Alterations in Cardiac Gene Expression During the Transition From
advertisement

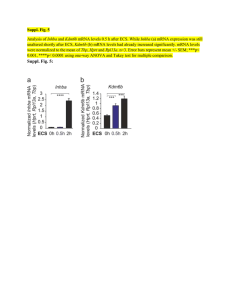
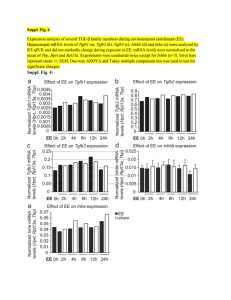
23 Alterations in Cardiac Gene Expression During the Transition From Stable Hypertrophy to Heart Failure Marked Upregulation of Genes Encoding Extracellular Matrix Components Marvin 0. Boluyt, Lydia O'Neill, Andrea L. Meredith, Oscar H.L. Bing, Wesley W. Brooks, Chester H. Conrad, Michael T. Crow, Edward G. Lakatta Abstract The failing heart is characterized by impaired cardiac muscle function and increased interstitial fibrosis. Our purpose was to determine whether the functional impairment of the failing heart is associated with changes in levels of mRNA encoding proteins that modulate parameters of contraction and relaxation and whether the increased fibrosis observed in the failing heart is related to elevated expression of genes encoding extracellular matrix components. We studied hearts of 18- to 24-month-old spontaneously hypertensive rats with signs and symptoms of heart failure (SHR-F) or without evidence of failure (SHR-NF) and of age-matched normotensive WistarKyoto (WKY) rats. Compared with WKY rats, SHR-NF exhibited left ventricular (LV) hypertrophy (2.2-fold) and right ventricular (RV) hypertrophy (1.5-fold), whereas SHR-F were characterized by comparable LV hypertrophy (2.1-fold) and augmented RV hypertrophy (2.4-fold; all P<.01). Total RNA was isolated from ventricles and subjected to Northern blot analysis. In SHR-F hearts, the level of a-myosin heavy chain mRNA was decreased in both ventricles to 1/3 and '/s of the SHR-NF and WKY values, respectively (both P< .01). Levels of ,l-myosin heavy chain, a-cardiac actin, and myosin light chain-2 mRNAs were not significantly altered in hearts of SHR-NF or SHR-F. Levels of a-skeletal actin were twofold greater in SHR-NF hearts compared with WKY hearts and were intermediate in SHR-F hearts. Levels of atrial natriuretic factor (ANF) mRNA were elevated threefold in the LV of SHR-NF (P<.05) but were not significantly increased in the RV of SHR-NF compared with WKY rats. During the transition to failure (SHR-F versus SHR-NF), ANF mRNA levels increased an additional 1.6-fold in the LV and were elevated 4.7-fold in the RV (both P<.05). Levels of sarcoplasmic reticulum Ca2ATPase (SRCA) mRNA were maintained in the LV of hypertensive and failing hearts at levels not significantly different from WKY values. In contrast, the level of RV SRCA mRNA was 24% less in SHR-NF compared with WKY rats, and during the transition to failure, this difference was not significantly exacerbated (29% less than the WKY value). The levels of fibronectin and pro-al(I) and pro-al(III) collagen mRNAs were not significantly elevated in either ventricle of the SHR-NF group but were fourfold to fivefold higher in both ventricles of SHR-F (all P<.05). The increase in fibronectin gene expression was at least partially explained by an elevation in the level of the EIILA-containing isoform, an alternatively spliced variant expressed during wound healing and pressure overload hypertrophy. Transforming growth factor-fl (TGF-fl1) mRNA abundance was not elevated in ventricles of SHR-NF but increased 1.3-fold in the LV and twofold in the RV during the transition to heart failure compared with SHR-NF values (both P<.05). The decrease in a-myosin heavy chain mRNA levels in SHR-F hearts represents a pretranslational basis for the slowed contraction previously observed in cardiac muscle from these hearts. The survey of specific contractile protein mRNAs provides no evidence of a downregulation of these genes during the transition to heart failure. The increase in fibronectin and collagen mRNA levels suggests that the previously observed increase in interstitial fibrosis in cardiac muscles of failing hearts is regulated at the level of gene expression. The increase in abundance of TGF-,f1 mRNA in conjunction with the upregulation of fibronectin and collagen genes suggests that activation of TGF-fl1 gene expression may be a mechanism initiating interstitial fibrosis during the transition from stable hypertrophy to failure. (Circ Res. 1994;75:23-32.) Key Words * heart failure * spontaneously hypertensive rats * myosin heavy chain * myosin light chain * a-actin * sarcoplasmic reticulum Ca`2-ATPase * fibronectin . collagen * transforming growth factor-fl linically diagnosed heart failure is a progressive disease with a poor prognosis.' Heart failure with hypertension.2 The hypertrophied heart that subsequently develops failure is characterized by altered hemodynamics,3 impaired cardiac muscle function,4 6 and increased fibrosis.7,8 Although cardiac hypertrophy is commonly associated with heart failure,' it is widely recognized as an adaptive response that normalizes wall stress and compensates for an increased load.9 When the load is chronically elevated for an extended period of time, such as in chronic hypertension, compensated hypertrophy may progress to pump failure. One difficulty in studying the development of heart failure has been the lack of a well-characterized animal model that C has many etiologies but is commonly associated Received July 19, 1993; accepted March 1, 1994. From the Laboratory of Cardiovascular Science, Gerontology Research Center, National Institutes of Health, Baltimore, Md; and the Department of Medicine, Boston Veterans Affairs Medical Center (Mass). Correspondence to Marvin 0. Boluyt, PhD, Laboratory of Cardiovascular Science, Gerontology Research Center, Room 3-E-10, 4940 Eastern Ave, Baltimore, MD 21224. © 1994 American Heart Association, Inc. 24 Circulation Research Vol 75, No 1 July 1994 clearly exhibits a transition from compensated hypertrophy to failure. The spontaneously hypertensive rat (SHR) has been found to develop impaired myocardial function after a period of stable hypertrophy. Trippodo and Frohlich10 have summarized the evidence supporting the use of the SHR as a model of human heart disease and heart failure. The intrinsic myocardial properties of these animals have been well characterized in terms of functional and morphological features.611-'13 Although the mechanism(s) that contributes to the transition from compensated cardiac hypertrophy to heart failure has remained obscure, several