ARVO 2015 Annual Meeting Abstracts
160 Visual fields and visual function, I
Sunday, May 03, 2015 3:15 PM–5:00 PM
Exhibit Hall Poster Session
Program #/Board # Range: 1029–1061/B0163–B0195
Organizing Section: Glaucoma
Contributing Section(s): Clinical/Epidemiologic Research
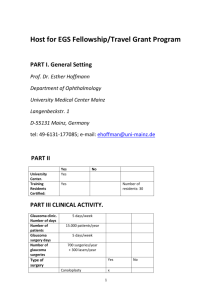
Program Number: 1029 Poster Board Number: B0163
Presentation Time: 3:15 PM–5:00 PM
Effects of early glaucoma on vection responses
Taylor Brin1, Eli Kisilevsky1, 2, Luminita Tarita-Nistor1, Esther G.
Gonzalez1, 3, Graham E. Trope3, Shaun Singer3, Martin J. Steinbach1,
3 1
. Vision Science Research Program, Toronto Western Hospital,
Toronto, ON, Canada; 2School of Medicine, University of Toronto,
Toronto, ON, Canada; 3Ophthalmology and Vision Sciences,
University of Toronto, Toronto, ON, Canada.
Purpose: Vection is the illusion of self-motion induced in stationary
observers by large moving scenes. We have previously shown that
patients with mild glaucoma have longer vection latencies but
vection duration is the same; i.e., the neural responses involved in
cancelling the illusion remain intact. No relationship between visual
field sensitivity and vection responses was found. The purpose of
this follow-up study was to investigate whether vection responses
correlate with estimated loss of retinal ganglion cells (RGC).
Methods: Twenty-one eyes of 14 patients with mild glaucoma and 9
control eyes were exposed to a random-dot pattern at 40cm viewing
distance in a dark room. The pattern was projected for 2 minutes on
a large screen and rotated clockwise at 45 deg/s to induce a sensation
of self-rotation. Vection latency, vection duration, and objective and
subjective measures of tilt were recorded. Visual acuity, visual field
sensitivity, and optical coherence tomography (OCT) exams were
obtained for each eye. Medeiros et al.’s combined index of structure
and function (CSFI) was used to estimate the amount of RGC loss.
This index incorporates measures from both visual field and OCT
tests.
Results: All control eyes but only 62% of eyes with glaucoma
responded to vection, and only these were included in the analysis.
CSFI for controls (mean 3 ± 5%) was significantly smaller than that
for glaucoma group (mean 17 ± 12%). Visual acuity was not different
between the two groups. Latency for controls (mean 7 ± 4s) was
significantly shorter than for the glaucoma group (mean 27 ± 31s),
but vection duration and tilt angles were the same for the two groups.
In the glaucoma group, objective measure of the body’s maximum tilt
angle during vection correlated with CSFI [r(11) = -.55, p = .026] and
with cup-to-disc ratio [r(11) = -.71, p = .006].
Clinical characteristics of eyes with glaucoma that did not respond to
vection were not different from those that did, except for acuity (i.e.,
worse by one line for those who did not respond to vection).
Conclusions: More than one third of eyes with mild glaucoma did
not respond to vection. Those that did had a delayed response and the
objective measure of the body tilt was associated with the estimated
number of RGC loss. These results suggest that vection can detect
anomalies in early glaucoma.
Commercial Relationships: Taylor Brin, None; Eli Kisilevsky,
None; Luminita Tarita-Nistor, None; Esther G. Gonzalez,
None; Graham E. Trope, None; Shaun Singer, None; Martin J.
Steinbach, None
Support: Glaucoma Research Society of Canada
Program Number: 1030 Poster Board Number: B0164
Presentation Time: 3:15 PM–5:00 PM
Steady-State Pattern Electroretinogram (ssPERG) Fixed Protocol
Reference Ranges of Healthy Eyes.
Anna Shengelia1, Peter H. Derr2, Alberto Gonzalez-Garcia2,
Mark Ghassibi3, 4, Jason L. Chien3, 4, Celso Tello3, 5, Robert Ritch3,
6 1
. Ophthalmology, New York Glaucoma Research Institute, New
York, NY; 2Diopsys Inc., Pine Brook, NJ; 3Moise and Chella Safra
Advanced Ocular Imaging Laboratory, Einhorn Clinical Research
Center, New York Eye and Ear Infirmary of Mount Sinai, New York,
NY; 4George Washington University School of Medicine and Health
Sciences, Washington, DC; 5Ophthalmology, Manhattan Eye, Ear and
Throat Hospital, Hofstra North Shore-LIJ School of Medicine, New
York, NY; 6Ophthalmology, New York Medical College, Valhalla,
NY.
Purpose: To establish reference ranges from healthy subjects for the
Steady State Pattern Electroretinogram (ssPERG) Fixed Protocols
responses.
Methods: 60 healthy eyes (60 subjects) were randomly selected.
Inclusion criteria were the following: best corrected visual acuity
20/30 or better, spherical refraction within ±5.00 D, cylinder
correction within ±3.00 D, normal Standard Automated Perimetry,
normal slit lamp biomicroscopy, intraocular pressure ≤22 mmHg,
normal stereoscopic disc photos, normal retinal nerve fiber layer
(RNFL) thickness by optical coherence tomography (OCT), normal
dilated fundus examination. ssPERGs were recorded using the
Diopsys NOVA System (Diopsys, Inc. Pine Brook, NJ). Each eye
was stimulated with the contrast sensitivity and the concentric field
protocols. Test duration was 30 seconds/eye and each test resulted in
a magnitude and magnitudeD response. Each response’s Magnitude,
MagnitudeD and the MagnitudeD/Magnitude ratio was evaluated.
Reference ranges were calculated for the Magnitude and MagnitudeD
parameters for both protocols. The reference ranges were validated
for normality of the residuals (Observed values – Predicted values)
across the entire age range and for three equal sized subgroups based
on age.
Results: Study population demographics were: 31.7% male;
68.3% female; 65.0% Caucasian; 10.0% African American; 10.0%
Hispanic; and 15.0% Asian. The age range was 25 to 86 years old.
The Magnitude was not significantly affected by the age (p=0.098).
However, age did have an effect on the MagnitudeD parameter
(p=0.004). The reference ranges with ±95% CI are as follows:
Magnitude (Predicted) = 1.604 – 0.006 * Age, Magnitude (±95%
CI) = 1.604 – 0.006 * Age (±1.96 * 0.39, MagnitudeD (Predicted) =
1.615 – 0.012 * Age, Magnitude (±95% CI) = 1.615 – 0.012 * Age
(±1.96 * 0.43.
Conclusions: The ssPERG fixed protocol reference ranges with
(±95CI) will provide researchers and clinicians the ability to compare
a healthy subject or patient’s ssPERG results to an age adjusted mean
value.
Commercial Relationships: Anna Shengelia, None; Peter H. Derr,
Diopsys Inc. Pine Brook, NJ (E); Alberto Gonzalez-Garcia, Diopsys
Inc. Pine Brook, NJ (E); Mark Ghassibi, None; Jason L. Chien,
None; Celso Tello, Diopsys Inc. Pine Brook, NJ (C); Robert Ritch,
Diopsys Inc. Pine Brook, NJ (C)
Program Number: 1031 Poster Board Number: B0165
Presentation Time: 3:15 PM–5:00 PM
Comparing Transient and Steady-State Multifocal-VEP (mfVEP)
using Dartboard Stimulation as Possible Tool for Objective
Perimetry
Folkert K. Horn, Franziska Selle, Bettina Hohberger, Jan J. Kremers.
Ophthalmology, Univ of Erlangen Nurnberg, Erlangen, Germany.
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Purpose: To optimize the stimulus conditions for steady-state
multifocal visual evoked potentials (ssmfVEP) and to compare the
measurements with conventional mfVEP.
Methods: All measurements used 4-channel VEP-recordings (best
of 4 algorithms) with 58 field dartboard stimulation (Roland Consult,
retiscan). M-sequence length (128, 255, 512 steps), the number of
reversals (2, 3, 4, 5, 6, 7, 8), and temporal frequency (6, 7, 9, 10, 12,
15 Hz) were varied. Measurements were obtained from 9 normal
subjects (mean age 39 years, 3 male, 6 female). All measurements
were performed in 8 identical m-sequence cycles. FFTs were
performed on each cycle and on averaged responses. Signal to noise
ratio (SNR) was computed using the signal amplitude at the stimulus
frequency and the noise defined as the averaged amplitudes at the
neighbouring frequencies at which no response is elicited by the
stimulus. All subjects additionally underwent conventional mfVEP
measurements with a single pattern reversal per M-step with 300
ms signal length followed by a 200 ms noise window used for SNR
calculation. Statistics: comparison of signal strength, SNR, and the
correlation between local mfVEP as measured transiently and with
steady-state stimulation.
Results: SNR in the ssmfVEP was highest (3.1±1.7) at 9 Hz
stimulation frequency and significantly (p<0.01, paired t-test) higher
than SNR in conventional mfVEP (2.3±1.3). The time to perform
one single ssmfVEP measurement at this frequency (4 reversals per
M-step) was 123 s, compared to 141 s with conventional mfVEP.
SNR and Amplitudes from ssmfVEP were significantly correlated
with those from conventional mfVEP in 7 of the 9 subjects.
Conclusions: The ssmfVEP may be useful for objective perimetry as
spectrum analysis can be used for automated evaluation of responses
leading to improved SNR. In comparison with conventional
transient mfVEP, the recording time can be shorter because the
total measurement period can be used for analysis and because no
additional time is needed for noise estimation and SNR calculation.
Commercial Relationships: Folkert K. Horn, None; Franziska
Selle, None; Bettina Hohberger, None; Jan J. Kremers, None
Clinical Trial: NCT00494923
Program Number: 1032 Poster Board Number: B0166
Presentation Time: 3:15 PM–5:00 PM
Functional Evaluation of Glaucoma Using the Amplitude of the
P50-N95 Wave of the Pattern Eletroretinogram Compared with
Standard Automated Perimetry
Fabio Lavinsky1, 2, Paulo Augusto D. Mello1, Nedio Castoldi2, Camila
Z. Benfica2. 1Department of Ophthalmology,, Paulista School of
Medicine, São Paulo Hospital, Federal University of São Paulo, Sao
Paulo, Brazil; 2Ophthalmology, Federal University of Rio Grande do
Sul, Porto Alegre, Brazil.
Purpose: To assess the results of the functional evaluation of
glaucoma using the amplitude of the P50-N95 wave of pattern
Eletroretinogram (PERG) compared with the mean deviation (MD) of
the standard automated perimetry (SAP).
Methods: A prospective transversal study was performed. A hundred
and thirty one eyes of eyes of 74 patients were examined with
PERG using the Rolandtm with 100% of contrast, reverse pattern in
Black and White with stimulus height of e 4 cm and with SAP using
HumphreyTM perimetry (Zeisstm), strategy SITA-Standrd 24-2. The
sample was divided in three groups based on SAP: 51 eyes with
primary open angle glaucoma (POAG) with MD=-7dB or worse,
58 with POAG with a MD better than -7dB and 30 controls. The
statistical analysis was performed using the linear mixed models of
the Statistical Package for Social Sciences SPSS, Chicago, IL,USA
version 2.0.
Results: The estimate marginal mean of P50-N95 wave amplitude
of PERG using linear mixed models was 3.83mV in the group with
POAG and SAP MD worse than -7dB (mean MD= -16.72dB),
3.79mV in the group with PAOG and SAP MD better than -7dB
(mean MD= -2.70dB); and in the control group 7.74mV (mean MD=
-1,49 dB). The difference of the N50-P95 wave amplitide of PERG
was statistically significant between the POAG with MD worse than
-7dB and the control group (p<0.001) and between the POAG with
MD better than -7dB and the control group (p<0.001). There was no
statistical significant difference between both POAG groups. In our
sample no POAG patient had a P50-N95 wave amplitude better than
10mV .
