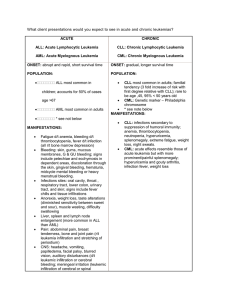
2015 Acute Leukemia Agenda
advertisement

Not for publication or presentation AGENDA CIBMTR WORKING COMMITTEE FOR ACUTE LEUKEMIA San Diego, CA Friday, February 13, 2015, 12:15 – 2:15 pm Co-Chair: Co-Chair: Co-Chair: Statisticians: Scientific Director: Assistant Scientific Director: 1. Steven Devine, MD, The Ohio State University, Columbus, OH; Telephone: 614-293-5655; Fax: 614-293-7526; E-mail: steven.devine@osumc.edu Marcos de Lima, MD, University Hospitals Case Medical Center, Cleveland, OH; Telephone: 216-286-6869; Fax: 216-201-5451; E-mail: marcos.delima@uhhospitals.org Brenda Sandmaier, MD, Fred Hutchinson Cancer Research Center, Seattle, WA; Telephone: 206-667-4961; Fax: 206-667-6124; E-mail: bsandmai@fredhutch.org Mei-Jie Zhang, PhD, CIBMTR Statistical Center, Milwaukee, WI; Telephone: 414-456-8375; Fax: 414-456-6513; E-mail: meijie@mcw.edu Hai-Lin Wang, MPH, CIBMTR Statistical Center, Milwaukee, WI; Telephone: 414-805-0647; Fax: 414-805-0714; E-mail: hwang@mcw.edu Daniel J. Weisdorf, MD, University of Minnesota Medical Center, Minneapolis, MN; Telephone: 612-624-3101; Fax: 612-625-6919; E-mail: weisd001@umn.edu Wael Saber, MD, MS, CIBMTR Statistical Center, Milwaukee, WI; Telephone: 414-805-0700; Fax: 414-807-0714; E-mail: wsaber@mcw.edu Introduction a. Minutes and Overview Plan from February 2014 meeting (Attachment 1) b. Introduction of incoming Co-Chair: Hanna Khoury, MD; Emory University Hospital; Atlanta, GA; E-mail: hkhoury@emory.edu 2. Accrual Summary (Attachment 2) 3. Presentations, published or submitted papers a. LK04-01 Holter Chakrabarty JL, Rubinger M, Le-Rademacher J, Wang HL, Grigg A, Selby GB, Szer J, Rowe JM, Weisdorf DJ, Tallman MS. Autologous is superior to allogeneic hematopoietic cell transplantation for Acute Promyelocytic Leukemia in second complete remission. Biol Blood Marrow Transplant, 2014 Jul;20(7):1021-5. b. LK07-03c McClune BL, Ahn KW, Wang HL, Antin JH, Artz AS, Cahn JY, Deol A, Freytes CO, Hamadani M, Holmberg LA, Jagasia MH, Jakubowski AA,Kharfan-Dabaja MA, Lazarus HM, Miller AM, Olsson R, Pedersen TL, Pidala J, Pulsipher MA, Rowe JM, Saber W, van Besien KW, Waller EK, Aljurf MD, Akpek G, Bacher U, Chao NJ, Chen YB, Cooper BW, Dehn J, de Lima MJ, Hsu JW, Lewis ID, Marks DI, McGuirk J,Cairo MS, Schouten HC, Szer J, Ramanathan M, Savani BN, Seftel M, Socie G, Vij R, Warlick ED, Weisdorf DJ. Allotransplantation for patients age ≥40 years with non-Hodgkin Lymphoma: Encouraging progression-free survival. Biol Blood Marrow Transplant, 2014 Jul;20(7):960-8. 1 Not for publication or presentation c. LK12-03 Bejanyan N, Weisdorf DJ, Logan BR, Wang HL, Devine SM, de Lima M, Bunjes DW, Zhang MJ. Survival of AML patients relapsing after allogeneic hematopoietic cell transplantation: a CIBMTR study. Biol Blood Marrow Transplant. 2014 [Epub ahead of print]. d. LK11-01 Goyal SD, Zhang MJ, Wang HL, Akpek G, Copelan EA, Freytes C, Gale RP, Hamadani M, Inamoto Y, Kamble RT, Lazarus HM, Marks DI, Nishihori T, Olsson RF, Reshef R, Ritchie DS, Saber W, Savani BN, Seber A, Shea TC, Tallman MS, Wirk B, Bunjes DW, Devine SM, de Lima M, Weisdorf DJ, Uy GL. Allogeneic hematopoietic cell transplant for acute myeloid leukemia: no impact of pretransplant extramedullary disease on outcome. Submitted. 4. e. LK12-01 Seftel MD, Neuberg D, Zhang MJ, Wang HL, Bergeron J, Couban S, DeAngelo DJ, de Lima M, Devine SM, Eapen M, Horowitz M, Pasquini M, Rizzo D, Saber W, Sallan S, Sandmaier BM, Weisdorf DJ. Superiority Of Pediatric Chemotherapy Over Allogeneic Hematopoietic Cell Transplantation for Philadelphia Chromosome Negative Adult ALL in First Complete Remission: A Combined Analysis of Dana-Farber ALL Consortium And CIBMTR Cohorts. Presentation at annual ASH meeting in San Francisco, CA, December 2014. Manuscript in preparation. f. LK12-02 Deol A, Sengsayadeth S, Jagasia M, Ahn KW, Wang HL, Sandmaier BM, Devine SM, de Lima M, Weisdorf DJ, Saber W. FLT3 Mutation Increases Relapse Risk After Allogeneic Hematopoietic Cell Transplant for Acute Myeloid Leukemia in First or Second Complete Remission: A CIBMTR Analysis. Presentation at annual ASH meeting in San Francisco, CA, December 2014. Manuscript in preparation. g. LK13-03 Munker R, Wang HL, Brazauskas R, Saber W, Weisdorf DJ. Allogeneic transplant for acute biphenotypic leukemia: characteristics and outcome in the CIBMTR database. Presentation at annual ASBMT meeting in San Diego, CA, February 2015. Studies in progress (Attachment 3) a. LK09-02 Monosomal Karyotype and chromo 7 abnormality in allo HCT for AML/MDS (M Pasquini/ M Battiwala) b. LK12-01 Chemo vs. AlloHCT for Ph- ALL (M Seftel/ D Neuberg) c. LK12-02 Allotx for FLT3/ITD positive AML in CR1 (A Deol/ S Sengsayadeth/ Jagasia M) d. LK13-01 Outcomes after RIC AlloHCT in older adult ALL (A Rosko/ M de Lima/ M Mohty/ V Bachanova) e. LK13-02 Impact of cytogenetic abnormalities in AlloHCT for Ph- ALL in CR1 (A Lazaryan/ V Bachanova/ D Weisdorf) f. LK13-03 Outcomes after allogeneic transplants for ABiL (R Munker) g. LK14-01 Effect of post-remission consolidation chemotherapy prior to alloHCT for ALL in CR1 (N Bejanyan/ A Lazaryan/ D Weisdorf) h. LK14-02 Prognostic factors in patients ≥60 years undergoing alloHCT for AML in CR1/CR2 (F Michelis/ V Gupta) i. LK14-03 Auto vs. ATO in relapsed APL (C Ganzel / M Tallman) j LK15-01 AlloHCT vs. other consolidation therapies per Alliance protocols in older AML in CR1 (A Artz / C Ustun) Manuscript Prep Manuscript Prep Manuscript Prep Analysis Protocol Development Analysis Protocol Development Protocol Development Analysis Protocol Development 2 Not for publication or presentation 5. Future/proposed studies a. PROP 1410-04/1411-60 Comparison of Outcomes between Conditioning Regimens using Reduced Intensity conditioning of Fludarabine plus Melphalan and Myeloablative Regimens Using IV Busulfan plus Fludarabine or IV Busulfan plus Cyclophosphamide in AML and MDS. (DA Hutcherson / HT Liu/ A Nooka / A Langston / M Bishop)(Attachment 4) b. PROP 1411-03 Outcomes of allogeneic transplant for core binding factor leukemias in second or subsequent complete remission. (L Costa / A Saad / S Mineishi) (Attachment 5) c. PROP 1411-20 Effect of in vivo T cell depletion on transplant outcomes in CMV seropositive and seronegative recipients with acute myeloid leukemia. (M Shanavas / D Kim) (Attachment 6) d. PROP 1411-49/1311-34 Impact of GVHD on outcome after allogeneic hematopoietic cell transplantation for acute lymphocytic leukemia: a retrospective registry study (M Yeshurun / JM Rowe / MS Tallman / V Bachanova) (Attachment 7) e. PROP 1411-69 Comparison of outcomes of older adolescents and young adults with Philadelphiachromosome/BCR-ABL1-negative acute lymphoblastic leukemia receiving post-remission consolidation chemotherapy with pediatric-inspired chemotherapy on CALGB 10403 or myeloablative allogeneic hematopoietic cell transplantation. (M Wieduwilt / W Stock) (Attachment 8) f. PROP 1411-71 Prognostic risk factors of patients undergoing allogeneic stem cell transplantation for acute erythroleukemia. (J Cerny / R Nath / Z Zhou) (Attachment 9) g. PROP 1411-74 Comparison of outcomes post allogeneic hematopoietic cell transplant between patients with de novo and secondary acute myeloid leukemia in first complete remission. (F Michelis / H Messner) (Attachment 10) h. PROP 1411-77/1312-09 Comparison of total body irradiation (TBI)-based with intravenous (i.v.) busulfan (Bu) containing chemotherapy-only myeloablative transplant conditioning regimens in adult patients with acute lymphoblastic leukemia (ALL) (P Kebriaei / I Aldoss / V Pullarkat / C Anasetti / D Marks) (Attachment 11) i. PROP 1411-85 Allogeneic (allo) stem cell transplant (SCT) for AML: A comparison of three different reduced intensity conditioning (RIC) regimens in the CIBMTR data base. (R Nath / Z Zhou / J Cerny) (Attachment 12) 6. Other Business 3 Not for publication or presentation Attachment 1 MINUTES AND OVERVIEW PLAN CIBMTR WORKING COMMITTEE FOR ACUTE LEUKEMIA Grapevine, TX Saturday, March 1, 2014, 2:45 pm - 4:45 pm Co-Chair: Co-Chair: Co-Chair: Statisticians: Scientific Director: Donald Bunjes, MD, University Hospital Ulm, Ulm, Germany Telephone: +49-731-500-45532; Fax: +49-731-500-45655; E-mail: donald.bunjes@uniklinik.ulm.de Steven Devine, MD, Ohio State Medical Center - James Cancer Center, Columbus, OH; Telephone: 614-293-9868; Fax: 614-293-6690; E-mail: steven.devine@osumc.edu John F. DiPersio, MD, PhD, Washington University School of Medicine, St. Louis, MO Telephone: 314-454-8491; Fax: 314-454-8315; E-mail: dipersi@im.wustl.edu Hailin Wang, MPH, CIBMTR Statistical Center, Milwaukee, WI Telephone: 414-805-0647; Fax: 414-805-0714; E-mail: hwang@mcw.edu Mei-Jie Zhang, PhD, CIBMTR Statistical Center, Milwaukee, WI Telephone: 414-456-8375; Fax: 414-456-6530; E-mail: meijie@mcw.edu Daniel Weisdorf, MD, University of Minnesota, Minneapolis, MN Telephone: 612-624-3101; Fax: 612-625-6919; E-mail: weisd001@umn.edu 1. Introduction The CIBMTR Acute Leukemia Working Committee was called to order at 2:45 pm on Saturday, March 1st, 2014, by Dr. Daniel Weisdorf. The chairs, scientific director and statisticians were presented. Attendees were asked to have their name badges scanned for attendance purposes and to maintain committee membership, and to fill out the Working Committee evaluations and voting sheets for proposals. The CIBMTR guidelines for voting on proposals were discussed. The guidelines are based on a scale from 1 to 9; 1= high scientific impact, 9= low scientific impact. The meeting was limited to presentation and discussion of proposals. Dr. Donald Bunjes briefly introduced committee’s accomplishments for the past year and progress of ongoing studies. Each proposal presentation was limited to 4 minutes (maximum 4 slides) to allow for adequate time for discussion (5-7 minutes). The minutes of the February 2013 meeting were approved without modifications. Dr. Daniel Weisdorf welcomed Dr. Brenda Sandmaier as newly appointed ALWC chair starting from March 2014 and presented a souvenir to departing chair Dr. Donald Bunjes. 2. Accrual summary Due to the full agenda, the accrual summary of registration and research cases between 1995 and 2013 were not presented to the committee but were available as part of the Working Committee attachments: 4 Not for publication or presentation Attachment 1 AML allogeneic ALL allogeneic AML autologous ALL autologous Research level 16733 9544 1402 222 3. Published/submitted papers and presentations Due to the full agenda, the 2013 presentations and published papers were mentioned, but not presented. Five papers were published, two submitted, one ASH presentation and one ASBMT tandem presentations were given during the past year. These include: a. LK08-02 Koreth J, Pidala J, Perez WS, Deeg HJ, Garcia-Manero G, Malcovati L, Cazzola M, Park S, Itzykson R, Ades L, Fenaux P, Jadersten M, Hellstrom-Lindberg E, Gale RP, Beach CL, Lee SJ, Horowitz MM, Greenberg PL, Tallman MS, DiPersio JF, Bunjes D, Weisdorf DJ, Cutler C. Role of reduced-intensity conditioning allogeneic hematopoietic stem-cell transplantation in older patients with de novo myelodysplastic syndromes: an international collaborative decision analysis. J Clin Oncol. 2013; 31(21):2662-70. b. LK02-05 Foran JM, Pavletic SZ, Logan BR, Agovi-Johnson MA, Perez WS, Bolwell BJ, Bornhauser M, Bredeson CN, Cairo MS, Camitta BM, Copelan EA, Dehn J, Gale RP, George B, Gupta V, Hale GA, Lazarus HM, Litzow MR, Maharaj D, Marks DI, Martino R, Maziarz RT, Rowe JM, Rowlings PA, Savani BN, Savoie ML, Szer J, Waller EK, Wiernik PH, Weisdorf DJ. Unrelated Donor Allogeneic Transplantation After Failure of Autologous Transplantation for Acute Myeloid Leukemia: A Study from the CIBMTR. Biol Blood Marrow Transplant. 2013; 19(7):1102-8. c. LK08-01 Lee SJ, Storer B, Wang H, Lazarus HM, Waller EK, Isola LM, Klumpp TR, Umejiego JB, Savani BN, Loren AW, Cairo MS, Camitta BM, Cutler CS, George B, Khoury HJ, Marks DI, Rizzieri DA, Copelan EA, Gupta V, Liesveld JL, Litzow MR, Miller AM, Schouten HC, Gale RP, Cahn JY, Weisdorf DJ. Providing Personalized Prognostic Information For Adult Leukemia Survivors. Biol Blood Marrow Transplant. 2013; 19(11):1600-7. d. LK10-03 Bachanova V, Marks DI, Zhang MJ, Wang H, de Lima M, Aljurf MD, Arellano M, Artz AS, Bacher U, Cahn JY, Chen YB, Copelan EA, Drobyski WR, Gale RP, Greer JP, Gupta V, Hale GA, Kebriaei P, Lazarus HM, Lewis ID, Lewis VA, Liesveld JL, Litzow MR, Loren AW, Miller AM, Norkin M, Oran B, Pidala J, Rowe JM, Savani BN, Saber W, Vij R, Waller EK, Wiernik PH, Weisdorf DJ. Ph+ ALL patients in first complete remission have similar survival after reduced intensity and myeloablative allogeneic transplantation: Impact of tyrosine kinase inhibitor and minimal residual disease. Leukemia 2013, Epub ahead of print. e. LK10-02 Warlick ED, Paulson K, Brazauskas R, Zhong X, Miller AM, Camitta BM, George B, Savani BN, Ustun C, Marks DI, Waller EK, Baron F, Freytes CO, Socie G, Akpek G, Schouten HC, Lazarus HM, Horwitz EM, Koreth J, Cahn JY, Bornhauser M, Seftel M, Cairo MS, Laughlin MJ, Sabloff M, Ringdén O, Gale RP, Kamble RT, Vij R, Gergis U, Mathews V, Saber W, Chen YB, Liesveld JL, Cutler CS, Ghobadi A, Uy GL, Eapen M, Weisdorf DJ, Litzow MR. Effect of Postremission Therapy before Reduced-Intensity Conditioning Allogeneic Transplantation for Acute Myeloid Leukemia in First Complete Remission. Biol Blood Marrow Transplant 2013, Epub ahead of print. 5 Not for publication or presentation Attachment 1 f. LK04-01 Holter-Chakrabarty JL, Rubinger M, Le-Rademacher J, Wang HL, Grigg A, Selby GB, Szer J, Rowe JM, Weisdorf DJ, Tallman MS. Autologous is Superior to Allogeneic Hematopoietic Cell Transplantation for Acute Promyelocytic Leukemia in Second Complete Remission. Submitted. g. LK07-03c McClune BL, Ahn KW, Wang HL, Antin JH, Artz AS, Cahn JY, Deol A, Freytes CO, Hamadani M, Holmberg LA, Jagasia MH, Jakubowski AA, Kharfan-Dabaja MA, Lazarus HM, Miller AM, Olsson R, Pedersen TL, Pidala J, Pulsipher MA, Rowe JM, Saber W, van Besien KW, Waller EK, Weisdorf DJ. Reduced-Intensity and Non-Myeloablative Hematopoietic Cell Transplantation in Older Patients with Non-Hodgkin Lymphoma (NHL): Encouraging Survival even in Advanced Age. Biol Blood Marrow Transplant 2014, Epub ahead of print. h. LK12-03 Bejanyan N, Weisdorf DJ, Logan B, Wang HL, Devine S, de Lima M, Bunjes D, Zhang MJ. Survival of AML patients Relapsing after Allogeneic Stem Cell Transplantation. Presentation at ASH meeting in New Orleans, LA, December 2013. Manuscript in preparation. i. LK11-01 Goyal S, Zhang MJ, Wang HL, Weisdorf DJ, Uy G. Extramedullary Involvement does not Affect the Outcome of Allogeneic Transplantation for Acute Myeloid Leukemia: a CIBMTR Analysis. Presentation at BMT Tandem meeting in Grapevine, Tx, February 2014. Manuscript in preparation. 