- Wiley Online Library
advertisement

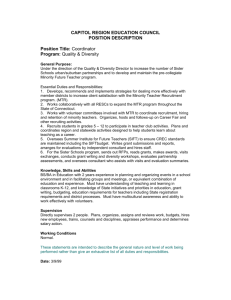
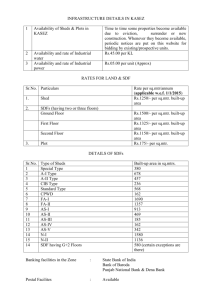
ARTHRITIS & RHEUMATISM Vol. 50, No. 9, September 2004, pp 2877–2881 DOI 10.1002/art.20654 © 2004, American College of Rheumatology Selective Gray Matter Damage in Neuropsychiatric Lupus A Magnetization Transfer Imaging Study S. C. A. Steens, F. Admiraal-Behloul, G. P. Th. Bosma, G. M. Steup-Beekman, H. Olofsen, S. le Cessie, T. W. J. Huizinga, and M. A. van Buchem Conclusion. This is the first study to demonstrate, using MTI, that in SLE patients with a history of NP symptoms and without explanatory focal abnormalities on MRI, the GM is particularly affected. These findings support the hypothesis that neuronal injury may underlie central nervous system manifestations in NPSLE. Objective. Damage of brain parenchyma in patients with primary diffuse neuropsychiatric systemic lupus erythematosus (NPSLE) has been indicated by magnetization transfer imaging (MTI). However, the location of MTI abnormalities is unknown. This study was undertaken to assess the distribution of MTI abnormalities over gray matter (GM) and white matter (WM) in SLE patients with a history of NP symptoms without explanatory magnetic resonance imaging (MRI) evidence of focal disease. Methods. MTI was performed in 24 female SLE patients with a history of diffuse NP symptoms and 24 healthy female controls. Magnetization transfer ratio (MTR) maps were calculated for GM and WM separately, and GM and WM MTR histograms were generated. Univariate and multivariate analyses with age as an additional covariate were performed on the histogram parameters peak location (PL), peak height (PH), and mean MTR. Results. Compared with controls, significantly reduced PH (mean ⴞ SD 136 ⴞ 22 arbitrary units versus 151 ⴞ 13 arbitrary units) and mean MTR (33.3 ⴞ 1.0 percent units versus 33.6 ⴞ 0.5 percent units) were found in the GM of NPSLE patients (P ⴝ 0.002 and P ⴝ 0.033, respectively, in multivariate analyses). No significant differences were observed for WM MTR parameters. Up to 75% of patients with systemic lupus erythematosus (SLE) experience neuropsychiatric symptoms indicative of central nervous system (CNS) involvement. In primary neuropsychiatric SLE (NPSLE), these NP manifestations are attributed to the SLE disease process itself, rather than to secondary factors such as infections or metabolic disorders (1). Focal neurologic NP syndromes are often associated with antiphospholipid antibodies; however, the cause of diffuse neurologic and psychiatric symptoms is largely unknown (2). Findings of conventional magnetic resonance imaging (MRI) of the brain are frequently unremarkable, and abnormalities are nonspecific (3,4). However, quantitative MRI techniques, such as magnetization transfer imaging (MTI), diffusion-weighted imaging, and MR spectroscopy (MRS), are now being assessed for their diagnostic value (4). Using MTI, a quantitative MRI technique that is sensitive to both macroscopic and microscopic CNS damage (4), abnormalities that had been invisible by conventional MRI were demonstrated in the brain parenchyma of NPSLE patients (5). Significant associations with parameters of neurologic, psychiatric, and neuropsychological function demonstrated the clinical relevance of these findings (6). Although the underlying pathogenesis of diffuse brain damage in NPSLE is largely unknown, recent findings of neuronal and astrocytic degradation products in the cerebrospinal fluid (CSF) of SLE patients have focused attention on the role of neuronal damage (7). Apart from small-vessel S. C. A. Steens, MD, F. Admiraal-Behloul, PhD, G. P. Th. Bosma, MD, MA, PhD, G. M. Steup-Beekman, MD, H. Olofsen, MSc, S. le Cessie, PhD, T. W. J. Huizinga, MD, PhD, M. A. van Buchem, MD, PhD: Leiden University Medical Center, Leiden, The Netherlands. Address correspondence and reprint requests to S. C. A. Steens, MD, Department of Radiology, C2-S, Leiden University Medical Center, PO Box 9600, 2300 RC, Leiden, The Netherlands. E-mail: s.c.a.steens@lumc.nl. Submitted for publication November 7, 2003; accepted in revised form May 12, 2004. 