Conclusions: The objective functional evaluation using the P50-N95
wave amplitude of PERG can be a useful test for the diagnosis and
for the follow-up of progression in glaucoma patients. In our sample,
there was a significant difference between the control group and
the POAG groups, however there was no statistically significant
difference between the POAG groups. Prospective longitudinal
studies evaluating the correlation between SAP progression and
P50-N95 worsening are needed to further evaluate this diagnostic
tool.
Commercial Relationships: Fabio Lavinsky, None; Paulo Augusto
D. Mello, None; Nedio Castoldi, None; Camila Z. Benfica, None
Program Number: 1033 Poster Board Number: B0167
Presentation Time: 3:15 PM–5:00 PM
Clinical Utility of Short Duration Transient Visual Evoked
Potential (SD-tVEP) Pathologic Indicators in Chronic Glaucoma
William E. Sponsel2, 1, Carolyn Majcher2, Sylvia L. Groth3, Rick
Trevino2. 1Biomedical Engineering, University of Texas San Antonio,
San Antonio, TX; 2Visual Science, University of Incarnate Word, San
Antonio, TX; 3Ophthalmology, University of North Carolina, Chapel
Hill, NC.
Purpose: To assess rates of abnormal SD-tVEP amplitude and
latency findings in adults with chronic glaucoma using the Diopsys
Nova-LX P100/N75-referenced high (Hc) and low (Lc) contrast
stimuli.
Methods: Clinical records of adults with chronic glaucoma
undergoing SD-tVEP evaluation with the Diopsys Nova system
between Aug 2013 and Apr 2014 were reviewed. In addition to
demographic information, the amplitude and latency of the SDtVEP under both Lc and Hc stimuli conditions were collected, as
was whether the VEP findings were interpreted by the device as
being normal or abnormal. The mean defect (MD) of the most recent
Humphrey 30-2 visual field was used to stage the severity of the
glaucoma as being mild (MD > -6dB), moderate (-6dB ≥ MD >
-12dB) or severe (MD ≤ -12dB).
Results: Complete data were available for 98 glaucomatous eyes
of 85 patients (49 eyes mild, 16 moderate, 33 severe). The mean
age was 68.2±1.3 yrs. Mean amplitudes were reported as normal
in >85% of eyes. The Lc rate of amplitude abnormality was mild:
8.6%; moderate: 5.0%; severe: 7.9% (R2 = 0.008, P = 0.94). The
Hc amplitude abnormality rate was mild: 5.7%; moderate: 0.0%;
severe: 21.1% (R2 = 0.584, P = 0.45). Lc and Hc latency abnormality
rates both showed strong associations with perimetric staging, but
Hc latency deficits were far more common (P = 0.02). The Lc rate
of latency abnormality was mild: 12.2%; moderate: 18.8%; severe:
33.3% (R2 = 0.991, P = 0.06). The Hc latency abnormality rate was
mild: 18.4%; moderate: 31.3%; severe: 57.6% (R2 = 0.994, P = 0.05).
Conclusions: Using the Diopsys NOVA-LX integrated analysis
software, rates of significant SD-tVEP latency abnormality increased
with glaucoma severity, with Hc deficits being significantly more
common than Lc defects. This Hc>Lc latency defect preponderance
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
arose at all stages, afflicting a majority of eyes with severe glaucoma.
SD-tVEP latency thus appears to have far greater clinical relevance
to glaucoma than amplitude, for which there was no observed
relationship with disease severity.
Association of proportion of glaucomatous eyes demonstrating
high contrast SD-tVEP latency deficit in relation to the Humphrey
30-2 mean deviation visual field pathologic category (mild <6dB,
moderate 6-12 dB, and severe >12dB).
Commercial Relationships: William E. Sponsel, Diopsys (R);
Carolyn Majcher, None; Sylvia L. Groth, None; Rick Trevino,
None
Program Number: 1034 Poster Board Number: B0168
Presentation Time: 3:15 PM–5:00 PM
Low Contrast and Blue-on-Yellow Multifocal Visual Evoked
Potential- Predictors of Progression in Pre Perimetric Glaucoma
Radha Govind1, 2, Alexander Klistorner2, 1, Hemamalini Arvind1,
Stuart L. Graham1. 1Australian School of Advanced Medicine,
Macquarie University, Sydney, NSW, Australia; 2Save Sight Institute,
University of Sydney, Sydney, NSW, Australia.
Purpose: There is a high potential for multifocal Visual Evoked
Potential (mfVEP) techniques to objectively measure functional
visual loss in glaucoma prior to Standard Automated Perimetry
(SAP). We conducted a prospective, observational clinical study in
a long-term cohort to evaluate the performance of Low Luminance
Achromatic (LLA) and Blue-on-Yellow (BonY) mfVEP stimuli
presentation in the detection of pre perimetric glaucoma.
Methods: Pre perimetric glaucoma (glaucomatous optic discs as
judged by stereo disc photography and normal standard visual
fields) subjects enrolled from a glaucoma clinic underwent complete
ophthalmic examination including LLA mfVEP, BonY mfVEP,
Ocular Coherence Tomography (OCT) and Heidelberg Retina
Tomograph (HRT) at baseline and annually thereafter. SAP was
performed at two baseline visits and followed up every 6 months.
Criteria for minimum scotoma for the various functional tests were
established. The mean follow up duration was 3.1±0.8 years.
Results: Seventy-two eyes of 46 subjects (Mean age 64.59±6.66
years) confirmed pre perimetric glaucoma. Of these, progression
on SAP was detected in 17 eyes (23.6%). Despite a normal SAP
at baseline in 72 eyes, low contrast mfVEP (22%), BonY mfVEP
(26%), OCT (86%) and HRT (81%) showed abnormalities. Amongst
17 progressive eyes, abnormalities were detected on low contrast
mfVEP (47%), BonY mfVEP (53%), OCT (82%) and HRT (88%)
prior to detection on HVF. OCT and HRT borderline values were
considered abnormal. Low contrast and BonY mfVEP identified
hemifield changes 9±5.5 months prior to progression on HVF. The
location of hemifield defect on low contrast mfVEP and BonY
mfVEP corresponded topographically to the defect detected on HVF
in 41% (7 out of 17) of eyes.
Conclusions: Amongst functional tests, LLA and BonY mf VEP
appear to have the potential to detect changes in function prior to
standard automated perimetry (SAP) with moderate topographic
correspondence. However, there was only a moderate level of
correlation with structural change.
Commercial Relationships: Radha Govind, None; Alexander
Klistorner, None; Hemamalini Arvind, None; Stuart L. Graham,
None
Support: NHMRC GRANT 570959 (AUSTRALIA)
Program Number: 1035 Poster Board Number: B0169
Presentation Time: 3:15 PM–5:00 PM
A novel color pupillometric test using a short illumination
paradigm allows discrimination of glaucoma patients from
normal controls
Dan Milea1, 2, Rukmini A. V3, Baskaran Mani1, 2, Alicia How2, Shamira
A. Perera1, 2, Tin Aung1, 2, Joshua Gooley3. 1Singapore Eye Research
Institute, Singapore, Singapore; 2Singapore National Eye Centre,
Singapore, Singapore; 3Duke-NUS, Singapore, Singapore.
Purpose: The aim of this study was to evaluate the ability of
chromatic pupillometry, using a novel photic stimulation paradigm,
to discriminate glaucoma patients from healthy controls, by detect
functional loss of intrinsically photosensitive retinal ganglion cells
(ipRGCs).
Methods: In this cross-sectional study, we included 40 patients
with primary open angle glaucoma (POAG) and 161 healthy
controls, aged 50 and above. Pupillometry and standard ophthalmic
examination were performed in all participants; POAG patients were
also evaluated with standard automated perimetry (Humphrey Visual
Field, HVF, Carl Zeiss Meditec, Dublin, CA) and scanning laser
ophthalmoscopy (Heidelberg Retinal Tomography, HRT, Heidelberg
Engineering, Heidelberg, Germany). Dose-response curves of the
pupillary light responses (PLR) to narrowband blue light (469nm) or
red light (631nm), at increasing corneal irradiances, over 2 minutes
(7 to 14 log photons cm-2 s-1), were constructed. Pupil diameter was
recorded using an infrared pupillography system.
Results: The pupillary light reflex was reduced in patients with
POAG at high irradiance levels, corresponding to the range of
ipRGCs activation. Pupillary responses to high-irradiance blue
light associated more strongly with disease severity compared with
responses to red light, with a significant linear correlation observed
between pupil diameter and HVF mean deviation (r = -0.44, p =
0.005) as well as HRT linear cup disc ratio (r = 0.61, p <0.001).
Conclusions: This novel colour pupillometric test using exposure to
continuously increasing blue light allows accurate discrimination of
glaucomatous eyes from normal eyes. Further studies are needed to
determine if this test may also estimate the degree of visual function
loss in glaucoma.
Commercial Relationships: Dan Milea, None; Rukmini A. V,
None; Baskaran Mani, None; Alicia How, None; Shamira A.
Perera, None; Tin Aung, None; Joshua Gooley, None
Support: Singapore National Eye Centre Health Research
Endowment Fund 1005/20/2013
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Program Number: 1036 Poster Board Number: B0170
Presentation Time: 3:15 PM–5:00 PM
A Novel Testing Sequence for RAPDx Pupillography
Alice L. Williams, Xuanchu Duan, Priyanka Gogte, Michael
Waisbourd, Lisa A. Hark, George L. Spaeth. Wills Eye Hospital,
Philadelphia, PA.
Purpose: The presence of a relative afferent pupillary defect
(RAPD), traditionally detected with the swinging flashlight method,
is a sign of optic nerve pathology but is often subjective. An objective
tool that identifies and quantifies the degree of an RAPD could
be useful in identifying and staging patients with glaucoma. The
purpose of this study is to compare the standard testing sequence
on the RAPDx pupillograph (Konan Medical USA, Irvine, CA) to a
customized sequence. This novel sequence evokes a pupil response
curve which more closely resembles that produced by the swinging
flashlight method and allows for the measurement of a novel
pupillary response parameter, the duration of maximum constriction
(MC).
Methods: Forty-eight (48) patients with glaucoma underwent
Humphrey visual field testing and RAPDx pupillography using a
standard sequence and a custom sequence. Exclusion criteria included
active inflammation of the eye, recent intraocular procedure, and any
non-glaucomatous condition that may cause an RAPD, anisocoria or
corectopia. RAPDx testing results included the response amplitude
asymmetry (RAA), response latency asymmetry (RLA), and MC.
These parameters were correlated with the visual field mean deviation
(MD). Two-tailed p-values of Pearson correlation coefficients were
calculated to determine the significance of these correlations.
Results: Disease severity, as measured by average MD between the
fellow eyes, was significantly correlated with higher RAA values (r=
-0.3, p=0.04 for the standard sequence and r= -0.3, p=0.04 for the
custom sequence). Average MD was also significantly correlated with
higher RLA values for the custom sequence (r= -0.36, p=0.02) but
not the standard sequence (r= -0.18, p=0.20). Correlations between
average MD values and the novel pupillary response parameter, MC,
failed to reach significance.
Conclusions: RAA and RLA, quantitative measures of asymmetric
pupillary response between the two eyes, correlate with disease
severity as measured by visual field MD in a group of patients with
glaucoma. The custom testing sequence produces RLA values that
correlate more closely to disease severity than those produced by the
standard testing sequence. Further research is needed to determine
the most useful testing sequences and combinations of clinical and
pupillary response parameters for detecting and staging glaucoma.
Commercial Relationships: Alice L. Williams, None; Xuanchu
Duan, None; Priyanka Gogte, None; Michael Waisbourd, None;
Lisa A. Hark, None; George L. Spaeth, None
Support: Wills Eye Hospital Innovation Grant
Program Number: 1037 Poster Board Number: B0171
Presentation Time: 3:15 PM–5:00 PM
Macular pigment optical density in healthy and patients with
open angle glaucoma
Jessica Y. Lee1, 2, Katia Suarez-Berumen3, Kiana Nouri3, Emily Cook4,
Alfred Solish4, Pinakin Davey2. 1Graduate College of Biomedical
Sciences, Western University of Health Sciences, Pomona, CA;
2
College of Optometry, Western University of Health Sciences,
Pomona, CA; 3College of Osteopathic Medicine of the Pacific
(COMP), Western University of Health Sciences, Pomona, CA;
4
Ophthalmology, Southern California Glaucoma Consultants,
Pasadena, CA.
