-815-9763 EnrollHub Help Desk at 1-844-815-9763 To resolve issues after registration, contact: Local Provider Services: Outside the Richmond area, dial toll free 800-533-1120 Richmond area, dial 804-342-0010 For EFT questions, contact Local Provider Services: Outside the Richmond area, dial toll free 800-533-1120 Richmond area, dial 804-342-0010 NOTE – Providers should allow one week from the date Anthem receives the EFT enrollment from EnrollHub, as reflected on the EnrollHub EFT enrollment summary screen. For ERA questions, contact E-Solutions at 1800-470-9630 or e-solutions.support@anthem.com ERA only Use the EDI website at www.anthem.com/edi E-Solutions at 1-800-470-9630 NOTE – Providers should allow four to six weeks from successful ERA registration before contacting E-Solutions. E-Solutions at 1-800-470-9630 or e-solutions.support@anthem.com NOTE – Providers should allow four to six weeks from successful ERA registration before contacting E-Solutions. December 2015 31 of 41 Medicaid information (Anthem HealthKeepers Plus offered by HealthKeepers, Inc.) Attention Medicaid Providers: ICD-10 coding for diabetic complications A benefit of ICD-10 codes is that providers can now report more clinical details concerning diabetic complications than they could in ICD-9. The increased specificity is possible because ICD-10 contains expanded combination codes for diabetic complications. A combination code describes two or more conditions within a single code. The ICD-10 code categories E08E13 contain the combination codes for diabetic complications. The codes include the type of diabetes mellitus, the body system affected and the complications affecting that body system. Get this useful ICD-10 coding tip sheet for diabetic complications here. Coverage guidelines and Clinical Utilization Management Guidelines update The Medical Policy and Technology Assessment Committee (MPTAC) approved Anthem Blue Cross and Blue Shield Medicaid coverage guidelines and Clinical Utilization Management (UM) Guidelines, developed or revised to support clinical coding edits for Medicaid members. These approved medical policies and Clinical UM Guidelines are publicly available on the provider website. Update: Home and hydration therapy medical necessity reviews Effective January 1, 2016, precertification requirements will change for certain home therapy codes for Anthem HealthKeepers Plus members. Requests must be precertified beginning January 1, 2016. Get the Home Therapy codes requiring precertification here. December 2015 32 of 41 Update: Scoliosis and spinal deformity medical necessity reviews Effective January 1, 2016, surgical interventions for scoliosis and spinal deformity procedure requests for Anthem HealthKeepers Plus members must be reviewed for precertification. Please submit all required clinical information at least 14 days before the requested procedure to allow a thorough clinical analysis. For precertification instructions, use this link. Home health and outpatient therapies will require separate authorizations Effective January 1, 2016, requests for home health and outpatient therapies for Anthem HealthKeepers Plus members will require a separate precertification for each skill requested. Providers are required, for dates of service beginning January 1, 2016, to submit each skill request separately to ensure there are no delays in processing. If providers are faxing in the precertification request, a separate Precertification Form for each skill request should be sent. Providers who use the Provider Self Service tool on http://www.Availity.com must submit a separate precertification request for each skill requested. For questions about these communications, contact Anthem HealthKeepers Plus Provider Services at 1-800-901-0020. Medicare-Medicaid Plan update This section of the newsletter addresses information about the Anthem HealthKeepers Medicare-Medicaid Plan or MMP. Members are enrolled in both Medicare and Medicaid under the Commonwealth Coordinated Care Plan, also known as the Duals Demonstration (“Demonstration”) Program. CDC predicts another moderately severe flu season predominated by influenza A (H3N2) HealthKeepers, Inc. is launching an annual member outreach campaign to encourage high-risk members enrolled in the Anthem HealthKeepers Medicare-Medicaid Plan (MMP), a Commonwealth Coordinated Care plan, to visit their providers for a flu vaccine. Outreach includes automated outbound telephone calls, text messages and newsletter articles. Providers may experience an increase in phone calls and early appointments for the flu vaccine as a result of this outreach campaign. Along with details about our outreach efforts, we’ve included highlights about the Centers for Disease Control and Prevention’s (CDC) 2015 report on influenza activity and the composition of the 2015/2016 vaccine, Read more about the impacts of flu season on your practice. December 2015 33 of 41 ICD-10 coding supports MMP providers in reporting more clinical details for diabetic complications In the preceding Medicaid section of this edition of the Network Update, we share information regarding the benefit of ICD-10 codes in that providers can