Standards for Low Secure Services
advertisement

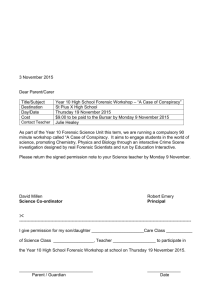
Standards for Low Secure Services CCQI publication number: CCQI 130 Editors: Sarah Tucker, Maddy Iqbal and Sam Holder Date: June 2012 The Quality Network ran a competition to find a piece of service user artwork to use on annual reports, standards and leaflets. This design was painted by a service user from Edenfield Centre. The team would like to thank all of the service users who submitted entries. Contents Page Preface 4 Method 5 A: Model of Care 7 1: 2: 3: 4: Admission Recovery Physical Health Care Discharge B: A Safe Therapeutic Environment 1: Physical Security 2: Relational Security 3: Procedural Security C: Service Environment 1: 2: 3: 4: 5: Environmental Design Risk assessment and management De-escalation and seclusion Access to external spaces Facilities for Visitors D: Workforce 1: Capacity and capability 2: Training and continuing professional development E: Governance 1: Reporting and management of adverse incidents 2: Business Continuity F: Equalities Appendix Appendix Appendix Appendix 3 1: 2: 3: 4: 7 8 10 11 12 12 13 14 17 17 17 18 19 19 20 20 20 23 23 23 25 Delegates, Standards Working Group Delegates, Standards Consultation Event Advisory Group Project Team 26 26 26 26 Preface It is a pleasure to welcome these Standards for Low Secure Services developed by the Quality Network. The Quality Network has worked closely with the Department of Health following the consultation on ‘The Good Practice Commissioning Guide for Low Secure Services’ which will provide guidance. These standards will form the basis of the self-and peer-reviews in the recently launched Quality Network’s dedicated low secure network. They are an accessible way for services to engage in comprehensive on-going service development and improvement for the benefit of patients in line with Department of Health policy. This new network will build on the Quality Network’s successful work with medium secure services over the past six years. This work has been valued by the specialised service commissioners and has provided demonstrable benefits in terms of quality improvement. The dedicated quality network for low secure services has the potential to further develop standards for these services and through the peer-review process further improve quality. Over the next year commissioners will be working closely with the Quality Network for Forensic Mental Health Services to use these standards to provide an on-going national structure for quality assurance and improvement in low secure services. Ged McCann Phil Brian Associate Director of Commissioning, Yorkshire and Humber Office, North of England Specialised Commissioning Group, Forensic and Secure Clinical Reference Group Assistant Director (Specialised Mental Health), West Midlands Office Midlands and East Specialised Commissioning Group, Advisory Group Quality Network for Forensic Mental Health Services 4 Method Context This third consultation draft of Standards for Low Secure Services has been developed by the Quality Network for Forensic Mental Health Services directly from the ‘Low Secure Services: Good practice commissioning guide – consultation draft’ Department of Health, February 2012. In addition some standards from the ‘Implementation Criteria for Recommended Specification: Adult Medium Secure Units’ (second edition CCQI 105) have been included. These standards have been developed with the purpose of forming the basis of the self- and peer-review questionnaires for the Quality Network for Forensic Mental Health Services low secure services self- and peer-reviews. Forming the foundation of the iterative annual review cycle the standards provide an accessible way for services to actively engage in on-going service development towards implementing the Department of Health recommendations. The Development of the Standards The standards have been developed in the following ways and stages: 1) The tense and where appropriate, the sentence structure of the Department of Health ‘Low Secure Services: Good practice commissioning guide – consultation draft’ has been edited. This provides user-friendly and easily accessible questions for use in self- and peer-review questionnaires. 2) Where these standards capture more than one criterion, the standard has been divided into separate criteria. This prevents ambiguous answers. 3) Where these standards make an ideal statement (e.g. ‘There should be….’) this has been edited to a statement of fact (e.g. ‘There is….’). This provides more user-friendly standards for the peer-review questionnaires. 4) The Standards for Low Secure Services have been mapped on to the Quality Network’s Implementation Criteria for Recommended Specification: Adult Medium Secure Units’. This enables comparison and avoids potential duplication. 5) The Standards for Low Secure Services have been mapped onto the Care Quality Commissions ‘Essential Standards of Quality and Safety’ (March 2010)1. This enables services to streamline the data collection process. The references denote the Outcome, Regulation and Prompt number onto which the implementation criteria have been mapped, following the format: Outcome Number, Regulation Number. Prompt Number, e.g. 1.17.1a denotes Outcome 1, Regulation 17, Prompt 1a. 6) On 27 March 2012 the Quality Network consulted an expert standards working group on a first consultation draft of these standards (see Appendix 1). Members of the working group were asked to identify omissions and to comment on clarity, measurability and importance. On the basis of feedback from this working group the Quality Network edited a second draft of the standards. 7) On 31 May 2012 the Quality Network consulted more widely at a standards consultation event on the second draft of these standards (see Appendix 2). Members of the event (which included patients) were asked to identify omissions, in particular, those in the ‘Implementation Criteria for Recommended Specification: Adult Medium Secure Units’ which did not appear in the Low Service Standards). Members were also asked to comment on clarity, measurability and importance. On the basis of feedback from this event the Quality Network edited this third edition of the standards. 