Medicare Part A Introduction to Skilled Nursing Facility Billing
advertisement

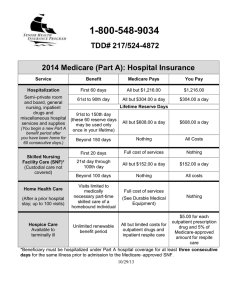
www.hcfa.gov Medicare Part A Introduction to Skilled Nursing Facility Billing EMPIRE MEDICARE SERVICES HCFA Medicare Part A and Part B Contracted Agent Medicare Billing Skilled Nursing Facility Table of Contents EXTENDED CARE BENEFIT IN A SNF.............................................................................. 1 RE-ESTABLISHING BENEFITS IN A SKILLED NURSING FACILITY ..................................... 3 RENEWAL OF BENEFITS IN A SKILLED NURSING FACILITY ............................................. 4 NEW BENEFITS WILL BE AVAILABLE TO PATIENT ............................................................. 5 UB-92 HCFA-1450 (FACSIMILE)................................................................................... 6 SKILLED NURSING FACILITY BILL TYPES........................................................................ 7 SNF CHARGE STRUCTURE REVENUE CODES .................................................................. 8 CODING FOR SKILLED NURSING FACILITIES ................................................................... 9 ONE DAY STAY............................................................................................................... 11 NO-PAY DISCHARGE BILLS ........................................................................................... 12 RESUBMITTING COST AVOIDED CLAIMS ....................................................................... 13 MAJOR CHANGES FOR BILLING UNDER SNF PPS ........................................................ 14 MDS ASSESSMENT SCHEDULE...................................................................................... 15 MDS 2.0 RUG-III CODES ............................................................................................ 16 RUG CODES (HIPPS).................................................................................................. 18 HIPPS MODIFIERS/ASSESSMENT TYPE INDICATORS ................................................... 19 PART B BENEFITS ......................................................................................................... 21 PART B SNF CHARGE STRUCTURE REVENUE CODES ................................................... 23 SNF BILLING ................................................................................................................ 24 HCPCS CODING REQUIREMENTS ................................................................................. 24 BILLING THERAPY SERVICES ........................................................................................ 25 UNDER PART B IN A SNF .............................................................................................. 25 PART B THERAPY BILLING ............................................................................................ 26 Empire Medicare Services Orientation 2000 Medicare SNF Billing EXTENDED CARE BENEFIT IN A SNF Medicare beneficiaries may be eligible for up to 100 days of Part coverage in a skilled nursing facility (SNF) if they meet both technical and medical qualifications for coverage. The benefit is dependent upon the resident’s need for skilled care. Medicare does not have a long term care custodial benefit. Technical Qualifications: • • • 3 day qualifying hospital stay - must occur while patient is enrolled in Medicare transfer to the SNF within 30 days of discharge - may exceed 30 days if patient is on “hold” for therapy - may exceed 30 days if patient transfers from one SNF to another (first admission must be within 30 days of hospital discharge; next SNF admission must be within 30 days of last covered day in 1st SNF) enrolled in Medicare Part A and have benefit days available to use Medical Qualifications: • • • requires skilled care (from a nurse or therapist) on a daily basis as a ‘practical matter’ services can only be provided in a SNF services are provided for a condition which the patient was treated in the hospital or for a condition which arose while the beneficiary was being treated in the hospital Benefit Periods There is no limit to the number of benefit periods that a beneficiary may qualify for. You may have more than one period of 100 days paid for in a SNF. In order to renew benefits, the SNF resident must: • • Empire Medicare Services Orientation 2000 be discharged to home for a period of at least 60 consecutive days (not requiring inpatient care under Part A in a SNF or hospital) remain in the SNF at a “non-skilled level of care” (custodial) - this requires claims coding by the SNF to indicate the change Page 1 Medicare SNF Billing If these requirements are not met, the beneficiary remains in the same benefit period and may potentially run out of Part A days (benefits exhaust). This beneficiary would be ineligible for new coverage (technically) even if he experiences a new medical condition, had a new hospitalization and return to the SNF meeting the medical requirements for coverage. Empire Medicare Services Orientation 2000 Page 2 Medicare SNF Billing RE-ESTABLISHING BENEFITS IN A SKILLED NURSING FACILITY 6/1 7/15 30 Days 8/14 9/14 45 benefit days used 60 Days Occurrence Code 22 or Discharge ♦ If the resident is “cut” or discharged on 7/15, the balance of benefits available may be used if the patient returns to the facility or is upgraded to “skilled level of care” within 30 days (8/14). NO NEW QUALIFYING HOSPITAL STAY IS REQUIRED ♦ If the resident returns to the facility or is upgraded to “skilled level of care at any point between day 31 and day 60 (8/15 – 9/14), THAT PATIENT MUST HAVE A QUALIFYING HOSPITAL STAY TO RESUME USING THE BALANCE OF REMAINING BENEFITS. ♦ If the resident returns to the facility or is upgraded to “skilled level of care” at any point after day 60 (9/15) that patient is eligible for a NEW BENEFIT PERIOD, BUT MUST HAVE A QUALIFYING HOSPITAL STAY and meet all other criteria in order for new benefits to apply. NOTE: Any unused benefit days from prior benefit period are “lost” if the patient enters a new benefit period. NOTE: A change in “diagnosis” does not affect the benefit period. Regardless of having a new diagnosis or readmission with the same diagnosis, application of benefits is contingent upon the receipt of skilled care in a SNF for a condition which the beneficiary was treated in a qualifying hospital stay. Empire Medicare Services Orientation 2000 Page 3 Medicare SNF Billing RENEWAL OF BENEFITS IN A SKILLED NURSING FACILITY EXAMPLE 1 SNF HOSP 1/10/99 3/15/99 9/1/99 37 benefit days used No pay discharge claim Occurrence Code 22 ♦ Patient cut 3/15/99 ♦ Occurrence Code 22 = 3/15/99 on last Part A covered claim ♦ Patient remained non-skilled (custodial care) until new hospital admit (9/1/99) ♦ No pay discharge bill 3/16/99 – 9/1/99 4 No special coding on discharge bill ♦ Benefit spells will not link ♦ New benefit period will be available Empire Medicare Services Orientation 2000 Page 4 Medicare SNF Billing EXAMPLE 2 SNF HOSP 1/10/99 4/18/99 9/1/99 100 benefit days used No pay discharge claim Benefits Exhausted (A3) ♦ Patient exhausts benefits on 4/18/99 ♦ Patient remains at skilled level of care until new hospital admission (9/1/99) ♦ No pay discharge bill must be submitted (per regulations) to place patient as inpatient from date of service 4/19/99 – 9/1/99 ♦ Spells of illness will link ♦ No new benefits will be available to patient EXAMPLE 3 SNF HOSP 1/10/99 4/18/99 6/1/99 9/1/99 100 benefit days used No pay discharge claim Benefits Exhausted (A3) ♦ Patient exhausts benefits on 4/18/99 ♦ Patient remains at skilled level of care until 6/1/99 ♦ No pay discharge bill DOS 4/19/99 – 10/1/99 may be coded with Occurrence Code 22 = 6/1/99 as long as the patient remained non-skilled for 60 consecutive days beginning 6/1/99 ♦ Spells of illness will not link NEW BENEFITS WILL BE AVAILABLE TO PATIENT Empire Medicare Services Orientation 2000 Page 5 Medicare SNF Billing UB-92 HCFA-1450 (FACSIMILE) 2 6 STATEMENT COVERS 5 FED. TAX NO. 12 PATIENT NAME 14 BIRTHDATE 32 CODE 4 TYPE OF BILL 3 PATIENT CONTROL NO. PS 15 SEX FROM 7 COV 8 N-C D. D. THROUGH 9 C-I D. 10 L-R 11 D. 13 PATIENT ADDRESS ADMISSION 19 20 17 DATE 18 HR TYPE SRC 16 MS CONDITION CODES 21 D HR 22 STAT 23 MEDICAL RECORD NO. OCCURREN 33 OCCURREN 34 OCCURREN 35 OCCURREN 36 CE DATE CODE CE DATE CODE CE DATE CODE CE DATE CODE 38 24 OCCURRENCE SPAN FROM 39 AMOUNT 26 27 28 29 30 37 A B C THROUGH VALUE CODE CODE 25 31 40 CODE VALUE CODES AMOUNT 41 CODE VALUE CODES AMOUNT a b c d 42 REV.CD. 46 48 NON-COVERED 44 HCPCS/RATES 45 SERV.DATE SERV.UNITS 47 TOTAL CHARGES CHARGES 43 DESCRIPTION 50 PAYER ASG INFO BEN 55 EST. AMOUNT 54 PRIOR PAYMENTS DUE 56 DUE FROM Ø 57 59 PATIENT NO. P.REL 60 CERT.-SSN-HIC.-ID 58 INSURED'S NAME 63 TREATMENT AUTHORIZATION CODES 67 PRIN.DIAG.CD. 61 GROUP NAME 64 ESC 65 EMPLOYER NAME 62 INSURANCE GROUP NO. 66 EMPLOYER LOCATION OTHER DIAG. CODES 68 CODE 69 CODE 80PRINCIPAL PROCEDURE 79 P.C. 52 REL 53 51 PROVIDER NO. 49 CODE DATE OTHER PROCEDURE CODE DATE 70 CODE 71 CODE 81OTHER PROCEDURE CODE DATE OTHER PROCEDURE CODE DATE 72 CODE 78 73 CODE OTHER PROCEDURE CODE 75 CODE 76 ADM. DIAG. 77 E-CODE 82 ATTENDING PHYS. ID DATE OTHER PROCEDURE CODE 74 CODE 83 OTHER PHYS. ID DATE 84 REMARKS OTHER PHY 85 PROVIDER REPRESENTATIVE 86 DATE X UB-92 HCFA-1450 Empire Medicare Services Orientation 2000 I CERTIFY THE CERTIFICATIONS ON THE REVERSE APPLY TO TYPE BILL AND ARE MADE A PART Page 6 Medicare SNF Billing SKILLED NURSING FACILITY BILL TYPES SNF Part A Type Span Type of Bill Discharge Status Non-covered Admit – Discharge 210 Anything but 30 Covered Admit – Discharge 211 Anything but 30 Covered or Non-covered Admit – Interim 212 30 Covered or Non-covered Interim – Interim 213 30 Covered or Non-covered Interim – Discharge 214 Anything but 30 215 – Late Charge Bill Part A Services (not permitted under PPS) 217 – Adjustment Bill Part A Services 218 – Cancel Only Bill Part A Services Ancillary Claims 22X – Part B Coverage Only 23X – Outpatient Claims Empire Medicare Services Orientation 2000 Page 7 Medicare SNF Billing SNF CHARGE STRUCTURE REVENUE CODES SNF PPS 0022 Room and Board 100 – All Inclusive 120 – Semi-Private (two beds) 13X – Semi-Private (three/four beds) 14X – Private Room 15X – Ward 16X – Other (sterile environment) 18X – Leave of Absence (9000-9044 RUGS II Groups) for demonstration SNFs Pharmacy IV Therapy Medical/Surgical Supplies Oncology Laboratory Lab-Pathology Radiology Radiology-therapeutic Nuclear Medicine CT Scan Operating Room Services Blood Storage Imaging Services Respiratory Services Physical Therapy Occupational Therapy Speech Therapy Pulmonary Function Audiology Cardiology EKG/ECG EEG Gastro-Intestinal Other Diagnostic Services Other Therapeutic Services 25X 26X 27X 28X 30X 31X 32X 33X 34X 35X 36X 39X 40X 41X 42X 43X 44X 46X 47X 48X 73X 74X 75X 92X 94X (Complex Medical Equipment) ***Ambulance 540 (SNF PPS Facilities) See your UB-92 billing book for value of “X” in each category 6/98 Empire Medicare Services Orientation 2000 Page 8 Medicare SNF Billing CODING FOR SKILLED NURSING FACILITIES SNF Discharge Status Required on 21X Bill Types Only Most often used: 01 02 