Adhesion molecule protein signature in ovarian cancer effusions is
advertisement

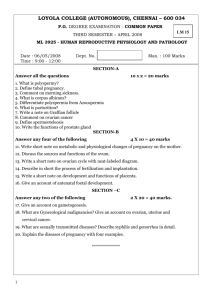
Original Article Adhesion Molecule Protein Signature in Ovarian Cancer Effusions Is Prognostic of Patient Outcome Geoffrey Kim, MD1; Ben Davidson, MD PhD2,4; Ryan Henning, BS1; Junbai Wang, PhD2; Minshu Yu, MD PhD1; Christina Annunziata, MD PhD1; Thea Hetland2,3; and Elise C. Kohn, MD1 BACKGROUND: Ovarian cancer cells in malignant effusions lack attachment to solid-phase matrix substrata and receive survival stimuli through cell–cell and cell–soluble matrix molecule interactions. We hypothesized that adhesion-related survival and proliferation pathway signals can inform clinical outcomes and guide targeted therapeutics. METHODS: Lysed cell pellets from a blinded set of benign (n ¼ 20) and malignant (n ¼ 51) peritoneal and pleural ovarian cancer patient effusions were applied to reverse-phase protein arrays and examined using validated antibodies to adhesion-associated protein endpoints. Results were subjected to hierarchical clustering for signature development. Association between specimen type, protein expression, and clinicopathologic associations were analyzed using the Mann-Whitney U test. Survival outcomes were estimated using the Kaplan-Meier method with log-rank comparison. RESULTS: A cell adhesion protein signature obtained from unsupervised clustering distinguished malignant from benign effusions (P ¼ 6.18E-06). Protein subset analyses from malignant cases defined 3 cell adhesion protein clusters driven by E-cadherin, epithelial cell adhesion molecule, and N-cadherin, respectively. The components of the E- and N-cadherin clusters correlated with clinical outcome by Kaplan-Meier statistics. Univariate analysis indicated that FAK and phosphorylated AKT were associated with higher overall and progression-free survival (PFS) (P ¼ .03), and Akt, phosphorylated paxillin, and E- and N-cadherin were associated with improved PFS (P .05). If 4 or 5 of the index adhesion proteins were high, PFS was improved by multivariate analysis (P .01). CONCLUSIONS: This hypothesis-testing examination of tumor cell adhesion molecules and pathways yielded potential predictive biomarkers with which to triage patients to selected molecular therapeutics and may serve as a platform for biomarker-based stratification for clinical application. Cancer 2012;118:1543-53. Published 2011 by the American Cancer Society*. KEYWORDS: adhesion molecules, ascites, ovarian cancer, proteomics array. INTRODUCTION Ovarian cancer remains the deadliest gynecologic malignancy, with an estimated 13,850 deaths out of almost 22,000 new cases in 2010, a fractional death rate of 63%.1 Widespread metastases to serosal surfaces with associated pleural and peritoneal effusions are common and contribute to mortality.2 Malignant epithelial cells, reactive mesothelial cells, and leukocytes are the primary cell types found in ovarian cancer effusions.3 The microenvironment within these malignant effusions is uniquely enriched in growth factors, cytokines, and soluble adhesion molecules that facilitate resistance to attachment-independent programmed cell death, a process known as anoikis.4,5 Resistance to anoikis allows cancer cells to survive despite the absence of extracellular matrix (ECM) substrata, allowing malignant cells to shed from their primary site of origin, survive in suspension, and later to implant at distant sites within the pleural or peritoneal cavity. The cancer cell overcomes anoikis through adhesion, either to other cancer cells within the effusion or to soluble ECM glycoproteins such as laminin, collagens, or fibronectin. These ECM components have been reported to act through the FAK pathway to contribute to anoikis resistance.6 Homotypic, or cell–cell, contact is another cellular protection mechanism and occurs via cell adhesion molecules. Members of the cadherin family of proteins or other cell adhesion molecules such as epithelial cell adhesion molecule Corresponding author: Elise C. Kohn, MD, 10 Center Drive, MSC 1906, Bethesda, MD 20892; Fax: (301) 480-5142; kohne@mail.nih.gov 1 Molecular Signaling Section, Medical Oncology Branch, National Cancer Institute, Bethesda, Maryland; 2Division of Pathology, The Norwegian Radium Hospital, Oslo University Hospital, Oslo, Norway; 3Department of Gynecologic Oncology, The Norwegian Radium Hospital, Oslo University Hospital, Oslo, Norway; 4The Medical Faculty, University of Oslo, Oslo, Norway *This article is a US Government work and, as such, is in the public domain in the United States of America. DOI: 10.1002/cncr.26449, Received: February 15, 2011; Revised: June 3, 2011; Accepted: June 20, 2011, Published online August 25, 2011 in Wiley Online Library (wileyonlinelibrary.com) Cancer March 15, 2012 1543 Original Article (EpCAM) mediate spheroid formation and promote cell survival and proliferation through ‘‘outside-in’’ signal transduction pathways.7-9 Ovarian cancer is unique in its expression of cadherin proteins. Unlike most epithelial surfaces, E-, P-, and N-cadherin have been reported expressed in normal ovarian epithelium10 and in the cells of malignant effusions.11 E-cadherin protein expression is increased in both ovarian cancer malignant effusions