- Wiley Online Library
advertisement

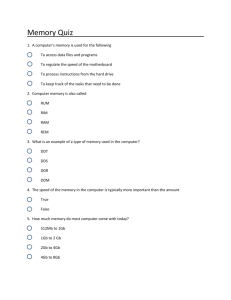
articles nature publishing group inteRVENTION AND pREVENTION A Pilot of a Video Game (DDR) to Promote Physical Activity and Decrease Sedentary Screen Time Ann E. Maloney1, T. Carter Bethea2, Kristine S. Kelsey3, Julie T. Marks4, Sadye Paez5, Angela M. Rosenberg5, Diane J. Catellier6, Robert M. Hamer2,6 and Linmarie Sikich2 Objective: We examined the feasibility of Dance Dance Revolution (DDR), a dance video game, in participants’ homes, to increase physical activity (PA) and to decrease sedentary screen time (SST). Methods and Procedures: Sixty children (7.5 ± 0.5 years) were randomized in a 2:1 ratio to DDR or to wait-list control (10-week delay). DDR use was logged, PA was measured objectively by accelerometry. SST was self-reported at weeks 0 and 10. At week 28, after both groups had access to DDR, accelerometry and SST were repeated. Results: Mean use of DDR was 89 ± 82 (range 0–660 min) min per week (mpw). The DDR group showed increased vigorous PA and a reduction in light PA; the control group showed no increase in moderate and/or vigorous PA (MVPA) although they also had a reduction in light PA. Differences between the groups were not observed. The DDR group also reported a decrease in SST of –1.2 ± 3.7 h per week (hpw) (P < 0.05), whereas the controls reported an increase of +3.0 ± 7.7 hpw (nonsignificant). The difference in SST between the groups was significant, with less SST in the DDR group. Between weeks 10 and 28, numeric reductions in SST were reported in both groups. In the DDR group, SST at week 28 (8.8 ± 6.0 hpw) was lower than baseline (10.5 ± 5.5 hpw; P < 0.03). Discussion: This pilot study suggests that DDR reduces SST and may facilitate slight increases in vigorous PA. Further study is needed to better characterize children and contexts in which DDR may promote a healthy lifestyle. Obesity (2008) 16, 2074–2080. doi:10.1038/oby.2008.295 INTRODUCTION The escalating epidemic of childhood overweight stems from multiple factors including decreased moderate and/or vigorous physical activity (MVPA) and increased sedentary behaviors (1). A study of objectively monitored MVPA found that only 3% of youth in first to third grade met the “Healthy People 2010” guidelines of engaging in 20-min bouts of vigorous activity at least 3 days per week (2). Multiple barriers to MVPA have been reported. Many families feel that it is not safe to play outdoors in their neighborhoods (3,4). Others view the distance to the nearest open play area or reliance upon working parents for transportation to MVPA opportunities as prohibitive (5,6). These issues may be particularly problematic in rural areas and among low-income families. In contrast, youth are exposed to many appealing sedentary screen time (SST) options (7,8). Further, caregivers often regard screen activities in the home as a safe and inexpensive form of child entertainment (9). In the United States, school-age children spend an estimated 3 h per day watching television (TV) and ~60 min per day (mpd) playing video games (10). Multiple studies correlate TV time with overweight status (11–15). TV may contribute to adiposity not only by displacing PA, but also by increasing snacking on unhealthy foods, which are frequently advertised on TV. In a large study of youth, each hour increase of TV watching was associated with an additional energy intake of 167 kcals/day (16). However, among children <8 years of age, the amount of traditional video game play was even more strongly associated with obesity than TV watching (17). Most efforts to reduce overweight have focused on increasing MVPA, decreasing sedentary behaviors or both (18–20). In a year-long cohort study of 11,887 youth 10–15 years old, BMI decreased by –0.06 kg/m2 in girls and –0.22 kg/m2 in boys each hour increase in daily MVPA and BMI increased by +0.05 kg/m2 with each hourly increase in SST in girls (21). Further models in which an hour of SST was replaced by an hour of MVPA showed reductions of ~0.5 BMI units in youth except lean boys. Department of Psychiatry, Center for Psychiatric Research, Maine Medical Center Research Institute, Scarborough, Maine, USA; 2Department of Psychiatry, University of North Carolina, Chapel Hill, North Carolina, USA; 3Department of Nutrition, University of North Carolina, Chapel Hill, North Carolina, USA; 4Constella Group, Durham, North Carolina, USA; 5Department of Allied Health Sciences, University of North Carolina, Chapel Hill, North Carolina, USA; 6Department of Biostatistics, University of North Carolina, Chapel Hill, North Carolina, USA. Correspondence: Ann E. Maloney (malona1@mmc.org) 1 Received 27 March 2007; accepted 29 October 2007; published online 3 July 2008. doi:10.1038/oby.2008.295 2074 VOLUME 16 NUMBER 9 | SEPTEMBER 