Dr Ronnie Lowe
advertisement

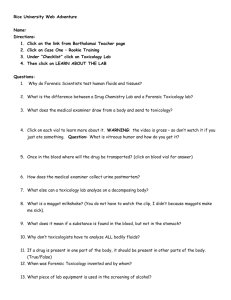
All you Need to Know about Forensics in Child Protection Cases Paediatric Child Protection Day Glasgow October 2015 AIMS & OBJECTIVES PRESENTATION OUTLINE Item One – What to do in child assault cases Item Two – What to look for Item Three – What samples to take Item Four – Referral to further departments Item Five – Summary What are abuse and Neglect? Abuse and neglect are forms of maltreatment of a child. Children may be abused in a family or community setting They may be abused by persons known to them They may be abused by an adult or other children Takes various forms from Physical to CSA Would you know what to do if you suspected abuse? Child maltreatment is defined as: all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment or commercial or other exploitation, resulting in actual or potential harm to the child’s health, survival, development or dignity in the context of a relationship of responsibility, trust or power. (Butchart, Putney, Furniss, and Kahane, 2006, p.9). 3UHYDOHQFH$JH6H[5DWLR Tayside Statistics 2013-2014 Table depicts the type of sexual assault examination undertaken within the Tayside area. Statistics for Tayside Population Served Population of 388k Area of 2896 sq miles Prevalence of Homicide 2.6 per 100k Number of Custody detainees 13000 per year 4th Largest Scottish Police Force 3 Territorial areas exist 40% have Mental Health Issues 19% rearrested 23% have polydrug abuse 10% LTC Diabetes IHD COPD ASTHMA Comparisons of Forensic Workload Data Analysis 2013-2014 Chart depicting where Assault cases sit as regards overall Tayside workload Photos Taser Nail scrapings Police Assault Intimate search Phys Ass Victim Sex Ass.Suspect M Section 5 RTA Medications Fit to detain/int Fit to release Mental health asses 0 20 40 60 80 100 120 140 160 Mar-May 2013 June-Aug 2013 Sept-Nov 2013 Dec13-Feb 14 7+$1.6%(72/2&$5'uuu “Every Contact leaves a trace” Devised concept by Locard in 1910 and he set up the first Forensic Laboratory in Lyon in two attic rooms of the Police Department. Highlighted that all contacts potentially leave DNA traces for analysis. Ideal Pattern of Investigation Do not allow Police to rush you into something you are not at ease with ¾ ¾ ¾ ¾ Story Chronology Early evidence Kit Intimate v Non-Intimate Samples ¾ Examination ¾ Photos ¾ Forensic Samples Consent – Fully informed written Forensic Samples Chronology of events Digital Photo documentatio n Interviews of relevant parties Physical Examination 2 Dr :KDWEDFNJURXQGLQIRUPDWLRQLVUHOHYDQWZKHQ H[DPLQLQJDUDSHYLFWLP" • History is key! • Not every rape case is the same • Prevent unnecessary examining/sampling of victim Neglect or Abuse? Poll answers 6WDUWZLWKWKHEDVLFV When? Where? Who? What? Time? Herpetic Eczema – neglect ? 6(5,(62)(9(176 Events leading up to the assault The assault What has happened in the time since? DSH Cigarette Burns Historical Child abuse Workhouse Abuse Victorian Times Abuse in School Place or Home Evaluating Skin Injuries: “The Kipling Principle” I Keep six honest serving-men (They taught me all I knew); Their names are What and Why and When And How and Where and Who. (Kipling 1902 ) Evaluating Skin Injuries: “The Kipling Principle” Types of skin injuries in mechanical trauma: closed injuries Bruise Bleeding, due to the rupture of blood vessels, generally located superficially in the skin and subcutaneous tissues with usually externally visible surface discoloration Caused by blunt-force trauma (collision/compression or stretching) Will not blanch under diascopy Synonyms (sometimes used for specific types of bruising and bleeding): contusion, hematoma, purpura, and ecchymosis Petechia Small red, purple, or brown spot caused by minor bleeding (0.1–2 mm – pinpoint to pinhead) in the skin, the mucous membranes and/or the