4. Studies in progress The studies which made progress during the past year were not presented in order to provide reasonable time to the new proposals for presentation and discussion. A summary of the progress was provided as an attachment to the committee members. These were: LK09-02: Impact of monosomal karyotype in the outcome of hematopoietic cell transplantation for Acute Myeloid Leukemia and Myelodysplasia (M Pasquini/ M Battiwala): The purpose of this study is to identify the impact of high risk cytogenetic subsets: specifically chromosome 7 abnormalities (either monosomy7 or del(7q)) and monosomal karyotype in outcomes for AML and MDS after allogeneic HCT and to evaluate the impact of conditioning intensity in the outcome of patients with AML and monosomal karyotype. Analysis is completed and draft manuscript is being prepared by PI. LK11-01: Impact of extramedullary disease on the outcome of allogeneic HCT in AML (S Goyal/ G Uy): The purpose of this proposal is (1) to describe the outcome of patients undergoing alloHSCT for AML with extramedullary involvement and (2) to assess patient, disease and transplant related factors which influence the outcome of alloHSCT in AML. There are 935 AML patients ≥18 years of age with extramedullary disease prior to HCT reported to the CIBMTR between 1995 and 2010. Analysis is completed and draft manuscript is being prepared by PI. LK12-01: Chemotherapy versus Allogeneic Hematopoietic Cell Transplantation in Philadelphia negative chromosome negative adult ALL (M Seftel): The purpose of the study is to compare HSCT outcomes of younger adults with Philadelphia chromosome negative (Ph-) Acute Lymphoblastic Leukemia (ALL) in first complete remission (CR1) treated with either allogeneic hematopoietic cell transplantation (alloHCT) or with a pediatric style chemotherapy regimen. Draft protocol has been circulated within Working Committee. Protocol finalization and data file preparation is underway. LK12-02: FLT3/ITD mutation in acute myeloid leukemia remains a poor prognostic factor compared to conventional cytogenetics with increased risk of relapse and decreased overall survival after 6 Not for publication or presentation Attachment 1 allogeneic stem cell transplantation in first complete remission (S Sengsayadeth): The purpose of this study is to (1) To study the prognostic significance of FLT3/ITD mutation in AML in patients receiving allo-HSCT in CR1 and (2) To study the impact of FLT3/ITD mutation on incidence of relapse, diseasefree survival (DFS), overall survival (OS) after allo-SCT in CR1. Protocol has been finalized and data file preparation is underway. LK12-03: Survival of AML patients relapsing after allogeneic stem cell transplantation (N Bejanyan/ D Weisdorf/ MJ Zhang): The purpose of this study is to (1) study the clinical outcomes including overall survival (OS) after post-transplant relapse among allogeneic transplant recipients with AML and (2) to identify prognostic factors for survival after post-transplant relapse. Analysis is completed and draft manuscript is being prepared by PI. LK13-01: Allogeneic Transplantation for older patients with Acute Lymphoblastic Leukemia reported to the CIBMTR and EBMT: Impact of age on transplant outcomes (A Rosko/ M de Lima/ M Mohty/ V Bachanova): The purpose of this study is to (1) To analyze outcomes of allogeneic donor transplantation for older patients with acute lymphoblastic leukemia ages 55 years and older who underwent reduced intensity conditioning (2) To define the prognostic factors (patient, disease and transplant related) that impact mortality, relapse and survival. Protocol development is underway. LK13-02: Prognostic significance of cytogenetic abnormalities in patients with Philadelphia-negative ALL undergoing allogeneic Hematopoietic Stem Cell Transplantation in complete remission (A Lazaryan/ V Bachanova): The purpose of this study is to (1) To develop allo-HCT specific cytogenetic classification of Ph-negative ALL for prognostication of relapse and survival outcomes following alloHCT (2) To validate within the CIBMTR database the prognostic significance of existing cytogenetic classifications of Ph-negative ALL in the context of the allo-HCT (3) To compare the performance of both CIBMTR-based and existing classifications of Ph-negative ALL treated with allo-HCT. Protocol development is underway. LK13-03: Allogeneic transplantation for Acute Biphenotypic Leukemia (ABiL): Disease characteristics, complications and outcomes (R Munker): The purpose of this study is to (1) Describe frequency of allogeneic transplant for ABiL, demographics and disease characteristics before transplant (2) Assess patient-, disease- and transplant- related factors which influence the outcome of allogeneic transplant for ABiL. Protocol development is underway. 5. Future/ Proposed studies Drs. Devine, de Lima and Bunjes led this section. The proposals were the following: a. PROP 1310-07 Outcome of allogeneic hematopoietic cell transplantation in patients with acute myeloid leukemia with antecedent history of Philadelphia-negative myeloproliferative Neoplasm (V Gupta) Dr. Gupta presented the proposal. The purpose of this study is to study the outcome of HCT in patients with leukemic transformation from Philadelphia-negative MPN and identify patient, disease and transplant related factors associated with outcome. There are 164 adult patients underwent 1st allo HCT for AML transformed from Ph- MPN between 1996 and 2012. There were comments about the analyzability of cases and completeness of cytogenetic information. b. PROP 1310-19 Allogeneic transplantation to treat secondary AML diagnosed after autologous transplant (L Metheny, M de Lima, H Mohty) 7 Not for publication or presentation Attachment 1 Dr. Metheny presented the proposal. The main purpose of this study is to evaluate overall survival of adult allogeneic HSCT patients with secondary AML following autologous transplant. There were 55 cases who received 1st allo HCT for AML/MDS between 2000 and 2011 after auto HCT for multiple myeloma/HD/NHL. Concern was raised regarding the selection bias of few patients who made through to receive allo HCT after developing secondary leukemia. c. PROP 1311-50 Outcome of umbilical cord blood transplantation (CBT) in adults with high risk acute myeloid leukemia (I Lewis) Dr. Lewis presented the proposal. The purpose of this study is to look at the prognostic significance of high risk cytogenetic or molecular markers in AML compared to other conventional prognostic markers in patients receiving CBT. There were 841 adult patients who received 1st UCB graft allo HCT for AML between 2001 and 2011. Issues regarding the heterogeneity of high risk group were mentioned and incompleteness of cytogenetic and molecular data was brought up. d. PROP 1311-56 Prognostic factors in patients ≥60 years undergoing allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first and second complete remission (FV Michelis, V Gupta) Dr. Michelis presented the proposal. The purpose of this study is to identify patient, disease, and transplant related characteristics associated with outcomes for older patients in particular (≥60 years) with AML undergoing allogeneic hematopoietic cell transplantation (HCT) in CR1 and CR2. There were 4396 adult patients receiving 1st BM/PB graft allo HCT for AML between 1999 and 2011 in CR1 and CR2. No major comments were received. e. PROP 1310-02/1310-04/1312-01 Risk index for Acute Leukemia Patients Receiving Allogeneic Hematopoietic Cell Transplantation (F Anwer, YX Hu, H Huang, R Krishnadasan, C Ustun, D Weisdorf, A Yeager) Dr. Anwer presented the proposal. The main purpose of this study is to create a risk index for acute leukemia patients (AL-RI) receiving allo transplant. There were 8282 adult patients receiving 1st allo HCT in complete remission for AML/ALL between 2001 to 2012. It was suggested that AML and ALL cases to be studied separately due to heterogeneity. f. PROP 1311-34 The graft versus leukemia effect following reduced intensity allotransplant for acute lymphoblastic leukemia (V Bachanova) Dr. Bachanova presented the protocol. The purpose of this study is to identify a graft vs. leukemia (GVL) effect after reduced intensity (RIC) HCT for T and B-ALL by comparing leukemia recurrence in patients with and without acute and/or chronic GVHD. There were 297 adult patients receiving 1st reduced intensity/non-myeloablative conditioning allo HCT in CR1/CR2 for ALL between 1998 and 2011. The issue of limited DLI and TKI information was brought up. g. PROP 1311-43 Effect of post-remission consolidation chemotherapy prior to allogeneic transplantation for acute lymphocytic leukemia in first complete remission: A Center for International Blood and Marrow Transplant Research Study (N Bejanyan, A Lazaryan, D Weisdorf) Dr. Bejanyan presented the proposal. The main purpose of this study is to study overall survival of ALL patients in first complete remission receiving 0 vs. 1 vs. ≥2 post-remission consolidation cycles prior to allo HCT. There were 379 adult patients receiving 1st bone marrow / peripheral blood graft allo HCT in CR1 for ALL between 2008 and 2011. It was suggested that consolidation drugs to be reviewed extensively. 8 Not for publication or presentation Attachment 1 h. PROP 1312-09 Comparison of total body irradiation (TBI)-based with intravenous (i.v.) busulfan (Bu) containing chemotherapy-only myeloablative transplant conditioning regimens in patients with acute lymphoblastic leukemia (P Kebriaei, D Marks) Dr. Kebriaei presented the proposal. The purpose of this study is to Compare transplant outcomes in patients receiving myeloablative TBI-based transplant conditioning with a chemotherapy-only regimen consisting of i.v. Bu and nucleoside analogue therapy. There were 611 adult patients receiving TBI/ivBu based conditioning 1st allo HCT for non-L3 ALL between 2005 and 2012 reported to CIBMTR, and 94 patients receiving ivBu+Clofarabine based conditioning 1st allo HCT from MDACC. Questions were raised regarding different HCT time period in 2 cohorts and relatively short follow-up in MDACC cohort. Also current sample size might not have enough statistical power to prove the hypothesis. i. PROP 1311-05 Second Allogeneic Transplantation using a Reduced Intensity Conditioning Preparative Regimen in the Case of Relapse or Graft Failure in Patients with Acute Leukemia (R Salit, C Delaney, T Gooley) Dr. Milano presented the proposal on behalf of Dr. Salit. The purpose of this study is to examine the early outcomes of patients receiving a second HCT with reduced intensity conditioning for graft failure or relapse of acute leukemia or MDS following their initial allogeneic transplant. There were 267 patients receiving 2nd allo HCT between 2000 and 2011 after graft failure or relapsed 1st allo HCT for AML/ALL/MDS. Nine additional proposals were submitted to the committee, but not presented as stated below: a. PROP 1310-16 Autologous Peripheral Blood Stem Cell Transplantation in Philadelphia-positive Acute Lymphoblastic Leukemia: An Option for Patients with No HLA-match Sibling Donor (G Akpek): insufficient number of autologous transplant cases. b. PROP 1311-38 Effect of Post-transplant Cyclophosphamide on Chronic Severe Graft vs. Host Disease and Relapse in Acute Leukemia (O Ramirez): incomplete documentation and insufficient number of cases (n=92) receiving post-transplant Cyclophosphamide c. PROP 1312-05 Dynamic Bayes Model Averaging for Improved Estimates of BMT/SCT Survival Benefit (P Chaudhary, T Triche, G Ramsingh): complexity of required data and lack of priority. d. PROP 1312-02 Allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia and myelodysplastic syndrome with t(6;9) (H Huang, HY Xian): insufficient number of cases with t(6;9) abnormality (n=46) e. PROP 1311-80 Standard cytotoxic induction vs. induction without cytotoxic chemotherapy prior to allogeneic stem cell transplant for acute myelogenous leukemia (A Hall, M Juckett): insufficient detailed information about the details of induction f. PROP 1311-42 Outcome of Intermediate-risk acute myeloid leukemia patients following matched related and unrelated allogeneic hematopoietic stem cell transplantation in first complete remission compared with second complete remission, stratified by age and comorbidities (F Cheema, R Munker, R Koshy): insufficient scientific impact 9 Not for publication or presentation Attachment 1 g. PROP 1311-44 Do patients with relapsed core binding factor Acute Myeloid Leukemia benefit from salvage allogeneic stem cell transplantation (G Hobbs, MA Perales, E Stein): insufficient scientific impact h. PROP 1311-11/1311-58 Impact of pre-transplant cytogenetic or molecular minimal residual disease on outcomes of allogeneic hematopoietic cell transplantation for acute myeloid leukemia in CR1 or CR2 (B Wirk, M Wieduwilt): insufficient molecular information 6. Other business After the new proposals were presented, each participant in the meeting had the opportunity to rate each proposal using paper ballots. Based on the voting results, current scientific merit and the impact of the study on the field, the following studies will move forward as the committee’s research portfolio for the upcoming year: a. PROP 1311-56 Prognostic factors in patients ≥60 years undergoing allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first and second complete remission b. PROP 1311-43 Effect of post-remission consolidation chemotherapy prior to allogeneic transplantation for acute lymphocytic leukemia in first complete remission: A Center for International Blood and Marrow Transplant Research Study Dr. Daniel Weisdorf expressed gratitude to the Committee members for their active role and valuable support to the Committee. Without additional comments, the meeting was adjourned at 4:30 pm. 10 Not for publication or presentation Attachment 1 Working Committee Overview Plan for 2014-2015 a. LK09-02: Impact of monosomal karyotype in the outcome of hematopoietic cell transplantation for Acute Myeloid Leukemia and Myelodysplasia. Analyses completed and manuscript is under preparation. Submission is anticipated by June 2015. b. LK11-01: Impact of extramedullary disease on the outcome of allogeneic HCT in AML. Manuscript preparation is underway. Submission of paper is expected by June 2014. c. LK12-01: Chemotherapy versus Allogeneic Hematopoietic Cell Transplantation in Philadelphia negative chromosome negative adult ALL. Data file preparation is underway. We plan to finish analysis by June 2014 and submit paper by June 2015. d. LK12-02: FLT3/ITD mutation in acute myeloid leukemia remains a poor prognostic factor compared to conventional cytogenetics with increased risk of relapse and decreased overall survival after allogeneic stem cell transplantation in first complete remission. Data file preparation is completed. We plan to finish analysis by June 2014 and submit paper by June 2015. e. LK13-01: Evaluating outcomes of reduced intensity conditioning allogeneic SCT in older adult lymphoblastic leukemia patients reported to the CIBMTR and EBMT. Protocol development is underway and we plan to move to data file preparation by June 2014. f. LK13-02: Prognostic significance of cytogenetic abnormalities in patients with Philadelphianegative acute lymphoblastic leukemia undergoing allogeneic hematopoietic stem cell transplant ation in complete remission. Protocol development and request of cytogenetics information is underway and we plan to move to data file preparation by June 2014 and finish analysis by June 2015. g. LK13-03: Allogeneic transplantation for Acute Biphenotypic Leukemia: Disease characteristics, complications and outcomes. Protocol development and request of patient forms is underway and we plan to move to data file preparation by June 2014 and finish analysis by June 2015. h. LK14-01: Effect of post-remission consolidation chemotherapy prior to allogeneic transplantation for acute lymphocytic leukemia in first complete remission: A Center for International Blood and Marrow Transplant Research Study. We anticipate developing the study protocol after July 2014 and move to data file preparation by June 2015. i. LK14-02: Prognostic factors in patients ≥60 years undergoing allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first and second complete remission. We anticipate developing the study protocol after July 2014 and move to data file preparation by June 2015. 11 Not for publication or presentation Attachment 1 Oversight Assignments for Working Committee Leadership (March 2014) Daniel Weisdorf LK12-01: Chemotherapy versus Allogeneic Hematopoietic Cell Transplantation in Philadelphia negative chromosome negative adult ALL LK13-02: Prognostic significance of cytogenetic abnormalities in patients with Philadelphia‐negative acute lymphoblastic leukemia undergoing allogeneic hematopoietic stem cell transplantation in complete remission Wael Saber LK12-02: FLT3/ITD mutation in acute myeloid leukemia remains a poor prognostic factor compared to conventional cytogenetics with increased risk of relapse and decreased overall survival after allogeneic stem cell transplantation in first complete remission LK13-01: Evaluating outcomes of reduced intensity conditioning allogeneic SCT in older adult lymphoblastic leukemia patients reported to the CIBMTR and EBMT Marcos de Lima LK09-02: Impact of monosomal karyotype in the outcome of hematopoietic cell transplantation for Acute Myeloid Leukemia and Myelodysplasia LK11-01: Impact of extramedullary disease on the outcome of allogeneic HCT in AML Steven Devine LK14-01: Effect of post-remission consolidation chemotherapy prior to allogeneic transplantation for acute lymphocytic leukemia in first complete remission: A Center for International Blood and Marrow Transplant Research Study LK14-02: Prognostic factors in patients ≥60 years undergoing allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first and second complete remission Brenda Sandmaier LK13-03: Allogeneic transplantation for Acute Biphenotypic Leukemia: Disease characteristics, complications and outcomes 12 Not for publication or presentation Attachment 2 Accrual Summary for the Acute Leukemia Working Committee Characteristics of recipients of allogeneic transplants for AML and ALL reporteda to the CIBMTR between 1995 and 2014 Variable AML ALL Number of patients 17318 9420 Number of centers 376 361 Age in decades Median (range) 42 (<1-83) 20 (<1-75) <10 1613 (9) 2373 (25) 10-19 1813 (10) 2320 (25) 20-29 2135 (12) 1676 (18) 30-39 2490 (14) 1236 (13) 40-49 3382 (20) 1036 (11) 50-59 3647 (21) 612 (6) 60-69 2021 (12) 164 (2) >=70 217 (1) 3 (<1) Gender Male 9130 (53) 5779 (61) Female 8186 (47) 3639 (39) Missing 2 (<1) 2 (<1) HCT-CI 0 2693 (16) 1236 (13) 1 655 (4) 227 (2) 2 509 (3) 144 (2) 3+ 1412 (8) 309 (3) N/A, earlier than 2007 11984 (69) 7487 (79) Missing 65 (<1) 17 (<1) Disease status prior to HCT Primary induction failure 2305 (13) 326 (3) CR1 8197 (47) 3718 (39) CR2 3668 (21) 3301 (35) >=CR3 