2008 | www.obesityjournal.org articles intervention and Prevention Effects were greater in overweight youth. Interestingly, it may be easier to reduce sedentary behaviors than to increase MVPA. In the Stanford Girls Enrichment Multisite Study of 8–10-year-old African-American girls, the intervention group was provided access to dance classes 5 days per week at local community centers and was taught strategies to reduce TV viewing, whereas the control group received health education talks and newsletters (7). There was a significant reduction in household TV viewing in the intervention group as compared to the control group. In contrast, both groups showed indistinguishable reductions in MVPA, despite expectations that MVPA would increase in the intervention group. In another study, there was no difference in the efficacy of coupling a dietary intervention with efforts to increase MVPA or with efforts to reduce sedentary behaviors; both strategies led to a 10.9% reduction in overweight among 90 children aged 8–12 over a 2-year period, although objective measures of MVPA and sedentary behaviors are not provided to determine whether they in fact changed (12). Dance Dance Revolution (DDR) is a popular active video game initially introduced in arcades and now available for home use. Numerous studies have demonstrated that individuals engage in MVPA while playing DDR (22–24). Children aged 8–12 years increased their resting energy expenditure by 172% while playing DDR (25), which was greater than the increases observed while playing the Eye-Toy (Sony Computer Entertainment, Foster City, CA), walking on a treadmill, or dancing to music (26). Thus, DDR may be an innovative strategy for increasing MVPA in youth that does not require significant changes in the environment of youth. In addition, DDR may displace some SST, which also may have health benefits. However, it is essential to rigorously evaluate the utility of DDR in promoting a healthy lifestyle given marketing pressures and the enthusiasm of the lay press. Madsen et al. (2007) recently published results of a feasibility study examining whether 30 youth aged 9–18 years with BMIs above the 95th percentile (mean BMI 38.3 ± 9 kg/m2) would engage in DDR consistently over a 6-month period and whether DDR use in this population was correlated with change in BMI (27). In this study, 12 of 26 (46%) children used DDR at least twice weekly during the first 3 months. However, this level of play was sustained in only 2 of 21 (9.5%) participants. Days of use of DDR were not associated with a change in BMI. Limitations of Madsen’s study include selection of obese youth who may be among the hardest to engage in MVPA, the sample’s broad age range, and the absence of objective measures of MVPA and SST. In addition, the analysis of BMI changes may be confounded by two factors. First, because all participants were recruited from a pediatric obesity clinic, they were likely receiving other intensive interventions that may be more potent than DDR or compete for time with DDR. Second, the decision to characterize DDR use as days of DDR play rather than duration of ongoing DDR play or DDR min per week (mpw) fails to distinguish between those who play for 5 mpd and those who play for more than an hour and those who played throughout the intervention period from those who played intensively for a much shorter period. It remains to be obesity | VOLUME 16 NUMBER 9 | SEPTEMBER 2008 determined whether DDR may have more appeal for younger children or children who have not yet developed severe obesity. In addition, future studies will benefit from assessment of SST, more direct assessment of MVPA and a comparison group. Additional work is also needed to identify situations in which DDR may offer advantages over other forms of MVPA and strategies that may facilitate the use of DDR. Although DDR may be advantageous in reducing weight, its greatest benefit may lie in developing healthy lifestyle habits early in life. Many studies have suggested that MVPA is already decreasing as children enter the second decade of life, so it may be beneficial to explore the use of DDR during elementary school years. Our study addresses some of these issues. First and foremost, it is focused on directly assessing DDR’s effect on two aspects of a healthy lifestyle—MVPA and SST—rather than on the more distant outcome of weight loss. Further, it focuses on a population of young children who could be targeted for preventative interventions rather than on individuals who are already obese. Finally, unlike the Madsen study, it includes a randomly assigned comparison group without access to DDR. The objectives of our “proof of concept” pilot study were to determine whether DDR could be used by young children in their homes to increase MVPA and/or decrease SST. Information