ppc jo urnal - Keck Graduate Institute
advertisement

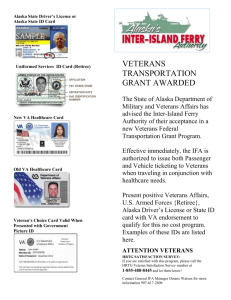
THE PPC JOURNAL Volume 6, Issue 2 Page 2 Pages 3-4 by Laura Cantu by Sam Arcas A Letter from Your PPC Rep Healthcare Access for Veterans Pages 8 – 10 Where Are They Now? In This Issue Welcome by Laura Cantu ………………………………………………………….……………........................….... Page 2 Healthcare Access for Veterans by Sam Arcas ………………………………………………….……………………………………....... Pages 3-4 2016 Presidential Candidates on Healthcare by Kayla Yoshida ……………………….…………………………………….……………………....….. Pages 5-6 A Chat with Dr. Rothfeld, MD by Andrew Gurewitz …………………………………………………...……....……………..…..…….... Page 7 Where Are They Now? ……………………….…........................................................................................................… Page 8-10 Library Comic Strip by Sara Littrell……………………………….…………………………………………………………... Page 11 Phabulously Phun Crossword (PPC) 2016 by Sam Arcas …………………………………………………………………………………………… Page 11 Volume 6, Issue 2 A Final Word from the PPC Rep To my fellow future-physicians, When did semester 2 module 1 happen? We have flown through this last half of the year! I am impressed with everything that our cohort has accomplished in this short year at KGI. We have become scribes, researchers, physician shadows, master's candidates, and more! You have joined and founded clubs, discovered new fields of research and medicine, and networked with inspiring leaders. Every day, someone in our cohort has achieved a goal, contributed to the community, and come one step closer to medical school. Moving forward into this final home stretch, I know that we will all be faced with our own challenges. But we have already overcome challenges on our way to this point and I encourage you to reach out to each other for support. We are surrounded by a wealth of knowledge and experience, together we are strong enough to navigate the stress of the next few months. As our MCAT dates creep up on us and deliverables begin to take their toll, know that it will be ok. You are made of magic, you just have to remember to use it. Laura Cantu 2 Volume 6, Issue 2 Healthcare Access for Veterans by Sam Arcas Picture this, you are a U.S. marine strapped inside of a huge flying tin can called the Boeing C-17 Globemaster. All around you sit fellow marine brothers and sisters, some who have served beside you in live combat. As your transport lands, you are elated to finally be on U.S. soil again, this time for good. The cargo door opens and you catch a glimpse of the crowd wherein your family is waiting to receive you. An intense feeling of happiness and joy rushes over you. But this is not without a lingering feeling of concern because you are wounded from combat and require long-term rehabilitation. The line ends with you. In front of you stand countless other veterans waiting for healthcare as well, some who have served as far back as World War 2. For those veterans fortunate enough to return home with no physical injuries, there still exists a strong possibility of mental health disorders. But for those with physical injuries and mental health disorders, the department of veterans affairs (VA) is something veterans can’t live without. Since the 1600s, U.S. soldiers disabled by war were offered monetary compensation and healthcare benefits for their wartime efforts.1 Over the years, these benefits evolved to include families of veterans, and have grown into the most extensive system of assistance for veterans in the world. Currently, the VA healthcare system consists of 152 hospitals, 800 outpatient clinics, 126 nursing homes, and 35 domiciliaries, employing over 270,000 and serving nearly 6 million enrolled veterans out of a total of 22 million nationwide.1,2 The state of California alone is home to 2 million veterans.3 But even for the 6 million enrolled, it remains a challenge for the VA to effectively serve all veterans. Problems such as ridiculous wait times for appointments, imperious bureaucracy, and fraudulent behavior have all caused public scrutiny of the VA. Collectively, these acts have led to an inconsistent and error prone scheduling system that may have cost the lives of veterans. In 2014, a budget of $164 billion dollars was dedicated to managing the VA’s numerous hospitals and outpatient clinics. But even with this amount of money, problems within the VA persisted, causing public outcry against the VA and its administration staff. For example, the VA was accused of excessively lacking to deliver overdue payments to private hospitals that provided veterans with “non-VA” services, which includes any kind of healthcare that the VA is unable to provide. For many veterans, a VA hospital either does not offer a very specific healthcare service or is too far a distance for veterans to travel. Thus, veterans are prompted to visit private hospitals. Some of the longer cases that the VA has lacked payment on extended as far back as 3 years. Due to these extreme cases of “payment tardiness”, private hospitals have completely terminated contracts with the VA, forcing veterans to either travel the long distance to a VA hospital, or worse, not pursue healthcare at all. Another problem with the VA stems from its administrators who have been alleged to directly