1 http://www.cqc.org.uk/_db/_documents/Essential_standards_of_quality_and_safety_FINAL_081209.pdf 5 6 No. DH Guidance LSU Standard Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care A: Model of Care 1: Admission There are clear admission procedures which centre on a multi-disciplinary assessment process taking account of a patients’ care, treatment (including physical health treatments) and security needs. There are clear inclusion criteria for the admission of patients to the unit which include all of the following: i. A definable clinical risk to others or a legal requirement to be in custody ii. Men and women aged 18 years and over and detained under the Mental Health Act. iii. Prisoners or Immigration Act detainees meeting the criteria for detention under the Mental Health Act. iv. People who will benefit from a period of rehabilitation. v. People who may require a long period of rehabilitation. vi. People who may have a history of offending behaviour with low levels of violence for example assault. vii. People who do not require the degree of security provided by medium or high secure care. viii. People with challenging behaviour. ix. People with co-morbid substance misuse issues (past or current). There are clear exclusion criteria for the admission of patients to the unit which include all of the following: i. People under 18 years who do not meet criteria for detention under the Mental Health Act or require treatment in a specialist service for children and adolescents. ii. People with a primary diagnosis of substance misuse without a secondary diagnosis of mental illness, who are not engaging with substance misuse interventions. iii. People requiring detention in medium or high security. iv. People with complex needs who can be managed and treated in adult services including psychiatric intensive care or rehabilitation services. A1.1 A1.2 A1.3 7 27 26 28 29 4.9.4l 5.14.5a A97 A96 A85 G3 B7 No. DH Guidance LSU Standard Patients who receive low secure services also receive an assessment for additional specialist treatment if they have a primary diagnosis of dementia, a learning disability of sufficient severity to preclude them from actively engaging, personality disorder, acquired brain injury or other neuro-cognitive deficits, Asperger’s and autistic spectrum disorder. Where low secure care is not considered the most suitable option for an individual, service staff offer advice and guidance on the management of the patient where applicable. A1.4 A1.5 A1.6 The provider identifies the responsible local commissioner for every individual planned admission, even where the service user is known to the service. A1.7 All patients will have an initial care plan in place within 24 hours of admission. 30 A1.9 4.9.4b 4.9.4d 4.9.4n 6.24.6c 31 4.9.4p B9 A95* All patients have a link person/care co-ordinator from their home area services whose responsibilities include the facilitation of ongoing links and the patient’s care pathway. There are clear criteria for admission to and transfer /discharge from services which will be agreed with commissioners and will be communicated to all referrers. The service ensures that the discharge procedures are operated in line with the pathway (appendix 4). A1.8 Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 6.24.6a 6.24.6b 7.11.7b B10* 4.9.4c 4.9.4o 6.24.6a 6.24.6e 6.24.6g 7.11.7e E2* B13 A80 B2 2: Recovery A2.1 Using the Care Programme Approach (CPA), the multi-disciplinary team takes a comprehensive, recovery-focussed approach aimed at building resilience and preventing relapse. 32 1.17.1a 1.17.1b 1.17.1c 2.18.2a 4.9.4a 4.9.4e 4.9.4g 4.9.4n 4.9.4r 6.24.6a 16.10.16d 21.20.21a A2.2 The recovery-focussed approach includes addressing accommodation, employment and learning needs, meaningful social contact and combating stigma. 32 1.17.1m 4.9.4a A94.5 A107 A2.3 The service makes provision for men and women aged over 18 years and complies with national guidance about and expectations governing the provision of single sex accommodation. 16 1.17.1a 4.9.4f 10.15.10a 10.15.10l E6 E7 F2w F3w F4w F9w 8 No. Standard There is evidence that the model of care and treatment focuses on risk management, engagement and rehabilitation within a safe and secure environment. A2.4 There are facilities for detained patients including those who require short periods of intensive care within a low secure environment. There is provision for patients requiring a period of engagement and treatment away from the main patient group. This may include the provision of 1.17.1h (Essential Standards of Quality & Safety, CQC, 2010) for de-escalation and seclusion. A2.5 A2.6 There are a variety of recreational activities and occupational facilities available. A2.7 There is a dedicated secure external garden/court yard which can be used for recreational activities. There are effective links with community organisations (e.g. housing, leisure, employment, education) and activities to support rehabilitation and sustainable discharge. A2.8 A2.9 DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) 17 1.17.1a 1.17.1b 1.17.1c 1.17.1f 1.17.1j 4.9.4a 4.9.4c 4.9.4e 7.11.7g 16.10.16b 16.10.16d 19 1.17.1h 20 1.17.1h 21 1.17.1h 4.9.4a 10.15.10a 21 10.15.10a 10.15.10m 21 1.17.1m 6.24.6a 6.24.6c 7.11.7b 1.17.1a 1.17.1b 1.17.1c 1.17.1f 1.17.1j 4.9.4a 4.9.4c 4.9.4e 7.11.7d 16.10.16d 1.17.1a 1.17.1b 4.9.4a 16.10.16c 16.10.16d 1.17.1c 2.18.2a 2.18.2b 4.9.4c 21.20.21a A2.10 There is evidence that the service places the patient at the centre of their care, supporting patient recovery and choice within the unit where this is clinically appropriate. 23 A2.11 Patients engage and participate in the formulating of, and ongoing review of, a multidisciplinary therapeutic evidence-based programme appropriate to their individual needs. 24 A2.12 Patients are given a copy of the management or care plan. A2.13 There is a core day described in each patient's individualised care plan (a description of the core day may also be found elsewhere e.g. in the ward programme or individual timetables). A2.14 Patients receive information about medication and its side effects. 25 1.17.1a 1.17.1e 4.9.4e 9.13.9d 16.10.16b A2.15 Treatments take into account the relevant NICE guidance. 