about potential effects on body mass and vital signs, and factors that may facilitate DDR play such as coaching, playing with others, and parental involvement were also explored. METHODS and procedures Participants Children between the ages of 7 and 8 were recruited through postings in schools, libraries, malls, and email solicitation on the University of North Carolina campus list serve. Those who had health issues that could interfere with DDR, such as broken limbs, poorly controlled exercise-induced asthma, significant abnormalities on screening physical exam, or who had previously played DDR more than two times were excluded. After screening, youth were randomly assigned to the DDR group or to the wait-list control group for 10 weeks for the primary component of this trial. Subsequently, all participants were provided with unlimited, in-home access to DDR with follow-up assessments completed at 28 weeks. The purpose of the second interval of data collection from weeks 10 to 28 was to provide naturalistic information about the sustainability of DDR in this age group. In addition, obtaining data from the control group provided additional information regarding behavioral changes associated with DDR use by children. This protocol and study consents and assents were reviewed and approved by the University of North Carolina Biomedical Institutional Review Board. All participants and guardians signed consent before participating in any study assessments or procedures. DDR intervention After baseline assessments were completed, families in the intervention group were provided with all equipment necessary to play DDR in the home (PlayStation2 game console (Sony Corporation of America, New York, NY), DDR MAX2 game (Konami of America, Redwood City, CA), and two padded dance mats). We provided two mats to encourage social and competitive play in the family home. Children were given a written physician prescription to play 120 mpw of DDR, preferably divided over four sessions. (This was done to increase the participant’s sense of obligation to play DDR. The 120 mpw goal was chosen because it seemed attainable and we did not want DDR to displace other forms of baseline MVPA). We provided logs to participants in which to record 2075 articles intervention and Prevention the daily minutes of DDR play, asked parents to verify and co-sign the reports and mail them to us at the end of each week in prepaid envelopes. Number of DDR games played (on each game console) was also recorded on 8-MB Playstation2 memory cards which we collected at week 10. Staff set up the equipment in the home, ensured it was operational, and provided the child and caregivers with a brief handout about operation of the game and strategies for improving skills. Research team members were available by pager to address equipment malfunctions. Youth enrolled kept all of the equipment provided. Hand controllers were not provided to encourage children to use the Playstation2 game for weight-bearing activity only. Half the DDR group was randomly selected to receive five weekly, 1:1 30-min coaching sessions to explore whether coaching encouraged more DDR use. Between weeks 10 and 28, no specific instructions regarding DDR play were provided. Wait-list control intervention Children and families in the control group were asked not to play any DDR, regardless of setting. After the initial 10 weeks were completed, the control group was provided with DDR resources. Assessments Activity measures. PA was objectively assessed using the ActiGraph accelerometer (MTI Health Systems, Ft. Walton Beach, FL), worn for 7 days during waking hours at weeks 0, 10, and 28. The ActiGraph detects acceleration ranging in magnitude between 0.05 G and 2.00 G with frequency response from 0.25 to 2.50 Hz and stores all data for subsequent analysis. The ActiGraph is valid and reliable for characterizing various levels of PA in youth aged 7–15 years (28). SST at week 0 (September 2004), week 10 (December 2004), and week 28 (April 2005) was assessed for a 7-day period using an instrument modified from a study focused on reducing SST (18). Children and parents co-reported the amount of time the child spent in various sedentary activities during the weekdays and weekends. This self-report measure completed jointly by participants and their parents asks about the time (in 15-min increments) the child spent in sleep, SST, light, moderate and vigorous activity for each of the 7 days of the prior week. Examples are provided of various levels of activity (e.g., doing crafts is “light,” walking is “moderate,” and running and jumping are “vigorous”). Parental reports of their children’s TV time have been shown to correlate well with objectively measured TV viewing (29,30). Health-related measures. Research staff collected anthropometrics