serosal surfaces due Types of skin injuries Closed Injuries Bruise Facts %UXLVHVDUH WKH FRPPRQHVW LQMXU\WR 6RIW7LVVXHV %UXLVLQJLV NQRZQWR EH LQFUHDVHGDV FKLOG½V PRELOLW\ $EXVLYH EUXLVHVDUH IRXQGDZD\ IURPERQ\ SURPLQHQFH V $UH ODUJHDQG P OWLSOH Bruises in Differing Age Groups Immobile babies Infants Mobile 0.01School aged Walkers 0.19 0.17 0.53 Abrasion From Latin ab- from and Maintain Constant Wound radereto scrape '(),1,7,2162)9$5,(7<2),1-85,(6 Syn. Scratch, Graze Description Defn. " a portion of Bruise (from Old English brysan-to crush, Old French bruser-to break Syn. Contusion, Ecchymosis Defn. "escape of blood from ruptured small vessels (vein, capillaries, arterioles) into the surrounding tissues" The resulting discolouration is seen through the overlying intact skin. Due to blunt force trauma. Site, shape, size, severity of bruising are very variable the body surface from which the skin or mucous membrane has been crushed or removed by rubbing" A superficial injury, not involving the full thickness of the skin, i.e. confined to epidermis/dermis. Laceration From Latin lacerare- to tear. Botanical termirregular edges Defn.Full thickness tearing of skin or tissue due to stretching and crushing by blunt force” Characteristics: Ragged edge, Associated bruising/abrasion, Tissue bridges Provides little specific information about the causal object BRUISING No blanching on diascopy ERYTHEMA Blanching does occur on diascopy. Petechiae Extensive petechiae in the face of a strangled child Abrasion Laceration A small paper cut wound Laceration of the scalp with tissue bridges of vessels and/or nerves within the tear Blunt- and sharp-force trauma (from left to right ): (1) Superficial blunt force – bruising. (2) Blunt penetrating trauma – damage to subcutaneous tissue (e.g., bones). (3) Blunt penetrating trauma – damage to subcutaneous tissue (e.g., bones). (4) Sharp penetrating trauma – damage to subcutaneous tissue (e.g., bones). (5) Superficial sharp-force trauma – superficial incision or abrasion with or without damage to the underlying dermis and subdermis 1 2 3 4 5 INJURIES in Blunt FORCE Trauma Injuries resulting from mechanical trauma (static or dynamic loading) Blunt-force trauma Erythema Bruising Abrasion Laceration Avulsion Blunt penetrating trauma Sharp-force trauma Incision/incised wound Puncture wound/stab wound/ penetrating injury Gunshot wound/missile wound/ velocity wound THERMAL Trauma Dry Contact Burn Steam Iron Inflicted Hot water Burn Mongolian Blue Spot Bruises fading in White Child Impression Marks on Skin Superficial Bruise Healing Bruise Color changes during the degradation of hemoglobin (Busuttil 2004; Saukko and Knight 2004a; Harris and Flaherty 2011) Color Hemoglobin and degradation products Red Hemoglobin pigment + local inflammatory reaction Blue Deoxygenated, unsaturated Hb Purple Brown Greenish Biliverdin – hematoidin Yellow Bilirubin Straw color Colour Changes over time of bruise D1 D2 D3 ----- ------- > Weeks Black eye, 2nd day Black eye, 3rd day Tramline Bruising Secondary to hitting with bar Tramline bruising caused by hitting with a stick Human Bite Mark on Abdomen Distinguishing bruise from Mongolian spot Incision in a Mongolian spot: no visible blood Incision in a bruise: visible blood Static Impact Injury Pattern injury in static (and dynamic impact) loading: extensive bruising on the trunk of an abused child (suggestive for gripping, punching, and prodding) Blood Module for Toxicology More evidence that alcohol and drugs are used in Rape victims of teenage years so we must remember to look for the culprits. Blood sample Kit OCD on labelling and tamper proof packaging. Photo documen tation More common to take photos of injuries for later use in Court Presentation FFLM Specimen Advice Updated every 6mm Available free at WWW.FFLM.AC.UK Toxicology Samples Blood and Urine