Purpose: The macular pigment optical density (MPOD) potentially
quench the free radicals and the reactive oxidative species in the
retina and may be protective to the ganglion cells, photoreceptors and
retinal pigment epithelial layer. One could postulate that patients with
accelerated death of ganglion cells like open angle glaucoma could
have decreased level of MPOD due to its pathophysiology. We sought
to investigate the level of MPOD in patients with glaucoma and
compare it to MPOD in ocular healthy individuals.
Methods: The MPOD was measured in 82 individuals (44
ocular healthy and 38 glaucoma patients) using the QuantifEye
heterochromatic flicker photometer in their dominant eye. The
statistical analysis was performed to evaluate the difference in
number of males and females, correlation between MPOD & age and
evaluate the difference in level of MPOD as a function of age, gender
and diagnosis.
Results: The males to females ratio was significantly different in
the glaucoma group versus ocular healthy group (Chi-square test
p=0.01) however the level of MPOD did not vary as a function of
gender (t-test p =0 39). Overall there was no association between age
and MPOD (Pearson correlation r=0.03; p=0.6). The mean MPOD
in the ocular healthy group was lesser than the glaucoma group 0.45
(SD 0.16) and 0.56 (SD 0.16) respectively which was significantly
different (independent samples t-test t-statistic=-2.87; p=0.005).
Conclusions: The macular pigment optical density in this study
was greater in glaucoma group compared to ocular healthy group.
This result contradicts prior published literature (Igras et al Br J
Ophthalmol. 2013). Further research is warranted to investigate the
reasons for the different findings in these studies to further understand
the role of MPOD in glaucoma pathogenesis.
Commercial Relationships: Jessica Y. Lee, None; Katia SuarezBerumen, None; Kiana Nouri, None; Emily Cook, None; Alfred
Solish, None; Pinakin Davey, None
Program Number: 1038 Poster Board Number: B0172
Presentation Time: 3:15 PM–5:00 PM
Development of a novel head-mounted perimeter
– Measuring the visual field of both eyes by showing the target
alternately and randomly to each eye –
Sayaka Yamao1, Chota Matsumoto1, Hiroki Nomoto1, Fumi Tanabe1,
Shigeki Hashimoto1, Sachiko Okuyama1, Yoshikazu Shimomura1,
Shinji Kimura2, Kenzou Yamanaka2, Makoto Aihara3. 1Department
of Ophthalmology, Kinki University Faculty of Medicine,
Osakasayama, Japan, Osakasayama, Japan; 2CREWT Medical
Systems, Inc., Tokyo, Japan; 3Shirato Eye Clinic, Tokyo, Japan.
Purpose: We developed a head-mounted perimeter with a
transmissive liquid crystal display for each eye that presents targets
separately and randomly to the right and left eyes. One of its features
is that it can measure the visual field concurrently with both eyes
open. This study was designed to compare the visual field sensitivity
of monocular and binocular perimetry using the head-mounted
perimeter.
Methods: We can measure the visual field wherever we like as
the perimeter is a head-mounted type. Its dimensions are W190 ×
D380 × H220 mm and weight is 1.6 kg. The target is presented on a
transmissive liquid crystal display with high intensity LED backlight.
Maximum brightness of the target is 10000 asb and backlight
brightness is 31.4 asb. The target can be shown in an arbitrary size
and form within 35° from the central visual field. We used Bayesian
estimate and adaptive measurement of maximum-likelihood estimate
as a threshold measurement algorithm. During the measurement, we
can continuously monitor both eyes and each visual fixation. The
location of the target is adjusted each time fixation disparity occurs.
We can measure the visual field in both eyes at one concurrent
examination by showing the target alternately and randomly to each
eye without the subject being aware of which eye is tested. This
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
study enrolled 11 normal subjects (age, 35.9 ± 7.18). All the subjects
underwent both monocular and binocular perimetry using the headmounted perimeter. The subjects were also checked if they noticed
which eye was tested. We weighed the sensitivity in all the individual
measurement points in monocular and binocular perimetry.
Results: The mean sensitivity with monocular perimetry for the right
and left eyes were 30.3 ± 4.02 dB and 30.4 ± 3.69 dB, respectively
and that with binocular perimetry for right and left were 30.6 ±
3.14 dB and 30.3 ± 3.32 dB, respectively. There was no statistically
significant difference in all the individual measurement points (P <
0.05). In addition, all the subjects could not recognize which eye was
tested.
Conclusions: The head-mounted perimeter enables us to measure
the visual field in both eyes concurrently with the same precision as
monocular perimetry while the subject is unaware of which eye is
tested. This could contribute to the diagnosis of feigned blindness.
Commercial Relationships: Sayaka Yamao, CREWT Medical
Systems, Inc. (F); Chota Matsumoto, CREWT Medical Systems,
Inc. (F); Hiroki Nomoto, CREWT Medical Systems, Inc. (F); Fumi
Tanabe, CREWT Medical Systems, Inc. (F); Shigeki Hashimoto,
CREWT Medical Systems, Inc. (F); Sachiko Okuyama, CREWT
Medical Systems, Inc. (F); Yoshikazu Shimomura, CREWT
Medical Systems, Inc. (F); Shinji Kimura, CREWT Medical
Systems, Inc. (E), CREWT Medical Systems, Inc. (P); Kenzou
Yamanaka, CREWT Medical Systems, Inc. (E), CREWT Medical
Systems, Inc. (P); Makoto Aihara, CREWT Medical Systems, Inc.
(C)
Support: CREWT Medical Systems, Inc.
Program Number: 1039 Poster Board Number: B0173
Presentation Time: 3:15 PM–5:00 PM
Detecting Functional Loss in Glaucoma with the Performance
Centered Portable Test (PERCEPT)
Ricardo Y. Abe1, 2, Carolina Gracitelli1, 3, Alberto Diniz-Filho1, 4,
Saif Baig1, Peter N. Rosen1, Erwin R. Boer1, 5, Felipe A. Medeiros1.
1
Visual Performance Laboratory, Department of Ophthalmology,
University of California San Diego, La Jolla, CA; 2Department
of Ophthalmology, University of Campinas, Campinas, Brazil;
3
Department of Ophthalmology, Federal University of São
Paulo, São Paulo, Brazil; 4Department of Ophthalmology and
Otorhinolaryngology, Federal University of Minas Gerais, Belo
Horizonte, Brazil; 5Department of Mechanical Engineering, Delft
University of Technology, Delft, Netherlands.
Purpose: To evaluate the ability of a tablet-enabled test
(PERformance CEntered Portable Test - PERCEPT) to detect
functional loss in glaucoma patients.
Methods: Cross-sectional study involving 35 eyes from 27 patients
with glaucomatous visual field defects on standard automated
perimetry (SAP) and 32 eyes from 21 control subjects without
visual field defects. The PERCEPT was based on the concept of
increasing visual task difficulty to improve detection of central visual
field losses in glaucoma patients. Subjects had to perform a foveal
8-alternative-forced-choice orientation discrimination task, while
detecting a simultaneously presented peripheral stimulus within a
limited presentation time and under low contrast level. Higher values
of the PERCEPT processing speed (PPS) test in milliseconds (ms)
implies worse visual performance to detect the stimuli. Retinal nerve
fiber layer (RNFL) thickness was assessed by spectral domain optical
coherence tomography (SD-OCT). Areas under the receiver operating
characteristic (ROC) curves were used to evaluate the ability of
the different parameters to discriminate glaucomatous from control
subjects.
Results: The PPS parameter showed significantly larger values in
glaucoma (746.9 ms) compared to controls (258.3 ms) (P < 0.001).
Areas under the ROC curves for the PPS parameter and average SDOCT RNFL thickness were 0.83 ± 0.04 and 0.82 ± 0.04, respectively
(P = 0.851). For detection of moderate or severe glaucoma (mean
deviation of SAP < -6 dB), ROC curve areas were 0.89 ± 0.03 and
0.92 ± 0.03, respectively (P = 0.471).
Conclusions: The PERCEPT processing speed parameter was able
to successfully discriminate eyes with and without visual field loss
on SAP and performed similarly to the SD-OCT parameter average
thickness. Due to its low-cost and portability, this tablet-enabled
platform may be a feasible test for screening of visual impairment.
Commercial Relationships: Ricardo Y. Abe, None; Carolina
Gracitelli, None; Alberto Diniz-Filho, None; Saif Baig, None;
Peter N. Rosen, None; Erwin R. Boer, None; Felipe A. Medeiros,
Alcon Laboratories Inc (F), Alcon Laboratories Inc (R), Allergan (F),
Bausch & Lomb (F), Carl Zeiss Meditec Inc (C), Carl Zeiss Meditec
Inc (F), Carl Zeiss Meditec Inc (R), Heidelberg Engineering Inc (F),
Merck Inc (F), National Eye Institute (F), Novartis (C), Reichert Inc
(F), Reichert Inc (R), Sensimed (F), Topcon Inc (F)
Support: EY021818, P30EY022589 and participant retention
incentive grants in the form of glaucoma medication at no cost
from Alcon Laboratories Inc, Allergan, Pfizer Inc, and Santen Inc.
Unrestricted grant from Research to Prevent Blindness, New York,
New York
Program Number: 1040 Poster Board Number: B0174
Presentation Time: 3:15 PM–5:00 PM
Development of a simple driving simulator (DS) with gazetracking system and factors and visual subfield relating to the
DS-collision in glaucoma patients
Aiko Iwase1, Makoto Araie2, Shiho Kunimatsu-Sanuki3, Hiroshi Ono4,
Yuto Susuki5, Yuko Ohno5. 1Ophthalmology, Tajimi Iwase Eye Clinic,
Tajimi, Japan; 2Kanto Central Hospital of the Mutual Aid Association
of Public School Teachers, Tokyo, Japan; 3Ophthalmology, Tohoku
University Graduate School of Medicine, Sendai, Japan; 4Honda
Motor Co, Tokyo, Japan; 5Division of Health Sciences, Osaka
University Graduate School of Medicine, Osaka, Japan.
Purpose: An adequate visual field (VF) is a requisite for safe
driving and effects of glaucoma on motor vehicle accident (MVA)
involvement have been vigorously studied. A driving simulator (DS)
is often used to create controlled conditions for evaluation of driving
performance, but most DSs are not equipped with gaze monitoring
system which is indispensable for correlating VF abnormalities
to MVA involvement. We studied effects of glaucomatous VF on
collision using a DS systen equipped with a gaze-tracking system.
Methods: A modified version of Honda safety Navi DS System
(Honda Motor Co., Tokyo) which reproduces the driver’s view from a
right-hand-drive car on the screen 114 cm apart was equipped with a
gaze-tracking system (NAC EMR-9, nac Image Technology, Tokyo),
and the driver’s gaze point (DGP) was monitored in real-time on a
personal computer display which also reproduced the driver’s view.
The instant when the driver first detected the hazard was determined
by a saccadic movement of the DGP toward the hazard. The driver’s
binocular integrated VF (IVF) calculated by merging the 2 monocular
Humphrey Field Analyzer 24-2 Swedish Interactive threshold
Algorithm (Carl Zeiss Meditec., CA) test results and centered on the
DGP just before detecting the hazard was projected onto the driver’s
view. 52 glaucoma patients (66.2+/-9.2 yrs.; mean deviation (MD)
of the better eye=-8.1+/-6.3 dB; mean IVF sensitivity=22.0+/-6.0
dB) participated in the DS experiment and were required to avoid an
oncoming right-turning car, the hazard, at an intersection. The Ethic
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Committee of Gifu Prefecture Medical Association approved the
study.