and solid metastases.12,13 However, the expression and role of the other cadherins is not as well-explored. Akt and extracellular signal-related kinase pathways are downstream intracellular pathways activated by homotypic and cell– matrix and cell–cell interactions and are critically involved in the survival and invasive properties of ovarian cancer cells found in effusions.14,15 New methods of examining expression of activated and total proteins in clinical samples have emerged. We and others have used the reverse-phase protein array (RPPA) to profile key signal transduction pathways in ovarian cancer.15-17 RPPA may be applied in a high-throughput fashion to allow simultaneous quantitative examination of a large number of cases.18,19 Use of this sensitive detection system allows analysis of expression patterns of multiple intra- and extracellular proteins, including phosphorylated (p-) proteins. Prior analysis of malignant ovarian effusion cells yielded identification of prominent signaling molecules and pathways.15 However, that study did not examine downstream integrin and adhesion molecule signaling. Advances in analytical software allow unbiased, unsupervised data examination, such as 2-way hierarchical clustering that can group samples with similar expression profiles. Clustering analyses are used to define protein signatures that may be used to differentiate benign from malignant samples and may be prognostic of clinical outcome. Here we report the results of RPPA profiling of viably flash-frozen cells from benign and malignant ovarian cancer–associated effusions. We hypothesized that proteomic expression profiling of cell adhesion and associated downstream intracellular proteins would yield both diagnostic and prognostic signal signatures. We correlated differential expression of adhesion and adhesion-related proteins with specimen type (benign vs malignant cells), clinicopathologic parameters, and overall and progression-free survival. MATERIALS AND METHODS Patients and Specimens Specimens and relevant clinical data were obtained prospectively and biobanked by the Departments of Gyneco- 1544 logic Oncology and Pathology, Norwegian Radium Hospital, under Ethics Committee–approved informed consent according to national Norwegian and institutional guidelines. The National Institutes of Health Office of Human Subjects Research reviewed and approved the examination of coded samples. Proteomic analyses using blinded samples were executed, and the results were forwarded to and analyzed by the primary site. The dataset consisted of 71 peritoneal and pleural effusions archived between May 1998 and June 2003. Benign (n ¼ 20) and malignant (n ¼ 51) peritoneal and pleural effusion samples were obtained from patients with ovarian cancer, carcinoma of the fallopian tube, and primary peritoneal carcinoma. To minimize contamination of tumor cell– specific expression, all specimens selected for the present study contained >50% carcinoma cells, the majority having a tumor cell population of 80%-100%. Benign effusions were obtained from patients with clinical suspicion of new or recurrent cancer in which morphological evaluation, immunohistochemistry, and flow cytometry ruled out the presence of malignant cells.20,21 Specimens were viably frozen within minutes of removal, in equal volumes of RPMI-1640 medium supplemented with 20% fetal calf serum and 20% dimethyl sulfoxide; samples were shipped overnight on dry ice and received solidly frozen, and stored at 80 C until use. RPPA and Immunoblot After rapid thaw on ice, samples were lysed with a TPERbased buffer (Pierce, Rockford, IL) as optimized by Winters et al.18 Samples were arrayed onto 25 replicate Whatman FAST slides (Whatman Ltd., Stanford, ME) using the Aushon 2470 arrayer (Burlington, MA) as described.18 Each case was printed in a 5-point 1:1 dilution curve to ensure that the linear detection range for all antibodies was achieved. Each sample dilution set was arrayed in triplicate on the same slide to minimize bias from ambient printing conditions, slide lot number, antibody incubation, and staining. All antibodies were obtained from Cell Signaling Technologies (Beverly, MA) and were used at 1:1000 dilution, optimized using the following control cell lysates as described.18 Anti-EPCAM is a mouse monoclonal antibody, and all others are rabbit polyclonal antibodies. Cell lysates from human microvascular endothelial cells with and without recombinant vascular endothelial growth factor treatment (50 ng/mL 5 minutes), HeLa cells treated with and without etoposide (25 lM 5 hours), HeLa cells treated with recombinant epidermal growth factor (100 ng/mL 2 hours), and Cancer March 15, 2012 Effusion Adhesion Molecule Signature/Kim et al untreated A431 cells were printed on all slides as internal controls for vascular cell activation, apoptosis, and receptor tyrosine kinase pathway activation, respectively. In addition, a sample buffer-only negative control was printed with each dilution replicate for ambient background. Location of cases was randomly assigned on the slides. Slides were subsequently blocked and stained as described.18 Effusion cell pellet lysates were subject to polyacrylamide gel electrophoresis and immunoblotted with indicated antibodies