2877 2878 STEENS ET AL disease as a suggested pathogenetic factor in diffuse brain damage (2), an anti-DNA antibody that crossreacts with a neuronal receptor, and potentially induces neuronal damage, has recently been identified in serum and CSF of patients with SLE (8). Neuronal damage may be the key to diffuse brain damage in NPSLE. According to this hypothesis, the gray matter (GM) would be preferentially affected in NPSLE because of its high concentration of neurons. To date, MTI analyses in NPSLE patients have focused on the brain as a whole and have not been applied to selectively study the GM compartment. To test the hypothesis of preferential GM involvement in diffuse NPSLE, we assessed the GM and white matter (WM) compartments separately by MTI, in SLE patients with a history of NP symptoms without MRI evidence of explanatory focal disease. PATIENTS AND METHODS Twenty-four female patients diagnosed as having SLE according to the 1982 American College of Rheumatology revised criteria (9) and 24 healthy female controls were included in the study (age range 19–65 years in both groups; mean age 35 years in the patient group and 39 years in the control group). All subjects provided written informed consent. Patients were recruited from the Leiden University Medical Center Department of Rheumatology. NPSLE was diagnosed based on clinical findings, after exclusion of other possible causes of NP symptoms (10). The mean duration of SLE was 8 years (range 1–29); time since the onset of NPSLE varied from 1 month to 18 years (mean 5 years). At the time of scanning, no active NP symptoms or concurrent neurologic or psychiatric diseases were present, and there was no indication of previous neurologic or psychiatric disease in any of the subjects. Patients were included only if MRI revealed no abnormalities that could possibly explain a history of NP symptoms. Patient characteristics, specific NP manifestations, and abnormalities on conventional MRI are described in a previous report on the same patient group (6). MRI was carried out with a 1.5T MR scanner (Philips, Best, The Netherlands). Scans were aligned parallel to the axial plane through the anterior and posterior commissure and covered the whole brain in all sequences. Conventional T1weighted spin-echo, fluid-attenuated inversion recovery and dual (proton density and T2-weighted) images (6) were acquired in all patients and interpreted by an experienced neuroradiologist (MAvB). For MTI, a 3-dimensional gradientecho pulse sequence with an echo time/repetition time of 6/106 msec and a flip angle of 12° was chosen, resulting in proton density contrast in the absence of MT saturation pulses (6). A 256 ⫻ 256 matrix with 50% acquisition and 220-mm field of view was used for 28 contiguous 5-mm slices. Two consecutive sets of axial images were acquired, with and without a sincshaped radiofrequency saturation pulse 1,100 Hz upfield of H2O resonance (6). Scanning time for MTI was ⫾11 minutes. The magnetization transfer ratio (MTR) for every Figure 1. Segmented magnetization transfer ratio (MTR) maps of gray matter (GM) and white matter (WM) at 4 different levels. Locations of the axial MTR maps are displayed on sagittal T1weighted magnetic resonance images shown to the left. voxel was calculated by the equation (M0 ⫺ Ms)/M0, with M0 representing the intensity of voxels in a nonsaturated state and Ms the intensity in a saturated state (6) (in-house software; Division of Image Processing, Department of Radiology, Leiden University Medical Center). Using Statistical Parametric Mapping ’99 (Wellcome Department of Cognitive Neurology, Institute of Neurology, London, UK [11]), Ms images were segmented automatically based on a cluster analysis using prior spatial probabilities, signal intensity information, and maximum image inhomogeneity correction. Probability maps for GM, WM, and CSF were inspected visually to confirm ade- Figure 2. Histograms of the magnetization transfer ratio (MTR) (in percent units [pu], after correction for volumes) for gray matter (solid lines) and white matter (broken lines) in healthy controls (gray lines) and patients with neuropsychiatric systemic lupus erythematosus (black lines). MTI STUDY REVEALS GM INVOLVEMENT IN NPSLE 2879 Table 1. MTR histogram parameters and results of univariate analysis and multivariate analysis with age as an additional covariate* Univariate analysis Multivariate analysis Parameter Healthy controls, mean ⫾ SD NPSLE patients, mean ⫾ SD Mean ⫾ SEM difference† P Mean ⫾ SEM difference† P GM PL, pu WM PL, pu GM PH, AU WM PH, AU GM, mean MTR, pu WM, mean MTR, pu 34.4 ⫾ 0.5 37.5 ⫾ 0.6 151 ⫾ 13 189 ⫾ 16 33.6 ⫾ 0.5 37.4 ⫾ 0.5 34.3 ⫾ 0.9 37.9 ⫾ 1.1 136 ⫾ 22 181 ⫾ 23 33.3 ⫾ 1.0 37.8 ⫾ 1.0 0.13 ⫾ 0.21 0.46 ⫾ 0.26 14.6 ⫾ 5.2 8.3 ⫾ 5.6 0.31 ⫾ 0.23 ⫺0.36 ⫾ 0.23 0.553 0.078 0.007 0.146 0.195 0.126 0.25 ⫾ 0.19 ⫺0.35 ⫾ 0.25 16.8 ⫾ 5.1 9.0 ⫾ 5.7 0.46 ⫾ 0.21 ⫺0.25 ⫾ 0.22 0.210 0.165 0.002 0.122 0.033 0.258 * MTR ⫽ magnetization transfer ratio; NPSLE ⫽ neuropsychiatric systemic lupus erythematosus; GM ⫽ gray matter; PL ⫽ peak location; pu ⫽ percent units; WM ⫽ white matter; PH ⫽ peak height; AU ⫽ arbitrary units (corrected for volumes). † Estimated by the least squares method. quate extraction of intracranial contents. To avoid partial volume effect on the segmentation of GM, WM, and CSF, voxels with a ⬎10% probability of belonging to the CSF were excluded. Of the remaining voxels, only those for which the probability of belonging to GM or WM reached ⬎80% were considered for the histogram analysis. Based on these conservative thresholds, binary masks were produced for the GM and WM and were applied to the original MTR maps, producing pure GM and WM MTR maps. From these MTR maps, histograms were generated and the corresponding peak location (PL), peak height (PH), and mean MTR were derived for GM and WM separately. Since the PH is dependent on both lesion load and the physiologic variation in volumes of the different compartments, a volume correction was performed by dividing the number of voxels for each MTR value by the total number of voxels for that tissue type (6). Univariate analyses and multivariate linear regression analyses with age as an additional covariate were performed to test for significant differences in GM and WM MTR parameters between healthy controls and NPSLE patients. Variances in MTR parameters between NPSLE patients and controls were assessed using Levene’s test. P values less than 0.05 were considered significant. RESULTS All images showed an accurate segmentation of GM and WM, as seen in the example presented in Figure 1. The stringent probability thresholds resulted in an exclusion of voxels with partial volume effects at the interfaces of GM, WM, and CSF (Figure 1), providing pure GM and WM MTR maps. WM mean MTR values were higher than those in the GM, although there was considerable overlap of MTR values between GM and WM in both the patient group and the control group (Figure 2). Univariate analysis revealed a significantly lower GM PH in NPSLE patients as compared with healthy controls (P ⫽ 0.007) (Table 1). A subsequent multivariate analysis with age as an additional covariate confirmed the significantly reduced GM PH in NPSLE patients (P ⫽ 0.002), and also revealed a significantly reduced GM mean MTR as compared with healthy controls (P ⫽ 0.033). The degree of variation among the NPSLE patients was significantly greater than that among controls for GM PH (P ⫽ 0.012) and GM mean MTR (P ⫽ 0.005) only. For GM PL and for all WM parameters, no significant differences were observed (P ⬎ 0.05). DISCUSSION Recently, MTI has been applied to detect and quantify global, functionally relevant brain damage in patients with NPSLE (5,6). However, no information on the anatomic distribution of MTI abnormalities has previously been obtained. This is the first study to demonstrate MTI abnormalities indicative of parenchymal brain damage specifically in the GM in SLE patients with a history of NP symptoms but without explanatory focal abnormalities on MRI. When NPSLE patients were compared with healthy controls, differences in volumetric MTR measures indicating loss of structural integrity of tissue were observed in the GM, but not the