Results: 15 of the 52 collided with the hazard. It took longer time for
the collision-involved examinees to detect the hazard than those not
(0.65+/-0.66 vs. 0.25+/-0.30 sec, P0.012). The decision tree method
correlated 3 IVF test points to the collision and sensitivity was lower
in the former than the latter at a point just inferior and right to the
fixation (22.0+/-3.8 vs. 29.8+/-5.8 dB, P0.016). Visual acuity and MD
of the dominant eye were also correlated with the collision (k=0.59,
Partition, JMP Pro11.0,SAS)
Conclusions: A DS with a gaze-tracking system was developed,
which enabled us to study the location and sensitivity of the patient’s
IVF subfield related to MVA involvement in a given scenario of DS.
Commercial Relationships: Aiko Iwase, None; Makoto Araie,
None; Shiho Kunimatsu-Sanuki, None; Hiroshi Ono, Honda Motor
Co (E); Yuto Susuki, None; Yuko Ohno, None
Program Number: 1041 Poster Board Number: B0175
Presentation Time: 3:15 PM–5:00 PM
Use of Mixture Item Response Theory to Identify Classes of
Functionally Impaired Glaucoma Patients from Analyses of
Patient-Reported Outcomes
Ling Bei1, Carolina Gracitelli1, 2, Linda M. Zangwill1, Robert
N. Weinreb1, Felipe A. Medeiros1. 1Hamilton Glaucoma Center,
University of California San Diego, La Jolla, CA; 2Ophthalomology,
Federal University of São Paulo, São Paulo, Brazil.
Purpose: To use mixture item response theory (IRT) to identify
subclasses of functionally impaired glaucoma patients by analysis of
results from the National Eye Institute Visual Function Questionnaire
(NEI VFQ-25).
Methods: This is a cross-sectional study involving 586 patients
with glaucomatous optic neuropathy. All subjects had testing with
standard automated perimetry (SITA Standard 24-2) and responded
the NEI VFQ-25 questionnaire for assessment of quality of life. The
25 items of the NEI VFQ-25 were subdivided into visual function and
socio-emotional subscales. Mixture item response theory was used
to identify subclasses of patients according to their questionnaire
responses. The Vuong-Lo-Mendell-Rubin likelihood ratio test was
used to investigate number of classes.
Results: Four classes of subjects were identified by the mixture IRT
model. The model had entropy of 0.836. The first class contained
the majority of subjects (411 patients) and showed normal results
for both the visual function and socio-emotional subscales. The
second class (51 patients) had abnormal results on both scales. The
third class had abnormal results only on the visual function scale
(57 patients), whereas a fourth class (67 patients) showed abnormal
results only on the socio-emotional scale. Compared to the reference
(normal) class, subjects in classes 2 and 3 had worse results on SAP
binocular mean sensitivity. However, subjects in class 4 (socioemotional) did not show abnormal visual field results compared to the
reference class.
Conclusions: Different subclasses of functionally impaired glaucoma
patients were identified from analysis of NEI VFQ-25 results by
mixture modeling. These findings suggest that the NEI VFQ-25 lacks
unidimensionality and that this needs to be taken into account when
evaluating the relationship between results of this questionnaire and
tests of visual function in glaucoma.
Commercial Relationships: Ling Bei, None; Carolina Gracitelli,
None; Linda M. Zangwill, Carl Zeiss Meditec Inc. (F), Heidelberg
Engineering GmbH (F), Nidek Inc. (F), Optovue Inc. (F), Topcon
Medical Systems Inc. (F); Robert N. Weinreb, Aerie (F), Alcon
Laboratories (C), Allergan Inc. (C), Amatek (C), Aquesys (C), Bausch
& Lomb (C), Carl Zeiss Meditec Inc. (C), Carl Zeiss Meditec Inc.
(F), Genentech (F), Heidelberg Engineering GmbH (F), Nidek Inc.
(F), Novartis (F), Optovue Inc. (F), Topcon Medical Systems Inc. (C),
Topcon Medical Systems Inc. (F), Valeant (C); Felipe A. Medeiros,
Alcon Laboratories Inc. (F), Alcon Laboratories Inc. (R), Allergan
Inc. (C), Allergan Inc. (F), Allergan Inc. (R), Bausch & Lomb (F),
Carl Zeiss Meditec Inc. (C), Carl Zeiss Meditec Inc. (F), Carl Zeiss
Meditec Inc. (R), Heidelberg Engineering GmbH (F), Merck Inc. (F),
National Eye Institute (F), Novartis (C), Reichert Inc. (F), Reichert
Inc. (R), Sensimed (F), Topcon Medical Systems Inc. (F)
Support: EY11008, U10EY14267, EY019869, EY021818,
P30EY022589 and participant retention incentive grants in the form
of glaucoma medication at no cost from Alcon Laboratories Inc,
Allergan, Pfizer Inc, and Santen Inc.Unrestricted grant from Research
to Prevent Blindness, New York, New York. CAPES 12309-13-3
Clinical Trial: NCT00221897
Program Number: 1042 Poster Board Number: B0176
Presentation Time: 3:15 PM–5:00 PM
A longitudinal evaluation of the spatial concordance in location of
visual field defects in glaucoma
Ankita Sutaria1, Darrell WuDunn1, Megan M. Tuohy1, Rongrong Hu1,
2
, Nabeel Awan1, Ira Altaras1, Lyne Racette1. 1Ophthalmology, Indiana
University Glick Eye Institute, Indianapolis, IN; 2Ophthalmology,
First Affiliated Hospital, College of Medicine, Zhejiang University,
Hangzhou, China.
Purpose: Glaucoma presents bilaterally in many patient, with a
lag between presentation in the right and left eyes. In this analysis
performed on the prospective data collected in an observational study,
we assessed whether the overlap in the location of abnormal visual
field (VF) between the right and left eyes increases over time.
Methods: The dataset included 97 patients diagnosed with primary
open-angle glaucoma were selected from the Diagnostic Innovations
in Glaucoma Study (DIGS) and from the African Descent and
Glaucoma Evaluation Study (ADAGES). The eye with the more
advanced visual defect was selected as the reference eye (RE).
The RE had a repeatable defect defined as a cluster of at least three
points and no more than 26 abnormal points on the patter deviation
plot (PDP). The fellow eye (FE) had at least ten follow up visits
separately by at least 5 months. The VF of the RE was compared to
each consecutive VF in the FE. The inter-eye concordance (IEC) ratio
was calculated using this formula: 2C/(A+B+2C), where A represents
locations abnormal in the right eye only, B represents locations
abnormal in the left eye only, and C represents locations abnormal
in both eyes (Boden et al, Ophthalmology, 2006; 113:918-23). The
slopes for the IEC ratio over time were calculated for each patient.
Results: Overall, a slightly positive mean slope was obtained
(0.00003). Although the mean slope was small, it was positive as
expected if the IEC increases over time. Furthermore, of the 97
patients included in the study, 71 (73.2%) had positive slopes.
Conclusions: Inter-eye concordance increased slightly over time
and more patients positive than negative slopes. The small slopes we
obtained are in part due to the strict criteria we used for concordance
given the known variability present in visual fields: the exact same
location had be abnormal. Our results suggest that defects may
develop in the same location in both eyes over time. In patients
with unilateral glaucoma, particular attention should be given to the
location showing defect in the affected eye.
Commercial Relationships: Ankita Sutaria, None; Darrell
WuDunn, None; Megan M. Tuohy, None; Rongrong Hu, None;
Nabeel Awan, None; Ira Altaras, None; Lyne Racette, None
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Support: Unrestricted grant from Research to Prevent Blindness
(Indianapolis, IN, USA); P30EY022589, EY021818, EY11008,
U10EY14267, and EY019869; Eyesight Foundation of Alabama;
Alcon Laboratories, Inc.; Allergan, Inc.; Pfizer, Inc.; Merck, Inc.;
Santen, Inc.; Edith C. Blum Research Fund of the New York
Glaucoma Research Institute (New York, NY, USA); and an
unrestricted grant from Research to Prevent Blindness (New York,
NY, USA)
Clinical Trial: NCT00221897; NCT00221923
Program Number: 1043 Poster Board Number: B0177
Presentation Time: 3:15 PM–5:00 PM
Speeding up visual field tests by incorporating spatial models
Nikki Rubinstein1, 2, Allison M. McKendrick1, Andrew Turpin2.
1
Optometry and Vision Sciences, The University of Melbourne,
Parkville, VIC, Australia; 2Computing and Information Systems, The
University of Melbourne, Parkville, VIC, Australia.
Purpose: Many perimetric test algorithms exploit spatial
relationships in the visual field (VF) for the initial location estimates
of sensitivities or in a post-processing phase. We define a new
algorithm (LiSZE: Likelihood Scaling ZEST) that uses spatial
information on every presentation to alter VF estimates. We
hypothesised that LiSZE would reduce test times without detriment
to output precision and accuracy.
Methods: LiSZE is a maximum likelihood Bayesian procedure,
which maintains a separate probability mass function (PMF) for each
VF location. For each presentation, the location whose PMF has the
largest standard deviation is tested, with the stimulus level set at the
mean of the PMF. The PMF is updated with a likelihood function
whose shape is dependent on the observer’s response. Any location in
the VF that is related to that tested – according to a spatial model – is
also updated with a modified likelihood function (scaled vertically
and translated via an eccentricity correction factor). Spatial models
were created based on: empirical data (Gardiner et al, Vis Res 2004),
computational models (Denniss et al, IOVS 2012), nearest neighbour
and random relationships.
LiSZE was tested using computer simulations on 163 glaucomatous
and 233 normal VFs (HFA 24-2 FT). ZEST was simulated as a
baseline. Output measures included: number of presentations and
visual sensitivity estimates. Errors were calculated by subtracting the
estimated VF from the input VF.
Results: Median error for each VF was used as a global index of
accuracy. LiSZE had similar accuracy to ZEST (median normal(dB)/
glaucoma(dB): ZEST 0.5/0, LiSZE 0/-0.5-0), but higher variability
(5th-95th percentile normal(dB)/glaucoma(dB): ZEST 1/1, LiSZE
2/1-1.5). We split results by input sensitivity (IS) to reveal differences
between the LiSZE spatial models. The random model performed
worst (absolute error and IQR worse than ZEST by up to 6dB for
IS <28dB). The empirical model was best, with similar accuracy
and better precision than ZEST (most IS had 1-2dB greater IQR
(variability) for ZEST than empirical model LiSZE). Inspection
of VF maps showed that LiSZE was able to detect localised VF
loss. LiSZE was faster than ZEST: median number of presentations
reduced by 10–25% for glaucoma and 25–46% for normals.
Conclusions: LiSZE has the potential to reduce VF test times.
Simulations suggest that the empirical model produces a similar error
profile to ZEST, while reducing test time.
Commercial Relationships: Nikki Rubinstein, None; Allison
M. McKendrick, Carl-Zeiss Meditec (R), Haag-Streit AG (C),
Heidelberg Engineering GmBH (F); Andrew Turpin, Centervue Inc.
(R), Haag-Streit AG (C), Heidelberg Engineering GmBH (F)
Support: ARC LP 130100055
Program Number: 1044 Poster Board Number: B0178
Presentation Time: 3:15 PM–5:00 PM
Cluster visual field progression and its relationship with optic
disc changes
Valeria Bono1, 2, Eduardo M. Normando1, 3, Ben Davis1, Laura
Crawley3, Faisal Ahmed3, Salvatore Cillino2, Philip Bloom3, M
Francesca Cordeiro1, 3. 1Glaucoma & Retinal Neurodegeneration
Research Group, Visual Neuroscience, UCL, Institute of
Ophthalmology, London, United Kingdom; 2Experimental
Biomedicine and Clinical Neuroscience, Ophthalmology Section,
University of Palermo, Palermo, Italy; 3Western Eye Hospital
& ICORG, Imperial College Healthcare Trust, London, United
Kingdom.
