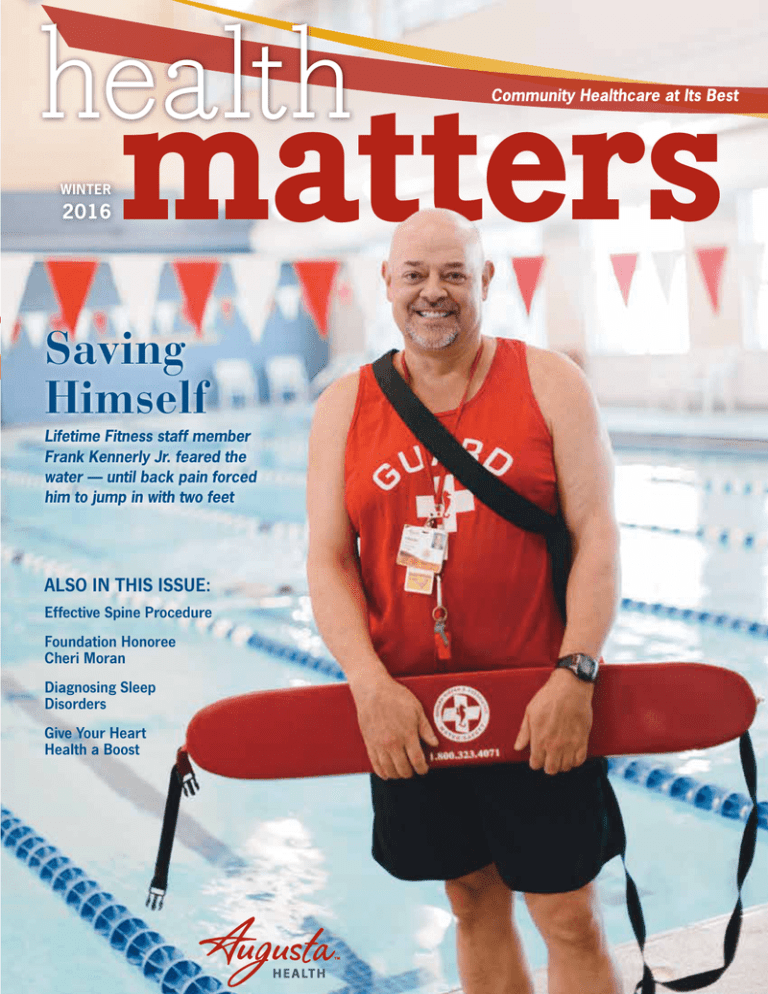
health
WINTER
2016
matters
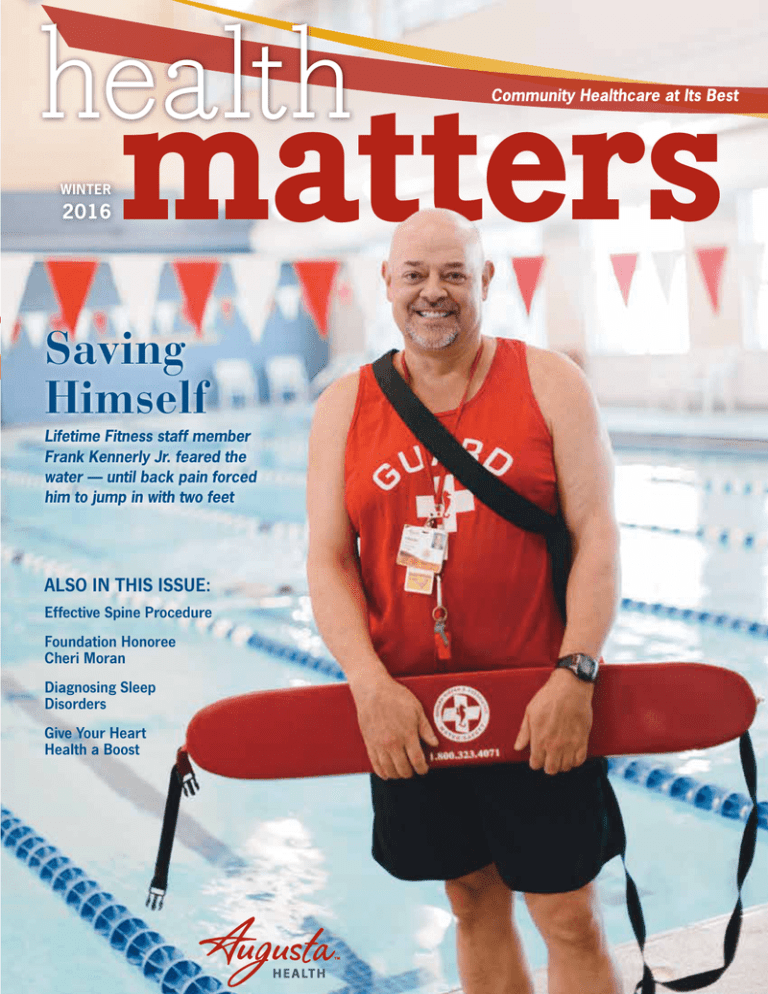
Saving
Himself
Lifetime Fitness staff member
Frank Kennerly Jr. feared the
water — until back pain forced
him to jump in with two feet
ALSO IN THIS ISSUE:
Effective Spine Procedure
Foundation Honoree
Cheri Moran
Diagnosing Sleep
Disorders
Give Your Heart
Health a Boost
Taking the
Lead
The Magazine of Augusta Health
Serving Staunton, Waynesboro and Augusta counties and surrounding communities
Augusta Health Board of Directors
Rev. John C. Peterson, Chairman
Mind-Body Connections
Happy winter! This season may not be most people’s favorite, but it
does offer an opportunity to do activities you wouldn’t do at other times
of the year. More calming and cerebral ones, such as reading and
cooking (check out two delicious recipes on pages 25 and 26), are
a great way to pass the time when the weather isn’t inviting.
Of course, if you are an outdoorsy individual, you may just want to get
out and brave the cold temperatures or wet and snowy conditions for
a brisk walk anyway.
Taking care of ourselves mentally and physically is actually one of the
main topics in this issue. Our Apple a Day section is devoted to heart
health. And protecting this key organ requires tending to our bodies
as well as our minds. It is important to stay trim and active and relieve
stress so that we do not put added pressure on our hearts. It is also
widely misunderstood that men are more at risk of heart attack than
women. However, we explain in this article how the signs of heart
attack are a bit different for women.
There is a lot more in store for you this winter issue. We offer a
glimpse of the many unique services and programs available at
Augusta Health, such as industrial therapy, a program that seeks to
help prevent and manage workplace injuries. And the Pain Management Clinic helps people living with chronic and acute pain. If you have
a sleep issue (and nearly 70 million Americans do), you may want to
consider contacting Augusta Health’s Sleep Center, which diagnoses
a range of problems through sleep studies.
As usual, people’s stories provide some of the best reading. Catherine
Radford, an avid bowler, was back at the lanes only two months after
a new spine procedure, known as XLIF. And our cover story subject,
Frank Kennerly Jr., one of our water safety instructors, inspires us to
conquer our fears. Also in this issue, we are proud to recognize Cheri
Moran, board chair of the Augusta Health Foundation, who received
the Spirit of Philanthropy award. Once you read this story on pages
14–15, you’ll know why.
In the spirit of good health, I wish you plenty of mental and physical
well-being, self-discovery and gratitude this winter!
Victor M. Santos, Vice-Chairman
Mary N. Mannix, President
William L. Pfost, Secretary and Treasurer
Charles “Mick” Andersen, MD
Beverly “Cheri” S. Moran
Debra S. Callison
A. Whit Morriss, MD
E. Stuart Crow
Burnie Powers
John B. Davis
Joseph L. Ranzini, MD
Laurel L. Landes
Arona E. Richard
John “Rob” O. Marsh, MD
Participating, Non-Voting Members:
Buckley Gillock, MD MS President
Eric Laser, MD MS President-Elect
Augusta Health Hospital Staff
President and CEO Mary Mannix, FACHE
Chief Information Officer Mike Canfield
Chief Nursing Officer Marvella Rea
Chief Operating Officer Lisa Cline
President AMG Karen Clark
V.P. Finance Robert Riley
V.P. Fund Development Tami Radecke
V.P. Human Resources Dan O’Connor
V.P. Legal Affairs Alex Brown
V.P. Medical Affairs, AMG Scott Just, MD
V.P. Planning and Development Kathleen Heatwole
Augusta Health Marketing Department
For more information or questions about services at Augusta Health, visit
our website at augustahealth.com.
Health Matters is published by the Augusta Health Marketing
Department, 64 Sports Medicine Drive, Fishersville, VA 22939.
All rights reserved.
The information contained herein is not a substitute for professional medical
care or advice. If you have medical concerns, seek the guidance of a healthcare
professional. Health Matters is aimed at connecting the community with
healthcare experts within Augusta Health to learn more about issues that
may be affecting your health.
If you are not receiving Health Matters, you can view it or request to be added
to the mailing list at augustahealth.com/health-matters.
Editor/Director of Marketing Vicki Kirby
Mary N. Mannix, FACHE
President and Chief Executive Officer
Augusta Health
2
HEALTH MATTERS Winter 2016
Web Developer/Marketing Asst. Brian McGill
contents
winter 2016
17
screening matters
3-D mammography is available at several locations
Around Augusta
4
News and tips from your community hospital
The Doctor Is In
6
Your health questions answered
spine matters
8
XLIF spine procedure quickens recovery time
lung matters
10
Understanding two chest specialities
pain matters
11
Pain Management Clinic addresses acute, chronic pain
foundation matters
14
Celebrating board chair Cheri Moran
palliative care matters
18
Hospice is just one type of palliative care
sleep matters
19
Sleep Center diagnoses, treats sleep-related problems
apple a day
21
Change your lifestyle, improve your heart health
Happenings
27
Classes and groups at Augusta Health
Day in the Life
Lifetime Fitness water safety instructor Frank Kennerly Jr.
