Articles
Intracellular MHC class II molecules promote
TLR-triggered innate immune responses by
maintaining activation of the kinase Btk
© 2011 Nature America, Inc. All rights reserved.
Xingguang Liu1, Zhenzhen Zhan1, Dong Li2, Li Xu1, Feng Ma2, Peng Zhang1, Hangping Yao2 & Xuetao Cao1,3
The molecular mechanisms involved in the full activation of innate immunity achieved through Toll-like receptors (TLRs) remain
to be fully elucidated. In addition to their classical antigen-presenting function, major histocompatibility complex (MHC) class II
molecules might mediate reverse signaling. Here we report that deficiency in MHC class II attenuated the TLR-triggered
production of proinflammatory cytokines and type I interferon in macrophages and dendritic cells, which protected mice from
endotoxin shock. Intracellular MHC class II molecules interacted with the tyrosine kinase Btk via the costimulatory molecule
CD40 and maintained Btk activation, but cell surface MHC class II molecules did not. Then, Btk interacted with the adaptor
molecules MyD88 and TRIF and thereby promoted TLR signaling. Therefore, intracellular MHC class II molecules can act as
adaptors, promoting full activation of TLR-triggered innate immune responses.
The ability of the innate immune system to recognize and eliminate
invading microbial pathogens has been largely attributed to Toll-like
receptors (TLRs) and TLR-triggered immune response. TLRs, the
key pattern-recognition receptors expressed on antigen-presenting
cells (APCs) such as macrophages and dendritic cells (DCs), have
important roles in the initiation of innate immune responses as well
as the subsequent induction of adaptive immune responses1. After the
recognition of pathogen-associated molecule patterns, TLRs initiate
shared and distinct signaling pathways by recruiting various combinations of four Toll–interleukin 1 (IL-1) receptor domain–containing
adapters proteins: MyD88, TIRAP (Mal), TRIF and TRAM. These
signaling pathways activate the transcription factors NF-κB and
AP-1, which are common to all TLRs, leading to the production of
inflammatory cytokines and chemokines. TLR3, TLR4, TLR7, TLR8
and TLR9 also activate the transcription factors IRF3 and/or IRF7,
leading to the production of type I interferon2–4. Full activation of
TLRs is essential for initiation of the innate immune response and
enhancement of adaptive immunity to eliminate invading pathogens;
however, TLR signaling is well regulated, positively and negatively, to
prevent inappropriate activation or overactivation, which may cause
autoinflammatory disorders5. So far, various signaling molecules have
been shown to be involved in the tight regulation of the TLR pathway
to maintain the immunological balance4,6. For example, the kinases
MEKK3 (ref. 7) and CaMKII (ref. 8) can be activated by TLR ligands
and then enhance TLR-triggered innate immune responses. However,
the identification of cofactors and their underlying mechanisms for
the initiation and full activation of TLR responses remain to be
fully elucidated.
Major histocompatibility complex (MHC) class II molecules
(encoded by H2) are expressed mainly by professional APCs, including DCs, macrophages and B cells. MHC class II molecules, which
are heterodimers composed of an α-chain and a β-chain, are type I
integral membrane proteins with short cytoplasmic domains and
four large extracellular domains9. Their main function is to present
peptides processed from extracellular proteins to CD4+ helper T cells
and to direct the processes of positive and negative selection, shaping
the repertoire during T cell maturation and lineage commitment10,11.
In addition to that classical function, cell surface MHC class II mol­
ecules can function as receptors to mediate reverse signal transduction after ligation with agonist antibodies, T cell antigen receptors
or CD4 molecules. Engagement of cell surface MHC class II may
regulate cell adhesion, cytokine production and the expression of
costimulatory molecules12–15 and may also induce the apoptosis,
proliferation or differentiation of B cells16,17. Engagement of MHC
class II mainly activates two distinct signal pathways. One increases
cAMP and subsequently induces the translocation of protein kinase C
to the nucleus18,19. Another increases activity of the Src family
tyrosine kinase Lyn and the non-Src family tyrosine kinase Syk.
These activated tyrosine kinases mediate activation of phospholipase
C-γ, leading to the production of inositol-(1,4,5)-trisphosphate and
­diacylglycerol, which mediate calcium mobilization and activation
of protein kinase C20,21.
MHC class II molecules can contribute to the responsiveness of cells
to microbial components, and pathogens have developed ­strategies
to downregulate expression of MHC class II molecules on APCs
and thereby evade immunological surveillance22,23. For example,
1National
Key Laboratory of Medical Immunology & Institute of Immunology, Second Military Medical University, Shanghai, China. 2Institute of Immunology,
Zhejiang University School of Medicine, Hangzhou, China. 3Chinese Academy of Medical Sciences, Beijing, China. Correspondence should be addressed to
X.C. (caoxt@immunol.org).
Received 25 October 2010; accepted 28 February 2011; published online 27 March 2011; doi:10.1038/ni.2015
416
VOLUME 12 NUMBER 5 MAY 2011 nature immunology
Articles
*
0.4
1.0
LPS
PBS
LPS
CpG Poly(I:C)
H2+/+
H2–/–
100
80
60
40
20
0
PBS
*
CpG Poly(I:C)
0 12 24 36 48 60 72
Time after LPS challenge (h)
*
6.0
4.0
2.0
0
PBS
LPS
4.0
3.0
2.0
1.0
0
*
PBS
LPS
IFN-β (ng/ml)
+/+
1.2
H2 chimeras
H2–/– chimeras
*
0.8
0.4
0
PBS
LPS
­ eficiency in MHC class II results in less production of lipopoly­
d
saccharide (LPS)-induced tumor necrosis factor (TNF) by human
peripheral blood monocytes and mouse macrophages24,25. However,
the detailed mechanisms by which MHC class II molecules are involved
in TLR-triggered innate immune responses remain ­uncharacterized.
MHC class II molecules and TLRs are both expressed mainly on
APCs; therefore, we sough to determine whether MHC class II mol­
e­cules have another, nonclassical function and somehow intersect
with the TLR signaling pathway. Here we found that MHC class
II–­deficient mice were more resistant to endotoxin shock induced
by either lethal challenge with LPS or infection with Gram-negative
bacteria, with less production of proinflammatory cytokines and type
I interferon in vivo. Deficiency in MHC class II attenuated the production of proinflammatory cytokines and type I interferon triggered
by TLR4, TLR3 or TLR9 in macrophages and DCs. Furthermore,
intra­cellular MHC class II molecules interacted with the tyrosine
kinase Btk via the costimulatory molecule CD40 in endosomes and
maintained activation of Btk, but cell surface MHC class II molecules
did not. Activated Btk interacted with MyD88 and TRIF, promoting
the activation of MyD88-dependent and TRIF-dependent pathways.
Therefore, intracellular MHC class II molecules are needed to promote the full activation of TLR signaling.