25 2.18.2d 9 Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care A93 C3 C32 D9 A94.1 A94 C22 D20 D2 D9 D19 A113 A100 A101 A10w No. A2.16 The programme of treatment includes psychological sessions. A2.17 The programme of treatment includes substance misuse therapy. A2.18 A2.19 A2.20 A2.21 A2.22 A2.23 A2.24 DH Guidance LSU Standard Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care A94.2* 1.17.1l 4.9.4n 4.9.4o The programme of treatment includes offence related therapy. The programme of treatment includes structured activity programmes. The programme of treatment includes structured leisure time. The programme of treatment includes unstructured free time. There are facilities appropriate to the patient group, e.g. a pool table and board/console games are provided. There are facilities for patients to make their own hot and cold drinks and snacks. Books and magazines are provided in recreation areas for patients. A94.3* A94.4* A94.6* A94.7 A94.8* 1.17.1h F12 5.14.5c F13 F14 3: Physical Health Care A3.1 A3.2 A3.3 A3.4 A3.5 A3.6 A3.7 A3.8 A3.9 A3.10 A3.11 Patients routinely undergo a full assessment of both physical and mental health needs. Care and treatment plans reflect both mental health and physical healthcare needs. Patients have access to a comprehensive range of primary healthcare services. Patients undergo follow-up investigations and treatment for physical conditions identified in their assessment during their admission. Patients have routine monitoring of medication including those used for physical health issues. Patients are supported in their personal care including dental hygiene. The service meets screening targets expected of primary care services. The service provides general health promotion activities including screening, diet advice and the opportunity to exercise (with appropriate supervision). The service provides targeted programmes on smoking cessation and health promotion. There is an identified duty doctor available at all times to attend the unit. Patients have access to comprehensive primary and secondary care services to meet existing or newly developed physical healthcare and treatment needs. 10 G3 A89 A1w 34 35 6.24.6c G3.1 35 1.17.1i 6.24.6i G1 G5 35 6.24.6c G4 35 9.13.9a 9.13.9b 9.13.9d 6.24.6j G5 G4w 36 36 D1* 1.17.1e 4.9.4a 5.14.5a 5.14.5c 36 G5 G11 G15 G12 G13 F10 G4w G6 B31 22 1.17.1e 1.17.1i 4.9.4a 4.9.4p 6.24.6i 6.24.6j G1 G5 G4 No. DH Guidance LSU Standard Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 4: Discharge A4.1 A4.2 A4.3 A4.4 A4.5 A4.6 A4.7 Social workers, care coordinators and offender managers are actively involved in care planning processes for treatment on the unit and postdischarge follow-up under Section 117 arrangements. Discharge targets are agreed as part of the discharge planning process. There is a multi-disciplinary assessment to determine readiness for discharge/transfer. The multi-disciplinary team supports the patient to develop and maintain links with community-based organisations that can provide socially inclusive, mainstream activities. The provider facilitates links to the home area services of each patient in terms of local statutory (health and social care) and voluntary services and maintains these to ensure timely and appropriate discharge/transfer arrangements are put in place. When a patient needs to transfer to services for older people, a joint review is undertaken to ensure effective hand-over takes place. The service ensures there are regular reviews for patients transferred from prison (a) on remand (b) on sentence to assess suitability for return to prison. 11 33 6.24.6c A123 A121 33 4.9.4c B15* 1.17.1m 4.9.4a 6.24.6c 6.24.6i 7.11.7b C22 4.9.4a 4.9.4c 6.24.6i B11* 4.9.4c A122 4.9.4c 16.10.16c B21* No. Standard DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care B: A Safe Therapeutic Environment B1 B2 B3 There is evidence that the three domains of security (physical, relational and procedural) are developed and managed in unison. There is evidence that the three domains of security (physical, relational and procedural) are used to inform decisions about individual/population care. The balance in emphasis between each domain of security (physical, relational and procedural) changes given the operational needs of the unit as a whole, or the needs of a particular patient and/or group of patients, and the setting in which the service is provided. 40 10.15.10c 40 10.15.10c 41 10.15.10c 42 10.15.10c A1 47 10.15.10a 10.15.10d A10 A18 A19.2 48 10.15.10a A15 A15.1 A15.3 49 10.15.10a 1: Physical Security B1.1 B1.2 There is a clearly delineated external perimeter. The external perimeter is designed to maintain service integrity, privacy, eliminate climb points and manage risk. (The exact nature of the external perimeter, for example fence height, cladding, angled weld mesh topping, and anti-climb capping, is determined by the size, layout and location of the low secure service). B1.3 B1.4 B1.5 B1.6 B1.7 B1.8 B1.9 B1.10 B1.11 Gates within the perimeter do not have bolts or opening mechanisms that can be used as footholds to assist climbing. Where fencing forms all or part of the secure external perimeter, it conforms to BS358 and is a minimum height of 3 metres. Access to the low secure unit for visitors, staff and patients is via an airlock. There is evidence that the secure external perimeter is regularly checked. There is a clearly defined internal perimeter (normally bounded by the secure doors leading to outside areas), which facilitates patients’ freedom of movement within the internal perimeter area. There are systems in place to ensure that buildings, equipment and technology are well maintained. Lockers are provided for staff away from the patient area for the storage of any items not allowed on the unit. All keys, including those held at reception, are controlled, issued and accounted for. All keys held by reception are accounted for at least twice in a 24-hour period. 12 53 A31 43 A4 46 42 10.15.10d 50 7.11.7m 10.15.10c 10.15.10f A7 A7.1 A20.1 F5 51 A13 A28 51 A28.1 No. B1.12 B1.13 B1.14 B1.15 B1.16 B1.17 B1.18 B1.19 B1.20 B1.21 Standard Access to spaces where sharp implements e.g. kitchen knives, utensils, equipment or tools are available are to be controlled. The use of sharp implements is monitored. There is evidence that the staff team have current knowledge and understanding of the units’ physical security measures and mechanisms. There is evidence that the staff team have current knowledge and understanding of the procedures that support the units’ physical security measures and mechanisms for effective operation. There is evidence that the staff team have current knowledge and understanding of their own security responsibilities and those of the wider team. There is evidence that the staff team have current knowledge and understanding of how relational and procedural measures impact on physical security. There is evidence that the staff team have current knowledge and understanding of what constitutes the internal perimeter. There is evidence that the staff team have current knowledge and understanding of alarm systems including those used for staff/patient safety and fire. DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 52 11.16.11c A71 52 11.16.11c A71 45 10.15.10c A92 C6 45 10.15.10c A92 C6 45 10.15.10c C4 45 10.15.10c 45 10.15.10c 45 4.9.4d 5.14.5a 7.11.7a 7.11.7d 7.11.7k 9.13.9g 10.15.10a 10.15.10b 10.15.10e 10.15.10g 10.15.10h 14.23.14a C7 10.15.10p F9.1* There is a system in place for staff to report any ligature points identified with prompt follow up action. There is a full-time security lead. A41* 2: Relational Security B2.1 B2.2 B2.3 B2.4 B2.5 There is evidence that staff have a knowledge and understanding of their patients and of the environment, and of the translation of that information into appropriate responses and care. There is evidence that the entire staff team works cohesively. This includes staff who do not have direct patient contact. All staff have an up to date enhanced CRB check. There are clear and effective systems for communication and handover within staff teams. There are regular multi-disciplinary team meetings for clinical matters and administration, and the team is consulted on relevant management decisions such as developing and reviewing operational policy. 