31
12
therapy
matters
Industrial Therapy
program aims
to prevent workrelated injuries
around Augusta
news and tips from your
community hospital
Go Girls!
Wellness and fitness group for adolescent girls emphasizes positive body image
Starting in the fall of 2014, Augusta Health partnered with the
University of Virginia Children’s Hospital to offer the Go Girls!
program for girls in the Shenandoah Valley. The weekly class is
held at the Waynesboro Family YMCA and focuses on both exercise
and overall wellness.
The main goal is to provide a fun place for girls and their families
to exercise and learn about wellness together, explains Kara Meeks,
RS, RD, CDE, Augusta Health’s community liaison. “It’s fun and it
is accessible to everyone since it’s free of charge,” she says.
girls for PCOS, realized the girls didn’t have access or opportunities
to exercise. She decided to become certified in Zumba and hold
classes after work.
The Waynesboro classes usually consist of 35–45 minutes of
exercise, such as dance and yoga; the remaining time is spent
discussing topics related to wellness, such as health, nutrition,
body image, self-esteem and personal safety. Volunteers have
spoken about seasonal foods and local produce, puberty, careers
in health sciences, how to make healthier snacks, exercise habits,
etc. The average age of the participants is 12½ years old, and class
size varies each week, ranging from 10 to 20 girls. Female family
members and friends of the girls are also welcome to participate.
PCOS
Christine Burt-Solorzano, MD, of the pediatric endocrinology division
at the UVA Children’s Hospital, spearheaded the program, which
is part of a UVA study partially funded by the National Institutes of
“Each week, we aim to provide a variety of exercise options as well
Health – Eunice Kennedy Shriver National Institute of Child Health
as education topics so that the girls have something different to look
and Human Development. Physical activity is one of the best treatforward to,” says Meeks. “I think the biggest thing I have seen with
ments for polycystic ovarian syndrome (PCOS), a hormonal disorder the girls is a change in their attitude toward physical activity and in
that can affect reproductive health. Dr. Burt-Solorzano, who treats
their self-image.”
Call Kara Meeks at (540) 932-4191
to learn more about Go Girls!
4
HEALTH MATTERS Winter 2016
Top Teacher
VCOM students honor William Faulkenberry, MD
This past November, the medical
students of Edward Via College
of Osteopathic Medicine (VCOM)
named William Faulkenberry, MD,
FACS, Preceptor of the Year for the
Augusta region. Every year VCOM
students who work with doctors in
their third year clinical rotations vote
on this award, which is given to one
doctor in each of VCOM’s regions.
Dr. Faulkenberry, a general surgeon practicing at Augusta Health,
William Faulkenberry, MD, FACS,
received a perfect 5.0 rating from
general surgeon
VCOM students and was chosen
from a group of 25 Augusta Health
credentialed preceptors. While Dr. Faulkenberry is proud of this
achievement, he is also modest and gives credit to the Augusta
Health staff who support him. “This is really a group effort,” says
The first-floor renovations
at Augusta Health should
be completed in May.
Dr. Faulkenberry. “It’s not a oneperson operation by any means, and
over the years lots of people have
gifted me with knowledge and teaching, and so this is a way for me to
give back a little bit.”
Beyond the recognition, Dr. Faulkenberry also explained that having students
at the hospital pays dividends because it
causes doctors and staff to learn as well.
“The learning process is two-way,” he says. “The
students ask questions, and I’ll have to look things up to clarify them
in my own mind so I can explain them. We get as much from the students as we give to them. I guess the most important aspect is that
having students here elevates all aspects of the medical staff to do
better and be better. Everything has to be better when you’re teaching.
So the students directly benefit, but so does the whole community.”
Updating Augusta Health
Renovations continue throughout Augusta Health this winter, as the
hospital finds more ways to better serve patients and the community.
The first floor corridor renovations are still under way and should be
completed in May, says Lisa Cline, MSN, MBA, chief operating officer at
Augusta Health. “It is a 14-phase project, and we are on phase seven,”
says Cline. “It’s going really well and looks beautiful.”
The hospital is also starting the design phases of the emergency room
and intensive care unit renovations, expanding the ER by about 12 to
15 beds and the ICU by six beds, says Cline. The ER expansion will take
about two to three years to complete.
Cline adds that the hospital is looking
into renovations to the radiology department later in the year, as well as creating
a corridor from the main lobby to the
Heart and Vascular Center. “Right now
it’s tricky to get to the Heart and Vascular
Center, so we want to make it easier for
patients to get there,” she says.
Renovations to the third floor of the
patient tower are also on track with new
flooring, paint, headboards, and retiled
bathrooms and showers. This project
will be completed at the end of 2016.
Lisa Cline, MSN, MBA, chief
operating officer at Augusta Health.
augustahealth.com5
the doctor is in
QA
What
screenings
indicate
heart
health?
A key factor in preventing heart disease is managing
your risk factors, which can include high blood pressure, high cholesterol or high blood glucose. Here are
key screenings for such risk factors:
Blood Pressure
High blood pressure usually has no symptoms, so
this screening is important for everyone. Your blood
pressure is considered high if it is over 140/90
mmHg, although a new study recently presented at
the American Heart Association suggests that blood
pressure may need to be below 120/80 mmHg —
especially for people with hypertension and/or
diabetes. People with a blood pressure of more
than 120/80 mmHg but less than 140/90 mmHg
should get checked at least every two years starting
at age 20. If your blood pressure is higher, your
doctor may want to check it more often.
Fasting Lipoprotein Profile
(Cholesterol and Triglycerides)
This is a blood test that measures your total cholesterol, LDL (bad) and HDL (good) cholesterol levels; as
well as your triglycerides, an artery-clogging fat. This
test should be done every four to six years starting
at age 20, or more often if your total cholesterol is
considered high — over 200 mg/dL.
Blood Glucose
High blood glucose levels put you at greater risk
of developing prediabetes and type 2 diabetes.
Untreated diabetes can lead to serious health problems, such as heart disease and/or stroke. Blood
glucose should be checked at least every three
years starting at age 45. If you are overweight and
have any additional risk factors, your doctor may
want to check it more often or before you are 45.
Body Weight/Body Mass Index (BMI)
Being obese can increase your chances of high
blood pressure, diabetes, heart disease and stroke.
Your doctor may ask for your waist circumference or
use your body weight to calculate your body mass
index (BMI) during routine visits starting at age 20.
Many people do not have ideal risk levels, and
having higher-than-optimal screening results
does not necessarily mean you will develop
heart disease. Making healthy lifestyle
changes can stop heart disease before
it begins, and screenings are a great
way to help you understand your
risks and motivate you to
put your health first.
Rodney Graber,
MD, FACC, is on
staff at Augusta
Health Cardiology
in Fishersville.
To make an appointment, call
(540) 332-4278 (Staunton) or
(540) 932-4278 (Waynesboro).
6
HEALTH MATTERS Winter 2016
your health questions answered
Q
What is prediabetes?
A
Prediabetes means that your blood glucose levels are higher
than normal but not yet high enough to be diagnosed as type
2 diabetes. Your doctor can run several different tests — such
as the A1C, Fasting Plasma Glucose or Oral Glucose Tolerance
Test (OGTT) — to determine if your blood sugar levels are high
enough to be considered prediabetic. Results indicating prediabetes are: an A1C of 5.7–6.4 percent; fasting blood glucose
of 100–125 mg/dL; or an OGTT two-hour blood glucose of
140–199 mg/dl.
According to the American Diabetes Association, there are no
clear signs or symptoms of prediabetes, so it is possible to
have it and not know it. However, some people with prediabetes may have symptoms of diabetes or even problems that
stem from diabetes. Common symptoms of type 2 diabetes
include: frequent urination; extreme thirst or hunger, even
while you are eating; fatigue; blurry vision; cuts or bruises that
are slow to heal; and tingling, pain or numbness in the hands
or feet. Problems from diabetes can include skin, foot and eye
complications; kidney disease; and high blood pressure that
can lead to stroke.
People diagnosed with prediabetes have a higher risk for
developing type 2 diabetes and cardiovascular disease. As
diabetes is a progressive disease, it is a lot easier to prevent
diabetes complications when you address these problems
early in the process, and not when the disease has already
developed. When diabetes is diagnosed, there is evidence
to suggest that one has already lost half of his or her insulinproducing pancreas cells. Prediabetes is a warning sign to tell
people that the disease process is on the way and significant
changes need to be made as far as diet, weight loss and exercise, to prevent diabetes from developing. Consult your doctor if you are concerned about having
prediabetes or have symptoms of type 2 diabetes. Ask for a
blood glucose screening if you have certain risk factors, such
as being overweight, with a body mass index above 25; being
inactive; having a family history of type 2 diabetes; or having
high blood pressure or cholesterol.
Nelly Maybee, MD, is on staff at Augusta
Health Diabetes and Endocrinology Clinic.
To make an appointment, call
(540) 245-7180 (Staunton) or
(540) 221-7180 (Waynesboro).
augustahealth.com
7
[spine] matters
not a
moment to
8
HEALTH MATTERS Winter 2016
focus on services
spare
XLIF procedure helps to eliminate
spine-related pain
W
hen Catherine Radford, a 73-yearold bowler from Rockbridge
County, started feeling shooting
pains in her leg so bad that she
could hardly walk, she headed
to Augusta Health. At Augusta
Health she saw Matthew Pollard, MD, director of
the Spine Center. He evaluated her and realized
that she was a candidate for a cutting-edge procedure called eXtreme Lateral Interbody Fusion,
or XLIF.