296 (2) 853 (9) Relapse 2799 (16) 1212 (13) Missing 53 (<1) 10 (<1) Time from diagnosis to HCT Median (range) 6 (<1-607) 12 (<1-499) <6 months 8224 (47) 2584 (27) 6 - 12 months 4335 (25) 2149 (23) >12 months 4739 (27) 4683 (50) Missing 20 (<1) 4 (<1) 13 Not for publication or presentation Variable AML Conditioning regimen intensity Myeloablative 13180 (76) RIC 2937 (17) NMA 494 (3) TBD 530 (3) Missing 177 (1) Graft type Bone marrow 6133 (35) Peripheral blood 9200 (53) Umbilical cord blood 1978 (11) Missing 7 (<1) Type of donor HLA-identical sibling 5970 (34) Identical twin 77 (<1) Other relative 862 (5) Unrelated 8384 (48) Cord blood 1978 (11) Missing 47 (<1) Year of HCT 1995-1996 1639 (9) 1997-1998 1441 (8) 1999-2000 1410 (8) 2001-2002 1775 (10) 2003-2004 2085 (12) 2005-2006 2522 (15) 2007-2008 2372 (14) 2009-2010 2056 (12) 2011-2012b 848 (5) b 2013-2014 1170 (7) Median follow-up of survivors (range), months 71 (1-223) a Patients have available comprehensive research form and consented for research b Cases continue to be reported in this interval Attachment 2 ALL 8703 (92) 441 (5) 58 (<1) 134 (1) 84 (<1) 4591 (49) 3218 (34) 1607 (17) 4 (<1) 2781 (30) 52 (<1) 516 (5) 4446 (47) 1607 (17) 18 (<1) 1296 (14) 1122 (12) 1056 (11) 1099 (12) 1115 (12) 1248 (13) 1051 (11) 621 (7) 411 (4) 401 (4) 73 (<1-223) 14 Not for publication or presentation Attachment 2 Accrual Summary for Acute Leukemia Working Committee Characteristics of recipients of autologous transplants for AML and ALL reporteda to the CIBMTR between 1995 and 2014 Variable AML ALL Number of patients 963 154 Number of centers 176 57 Age in decades Median (range) 44 (<1-78) 29 (1-66) <10 61 (6) 16 (10) 10-19 68 (7) 25 (16) 20-29 118 (12) 38 (25) 30-39 166 (17) 19 (12) 40-49 179 (19) 27 (18) 50-59 210 (22) 22 (14) 60-69 153 (16) 7 (5) >=70 8 (<1) 0 Gender Male 486 (50) 96 (62) Female 477 (50) 58 (38) Disease status prior to HCT Primary induction failure 10 (1) 2 (1) CR1 629 (65) 98 (64) CR2 241 (25) 43 (28) >=CR3 14 (1) 6 (4) Relapse 66 (7) 5 (3) Missing 3 (<1) 0 Time from diagnosis to HCT Median (range) 7 (<1-584) 9 (2-153) <6 months 405 (42) 22 (14) 6 - 12 months 261 (27) 72 (47) >12 months 297 (31) 60 (39) Conditioning regimen intensity Myeloablative 784 (81) 148 (96) NMA 4 (<1) 1 (<1) TBD 172 (18) 5 (3) Missing 3 (<1) 0 Graft type Bone marrow 168 (17) 25 (16) Peripheral blood 792 (82) 128 (83) Missing 3 (<1) 1 (<1) 15 Not for publication or presentation Variable AML Year of HCT 1995-1996 267 (28) 1997-1998 222 (23) 1999-2000 107 (11) 2001-2002 89 (9) 2003-2004 65 (7) 2005-2006 86 (9) 2007-2008 99 (10) 2009-2010 17 (2) b 2011-2012 4 (<1) b 2013-2014 7 (<1) Median follow-up of survivors (range), months 87 (1-226) a Patients have available comprehensive research form and consented for research b Cases continue to be reported in this interval Attachment 2 ALL 55 (36) 45 (29) 16 (10) 12 (8) 5 (3) 9 (6) 10 (6) 1 (<1) 0 1 (<1) 121 (2-217) 16 Not for publication or presentation Attachment 3 TO: Acute Leukemia Working Committee Members FROM: Daniel J. Weisdorf, MD; Scientific Director and Wael Saber, MD, MS; Assistant Scientific Director for the Acute Leukemia Working Committee RE: Studies in Progress Summary LK09-02: Impact of monosomal karyotype in the outcome of hematopoietic cell transplantation for Acute Myeloid Leukemia and Myelodysplasia (M Pasquini/ M Battiwalla) The purpose of this study is to identify the impact of high risk cytogenetic subsets: specifically chromosome 7 abnormalities (either monosomy7 or del(7q)) and monosomal karyotype in outcomes for AML and MDS after allogeneic HCT and to evaluate the impact of conditioning intensity in the outcome of patients with AML and monosomal karyotype. Analysis is completed and draft manuscript is being prepared by PI. LK12-01: Chemotherapy versus Allogeneic Hematopoietic Cell Transplantation in Philadelphia negative chromosome negative adult ALL (M Seftel) The purpose of the study is to compare HSCT outcomes of younger adults with Philadelphia chromosome negative (Ph-) Acute Lymphoblastic Leukemia (ALL) in first complete remission (CR1) treated with either allogeneic hematopoietic cell transplantation (alloHCT) or with a pediatric style chemotherapy regimen. Analysis is completed and 1st draft manuscript is available. LK12-02: FLT3/ITD mutation in acute myeloid leukemia remains a poor prognostic factor compared to conventional cytogenetics with increased risk of relapse and decreased overall survival after allogeneic stem cell transplantation in first complete remission (S Sengsayadeth) The purpose of this study is to (1) To study the prognostic significance of FLT3/ITD mutation in AML in patients receiving allo-HSCT in CR1 and (2) To study the impact of FLT3/ITD mutation on incidence of relapse, disease-free survival (DFS), overall survival (OS) after allo-SCT in CR1. Analysis is completed and 1st draft manuscript is available. LK13-01: Allogeneic Transplantation for older patients with Acute Lymphoblastic Leukemia reported to the CIBMTR and EBMT: Impact of age on transplant outcomes (A Rosko/ M de Lima/ M Mohty/ V Bachanova) The purpose of this study is to (1) To analyze outcomes of allogeneic donor transplantation for older patients with acute lymphoblastic leukemia ages 55 years and older who underwent reduced intensity conditioning (2) To define the prognostic factors (patient, disease and transplant related) that impact mortality, relapse and survival. Analysis is underway. LK13-02: Prognostic significance of cytogenetic abnormalities in patients with Philadelphia-negative ALL undergoing allogeneic Hematopoietic Stem Cell Transplantation in complete remission (A Lazaryan/ V Bachanova) The purpose of this study is to (1) To develop allo-HCT specific cytogenetic classification of Ph-negative ALL for prognostication of relapse and survival outcomes following allo-HCT (2) To validate within the CIBMTR database the prognostic significance of existing cytogenetic classifications of Phnegative ALL in the context of the allo-HCT (3) To compare the performance of both CIBMTR-based and 17 Not for publication or presentation Attachment 3 existing classifications of Ph-negative ALL treated with allo-HCT. Protocol development and cytogenetic data review is underway. LK13-03: Allogeneic transplantation for Acute Biphenotypic Leukemia (ABiL): Disease characteristics, complications and outcomes (R Munker) The purpose of this study is to (1) Describe frequency of allogeneic transplant for ABiL, demographics and disease characteristics before transplant (2) Assess patient-, disease- and transplant- related factors which influence the outcome of allogeneic transplant for ABiL. Analysis is underway. LK14-01: Effect of post-remission consolidation chemotherapy prior to allogeneic transplantation for acute lymphocytic leukemia in first complete remission (N Bejanyan/ A Lazaryan/ D Weisdorf) The purpose of this study is to (1) To study relapse, TRM and survival outcomes of ALL patients in CR1 receiving 0 vs. 1 vs. ≥2 post-remission consolidation cycles prior to allo-HCT. (2) To study relapse, TRM and survival outcomes in subgroup of ALL patients with MRD positivity who receive 0 vs. 1 vs. ≥2 postremission consolidation cycles prior to allo-HCT. Protocol development is underway. LK14-02: Prognostic factors in patients ≥60 years undergoing allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first and second complete remission (F Michelis/ V Gupta) The purpose of this study is to (1)To identify patient, disease, and transplant related characteristics associated with outcomes for older patients in particular (≥60 years) with AML undergoing allo-HCT in CR1 and CR2. (2) To compare outcomes between patients within different age (<60 yrs vs. ≥60 yrs) or remission status (CR1 vs. CR2) group. (3) To assess the impact of HCT-CI (0-2 vs. ≥3) on outcomes in all patients with HCT-CI available and a subgroup of CR2 patients only. Protocol development is underway. LK14-03: Autologous transplant vs. arsenic trioxide in relapsed Acute Promyelocytic Leukemia (C Ganzel / M Tallman) The purpose of this study is to compare between the 2 treatment groups for demographics, details of disease presentation, frontline treatment and outcomes including disease free survival and overall survival. Analysis is under way. LK15-01: Comparison of Allogeneic Hematopoietic Cell Transplantation (AlloHCT) with Other Consolidation Therapies Per Alliance Protocols in Older (≥60 years) AML Patients in First Complete Remission (CR1) (A Artz / C Ustun) The purpose of this study is to (1) To compare DFS and TRM between alloHCT and non-alloHCT consolidations (2) To find the frequency of acute and chronic graft-versus-host disease (GVHD) in the alloHCT cohort (3) To identify patient or disease characteristics (age, cytogenetic risk group, etc.) which preferentially benefit patients receiving alloHCT vs. non-alloHCT consolidation therapy. Data preparation and protocol review is underway. 18 Not for publication or presentation Attachment 4 Study Proposal 1410-04/1411-60 Study Title: Comparison of Outcomes between Conditioning Regimens using Reduced Intensity conditioning of Fludarabine plus Melphalan and Myeloablative Regimens Using IV Busulfan plus Fludarabine or IV Busulfan plus Cyclophosphamide in AML and MDS Donald A Hutcherson, RPh, Pharmacy BS, Emory University Hospital/Winship Cancer Institute, Don.Hutcherson@emoryhealthcare.org Hongtao Liu, MD, Ph.D., The University of Chicago Medical Center, hliu2@medicine.bsd.uchicago.edu Ajay Nooka, Doctor of Medicine, Emory University Hospital/Winship Cancer Institute, anooka@emory.edu Amelia Langston, Doctor of Medicine, Emory University Hospital/Winship Cancer Institute, Amelia.Langston@emoryhealthcare.org Michael Bishop, MD, The University of Chicago Medical Center, mbishop@medicine.bsd.uchicago.edu Hypothesis: Busulfan plus cyclophosphamide (Bu/Cy) provides superior disease free survival in younger patients compared to either fludarabine plus melphalan (Flu/Mel) or busulfan plus fludarabine (Bu/Flu) while Bu/Flu and Flu/Mel produce less TRM in older patients and comparable overall survival. Specific Aims: This study will compare short term outcomes of engraftment rates, reported infections prior to day 100, sinusoidal obstruction syndrome (SOS), survival at day 100, non-relapse mortality, regimen related toxicities, best response to transplant and aGVHD for site and overall grade. Long term outcomes will include incidence of cGVHD, cause of death, disease-free and overall survival. Multivariate analysis will be performed to compare outcomes by disease (AML or MDS), disease status, age, sex, race, transplant type, product type, degree of match, GVHD prophylaxis (tacrolimus, cyclosporine, sirolimus, methotrexate dosing, mycophenolate, anti-lymphocyte globulin, other), recipient and donor CMV status, comorbidity scores, busulfan dose, busulfan frequency (Q 24h vs. q6h) and drug timing of administration (if available, Bu/Flu sequential vs concurrent and Cy/Bu vs Bu/Cy). Scientific Justification: Few randomized clinical trials have been performed to compare myeloablative transplantation using Bu/Cy to Bu/Flu or either of these against reduced intensity Flu/Mel in AML/MDS. Several reports have found the busulfan regimens had similar long term outcomes. Liu, et al report the results of allogeneic transplant study for Bu/Cy vs Bu/Flu in 108 patients with a median age 30.5 (12 – 54) with AML in first CR. While the Bu/Flu provided lower incidence of grade III-IV regimen related toxicity than Bu/Cy, there was no difference seen in treatment related mortality, incidence of relapse, overall or disease-free survival at 5 years [1]. Lee, et al studied leukemia and MDS patients aged 17 to 59 treated in a randomized Phase III trial with either Bu/Cy or Bu/Flu. This trial demonstrated better overall, relapsefree and event-free survival for Bu/Cy at 2 years [2]. As part of a subset analysis of study CIBMTR SC0901, Bredeson, et al compared outcomes of 601 Bu/Cy vs. 424 Bu/Flu transplants for AML, MDS and CML. While the groups were not well balanced for age, performance status and other factors, in this large series no difference could be seen in mortality, treatment failure, relapse, treatment related mortality and VOD[3]. 19 Not for publication or presentation Attachment 4 With regards to Flu/Mel, several retrospective registry analyses compared the outcomes after RIC and MA SCT in older AML patients. Two separate analyses using EBMT data compared RIC and MA SCT using matched related donor (MRD) or matched unrelated donor (MUD). Not surprisingly, these two studies reached similar conclusion. Both RIC MRD and MUD transplant recipients more than 50 years had reduced adjusted non-relapse mortality, but higher cumulative incidence of relapse resulting in similar leukemia-free survival compared to patients who had MAC MRD or MUD transplant [4,5]. Similar results were found in patients with MDS or secondary AML who received RIC vs MA MRD SCT with increased relapse rate, but decrease NRM in RIC SCT, and comparable PFS and OS in the older patients [6]. Recently, Luger et al published so far the largest retrospective comparison of MA (3731 patients) with RIC/NMA (non-myeloablative) (1448 patients) regimens in AML/MDS patients using the CIBMTR data between 1997 and 2004. NMA conditioning resulted in inferior DFS and OS, but there was no difference in DFS and OS between RIC and MA regimens with adjusted OS at 5 years was 34, 33 and 26% for MA, RIC and NMA transplants, respectively [7]. The findings from these retrospective studies were further confirmed by so far the only prospective, open-label randomized phase III trial to compare RIC and standard MA conditioning in patients with acute myeloid leukemia in first complete remission [8]. One hundred ninety-five Patients aged 18–60 years with intermediate-risk or high-risk AML in CR1 were randomly assigned to receive RIC or standard conditioning. RIC SCT results in a similar incidence of nonrelapse mortality and reduced toxic effects compared with standard conditioning without affecting survival outcomes [8]. These studies established the role of RIC in the allo-SCT of acute leukemia patients, especially for older patients or patients with co-morbidities not suitable for MA regimens. All these retrospective and prospective studies compared mixed myeloablative regimens; mainly TBI based regimen, Busulfan/cyclophosphamide (Bu/Cy) and mixed RIC regimens, mainly fludarabine/melphalan. While TBI-based regimen might still provide marginal survival benefit for ALL patients, due to the poor tolerability of older patients to TBI based regimen, and comparable outcomes between TBI/Cy vs Bu/Cy have been demonstrated in allo-SCT for acute leukemia; although Bu/Cy and Bu/Flu might not be completely same [2]; Flu/Bu has been more widely used as a myeloablative regimen in elderly patients. On the other hand, Flu/Mel was one of most commonly used RIC regimens for AML/MDS. While Bu/Flu is usually chosen for ALL patients due to the results from Moffitt cancer center [9]; the option between Bu/Flu and Flu/Mel for AML and high risk MDS is still unclear. So far, there is no direct comparison between Bu/Flu (IV) and Flu/Mel regimen in allo-SCT for acute leukemia, except a small early study to compare the kinetics of myeloablation between Bu/Flu and Flu/Mel in allogeneic peripheral blood stem cell transplantation [10]. Thus, one approach is to give Bu/Flu if it is felt that the patient could tolerate without increased risk of VOD for patients with AML/high risk MDS, and Flu/Mel if not candidate for Bu/Flu. For the patients with better performance status, one must consider whether Bu/Cy may give better disease control than other regimens allowing for improved overall survival. While the desire to find better tolerated conditioning regimens, especially for older patients, has increased the substitution of fludarabine for cyclophosphamide, Flu/Mel has remained a widely used reduced intensity regimen. Using data from the CIBMTR database, we hope to determine whether one of these regimens might provide a better platform for transplanting specific patient populations and if the most common selections in GVHD prophylaxis alter patient outcomes for these regimens. Patient Eligibility: AML or MDS Ages > 18 Related or unrelated donor (Related haploidentical donor or UCB transplants excluded) Myeloablative dosing of IV Bu/Cy, IV Bu/Flu or RIC Flu/Mel Transplantation dates 2002 through 2012 20 Not for publication or presentation Attachment 4 Data Requirements: This project’s goal is to use existing data in the database. Sample Requirements from Data repository: None Study Design (Scientific Plan): All AML and high risk MDS patients received allo-SCT in CR1 and beyond who were conditioned with fludarabine/Busulfan (IV, >=8mg/kg), cyclophosphamide/Busulfan (IV, >8mg/kg), or fludarabine/melphalan (<=140mg/m2) with information available in the designated time period will be included in the analysis. Descriptive tables of patient-, disease-, and transplant related factors will be prepared. The tables will list median and range for continuous variables and percent of total for categorical variables. Characteristics of patients will be compared using the chi-square test for categorical variables and the Wilcoxon two-sample test for continuous variables. Outcomes will be defined as above. Comparing the outcomes between the Bu regimens and Flu/Mel transplant groups will require adjustment for baseline patient characteristics. To adjust for differences in the baseline characteristics, Cox proportional hazards regression will be used. Probability of DFS and OS will be calculated using the Kaplan-Meier estimator. Comparison of survival curves will be done using the logrank test. References: 1. H. Liu, X. Zhai, Z. Song, et al., Busulfan plus fludarabine as a myeloablative conditioning regimen compared with busulfan plus cyclophosphamide for acute myeloid leukemia in first complete remission undergoing allogeneic hematopoietic stem cell transplantation: a prospective and multicenter study, J Hematol Oncol, 6 (2013), p. 15. 