RESULTS
H2 deficiency protects mice from LPS and bacterial challenge
MHC class II–deficient (H2−/−) mice (with a 78.8-kilobase deletion
in H2) and wild-type (H2+/+) littermate mice had similar numbers
of splenic macrophages and DCs, as well as peritoneal macrophages
and bone marrow–derived macrophages and DCs (Supplementary
Fig. 1a,b). Furthermore there were no substantial differences between
H2−/− and H2+/+ mice in the expression of CD40, CD80 or CD86
on splenic DCs or immature or mature bone marrow–derived DCs
(Supplementary Fig. 1c). Therefore, H2−/− mice had normal myeloid development and macrophage differentiation. To investigate the
role of MHC class II molecules in the TLR-triggered innate immune
response, we challenged H2−/− mice with the TLR ligands LPS, CpG
ODN or poly(I:C). H2−/− mice produced significantly less TNF, IL-6
and interferon-β (IFN-β) than H2+/+ mice did in response to challenge
with LPS, CpG ODN or poly(I:C) (Fig. 1a–c). Accordingly, H2−/−
mice had prolonged survival relative to that of H2+/+ mice after lethal
nature immunology VOLUME 12 NUMBER 5 MAY 2011
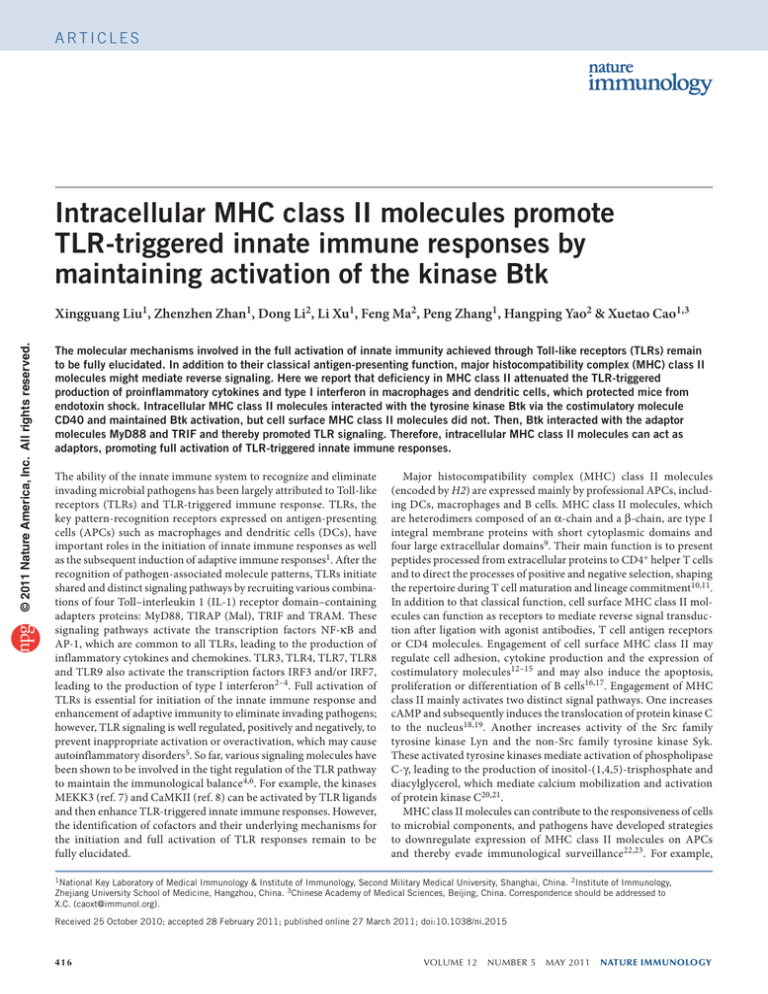
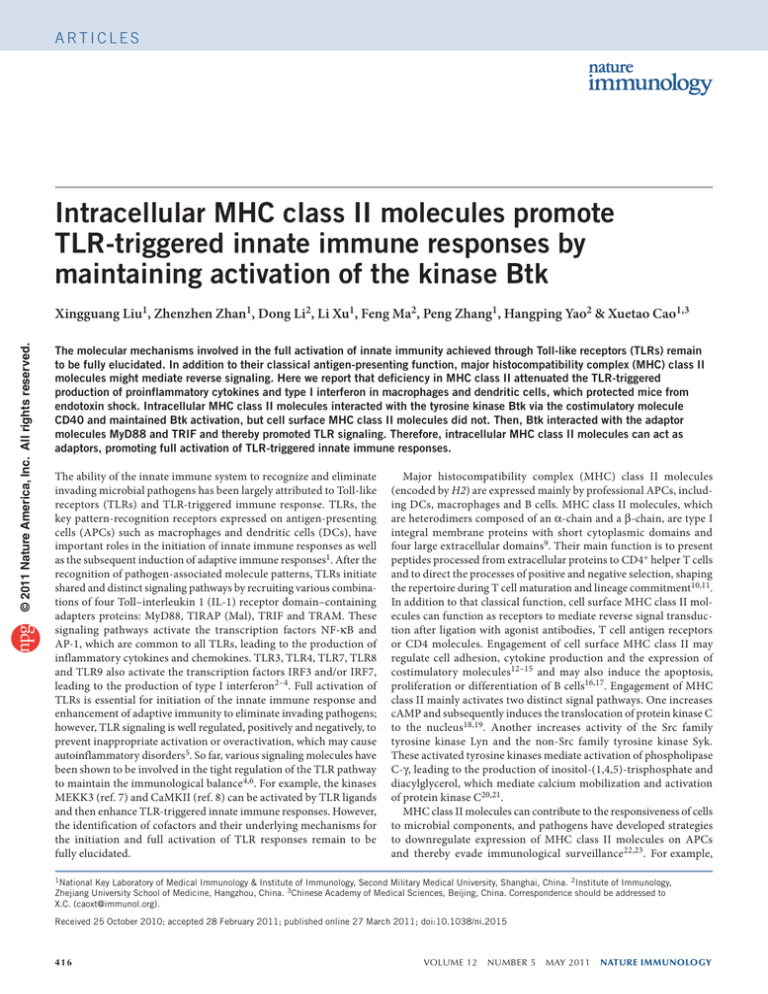
Figure 1 Deficiency in MHC class II protects mice from challenge with
TLR ligands. (a–c) Enzyme-linked immunosorbent assay (ELISA) of
TNF (a), IL-6 (b) and IFN-β (c) in the serum of H2−/− or H2+/+ mice (n = 5
per genotype) 2 h after intraperitoneal administration of PBS or LPS,
CpG-ODN (CpG) or poly(I:C) (at a dose of 15, 20 or 20 mg per kg body
weight, respectively). *P < 0.01 (Student’s t-test). (d) Survival of H2−/−
mice and H2+/+ mice (n = 10 per genotype) given intraperitoneal injection
of LPS (15 mg per kg body weight). P < 0.01 (Wilcoxon test). (e) ELISA
of TNF, IL-6 and IFN-β in serum from wild-type mice lethally irradiated
and given intravenous transplantation of 1 × 107 bone marrow cells from
H2−/− or H2+/+ mice 3 weeks before challenge with PBS or LPS, assessed
2 h after challenge. *P < 0.01 (Student’s t-test). Data are from three
independent experiments (mean ± s.e.m.).
challenge with LPS (Fig. 1d). H2−/− mice were also more resistant to
lethal challenge with high-dose poly(I:C) (data not shown). Given that
H2−/− mice have considerably fewer CD4+ T cells in thymus, spleen
and lymph nodes, we further explored the effects of the lack of CD4 +
T cells on the resistance of H2−/− mice to sepsis. We transplanted
bone marrow cells from H2+/+ or H2−/− mice into lethally irradiated wild-type mice. The reconstituted H2−/− mixed–bone marrow
chimeras had numbers of CD4+ T cells in spleen and lymph nodes
similar to those in H2+/+ chimeras but had no expression of MHC
class II in macrophages or DCs (data not shown). The LPS-induced
in vivo production of TNF, IL-6 and IFN-β was much lower in the
reconstituted H2−/− chimeras than in H2+/+ chimeras (Fig. 1e), which
therefore excluded the possibility that the lack of CD4+ T cells was
involved in the resistance of H2−/− mice to sepsis. These data demonstrate that H2−/− mice showed impaired TLR-triggered inflammatory
innate responses and were more resistant to endotoxin shock, which
indicates that MHC class II molecules have an important role in the
full activation of TLR-triggered immune responses.
To assess the role of MHC class II molecules in the host innate
response to infection with intact Gram-negative bacteria, we injected
H2−/− mice intraperitoneally with Escherichia coli serotype 0111:B4,
the most frequent cause of bacterial sepsis in humans. The production
of TNF and IL-6 in the serum of H2−/− mice after injection of E. coli
was significantly less than that in H2+/+ mice (Fig. 2a,b). The survival
of H2−/− mice after lethal challenge with E. coli was also prolonged
(Fig. 2c). These data indicate that deficiency in MHC class II attenuates
the inflammatory innate response of host to Gram-negative bacteria
and protects mice from lethal challenge by Gram-negative bacteria.
Impaired cytokine production in TLR-triggered H2−/− APCs
Next we assessed whether deficiency in MHC class II attenuated the production of proinflammatory cytokines and type I
a
b
3
H2+/+
H2–/–
*
2
1
4
3
*
c
H2+/+
H2–/–
100
Survival (%)
*
*
2.0
0
d
*
1.2
0.8
3.0
CpG Poly(I:C)
H2+/+
H2–/–
H2+/+
H2–/–
*
IL-6 (ng/ml)
LPS
4.0
Survival (%)
IFN-β (ng/ml)
1.6
PBS
b
TNF (ng/ml)
1.0
e
TNF (ng/ml)
*
2.0
0
© 2011 Nature America, Inc. All rights reserved.
*
3.0
0
c
H2+/+
H2–/–
*
4.0
IL-6 (ng/ml)
5.0
IL-6 (ng/ml)
TNF (ng/ml)
a
2
1
80
60
40
20
0
0
PBS
E. coli
0
PBS
E. coli
+/+
H2
H2–/–
0 12 24 36 48 60 72
Time after E. coli challenge (h)
Figure 2 Deficiency in MHC class II protects mice from sepsis induced
by live E. coli. (a,b) ELISA of TNF (a) and IL-6 (b) in serum from H2−/−
or H2+/+ mice (n = 3 per genotype) 4 h after intraperitoneal infection
with E. coli 0111:B4 (1 × 107 colony-forming units per mouse).
*P < 0.01 (Student’s t-test). (c) Survival of mice (n = 10 per genotype)
treated as described in a,b. P < 0.01 (Wilcoxon test). Data are from
three independent experiments (mean ± s.e.m.).