“XLIF is a new way to approach spinal problems
that allows the patient to avoid many of the downsides of a typical back operation,” says Dr. Pollard.
“There is less pain. It’s a less invasive surgery, with
a quicker recovery.”
Radford found these advantages to be true. “After
the surgery, I did have a little bit of pain from the
surgery [itself], but I didn’t have any pain in my
leg like I did before,” she says. “And they kept me
comfortable. After that I went to physical therapy,
and since I’ve been home I haven’t had any pain
of that type.”
Minimally Invasive
XLIF is a minimally invasive procedure, so rapid
recoveries like Radford’s are typical. Patients
been going ever
“I’ve
since and haven’t had
any pain.”
Catherine Radford
receive the procedure
while lying on their sides,
which differs from traditional open back surgery.
The major back muscles
are preserved. This technique helps reduce time
spent in the hospital and
blood loss during surgery.
Patients are often able
to walk immediately
after surgery.
In Radford’s case, she
was back to bowling
within two months. “I
had my surgery on June
30, and then they transferred me to physical
and occupational
therapy, and then I came home,” she says.
“I started bowling
in the third week of
August, and I’ve been
going ever since and
haven’t had any pain.”
While XLIF is a new
technology, it is widely
established as an
effective procedure.
Dr. Pollard is highly
experienced with the
technique, having
performed the operation over 100 times
since 2009.
Catherine Radford resumed bowling only two
months after undergoing the eXtreme Lateral
Interbody Fusion spine procedure.
Matthew Pollard, MD, is
director of the Augusta Health
Spine Center.
Learn more about the Augusta Health Spine
Clinic at augustahealth.com/spine-clinic.
augustahealth.com9
[lung] matters
focus on services
Breathing Better
W
hat is the difference between a pulmonologist and thoracic surgeon? It is a
common question because both treat the
same area of the body: the chest. However, the one major difference between
them involves surgery. That is to say, thoracic surgeons
perform surgery; pulmonologists don’t.
Pulmonologists are specifically trained in diseases and
conditions of the lungs, such as chronic obstructive
pulmonary disease (COPD), asthma, chronic cough,
shortness of breath and pneumonia, but they do not
perform open surgery. However, the two specialties
work closely together, as a patient is often referred to
a thoracic surgeon by a pulmonologist or a primary
care doctor, notes pulmonologist Jason Lawrence, MD.
Dr. Lawrence offers the example of a patient who has
been treated for pneumonia and still has an abnormal
X-ray. The pulmonologist will do a CT scan and find
that the problem is empyema, pus that accumulates in
between the lungs and inner surface of the chest. The
doctor will then put in a chest tube to drain the area
(pleural drainage). However, if that doesn’t improve,
the pulmonologist will refer the patient to a thoracic
surgeon for further treatment. “We try to do the least
invasive means first,” says Dr. Lawrence.
Pulmonology Procedures
Pulmonologists perform minimally invasive procedures,
including: a bronchoscopy with transbronchial biopsy, a
procedure in which a bronchoscope is inserted through
the nose or mouth to collect several pieces of lung tissue;
and an endobronchial ultrasound (EBUS), which is used
to diagnose lung cancer, infections and other diseases
causing enlarged lymph nodes in the chest.
Thoracic surgeons also commonly assist pulmonologists with video-assisted
thoracoscopic surgery
(VATS), which helps with
lung biopsies for interstitial
lung diseases (ILD) and
treatment of empyema,
explains Dr. Lawrence. Pulmonologists try to diagnose
and care for all forms of lung
conditions with the most
minimally invasive treatments; however, if surgery is
necessary, thoracic surgeons
are the best option. Thoracic
Jason Lawrence, MD, is
surgeons perform various
on staff at Augusta Health
surgeries, except for cardiac
surgery, in the chest area.
Pulmonology.
10
HEALTH MATTERS Winter 2016
Pulmonologists, thoracic
surgeons treat different
chest issues
The one major difference
between them involves surgery.
That is to say, thoracic surgeons
perform it; pulmonologists don’t.
[pain] matters
focus on services
Pain,
Pain
Go
Away
Pain Management Clinic helps patients deal with
back pain and more
B
ack pain is an extremely common problem across the United
States. In fact, it will affect 8 out of 10 people at some point in
their lives, according to the National Institutes of Health. The
physicians in Augusta Health’s Pain Management Clinic see this
firsthand with the patients that come in for treatment.
“We see all kinds of chronic and acute pain,”
says Jared Davis, MD, physician at the Augusta
Health Pain Management Clinic. “But the most
common is back pain and lower back pain. Back
pain is something that most people will experience, and we want them to be able to manage
that pain before it becomes something that’s
chronic and affects their ability to live their lives.”
Dr. Davis and the other physicians in the Pain
Management Clinic take an interventional
approach to pain management, which means
they treat pain comprehensively, rather than
focusing on just the pain itself.
Jared Davis, MD, is on staff
at Augusta Health Pain
Management Clinic.
“A multidisciplinary approach to pain management is very important because pain really affects
multiple parts of the patient,” says Dr. Davis. “We’re not focused on just
treating physical symptoms but also on other types of treatment, whether it’s
the treatment of the actual underlying problem or the psychological impact
of pain on people’s lives. It’s a multifaceted approach, and we work with
other services such as orthopedics, physical therapy, psychiatry [and others].”
The Pain Management Clinic at Augusta Health is equipped to treat all
kinds of pain issues, from what Dr. Davis calls the “bread and butter
pain procedures” to more advanced treatments such as neuromodulation — which is a spinal cord stimulation therapy to help treat pain — and
radiofrequency ablations — which can be used to cauterize nerve endings
that may be contributing to pain.
“Technology has been advancing, and we have the latest techniques and equipment,” says Dr. Davis. “It’s really cool to be a part of a community hospital that
has access to these options that usually only bigger institutions have access to.”
Pain Pro
To help serve even more patients in the Pain Management Clinic, Augusta Health recently brought
Ruzbeh Toussi, DO, MPH, on board. Dr. Toussi comes to Augusta Health from UVA, where he
recently finished a pain training fellowship. Although he hasn’t been on the staff long, he’s already
becoming an important part of the multidisciplinary pain management team at the hospital.
“Everyone I’ve been involved with has been great,” says Dr. Toussi. “I think [the multidisciplinary
approach] brings different perspectives together, which is good. For example, both Dr. Davis and
I are anesthesia-trained and we work with a physical therapist, so we have different perspectives
on the treatment of pain and a different eye on the patients’ problems. The more minds working
together to solve a problem, the more successful we are.”
Ruzbeh Toussi,
DO, MPH,
is on staff
at Augusta
Health Pain
Management
Clinic.
augustahealth.com11
[therapy] matters
working
smarter
Program helps companies improve
health and safety
G
Augusta Health
physical therapist
Gail Tarleton.
ail Tarleton has had to crawl through pipes
and go on the rooftops of buildings for work.
And she often has to wear her steel-toed
boots and hard hat. Tarleton doesn’t have the
job you’d expect, however. She is a physical
therapist and board-certified orthopedic clinical specialist
in Augusta Health’s Industrial Therapy program.
Industrial therapy is not new to Augusta Health, but
about three years ago the program began to incorporate
preventive and educational services as well. “We’re going
to the industries in order to prevent injuries rather than
wait for them to happen,” says Tarleton. “Any job that
involves physical tasks could benefit from our services.”
Augusta Health’s Therapy at the Lifetime Center (TLC)
has a team of six physical and occupational therapists
who specialize in the prevention and management of
workplace injuries. Tarleton and the industrial therapy
team perform a number of services out in the field,
working with a variety of companies. One of the main
preventive tasks the team does is a functional job assessment, which requires them to evaluate the essential
actions of a job. This process involves taking detailed
measurements of how often employees are lifting, pushing, pulling, gripping and bending, and how much weight
is involved with these tasks. They also look at how long
employees sit, stand and move in a workday. This report
equally helps the company and employees.
going to the indus“We’re
tries in order to prevent
injuries rather than waiting for them to happen.”
Gail Tarleton, physical therapist and orthopedic clinical specialist
12
HEALTH MATTERS Winter 2016
focus on services
“We’re coming in with a different set of eyes,” says
Tarleton. For instance, the team worked with a manufacturing company that had a problem area moving
large, heavy sheets of metal from an upright, stacked
position to the machine to be cut. Thanks to recommendations from the team, the company was able to
eliminate a whole step in the process, which reduced
the risk of injuries and saved time as well.
Gail Tarleton performs a
functional job assessment
to evaluate the essential
actions of a job.
Ergonomic Assessments
The team also regularly visits offices to complete workstation ergonomic assessments, which help employees
set up their desks to prevent repetitive motion injuries.
Studies show that people who sit at a desk most of the
day commonly suffer from neck and back pain and musculoskeletal injuries, including carpal tunnel syndrome.
One of the best things to do is take “active breaks,”
explains Tarleton. “We tell people to get out of their
chair every 40 minutes and stretch or walk around.”
Another new part of the Industrial Therapy program
focuses on education. In addition to assessments, the
team gives safety talks and assists with setting up a company’s wellness program. Both target injury prevention
and creating a healthier and safer work environment.
“That’s what we really want to do,” says Tarleton.
“Trying to figure out where injuries could happen and
educating people and making safety a priority in the
industry will cut back the healthcare expenses down
the road.”
Program Offerings
Here is a list of all the services provided in
the Industrial Therapy program.