2. J. Lee, J Young-Don, et al. Randomized Trial of Myeloablative Conditioning Regimens: Busulfan Plus Cyclophosphamide Versus Busulfan Plus Fludarabine. JCO 31, Feb 20, 2013, p. 701. 3. Prospective cohort study comparing intravenous busulfan to total body irradiation in hematopoietic cell transplantation. Christopher Bredeson, et al. Blood Dec 2013, 122 (24) 3871-3878. 4. Ringden, O., et al., Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol, 2009. 27(27): p. 4570-7. 5. Aoudjhane, M., et al., Comparative outcome of reduced intensity and myeloablative conditioning regimen in HLA identical sibling allogeneic haematopoietic stem cell transplantation for patients older than 50 years of age with acute myeloblastic leukaemia: a retrospective survey from the Acute Leukemia Working Party (ALWP) of the European group for Blood and Marrow Transplantation (EBMT). Leukemia, 2005. 19(12): p. 2304-12. 6. Martino, R., et al., Retrospective comparison of reduced-intensity conditioning and conventional high-dose conditioning for allogeneic hematopoietic stem cell transplantation using HLA-identical sibling donors in myelodysplastic syndromes. Blood, 2006. 108(3): p. 836-46. 7. Luger, S.M., et al., Similar outcomes using myeloablative vs reduced-intensity allogeneic transplant preparative regimens for AML or MDS. Bone Marrow Transplant. 47(2): p. 203-11. 8. Bornhauser, M., et al., Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 9. Santarone, S., et al., Fludarabine and pharmacokinetic-targeted busulfan before allografting for adults with acute lymphoid leukemia. Biol Blood Marrow Transplant, 2011. 17(10): p. 1505-11. 10. Chunduri, S., et al., Comparable kinetics of myeloablation between fludarabine/full-dose busulfan and fludarabine/melphalan conditioning regimens in allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant, 2006. 38(7): p. 477-82. 21 Not for publication or presentation Attachment 4 Characteristics of Study Population Variable Number of patients Number of centers Age in decades Median (range) 18-29 30-39 40-49 50-59 60-69 >=70 Karnofsky score <90% >=90% Missing White blood count at diagnosis (x10^9/L) Median (range) <= 10 10 - 100 > 100 Missing Disease AML MDS Disease status prior to HCT Primary induction failure CR1 CR2 >=CR3 Relapse Disease status prior to HCT for MDS MDS early MDS advanced MDS Other Conditioning regimen Bu+Cy Bu+Cy+Arac Bu+Cy+VP16 Bu+Cy+Thio Bu+Cy+other MAC IVBu+Cy MAC IVBu+Flu 1569 1466 134 97 RIC Flu+Mel 885 96 48 (18-71) 228 (15) 224 (14) 448 (29) 544 (35) 122 (8) 3 (<1) 53 (19-75) 149 (10) 161 (11) 307 (21) 543 (37) 297 (20) 9 (<1) 59 (18-75) 33 (4) 39 (4) 105 (12) 286 (32) 388 (44) 34 (4) 512 (33) 984 (63) 73 (5) 517 (35) 835 (57) 114 (8) 347 (39) 510 (58) 28 (3) 6 (<1-2247) 844 (54) 461 (29) 102 (7) 162 (10) 5 (<1-5500) 797 (54) 379 (26) 80 (5) 210 (14) 4 (<1-9973) 489 (55) 205 (23) 45 (5) 146 (16) 1201 (77) 368 (23) 1056 (72) 410 (28) 606 (68) 279 (32) 196 (12) 595 (38) 234 (15) 17 (1) 159 (10) 150 (10) 532 (36) 205 (14) 13 (<1) 156 (11) 145 (16) 246 (28) 91 (10) 3 (<1) 121 (14) 105 (7) 250 (16) 13 (<1) 154 (11) 249 (17) 7 (<1) 84 (9) 181 (20) 14 (2) 1450 (92) 46 (3) 36 (2) 11 (<1) 26 (2) 0 0 0 0 0 0 0 0 0 0 22 Not for publication or presentation Variable Bu+Flu Bu+Flu+Mel Bu+Flu+TBI Bu+Flu+Thio Bu+Flu+other Flu+Mel Flu+Mel+BCNU Flu+Mel+other Time from diagnosis to HCT Median (range) <6 months 6 - 12 months >12 months Missing GVHD prophylaxis No GVHD prophylaxis Ex-vivo T-cell depletion CD34 selection Post-tx cy FK506 + MMF +- others FK506 + MTX +- others FK506 + others FK506 alone CSA + MMF +- others CSA + MTX +- others CSA + others CSA alone Other GVHD prophylaxis Missing ATG/Campath ATG + CAMPATH ATG alone CAMPATH alone No ATG or CAMPATH Missing Type of donor HLA-identical sibling Well-matched unrelated Partially matched unrelated Mismatched unrelated Attachment 4 MAC IVBu+Cy MAC IVBu+Flu 0 1295 (88) 0 73 (5) 0 69 (5) 0 7 (<1) 0 22 (2) 0 0 0 0 0 0 RIC Flu+Mel 0 0 0 0 0 713 (81) 129 (15) 43 (5) 6 (<1-607) 844 (54) 350 (22) 374 (24) 1 (<1) 7 (<1-173) 635 (43) 426 (29) 404 (28) 1 (<1) 7 (<1-275) 378 (43) 265 (30) 242 (27) 0 11 (<1) 28 (2) 6 (<1) 27 (2) 107 (7) 927 (59) 42 (3) 41 (3) 45 (3) 263 (17) 17 (1) 37 (2) 17 (1) 1 (<1) 14 (<1) 47 (3) 26 (2) 15 (1) 321 (22) 805 (55) 58 (4) 44 (3) 23 (2) 75 (5) 6 (<1) 16 (1) 8 (<1) 8 (<1) 20 (2) 3 (<1) 3 (<1) 1 (<1) 165 (19) 225 (25) 55 (6) 54 (6) 134 (15) 120 (14) 63 (7) 33 (4) 7 (<1) 2 (<1) 0 303 (19) 14 (<1) 1230 (78) 22 (1) 0 678 (46) 35 (2) 699 (48) 54 (4) 1 (<1) 241 (27) 159 (18) 434 (49) 50 (6) 555 (35) 718 (46) 194 (12) 33 (2) 402 (27) 746 (51) 232 (16) 25 (2) 203 (23) 434 (49) 146 (16) 33 (4) 23 Not for publication or presentation Variable Unrelated TBD Graft type Bone marrow Peripheral blood Year of HCT 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Median follow-up of survivors (range), months Attachment 4 MAC IVBu+Cy MAC IVBu+Flu 69 (4) 61 (4) RIC Flu+Mel 69 (8) 405 (26) 1164 (74) 259 (18) 1207 (82) 131 (15) 754 (85) 28 (2) 67 (4) 157 (10) 191 (12) 184 (12) 172 (11) 231 (15) 212 (14) 229 (15) 45 (3) 53 (3) 58 (3-143) 31 (2) 56 (4) 58 (4) 122 (8) 140 (10) 161 (11) 185 (13) 259 (18) 193 (13) 130 (9) 131 (9) 51 (3-127) 51 (6) 83 (9) 100 (11) 128 (14) 110 (12) 101 (11) 84 (9) 67 (8) 18 (2) 55 (6) 88 (10) 60 (3-124) Selection criteria: st 1 HCT for adult AML/MDS between 2002 and 2012 after CAP modeling Myeloablative conditioning of IV Bu/Cy, IV Bu/Flu or RIC Flu/Mel Bone marrow or peripheral blood graft Excluding identical twin and haploidentical donor Complete research form Patient consent 24 Not for publication or presentation Attachment 5 Study Proposal 1411-03 Study Title: Outcomes of autologous and allogeneic transplant for core binding factor leukemias in second or subsequent complete remission Luciano J. Costa, MD, PhD, University of Alabama at Birmingham, AL, ljcosta@uabmc.edu Ayman Saad, MD, University of Alabama at Birmingham, AL, asaad@uabmc.edu Shin Mineishi, MD, University of Alabama at Birmingham, AL, smineishi@uabmc.edu Hypothesis: Patients with core binding factor (CBF) leukemias in second or subsequent remission have outcomes with autologous HCT (auto-HCT) that are comparable to outcomes with allogeneic HCT (allo-HCT). Specific Aims: 1. To describe outcomes of auto-HCT and allo-HCT in patients with CBF leukemia in second or subsequent remission 2. To compare leukemia free survival (LFS), overall survival (OS) and non-relapse mortality (NRM) between auto-HCT and allo-HCT in the above setting adjusting for co-variables that may independent affect outcomes. Scientific Justification: Acute myelogenous leukemia with inv(16), t(16;16) or t(8;21) (CBF AML) account for approximately 15% of cases of AML1,2, typically present in younger patients and have a relatively favorable prognosis when compared to other cytogenetic subtypes of AML. Conventional cytotoxic chemotherapy containing high doses of cytarabine is currently the preferred post-remission therapy and HCT is not typically pursued in CR13. Even though the initial remission rate is approximately 90%1-3 , up to 50% of patients in CR will experience relapse1,2. Nevertheless, the 5-year survival is above 50%1,2, indicating that many patients will experience leukemia relapse but benefit from subsequent therapy that, in most cases, will include HCT. The vast majority of HCT performed for AML are allogeneic transplants, aiming at the proven benefit of graft-versus-leukemia (GVL) effect. The benefit of GVL is at least partially overcome by the risk of graft versus host disease (GVHD). Although the balance of GVL/GVHD clearly favors allo-HCT in intermediate and high risk leukemias, this is less clear in CBF-AML where the risk of relapse is lower4. In fact, outcomes of auto-HCT in CBF leukemia have been reported to be similar to allo-HCT in a large US intergroup study3. A large retrospective European study also identified near “identical” outcomes between auto-HCT and genoidentical allo-HCT for patients in CR15. Very similar outcomes were also seen in a large Japanese study6 and in a German individual patient data meta-analysis7. Much less is known about the outcomes of patients in CR2+ with auto-HCT and with alternative donor transplantation8. Patient Eligibility Population: Diagnosis of AML with inv (16), t(16;16) or t(8;21) Second or subsequent complete remission at time of transplant First HCT of any type No age restriction. Data available at least to day+100. 25 Not for publication or presentation Attachment 5 Transplant between 1992 and 2012 Data Requirements: No supplemental data collection is required. Sample Requirements: No samples required. Study Design: Variables to be analyzed: Patient related: Age Sex HCT-CI prior to transplant KPS prior to transplant Race/ethnicity Disease related: Presence of kit mutation9, if known Number of lines of therapy prior to transplant. CR2 vs CR3+ Transplant related: Auto-HCT vs. Allo-HCT (main effect) Conditioning regimen (MA vs. RIC vs. NMA) Mobilization regimen (for auto-HCT) Donor source (MRD, MMRD, MUD, MMUD). Graft type (peripheral blood, bone marrow, cord blood). Time from diagnosis to transplant Calendar year of transplant Outcomes: Engraftment kinetics Rate and severity of acute and chronic GVHD. Duration of follow up and survival status. Occurrence and timing of relapse. Cause of death Occurrence of second transplant (timing and type) Analysis plan: LFS, OS, NRM and cumulative incidence of relapse (CIR) will be described for both auto-HCT and alloHCT. Relapse and non-relapse death will be treated as competing events. If numbers allow, outcomes of allo-HCT will be described for different donor types (MRD, MMRD, MUD/MUD, cord blood). A multivariate analysis (MVA) including patient-related, disease-related and transplant-related variables will be performed to identify factors associated with the main endpoints of LFS and OS. Type of HCT (auto-HCT or allo-HCT), the main interest of the study, will be “forced” into each of the multivariate models. If the number of patients allows we will perform propensity score matching prior to comparing transplant strategies (as an alternative to MVA). 26 Not for publication or presentation Attachment 5 References: 1. Grimwade D, Hills RK, Moorman AV, et al: Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 116:354-65, 2010 2. Byrd JC, Mrozek K, Dodge RK, et al: Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100:4325-36, 2002 3. Slovak ML, Kopecky KJ, Cassileth PA, et al: Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 96:4075-83, 2000 4. Burnett AK, Goldstone AH, Stevens RM, et al: Randomised comparison of addition of autologous bone-marrow transplantation to intensive chemotherapy for acute myeloid leukaemia in first remission: results of MRC AML 10 trial. UK Medical Research Council Adult and Children's Leukaemia Working Parties. Lancet 351:700-8, 1998 5. Gorin NC, Labopin M, Frassoni F, et al: Identical outcome after autologous or allogeneic genoidentical hematopoietic stem-cell transplantation in first remission of acute myelocytic leukemia carrying inversion 16 or t(8;21): a retrospective study from the European Cooperative Group for Blood and Marrow Transplantation. J Clin Oncol 26:3183-8, 2008 6. Kuwatsuka Y, Miyamura K, Suzuki R, et al: Hematopoietic stem cell transplantation for core binding factor acute myeloid leukemia: t(8;21) and inv(16) represent different clinical outcomes. Blood 113:2096-103, 2009 7. Schlenk RF, Benner A, Krauter J, et al: Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol 22:3741-50, 2004 8. Hospital MA, Prebet T, Bertoli S, et al: Core-binding factor acute myeloid leukemia in first relapse: a retrospective study from the French AML Intergroup. Blood 124:1312-9, 2014 9. Paschka P, Marcucci G, Ruppert AS, et al: Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol 24:3904-11, 2006 27 Not for publication or presentation Attachment 5 Characteristics of Study Population Variable Number of patients Number of centers Age in decades Median (range) <10 10-19 20-29 30-39 40-49 50-59 60-69 >=70 Gender Male Female Recipient race Caucasian African-American Asian Pacific islander Native American Other Unknown Karnofsky score <90% >=90% Missing White blood count at diagnosis Median (range) <= 10 10 - 100 > 100 Missing HCT-CI 0 1 2 3+ N/A, earlier than 2007 CR2 421 143 >=CR3 28 19 34 (2-75) 49 (12) 60 (14) 73 (17) 63 (15) 85 (20) 67 (16) 19 (5) 5 (1) 43 (5-67) 1 (4) 1 (4) 6 (21) 4 (14) 6 (21) 5 (18) 5 (18) 0 243 (58) 178 (42) 16 (57) 12 (43) 345 (82) 22 (5) 39 (9) 1 (<1) 2 (<1) 2 (<1) 10 (2) 18 (64) 5 (18) 2 (7) 1 (4) 0 0 2 (7) 74 (18) 325 (77) 22 (5) 3 (11) 22 (79) 3 (11) 30 (<1-462) 107 (25) 195 (46) 56 (13) 63 (15) 17 (1-158) 6 (21) 12 (43) 2 (7) 8 (29) 118 (28) 18 (4) 12 (3) 46 (11) 225 (53) 9 (32) 1 (4) 2 (7) 4 (14) 12 (43) 28 Not for publication or presentation Variable Missing Conditioning regimen intensity Myeloablative RIC NMA TBD Missing Time from diagnosis to HCT Median (range) <6 months 6 - 12 months >12 months Graft type Bone marrow Peripheral blood Umbilical cord blood Type of donor HLA-identical sibling Other related Well-matched unrelated Partially matched unrelated Mismatched unrelated Unrelated TBD Cord blood Donor/Recipient sex match M/M M/F F/M F/F TBD Donor/Recipient CMV match -/-/+ +/+/+ TBD GVHD prophylaxis No GVHD prophylaxis Ex-vivo T-cell depletion CD34 selection Attachment 5 CR2 2 (<1) >=CR3 0 344 (82) 68 (16) 5 (1) 3 (<1) 1 (<1) 20 (71) 5 (18) 2 (7) 1 (4) 0 17 (2-95) 7 (2) 47 (11) 367 (87) 24 (15-59) 0 0 28 118 (28) 217 (52) 86 (20) 7 (25) 11 (39) 10 (36) 101 (24) 17 (4) 126 (30) 50 (12) 13 (3) 28 (7) 86 (20) 1 (4) 1 (4) 10 (36) 5 (18) 1 (4) 0 10 (36) 148 (35) 103 (24) 94 (22) 73 (17) 3 (<1) 10 (36) 5 (18) 6 (21) 7 (25) 0 98 (23) 118 (28) 42 (10) 126 (30) 37 (9) 2 (7) 11 (39) 4 (14) 11 (39) 0 3 (<1) 19 (5) 8 (2) 0 1 (4) 1 (4) 29 Not for publication or presentation Variable Post-tx cy FK506 + MMF +- others FK506 + MTX +- others FK506 + others FK506 alone CSA + MMF +- others CSA + MTX +- others CSA + others CSA alone Other GVHD prophylaxis Missing Year of HCT 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Median follow-up of survivors (range), months Attachment 5 CR2 1 (<1) 28 (7) 138 (33) 18 (4) 11 (3) 66 (16) 99 (24) 13 (3) 12 (3) 4 (<1) 1 (<1) >=CR3 0 7 (25) 10 (36) 0 1 (4) 5 (18) 2 (7) 0 1 (4) 0 0 21 (5) 24 (6) 24 (6) 30 (7) 39 (9) 32 (8) 24 (6) 31 (7) 51 (12) 58 (14) 36 (9) 20 (5) 31 (7) 61 (3-168) 0 0 1 (4) 3 (11) 5 (18) 2 (7) 0 1 (4) 2 (7) 2 (7) 7 (25) 2 (7) 3 (11) 46 (3-98) Hailin comments: 468 cases selected for allo HCT in >=CR2 with CBF 10 cases selected for auto HCT in >=CR2 with CBF (36 if including all disease status) Selection: st nd 1 allo HCT for CBF AML in 2 or subsequent CR between 2000 and 2012 after CAP modeling Excluding syngeneic twin donor Complete research form Patient consent 30 Not for publication or presentation Attachment 6 Study Proposal 1411-20 Study Title: Effect of in vivo T cell depletion on transplant outcomes in CMV seropositive and seronegative recipients with acute myeloid leukemia Mohamed Shanavas, MD, FRACP, FRCPA, Princess Margaret Cancer Centre, University of Toronto, ON Canada, Mohamed.shanavas@uhn.ca Dennis Kim MD, PhD, Princess Margaret Cancer Centre, University of Toronto, ON Canada, dr.dennis.kim@uhn.ca Hypothesis: There is likely an interaction (effect modification) between T-Cell depletion (TCD) and recipient CMV serostatus in allogeneic hematopoietic cell transplantation (allo-HCT). In vivo TCD may result in higher relapse rate and inferior overall survival in CMV seropositive but not in CMV seronegative recipients undergoing allo-HCT for acute myeloid leukemia (AML). Specific Aim: To assess the effect of in vivo TCD on transplant outcomes in AML by stratified analysis based