using standard methods.22 Reproducibility and Reliability Relative total arrayed protein was quantitated by colloidal gold stain (BioRad, Hercules, CA) using slides 1, 8, 16, and 25. Stained slides were scanned and saved as .tif files, and spot intensity was measured as reported.18 Reproducibility of slide printing was assessed through assessment of the correlation coefficient (R2) between total protein in slides 1, 8, 16, and 25. Reliability of printing was assessed by the coefficient of variation (CV) of the control lysates (n ¼ 6) and randomly selected patient sample lysates (n ¼ 8) on each slide followed by comparison of intraslide CV. Endpoint Analyses Proteomic endpoints were examined using specific and sensitive antibodies with optimized titers. All phosphorylation endpoints tested (p-protein) were activating signaling events. All antibodies were verified to have a single band on immunoblot, and only optimized antibody lots were applied. The negative control slide was incubated with antibody diluent without primary antibody. Each array was scanned, spot intensity was integrated over a fixed area and normalized to total protein colloidal gold stain from the most proximate of the colloidal gold controls, and a standardized, single data relative intensity unit value was generated for each spot (ImageQuant Ver. 5.2; Molecular Dynamics, Sunnyvale, CA). This data point was used in the statistical analyses. Data are expressed as the mean of triplicate spots. Statistical Analysis Hierarchical clustering and cell plots were performed with JMP7 software (SAS, Cary, NC). Statistical analysis was performed applying the SPSS-PC package (version 17.0; SPSS, Chicago, IL). A 2-sided value of P < .05 was considered significant. The association between specimen type (benign vs malignant) and protein expression by array and associations between protein expression and clinicopathologic parameters were analyzed using the Mann-Whitney U test. Clinicopathologic parameters were grouped as follows: Cancer March 15, 2012 Table 1. Clinicopathologic Data for 51 Ovarian Cancer Patients Parameter No. of Patients Age, y, mean (range) 62 (44-83) FIGO stage II III IV NA 1 28 21 1 Grade I II III NA 3 13 29 6a Residual disease £1 cm >1 cm NA 23 22 6b Histology Serous Endometrioid Mixed type Undifferentiated 44 1 5 1 Effusion site Peritoneum Pleura 42 9 FIGO, International Federation of Gynecology and Obstetrics; NA, not available. a Four inoperable patients for whom the primary tumor was unavailable for evaluation of histological grade and 2 patients who underwent operation at another hospital and for whom the primary tumor was not accessible for review. b Four inoperable patients and 2 patients who underwent operation at other hospitals where residual disease volume was not registered. age, 60 versus >60 years; histological grade, 1-2 versus 3; International Federation of Gynecology and Obstetrics (FIGO) stage, III versus IV; optimal versus suboptimal surgical debulking; previous chemotherapy, yes versus no; and response to chemotherapy for primary disease and for disease recurrence, complete versus partial response/stable disease/ progression/allergic or adverse reaction. Survival data were available for the 51 patients with malignant effusions. Overall survival and progression-free survival (PFS) were estimated using the Kaplan-Meier method, and groups were compared using the log-rank test. For this analysis, protein expression was grouped as low or high based on median values; the 4and 5-high groups were determined by having either 4 or 5 of the indicator univariate proteins highly expressed. RESULTS Patient Characteristics Anonymized benign (n ¼ 20) and malignant (n ¼ 51) ovarian cancer patient effusion cell pellets obtained from 1545 Original Article Table 2. Coefficient of Variation (%) of Control and Selected Patient Lysates Sample Slide 1 Slide 8 Slide 16 Slide 25 HeLa untreated HeLaþEGF HeLaþetoposide A431 untreated HMVECþVEGF HMVEC untreated Patient 20 Patient 52 Patient 54 Patient 58 Patient 27 Patient 14 Patient 30 Patient 29 1.55 1.77 1.51 3.36 4.33 3.25 3.11 2.42 1.45 2.71 3.52 2.01 3.47 1.84 2.05 2.31 2.94 3.79 4.88 3.57 0.81 2.58 4.02 2.40 3.68 3.71 5.02 5.88 2.30 4.33 3.13 0.55 2.98 0.96 2.55 5.72 2.75 1.45 3.50 4.86 2.24 4.85 2.56 2.44 2.66 1.44 5.22 3.45 1.41 1.69 2.86 3.82 4.70 2.63 2.41 1.27 Median CV Mean CV 2.57 2.59 3.63 3.40 2.86 3.01 2.60 2.75 CV, coefficient of variation; EGF, epidermal growth factor; VEGF, vascular endothelial growth factor. therapeutic or diagnostic effusion sampling were used. Table 1 describes the clinicopathologic characteristics of the patient cohort. Most patients had high grade, advanced stage serous cancers at diagnosis, consistent with the normal distribution of epithelial ovarian cancer worldwide. Approximately equal numbers of patients underwent optimal or suboptimal debulking and most effusions were ascites. Quality Assessment Each case was printed in 5-point 1:1 serial dilution in triplicate. Quality control was validated before examination of specific protein endpoints. Intraslide reliability was examined by determining the CV of total protein measures in control lysates and randomly selected patient lysates, consisting of 6 controls and 8 patient samples. Table 