Interleukin 6 Reduces Lipoprotein Lipase Activity
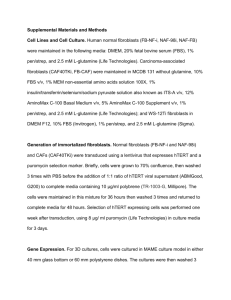
advertisement

(CANCER RESEARCH 52, 4113-4116. August 1. 1992| Interleukin 6 Reduces Lipoprotein Lipase Activity in Adipose Tissue of Mice in Vivo and in 3T3-L1 Adipocytes: A Possible Role for Interleukin 6 in Cancer Cachexia Andrew S. Greenberg,1 Richard P. Nurdan, Joseph Mclntosh, Juan Carlos Calvo, Robert O. Scow, and David Jablons2 Laboratory of Cellular and Developmental Biology, National Institute of Diabetes, Digestive and Kidney Disease ¡A.S. G., R. O. S.J; Laboratory of Genetics [R. P. N.I and Surgery Branch fJ. M., D. J.J, National Cancer Institute; and Laboratory of Theoretical and Physical Biology, National Institute of Child Health and Development [J. C. C.J, NIH, Bethesda, Maryland 20892 ABSTRACT To investigate whether interleukin 6 (11-6) might be a potential me diator of the depleted fat reserves observed in malignancy-associated cachexia, we measured lipoprotein lipase (LPL) activity in adipose tis sue of mice after administration of IL-6 or tumor necrosis factor and in cultured adipocytes after addition of these cytokines. Injection of IL-6 i.p. reduced adipose tissue LPL activity by 53% within 4.5 to 5.5 h. Injection of tumor necrosis factor elevated serum IL-6 levels and re duced adipose tissue LPL activity by 70%. Both human and murine IL-6 reduced heparin-releasable LPL activity in 3T3-L1 adipocytes in a dosedependent manner; half-maximal inhibition of LPL activity was achieved with 5000 hybridoma growth factor units/ml. Thus, IL-6 re duces stores crosis diated adipose LPL activity and may contribute to the loss of body fat associated with some cases of cancer cachexia. Since tumor ne factor increases circulating IL-6, some of its effects may be me or potentiated by IL-6. INTRODUCTION Animals and humans with chronic infections or cancer may develop the syndrome of cachexia which is characterized by severe wasting of both protein and fat stores. The syndrome is often associated with elevated serum triglycérides(1-3) and reduced serum LPL3 activity (4-6). LPL, produced in adipo cytes and found at the endothelial cell surface, hydrolyzes cir culating triglycéridesto fatty acids, which serve as the major source of acyl groups used in fat storage in the adipocyte (7). Cerami et al. (8, 9) discovered a factor produced by endotoxinstimulated macrophages that suppresses adipocyte LPL activ ity. This factor, termed cachetin for its presumptive role in lowering LPL activity and promoting the cachetic syndrome, was later found to be identical to TNF (10). When injected into animals, cachetin/TNF lowers adipose tissue LPL activity (11). We recently reported that administration of recombinant TNF to humans and mice induces the appearance of circulating IL-6 (12, 13). IL-6 is a cytokine that appears to act as an important systemic regulatory hormone in response to infection and trauma (14); increased serum concentrations of IL-6 have been measured in patients with sepsis (15), acquired immuno deficiency syndrome (16), and plasma cell leukemia (17). In creased concentrations of circulating IL-6 are detectable in an imals bearing tumors of multiple different histologies (13, 18, 19), and serum IL-6 levels increase in direct proportion to the amount of tumor burden (13, 19). Since TNF increases serum IL-6 levels and since IL-6 activity is elevated in the presence of malignancy and infections, we investigated whether IL-6 might be a mediator of the depleted fat stores of the cachetic state. In this paper, we