now report more clinical details concerning diabetic complications than they could in ICD-9. The information also applies to providers who participate in our MMP network. See page 32 for the full article or select this LINK. Medicare information (Anthem’s Medicare Advantage and Medicare Supplement plans) Avoid denials of Medicare Advantage diagnostic claims by completing item 20 (CMS-1500) correctly – Individual membership only The Centers for Medicare & Medicaid Services (CMS) requires that providers billing for diagnostic tests subject to the anti-markup payment limitation complete Item 20 on the CMS-1500 form. A “YES” check indicates that an entity other than the entity billing for the service performed the diagnostic test. A "NO" check indicates "no anti-markup tests are included on the claim." When "YES" is annotated, Item 32 is required to be completed. Claims for Anthem individual Medicare Advantage members received with Item 20 checked as “YES” and incomplete or missing information in Item 32 will be denied with denial Z01 “Claim must be billed with Provider’s NPI”. To prevent unnecessary denial of claims, only complete Item 20 when you are billing diagnostic tests subject to the anti-markup payment limitation. For more information on diagnostic tests subject to the anti-markup payment limitation refer to Medicare Claims Processing Manual, Chapter 35, Section 30. December 2015 34 of 41 Please include modifiers to help ensure accurate payment Codes not recognized by original Medicare are considered by Anthem Medicare Advantage as not reimbursable unless otherwise noted for both individual and group-sponsored claims. During the past year, some providers have found that certain individual and group-sponsored claims are denied for missing or inconsistent modifiers as the claims are not consistent with Centers for Medicare & Medicaid Services (CMS) payment guidelines. Please ensure you use the most current and appropriate CMS codes and modifiers when submitting your claims. Check Important Medicare Advantage Updates at www.anthem.com/medicareprovider for additional information. Oxygen DME precertifications will be reduced in 2016 Providers who prescribe durable medical equipment for oxygen delivery for Anthem individual and group-sponsored Medicare Advantage members will find that fewer items will require precertification in 2016. Detailed precertification requirements for individual Medicare Advantage members are available to the contracted provider by accessing the Provider Self-Service Tool within Availity. Go to Auths and Referrals/Authorizations from the left navigation menu. Select Anthem Medicare Advantage from the drop down box. You will be directed to the Medicare Advantage Precertification site which includes the precertification submissions and inquiries link and Patient360, which can be found under the Patient Information tab. Providers will find precertification requirements there as well via the Precertification look-up tool. Please visit www.anthem.com/medicareprovider to learn more about this online provider self-service tool. Precertification Guidelines found at the Medical Policy, UM Guidelines and Precertification Requirements link on the Anthem provider home page at www.anthem.com for further information on existing precertification requirements. Anthem to review ER level 5 professional claims Anthem is initiating a review of ER professional claims billed with a level 5 ER E/M code (99285 or G0384) to ensure the documentation meets or exceeds the components necessary to support its billing. The review for the necessary components will be based on the coding guidelines outlined in the American Medical Association (AMA) CPT coding reference. Documentation will be requested and the review will be performed on a pre-pay basis. The review for selected ER professional claims with level 5 E/M codes is scheduled to begin January 1, 2016. December 2015 35 of 41 Register for imaging site scores by March 1, 2016, to avoid unnecessary line-item denials Please note: The following information does not apply to providers with delegated risk agreements On November 1, 2015, Anthem Medicare Advantage plans began collecting information about the imaging capabilities of all Anthem Medicare Advantage contracted providers who provide the technical component of a number of outpatient diagnostic imaging services for our individual Medicare Advantage members. AIM’s online registration tool, OptiNet®, will continue to collect modality-specific data from providers who render imaging services in areas such as: facility qualifications, technician and physician qualifications, accreditation, equipment, and technical registration. This information is used to determine conformance to industry-recognized standards, including those established by the American College of Radiology (ACR) and the Intersocietal Accreditation Commission (IAC). This data will continue to be used to calculate site scores for providers who render imaging services to our individual Medicare Advantage members. Each modality or piece of equipment will receive its own score. Providers with an imaging site score of 76 or higher for the applicable