interfere with the patient appointment scheduling system, effectively altering scheduling so that less patients are seen daily by doctors.4,5 This fraudulent behavior painted the façade to regulatory officials that patients were receiving timely appointments, when in reality they were not. As a result of such gross manipulation and abuse of power, a system-wide scheduling catastrophe ensued, causing patients to wait an exorbitant amount of time to see a doctor, some as long as 6 months. Although it was difficult to gauge exactly how and how many veterans were affected by this catastrophe, a single VA hospital in the Southwest estimated that 40 patients had died due to being denied timely appointments.5 3 In the grand scheme of things, it is incomprehensible how the VA system allowed itself to be victim to such irresponsible and negligent behavior. In any case, the issue persists that millions of veterans remain neglected by a healthcare institution that promised lifelong healthcare in exchange for military service. Government officials and veteran advocacy groups agree that in order to change the VA’s way of offering healthcare, the entire system must be revamped to hold employees accountable for their actions, create an employee-wide culture of service, and strictly regulate these changes in the future. However, all of these changes must be practiced long-term in order to fully take effect, and we cannot expect our veterans to wait any longer for healthcare that they desperately need. Over the past few years, the most practical and effective measure taken was the “Veterans Choice” program, initiated by the “Veterans Choice” Act. This allowed veterans to visit non-VA institutions if they lived more than 40 miles away from a VA hospital or if their appointment wait time exceeded two weeks. With a budget of $10B wholly dedicated to this program, the VA provided prompt payment directly to non-VA healthcare institutions that took care of veterans. Due to this program’s success, more private institutions have begun providing healthcare again to veterans at the expense of the VA. Additionally, 2 programs in New Jersey have begun training veterans with extensive knowledge of the VA healthcare system, to educate and instruct other veterans on how to navigate the system complexities and effectively utilize their healthcare benefits. Lastly, for senior citizen veterans who require 4 Volume 6, Issue 2 in-home care or live in a long-term care facility, solutions have proposed to lower taxes to ease the cost of living and certain healthcare expenses are even allowed by the IRS to be taxdeductible, with the hope of easing the cost of living for senior citizen veterans. With a veteran healthcare system that was once in shambles, there lies hope for our veterans yet. Our nation’s leaders recognize that VA healthcare is not perfect and must continuously be improved until veterans receive the exact healthcare they deserve. Although some legislation has targeted the faulty points of VA healthcare, much more must be done in order to truly make the VA healthcare system the beacon of hope and good will that it was constructed to be. We cannot rely on veterans to be responsible for helping their own receive benefits promised to them. Additionally, although deferring care to non-VA hospitals helps to ease much of the strain that is put on the VA, the VA needs to address those veterans that are “out of their reach” and healthcare should be easily accessible to every single veterans that accessible to every single veterans that is enrolled. References: History - Department of Veteran Affairs (VA). at <http://www.va.gov/about_va/vahistor y.asp> Viranga Panangala, S. Healthcare for Veterans: Answers to Frequently Asked Questions. (2015). Bureau, U. C. How Do We Know? A Snapshot of Our Nation’s Veterans. at <http://www.census.gov/library/infogr aphics/veterans.html> Congress acts to address VA issues. AHA News 50, 1–3 (2014). McDonnell, P. J. Cheating at expense of veteran care. Ophthalmol. Times 39, 4–4 (2014). Volume 6, Issue 2 2016 Presidential Candidates on Healthcare by Kayla Yoshida The presidential election year is upon us once again. What does that mean for us? Well, for one, it means that we will all be voting for a new president come November 8th. However, it also means that we, members of the PPC Class of 2016, will have an opportunity to voice our opinions on important healthcare policy by making an informed vote. Which presidential candidate will you vote for, and why? While the candidates have shared their visions for the future through recent events such as rallies, press conferences, and official committee debates, it is rare that we see them all laid out on the table in one place. Here, I will take you on a quick tour through the current field of presidential candidates. This will definitely be valuable in your medical school interviews to come! First up is Hillary Clinton, former Secretary of State and the leading candidate for the democratic national committee nomination, who stands as a large supporter of the currently instated Affordable Care Act (ACA).1 Clinton opposes the ‘Medicare-for-all’ or ‘single-payer system’ and believes that the future of the nation is in ObamaCare. The premise of Secretary Clinton’s plan is that the ACA is working. And in some regards, she may be right. According to the Commonwealth Fund Biennial Health Insurance Survey, since the enactment of ObamaCare in 2010, the percentage of uninsured working-age Americans has decreased significantly from 20% to 16% by 2014. 