Purpose: Glaucoma diagnosis and follow up of progression is often
based on structural and functional assessments. This study aimed
to assess clustered progression and evaluate its correlation with
the corresponding disc changes (RA sectors) obtained from HRT
examinations.
Methods: 51 eyes from OHT and glaucoma patients with a minimum
of 5 reliable visual field tests (HFA II i 24-2) and HRT with a
follow-up >4 years were analyzed retrospectively. Linear regression
of clusters defined by the Glaucoma Hemifield Test (GHT) was
performed based on the mean threshold in each cluster. Global and
sectoral rates of change in RAs were assessed and correlated with
functional clustered measures. Clustered rates of VF and RA change
were flagged as statistically significant progression if the gradients
over time were negative with p<0.05.
Results: GHT cluster analysis and RA rates classified 78,5%
(clusters ≥ 1) and 86.3% eyes as progressing, respectively, with poor
agreement (k=0.06). The median number of progressing cluster was
1.3 and visual field progression was greater and more frequently
seen in clusters 4 (23.1%) and cluster 1 (21.5%). 88.6% of eyes
with progression in both clusters and rim areas showed correlation
between rim area sectors and corresponding visual field clusters.
Conclusions: Visual field clusters successfully detected spatial
locations of sensitivity loss showing concordance with structural rim
area measures. This suggests GHT clusters to be a sensitive method
for the early identification of glaucomatous visual field loss.
Percentage of subjects with progression in GHT cluster and HRT.
Commercial Relationships: Valeria Bono, None; Eduardo M.
Normando, None; Ben Davis, None; Laura Crawley, None; Faisal
Ahmed, None; Salvatore Cillino, None; Philip Bloom, None; M
Francesca Cordeiro, None
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Program Number: 1045 Poster Board Number: B0179
Presentation Time: 3:15 PM–5:00 PM
Measuring Glaucoma Progression Using a Common Factor
Model
Richard A. Bilonick1, 2, Yun Ling1, Gadi Wollstein1, Hiroshi Ishikawa1,
3
, Larry Kagemann1, 3, Ian A. Sigal1, Michelle G. Sandrian1, 3,
Joel S. Schuman1, 3. 1UPMC Eye Center, Eye and Ear Institute,
Ophthalmology and Visual Science Research Center, Department
of Ophthalmology, University of Pittsburgh School of Medicine,
Pittsburgh, PA, Pittsburgh, PA; 2Department of Biostatistics, Graduate
School of Public Health, University of Pittsburgh, Pittsburgh, PA,
Pittsburgh, PA; 3Department of Bioengineering, Swanson School of
Engineering, University of Pittsburgh, Pittsburgh, PA, Pittsburgh, PA.
Purpose: To construct a common factor (CF) model to determine
what the visual field [VF] measurements (mean deviation [MD],
pattern standard deviation [PSD], and visual field index [VFI]) have
in common and what is unique to each. The common factor can then
be estimated and used as an optimal index for glaucoma progression.
Methods: MD, PSD, VFI, baseline age, and glaucoma diagnosis
(healthy [H] vs glaucoma [G]) were available for 57 subjects. Ages
ranged from 41–76 yrs. 32% (18) of left and 39% (22) of right eyes
had glaucoma. CF model is illustrated by the path diagram (Figure).
True CF slopes for each eye are represented by latent variables (OS
& OD) which were scaled to have mean 0 and standard deviation
(SD) 1. VF slopes were also linearly transformed to mean 0 and SD
1 so that the factor loadings (λ1 for MD, λ2 for PSD, and λ3 for
VFI) represent the correlation between each VF measurement and
the latent CF slope. The residual error variances (e1, e2, an e3) equal
1-.λ2. The latent factors OS and OD were allowed to have correlation
ρ. Each latent factor was dependent on age and diagnosis (H=0,
G=1). Onyx visual SEM software produced the path diagram and
initial parameter estimates shown in Figure. Onyx cannot currently
include constraints necessary for the residual error variances but was
used to generate the equivalent OpenMx SEM code. This code was
then modified to include the constraints. R software for statistical
computing was used to determine the full information maximum
likelihood parameter estimates.
Results: Parameter estimates and 95% confidence intervals are
shown in Table. ρ was 0.508 and was statistically significant (SS).
Age effect was near zero and not SS. The effect for diagnosis showed
that the latent progression slope for eyes with glaucoma was lower
than for healthy and the difference was SS. The correlations between
the visual field measurements and the latent progression factors were
similar for MD and PSD (ratio not SS) and substantially lower than
for VFI (SS). Thus VFI was the most precise at assessing glaucoma
progression.
Conclusions:
The CF model calibrated the VF measurements and determined what
they had in common (λ) and what was unique (e). VFI was shown
to be substantially more precise than both MD and PSD and the CF
slopes differed between healthy and glaucoma.
Commercial Relationships: Richard A. Bilonick, None; Yun Ling,
None; Gadi Wollstein, None; Hiroshi Ishikawa, None; Larry
Kagemann, None; Ian A. Sigal, None; Michelle G. Sandrian,
None; Joel S. Schuman, Zeiss (P)
Support: NIH R01-EY013178, P30 EY008098; Eye and Ear
Foundation (Pittsburgh, PA); Research to Prevent Blindness (New
York, NY).
Program Number: 1046 Poster Board Number: B0180
Presentation Time: 3:15 PM–5:00 PM
Distributions of glaucomatous visual field progression rates: a
comparison of three parametric models
Andrew J. Anderson. Department of Optometry & Vision Sciences,
The University of Melbourne, Parkville, VIC, Australia.
Purpose: Parametric models of the distribution of glaucomatous
visual field progression rates (in dB/year) can be used in Bayesian
methods for improving progression rate estimation, for summarising
how distributions differ between different populations and as
a function of glaucoma risk factors, and for overcoming the
problems that arise when zero-frequency histogram bins occur at
intermediate progression rates in empirical data. Here we compare
three parametric models to test if one is clearly preferred for fitting
published distributions of visual field progression rates for glaucoma.
Methods: We used a modified Gaussian model, a modified
Cauchy model and a modified hyperbolic secant model, each of
which had three free parameters. The modification allowed the
shape of the model’s distribution either side of the mode to be
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
independently varied to allow for the asymmetric tails seen in visual
field progression rate distributions. Models were fit to published
distributions of the overall (i.e. non-pointwise) rates of visual field
loss in glaucoma cohorts from Canada, Sweden and the USA, using a
maximum-likelihood procedure. Goodness-of-fit was quantified with
a coefficient of determination, R2.
Results: For the Canadian data, log10 likelihoods for the modified
Gaussian, Cauchy and hyperbolic secant models were -3036.8,
-2891.1 & -2893.9 (R2: 0.77, 0.99 & 0.94), respectively, indicating
that the modified Cauchy model fitted best and was 583 times
(-2891.1 minus -2893.9 = 2.8 log units) more likely than the next best
fitting model, the modified hyperbolic secant. For the Swedish data,
likelihoods were -695.2, -701.3 and -684.1 (R2: 0.92, 0.96 & 0.98),
indicating the modified hyperbolic secant gave the best fit (by 1.0x106
times). For the USA data, likelihoods were -412.3, -412.1 and -402.8
(R2: 1.00, 0.94 & 0.92), indicating the modified hyperbolic secant
gave the best fit (by 2.8x109 times). Summing likelihoods across
datasets, the hyperbolic secant was strongly favoured (by 26.7 log
units) compared to the next best fitting model, the modified Cauchy.
Conclusions: Parametric models can describe well the distribution
of visual field progression rates in treated glaucoma. Although the
optimum model differs depending upon the particular dataset fitted,
a modified hyperbolic secant performed well for all distributions
investigated and was strongly favoured when evidence was summed
across datasets.
Commercial Relationships: Andrew J. Anderson, None
Support: Australian Research Council Future Fellowships
FT120100407
Program Number: 1047 Poster Board Number: B0181
Presentation Time: 3:15 PM–5:00 PM
Age as a predictor of future rate of visual field change in
glaucoma: Traditional statistics and tree-based modeling
Shaban Demirel, Brad Fortune, Steven L. Mansberger, Stuart K.
Gardiner. Devers Eye Institute, Legacy Research Institute, Portland,
OR.
Purpose: In perimetry, mean deviation (MD) is corrected for age.
However, age is also a risk factor for glaucomatous progression. We
therefore aim to determine whether age influences cross-sectional and
longitudinal structure-function relations in eyes with glaucoma and
glaucoma suspect eyes.
Methods: Structural (OCT, Spectralis), functional (HFA 24-2, Carl
Zeiss Meditec), ocular (IOP, central corneal thickness; CCT) and
systemic blood pressure data were collected every six months from
participants enrolled in the longitudinal Portland Progression Project.
Data from the most recent 7 visits where perimetry was reliable
and OCT was of acceptable quality were used (n=173, both eyes if
available). We investigated the cross-sectional structure-function
relation by using structural (global retinal nerve fiber layer thickness;
RNFLT), ocular and systemic data from the 1st visit to predict MD
at the 1st visit (MD1). We investigated the longitudinal structurefunction relation by using the rate of RNFLT change over time,
together with the average ocular and systemic measures during the
sequence, to predict the rate of MD change over time (MDR). Age
at the 1st visit was used in both analyses. Traditional multivariate
statistics (generalized estimating equations) and tree-based models
were used.
Results: Global RNFLT (P<0.001) and age (P=0.027) were the only
significant predictors of MD1. This suggests that age influences the
cross-sectional structure-function relation. For each 1mm thinner
RNFLT, MD1 was 0.1dB worse and for each decade older, MD1 was
0.3dB worse. RNFLT and age were the most important predictors of
MD1 in tree-based models. The rate of change of RNFLT (P=0.004)
and baseline age (P<0.001) were the only significant predictors
of MDR. This suggests that age also influences the longitudinal
structure-function relation. For each 1 mm/yr thinning of RNFLT,
MDR was 0.05 dB/yr worse and for each decade older, MDR was
0.02 dB/yr worse. Age and the rate of RNTLT change were the most
important predictors of MDR in tree-based models.
Conclusions: Age significantly influences both the crosssectional and longitudinal structure-function relation in glaucoma.
Furthermore, the rate of visual field change is significantly influenced
by age, whereas it was not influenced by IOP, CCT or blood pressure
in this clinically managed cohort.
Commercial Relationships: Shaban Demirel, Carl Zeiss Meditec
(F), Heidelberg Engineering (F); Brad Fortune, None; Steven L.
Mansberger, Alcon (C), Allergan (C), Allergan (S), Envisia (C),
Forsight Vision5 (C), Mobius (S), NEI (S), Santen (C), Welch Allyn
(C); Stuart K. Gardiner, Carl Zeiss Meditec (C)
Support: EY019674 (SD), EY020922 (SKG) and The Legacy Good
Samaritan Foundation.
Program Number: 1048 Poster Board Number: B0182
Presentation Time: 3:15 PM–5:00 PM
Contrast Sensitivity by M&S Smart System II and Visual field
Parameters in Patients with Primary Open-Angle Glaucoma
Jessica L. Liu1, 2, Sachin Jain1, Tieu Vy Nguyen1, J Jason McAnany1,
Jacob T. Wilensky1, Ahmad A. Aref1, David Hillman1, Thasarat S.
Vajaranant1. 1Ophthalmology and Visual Sciences, University of
Illinois at Chicago, Chicago, IL; 2Saint Louis University School of
Medicine, St. Louis, MO.
Purpose: Loss of contrast sensitivity (CS) may occur early in
glaucoma, and precede clinically detectable changes in visual
acuity (VA) and visual field (VF). CS testing by a computerized
vision-testing device (M&S Smart System II) has been validated
against thea gold standard Pelli-Robson CS testing. We determined
relationships between CS by the M&S Smart System II and routine
visual functional measures in patients with glaucoma.