on CMV serostatus of recipients. Exploratory Aims: To explore whether this effect of T cell depletion varies between alemtuzumab and ATG To explore the effect of donor CMV serostatus on these outcomes To explore the effect of CMV reactivation in these outcomes Outcomes of interest are: Cumulative Incidence of Relapse (CIR) Non-relapse mortality (NRM) Overall survival (OS) Leukemia-free survival (LFS) Acute Graft versus host disease (acute GVHD) Chronic Graft versus host disease (chronic GVHD) Scientific Justification: A number of studies have reported an association between CMV reactivation / seropositivity and reduced relapse risk after allogeneic HCT for acute myeloid leukemia.1-3 However, this finding was not reproduced in cohorts with significant proportion of T cell depleted transplants.4, 5 This may suggest an interaction between the effects CMV and T cell depletion in this setting. In a single institution retrospective study we have observed that in CMV seropositive recipients low relapse rate was seen only in non-TCD transplants; whereas CMV seropositive recipients undergoing TCD with in vivo alemtuzumab actually had a paradoxically increased relapse rate (unpublished data, manuscript under review, and in available on request).6 In the same study we also observed that TCD did not result in increased relapse risk in CMV seronegative recipients. The above findings can be explained by opposing actions of CMV on tumor immunity. On one hand, CMV reactivation has an immune stimulating effect by facilitating maturation of NK and T cells;7-9 on the 31 Not for publication or presentation Attachment 6 other hand, latent CMV infection has an immunosuppressive effect by increasing the concentrations of TGF-β and cellular IL-10 in the tumor microenvironment.10 It is possible that the net effect of this complex interaction may favor antileukimic effect in the presence of competent immune effectors; whereas in T/NK cell depleted patients the overall effect may be reversed towards the direction of decreased tumor immunity. This finding raises a potential safety concern with in vivo T-cell depletion in CMV seropositive patients. However, this needs to be confirmed in a larger database. Similarly it needs to be seen whether this is specific for alemtuzumab or not? The effect of CMV reactivation and donor CMV status also need to be explored if sample size is sufficiently large for stratified analysis. The large size of the CIBMTR registry should provide an opportunity to explore these in a well-powered study. Patient Eligibility Population: Inclusion criteria (should meet all the criteria): Diagnosis of AML First allogeneic HCT Year of HCT between 2000 and 2011 Age 18 years and older at the time of HCT Transplant in complete remission or leukemia free status Transplant from matched related or 10/10 unrelated donor Peripheral blood or bone marrow graft Exclusion criteria: Syngeneic transplants Cord-blood transplants Haplo-identical transplants Transplant with partially matched donors Transplant for leukemia not in remission Ex vivo T cell depletion or manipulation Post transplant DLI prior to relapse Post transplant tumor vaccination Prior history of CLL (possibility of prior alemtuzumab) Prior history of treatment for aplastic anemia (possibility of ATG) Data Requirement: CIBMTR Data Collection forms needed: Recipient baseline Data; Form 2000 Infectious Disease Markers; Form 2004 AML pre-HCT data; Form 2010 100 day post HCT data; Form 2100 6 months – 2 year post HCT data; Form 2200 Yearly follow up for greater than 2 years Data; Form 2300 Pre-transplant Essential Data; Form 2400 Post transplant Essential Data; Form 2450 Recipient Death Data; Form 2900 Other data requirements: Supplemental data requirement: None 32 Not for publication or presentation Attachment 6 Non –CIBMTR data used: None Study Design: Variables to be analyzed: Patient related: Age at HCT Gender Karnofsky Performance Score: <90 vs. >90 (if available) Donor related Gender CMV serostatus Donor type: Matched related vs. matched unrelated Disease related: Type of AML: Denovo AML vs. secondary AML vs. therapy related AML Cytogenetics: good risk vs. intermediate vs. poor risk vs. not available (defined according to SWOG/ECOG definition11) Status at HCT: CR1 vs. CR2 Transplant related: Year of transplant: 2000-2005 vs. 2006-2011 Conditioning regimen MAC vs. RIC vs. NMA (as defined by CIBMTR12) TBI vs. No TBI with dose of TBI if available Type of in vivo T cell depletion: ATG vs. Alemtuzumab vs. none Type of ATG if available: horse vs. rabbit Total dose of alemtuzumab if available GVHD prophylaxis: Calcineurin inhibitor (CNI) + MTX vs. CNI + MMF vs. others Source of stem cells: Bone marrow vs. Peripheral blood Outcome variables: Time from HCT to death Time from HCT to relapse Onset of acute GVHD Maximum grade of acute GVHD Onset of chronic GVHD Maximum grade of chronic GVHD (if available) Type of chronic GVHD (extensive vs. limited) CMV reactivation Onset Treatment Biological Sample Requirements: None Effect of T Cell depletion on Transplant outcomes will be analyzed separately for CMV seropositive and seronegative recipients. Kaplan Meir method and log rank test will be used for time to event endpoints without competing risks, and cumulative incidence method and Gray’s tests for time to event endpoints with competing risks. 33 Not for publication or presentation Attachment 6 Test for interaction between T cell depleted status and recipient CMV serostatus will be performed in the multivariable analysis of relapse. If interaction is confirmed, further analysis of risk factors for relapse, NRM, OS, LFS, acute GVHD, and chronic GVHD will be performed by stratified multivariable analysis (stratified by recipient CMV serostatus) Graft versus host disease will be used as a time dependent covariable in multivariable analysis if information about the time of onset in available in sufficient proportion of patients. Further plan will be developed depending on sample size after discussion with statistical team at CIBMTR. References: 1. Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM, et al. CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood 2013; 122: 1316-1324. 2. Manjappa S, Bhamidipati PK, Stokerl-Goldstein KE, DiPersio JF, Uy GL, Westervelt P, et al. Protective effect of cytomegalovirus reactivation on relapse after allogeneic hematopoietic cell transplantation in acute myeloid leukemia patients is influenced by conditioning regimen. Biol Blood Marrow Transplant 2014; 20: 46-52. 3. Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M, et al. Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood 2011; 118: 1402-1412. 4. Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J, et al. CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood 2013; 122: 33593364. 5. Ljungman P, Brand R, Einsele H, Frassoni F, Niederwieser D, Cordonnier C. Donor CMV serologic status and outcome of CMV-seropositive recipients after unrelated donor stem cell transplantation: an EBMT megafile analysis. Blood 2003; 102: 4255-4260. 6. Shanavas M, Uhm J, Alam N, Gupta V, Kuruvilla J, Lipton H. Protective Effect Of CMV In Myeloid Malignancies Undergoing HCT Is Altered In The Presence Of Alemtuzumab; Evidence For Effect Modification. Unpublished article, Manuscript under review 7. Scheper W, van Dorp S, Kersting S, Pietersma F, Lindemans C, Hol S, et al. γδT cells elicited by CMV reactivation after allo-SCT cross-recognize CMV and leukemia. Leukemia 2013; 27: 1328-1338. 8. Gumá M, Budt M, Sáez A, Brckalo T, Hengel H, Angulo A, et al. Expansion of CD94/NKG2C+ NK cells in response to human cytomegalovirus-infected fibroblasts. Blood 2006; 107: 3624-3631. 9. Chiesa MD, Falco M, Bertaina A, Muccio L, Alicata C, Frassoni F, et al. Human Cytomegalovirus Infection Promotes Rapid Maturation of NK Cells Expressing Activating Killer Ig–like Receptor in Patients Transplanted with NKG2C−/− Umbilical Cord Blood. The Journal of Immunology 2014; 192: 1471-1479. 10. Mason GM, Poole E, Sissons JGP, Wills MR, Sinclair JH. Human cytomegalovirus latency alters the cellular secretome, inducing cluster of differentiation (CD)4+ T-cell migration and suppression of effector function. Proceedings of the National Academy of Sciences 2012; 109: 14538-14543. 11. Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 2000; 96: 4075-4083. 12. Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 2009; 15: 1628-1633. 34 Not for publication or presentation Attachment 6 35 Not for publication or presentation Attachment 6 The plots on the right hand side show increased relapse and inferior OS in CMV with TCD in CMV seropositive recipients. This effect was not seen in CMV seronegative recipients. Characteristics of Study Population Variable Number of patients Number of centers Age in decades Median (range) 18-29 30-39 40-49 50-59 60-69 >=70 Gender Male Female Karnofsky score <90% >=90% Missing White blood count at diagnosis Median (range) <= 10 10 - 100 > 100 Missing Type of AML De-novo Transformed from MDS/MPS Therapy linked Cytogenetics scoring Normal Favorable Intermediate Poor Missing Disease status prior to HCT CR1 CR2 Conditioning regimen intensity Myeloablative RIC NMA TBD Missing TCD CMV- TCD CMV+ 335 611 96 121 noTCD CMV- noTCD CMV+ 1102 1954 150 184 52 (18-74) 50 (15) 41 (12) 55 (16) 107 (32) 76 (23) 6 (2) 54 (18-78) 61 (10) 60 (10) 122 (20) 202 (33) 152 (25) 14 (2) 47 (18-74) 190 (17) 171 (16) 287 (26) 333 (30) 112 (10) 9 (<1) 47 (18-75) 303 (16) 328 (17) 515 (26) 552 (28) 234 (12) 22 (1) 196 (59) 139 (41) 317 (52) 294 (48) 631 (57) 471 (43) 957 (49) 997 (51) 87 (26) 232 (69) 16 (5) 169 (28) 405 (66) 37 (6) 288 (26) 756 (69) 58 (5) 512 (26) 1353 (69) 89 (5) 7 (<1-322) 169 (50) 107 (32) 13 (4) 46 (14) 7 (<1-1300) 306 (50) 185 (30) 47 (8) 73 (12) 9 (<1-1048) 508 (46) 391 (35) 79 (7) 124 (11) 10 (<1-999) 850 (44) 689 (35) 175 (9) 240 (12) 249 (74) 18 (5) 68 (20) 462 (76) 40 (7) 109 (18) 887 (80) 71 (6) 144 (13) 1566 (80) 99 (5) 289 (15) 78 (23) 26 (8) 80 (24) 69 (21) 82 (24) 173 (28) 42 (7) 134 (22) 124 (20) 138 (23) 316 (29) 91 (8) 232 (21) 250 (23) 213 (19) 634 (32) 183 (9) 427 (22) 378 (19) 332 (17) 243 (73) 92 (27) 469 (77) 142 (23) 829 (75) 273 (25) 1410 (72) 544 (28) 175 (52) 135 (40) 19 (6) 4 (1) 2 (<1) 288 (47) 273 (45) 27 (4) 23 (4) 0 887 (80) 144 (13) 58 (5) 13 (1) 0 1496 (77) 307 (16) 118 (6) 33 (2) 0 36 Not for publication or presentation Variable TBI No Yes ATG/Campath ATG + CAMPATH ATG alone CAMPATH alone No ATG or CAMPATH GVHD prophylaxis Post-tx cy FK506 + MMF +- others FK506 + MTX +- others FK506 + others FK506 alone CSA + MMF +- others CSA + MTX +- others CSA + others CSA alone Other GVHD prophylaxis Graft type Bone marrow Peripheral blood Type of donor HLA-identical sibling Well-matched unrelated Donor/Recipient CMV match -/-/+ +/+/+ Donor/Recipient sex match M/M M/F F/M F/F Year of HCT 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 Attachment 6 TCD CMV- TCD CMV+ noTCD CMV- noTCD CMV+ 278 (83) 57 (17) 538 (88) 73 (12) 600 (54) 502 (46) 1172 (60) 782 (40) 0 302 (90) 33 (10) 0 1 (<1) 532 (87) 78 (13) 0 0 0 0 1102 0 0 0 1954 1 (<1) 50 (15) 137 (41) 6 (2) 15 (4) 31 (9) 64 (19) 13 (4) 12 (4) 6 (2) 1 (<1) 81 (13) 243 (40) 17 (3) 42 (7) 63 (10) 107 (18) 16 (3) 33 (5) 8 (1) 11 (<1) 143 (13) 457 (41) 48 (4) 16 (1) 75 (7) 313 (28) 11 (<1) 22 (2) 6 (<1) 7 (<1) 204 (10) 724 (37) 82 (4) 32 (2) 165 (8) 640 (33) 16 (<1) 71 (4) 13 (<1) 59 (18) 276 (82) 117 (19) 494 (81) 220 (20) 882 (80) 406 (21) 1548 (79) 74 (22) 261 (78) 188 (31) 423 (69) 564 (51) 538 (49) 1207 (62) 747 (38) 238 (71) 0 97 (29) 0 0 322 (53) 0 289 (47) 768 (70) 0 334 (30) 0 0 828 (42) 0 1126 (58) 135 (40) 89 (27) 61 (18) 50 (15) 217 (36) 181 (30) 100 (16) 113 (18) 422 (38) 277 (25) 209 (19) 194 (18) 610 (31) 584 (30) 347 (18) 413 (21) 12 (4) 11 (3) 19 (6) 24 (7) 29 (9) 30 (9) 39 (12) 37 (11) 52 (16) 40 (12) 22 (7) 20 (3) 24 (4) 37 (6) 43 (7) 48 (8) 84 (14) 73 (12) 64 (10) 73 (12) 63 (10) 49 (8) 59 (5) 60 (5) 54 (5) 54 (5) 99 (9) 137 (12) 114 (10) 114 (10) 129 (12) 130 (12) 119 (11) 99 (5) 108 (6) 152 (8) 141 (7) 226 (12) 219 (11) 201 (10) 163 (8) 194 (10) 214 (11) 176 (9) 37 Not for publication or presentation Variable 2011 Median follow-up of survivors (range), months Attachment 6 TCD CMV- TCD CMV+ 20 (6) 33 (5) 70 (3-169) 70 (2-172) noTCD CMV- noTCD CMV+ 33 (3) 61 (3) 70 (1-171) 68 (1-168) Selection: st 1 allo HCT for adult AML in CR1/CR2 between 2000 and 2011 after CAP modeling HLA-identical sibling or well-matched unrelated donor excluding ex-vivo TCD excluding prior history of CLL or aplastic anemia complete research form patient consent 38 Not for publication or presentation Attachment 7 Study Proposal 1411-49/1311-34 Study Title: Impact of GVHD on outcome after allogeneic hematopoietic cell transplantation for acute lymphocytic leukemia: a retrospective registry study Moshe Yeshurun, MD, BMT unit, Institute of hematology, Rabin Medical Center, Petach-Tikva, Israel, moshe.yeshurun@gmail.com Jacob M. Rowe, MD, Department of hematology, Shaare Zedek Medical Center, Jerusalem, Israel, rowe@rambam.health.gov.il Martin S. Tallman, MD, Leukemia Service, Memorial Sloan-Kettering Cancer Center, New York, N.Y., USA, TallmanM@mskcc.org Veronika Bachanova, MD, PhD, Division of Hematology, Oncology and Transplantation, University of Hypothesis: The graft-versus-leukemia (GVL) effect and the graft-versus-host disease (GVHD) are closely associated. However, the strength of this association has been shown to differ significantly between different hematological malignancies. The increased non-relapse mortality (NRM) associated with GVHD, particularly in its severe forms, may potentially outweigh the favorable GVL effect on disease relapse. Nevertheless, there are no sound data on the net impact of acute and chronic GVHD on survival of patients with acute lymphocytic leukemia (ALL) after allogeneic hematopoietic cell transplantation (alloHCT). Specific Aims: 1. Identify any differential GVHD-associated GVL influences after alloHCT for ALL, using either myeloablative or reduced intensity conditioning regimens. 2. Study the impact of acute and chronic GVHD and its extent on relapse, NRM, DFS and OS rates after alloHCT for ALL. Scientific Justification: The GVL effect following alloHCT is the single most potent antileukemic strategy for adult patients with ALL as reflected by a significantly reduced relapse rate post alloHCT compared to relapse rates with standard chemotherapy or after autologous stem cell transplantation (1). While the GVL effect may occur in the absence of clinical GVHD (2), there are ample of data suggesting that acute and chronic GVHD are associated with an augmented GVL effect (3). Nevertheless, GVHD affecting more than 50% of transplanted patients, remains a major cause of morbidity and mortality after allogeneic transplantation. Hence, the increased non-relapse mortality (NRM) associated with GVHD, particularly in its severe forms, may potentially offset the favorable GVL effect on disease relapse, thus resulting in a non-favorable net impact on survival. Indeed, in a recent retrospective analysis on behalf the CIBMTR, GVHD did not prove to have a beneficial impact on the overall survival (OS) of AML patients in the myeloablative conditioning (MAC) setting (4). In fact, acute GVHD emerged as an adverse prognostic factor on OS. Lacking any protective effect against relapse, acute GVHD had a detrimental effect on NRM, which translated into inferior survival of patients with acute GVHD compared to patients without any GVHD (HR 1.71, p<0.0001). As for chronic GVHD, despite its favorable protective effect against relapse (HR 0.68, p< 0.0001), this influence was offset by increased NRM (HR 2.24, p< 0.0001) and consequently by comparable OS. In the RIC setting, 39 Not for publication or presentation Attachment 7 acute GVHD had actually a protective effect against relapse (HR 0.63, P<0.0001); nevertheless, it was offset by increased NRM (HR 3.66, p<0.0001), thus resulting in comparable OS rates in patients with acute GVHD and in patients without any GVHD. However, the chronic GVHD-associated protective effect against relapse (HR 0.53, p<0.0001) was only partially offset by increased NRM (HR 2.1, P<0.0001), which translated into superior survival of patients with chronic GVHD compared to patients without any GVHD (0.74, p=0.007) after RIC alloHCT. These results are in contrast to a recent report of the Seattle group arguing that even after RIC alloHCT any potential benefit associated with chronic GVHD is outweighed by increased NRM and thus does not translate into a better survival (5). In a recent EBMT megafile analysis, the strength of the GVHD / GVL association has been shown to differ significantly between hematological malignancies (6). AML appeared relatively insensitive to development of acute GVHD and limited chronic GVHD; nevertheless, relevant reductions in relapse risk have been reported in patients experiencing extensive chronic GVHD. ALL however proved to be highly sensitive to acute and chronic GVHD, comparably to CML. The higher sensitivity of ALL to GVHD compared to AML had previously been shown by Weiden et al (7). Also, patients with ALL and AML may differ in their vulnerability to GVHD, which may translate into different NRM rates. Accordingly, the net impact of acute and chronic GVHD on survival may differ between patients with AML and ALL. Furthermore, the net impact of GVHD on OS of ALL patients may vary after MAC and RIC alloHCT. Thus, the objective of the current retrospective study is to assess the impact of the different variants of GVHD (i.e. acute or chronic, limited or extensive) on transplant outcomes of ALL patients after alloHCT. Patient Eligibility Population: Inclusion criteria: 1. Patients with ALL 16 years or older 2. Any disease status at transplantation 3. Transplanted between the years 1993 and 2012 4. MAC or RIC preparative regimens (8) 5. First transplantation only 6. Peripheral blood, bone marrow and cord blood grafts Exclusion criteria: 1. Ex-vivo T cell depleted grafts 2. Haploidentical transplants 3. Patients who failed to engraft or who died before engraftment 4. Patients who received pre-emptive DLI Outcomes: Acute and chronic GVHD: Occurrence of grade II, III, and/or IV skin, gastrointestinal or liver abnormalities fulfilling the Consensus criteria of acute GVHD, and limited and extensive chronic GVHD. Non-relapse mortality: death without relapse or progression, where relapse or progression are competing risks. Those who survive without recurrence or progression are censored at the time of last contact. Relapse/progression: progressive disease or recurrence of disease are counted as events. Treatment related death, defined as death without relapse or progression, is the competing event. Those who survive without recurrence or progression are censored at the time of last contact. 