hypotheses have been formulated. There is evidence to suggest that a loss of contractile protein from the myocardium may contribute to the impaired function observed in cardiac muscle from failing human hearts.14 Myocyte dropout due to myocardial cell death and hypertrophy of the remaining viable myocytes has been proposed to account for impaired function and failure during aging and hypertension.15-17 Since left ventricular (LV) mass of SHR increases progressively with age and does not diminish during failure as myocytes are lost, additional nascent hypertrophy of surviving myocytes may occur. Increased expression of muscle-specific genes such as a-skeletal actin, which is transiently upregulated during hypertrophy,18 would constitute evidence in support of this hypothesis. Hypertrophied and, particularly, failing hearts are characterized by an accumulation of extracellular matrix proteins and a corresponding increase in cardiac muscle stiffness.78 Since fibronectin and collagen types I and III are major components of the interstitial fibrillar network, it has been hypothesized that upregulation of genes encoding these components by fibroblasts accounts, in part, for the increase in fibrosis observed during the transition to failure and contributes to the decline in contractile performance.8 Of particular interest is the fibronectin mRNA-splicing variant encoding the EIIIA segment. This isoform is expressed during wound healing,19 embryogenesis,20 and pressure-overload hypertrophy.2' The purpose of this investigation was to determine whether there are alterations in expression of genes that code for proteins potentially involved in functional impairment observed in the myocardium of SHR with signs and symptoms of heart failure (SHR-F). To differentiate alterations in gene expression associated with hypertrophy from those affiliated with failure, we compared relative mRNA levels in hearts of three agematched groups: normotensive Wistar-Kyoto (WKY) rats, hypertensive rats without failure (SHR-NF), and SHR-F. Since the increased hemodynamic load imposed on the heart exerts its primary effect on the LV but may impact the right ventricle (RV) significantly during failure, we measured relative mRNA levels in the RV and LV. Specifically, we studied the mRNA levels of several contractile proteins, including and ,B-myosin heavy chain (a- and ,B-MHC, respectively), a-cardiac actin, and myosin light chain-2 (MLC2) to investigate the possibility that a generalized paucity of contractile protein mRNAs could contribute to the observed contractile deficits and to determine whether a pretranslational basis exists for the myosin isoform shift. The levels of a-skeletal actin and and ,B-MHC a- a- mRNA were studied as markers of cardiac hypertrophy to determine whether there was any basis for nascent hypertrophy in hearts with chronic hypertension and failure. Atrial natriuretic factor (ANF) gene expression was studied because it has been considered to be one of several criteria indicating the initiation of a pathological response.2 Since previous studies have shown a decrease in sarcoplasmic reticulum Ca2+-ATPase (SRCA) gene expression in hypertrophied heart23 and in hearts of human patients with heart failure,24 we investigated the levels of SRCA in hearts of rats undergoing a transition from stable hypertrophy to failure. To determine whether increased expression of fibroblast-specific genes underlies the increase in fibrosis previously observed in failing hearts, we measured relative levels of fibronectin and collagen mRNAs. Since the elaboration of extracellular matrix by fibroblasts is influenced by transforming growth factor-n (TGF-13)25 and since pressure-overload cardiac hypertrophy is associated with an increase in TGF-,1 ,21 we also studied the levels of TGF-f,1 mRNA. Materials and Methods Animals Male retired breeder SHR and WKY rats (6 to 9 months old) were purchased from Taconic Farms, Inc, and boarded in the animal facility at the Boston Department of Veterans Affairs Medical Center until the time of study (18 to 24 months of age). Beginning at 18 months of age, rats were monitored for evidence of rapid labored respiration and studied within 1 week of identification.6 At autopsy, animals were examined for pleural/pericardial effusions, atrial thrombi, and RV hypertrophy. Several SHR with no findings other than RV hypertrophy were excluded from the study. Individual chambers were quickly dissected, and chamber weights were recorded. LV, lung, and liver weights were determined before and after drying sections of these tissues in an oven at 60WC.6 Cardiac tissue samples were frozen within minutes of the death of the animal and stored in liquid nitrogen until studied. RNA Analysis RNA was isolated from LV and RV by the method of Chomczynski and Sacchi.26 Ten micrograms of total RNA was size-fractionated by electrophoresis through 1% agarose gels, transferred electrophoretically at 5 V/cm to a nylon (Duralon) membrane, and hybridized with "2P-radiolabeled probes overnight at 63.5°C for cDNA probes and 60°C for oligonucleotide probes.27 Hybridization intensity was quantified in disintegrations per minute directly from blots with a Betascope 603 (Betagen Corp). This apparatus contains an electronic sensor that responds to beta radiation from all areas of the blot directly with an efficiency of at least 15%. Signals visualized on computer screen were identified by position relative to 18S and 28S rRNA migration, delineated by 9x9-mm rectangles, and quantified. Each blot was subsequently stripped and reprobed. The signal from each sample was normalized to the signal obtained with a probe specific for the 18S ribosomal RNA. Probes Complementary DNA probes were synthesized from a template by the random-prime method.2829 The templates for the a-cardiac actin, a-skeletal actin, and ANF probes were 180- to 700-bp cDNA sequences, which were obtained by polymerase chain reaction (PCR) with primers complementary to the published sequences for rat mRNA.30-32 The PCR-generated probe sequences were verified by DNA sequence analysis. The fibronectin probe was a 2.2-kb prod- Boluy et al Gene Expression in the Failing Heart uct of an EcoRI digest of the 3-kb pRCabFN2 clone generously supplied by K. Boheler. This probe does not distinguish between alternatively spliced fibronectin mRNA variants. To identify EIIIA+ fibronectin mRNA, an oligonucleotide specific for this segment was constructed with the following sequence: 5YCCACCGTGCAAGGCAACCACACTGACTGTGTACTCAG3' . The probes for pro-al(I) and proal(III) collagen were cDNAs kindly provided by M.