and body composition data on participants using the Tanita TBF-310 scale and a stadiometer. Seated pulse and blood pressure were measured using an Omron HEM-637 wrist sphygmomanometer. Staff performed manual determinations on children with small wrist circumference. Other measures. Youth wore open-faced pedometers during the baseline week and the first 10 weeks of the study. They were asked to record daily steps on self-report logs cosigned by their parents and mailed in prepaid envelopes for family convenience on a weekly basis. Participants in the study and their parents also completed a satisfaction survey upon completion of the study. Fourteen youth and their parents attended focus groups to provide additional feedback at the end of the study. Data management Data were analyzed using SAS (v9.1.2, Cary, NC). ActiGraph readings were processed using methods similar to those reported by Puyau (31). Occasional missing accelerometry data within a child’s 7-day record were replaced by imputation based on the Expectation Maximization algorithm (32). However, if there were valid data for <80% of waking hours or no data from at least one weekend day, no imputation was performed. Rather, all accelerometer data from that participant at that time point were disregarded and considered missing. Analyses were performed with and without imputation. ActiGraph data were reduced by defining thresholds for four levels of activity based on the number of 2076 metabolic equivalents expended (Table 1). The sum of the times spent in all four activity levels reflects the total time the ActiGraph was worn since sedentary activity is also measured. Statistical analyses Within-group analyses were evaluated using paired t-tests. Betweengroup differences were evaluated using the Satterthwaite two-group t-test method, which assumes that variances between groups are unequal. We did not correct for multiple comparisons in this pilot study. RESULTS A total of 122 prospective participants were screened, and 60 children (30 boys, 30 girls, age 7.5 ± 0.5 years) signed consents and participated in the study. The sample was predominantly white, middle class, and of normal BMI (17.6 ± 2.7); z-score 0.56 ± 0.92. After baseline assessments, youth were randomized into DDR (n = 40) and control (n = 20) groups. The intervention and control groups were similar in age, sex, race, anthropometric measurements, and family characteristics (Table 2). The entire sample was retained at week 10 and 90% participated at week 28. The children were highly compliant with most of the assessment measures. ActiGraph wear times averaged 12.5, 10.2, and 9.3 h per day at weeks 0, 10, and 28, respectively. This corresponds to ~90, 73, and 66% of waking hours. However, the Actigraphs malfunctioned in 5 of 54 cases (~10%), resulting in missing data. At baseline, 39 youth in the intervention group and 20 in the control group had valid ActiGraph readings. At 28 weeks, 37 youth in the intervention group and 14 in the control group had valid ActiGraph results. In contrast, only 63% of participants completed all pedometer logs. Table 1 ActiGraph criteria for types of activity Type PA METs Cutpoints (counts per minute) 0–2 >100 >2–3.5 101–1,159 Moderate PA >3.5–5.9 1,160–5,200 Vigorous PA >6 >5,200 Sedentary PA Light PA METs, metabolic equivalents; PA, physical activity. Table 2 Sample characteristics (n = 60) Variable Age (years) Non-white/white Height (inches) Basic DDR (n = 40) Wait list (n = 20) Mean (s.d.) Mean (s.d.) 7.5 (0.5) 7.6 (0.5) 10/40 5/15 49.4 (2.2) 51.0 (2.8) Weight (pounds) 60.21 (11.4) 67.95 (17.6) Female (no (%)) 19 (48) 11 (55) 17.2 (2.4) 18.0 (3.3) BMI (kg/m ) 2 % College graduate parent 90 100 % Income ≥$60,000 73 70 7 3 TV/DVD or VCR child’s bedroom DDR, Dance Dance Revolution; DVD, digital versatile disc; TV, television; VCR, videocassette recorder. VOLUME 16 NUMBER 9 | SEPTEMBER 2008 | www.obesityjournal.org articles intervention and Prevention Use of DDR Changes in SST Self-reported DDR use was 89 ± 82 mpw over the first 10 weeks. Peak use occurred during the first week (147 ± 145 mpw) and gradually decreased to half the “prescribed” level (60 ± 61 mpw) (Figure 1). Memory cards revealed that all 40 youth played DDR and only one played an additional, non-DDR game. The DDR group showed a reduction in the amount of SST between week 0 (10.5 ± 5.5 h per week (hpw)) and week 10 (9.3 ± 4.9 hpw; Δ = –1.2 ± 3.7 hpw, P < 0.05), whereas SST increased in controls from 9.3 ± 5.7 hpw to 12.3 ± 7.2 hpw (Δ = +3.0 ± 7.7 hpw, P < 0.09). The between-group patterns of SST changes differed significantly (P < 0.03), corresponding to an absolute reduction in ~4.2 hpw of SST for subjects relative to controls. Interestingly, SST decreased further by 1.0 ± 5.7 hpw in the DDR group over the next 18 weeks. From week 10 to week 