40 Not for publication or presentation Attachment 7 Progression-free survival (PFS): survival without recurrence or tumor progression. Recurrence of progression of disease and death are counted as events. Those who survive without recurrence or progression are censored at the time of last contact. Overall survival: time to death. Death from any cause will be considered an event. Surviving patients will be censored at the time of last follow-up. Data Requirements: None Sample Requirements: None Variables to be analyzed: Time dependent acute (Grade II-IV) and chronic GVHD (limited and extensive) Patient-related: Age at transplant (decades) Gender: male vs. female Karnofsky performance status transplant: <90% vs. ≥90% Co-morbidity index 0-2 vs. ≥3 Disease-related: B vs. T cell origin Cytogenetics: t(9:22) vs. other high risk (hypoploidity, t(4:11)) vs. intermediate risk WBCx109/L: <30 vs. >30 for B-ALL , <100 vs. >100 for T-ALL Extramedullary disease at diagnosis: CNS (yes/no), other (yes/no) Time to achieve CR1: <4 weeks vs. 4-8 weeks vs. >8 weeks Disease status at transplantation: CR1 vs. CR2 vs. CR≥3 vs. no remission Transplant-related: Time from diagnosis to transplant Time from remission to transplant Conditioning regimen intensity: MAC vs. RIC/NMA TBI based vs. non TBI based conditioning Type of donor: HLA-identical sibling vs. other related vs. well-matched unrelated (8/8) vs. partially matched unrelated (7/8) vs. mismatched unrelated donor (7/8>) vs. cord blood Donor-recipient gender match: F-M vs. all other donor-recipient gender combinations. Donor age : continuous, median (range) Donor-recipient CMV status: -/- vs. others Source of stem cells: BM vs. PBSC vs. UCB Year of transplant: by decades GVHD prophylaxis: CSA-based vs Tacro-based vs. other In-vivo T cell depletion (ATG, Campath) yes vs. no Study Design: This is a retrospective registry study on behalf of the CIBMTR. Patients will be stratified according to conditioning regimen intensity (MAC vs. RIC). Variables related to patients, disease, and transplantation will be compared using the chi-square test for categorical variables and the Mann-Whitney test for continuous variables. Patients will be divided into 4 groups: 41 Not for publication or presentation Attachment 7 (1) those without any GVHD, (2) those with acute GVHD only, (3) those with chronic GVHD only, (4) those with acute GVHD and chronic GVHD. We will consider only GVHD which occurred before relapse. Time to onset of GVHD will be determined as time to onset to acute GVHD or chronic GVHD, whichever came first. Acute and chronic GVHD will be treated as time dependent covariates. To examine the influence of acute GVHD and chronic GVHD on NRM, relapse, DFS and OS, separate analyses will be conducted for recipients of MAC and RIC regimens. Cox regression models will be built to adjust for effects of other patient, disease, and treatment variables. The results of multivariate analysis will be expressed as hazard ratio with the 95% confidence interval. The probabilities of NRM and relapse will be calculated using cumulative incidence. Data on patients without an event will be censored at last follow-up. Probability of DFS and OS will be calculated with the Kaplan-Meier estimator. We will also perform a landmark analysis for relapse and OS for all patients who survived at least 30 days and 1 year disease-free after their transplantation. References: 1. Glodstone AH, Richards SM, Lazarus HM, et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the international ALL trial (MRC UKALL XII/ECOG E2993). Blood. 2008; 111: 18271833. 2. Horowitz MM, Gale RP, Sondel PM, et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood. 1990; 555-562. 3. Passweg JR, Tiberghien P, Cahn JY, et al. Graft-versus-leukemia effects in T lineage and B lineage acute lymphoblastic leukemia. Bone Marrow Transplant. 1998; 21: 153-158. 4. Weisdorf D, Zhang MJ, Arora M, et al. Graft-versus-host disease induced graft-versus-leukemia effect: greater impact on relapse and disease-free survival after reduced intensity conditioning. Biol Blood Marrow Transpl. 2012; 18: 1727-1733. 5. Storb R, Gyurkocza B, Storer BE, et al. Graft-versus-tumor effects after allogeneic hematapoietic cell transplantation. J Clin Oncol. 2013; 31: 1530-1538. 6. Stern M, de Wreede LC, Brand R, et al. Sensitivity of hematological malignancies to graft-versushost effects: an EBMT megafile analysis. Leukemia. 2014; 28: 2235-2240. 7. Weiden PL, Flournoy N, Thomas ED, et al. Antileukemic effects of graft versus host disease in human recipients of allogeneic marrow grafts. N Engl J Med. 1979; 300: 1068-1070. 8. Bacigalupo A, Ballen K, Rizzo D, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009; 15: 1628-1633. 42 Not for publication or presentation Attachment 7 Characteristics of Study Population Variable Number of patients Number of centers Age in decades Median (range) 18-29 30-39 40-49 50-59 60-69 >=70 Gender Male Female Karnofsky score <90% >=90% Missing White blood count at diagnosis Median (range) <= 10 10 - 100 > 100 Missing HCT-CI 0 1 2 3+ N/A, earlier than 2007 Missing Philadelphia positive No Yes FAB classification T-cell B-cell Unspecified Extramedullary disease at diagnosis N (%) 3334 256 33 (16-72) 1433 (43) 710 (21) 633 (19) 441 (13) 116 (3) 1 (<1) 2005 (60) 1329 (40) 959 (29) 2218 (67) 157 (5) 13 (<1-2000) 1188 (36) 1032 (31) 405 (12) 709 (21) 513 (15) 125 (4) 79 (2) 165 (5) 2444 (73) 8 (<1) 2665 (80) 669 (20) 513 (15) 1996 (60) 825 (25) 43 Not for publication or presentation Variable No Yes Missing EMD at CNS at diagnosis No Yes Missing EMD at other site at diagnosis No Yes Missing Disease status prior to HCT Primary induction failure CR1 CR2 >=CR3 Relapse Time from diagnosis to HCT Median (range) <6 months 6 - 12 months >12 months Conditioning regimen intensity Myeloablative RIC NMA TBD Missing TBI No Yes Graft type Bone marrow Peripheral blood Umbilical cord blood Type of donor HLA-identical sibling Well-matched unrelated Partially matched unrelated Mismatched unrelated Attachment 7 N (%) 2784 (84) 435 (13) 115 (3) 2996 (90) 223 (7) 115 (3) 2976 (89) 243 (7) 115 (3) 147 (4) 1699 (51) 861 (26) 175 (5) 452 (14) 8 (<1-279) 1198 (36) 912 (27) 1224 (37) 2947 (88) 265 (8) 41 (1) 40 (1) 41 (1) 690 (21) 2644 (79) 965 (29) 1966 (59) 403 (12) 1092 (33) 1027 (31) 484 (15) 145 (4) 44 Not for publication or presentation Variable Unrelated TBD Cord blood Donor/Recipient sex match M/M M/F F/M F/F TBD Donor/Recipient CMV match -/-/+ +/+/+ TBD GVHD prophylaxis No GVHD prophylaxis Post-tx cy FK506 + MMF +- others FK506 + MTX +- others FK506 + others FK506 alone CSA + MMF +- others CSA + MTX +- others CSA + others CSA alone Other GVHD prophylaxis Missing In-vivo TCD No Yes Missing GVHD occurance AGVHD + cGVHD before relapse AGVHD before relapse CGVHD before relapse No GVHD before relapse GVHD occured but time unknown Year of HCT 2000 2001 Attachment 7 N (%) 183 (5) 403 (12) 1282 (38) 757 (23) 713 (21) 565 (17) 17 (<1) 774 (23) 832 (25) 365 (11) 1091 (33) 272 (8) 42 (1) 9 (<1) 346 (10) 1070 (32) 149 (4) 54 (2) 307 (9) 1120 (34) 114 (3) 80 (2) 26 (<1) 17 (<1) 2423 (73) 712 (21) 199 (6) 613 (18) 690 (21) 680 (20) 1255 (38) 96 (3) 232 (7) 274 (8) 45 Not for publication or presentation Variable 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Median follow-up of survivors (range), months Attachment 7 N (%) 301 (9) 266 (8) 338 (10) 369 (11) 367 (11) 297 (9) 298 (9) 210 (6) 132 (4) 139 (4) 111 (3) 70 (1-173) Selection Criteria: st 1 HCT for ALL between 2000 and 2012 after CAP modeling Age >=16 Excluding identical twin or haploidentical donor Excluding post-HCT pre-emptive DLI Excluding engraftment failure cases Complete research form Patient consent 46 Not for publication or presentation Attachment 8 Study Proposal 1411-69 Study Title: Comparison of outcomes of older adolescents and young adults with Philadelphia-chromosome/BCRABL1-negative acute lymphoblastic leukemia receiving post-remission consolidation chemotherapy with pediatric-inspired chemotherapy on CALGB 10403 or myeloablative allogeneic hematopoietic cell transplantation Matthew Joseph Wieduwilt, MD, PhD, UC San Diego Moores Cancer Center, CA, mwieduwilt@ucsd.edu Wendy Stock, MD, PhD, University of Chicago, IL, wstock@medicine.bsd.uchicago.edu Hypothesis: Post-remission consolidation with pediatric-inspired chemotherapy as administered on CALGB 10403 improves overall survival, leukemia-free survival, relapse, and non-relapse mortality compared with myeloablative allogeneic hematopoietic cell transplantation (HCT) in adult Philadelphiachromosome/BCR-ABL1 negative acute lymphoblastic leukemia patients aged 16-39 years. Specific Aims: 1. Compare overall survival between older adolescent and young adults aged 16-39 years with Ph/BCRABL1 negative acute lymphoblastic leukemia in first complete remission receiving consolidation therapy with pediatric-inspired chemotherapy or myeloablative allogeneic hematopoietic cell transplantation 2. Compare relapse-free survival in the same populations 3. Compare non-relapse mortality in the same populations 4. Compare CNS relapse rate in the same populations 5. Determine patient and disease factors influencing outcomes of consolidation with pediatric-inspired chemotherapy versus allogeneic hematopoietic cell transplantation Scientific Justification: The optimal post-remission treatment strategy for younger patients with Philadelphia-chromosome negative acute lymphoblastic leukemia in first complete remission has not been well established, especially in the era of pediatric-inspired chemotherapy regimens consisting of more intensive consolidation than administered in traditional adult protocols. Previous studies comparing allogeneic HCT to chemotherapy suggested superiority of consolidation with allogeneic HCT to chemotherapy including autologous HCT. MRC UK ALL XII/E2993 compared an adult chemotherapy backbone or autologous HCT to myeloablative allogeneic HCT in Ph-negative ALL patients aged 15-59 years. An overall survival benefit was seen in standard-risk ALL patients with a donor primarily due to higher rate of relapse in the no donor group that combined chemotherapy with autologous HCT1. However, studies comparing only allogeneic HCT to chemotherapy alone without inclusion of autologous transplant have shown no clear benefit of transplant2. A metanalysis of 13 trials comparing allogeneic HCT to chemotherapy with or without autologous HCT concluded that the benefit of allogeneic HCT in first CR Ph-negative ALL was limited to patients under the age of 352, within the same age group that is currently being recommended for treatment with pediatric-inspired chemotherapy by the NCCN and other groups. The application of pediatric-inspired chemotherapy with its more intensive consolidation appears to have improved outcomes for older adolescents and young adults with Ph-negative ALL. A meta-analysis of 11 clinical trials showed superior all-cause mortality, event-free survival, and relapse rates in 47 Not for publication or presentation Attachment 8 adolescents and younger adults, principally under the age of 25 years, treated with pediatric-inspired chemotherapy relative to conventional adult chemotherapy3. Whether this benefit will be seen in Phnegative ALL patients older than 20-21 years remains to be seen, but current NCCN guidelines recommend the use of a pediatric-inspired regimen based on retrospective data and results of singlearm phase II trials. The DFCI Adult ALL Consortium recently reported the results of 74 Ph-negative ALL aged 18-50 treated with pediatric-inspired chemotherapy4. A 4-year EFS of 62% was observed in Ph- ALL similar to outcomes with the GRAALL-2003 regimen. The small numbers of Ph- ALL patients treated on this study and the participation of only 13 centers in the northeastern US and Canada limits interpretation and generalizability of this study, however. A recent national, large, single-arm, prospective Intergroup study led by the Alliance for Clinical Trials in Oncology (Study CALGB 10403) studied the safety, tolerability, and efficacy of applying the COG AALL 0232 Standard-risk arm regimen to older adolescents and young adults aged 16-39 years with Philadelphia-chromosome negative ALL5. The study opened in November 2007 and completed enrollment with 318 patients in August 2012. The 2-year EFS rate is 66% with a 2-year OS rate of 78%. Age > 20 years and initial WBC count >30,000/microliter were significantly associated with inferior EFS and OS. The study now has a median of 30 months follow-up. Given the large size of the study and its representative sampling of patients from all areas of the US, it serves as an excellent study to compare outcomes of pediatric-inspired post-remission therapy to myeloablative allogeneic HCT. A major limitation of individual allogeneic HCT trials as well as meta-analyses is that the comparator chemotherapy regimens are of relatively low intensity in consolidation compared with modern pediatric-inspired chemotherapy regimens. Pediatric-inspired post-remission chemotherapy may improve relapse rates conceivably leading to superior survival with chemotherapy relative to allogeneic HCT with lower non-relapse mortality and lower morbidity. This study is designed to compare overall survival, leukemia-free survival, relapse, and non-relapse mortality in Ph-negative ALL patients aged 1639 years undergoing post-remission therapy with pediatric-inspired chemotherapy on CALGB 10403 versus myeloablative allogeneic HCT. Results from this study could further inform the ongoing debate on the role of allogeneic HCT for Ph-negative ALL in first remission. Patient Eligibility Population: Patients age 16-39 with a diagnosis of Philadelphia-chromosome/BCR-ABL1 negative acute lymphoblastic leukemia undergoing post-remission chemotherapy on CALGB C10403 or allogeneic hematopoietic cell transplantation in CR1 from 11/1/2007 through 8/31/2012 (enrollment period of CALGB C10403) and 11/1/2002-10/31/2007. Excluded are Philadelphia-chromosome/BCR-ABL1 positive ALL, ALL with t(8;14)/Burkitt leukemia (FAB L3), biphenotypic leukemia, and patients with Down syndrome. Data Requirements: Variables to be described: Chemotherapy and transplant populations Patient-related: Number of patients Number of centers Age, years: continuous/range Age, years: 16-19, 20-29, 30-39, ≤35, >35 years Gender: male, female Race: non-Hispanic white vs. Hispanic white vs. Black 48 Not for publication or presentation Attachment 8 Body mass: Obese vs. non-obese Karnofsky performance score: < 90, ≥90 Disease-related: Lineage: T-lineage vs. B-lineage ALL WBC at diagnosis, B-lineage ALL (x109/L): continuous and <30, ≥30 WBC at diagnosis, T-lineage ALL (x109/L): continuous and <100, ≥100 Cytogenetics risk group at diagnosis: Poor (hypodiploid (<44 chromosomes), MLL rearranged, complex (>4 abnormalities) vs. other Extramedullary disease at diagnosis: yes vs. no CNS disease at diagnosis: yes vs no Testicular disease at diagnosis: yes vs. no Time to documentation