Preventive Services Functional Job Assessments: Industrial therapists go into a business and assess
each essential function of the job. They
take detailed measurements of how often
employees are lifting, pushing, pulling, gripping and bending, and how much weight is
involved with these tasks. They also look at
how long employees sit, stand and move in a
workday. This information is helpful in hiring
employees, helping employees return to work,
communicating with doctors and complying
with The Americans with Disability Act (ADA). Post-Offer Screen: This is a functional
test industrial therapists can carry out to
see if an employee is able to carry out the
essential functions of that job. It is done
after an employee is offered a job, similar
to a drug screen.
If you have interest in industrial therapy services, contact
Therapy at the Lifetime Center (TLC) at (540) 332-5935 and
ask to speak with one of our physical or occupational therapists on the industrial therapy team. Also, learn more about
therapy services at augustahealth.com/therapy.
Ergonomic Assessment: This is an
assessment of a specific area of concern
at a plant or in a company. Industrial
therapists will assess the employees doing
the job to see if a safer alternative is available. Ergonomic assessments also include
the evaluation of computer workstations.
Safety Education Program: This
can be custom-designed based on a
company’s needs. Some typical topics
include: preventing back injuries, preventing repetitive motion injuries, ergonomics
with computer use, etc. Assist With Wellness Program: The
Affordable Care Act is providing incentives
for companies that set up “health-contingent wellness programs.” Augusta Health’s
Industrial Therapy program team can help
with their creation and installment.
Rehabilitation Services After
Work-Related Injuries
Traditional Physical and Occupational Therapy: After a physician refers
an injured worker to therapy, industrial
therapists provide evidence-based treatments
to help the worker heal and return to work
safely. This primarily consists of individualized and specific exercises and manual
therapy. Therapists communicate closely
with parties involved in the workers’ compensation process.
Work Conditioning: This service helps
injured patients with a safe return to work
by incorporating strength, flexibility and
endurance exercises with work-specific
tasks as proper body mechanics are taught.
Functional Capacity Assessment:
This is used when an injured worker has
reached maximal medical gains and industrial therapists are trying to answer the
question, “What is this person’s capacity
for work?” It is an in-depth, six-hour, twoday assessment.
augustahealth.com13
[foundation] matters
do-g oder
Award recognizes Augusta Health Foundation
board chair Cheri Moran
M
aking a brand-new nonprofit foundation successful
takes leadership, passion and commitment. Sounds
like the perfect description for Cheri Moran.
As board chair for the Augusta Health Foundation,
Moran not only has helped to create a strong team of
directors, but she also has contributed her formidable experience with
other boards — allowing the Foundation to end its first year with an
impressive $500,000 in donations. Those funds go directly to programs
that support chronic disease education, mental health counseling,
music therapy, Camp Dragonfly and hospice care for those who would
otherwise struggle to afford it.
Because of her efforts, late last year Moran received the Spirit of
Philanthropy award from the Shenandoah Chapter of the Association
of Fundraising Professionals. “She has made an incredible difference
to Augusta Health and to the greater community,” says Tami Radecke,
executive director of the Foundation. “Cheri was willing to step up
and be the inaugural chair of the board, and that’s no easy task. A
large part of our success can be directly attributed to her leadership.”
Lifetime of Giving
In many ways, contributing her time and insights has always been part
of Moran’s life. After moving to the Shenandoah Valley with her husband 40 years ago, she joined the Kiwanis Club, then the Blue Ridge
Community College Education Board. She remembers listening to a
single mother of three talk about completing her education because of
a scholarship provided through board efforts. “I guess I got bit by the
philanthropy bug after that,” Moran says. “I began to see what it’s like
to make a difference and change the lives of people in the community.”
Joining the Augusta Health Foundation board stemmed from her
commitment to give back to the community. “The board serves as
advocates for patients and staff; we make sure that the activities of
the Foundation fit its mission,” she says. Making sure that those in the
area have access to health resources — or even to transportation for
medical treatments — is a priority for everyone at Augusta Health,
she notes.
14
HEALTH MATTERS Winter 2016
Tami Radecke,
executive
director of the
Augusta Health
Foundation,
left, with
honoree Cheri
Moran, board
chair of the
Foundation.
Quilts of Comfort Auction
One major initiative that benefits the Augusta Health
Foundation is the Quilts of Comfort auction, which was
held on Nov. 7, 2015, at Augusta Expo in Fishersville.
Bringing together about 200 participants and dozens
of quilters, the event was hugely successful, says Lori
Showalter, chair of the event.
Previous Quilts of Comfort auctions were held in April,
but last year, organizers wanted to recognize November as National Hospice Month and also encourage
people to give quilts as holiday gifts. More than 50
quilts were featured in a live auction, with smaller
handmade items showcased in a silent auction. The
highest price paid for a quilt was $3,500 — and overall,
the event brought in just over $34,000.
The funds benefit one of the Foundation’s top priorities: the Shenandoah House Gifted Care Program,
which helps to cover room and board expenses for
those in hospice who would not be able to afford
care otherwise.
“To see people come together for this was amazing,”
says Showalter. “From the quilters who donated the
materials and their talents to the people who bid as
a way to support the program, it felt like such a community effort. It was an incredible event, and we can’t
wait to do it again next year.”
focus on services
In her career,
working for
Union Bank
and Trust, Moran
encourages employees to support local
nonprofits and enjoys
the community focus of the
bank. That pairing of personal
and professional endeavors highlights
the passion that Moran brings to every task,
whether it’s leading a discussion about emergency room
needs or hearing from recipients of grants from the Cancer Bridge Fund,
which offers services and supplies to those affected by the disease.
“For a foundation to be beneficial, particularly in its first year, it
requires deep involvement from its board members and staff,” says
Moran. “It’s very exciting to be able to see community needs being
met because of the teamwork and philanthropy displayed by every
single person involved here. It’s a wonderful board and a fantastic
organization, and I feel proud and honored to be part of it.”
To learn more about or make a gift to the
Augusta Health Foundation, visit augustahealth.
com/Foundation, call (540) 332-5174 or
email ahfoundation@augustahealth.com.
augustahealth.com15
[cancer] matters
focus on services
Comprehensive
Cancer Care
Augusta Health Cancer Center offers
person-centered care
T
he Augusta Health Cancer Center, a Duke Health Affiliate
and one of the leading cancer centers in west central Virginia,
uses a holistic approach. “We don’t just treat the disease; we
get to know, understand and address the needs of the whole
person,” explains Rob Kyler, MD, radiation oncologist.
A wide range of comprehensive support services, cutting-edge technology and treatment options are all conveniently clustered together in one
location and under one roof for easy access. A radiation oncology and
general oncology/hematology practice, located within the center, provides care management for all solid tumors and blood disorders. Whether
you have breast, lung, gastrointestinal or prostate cancer or lymphoma,
or less common cancers like ovarian or melanoma, a compassionate and
experienced team is ready to deliver high-quality, patient-centered care.
Resources
The Cancer Center offers the following:
• Expert and Knowledgeable Physicians: Three board-certified
oncologists/hematologists and two board-certified radiation oncologists. A Symptom Management Clinic with same-day drop-in
urgent care availability is embedded within the oncology practice.
• State-of-the-Art Technology: Equipment including intensitymodulated, image-guided and dynamic arc radiation therapy; CT
simulation and 4-D computerized treatment planning; and programmable smart infusion pumps.
• Clinical Competence: Nurses with a combined 345 years of experience and who are validated by the Oncology Nursing Society.
They have the background and the training to administer all types
of therapeutics including chemotherapy, biological and targeted
therapy, antibiotics, nausea therapy and blood products.
• Optimal Access: An Infusion Center open 365 days of the year,
seven days a week. There is an on-site Infusion pharmacy for faster
dispensing turn-around times and ample space with 21 infusion bays.
• Multitude of Supportive Services: A full-time social worker to
help connect you and your family with the best local and national
resources; a financial counselor to assist with understanding your
insurance coverage as well as medication assistance programs; an
oncology dietitian for your nutritional needs; and two full-time
patient navigators who serve as a primary point of contact to
answer your questions and guide you through the medical maze.
16
HEALTH MATTERS Winter 2016
Cancer Patient and Family
Advisory Council
The Augusta Health Cancer Patient and Family Advisory Council began in May 2015 as a way to enhance
services. It provides “a patient voice” and acts as
a “sounding board” to the Cancer Center, and also
strengthens communication between patients and
caregivers. It comprises current and former patients,
family members and staff, according to Krystal Moyers,
MEd, CHES, health educator, Community Outreach.
“We gain insight from them on existing and potential
services, new procedures or processes, and new
equipment,” Moyers says. “It could be small or large in
scope; our last meeting was about the wearable home
ambulatory infusion pumps. The hospital has been
going through a lot of construction, so we get feedback
on that as well.”
Another large part of discussion during meetings has
been spiritual care and emotional support services,
Moyers says. “It wasn’t necessarily that we had a lack
of them, but how we could better inform our patients
that they existed,” she says. “We’re working on better
directional signage, as well as talking with construction
managers to update the chapel into a more modern
space to be used for prayer, meditation and quiet
reflection for patients and families, no matter what
their belief systems.”
Members have different reasons for joining, but they all
have expressed wanting to help others throughout their
journeys with cancer. “This was a really vulnerable and
traumatic part of their lives, and now they want to give
back, which I think is really amazing,” Moyers says.
Learn more about the Augusta Health Cancer
Center at augustahealth.com/cancer-center.