13 55 6.24.6b 22.4.22b 50 12.21.12a 12.21.12d A88* 12.21.12b A102 16.10.16c 16.10.16d 23.5.23a 24.6.24a A103 No. Standard DH Guidance LSU There are regular meetings where staff discuss and reflect on relational security issues. B2.6 B2.7 B2.8 This includes as a minimum: discussion of boundaries, therapy, patient mix, patient dynamic, patient’s personal world, physical environment, visitors and other external communication and may be facilitated by the See, Think, Act Relational Security Explorer. All staff can demonstrate an understanding of their role in relation to meeting the complex needs of patients. The induction training programme covers relational security. This includes as a minimum material on: boundaries, therapy, patient mix, patient dynamic, patient’s personal world, physical environment, visitors and other external communication. This may be facilitated by the See, Think, Act training slides. Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 7.11.7g 12.21.12b B30 12.21.12a A108 12.21.12b 14.23.14a C5 There is annually updated staff training on relational security. B2.9 B2.10 B2.11 This includes as a minimum material on: boundaries, therapy, patient mix, patient dynamic, patient’s personal world, physical environment, visitors and other external communication. This may be facilitated by the See, Think, Act training slides. A92 Contact with visitors and other external communication is regularly risk assessed. There is a mechanism for measuring and monitoring relational security against established outcomes such as those in ‘See Think Act: Your guide to Relational Security’ (DH 2010). 7.11.7h 16.10.16b A51, A72, A93, C3 2.18.2d 22.4.22c C17 7.11.7h RS. RS. RS. RS. RS. 1.17.1m A107 1.17.1m A94.5* 64 10.15.10h A50 65 2.18.2d 22.4.22b 22.4.22c 66 10.15.10h Please refer to ‘We know we are getting it right when:’ sections in See, Think Act B2.12 B2.13 B2.14 Staff have an understanding of their role in relation to Relational Security in respect of the alcohol and controlled or illegal substances policies. 101 The unit has access to a range of education professionals which include teachers, a special educational needs co-ordinator, an educational psychologist, and career guidance. The programme of treatment includes access to real opportunities to work. 1 2 3 4 5 3: Procedural Security B3.1 B3.2 B3.3 There is an up to date index of procedural security policies used in the low secure service, including contingency and business continuity plans. Policies and procedures acknowledge the need for proportionality and discretion and are in accordance with the Mental Health Act Code of Practice and guidance issued by NICE and professional associations. Policies, procedures and contingency plans are reviewed at least annually and updated where required. 14 A50.1 No. Standard B3.4 Staff have ready access to and demonstrate up to date knowledge of policies and procedures governing the service and guiding their practice. B3.5 There are operational policies and procedures governing, but not limited to, the safety of patients, visitors and staff, risk, adverse incidents and operational management. B3.6 B3.7 B3.8 B3.9 B3.10 B3.11 B3.12 B3.13 B3.14 B3.15 B3.16 B3.17 B3.18 B3.19 B3.20 In addition to organisation-wide policies, there are specific policies and procedures tailored to meet the needs of the low secure service. These policies are authorised by the wider organisation’s senior management structure or board. Staff, patients and visitors feel safe on the unit. Staff, patients and visitors are clear about rules and policies governing any prohibited items including cameras and electronic devices and other items that may be restricted such as mobile phones. There are policies governing access to and appropriate use of the internet by staff and patients. Policies governing access to and appropriate use of the internet by staff and patients contain particular advice around the appropriate use of social networking sites, confidentiality and risk. There is a readily available policy for the authorisation and governance of practice of, searching patients, patient rooms, communal areas and visitors. This policy is in accordance with the requirements of the Mental Health Act Code of Practice. There is a policy on observation. There is an anti bullying policy (for those who are bullying and those who are bullied). There is a policy on prevention of suicide and management of self harm. There is a policy on transportation of patients (e.g. to court or acute hospital). DH Guidance LSU 66 15 C4 58 4.9.4b 6.24.6d 7.11.7a 9.13.9b 10.15.10b 10.15.10e 59 23.5.23a 24.6.24a F2 A93 A124 A125 60 60 10.15.10c A72 A73 F15 61 61 2.18.2a A73 F15 62, 63 22.4.22c A51 A55* 7.11.7a 14.23.14d A56* 4.9.4l A57* A58* There is a policy on the control of prescribed medication and drugs. The unit has a robust policy on the use of and access to alcohol and controlled or illegal substances by patients and their visitors. Policies regarding alcohol and controlled or illegal substances cover the role of Relational Security. Policies regarding alcohol and controlled or illegal substances cover the management of incidents where drugs and alcohol are brought in by patients and their visitors. There is a policy on the prosecution of offences within the unit which is agreed with the police and CPS. Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 101 9.13.9a 9.13.9b 9.13.9d 9.13.9e 9.13.9f 9.13.9g A64* 1.17.1l A62 A63 101 101 9.13.9b A65* No. B3.21 B3.22 B3.23 B3.24 B3.25 Standard There is a smoking policy. There is a policy on the management of patient’s monies. There is a policy on the censorship of material including pornography. There is a policy on the control of mail and use of telephones. There is a policy on visiting procedures including child protection issues. B3.26 There is a policy on patient confidentiality. B3.27 There is a policy for managing critical incident reviews. B3.28 There is a policy for response to staff alarms. There is a policy on child visiting/child contact which is annually reviewed. There is a policy on safeguarding children which complies with National Quality Principles which is reviewed annually. There is a clear written policy for referrals, admissions, transfers and discharges. There are clear policies on disciplinary and grievance procedure; whistle blowing policy, discrimination, harassment, bullying and violence. B3.29 B3.30 B3.31 B3.32 B3.33 There is a clear complaints procedure. B3.34 There is a procedure regarding obtaining consent from patients. B3.35 B3.36 DH Guidance LSU The procedure for resuscitation of patients is clearly documented, resuscitation equipment is available and its location is clearly identified. Staff demonstrate a working knowledge of mental health legislation and its application including their authority in relation to escorting patients outside the secure perimeter. 16 Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care A67* 7.11.7m A68* A69* 10.15.10k A70* 7.11.7e A74* 2.18.2a 6.24.6b 6.24.6e 4.9.4b 6.24.6d 16.10.16b 16.10.16c A75* A76* A83 A128* 7.11.7a 22.4.22b A129* 4.9.4c 7.11.7e B8* 7.11.7a 14.13.14d 16.10.16b C11* 1.17.1h 6.24.6f 7.11.7a 16.10.16a 17.19.17a 17.19.17e 2.18.2a 2.18.2b 2.18.2c 2.18.2h 6.24.6e 11.16.11a 11.16.11c 11.16.11d 11.16.11h 67 12.21.12b 22.4.22c C1* A81 A82 C38 No. Standard DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care C: Service Environment 1: Environmental Design C1.1 C1.2 C1.3 C1.4 C1.5 C1.6 C1.7 C1.8 C1.9 C1.10 C1.11 C1.12 C1.13 C1.14 There is evidence of active planning for and consideration of the impact on the therapeutic environment and safety of ward size and layout, patient numbers and population. The patient and staff environment is homely, light and bright. All accommodation is provided in single rooms, with all new builds and upgrading programmes providing ensuite accommodation. There is a designated dining area. There is a multi-faith room available for use by all patients. There are unrestricted lines of sight and no concealed unsecured areas. Furnishings minimise the potential for fixtures and fittings being used as weapons, barriers or ligature points. Doors in rooms used by patients have observation panels with integrated blinds/obscuring mechanisms. These can be operated by patients with an external override feature for staff. Staff can override any locks that are lockable from the inside e.g. patient bedrooms and bathrooms. Patient bedroom and bathroom doors are designed to prevent holding, barring or blocking. There are lockable facilities (with staff override feature) for patient’s personal possessions with maintained records of access. Patients have access to a telephone in a private area, within the limits of safety and risk assessment. Patients can wash and use the toilet in privacy unless clinical risk prevents this. There is a cleaning programme which is regularly audited. 68 7.11.7g 10.15.10f 10.15.10i 10.15.10a 69 10.15.10a F16 F17 A45 4.9.4f 10.15.10f 10.15.10l F3* 5.14.5f F11 1.17.1i D7* 69 10.15.10p A46 70 10.15.10p 71 73 73 7.11.7m 10.15.10c A66 7.11.7h D15 10.15.10f 10.15.10m F3.1* 8.12 F1.1* 76 4.9.4a 4.9.4l 4.9.4n 5.14.5a A99 A89 76 6.24.6c 16.10.16b 74 2: Risk assessment and management C2.1 C2.2 There is evidence of a multi-disciplinary approach to the identification, assessment and management of risk. Individual risk management programmes are developed to identify the types of supervision, therapeutic intervention and treatment required. 17 No. Standard DH Guidance LSU C2.3 Risk management programmes can be readily adapted to meet a changed risk assessment resulting from adverse incidents, observed behaviour or concerns about security. 77 C2.4 Risk assessment and management is informed by relational security issues. 78 C2.5 C2.6 C2.7 C2.8 There is an agreed approach to risk assessment including which planning tools are used. All staff working directly with patients are trained to incorporate risk identification and management into individual care, treatment and support plans. Staff are skilled at identifying and assessing potential risk factors/situations, planning how to manage identified risks and managing identified risks. Risk reduction is assessed and evidenced through setting and monitoring treatment outcomes. These outcomes inform discussions with the Ministry of Justice (MoJ) regarding restricted patients, transferred prisoners and/or MAPPA (where relevant) and subsequent decisions about: i. escorted, unescorted or trial leave ii. rescinding leave iii. failure to return from leave and absconding iv. remission to prison v. transfer to higher level of security vi. discharge pathways vii. s117 follow-up care requirements viii. preparation for Community Treatment Order (CTO) arrangements. Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 4.9.4n 6.24.6d 7.11.7h 9.13.9b 10.15.10c 14.23.14d 16.10.16b 7.11.7h 10.15.10c 16.10.16b 79 7.11.7h 16.10.16b 81 13.22.13a 16.10.16b A86.1 81 13.22.13a 14.23.14a 16.10.16b A86.1 82 6.24.6b 16.10.16b 16.10.16d A115 A116 A117 A118 A119 83 4.9.4q 7.11.7b 7.11.7f 7.11.7g 7.11.7h 14.23.14d A52 A53 A2w 84 1.17.1a 1.17.1h 7.11.7i 10.15.10a 10.15.10f E6 A3w 85 4.9.4q 86 9.13.9a 9.13.9b 9.13.9d 9.13.9e 9.13.9g 3: De-escalation and seclusion C3.1 C3.2 C3.3 C3.4 There are clear policies and procedures governing the use of de-escalation techniques and the management of challenging behaviour including the appropriate use of control and restraint and of seclusion. There is evidence that the service has considered how best to provide appropriate de-escalation facilities and considered the need for providing an en-suite seclusion room that will maintain the patient’s safety, privacy and dignity. Seclusion is only used as a last resort, and for the shortest clinically appropriate period. Its use is monitored according to the Mental Health Act Code of Practice. Where required rapid tranquilisation complies with NICE guidance (http://www.nice.org.uk/nicemedia/pdf/cg025fullguidel ine.pdf) 18 A54 No. DH Guidance LSU Standard Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 4: Access to external spaces C4.1 C4.2 Access for patients to outside areas including secure gardens and courtyards is determined by an individual risk assessment and takes account of all factors that may assist escape, e.g. weather. Staff facilitate safe access for patients to outside areas including those on s17 leave by implementing the following safeguards: i. Consideration of appropriate staff supervision (numbers and skill mix) given the mix and number of patients outside or on leave at any one time. ii. Retaining appropriate staffing levels and skill mix on the unit whilst patients are outside or on leave. iii. Provision of appropriate escorts given the nature, purpose and location of leave. 