417
IFN-β (ng/ml)
0.6
IFN-β (ng/ml)
0.8
0.6
0.4
0.2
0
0.4
Poly(l:C)
0
Poly(l:C)
**
H2+/+
H2–/–
M
α+ oc
β- k
ch
ai
n
M
α+ oc
β- k
ch
ai
n
**
0.8
0.6
0.4
0.2
0
**
M
ed
LP
S
C
Po pG
ly
(l:
C
)
** **
CpG
**
Ctrl
siRNA
**
LP
S
C
p
Po G
ly
(l:
C
)
**
IFN-β (ng/ml)
**
2.5
2.0
1.5
1.0
0.5
0
H2+/+
H2–/–
0.2
α+
β- k
ch
a
α- in
ch
a
β- in
ch
ai
n
0
CpG
**
** **
**
M
α+ oc
β- k
ch
a
α- in
ch
a
β- in
ch
ai
n
IL-6 (ng/ml)
1.0
** **
LPS
** **
M
oc
**
IL-6 (ng/ml)
**
4.0
3.0
2.0
1.0
0
**
M
α+ oc
β- k
ch
ai
n
α+ Mo
c
β- k
ch
ai
n
TNF (ng/ml)
IL-6 (ng/ml)
M
α+ oc
β- k
ch
a
α- in
ch
a
β- in
ch
ai
n
2.0
1.5
1.0
0.5
0
Poly(l:C)
α+
β- k
ch
ai
n
M
α+ oc
β- k
ch
ai
n
e
2.0
CpG
**
M
ed
Counts
0
3.0
interferon in TLR-triggered macrophages and DCs in vitro. H2 −/−
peritoneal macrophages had lower expression of TNF, IL-6, IFN-α
and IFN-β mRNA and protein than did macrophages from H2 +/+
mice in response to LPS, CpG-ODN or poly(I:C) (Fig. 3a and
Supplementary Fig. 2). Similarly, we also detected less production
of TNF, IL-6 and IFN-β in H2 −/− DCs (Fig. 3a). H2 −/− peritoneal
macrophages responded normally to the phorbol ester PMA, to
IL-1β and to MDP (the ligand for the intracellular bacteria sensor
Nod2) and produced amounts of TNF and IL-6 similar to those
produced by H2+/+ macrophages (Supplementary Fig. 3a), which
indicated that deficiency in MHC class II selectively impaired the
activation of TLR signaling. We also did a ‘rescue’ experiment by
transfecting expression vectors encoding MHC class II α-chain
and β-chain into H2 −/− peritoneal macrophages and found that
overexpression of both MHC class II α-chain and β-chain restored
the production of TNF, IL-6 and IFN-β induced by LPS, CpG-ODN
or poly(I:C), whereas overexpression of either α-chain or β-chain
alone did not (Fig. 3b,c); this suggested that both the α-chain and
β-chain are required for full activation of TLR-triggered macrophages. In addition, there was no substantial difference between
H2 −/− and H2 +/+ mice in the expression of TLR4, TLR3 or TLR9
protein and mRNA in peritoneal macrophages and bone marrow–
derived DCs (Supplementary Fig. 3b,c). Overexpression of MHC
class II α-chain and β-chain in H2 −/− peritoneal macrophages did
not affect the expression of TLR4, TLR3 or TLR9 (Supplementary
Fig. 4). Thus, MHC class II expression did not affect the expression pattern of TLRs, which excluded the possibility that the
418
PB
S
LP
S
C
Po pG
ly
(l:
C
)
IFN-β (ng/ml)
PB
S
LP
S
C
Po pG
ly
(l:
C
)
IL-6 (ng/ml)
S
LP
S
C
Po pG
ly
(l:
C
)
f
TNF (ng/ml)
Figure 3 Deficiency in MHC class II
attenuates TLR-triggered production
H2+/+
1.2
5.0
4.0
*
*
*
of proinflammatory cytokines and type I interferon in macrophages and
H2–/–
4.0
3.0
*
0.8
* *
3.0
*
2.0
DCs. (a) ELISA of cytokines in supernatants of H2−/− or H2+/+ macrophages
2.0
*
*
0.4
1.0
(top row) or DCs (bottom row) left unstimulated (Med) or stimulated for
1.0
0
0
0
6 h with LPS (100 ng/ml), CpG ODN (CpG; 0.3 µM) or poly(I:C) (10 µg/ml).
(b,c) ELISA of cytokines in supernatants of H2−/− or H2+/+ macrophages
given mock transfection (Mock) or transfected with vectors for the expression
of MHC class II α-chain and β-chain (α+β-chain) or MHC class II α-chain
alone (α-chain) or β-chain alone (β-chain) and, 36 h later, stimulated for 6 h with LPS (b), or CpG ODN or poly(I:C) (c). (d) Immunoblot analysis of the
expression of MHC class II β-chain (MHCIIβ) and β-actin in lysates (left) and flow cytometry analysis of the surface expression of MHC class II (MHCII;
right) of macrophages 48 h after transfection with control siRNA (Ctrl (left) or solid line with no shading (right)) or siRNA specific for MHC class II
β-chain (siRNA (left) or solid line with gray shading (right)). Dotted line (right), isotype-matched control antibody. (e) ELISA of cytokines in supernatants
of macrophages transfected as in d and, 48 h later, left unstimulated or stimulated for 6 h with LPS, CpG ODN or poly(I:C). (f) ELISA of cytokines in
serum from wild-type mice first depleted of endogenous macrophages and then transplanted with 1 × 10 7 H2−/− or H2+/+ bone marrow–derived cells
6 h before challenge with LPS, CpG ODN or poly(I:C), measured 2 h after challenge. *P < 0.05 and **P < 0.01 (Student’s t-test). Data are from three
independent experiments (a–c,e–f; mean ± s.e.m.) or are representative of three independent experiments with similar results (d).
PB
© 2011 Nature America, Inc. All rights reserved.
MHCIIβ
β-actin
100
80
60
40
20
0
100 101 102 103
MHCII
0.2
** **
TNF (ng/ml)
0
d
Ctrl siRNA
**
0.4
c
H2+/+
H2–/–
**
0.6
** **
**
2.5
2.0
1.5
1.0
0.5
0
M
oc
0.5
**
**
LPS
LPS
4.0
3.0
2.0
1.0
0
LP
S
C
Po pG
ly
(l:
C
)
1.0
**
b
H2+/+
H2–/–
M
ed
LP
S
C
Po pG
ly
(l:
C
)
M
ed
LP
C S
Po pG
ly
(l:
C
)
1.5
**
**
TNF (ng/ml)
** **
M
ed
LP
C S
Po pG
ly
(l:
C
)
DC
**
IL-6 (ng/ml)
M
ed
LP
S
Po CpG
ly
(l:
C
)
0
1.0
0.8
0.6
0.4
0.2
0
M
ed
1.0
** **
IFN-β (ng/ml)
** **
**
IFN-β (ng/ml)
2.0
2.0
1.5
1.0
0.5
0
M
ed
LP
S
C
Po pG
ly
(l:
C
)
2.0
1.5
1.0
0.5
0
Macrophage
**
M
ed
LP
C S
Po pG
ly
(l:
C
)
TNF (ng/ml)
3.0
TNF (ng/ml)
a
IL-6 (ng/ml)
Articles
attenuation of TLR responses achieved by deficiency in MHC
class II was due simply to lower expression of TLRs.
We further observed the effect of knockdown of MHC class II on
cytokine production by TLR-activated macrophages. The endogenous expression of total or cell surface MHC class II in peritoneal
macrophages was diminished considerably by MHC class II–specific
small interfering RNA (siRNA; Fig. 3d). MHC class II–specific siRNA
resulted in significantly less production of TNF, IL-6 and IFN-β in
peritoneal macrophages stimulated with LPS, CpG-ODN or poly(I:C)
(Fig. 3e). To further confirm that the impaired TLR-triggered inflammatory response in vivo was due to deficiency in MHC class II in
myeloid cells, we adoptively transferred H2+/+ or H2−/− bone marrow–
derived macrophages into wild-type mice depleted of endo­genous
macrophages by pretreatment with clodronate liposomes. Mice
reconstituted with H2−/− macrophages produced less proinflammatory cytokines and IFN-β in response to LPS, CpG-ODN or poly(I:C)
challenge than did mice reconstituted with H2+/+ macrophages
(Fig. 3f). Therefore, deficiency in MHC class II attenuated the
TLR-triggered production of proinflammatory cytokines and type I
interferon in APCs, including macrophages and DCs.
Impaired TLR signaling in H2−/− macrophages
We further investigated the effect of deficiency in MHC class II on
TLR-activated downstream signal pathways in macrophages. We
observed impaired phosphorylation of the kinases Erk, Jnk and p38
and inhibitor IκBα in LPS-stimulated H2−/− peritoneal macrophages
(Fig. 4a). Deficiency in MHC class II resulted in less LPS-induced
VOLUME 12 NUMBER 5 MAY 2011 nature immunology
© 2011 Nature America, Inc. All rights reserved.
*
*
7
6
5
4
3
2
1
0
*
2
0
M
M
ed
LP
S
C
Po pG
ly
(I:
C
)
*
4
ed
0
H2
*
pG
2
–/–
6
C
4
+/+
H2
IRF7 activation
(fold)
*
ed
L
Po PS
ly
(I:
C
)
AP-1 activation
(fold)
M
5
4
3
2
1
0
*
*
+/+
H2
–/–
H2
ed
L
Po PS
ly
(I:
C
)
IB: TRIF
*
6
M
IB: MyD88
*
6
5
4
3
2
1
0
8
TBK1 activity
(103 c.p.m.)
LPS (min) 30 0 15 30 45 60 90 0 15 3045 6090
IP: TRIF – + + + + + + + + + + + +
IP: IgG
+ – – – – – – – – – – – –
IB: TBK1
M
LPS (min) 30 0 15 30 45 60 90 0 15 30 45 60 90
IP: MyD88 – + + + + + + + + + + + +
IP: IgG
+ – – – – – – – – – – – –
IB: IRAK1
f
*
ed
LP
S
C
Po pG
ly
(I:
C
)
+/+
H2
M
–/–
H2
* *
TAK1 activity
(103 c.p.m.)
e
S
+/+
H2
10
8
6
4
2
0
pG
–/–
H2
C
M
p-p38
p38
p-lκBα
p-IRF3
IRF3
*
ed
Jnk
d
H2
LPS (min) 0 30 60 90 0 30 60 90
Nuclear
IRF3
Lamin A
p-Jnk
*
LP
H2
Erk
+/+
*
S
C
Po pG
ly
(I:
C
)
–/–
12
10
8
6
4
2
0
IRAK1 activity
(103 c.p.m.)