[screening] matters
focus on services
A Picture of
Health
3-D mammography available at Augusta Health Women’s
Imaging Center, Stuarts Draft Outpatient Center
T
The improved
images
from digital
mammograms
may reduce
the need for
callbacks. The
unit’s different
compression
paddles also
seem to be
easier on
patients’
comfort levels.
he Women’s Imaging Center at Augusta Health has always offered state-ofthe-art care for patients in the Shenandoah Valley area and has continued
to do so by expanding its digital mammography program. 3-D mammograms
are now available at its new urgent care clinic and outpatient center in
nearby Stuarts Draft, which opened in May 2015.
Augusta Health started performing 3-D mammograms, also known as breast tomosynthesis, in July 2014. The 3-D mammogram is similar to a traditional 2-D mammogram,
explains Amy Patterson, a breast sonographer at Augusta Health. The main benefit
to 3-D is that it creates a layered image that allows for more detail to be seen by the
radiologist. The improved images from these mammograms may reduce the need for
callbacks. The unit’s different compression paddles also seem to be easier on patients’
comfort levels, notes Patterson.
3-D is the newest addition to Augusta Health’s digital mammography program,
which started in 2007. Augusta Health has always made it a priority to offer its
patients the most advanced forms of treatment and diagnosis, which is why it is
important to make the latest technology in digital imaging mammography available,
Patterson says. “It provides a benefit to our patients who we care about deeply, and
we want to offer the best possible exam in order for them to receive the best care,”
she says.
Amy Patterson is a breast
sonographer at Augusta Health.
For more information about Augusta
Health’s digital mammography program, visit augustahealth.com/
womens-imaging.
augustahealth.com17
[palliative care] matters
focus on services
Soothing
Services
Hospice and palliative care are not one and
the same, explains Patrick Baroco, MD
W
hile the term
palliative
care — which
refers to medical care focused
on relieving the
pain and symptoms of people
with serious illnesses — is often
confused with hospice care, hospice is actually just one type of
palliative care.
“I prefer to think about [the
distinction] as between hospice
and non-hospice palliative
care,” says Patrick Baroco, MD,
medical director of Hospice of
the Shenandoah and director
of palliative care at Augusta
Health. “Non-hospice palliative care is appropriate for
people of any age and illness,
including when they’re receiving curative treatment. Over
time, for some patients, care
will become more palliative
[rather than curative] because
we have fewer options to treat
the disease itself. When they
get to the point where they’re
only receiving palliative care,
that’s a hospice situation.”
Because Augusta Health has
this continuum, when patients
move from non-hospice
18
HEALTH MATTERS Winter 2016
palliative care to hospice palliative care, the transition is more comfortable.
“It’s important to me as a physician that I have
an established relationship with the patient,” Dr.
Baroco says. “They know me, they know we have
a plan of care, and they know in advance what, if
anything, changes when we move to hospice, so
bringing in the hospice team is not as scary.”
Both hospice and non-hospice palliative care
bring a “team” approach to the care of patients
with serious medical illness, recognizing that these
patients have medical needs as well as social, spiritual and emotional needs. To address this, both
hospice and non-hospice palliative care provide
a team of physicians and advanced-practice providers, nurses, social workers and a chaplain.
“We know that a patient with, say, cancer, isn’t only
dealing with that cancer, they’re also dealing with
worries about paying for medical care and about
how their family will be cared for if they don’t survive and other complicated issues,” says Dr. Baroco.
“Our goal is to provide medical care but also make
sure [patients] have access to other resources.” In
this regard, Dr. Baroco describes hospice as “a more
intensive form of care,” with more intensive nursing
care, community volunteers and healthcare aides
added to the team.
Living with a serious medical illness can be
difficult, and Dr. Baroco hopes that his team —
whether it be hospice or non-hospice palliative
care — can lend a hand and make things a bit
easier for patients and families.
A Common Myth
Patrick Baroco, MD, medical director of Hospice of the Shenandoah
and director of palliative care at
Augusta Health, says that one of
the most common misconceptions
about palliative care is that it
means that the doctor is “throwing
in the towel.”
“It certainly doesn’t [mean that],”
he says. “For example, we have
patients who have cancer and
every expectation of a cure; however, at the same time they have
significant nausea or pain and we
help them manage that with palliative care. We’re adding a layer of
support on top of the care patients
are already receiving, not replacing that care.”
Learn more about palliative
care at getpalliativecare.
org. Learn more about
Hospice of the Shenandoah
at augustahealth.com/
hospice.
[sleep] matters
focus on services
Rest Easy
Sleep Center diagnoses, treats
sleep problems
E
veryone suffers from sleep deprivation from time to time.
However, those who experience chronic sleep deficiency
may have a sleep disorder.
Sleep plays a vital role in our physical and mental health
and overall well-being, and a sleep disorder can lead to
short-term and long-term damage. According to the National Institutes of Health, nearly 70 million Americans are affected by chronic
sleep disorders and intermittent sleep problems. The Sleep Center at
Augusta Health diagnoses a range of sleep-related problems through
sleep studies.
One of the most common disorders the center helps treat is sleep
apnea, a condition in which there are frequent disruptions to normal
breathing during sleep. To assist with determining the cause and
proper treatment, a sleep study is usually necessary. A sleep study
measures how well you sleep and “is primarily a tool used to evaluate
breathing problems while sleeping,” says Evan Wenger, MD, director
of the Sleep Center. The center has four private bedrooms that provide patients with a comfortable environment for the overnight study.
A sleep technologist guides patients through the process; patients
wear elastic belts that monitor breathing, as well as additional sensors
that record airflow, blood oxygen levels, sleep stages, eye movement
and leg movements. A home sleep test is also an option depending
on a patient’s specific circumstances.
Positive airway pressure (PAP), which involves a bedside machine
with a ventilator that applies mild air pressure to keep the airways
open, is a common treatment for sleep apnea. There are several
variations of this therapy, and the proper type of PAP therapy is
determined based on a patient’s type of sleep apnea and associated
medical conditions. There are alternatives to PAP therapy for some
patients, such as an oral appliance that typically advances the jaw
forward to maintain an open airway. Surgery is sometimes considered
if other treatment options fail. The treatment plan, however, is based
on a person’s overall health, associated medical conditions and the
type of disorder, explains Dr. Wenger.
Technologists Hazel Moran,
RPSGT, and Daniel C. Sarco,
RPSGT, guide patients through
the sleep study process.
Augusta Health’s Sleep Center is fully
accredited with the American Academy
of Sleep Medicine (AASM). Patients are
not required to have a referral, but Evan
Wenger, MD (right), will evaluate each
consultation request before scheduling
the appointment. The referral form should
be faxed to the Sleep Center with patient
information from the office referring the
patient for a sleep consultation/study.
Treating Sleep Disorders
Besides sleep-related problems, the center provides treatment for
a variety of sleep disorders, such as insomnia, excessive sleepiness,
parasomnias (including sleep walking, talking, acting out dreams, etc.)
and nocturnal leg movements.
Patients as young as 5 can be seen at the center. “Many people in
our community have sleep problems, which impact well-being and
long-term health,” says Dr. Wenger. “Being able to provide treatment,
which improves the quality of life to people in our community, is
important to Augusta Health.”
Learn more about the Sleep Center at
augustahealth.com/sleep-center.
augustahealth.com19
[balance] matters
focus on services
Balanced
Truth
The
Learn how to prevent falls
A
ccording to the Centers for Disease
Control and Prevention, 1 in every
3 adults ages 65 or older falls, and
over 2 million are treated in emergency rooms each year for fallrelated injuries. In fact, falls are
the No. 1 cause of bone fractures, trauma
such as head injury and fatal injury among
older people in the United States.
Fortunately, falling is not
an inevitable part of aging
and can be avoided with
simple and practical lifestyle
adjustments.
Even though falls are so frequent, less
than half of people tell their doctors when
they happen. It is important to alert your
doctor when you experience a fall to determine the cause and to prevent another
one from occurring. Common risk factors
include the following:
Exercise
One way you can help prevent
a fall is to exercise. Leg-strengthening exercises and walking can
benefit your lower body muscles as
well as your bones, which can reduce
the risk of fracture if you do fall. Also try
balance routines such as tai chi to improve your
balance, or find low-cost classes for seniors at your
local hospital or community center. Eating healthy and
getting enough vitamin D — found in foods like fish and
egg yolks; and fortified milk, orange juice and cereals — can
also strengthen your bones.
• Lower body weakness
• Vitamin D deficiency
• Difficulties with walking
and balance
• Use of medicines, such as
tranquilizers, sedatives or
antidepressants
• Vision problems
Talk to Your Doctor
• Foot pain or poor
footwear
Another way to prevent a fall is to discuss your medications and
health with your doctor. He or she can treat you for weak bones,
if needed, and can check to see if any medications you are
taking are making you dizzy or drowsy. Sometimes a combination of medications is causing a problem, and your doctor can
prescribe you something else. It is also important to see your eye
doctor every year to ensure that your glasses or contact lenses
are the right strength and that your vision is healthy.
• Home
hazards or
dangers
Eliminate Hazards at Home
Learn more about
preventing falls at
stopfalls.org.
20
HEALTH MATTERS Winter 2016
Get rid of throw rugs and clutter that can cause you to trip.
Install grab bars and use non-slip mats in the bathroom, and
use curtains and shades that reduce glare from windows. Keep
things you use the most in easy-to-reach places, and make sure
your light bulbs are bright or install extra light fixtures to illuminate hidden hazards. Wear sturdy shoes such as sneakers, even
at home, and make sure they have non-slip soles.
The Heart of It
Engage in these behaviors to improve your cardiac health.
nutrition and fitness
Natural sweeteners
Americans consume too many added sugars (those added to foods or beverages
during processing or preparation). Reducing intake of these can improve our heart
health. Consider reducing your added sugars to no more than approximately
6 teaspoons
9 teaspoons
a day for women and
a day for men, per American Heart Association recommendations.