2 shows the CV within each slide and across the 4 slides stained with colloidal gold. The mean and median CV were less than 4% for each slide (range, 0.55%5.72%), and mean and median CV for all samples was <10%, demonstrating intraslide reliability of printing. Reproducibility of printing across slides was assessed by analysis of total protein staining over a series of 4 slides (slides 1, 8, 16, and 25). An equivalence plot is shown in Figure 1, demonstrating results for RPPA slide 1 versus RPPA slide 25 (R2 ¼ 0.905; inset table shows all equivalence regressions). Excellent reproducibility in total protein printing was observed between slides, with a median regression coefficient of 0.91 (range, 0.88-0.93). Cell Adhesion Protein Signature Discriminates Benign From Malignant Cells We first tested the ability of the expression values of cell adhesion and adhesion-related target proteins to discrimi- 1546 nate benign from malignant effusions using unsupervised hierarchical clustering. Figure 2A shows near complete segregation of the benign and malignant samples. The aggregate protein expression data were then median-centered and used to define a cell adhesion protein (CAP) signature. Evaluation of clustering of benign versus malignant cases as a function of protein distribution clusters was examined. The biology leading to a differential distribution of the benign and cancer samples between the 2 protein clusters is significantly different (P ¼ 2E-05) (Figure 2B). The relative organization of protein expression in all samples weighted by the CAP signature is shown in Figure 2C. A statistically significant difference in expression of the average CAP signature was found between the benign (n ¼ 20) and malignant (n ¼ 51) samples (P ¼ 6.18E-06) (Figure 2D). Proteins with statistically significant differences in expression between benign and malignant samples are presented in the inset in Figure 2. These individual findings are consistent with the dendrogram linkage in Figure 2 and implicate survival, proliferation, and cell–matrix and cell–cell molecule signaling events. We confirmed differential expression of these proteins in randomly selected representative effusion cell pellet lysates using immunoblots for index proteins with a surrogate total protein measure using glyceraldehyde dehydrogenase expression (Figure 2E). Cell Adhesion Protein Expression Correlates With Clinicopathologic Parameters Clinicopathologic parameters such as age, FIGO stage, and the presence of residual disease after cytoreductive surgery are the most important known clinical predictors Cancer March 15, 2012 Effusion Adhesion Molecule Signature/Kim et al Figure 1. RPPA quality control is shown in a unity graph comparing colloidal gold stain results of arrays 1 and 25 (R2 ¼ 0.905). Results are presented as relative intensity units. Inset table shows comparative regression coefficients for other quality control comparisons between arrays 1, 8, 16, and 25. of disease outcome in ovarian cancer.23 We examined the relationship of expression levels of individual arrayed total and p-proteins with these parameters (Table 3). The expression of p-Pyk2 and the ratio of p-Pyk2 to p-FAK were higher in younger patients, as was the expression of EpCAM and the EpCAM to P-cadherin ratio. We also found that the expression of P-cadherin and ratio of total Pyk to total FAK were higher in FIGO stage III when compared with the samples derived from FIGO stage IV. The expression of EpCAM and the ratio of the expression of EpCAM to N-cadherin were associated with greater residual disease after debulking surgery. Cell Adhesion Protein Clusters Prognosticate Outcome in Malignant Samples We next analyzed protein by a 2-way unsupervised expression profile using all malignant samples (Figure 3A). Three clusters, median-centered around the CAP (defined in Figure 2B), were segregated and renamed by the dominant cell adhesion protein in the cluster: E-cadherin, EpCAM, and N-cadherin clusters (Figure 3B, 3C, and 3D, respectively). Figure 3E shows that high extracellular signal-related kinase is prognostic of better overall survival and high p-paxillin, P-cadherin, and E-cadherin to Cancer March 15, 2012 improved progression-free survival. This led to independent evaluation of the driver proteins in the clusters. Kaplan-Meier estimates (Figure 4) revealed that overexpression of FAK was associated with longer overall survival and PFS and that overexpression of E-cadherin, ppaxillin, Akt, and p-AKT were associated with higher PFS. FAK, E-cadherin, and p-paxillin were clustered together in the E-cadherin signature, suggesting that this group of proteins may make up an important signaling pathway in the malignant cells found in effusions. Higher expression of most of this group of proteins and AKT was associated with better PFS on univariate analysis (Figure 4A-H). Statistically significantly improved PFS was observed in a multivariate analysis if 4 or 5 of those index proteins were highly expressed as a cassette (P ¼ .012 and P ¼ .001, respectively; univariate survival curve) (Figure 4I and 4J). DISCUSSION The presence of malignant cells in effusions of ovarian cancer patients has long had clinical prognostic implications and can impact treatment planning