03 05 20 30 50 51 Discharged to Home Transferred to Hospital (PPS) Transfer to Another SNF Transferred to Non-PPS Hospital Expired Still Patient (Interim Bills – 212/213) Discharge to Hospice (Home) Discharge to Hospice (Medical Facility) 07 20 21 39 40 55 Non-Hospice Related Demand Bill Denial Notice for Other Insurer Private Room Medically Necessary Same Day Transfer SNF Bed Not Available (When patient admission is delayed by 30 days) Medical Appropriateness (When therapy is delayed) SNF Readmission (Patient is readmitted within 30 days) Facility Accepts Other Insurance Payment in Full PPV/Flu Administered (not required) SNF Condition Codes Most often used: 56 57 77 A6 (Plus codes for adjustments. See special listing) Empire Medicare Services Orientation 2000 Page 9 Medicare SNF Billing SNF Occurrence Codes Most often used: 11 21 22 24 35 44 45 A3 – – – – – – – – Onset of Illness (Most Recent) UR Notice Received Date Active Care Ended Date Other Insurance Denied Date Treatment Started for Physical Therapy Date Treatment Started for Occupational Therapy Date Treatment Started for Speech Therapy Benefits Exhausted SNF Occurrence Span Codes Most often used: 70 – 71 – 74 – 74 – 78 – M1 – Qualifying Stay Prior Inpatient Stay Non-covered Level of Care * While patient remains in SNF * Show non-covered charges Leave of Absence * While patient is on temporary leave * Do not show non-covered charges Prior SNF Stay Provider Liability on Non-covered Days (Provider Reported) SNF Value Codes Most often used: Empire Medicare Services Orientation 2000 09 – Medicare Co-insurance 46 – Grace Days 50 – Physical Therapy Sessions * Cumulative sessions under Part B 51 – Occupational Therapy Sessions * Cumulative sessions under Part B 52 – Speech Therapy Sessions * Cumulative sessions under Part B Page 10 Medicare SNF Billing ONE DAY STAY Reimbursement for One Day Stays The Medicare Program does not normally reimburse a SNF for date of discharge, death, or when the patient does not meet “midnight census” criteria. In certain instances, a SNF can be reimbursed for a single day stay if that patient dies or is transferred back to an acute care facility on the day of admission. 1. Coding for same day transfer: ♦ ♦ ♦ ♦ Admit date Patient status Condition code Covered days NOTE: = = = = Through date 02 40 1 SNF will be reimbursed for one day. Intermediary does not take a SNF benefit day. (Hospital benefit day will be applied). 2. Coding when admit and date of death are the same: ♦ ♦ ♦ Admit date Patient status Covered day NOTE: Empire Medicare Services Orientation 2000 = = = Through date 20 1 SNF will be reimbursed for one day. Intermediary does apply one SNF benefit day. Page 11 Medicare SNF Billing NO-PAY DISCHARGE BILLS Medicare requires that skilled nursing facilities (SNFs) submit no pay discharge bills for Part A residents who live in their facilities. Tracking is done by Medicare fiscal intermediaries for the purpose of benefit period management. Because a Medicare beneficiary may have more than one benefit period in a lifetime, it is necessary to account for time lived in hospitals and skilled nursing homes. A new benefit period is available to those individuals who are able to “break” or end a benefit period by meeting one of the following criteria: ♦ 60 consecutive days facility free OR ♦ 60 consecutive days living in a SNF at a custodial (non-skilled) level of care The Medicare patient must then have a new qualifying hospital stay of at least 3 days (not counting day of discharge) and be admitted to the SNF within 30 days of hospital discharge. The beneficiary will again be eligible for up to 100 days of Part A SNF coverage if he meets medical criteria. SNFs are required to submit no-pay discharge claims for their residents who are entitled to Part A according to Section 527 of the HCFA Intermediary Manual 12. In the past, Empire Medicare Services has accepted a single no-pay discharge claim for the period of time the beneficiary was not paid under Medicare Part A. With the start of new billing requirements due to the RUGS III Demonstration Project and SNF PPS, no-pay discharge claims MUST be split to reflect the changes in billing methodologies. In addition to all other billing requirements, discharge claims must include: For RUGS III demonstration providers ♦ a 9000 revenue code for accommodation charges (FL 42) For SNF PPS providers ♦ A line of data using revenue code 0022 (FL 42) ♦ A HIPPS code (you may use AAA00) (FL 44) ♦ 0 in the units field (FL 46) ♦ 0 in the charges field (FL 47) ♦ Semi-private accommodation revenue code, rate, units, charges (non-covered) Claims that do not include the special coding requirements will be returned to provider for correction and resubmission. Empire Medicare Services Orientation 2000 Page 12 Medicare SNF Billing RESUBMITTING COST AVOIDED CLAIMS Providers may submit electronic adjustments for impatient claims that have been cost avoided because records show that another insurance company is responsible for payment of charges. Adjustment claims would be submitted with Type of Bill (TOB) 217. When submitting the electronic adjustment request, use one of the following Condition Codes as appropriate. D7 CHANGE TO MAKE MEDICARE SECONDARY Condition code D7 must be submitted with a MSP Value Code and amount paid by the other insurer must be present on the adjustment claim along with: name and address of the other insurer and employment information (if any). * See MSP section of training manual D8 CHANGE TO MAKE MEDICARE PRIMARY Condition code D8 must be accompanied by remarks indicating the