case study: 29826-rt, 29827-rt
advertisement

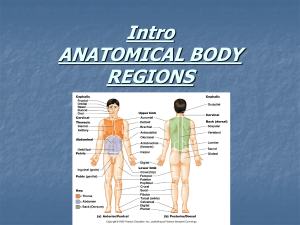
Dial-In Instructions Conference Name: Shoulder Coding Strategies for ASC’s: How to obtain maximum reimbursement Scheduled Conference Date: Wednesday, January 11th, 2006 Scheduled Conference Time: 1:00 p.m.–2:30 p.m. (Eastern), 12:00 p.m.–1:30 p.m. (Central), 11:00 a.m.–12:30 p.m. (Mountain), 10:00 a.m.–11:30 a.m (Pacific) Scheduled Conference Duration: 90 Minutes PLEASE NOTE: If the audioconference occurs April through October, the time reflects daylight savings. If your area does NOT observe Daylight Savings, times will be one hour earlier. Your registration entitles you to: ONE telephone connection to the audioconference. Invite as many people as you wish to listen to the audioconference on your speakerphone. Permission is given to make copies of the written materials for anyone else who is listening. In order to avoid delays in connecting to the conference, we recommend that you dial into the audioconference 15 minutes prior to the start time Dial-In Instructions: 1. Dial 877-407-2989 and follow the voice prompts. 2. You will be greeted by an operator 3. Give the operator your pass code 011106 and the last name of the person who registered for the audioconference. 4. The operator will then verify the name of your facility. 5. You will then be placed into the conference. Technical Difficulties 1. If you experience any difficulties with the dial-in process, please call the Conference Center reservation line at 877- 407-7177. 2. If you should need technical assistance during the audio portion of the program, please press the * key followed by the 0 key on your touch-tone phone and an operator will assist you. If you are disconnected during the conference, dial 877- 407-2989. Q&A Session 1. To enter the questioning queue during the Q&A session, callers need to push the star key followed by the 1 key on their touch-tone phones. Note: This portion of the program generally falls after the first hour of presentation. Please do not try to enter the queue before this portion of the program. 2. If you prefer not to ask your question on the air, you can fax your question to 877- 808-1533 or 201-612-8027. (Please note: You can only fax your question during the program.) Prior to the program If you prefer not to ask your question on the air, you can send your questions via email to jsherman@hcpro.com. Cutoff date and time for questions: 1/9/2006 @ 5:30 PM EST. Please note that not all questions will be answered. Program Evaluation Survey In your materials on page 2, we have included a Program evaluation letter that has the URL link to our program survey. We would appreciate it if when you return to your office you could go to the link provided and complete the survey. Continuing Education documentation If CE’s are offered with this program a separate link containing important information will be provided along with the program materials. Please follow the instructions provided in the CE Documentation. 200 Hoods Lane PO Box 1168 Marblehead MA 01945 TEL 781 639 1872 FAX 781 639 7857 URL www.hcpro.com Program Evaluation Dear Audioconference Participant, Thank you for attending the HCPro audioconference today. We hope that you find the information provided valuable. In our effort to ensure that our customers have a positive experience when taking part in our audioconferences we are requesting your feedback. We would also like to request that you forward the link to others in your facility that attended the audioconference. We realize that your time is valuable, so we’ve limited the evaluation to a few brief questions. Please click on the link below. h t t p : / / w w w. z o o m e r a n g . c o m / s u r v e y. z g i ? p = W E B 2 2 4 V 9 T Y F L 8 R The information provided from the evaluation is crucial towards our goal of delivering the best possible products and services. To insure that your completed form receives our attention, please return to us within six days from the date of this audioconference. We appreciate your time and suggestions. We hope that you will continue to rely on HCPro audioconferences as an important resource for pertinent and timely information. Sincerely, Frank Morello Director of Multimedia HCPro, Inc. presents . . . Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement A 90-minute interactive audioconference Wednesday, January 11, 2006 1:00 p.m.–2:30 p.m. (Eastern) 12:00 p.m.–1:30 p.m. (Central) 11:00 a.m.–12:30 p.m. (Mountain) 10:00 a.m.–11:30 a.m. (Pacific) In our materials we strive to provide our audience with useful, timely information. The live audioconference will follow the enclosed agenda. Occasionally our speakers will refer to the materials enclosed. We have noticed that other non-HCPro audioconference materials follow the speaker’s presentation bullet-by-bullet, page-by-page. Because our presentations are less rigid and rely more on speaker interaction, we do not include each speaker’s entire presentation. The materials contain helpful forms, crosswalks, policies, charts, and graphs. We hope that you find this information useful in the future. HCPro is not affiliated in any way with the Joint Commission on Accreditation of Healthcare Organizations, which owns the JCAHO trademark. ii Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement The “Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement” audioconference materials package is published by HCPro, 200 Hoods Lane, P.O. Box 1168, Marblehead, MA 01945. Copyright 2006 HCPro, Inc. Attendance at the audioconference is restricted to employees, consultants, and members of the medical staff of the Licensee. The audioconference materials are intended solely for use in conjunction with the associated HCPro audioconference. Licensee may make copies of these materials for your internal use by attendees of the audioconference only. All such copies must bear this legend. Dissemination of any information in these materials or the audioconference to any party other than the Licensee or its employees is strictly prohibited. Advice given is general, and attendees and readers of the materials should consult professional counsel for specific legal, ethical, or clinical questions. HCPro is not affiliated in any way with the Joint Commission on Accreditation of Healthcare Organizations, which owns the JCAHO trademark. For more information, contact HCPro, Inc. 200 Hoods Lane P.O. Box 1168 Marblehead, MA 01945 Phone: 800/650-6787 Fax: 781/639-0179 E-mail: customerservice@hcpro.com Web site: www.hcpro.com Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement iii 200 Hoods Lane P.O. Box 1168 Marblehead, MA 01945 Tel: 800/650-6787 Fax: 800/639-8511 Dear colleague, Thank you for participating in our “Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement” audioconference with Lolita Jones, RHIA, CCS, and Susan Vogelberger, CPC, CPC-H, moderated by Ilene MacDonald. We are excited about the opportunity to interact with you directly and encourage you to take advantage of the opportunity to ask our experts your questions during the audioconference. If you would like to submit a question before the audioconference, please send it to jsherman@hcpro.com and provide the program date in the subject line. We cannot guarantee your question will be answered during the program, but we will do our best to take a good cross-section of questions. If at any time you have comments, suggestions, or ideas about how we might improve our audioconferences, or if you have any questions about the audioconference itself, please do not hesitate to contact me. And if you would like any additional information about other products and services, please contact our Customer Service Department at 800/650-6787. Along with these audioconference materials, we have enclosed a fax evaluation. We value your opinion. After the audioconference, please take a minute to complete the evaluation to let us know what you think. Thanks again for working with us. Best regards, Jon Sherman Audioconference coordinator Fax: 781/639-2982 E-mail: jsherman@hcpro.com iv Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement Contents Agenda . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .vi Speaker profiles . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .vii Exhibit A . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .1 Presentation by Lolita Jones, RHIA, CCS, and Susan Vogelberger, CPC, CPC-H Resources . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement v Agenda I. Anatomy of the Shoulder A. Bones B. Muscles/tendons II. Terminology III. Open Guidelines A.. Acute vs. Chronic Rotator Cuff i. Definition ii. Documentation iii. CPT iv. ICD-9 B. Case Studies i. RTC ii. Mumford Procedure iii. Subacromial decompression iv. Bankart procedure v. Capsulorrhaphy vi. Manipulation IV. Arthroscopic Guidelines A. Modifier -59 B. ICD-9 V Codes C. Miniarthrotomy D. Case Studies Live Q&A vi Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement Speaker profiles Lolita Jones, RHIA, CCS Lolita Jones is the principal of Lolita M. Jones Consulting Services and vice president of educational programs at Medical Marketing Resources, Inc. She has over 15 years of experience in publishing, training, and auditing for the hospital outpatient and freestanding ambulatory surgery center (ASC) markets. Susan Vogelberger, CPC, CPC-H Susan Vogelberger, founder and president of the Mahoning County Local Chapter of Professional Coders, is currently employed by the Orthopaedic Surgery Center at Beeghly Medical Park in Boardman, OH, as the business office coordinator/coder. Although her specialty is coding outpatient surgery, she is proficient in all areas of coding and is also employed by Bryant & Stratton College as a PMCC instructor and presenter of various workshops. She has been referenced and has authored articles regarding coding topics in several publications. Vogelberger is an independent auditor and owner of Healthcare Consulting & Coding Education based in Boardman. She serves on the editorial advisory board of the Hand Surgery Coding Alert and has lectured during numerous coding seminars across the country. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement vii Exhibit A Presentation by Lolita Jones, RHIA, CCS, and Susan Vogelberger, CPC, CPC-H EXHIBIT A 2 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 3 EXHIBIT A 4 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A Terminology The Bankart lesion is a specific injury to a part of the shoulder joint called the labrum. The shoulder joint is a ball and socket joint, similar to the hip; however, the socket of the shoulder joint is extremely shallow, and thus inherently unstable. To compensate for the shallow socket, the shoulder joint has a cuff of cartilage called a labrum that forms a cup for the end of the arm bone (humerus) to move within. This cuff of cartilage makes the shoulder joint much more stable, yet allows for a very wide range of movements (in fact, the range of movements your shoulder can make far exceeds any other joint in the body). When the labrum of the shoulder joint is torn, the stability of the shoulder joint is compromised. A specific type of labral tear is called a Bankart lesion. A Bankart lesion happens when an individual sustains a shoulder dislocation. As the shoulder pops out of joint, it often tears the labrum, especially in younger patients. The tear is to part of the labrum called the inferior glenohumeral ligament. Terminology Typical symptoms of a Bankart lesion include a catching, aching, and susceptibility to dislocation; often patient will complain that they cannot "trust" their shoulder. Diagnosis can be difficult as these injuries do not always show up well on MRI scans. This is more of a clinical diagnosis with the definitive diagnosis of a Bankart lesion made at the time of surgery. Patients who sustain a Bankart injury are at much higher risk for dislocating their shoulder again. Treatment of a Bankart lesion often depends on whether or not a patient has recurrent episodes of shoulder instability. When there is suspicion for a Bankart lesion, attempts at physical therapy to strengthen the shoulder may help to reduce the risk of repeat dislocation. If strengthening does not help the problem, shoulder arthroscopy can be performed, and the injury can be definitively diagnosed and treated. A Bankart repair is surgery to repair the torn ligament back to the shoulder socket. The actual Bankart repair can either be performed through an arthroscope or through an incision over the front of the shoulder. Whether or not a Bankart repair is done arthroscopically or through an incision (a so-called open Bankart repair) depends on several factors. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 5 EXHIBIT A Terminology Shoulder instability is a problem that occurs when the structures that surround the glenohumeral (shoulder) joint do not work to maintain the ball within its socket. If the joint is too loose, is may slide partially out of place, a condition called shoulder subluxation. If the joint comes completely out of place, this is called a shoulder dislocation. Patients with shoulder instability often complain of an uncomfortable sensation that their shoulder may be about to slide out of place--this is what physicians call apprehension. If therapy fails, there are surgical options that can be considered. Depending on the cause of the instability, the surgical treatments may be quite different. Terminology If the cause of the shoulder instability is a loose shoulder joint capsule, then a procedure to tighten the capsule of the shoulder may be considered. This can be done with an arthroscope in a procedure called a thermal capsular shrinkage. In this surgery, a heated probe shrinks the shoulder capsule to tighten the tissue. The more standard method of this procedure is called an open capsular shift. In this surgery, the shoulder joint is opened through a larger incision, and the capsule is tightened with sutures. The advantage of the open capsular shift is that the results are more predictable. The advantage of the arthroscopic procedure is that the recovery is faster and the incision is smaller. Sometimes a particular problem is better suited to one procedure or the other, discuss this with your doctor. If the problem is due to a tearing of the ligaments around the shoulder, called the labrum, then a procedure called a Bankart repair can be performed to fix this ligament. A Bankart repair can also be done either through an incision or an arthroscope. Again, the results of the open procedure are more predictable (more patients get better), but the arthroscopic procedure does not leave as large an incision. 6 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A Coding for Rotator Cuff Tears The rotator cuff consists of four muscles; the superspinatus, infraspinatus, subscapularis, and teres minor that fuse together to maintain stability of the shoulder. Arthroscopic: 29827 is for an acute or chronic injury. Open: 23410 is for an acute injury with early repair. 23412 is for chronic tears, degenerative conditions usually in older patients occurring over time. 23410 and 23412 describe rotator cuff repairs involving one or two tendons or major muscles of the rotator cuff. 23420 describes a repair of a complete shoulder rotator cuff avulsion and refers to the repair of all three major muscles/tendons of the shoulder cuff, usually with extensive releases and mobilizations, tissue repositioning, and/or use of fascial or synthetic grafting. For mini-open rotator cuff repair, use 23412. Acute vs. Chronic Acute vs. chronic is up to interpretation as there is no standardized definition to distinguish between the two. A commonly used time frame is three months or less for acute, and greater than three monthsfor chronic. Most RTC repairs are for chronic conditions. A chronic tear could have an acute episode but should still be coded as chronic. Chronic vs. acute should be determined by the physician and clearly documented in the patient’s record. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 7 EXHIBIT A Bundling Issues Procedures often performed with a RTC repair include acromioplasty (29826, 23130), distal clavicle resection (29824, 23120), debridement (29823, 29824), and biceps tenodesis 29999, 23430). Remember to check the Medicare Correct Coding Guide for bundling issues and appropriate application of modifiers. Example RTCRepair Repair Exampleof of Open Open RTC “………The placed abductedposition. position. We with a 7-cm Saber type type “………The armarm waswas placed in in abducted Weproceeded proceeded with a 7-cm Saber incision. Sharp dissection wascarried carried down down through the soft tissue untiluntil the the fascia incision. Sharp dissection was through the soft tissue fascia over the acromion was encountered. Medial and lateral skin flaps were elevated. over The the deltoid acromion anddetached lateral skin were elevated. waswas split encountered. along its anteriorMedial raphe and fromflaps the anterior portion The deltoid was splitExposure along itsincluded anteriorthe raphe and detachedjoint from thedistal anterior of the acromion. acromio-clavicular . The one portion cm of theofacromion. Exposure included acromio-clavicular joint . The distal one cm the clavicle was excised. We thenthe proceeded with a Neer acromioplasty. At this we were to visualize the superior surface of the rotator cuff tear of thepoint clavicle wasable excised. We then proceeded with a Neer acromioplasty. At this which corresponded to the previous arthroscopic description. pointconfiguration, we were able to visualize the superior surface of the rotator cuff tearThe tendon was debrided to a stable viable edge. A bone trough was created in the configuration, which corresponded to the previous arthroscopic description. The greater Wea first proceeded with repairing thetrough infratendinous split ininthe tendon was tuberosity. debrided to stable viable edge. A bone was created the supraspinatus. This proceeded with a with total of four #2 Ethibond sutures passed greater tuberosity. We first proceeded repairing the infratendinous splitinina the figure-of-eight fashion. The supraspinatus avulsion was then reattached to the supraspinatus. This proceeded with a total sutures. of four #2 Ethibond passed in a greater tuberosity utilizing two #2 Ethibond These suturessutures were passed figure-of-eight Theasupraspinatus avulsion wassuture then was reattached to the through thefashion. tendon using modified Bunnell stitch. The passed through greater utilizing #2a Ethibond sutures. These were the tuberosity bone tunnels and tiedtwo over bone bridge. The repair wassutures reinforced withpassed a series of 0 the Vicryl figue-of-eight along the tendinous A watertight closure through was through tendon using astitches modified Bunnell stitch. edge. The suture was passed achieved. The repair was stable to the arm in the abducted position and with range the bone tunnels and tied over a bone bridge. The repair was reinforced with a series of motion. The wound was irrigated with copious amounts of antibiotic saline of 0 Vicryl figue-of-eight stitches along the tendinous edge. A watertight closure was throughout procedure. The deltoid was reattached to the acomion achieved. The the repair was stable to the arm in the abducted positionusing and four with#2 range Ethibond sutures in a Job irrigated type stitch. The split in the acromioclavicular joint was of motion. The wound with copious amounts antibiotic saline approximated with 0 was Vicryl suture using figure-of-eight stitch. of The split in the anterior throughout the procedure. The deltoid was reattached to the acomion using four #2 raphe to the deltoid was re-approximated with 0 Vicryl suture using figure-of-eight Ethibond in a Jobwas type stitch. split in the acromioclavicular joint was stitch.sutures A pain catheter placed in aThe subacromial position………….” approximated with 0 Vicryl suture using figure-of-eight stitch. The split in the anterior raphe to the deltoid was re-approximated with 0 Vicryl suture using figure-of-eight stitch. A pain catheter was placed in a subacromial position………….” 8 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A Debridement Debridement In 2002 the AAOS came out with guidelines for limited vs. extensive In 2002 the AAOS came out with guidelines for limited vs. extensive debridement. Debridement that addresses only the glenoid labrum or debridement. Debridement that addresses only the glenoid labrum or is performed thefront front the shoulder is reported is performedin in either either the or or thethe backback of theofshoulder is reported using 29822. thefront front and back are addressed, use code 29823. using 29822. IfIf both both the and back are addressed, use code 29823. CPT 29822includes: includes: CPT 29822 Diagnostic shoulder Diagnostic shoulderarthroscopy arthroscopy Synovectomy Synovectomy Labral debridement Labral debridement Removal of osteophyte from humerus/glenoid Removal of osteophyte from humerus/glenoid Articular shaving and/or chondroplasty CPT 29823 includes: Articular shaving and/or chondroplasty Diagnostic shoulder arthroscopy CPT 29823 includes: Articular shaving/limited synovectomy Diagnostic shoulder arthroscopy Synovectomy Articular shaving/limited synovectomy Biceps tendon and/or rotator cuff debridement Synovectomy Labrum debridement Removal of osteophyte humerous/glenoid Biceps tendon and/or from rotator cuff debridement Removaldebridement of osteochondral and/or chondral bodies (attached) Labrum Abrasion arthroplasty Removal of osteophyte from humerous/glenoid Removal of osteochondral and/or chondral bodies (attached) Abrasion arthroplasty SLAP ofthe theShoulder Shoulder SLAPLesion Lesion of (Superior Labrum Anterior-Posterior) is is a term used to describe a specific type SLAPSLAP (Superior Labrum Anterior-Posterior) a term used to describe a specific type of injury to the shoulder joint. The The shoulder a ball-and-socket type of jointof and is and is of injury to the shoulder joint. shoulderis is a ball-and-socket type joint anatomically referred to as the gleno-humeral joint, describing the two bony anatomically assocket the gleno-humeral joint,adescribing bony structuresreferred involved.toThe is the glenoid cavity, cup-shaped the piecetwo of bone structures involved. The socket is scapula. the glenoid a glenoid cup-shaped ofby bone that juts out from the corner of the The cavity, rim of the cavity ispiece formed that juts out from theball scapula. The of the glenoid cartilage calledthe thecorner labrum. of The that fits into therim socket is the head ofcavity the is formed by humerus. partThe of the labrum the twoistendons of the cartilage calledThe thesuperior labrum. ball that anchors fits intoone theofsocket the head of the bicepsThe muscle. The other is attached the front of the to theof the humerus. superior partbiceps of thetendon labrum anchorsinone of the twochest tendons coracoid process, an extension of the shoulder blade. What makes SLAP possible is bicepsthemuscle. The other tendon is the attached front ofAs the way the upper bicepsbiceps tendon hooks over head ofin thethe humerus. thechest arm isto the coracoid process, an extension of the shoulder blade. What makes SLAP possible is forcefully bent inward at the shoulder, the humerus acts as a lever and tears the the way thetendon upperand biceps over the head ofan the humerus. As the arm is bicep labrumtendon cartilagehooks from the glenoid cavity in anterior-posterior direction. forcefully bent inward at the shoulder, the humerus acts as a lever and tears the bicep tendon and labrum cartilage from the glenoid cavity in an anterior-posterior direction. There are several ways to code SLAP lesions depending on the type of lesion and the method of repair. Type I is repaired by debridement and is coded 29822. Repairs of types II and IV are coded 29807 because an actual repair is performed. ThereType are III several ways to code SLAP on29807. the type tears can be either debrided or lesions repaired depending using 29822 or Do of notlesion report and 29806 capsulorrhaphy withI aisSLAP repairby unless there is a capsular defect in29822. an area the method of repair. Type repaired debridement and is coded different than II theand SLAP Repairs of types IV lesion. are coded 29807 because an actual repair is performed. Type III tears can be either debrided or repaired using 29822 or 29807. Do not report 29806 capsulorrhaphy with a SLAP repair unless there is a capsular defect in an area different than the SLAP lesion. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 9 EXHIBIT A Types of SLAP Lesions Type I Degenerative fraying of the superior portion of the labrum, labrum remains firmly attached to the glenoid rim Type II Separation of the superior portion of the glenoid labrum and the tendon of the biceps brachii muscle from the glenoid rim Type III Bucket-handle tears of the superior portion of the labrum without involvement of the brachii (long head) attachment Type IV Bucket-handle tears of the superior portion of the labrum extending into the biceps tendon Type V Anterior inferior Bankart lesion that extends upward to include a separation of biceps tendon Type VI Unstable radial of flap tears associated with separation of the biceps anchor Type VII Anterior extension of the SLAP lesion beneath the middle glenohumeral ligament Arthroscopic CodingGuidelines Guidelines Arthroscopic Coding Arthroscopic Shoulder Shoulder Heat A. A.Arthroscopic HeatApplication Application Assignunlisted unlisted arthroscopy arthroscopy CPT code 29999 to report the use heat Assign CPT code 29999 to report theofuse oftoheat to shrink the capsule in the shoulder performed through an arthroscope. shrink the capsule in the shoulder performed through an arthroscope. (Source: CPT Assistant newsletter, August 1998, page 11.) (Source: CPT Assistant newsletter, August 1998, page 11.) B. Arthroscopic Shoulder Decompression of Subacromial Space with Partial Acromioplasty B. Arthroscopic Shoulder Decompression of Subacromial Space with Partial Acromioplasty The arthroscopic procedure involves exposing the subacromial space, bursectomy, debridement, detaching theexposing coracoacromial ligament andspace, The arthroscopic procedure involves the subacromial removing thedebridement, undersurface of the acromion. When subacromial bursectomy, detaching the coracoacromial ligament and decompression is performed, a flat undersurface of the acromion and removing the undersurface of the acromion. When subacromial outlet acromioclavicular joint is produced, which enlarges the supraspinatus decompression is performed, a flat undersurface of the acromion and and prevents impingement. acromioclavicular joint is produced, which enlarges the supraspinatus outlet and prevents impingement. Coding Tip: The partial acromioplasty, arch decompression, excision of bursal tissue and release of the coracoacromial ligament would not be reported separately, as these are considered to decompression, be inclusive components of of Coding Tip: The partial acromioplasty, arch excision code tissue 29826. and [Source: Mayof2001 Assistant newsletter, AMA] bursal release the CPT coracoacromial ligament would not be reported separately, as these are considered to be inclusive components of code 29826. [Source: May 2001 CPT Assistant newsletter, AMA] 10 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A Arthroscopic Coding Guidelines Arthroscopic Coding Guidelines C. Arthroscopic Rotator Cuff Repair C. Arthroscopic Rotator Cuff Repair Rotator cuff injuries are strains or tears of one or more rotator muscles or tendons, theinjuries most common site being the supraspinatous muscle. Rotator cuff are strains or tears of one or more rotatorAcute muscles or tears result suchsite as falls on the an outstretched hand or injuries Acute tendons, thefrom mosttrauma, common being supraspinatous muscle. fromresult football throwing, baseball pitching. Racquetballhand serving tears from trauma, such or assoftball falls on an outstretched ororinjuries manipulation of a frozen shoulder. Chronic tears originate from over-use or from football throwing, baseball or softball pitching. Racquetball serving or constant stress. Assign CPT code 23410 or 23412 for repairs involving manipulation of a frozen shoulder. Chronic tears originate fromcode over-use or one or two tendons or major muscles of the rotator cuff. Assign CPT constant stress. CPT code 23410 or 23412 for repairs involving 23420 for a repairAssign of a complete shoulder (rotator) cuff avulsion, referring to theorrepair all threeormajor muscles/tendons of rotator the shoulder Source: one two of tendons major muscles of the cuff. cuff. Assign CPT code February CPT newsletter, AMA. 23420 for a2002 repair ofAssistant a complete shoulder (rotator) cuff avulsion, referring to the repair of all three major muscles/tendons of the shoulder cuff. Source: February 2002 CPT Assistant Clinical Tip: The major musclesnewsletter, of the rotatorAMA. cuff: supraspinatus, infraspinatus and teres minor. Clinical Tip: The major muscles of the rotator cuff: supraspinatus, infraspinatus and teres minor. Coding Resource: Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 11 EXHIBIT A Arthroscopic Coding Guidelines Arthroscopic Coding Guidelines D. Limited versus Extensive Arthroscopic Shoulder Debridement Code 29822 describes limited arthroscopic shoulder debridement, while code 29823 a describes extensive arthroscopic shoulder debridement. The D. facility Limited versus Extensive Arthroscopic Shoulder Debridement needs to develop a guideline that defines limited versus extensive . Code 29822 describes limited arthroscopic shoulder debridement, while code 29823 a describes extensive arthroscopic shoulder debridement. The facility needs to develop a guideline that defines limited versus extensive . CASE 29822-RT (Limited CASESTUDY: STUDY: 29822-RT (Limited Debridement) Debridement) Preoperative Diagnosis: Preoperative Diagnosis: Painful rightright shoulder. Painful shoulder. Postoperative Diagnosis:Posterior superior labral tear with internal Postoperative Diagnosis:Posterior superior labral tear with internal impingement of the right shoulder. impingement of the right shoulder. Operation: Evaluation under anesthesia, arthroscopy, arthroscopic Operation:ofEvaluation under anesthesia, debridement superior posterior labral tear. arthroscopy, arthroscopic debridement of superior posterior labral tear. Anesthesia: General endotracheal. Anesthesia: General endotracheal. Operative Note: After adequate general endotracheal anesthesia was obtained, theNote: patient’s right shouldergeneral was examined. She was found to was Operative After adequate endotracheal anesthesia have no anterior, posteriorright or inferior instability of the shoulder. obtained, the patient’s shoulder was examined. She The was found to shoulder compared with the left shoulder and these symmetrical. have nowas anterior, posterior or inferior instability of thewere shoulder. The The patient was placed inthe left lateral decubitus position with good axillary shoulder on was compared with theand left neck shoulder and these were symmetrical. clearance a bean bag with head in neutralposition. After sterile Theand patient was inthe leftwas lateral decubitus position good axillary prep drape, theplaced right shoulder arthroscoped through with standard clearance on a bean bag with head and neck in neutralposition. anterior anposterior portals. The anterior portal was made inside out After sterile prep and thespace. right shoulder was through thedrape, triangular The patient wasarthroscoped noted to have athrough healthy standard anterior anposterior portals. The anterior portalsmooth. was made inside out glenoid and humeral head. These were completely through the triangular space. The patient was noted to have a healthy glenoid and humeral head. These were completely smooth. 12 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A CASE STUDY: 29822-RT (Limited CASE STUDY: 29822-RT (Limited Debridement) Debridement) The biceps was probed and was stable. There was no evidence of SLAP The biceps was probed and of was stable. Therehealthy was no and evidence of SLAP lesion. The under surface the cuff was normal and no lesion. The under surface of the cuff was healthy and normal and no evidence of any tears, erythema or inflammation. The posterior superior evidence of any tears, erythema or inflammation. The posterior superior labrum had tear. ItItwas was unstable. It debrided was debrided labrum hadaasmall small tear. notnot unstable. It was with a with a shaver. andposterior posterior ligaments checked and were intact shaver.The Theanterior anterior and ligaments werewere checked and were intact all the wayaround around to to the head. WithWith full external rotation, there there all the way thehumeral humeral head. full external rotation, evidenceof ofpinching pinching ofofthe posterior superior labrum but again waswas evidence the posterior superior labrum butno again no instability.The Theanterior anterior glenohumeral ligament complex was intact, probed instability. glenohumeral ligament complex was intact, probed and was quite stable. The shoulder was re-arthroscoped through the andanterior was quite was re-arthroscoped through the portal.stable. BicepsThe was shoulder checked and was stable and healthy. There was anterior portal.of Biceps was checked and was stable and healthy. There was no evidence any inflammation as it passed through the groove. The no posterior evidence ofwas anyintact inflammation asNo it passed through the groove. cuff and healthy. other abnormalities were noted. The The arthroscope inflow cannula wereNo then placed in the subacromial posterior cuff wasand intact and healthy. other abnormalities were noted. which wasand quiteinflow healthy. There was no then redness, erythema Thespace arthroscope cannula were placed in theorsubacromial inflammation. Thequite bursahealthy. was smooth and was thin. no Superior surface of the cuff space which was There redness, erythema or was intact. The under surface of the acromion was healthy without any inflammation. The bursa was smooth and thin. Superior surface fraying. The CA ligament was healthy and normal without any evidence ofof the cuff wasinflammation. intact. TheThis under the acromion was healthy without any wassurface checkedof through both the posterior and anterior fraying. The ligamentwere wasnoted healthy and normal without any evidence of portals. No CA abnormalities in the subacromial space. The arthroscope and were removed. Thethe portals were closed with inflammation. Thisinflow wascannula checked through both posterior and anterior buriedNo 4-0abnormalities Vicryl. Sterile dressing was applied. patient wasspace. then portals. were noted in the The subacromial The awakened and taken to the recovery room in satisfactory condition. arthroscope and inflow cannula were removed. The portals were closed with buried 4-0 Vicryl. Sterile dressing was applied. The patient was then awakened and taken to the recovery room in satisfactory condition. CASE STUDY:29826-RT, 29826-RT, CASE STUDY: 29823-RT (Extensive (Extensive Debridement) 29823-RT Debridement) Anesthesia: Generalendotracheal endotracheal tube Anesthesia: General tube Preoperative Diagnosis: Preoperative Diagnosis: 1. Posterior labral tear, question clinical significance. 