Weight matters
Being overweight puts strain on your heart and makes
you more prone to heart disease, diabetes and sleep
apnea. How do you know if you are overweight?
A BMI of
30
or higher is considered obese.
Calculate your BMI at calculator.net/
bmi-calculator.html.
Berry good
Eating a variety of fruits and vegetables may help
control your weight and blood pressure. The American Heart Association recommends filling at least
half your plate with fruits and veggies in order
to make it to the recommended 4–5 servings
of each per day. (And all produce, whether
canned, dried, fresh or frozen, counts.)
augustahealth.com21
The cold weather should not keep you from
exercising. See the class schedule for Augusta
Health’s Lifetime Fitness starting on page 27.
22
HEALTH MATTERS Winter 2016
young
stay
at heart
Certain lifestyle changes
can help keep cardiac
disease at bay
W
e need to take better care of our hearts.
Heart disease is the
leading cause of death
among both men and
women in America.
More than 600,000 people die of heart
disease every year. Coronary artery disease (CAD) is the most common type
of heart disease and accounts for over
half of heart disease-related deaths.
Certain risk factors can make us more
susceptible to heart disease. There
are some we can’t change, such as age
and family history of heart disease or
preeclampsia during pregnancy, but
there are several lifestyle risks that we
can change. Almost half of all Americans have at least one of these key risk
factors: high cholesterol, high blood
pressure, unhealthy weight and diet,
diabetes and prediabetes, or tobacco
use. If you have one of these factors
or are at risk for one of these factors, making a few lifestyle changes
can mean the difference between life
and death.
Exercise
Physical activity lowers blood pressure,
reduces LDL “bad” cholesterol and
raises HDL “good” cholesterol. This
can decrease your risk of obesity and
diabetes. The American Heart Association recommends either 150 minutes of moderate exercise per
week or 75 minutes of vigorous exercise per week,
or a combination of both. This might translate to
30 minutes of moderately intense activity five days
a week. If you need to, break up the session into
10-minute intervals. Daily activities such as gardening
and walking the dog also count. Exercise also helps
relieve stress, which can contribute to heart attack
and disease.
What Causes Coronary
Artery Disease?
CAD is caused by a buildup of plaque in the arteries that supply blood to the heart. Plaque is made up of cholesterol, fatty
substances and other materials. Plaque can harden and narrow passage through the artery, or can rupture inside an artery and form
a blood clot on the plaque’s surface. Both scenarios can result in
chest pain, called angina. Stroke or heart attack are a result of the
disrupton of blood and oxygen flow to the heart. More than 700,000
people suffer from heart attacks every year. For three out of four of
them, it is their first heart attack.
continued
augustahealth.com23
Diet
A heart-healthy diet consists of fruits, vegetables and whole grains. Eating low-fat proteins,
such as beans; healthy fats, such as avocados
and nuts; and certain fish can also help lower
your risk for heart disease. Steer clear of foods with saturated and trans fats, and reduce sodium intake. If you find
yourself craving comfort foods, try substituting the highfat ingredients, such as sour cream or butter, for healthier,
low-fat ingredients, like Greek yogurt. If sweets are your
weakness, practice what is known as “two-bite baking”: when
you make cookies, brownies or any other baked good, take
the equivalent of two bites and give the rest away.
Smoking and Drinking
The chemicals in tobacco can damage the arteries in your heart, contributing to the narrowing
of passageways. The carbon monoxide in cigarette smoke also reduces the amount of oxygen
in your blood, which causes your heart to work
a lot harder. This, along with nicotine, raises your blood pressure. Quitting smoking or better yet, never starting, is a good
way to lower your risk of heart disease. Likewise, drinking
too much alcohol can also increase your blood pressure. The
American Heart Association recommends an average of one
to two drinks a day for men and one drink a day for women.
Age and Heredity
While there is nothing you can do to change your age
or family history, knowing everything you can about
your family’s health can help you stay one step ahead
of heart disease. If you don’t know a full history, start
with your immediate family. Find out if your parents, siblings
or grandparents had heart disease or stroke and how old
they were when they developed these diseases. While you are
not guaranteed to have one of these conditions just because
someone in your family did, you are more at risk and can use
the information to make healthy lifestyle choices.
Blood Pressure and Cholesterol
Women and Heart Health
For women, age becomes a risk factor for heart disease at 55
years old. According to the National Heart, Lung and Blood
Institute, women are more apt to develop heart disease after
menopause, and women who have gone through early menopause are twice as likely to develop heart disease as women of
the same age who have not yet gone through menopause. This
is partially due to the decrease of estrogen being produced in
the body.
Symptoms of heart attack can also be different in women
than in men. Heart attack symptoms include:
•Uncomfortable pressure, squeezing, fullness or pain in
the center of your chest that lasts more than a few minutes,
or goes away and comes back.
•Pain or discomfort in one or both arms, the back, neck,
jaw or stomach.
•Shortness of breath, with or without chest discomfort.
•Other signs such as breaking out in a cold sweat, nausea
or lightheadedness.
Many people have risk factors such as high
cholesterol or blood pressure and don’t know
it. Your blood pressure is considered high if it
is over 140/90, although a new study recently
presented at the American Heart Association suggests
that blood pressure may need to be much lower — below
120/80 — especially for people with hypertension. Cholesterol is considered high when it is more than 200 mg/dL.
As with men, the most common heart attack symptom in
women is chest pain or discomfort. However, it is important
to note that women are more likely to experience the other
symptoms, particularly shortness of breath, nausea or
vomiting, and back or jaw pain. Because these symptoms
may seem unusual for a heart attack, women may dismiss
them as the flu, stress or other illness, which can delay
critical action.
It is important to get regular health screenings so you can
take action to prevent or reduce your risk of heart disease,
especially for those with a family history. Screenings include
blood pressure, cholesterol, glucose and body mass index
measurements.
It is important for women
to know the signs of a heart
attack, their family history
and the state of their own
health to protect themselves
from heart disease. If you are
experiencing a symptom or
know of your risk factors, do
not dismiss or ignore them —
take action.
Learn more about screenings for heart disease in
The Doctor Is In on page 6.
24
HEALTH MATTERS Winter 2016
To watch a short film
featuring actress Elizabeth
Banks about heart attack
symptoms in women, visit
goredforwomen.org/
about-heart-disease/
symptoms_of_heart_
disease_in_women/
just-a-little-heart-attack.
Corn Chowder
Ingredients
1 Tbsp vegetable oil
2 Tbsp finely diced celery
2 Tbsp finely diced onion
2 Tbsp finely diced green pepper
1 package (10 oz.) frozen whole-kernel corn
1 cup peeled, diced, raw potatoes, cut into
½-inch squares
1 cup water
¼ tsp salt
Ground black pepper, to taste
¼ tsp paprika
2 cups low-fat (1 percent) or skim milk, divided
2 Tbsp flour
2 Tbsp chopped fresh parsley
Directions
1.Heat oil in a medium-sized sauté pan.
2. Add celery, onion and green pepper and sauté
for two minutes.
3. Add corn, potatoes, water, salt, pepper and paprika.
Bring to a boil; reduce heat to medium; and cook,
covered, for about 10 minutes or until potatoes
are tender.
Yield
4 servings
Calories 186
Total fat 5g
Saturated fat 1g
Cholesterol 5mg
Sodium 205mg
4. Place ½ cup milk in a jar with a tight-fitting lid.
Add flour, close lid and shake vigorously.
5. A dd mixture gradually to cooked vegetables, and
then add remaining milk.
6.Cook, stirring constantly, until mixture comes to
a boil and thickens. Serve garnished with chopped
fresh parsley.
augustahealth.com25
Apple Coffee Cake
Ingredients
5 cups tart apples, cored, peeled
and chopped
1 cup sugar
1 cup dark raisins
½ cup pecans, chopped
¼ cup vegetable oil
2 tsp vanilla
1 egg, beaten
2½ cups sifted all-purpose flour
1½ tsp baking soda
2 tsp ground cinnamon
Directions
1.Preheat oven to 350° F. Lightly oil a 13×9×2-inch pan.
2. In a large mixing bowl, combine apples with
sugar, raisins and pecans; mix well. Let stand for
30 minutes.
3. Stir in oil, vanilla and egg. Sift together flour, baking
soda and cinnamon; stir into apple mixture about
1
⁄3 at a time, stirring just enough to moisten dry
ingredients.
4. Turn batter into pan. Bake 35 to 40 minutes, until
a toothpick inserted in the center of the cake comes
out clean.
5. C
ool cake slightly before serving.
26
HEALTH MATTERS Winter 2016
Yield
20 servings
Calories 188
Total fat 5g
Saturated fat 1g
Cholesterol 11mg
Sodium 68mg
happenings
AUGUSTA HEALTH LIFETIME FITNESS GROUP
CLASSES AND PROGRAMS
Non-members may purchase a 10-class
pass for $100. Classes run on an ongoing
basis. Other classes not listed here can
be found on our website at augustahealth.
com/lifetime-fi
tness. For more information, call Heather Moneymaker, group
fitness coordinator at Lifetime Fitness,
at (540) 332-5571.
Yoga Classes
Mondays, 5:30 p.m.; Tuesdays,
9 a.m.; Thursdays, 9 a.m.; Saturdays,
9:15 a.m.
Multi-Level Yoga: Wednesdays, 9:15 a.m.;
Thursdays, 5:30 p.m.; Fridays, 9:15 a.m.
classes, groups and events at Augusta Health
Les Mills Body Combat
Mondays, 5:30 p.m.; every other
Wednesday, 5:15 a.m.; Wednesdays,
9 a.m.; Thursdays, 4:30 p.m.; Saturdays,
9 a.m.