wherever possible. More likely to refuse blood sampling Forensic Sampling Corroboration Contamination Suspects Forensic Sample Events preceding the assault 9LFWLPVDFWLRQV $OFRKRORUGUXJXVH" ,QWHUDFWLRQVZLWKDVVDLODQW 1RQVH[XDODVVDXOW" 7+($66$8/7 Penetration? Digital/penile/other object Where? Condom/lubricant use Oral sex? By assailant or victim Where? Where? Restraints used? Did the assailant ejaculate? Any licking/biting/kissing? Assailant or material? Injuries obtained? Genital/non-genital To victim or assailant Loss of consciousness? Actions from time of assault to reporting Has the victim: Showered/bathed? Defecated/urinated? Changed clothes? Brushed teeth? Drank/eaten? Other sexual contact? Any bleeding? Used/changed sanitary towel or tampon? What evidence should be collected during examination? And how is such evidence interpreted by the court? Dependent on history Clothes Transfer of fibres or DNA or from locus Mouth Blood Toxicology Proof of DFSA Urine Mouth swab and rinse Toxicology Presence of DNA and spermatozoa Proof of DFSA Skin Relevant sites Presence of cells or saliva Hands Plus finger nail scrapings/clippings Presence of DNA or trace evidence Hair Cuttings and combings from head and pubic area Transfer between assailant and victim Documentation of injuries Non-genital and genital Photo documentation where possible 6ZDEVIRU'LIIHULQJ(YHQWV Female Male Vulval (dry + wet) Shaft and external foreskin (dry + wet) Low vaginal (dry + wet) Coronal sulcus (dry + wet) High vaginal (x2) Glans (dry + wet) Endocervical (x2) Anal Perianal (x2) Anal canal (x2) Rectal (x2) All can show presence of DNA or spermatozoa, proving that sexual intercourse occurred. Question of consent ORDER IS IMPORTANT +2:/21*'2(66(0(15(0$,1'(7(&7$%/( )2//2:,1*,17(5&2856(" Endocervical 144hours (6d) Internal vaginal 120hours (5d) External vaginal 120hours (5d) Rectal 65hours Anal ( if not defecated) 46hours Lips of mouth 9hours Oral 6hours Cleveland Affair 1987 Difference in opinion of Paeds + Police Surgeons. Recommendations of Report were: Consistent vocabulary to describe physical signs. Make full + accurate records Repeated examinations of child should not take place purely for evidential purposes. In every case should seek informed consent of parents for examinations. 07/10/2015 Child Protection 71 Victoria Climbie Report 2003 Most far reaching inquiry into child death ever held in UK. 108 Recommendations 110,000 downloaded copies in first week Key Findings: Lack of simple good practice Gross failure of systems Organisational malaise Inadequate “front door” service Laming “ I regard the skills and experience of GPs as a vital component in any effective scheme of child protection” 07/10/2015 Child Protection 72 Children Bill 2004 Co-operation to improve well being Statutory responsibility on Health/Police Local safeguarding boards Lead Member PCT must ensure welfare of children Key Laming Proposals 07/10/2015 “Accountability structure” Children’s database of all under 16 year olds Exchange information more freely Give Children a voice 24 hour children’s social work service Child Protection 73 Principles of Medical Examination To make what must be an unpleasant and painful examination as unthreatening as possible To collect useful forensic evidence – Valid uncontaminated swabs Careful injury recording : size, shape, colour, position To give opinion as far as appropriate and defensible lack of injury does not imply account false. To give objective opinion in Court To differentiate between forensic and therapeutic aims RAPE IS NOT A MEDICAL DIAGNOSIS Role of the Forensic physician FORENSIC – – – – Obtain relevant medical hx Sample the relevant areas Document Injuries Present the Evidence THERAPEUTIC – Emergency Contraception – STIs – Psychological Evidence Based Forensic Sampling EBF Sampling CONSENT Consent in