reason that Medicare should pay primary for the dates shown on the rejected claim. Reasons might include: ♦ ♦ ♦ ♦ Insurance policy holder has retired. Code claim with Occurrence Code 18 and date (beneficiary) or Occurrence Code 19 and date (spouse) Policy does not cover SNF services. Code claim with Occurrence Code 24 and date other insurance denies Benefits are exhausted under policy. Code claim with Occurrence Code 24 and date policy B/E. MSP files have been updated to show Medicare is primary. Adjustment requests which do not contain sufficient information in the remarks field to demonstrate why Medicare is the primary will be returned to provider (RTP) with the following reason code: 74002 Empire Medicare Services Orientation 2000 “Remarks on this adjustment requesting primary payment for an inpatient cost avoided claim are either missing or not sufficient to make primary payment.” Page 13 Medicare SNF Billing MAJOR CHANGES FOR BILLING UNDER SNF PPS ♦ ♦ A new revenue code (0022) has been created to indicate that a RUG-III classification group identifier is being billed on a Part A claim. 4 Revenue code 0022 is to appear on 21X bills for each line of data indicating a RUG-III group code is present 4 Each line of data using revenue code 0022 will be separately calculated for reimbursement based on payment tables in FI pricer software A HIPPS code has been created to indicate the 44 RUG-III groups will be utilized to indicate the medical classification assigned by the grouper program that interprets MDS 2.0 data 4 RUG-III codes are a 3 position alpha code ♦ For billing purposes, 19 two position modifiers have been developed and will be added to the RUG-III classification group to indicate what assessment has been completed during the billing period ♦ Medicare beneficiaries must be assessed on a specific schedule to determine covered level of care for billing Part A claims ♦ Each Medicare assessment provides a specific number of covered days which can be billed for the resident who is determined to be at a “skilled level of care” ♦ All services received by SNF resident must be coded on the Part A claim (no vendor billing) ♦ Part B benefits (not covered under the extended care services, i.e., flu shots) are billed separately Empire Medicare Services Orientation 2000 Page 14 Medicare SNF Billing MDS ASSESSMENT SCHEDULE Assessment Reference Date Reason for Assessment #AA8b MDS 2.0 Users Guide Number of Applicable Medicare Days 1–5 1 Medicare 5 Day Assessment 14 DAY 14 Comprehensive 11 – 14 7 Medicare 14 Day DAY 30 Full 21 – 29 2 Medicare 30 Day DAY 60 Full 50 – 59 3 Medicare 60 Day DAY 90 Full 80 – 89 4 Medicare 90 Day Medicare Assessment Schedule DAY 5 Comprehensive* May be completed OR Days (1 - 5) at day 14 16 Days (16 – 30) 30 Days (31 – 60) 30 Days (61 - 90) 10 Days (91 – 100) *If a resident expires or transfers to another facility before day 8, an MDS is prepared as completely as possible allowing for RUG classification and Medicare payment. *Full Assessment Empire Medicare Services Orientation 2000 = Entire MDS *Comprehensive Assessment = MDS + RAP’s Page 15 Medicare SNF Billing MDS 2.0 RUG-III CODES ADL INDEX END SPLITS MDS RUG-III CODES ULTRA HIGH Rx 720 minutes a week minimum At least 2 disciplines, 1st -5 days, 2nd - at least 3 days 16-18 9-15 4-8 NOT USED NOT USED NOT USED RUC RUB RUA VERY HIGH Rx 500 minutes a week minimum At least 1 discipline - 5 days 16-18 9-15 4-8 NOT USED NOT USED NOT USED RVC RVB RVA HIGH Rx 325 minutes a week minimum 1 discipline 5 days a week 13-18 8-12 4-7 NOT USED NOT USED NOT USED RHC RHB RHA MEDIUM Rx 150 minutes a week minimum 5 days across 1, 2 or 3 disciplines 15-18 8-14 4-7 NOT USED NOT USED NOT USED RMC RMB RMA LOW Nrsg. Rehab 6 days in at least 2 activities and Rehabilitation therapy Rx 3 days/ 45 minutes a week minimum 14-18 4-13 NOT USED NOT USED RLB RLA EXTENSIVE SERVICES - (if ADL <7, beneficiary classifies to Special Care) IV feeding in the past 7 days (K5a) IV medications in the past 14 days (P1ac) Suctioning in the past 14 days (P1ai) Tracheostomy care in the last 14 days (P1aj) Ventilator/respirator in the last 14 days (P1al) 7-18 7-18 7-18 new grouping: count of other categories code into plus IV Meds + Feed SE3 SE2 SE1 17-18 15-16 NOT USED NOT USED SSC SSB 7-14 NOT USED SSA 17-18D 17-18 12-16D 12-16 4-11D 4-11 Signs of Depression CC2 CC1 CB2 CB1 CA2 CA1 CATEGORY REHABILITATION SPECIAL CARE -- (if ADL <7 beneficiary classifies to Clinically Complex) Multiple Sclerosis (I1w) and an ADL score of 10 or higher Quadriplegia (Ilz) and an ADL score of 10 or higher Cerebral Palsy (Ils) and an ADL score of 10 or higher Respiratory therapy (P1bdA must = 7 days) Ulcers, pressure or stasis; 2 or more of any stage (M1a,b,c,d) and treatment (M5a, b,c,d,e,g,h) Ulcers, pressure; any stage 3 or 4 (M2a) and treatment (M5a,b,c,d,e,g,h) Radiation therapy (P1ah) Surgical, Wounds (M4g) and treatment (M5f,g,h) Open Lesions (M4c) and treatment (M5f,g,h) Tube Fed (K5b) and Aphasia (I1r) and feeding accounts for at least 51 percent of daily calories (K6a=3 or4) OR at least 26 percent of daily calories and 501cc daily intake (K6b=2,3,4 or 5) Fever (J1h) with Dehydration (J1c), Pneumonia (Ie2),Vomiting (J1o) or Weight loss (K 3a) Fever (J1h) with Tube Feeding (K5b) and, as above, (K6a=3 or 4) &/or (K6b = 2,3,4,or 5) CLINICALLY COMPLEX -Burns (M4b) Coma (B1) and Not awake (N1 = d) and completely ADL dependent (G1aa, G1ba, G1ha, G1ia = 4 or 8) Septicemia (I2g) Pneumonia (I2e) Foot / Wounds (M6b,c) and treatment (M6f) Internal Bleed (J1j) Dialysis (P1ab) Tube Fed (K5b) and feeding accounts