demonstrate that IL-6 significantly lowers adipose tissue LPL activity in vivo and directly inhibits LPL activity in cultured adipocytes. MATERIALS AND METHODS Cytokines. rHIL-6, a kind gift of Drs. Gordon Wong and Robert Donahue of Genetics Institute (Cambridge, MA), had less than 5 endotoxin units/mg protein and an activity of 4-6 x IO6 TI 165 plasmacytoma units/mg. rHIL-6 was dissolved in HBSS containing 2% human albumin, and the activity was assayed with the B9 hybridoma assay (see below). rHTNF, a kind gift of the Cetus Corp. (Emeryville, CA), had an activity of 2 x IO7 units/mg in the L929 assay (see below) and an endotoxin content of <0.1 ng/mg protein. TNF was dissolved in HBSS with 2% human serum albumin, and activity was confirmed using the L929 assay (20). Native murine IL-6 was purified by a modification of the procedure of Nordan et al. (21). Briefly, serum-free supernatant from the P388D1 murine macrophage cell line was applied to an affinity column contain ing the rat anti-murine IL-6 monoclonal antibody, D6906B4 (22), cou pled to Sepharose 4B. After extensive washing with phosphate-buffered saline, the murine IL-6 was eluted with 0.2 M glycine-HCI/0.02% Tween 20, pH 2.O. The affinity-purified murine 1L-6 was applied to a C-4 reverse phase HPLC column (214TP54, Vydac) and eluted with a gradient of 40% to 50% acetonitrile/0.1% trifluoroacetic acid over 20 minutes. IL-6, which eluted as a single peak, was lyophilized and resuspended in phosphate-buffered saline/0.02% Tween 20 and stored at 4°C.Activity was determined with the B9 assay. B9 Bioassay of IL-6 Activity. Recombinant, purified murine, and serum IL-6 activities was assayed by a [3H]dThd uptake assay using the IL-6-dependent murine hybridoma subclone B9 as described previously (22, 23). Culture medium consisted of RPMI 1640 supplemented with 10% fetal calf serum, 5 x 10~5 M 2-mercaptoethanol, and 50 jig/ml gentamicin. B9 cells were maintained in culture medium supplemented with IL-6 at 100 HGF units/ml. For the assay, 2000 washed B9 cells were cultured with 2-fold serial dilutions of the test sample in a final volume of 200 u\ of culture medium. After an 84-h incubation at 37'C in a humidifed atmosphere of 5% CO2-95% air, the cultures were pulsed for 4 h with 0.5 ¿iCi[3H]dThd (6.7 Ci/mmol) and harvested over glass fiber filters. The incorporation of [3H]dThd into DNA was determined Received 1/14/92; accepted 5/12/92. in a liquid scintillation counter. Preparations of known activity of The costs of publication of this article were defrayed in part by the payment of rHIL-6 were diluted in heat-inactivated bovine calf serum and tested page charges. This article must therefore be hereby marked advertisement in accord ance with 18 U.S.C. Section 1734 solely to indicate this fact. concurrently as standards. One hybridoma growth factor unit of IL-6 is 1To whom requests for reprints should be addressed, at LCDB. NIH. Building defined as that amount which gives half-maximal stimulation of thy 6, Rm. BI-13, Bethesda. MD 20892. 