of CR1: ≤4 weeks, >4-8 weeks, >8 weeks Cycles of chemotherapy prior to transplantation: 1,2,3, >3 Transplant population Transplant-related: Graft source: peripheral blood , bone marrow Conditioning regimen intensity: myeloablative, reduced intensity, NMA Conditioning regimen GVHD prophylaxis: FK506 + MTX +- others vs. CSA + MTX +- others vs. ex vivo T-cell depletion vs. others Type of donor: Matched related donor, well-matched unrelated donor, partially matched unrelated donor, mismatched unrelated donor, unrelated donor match unknown, mismatched related donor Donor age: continuous Sex match: M-M, M-F, F-M, F-F D/R CMV status: +/+, +/-, -/+, -/ Years of transplant: 11/1/2007-8/31/2012 or 11/1/2002-10/31/2007 Median follow up: months Duration of CR1: <6 months, 6-12 months, >12 months, not available Variables to be analyzed: Main effect: Post-remission therapy: post-remission chemotherapy on CALGB 10403 vs. myeloablative allogeneic HCT in CIBMTR Patient-related: Age, years: 16-19, 20-29, 30-39 Age, years: ≤35, >35 years Karnofsky performance score (%): < 90 vs. 90-100 Gender: Male vs. female Body mass: Obese vs. non-obese Race: non-Hispanic white vs. Hispanic white vs. Black Disease-related: Lineage: T-lineage vs. B-lineage ALL WBC at diagnosis, B-lineage ALL (x109/L): continuous and <30, ≥30 WBC at diagnosis, T-lineage ALL (x109/L): continuous and <100, ≥100 49 Not for publication or presentation Attachment 8 Cytogenetics risk group at diagnosis: Poor (hypodiploid (<44 chromosomes), MLL rearranged, complex (>4 abnormalities) vs. other Extramedullary disease at diagnosis: yes vs. no CNS disease at diagnosis: yes vs no Testicular disease at diagnosis: yes vs. no Time to documentation of CR1: ≤4 weeks, >4-8 weeks, >8 weeks Cycles of chemotherapy prior to transplantation: 1,2,3, >3 Transplant-related: Donor type: Matched related donor, vs. matched unrelated donor vs. mismatched unrelated donor Conditioning regimen intensity: myeloablative, reduced intensity, NMA Conditioning regimen: TBI-based vs. no In vivo T-cell depletion with ATG, Campath: yes vs no Graft source: Peripheral blood vs. bone marrow Years of transplant: 11/1/2007-8/31/2012 or 11/1/2002-10/31/2007 GVHD prophylaxis: FK506 + MTX +- others vs. CSA + MTX +- others vs. ex vivo T-cell depletion vs. others Sex match: F-M vs other D/R CMV status: -/- vs. other Outcomes and definitions: Overall survival (OS): Time from documentation of CR1 to death from any cause. Surviving patients censored at last time reported alive. Leukemia-free survival (LFS): Time from documentation of CR1 to leukemia relapse or death from any cause. Surviving patients censored at last time reported alive and leukemia-free. Relapse: Relapse after documentation of CR1 is the event. Death in remission is the competing risk. Non-relapse mortality (NRM): Death in the first 28 days post-transplant or death in continuous remission. Relapse is the competing risk. Study Design: Patient, disease and treatment-related factors will be compared between pre-conditioning cytogenetically normal and abnormal patients using Chi-square test for categorical and Mann-Whitney test for continuous variables. Probabilities of overall survival and leukemia-free survival will be calculated using the Kaplan-Meier estimator. Log-rank testing will be used to compare survival curves. Cumulative incidence curves will be made to present relapse and non-relapse mortality with time to relapse and time to NRM as competing risks. Differences between curves in setting of competing risks will be tested using the Gray method6. Prognostic factors for OS, LFS, relapse, and NRM will be analyzed using the proportional hazards model with the competing-risk regression model7. Further development of design pending assessment of feasibility. References: 1. Goldstone AH, Richards SM, Lazarus HM, et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional 50 Not for publication or presentation 2. 3. 4. 5. 6. 7. Attachment 8 consolidation/maintenance chemotherapy in all patients: final results of the International ALL Trial (MRC UKALL XII/ECOG E2993).Blood. 2008 Feb 15;111(4):1827-33. Gupta V, Richards S, and Rowe J. Allogeneic, but not autologous, hematopoietic cell transplantation improves survival only among younger adults with acute lymphoblastic leukemia in first remission: an individual patient data meta-analysis. Blood. 2013 Jan 10;121(2):339-50. Ram, R, Wolach, O, Vidal, L, et al. Adolescents and young adults with acute lymphoblastic leukemia have a better outcome when treated with pediatric-inspired regimens: systematic review and metaanalysis. Am J Hematol. 2012 May;87(5):472-8. DeAngelo, DJ, Stevenson, KE, Dahlberg, SE, et al.Long-term outcome of a pediatric-inspired regimen used for adults aged 18-50 years with newly diagnosed acute lymphoblastic leukemia. Leukemia. 2014 Jul 31. doi: 10.1038/leu.2014.229. [Epub ahead of print]. Stock, W, Luger, SM, Advani, AS, et al. Favorable Outcomes for Older Adolescents and Young Adults (AYA) with Acute Lymphoblastic Leukemia (ALL): Early Results of U.S. Intergroup Trial C10403. 56th ASH Annual Meeting and Exposition, Abstract 796, 2014. Gray R. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1140-1154 (1988). Fine J, Gray R. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496-509 (1999). 51 Not for publication or presentation Attachment 8 Characteristics of Study Population Variable N (%) Number of patients 470 Number of centers 134 Age in decades Median (range) 26 (16-40) 16-19 105 (22) 20-29 203 (43) 20-39 162 (34) Male 318 (68) Female 152 (32) Gender Recipient race Caucasian 386 (82) African-American 18 (4) Asian 43 (9) Pacific islander 2 (<1) Native American 1 (<1) Other Unknown 9 (2) 11 (2) Obese No 367 (78) Yes 96 (20) Missing 7 (1) Karnofsky score <90% 87 (19) >=90% 358 (76) Missing 25 (5) White blood count at diagnosis Median (range) 15 (<1-1410) <= 10 167 (36) 10 - 100 155 (33) > 100 70 (15) Missing 78 (17) FAB classification T-cell 109 (23) 52 Not for publication or presentation Variable Attachment 8 N (%) B-cell 229 (49) Unspecified 132 (28) Cytogenetics scoring Normal 155 (33) Poor 69 (15) Other 62 (13) TBD (needs review) Not tested Missing 101 (21) 21 (4) 62 (13) Extramedullary disease at diagnosis No 372 (79) Yes 72 (15) Missing 26 (6) EMD at CNS at diagnosis No 417 (89) Yes 27 (6) Missing 26 (6) EMD at other site at diagnosis No 396 (84) Yes 48 (10) Missing 26 (6) Time to achieve CR1 Median (range) 7 (<1-113) <=4 weeks 69 (15) 4-8 weeks 184 (39) >8 weeks 184 (39) Missing 33 (7) Time from CR1 to HCT Median (range) 3 (<1-35) <6 months 363 (77) 6-12 months 65 (14) >12 months 10 (2) Missing 32 (7) Total cycles of induction for CR1 cases 1 42 (9) 2 25 (5) 53 Not for publication or presentation Variable Attachment 8 N (%) 3 14 (3) 4 22 (5) N/A, earlier than 2007 Missing 277 (59) 90 (19) Conditioning regimen intensity Myeloablative 450 (96) RIC 11 (2) NMA 1 (<1) TBD 1 (<1) Missing 7 (1) Graft type Bone marrow 166 (35) Peripheral blood 304 (65) Type of donor HLA-identical sibling 227 (48) Well-matched unrelated 135 (29) Partially matched unrelated 63 (13) Mismatched unrelated 12 (3) Unrelated TBD 33 (7) Donor/Recipient sex match M/M 210 (45) M/F 85 (18) F/M 107 (23) F/F 67 (14) TBD 1 (<1) Donor/Recipient CMV match -/- 125 (27) -/+ 92 (20) +/- 63 (13) +/+ 180 (38) TBD 10 (2) GVHD prophylaxis No GVHD prophylaxis 6 (1) Ex-vivo T-cell depletion 8 (2) CD34 selection 9 (2) FK506 + MMF +- others 28 (6) 54 Not for publication or presentation Variable FK506 + MTX +- others FK506 + others FK506 alone CSA + MMF +- others CSA + MTX +- others CSA + others Attachment 8 N (%) 148 (31) 20 (4) 6 (1) 10 (2) 211 (45) 6 (1) CSA alone 13 (3) Other GVHD prophylaxis 4 (<1) Missing 1 (<1) Year of HCT 2003 71 (15) 2004 63 (13) 2005 74 (16) 2006 69 (15) 2007 54 (11) 2008 43 (9) 2009 35 (7) 2010 14 (3) 2011 24 (5) 2012 23 (5) Median follow-up of survivors (range), months 61 (2-122) Selection: st 1 allo HCT for Ph- ALL in CR1 between 2003 and 2012 after CAP modeling Age 16-40 years old HLA-identical sibling or unrelated donor Bone marrow or peripheral blood graft Complete research form Patient consent 55 Not for publication or presentation Attachment 9 Study Proposal 1411-71 Study Title: Prognostic risk factors of patients undergoing allogeneic stem cell transplantation for acute erythroleukemia Jan Cerny , MD, PhD, FACP, University of Massachusetts Medical Center, MA, jan.cerny@umassmemorial.org Rajneesh Nath, MD, University of Massachusetts Medical Center, MA, rajneesh.nath@umassmemorial.org Zheng (Frank) Zhou, MD, PhD, University of Massachusetts Medical Center, MA, zheng.zhou@umassmemorial.org Hypothesis: Treatment with allogeneic transplant improves survival of patients with AEL. Karyotype is the strongest prognostic factor for overall survival (OS) and cumulative incidence of relapse (RFS) of transplanted patients. Specific Aims: To evaluate: 1. OS 2. relapse free survival (RFS) 3. Nonrelapse mortality (NRM) 4. rates of aGVHD and cGVHD Of patients with AEL undergoing allogeneic transplantation and how are they effected by: - cytogenetics - transplant conditioning (intensity- ablative vs nonabalative) - pretranslant treatment (chemotherapy vs hypomethylating agents) - disease status or response at transplant - other clinical characteristics (age at SCT, sex, CMV, level of matching, ABO compatibility, donor type) We expect to see that younger patients (<60) and patients with high risk cytogenetics will receive induction chemotherapy and will be more likely to receive myeloablative conditioning. On the contrary, older patients (>=60) and patients with normal cytogenetics will be more likely to be treated with nonmyeloablative approaches and more likely to receive hypomethylating agent as induction therapy. Scientific Justification: Acute erythroleukemia (AEL) is a rare subtype of AML with a poor prognosis. Allogeneic stem cell transplant (alloSCT) improves the outcomes of AEL, 1,2 however only a small percentage of patients are typically able to receive alloSCT and studies prior to 2008 WHO reclassification included patients with >30%.1 Cytogenetics is a known prognostic factor for survival while single gene mutations are rather rare.1 What is not known are other clinical characteristics that impact postransplant outcome such as intensity of transplant conditioning, best GVHD prophylaxis and risk of CMV reactivation. Pretransplant therapy impacts outcome with 7+3 being used as induction chemotherapy. AEL patients achieved high rates of responses (~60%) with hypomethylating agent treatment alone.3 In our experience (data submitted for Tandem meeting 2015) patients who were able to undergo an alloSCT had a superior OS of 33 months 56 Not for publication or presentation Attachment 9 compared to 7 months without transplant (p=0.036).2 Patients with high risk karyotype received induction chemotherapy while patients with normal karyotype responded to hypomethylating agent. Patient Eligibility Population: All patients who have undergone an allogeneic stem cell transplant for AEL (previously AML M6) between January 2000 and December 2013. Data Requirements: - Age - Gender - Cytogenetics risk category - Molecular genetics (where available) - Type of induction (chemo vs hypomethylating agent) - Best response and its duration - Karnofsky - HSCT-comorbidity index - Disease Status at SCT - Time from diagnosis to SCT - Bone marrow blast percentage - Stem cell source (BM, PBSC, Cord blood) - Donor age - Donor-Recipient Sex Match - Donor recipient CMV status - Conditioning regimen used - Documented organ toxicity - GVHD prophylaxis regimen - T cell antibody use - Date of SCT - Time to Neutrophil engraftment time - Time to Platelet engraftment time - Immune recovery (objective measures, including CD4 counts recovery, …) - Mixed chimerism at 30 days, 6 months and 1 year - Post-transplant infection (bacteria, fungal and/or viral) - Acute GVHD, organ involved and grade - Chronic GVHD, organ involved and grade - Relapse-free survival at different time points (day 100, 1 year, 3 and 5 years) - Overall survival at different time points (day 100, 1 year, 3 and 5 years) Sample Requirements: N/A Study Design: Retrospective analysis of adult AEL patients in the CIBMTR database, who underwent allogeneic stem cell transplantation Study endpoints: Primary endpoints: - Overall survival (OS) at Day +100, 1 year and 3 years 57 Not for publication or presentation Attachment 9 Secondary endpoints: - Time to engraftment (neutrophil, platelet and immunorecovery) - NRM at Day +100, 1 year and 3 years - RFS at Day+100, 1 year and 3 years - Incidence and severity of GVHD (acute and chronic) - Mixed Chimerism (%) at day 30, 6 months and 1 year Outcomes: NRM is defined as death during continuous disease remission after transplant; Relapse is defined as clinical or hematological recurrence; RFS are clinical or hematological relapses or deaths from any cause; OS is death from any cause Surviving patients will be censored at the time of last clinic follow-up or the date of last contact, whichever is later Methods of analysis: Comparison will be made for myeloablative vs nonmyeloablative conditioning regimens with respect to the study endpoints listed above. Survival Analysis Multivariate Cox proportional hazard regression will be used with adjustment for patient baseline clinical and disease characteristics to determine significance of difference in outcomes related to the condition regimens and pretransplant therapy intensity (chemo vs hypomethylating agents). Hazard ratio with 95% confidence interval (CI) will be obtained. Cumulative incidence and Competing risk Rates of relapse, NRM, success in engraftment (neutrophil, platelet and CD4) and GVHD (acute and chronic) will be estimated using cumulative incidence approach. In the analysis of the cumulative incidence of engraftments, early mortality will be considered as competing risk; In the analysis of GVHD, relapse and mortality will be considered a competing risk. Kaplan-Meier Curves OS, NRM and RFS will be compared with stratification by condition regimens and pretransplant therapy intensity (chemo vs hypomethylating agents) using Kaplan-Meier curves. References: 1. 2. 3. Hasserjian RP, Zuo Z, Garcia C, Tang G, Kasyan A, Luthra R, Abruzzo LV, Kantarjian HM, Medeiros LJ, Wang SA. Acute erythroid leukemia: a reassessment using criteria refined in the 2008 WHO classification. Blood. 2010 Mar 11;115(10):1985-92. Kodali S, Tipirneni E, Zhou Z, Ramanathan M, Nath R, Cerny J. Allogeneic stem cell transplant improves the outcome of patients with acute erythroleukemia: single center analysis. (submitted for Tandem Meeting 2015) Vigil C, Cortes J, Kantarjian HM, Garcia-Manero G, Lancet JE, List AF. Hypomethylating therapy for the treatment of acute erythroleukemia patients. Program and abstracts of the 51st American Society of Hematology Annual Meeting and Exposition; December 5-8, 2009; New Orleans, Louisiana. Abstract 2069. 