28, access to DDR in the control group coincided with a significant decline in SST (Δ = –2.9 ± 8.4 hpw, nonsignificant) as shown in Figure 2. Changes in PA Accelerometer measurements of PA are provided in Table 3. There were no statistical differences between the intervention and the control groups in vigorous, moderate, light, or sedentary PA, contrary to our expectations. However, there was a significant increase in vigorous PA in the intervention group (from 10.0 ± 7.7 mpw to 16.2 ± 11.8 mpw, P < 0.0005). No ­with­in-group differences were seen in moderate PA in either group. However, light PA decreased in both the DDR group and the control group at week 10 (DDR: 15.6 ± 38.9 mpd, P < 0.02; control: 28.2 ± 54.8 mpd, P < 0.03). The increase in vigorous PA and reduction in light PA persisted through week 28 and remained statistically different from baseline in the intervention group (P < 0.01 and P < 0.002). There were no within-group changes noted in moderate PA in either the intervention or control groups noted during the first 10 weeks. However, moderate PA did increase in the control group once they were given access to DDR (from 112.1 ± 36.7 to 135.9 ± 31.4, P < 0.005). Exploratory measures Changes in anthropometrics. Children in all groups demon- strated increases in BMI during the first 10 weeks consistent with typical development. Across all groups, BMI z-scores were stable from baseline to week 10. Week 28 attrition prohibited drawing conclusions about trends in total body mass (Table 4). Systolic blood pressure increased significantly and to a similar extent in both the DDR and control group between week 0 and week 10 (4.9 ± 10.5 mm Hg, P < 0.006 and 10.6 ± 13.6 mm Hg, P < 0.003 respectively), with no between-group differences. There were no significant differences in diastolic blood pressure or pulse. 9 12 10 8 6 4 2 0 −2 −4 −6 −8 + Intervention Control * Pre–post ∆ P < 0.05 ** Pre–post ∆ P < 0.03 * + Between group ∆ P < 0.006 ** Week 10 10 8 Week 28 W k k W 7 k W 6 k W 5 k W 4 k W 3 k W k W k k W W 2 Hours/week Change in sedentary screen time (Dennison) 1 DDR (min/wk) Home DDR use 300 275 250 225 200 175 150 125 100 75 50 25 0 Figure 2 Dance Dance Revolution (DDR) reduces sedentary screen time. All pre–post comparisons are from baseline. Figure 1 Dance Dance Revolution (DDR) use in 7–8-year olds. Table 3 Mean physical activity recorded by ActiGraph (minutes per day) DDR group Week Week 0 10 38 37 Δ 28–0 Week Week Δ Week Δ 0 10 10–0 28 28–0 14 14 20 14 20 38 37 t = 0.06, P < 0.95 Light PA 344.8 331.2 –15.6 321.5 (51.3) (34.3) (38.9) (50.1) –22.8 (42.3) t = 2.43, P < 0.02 t = 3.27, 344.3 316.1 –28.2 313.9 –27.8 t = 2.3, t = 2.5, P < 0.002 (43.5) (49.5) (54.8) (59.5) (41.6) P < 0.033 P < 0.027 t = 1.01, P < 0.31 Moderate 138.4. 131.2 –7.2 139.6 PA (33.3) (33.4) (28.3) (30.0) 1.2 (33.0) t = –0.05, P < 0.96 t = –0.99, 116.4 112.1 –4.3 135.9 19.5 P < 0.33 (26.8) (36.7) (34.3) (31.4) (22.4) t = 0.12, t = –3.36, P < 0.91 P < 0.005 t = 0.14, P < 0.89 Vigorous PA 4.5 t = –3.8, t = –2.71, (10.1) P < 0.0005 P < 0.01 t = –1.42, t = –0.01, P < 0.173 P < 0.99 t = 0.91, P < 0.37 14.9 (10.1) 20 Between group 10–0 t = 0.12, P < 0.91 6.0 (9.5) 20 Within group 28–0 37 16.2 (11.8) 20 Within group 10–0 –0.5 (48.4) 10.0 (7.7) 38 Week 28 Within group 28–0 (P) Sedentary 292.0 289.7 –0.8 290.9 PA (62.0) (51.7) (43.0) (56.6) n 39 Δ 10–0 Wait-list control group (access to DDR at w10–w28 only) Within group 10–0 (P) 318.7 309.8 –8.9 299.9 –28.5 t = 0.72, t = 2.69, t = 0.61, (50.0) (42.8) (55.2) (36.5) (39.7) P < 0.479 P < 0.019 P < 0.544 9.3 (5.7) 12.7 3.4 (10.1) (10.8) 10.2 (6.4) 0.0 (9.3) All values are mean (s.d.). Boldface signifies P < 0.05. DDR, Dance Dance Revolution; PA, physical activity. obesity | VOLUME 16 NUMBER 9 | SEPTEMBER 2008 2077 articles intervention and Prevention Table 4 Health-related measures DDR group Control group Within group 10–0 (P) Within group 28–0 (P) Significance between group 10–0 (P) Week 0 Week 10 Δ 10–0 Week 28 (n = 14) NS 18.0 (3.3) 18.3 (4.0) 0.3 (1.7) 18.7 (3.6) NS 57.2 (28.5) NS 65.8 (24.4) 66.0 (24.2) 68.8 (26.4) NS 0.54 (1.1) NS 0.61 (0.93) 0.61 (0.90) 0.72 (0.98) NS 4.9 (10.5) t = –2.91, P < 0.006 99.6 (12.7) 110.2 (11.8) 10.6 (13.6) t = –3.4, P < 0.003 t = –1.76, P < 0.08 66.8 (9.0) 0.4 (11.5) NS 64.1 (9.6) 67.1 (10.3) 3.1 (11.6) NS t = –0.84, P < 0.41 92.0 (11.4) 1.7 (13.9) NS 87.1 (12.0) 86.5 (19.4) –1.2 (17.5) NS t = 0.67, P < 0.51 Week 0 Week 10 Δ 10–0 Week 28 (n = 27) BMI 17.1 (2.4) 17.4 (2.3) 0.3 (0.5) 16.8 (2.2) BM% 65.5 (26.5) 66.5 (27.2) BMI z-score 0.54 (0.93) 0.57 (0.96) SBP 102.9 (10.1) 107.8 (7.2) DBP 66.5 (7.0) Pulse 90.7 (12.6) t = 0.08, P < 0.93 All values are mean (s.d.). DBP, diastolic blood pressure; DDR, Dance Dance Revolution; NS, nonsignificant; SBP, systolic blood pressure. Satisfaction with DDR. We conducted