for: at least 51% of daily calories (K6a = 3 or 4) OR 26 percent of daily calories and 501cc daily intake (K6b = 2, 3, 4 or 5) Dehydration (J1c) Oxygen therapy (P1ag) Transfusions (P1ak) Hemiplegia (I1v) and an ADL score or 10 or higher Chemotherapy (P1aa) No. Of Days in last 14 there were Physician Visits and order changes: visits >=1 days and order changes >=4 days; or visits >=2 days and order changes on >=2 days Diabetes mellitus (I1a) and injections on 7 days (O3 >= 7) and order changes >=2 days (P8 >= 2) Empire Medicare Services Orientation 2000 Signs of Depression Signs of Depression Page 16 Medicare SNF Billing IMPAIRED COGNITION Score on MDS2.0 Cognitive Performance Scale >= 3 BEHAVIOR ONLY Coded on MDS 2.0 items: 4+ days a week - wandering, physical or verbal abuse, inappropriate behavior or resists care; or hallucinations, or delusions checked PHYSICAL FUNCTION REDUCED No clinical conditions used 6-10 6-10 4-5 4-5 Nursing Rehabilitation* not receiving Nursing Rehabilitation not receiving IB2 IB1 IA2 IA1 6-10 6-10 4-5 4-5 Nursing Rehabilitation* not receiving Nursing Rehabilitation not receiving BB2 BB1 BA2 BA1 16-18 16-18 11-15 11-15 9-10 9-10 6-8 Nursing Rehabilitation* not receiving Nursing Rehabilitation not receiving Nursing Rehabilitation not receiving Nursing Rehabilitation PE2 PE1 PD2 PD1 PC2 PC1 PB2 6-8 4-5 4-5 not receiving Nursing Rehabilitation not receiving PB1 PA2 PA1 Default *To qualify as receiving Nursing Rehabilitation, the rehabilitation must be in at least 2 activities, at least 6 days a week. As defined in the Long Term Care RAI Users Manual, Version 2 activities include: Passive or Active ROM, amputation care, splint or brace assistance and care, training in dressing or grooming, eating or swallowing, transfer, bed mobility or walking, communication, scheduled toileting program or bladder retraining Empire Medicare Services Orientation 2000 Page 17 Medicare SNF Billing RUG CODES (HIPPS) RUG-III Code Payment Code Rehab Groups RUC RUB RUA RVC RVB RVA RHC RHB RHA RMC RMB RMA RLB RLA RUCXX RUBXX RUAXX RVCXX RVBXX RVAXX RHCXX RHBXX RHAXX RMCXX RMBXX RMAXX RLBXX RLAXX Extensive Care SE3 SE2 SE1 SE3XX SE2XX SE1XX Special Care SSC SSB SSA SSCXX SSBXX SSAXX RUG-III Code Payment Code Impaired Cognition IB2 IB1 IA2 IA1 IB2XX IB1XX IA2XX IA1XX Behavior Only BB2 BB1 BA2 BA1 BB2XX BB1XX BA2XX BA1XX Physical Function Reduced PE2 PE1 PD2 PD1 PC2 PC1 PB2 PB1 PA2 PA1 PE2XX PE1XX PD2XX PD1XX PC2XX PC1XX PB2XX PB1XX PA2XX PA11XX Default AAA00 Clinically Complex CC2 CC1 CB2 CB1 CA2 CA1 Empire Medicare Services Orientation 2000 CC2XX CC1XX CB2XX CB1XX CA2XX CA1XX Page 18 Medicare SNF Billing HIPPS MODIFIERS/ASSESSMENT TYPE INDICATORS The HIPPS rate codes established by the Health Care Financing Administration (HCFA) contains a 3-position alpha code to represent the RUG-III group medical classification of the SNF resident plus a two position modifier to indicate which assessment was completed. Together they consist of a 5-position HIPPS rate code for the purpose of billing Part A covered days to the fiscal intermediary. Each of the 19 modifiers refers to a specific assessment as explained in the following table. DESCRIPTION OF ASSESSMENT MODIFIER CODE Regular Assessments Admission/Medicare 5 Day Comprehensive Medicare 5 Day (Full) Medicare 14 Day (Full or Comprehensive) Medicare 30 Day (Full) Medicare 60 Day (Full) Medicare 90 Day (Full) Quarterly Review–Medicare 90 Day (Full) Significant Change in Status Assessment (SCSA) Other Medicare Required Assessment (OMRA) EXAMPLE: 11 01 07 02 03 04 54 38 08 A completed assessment for a SNF resident at day 30 who scores in the RUG-III group SSC would have a HIPPS rate code of SSC02 Significant Correction of Prior Full Assessment Significant Correction of Prior Full – 5 Day Significant Correction of Prior Full – 14 Day Significant Correction of Prior Full – 30 Day Significant Correction of Prior Full – 60 Day Significant Correction of Prior Full – 90 Day EXAMPLE: Empire Medicare Services Orientation 2000 41 47 42 43 44 Correction to above 30 day assessment example with a new RUG-III group of SEC would have a HIPPS code of = SEC42 Page 19 Medicare SNF Billing DESCRIPTION OF ASSESSMENT MODIFIER CODE OMRA (Replacement) Significant Change in Status Assessment (SCSA) (Replacement) Significant Change in Status – Replacing Significant Change in Status – Replacing Significant Change in Status – Replacing Significant Change in Status – Replacing EXAMPLE: 14 Day 30 Day 60 Day 90 Day 37 32 33 34 If a resident experienced a change in medical status outside the regular schedule, a SCSA is required. A SCSA the assessment completed within the window of a regularly scheduled assessment it replaces that assessment. An assessment done on day 27 would replace the 30-day assessment. The HIPPS code for a resident who had a SCSA on day 28 would be SEC32. Default Code: A modifier is required with the use of the default code (AAA) when days are billed on the UB-92 to the Medicare fiscal intermediary for services which are determined to be “covered care”, but no assessment has been completed to classify the resident. The default modifier is 00 . . . the HIPPS code would appear as AAA 00. Updated 7/98 Empire Medicare Services Orientation 2000 Page 20 Medicare SNF Billing PART B BENEFITS Who is eligible? Payment can be made under Part B for medical and other health services for inpatients in a SNF if: 1. 2. 3. 