2 Work done in partial fulfillment of Ph.D. requirements, Dept. of Genetics, midine incorporation into B9 cells. The specificity of the assay was George Washington University, Washington, DC. verified by inhibition with a neutralizing rabbit anti-murine IL-6 anti3 The abbreviations used are: LPL, lipoprotein lipase: IL-6. interleukin 6; TNF, serum (24). tumor necrosis factor; HBSS, 4-(2-hydroxyethyl)-l-piperazineethanesulfonic acidAnimal Methods. Female C57BL/6 mice, 12 weeks of age, were buffered saline solution: rl I, recombinant human: diluì,thymidine uptake; HGF, hybridoma growth factor. obtained from The Jackson Laboratory, Bar Harbor, ME, or from the 4113 INTERI.El KIN 6 REDITES Small Animal Section, National Cancer Institute, Bethesda, MD. The animals were fed aülibitum. rHTNF and rHIL6 were prepared in HBSS and injected ¡.p.in groups of six animals for each experiment. Animals received an injec tion of either 1 ml of HBSS alone (vehicle), or 1 ml of HBSS containing 100 ¿<g of rHIL-6, or 1 ml of HBSS containing 10 ng of rHTNF. Tailbleeds were performed 4 h after i.p. injection to determine serum cytokine activity. Blood was collected in serum separator tubes (SST, Becton Dickinson), and the sera were assayed immediately for IL-6, TNF, or both, or frozen at -70°C prior to analysis. To measure in vivo adipose tissue LPL activity, animals were sacri ficed by cervical dislocation 4.5 to 5.5 h after injection, and the entire periovarian and periuterine fat pads were removed. Adipose Tissue Lipoprotein Lipase Activity. Lipolytic activity in the fat pads was determined by a modification of the methods of Peterson et al. (25) and Langer et al. (26). The adipose tissue was weighed and homogenized with a Polytron tissue grinder in 9 volumes (w/v) of homogenization solution consisting of ice-cold 0.025 M ammonium chloride buffer (pH 8.2) containing 5 lU/ml heparin, 10 Mg/rnl leupeptin, 1 jig/ml pepstatin, 25 KIE/ml Trasylol, 0.125% Triton X-IOO. 0.04% (w/v) sodium dodecyl sulfate, and 5 mM EDTA. The homogenates were centrifuged at 27.000 x g for 20 min at 4"C. The fat cake was gently pierced, and 10 ¿il of infranatant were removed and mixed with 10 ill of homogenization solution without Triton and sodium dodecyl sulfate and assayed for LPL activity in duplicate. A stock lipid emulsion containing 0.005 mmol of tri[9.10-'H|triolein (l.OCi/mmol). 1.13 mmol of trioleoylglycerol. 60 mg of i-«-phosphatidylcholine, and 9 ml of glycerol was prepared according to the method of Nilsson-Ehle and Schotz (27). Before assay an activated substrate mixture was prepared by mixing 1 volume of the stock emulsion with 5 volumes of heat-inactivated fasted rat serum (heated at 60°Cfor 10 min) and 19 volumes of an assay solution that resulted in a final con centration of 12% bovine serum albumin. 300 II) heparin/ml. 0.2 M NaCI, and 0.2 MTris-HCl (pH 8.1) (25); the mixture was incubated at 37°Cfor 15 to 30 min. For assay, 100 n\ of the activated substrate mixture, containing 2.0 ¿<Ci of tripHjoleolyglycerol/ml and 23 nmol of irioleoglycerol, were added to the adipose tissue extract, brought to a total volume of 200 Mlwith 0.9% NaCI, and incubated at 37°Cfor 30 min. Radiolabeled fatty acids produced by lipolysis were extracted and measured by the method of Vaughn and Belfrage (28). The LPL activity was linear for duration of the assay. Lipolytic activity measured in the assay was due to lipoprotein lipase since activity was inhibited by more than 80% by the inclusion of l MNaCI or omission of fasted rat serum. One milliunit of lipolytic activity represents release of 1 nmol of fatty acid/min. 3T3-L1 Cell Culture. 3T3-L1 mouse embryo fibroblasts were ob tained from American Type Culture Collection (Rockville, MD) and cultured as described previously (29. 