two focus groups for youth and two for parents, as well as satisfaction surveys for all youth enrolled. We found that most youth described the game as fun and learned it easily using the lesson mode, whereas a few were frustrated with the pace. Most raised their scores and were proud of their dancing success, using provided stickers and logs and disposable cameras to help them track their improvements. Several parents commented that DDR was a nonviolent video game, and they enjoyed playing DDR with their children. Several noted that peers and siblings played alongside the study subjects. In the satisfaction survey at the end of the 28 weeks, 95% of youth endorsed liking DDR, and 93% of parents agreed. We also found in surveys that 15 parents had purchased pedometers on their own, with no prompting from us, to promote encouragement or possibly comparisons with their children who were keeping track of parent PA by counting steps. We had not predicted this pedometer-­purchasing behavior, but it came to our attention from feedback sessions. Further study is needed to find out about the effect, if any, on children influencing parental behavioral, awareness of PA, or even changes made as a family unit. More than half (54%) of the parents believed that DDR ultimately did increase their child’s PA and would recommend DDR to others. DISCUSSION This pilot study was successful in encouraging children aged 7–8 years to play DDR for a mean of 89 mpw in their homes, with ~33% decline in use over 10 weeks. During this period, youth in the DDR group also increased their vigorous PA significantly by 6 mpd (or 42 mpw), whereas no increase in vigorous PA was observed in the control group. Nonetheless, this small pilot study failed to detect a difference between vigorous PA in the DDR and control groups. In contrast, a significant difference was detected in SST habits. The DDR group showed a significant reduction in SST from 10.5 ± 5.5 hpw to 9.3 ± 4.9 hpw in comparison to the control group which showed an 2078 increase in SST from 9.3 ± 5.7 hpw to 12.3 ± 7.2 hpw (between group P < 0.03). Further, children and their families reported in focus groups enjoying DDR and scored themselves 2.9 on a scale of proficiency at DDR (anchors: 1 = not so great, 2 = solid beginner, 3 = advanced; doing pretty hard songs, and 4 = expert, could be in a contest). Coaching did not improve results. Finally, even among this health conscious and middleclass sample, mean levels of vigorous PA were <20 mpd. As expected, no significant changes were observed in anthropometric measures that were observed in this brief intervention in nonobese youth in this pilot. Our results are consistent with those of Epstein who found that 8–12 year olds found DDR more appealing than dancing to music, bicycling, or playing an interactive bicycle game with 7-point Likert ratings of 6.1 for DDR, 5.8 for the interactive bicycle game, 4.9 for bicycling, and 3.3 for dancing to music (26). Similarly, the initial amount of DDR play observed in our sample was similar to that seen by Madsen (2007), 88 ± 16 mpw during the first 3 months and 63.3 mpw over the entire 6-month period (27). In contrast to this study, neither of these studies specifically assessed SST or objectively assessed MVPA. However, our study suggests that DDR may be an innovative strategy for increasing MVPA in youth that does not require significant changes in the environment of youth. In addition, DDR may displace some SST, which also may have health benefits. Limitations This pilot study has several limitations. The sample was small; therefore, only large effects were detectable between groups, and outliers can affect findings significantly. However, a sample size of ~500 would be required to demonstrate statistical differences given the effect size of ~0.25 for vigorous PA suggested by this study, or at least ~240 to detect BMI changes, had that been our goal (using methods based on this pilot’s s.d. ratios of BMI) (33). The study is also limited somewhat VOLUME 16 NUMBER 9 | SEPTEMBER 2008 | www.obesityjournal.org articles intervention and Prevention by available outcome measures. Five of fifty-four Actigraphs (~10%) malfunctioned resulting in missing data. Actigraphs are known to be insensitive to some sorts of movement such as bicycling and swimming. In addition, there are few measures available other than self-reports for assessing SST and other ways that individuals spend their time. Although self-report measures may be subject to bias, they have been found to correlate adequately with video observation of children’s TV viewing (26,27). In contrast, there is no demonstrated relationship between the SST self-report or video monitoring and sedentary PA as assessed using the Actigraph. Also, it is likely that SST represents a relatively small proportion