87 7.11.7h 10.15.10c 10.15.10m 88 1.17.1m 14.23.14c A60 A61 5: Facilities for Visitors C5.1 There are facilities for visitors within the secure perimeter. 89 10.15.10a C5.2 There are separate, appropriately furnished facilities for children’s visits. 89 10.15.10a 91 7.11.7m 10.15.10c C5.4 C5.5 C5.6 There are lockers for visitors away from patient areas to store prohibited or restricted items whilst they are on the unit. All visitors access the unit by the main reception airlock. The unit works with visitors and families on their health and well being, for example, coping with stress, conflict resolution and sustainable transport plans for visiting. 19 A128.1 A12w A13w 91 D12* No. Standard DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care D: Workforce 1: Capacity and capability D1.1 D1.2 D1.3 D1.4 D1.5 D1.6 D1.7 There is a cohesive multi-disciplinary team in place who have the capacity and capability required to meet the complex needs of patients. There is a robust leadership structure in place which sets out professional, organisational and line management accountabilities. The staffing capacity is sufficient to deliver the care and treatment model and maintain a safe environment at all times. The unit is staffed by permanent staff and agency staff are used only in exceptional circumstances. Extra nursing cover is available when needed, e.g. there is access to additional on-call staff in an emergency. The staff mix and ratios are sufficiently flexible to meet the changing levels of risk. The multi-disciplinary team includes: medical staff nursing staff social workers pharmaceutical staff psychologists art therapist psychotherapist occupational therapist and education professionals. 92 13.22.13a A104 B17 B18 92 23.5.23a 24.6.24a C27 C27.1 93 7.11.7b 7.11.7g 13.22.13a A110 B18 A112 A111 93 13.22.13a 94 A86.1 B18 A104 D1.8 The service has the capacity to respond to patient need and gender specific issues. 95 1.17.1h 12.21.12b 13.22.13a A1w C4.1w E6w E7w D1.9 All staff have a working knowledge of mental health legislation and its application. 96 12.21.12b 22.4.22c C38 2: Training and continuing professional development D2.1 The multi-disciplinary team has the capacity and capability to provide a range of multi-disciplinary therapeutic interventions and clinical treatments within the agreed model of care. 97 13.22.13a D2.2 The staff at the service have completed the training and education recommended by their professional association or regulatory body. 97 12.21.12b 14.23.14.a 20 C15 No. Standard DH Guidance LSU D2.3 The staff at the service have completed the mandatory and appropriate non-mandatory training provided by the organisation. 97 D2.4 There is a system in place to continually identify and review staff training needs on an annual basis. 97 D2.5 Training needs are monitored within the staff appraisal system. 97 D2.6 D2.7 There is annually reviewed training and development strategy, which includes the provision of security training. There is a strategic plan for training, encompassing all known initiatives and that is subject to regular review. D2.8 All staff receive supervision on a monthly basis. D2.9 All staff receive training regarding Safeguarding Children and Safeguarding Vulnerable Adults. D2.10 D2.11 D2.12 D2.13 D2.14 D2.15 D2.16 D2.17 All staff receive equality awareness training. Staff receive training on Physical Security as part of the induction programme and prior to being issued with keys, swipe cards or other means of operating Physical Security mechanisms. Staff receive training on Procedural Security as part of the induction programme and prior to being issued with keys, swipe cards or other means of operating Physical Security mechanisms. Staff receive training on Relational Security as part of the induction programme and prior to being issued with keys, swipe cards or other means of operating Physical Security mechanisms. All staff including non clinical staff receive training in the management of violence and aggression. Training addressing the management of violence and aggression includes de-escalation techniques and the use of control and restrain procedures. All staff have a working knowledge of mental health legislation and its application. Training is provided on disciplinary and grievance procedure; whistle blowing policy, discrimination, harassment, bullying and violence policies. 21 97 97 97 Essential Standards of Quality & Safety (CQC – March 2010) 4.9.4d 5.14.5a 7.11.7a 7.11.7d 7.11.7k 9.13.9g 10.15.10b 10.15.10e 10.15.10g 10.15.10h 14.23.14a 4.9.4d 12.21.12a 12.21.12b 14.23.14a 14.23.14c 4.9.4d 12.21.12a 12.21.12b 14.23.14a 14.23.14c Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care C7 A90.1 B24 A90.1 14.23.14.a A91* 12.21.12b 14.23.14a C18.1* 14.23.14c A90 B28 7.11.7a 7.11.7e 7.11.7i 12.21.12b 22.4.22b 12.21.12b A130 A15w C10 97 12.21.12b 14.23.14a C5 97 12.21.12b 14.23.14a C5 97 12.21.12b 14.23.14a C5 97 12.21.12b 14.23.14d C8 97 12.21.12b 14.23.14d C9 97 12.21.12b 22.4.22c C38 12.21.12b 14.23.14.a 14.23.14d 16.10.16b C11.1* No. D2.18 D2.19 D2.20 D2.21 D2.22 D2.23 D2.24 Standard Training is provided on the management of relationships between patients and between patients and staff. Training is provided on the user perspective and user participation. Staff are made aware of complaints that are relevant to their work and the outcome of the complaints process. Staff take up of supervision and support is regularly monitored and audited. Frontline staff have regular supervision totalling at least one hour per week and are able to contact a senior colleague as necessary. There are records of robust clinical supervision. There is adequate time made available for supervision to be delivered. 22 DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care 12.21.12b 14.23.14.a C13* 12.21.12b 14.23.14.a C14* 16.10.16a 16.10.16c 17.19.17a D14 12.21.12b 14.23.14c B27 12.21.12b 14.23.14c B29 14.23.14c C20* 14.23.14c C20.2* No. Standard DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care E: Governance 1: Reporting and management of adverse incidents E1.1 E1.2 E1.3 E1.4 E1.5 There is a structure in place for reporting, managing and investigating Serious and Untoward Incidents (SUIs). The unit’s senior management are accountable for the unit’s Serious and Untoward Incident reporting, managing and investigating structure. The unit uses the Department of Health and NPSA definition of a Serious and Untoward Incident to define SUIs within the service: ‘The definition of an adverse incident is an event or circumstance that could have or did lead to unintended, unexpected harm, loss or damage’. All Serious Untoward Incident investigations are in line with guidance on the discharge of mentally disordered people and their continuing care in the community. There is a system in place to report incidents to the relevant commissioners in line with the lead commissioners reporting policy on Serious and Untoward Incidents. This includes initial notification within 24 hours of the incident and a full detailed SUI report within 7 days of the incident. 