30). Briefly, cells were seeded at a density of 2 to 4 x IO5 cells/60-mm dish (Costar) and cultured in 4 ml of Dulbecco's modified Eagle's medium-25 mMglucose) (GIBCO), sup COi-95% air. Fifty- and 100-Mlaliquots of the media were removed and immediately assayed for LPL activity. Heparin-releasable LPL activity in the culture medium was assayed as decribed above with the following exceptions. The preactivated stock mixture consisted of I volume of the stock emulsion, 19 volumes of 3% bovine serum albumin in 0.2 M Tris-HCl (pH 8.1), and 5 volumes of heat-inactivated fasted rat serum (heated at 60°Cfor 10 min); this mixture was incubated at 37°Cfor 15 to 30 min. For assay, 100 ^1of the activated substrate mixture were added to an aliquot of culture medium, brought to a total volume of 200 n\ with 0.9% NaCI, and incubated at 37°Cfor 60 min. Fatty acids were recovered and enzyme activity was defined as noted above. Statistics. Differences between groups were assessed using Student's unpaired t test. The calculations were performed using CL1NFO soft ware (BBN Software Products. Cambridge. MA). All data are given as means ±SE. RESULTS IL-6 Serum Levels. Previous studies demonstrated that i.p. administration of IL-6 results in a more persistent elevation of serum IL-6 concentration than i.v. administration (32). Since animals with tumors have chronically elevated levels of circu lating IL-6, the i.p. route of administration was used for the studies in this paper. Circulating IL-6 concentrations (Table 1) 4 h after administration of either 10 ng of rHTNF or 100 Mgof rHIL-6 were elevated to levels similar to those found in mice with large tumor burdens (13, 19). The injection of HBSS ve hicle in the control animals produced no detectable serum IL-6 activity. Representative sera from mice that received IL-6 were analyzed for TNF activity by the L929 cytolytic assay, and none was detected (data not shown). Thus, under our experimental conditions, TNF injection increased circulating IL-6. Adipose Tissue LPL Activity. Injection of rHIL-6 into mice reduced adipose tissue LPL activity by 53% (Table 2), while in mice treated with rHTNF, adipose tissue LPL activity was low ered by 70%. The entire periuterine and periovarian fat pads were carefully removed and used for the LPL assay. Since there was no obvious difference between the fat pad weights of the control and cytokine-treated groups, cytokine treatment did not appear to reduce the triglycéridecontent of the tissues during the brief time period examined here. Table 1 Effect of TNF or II.-6 on serum IL-6 activity in mice Mice were given i.p. injections in the morning of HBSS vehicle (control) or cytokines rHIL-6 and rHTNF, at 100 and 10 Mg.respectively. Tailbleeds were performed 4 h later and the serum IL-6 levels were determined using the B9/HGF assay. Values represent the mean ±SE of six animals. plemented with 10% fetal bovine serum (GIBCO or INOVAR) and 8.0 ng of pantothenic acid per ml, referred to as complete medium. Cultures were maintained at 37°Cin an atmosphere of 5% CO;-95% air, and the medium was changed every 2 days. Two days after reaching confluence, 3T3-L1 cells were stimulated to differentiate by the addition of 5 ^g/ml of insulin and 0.39 Mg/ml of dexamethasone (30. 31). The medium was removed after 48 h, and the cultures were incubated with 50 ng/ml of insulin for an additional 48 h. Thereafter, the cells were maintained in complete medium without any added hormones and used for assay when greater than 95% of cells contained fat droplets (usually after at least 10 days from the initial insulin and dexamethasone treatment). 