c
ed
b
+/+
H2
LP
–/–
H2
LPS (min) 0 15 30 45 60 0 15 30 45 60
p-Erk
NF-κB activation
(fold)
a
IRF3 activation
(fold)
Articles
Figure 4 Deficiency in MHC class II impairs the MyD88-dependent and TRIF-dependent activation of mitogen-activated protein kinases, NF-κB, IRF3
and IRF7 in TLR-triggered macrophages. (a) Immunoblot analysis of phosphorylated (p-) or total protein in lysates of H2−/− or H2+/+ macrophages
stimulated for 0–60 min (above lanes) with LPS (100 ng/ml). (b) Immunoblot analysis of IRF3 among nuclear proteins from macrophages stimulated
with LPS; lamin A serves as a loading control. (c) Luciferase activity in lysates of H2−/− or H2+/+ macrophages transfected with luciferase reporter
plasmids for NF-κB, AP-1, IRF3 or IRF7 (vertical axes) and, 36 h later, left unstimulated or stimulated for 4 h with LPS (100 ng/ml), CpG ODN (0.3 µM)
or poly(I:C) (10 µg/ml); results are presented relative to the activity in unstimulated H2+/+ macrophages, set as 1. (d,e) Immunoblot analysis (IB) of
IRAK1 and MyD88 (d) or TBK1 and TRIF (e) immunoprecipitated (IP) with anti-MyD88 (d) or anti-TRIF (e) from lysates of H2−/− or H2+/+ macrophages
stimulated for 0–90 min (above lanes) with LPS; immunoglobulin G (IgG) serves as an immunoprecipitation control. (f) In vitro kinase assay of IRAK1,
TAK1 and TBK1 in lysates of H2−/− or H2+/+ macrophages left stimulated (Med) or stimulated for 30 min with LPS, CpG ODN or poly(I:C), assayed
with the substrates MBP (for IRAK1), MKK4 (for TAK1) or recombinant IRF3 (for TBK1). *P < 0.01 (Student’s t-test). Data are from one experiment
representative of three independent experiments with similar results (a,b,d,e; mean ± s.d. of four samples in c) or are from three independent
experiments (f; mean ± s.e.m.).
phosphorylation and nuclear translocation of IRF3 (Fig. 4a,b). We
obtained similar results with H2−/− peritoneal macrophages stimulated with CpG ODN or poly(I:C) (Supplementary Fig. 5). We
further evaluated the effect of deficiency in MHC class II on the
transactivation of NF-κB, AP-1, IRF3 and IRF7. Transactivation of
reporters for NF-κB and AP-1 was lower in H2−/− peritoneal macro­
phages stimulated with LPS, CpG ODN or poly(I:C) (Fig. 4c).
Deficiency in MHC class II also impaired the transactivation of an
IRF3 reporter induced by LPS or poly(I:C) and the transactivation of
an IRF7 reporter induced by CpG ODN (Fig. 4c). To assess the functional integrity of intracellular signal pathway in H2−/− macrophages,
we monitored the activation of mitogen-activated protein kinases and
NF-κB induced by TNF. Phosphorylation of Jnk, p38 and IκBα in
TNF-stimulated H2−/− peritoneal macrophages was similar to that in
TNF-stimulated H2+/+ macrophages (Supplementary Fig. 6), which
indicated that deficiency in MHC class II selectively impaired TLRtriggered activation of mitogen-activated protein kinases and NF-κB.
Immunoprecipitation showed that the interaction of MyD88 with the
kinase IRAK1 or of TRIF with the kinase TBK1 was much lower in
H2−/− macrophages stimulated with LPS than in H2+/+ macrophages
stimulated with LPS (Fig. 4d,e). In vitro kinase assays showed that
the activation of IRAK1, TAK1 and TBK1 induced by LPS, CpG
ODN or poly(I:C) was impaired in H2−/− macrophages relative to
that in H2+/+ macrophages (Fig. 4f). Collectively, these data suggest
that MHC class II molecules promote TLR-triggered production of
proinflammatory cytokines and type I interferon by enhancing the
activation of both MyD88-dependent and TRIF-dependent pathways
in macrophages.
MHC class II molecules maintain TLR-triggered Btk activation
Next we explored which signal molecules mediate the nonclassical
function of MHC class II molecules in promoting intracellular TLR
signaling. Given that activation of tyrosine kinases is involved in TLR
nature immunology VOLUME 12 NUMBER 5 MAY 2011
signaling, we screened the activation status of various tyrosine kinases
in TLR-triggered H2−/− and H2+/+ macrophages. Many such kinases
showed similar activation in H2−/− and H2+/+ macrophages stimulated
with LPS, except Btk, a member of the Btk-Tec family of cytoplasmic
tyrosine kinases26. Activation of Btk was associated with phosphorylation of two tyrosine residues: Tyr550 and Tyr222. Tyr550 in the activation loop is transphosphorylated, leading to autophosphorylation at
Tyr222, which is necessary for full activation27. TLR ligand-induced
phosphorylation of Btk was much lower in H2−/− macrophages than
in H2+/+ macrophages (Fig. 5a,b), which indicated that MHC class II
molecules may increase TLR-triggered activation of Btk. We found
no substantial difference between H2−/− and H2+/+ macrophages
in PMA-triggered Btk activation (Supplementary Fig. 7a), which
suggested that deficiency in MHC class II selectively impairs TLR­triggered Btk activation. Overexpression of MHC class II α-chain and
β-chain in wild-type macrophages did not induce Btk activation (data
not shown), whereas overexpression of MHC class II α-chain and
β-chain in H2−/− peritoneal macrophages did restore the activation
of Btk triggered by LPS, CpG-ODN or poly(I:C) (Supplementary
Fig. 7b,c). These data indicate that MHC class II molecules act in
synergy with TLR signaling to maintain Btk activation.
To investigate the role of Btk in TLR signaling, we examined the
effect of Btk deficiency on TLR-triggered production of proinflammatory cytokines and type I interferons in macrophages. Btk−/−
peritoneal macrophages produced significantly less TNF, IL-6 and
IFN-β than Btk+/+ macrophages did in response to LPS, CpG-ODN
or poly(I:C) (Fig. 5c). We further observed the effect of knockdown
of Btk on the production of cytokines in TLR-activated macrophages.
Btk-­specific siRNA substantially downregulated endogenous expression of Btk (Supplementary Fig. 8a), which led to much lower production of TNF, IL-6 and IFN-β in macrophages stimulated with LPS,
CpG-ODN or poly(I:C) (Supplementary Fig. 8b–d). In addition,
LFM-A13, an inhibitor of Btk, also resulted in much less ­production
419
Articles
p-Btk(Y550)
p-Btk(Y222)
p-Btk(Y222)
3.0
d
5.0
4.0
3.0
2.0
1.0
0
1.5
**
2.0
**
1.0
0
Btk
**
1.0
0.6
**
**
0.5
0
Med LPS CpG Poly(l:C)
*
**
**
3.0
2.5
2.0
1.5
1.0
0.5
0
IFN-β (ng/ml)
0 5 15 30 45 60 0 5 15 30 45 60
p-Btk(Y550)
Btk
c
H2+/+
M
e
C d
pG
Po
l
M y (l :
e C
C d )
pG
Po
ly
(l :
C
)
LPS (min)
H2–/–
H2+/+
IL-6 (ng/ml)
b
H2–/–
TNF (ng/ml)
a
0.4
0.2
0
Med LPS CpG Poly(l:C)
*
**
**
Btk+/+
Btk–/–
**
**
Med LPS CpG Poly(l:C)
*
**
H2+/+
H2–/–
© 2011 Nature America, Inc. All rights reserved.
of TNF, IL-6 and IFN-β in macrophages stimulated with LPS,
CpG-ODN or poly(I:C) (Supplementary Fig. 9). These data suggest
that Btk is required for full activation of TLR signaling.
Given the positive role of Btk in TLR-triggered cytokine production and the lower activation of Btk in TLR-triggered H2−/− macrophages, we sought to determine whether Btk contributes to MHC
class II–mediated full activation of TLR signaling. We transfected
H2−/− and H2+/+ macrophages with plasmid encoding constitutively
active Btk, with substitution of lysine for glutamic acid at position 41
(Btk(E41K)), and found that overexpression of Btk(E41K) potently
enhanced the production of TNF, IL-6 and IFN-β induced by LPS,
CpG ODN or poly(I:C) in H2+/+ macrophages relative to that in
mock-transfected control cells (Fig. 5d). Furthermore, overexpression of Btk(E41K) restored the impaired production of inflammatory
cytokines and type I interferon in H2−/− macrophages activated with
LPS, CpG ODN or poly(I:C) (Fig. 5d). Together these data suggest
that MHC class II molecules facilitate TLR-triggered inflammatory
responses by enhancing Btk activation.
Intracellular MHC class II molecules bind Btk via CD40
We further investigated the mechanisms underlying the involvement of MHC class II molecules in the activation of TLR signaling.