Methods: We recruited patients with primary open-angle glaucoma
(POAG) without other eye conditions. Each patient underwent 1)
VA and CS testing in a standardized manner using a calibrated M&S
Smart System II; and 2) VF testing (Humphrey SITA 24-2). Inclusion
criteria included VA > 20/40 and reliable VF testing (fixation
losses, false positives and false negatives < 33%). Spearman rank
correlations were used to determine relationships within CS, VA,
and VF parameters including mean deviation (MD), pattern standard
deviation (PSD), and visual field index (VFI). Only the better eye
was recruited for analysis based on MD. Based on the Bonferroni
correction for multiple comparisons, correlations were considered
statistically significant if p-value < 0.005 (two-tailed).
Results: A total of 108 eyes of 108 patients met the inclusion criteria
and were included for analysis. The mean age of the patients included
was 65.81±12.74 years old. The mean BCVA was 20/25 (logMAR:
0.09±0.10) and the mean CS was 1.37±0.16. The spearman rank
correlation coefficients are shown in Table 1. Amongst the VF
parameters, VA correlated most strongly with MD. CS correlated
most strongly with MD and VFI.
TABLE 1: Correlations between Contrast Sensitivity Testing and
Visual Functional Measures
Conclusions: When compared to VA, CS correlates to a greater
degree with all three VF parameters. Our results suggest that CS
can serve as a surrogate for VF measures, supporting routine use
of CS testing. Given that CS testing by the M&S System can be
done quickly, incorporation into a budy clinical practice is practical.
Patients with POAG often experience decreased vision without
discernable changes in their VA. Since VF testing is not routinely
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
performed at each visit, CS testing could be used more frequently to
monitor subjective deterioration in quality of vision in patients with
POAG. The strong correlations between CS, MD and VFI drive home
these conclusions.
Enroth-Cugell (t = -4.92, p < 0.0001) but not for the method of KingSmith & Kulikowski (t = +0.67, p = 0.25).
Conclusions: These data provide support for comparing
glaucomatous defects with sinusoids and luminance increments using
the method of King-Smith & Kulikowski rather than the method of
Shapley & Enroth-Cugell.
Commercial Relationships: Jessica L. Liu, None; Sachin Jain,
None; Tieu Vy Nguyen, None; J Jason McAnany, None; Jacob T.
Wilensky, None; Ahmad A. Aref, None; David Hillman, None;
Thasarat S. Vajaranant, None
Support: ISPB grant, K23EY022949 (TSV), UIC core grant, dept
RBP, Unrestricted Grant from Research to Prevent Blindness
Program Number: 1049 Poster Board Number: B0183
Presentation Time: 3:15 PM–5:00 PM
Comparing Defect Depths for Different Perimetric Stimuli
William H. Swanson1, Andrew J. Anderson2. 1School of Optometry,
Indiana University, Bloomington, IN; 2Department of Optometry &
Vision Sciences, The University of Melbourne, Melbourne, VIC,
Australia.
Purpose: Perimetric defect depths for sinusoids (e.g. frequencydoubling stimuli) must be converted into Weber contrast before
being compared to defects for luminance increments (e.g. Goldmann
stimuli). Shapley & Enroth-Cugell (1984) used (Peak-Trough)/
Trough for this conversion, while King-Smith & Kulikowski (1975)
used (Peak-Mean)/Mean. Here we compare the performance of these
conversion methods.
Methods: One eye each was tested for 41 patients with glaucoma and
19 age-similar controls free of ocular disorders, on custom testing
stations. The first dataset tested 11 patients using static 200 msec
presentations of Gaussian blobs with standard deviations of 0.25° and
0.50°, and a Gabor sinusoid in cosine phase at 0.5 cycle/degree with
a standard deviation of 0.50°. The maximum for (Peak-Mean)/Mean
was 800% for the blobs and 434% for the Gabor. The three stimuli
were compared at 30 locations within ±9° of the horizontal midline.
The second dataset tested 21 patients using stimuli scaled with visual
field location. Each Gaussian blob had a standard deviation that was
½ the standard deviation of the Gabor at that visual field location, and
the two stimuli were compared at 14 locations across the visual field.
The blobs were presented using static 200 msec presentations and the
Gabors were presented as 3 cycles of 5 Hz counterphase flicker. The
maximum for (Peak-Mean)/Mean was 800% for the blobs and 70%
for the Gabors. The third dataset tested 20 patients with the same
stimuli and locations as the second dataset, but with more stimulus
presentations per location.
Results: The Akaike Information Criterion favored the method of
King-Smith & Kulikowski for all three datasets: log likelihoods (base
10) of 17.8, 2.1 and 2.5 for datasets 1, 2 & 3, respectively. BlandAltman analysis of the first dataset found that disagreement became
greater at higher threshold elevations for the method of Shapley &
Results for Experiment 1. For each visual field location of each
patient, threshold elevation was computed as the contrast threshold
for the patient divided by the mean contrast threshold for the control
group at that location.
Commercial Relationships: William H. Swanson, Carl Zeiss
Meditec (C), Heidelberg Engineering (C); Andrew J. Anderson,
None
Support: NIH grants R01EY007716, R01EY024542,
5P30EY019008, Australian Research Council grant FT120100407
Program Number: 1050 Poster Board Number: B0184
Presentation Time: 3:15 PM–5:00 PM
Evaluation of Damato Multifixation Campimetry Online, an
online visual field test, in detection of glaucomatous defects
Ane Sophie Olsen1, Mark Alberti1, Morten D. De La Cour1, Lisbeth
Serup2, Bertil E. Damato3, Miriam Kolko4, 5. 1Ophthalmology,
Glostrup Hospital, University of Copenhagen, Glostrup, Denmark;
2
Private ophthalmologist, Copenhagen, Denmark; 3UCSF, San
Francisco, CA; 4Ophthalmology, Roskilde University Hospital,
Roskilde, Denmark; 5Department of Neuroscience and Pharmacology,
University of Copenhagen, Copenhagen, Denmark.
Purpose: To study Damato Multifixation Campimetry Online
(DMCO), a free of charge Internet-based visual field test. The
focus was on: (i) the sensitivity and the specificity of DMCO in the
detection of glaucomatous visual field loss and (ii) algorithms for the
interpretation of DMCO results.
Methods: A standard laptop, a wireless mouse and a 22” computer
monitor was placed on a height-adjustable table. Participants
were asked to wear their usual spectacles. DMCO is an automated
supra-threshold test of the central 24° visual field using dark stimuli
examining 42 fixation targets located sequentially on different parts
of the computer screen. Three versions of DMCO exist; the different
versions differ in visual stimuli: DMCO Standard uses black stimuli,
DMCO Basic requires the patient to identify a numbered fixation
target and DMCO Advanced incorporates light-grey, dark-grey and
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
black stimuli. The three DMCO versions were tested in a blinded
fashion. Fifteen algorithms were devised to define abnormality and
these were evaluated using the Humphrey Visual Field Analyzer
(HFA) 30-2 and the Glaucoma Staging System as gold standard.
Receiver operating characteristic (ROC) curves were used to
determine the algorithm demonstrating the greatest agreement
between the DMCO version and the gold standard.
Results: Fifty-two glaucomatous, 36 normal and 9 borderline
glaucomatous patients participated. The algorithm demonstrating
greatest agreement with the gold standard combined results from
two successive DMCO Standard tests attaining sensitivity of 11.8%,
71.4%, 100% and 100% in eyes with mild, moderate, advanced and
severe loss, respectively. A specificity of 98.1% was achieved in eyes
without abnormal HFA results. Fifteen algorithms were created and
the area under the ROC curves (AUC) ranged from 0.79 to 0.90.
Median duration per eye to complete the DMCO Standard test was
86 seconds for participants in the control group and 125 seconds for
participants with glaucoma.
Conclusions: This study demonstrated that DMCO was able to find
glaucomatous visual field defects in this preselected population.
Future studies should evaluate DMCO in a non-selected population.
Commercial Relationships: Ane Sophie Olsen, None; Mark
Alberti, None; Morten D. De La Cour, None; Lisbeth Serup,
None; Bertil E. Damato, None; Miriam Kolko, None
Program Number: 1051 Poster Board Number: B0185
Presentation Time: 3:15 PM–5:00 PM
A Comparison of the Heidelberg Edge Perimeter and the Octopus
Visual Field Analyzer in Detecting Glaucomatous Visual Field
Defects
Christine Talamini, Priyanka Gogte, Michael Waisbourd, Jonathan
S. Myers, Lisa A. Hark, L Jay Katz. Wills Eye Hospital, Philadelphia,
PA.
Purpose: To compare the Heidelberg Edge Perimeter (HEP) and
the Octopus Visual Field (OVF) Analyzer in the detection of visual
field defects in patients with glaucoma. Preliminary studies suggest
that the HEP may detect glaucomatous changes earlier than current
standard perimetric testing.
Methods: Visual fields were obtained on 45 eyes (30 patients) with
glaucoma using the G top strategy on the OVF Analyzer (Haag-Streit,
Koeniz, Switzerland) and the Standard Automated Perimetry strategy
with the advanced staircase thresholding algorithm on the HEP
(Heidelberg Engineering, Heidelberg, Germany). All patients were
greater than 18 years of age, had a best-corrected visual acuity of
20/40 or better, refraction within ± 5.0 diopters spherical correction
and ± 3.0 diopters cylindrical correction. Patients were identified
as having characteristic glaucomatous disc damage and visual field
defects, which were verified by a glaucoma specialist. All patients
had reliable visual fields (indices <33%). The absolute values of the
HEP and OVF mean deviation (MD) and pattern standard deviation
(PSD) were compared.
Results: Forty-five eyes of 30 patients were included. The mean age
was 72.3 ± 10.2 years, 14 were male and 16 were female. The mean
MD and PSD values from OVF were 10.36 ± 6.35 and 4.75± 2.30,
respectively. The mean MD and PSD values from HEP were 7.57 ±
6.71 and 5.33 ± 3.21, respectively. Pearson correlation coefficients
showed high correlations for both the MD and PSD values: MD HEP
vs. OVF: r=0.86, r2=0.76, P<0.0001, PSD HEP vs. OVF: r=0.83,
r2=0.60, P<0.0001.
Conclusions: Global index values between the HEP and OVF are
closely correlated. This suggests that the HEP provides similar
detection of glaucomatous changes in patients with glaucoma.
Studies comparing the spatial defects detected on HEP and OVF
are underway. 1. Mulak et al. Adv Clin Exp Med. 2012 SepOct;21(5):665-70. 2. King et al. Graefe’s Arch Clin Exp Ophthalmol.
2002, 240:481-487.
Commercial Relationships: Christine Talamini, None; Priyanka
Gogte, None; Michael Waisbourd, None; Jonathan S. Myers, Haag
Streit (R); Lisa A. Hark, None; L Jay Katz, None
Support: Wills Eye Hospital Innovation Grant WEF#15064,
Heidelberg Edge Perimeter supported by grant from Heidelberg
Engineering
Program Number: 1052 Poster Board Number: B0186
Presentation Time: 3:15 PM–5:00 PM
The Pattern of Glaucomatous Visual Field Deterioration Over the
Entire Perimetric Range
Andrew Chen1, Francisco Otarola1, 2, Esteban Morales1, Abdelmonem
A. Afifi3, Joseph Caprioli1. 1Jules Stein Eye Institute, University of
California, Los Angeles, Los Angeles, CA; 2Fundacion Oftalmologica
los Andes, Universidad de los Andes, Santiago, Chile; 3Department
of Biostatistics, University of California, Los Angeles, Los Angeles,
CA.
Purpose: Evaluation of a nonlinear logistic function as a model to
represent the process of glaucomatous damage over the entire visual
field (VF) range compared to linear and exponential functions.
Methods: Reliable patient VF data, defined as <30% fixation
loss, <30% false positive, and <30% false negative rates, from the
Advanced Glaucoma Intervention Study (AGIS) and the Stein Eye
Institute’s glaucoma division were used. All test were performed with
a Humphrey Field Analyzer with a 24-2 test pattern, size III white
stimulus and full threshold strategy or Swedish Interactive Threshold
Algorithm (SITA) Standard and SITA Fast. The following functions
were used to assess the pattern of threshold sensitivity deterioration at
each VF location:
Linear: y = a + bx; Exponential: ln(y) = a + bx; Logistic: y = g / (1 +
exp( a + bx). VF locations of interest include those with an average
of the initial two sensitivities greater than 30 dB, 26 dB, and 22 dB
and with an average of the final two sensitivities less than 10 dB.