-L. Chu.34-35 The probe for TGF-lI was generously provided by M. Sporn.36 The probes for c-MHC, l3-MHC, and the 18S ribosomal RNA were end-labeled synthetic oligonucleotides.37 The probe for cardiac SRCA was also a synthetic end-labeled oligonucleotide complementary to the terminal 33 bases of the coding portion of the rat gene38 with the following sequence: 5' CTC CAG TAT TGC AGG CTC 25 TABLE 1. Biometric Data of Wistar-Kyoto Rats and Rats Without and With Heart Failure WKY (n=12) 20.2+0.3 Age, mo BW, g LVW, g RVW, g LVW/BW, mg/g SHR-NF (n=12) 19.6+0.4 SHR-F (n=16) 19.4+0.6 Results 372+20* 382+12* 1 .40 + 0.08 1.38 +0.05 0.26±0.02* 0.44+0.02*t 3.78+0.13* 3.66±0.13* RVW/BW, mg/g 0.70±0.03* 1.14+0.04*t LV W/D 4.70+0.03 4.85+0.04*t Liver W/D 3.32±0.03 3.52+t0.07*t Lung W/D 5.62±.020 5.48+0.06 WKY indicates Wistar-Kyoto rats; SHR-NF, spontaneously hypertensive rats (SHR) without heart failure; SHR-F, SHR with heart failure; BW, body weight; LVW, left ventricular (LV) wet weight; RVW, right ventricular (RV) wet weight; and W/D, wet weight-to-dry weight ratios (g/g). Values are mean-SEM. *P<.01 vs WKY; tP<.01 vs SHR-NF. Biometric and Clinical/Pathological Data Body weight of both SHR-NF and SHR-F was '==50% of the age-matched WKY rats for this cohort of rats (Table 1). LV weight was similar for all three groups. The LV weight-to-body weight ratio in SHR-NF and SHR-F was more than twofold greater than the WKY value. There was no difference in the magnitude of LV hypertrophy in SHR-F compared with SHR-NF. The RV weight-to-body weight ratio was elevated 49% in SHR-NF compared with WKY rats and was an additional 63% greater in SHR-F compared with SHR-NF. Thus, the transition from stable hypertrophy to heart failure in SHR was characterized by a marked augmentation of hypertrophy in the RV but no additional LV hypertrophy. Among the SHR-F, 100% had visibly detectable fibrosis, 69% exhibited pleural effusion, 81% were iden- tified with atrial thrombi, and 94% had rapid/labored respiration. The LV wet weight-to-dry weight ratio was slightly elevated in SHR-F compared with WKY and SHR-NF values (Table 1). The liver wet weightto-dry weight ratio was significantly elevated in the SHR-F group, suggesting elevated right-side filling pressures. Lung wet weight-to-dry weight ratios were not different among the groups, indicating that the lung may be protected against fluid accumulation during elevated hemodynamic pressures, as suggested by Erdmann et al.39 Findings consistent with the presence of heart failure are consonant with previous studies of the SHR.6,11-13 Contractile Protein mRNA Levels Previous studies of contractile function in the myocardium of these rats indicated impaired muscle func- CAG GTA GTT TCG GGC 3. Statistical Analysis One-way ANOVA was used to evaluate differences among the three groups, and post hoc comparisons between groups were performed by Tukey's procedure. Differences were considered significant at P<.05. 721-+-26 1.23-+0.04 0.34+0.01 1.72±0.03 0.47+0.01 4.57±0.03 3.26+0.03 5.77+0.27 LV a-MHC- flpe*neem..nc_m. 18SLane 1 l 2 3 4 5 6 7 8 9 10 11 1213 14 1L5 16 WKY SHR-Fl SHR-NF- 14 T LV 12 0U 10 C) 8 MM** %*"m RV r 6t * * 4 FIG 1. a-Myosin heavy chain (a-MHC) mRNA levels in hearts of Wistar-Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR- F). Top, Autoradiograph of Northern blot with total RNA from left ventridcles (LVs) hybridized with an oligonucleotide probe specific for a-MHC. Signals were quantified on a Betascope 603, followed by autoradiography. Membranes were subsequently stripped and hybridized with an oligonucleotide probe for the 18S ribosomal RNA. Bottom, Bar graphs showing Northern blot data for LV and right ventricle (RV). Differences in loading were corrected by normalizing the signal to that obtained for 18S ribosomal RNA from the same lane. Values are mean-+-SEM for 8 to 12 samples per group. Values represent arbitrary units; the a-MHC value for the LV of the SHR-F group was arbitrarily set at 1.00, and the remaining values were adjusted correspondingly. **P<.01 vs SHR-NF by ANOVA and Tukey's procedure. 2 SHR-F SHR-F 26 Circulation Research Vol 75 No 1 July 1994 LV 8-MHC- on 18S- Lane s- _~ 0 a" mt em- IN t 2 3 4 5 6 WKY-J I FIG 2. p-Myosin heavy chain (,B-MHC) mRNA levels in hearts of Wistar Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR-F). Top, Northern blot analysis with an oligonucleotide probe specific for f-MHC. Bottom, Bar graphs showing Northern blot data. Differences in loading were corrected by normalizing the signal to that obtained for 18S ribosomal RNA from the same lane. Values are mean+SEM for 8 to 12 samples per gop 7 8 9 10 11 1213 14 SHR-W-F 15 16 -SHR-F---l- 3- RV LV U) CD ua group. Values represent arbitrary units; the p-MHC value for the left ventricle (LV) of the WKY group was arbitrarily set at 1.00, and the remaining values were adjusted correspondingly. RV indicates right ventricle. 2 -T- I r 1- o SHR-NF SHR-F WKY SHR-NF tion and an MHC shift in favor of the f3-isoform during the transition from stable hypertrophy to failure.6 In the present study, heart failure was associated with a decrease in a-MHC mRNA in both ventricles. Compared with the WKY value, the LV level of a-MHC mRNA was not significantly different in the ventricles of SHR-NF but decreased in the LV of SHR-F to less than one third of the SHR-NF value (Fig 1). Although a-MHC mRNA levels were :"2.5 -fold higher in the RV than in the LV of all groups (P<.05 by paired t test), the relative loss in the SHR-NF was similar (Fig 1). Levels of ,B-MHC were not significantly upregulated but remained comparable to the WKY values in ventricles of both SHR-F and SHR-NF and were comparable in both the LV and RV (Fig 2). Given the interanimal variability in f3-MHC mRNA levels and the size of the sample reported here (n=10 to 12 per group), an increase of less than twofold would be statistically undetectable at the 95% confidence level (power analysis).41n The LV levels