3T3-L1 LPL Assay. Cells were assayed for heparin-releasablc LPL activity using the method of Nilsson-Ehle and Schotz (27) as modified by Kawakami et al. (1). The evening before an assay, cells received 4 ml of complete media. The next day, cytokines at the concentrations noted in Fig. 1 were added. After 8 h, the medium was removed and replaced with 2 ml of complete medium supplemented with 10 units of heparin/ ml. The cells were incubated for 60 min at 37°Cin an atmosphere of 5% LPL ACTIVITE Injection group Time (h) Scrum IL-6 activity (HGF units/ml) <20 452 ±113 54.1 ±204 Control IL-6 TNF Table 2 Effects of IL-6 and T\F in vivo on LPL activity in murine aJipóse tissue rHTNF (10 Mg) or rHIL-6 (100 Mg) in HBSS was administered i.p. in the morning to mice. From 4.5 to 5.5 h later, the entire periovarian and perimetric fat pads were removed, homogenized with a Polytron. and assayed for lipoprotein lipase activity. Values are means ±SE of two experiments with six animals/ experiment. 41 14 Group Control IL-6 TNF " P < 0.005 relative to control. h P < 0.001 relative to control; P n (milliunits/g wet wt) 12 12 12 492 ±64 2.10 ±26" I50± 15* < 0.05 relative to IL-6. INTERLEl'KIN 6 REDUCES 3T3-L1 Adipocyte LPL Activity. Previous studies have indi cated that the heparin-releasable fraction of LPL activity in 3T3-L1 adipocytes reflects whole cell LPL activity (8). Treat ment of the 3T3-L1 adipocytes with IL-6 reduced LPL activity in a dose-dependent manner (Fig. 1). Maximal reduction of heparin-releasable LPL activity was seen with 50,000 HGF units/ml of murine IL-6 (78% reduction), while 5000 HGF units/ml of murine IL-6 reduced LPL activity by 50% (Fig. 1). Recombinant human IL-6 gave similar results; 5000 HGF units reduced heparin-releasable LPL activity by 43% and 50,000 HGF units/ml of rHIL-6 by 70%. As previously reported (31), a maximally effective rHTNF concentration of 50 ng/ml low ered LPL activity by 96%. DISCUSSION Lipoprotein lipase plays an important role in adipocyte me tabolism by hydrolyzing circulating triglycéridesto fatty acids for subsequent storage as fat in the adipocyte. Thus, a reduction in the activity of LPL would contribute to a decrease in total body fat stores. Reduced lipoprotein lipase activity has been documented in patients and animals with the cachetic syn drome (4-6). An intensive search for mediators of cachexia has been conducted in a number of laboratories, with special em phasis on the role of TNF/cachetin (12). However, elevated TNF concentrations have generally not been found in cancer patients with cachexia (33, 34). In addition, animals with tu mors of different etiologies have circulating TNF concentra tions that were undetectable or minimal (13, 35), but serum IL-6 concentrations were elevated in parallel with tumor burden (13, 19). Similarly, other illnesses which can result in the cachectic syndrome, such as infectious disease, have been asso ciated with elevated serum concentrations of IL-6 (15, 16, 36). In this study, IL-6 was shown to reduce LPL activity in adipose tissue in vivo when injected i.p. in mice. Thus, this cytokine may be important in promoting the depletion of fat stores observed in the cachetic syndrome associated with dis ease states. Further support for this hypothesis stems from a LPL ACTIVITY recent study in which the introduction of a retroviral expression vector containing the IL-6 coding sequence into the bone mar row of mice resulted in high serum concentrations of IL-6 and mice with markedly decreased amounts of s.c. fat (37). The evidence presented in this paper indicates that the 3T3-L1 adipocyte is a direct target for IL-6 action. IL-6, like TNF, reduces LPL activity when added to the culture medium. Although TNF decreases the rate of