When:
Martial Arts
Extra fee, class passes excluded.
Beginner: Mondays and Wednesdays,
7–8 p.m.
Intermediate: Mondays and Wednesdays,
8–9 p.m.
Cost: $55 a month for members, $85
for non-members
Basic:
Tai Chi
Free to cancer recovery patients; sponsored by Augusta Health Cancer Center.
Arthritis and Diabetes: Tuesdays, 11:15 a.m.
Beginner: Wednesdays, 11 a.m.
Intermediate: Thursdays, 11:15 a.m.
Multi-Level: Tuesdays, 7 p.m.
Chi Kung
Intermediate: Tuesdays, 10:15 a.m.
Advanced: Thursdays, 10:15 a.m.
Aquatic Classes
Aqua Power: Mondays, Wednesdays and
Fridays, 7:45 a.m.; Tuesdays, 9 a.m.;
Mondays, 4:45 p.m. (Fitness Pool)
Aqua Express: Thursdays, 4:45 p.m.;
Fridays, 7:45 a.m.
Deep Water Conditioning: Mondays
and Thursdays, 9 a.m. (Fitness Pool)
Aqua Boot Camp: Mondays, 5:45 p.m.;
Tuesdays, 7:45 a.m. (Fitness Pool)
Therapeutic/Rehabilitative
Aqua Classes
Mondays, Tuesdays, Thursdays
and Fridays, 9 a.m.; Tuesdays and Thursdays, 10 a.m.; Wednesdays, 4:45 p.m.
(Therapy Pool)
Range of Motion (ROM): Mondays and
Fridays, 10 a.m. (Therapy Pool)
Lipid Panel Screenings
What: Total cholesterol, HDL, LDL, TC/
HDL ratio, triglyceride and glucose levels
are tested. Results can be kept on file and
sent to your physician. This is a great tool
to monitor your health!
Cost: $25 for members, $30 for
non-members
Information and reservations: Call Angela
Kaltenborn, medical fitness coordinator,
at (540) 332-5527, or email her at akaltenborn@augustahealth.com.
RxEX Program — now available
on land or in the water!
What: This monitored medical exercise
program offered at Lifetime Fitness is by
physician referral only. It is an eight-week
exercise program with pre- and postcourse health evaluations. Participants will
exercise twice a week with staff and have
access to Lifetime Fitness throughout the
eight weeks. Outcome measurements will
be sent to the referring physician upon
completion of the program.
Cost: $64 for the RxEX Medical Program
Information: Call Angela Kaltenborn, medical fitness coordinator, at (540) 332-5527,
or email her at akaltenborn@augusta
health.com.
Aqua Lite:
Zumba Dance
When: Mondays, 9:15 a.m.; Tuesdays,
3:45 p.m.; Wednesdays, 5:30 p.m.
TRX Suspension Small
Group Training Class
Tuesdays, 5:15 a.m. (45 min.);
Wednesdays, 12:15 p.m. (45 min.)
and 5:30 p.m. (60 min.); Fridays,
12:15 p.m. (45 min.)
When:
BODYPUMP
When: Mondays, 4:30 p.m;
Thursdays, 9 a.m.
Information: Call Heather
Moneymaker at (540) 3325571 or email her at
RxEX Cancer Program
What: This monitored medical exercise
program at Lifetime Fitness is for members of the community who have had or
currently have cancer. The program is
designed to improve a person’s stamina,
strength and fitness through monitored
exercise. Participants will meet with certified cancer specialists twice a week to be
assisted with an individual workout routine.
Program outcomes will be sent to the
referring physician.
Cost: Call Membership Services at Lifetime Fitness at
(540) 332-5843.
Information: Call Angela
Kaltenborn, medical fitness coordinator, at (540)
332-5527, or email her
at akaltenborn@augusta
health.com.
hmoneymaker@
augustahealth.com.
More classes may
be available.
continued
augustahealth.com27
happenings
RxEX Prehab Program
What: This monitored medical exercise
program at Lifetime Fitness is for members of the community who are scheduled
for joint replacement surgery. The program
is specifically designed to strengthen the
joint during the few weeks prior to surgery.
Participants will meet with exercise
specialists twice a week and work out in
a small group setting of three participants.
Program outcomes will be sent to the referring physician.
Cost: $64 for the RxEX Prehab Program
Information: Call Angela Kaltenborn, medical fitness coordinator, at (540) 332-5527,
or email her at akaltenborn@augusta
health.com.
RxEX Youth Program
What: This monitored medical exercise
program offered at Lifetime Fitness is
for youth in the community 8–12 years
old. The program is designed to improve
your child’s fitness and wellness through
monitored exercise and age-appropriate
nutrition. Your child will meet with an exercise specialist twice a week and work out
in a small group setting of three participants.
Nutrition classes will focus on increasing
awareness about food choices, portion sizes
and healthier options. All participants are
eligible to take part in Fun Friday, an aquatic
hour of fun in the pool. Program outcomes
will be sent to the referring physician.
Cost: $99 for the RxEX Youth Program
Information: Call Angela Kaltenborn, medical fitness coordinator, at (540) 332-5527,
or email her at akaltenborn@augusta
health.com.
RxEX Diabetes Program
This monitored medical exercise program at Lifetime Fitness is for anyone with
prediabetes or diabetes. The program is
designed to strengthen the heart and bones,
improve insulin sensitivity and promote
weight management. Participants will meet
with exercise specialists twice a week and
work out in small group settings of three
participants. Nutrition classes for the RxEX
Diabetes program will focus on intake of
quality carbohydrates as well as nutrition
recommendations while exercising with
diabetes. Program outcomes will be sent
to the referring physician.
Cost: $99 for the RxEX Cancer Program
Information: Call Angela Kaltenborn, medical fitness coordinator, at (540) 332-5527,
or email her at akaltenborn@augusta
health.com.
What:
RxEX Cardiac Program
What: This monitored medical exercise
program is a continuation of Cardiac Rehab
Phase II, and is available to anyone completing or who has completed Cardiac Rehab
within the past 3 months. The focus of the
program is on improving the heart’s function
and increasing cardiovascular endurance.
The participant’s blood pressure, heart rate
and oxygen saturation levels are monitored
throughout the program as necessary, and
a follow-up appointment with Cardiac Rehab
staff is performed upon completion of the
program. Program outcomes will be sent
to the referring physician.
Cost: Call Membership Services at Lifetime
Fitness at (540) 332-5843.
Information: Call Angela Kaltenborn, medical
fitness coordinator, at (540) 332-5527, or
email her at akaltenborn@augustahealth.com.
NUTRITION SERVICES AT LIFETIME FITNESS
Augusta Health Lifetime Fitness is proud
to offer a registered dietitian for
individualized nutrition counseling.
Packages and prices are listed
below and can be scheduled
directly with the registered dietitian.
Energize Package
If you’re only exercising to help shed the
What:
28
HEALTH MATTERS Winter 2016
pounds, you’re
missing half the
picture. Partner
with the dietitian to
learn how modifying
your diet can help you reach a healthier
weight. The program includes personalized
nutrition advice, dietary intake analysis and
body-fat measurements. Package consists
of one 60-minute initial consult with the registered dietitian as well as three 30-minute
follow-ups.
Cost: $150 for members, $175 for
non-members
Information: Call Julia Kearns, registered
dietitian, at (540) 221-7894, or email her
at jkearns@augustahealth.com.
Lifestyle Package
What: This package is designed for nutrition newcomers. If you’re looking to begin
a healthy eating program, start here. The
sessions cover topics including basic nutrition and you, label reading, planning and
prep, and special-occasion eating. Package
consists of one 60-minute initial consult
with the registered dietitian as well as
three 30-minute follow-ups.
Cost: $150 for members, $175 for
non-members
Information: Call Julia Kearns, registered
dietitian, at (540) 221-7894, or email her at
jkearns@augustahealth.com.
Prescription Package
What: Do you have diabetes, heart disease,
high blood pressure or another chronic
condition? Learn how to improve your
well-being through the foods you eat. There
is no physician referral needed! You will
receive personalized nutrition advice and an
individualized dietary intake analysis. Package consists of one 60-minute initial consult
with the registered dietitian as well as three
30-minute follow-ups.
Cost: $150 for members, $175 for nonmembers
Information: Call Julia Kearns, registered
dietitian, at (540) 221-7894, or email her
at jkearns@augustahealth.com.
60 for 60
What: This is a one-time, one-hour session to
discuss your dietary needs. Members get 60
minutes with the dietitian for only $60.
classes, groups and events at Augusta Health
(A slightly higher fee applies to non-members.) Appointment includes a three-day
food recall review, instruction on your calorie
needs, Q&A time and materials to take home.
Cost: $60 for members, $75 for
nonmembers
Information: Call Julia Kearns, registered
dietitian, at (540) 221-7894, or email her
at jkearns@augustahealth.com.
Nutrition Tune-Up
What: This program is designed for clients
who have previously completed any nutrition package or corporate program. The
tune-up provides further guidance and
accountability based upon your goals. The
program includes three 30-minute followup sessions and additional goal setting.
Cost: $90 for members, $100 for
non-members
Information: Call Julia Kearns, registered
dietitian, at (540) 221-7894, or email her
at jkearns@augustahealth.com.
Rising Stars
Learn to play through competitive
drills and games. Beginner and intermediate, ages 11–17.
When: Saturdays, 11 a.m.–12:15 p.m.
Cost: $95.62
What:
Aces
What: Advanced and competitive, ages 12–17.
When: Saturdays, 12:15–1:45 p.m.