of a-cardiac actin and MLC2 mRNAs were not significantly altered during hypertension or failure (Table 2). It should be noted that given the variability and sample size (n=5 or 6 per group), the smallest difference detectable at the 95% confidence level would be a 37% decrease for a-cardiac actin and a 55% decrease for MLC2. LV levels of a-skeletal actin mRNA were twofold greater in hearts of the SHR-NF compared with the WKY group and were intermediate in the SHR-F group (Table 2). ANF mRNA Levels Elevated levels of ANF mRNA were present in both ventricles of failing hearts. Steady-state levels of ANF mRNA were elevated threefold in the LV of SHR-NF compared with WKY rats but were not significantly increased in the RV (Table 2). In SHR-F, ANF mRNA levels were increased an additional 1.6-fold in the LV relative to SHR-NF levels and were incremented 4.7fold in the RV. ANF mRNA abundance was 2.5- to SHR-F 9-fold greater in the LV compared with the RV (P<.05). SRCA mRNA Levels Levels of SRCA mRNA were maintained in the LV of hypertensive and failing hearts at levels not significantly different from WKY values (Fig 3). Given the sample size of five or six per group and the variability observed, the smallest change detectable in the LV at the 95% confidence level would be a 40% decrease. In contrast, the level of RV SRCA mRNA was 24% less in SHR-NF compared with WKY rats, and during the transition to failure, this decrease was not significantly exacerbated (29% less than the WKY value). TABLE 2. Atrial Natriuretic Factor, a-Cardiac Actin, a-Skeletal Actin, and Myosin Light Chain-2 Gene Expression in Hearts of Wistar-Kyoto Rats and Spontaneously Hypertensive Rats Without and With Heart Failure WKY SHR-NF SHR-F LV RV 1.00+0.34 0.21 +.05 3.21+0.45* 0.35+0.06 5.19±0.39*t LV 1.00+0.10 2.26+0.26* 1.63+0.21 LV 1.00+0.15 0.81±0.12 0.94±0.10 ANF 2.01 0.43*t SK CA MLC2 LV 1.00 +0.26 1.02 +0.24 0.91±0.17 WRY indicates Wistar Kyoto rats; SHR-NF, spontaneously hypertensive rats (SHR) without heart failure; SHR-F, SHR with heart failure; ANF, atrial natriuretic factor; LV, left ventricle; RV, right ventricle; SK, a-skeletal actin; CA, a-cardiac actin; and MLC2, myosin light chain-2. Values are mean-+-SEM for 5 to 14 samples per group. *PC.<5 vs WKY; tP<.05 vs SHR-NF. Boluyt et al Gene Expression in the Failing Heart LV 27 EIIIAA SRCA Ufl"P 1 8 S- Lane 18SLane RV 1.4 WKY SHR-NF SHR-F WKV Levels of sarcoplasmic reticulum Ca2 7 8 9 10 11 1213 14 15 SHR-FW L A F SHR-NF-FIG 5. Autoradiogram of Northern blot analysis showing levels of EIIIA+ fibronectin mRNA in the left ventricle of Wistar-Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR-F). The blot was probed with an oligonucleotide specific for the EIIIA segment of fibronectin mRNA. The blot was subsequently stripped and probed for the 1 8S ribosomal RNA, indicating approximately equivalent loading of lanes. Betascope analysis indicates a threefold to fivefold increase in levels of EIIIA+ fibronectin in SHR-F compared with SHR-NF and WKY rats. However, quantification must be interpreted with caution, since the WKY and SHR-NF values were barely distinguishable from the background signal. L indicates 20 gg of rat liver RNA (positive for fibronectin but negative for EIIIA+ fibronectin33); A, 20 gg of atrial RNA (positive for EIIIA+ fibronectin41); and F, 10 gg of neonatal rat cardiac fibroblast RNA. 1 2 3 4 5 6 7 8 9 10 11 1213 14 WKYSHR-F SHR-NF-^J FIG 3. 1 2 3 4 5 6 L-WKYJ I fhlf SHR-NF SHR-F -ATPase (SRCA) mRNA in the ventricles of Wistar-Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure analysis for the (SHR-F). Top, Autoradiogram of Northern blot left ventricle (LV). Blots were probed with an EIIIA-containing isoform (Fig 5). Pro-al(I) and proal(IIJ) collagen mRNA levels in the LV and RV of oligonucleotide specific for the cardiac SRCA. Bottom, Bar graphs showing mean+SEM of five or six determinations from each SHR-F were also elevated threefold to fourfold over WKY and SHR-NF values (Figs 6 and 7). Although the levels of pro-al (I) and pro-al(III) collagen mRNAs did not differ between the LV and RV, fibronectin mRNA abundance was twofold to fourfold greater in the LV than in the RV (P<.05). Levels of TGF-f31 mRNA did not differ between SHR-NF and WKY rats in either ventricle. However, there was a small but significant increase in TGF-f3 mRNA levels in both ventricles of SHR-F (Fig 8). Despite a nearly fourfold higher level of TGF-P3 gene expression in the LV compared with the RV (P<.05), the magnitude of the increment exhibited during the transition to heart failure was similar in both ventricles. group for the LV and seven determinations per group for the right ventricle (RV) by Northern blot analysis. Values represent arbitrary units; the WKY values were set at 1 .00 for each ventricle, and the remaining values were adjusted accordingly. *Pc.05 vs WKY rats by ANOVA and Tukey's procedure. Extracellular Matrix-Associated mRNA Levels Levels of fibronectin and collagen mRNAs were increased in both ventricles of failing hearts. The levels of fibronectin mRNA were not significantly elevated either ventricle of the SHIR-NE in group but were fourfold to fivefold higher in both ventricles of SHR-F (Fig 4). The increase in fibronectin gene expression was at least partially explained by an elevation in the level of the LV FN- S. 18S- * W lsr T LV i z E RV [ 10 0 c io FIG 4. Levels of fibronectin mRNA in ventricles of WistarKyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR-F). Top, Autoradiogram of Northern blot analysis. Blots were probed with a cDNA probe for rat fibronectin. Bottom, Bar graphs showing data from Northern blot. Values are mean+SEM of 8 to 11 samples per group. Values represent arbitrary units; the WKY left ventricular (LV) value was set at 1.00, and the remaining values were adjusted accordingly. RV indicates right ventricle. **P<.05 vs SHR-NF by ANOVA and Tukey's procedure. wW t w 1 2 3 4 5 6 7 8 9 10 11 1213 14 15 16 WKY- SHR-NF SHR F Lane 0 flflWflW * 5 U. WKY SKR-NF SHR-F WKY SHR-NF * 28 Circulation Research Vol 75, No 1 July 1994 LV C1- 18S. meOn . -4 *b*nfl e * t1 ' 00 qo 1 2 3 4 5 6 7 8 9 10 11 1213 14 15 16:17 18 x SHR-W---WKY SHR-Fl Lane $ LV z E E RV -F 4 * * S FIG 6. Levels of pro-al (1) collagen mRNA in ventricles of