2 However, it is debatable whether this is due to confounding factors, such as the timely end of the Great confounding factors, such as the timely end of the Great Recession in June of 2009. Furthermore, other researchers project that under the ACA, insurance premiums are increasing due to low nationwide enrollment and an inability to file income tax returns. 3 While a stated proponent of the ACA, Hillary has at the same time promoted her own piece of legislation. For instance, in September of 2015, she promoted her own addendum to the ACA labelled the “Affordable Healthcare and Prescription Drug Platform” and separately released a plan to address the outrage caused by pharmaceutical monopolies such as those made by Turning Pharmaceuticals (Martin Shkreli, CEO) in August of 2015.1 Moreover, Secretary Clinton has announced plans to allocate $2 billion toward Alzheimer’s research and drug development.1 All in all, Senator Clinton strives to defend the ACA in hopes of improving access to healthcare. Next up is Senator Bernie Sanders, who has served as senator for the state of Vermont since 2007. This trademark ‘democratic socialist’ is a large proponent for the ‘Medicare-for-all’, single-payer system. While Bernie’s ideas call for radical change, his supporters are passionately behind his plans and surprisingly youthful. Senator Sander’s main goal is to eliminate private insurance companies, while creating universal healthcare consisting of exclusively public insurance (Medicare). While just an estimate, this system is projected to cost 20% less than the average cost of health insurance today. 1 Furthermore, in an effort to mimic the Canadian healthcare 5 Volume 6, Issue 2 Furthermore, in an effort to mimic the Canadian healthcare system, Bernie states, “I believe we've got to go further. I want to end the international embarrassment of the United States of America being the only major country on earth that doesn't guarantee health care to all people as a right, not a privilege.” -Bernie Sanders at the 2nd Democratic Primary Debate Senator Sanders agrees ObamaCare has moved the nation in the right direction but is still looking for more. Alike to Secretary Clinton, he put his interests in curtailing ‘big-pharma’ by proposing the Prescription Drug Affordability Act of 2015 in partnership with U.S. Representative Elijah Cummings.1 Senator Sanders offers his trademark ‘political revolution’ and intends to do so to make healthcare a right for all American citizens. It seems that Clinton and Sanders aim to build upon what has been laid out to date through ObamaCare. On the other hand, it seems that republican candidates stand firmly to repeal ObamaCare. While it may be easier to pinpoint what is lacking in the current healthcare policy, it often takes great ingenuity to propose a new system that aims to address these problems. The fear of ‘all talk, no walk’ is a leading concern for GOP supporters. Only time will tell if these republican candidates can act upon their intentions. Noteable GOP contenders on healthcare include, Dr. Ben Carson, a pediatric neurosurgeon, and Senator Ted Cruz, Senator for the state of Texas and the self-proclaimed leader of the effort to repeal the ACA. First up is Dr. Ben Carson. The retired 6 Senator Ted Cruz, a front-runner for the republican nomination, currently leads the effort to replace the ACA with the Health Care Choice Act (HCCA).1 The HCCA would repeal only Title 1 of the ACA, with the restoration of the free-market for health insurance as a desired result. In theory, market competition would rise and patients would be empowered to choose their own health insurance. Senator Cruz brands the HCCA as personal, portable, affordable healthcare. Unlike many of his fellow candidates, it seems so far that Cruz offers the most concrete plan to transform the current state of healthcare. For instance, he plans to reinstate the ability for patients to purchase health insurance across state-lines by creating a private system with many different companies (the direct opposite of ObamaCare). Cruz projects that this will restore the free marketplace and directly diminish the role of government within health affairs. He also believes in Carson’s design for health savings accounts for those who are able. Finally Cruz calls for the de-linkage of health insurance from employment, making health insurance ‘portable’ with the patient. Other GOP candidates, not to mention Donald Trump, have similar beliefs, but have however shown little leadership in spearheading new healthcare policy reform. This coming election questions the boundaries of conservative and socialist, as well as whether healthcare is a right or a privilege. Nonetheless, healthcare is a necessity and must continue to be a chief concern for our nation’s president. This election season next president. This election season proves to be an exciting time for healthcare reform, so you can trust that this PPC will be following these presidential candidates closely… after MCATstudying of course. References: The Lucy Burns Institute. 