First we sought to determine whether MHC class II molecules interacted directly with TLRs. Immunoprecipitation with antibody to
MHC class II, TLR4, TLR9 or TLR3 showed that MHC class II mol­
e­cules did not interact with TLR4, TLR9 or TLR3 (Supplementary
Fig. 10). So far, there has been no report to our knowledge showing
that MHC class II molecules can recognize TLR ligands; therefore,
we predicted that MHC class II molecules may not form a complex
with the TLR as a cofactor to promote TLR signaling. MHC class II
molecules are also abundant in the intracellular endosomal compartment9,10, whereas after stimulation by their respective ligands, TLR3
and TLR9 located on the endoplasmic reticulum membrane and
TLR4 on the plasma membrane translocate into endosome. In the
endosome, TLRs initiate signals by a MyD88- or TRIF-dependent
pathway1. Thus, we investigated whether deficiency in MHC class II
disrupted endosomal trafficking of TLR4, TLR3 or TLR9 in TLRtriggered macrophages. Confocal microscopy showed that the
translocation of TLR4, TLR3 or TLR9 into endosomes in H2−/−
macrophages was similar to that in H2+/+ macrophages, after stimu­
lation with TLR ligands (Supplementary Fig. 11). The similar
subcellular distribution of intracellular MHC class II molecules and
TLR4, TLR3 and TLR9 inspired us to explore whether intracellular
420
IFN-β (ng/ml)
IL-6 (ng/ml)
TNF (ng/ml)
Figure 5 MHC class II molecules promote TLR-triggered
*
*
*
*
*
**
**
inflammatory innate responses by maintaining Btk
0.8
**
**
**
*
activation. (a,b) Immunoblot analysis of Btk phosphorylated
**
0.4
at Tyr550 (p-Btk(Y550)) or Tyr222 (p-Btk(Y222)) or total
0
Btk in lysates of H2−/− or H2+/+ peritoneal macrophages
Mock E41K Mock E41K Mock E41K
Mock E41K Mock E41K Mock E41K
Mock E41K Mock E41K Mock E41K
LPS
CpG Poly(l:C)
LPS
CpG Poly(l:C)
LPS
CpG Poly(l:C)
left unstimulated or stimulated for 0–60 min with LPS
(100 ng/ml; a) or for 30 min with CpG ODN (0.3 µM) or poly(I:C)
(10 µg/ml; b). (c) ELISA of TNF, IL-6 and IFN-β in supernatants of Btk+/+ or Btk−/− peritoneal macrophages left unstimulated or stimulated for 6 h with
LPS, CpG ODN or poly(I:C). (d) ELISA of TNF, IL-6 and IFN-β in supernatants of H2−/− or H2+/+ peritoneal macrophages mock-transfected or transfected
with constitutively active Btk(E41K) and, 48 h later, stimulated for 6 h with LPS, CpG ODN or poly(I:C). *P < 0.05 and **P < 0.01 (Student’s t-test).
Data are representative of three independent experiments with similar results (a,b) or are from three independent experiments (c,d; mean ± s.e.m.).
1.2
MHC class II molecules interact with some intermediate proteins
and thereby integrate into the TLR signaling pathway.
Given that the impaired activation of Btk in TLR-triggered H2−/−
macrophages contributed to the lower production of inflammatory
cytokines and type I interferon, we sought to determine whether
MHC class II molecules interact with Btk. Immunoprecipitation
showed that MHC class II molecules interacted with Btk (Fig. 6a).
Specifically, intracellular MHC class II molecules associated with Btk,
but plasma membrane MHC class II molecules did not. As MHC
class II molecules have only short cytoplasmic domains, MHC class II
might not directly interact with Btk; therefore, some other molecules
might mediate the interaction of MHC class II with Btk. We immuno­
precipitated proteins from lysates of LPS-stimulated macrophages
with antibody to MHC class II and then used reverse-phase nanospray liquid chromatography–tandem mass spectrometry to identify
possible MHC class II–associated proteins, which might be involved
in the association and activation of Btk, in the immunoprecipitates.
Among the several proteins we detected (data not shown), CD40
attracted our attention because CD40 has been found to mediate Btk
activation after stimulation of human B lymphocytes with its ligand,
CD40L28. Further immunoprecipitation confirmed the finding that
intracellular MHC class II molecules associated with CD40, but those
at the plasma membrane did not (Fig. 6b). Confocal microscopy also
showed that intracellular MHC class II localized together with CD40
and Btk in the endosomes of macrophages stimulated with LPS for
15 min (Fig. 6c–f), which indicated that intracellular but not plasma
membrane MHC class II forms a complex with CD40 and Btk after
TLR activation.
Binding of Btk with CD40 is required for full TLR response
Immunoprecipitation with antibody to Btk (anti-Btk) also showed
that Btk interacted with CD40 and MHC class II molecules
(Supplementary Fig. 12a). To determine which domain of Btk
was required for the interaction of Btk with CD40, we constructed
mutants of Btk with deletion of various domains and transfected the
mutants into Btk-deficient macrophages to observe the restoration
of LPS-induced cytokine production in the Btk-deficient macrophages. Overexpression of mutant Btk with deletion of the pleckstrin homo­logy domain or the kinase domain was unable to restore
LPS-induced TNF production (Supplementary Fig. 12b). We transfected those two Btk mutants or wild-type Btk into macrophages,
followed by immunoprecipitation. We found that mutant Btk with
deletion of the pleckstrin homology domain did not interact with
VOLUME 12 NUMBER 5 MAY 2011 nature immunology
Articles
a
15 0
5 15 15 0
5 15
LPS (min) 15 0
5 15 15 0
5 15
IP: MHCll
– +
+ –
+
–
+
–
IP: MHCll
+
–
+
–
+
–
– +
+ –
+
–
IB: Btk
IB: CD40
IB: MHCll
IB: MHCll
MHCll
CD40
– +
+ –
IP: IgG
e
Merge
LPS
0 min
Btk
+
–
– +
+ –
CD40
MHCll
+
–
LPS
0 min
Merge
LPS
15 min
LPS
0 min
LPS
15 min
f
Btk
MHCll
Merge
EEA1
Merge
LPS
15 min
LPS
15 min
g
Cd40+/+
*
*
CD40 (Supplementary Fig. 12c). Therefore the pleckstrin homology
domain of Btk is required for the interaction of Btk with CD40.
As described above (Fig. 5 and Supplementary Figs. 8 and 9),
Btk activation was required for full activation of TLR signaling.
We sought further to confirm that it was CD40 that mediated the
interaction of MHC class II and Btk required for the TLR response.
Immunoprecipitation of proteins from lysates of TLR-triggered
CD40-deficient macrophages showed that MHC class II molecules did
not interact with Btk without CD40 (Supplementary Fig. 13), which
suggested that MHC class II molecules interact with Btk via CD40 in
TLR responses. Btk activation triggered by LPS, CpG ODN or poly(I:C)
was also impaired in Cd40−/− macrophages (Supplementary Fig. 14).
Furthermore, Cd40−/− macrophages produced less proinflammatory
IB: TRIF
IB: Btk
b
Mock
HA-Btk
Flag-MyD88
Flag-TRIF
IP: HA
IB: Flag
IB: HA
TCL: Flag
+
–
+
–
+
–
+
+
–
+
+
–
–
+
+
–
+
–
+
+
)
C
(l:
Po
ly
S
C
ed
LP
M
pG
IFN-β (ng/ml)
S
C
Po pG
ly
(l:
C
)
ed
M
Btk enhances TLR signaling by binding MyD88 and TRIF
We sought to elucidate the underlying molecular mechanisms by
which the greater Btk activation contributed to the enhancement of
TLR-triggered innate immune response by intracellular MHC class II.
Given that signaling through TLR4, TLR9 and TLR3 was down­
regulated by deficiency in MHC class II, the common adapters
MyD88 and TRIF might be the potential targets of Btk and might be
c
40
30
*
**
20
10
0
Ctrl MyD88 25
50
100
MyD88+E41K
40
30
*
**
20
10
0
Ctrl TRIF 25
50 100
TRIF+E41K
IRF3 activation (fold)
H2–/–
H2+/+
LPS (min) 30 0 15 30 60 90 0 15 30 60 90
IP: Btk
– + + + + + + + + + +
+ – – – – – – – – – –
IP: IgG
IB: MyD88
cytokines and IFN-β than did Cd40+/+ macrophages in response
to stimulation with LPS, CpG ODN or poly(I:C) (Fig. 6g). These
data indicate that CD40-mediated interaction of intracellular MHC
class II molecules with Btk is involved in the positive regulation of
TLR-triggered innate response.
NF-κB activation (fold)
a
LP
)
C
(l:
Po
ly
S
pG
C
LP
M
ed
IL-6 (ng/ml)
TNF (ng/ml)
3.0
1.5
* Cd40–/–
0.6
Figure 6 Intracellular MHC class II molecules interact with
*
*
*
*
*
CD40 and Btk. (a,b) Immunoblot analysis of Btk (a), CD40 (b)
1.0
2.0
0.4
or MHC class II (a,b) immunoprecipitated with antibody to
*
0.5
0.2
1.0
MHC class II from cytoplasmic and plasma membrane proteins
0
0
0
in lysates of peritoneal macrophages stimulated for 0–15 min
with LPS. Immunoglobulin G serves as an immunoprecipitation
control. (c–f) Confocal microscopy of macrophages left
unstimulated (0 min) or stimulated for 15 min with LPS
(100 ng/ml), then labeled with antibodies to the appropriate molecules (above images). Original magnification, ×630. (g) ELISA of TNF, IL-6 and
IFN-β in supernatants of Cd40+/+ or Cd40−/− peritoneal macrophages left unstimulated or stimulated for 6 h with LPS (100 ng/ml), CpG ODN (0.3 µM)
or poly(I:C) (10 µg/ml). *P < 0.01 (Student’s t-test). Data are representative of three independent experiments with similar results (a–f) or are from
three independent experiments (g; mean ± s.e.m.).
NF-κB activation (fold)
© 2011 Nature America, Inc. All rights reserved.
c
Plasma
membrane
Cytoplasmic
LPS (min)
IP: IgG
d
b
Plasma
membrane
Cytoplasmic
12
*
**
8
4
0
Ctrl TRIF 25
50 100
TRIF+E41K
Figure 7 Activated Btk interacts with MyD88 and TRIF, promoting the activation of MyD88-dependent and TRIF-dependent pathways. (a) Immunoblot
analysis of MyD88, TRIF or Btk immunoprecipitated with anti-Btk from lysates of H2−/− or H2+/+ macrophages stimulated for 0–90 min with LPS.