4. Part A benefits are exhausted. Part A benefits have been “cut.” Patient is not enrolled in Part A. Patient does not qualify for Part A coverage because the qualifying hospital stay or transfer requirements were not met. (Patient was admitted from home or admitted more than 30 days from qualifying stay). What services are covered? Part B benefits cover the following services: 1. 2. 3. 4. 5. 6. 7. 8. 9. Diagnostic x-rays, labs, tests (if SNF is hospital based). X-rays, radium and radioactive isotope therapy, including materials and services of technician (If SNF is hospital -based). Surgical dressings, splints, casts, and other devices used for the reduction of fractures and dislocations. Prosthetic devices (other than dental). Leg, arm, back, and neck braces, trusses and artificial legs, arms and eyes (including adjustment and repair and replacement parts). Physical, Occupational and speech therapy; or outpatient speech pathology services. Drugs-limited to PPV, flu, hepatitis B vaccines, oral cancer. Hemophilia clotting factors. Ambulance services.(submit to carrier) Is there any coverage for “outpatient” SNF patients? Yes, facilities that provide “walk-in” services at their SNF must have special certification to treat outpatients. In addition to the services mentioned above, the facility may provide and bill for durable medical equipment if it is being provided for residents for use in their homes. NOTE: Empire Medicare Services Orientation 2000 DME is billed to a special carrier; not to Medicare Part A. Page 21 Medicare SNF Billing What revenue codes are used? 1. For all inclusive ancillary billers Revenue Code – 24X (not valid after the start of SNF PPS) 2. Charge structure providers – see attached listing How often should Part B services be billed? Part B services should be billed on a monthly basis. It is also allowable to bill quarterly (every 3 months) for all-inclusive providers. Facilities must be very careful not to bill for periods of time in which a person is an inpatient at an acute care hospital. Part B ancillary claims will overlap inpatient claims and require adjustments to correct. Do we have to submit no-pay discharge bills if we are currently billing Part B benefits only? Yes, if you have ever billed Part A services for that patient, unless the last covered day was coded with Occurrence code 22 (and date). If a patient is within their 100 days of Part A benefits, do we also bill separately for the Part B services? No. The Part B services are included in the Part A reimbursement as long as the patient is covered by the Part A benefits. Part B benefits are only billable if the patient is not being covered under Part A. Empire Medicare Services Orientation 2000 Page 22 Medicare SNF Billing PART B SNF CHARGE STRUCTURE REVENUE CODES DIAGNOSTIC X-RAYS, DIAGNOSTIC LABORATORY TESTS 30X 31X 32X 73X 74X X-RAYS, RADIUM AND RADIOACTIVE ISOTOPE THERAPY (including materials and services of technicians): 33X 34X 35X MEDICAL AND SURGICAL SUPPLIES AND DEVICES 27X PROSTHETIC DEVICES (other than dental) which replace all or part of an internal body organ (including contiguous tissue) or all or part of the function of the permanently inoperable or malfunctioning internal body organ, including replacement or repairs of such items 274 * 42X* 43X* 44X* PHYSICAL THERAPY OCCUPATIONAL THERAPY SPEECH THERAPY SPECIALTY DRUGS 63X * (PPV, FLU, HEP B, Immunosuppressive Drugs, Hemophelia Clotting, Oral Cancer and anti-emetic drugs) * Requires HPCPS NOTE: Lab and X-ray services may only be billed if you have certified units within your facility Until Part B Consolidated Billing is in effect, vendors may continue to bill directly for their services to the carrier, and outpatient hospitals may bill services directly to the fiscal intermediary. Empire Medicare Services Orientation 2000 Page 23 Medicare SNF Billing SNF BILLING HCPCS CODING REQUIREMENTS There are no HCPCS codes required on Medicare Part A claims. In the realm of Part B billing, the requirements differ from inpatient billing (bill types 221 and 223) to outpatient billing (bill types 231 and 233). For inpatient Part B billing, HCPCS codes are required on the following revenue codes: 274 – prosthetic/orthotic devices 420 – physical therapy * 430 – occupational therapy * 440 – speech therapy * 636 – drugs requiring detailed coding (PPV, flu, etc.) 771 – administration of a drug (used when 636 is billed) * See Medicare News Update 1997-13, 1998-3, 1998-8 Effective for dates of service 7/1/98 HCPCS are required for therapy services on Part B claims. Effective with consolidated billing HCPCS will be required for all Part B services. For outpatient Part B billing, HCPCS codes are required on the following revenue codes: 30X – all lab revenue codes 31X – all lab path revenue codes 320 – angiocardiography 323 – arteriography 274 – prosthetic/orthotic devices 636 – drugs requiring detailed coding (PPV, flu, etc.) *See Medicare News Update 1996-1, 1996-13 Empire Medicare Services uses the St. Anthony's Level II Code Book for HCPCS reference. If your billers select a code from their reference source, the validity of this code can be checked using the OmniPro system. As is the case for diagnosis and revenue codes, the OmniPro files will mirror our internal computer (Fiscal Intermediary Shared System) and allow the biller to determine if the selected code will be accepted during claims processing. Empire Medicare Services Orientation 2000 Page 24 Medicare SNF Billing BILLING THERAPY SERVICES UNDER PART B IN A SNF Physical, occupational and speech therapy are billable to the Medicare fiscal intermediary (FI) if those services are deemed to be “restorative” in nature by Medicare definition . (See sections 220, 230.3, 542 of HIM-12) Coding Requirements