Root mean squared error (RMSE) values were used to evaluate the
goodness-of-fit for each regression model. The error was defined as a
difference between the sensitivities predicted by the function and the
observed sensitivities.
Results: 798 eyes from 583 patients were included. Average
(±SD) follow-up time was 8.7 (± 2.2) years, and each eye had an
average of 15.2 (±4.9) VF tests. For the VF locations with an initial
sensitivity greater than 22 dB and final sensitivity less than 10 dB
(938 locations), the logistic function had the lowest RMSE in 73.1%
of the locations, the exponential function in 18.2%, and the linear
function in 8.7%. This pattern held true for the subset of points with
an average initial sensitivity greater than 26 dB and greater than 30
dB with a final sensitivity less than 10 dB.
Conclusions: A pointwise logistic regression had the best ability to
fit perimetric progression in a subset of locations that traverse the
entire range of perimetric measurements from normal to perimetric
blindness compared to linear and exponential functions. Our results
show that perimetric measurements of glaucomatous visual field
loss from early to advanced stages of glaucoma follows a pattern
best represented by a logistic function. As such, the behavior of
glaucomatous VF loss is nonlinear, and the rate of deterioration
changes with the course of the disease.
Commercial Relationships: Andrew Chen, None; Francisco
Otarola, None; Esteban Morales, None; Abdelmonem A. Afifi,
None; Joseph Caprioli, None
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Program Number: 1053 Poster Board Number: B0187
Presentation Time: 3:15 PM–5:00 PM
Factors associated with paracentral visual field involvement in
glaucomatous eyes with optic disc hemorrhages
Verena Juncal1, Flávio Lopes1, Paula Alhadeff2, Robert Ritch2, Tiago
S. Prata1. 1Ophthalmology and Visual Sciences Department, Federal
University of São Paulo, Sao Paulo, Brazil; 2New York Eye and Ear
Infirmary, New York, NY.
Purpose: To assess factors associated with paracentral visual field
(VF) involvement in glaucomatous eyes with disc hemorrhages (DH).
Methods: In this observational study, we enrolled glaucomatous
patients with DHs from two Glaucoma Services. Disc photographs
of all patients were evaluated for the presence of DH by 2 glaucoma
specialists. On the basis of 2 reliable, consistent 24-2 Swedish
interactive threshold algorithm standard VFs, patients were divided
into two groups: those with parafoveal scotoma (PFS group: ≥3
adjacent points with P<5% within the central 10 degrees of fixation,
≥1 point with P<1% lying at the innermost paracentral points, in the
same hemifield) and those without PFS (controls). Clinical and ocular
data from the time of DH detection were collected and compared
between groups.
Results: A total of 130 patients were included (PFS group = 77
patients [mean age, 68.2 years]; controls = 53 patients [mean age,
65.1 years]; p=0.12). The PFS group had a higher prevalence of
caucasian patients than controls (82% vs 50%; p<0.01). Eyes with
PFS had a more negative spherical equivalent and a worse mean
deviation index (p≤0.01). Although eyes with PFS had lower IOP
values than controls at the time of DH detection (median, 15 mmHg
vs 18 mmHg), this difference did not reach statistical significance
(p=0.10). No significant differences were found regarding gender,
systemic risk factors (hypotension and migraine), central cornea
thickness, type of glaucoma, frequency of previous intraocular
surgery, optic disc phenotypes, presence of peripapillary atrophy,
localized retinal nerve fiber layer defects, DHs location and DHs
recurrences (p≥0.25). Logistic regression analysis revealed PFS to be
significantly associated with Caucasian race (OR, 2.2), myopia (<3D; OR, 3.4) and lower IOP (<16 mmHg; OR, 2.1;p≤0.04). Including
all significant factors in a multivariable analysis (controlling for VF
mean deviation index), only myopia (as a continuous or categorical
variable) remained significant in this model (p=0.03).
Conclusions: In this large series, the presence and extent of myopia
were found to be significantly associated with paracentral VF
involvement in glaucomatous eyes with DH. Our results may help
clinicians in the identification and surveillance of these eyes at higher
risk of central field loss.
Commercial Relationships: Verena Juncal, None; Flávio Lopes,
None; Paula Alhadeff, None; Robert Ritch, None; Tiago S. Prata,
None
Program Number: 1054 Poster Board Number: B0188
Presentation Time: 3:15 PM–5:00 PM
Rate of visual field progression in normal tension glaucoma
patients
Yeon Ggoch Park, Ji Won Kim, Kyu-Ryong Choi. Ewha Womans
University, Mokdong Hospital, Seoul, Korea (the Republic of).
Purpose: To investigate the rate of visual field progression in patients
with normal tension glaucoma (NTG) and analysis the clinical
characteristics between progressing and non-progressing group.
Methods: Records with five or more visual field tests of 265 eyes
(265 patients) which had been diagnosed with NTG at Ewha Womans
University, Mokdong hospital was reviewed. Patients were classified
into progressing and non-progressing groups by visual field trend
analysis. Kaplan - Meier survival curves was used to estimate five
year progression rate.
Results: Among 256 eyes with medically treated NTG, 59 eyes
(22.3%) were classified into the progressing group. The mean
baseline IOP was higher in the progressing group (p=0.027) and
mean baseline MD were different between progressing and nonprogressing group (-3.91±2.95dB vs -2.67±2.81dB, p=0.042). The
5 years progressing rate of medically treated NTG was 16% and 5
years progressing rate of under age 40 was 12% and over age 40 was
16%. And 5 years progressing rate of mono-therapy group was 15%
and double-therapy group was 21%.
Conclusions: After 5 years, 16% of medically treated NTG showed
a confirmed localized VF progression. Special attention and proper
treatment should be given to patients with high baseline IOP or worse
baseline MD in visual field test.
Commercial Relationships: Yeon Ggoch Park, None; Ji Won Kim,
None; Kyu-Ryong Choi, None
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Program Number: 1055 Poster Board Number: B0189
Presentation Time: 3:15 PM–5:00 PM
Long-term clinical course of normotentive preperimetric
glaucoma
Yusuke Manabe, Hiroko Inuzuka, Akira Sawada, Tetsuya Yamamoto.
Ophthalmology, Gifu University Graduate School of Medicine, Gifu,
Japan.
Purpose: To evaluate the long-term clinical course of normotensive
preperimetric glaucoma (PPG).
Methods: We retrospectively investigated 65 eyes of 65 patients
diagnosed initially as preperimetric normal tension glaucoma (NTG)
between 1985 and 2006, and followed for at least 5 years with having
reliable visual field examinations by standard automated perimetry
(program central 30-2) more than 10 times. We reviewed the patients’
data including best corrected visual acuity and visual field from our
records. At their latest consecutive two visual field examinations
the patients without glaucomatous visual field defect, which was
judged by the Anderson’s criteria, were excluded. A normal visual
field was judged at three initial baseline examinations. When the
visual field defect met the Anderson’s criteria at least two consecutive
examinations and the results at following examinations are quite
consistent, the eye was classified as developing a glaucomatous
visual field defect.
Results: The mean age at diagnosis was 52.4 ± 11.4 years with a
range of 16 to 73 years. Men were 25 and women were 40. The mean
follow-up period was 16.1 ± 5.6 years with a range of 7 to 26 years.
Seven eyes had no ocular hypotensive drugs at their final visits and
2 eyes patients had received glaucoma surgery during the follow-up
period. The mean period to development of glaucomatous visual
field loss from their diagnosis was 6.8 ± 4.1 years with a range of
0.6 to 16.0 years. The mean deviation slope (MD slope) was -0.22
± 0.27 dB/year with a range of -0.93 to 0.25 dB/year. There was a
statistically significant visual filed defect deterioration in 38 eyes
(58.5%).
Conclusions: Approximately half of initially preperimetric NTG
showed significant visual filed loss progression during a mean followup of 16 years. However, the rates of visual field loss progression
varied considerably among individuals.
Commercial Relationships: Yusuke Manabe, None; Hiroko
Inuzuka, None; Akira Sawada, None; Tetsuya Yamamoto, None
Program Number: 1056 Poster Board Number: B0190
Presentation Time: 3:15 PM–5:00 PM
Variability of peripheral test points, central test points and visual
field indices in the Medmont M700 perimeter
John G. Pearce. John Curtin School of Medical Research, Australian
National University, Canberra, ACT, Australia.
Purpose: The Medmont M700 automated perimeter is widely used
in many countries, but literature regarding its repeatability, and
comparisons with the Humphrey Field Analyser (HFA), are scarce.
We therefore intend to create some clinically applicable confidence
intervals for the M700 Overall and Pattern Defect indices, and
compare these with similar HFA descriptors. We will also examine
the variance of points of equal decibel values in the central and
peripheral fields of the same M700 visual field tests.
Methods: Twenty four glaucoma patients with varying degrees of
glaucomatous field loss were enrolled in the study, and twenty one
patients (forty eyes) had usable results for the study. A Central 30°
and a Macula (10°) test using the M700 (version 3.9.7) fast threshold
strategy was performed on each eye on the same day. To determine
retest variability, the tests were repeated one week later at the same
time of day, which minimised the possibility of circadian variations
affecting the results.
Results: For sensitivities of 0 – 5 dB and 25 - 35 dB, points in the
outer 20° of the Central 30° test showed similar retest variance to
points of equal decibel value in the central 10° of the same test. For
sensitivities of 5 – 25 dB, points in the outer 20° of the Central 30°
test showed slightly lower variance than points of equal decibel value
in the central 10° of the same test. The M700 OD index appears to be
quite different to the Mean Deviation (MD) index in the HFA when
grading glaucoma severity, and significantly different to the Average
Defect index in earlier Medmont programs. For Overall Defect (OD),
the 95% confidence interval (CI95) was ± 2.1 dB. The CI95 for Pattern
Defect (PD) varied with glaucoma severity: for PD < 2.8, CI95 = (±
1.25 dB), for PD 2.81 to ≤ 5.7 CI95 = (± 1.14 dB) and for PD > 5.7
CI95 = (± 3.1 dB).
Conclusions: In glaucoma patients, for points of equal decibel
values, variance does not seem to increase with increasing
eccentricity with the M700 stimulus layout. OD values obtained
with the M700 did not appear to correlate well with the amount of
visual field loss, and should not be directly compared to MD values
obtained with the HFA. As a result, the M700 OD value should not
be used to stage glaucomatous field loss in the same way as the MD
figure is used with the HFA. PD values in the M700 appeared to
correlate well with the degree of glaucomatous field loss.
Commercial Relationships: John G. Pearce, None
Support: I receive payments from the Nursing and Allied Health
Scholarship Support Scheme run by the Australian Federal
Government towards my study costs.
Program Number: 1057 Poster Board Number: B0191
Presentation Time: 3:15 PM–5:00 PM
Static Perimetry in the Visual Field Far Periphery in Optic Nerve
Disease
Johnathan S. Fagg, Trina Eden, Kimberly Woodward, Chris A.
Johnson, Michael Wall. Ophthalmology, University of Iowa-Carver
College of Medicine, Iowa City, IA.
Purpose: To determine if visual field testing in the far periphery
is feasible and is a sensitive perimetric test to detect visual loss
compared with the 24-2 SITA Standard test in patients with glaucoma
and idiopathic intracranial hypertension (IIH).
Methods: We tested one eye of 29 subjects, 12 with glaucoma and
17 with idiopathic intracranial hypertension (mean deviation < -4
dB) with SITA Standard size III for the central visual field and from
30° to 60° with full threshold 60-4 using Goldmann stimulus sizes
V and VI for the peripheral field. Superior and nasal edge 60-4 test
locations were not used due to high retest variability giving 52, 24-2
test locations and 49 locations for the 60-4 test. Pointwise probability
plots for all three tests were generated based on 60 normals tested
twice. The number of abnormal test locations for the tests were
weighted based on significance level using the method of Asman et
al. 1992, summed and compared using ANOVA.