Wistar-Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR-F). Top, Autoradiogram of Northern blot analysis. Blots were probed with a cDNA probe for rat fibronectin. Bottom, Bar graphs showing data from Northern blot. Values are mean-+-SEM of 6 to 13 samples per group. Values represent arbitrary units; the WKY left ventricular (LV) value was set at 1.00, and the remaining values were adjusted accordingly. RV indicates right ventricle. **P<.05 vs SHR-NF by ANOVA and Tukey's procedure. c 2 S I U t Di WKY SHR-NF nnm-r Discussion mRNA levels but no increase in levels of ca-skeletal actin mRNA (which was increased in SHR-NF compared with WKY rats). There was no significant decrease in SRCA mRNA levels in either ventricle during the transition to failure. The most striking characteristic distinguishing failing hearts from nonfailing hearts of hypertensive rats was a threefold to fivefold increase in fibronectin and collagen mRNAs in both ventricles. The marked increase in mRNAs encoding extracellular matrix component proteins in failing hearts was accompanied by a small but significant elevation in TGE-j3, mRNA, suggesting that increased expression of the TGF-f1 gene may be a mechanism contributing to the elaboration of extracellular matrix and deterioration of function that characterize the failing heart. The transition from compensated hypertrophy to heart failure in the SHR is associated with augmented RV hypertrophy, no additional LV hypertrophy, impaired LV muscle function,6" 12 and marked alterations in the expression of both myocyte-specific and fibroblast-specific genes. The present results document a significant loss of a-MHC mRNA from both ventricles of failing hearts, with no significant change in 3-MHC mRNA levels. There was no evidence of a generalized decrease in LV contractile protein mRNA levels during failure, because the abundance of a-cardiac actin and MLC2 mRNA was maintained at values similar to those of nonfailing and nonhypertensive control hearts. Failing hearts exhibited a biventricular increase in ANF LV 0 C3- 18S - Lane 0 1 n tl 7 8 9 10 11 12 13 14 1S 16 17 18 l SHR-F- -J s SHR-NF-- 1 2 3 4 5 6 ---WKY--l l * * 6 LV (o RV T 5 .4 z E * * 4 3 0 c ci 2 OL WKY SHR-NF SHR-F WKY SH FIG 7. Levels of pro-al(lIl) collagen mRNA in ventricles of Wistar-Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR-F). Top, Autoradiogram of Northern blot analysis. Blots were probed with a cDNA probe for rat fibronectin. Bottom, Bar graphs showing data from Northern blot. Values are mean±SEM of four to seven samples per group. Values represent arbitrary units; the WKY left ventricular (LV) value was set at 1.00, and the remaining values were adjusted accordingly. RV indicates right ventricle. **P<.05 vs SHR-NF by ANOVA and Tukey's procedure. Boluyt et al Gene Expression in the Failing Heart LV V 0W %l # TGF-BU0LA 185-iw VW Lane W W 1 2 3 4 5 6 LR WKYV " # $ t W tt WV 7 8 9 10 11 1213 SHR-F-J SHR-NF----J RV TGF-1 . V0 18isS- 0* Lane 1 2 3 4 5 6 L-WKY * h eto $0fl * 7 8 9 10 11 1213 14 15 SHR-NFSHR-F- 12 RV LV 8 lr ;R. 2 _L WKY SHR-NF SHR-F WKY SHR-NF SHR-F FIG 8. Levels of transforming growth factor-fl, (TGF-j,8) mRNA in ventricles of Wistar-Kyoto (WKY) rats, spontaneously hypertensive rats (SHR) without heart failure (SHR-NF), and SHR with heart failure (SHR-F). Top, Autoradiogram of Northern blot analysis. Blots were probed with a cDNA probe for rat TGF-f,1. Bottom, Bar graphs showing data from Northern blot. Values represent arbitrary units and are mean+SEM of four to six samples per group. LV indicates left ventricle; RV, right ventricle. **P<.05 vs SHR-NF by ANOVA and Tukey's procedure. Contractile Protein Gene Expression The decrease in a-MHC mRNA levels in the LV of failing hearts is in agreement with our previous findings of a complete disappearance of the V, and V2 myosin isoforms from LV papillary muscles of failing hearts." This correspondence between protein and mRNA suggests that the isoform shift is due to transcriptional regulation or selective destabilization of the a-MHC mRNA. Although caution must be taken when comparing mRNA values from ventricular wall tissue to protein measurements made in papillary muscles, the available evidence suggests that this is reasonable, since papillary and ventricle wall myosin isoform distributions are similar in hearts of male Wistar rats,42 and that even when initial values differ as in aging, the direction and magnitude of the isoform shift in free wall and papillary muscle tissue is similar.42 On the basis of the previously reported shift to 100% V3 myosin isoform in papillary muscles," we predicted a corresponding increase in fl-MHC mRNA levels in the LV. There was, however, no significant increase in f-MHC mRNA levels in either ventricle of SHR-F. Since the papillary muscles of WKY rats were comprised of 5:'80% fl-MHC and the /3-isoform presumably predominated in the ventricles as 29 well, only a small (25% to 40%) increase in f-MHC mRNA levels would be required to account for the observed increase in P-MHC protein.1' Thus, it is not surprising that no significant increase in /3-MHC mRNA levels was observed. Since evidence exists that a loss of contractile protein from the myocardium may contribute to the impaired function observed in cardiac muscle from failing human hearts,14 we have determined whether contractile protein mRNA levels are depressed in the SHR model of heart failure. The present data indicate that levels of a-cardiac actin, a-skeletal actin, and MLC2 mRNA are not significantly altered during the transition to failure. Thus, in the SHR model of heart failure, there is no grossly detectable downregulation of contractile protein gene expression. The present study did not directly address the issue of contractile protein content of failing myocardium and therefore does not exclude the possibility that there are alterations in protein content that are due to changes in protein turnover. Expression of Hypertrophy-Associated Genes Evidence has accumulated that myocyte dropout due to myocardial cell death and subsequent hypertrophy of the remaining viable myocytes occurs in the heart during aging and hypertension. 