2016 Presidential Candidates on Healthcare. 2015. https://ballotpedia.org/2016_presidentia l_candidates_on_healthcare (accessed January 2016). ObamaCare Facts. Rise in Healthcare Coverage and Affordability. January 15, 2015. http://obamacarefacts.com/2015/01/15 /rise-in-healthcare-coverage-andaffordablity/ (accessed January 2016). Tanner, Michael. What's Wrong with Obamacare? October 28, 2015. http://www.nationalreview.com/article/ 426121/obamacare-bad-news (accessed January 2016). Photo References: http://www.motherjones.com/politics/ 2015/04/bernie-sanders-hillary-clintondemocrat-2016-press-questions http://www.washingtontimes.com/news /2015/mar/23/ted-cruz-immigrationcrackdown-advocacy-sparksfie/?page=all Volume 6, Issue 2 A Chat with Dr. Alan Rothfeld, MD by Andrew Gurewitz In continuing with the faculty profile section, this issue we will delve deeper into the life of everyone’s favorite clinical pharmacology professor Alan Rothfeld MD. He graduated from medical school in 1974 and then completed a fellowship in pulmonology/critical care medicine in 1979. After completing the fellowship he was recruited by USC where he was an attending physician as well as professor in their medical school. In recent year he began to transition to a hospital administration role. He worked as essentially a medical director for a hospital system and set up a few clinics in the Los Angeles area. If you want to hear a good story ask him about the cheap vegetables. He joined the KGI faculty in 2007 after a chance meeting with a KGI faculty member who addressed the need for a clinical faculty member. He said that teaching here was a refreshing change from teaching medical students although he admits now that the PPC class is half of the SALS class, things have become more like teaching medical students. Having such a distinguished career in Having such a distinguished career in medicine I was curious as to how medicine has changed over his career. Some of the changes that that he has seen include better protocols, improvements in patient safety, the overuse of antibiotics and something that he stresses in clin pharm – Medical Care is the leading cause of death in the United States. I then asked for 3 areas that can be fixed in modern medicine. His responses were quite clear: 1) curtail the use of medicine 2) simplify the payment system 3) Rationalize physician practices. Being an attending physician to medical students I was curious if he had any advice that he would give potential medical students. He said that satisfaction needs to be emphasized, remind them that you don’t have to be OCD in practice and be true to your own personality. Like many of you are or should be doing I am working on my personal statement and one of the most difficult questions is why medicine. According to him he felt that medicine was relevant and not theoretical and is the best education theoretical and is the best education you can get, you can’t fool nature. When I asked him why medicine now his response was intellectual satisfaction, seeing how medicine has changed and the ability to command vast resources to solve problems. My final question concerned the opioid epidemic sweeping the country and what he thought could be done about it. I was quite surprised, I was expecting him to say that it was caused by overzealous physicians but instead he said that the problem lies with the state relicensing of physician, making them take a pain control class a few years ago. Before that class was mandatory no one was really using narcotics but since then the use has been on the rise until recently. The problem with all of this according to him is now we have patients that are addicted to narcotic pain control. According to Dr.Rothfeld, physicians have realized this and greatly curtailed the use of narcotic pain control in their practice. Overall I enjoyed my time with Dr. Rothfeld, he seemed more than willing to chat about anything medicine related and was a great resource about our future career. 7 Where Are They Now? Volume 6, Issue 2 Jixi (Lucy) He PPC ‘13, MBS’14 Ben-Gurion University Medical School for International Health, MD Class of 2019 How has your PPC/KGI experience impacted your career path and where you are at today? Some of the courses I've taken at KGI directly contributed to my knowledge at med school (like clinical pharmacology, medical devices, pharmaceutical discovery and development, biostatistics etc) and the others made me feel privileged that I got to learn all those things that med school wouldn't provide (like accounting, marketing, having the chance to actually work with Amgen in our master project, and the wine club was probably the best club I've ever joined). I'm very glad that PPC/MBS (KGI) gave me so many chances to learn all about the health related industries. When the teachers here talk about drug approval, biologics, patent exclusivity, I secretly smile inside. If you had to offer one piece of advice to your past PPC self, what would it be? To my past self? My serious advice would be: DON'T relax the summer before med school, start STUDYING for med school the moment you get your first acceptance. Always think about how to provide patients (and the