98 6.24.6d 10.15.10e 16.10.16a 20.18.20f 20.18.20g 98 20.18.20b 23.5.23a 24.6.24a A125 99 100 10.15.10e 16.10.16a 20.18.20a 20.18.20f 20.18.20g A126* A127* E1.6 Untoward incidents are continually monitored to identify trends and learning points. 4.9.4b 6.24.6d 9.13.9b 16.10.16a 16.10.16b 16.10.16c E1.7 There are mechanisms in place to share learning beyond the immediate service/provider concerning incidents. 6.24.6d A127.1* E2.1 The unit has a contingency plan in place, which has been agreed with the police, regarding the reporting and managing of: loss of control serious operational failures including those resulting from fire (in agreement with the local fire and emergency services) escapes absconds failure to return and hostage taking. 10.15.10e 10.15.10h A78 2: Business Continuity 23 102 No. E2.2 E2.3 E2.4 E2.5 E2.6 E2.7 E2.8 E2.9 Standard The unit has contingency plans in place which outline the arrangements for maintaining service integrity and patient and staff safety in the event of an operational, security or systems failure. The business continuity plan incorporates the contingency plans, which have been agreed with the police. The business continuity plan addresses: the chain of operational control communications patient and staff safety and security maintaining continuity in treatment and accommodation. There is a strategic approach to planning to meet the service needs. Clinicians and managers maintain good links with the Home Office and ensure their target deadlines/requirements are met. There is a clinical governance strategy, which is implemented. Contingency plans are annually tested by desktop exercises. Contingency plans are tested by a live exercise involving one or other of the emergency services every 24 months. 24 DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) 103 10.15.10b 10.15.10h 104 10.15.10h 104 6.24.6a 6.24.6b Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care C18* C23* 16.10.16e C29* 6.24.6d A79* 4.9.4b A79.1 No. Standard DH Guidance LSU Essential Standards of Quality & Safety (CQC – March 2010) Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care F: Equalities F1 The service complies with equalities, mental health and human rights legislation. 105 F2 All operational and clinical procedures, processes and policies reflect the requirements of equalities, mental health and human rights legislation. 105 F3 There is an implemented policy to ensure systems are in place to allow for translation services and sign language. Written information must be provided in an appropriate number of languages and formats. 1.17.1g 7.11.7d 22.4.22b 22.4.22c 1.17.1g 7.11.7d 12.21.12a 22.4.22b 22.4.22c 1.17.1a 1.17.1e 4.9.4e 17.19.17e 1.17.1a 1.17.1e 1.17.1g 4.9.4e 4.9.4g 16.10.16b 22.4.22c 1.17.1a 1.17.1c 1.17.1h 2.18.2a 2.18.2h 17.19.17a C37 C38 A84 C38 D6* D6.1 D17 C41 A11w F4 Patients are provided with a range of information, in appropriate formats, regarding their rights under equalities, mental health and human rights legislation. 106 F5 Patients have access to a range of appropriate advocacy services. 106 F6 There are systems and support to enable a successful independent civil advocacy service to be operated. 1.17.1a D11* The service provides patients with information regarding what patients can expect from the service. 1.17.1a 1.17.1e 1.17.1g 4.9.4e 4.9.4g 10.16.10b D17 There is an implemented policy setting out the consultation and involvement of carers in the care provided. The unit’s policy and procedures are agreed through discussion with the whole unit. The views of patients, their carers and others are sought and taken into account in designing, planning, delivering and improving healthcare services. 1.17.1j 4.9.4a 16.10.16d D8* 1.17.1a D23 1.17.1j 4.9.4b E1* Feedback from patients and carers is used to improve the quality of the unit 1.17.1j 16.10.16a 16.10.16c D22 F7 F8 F9 F10 F11 F12 F13 F14 Staff receive training in equality issues and their impact upon patient care. Staff understanding of equality issues are monitored through the appraisal system. Complaints are continually monitored to identify trends and learning points which are reviewed quarterly. 25 107 108 108 C42 D10 D1w C10 14.23.14c 16.10.16a C1.1* No. F15 Standard There is an implemented policy to meet the individual cultural needs of patients. F17 Staff demonstrate respect for patients. F19 Essential Standards of Quality & Safety (CQC – March 2010) Systems are in place that ensure patients (particularly those vulnerable to exploitation e.g. financially, emotionally or sexually) are not subject to bullying by other patients or visitors or staff and that this is managed effectively. F16 F18 DH Guidance LSU Patients are encouraged to personalise their bedroom spaces appropriately. (Pictures of nude bodies or pictures of children may be inappropriate) Patients are provided with meals which are of a high quality, offer choice, address nutritional/balanced diet and specific dietary requirements and which are also sufficient in quantity, are varied and appealing and reflect individual’s cultural and religious needs. (Better Hospital Food – Department of Health 2004). 26 Implementation Criteria for Recommended Specification: Adult Medium Secure Units with supplement Standards and Criteria for Women in Medium Secure Care C2* 1.17.1a 1.17.1b 1.17.1g 1.17.1i 2.18.2b 4.9.4a 5.14.5d 1.17.1a 1.17.1b 1.17.1c 7.11.7i 17.19.17e D5* D13 10.15.10a 10.15.10l D21 5.14.5a 5.14.5b 5.14.5c 5.14.5d 5.14.5f 5.14.5h F10.1* 27 Appendix 1: Delegates, Standards Working Group First Name Surname Role Nigel André Phil Brian Jean Callender Paul Diane Cartmell Clayton Sheryle Cleave Clinical Nurse Manager Marc Cookson Clinical Nurse Manager Maureen Cushley Senior Nurse Manager Paul Gilluley Stephen Simon Carly Joanne Godwin Lloyd Morgan Spears Consultant Forensic Psychiatrist Deputy General Manager Head of Clinical Services Consultant Psychiatrist Clinical Team Leader Joseph Neil Vella Woodward Consultant Psychiatrist Security Manager 28 Clinical Team Leader Head of Secure Services Commissioning Ward Manager Organisation Northumberland Tyne and Wear NHS Foundation Trust West Midlands Commissioning Team Northumberland