modality will see no change in reimbursement. Providers who score less than 76 or who do not complete the survey by March 1, 2016, will receive a line-item denial for the technical component of the outpatient diagnostic imaging service only. Globally billed claims will deny in total if the provider scores less than 76 or if the provider does not complete the survey. If billing globally and the claim is denied, the provider has the option to resubmit a corrected claim for the professional component (interpretation) with modifier 26 for payment consideration. Other services on the claim, including the professional component of the outpatient diagnostic imaging service, will be processed as usual as long as required authorizations are in place. Anthem strongly encourages any provider who scores below 76 to improve his or her site score for the applicable modality before the line-item denial of claims begins on claims submitted for dates of service on or after March 1, 2016. Providers who have not registered and therefore have no score also will be subject to line-item denials for claims submitted for dates of service on or after March 1, 2016. The provider registration is available online at www.aimspecialtyhealth.com/goweb. Simply select Anthem MA from the drop down menu. If you have questions or need help completing the registration, please call AIM Customer Service at 800-2522021. Please note that the line-item denial for a site score below 76 for the applicable modality applies only to individual Medicare Advantage claims at this time. Check Important Medicare Advantage Updates at www.anthem.com/medicareprovider for additional information. 56997WPPENMUB 10/21/2015 December 2015 36 of 41 More $0 copay medications available to Medicare Advantage members with chronic conditions Individual Medicare Advantage prescription drug plans in 2016 will continue to offer select drugs at a $0 member co-pay for the following conditions: high blood pressure, high cholesterol and diabetes. The 2015 medication list (glipizide, lisinopril, losartan, metformin, and simvastatin) will continue to be included. New medications on this list in 2016 include benazepril, enalapril, enalapril-hctz, lisinopril-hctz, glimepiride, glipizide ER, losartan-hctz, metformin ER, atorvastatin, lovastatin and pravastatin. Group-sponsored plans will continue to offer the Select Generics benefit, which offers $0 copay for select generic drugs. Avastin for ophthalmic use – C9257 can be billed in office setting for network providers Beginning January 1, 2016, C9257, Avastin 0.25mg (for ophthalmic use), will be payable for facilities and professional providers when other criteria are met for individual Medicare Advantage claim. In addition, Anthem will no longer require a prior authorization for Avastin for ophthalmic injection. Check Important Medicare Advantage Updates at www.anthem.com/medicareprovider for more information. Enhanced reimbursement available for certain Part B injectable drugs Beginning first quarter 2016, Anthem individual Medicare Advantage plans will reimburse providers with enhanced payments for using less expensive but therapeutically equivalent select Part B injectable drugs. The reimbursement change is specific to only the following drugs: Therapeutic Class – Antiemetics. HCPCS (drug) – J1626 (Kytril), J2405 (Zofran) Therapeutic Class – Folinic Acid. HCPCS (drug) – J0640 (Leucovorin) Therapeutic Class – Osteoporosis. HCPCS (drug) – J3489 (Reclast) Check Important Medicare Advantage Updates at www.anthem.com/medicareprovider for additional information. December 2015 37 of 41 Anthem place of service claims adjudication mirrors CMS guidelines CMS recently revised place of service (POS) code sets by adding new POS code 19 for “Off Campus-Outpatient Hospital” and revising POS code 22 from “Outpatient Hospital” to “On Campus-Outpatient Hospital.” Please ensure your claims include these new and revised POS codes where applicable. Anthem mirrors CMS guidelines when performing Place of Service claims adjudication. Anthem individual Medicare Advantage plan names changing for 2016 Anthem has introduced a standard nomenclature to its affiliated Medicare Advantage plans. In most instances, plan names start with the local brand name, followed by the word “MediBlue,” then a plan descriptor, such as “Access,” and finally the plan type. For instance, a standard HMO would be referred to as “Anthem MediBlue Essential (HMO),” while a standard PPO would be called “Anthem MediBlue Access (PPO).” Group-sponsored Medicare Advantage plans are not impacted by these changes. No member ID prefixes are changing for 2016. Check Important Medicare Advantage Updates at www.anthem.com/medicareprovider for a list of current and 2016 plan names. Keep up with Medicare Advantage news at Important Medicare Advantage Updates Please continue to check Important Medicare Advantage Updates at www.anthem.com/medicareprovider for the latest Medicare Advantage information, including: Important 2016 coverage changes for diabetic supplies Medicare Advantage reimbursement policies 2016 Medicare Advantage plan changes ICD-10-CM Educational Material Now Available Providers