WM. Moreover, the increased variance of PH and mean MTR values in the NPSLE patients, reflecting variation of cerebral lesion load in this group of patients who were heterogeneous in terms of symptoms and disease duration, was found only in the GM. These findings of GM involvement correspond with results of histologic, immunologic, and other quantitative neuroimaging studies. The exact histologic changes in NPSLE remain unclear. However, several histopathologic studies have demonstrated vasculopathy and microinfarcts in patients with NPSLE (2). Strikingly, the classic histopathologic study by Johnson and Richardson showed vascular changes predominantly in the cerebral cortex and brain stem of SLE patients (12). Moreover, a recent immuno- 2880 chemical study demonstrated increased levels of the light subunit of the neurofilament triplet protein and the glial fibrillary acidic protein in the CSF of NPSLE patients, indicating neuronal and astrocytic degeneration (7). Due to the high concentration of neurons in GM, neuronal and astrocytic damage will probably lead to a decrease of mainly GM structural integrity, which is in accordance with the findings of the present study. Pathogenetically, thrombotic vasculopathy and cerebral infarcts may account for some focal NP syndromes; however, it is unlikely that all diffuse neurologic and psychiatric manifestations in NPSLE are attributable solely to these factors. In fact, there has been a gradual realization that SLE and NPSLE may represent a more diffuse disease process, including nonthrombotic vascular injury at the endothelial level and involvement of complement cascades, cytokines, autoantibodies, and hormones (2). Since GM is more susceptible than WM to many disease processes, such as hypoperfusion (13), it will be particularly affected by any kind of CNS injury. Small-vessel disease itself may also increase blood–brain barrier permeability, which facilitates the entrance of antineuronal antibodies such as the recently identified anti–N-methyl-D-aspartate antibody into the brain parenchyma (2,8). In either case, because of the higher concentration of neurons in GM, the GM will be particularly affected. Abnormal GM has also been observed using spin-spin (T2) relaxation time measurements and MRS (3,4). An increase in T2 relaxation time indicated cerebral edema and significant metabolic disturbance (14), while MRS revealed a decreased N-acetylaspartate:creatine (NAA:Cre) ratio, indicative of neuronal injury (15). With both techniques, however, WM abnormalities in NPSLE patients were also observed. Two explanations with respect to the lack of abnormal MTR findings in the WM in the present study can be suggested. First, our patients may comprise a subgroup of NPSLE patients without WM involvement, since only patients who did not have focal lesions that could explain the history of NPSLE were included. Second, MTI and MRS reflect different histologic conditions. MTI mainly reflects myelin and axonal concentrations, whereas the NAA:Cre ratio is a neuronal marker. If neuronal damage is the dominant underlying histologic change, it comes as no surprise that MTR values in the WM are normal, since in the WM these values are determined mainly by the integrity of myelin and axonal concentrations. In the GM, however, myelin is present in a much lower concentration and therefore contributes less to the observed STEENS ET AL MTR values. The effect of neuronal loss might therefore be easier to detect with MTI in that compartment. It could be argued that decreases in GM MTR could be due to retrograde neuronal degeneration resulting from transection of axons traversing WM lesions. However, no significant differences in WM MTR histogram parameters were observed between NPSLE patients and healthy controls, and therefore it is unlikely that our GM MTR findings are secondary to a WM abnormality. Another potential confounder is the presence of cerebral atrophy, which is known to occur in NPSLE (3,4). Cerebral atrophy increases the number of voxels at the parenchymal cortex containing a mixture of GM and CSF, and classification of those voxels as GM could