at time of diagnosis and at disease recurrence.24,25 Dissection of the biochemical processes that allow for cell survival in 1547 Original Article Figure 2. Unsupervised clustering of benign and malignant effusion data is shown. (A) Unsupervised 2-way hierarchical clustering of malignant (c, red) and benign (b, green) samples is shown. Most benign cases express low relative amounts of total and activated adhesion proteins. Inset shows P value for greater differential protein expression in malignant samples. (B) Statistical evaluation of the differential distribution of benign and cancer samples between clusters is shown. (C) Median-centered cell adhesion protein (CAP) signature is shown. The CAP average was derived from the average signal intensity of all proteins examined. (D) The CAP signature significantly segregates benign from malignant samples (P ¼ 6.2E-06). (E) Immunoblots of representative randomly selected effusion cell lysates are shown. After approximation of protein content, immunoblots were run from randomly selected lysates. Representative replicate blots are shown; relative protein loading is addressed with glyceraldehyde dehydrogenase protein content in the lysates. 1548 Cancer March 15, 2012 Effusion Adhesion Molecule Signature/Kim et al Table 3. Expression of Cell Adhesion–Related Proteins Is Higher in Younger, Stage III, Suboptimally Debulked Patients P Parameter Age <60 vs 60 y p-Pyk2 EpCAM EpCAM:P-cadherin ratio p-Pyk2:p-FAK ratio .016 .022 .019 .017 FIGO stage III vs IV P-cadherin Pyk:FAK ratio .049 .031 Residual disease >1 vs 1 cm EpCAM EpCAM:N-cadherin ratio .016 .03 EpCAM, epithelial cell adhesion molecule; FIGO, International Federation of Gynecology and Obstetrics. attachment-independent conditions may facilitate discovery of signaling molecules that are aberrantly expressed early in the process of ovarian cancer dissemination and in the later stages of disease recurrence and progression. This led us to hypothesize that a signature of cell–cell and CAP pathways in ovarian cancer effusions will uncover discriminating prognostic and potentially predictive informative biomarkers and/or therapeutic targets. We thus measured key cell–cell adhesion molecules within the cadherin and integrin signaling pathways to evaluate the relationship of cell–cell and cell–ECM signaling proteins with outcome and to posit a model where this signature may be applied. Selected survival signals with their immediate and downstream signal transduction effectors were included to complement the adhesion molecule data. Protein expression Figure 3. Unsupervised clustering of malignant samples is shown. (A) Unsupervised 2-way hierarchical clustering of 51 malignant samples segregates 2 groups through expression of adhesion proteins. (B-D) E-cadherin (B), EpCAM (C), and N-cadherin (D) cell adhesion protein clusters were generated by from the unsupervised clustering in (A). Results are median-centered around the cell adhesion protein derived in Figure 2B. (E) Outcome linear regression is shown. Cluster results incorporate progression-free and overall survival. Cancer March 15, 2012 1549 Original Article Figure 4. Survival estimates based on expression of individual proteins are shown. Kaplan-Meier survival was estimated around the median protein expression value for the indicated proteins (A-H) with overall survival (A and C) or progression-free survival (PFS) and univariate P value indicated on the graph. (I, J) Univariate survival (PFS) analysis was based on segregation by having 4 (I) or 5 (J) of the 6 index proteins highly expressed. by reverse-phase proteomic array indicated that both cell– cell and cell–integrin signaling events are active in the suspended cells of the effusions, and that both pathways had prognostic load in survival analyses. The ability to quanti- 1550 tate these proteins and relate their quantity to survival risks is a step in credentialing them as biomarkers for ovarian cancer outcome and therapy. Small molecule inhibitors against several of the proteins that were identified as Cancer March 15, 2012 Effusion Adhesion Molecule Signature/Kim et al prognostically important in our study are under clinical investigation.26,27 Our findings can be considered support for a prospective evaluation guiding targeted therapy selection for patients with malignant ovarian cancer effusions, which also will provide further evidence of the potential therapeutic predictive and prognostic value of the expression of these proteins. Cadherins are transmembrane proteins that mediate homotypic cell adhesion through their extracellular domains and connect to the actin cytoskeleton.28 They provide the transmembrane component of adherens junctions that are critical for cell polarity and tissue integrity. Cadherin expression has been found to be cell type– dependent, with most normal epithelial cells expressing E-cadherin and most cells of mesenchymal origin expressing N-cadherin. E-cadherin was initially identified as a tumor suppressor gene and later confirmed in a number of cancers, including diffuse gastric carcinomas29 and ovarian cancer.10,30-32 It has been shown to suppress cellular transformation by blocking nuclear b-catenin signaling.33 Inappropriate expression of cadherins, such as loss