1. 2. Posterior labral tear, question clinical significance. Subacromial impingement. 2. Subacromial impingement. Postoperative Diagnosis: 1. Posterior/inferior Postoperative Diagnosis:labral tear. Anterior/superior labral labral tear. 1. 2. Posterior/inferior tear. Subacromial impingement. 2. 3. Anterior/superior labral tear. 3. Subacromial impingement. Procedure Performed: 1. Exam under anesthesia. Procedure Performed: 2. Diagnostic arthroscopy of glenohumeral joint 1. 3. Exam under anesthesia. Debridement of anterior/superior and posterior/inferior labral tears. Arthroscopic subacromial 2. 4. Diagnostic arthroscopy ofdecompression. glenohumeral joint 3. Debridement of anterior/superior and posterior/inferior labral tears. Complications: None 4. Arthroscopic subacromial decompression. Complications: None Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 13 EXHIBIT A CASE STUDY: 29826-RT, CASE STUDY: 29826-RT, 29823-RT (ExtensiveDebridement) Debridement) 29823-RT (Extensive Operative Findings: Operative Findings: 1. Intact humeral articular cartilage. 1. Intact humeral articular cartilage. 2. Small defect,posterior/inferior posterior/inferior glenoid, adjacent to 2. Smallosteochondral osteochondral defect, glenoid, adjacent to degenerative the posterior posteriorlabrum. labrum. degenerativefraying fraying of of the 3.Posterior/inferior tearwithout withoutfrank frank detachment periosteal 3.Posterior/inferior labral labral tear detachment and and periosteal strippingofofthe theposterior posterior labrum fraying nearnear its insertion, stripping labrumwith withdegenerative degenerative fraying its insertion, onto theglenoid. glenoid. onto the 4. Degenerativetearing tearing of labrum withwith stable 4. Degenerative of the theanterior/superior anterior/superior labrum stable superior/anterior labrum. superior/anterior labrum. 5. Intact anterior/inferior and posterior/superior labrum. 5. Intact anterior/inferior and posterior/superior labrum. 6. Intact biceps tendon with stable biceps labral anchor. 6. Intact biceps withbursal stablesurface. biceps labral anchor. 7. Intact rotatortendon cuff from 7. Intact rotator cuff from bursal surface. 8. Subacromial bursal thickening synovitis. 8. Subacromial bursal thickening synovitis. 9. Large spur on surface of acromion. 10. Fullspur rangeon ofsurface motion ofofthe glenohumeral joint. 9. Large acromion. Stable glenohumeral examination with 2+ anterior 10.11. Full range of motion of the glenohumeral joint. translation and tightened to 0+ with progressive external rotation. 11. Stable glenohumeral examination with 2+ anterior translation and 12. No discernible posterior translation. tightened to 0+ with progressive external rotation. 12. No discernible posterior translation. CASE STUDY: CASE STUDY:29826-RT, 29826-RT, 29823-RT (Extensive 29823-RT (ExtensiveDebridement) Debridement) Operative Indications:The patient is a 38-year-old who injured himself Operative Indications:The patient is the a 38-year-old who injured himself playing basketball. He has had pain in right shoulder. This has been playing basketball. He has had pain in Risks the right This has been refractory to conservative management. and shoulder. benefits of the above listed procedure was discussed with the patient who understood risksabove as refractory to conservative management. Risks and benefits the of the wellprocedure as benefits was and signed the informed consent form. the risks as listed discussed with thepreoperative patient who understood well as benefits and signed the informed preoperative consent form. Operative Description in Detail: The patient was brought to the operating room.General endotracheal anesthesia induced. He was examined under Operative Description Detail: patient brought anesthesia and findings in were noted The as above. Hewas has a stable to the operating room.General anesthesia induced. wasdecubitus examined under glenohumeralendotracheal examination. He was positioned in theHe lateral anesthesia and notedThe as above. He haswas a stable position with thefindings left sidewere downward. right shoulder placed in the Arthrex shoulder holder, prepped and positioned draped in a in standard fashion. glenohumeral examination. He was the lateral decubitus Standard arthroscopic portals were established posteriorly andwas anteriorly. position with the left side downward. The right shoulder placed in the Diagnostic arthroscopy carriedand through the portal with findings as noted Arthrex shoulder holder,was prepped draped in a standard fashion. above. The anterior/superior labral tear was debrided. The arthroscope Standard arthroscopic portals were established posteriorly and anteriorly. was redirected anteriorly. The posterior labral tear was then debrided. Diagnostic arthroscopy through the portal with findings as noted The posterior labral tearwas was carried then probed aggressively. above. The anterior/superior labral tear was debrided. The arthroscope was redirected anteriorly. The posterior labral tear was then debrided. The posterior labral tear was then probed aggressively. 14 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A CASE 29826-RT, CASE STUDY: STUDY: 29826-RT, 29823-RT Debridement) 29823-RT (Extensive (Extensive Debridement) no evidenceofofperiosteal periosteal stripping. It was just just a flapatear the ThereThere waswas no evidence stripping. It was flapthrough tear through the labrum adjacenttotothe the osteochondral defect. AfterAfter debridement of both of both labrum that that waswas adjacent osteochondral defect. debridement the osteochondral defectand and the thethe remaining labrum was stable, the osteochondral defect thelabral labraltear, tear, remaining labrum was stable, there was no evidence of posterior instability. The anterior/superior tear was there was no evidence of posterior instability. The anterior/superior tear was debrided, once again was felt not to be amenable for repair. The arthroscope debrided, once again felt notspace. to be Aamenable for repair. was reentered into thewas subacromial standard lateral portal wasThe arthroscope was reentered subacromial space. A standard portal was established into at thethe junction of the anterior middle third of the lateral acromion. A 5.5 sternal resector and Arthrocare were middle then used throughout the procedureAfor established at the junction of thewand anterior third of the acromion. 5.5 subacromial decompression. A 5.5 barrel was usedthroughout to perform the procedure for sternal resector and Arthrocare wand werebur then used acromioplasty until the anterior third of the acromion was up in the middle and subacromial decompression. 