Cost: $114.75
Circuit Aces
What: Advanced and competitive, ages 12–17.
When: Tuesdays and Thursdays, 4:30–6 p.m.
Cost: $229.50
Times and fees for tennis classes and programs are subject
to change. For more information, call Chad Reed, tennis
coordinator/pro, at (540) 332-5280 or email creed@
augustahealth.com.
†
SUPPORT GROUPS
AUGUSTA HEALTH LIFETIME FITNESS TENNIS
PROGRAM SCHEDULE†
Adults 1*2*3* Tennis
What: Learn how to play, improve skills
and practice. Ages 18 and older.
When: Thursdays, 6–7:30 p.m.
Cost: $76.50
Adult Cardio Tennis
This “workout” tennis program
is sure to leave you energized. Ages 18
and older.
When: Mondays, 6:15–7:15 p.m.;
Wednesdays, 10:15–11:15 a.m.
Cost: $60
What:
Munchkin Tennis
What: Ages 10 and under, tennis format.
Beginner, ages 4–6.
When: Saturdays, 9–9:45 a.m.
Cost: $57.50
Future Stars
What: Ages 10 and under, tennis format.
Beginner and intermediate, ages 7–10.
When: Saturdays, 9:45–11 a.m.
Cost: $95.62
Friends Listening to Friends Group
What: For newly diagnosed cancer patients who
have fears, questions or concerns. This group
also addresses life after cancer treatments.
When: Tuesdays, 11 a.m.–12:15 p.m.
Where: Augusta Health Cancer Center
Conference Room
Information: For more information about
any cancer group, call Leigh Anderson at
(540) 245-7105.
Shenandoah Valley Stroke Club
What: This support group is for those who
have suffered a stroke and their family
members, care partners and friends.
When: First Friday of every month at noon.
Information: Call Shelley Payne at
(540) 332-4047 or (540) 932-4047.
Celiac Sprue Support Group
What: Group meetings feature free
samples of gluten-free foods, recipes
from support group members, visits
from food-service providers and a
wealth of practical tips.
When: Third Thursday in April, July
and October, 5–7 p.m.
Where: To Be Determined
Information: Call Mary
E. Albert, RD, at (540)
941-2537.
Heart to Heart — Support Group
What: If someone you love has died and
you’d like the “heart-to-heart” support of
others who have also lost someone, we
invite you to attend our support group. We
understand this is a very difficult time in
your life. Talking and sharing with others
going through a similar experience can
provide tremendous support and be
extremely helpful in learning how to cope
and live with your grief. Support groups
are open to the community and provided
free of charge.
When: New groups begin throughout
the year.
Where: Augusta Health Community
Care Building
Information: To find out starting dates
and to learn more, contact Debbie Brown,
bereavement coordinator, Hospice of
the Shenandoah, at (540) 932-4911
or at dbrown@augustahealth.com.
Ostomy Support Group
What: In this group meeting, you’ll share
ideas and improve your quality of life after
ostomy surgery.
When: Second Monday of every
other month, 6–8 p.m.
Where: Augusta Health
Community Care Building,
Room 3
Information: Call (540)
332-4346 for details.
COMMUNITY OUTREACH
AND EDUCATION
Gain Independence From
Tobacco (GIFT): Begin Your
Journey to Stop Smoking/Stop
Using Smokeless Tobacco
What: To quit tobacco, you must first
examine how and why you use tobacco.
Then, you can create an individual quit
plan. The GIFT program is provided by
a Certified Tobacco Treatment Specialist.
Evidence-based guidelines and recommendations are given on an individual basis.
Don’t let fear keep you from quitting.
Information: The next class begins Monday, April 11, at 6–7:30 p.m., in the ACC
building. Call (540) 332-4988 for class
information. If you want to start “quitting” before the next class, the tobacco
treatment specialist provides one-on-one
consultations.
continued
augustahealth.com29
happenings
classes, groups and events
at Augusta Health
Big Squeeze
What: Big
Squeeze is a
free blood pressure screening
and education
program at
communitybased sites.
When: Wednesday,
April 6, 5–6 p.m.
Where: Valley Mission, Staunton
Information: To learn more,
call Krystal Moyers at (540)
932-4976.
Go Girls!
What: Go Girls! is a fitness and wellness support group for girls (ages 7 to
21), which includes exercise and discussion around a wellness topic.
When: Tuesdays, 5 p.m.
Where: Waynesboro Family YMCA
Information: Call Kara Meeks at (540) 932-4191 for more details.
Friends and Family CPR
What: An American Heart Association
course that teaches the basic lifesaving
skills of CPR including hands-only CPR,
child CPR, infant CPR and AED use.
When: May 10, Aug. 4, 5:30–8 p.m.
Where: Augusta Health, ACC Room 3
Information: Free. Registration is required.
Call Krystal Moyers at (540) 932-4976.
new in town
new physicians and health professionals on staff
Marsha Alford, NP
Specialty: Palliative Care/Urgent Care
Augusta Health Palliative Care
Augusta Health Urgent Care
22 North Medical Park Drive
Fishersville, Virginia
(540) 245-7262
Jennifer An, MD
Specialty: OB-GYN
Ob-Gyn Associates Women’s Health
at The Woman’s Center, Fishersville
9 S. Medical Park Drive
Fishersville, Virginia
(540) 332-5577 Staunton
(540) 932-5577 Waynesboro
OB-GYN Associates Women’s Health,
Lexington
130-C Walker Street
Lexington, Virginia
(540) 332-5577 Staunton
(540) 932-5577 Waynesboro
Blake Brown, PA-C
Specialty: Hospitalist
Augusta Health Hospitalists
78 Medical Center Drive
Fishersville, Virginia
(540) 932-4075
Sandra Farnum, NP
Specialty: Urgent Care
Augusta Health Urgent Care
851 Statler Boulevard
Staunton, Virginia
(540) 245-7470
Hospice Volunteer Training — Living
at the End Of Life
What: Are you interested in becoming a
hospice volunteer and making a difference
in the lives of others? Come join us for this
interactive, four-week course in preparation for your journey.
When: Mondays and Thursdays,
5:30–8:30 p.m. Classes begin Feb. 29.
Information: There is no fee for this class.
To register for this course, call (540) 3324904 or visit augustahealth.com/hospice.
This list of new physicians and practitioners at Augusta Health was made possible
by Chris Morgenstern, physician liaison at Augusta Health.
30
HEALTH MATTERS Winter 2016
day in the life
celebrating Augusta Health talent
first time I swam, I did
“The
one length and was exhausted.
But after a year, I worked up
to swimming a mile. I could
hardly believe it.”
Frank Kennerly Jr.
T
wo years ago, Frank
Kennerly Jr. was sitting
in his car outside Augusta
Lifetime Fitness, trying to gather the nerve
to go inside. His doctor
had insisted he try aquatic therapy to
ease chronic lower back pain, but all
Kennerly could think about were the
barriers to recovery: a lifelong fear of
water, being overweight and starting
something new at age 55.
But when he chose to open the car door,
it was like starting a whole new life.
The genuine warmth and friendliness
he encountered from staff members,
such as lifeguard Greg Harris and his
aqua therapist, Amanda, helped to
ease his fears. Even more importantly,
it began to lessen his pain and increase
his motivation. Before long, he moved
from floating to swimming and ditched
a junk food habit so he could have
more energy.
“It took months of daily practice, with
encouragement by all the lifeguards
and other swimmers, but finally, things
seemed to fall into place,” he recalls.
“The first time I swam, I did one length
and was exhausted. But after a year, I
worked up to swimming a mile. I could
hardly believe it.”
By this point, he’d lost 100 pounds, was
a regular at the pool and hadn’t taken
a pain pill in 18 months. One of the
lifeguards suggested Kennerly take
the Red Cross Lifeguard Certification,
and with the same determination he’d
shown with learning to swim, he went
for it and passed on his first attempt.
But Kennerly didn’t stop there. In
January 2015, he joined the Lifetime Fitness team as a water safety
instructor, and he now spends his
days teaching children and adults
to swim and be safe in the water.
Remembering that first day of
aquatic therapy only two years ago,
Staying Afloat
Lifetime Fitness water safety instructor
was once physical therapy patient.
when he almost didn’t get out of
his car, Kennerly is astounded that
he’s now a certified pool operator
and lifeguard. He’s grateful that he
gets to see his mentors and advocates every day at work, and that
he has the chance to inspire others
to change their lives, too.
“There were times I could have given
up, but the folks around me would
not allow that to happen,” he says.
“Now that I have the opportunity to
stand with these excellent individuals, it seems almost incredible. On a
daily basis, I get to serve hundreds of
people who are on their own path to
get better, or maintain their physical and social well-being. It’s truly
an honor.”
Learn more about Augusta Health’s
Lifetime Fitness Center at augusta
health.com/lifetime-fitness or see
the Happenings section in this issue.
augustahealth.com31
Non-Profit Organization
Augusta Hospital Corporation
P.O. Box 1000
Fishersville, VA 22939
US POSTAGE
PAID
Augusta Hospital Corporation
If you are not receiving Health Matters, you can view
it online or request to be added to the mailing list at
augustahealth.com/health-matters.
AUG-014
parking
pass
Augusta Health offers free valet
parking for Emergency Department
Let an Augusta Health valet
park your car when you go to
the Emergency Department.
As of Nov. 30, 2015, Augusta Health now offers valet services
for the community in the Emergency Department. This
service area has a high volume of patient traffic as well as
need. Patients routinely come to the Emergency Department sick, anxious, injured
and in need of assistance quickly. All
valet services at Augusta Health
are free of charge.
Hours of operation for
Emergency Department valet
services are:
Monday–Friday, 11 a.m. to 9 p.m.