also have resulted in decreased GM MTR values. However, with the stringent classification thresholds used, partial voluming effects were reduced as much as possible. Patients and healthy controls were matched for age (P ⫽ 0.193 by independent-samples t-test). However, since MTR parameters may be differently associated with age in healthy subjects and SLE patients, a multivariate analysis was performed in which age was included as an additional covariate, thereby reducing the residual variance. The significantly reduced GM PH in NPSLE patients was confirmed in this analysis, and additionally, a significantly reduced GM mean MTR was noted. Both the higher least square mean, estimating the mean difference between the groups, and a lower standard error contributed to this significant difference. A potential difference in association between age and MTR parameters in controls and NPSLE patients will be the subject of further study. In conclusion, this is the first study to demonstrate that in SLE patients with a history of NP symptoms and without explanatory focal abnormalities seen on MRI, damage occurs in the GM. This observation supports the model of neuronal damage in diffuse NPSLE, and can be explained by the greater susceptibility of GM to the sequelae of small-vessel disease or to the presence of antineuronal antibodies, for which new evidence (8) has recently been found. REFERENCES 1. Hermosillo-Romo D, Brey RL. Diagnosis and management of patients with neuropsychiatric systemic lupus erythematosus (NPSLE). Best Pract Res Clin Rheumatol 2002;16:229–44. 2. Scolding NJ, Joseph FG. The neuropathology and pathogenesis of systemic lupus erythematosus. Neuropathol Appl Neurobiol 2002; 28:173–89. 3. Sibbitt WL, Sibbitt RR, Brooks WM. Neuroimaging in neuropsy- MTI STUDY REVEALS GM INVOLVEMENT IN NPSLE 4. 5. 6. 7. 8. 9. chiatric systemic lupus erythematosus. Arthritis Rheum 1999;42: 2026–38. Huizinga TW, Steens SC, van Buchem MA. Imaging modalities in central nervous system systemic lupus erythematosus. Curr Opin Rheumatol 2001;13:383–8. Bosma GP, Rood MJ, Huizinga TW, de Jong BA, Bollen EL, van Buchem MA. Detection of cerebral involvement in patients with active neuropsychiatric systemic lupus erythematosus by the use of volumetric magnetization transfer imaging. Arthritis Rheum 2000; 43:2428–36. Bosma GP, Middelkoop HA, Rood MJ, Bollen EL, Huizinga TW, van Buchem MA. Association of global brain damage and clinical functioning in neuropsychiatric systemic lupus erythematosus. Arthritis Rheum 2002;46:2665–72. Trysberg E, Nylen K, Rosengren LE, Tarkowski A. Neuronal and astrocytic damage in systemic lupus erythematosus patients with central nervous system involvement. Arthritis Rheum 2003;48: 2881–7. DeGiorgio LA, Konstantinov KN, Lee SC, Hardin JA, Volpe BT, Diamond B. A subset of lupus anti-DNA antibodies cross-reacts with the NR2 glutamate receptor in systemic lupus erythematosus. Nat Med 2001;7:1189–93. Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield 2881 10. 11. 12. 13. 14. 15. NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1982;25:1271–7. ACR Ad Hoc Committee on Neuropsychiatric Lupus Syndromes. The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum 1999;42:599–608. Ashburner J, Friston KJ. Voxel-based morphometry: the methods. Neuroimage 2000;11:805–21. Johnson RT, Richardson EP. The neurological manifestations of systemic lupus erythematosus. Medicine (Baltimore) 1968;47: 337–69. Takahashi S, Higano S, Ishii K, Matsumoto K, Sakamoto K, Iwasaki Y, et al. Hypoxic brain damage: cortical laminar necrosis and delayed changes in white matter at sequential MR imaging. Radiology 1993;189:449–56. Sibbitt WL, Brooks WM, Haseler LJ, Griffey RH, Frank LM, Hart BL, et al. Spin-spin relaxation of brain tissues in systemic lupus erythematosus: a method for increasing the sensitivity of magnetic resonance imaging for neuropsychiatric lupus. Arthritis Rheum 1995;38:810–8. Brooks WM, Sabet A, Sibbitt WL, Barker PB, van Zijl PC, Duyn JH, et al. Neurochemistry of brain lesions determined by spectroscopic imaging in systemic lupus erythematosus. J Rheumatol 1997;24:2323–9.