LPL gene transcription (31, 38, 39), the mechanism of action for IL-6 is unknown. As with other actions attributed to IL-6 (14), both murine and recombinant human IL-6 were equipotent in their effects on the adipocyte, indicating no species specificity in the murine re sponse. Many cytokines, including TNF, interleukin 1, interleukin 2, and tt-interferon elevate serum IL-6 concentrations when in jected into animals (12). Moreover, many types of cells, includ ing fibroblasts, monocytes, and endothelial cells, elaborate IL-6, and the production of this cytokine increases in response to TNF as well as other cytokines (40). The 3T3-L1 preadipocyte cell line is a clonal population of cells derived from mouse fibroblasts (41), raising the possiblity that the TNF effects on differentiated adipocytes observed in this study might be medi ated by the increased production of IL-6. Alternatively, the presence of IL-6 might potentiate the direct actions of TNF on differentiated adipocytes. Whether alone or in conjunction with TNF, the data clearly suggest a role for IL-6 in the development of the cachectic syndrome. 100 -, ACKNOWLEDGMENTS The authors thank Drs. C. Londos and A. Kimmel as well as Dr. M. Lotze for many constructive conversations. Dr. S. Roberts for valuable advice during preparation of the manuscript as well as assistance with statistical analysis, and also Dr. S. Steinberg for assistance with the statistical analysis. Note Added in Proof Further support for the role of IL-6 in cancer cachexia is found in the recent paper by Strassman et al. (F.vidence for the involvement of interleukin 6 ¡n experimental cancer cachexia, J. Clin. Invest., K9: 1681-1684. 1992). who found that injection of anti-IL-6 antibody ¡ntumor-bearing mice significantly inhibited the appearance of various parameters of cachexia. 01 § t Q- c O o O. « REFERENCES 80 - 40 ^ LU LU CONTROL 500 5000 50,000 MURINE INTERLEUKIN-6 (HGF units/ml) 50 NG/ML TNF Fig. I. The effect of IL-6 and TNF on LPL activity in cultured adipocytes. 3T3-L1 adipocytes were treated with the indicated concentrations of TNF and IL-6. The cells were analyzed for heparin-releasable LPL activity 8 h after the addition of cytokine. Data arc presented as a percentage of control LPL activity, which was 104 milliunits/plate for IL-6 experiments and 72 milliunits/plate for TNF experiments. Values for IL-6 experiments are means ±SE (hars) (n = 6) of Ì experiments and for TNF means ±SE (n = 5) of two experiments. *. signifi cantly different from HGF controlunits/ml. P < 0.0001: # significantly different from murine IL-6 "value at 50.000 P s 0.0001 4115 1. Kern. K. A., and Norton. J. A. Cancer cachexia. J. Parenteral Enterai Nutr.. 12: 286-298. 1988. 2. Gossberg. S. F.. and O'Leary. W. M. Hyperlipaemia following viral infection in the chicken embryo: a new syndrome. Nature (Lond.), 20H: 954-956. 1965. 3. Lees, R. S.. Beisel. W. R., and Bartelloni. P. J. Effects of an experimental viral infection on plasma lipid and lipoprotein metabolism. Mctab. Clin. Exp.. 21: 825-833, 1972. 4. Rouzcr. C. A., and Cerami, A. Hypertriglyccridemia associated with Trypanosonta brucei brucei infection ¡nrabbits: role of defective triglycéridere moval. Mol. Biochem. Parásito!.. 2: 31-38. 1980. 5. Vlassara. H.. Speigel, R. J., San Doval. D.. and Cerami. A. Reduced lipo protein lipase activity in patients with malignancy-associated weight loss. Horm. Metab. Res.. 18: 698-703. 1986. 6. Lanza-Jacoby, S., Lansey, S. C., Miller, E. E., and Cleary, M. P. Sequential changes in the activities of lipoprotein lipase and lipogenic en/ymes during tumor growth in rats. Cancer Res.. 44: 5062-5067, 1984. 