15-17 Hypertrophy of myocytes can be viewed as a physiological adaptation that serves to normalize wall stress as hemodynamic load is chronically elevated.9 When hypertrophic adaptive mechanisms fail to adequately normalize wall stress, dysfunction and overt heart failure ensue. Hallmarks of hypertrophy include a transient upregulation of ca-skeletal actin gene expression'8 and a sustained elevation in ANF mRNA levels.22,43 The twofold to threefold higher levels of a-skeletal actin and ANF mRNA levels observed in SHR-NF compared with WKY rats is consistent with the notion that some myocytes in hearts of hypertensive rats are exhibiting a nascent hypertrophic response. It should be noted that the changes in steadystate ANF mRNA levels described here occur in the context of advanced age, which is also associated with elevated ANF mRNA levels.44 Despite an additional elevation in ANF mRNA levels and overt signs of pump failure, the LVs of SHR-F do not exhibit additional increases in mass or expression of the a-skeletal actin gene. In aggregate, these findings suggest that the capacity for hypertrophy has been reached or exceeded by some SHR and that an accumulation of connective tissue, a loss of myocytes, or both limits further adaptation. Factors that may affect the capacity for hypertrophy include absolute cell-size limits imposed by physical characteristics, such as diffusion distance, metabolic competition for increasingly limited pools of substrate, and interactions with the extracellular connective tissue matrix. SRCA Gene Expression Studies of human heart tissue suggest a diminished level of SRCA mRNA in patients with end-stage failure.24 These changes have been postulated to be responsible, in part, for the diastolic dysfunction that characterizes some types of heart failure. It should be noted that the genetic determinants of hypertension in the SUR model differ in some respects from factors under- 30 Circulation Research Vol 75, No 1 July 1994 lying essential hypertension in humans,45 raising the possibility that the mechanisms responsible for heart failure in humans and SHR may differ in some respects as well. Expression of the SRCA gene decreases after aortic constriction in the rat heart and is associated with depressed sarcoplasmic reticulum pump function.23 In the SHR model of heart failure, a deficit in the function of papillary muscles is observed.6,11' 2 In aggregate, these observations suggest that the expression of the SRCA gene may be diminished during the transition from stable hypertrophy to failure. Interestingly, no decrease was observed in LV SRCA mRNA levels as a result of either hypertension or during the transition to failure, although a 24% decrease was observed in the RV of SHR-NF, with no further decrease during the transition to failure. Conclusions concerning SRCA mRNA levels in the LV are limited by the small number of observations in each group. Thus, although these results do not exclude the possibility that a small (<40%) decrease in SRCA mRNA levels during the transition to failure may occur, they do rule out changes on the order of magnitude previously observed in pressure-overload hypertrophy23 and senescence.46,47 A possible explanation for the lack of a decrease in LV SRCA mRNA levels during either hypertension or failure in the present study is that the animals are at an age when the expression of the SRCA gene is already depressed in the LV of Wistar rats.46 The aortic constriction-induced downregulation of SRCA gene expression is preserved in hearts of senescent Long-Evans rats; however, these rats do not exhibit the age-associated decrease in SRCA mRNA levels that occurs in the Wistar rats.48 The present results in a rat model of heart failure suggest that SRCA mRNA levels may require more investigation into the interactive effects of age on SRCA expression. Expression of Extracellular Matrix-Associated Genes The most striking aspect of the present study is the threefold to fivefold increase in collagen and fibronectin mRNA levels between SHR-NF and SHR-F. This suggests that the onset of failure triggers a mechanism that upregulates fibronectin and collagen gene expression. Since increases in fibrillar collagen in the interstitium contribute to tissue stiffness, increases in fibronectin and collagen gene expression may contribute to impaired function.8 The upregulation of TGF-,f1 gene expression observed in failing hearts may be consistent with a stimulatory role for this growth factor, leading to accumulation of extracellular matrix. Active TGF-f,1 increases fibronectin and collagen expression in a variety of cell types and stimulates their incorporation into extracellular matrix.25 Villareal and Dillman21 noted a transient sequential increase in TGF-,31, fibronectin, and collagen mRNA levels after aortic constriction in rats, which suggests that activation of TGF-,81 gene expression is one of the mechanisms by which fibronectin and collagen genes are activated in the heart in vivo. In contrast to the transient sequential increase in the expression of extracellular matrix components after aortic constriction,2' the elevated levels of TGF-f31, fibronectin, and collagen were evident simultaneously in hearts of all rats exhibiting signs of failure, suggesting that increased expression of these genes is sustained in the failing heart. Expressions of a number of genes have been investigated for their potential diagnostic value in human heart failure.24,49 The current results suggest that fibronectin (particularly the EIIIA+ isoform), collagen type I, collagen type III, and TGF-f31 mRNAs merit similar evaluation. The EIIIA+ isoform of fibronectin is expressed at high levels during embryogenesis20 and wound healing19 and in hearts of aortic-constricted,21 SHR,41 and thyroxine-treated50 rats. The structural properties are not well understood, but it is postulated that EIIIA+ isoforms of fibronectin may be important in the deposition of nascent extracellular matrix.'9-21 The current findings are consistent with this notion and suggest that factors associated with injury and healing processes may be at work during the transition from stable hypertrophy to failure. The finding that mRNAs coding for extracellular matrix proteins were elevated in both the LV and RV of failing hearts is consistent with the hypothesis of Weber and coworkers8,51 that circulating substances may be the trigger for extracellular