on the UB-92 ONSET OF ILLNESS Occurrence Code 11 and date are required on Part B claims (they are not required on Part A claims) ♦ ♦ ♦ If the Part B services are a continuation of therapy begun when the resident was first admitted to the SNF (under Part A) the onset of illness date should reflect this. If you do not know when the patient became ill or was injured (prior to admission) you may use the SNF admission date for the Occurrence Code 11 date If the Part B services are based on new injury or illness (not associated with a SNF Part A admission), determine the date for Occurrence Code 11 based on when it was noted in the patient's medical record that there has been a change in condition requiring a restorative therapy program. START DATE OF THERAPY Occurrence Code 35 for physical therapy (PT), 44 for occupational therapy (OT), and 45 for speech therapy (ST) and date are required on Part B claims ♦ ♦ If the Part B services are a continuation of therapy that began under Part A, the start date for therapy would be when services were originally initiated under Part A. If the Part B services are not associated with Part A services, the start date would be the first services rendered after the patient was noted to have had a change in condition requiring a restorative therapy program. Empire Medicare Services Orientation 2000 Page 25 Medicare SNF Billing PART B THERAPY BILLING Type of Bill 12X 13X 22X 23X 74X 75X 83X Hospital inpatient ancillary Hospital outpatient SNF inpatient ancillary SNF outpatient ORF (Outpatient Rehabilitation Facility) CORF (Comprehensive Outpatient Rehabilitation Facility) Ambulatory surgery center Billing Frequency Repetitive services, such as PT, OT, and SLP, must be billed on a monthly basis and not on a visit by visit basis. Revenue Codes 420 430 440 Physical Therapy Occupational Therapy Speech-language Pathology Primary Diagnosis The primary diagnosis on the claim should be the diagnosis for which the patient is receiving therapy services. Occurrence Codes Occurrence codes and associated dates define a significant event relating to the bill that may affect processing. The following occurrence codes need to be used by all outpatient therapy providers: 11 Date of onset of symptoms or illness which resulted in the patient’s current need for the therapy. This code must be present on all physical, occupational and speech therapy and CORF claims. It should not change during the episode of care unless the patient has a new onset or exacerbation of an illness. 35 44 45 Date of initial PT service at provider Date of initial OT service at provider Date of initial SLP service at provider ORFs also use the following occurrence codes: 17 Date OT treatment plan was established or last reviewed 29 Date PT treatment plan was established or last reviewed 30 Date SLP treatment plan was established or last reviewed Empire Medicare Services Orientation 2000 Page 26 Medicare SNF Billing CORFs use: 28 Date CORF treatment plan was established or last reviewed. Value Codes A value code is a code that relates amounts or values to specific data elements. Right justify the whole number therapy visit amount to the left of the dollar/cents delimiter and zero fill the cents field. The following value codes need to be used when billing therapy services: 50 Number of PT visits from the start of care at the billing provider through the current billing period 51 Number of OT visits from the start of care at the billing provider through the current billing period 52 Number of SLP visits at the billing provider from the start of care through the current billing period EXAMPLE: If the patient had 10 physical therapy visits in the first billing period, and20 physical therapy visits in the second billing period, the cumulative number of physical therapy visits would be 30, this would be shown on the claim as value code: 50 Health Care Financing Administration Common Procedure Coding System (HCPCS) HCPCS codes are comprised of two levels. Level I contains the American Medical Association's (AMA) Physicians' Current Procedural Terminology, Fourth Edition (CPT4) codes. These consist of all numeric codes. Level II contains the codes for physician and non-physician services that are not included in CPT-4, e.g., ambulance, durable medical equipment (DME), orthotics, and prosthetics. These are alpha/numeric codes maintained jointly by the Health Care Financing Administration (HCFA), the Blue Cross and Blue Shield Association (BCBSA), and the Health Insurance Association of America (HIAA). Providers rendering outpatient therapy services are required to submit claims with HCPCS codes for dates of service on or after April 1, 1998. A grace period was allowed until July 1, 1998 dates of service. HCPCS codes for reporting outpatient physical, occupational, and speech therapy include the following: 11040* 29105* 29260 29520* 90911 92598 96110 97012 11041* 29125* 29280 29530* 92506 95831 96111 97014 11042* 29126* 29345* 29540* 92507 95832 96115 97016 11043* 29130* 29365* 29550* 92508 95833 97001 97018 11044* 29131 29405* 29580* 92510 95834 97002 97020 29065* 29200* 29445* 29590* 92525 95851 97003 97022 Empire Medicare Services Orientation 2000 Page 27 Medicare SNF Billing 29075* 29220 29505* 64550 92526 95852 97004 97024 29085 29240 29515* 90901 92597 96105 97010 97026 97028 97036 97116 97150 97504*** 97542 97770 97032 97039 97122** 97250** 97520 97545 97799 97033 97110 97124 97260** 97530 97546 G0169**** 97034 97112 97139 97261** 97535 97703 V5362 97035 97113 97140 97265** 97537 97750 V5363 V5364 *These codes apply in all settings (bill types 12X, 22X, 23X, 74X, and 75X), except hospital outpatient departments (bill types 13X and 83X). When delivered in hospital outpatient settings, these services are not considered rehabilitation services and will not be subject to the outpatient rehabilitation prospective payment system. **1998 codes ***97504 should not be billed with 97116. ****G0169 is a new code for 2000. These codes are the ones commonly utilized for outpatient rehabilitation services. Other codes may be considered for payment if they are determined to be medically necessary and are performed within the scope of practice of the therapist rendering the service. Inclusion of a HCPCS code on this list does not assure coverage of a specific service. Current coverage criteria still apply. SELECTING HCPCS CODES ♦ Use the HCPCS code available that best describes the service rendered. There is not a specific code available for every service, e.g., transfer training. ♦ Use unlisted HCPCS code only when absolutely necessary. A description of what is being billed under the unlisted code must be put in the remarks field of the claim. ♦ HCPCS 97010, 97545, and 97546 are considered bundled charges and should not be billed on Medicare claims. EVALUATIONS Evaluation HCPCS codes are inclusive of all procedures needed to evaluate the patient. Initial evaluations can be billed when there is an expectation that the patient will require covered therapy services. Re-evaluations can be billed when the patient exhibits a demonstrable change in physical functional ability necessitating revised treatment goals. Monthly reevaluations/assessments for a patient undergoing restorative SLP programs are considered part of the treatment session and are not separately billable. Empire Medicare Services Orientation 2000 Page 28 Medicare SNF Billing UNITS OF SERVICE Units of service are based on the number of times the procedure, as defined by the HCPCS code, is performed. ♦ If the HCPCS code has a time definition, the units are based on a multiple of that time factor. If more than one type of treatment is rendered that fit the same HCPCS, add all of the time together for these treatments before figuring units. ♦ If the HCPCS code is not defined by a specific time frame, report one unit. To bill more than one unit there must be a physician order/certification that the therapy session should be rendered more than once daily. It must be reasonable and necessary for the patient’s condition, and it must be reflected on the plan of treatment. ♦ Only whole numbers are used for units. EXAMPLES A. A patient receives OT, HCPCS code 97530 for 60 minutes. 97530 is therapeutic activities, direct (one on one) patient contact by the provider (use of dynamic activities to improve functional performance) each 15 minutes REPORT: 430 Revenue Code 97530 HCPCS/Rate 4 Service Unit B. A patient receives ST, HCPCS code 92526 for 30 minutes. 92526 is treatment of swallowing dysfunction and/or oral function for feeding REPORT: 440 Revenue Code 92526 HCPCS/Rate 1 Service Unit C. A patient receives PT, HCPCS code 97116 for 10 minutes. 97116 is therapeutic procedure, one or more areas, each 15 minute gait training (includes stair climbing) REPORT: 420 Revenue Code 97116 HCPCS/Rate 1 Service Unit CPT codes and descriptions only are copyright 1998 American Medical Association (or such other date publication of CPT). Line Item Dates of Service Line item dates of service must be reported beginning with services provided on October 1, 1998. Empire Medicare Services Orientation 2000 Page 29 Medicare SNF Billing Discipline Specific Modifiers Providers are required to report the following modifiers to distinguish the type of therapist who performed the outpatient rehabilitation service. If the service was not delivered by a therapist, then the discipline of the plan of treatment under which the service is delivered should be reported. Modifiers are added to the end of the HCPCS code. GN GO GP EXAMPLE: Speech-language pathologist or under SLP plan of treatment Occupational therapist or under OT plan of treatment Physical therapist or under PT plan of treatment Therapeutic activities rendered by a Certified Occupational Therapist Assistant (COTA) would be billed: 430 97530GO Billing for Prior Dates of Service DATES OF SERVICE 10/01/97 THROUGH 4/01/98 – HOSPITALS ONLY Beginning with dates of 10/01/97, hospitals were required to use HCPCS codes for outpatient physical and occupational therapy services. The following HCPCS codes were used. PT Evaluation PT Re-evaluation PT Treatments OT Evaluation OT Re-evaluation OT Treatments Q0103 for dates of service 10/01/97 – 12/31/97 97001 for dates of service beginning 1/1/98 Q0104 for dates of service 10/01/97 – 12/31/97 97002 for dates of service beginning 1/01/98 97010 – 97799 Q0109 for dates of service 10/01/97 – 12/31/97 97003 for dates of service beginning 1/1/98 Q0110 for dates of service 10/01/97 – 12/31/97 97004 for dates of service beginning 1/01/98 97010 – 97799 Units of service: Each HCPCS code was counted as one unit per day regardless of the length of time performed or time element in the HCPCS description. DATES OF SERVICE PRIOR TO 4/01/98 (PRIOR TO 10/01/97 FOR HOSPITALS) Prior to 10/01/97 for hospitals and prior to 4/01/98 for SNF, ORF, and CORF, therapy was billed on a visit basis. Under this system, each therapy visit was counted as one unit no matter how many treatments were done during that visit. No HCPCS codes were required. Empire Medicare Services Orientation 2000 Page 30 Medicare SNF Billing Notes Empire Medicare Services Orientation 2000