5.5 barrel bur usedmultiple to perform posterior thirds. Adequacy of theAacromioplasty waswas checked times and acromioplasty the anterior third of was in the middle deemed to beuntil acceptable. The rotator cuffthe wasacromion probed from theup bursal surface and and no evidence cuff tear. The removed from shoulder and attention posterior thirds. ofAdequacy of arthroscope the acromioplasty was the checked multiple times and turned closing. The subacromial space portal sites were with _% deemed to towards be acceptable. The rotator cuff was probed frominjected the bursal surface and Marcaineof with Epinephrine. port sites were closed with nylon and sutures. no evidence cuff tear. TheThe arthroscope removed frominterrupted the shoulder attention Sterile dressing consisting of Betadine soaked Adaptic, 4 x 4s and Elastoplast was turned towards The space sites were injected with _% placed on theclosing. shoulder. Thesubacromial patient was placed in aportal sling an swath, awakened, Marcaine with and Epinephrine. port room sitesinwere with extubated, taken to theThe recovery stableclosed condition. Heinterrupted tolerated thenylon sutures. procedure well. There were complications. Sterile dressing consisting ofno Betadine soaked Adaptic, 4 x 4s and Elastoplast was placed on the shoulder. The patient was placed in a sling an swath, awakened, extubated, and taken to the recovery room in stable condition. He tolerated the procedure well. There were no complications. Arthroscopic Coding Guidelines Arthroscopic Coding Guidelines E. Postoperative Pain Management E. Postoperative Pain Management October 2001 CPT Assistant newsletter, AMA: October 2001 CPT Assistant newsletter, AMA: • • When general anesthesia is administered and pain management injections are When general anesthesia is administered and pain management injections are performed analgesia, they separate and distinct services performedtotoprovide provide postoperative postoperative analgesia, they are are separate and distinct services and are reported tothe theanesthesia anesthesia code. Whether the block procedure and are reportedin in addition addition to code. Whether the block procedure (insertion narcotic local anesthetic agent) (insertionofofcatheter, catheter, injection injection ofofnarcotic or or local anesthetic agent) occursoccurs preoperatively, during procedure is immaterial. preoperatively,postoperatively, postoperatively, ororduring thethe procedure is immaterial. If, on theother otherhand, hand, the block is used primarily for the itself, itself, • • If, on the blockprocedure procedure is used primarily foranesthesia the anesthesia serviceshould should be be reported reported using anesthesia code alone. In a combined thethe service usingthe the anesthesia code alone. In a combined epidural/generalanesthetic, anesthetic, the be be reported separately. epidural/general theblock blockcannot cannot reported separately. Example: Example: [NOTE: Many third-party payers do not accept CPT anesthesia codes from hospitals.] • Many third-party do not accept anesthesia brachial codes from hospitals.] • [NOTE: Shoulder surgery couldpayers be performed under CPT an interscalene plexus block Shoulder surgery could postoperative be performedanalgesia. under anThis interscalene brachialusing plexus that would also provide would be reported the block anesthetic codeprovide (e.g., 01620). If the block were intended to reported alleviate using the that would also postoperative analgesia. Thisprimarily would be postsurgical pain, and a general anesthetic was administered for the shoulder anesthetic code (e.g., 01620). If the block were intended primarily to alleviate procedure, the block be separately reportable. postsurgical pain, andwould a general anesthetic was administered for the shoulder procedure, the block would be separately reportable. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 15 EXHIBIT A CASE STUDY: 29826-RT, 23120, 64415-59 (Post Op Pain Block) OPERATIVE REPORT DATE: 12/01/200X PREOPERATIVE DIAGNOSIS: Possible rotator cuff tendonitis, acromioclavicular arthritis, and frozen shoulder, right shoulder. POSTOPERATIVE DIAGNOSIS: Frozen shoulder, subacromial bursitis-impingement, and acromioclavicular arthritis, right shoulder. OPERATIVE PROCEDURE: Arthroscopic subacromial decompression with open distal clavicle resection and manipulation under anesthesia, right shoulder. SURGEON: ASSISTANT: CASE STUDY: 23120, CASE STUDY:29826-RT, 29826-RT, 23120, 64415-59 (Post Block) 64415-59 (PostOp OpPain Pain Block) INDICATION FOR PROCEDURE: The patient is a 51-year-old male with recalcitrant shoulder painFOR and aPROCEDURE: frozen shoulder. The He had failedisrehabilitative andmale injection INDICATION patient a 51-year-old with recalcitrant treatments requested intervention. shoulder painand and a frozenoperative shoulder. He had failed rehabilitative and injection treatments and requested operative intervention. FINDINGS AT OPERATION: Preop motion was 90 degrees of flexion and 30 degrees of external and internal rotation. There was significant subacromial bursitis FINDINGS AT OPERATION: Preop motion was 90 degreesspur. of flexion and 30 with very thickened coracoacromial ligament and a subacromial The intradegrees external were and internal articularofstructures normal. rotation. There was significant subacromial bursitis with very thickened coracoacromial ligament and a subacromial spur. The intraarticular structures were normal. DESCRIPTION OF PROCEDURE: The patient was brought to the operative suite and general anesthesia was smoothly induced. The shoulder was examined and interscalene block placedsuite the above notedOF limitation of motion was found. Anwas DESCRIPTION PROCEDURE: The patient brought to the was operative forgeneral postop pain control and patient was placed in theshoulder beach chair The wasposition. examined and and anesthesia wasthe smoothly induced. right noted shoulder was manipulated with palpable and audible crepitaceblock into 150 was theThe above limitation of motion found. degrees of elevation, external rotation was was to 80 withAn theinterscalene opposite shoulder being 90,placed forand postop pain control and the patient was placed in the beach chair position. internal rotation was equivalent at 70. Adduction and abduction were equivalent. The right shoulder manipulated and audible into 150 The shoulder was was prepped and drapedwith in a palpable sterile fashion. Throughcrepitace anterolateral, degrees of elevation, external rotation wasshoulder to 80 with opposite direct lateral, and posterolateral portals, the wasthe examined andshoulder treated being 90, arthroscopically. joint was entered. The humeral and internal rotationThe wasglenohumeral equivalent at 70. Adduction andglenoid, abduction werehead, equivalent. biceps tendon, andprepped labrum were cuff was intact. The shoulder was and intact. drapedThe in arotator sterile fashion. Through anterolateral, direct lateral, and posterolateral portals, the shoulder was examined and treated arthroscopically. The glenohumeral joint was entered. The glenoid, humeral head, biceps tendon, and labrum were intact. The rotator cuff was intact. 16 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A CASE STUDY: 29826-RT, 23120, 64415-59 (Post Op Pain Block) The arthroscopic instruments were placed in the subacromial space. The bursa was resected. The coracoacromial ligament was released from the acromion with the cautery. Utilizing a bur and a shaver, the acromion was flattened . The anterior portion was excised and the rotator cuff was found to have a significant partial-thickness bursal side tear, but no full-thickness tear and the arthroscopic instruments were removed. A small incision was made over the distal clavicle. The deltoidtrapezial raphe was taken down in a subperiosteal fashion off of the distal clavicle and the distal 2.5 cm of clavicle was excised with a saw. Bone wax was placed over the cut end. The deltotrapezial raphe was closed with #1 Nurolon. A small closed suction drain was placed and the wound was closed with 2-0 Vicryl and a Monocryl for the skin. Steri-Strips were applied. The acromioplasty was checked manually before closure. A sterile compressive dressing was applied. The patient was awakened and taken to the recovery room in good condition. There were no complications. Blood loss was minimal. Postoperative plans are to rehabilitate the patient’s shoulder. CASE STUDY: 29826-RT, 29827-RT OPERATIVE REPORT OPERATION: Arthroscopic acromioplasty and arthroscopic rotator cuff repair, right shoulder. ANESTHESIA: Scalene block. PREOPERATIVE DIAGNOSIS: Full thickness rotator cuff tear, supraspinatus insertion site with impingement syndrome of the right shoulder. POSTOPERATIVE DIAGNOSIS: Full thickness rotator cuff tear, supraspinatus insertion site with impingement syndrome of the right shoulder. OPERATIVE PROCEDURE: The patient was brought to the operative suite, scalene block right shoulder followed by intravenous sedation anesthesia performed. The right shoulder was examined and demonstrated full passive loss of shoulder motion. The patient was then placed in the supine beach chair position and the right shoulder was prepped and draped in the usual sterile fashion. A 30-degree arthroscope was introduced through the posterior portal, intra-articular structures were visualized demonstrating significant synovitis at the rotator interval and superior aspect of the cuff. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 17 EXHIBIT A CASE STUDY: 29826-RT, 29827-RT This area was initially cauterized and then debrided with the full radius resector. Hemostasis was achieved. The long head of the biceps also had synovitis at its intra-articular portion under the cuff tear. There was no fraying or fibrillation of the biceps. The area of hyperemia was also cauterized. The superior glenoid labrum was intact. There was some degree of fraying and fibrillation in this area but no evidence for a type 2 slap lesion. Anterior-inferior capsule labrum, posterior-inferior capsule labrum were normal. Humeral head and articular surfaces of the glenoid and humeral head were normal. There was full thickness tear of the supraspinatus insertion site over approximately a 3 cm area from the rotator interval to the posterior-superior corner of the greater tuberosity. The tear was retracted to approximately the mid humeral head. The biceps tendon anchor and bicipital groove were normal, subscapularis was normal and posterior cuff was normal. The arthroscope was then placed in the subacromial space, there was marked bursal thickening and hypertrophy. A partial bursectomy was carried out, there were some minor changes on the undersurface of the acromion. Soft tissue was removed from the acromion with the cautery device and shaver. A minimal acromioplasty was required, plus 3 to 4 mm of bone anteriorly and tapering this posteriorly. The acromioclavicular joint was visualized but not resected. The soft tissue was removed from the greater tuberosity, a bone trough was made over the greater tuberosity from the bicipital groove to the posterior most extent of the cuff. This was approximately a 2 to 2.5 cm bone trough. CASE STUDY: 29826-RT, 29827-RT The cuff was mobilized by release of the intra-articular portion of the capsule, release of the coracohumeral ligament at the base of the coracoid. This was done with a cautery device. The cuff was then mobilized and pulled to the bone trough, two 5 mm Arthrex anchors were placed in the lateral most aspect of the bone trough, and the sutures were tied with three simple sutures and one mattress suture. An excellent anatomic repair was achieved with the cuff being opposed to the tuberosity with firm fixation. The arthroscopic equipment was removed from the shoulder, the portal sites were closed with #3-0 Prolene and Steri-Strips. Sterile dressings were applied. The patient was reversed from anesthetic and brought to the recovery room in stable and satisfactory condition. COMPLICATIONS: None. 18 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A CASE STUDY: 29807-RT, 29826-RT, 29824-RT OPERATIVE REPORT PREOPERATIVE DIAGNOSIS: 1. Acromioclavicular joint arthritis right shoulder. 2. Possible superior labrum anterior and posterior lesion or labrum tear right shoulder. POSTOPERATIVE DIAGNOSIS: 1. Osteoarthritis right acromioclavicular joint. 2. Anterior superior labrum anterior and posterior lesion right shoulder. TITLE OF THE OPERATION: 1. Arthroscopic superior labrum anterior and posterior lesion repair with one 3.0 mm Fast-Tac suture anchor. 2. Arthroscopic distal clavicle excision right shoulder. ANESTHESIA: General. CASE STUDY: 29807-RT, 29826-RT, 29824-RT PREOPERATIVE NOTE: The patient is a 57-year-old gentleman with a long history of right shoulder pain. Preoperative evaluation indicated pain emanating from an arthritic AC joint, and we suspected a SLAP lesion as well. We did not suspect the rotator cuff or impingement. Therefore, the above procedure was recommended. DETAILS OF THE PROCEDURE: Under general anesthetic, the patient was placed supine in the semi-sitting position with the head on a Mayfield headrest. The right shoulder was scrubbed, prepped and draped in the usual manner. The posterior viewing scrubbed, prepped and draped in the usual manner. The posterior viewing portals were established through the glenohumeral joint. The articular cartilage in the glenoid and humeral sides was normal. The posterior labrum and direct superior labrum was normal. However, the anterior superior labrum was detached. There was a SLAP lesion under the biceps anchored anteriorly coming down to the approximately 1 o’clock. We probed this through an anterior portal in the rotator interval and found this to be true. The biceps tendon anchor was normal except for the anterior portion of the anterior superior labrum. The biceps tendon exited the joint normally. The rotator cuff was normal. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 19 EXHIBIT A CASE STUDY: 29807-RT, 29826-RT, 29824-RT We prepared the anterior superior glenoid neck with a shaver and a bur after using the periosteal elevator to mobilize the soft tissue. Next, we placed a single 3.0 Bio Fast-Tac suture anchor at approximately 12:30 on the anterior superior glenoid rim. We used standard arthroscopic knot tying techniques to tie down the anterior superior labrum with the anterior portion of the biceps anchor. Fortunately, the majority of the biceps anchor was intact. We had established this using a peel-back sign intraoperatively. Once the labrum was repaired, we probed it and found it to be stable. Next, the subacromial space was entered. A lateral working portal was established. We excised enough of the subacromial bursa to visualize the anterior acromion. We denuded the anterior acromion across to the AC joint removing the inferior AC joint ligaments. The distal clavicle was clearly identified. We removed the osteophyte on the medial end of the anterior acromion, which was in part partial of the AC joint osteophyte. We then did approximately an 8 mm distal clavicle excision through the same anterior portal that we used for the labrum repair by redirecting it directly into the AC joint. We removed all the clavicle up to, but not including the superior AC joint ligaments. CASE STUDY: 29807-RT, 29826-RT, 29824-RT Next, the arthroscopic instruments were removed. The portals were closed with 4-0 nylon. A sterile dressing was applied followed by a Don Joy shoulder immobilizer. Sponge and instrument counts are correct. The patient tolerated the procedure well and was transferred to the recovery room in satisfactory condition. POSTOPERATIVE PLAN: The patient will be discharged home today and I will see him in the office in a few days time for follow-up. 20 Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A CASE STUDY: 29806-LT, 29807-59LT OPERATIVE REPORT PREOPERATIVE DIAGNOSIS: Recurrent anterior instability of the left shoulder POSTOPERATIVE DIAGNOSIS: Recurrent anterior instability of the left shoulder with Bankart lesion and SLAP lesion ( superior labrum anterior and posterior ) OPERATION: Evaluation under anesthesia, arthroscopy, arthroscopic Bankart repair and SLAP repair ANESTHESIA: General endotracheal CASE STUDY: 29806-LT, 29807-59LT OPERATIVE NOTE: After adequate general endotracheal anesthesia was obtained, the patient’s shoulders were examined. The left shoulder was easily subluxable. The right shoulder was stable. There was no posterior or inferior instability of either shoulder. The patient was placed in the right lateral decubitus position with good axillary clearance on the bean bag with the head and neck in neutral position. Peroneal nerve on the right leg was cleared. After sterile prep and drape, the shoulder was placed in 12 pounds of traction and arthroscoped through standard posterior and anterior portals. The anterior portal was made inside out through the triangular space. A second accessory portal was made just above the subscapularis tendon. The patient was noted to have an intact humeral head with minimal chondromalacia. The glenoid was intact. The anterior and superior labrum were torn. There was some fraying along the posterior labrum. This was probed and was stable though. The superior labrum was hypermobile consistent with a type 2 SLAP lesion and anteriorly, the patient had a Bankart lesion.. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 21 EXHIBIT A CASE STUDY: 29806-LT, 29807-59LT This anterior Bankart lesion was probed and was detached. The capsule labral complex although was reasonably healthy other than this lesion. The rotator cuff and biceps were intact. The capsule labral complex was released off the scar tissue of the anterior neck with an elevator, cleaned with a shaver and a bur was used to create a good bleeding bed along the anterior and superior aspects of the glenoid. The Bankart was then repaired using two Suretacs and SLAP lesion was repaired with an Acufex suture anchor superiorly. Once this was done, everything was probed was quite stable. The heads of the Suretacs were smoothed down to the level of the glenoid. The arthroscope and inflow cannula were removed. The portals were closed with buried 4-0 Vicryl. The patient was placed in a shoulder immobilizer after placing a sterile dressing. He was then awakened and taken to the recovery room in satisfactory condition. Resources • • • • • • • • • • • • • • • • • • • 22 www.aaos.org www.aaos.org/wordhtml/bulletin/archive.asp www.arthroscopy.com www.animatedmedical.com www.orthosupersite.com www.ortho.hyperguides.com www.vh.org.adult/provider/anatomy/atlasofanatomy www.fpnotebook.com/ORT.htm www.gpoaccess.gov/fr www.hope.edu/academic/kniesiology/athtrain/program/studentprojects/ fischer/sld001.htm (animated bankhart repair) www.cms.hhs.gov www.ama-assn.org www.ntis.gov/product/correct-coding.htm www.assh.org www.medscape.com/homeindex?src=hdr www.nlm.nih.gov/medlineplus/encyclopedia.html www.ortho.hyperguides.com www.cdc.gov www.oig.hhs.gov Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement EXHIBIT A Disclaimer The purpose of these handouts is to accompany the presentations conducted by Susan Vogelberger, CPC, CPC-H. There is no guarantee that the use of this publication will prevent differences of opinion with providers or insurance carriers regarding reimbursement issues. Ms. Vogelberger, or any third party sponsor, provided nor implied or expressed warranty regarding the content of this seminar and/or publication due to the constant changing of regulations, laws and policies. It is further noted that any and all liability arising from the use of this publication and/or information supplied at this seminar is the sole responsibility of the participant, and their respective employers, who by purchase of this publication and/or attendance at this seminar evidences agreement to hold harmless the aforementioned parties, their employees and affiliates. The intent of this publication is to be used as a teaching tool accompanying the oral presentation only. The use of copyrighted pages are reprinted with permission and/or fall under “Fair Use” as referenced in the US Copyright Law, Chapter 1, Section 107. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 23 Resources RESOURCES Orthopedic Coding Guide Audioconference Attendees SAVE 20%! for Ambulatory Surgery Centers A one-stop solution for the entire orthopedic coding process Orthopedic Coding Guide for Ambulatory Surgery Centers is a book that walks you, step-by-step, through the complete orthopedic coding process. Whether you're new to orthopedic coding or a seasoned pro, you'll turn to this resource again and again for the guidance you need on accurate and effective orthopedic coding. ICD-9-CM, CPT, and HCPCS Level II information together in one spot Orthopedic Coding Guide for Ambulatory Surgery Centers combines ICD-9-CM, updated 2006 CPT, and HCPCS Level II orthopedic coding information in one convenient place to save you time. Chances are, multiple staff members are involved in the coding process at your ASC. With a copy of Orthopedic Coding Guide for Ambulatory Surgery Centers in your resource library, every member of your team will have access to the only book dedicated to orthopedic-specific coding for ASCs. Mail, fax, or phone-in your order today! Save 20% when you respond to this special offer, exclusively for audioconference attendees. HCPro, Inc • 200 Hoods Lane • P.O. Box 1168 • Marblehead, MA 01945 Phone 800/650-6787 • Fax 800/639/8511 Yes! Send me a copy of Orthopedic Coding Guide at the special discounted price of just $103.20—that’s a 20% savings reserved exclusively for audioconference attendees! Manual Orthopedic Coding Guide Price $103.20 (Regularly $129) Order online at www.hcmarketplace.com – Enter your source code at checkout to save 20%! Your order is fully covered by HCPro’s risk-free, money-back guarantee. Code Quantity OCGASC Shipping ($21.95.00 to AK, HI, PR) *Shipping is $18 for orders over $100. **Your state sales tax Grand Total Total $18.00* $ $ Your source code is: MB40706A Ship to: Your Name & Title Organization Street Address City/State/Zip FOUR EASY WAYS TO PAY! (Please check one) . Bill me Charge VISA MasterCard AmEX Check enclosed (pay to HCPro) Bill my facility with P.O. # Account # ______________________________________________Expires __________________ _____________________ Signature _______________________________________________________________________________________________ Thank you for your order! * *Tax Information—States that tax products and shipping and handling: CA, IL, MA, MD, NJ, VA, VT, FL, CT, GA, IN, MI, NC, NY, OH, PA, SC, TN, TX, WI; States that tax products only: AZ. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 25 RESOURCES Speaker resources Lolita M. Jones, RHIA, CCS Lolita M. Jones Consulting Services 1921 Taylor Avenue Fort Washington, MD 20744 Phone: 301/292-8027 Fax: 301/292-8244 E-mail: LolitaMJ@aol.com Susan Vogelberger, CPC, CPC-H The Orthopeadic Surgery Center At Beeghly Medical 6505 Market Street, Building B Suite 101 Boardman, OH 44512-3458 Phone: 330/758-1065 E-mail: susanv.hcce@zoominternet.net HCPro sites HCPro: www.hcpro.com With more than 17 years of experience, HCPro, Inc., is a leading provider of integrated information, education, training, and consulting products and services in the vital areas of healthcare regulation and compliance. The company’s mission is to meet the specialized informational, advisory, and educational needs of the healthcare industry and to learn from and respond to our customers with services that meet or exceed the quality they expect. Visit HCPro’s Web site and take advantage of our online resources. At hcpro.com you’ll find the latest news and tips in the areas of • • • • • • • • 26 accreditation corporate compliance credentialing health information management infection control long-term care medical staff nursing Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement RESOURCES • • • • pharmacy physician practice quality/patient safety safety HCPro offers the news and tips you need at the touch of a button—sign up for our informative, FREE e-mail newsletters, check out our in-depth how-to information in our premium newsletters, and get advice from our knowledgeable experts. The Greeley Company: www.greeley.com Get connected with leading healthcare consultants and educators at The Greeley Company’s Web site. This online service provides the fastest, most convenient, and most up-to-date information about our quality consulting, national-education offerings, and multimedia training products for healthcare leaders. Visitors will find a complete listing of our services that include consulting, seminars, and conferences. If you’re interested in attending one of our informative seminars, registration is easy. Simply go to www. greeley.com and take a couple of minutes to fill out our online form. Visitors of www.greeley.com will also find • faculty and consultant biographies. Learn about our senior-level clinicians, administrators, and faculty who are ready to assist your organization with your consulting needs, seminars, workshops, and symposiums. • detailed descriptions of all The Greeley Company consulting services. • a list of Greeley clients. • catalogue and calendar of Greeley’s national seminars, conferences, and available CMEs. • user-friendly online registration/order forms for seminars. HCPro’s Healthcare Marketplace: www.hcmarketplace.com Looking for even more resources? You can shop for the healthcare management tools you need at HCPro’s Healthcare Marketplace at www.hcmarketplace.com. Our online store makes it easy for you to find what you need, when you need it, in one secure and user-friendly e-commerce site. At HCPro’s Healthcare Marketplace you’ll discover all of the newsletters, books, videos, audioconferences, online learning, special reports, and training handbooks that HCPro has to offer. Shopping is secure and purchasing is easy with a speedy checkout process. Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement 27 attended OF ATTENDANCE Rob Stuart Senior Vice President / Chief Operating Officer January 11, 2006 a 90-minute audioconference on “Shoulder Coding Strategies for ASCs: How to obtain maximum reimbursement” C ER TIFICATE