matrix production in heart failure. It should be noted, however, that the magnitude of RV hypertrophy in SHR-F suggests that load-related hypertrophy could account for the activation of extracellular matrix production. However, reports that inhibitors of angiotensin-converting enzyme can reverse the accumulation of fibrotic material52 and prevent the development of fibrosis and heart failure53 provide further support for the hypothesis that a circulating substance may be the trigger. Since cardiac fibroblasts are the source of collagen types I and III,54 it is important to identify and characterize factors and conditions that alter production of extracellular matrix components by these cells. Evidence from studies of hormonal effects on noncardiac fibroblasts suggests the possible involvement of angiotensin II, vasopressin, and aldosterone in modulating gene expression.851 Furthermore, angiotensin II increases proliferation of cultured cardiac fibroblasts.55,56 Norepinephrine, a physiological agent known to influence cardiac myocyte hypertrophy under certain conditions,57 also increases incorporation of labeled thymidine in cultured cardiac fibroblasts.58 Studies of factors influencing fibronectin and collagen gene expression in cardiac fibroblasts, as well as potential interactions between myocytes and fibroblasts in the heart, should provide invaluable insights into the pathophysiology of heart failure. Acknowledgments This study was supported by Medical Research Funds from the Department of Veterans Affairs. Dr Boluyt was supported by a National Research Council associateship. We thank Ken Boheler, Kenneth R. Chien, Mon-Li Chu, and Michael Sporn for generously providing fibronectin, MLC2, collagen, and TGF-j31 probes, respectively. We are grateful to Kathleen G. Robinson and Xilin Long for their assistance with technical aspects of this study and to Paula Wernick for assistance in preparing the manuscript. References 1. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham Study. N Engl J Med. 1971;285:1441-1446. Boluyt et al Gene Expression in the Failing Heart 2. Caird FI, Kennedy RD. Epidemiology of heart disease in old age. In: Caird FI, Dall JLC, Kennedy RD, eds. Cardiology in Old Age. New York, NY: Plenum Publishing Corp; 1976:1-10. 3. Pfeffer JM, Pfeffer MA, Fishbein MC, Frohlich ED. Cardiac function and morphology with aging in the spontaneously hypertensive rat. Am J Physiol. 1979;237:461-468. 4. Mirsky I, Pfeffer JM, Pfeffer MA, Braunwald E. The contractile state as a major determinant in the evolution of left ventricular dysfunction in the spontaneously hypertensive rat. Circ Res. 1983; 53:767-778. 5. Spann JF, Buccino RA, Sonnenblick EH, Braunwald E. Contractile state of cardiac muscle obtained from cats with experimentally produced ventricular hypertrophy and heart failure. Circ Res. 1967;21:341-354. 6. Conrad CH, Brooks WW, Robinson KG, Bing OHL. Impaired myocardial function in spontaneously hypertensive rats with heart failure. Am J Physiol. 1991;260:H136-H145. 7. Conrad CH, Brooks WW, Sen S, Robinson KG, Bing OHL. Increased collagen content may contribute to increased myocardial stiffness and heart failure in the spontaneously hypertensive rat. JAm Coll Cardiol. 1990;15:48A. Abstract. 8. Weber KT, Brilla CG. Pathological hypertrophy and cardiac interstitium: fibrosis and renin-angiotensin-aldosterone system. Circulation. 1991;83:1849-1865. 9. Grossman W. Cardiac hypertrophy: useful adaptation or pathological process? Am J Med. 1980;69:576- 584. 10. Trippodo NC, Frohlich ED. Similarities of genetic (spontaneous) hypertension: man and rat. Circ Res. 1981;48:309-319. 11. Bing OHL, Brooks WW, Conrad CH, Sen S, Perreault CL, Morgan JP. Intracellular calcium transients in myocardium from spontaneously hypertensive rats during the transition to heart failure. Circ Res. 1991;68:1390-1400. 12. Perreault CL, Bing OHL, Brooks WW, Ransil BJ, Morgan JP. Differential effects of cardiac hypertrophy and failure on right versus left ventricular calcium activation. Circ Res. 1990;67: 707-712. 13. Brooks WW, Healey N, Sen S, Conrad CH, Bing OHL. Oxygen cost of stress development in hypertrophied and failing hearts from spontaneously hypertensive rat. Hypertension. 1993;21:56-64. 14. Pagani ED, Alousi AA, Grant AM, Older TM, Dziuban SW Jr, Allen PD. Changes in myofibrillar content and Mg-ATPase activity in ventricular tissues from patients with heart failure caused by coronary artery disease, cardiomyopathy, or mitral valve insufficiency. Circ Res. 1988;63:380-385. 15. Anversa P, Hiler B, Ricci R, Guideri G, Olivetti G. Myocyte cell loss and myocyte hypertrophy in the aging rat heart. J Am Coll 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. Cardiol. 1986;8:1441-1448. 16. Capasso JM, Palackal T, Olivetti G, Anversa P. Left ventricular failure induced by long-term hypertension in rats. Circ Res. 1990; 66:1400-1412. 17. Engelmann GL, Vitullo JC, Gerrity RG. Morphometric analysis of cardiac hypertrophy during development, maturation, and senescence in spontaneously hypertensive rats. Circ Res. 1987;60:487-494. 18. Schwartz K, de la Bastie D, Bouvaret P, Oliviero P, Alonso S, Buckingham M. a-Skeletal muscle actin mRNAs accumulate in hypertrophied adult rat hearts. Circ Res. 1986;59:551-555. 19. ffrench-Constant C, Van De Water L, Dvorak HF, Hynes RO. Reappearance of an embryonic pattern of fibronectin splicing during wound healing in the adult rat. J Cell Biol. 1989;109: 903-914. 20. Norton PA, Hynes RQ. Alternative splicing of chicken fibronectin in embryos and in normal and transformed cells. Mol Cell Biol. 1987;7:4297-4307. 21. Villareal FJ, Dillman WH. Cardiac hypertrophy-induced changes in mRNA levels for TGF-I3i, fibronectin, and collagen. Am J 40. 41. 42. 43. 44. 45. Physiol. 1992;31:H1861-H1866. 22. Chien KR, Knowlton KU, Zhu H, Chien S. Regulation of cardiac gene expression during myocardial growth and hypertrophy: molecular studies of an adaptive physiologic response. FASEB J. 46. 1991;5:3037-3046. 23. de la Bastie D, Levitsky D, Rappaport L, Mercadier J-J, Marotte F, Wisnewsky C, Brovkovich V, Schwartz K, Lompr6 A-M. Function of the sarcoplasmic reticulum and expression of its Ca2+ATPase gene in pressure overload-induced cardiac hypertrophy in the rat. Circ Res. 1990;66:554-564. 