7. Eckel, R. H. Adipose tissue lipoprotein lipase. In: 3. Borens/tajn (ed.). Li poprotein Lipase. pp. 149-185. Chicago: Evener. 1987. 8. Kawakami. M.. Pekala. P. H., Lane. M. D.. and Cerami, A. I.ipoprotcin lipase suppression in 3T3-L1 cells by an endotoxin induced mediator from exúdatecells. Proc. Nati. Acad. Sci. USA, 79: 912-916. 1982. 9. Beutler. B., Hamhoney. J.. Le Trang. N.. Pekala. P.. and Cerami, A. Purifi cation of cachectin, a lipoprotein lipase-suppressing hormone secreted by endotoxin-induced RAW 264.7 cells. J. Exp. Med., 161: 984-995. 1985. H). Beutler, B. A.. Greenwald, D.. Hulmes, J. D., Chang. M., Pan, U-C. E., Mathison. J.. Ulevich, R., and Cerami, A. Identity of tumor necrosis factor and the macrophage-secreted factor cachetin. Nature (Lond.). il fi: 552-554. 1985. INTERLEUKIN 6 REDUCES LPL ACTIVITY 11. Semb, H., Peterson, J., Tavernier, J., and Olivecrona, T. Multiple effects of tumor necrosis factor on lipoprotein lipase in vivo. J. Biol. Chem., 261: 8390-8394, 1987. 12. Jablons, D. M., Mulé,J. J., Mclntosh, J. K., Sehgal, P. B., May, L. T., Huang. C. M., Rosenberg, S. A., and Lotze, M. T. IL-6/IFN-/3-2 as a circu lating hormone. Induction by cytokine administration in humans. J. Immunol., 142: 1542-1547, 1989. 13. Mclntosh, J. K., Jablons, D. M., Mulé,J. J., Nordan, R. P., Rudikoff, S., Lotze, M. T., and Rosenberg, S. A. In vivo induction of IL-6 by administra tion of exogenous cytokines and detection of de novo serum levels of IL-6 in tumor-bearing mice. J. Immunol., ¡43:162-167, 1989. 14. J. Van Snick. Interleukin-6: an overview. Annu. Rev. Immunol., 8: 253-278, 1990. 15. Helfgott, D. C., Tatter, S. B., Santhanam, U., Clarick, R. H., Bhardwaj, N., May, L. T., and Sehgal, P. B. Multiple forms of Ifn-/32/H-6 in serum and body fluids during acute bacterial infection. J. Immunol., 142: 948-953, 1989. 16. Breen, E. C., Rezai, A. R., Nakajima, K., Beali, G. N., Mitsuasu, R. T., Hirano, T., Kishimoto, T., and Martinez-Maza, O. Infection with HIV is associated with elevated II-6 levels and production. J. Immunol., 144: 480484, 1990. 17. Bataille, R., Jourdan, M., Zhang, X-G.. and Klein, B. Serum levels of IL-6, a potent myeloma cell growth factor, as reflect of disease severity in plasma cell dyscrasias. J. Clin. Invest., 84: 2008-2011, 1989. 18. Utsumi, K., Takai, Y., Tada, T., Ohzeki, S., Fujiwara, H.. and Hamaoka, T. Enhanced production of IL-6 in tumor-bearing mice and determination of cells reponsible for its augmented production. J. Immunol., 145: 397-403, 1990. 19. Gelin, J„Moldawer, L. L., Lonnroth, C.. deMan, P., Svanborg-Eden, C., Lowry, S. F., and Lundholm, K. G. Appearance of hybridoma growth factor/ interleukin-6 in the serum of mice bearing a methylcholanthrene-induced sarcoma. Biochem. Biophys. Res. Commun., 157: 575-579, 1988. 20. Flick, D. A., and Gifford, G. E. Comparison of in vitro cell cytotoxic assays for tumor necrosis factor. J. Immunol. Methods, 68: 167-175, 1984. 21. Nordan, R. P., Pumphrey, J. G., and Rudikoff, S. Purification and NH2terminal amino acid sequence of a plasmacytoma growth factor derived from the murine macrophage cell line P388D1. J. Immunol., 139: 813-817. 1987. 22. Vink, A.. Coulie, P. G., Wauters, P., Nordan, R. P., and Van Snick, J. B. Cell growth and differentiation activity of interleukin-HPl and related murine plasmacytoma growth factors. Synergy with interleukin-1. Eur. J. Immunol., /«:607-612, 1988. 