of sedentary and light PA and accounts for little of its variance. The study also would have been improved by monitoring the amount of DDR play throughout the entire 28 weeks rather than just the initial 10 weeks. Although we had hypothesized that pedometer data would complement Actigraph data, it is possible that they actually skewed the baseline data by providing real-time feedback at a time of heightened awareness of the importance of PA (or possible parental dyadic interactions we did not measure). Pedometers were meant to provide inexpensive information and to promote comparisons with the other measures, but compliance in this age group with logs was a limiting factor. Another potential confound is the potential lack of generalizability of this pilot sample. Most participants were upper middle class and already had numerous opportunities to participate in MVPA. Further, most parents were reported believing that healthy lifestyles and physical fitness were important at baseline. Consequently, it is possible that DDR was less compelling than it would be for youth with fewer opportunities for MVPA. In addition, seasonal variations in various types of PA and SST among US children are not well defined. It is possible that some of the within-group changes that appear encouraging in the DDR group reflect seasonal differences rather than benefits of DDR, particularly because between-group differences were not observed. This study found that DDR significantly reduced SST in 7–8-year-old youth. However, robust changes in MVPA were not different between the treatment and control groups. This study is consistent with other studies that have found it relatively difficult to increase MVPA in youth and somewhat easier to reduce SST. The extent of relative reduction in SST (4.2 hpw) was not seen by Robinson (7), although it is comparable to a related outcome (reduction in family TV watching (4.9 hpw)) reported by Robinson. It should be noted that DDR likely costs less than Robinson’s intervention program. Both studies emphasize the challenges associated with enhancing a range of healthy lifestyle behaviors especially with focused, singletechnique approaches. It seems unlikely that DDR and other active home-based video games will consistently facilitate a healthy lifestyle among children. However, the fact that some individuals in the DDR group did show marked increases in vigorous PA suggests that DDR should be studied further to determine the characteristics of youth and communities that might benefit from its use. Further, it is likely to be useful to see whether additional obesity | VOLUME 16 NUMBER 9 | SEPTEMBER 2008 supports can be easily implemented to maintain interest and enthusiasm in the game. Potential contexts might include use of DDR in after-school programming or even during school days (outside of physical education classes), using more varied songs, and using competition as a motivator. Investigations could take place to evaluate the quality of the reinforcers and supports needed at various developmental stages and settings, which may evolve with newer in versions of this kind of active game. Acknowledgments We acknowledge the efforts of the children and parents who participated in the DANCER study, the DDR trainers: Jamie Regulski, Hillary Smith, Michael Bade, Justin Wilhelm, Jessie Campbell, and Silke Ullmann; research assistants: Jonathan Bloom, Jonas Horowitz, Cathy Jones, Amy Levine, Cheree Porter, Marta Rojas, Emily Williams, and Traci Yates. We are grateful to Abby Sheer and Peter Robichaux for the database development. Physical examinations were provided by Drs Adams, Ambler, and Meikranz, as well as the other MD authors. We also acknowledge the assistance of Manuel Matsikas (EB Games corporate) and Steve Trinkley (HeartratemonitorsUSA). The Tanita Scale, used to obtain bioelectrical impedance measures and weight, was loaned from the University of North Carolina (UNC) Center for Nutrition Research Unit, Body Composition Core National Institutes of Health (NIH)-DK056350. We thank Drs Bulik, Brownley, Ward, and Stevens for reviews and suggestions, and the Subject Core lead by J.M., and for ActiGraph data, capably transformed by Larry Johnston. The Center for Development and Learning hosted the measurement events for the protocol. This research was funded by an unrestricted grant from “Get Kids in Action,” a partnership between the Gatorade Foundation via the UNC at Chapel Hill, School of Public Health. Research support was provided for A.E.M. in part by the NIH grant T32-MH19011 and Maine Medical Center Research Institute and for T.C.B in part by the NIH grant T32 HD 40127. Disclosure The authors declared no conflict of interest. © 2008 The Obesity Society References 1. Active healthy living: prevention of childhood obesity through increased physical activity. Pediatrics 2006;117:1834–1842. 