of Ecadherin and expression of N-cadherin or P-cadherin, is associated with epithelial-to-mesenchymal transition, a proposed mechanism involved in metastatic dissemination34,35 and chemotherapy drug resistance.36 Loss of adherent matrix contact survival signals is compensated with increased spheroid cell–cell survival, a hallmark of suspended cells of effusions that is associated with increased cadherin expression.34,37 Normal ovarian surface epithelium and ovarian cancer have been described to express E, P-, and N-cadherin38,39; these cells are known to actively remodel their environment during healing of ovulation wounds, a form of physiologic migration and invasive behavior. Thus, increased and varied cadherin quantities and patterns may represent targetable survival signals. We suggest that the balance between the cadherins may be different in ovarian cancers with different degrees of aggressiveness, and that this may also be manifest in part by the ability of the cancer to survive absent scaffolding, such as in an effusion. Patel et al10 evaluated solid and effusion tumor samples, showing that P-cadherin was the predominant cadherin in ascites and was associated with disease progression. Tothill et al40 stratified ovarian cancer by gene expression profiles and identified 2 groups, a stromal-like group enriched for integrin, adhesion, motility, and angiogenesis signals (C1) and a mesenchymal subtype with prominent cadherin and developmental signaling genes (C5).40 Both C1 and C5 had relatively Cancer March 15, 2012 low E-cadherin membrane staining, consistent with their stromal/mesenchymal-like behavior and poor outcome. Our opposite findings of high E-cadherin protein association with improved outcome may be related to evaluation of solid versus suspension tumor, or examination of gene versus protein. The median age, proportion of high stage and grade, serous histological predominance, and proportion of optimally debulked patients in their C1 and C5 series parallels that of our effusion cases. Similar to our findings, Elloul et al13 found up-regulation of E-cadherin protein in ovarian cancer effusions. Further study will be needed to understand these dichotomous results. We sought to identify a prognostic signature of celladhesion molecules and downstream effector molecules to build a prognostic adhesion protein signature that could later be examined for prediction of targeted drug activity. Our confirmation of high E-cadherin expression itself as a positive prognostic factor provides support for the technique and analytical platforms applied. Total FAK, activated paxillin, E-cadherin, and P-cadherin were clustered together in an unsupervised analysis, and all are positively correlated with a longer progression-free survival. FAK and paxillin are recognized mediators of integrin signaling. These molecules may regulate contact inhibition and decrease the migratory capabilities of effusion cells in the context of cadherin-mediated cell–cell contact by promoting proper assembly of those contacts.41,42 Although cadherin-mediated adhesion can facilitate resistance to anoikis via cell–cell contact and spheroid formation, these cells may be less motile and have less of an invasive drive.43 Our data suggest that ovarian cancer cells are able to survive in a cadherin-independent fashion, described by underexpression of the E-cadherin signature in those cases with a worse clinical outcome. Activated FAK, PYK2, and AKT in the N-cadherin group are consistent with activation of prosurvival effects,6,27,44 although individually, high FAK expression predicts better outcome. The segregation of the malignant samples by CAP signature has implications in clinical practice, as cell adhesion molecule expression relationship to drug response is emerging as a potential biomarker.45,46 Paclitaxel resistance in an ovarian cancer cell line was associated with a more mesenchymal, motile, and invasive phenotype, with reduced expression levels of E-cadherin.45 Restoration of E-cadherin expression in gefitinib-resistant cell lines resulted in renewed sensitivity to gefitinib, a small molecule inhibitor of the epidermal growth factor receptor.45,46 Cells with little to no E-cadherin expression may be more resistant to cytotoxic and targeted 1551 Original Article the multiple adhesion signaling protein endpoints analyzed. This type of pretreatment evaluation of the CAP signature in malignant effusions can thus be performed using pathologic waste remaining after therapeutic or diagnostic taps. A proposed schema for application of the adhesion protein signature for treatment decisions is presented in Figure 5. Our findings confirm individual protein studies and show greater potential value from an adhesion protein and pathway signature over single protein endpoint information. FUNDING SOURCES Figure 5. Proposed schema for pretreatment evaluation and treatment stratification of ovarian cancer patients with malignant ascites is shown. This potential clinical trial schema would examine and further credential the RPPA adhesion protein signatures. It suggests potential clinical applications of signature expression in effusions. chemotherapy,36 but therapy directed at CAPs such as EpCAM may have beneficial effects.47 The