relation to complainants of sexual assaults www.fflm.ac.uk Fully informed and written consent for physical & forensic sampling examination History of the Incident Direct Questions? – Oral – Anal Try and record questions and responses verbatim Use of Proforma essential Risk assessment Drug and alcohol use – – – – Prior During After Drug assisted sexual assault Relevant Medical history Identify medical problems That may be attributable to the assault – Injuries old or new – Pain – Bleeding Identify any Mental health issues that may effect interpretation of clinical findings – DSH – Behaviour problems Oral & Vaginal Oral – – – – Dentures Fixtures Recent illness Peno-oral penetration in preceding 10 days Vaginal – Peno vaginal penetration Condoms – Lubricants – LMP – Medical & Surgery in past Relevant Medical History Anal Peno – anal or Peno - Vaginal Peno-anal – Condoms – Lubricant Peno-vaginal penetration in previous 10 days – Condoms – Lubricants Medical & Surgical Medical Conditions – – – – Constipation Bleeding Easy bruising Dermatological issues Surgery – Old scars – Absent organs Fellatio Sample mouth up to 2 days after incident Mouth Swab Module Specimen Samples Taken Beware of FRQWDPLQDWLRQ & need corroboration. Hair sample kits . These enable hair to be sampled in order to determine time date and drug in system. Useful in date rape drugs Skin swabs Double swab technique Wet then dry Soft twisting circular rotation Urine sampl e Just first speci men no need for sterile urine or mid strea Substance Facilitated Sexual assault Easy to administer – Spiked drink Readily available Rapid action of onset – Amnesia – LOC Difficult to detect Alcohol BZDs – Rohypnol GHB Date Rape – Legal Highs Urine Module Collect if reported within 5 days Consult if > 5 days – Hair sampling toxicology Sodium Fluoride Police can collect – Early evidence kits – Along with clothes collection Skin Swabs Licked? Kissed? Sucked? Bitten? Ejaculated on ? Assailant’s blood? How to take skin swab? Double swab technique – One wet – One dry – Dry swab if skin moist No use if already washed – Listed as – skin swab cheek wet – Skin swab cheek dry Hair Module Head Pubic Area – FB – Body fluid = cut or swab – Fibres Tape lifting – Hair toxicology Substances – 50 hairs crown close to scalp Comb Cut DO NOT PLUCK!!! Comb for transfer of pubic hairs during SI – Transfer of pubic hair – – – – Female-male 23.8% Male-female 10.9% Female Genitalia Spermatozoa in Vagina – Should be found for 24hrs – May be found up to 3 days – Occasionally up to 7 days Seminal Choline < 24 hrs Endocervical swab after vaginal intercourse > 2 < 7 days Retain FBs – Tampons – condoms Female Genitalia swabs – – – – – – 2 Vulval swabs [1w & 1d] 2 Low vagina swabs [1w&1d] Pass single use Speculum 2 High vaginal swabs Retain speculum Lubricate speculum KY Gel Anal orifice Spermatozoa in anal canal or rectum – 65 hours after intercourse – Sample if reported within 3 days Don’t forget about drainage from the vagina – cross contamination Anal orifice 2 perianal swabs [1w & 1d] Pass single use Proctoscope 3cm 1 rectal swab 1 anal canal swab as you withdraw proctoscope – Retain proctoscope – – – – Blood urine or Hair for Toxicology Blood – Best done within 12 hrs for Toxicology – Drug metabolite breakdown Urine – Cannabis in urine up to 30 days Hair sample – Enables dating of drug taken – Need 2 samples one D1 Second 6W later Basic Details Required Height Weight Hair Colour Dyed Permed Cut last ntation Injuries Assessment Type of Injuries Standardised nomenclature Site Shape Dimensions Colour or colour surfacing Wound edges Restraint Defence Aggressive Sexual OLD Coincidental Alerting signs Unexplained delay in presenting changes in detail as the history is repeated inconsistency between history and clinical findings/developmental stage Why do we see victims of abuse? Medical