24. Arai M, Alpert NR, MacLennan DH, Barton P, Periasamy M. Alterations in sarcoplasmic reticulum gene expression in human heart failure: a possible mechanism for the alterations in systolic 47. 31 and diastolic properties of the failing myocardium. Circ Res. 1993; 72:463-469. Ignotz RA, Massague J. Transforming growth factor-p stimulates the expression of fibronectin and collagen and their incorporation into the extracellular matrix. J Biol Chem. 1986;261:4337-4345. Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156-159. Church GM, Gilbert W. Genomic sequencing. Proc Natl Acad Sci USA. 1984;81:1991-1995. Feinberg AP, Vogelstein B. Addendum: A technique for radiolabeling DNA restriction endonuclease fragments to high specific activity. Anal Biochem. 1984;137:266-267. Feinberg AP, Vogelstein B. A technique for radiolabeling DNA restriction endonuclease fragments to high specific activity. Anal Biochem. 1983;132:6-13. Mayer Y, Czosnek H, Zoolon PE, Yaffe D, Nudel U. Expression of the genes coding for the skeletal muscle and cardiac actins in the heart. Nucleic Acids Res. 1984;12:1087-1101. Shani M, Nudel U, Zevin-Sonkin D, Zakut R, Givol D, Katcoff D, Carmon Y, Reiter J, Frischauf AM, Yaffe D. Nucleic Acids Res. 1981;9:579-589. Maki M, Takayanagi R, Misono KS, Pandey KN, Tibbets C, Inagami T. Structure of rat atrial natriuretic factor precursor deduced from cDNA sequence. Nature. 1984;309:722-724. Schwarzbauer JE, Patel RS, Fonda D, Hynes RO. Multiple sites of alternative splicing of the rat fibronectin gene. EMBO J. 1987;6: 2573-2580. Chu M-L, Myers JC, Bernard MP, Ding J-F, Ramirez F. Cloning and characterization of five overlapping cDNAs specific for the human pro-al(I) collagen chain. Nucleic Acids Res. 1982;10: 5925-5934. Chu M-L, Weil D, de Wet W, Berard M, Sippola M, Ramirez F. Isolation of cDNA and genomic clones encoding human proal(III) collagen. J Biol Chem. 1985;260:4357-4363. Qian SW, Kondaiah P, Roberts AB, Sporn MB. cDNA cloning by PCR of rat transforming growth factor 8-1. Nucleic Acids Res. 1990;18:3059. O'Neill L, Holbrook NJ, Fargnoli J, Lakatta EG. Progressive changes from young adult age to senescence in mRNA for rat cardiac myosin heavy chain genes. Cardioscience. 1991;2:1-5. Lompre AM, de la Bastie D, Boheler KR, Schwartz K. Characterization of the rat heart sarcoplasmic reticulum Ca 2-ATPase mRNA. FEBS Lett. 1989;249:35-41. Erdmann AJ III, Vaughan TR Jr, Brigham KL, Woolverton WC, Staub NC. Effect of increased vascular pressure on lung fluid balance in unanesthetized sheep. Circ Res. 1975;37:271-284. Devore J. Probability and statistics for engineering and the sciences. Monterey, Calif: Brooks/Cole; 1982:263-264. Mamuya WS, Chobanian A, Brecher P. Age-related changes in fibronectin expression in spontaneously hypertensive, WistarKyoto, and Wistar rat hearts. Circ Res. 1992;71:1341-1350. Effron MB, Bhatnagar GM, Spurgeon HA, Ruano-Arroyo G, Lakatta EG. Changes in myosin isoenzymes, ATPase activity, and contraction duration in rat cardiac muscle with aging can be modulated by thyroxine. Circ Res. 1987;60:238-245. Mercadier J-J, Samuel J-L, Michel JB, Zongazo MA, de la Bastie D, Lompre AM, Wisnewsky C, Rappaport L, Levy B, Schwartz K. Atrial natriuretic factor gene expression in rat ventricle during experimental hypertension. Am J Physiol 1987;257:H979-H987. Boluyt MO, O'Neill L, Lakatta EG, Crow MT. Progressive elevation of atrial natriuretic factor mRNAs in rat heart with advancing age. J Mol Cell Cardiol. 1992;24(suppl III):S.35. Abstract. McGiff JC, Quilley CP. The rat with spontaneous genetic hypertension is not a suitable model of human essential hypertension. Circ Res. 1981;48:455-463. Lompr6 AM, Lambert F, Lakatta EG, Schwartz K. Expression of sarcoplasmic reticulum Ca2+-ATPase and calsequestrin genes in rat heart during ontogenic development and aging. Circ Res. 1991; 69:1380-1388. Maciel LMZ, Polikar R, Rohrer D, Popovich BK, Dillman WH. Age-induced decreases in the messenger RNA coding for the sarcoplasmic reticulum Ca'2-ATPase of the rat heart. Circ Res. 1990;67:230-243. 48. Buttrick P, Malhotra A, Factor S, Geenan D, Leinwand L, Scheuer J. Effect of aging and hypertension on myosin biochemistry and gene expression in the rat heart. Circ Res. 1991;68:645-652. 32 Circulation Research Vol 75, No 1 July 1994 49. Feldman AM, Ray PE, Silan CM, Mercer JA, Minobe W, Bristow MR. Selective gene expression in failing human heart: quantification of steady-state levels of messenger RNA in endomyocardial biopsies using the polymerase chain reaction. Circulation. 1991;83: 1866-1872. 50. Mamuya WS, Brecher P. Fibronectin expression in the normal and hypertrophic rat heart. J Clin Invest. 1992;89:392-401. 51. Weber KT, Brilla CG, Campbell SE, Guarda E, Zhou G, Sririam K. Myocardial fibrosis: role of angiotensin II and aldosterone. Basic Res Cardiol. 1993;88(suppl I):107-124. 52. Brilla CG, Janicki JS, Weber KT. Cardioreparative effects of lisinopril in rats with genetic hypertension and left ventricular remodeling. Circulation. 1991;83:1771-1779. 53. Brooks WW, Conrad CH, Robinson KG, Bing OHL. Prevention of changes in intrinsic muscle properties associated with heart failure by captopril in the spontaneously hypertensive rat. Circulation. 1991;86(suppl I):I-861. Abstract. 54. Eghbali M, Blumenfeld 00, Seifter S, Buttrick PM, Leinwand LA, Robinson TF, Zern MA, Giambrone MA. Localization of types I, III, and IV collagen mRNAs in rat heart cells by in situ hybridization. J Mol Cell Cardiol. 1989;21:103-113. 55. Schorb W, Booz GW, Dostal DE, Conrad KM, Chang KC, Baker KM. Angiotensin II is mitogenic in neonatal rat cardiac fibroblasts. Circ Res. 1993;72:1245-1254. 56. Sadoshima J, Izumo S. Molecular characterization of angiotensin II-induced hypertrophy of cardiac myocytes and hyperplasia of cardiac fibroblasts: critical role of the AT, receptor subtype. Circ Res. 1993;73:413-423. 57. Simpson P. Stimulation of hypertrophy of cultured neonatal rat heart cells through an a1-adrenergic receptor and induction of beating through an al- and 813-adrenergic receptor interaction. Circ Res. 1985;56:884-894. 58. Bhambi B, Eghbali M. Effect of norepinephrine on myocardial collagen gene expression and response of cardiac fibroblasts after norepinephrine treatment. Am J Pathol. 1991;139:1131-1142.