(b) Immunoblot analysis of HEK293 cells 48 h after cotransfection of Flag-tagged MyD88 or Flag-tagged TRIF plus hemagglutinin (HA)-tagged Btk,
followed by immunoprecipitation with anti-hemagglutinin. TCL, immunoblot analysis of total cell lysates with anti-Flag. (c) Luciferase assay of the
activation of NF-κB or IRF3 in lysates of HEK293 cells 24 h after transfection of luciferase reporter plasmid for NF-κB or IRF3, plus empty vector
control (Ctrl) or plasmid expressing MyD88 or TRIF either alone (MyD88 or TRIF) or together with plasmid expressing Btk(E41K) (MyD88+E41K or
TRIF+E41K; dose, horizontal axis); results were normalized to renilla luciferase activity and are presented relative to the activity in cells transfected
with empty vector control, set as 1. *P < 0.05 and **P < 0.01 (Student’s t-test). Data are from one experiment representative of three independent
experiments with similar results (mean ± s.d. of six samples in c).
nature immunology VOLUME 12 NUMBER 5 MAY 2011
421
Articles
© 2011 Nature America, Inc. All rights reserved.
more activated in the presence of MHC class II. Immunoprecipitation
with anti-Btk showed that Btk precipitated together with MyD88
and TRIF in H2+/+ macrophages after LPS stimulation and that
this coimmuno­precipitation was diminished in H2−/− macrophages
(Fig. 7a and Supplementary Fig. 15). We transfected hemagglutinin-tagged Btk together with Flag-tagged MyD88 or Flag-tagged
TRIF into HEK293 human embryonic kidney cells; coimmunoprecipitation showed that Btk interacted with either MyD88 or TRIF
(Fig. 7b). We further examined the effect of Btk on the activation
of a reporter for NF-κB or IRF3. Overexpression of constitutively
active Btk(E41K) enhanced the MyD88- or TRIF-induced activation
of NF-κB and the TRIF-induced activation of IRF3 (Fig. 7c). These
data indicate that MHC class II molecules contribute to the maintenance of TLR-triggered Btk activation and subsequently enhance the
interaction of Btk with MyD88 and TRIF, which promotes the activation of MyD88-dependent and TRIF-dependent signal pathways,
finally leading to full activation of TLR-triggered innate responses
(Supplementary Fig. 16).
DISCUSSION
It is well known that MHC class II molecules have a crucial role in
the development and function of the immune system. In addition
to the classical function of MHC class II molecules in presenting
antigen to CD4+ T cells, MHC class II molecules can activate various
cellular functions in immune or non-immune cells when crosslinked
by antibody or superantigen12–14. These nonclassical functions are
accomplished by MHC class II molecules at the cell surface acting
as signal-transduction receptors. However, so far there has been no
insight into any nonclassical functions of intracellular MHC class II
molecules. Given reports that the expression of MHC class II can affect
the response of macrophages to LPS24,25, we speculated that MHC
class II molecules may be involved in the activation of TLR sig­naling.
Here we have provided evidence that deficiency in MHC class II
impaired TLR-triggered production of proinflammatory cytokines
and type I interferon in macrophages and DCs, and this protected
mice from lethal challenge with TLR ligands and live Gram-negative
bacteria. A lower abundance of activated Btk in TLR-triggered H2−/−
macrophages led to less interaction of Btk with MyD88 and TRIF,
which attenuated the activation of MyD88- and TRIF-dependent
pathways; this suggested that MHC class II molecules are required
for full activation of TLR-triggered innate responses. Therefore, we
have demonstrated a nonclassical function of MHC class II molecules
in the TLR-triggered innate immune response.
Some reports have suggested a role for Btk in TLR signaling. Btk is
phosphorylated in LPS-stimulated human monocytes and can interact
with multiple components of TLR pathways, including TLR4, TLR6,
TLR8, TLR9, MyD88, Mal and IRAK129. Btk phosphorylates Mal,
which resulting in degradation of Mal30,31. Studies of peripheral blood
monocytes from patients with Btk-deficient X-linked agammaglobulinemia and macrophages from Btk-mutant mice with X-linked
immunodeficiency have indicated that Btk-dependent signaling
is involved in the LPS-induced production of TNF and IL-1β32,33.
However, it remained unclear whether Btk affects the production of
cytokines by macrophages in response to other TLR ligands or whether
it activates an altered signal pathway. Here we have shown that Btk
interacted with TRIF and promoted TRIF-dependent activation of
IRF3 and NF-κB, leading to enhanced TLR3- and TLR4-triggered
production of type I interferons and proinflammatory cytokines. In
addition, the constitutively active mutant Btk(E41K) also enhanced
MyD88-triggered activation of NF-κB, AP-1 and IRF7. Given those
findings and the observations that Btk interacted with TLRs, MyD88,
422
Mal and IRAK1, we conclude that Btk is necessary but is not essential
for the full activation of MyD88- and TRIF-dependent pathways by
interacting with multiple components in TLR signaling. As deficiency
in MHC class II impairs Btk activation, H2−/− mice and cells (macro­
phages and DCs) derived from them had lower but not completely
abolished cytokine production and less death in response to challenge
with TLR ligands. The data showing that overexpression of the constitutively active mutant Btk(E41k) corrected the lower abundance of
proinflammatory cytokines and type I interferons in TLR-triggered
H2−/− macrophages indicate that Btk activation has a pivotal role in
MHC class II–mediated full activation of TLR signaling.
Reverse signaling mediated by MHC class II at the cell surface is
involved in many cellular processes of B cells and DCs. The short
cytosolic domain of MHC class II molecules seems inconsistent with
these complex signal-transduction pathways, which suggests that the
presence of membrane-associated signaling components that might
provide this functionality. Indeed, a variety of cell surface molecules
have been reported to immunoprecipitate together with and/or
couple with MHC class II molecules. These MHC class II–associated
molecules belong to various families, including the immunoglobulin
superfamily (CD19), the tetraspanin family (CD37, CD53, CD81 and
CD82), lectin (CD23) and the complement receptor family (CD21
and CD20)34–36. Furthermore, MHC class II molecules can associate
with CD40 on human B cells37. Here we found that MHC class II
molecules interacted with CD40 in the endosomes of TLR-activated
macrophages. However, which region of MHC class II interacts with
these molecules is still unclear. Several studies have shown that eight
membrane-proximal amino acids of the cytoplasmic domain and
transmembrane domain of MHC class II β-chain are required for
distinct MHC class II–mediated signaling38,39, which suggests that
these regions may also be required for the interaction of MHC class II
with other molecules. Notably, we found that intracellular MHC
class II molecules interacted with Btk after TLR ligation as early as
5 min after activation, but cell surface MHC class II molecules did
not. This rapid interaction of intracellular MHC class II and Btk is
consistent with rapid activation of the Btk and TLR signaling pathway.
We further confirmed that MHC class II molecules formed a complex
with CD40 and Btk in the endosomes of TLR-activated macrophages
and that intracellular CD40 mediated the interaction of MHC class II
and Btk. Although Btk has been reported to become activated after
stimulation of human B lymphocytes with CD40L, the underlying
mechanism is not clear. Thus, the mechanism by which the inter­action
of MHC class II molecules with CD40 maintains activation of Btk
needs further investigation.
Coexpression of MHC class II (HLA-DR) in HEK293 cells overexpressing TLR2 or TLR4 results in much higher TLR2- or TLR4triggered expression of human β-defensin40. Furthermore, in lysates
of HEK293 cells overexpressing HLA-DR, radiolabeled recombinant
TLR2 protein precipitates in vitro together with HLA-DR protein
immunoprecipitated with anti-HLA-DR. So, TLR2 was proposed
to associate with HLA-DR40. However, whether or not TLR2 and
HLA-DR interact physically needs further investigation. In our
study, we did not find direct interaction of cell surface MHC class II
molecules with TLRs in macrophages, which suggests that MHC
class II molecules may not form a complex with TLRs. In addition,
we found that ligation of MHC class II by specific antibody did not
induce the production of TNF, IL-6 or IFN-β in macrophages or DCs,
which indicated that ligation of cell surface MHC class II alone did
not induce the activation of signaling involved in the production of
inflammatory cytokines in macrophages and DCs (data not shown).
Instead, we found here that intracellular MHC class II molecules
VOLUME 12 NUMBER 5 MAY 2011 nature immunology
© 2011 Nature America, Inc. All rights reserved.
Articles
interacted with Btk via CD40 and subsequently maintained Btk activation and thereby promoted TLR signaling through interaction of
Btk with the adapters MyD88 and TRIF, but cell surface MHC class II
molecules did not.
Clinical observations have shown that HLA-DR expression
in peripheral blood monocytes is much lower in patients with
septic shock than in normal subjects 41,42. Such patients release
much less TNF and IL-1β than do normal subjects in response to
LPS. In addition, the ability of monocytes to express HLA-DR antigen correlates directly with the clinical course of trauma patients43
and septic patients44. However, treatment with IFN-γ restores HLADR expression and thus substantially enhances the induction of
TNF by LPS in vitro in such situations44. The recovery of monocyte function results in clearance of sepsis and improved survival
of the patients 44. Thus, those clinical observations, together with
our in vitro and in vivo data, demonstrate that MHC class II mol­
ecules are required for full activation of macrophages in response to
TLR ligands.
In conclusion, our study has demonstrated that intracellular MHC
class II molecules interacted with Btk and maintained Btk activation
after stimulation with TLR ligands. Activated Btk interacted with
MyD88 and TRIF, promoting the activation of MyD88-dependent and
TRIF-dependent pathway and thus leading to the enhanced production of proinflammatory cytokines and type I interferons. Therefore,
intracellular MHC class II molecules are required for TLR-triggered
full activation of macrophages and DCs. Our findings provide new
insight into the regulation of TLR-triggered inflammatory responses
and also indicate a previously unknown nonclassical role for MHC
class II molecules in innate immunity.
