ARTICLE IN PRESS
doi:10.1510/icvts.2007.159558
Interactive CardioVascular and Thoracic Surgery 6 (2007) 818–819
www.icvts.org
Case report - Assisted circulation
Acute ventricular septal defect treated with an Impella recovery as
a ‘bridge therapy’ to heart transplantation
Francesco Patanè*, Edoardo Zingarelli, Fabrizio Sansone, Mauro Rinaldi
Department of Cardiac Surgery, San Giovanni Battista Hospital, C.so Bramante 88, 10126 Turin, Italy
Received 21 May 2007; received in revised form 1 July 2007; accepted 3 July 2007
Abstract
We present the case of a 59-year-old male, admitted to hospital for cardiogenic shock due to massive infero-lateral myocardial infarction.
Angiography showed occlusion of the right coronary artery and widespread critical lesions of both the anterior descending and circumflex
artery. Echocardiography showed inferior akinesia with a large posterior ventricular septal defect (VSD). The haemodynamic instability
induced us to use a left ventricular assist device (L-VAD) like Impella for easiness of its percutaneous implantation and for its duration. We
obtained the stabilisation of the patient and the improvement of the clinical conditions. The location of the ventricular septal defect
(VSD), from one side, and the serious and widespread coronaropathy (not suitable for any kind of revascularisation), from the other side,
led us to choose heart transplantation for this patient. Heart transplantation was performed on the 12th day after myocardial infarction
without complication and the patient was discharged on the 35th postoperative day. In our opinion, when the position of the VSD is
unseemly and there coexists a widespread coronaropathy not eligible for revascularisation, heart transplantation may represent an
efficacious alternative. Moreover, the use of L-VAD, reducing interventricular shunt and ensuring an adequate cardiac output, allows to
obtain clinical stabilisation before heart transplantation.
2007 Published by European Association for Cardio-Thoracic Surgery. All rights reserved.
Keywords: Ventricular septal defect; Left ventricular assist device; Heart transplantation
1. Patient characteristics
We describe the case of a 59-year-old male admitted to
hospital for cardiogenic shock with hypotension, oligoanuria
and dyspnoea; angina appeared three days before. ECG
showed an infero-lateral myocardial infarction. Echocardiography showed a large VSD just behind the posterior leaflet
of the mitral valve and in connection with mitral annulus;
mitral regurgitation was trivial and the right ventricle was
seriously impaired with severe hypokinesia (TAPSE 12 mm);
QPyQS was )2 and systolic pulmonary artery pressure
(PAPs) was 85 mmHg. Angiography showed occlusion of the
right coronary artery and a widespread coronaropathy of
both the anterior descending and circumflex artery. The
patient was reanimated because of cardiac arrest: the
worsening of his condition forced us to use intra-aortic
balloon pump (IABP) and L-VAD (Impella Recovery P7: 4
lymin flow) as a ‘bridge to heart transplantation’: its
percutaneous implantation without sternotomy makes the
procedure very easy with a low risk of infections and
mechanical complication during heart transplantation;
moreover, its duration is enough to assure the suitable
donor’s finding.
We obtained an improvement both in clinical conditions
and biological parameters of the patient: there was a
reduction of bilirubin, transaminase and creatinine (the
*Corresponding author. Tel.: q39-11-6335510; fax: q39-11-6335509.
E-mail address: f_patane@hotmail.com (F. Patanè).
2007 Published by European Association for Cardio-Thoracic Surgery
patient needed a short period of dialysis) with a slow
improvement of renal and hepatic function. Heart transplantation was performed on the 8th day after positioning
L-VAD and the patient was discharged on the 35th postoperative day.