trifunctional anti-EpCAM monoclonal antibody catumaxomab has demonstrated benefit and has been approved in Europe for the palliative relief of malignant ascites.48,49 Our intermediate EpCAM signature may be applied in a trial setting to select a patient population for catumaxomab use. In a similar context, small molecule inhibitors of FAK and its upstream partner, src, are now under clinical investigation. Dasatinib, an abl and src kinase inhibitor, is being studied in solid tumors as a single agent, and in our group in combination with bevacizumab (NCT00792545). Collection and proteomic adhesion protein signatures evaluation of paired tissue biopsies and fluid samples before and during therapy may provide insight into susceptibility or resistance to the clinical intervention. Such findings will form the basis for subsequent clinical investigation. The effusion adhesion protein clusters identified herein may have value as a predictive biomarker tool with which to examine stratification or selection of patients who might have increased benefit from agents such as catumaxomab, FAK, or Src inhibitors for treatment of effusion-associated ovarian cancer. We have demonstrated that small numbers of cells, such as those obtained from a needle core biopsy50,51 or spun down from a small diagnostic volume of effusion, can be applied to RPPA and 1552 This study was supported by the Intramural Program of the Center for Cancer Research, National Cancer Institute, and by a grant from the Norwegian Cancer Society and by the Inger and John Fredriksen Foundation for Ovarian Cancer Research. CONFLICT OF INTEREST DISCLOSURES The authors made no disclosures. REFERENCES 1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277-300. 2. Bonnefoi H, A’Hern RP, Fisher C, et al. Natural history of stage IV epithelial ovarian cancer. J Clin Oncol. 1999;17: 767-775. 3. Davidson B. Malignant effusions: from diagnosis to biology. Diagn Cytopathol. 2004;31:246-254. 4. Frisch SM, Francis H. Disruption of epithelial cell-matrix interactions induces apoptosis. J Cell Biol. 1994;124:619-626. 5. Liotta LA, Kohn E. Anoikis: cancer and the homeless cell. Nature. 2004;430:973-974. 6. Frisch SM, Vuori K, Ruoslahti E, Chan-Hui PY. Control of adhesion-dependent cell survival by focal adhesion kinase. J Cell Biol. 1996;134:793-799. 7. Fouquet S, Lugo-Martinez VH, Faussat AM, et al. Early loss of Ecadherin from cell-cell contacts is involved in the onset of Anoikis in enterocytes. J Biol Chem. 2004;279: 43061-43069. 8. Kang HG, Jenabi JM, Zhang J, et al. E-cadherin cell-cell adhesion in ewing tumor cells mediates suppression of anoikis through activation of the ErbB4 tyrosine kinase. Cancer Res. 2007;67:3094-3105. 9. Maetzel D, Denzel S, Mack B, et al. Nuclear signalling by tumourassociated antigen EpCAM. Nat Cell Biol. 2009; 11:162-171. 10. Patel IS, Madan P, Getsios S, Bertrand MA, MacCalman CD. Cadherin switching in ovarian cancer progression. Int J Cancer. 2003;106:172-177. 11. Sivertsen S, Hadar R, Elloul S, et al. Expression of Snail, Slug and Sip1 in malignant mesothelioma effusions is associated with matrix metalloproteinase, but not with cadherin expression. Lung Cancer. 2006;54:309-317. 12. Davidson B, Berner A, Nesland JM, et al. E-cadherin and alpha-, beta-, and gamma-catenin protein expression is up-regulated in ovarian carcinoma cells in serous effusions. J Pathol. 2000;192:460469. 13. Elloul S, Silins I, Trope CG, Benshushan A, Davidson B, Reich R. Expression of E-cadherin transcriptional regulators in ovarian carcinoma. Virchows Arch. 2006;449:520-528. 14. Elstrand M, Phuc Dong H, Odegaard E, et al. Mammalian target of rapamycin is a biomarker of poor survival in metastatic serous ovarian carcinoma. Hum Pathol. 2010;41:794-804. Cancer March 15, 2012 Effusion Adhesion Molecule Signature/Kim et al 15. Davidson B, Espina V, Steinberg SM, et al. Proteomic analysis of malignant ovarian cancer effusions as a tool for biologic and prognostic profiling. Clin Cancer Res. 2006;12: 791-799. 16. Sheehan KM, Calvert VS, Kay EW, et al. Use of reverse phase protein microarrays and reference standard development for molecular network analysis of metastatic ovarian carcinoma. Mol Cell Proteomics. 2005;4:346-355. 17. Annunziata CM, Walker AJ, Minasian L, et al. Vandetanib, designed to inhibit VEGFR2 and EGFR signaling, had no clinical activity as monotherapy for recurrent ovarian cancer and no detectable modulation of VEGFR2. Clin Cancer Res. 2010;16:664-672. 18. Winters M, Dabir B, Yu M, Kohn EC. Constitution and quantity of lysis buffer alters outcome of reverse phase protein microarrays. Proteomics. 2007;7:4066-4068. 19. Carey MS, Agarwal R, Gilks B, et al. Functional proteomic analysis of advanced serous ovarian cancer using reverse phase protein array: TGF-beta pathway signaling indicates response to primary chemotherapy. Clin Cancer Res. 2010;16: 2852-2860. 20. Davidson B, Risberg B, Kristensen G, et al. Detection of cancer cells in effusions from patients diagnosed with gynaecological malignancies. Evaluation of five epithelial markers. Virchows Arch. 1999;435:43-49. 21. Davidson B, Nielsen S, Christensen J, et al. The role of desmin and N-cadherin in effusion cytology: a comparative study using established markers of mesothelial and epithelial cells. Am J Surg Pathol. 