2. Pate RR, Freedson PS, Sallis JF et al. Compliance with physical activity guidelines: prevalence in a population of children and youth. Ann Epidemiol 2002;12:303–308. 3. Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics 2000;105:E83. 4. Gomez JE, Johnson BA, Selva M, Sallis JF. Violent crime and outdoor physical activity among inner-city youth. Prev Med 2004;39:876–881. 5. Sallis JF, Nader PR, Broyles SL et al. Correlates of physical activity at home in Mexican-American and Anglo-American preschool children. Health Psychol 1993;12:390–398. 6. Cohen DA, Ashwood JS, Scott MM et al. Public parks and physical activity among adolescent girls. Pediatrics 2006;118:e1381–e1389. 7. Robinson TN, Killen JD, Kraemer HC et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13(Suppl 1):S65–S77. 8. Wiecha JL, Sobol AM, Peterson KE, Gortmaker SL. Household television access: associations with screen time, reading, and homework among youth. Ambul Pediatr 2001;1:244–251. 9. Gordon-Larsen P, Griffiths P, Bentley ME et al. Barriers to physical activity: qualitative data on caregiver-daughter perceptions and practices. Am J Prev Med 2004;27:218–223. 10. Jordan AB, Hersey JC, McDivitt JA, Heitzler CD. Reducing children’s television-viewing time: a qualitative study of parents and their children. Pediatrics 2006;118:e1303–e1310. 11. Grund A, Krause H, Siewers M, Rieckert H, Muller MJ. Is TV viewing an index of physical activity and fitness in overweight and normal weight children? Public Health Nutr 2001;4:1245–1251. 2079 articles intervention and Prevention 12. Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med 2000;154: 220–226. 13. Gortmaker SL, Peterson K, Wiecha J et al. Reducing obesity via a schoolbased interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409–418. 14. Ludwig DS, Gortmaker SL. Programming obesity in childhood. Lancet 2004;364:226–227. 15. Vandewater EA, Shim MS, Caplovitz AG. Linking obesity and activity level with children’s television and video game use. J Adolesc 2004;27:71–85. 16. Wiecha JL, Peterson KE, Ludwig DS et al. When children eat what they watch: impact of television viewing on dietary intake in youth. Arch Pediatr Adolesc Med 2006;160:436–442. 17. Flynn MA, McNeil DA, Maloff B et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obes Rev 2006;7(Suppl 1):7–66. 18. Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med 2004;158:170–176. 19. Sharma M. School-based interventions for childhood and adolescent obesity. Obes Rev 2006;7:261–269. 20. Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr 2007;19:354–361. 21. Berkey CS, Rockett HR, Gillman MW, Colditz GA. One-year changes in activity and in inactivity among 10- to 15-year-old boys and girls: relationship to change in body mass index. Pediatrics 2003;111:836–843. 22. Unnithan VB, Houser W, Fernhall B. Evaluation of the energy cost of playing a dance simulation video game in overweight and non-overweight children and adolescents. Int J Sports Med 2006;27:804–809. 2080 23. Wetzsteon RJ, Swanson KA, Pickett K et al. Energy expenditure and ground reaction forces of an active video game, dance dance revolution, in healthy weight and overweight children. American College of Sports Medicine: Denver, CO, 2006. 24. Tan B, Aziz AR, Chua K, Teh KC. Aerobic demands of the dance simulation game. Int J Sports Med 2002;23:125–129. 25. Lanningham-Foster L, Jensen TB, Foster RC et al. Energy expenditure of sedentary screen time compared with active screen time for children. Pediatrics 2006;118:e1831–e1835. 26. Epstein LH, Beecher MD, Graf JL, Roemmich JN. Choice of interactive dance and bicycle games in overweight and nonoverweight youth. Ann Behav Med 2007;33:124–131. 27. Madsen KA, Yen S, Wlasiuk L, Newman TB, Lustig R. Feasibility of a dance videogame to promote weight loss among overweight children and adolescents. Arch Pediatr Adolesc Med 2007;161:105–107. 28. Janz KF. Validation of the CSA accelerometer for assessing children’s physical activity. Med Sci Sports Exerc 1994;26:369–375. 29. Robinson J, Winiewicz D, Fuerch J, Roemmich J, Epstein L. Relationship between parental estimate and an objective measure of child television watching. Int J Behav Nutr Phys Act 2006;3:43. 30. Anderson DR, Field DE, Collins PA, Lorch EP, Nathan JG. Estimates of young children’s time with television: a methodological comparison of parent reports with time-lapse video home observation. Child Dev 1985;56:1345–1357. 31. Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res 2002;10:150–157. 32. Catellier DJ, Hannan PJ, Murray DM et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc 2005;37(Supp1 11):S555–S562. 33. Elshoff JD, nQuery Advisor. Statistical Solutions: Cork, Ireland, 1998. VOLUME 16 NUMBER 9 | SEPTEMBER 2008 | www.obesityjournal.org