Assessment & treatment of injuries Assessment & treatment of medical conditions Referral to other services e.g. Psychology Reassurance for the child Social Aiding social work in the assessment of risk Legal Collection of forensic evidence The medical examination cannot answer The exact cause of the injury When it happened - especially once the injury has healed Who did it? How much force? How often? Over what time period? Physical Abuse Does the history fit with the clinical signs? Do the history & clinical signs fit with the developmental stage of the child? Presentations Unexplained bruising fracture(s) different ages/inconsistent with story/development Abusive head trauma bite mark burns: scalds or contact non-organic failure to thrive fabricated or induced illness recurrent vulvo-vaginitis/ vaginal bleeding repeated DNA’s Typi cal acci dent al injur ies y pi ca l ab us iv e in ju ri Labelling & Packaging Description RL 1 – A&B Time Place Date Swab type dry or wet Mary Smith 09.00 30.01.2014 Dr Lowe Signed Handed to SIO TIME Labels Label sequentially Eg RL 1 A & RL 1 B Swabs from the same site may go in the same bag Frozen storage DNA analysis Control swab unopened Control water swab Return unused ampoules from packs Examination of the Accused Find out – Details of allegation Date time location nature – Discuss samples required Intimate Non Intimate – Nothing wrong with discussion with examiner of victim if required Introduce yourself Consider chaperone Get Consent – – – – – – Verbal v written Fully informed Disclosure Confidentiality No comment interview May need Sherriff Warrant Examination of the Accused Medical History – Current – PMSH – O&G – Substance use Examine – Clothing – Complete physical examination for Old & new injuries Tattoos Piercings Sample harvest Examination of the Suspect Penile Persistence of Cells Sampling the penis If incident within past 48 hours Even if washed or bathed since incident Two swabs [ 1W & 1D] obtained sequentially from the coronal sulcus Two swabs [ 1W & 1D] obtained sequentially from the glans and shaft Role of the Forensic physician FORENSIC – – – – Obtain relevant medical history Sample the relevant areas Document Injuries Present the Evidence THERAPEUTIC – Hiv hep risk – STIs – Psychological – Some assessment important – DM Suicide case secondary to wrongful accusation Intimate Samples Examination of the Accused Blood semen Other tissue fluid Dental Impression Swab from orifice other than mouth Swabs from body surfaces are only intimate if for purpose of obtaining suspect’s body fluids Non Intimate Samples Hair other than pubic hair Nail scrapings Saliva Footprint or other similar impression Swab from body surface or mouth Indecent Assault Manual contact with genitalia or anus Swab hands – Wet and Dry samples – Double swab technique Oral Contact with genitalia or anus Swab around mouth – Double swab technique Bites Can be human or animal or self inflicted %LWHVFDQEHGXHWRDQRWKHUFKLOGDGXOWRU VHOILQIOLFWHG %LWHVDUHRQO\LQMXU\ZKHUHSHUSHWUDWRU FDQEHLGHQWLILHGXVLQJ'1$DQDO\VLVDQG GHQWDOLPSUHVVLRQV &KDUDFWHULVWLFVRIELWHPDUNDUH 2YDORUFLUFXODUPDUNV 7ZRRSSRVLQJDUFKHV 0HDVXUHLQWHUFDQLQHGLVWDQFH DQGKXPDQLVXVXDOO\!FP 6ZDEIRUVDOLYD 3KRWRJUDSKWDNHQDWKRXU LQWHUYDOV $QLPDOELWHVWHQGWRWHDUWKH IOHVKDQGKDYHGLIIHUHQWLQWHUFDQLQH GLVWDQFHV 5DUHO\FRQIXVHGZLWKEXUQVRU LPSULQWVRIVKRHV Thermal Injuries Accidental – Intentional - Neglect Burns occur as child explores Accidents follow brief lapses in usual protection Neglect is part of inadequate parenting Study of A&e ATTENDANCE FOR 17,237 BURNS OR SCALDS IN CHILDREN < 5 YEARS OF AGE:= 65.7% Scalds 34.3% thermal burns Head & Neck – upper torso – upper limbs most commonly effected 86% caused by accidents 1.2% intentional injuries 5.5% attributed to neglect Referral to further departments Communication Communication &20081,&$7,21 