people around you) with maximal comfort because when medicine fails at least you can try to make them smile (watch Patch Adams!). My lighthearted advice: Don't give up what's most important to you (i.e. EAT, SLEEP, and be SANE) I haven't stopped going to band, and I've developed newfound interests in cooking and origami because that relaxes me. Actually this is a serious advice too: BE HEALTHY YOURSELF! How can I take care of others when I'm sick? Would you be receptive to being in contact with current PPC students? I would love to! I also have a not so active blog if people want to check out how's life and study in Israel. Shalomdoctor.com My email: jixi@post.bgu.ac.il 8 Where Are They Now? Volume 6, Issue 2 Kate Brown PPC ‘12, MS’13 Touro College of Osteopathic Medicine, New York, DO Class of 2017 How has your PPC/KGI experience impacted your career path and how has it contributed to where you are at today? While I am not sure what I would be doing if it weren't for KGI, I am confident that I wouldn't be in medical school. KGI’s ample research opportunities allowed me to get involved in a few different projects and the small class sizes made it reasonably easy to get to know the professors and to gain leadership skills. The countless lunch lectures helped me figure out what kind of school was a good fit and the MBS-style internships and classes gave me plenty to talk about during interviews. If you had to offer one piece of advice to your past PPC self, what would it be? (perhaps one serious and one lighthearted). The first piece of advice I would give is try not to compare yourself too much to other students. I think it is easy to get caught up in the “this student got this MCAT score and got an interview here, so I need to get the same score to have a chance” or “this student is doing three research projects, should I be doing more research?” You each have something that makes you a unique applicant. If you don’t know what makes you stand out, Joon will tell you (he told me). I was a nontraditional student who overcame some significant hurdles in obtaining my degree and I often felt pressured into keeping up with other pre-meds. What I didn’t realize until I had overexerted myself was that schools weren’t comparing me against other traditional students. I was being compared against other nontraditional students with similar circumstances (whose average GPA and MCAT scores were lower than their published numbers). Focus on doing your best and try not to worry about what everyone else is doing. Would you be receptive to being in contact with current PPC students and if so, what would be the best place to reach you? Yes, I would be happy to talk to any student. My email address is KBrown9@student.touro.edu 9 Where Are They Now? Volume 6, Issue 2 Erica Liu PPC ‘13 Rosalind Franklin University Physician Assistant Program, Class of 2019 How has your PPC/KGI experience impacted your career path and where you are at today? How has your PPC/KGI experience impacted your career path and where you are at today? My time in the PPC program helped me to better articulate my beliefs and goals. During my time at KGI, I also began to develop greater professionalism and improved public speaking skills. All of these were tremendous assets when it came time to apply to PA school; I felt like I could comfortably convey to various admissions committees/interviewers the things that are really integral to who I am (which is actually much harder to do than one might think). I actually switched from the med school track to the PA school track during my time at KGI. Though I don’t actually think that anything in the PPC/KGI experience directly contributed to my decision, I was fortunate to be in an environment that was very supportive of all medical professions. In fact, anytime that we visited a med school or hosted a representative from a med school that has a PA program, Joon made sure that we were given information on both programs. Funnily enough, one of these sessions was with an admissions counselor from Rosalind Franklin University, which is where I now go to school! If you had to offer one piece of advice to your past PPC self, what would it be? When telling people that you have decided to switch career paths, use these conversations to advocate for your chosen profession and to educate others about your new career path. And don’t preempt your explanations with excuses! Though others may sometimes doubt the legitimacy of the PA profession or cast it as hopelessly inferior to being an MD, you shouldn’t feel pressured to disparage your own profession simply for the sake of fitting in. Also, always order a side of truffle sauce with your fries at Eureka Burger! Would you be receptive to being in contact with current PPC students? Sure – my email address is ericaliu228@gmail.com 10 Volume 6, Issue 2 Art by Sara Littrell Concept by Cyrus Nguyen Phabulously Phun Crossword (PPC) 2016 By Sam Arcas A Work in Progress 12 Volume 6, Issue 2 Volume 6, Issue 2 13 Volume 6, Issue 2 14 Volume 6, Issue 2 15 Volume 6, Issue 2 16 Volume 6, Issue 2 17 Volume 6, Issue 2 18 Volume 6, Issue 2 19 Volume 6, Issue 2 20 Volume 6, Issue 2 21 Volume 6, Issue 2 22 Volume 6, Issue 2 Walking is man’s best medicine. - Hippocrates 23 Volume 6, Issue 2 24