2001;25:1405-1412. 22. Rasool N, LaRochelle W, Zhong H, Ara G, Cohen J, Kohn EC. Secretory leukocyte protease inhibitor antagonizes paclitaxel in ovarian cancer cells. Clin Cancer Res. 2010;16:600-609. 23. du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115: 1234-1244. 24. Curtin JP, Malik R, Venkatraman ES, Barakat RR, Hoskins WJ. Stage IV ovarian cancer: impact of surgical debulking. Gynecol Oncol. 1997;64:9-12. 25. Akahira JI, Yoshikawa H, Shimizu Y, et al. Prognostic factors of stage IV epithelial ovarian cancer: a multicenter retrospective study. Gynecol Oncol. 2001;81:398-403. 26. Peng DJ, Wang J, Zhou JY, Wu GS. Role of the Akt/mTOR survival pathway in cisplatin resistance in ovarian cancer cells. Biochem Biophys Res Commun. 2010;394:600-605. 27. Parsons JT, Slack-Davis J, Tilghman R, Roberts WG. Focal adhesion kinase: targeting adhesion signaling pathways for therapeutic intervention. Clin Cancer Res. 2008;14:627-632. 28. Yap AS, Brieher WM, Gumbiner BM. Molecular and functional analysis of cadherin-based adherens junctions. Annu Rev Cell Dev Biol. 1997;13:119-146. 29. Perl AK, Wilgenbus P, Dahl U, Semb H, Christofori G. A causal role for E-cadherin in the transition from adenoma to carcinoma. Nature. 1998;392:190-193. 30. Faleiro-Rodrigues C, Macedo-Pinto I, Pereira D, Lopes CS. Prognostic value of E-cadherin immunoexpression in patients with primary ovarian carcinomas. Ann Oncol. 2004; 15:1535-1542. 31. Shim HS, Yoon BS, Cho NH. Prognostic significance of paired epithelial cell adhesion molecule and E-cadherin in ovarian serous carcinoma. Hum Pathol. 2009;40:693-698. Cancer March 15, 2012 32. Voutilainen KA, Anttila MA, Sillanpaa SM, et al. Prognostic significance of E-cadherin-catenin complex in epithelial ovarian cancer. J Clin Pathol. 2006;59:460-467. 33. Gottardi CJ, Wong E, Gumbiner BM. E-cadherin suppresses cellular transformation by inhibiting beta-catenin signaling in an adhesion-independent manner. J Cell Biol. 2001;153:1049-1060. 34. Elloul S, Vaksman O, Stavnes HT, Trope CG, Davidson B, Reich R. Mesenchymal-to-epithelial transition determinants as characteristics of ovarian carcinoma effusions. Clin Exp Metastasis. 2010;27:161-172. 35. Wheelock MJ, Shintani Y, Maeda M, Fukumoto Y, Johnson KR. Cadherin switching. J Cell Sci. 2008;121:727-735. 36. Singh A, Settleman J. EMT, cancer stem cells and drug resistance: an emerging axis of evil in the war on cancer. Oncogene. 2010;29:4741-4751. 37. Kassis J, Klominek J, Kohn EC. Tumor microenvironment: what can effusions teach us? Diagn Cytopathol. 2005;33:316-319. 38. Hudson LG, Zeineldin R, Stack MS. Phenotypic plasticity of neoplastic ovarian epithelium: unique cadherin profiles in tumor progression. Clin Exp Metastasis. 2008;25:643-655. 39. Sundfeldt K, Piontkewitz Y, Ivarsson K, et al. E-cadherin expression in human epithelial ovarian cancer and normal ovary. Int J Cancer. 1997;74:275-280. 40. Tothill RW, Tinker AV, George J, et al. Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin Cancer Res. 2008;14:5198-5208. 41. Huttenlocher A, Lakonishok M, Kinder M, et al. Integrin and cadherin synergy regulates contact inhibition of migration and motile activity. J Cell Biol. 1998;141:515-526. 42. Yano H, Mazaki Y, Kurokawa K, Hanks SK, Matsuda M, Sabe H. Roles played by a subset of integrin signaling molecules in cadherin-based cell-cell adhesion. J Cell Biol. 2004;166:283-295. 43. Hofmann C, Obermeier F, Artinger M, et al. Cell-cell contacts prevent anoikis in primary human colonic epithelial cells. Gastroenterology. 2007;132:587-600. 44. Wu C, Cipollone J, Maines-Bandiera S, et al. The morphogenic function of E-cadherin-mediated adherens junctions in epithelial ovarian carcinoma formation and progression. Differentiation. 2008;76:193-205. 45. Kajiyama H, Shibata K, Terauchi M, et al. Chemoresistance to paclitaxel induces epithelial-mesenchymal transition and enhances metastatic potential for epithelial ovarian carcinoma cells. Int J Oncol. 2007;31:277-283. 46. Witta SE, Gemmill RM, Hirsch FR, et al. Restoring E-cadherin expression increases sensitivity to epidermal growth factor receptor inhibitors in lung cancer cell lines. Cancer Res. 2006;66:944-950. 47. Xiang W, Wimberger P, Dreier T, et al. Cytotoxic activity of novel human monoclonal antibody MT201 against primary ovarian tumor cells. J Cancer Res Clin Oncol. 2003; 129:341-348. 48. Burges A, Wimberger P, Kumper C, et al. Effective relief of malignant ascites in patients with advanced ovarian cancer by a trifunctional anti-EpCAM x anti-CD3 antibody: a phase I/II study. Clin Cancer Res. 2007;13:3899-3905. 49. Heiss MM, Murawa P, Koralewski P, et al. The trifunctional antibody catumaxomab for the treatment of malignant ascites due to epithelial cancer: results of a prospective randomized phase II/III trial. Int J Cancer. 2010;127:2209-2221. 50. Posadas EM, Kwitkowski V, Kotz HL, et al. A prospective analysis of imatinib-induced c-KIT modulation in ovarian cancer: a phase II clinical study with proteomic profiling. Cancer. 2007;110:309-317. 51. Posadas EM, Liel MS, Kwitkowski V, et al. A phase II and pharmacodynamic study of gefitinib in patients with refractory or recurrent epithelial ovarian cancer. Cancer. 2007;109: 1323-1330. 1553