23. Aarden, L. A., Degroot, E. R.. Schaap, O. L., and Lansdorf, P. M. Produc tion of hybridoma growth factor by human monocytes. Eur. J. Immunol., 17: 1411-1416,1987. 24. Hubert, D. M., Cancro, M. P., Sberle, P. A., Nordan, R. P., Van Snick, J., Gerhardt, J., and Rudikoff, S. T cell derived IL-6 is differentially required for antigen specific antibody secretion in primary versus secondary B cell. J. Immunol.. 143: 4010-4024, 1989. 25. Peterson, J., Olivecrona, T., and Bentsson-Olivecrona, G. Distribution of 4116 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. lipopoprotein lipase and hepatic lipase between plasma and tissues: effect of hypertriglyceridemia. Biochim. Biophys. Acta, 837: 262-270, 1985. Langer, C. A., Birkenmeier, E. H., Ben-Zeev, O., Schotz, M. C., Sweet, H. O., Davisson, M. T., and Gordon, J. I. The fatty liver dystrophy (fid) muta tion. J. Biol. Chem., 264: 7994-8003. 1989. Nilsson-Ehle, P., and Schotz, M. C. A stable, radioactive substrate emulsion for assay of lipoprotein lipase. J. Lipid Res., 17: 536-541, 1970. Belfrage, P., and Vaughn, M. Simple lipid-liquid partition system for isola tion of labeled oleic acid from mixture with glycerides. J. Lipid Res., 10: 341-344, 1969. Mackall, J. C., Student, A. K., Polakis, S. E., and Lane, M. D. Induction of lipogenesis during differentiation in a "pre-adipocyte" cell line. J. Biol. Chem., 251: 6462-6464, 1976. Rubin, C. S., Hirsch, A, Fung, C., and Rosen. O. M. Development of hor mone receptors and hormonal responsiveness in vitro. 3. Biol. Chem., 253: 7570-7578.1978. Zechner, R., Newman, T. C., Sherry, B., Cerami, A., and Breslow, J. L. Recombinant human cachetin/tumor necrosis factor but not interleukin-la downregulates lipoprotein lipase gene expression at the transcriptional level in mouse 3T3-L1 adipocytes. Mol. Cell. Biol., 8: 2394-2401, 1988. Mulé, J. J., Mclntosh, J. K., Jablons, D. M., and Rosenberg, S. A. Antitumor activity of recombinant interleukin-6 in mice. J. Exp. Med., ///; 629-636, 1990. Socher, S. H., Martinez, D., Craig, J. B., Kühn.J. G.. and Oliff, A. Tumour necrosis factor not detectable in patients with clinical cancer cachexia. J. Nati. Cancer Inst., «ft-595-598, 1988. Waage. A., Espevik, T., and Lamvik, J. Detection of tumour necrosis factorlike cytotoxicity in serum from patients with septicaemia but not from un treated cancer patients. Scand. J. Immunol., 24: 739-743, 1986. Moldawer, L. L., Gelin, J., Schersten, T., and Lundholm, K. G. Circulating interleukin-1 and tumor necrosis factor during inflammation. Am. J. l'In si ol., 253: R922-R928, 1987. Waage, A, Brandtzaeg, P., Halstensen. A., Kierulf, P.. and Expevik, T. The complex pattern of cytokines in serum from patients with meningococcal septic shock. Association between interleukin-6, interleukin-1, and fatal out come. J. Exp. Med.. 769: 333-338, 1989. Brandt. S. J., Bodine, D. M., Umiliar. C. E., and Nienhuis, A. W. Dysregulated interleukin 6 expression produces a syndrome resembling Casleman's disease in mice. J. Clin. Invest., 86: 592-599, 1990. Fried, S. K., and Zechner, R. Cachectin/tumor necrosis factor decreases human adipose tissue lipoprotein lipase mRNA levels, synthesis, and activity. J. Lipid Res., 30: 1917-1923, 1989. Cornelius, P., Enerback, S., Bjursell, G., Olivecrona, T., and Pekala, P. H. Regulation of lipoprotein lipase mRNA in 3T3-L1 cells by tumour necrosis factor. Biochem. J., 249: 765-769. 1988. Kishimoto, T. The biology of interleukin-6. Blood, 74: 1-10, 1989. Green, H., and Kehinde, O. Sublines of mouse 3T3 cells that accumulate lipid. Cell, /: 113-116, 1974.