Results: We found 25.4% more abnormal test locations with size V
in the far periphery compared to size III ( p =< 0.001). There were
similar numbers of abnormal test locations in similar spatial locations
with size III and size VI testing. There were five cases (3 glaucoma
and 2 IIH) with normal central visual field testing and abnormalities
of the far periphery.
Conclusions: Threshold static automated perimetry shows visual
field defects in the peripheral field when central visual field testing is
normal. Static threshold perimetry of the far periphery shows promise
for detecting visual loss in glaucoma and idiopathic intracranial
hypertension.
Commercial Relationships: Johnathan S. Fagg, None; Trina
Eden, None; Kimberly Woodward, None; Chris A. Johnson, None;
Michael Wall, None
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Support: VA Merit Review
Program Number: 1058 Poster Board Number: B0192
Presentation Time: 3:15 PM–5:00 PM
Sensitivity and Variability of Peripheral Visual Field (PVF)
Testing
Tamara L. Berezina, Christopher Kuriakose, Albert S. Khouri, Robert
D. Fechtner. Institute of Ophthalmology and Visual Science, Rutgers
- New Jersey Medical School, Newark, NJ.
Purpose: Humphrey Field Analyzer (HFA) program 60-4 with
stimulus size III has been used for monitoring peripheral visual field
defects due to certain drug toxicities. Large threshold intersubject
variability has been reported for PVF testing using this program.
We tested the hypothesis that the smaller intersubject variability and
higher threshold values may be achieved with stimulus size V for this
program.
Methods: Peripheral visual field testing using HFA 60-4 program
with stimulus III (n=33) and stimulus V (n=33) was performed
in healthy volunteers (based on a normal visual acuity, slit lamp
and fundus exam on comprehensive ophthalmic evaluation). Only
reliable PVF tests were included (fixation loss, false positive and
negative <30%). Each of the 60 measured threshold visual sensitivity
(TVS) (decibels) locations was labeled with a NTSI (nasal/temporal/
superior/inferior) coordinate system. Points were organized into
inner, middle, and outer eccentricity rings and zones. Number of
location points with low, middle, and high variability of the threshold
sensitivities were calculated for both stimulus sizes. We defined
variability as low for those test locations where the value of SD does
not exceed 15% of its mean TVS value, middle if SD is in the range:
>15% ≤ 40% of the mean, and high if SD is more than 40% of the
mean value. Student’s t-test was used to compare individual and
mean threshold visual sensitivity with stimulus size III and V. Chisquare test was used to compare proportions.
Results: Threshold visual sensitivities for individual location points
as well as mean threshold sensitivities for inferior, superior, nasal,
and temporal zones were higher with stimulus size V (p<0.01). The
number of location points with high and middle variability of TVS
was greater using stimulus size III vs. stimulus size V (p= 0.0296).
More test locations with stimulus size V had low variability (Figure).
Conclusions: Since TVS is higher with stimulus V and variability
is lower we believe PVF testing with stimulus V is a more efficient
strategy when looking for peripheral change over time.
Program Number: 1059 Poster Board Number: B0193
Presentation Time: 3:15 PM–5:00 PM
Upper Limits of the Best Sphere Correction for Astigmatism in
Threshold Visual Fields
Thomas Callan1, Patricia Sha1, Jennifer Luu1, John G. Flanagan2.
1
Clinical Affairs, Carl Zeiss Meditec Inc, Dublin, CA; 2University of
California, Berkeley, CA.
Purpose: To investigate the amount of spherical equivalent power
that can be used in lieu of an astigmatic trial lens up to a decrease
in mean deviation (MD) of 1 decibel (dB). The Humphrey Field
Analyzer (HFA) advocates correction of astigmatism at 1.25 diopters
of cylinder (DC).
Methods: Six normal subjects with previous perimetry experience
and known spherical refractive errors were tested with the HFA 24-2
SITA Standard program. Two baseline visual fields were performed
with the spherical refraction corrected for each subject. Additional
visual fields were performed with myopic astigmatic refractive errors
of 1.50, 2.00, 2.50, 3.00 and 3.50 DC induced using trial lenses. For
these tests, the spherical equivalents of the refractive errors were
corrected with the appropriate power spherical lens.
Results: The difference from the Baseline MD (average of the
first two tests) was calculated for each visual field. The results of
the different amounts of astigmatic blur corrected by utilizing the
spherical equivalent and the effect on the MD are shown in Table
1. It was not until the astigmatic refractive error reached 3.50 D
astigmatism did the mean deviation decrease by more than 1 dB.
Conclusions: Spherical equivalent lens correction of astigmatism
is effective for refractive errors greater than the manufacturer’s
recommendation of correction at 1.25 DC. In this study, astigmatic
refractive errors up to 2 DC were corrected with the spherical
equivalent before the mean deviation changed more than 0.5 dB, and
3DC for 1 dB.
Table 1: Mean Deviation Difference for Each Astigmatism Amount
(n=6)
Commercial Relationships: Thomas Callan, Carl Zeiss Meditec,
Inc. (E); Patricia Sha, Carl Zeiss Meditec, Inc. (E); Jennifer Luu,
Carl Zeiss Meditec, Inc. (E); John G. Flanagan, Carl Zeiss Meditec,
Inc. (F)
Commercial Relationships: Tamara L. Berezina, None;
Christopher Kuriakose, None; Albert S. Khouri, None; Robert D.
Fechtner, Carl Zeiss Meditec, Inc. (C)
Support: The Glaucoma Research and Education Foundation, Inc.,
New Jersey, An unrestricted gift from Joseph and Marguerite DiSepio
Charitable Foundation, Monroe Township, NJ.
Program Number: 1060 Poster Board Number: B0194
Presentation Time: 3:15 PM–5:00 PM
Long-Term Evaluation of Visual Field Enhancement in
Glaucomatous Eyes Following Surgical Intraocular Pressure
Reduction
Iman Goharian1, Justin Shaw1, Stuart K. Gardiner2, Tracy M. Wright1,
David S. Greenfield1. 1Bascom Palmer Eye Institute, University of
Miami Miller School of Medicine, Palm Beach Gardens, FL; 2Devers
Eye Institute, Legacy Health, Portland, OR.
Purpose: Short-term enhancement of visual field (VF) sensitivity
after surgical reduction of intraocular pressure (IOP) in glaucomatous
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
eyes has been reported. The purpose of the present study was to
examine the hypothesis that long-term VF enhancement occurs in
glaucomatous eyes undergoing IOP-lowering surgery.
Methods: Patients with uncontrolled IOP requiring trabeculectomy
or aqueous drainage device implantation were enrolled. Controls
consisted of medically treated glaucoma patients with stable IOP.
Two baseline preoperative VFs and 3 follow-up VF exams at 12,
24, and 36 months postoperatively were used for analysis. The same
number of VF examinations was used for control eyes. VF locations
with significant change were defined as exceeding 95% test-retest
confidence limits based upon the mean sensitivity using the 2
baseline VF exams. The number of significantly changing locations
per eye from the mean baseline fields were compared between groups
using a Poisson generalized estimating equation model.
Results: Twenty eyes (baseline MD -7.0±5.0 dB) of 20 surgically
treated glaucoma patients (mean age 69.2±10.1 years) and 41 eyes
(baseline MD -5.6±4.2 dB) of 28 controls (mean age 67.4±7.3 years)
were enrolled. Mean postoperative IOP (10.83±6.45 mmHg) was
significantly (p=0.03) decreased at 3 years of follow-up compared
with baseline (17.1±6.32 mmHg) in the surgical eyes, but was similar
(p=0.72) in control eyes (13.4±6.46 and 13.7±3.14 mmHg). At 3
years of follow-up, the mean number of test locations with improving
VF sensitivity was similar between the surgical and control group in
central (0.45±0.89 vs. 0.77±1.13, p=0.273), peripheral (2.10±2.88
vs. 1.92±3.37, p=0.829) and all VF test locations (2.55±3.43 vs.
2.69±4.09, p=0.886). The mean number of test locations with
decreasing VF sensitivity was similar between the surgical and
control group in central (1.35±2.01 vs. 1.18±1.90, p=0.743),
peripheral (3.10±3.88 vs. 3.33±3.88, p=0.825) and all test locations
(4.45±5.58 vs. 4.51±5.41, p=0.966).
Conclusions: VF loss and improvement were comparable through
3 years of post-operative follow-up. This suggests that ongoing
glaucomatous damage may erode early postoperative enhancement of
VF sensitivity after IOP-lowering surgery.
Commercial Relationships: Iman Goharian, None; Justin Shaw,
None; Stuart K. Gardiner, None; Tracy M. Wright, None; David
S. Greenfield, None
Support: University of Miami Core Grant (P30-EY014801); an
unrestricted grant from Research to Prevent Blindness; Department of
Defense Grant (W81XWH-09-1-0675)
HVF. The number of eyes with postoperative VF progression was
assessed, and risk factors for VF progression were evaluated.
Results: Of 108 eyes (90 patients) included in the study, 10 (9.3%)
progressed by VFI criteria. By TD and PSD criteria, 18 (16.7%) and
20 (18.5%) showed VF progression. Preoperative mean deviation
was -7.92 ± 3.71 for eyes that progressed by PSD criteria and -4.23 ±
4.71 for eyes that did not progress (p<0.001). Average postoperative
mean deviation was -8.66 ± 3.77 for eyes that progressed and
-3.59 ± 5.27 for eyes that did not progress (p<0.001). Eyes that
progressed had more myopic preoperative refraction (-3.75 ± 3.31
vs. -1.67 ± 3.64, p=0.019) and were treated with a greater number of
glaucoma medications postoperatively (2.40 ± 1.05 vs. 1.83 ± 1.05,
p= 0.036). Axial length was similar between the two groups (24.87
± 1.3 vs. 24.62± 1.58, p=0.46). Preoperative and postoperative IOP
measurements did not significantly differ between the two groups.
Of the eyes that progressed, 6/20 (30%) had a ≥50% IOP increase
postoperatively (IOP spike) compared to 11/88 (12.5%) (p=0.083) in
the group that did not progress.
Conclusions: A significant proportion of glaucoma patients have
postoperative visual field progression after phacoemulsification.
Postoperatively, there was a trend towards a greater proportion of
IOP spike in patients that had visual field progression. Our data
demonstrate that patients with more severe disease preoperatively or
myopic refraction were more likely to have visual field progression
after phacoemulsification.
Commercial Relationships: Divakar Gupta, None; Karine D.
Bojikian, None; Slabaugh Mark, None; Philip P. Chen, None
Support: Research to Prevent Blindness
Program Number: 1061 Poster Board Number: B0195
Presentation Time: 3:15 PM–5:00 PM
Visual Field (VF) Progression after Cataract Surgery in
glaucoma patients with and without postoperative intraocular
pressure (IOP) spike
Divakar Gupta1, Karine D. Bojikian1, Slabaugh Mark2, Philip P.
Chen1. 1Ophthalmology, University of Washington, Seattle, WA;
2
Department of Ophthalmology and Visual Science, The Ohio State
University, Columbus, OH.
Purpose: To evaluate the risk factors and frequency of short-term
VF progression after phacoemulsification in patients with glaucoma,
specifically evaluating the effect of postoperative IOP spike.
Methods: Charts of glaucoma patients having phacoemulsification
by the same surgeon between January 1999 and May 2013 were
reveiewed. Patients included in this study were considered to have
stable glaucoma and had at least one Humphrey VF in the 18 months
prior to surgery and two VFs during the 2 years after surgery. Visual
field progression was defined as a 1) decrease in visual field index
(VFI) by three percentage points or 2) at least three points that
decreased by 5dB, with at least one point that decreased by 10dB on
total deviation (TD) plot or pattern standard deviation (PSD) plot on
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.