Must Enroll with Medicare to be able to Prescribe Part D Beginning June 1, 2016 Anthem encourages high-risk members to get annual flu shot 6815WPPENMUB 10/16/2015 December 2015 38 of 41 Pharmacy update CVS/specialty is the exclusive 1 in-network specialty pharmacy for Anthem members with medical benefit coverage for specialty medications As the exclusive Anthem provider for specialty injectable and infusion medication, CVS/specialty is able to ship to a physician’s office or to the patient’s location of choice. Coram, a division of CVS/specialty, can also administer infusion drugs in one of its infusion suites or in the patient’s home. Whether it is an infusion or injection medication, CVS/specialty can support ongoing patient care. Injectables Patients have 24/7 access to a pharmacist-led Care Team that includes specially-trained nurses, nutritionists, and support staff. This team supports, motivates and educates patients and caregivers throughout treatment. Patients can have their specialty medications delivered to the location of their choice which may be their home or physician’s office. CVS/specialty is the only pharmacy that can ship medications to physicians’ offices. If the treating provider does not use CVS/specialty for specialty drugs shipped to the physician’s’office, claims will process according to the member’s outof-network benefits as applicable. Phone, fax or e-scribe your prescription to any CVS/pharmacy or CVS/specialty pharmacy. Phone 1-800-237-2767 | fax 1-800-323-2445 Infusions As a division of CVS/specialty, Coram’s infusion nurses are experienced in administering infusion medications to complex patients with rare or autoimmune disorders. Patients can choose to receive infusions from experienced staff nurses in the convenience of their home, or at a local Coram infusion suite. Both options may reduce the risk of infection and help patients save money by moving infusions to lower cost sites of care. Coram offers convenient care nationwide in more than 65 infusion suites. To find a Coram infusion suite near you, go to coramhc.com/locations. Phone or fax your infusion referral to Coram. Phone 1-866-899-1661 | fax 1-866-843-3221 1 Subject to applicable state law. December 2015 39 of 41 Searchable Formulary Tool gives providers easier access to formulary/drug list information Anthem Blue Cross and Blue Shield (Anthem) recently launched a new Searchable Formulary Tool, providing access to all relevant medication information about five of Anthem’s drug lists, including – clinical edits like prior authorization or step therapy, dosage/strength options, and details about brands and generics. Providers can quickly access the Searchable Formulary Tool through the Pharmacy site where Anthem’s drug lists are housed. The following five drug lists are set up with searchable capabilities: National Select Preferred Essential Generic Premium Once you select the applicable drug list, you can search the drug list for a wealth of information including: Tier status Clinical programs/edits including quantity limits, dose optimizations, prior authorizations and step therapies Drug label name Generic drug name Generic drug indicator Therapeutic class and category Available dosage/strength options If needed, you can also access printable versions of these drug list PDFs. Additionally, members with our pharmacy benefit will have the added functionality of benefit-specific drug list search capabilities, which eliminates the need to identify and select the drug list that applies to their pharmacy benefit. December 2015 40 of 41 Pharmacy information available on anthem.com For more information on copayment/coinsurance requirements and their applicable drug classes, drug lists and changes, prior authorization criteria, procedures for generic substitution, therapeutic interchange, step therapy or other management methods subject to prescribing decisions, and any other requirements, restrictions, or limitations that apply to using certain drugs, visit: http://www.anthem.com/pharmacyinformation. The commercial drug list is reviewed and updates are posted to the website quarterly (the first of the month for January, April, July and October). For Anthem HealthKeepers Plus (Medicaid), visit SSB Pharmacy Information. To locate the “Marketplace Select Formulary” and pharmacy information for health plans offered on the Health Insurance Marketplace (also called the exchange), go to Customer Support, select your state, Download Forms and choose “Select Drug List.” For State-sponsored Business, visit SSB Pharmacy Information. Website links for the Federal Employee Program formulary Basic and Standard Options are Basic Option: https://www.caremark.com/portal/asset/z6500_drug_list807.pdf; and Standard Option: https://www.caremark.com/portal/asset/z6500_drug_list.pdf. This drug list is also reviewed and updated regularly as needed. For the Blue Cross and Blue Shield Service Benefit Plan (also called the Federal Employee Program or FEP), FEP Pharmacy Policy updates have been added to the FEP Medical Policy Manual and may be accessed at www.fepblue.org > Benefit Plans > Brochures and Forms > Medical Policies. December 2015 41 of 41