Phone Numbers Police Involvement Custody Nurse Involvement Consent issues if child < 16 Gillick Competence Fraser competence Parental responsibility Forensic Samples Persistence of Forensic Material SUMMARY 9 Don’t be rushed into things 9 Think outside the box 9 Use Common Sense 9 Logical Reflection 9 Fully informed consent 9 Full Contemporaneous notes 9 Obsessive Record Keeping 9 Better to over sample than under sample Facts Basics History Chronology Examination Sampling Chronological History Do not rush events Need MRT approach IRD History informs what to: look for where when and why Liaise with Police asap to ensure no miscommunication occurs TEAMWORK 24-7-365 COMMUNICATION Trust intuition Work with anxiety Always ask No question is irrelevant Better to get patient care in an emergency, worry about the process and documentation later. Ask for training sessions, formal and informal in down time if you have an interest. COLLABORATION Teamwork Sharing Information Working Proactively Always act Plan Do Study Act Look out for Risk factors PACE Animation Page EMPATHETIC Interaction with encouragement to report ANY QUESTIONS? Discussion Item One – What to do in STI sexual assault case Any Immediate Medical Treatment required? What exactly happened? Time date place sexual acts . Reassure patient EMPATHY. Contacts for further advice Custody Nurse desk Dundee Police HQ 01382 591585 Nurse all have Msc in Forensic Medicine Take further details and appropriately advise. Early Evidence Kits. Further assistance History. Time Date Assault type Two important aspects of any Sexual assault examination THERAPEUTIC ASPECT OF EXAMINATION Medical examiners have two aspects to any examination Is it beneficial or harmful for the patient Do I have fully informed and written consent Full history etc Samples Photos of injuries Am I competent in performing the examination “One stop shop” FORENSIC ASPECT OF EXAMINATION Time periods for gaining forensic samples. Consent Sample packs Genital packs Finger packs Pubic hair packs Toxicology packs Labeling Proforma sheets Two Content Layout with Table First bullet point here Second bullet point here Third bullet point here Working together to Safeguard Children • Guide for Inter-agency working. • Launched April 2006 • Provides national framework for local agencies to work together. • Ensure welfare of the child • GPs & other PHCT members have key roles in identifying children at risk & in subsequent detection and protection. • Based on the Victoria Climbe inquiry • Includes the introduction of local safeguarding children boards What evidence should be collected during examination? And how is such evidence interpreted by the court? • Dependent on history • Clothes • Transfer of fibres or DNA or from locus • Mouth • Mouth swab and rinse • Presence of DNA and spermatozoa • Skin • Relevant sites • Presence of cells or saliva • Hands • Plus finger nail scrapings/clippings • Presence of DNA or trace evidence •Blood • Toxicology • Proof of DFSA • Urine • Toxicology • Proof of DFSA • Hair • Cuttings and combings from head and pubic area • Transfer between assailant and victim • Documentation of injuries • Non-genital and genital • Photodocumentation where possible • Proof of violence or force applied • Female • • • • Vulval (dry + wet) Low vaginal (dry + wet) High vaginal (x2) Endocervical (x2) •Anal • Perianal (x2) • Anal canal (x2) • Rectal (x2) • Male • Shaft and external foreskin (dry + wet) • Coronal sulcus (dry + wet) • Glans (dry + wet) •All can show presence of DNA or spermatozoa, proving that sexual intercourse occurred. •Question of consent •ORDER IS IMPORTANT How long does semen remain detectable following intercourse? • Endocervical 144hours (6d) • Internal vaginal 120hours (5d) •External vaginal 120hours (5d) •Rectal 65hours •Anal 46hours •Lips of mouth 9hours •Oral 6hours