2. Surgery procedure and pathological characteristics
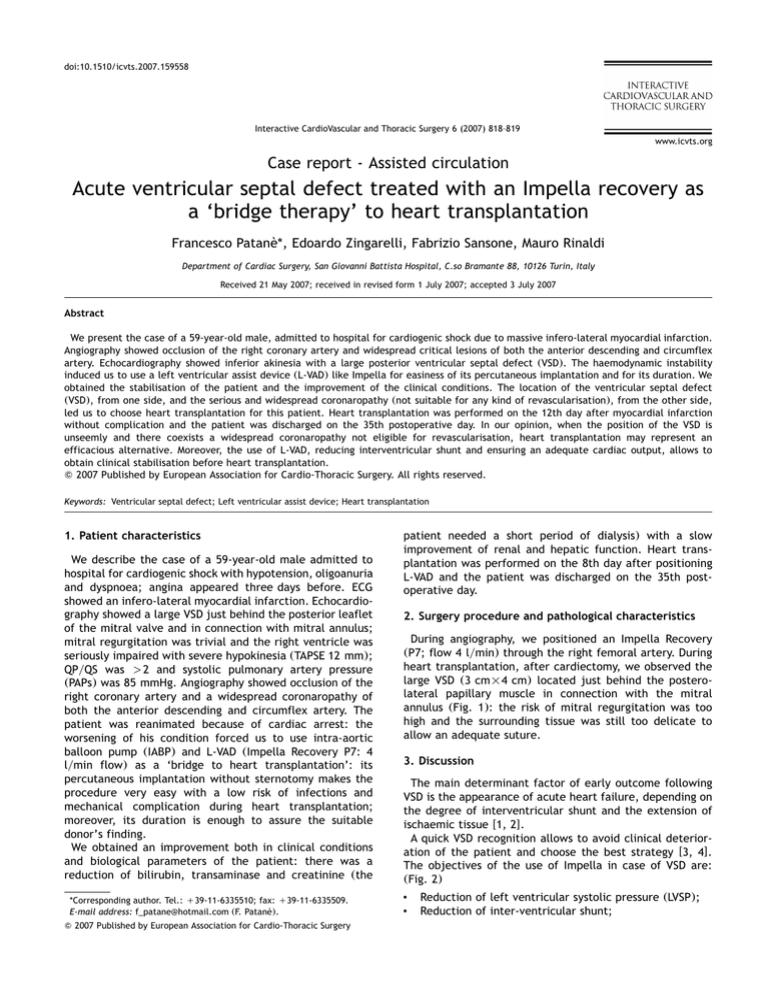
During angiography, we positioned an Impella Recovery
(P7; flow 4 lymin) through the right femoral artery. During
heart transplantation, after cardiectomy, we observed the
large VSD (3 cm=4 cm) located just behind the posterolateral papillary muscle in connection with the mitral
annulus (Fig. 1): the risk of mitral regurgitation was too
high and the surrounding tissue was still too delicate to
allow an adequate suture.
3. Discussion
The main determinant factor of early outcome following
VSD is the appearance of acute heart failure, depending on
the degree of interventricular shunt and the extension of
ischaemic tissue w1, 2x.
A quick VSD recognition allows to avoid clinical deterioration of the patient and choose the best strategy w3, 4x.
The objectives of the use of Impella in case of VSD are:
(Fig. 2)
•
•
Reduction of left ventricular systolic pressure (LVSP);
Reduction of inter-ventricular shunt;
ARTICLE IN PRESS
F. Patanè et al. / Interactive CardioVascular and Thoracic Surgery 6 (2007) 818–819
819
Fig. 2. Physiopathology of the use of L-VAD in case of VSD.
Fig. 1. Macroscopic examination shows a large ventricular septal defect just
behind the postero-lateral papillary muscle and in connection with the mitral
annulus.
•
•
Improvement of cardiac output (CO);
Improvement of right ventricular function.
We observed a reduction of pulmonary artery pressure
(PAP) and SVO2 with an improvement of CO, which showed
a reduction of interventricular shunt. Echocardiography was
not useful in measuring the entity of interventricular shunt
because of the interferences of Impella with the echocardiographic feeler.
In our case, VSD is not suitable for standard surgical
approach for these reasons:
•
•
Location of VSD, very close to postero-lateral papillary
muscle, posterior leaflets of the mitral valve and in
connection with the mitral annulus, without enough
tissue to suture the patch preserving mitral valve function (Fig. 1).
Coronaric anatomy: the widespread coronaropathy, the
shortage of the run-off and the unfavourable anatomy
•
of the vessels like ‘rosary crown’, determined the uselessness of surgical revascularisation;
The age of the patient.
In conclusion, our experience confirms that the use of
Impella is useful in the stabilisation of these patients;
moreover, in patients with VSD not suitable to the surgical
repair, cardiac transplant represents a valid alternative.
References
w1x Levy B, Perrin O, Thisse JY, Houppe JP, Villemot JP, Danchin N.
Myocardial infarction caused by thrombosis of the common trunk of the
left coronary artery without collateral circulation. Treatment by intraaortic counterpulsation and subsequent heart transplantation. Arch Mal
Coeur Vaiss 1992 Dec;85:1861–1863.
w2x Tatou E, Gomez MC, Leneuf P, Eicher JC, Jazayeri S, Charve P, Girard
C, Brenot R, David M. Cardiogenic shock complicating extensive infarction with ventricular septal defect. Circulatory assistance and heart
transplantation. Arch Mal Coeur Vaiss 2001 Mar;94:236–240.
w3x Baillot R, Pelletier C, Trivino-Marin J, Castonguay Y. Postinfarction
ventricular septal defect: delayed closure with prolonged mechanical
circulatory support. Ann Thorac Surg 1983 Feb;35:138–142.
w4x Deja MA, Szostek J, Widenka K, Szafron B, Spyt TJ, Hickey MS,
Sosnowski AW. Post infarction ventricular septal defect — can we do
better? Eur J Cardiothorac Surg 2000 Aug;18:194–201.