Methods
Methods and any associated references are available in the online version
of the paper at http://www.nature.com/natureimmunology/.
Note: Supplementary information is available on the Nature Immunology website.
Acknowledgments
We thank P. Ma, M. Jin and Y. Li for technical assistance; and N. Li, H. An,
T. Chen, S. Xu and C. Han for discussions. Supported by the National Key
Basic Research Program of China (2007CB512403), National 115 Key Project
(2008ZX10002-008, 2009ZX09503-023) and the National Natural Science
Foundation of China (30721091).
AUTHOR CONTRIBUTIONS
X.C. and X.L. designed the experiments; X.L., Z.Z., D.L., L.X., F.M., P.Z. and
H.Y. did the experiments; X.C. and X.L. analyzed data and wrote the paper; and
X.C. was responsible for research supervision, coordination and strategy.
COMPETING FINANCIAL INTERESTS
The authors declare no competing financial interests.
Published online at http://www.nature.com/natureimmunology/.
Reprints and permissions information is available online at http://npg.nature.com/
reprintsandpermissions/.
1. Takeda, K., Kaisho, T. & Akira, S. Toll-like receptors. Annu. Rev. Immunol. 21,
335–376 (2003).
2. Barton, G.M. & Medzhitov, R. Toll-like receptor signaling pathways. Science 300,
1524–1525 (2003).
3. O’Neill, L.A. & Bowie, A.G. The family of five: TIR-domain-containing adaptors in
Toll-like receptor signalling. Nat. Rev. Immunol. 7, 353–364 (2007).
4. Kawai, T. & Akira, S. TLR signaling. Semin. Immunol. 19, 24–32 (2007).
5. Marshak-Rothstein, A. & Rifkin, I.R. Immunologically active autoantigens: the role
of toll-like receptors in the development of chronic inflammatory disease.
Annu. Rev. Immunol. 25, 419–441 (2007).
6. Liew, F.Y., Xu, D., Brint, E.K. & O’Neill, L.A. Negative regulation of Toll-like
receptor-mediated immune responses. Nat. Rev. Immunol. 5, 446–458 (2005).
nature immunology VOLUME 12 NUMBER 5 MAY 2011
7. Huang, Q. et al. Differential regulation of interleukin 1 receptor and Toll-like receptor
signaling by MEKK3. Nat. Immunol. 5, 98–103 (2003).
8. Liu, X. et al. CaMKII promotes TLR-triggered proinflammatory cytokine and type I
interferon production by directly binding and activating TAK1 and IRF3 in
macrophages. Blood 112, 4961–4970 (2008).
9. Schafer, P.H., Pierce, S.K. & Jardetzky, T.S. The structure of MHC class II: a role
for dimer of dimers. Semin. Immunol. 7, 389–398 (1995).
10.McDevitt, H.O. Discovering the role of the major histocompatibility complex in the
immune response. Annu. Rev. Immunol. 18, 1–17 (2000).
11.Al-Daccak, R., Mooney, N. & Charron, D. MHC class II signaling in antigenpresenting cells. Curr. Opin. Immunol. 16, 108–113 (2004).
12.Mourad, W., Geha, R.S. & Chatila, T. Engagement of major histocompatibility
complex class II molecules induces sustained, lymphocyte functionassociated molecule 1-dependent cell adhesion. J. Exp. Med. 172, 1513–1516
(1990).
13.Spertini, F., Chatila, T. & Geha, R.S. Signals delivered via MHC class II molecules
synergize with signals delivered via TCR/CD3 to cause proliferation and cytokine
gene expression in T cells. J. Immunol. 149, 65–70 (1992).
14.Hauschildt, S., Bessler, W.G. & Scheipers, P. Engagement of major histocompatibility
complex class II molecules leads to nitrite production in bone marrow derived
macrophages. Eur. J. Immunol. 23, 2988–2992 (1993).
15.Trede, N.S., Geha, R.S. & Chatila, T. Transcriptional activation of IL-1β and tumor
necrosis factor α genes by MHC class II ligands. J. Immunol. 146, 2310–2315
(1991).
16.Cambier, J.C. & Lehmann, K.R. Ia-mediated signal transduction leads to proliferation
of primed B lymphocytes. J. Exp. Med. 170, 877–886 (1989).
17.Drenou, B. et al. Caspase-independent pathway of MHC class II antigenmediated apoptosis of human B lymphocytes. J. Immunol. 163, 4115–4124
(1999).
18.Bishop, G. Requirements of class II-mediated B cell differentiation for class II
cross-linking and cyclic AMP. J. Immunol. 147, 1107–1114 (1991).
19.Cambier, J.C. et al. Ia binding ligand and cAMP stimulate translocation of PKC in
B lymphocytes. Nature 327, 629–632 (1987).
20.Mooney, N.A., Grillot-Courvalin, C., Hivroz, C., Ju, L.Y. & Charron, D. Early
Biochemical events after MHC class II-mediated signaling on human B lymphocytes.
J. Immunol. 145, 2070–2076 (1990).
21.Lane, P.J.L., McConnell, F.M., Schieven, G.L., Clark, E.A. & Ledbetter, J.A. The
role of class II molecules in human B cell activation: association with phosphatidyl
inositol turnover, protein tyrosine phosphorylation, and proliferation. J. Immunol.
144, 3684–3692 (1990).
22.Neumann, J., Eis-Hübinger, A.M. & Koch, N. Herpes simplex virus type 1
targets the MHC class II processing pathway for immune evasion. J. Immunol. 171,
3075–3083 (2003).
23.Lapaque, N. et al. Salmonella regulates polyubiquitination and surface expression
of MHC class II antigens. Proc. Natl. Acad. Sci. USA 106, 14052–14057
(2009).
24.Piani, A. et al. Expression of MHC class II molecules contributes to lipopolysaccharide
responsiveness. Eur. J. Immunol. 30, 3140–3146 (2000).
25.Beharka, A.A., Armstrong, J.W. & Chapes, S.K. Macrophage cell lines derived from
major histocompatibility complex II-negative mice. In Vitro Cell. Dev. Biol. Anim. 34,
499–507 (1998).
26.de Weers, M. et al. B-cell antigen receptor stimulation activates the human Bruton’s
tyrosine kinase, which is deficient in X-linked agammaglobulinemia. J. Biol. Chem. 269,
23857–23860 (1994).
27.Wahl, M.I. et al. Phosphorylation of two regulatory tyrosine residues in the activation
of Bruton’s tyrosine kinase via alternative receptors. Proc. Natl. Acad. Sci. USA 94,
11526–11533 (1997).
28.Brunner, C., Avots, A., Kreth, H.W., Serfling, E. & Schuster, V. Bruton’s tyrosine kinase
is activated upon CD40 stimulation in human B lymphocytes. Immunobiology 206,
432–440 (2002).
29.Jefferies, C.A. et al. Bruton’s tyrosine kinase is a Toll/interleukin-1 receptor domainbinding protein that participates in nuclear factor κB activation by Toll-like receptor 4.
J. Biol. Chem. 278, 26258–26264 (2003).
30.Gray, P. et al. MyD88 adapter-like (Mal) is phosphorylated by Bruton’s tyrosine
kinase during TLR2 and TLR4 signal transduction. J. Biol. Chem. 281,
10489–10495 (2006).
31.Mansell, A. et al. Suppressor of cytokine signaling 1 negatively regulates Toll-like
receptor signaling by mediating Mal degradation. Nat. Immunol. 7, 148–155
(2006).
32.Horwood, N.J. et al. Bruton’s tyrosine kinase is required for lipopolysaccharideinduced tumor necrosis factor-α production. J. Exp. Med. 197, 1603–1611
(2003).
33.Mukhopadhyay, S. et al. Macrophage effector functions controlled by Bruton’s
tyrosine kinase are more crucial than the cytokine balance of T cell responses for
microfilarial clearance. J. Immunol. 168, 2914–2921 (2002).
34.Bonnefoy, J.Y. et al. The low-affinity receptor for IgE (CD23) on B lymphocytes
is spatially associated with HLA-DR antigens. J. Exp. Med. 167, 57–72 (1988).
35.Bradbury, L.E. et al. The CD19/CD21 signal transducing complex of human
B lymphocytes includes the target of antiproliferative antibody-1 and Leu-13
molecules. J. Immunol. 149, 2841–2850 (1992).
36.Léveillé, C., AL-Daccak, R. & Mourad, W. CD20 is physically and functionally
coupled to MHC class II and CD40 on human B cell lines. Eur. J. Immunol. 29,
65–74 (1999).
423
Articles
41.Appel, S.H., Wellhausen, S.R., Montgomery, R., DeWeese, R.C. & Polk, H.C. Jr.
Experimental and clinical significance of endotoxin-dependent HLA-DR expression
on monocytes. J. Surg. Res. 47, 39–44 (1989).
42.Astiz, M., Saha, D., Lustbader, D., Lin, R. & Rackow, E. Monocyte response to
bacterial toxins, expression of cell surface receptors, and release of anti-inflammatory
cytokines during sepsis. J. Lab. Clin. Med. 128, 594–600 (1996).
43.Hershman, M.J., Cheadle, W.G., Wellhausen, S.R., Davidson, P.F. & Polk, H.C. Jr.
Monocyte HLA-DR antigen expression characterizes clinical outcome in the trauma
patient. Br. J. Surg. 77, 204–207 (1990).
44.Docke, W.D. et al. Monocyte deactivation in septic patients: restoration by IFN-γ
treatment. Nat. Med. 3, 678–681 (1997).
© 2011 Nature America, Inc. All rights reserved.