Tyne and Wear NHS Foundation Trust Northumberland Tyne and Wear NHS Foundation Trust Northumberland Tyne and Wear NHS Foundation Trust West London Mental Health Trust West London Forensic Service Ridgeway St. Andrew's Healthcare Janet Shaw Unit Northumberland Tyne and Wear NHS Foundation Trust Gerry Simon Clinic Ridgeway Appendix 2: Delegates, Standards Consultation Event First Name Surname Role Organisation Paul Guy Colin Gilluley Cross Reynolds Chair James Lee Consultant Forensic Psychiatrist Andrew Anne Duff-Miller Herbert Shirish Bhatkal Consultant Psychiatrist Unit Manager Consultant in Rehabilitation Psychiatry Lorna Elliot Modern Matron Zena Nasser Consultant Psychiatrist LSU Melanie Evans Assistant Director Phil Shackell Steven Chris Pratish Woolgar Harden Thakkar Interim Deputy Director of Secure Commissioning (Specialised Mental Health and Learning Disabilities) Director of Policy and Regulation Group Security Officer Consultant Forensic Psychiatrist Jennifer Berry Commissioner Adam Townsend Kate Axford David Phil Naomi Munns Broxton Collier Ward Manager Occupational Therapy Professional Lead Clinical Governance Manager Therapy Manager Ward Manager Service User Mgcini Nkomo Senior Nurse Dumisani Lupahla Ward Manager Syed Consultant Forensic Psychiatrist Forensic Security Liaison Manager Shaftesbury Clinic Sallie Husain HamiltonHolman Williams Partnerships in Care Partnerships in Care Ridgeway South Of England Specialised Commissioning Group -Specialised Mental Health and Learning Disabilities St. Andrew's Healthcare The Dene and Pelham Woods St. Magnus St. Andrew's Healthcare St. Andrew's Healthcare St. Andrew's Healthcare West London Forensic Services St. Andrew's Healthcare Birmingham Wickham Unit Shaftesbury Clinic Rick Driscoll Johanna Tahti Peter Fornah Neil Woodward Ward Manager Consultant Forensic and Rehabilitation Psychiatrist Doctor for female LS services Ward Manager for Female LS Services Security Manager John McCarron Senior Nurse James Jackie Alexander Somers Security Manager Ward Manager Marcus 29 Ward Manager QNFMHS Advisory Goup Department of Health Ash Ward Challenging Behaviour Service - Memorial Hospital Derby Ward Farmfield Hospital Horton Rehabilitation Services Horton Rehabilitation Services Kent & Medway NHS & SC Partnership Trust North London Forensic Services North of England Specialised Commissioning Thornford Park Hospital Cygnet Hospital Beckton Cygnet Hospital Beckton Ridgeway Shelton Hospital Shrewsbury Wells Road Centre St. Andrew's Healthcare Alison James Lesley Joseph Carr Cooper Wilson Vella Ward Manager Hollis McClatchie Brian Seb Mandisodza Pringle Service Co-ordinator Consultant Psychiatrist Matron - Secure and Forensic Low Secure Services Registered Unit Manager Service User Expert Arlena Ruben Charge Nurse and Recovery Lead Lina Aimola Research Fellow Alice Taylor consultant clinical psychologist Colette Emmanuel Gary Gordon Hamer Onukwube Stobbs Tsubira Service Manager Clinical Services Manager Registered Unit Manager Senior Occupational Therapist Imogen Mortiboys Clinical Services Manager James Mullins James Jeni Tighe Chamberlain Integrated clinical lead, forensic mental health services (sept) Clinical Nurse Research Fellow Unit Manager John Scott Security Team John John Hall Abu Kaysi Thinn Forensic Case Manager Clinical Team Leader Locum Consultant Forensic Psychiatrist Keith Russell General Manager Larte Leanne Lisa Lawson Smith Cairns Nominated Individual Lead Nurse Clinical Services Manager Nick Badoorally Ward Manager Patrick Simon Steve Susan O'Sullivan Lloyd Godwin Guchu Medical Director Head of Clinical Services Deputy Head of Service Clinical Team Leader St. Andrew's Healthcare Partnerships in Care Brooklands Gerry Simon Clinic Hellingly and Chichester Low Secure Services Sutton's Manor QNFMHS The Dene and Pelham Woods Royal College of Psychiatrists North London Forensic Services St. Mary's Hospital Cygnet Hospital Beckton North London Clinic St. Luke's Healthcare St. Andrew's Healthcare Birmingham Robin Pinto Low Secure Unit The Bracton Centre Thornford Park Hospital The Dene and Pelham Woods Ridgeway Sutton's Manor Brockfield House Secure and Forensic Low Secure and Community Services Sussex Partnerships NHS Foundation Trust St. Luke's Healthcare Kemple View St. Andrew's Healthcare Jupiter House Low Secure and Forensic Services St. Magnus St. Andrew's Healthcare Ridgeway Sutton's Manor Further Acknowledgements: We are grateful to Dr Stephen Pereira, Chair of NAPICU and Dr Faisil Sethi, Vice Chair of NAPICU for their advice and sight of the ‘NAPICU Response to Department of Health: Psychiatric Intensive Care Unit and Low Secure Services Good Practice Commissioning Guides: March 2012’ . 30 Appendix 3: Advisory Group First Name Surname Role Head of Secure Services Commissioning Secure Services Commissioning/ National QIPP Programme Phil Brian Rosie Ayub Ian Carmichael Service User Expert Sheryle Cleave Clinical Nurse Manager Paul Gilluley Stephen Godwin Consultant Forensic Psychiatrist Deputy General Manager Julian Haines Social Work Manager Quazi Haque Mary Harty Harry Kennedy Jeremy Kenney-Herbert Mat Kinton Clive Long Janet Parrot Group Medical Director Consultant Forensic Psychiatrist & Associate Medical Director Executive Clinical Director & Consultant Forensic Psychiatrist Clinical Director/Consultant Forensic Psychiatrist Mental Health Act Policy Advisor Associate Director of Psychology and Psychological Therapies Consultant Forensic Psychiatrist/Chair Forensic Faculty Susan Riding Carer Representative Pete Snowden Medical Director Anita Trenfield Carer Representative 31 Organisation West Midlands Commissioning Team Yorkshire and Humber Secure and Specialist Mental Health Commissioning Team Quality Network for Forensic Mental Health Services Northumberland Tyne and Wear NHS Foundation Trust West London Forensic Service Ridgeway North London Forensic Service/ National Group for Social Work Managers in Secure Services Partnerships in care South West London & St Georges Mental Health NHS Trust National Forensic Mental Health Service, Central Mental Hospital Reaside Clinic Care Quality Commission St. Andrew’s Healthcare Royal College of Psychiatrists Quality Network for Forensic Mental Health Services Partnerships in Care Quality Network for Forensic Mental Health Services Appendix 4: Project Team Name Role Sarah Tucker Programme Manager Michael Gray Deputy Programme Manager - MSU Sam Holder Deputy Programme Manager - LSU Sarah Stubbs Project Worker Ilham Sebah Project Worker Service User Experts Abdirisak Hussein Alex Sunyata Ian Carmichael Pebble Carmichael Seb Pringle Carer Representatives Anita Trenfield Susan Riding 32 33 34