37.Léveillé, C., Chandad, F., Al-Daccak, R. & Mourad, W. CD40 associates with the
MHC class II molecules on human B cells. Eur. J. Immunol. 29, 3516–3526
(1999).
38.Harton, J.A., Van Hagen, A.E. & Bishop, G.A. The cytoplasmic and transmembrane
domains of MHC class II β chains deliver distinct signals required for MHC class IImediated B cell activation. Immunity 3, 349–358 (1995).
39.Harton, J.A. & Bishop, G.A. Length and sequence requirements of the cytoplasmic
domain of the Aβ molecule for class II-mediated B cell signaling. J. Immunol. 151,
5282–5289 (1993).
40.Frei, R. et al. MHC class II molecules enhance Toll-like receptor mediated innate
immune responses. PLoS ONE 5, e8808 (2010).
424
VOLUME 12 NUMBER 5 MAY 2011 nature immunology
© 2011 Nature America, Inc. All rights reserved.
ONLINE METHODS
Mice and reagents. Mice homozygous for deletion of all genes encoding classical MHC class II (B6.129S-H2dlAb1-Ea; Mouse Genome Informatics accession code, 003584), Btk-deficient mice (B6.129S-Btktm1Wk/J; Mouse Genome
Informatics accession code, 002536) and Cd40-deficient mice (B6.129P2Cd40tm1Kik/J; Mouse Genome Informatics accession code, 002928) were
from Jackson Laboratories and were bred in specific pathogen–free conditions. Littermate mice 6 weeks of age were used (matched for body weight
and sex). All animal experiments were in accordance with the National
Institute of Health Guide for the Care and Use of Laboratory Animals, with the
approval of the Scientific Investigation Board of the Second Military Medical
University, Shanghai. LPS (E. coli 0111:B4), CpG ODN and poly(I:C) have
been described45. E. coli 0111:B4 was obtained from the China Center for
Type Culture Collection. LFM-A13 was from Cayman Chemical. Recombinant
MBP was from Upstate Biotechnology. Recombinant MKK4 was from Merck.
Antibody to MHC class II (107610) was from BioLegend. Recombinant IRF3
and anti-TRIF (ab13810), anti-Btk (ab25971), anti-CD40 (ab13545), antiTLR4 (ab22048), anti-TLR3 (ab62566), anti-TLR9 (ab52967) and antibody
to Btk phosphorylated at Tyr222 (ab51210) or Tyr550 (ab52192) were from
Abcam. Anti-IRAK1 (D51G7), anti-TBK1 (D1B4), anti-IRF3 (D83B9), antihemagglutinin (6E2), anti-EEA1 (2411), anti-Erk (9102), anti-Jnk (56G8),
anti-p38 (9212) and antibodies to Erk phosphorylated at Thr202-Tyr204
(E10), to Jnk phosphorylated at Thr183-Tyr185 (G9), to p38 phosphorylated
at Thr180-Tyr182 (9211), to IRF3 phosphorylated at Ser396(4D4G) or to IκBα
phosphorylated at Ser32-Ser36 (5A5) were from Cell Signaling Technology.
Anti-MyD88 (3244-100) was from BioVision. Anti–lamin A (133A2) and
anti-β-actin (sc-130656) were from Santa Cruz. Anti-Flag (M2) was from
Agilent Technologies.
Plasmid constructs. Recombinant vectors encoding mouse MHC class II
α-chain (NM_010378.2) or β-chain (NM_207105.2), TRIF (BC094338),
MyD88 (NM_010851) or Btk (NM_013482.2; GenBank accession numbers
in parentheses) and mutants thereof were constructed by PCR-based amplification from cDNA of mouse macrophages and then were subcloned into
the pcDNA3.1 eukaryotic expression vector (Invitrogen) as described45. All
constructs were confirmed by DNA sequencing. Luciferase reporter plasmids
for NF-κB, AP-1, IRF3 and IRF7 have been described45,46.
Cell culture and transfection. Bone marrow–derived DCs from C57BL/6J
mice were generated as described46. The HEK293 cell line (American
Type Culture Collection) was transfected with JetPEI reagents (PolyPlus).
Thioglycollate-elicited mouse peritoneal macrophages were prepared and
cultured in endotoxin-free RPMI-1640 medium with 10% (vol/vol) FCS
(Invitrogen) as described46 and were transfected by nucleofection with a
Mouse Macrophage Nucleofector kit (Amaxa).
RNA-mediated interference. The sequences of siRNA targeting MHC
class II β-chain and Btk were 5′-CCACACAGCTTATTAGGAA-3′ and
5′-GGAGTCTAGTGAAATGGAA-3′, respectively; the control siRNA
sequence was 5′-TTCTCCGAACGTGTCACGT-3′. The siRNA duplexes were
transfected into mouse peritoneal macrophages with INTERFERin reagent
(Polyplus) according to a standard protocol.
Cytokine detection. TNF, IL-6 and IFN-β in supernatants and serum were
measured with ELISA kits (R&D Systems).
RNA quantification. A LightCycler (Roche) and SYBR RT-PCR kit (Takara)
were used for quantitative real-time RT-PCR analysis as described45. Data were
normalized to β-actin expression.
Assay of luciferase reporter gene expression. HEK293 cells or mouse macrophages were transfected with a mixture of the appropriate luciferase reporter
plasmid, pRL-TK-renilla-luciferase plasmid and the appropriate additional
constructs. The total amount of plasmid DNA was made equal by the addition
of empty control vector. After 24 h or 36 h, cells were left untreated or were
treated with LPS, CpG ODN or poly(I:C). Luciferase activity was measured
doi:10.1038/ni.2015
with a Dual-Luciferase Reporter Assay System according to the manufacturer’s
instructions (Promega). Data were normalized for transfection efficiency by
the division of firefly luciferase activity with that of renilla luciferase.
Immunoprecipitation and immunoblot analysis. Cells were lysed with cell
lysis buffer (Cell Signaling Technology) supplemented with protease inhibitor
‘cocktail’. Protein concentrations in the extracts were measured by BCA
assay (Pierce). Immunoprecipitation and immunoblot analysis were done
as described45,46.
Nanospray liquid chromatography–tandem mass spectrometry.
Macrophages (3 × 108) were stimulated for 15 min with LPS and then were
lysed for immunoprecipitation with antibody to MHC class II. Proteins were
eluted and digested, followed by analysis by reverse-phase nanospray liquid
chromatography–tandem mass spectrometry. The spectra from tandem mass
spectrometry were automatically used for searching against the nonredundant
International Protein Index mouse protein database (version 3.72) with the
Bioworks browser (rev.3.1).
In vitro kinase assay. Proteins in total cell extracts (100 µg) were immunoprecipitated with the appropriate antibody, and kinase activity was measured
as described45.
Confocal microscopy. Macrophages plated on glass coverslips in six-well
plates were left unstimulated or stimulated with LPS, then were labeled with
antibody to MHC class II, anti-CD40, anti-Btk, anti-TLR4, anti-TLR3, antiTLR9 or anti-EEA1 (endosome marker). Cells were viewed with a Leica TCS
SP2 confocal laser microscope.
Establishment of endotoxin shock model and bacterial sepsis model. The
endotoxin shock mouse model was established by intraperitoneal injection of
LPS (15 mg per kg body weight) as described45. E. coli 0111:B4 in midlogarithmic growth were collected and concentrations were measured by counting of
viable bacteria on agar plates. For injection, bacteria were washed twice with
nonpyrogenic PBS. Mice were injected intraperitoneally with 0.5 ml bacteria
suspension (1 × 107 colony-forming units)47.
Bone marrow transplantation. Bone marrow cells (1 × 107) from H2+/+ or
H2−/− mice were transplanted into lethally irradiated wild-type C57BL/6J
mice (cumulative dose, 10 Gy) by injection into the tail vein. After 3 weeks,
CD4+ T cells in spleen and lymph nodes were counted and expression of MHC
class II on macrophages and DCs was analyzed by flow cytometry.
Macrophage reconstitution. Bone marrow cells from H2+/+ or H2−/− mice
were cultured for 7 d in mouse macrophage colony-stimulating factor
(50 ng/ml; PeproTech) for the preparation of bone marrow–derived macrophages. Clodronate liposomes (Sigma) were injected intraperitoneally into
wild-type mice (50 mg in 200 µl per mouse) for the depletion of endogenous
macro­phages. Then, 2 d later, H2+/+ or H2−/− bone marrow–derived macrophages
(1 × 107) were transplanted (by injection into the tail vein) into the mice
depleted of macrophages, followed 6 h later by challenge with LPS48.
Statistical analysis. The statistical significance of comparisons between two
groups was determined with Student’s t-test. The statistical significance of
survival curves were estimated according to the method of Kaplan and Meier,
and curves were compared with the generalized Wilcoxon test. P values of less
than 0.05 were considered statistically significant.
45.Wang, C. et al. The E3 ubiquitin ligase Nrdp1 ‘preferentially’ promotes TLRmediated production of type I interferon. Nat. Immunol. 10, 744–752 (2009).
46.An, H. et al. Phosphatase SHP-1 promotes TLR- and RIG-I-activated production of
type I interferon by inhibiting the kinase IRAK1. Nat. Immunol. 9, 542–550
(2008).
47.Haziot, A. et al. Resistance to endotoxin shock and reduced dissemination of gramnegative bacteria in CD14-deficient mice. Immunity 4, 407–414 (1996).
48.Han, C. et al. Integrin CD11b negatively regulates TLR-triggered inflammatory
responses by activating Syk and promoting degradation of MyD88 and TRIF via
Cbl-b. Nat. Immunol. 11, 734–742 (2010).
nature immunology