58 Not for publication or presentation Attachment 9 Characteristics of Study Population Variable N (%) Number of patients 379 Number of centers 139 Age in decades Median (range) 49 (<1-73) <10 26 (7) 10-19 23 (6) 20-29 32 (8) 30-39 41 (11) 40-49 75 (20) 50-59 105 (28) 60-69 73 (19) >=70 4 (1) Male 232 (61) Female 147 (39) Gender Karnofsky score <90% 127 (34) >=90% 234 (62) Missing 18 (5) White blood count at diagnosis Median (range) <= 10 3 (<1-333) 300 (79) 10 - 100 33 (9) > 100 3 (<1) Missing 43 (11) 0 61 (16) 1 18 (5) 2 19 (5) 3+ 24 (6) HCT-CI N/A, earlier than 2007 Missing 253 (67) 4 (1) Disease status prior to HCT 59 Not for publication or presentation Variable Primary induction failure Attachment 9 N (%) 60 (16) CR1 216 (57) CR2 35 (9) >=CR3 1 (<1) Relapse 67 (18) Cytogenetics scoring Normal Favorable Intermediate Poor TBD (needs review) Not tested Missing 93 (25) 1 (<1) 58 (15) 136 (36) 18 (5) 7 (2) 66 (17) Time from diagnosis to HCT Median (range) <6 months 5 (1-115) 222 (59) 6 - 12 months 98 (26) >12 months 59 (16) Conditioning regimen intensity Myeloablative RIC 252 (66) 94 (25) NMA 17 (4) TBD 14 (4) Missing 2 (<1) Graft type Bone marrow Peripheral blood Umbilical cord blood 83 (22) 253 (67) 43 (11) Type of donor HLA-identical sibling Other related Well-matched unrelated Partially matched unrelated 117 (31) 18 (5) 129 (34) 47 (12) Mismatched unrelated 12 (3) Unrelated TBD 13 (3) Cord blood 43 (11) 60 Not for publication or presentation Variable Attachment 9 N (%) Donor/Recipient CMV match -/- 81 (21) -/+ 107 (28) +/- 43 (11) +/+ 120 (32) TBD 28 (7) Donor/Recipient sex match M/M 151 (40) M/F 90 (24) F/M 81 (21) F/F 56 (15) TBD 1 (<1) GVHD prophylaxis No GVHD prophylaxis 4 (1) Ex-vivo T-cell depletion 9 (2) CD34 selection 15 (4) Post-tx cy 2 (<1) FK506 + MMF +- others 54 (14) FK506 + MTX +- others 111 (29) FK506 + others 11 (3) FK506 alone 12 (3) CSA + MMF +- others 32 (8) CSA + MTX +- others 82 (22) CSA + others 18 (5) CSA alone 22 (6) Other GVHD prophylaxis Missing 5 (1) 2 (<1) Year of HCT 2000 19 (5) 2001 33 (9) 2002 27 (7) 2003 30 (8) 2004 34 (9) 2005 32 (8) 2006 40 (11) 2007 38 (10) 61 Not for publication or presentation Variable Attachment 9 N (%) 2008 41 (11) 2009 39 (10) 2010 20 (5) 2011 18 (5) 2012 8 (2) Median follow-up of survivors (range), months 64 (3-144) Selection: st 1 allo HCT for AEL between 2000 and 2012 after CAP modeling Excluding syngeneic twin donor Complete research form Patient consent 62 Not for publication or presentation Attachment 10 Study Proposal 1411-74 Study Title: Comparison of outcomes post allogeneic hematopoietic cell transplant between patients with de novo and secondary acute myeloid leukemia in first complete remission. Fotios Vasilios Michelis, MD, PhD, Allogeneic Blood and Marrow Transplant Program, Princess Margaret Cancer Centre, Toronto, Canada, Fotios.Michelis@uhn.ca Hans A. Messner, MD, PhD, Allogeneic Blood and Marrow Transplant Program, Princess Margaret Cancer Centre, Toronto, Canada, Hans.Messner@uhn.ca Specific Aim: To compare the outcomes of patients with de novo AML and AML secondary to a previous malignancy (hematological and solid tumor) undergoing allogeneic hematopoietic cell transplantation (HCT) in first complete remission (CR1). Outcomes of interest: a. Overall survival (OS) b. Leukemia-free survival (LFS) c. Cumulative Incidence of Relapse (CIR) d. Non-relapse mortality (NRM) Scientific Justification: The development of AML may occur de novo or subsequent to a previous diagnosis of solid tumors, hematopoietic malignancies or myelodysplasia.1-4 The occurrence of AML following a previous malignancy may be the consequence of cytoreductive therapy for the primary disease, and thus can be considered treatment related (tAML). However, AML may also develop without cytotoxic management as for instance reported for cases where primary solid tumors were treated with surgery alone3,5, reflecting different mechanisms (non-tAML) such as genetic instability that already may have been associated with the development of the primary malignancy. The concept of progression to AML in the absence of cytotoxic measures is well accepted for myelodysplastic syndrome (MDS) and other hematopoietic malignancies. Past studies have often merged patients of both categories (secondary tAML and secondary non-tAML), characterizing them all as secondary AML (sAML).5-8 Treated conservatively, a worse prognosis was commonly reported for patients with sAML compared to de novo AML.4,9-14 It remains debated whether or not the decreased rate of survival reflects biological differences in the disease process, differences in the frequency of well recognized high risk factors such as unfavorable karyotype, or differences in management. In contrast to de novo AML, the role of allogeneic hematopoietic cell transplantation (HCT) as part of the management of sAML is not well established and the effect on the above described subtypes of sAML (secondary tAML and secondary non-tAML) is relatively unknown. In our own experience at Princess Margaret Cancer Centre, we recently submitted a retrospective analysis comparing the outcomes of 180 patients with de novo and 84 patients with sAML post allogeneic HCT in first complete remission (CR1)(manuscript revision re-submitted to Bone Marrow Transplantation on October 29, 2014, available on request).15 The study showed that the outcomes for both AML subtypes post HCT are comparable, as was demonstrated in univariate (Appendix 1), multivariable and propensity score matched analysis (Appendix 2). Also, a separate subgroup analysis was performed for sAML patients with primary solid tumors, primary MDS and other primary hematopoietic malignancies that 63 Not for publication or presentation Attachment 10 have emerged with or without exposure to cytotoxic therapies, and this also demonstrated no significant difference between these subgroups. One of the limitations of our single-centre study was the relatively small number of patients involved. Large-scale studies to investigate the role of allo-HCT in sAML are not available, and information in the literature is largely derived from subset analyses. For this reason we would like to use a larger database to compare outcomes between de novo and sAML post-HCT. The large size of the CIBMTR registry provides an opportunity to investigate these subgroups in a well powered study. The data from this study will provide useful information as below: a. Verification of the results from our previously published study demonstrating the comparable outcomes between de novo and sAML undergoing HCT in CR1. This is significant because it would stress the need for patients with sAML, who are considered high-risk for relapse, to undergo HCT in CR1 (provided a suitable donor is available), and thus improve the referral of these patients to transplant centers. b. Comparison of outcomes post-HCT for subtypes of sAML such as those arising from previously treated solid tumors, previously treated hematological malignancies and hematological malignancies progressing to sAML without previous cytotoxic treatment. Our previously published work demonstrated comparable outcomes. c. Patient counseling concerning the risks and benefits of allogeneic HCT in sAML d. Design of future clinical trials comparing allogeneic and non-allogeneic treatment options for sAML. Patient Eligibility Population: Using the CIBMTR database, patients with AML who underwent HCT between 1999 and 2013 and meet the following criteria will be identified. Eligible patients: Inclusion criteria (should meet all the criteria): Age 18 years and older at the time of HCT First allogeneic transplant Diagnosis of AML, either de novo or sAML (subdivided into therapy-related and secondary to previous haematological malignancy) Patients undergoing HCT in CR1 Transplant from either a matched related donor or unrelated donor (9/10 or 10/10) Exclusion criteria: Syngeneic transplants In vitro T cell depletion Cord-blood transplants Haplo-identical transplants Acute promyelocytic leukemia Previous allogeneic transplant Variables to be analyzed: Patient-related: Age at HCT Gender 64 Not for publication or presentation Attachment 10 Karnofsky Performance scores: <90 vs ≥90 Hematopoietic cell transplant-comorbidity index16(HCT-CI)(depending on availability of data) Disease-related: Type of AML: de-novo versus therapy related versus secondary AML with previous diagnosis of MDS/MPD Previous autologous transplant (yes/no) Cytogenetics: good risk vs. intermediate vs. poor risk vs. unknown/not available (defined according to SWOG/ECOG definition17) Time from diagnosis of AML to transplant Number of courses of chemotherapy to CR1 Transplant related: Conditioning regimen: MAC vs. RIC vs. NMA as defined by CIBMTR18 TBI in conditioning regimen: no TBI versus TBI with dose in cGY included Donor age Donor type: MSD vs. 9/10 MUD vs 10/10 MUD Donor-recipient gender: M-M vs. M-F vs. F-M vs. F-F CMV status of donor and recipient: +/+ vs. +/- vs. -/+ vs. -/ ABO incompatibility: none vs. minor vs. major vs. bidirectional Source of hematopoietic cells: BM vs. PBSC Median CD34 cell dose, x 106/kg Date of transplant GVHD prophylaxis: Calcineurin inhibitor (CNI) + MTX vs. CNI + MMF vs. others Received Serotherapy with either campath or ATG: yes/no Outcomes of interest: Hematopoietic recovery (neutrophil and platelet recovery) Acute GVHD Chronic GVHD Cumulative incidence of Relapse Cumulative incidence of NRM LFS OS Statistical analysis: This is a retrospective study of CIBMTR data between 1999 and 2013. The purpose of the proposed study is to compare the outcomes of patients undergoing allo-HCT for de novo AML vs sAML in CR1. Moreover, post-HCT outcomes would be investigated for subgroups of sAML, such as therapy related versus secondary AML with previous diagnosis of MDS/MPD. Patient, disease and transplant related variables will be compared between the groups using chi-square test for categorical variables and Mann-Whitney test for continuous variables. Statistical endpoints will be calculated using Kaplan-Meier Method and will be compared using log-rank test for overall survival, while non-relapse mortality (NRM), cumulative incidence of relapse (CIR) and GVHD incidence will be calculated using the cumulative incidence method considering competing risks and will be compared using Gray method. Multivariate analysis will also be performed using Cox’s proportional hazard model for overall survival, and using Fine-Gray method for NRM, CIR and GVHD incidence. All variables with a p-value <0.1 in the univariate analysis will be considered for entry into multivariate analysis, in which all 65 Not for publication or presentation Attachment 10 p-values will be tested as two-sided and p-value <0.05 will be used as statistically significant. A propensity score matched analysis may also be performed,19-20 which would involve the generation of matched pairs of patients between the de novo and sAML groups, and the subsequent comparison of the matched subgroups. Further plan will be developed depending on sample size after discussion with statistical team at CIBMTR. References: 1. Leone G, Mele L, Pulsoni A, Equitani F, Pagano L. The incidence of secondary leukemias. Haematologica 1999; 84: 937-945. 2. Witherspoon RP, Deeg HJ. Allogeneic bone marrow transplantation for secondary leukemia or myelodysplasia. Haematologica 1999; 84: 1085-1087. 3. Pagana L, Pulsoni A, Tosti ME, Avvisati G, Mele L, Mele M, et al. Clinical and biological features of acute myeloid leukaemia occurring as second malignancy: GIMEMA archive of adult acute leukaemia. Br J Haematol 2001; 112: 109-117. 4. Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 2009; 114: 937-951. 5. Abdelhameed A, Pond GR, Mitsakakis N, Brandwein J, Chun K, Gupta V, et al. Outcome of patients who develop acute leukemia or myelodysplasia as a second malignancy after solid tumors treated surgically or with strategies that include chemotherapy and/or radiation. Cancer 2008; 112: 15131521. 6. Anderson JE, Gooley TA, Schoch G, Anasetti C, Bensinger WI, Clift RA, et al. Stem cell transplantation for secondary acute myeloid leukemia: evaluation of transplantation as initial therapy or following induction chemotherapy. Blood 1997; 89: 2578-2585. 7. Ostgård LS, Kjeldsen E, Holm MS, Brown Pde N, Pedersen BB, Bendix K, et al. Reasons for treating secondary AML as de novo AML. Eur J Haematol 2010; 85: 217-226. 8. Preiss BS, Bergmann OJ, Friis LS, Sørensen AG, Frederiksen M, Gadeberg OV, et al. Cytogenetic findings in adult secondary acute myeloid leukemia (AML): frequency of favorable and adverse chromosomal aberrations do not differ from adult de novo AML. Cancer Genet Cytogenet 2010; 202: 108-122. 9. Dann EJ, Rowe JM. Biology and therapy of secondary leukaemias. Best Pract Res Clin Haematol 2001; 14: 119-137. 10. Josting A, Wiedenmann S, Franklin J, May M, Sieber M, Wolf J, et al. Secondary myeloid leukemia and myelodysplastic syndromes in patients treated for Hodgkin's disease: a report from the German Hodgkin's Lymphoma Study Group. J Clin Oncol 2003; 21: 3440-3446. 11. Kayser S, Döhner K, Krauter J, Köhne CH, Horst HA, Held G, et al. The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood 2011; 117: 2137-2145. 12. Della Porta MG. Prognosis of secondary acute myeloid leukemia. Leuk Res 2013; 37: 857-858. 13. Park SH, Chi HS, Cho YU, Jang S, Park CJ. Evaluation of prognostic factors in patients with therapyrelated acute myeloid leukemia. Blood Res 2013; 48: 185-192. 14. Ornstein MC, Mukherjee S, Mohan S, Elson P, Tiu RV, Saunthararajah Y, et al. Predictive Factors for Latency Period and a Prognostic Model for Survival in Patients with Therapy-related AML. Am J Hematol 2014; 89: 168-173. 15. Michelis FV, Atenafu EG, Gupta V, Kim DD, Kuruvilla John, Lipton JH, Loach D, Seftel MD, Uhm J, Alam N, Lambie A, McGillis L, Messner HA. Comparable outcomes post allogeneic hematopoietic cell transplant for patients with de novo and secondary acute myeloid leukemia in first remission. Revision re-submitted to Bone Marrow Transplant, October 29, 2014. 66 Not for publication or presentation Attachment 10 16. Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912–2919. 17. Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, Paietta E, Willman CL, Head DR, Rowe JM, Forman SJ, Appelbaum FR. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075-4083 18. Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, Apperley J, Slavin S, Pasquini M, Sandmaier BM, Barrett J, Blaise D, Lowski R, Horowitz M. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628-1633 19. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998; 17: 2265-2281. 20. Liem YS, Wong JB, Hunink MM, de Charro FT, Winkelmayer WC. Propensity scores in the presence of effect modification: A case study using the comparison of mortality on hemodialysis versus peritoneal dialysis. Emerg Themes Epidemiol 2010; 7: 1. Appendix 1: Appendix 1. Univariate comparison of OS for patients with de novo (n=180) and sAML (n=84) after allogeneic HCT (p=0.18). 67 Not for publication or presentation Attachment 10 Appendix 2: Appendix 2. Univariate comparison between de novo and sAML following propensity score matched analysis (62 pairs) A) for OS, p=0.54, B) for LFS, p=0.40. 68 Not for publication or presentation Attachment 10 Characteristics of Study Population Variable De-novo AML sAML Number of patients 2880 1050 Number of centers 211 159 47 (18-75) 55 (18-76) 18-29 493 (17) 83 (8) 30-39 473 (16) 66 (6) 40-49 737 (26) 228 (22) 50-59 799 (28) 382 (36) 60-69 346 (12) 265 (25) >=70 32 (1) 26 (2) Male 1519 (53) 534 (51) Female 1361 (47) 516 (49) <90% 718 (25) 337 (32) >=90% 2050 (71) 648 (62) 112 (4) 65 (6) Median (range) 9 (<1-999) 4 (<1-700) <= 10 1310 (45) 663 (63) 996 (35) 255 (24) 264 (9) 26 (2) 310 (11) 106 (10) 2880 0 Transformed from MDS/MPS 0 775 (74) Therapy linked 0 275 (26) No 2865 (99) 1029 (98) Yes 15 (<1) 21 (2) 0 573 (20) 173 (16) 1 138 (5) 38 (4) 2 110 (4) 43 (4) Age in decades Median (range) Gender Karnofsky score Missing White blood count at diagnosis 10 - 100 > 100 Missing Type of AML De-novo Prior auto HCT HCT-CI 69 Not for publication or presentation Variable Attachment 10 De-novo AML sAML 230 (8) 132 (13) 1822 (63) 662 (63) 7 (<1) 2 (<1) 922 (32) 243 (23) 101 (4) 27 (3) Intermediate 694 (24) 240 (23) Poor 654 (23) 311 (30) TBD (needs review) 8 (<1) 12 (1) Not tested 87 (3) 35 (3) 414 (14) 182 (17) 5 (<1-82) 5 (1-118) 0-3 months 272 (9) 166 (16) 3-6 months 1730 (60) 587 (56) 6-12 months 783 (27) 262 (25) 95 (3) 35 (3) 1 1111 (39) 356 (34) 2 524 (18) 116 (11) 3 71 (2) 23 (2) 4 24 (<1) 11 (1) 5 33 (1) 16 (2) 1117 (39) 528 (50) 2106 (73) 607 (58) 536 (19) 311 (30) NMA 139 (5) 91 (9) TBD 48 (2) 31 (3) Missing 51 (2) 10 (<1) No 1775 (62) 734 (70) Yes 1105 (38) 316 (30) HLA-identical sibling 1438 (50) 363 (35) Well-matched unrelated 1115 (39) 488 (46) 3+ N/A, earlier than 2007 Missing Cytogenetics scoring Normal Favorable Missing Time from diagnosis to HCT Median (range) >12 months Total cycles of induction for CR1 cases Missing Conditioning regimen intensity Myeloablative RIC TBI Type of donor 70 Not for publication or presentation Variable Attachment 10 De-novo AML sAML 327 (11) 199 (19) M/M 963 (33) 370 (35) M/F 818 (28) 308 (29) F/M 554 (19) 163 (16) F/F 540 (19) 207 (20) 5 (<1) 2 (<1) -/- 722 (25) 275 (26) -/+ 782 (27) 327 (31) +/- 302 (10) 112 (11) +/+ 988 (34) 305 (29) TBD 86 (3) 31 (3) 1444 (50) 481 (46) Minor mismatch 546 (19) 208 (20) Major mismatch 510 (18) 214 (20) Bidirectional mismatch 147 (5) 67 (6) Missing 233 (8) 80 (8) 611 (21) 181 (17) 2269 (79) 869 (83) No GVHD prophylaxis 30 (1) 10 (<1) Ex-vivo T-cell depletion 66 (2) 37 (4) CD34 selection 78 (3) 24 (2) 14 (<1) 6 (<1) FK506 + MMF +- others 310 (11) 148 (14) FK506 + MTX +- others 1062 (37) 413 (39) 107 (4) 36 (3) 70 (2) 23 (2) CSA + MMF +- others 188 (7) 121 (12) CSA + MTX +- others 787 (27) 173 (16) CSA + others 48 (2) 18 (2) CSA alone 89 (3) 30 (3) 23 (<1) 8 (<1) Partially matched unrelated Donor/Recipient sex match TBD Donor/Recipient CMV match Donor/recipient ABO match Matched Graft type Bone marrow Peripheral blood GVHD prophylaxis Post-tx cy FK506 + others FK506 alone Other GVHD prophylaxis 71 Not for publication or presentation Variable Attachment 10 De-novo AML sAML 8 (<1) 3 (<1) 2000 142 (5) 38 (4) 2001 155 (5) 46 (4) 2002 172 (6) 59 (6) 2003 165 (6) 74 (7) 2004 262 (9) 101 (10) 2005 332 (12) 108 (10) 2006 303 (11) 117 (11) 2007 291 (10) 119 (11) 2008 319 (11) 125 (12) 2009 298 (10) 113 (11) 2010 241 (8) 83 (8) 2011 95 (3) 42 (4) 2012 105 (4) 25 (2) 66 (2-172) 71 (3-171) Missing Year of HCT Median follow-up of survivors (range), months Selection: st 1 allo HCT for adult AML in CR1 between 2000 and 2012 after CAP modeling HLA-identical sibling or well/partially matched unrelated donor Excluding FAB M3 (APL) Complete research form Patient consent 72 Not for publication or presentation Attachment 11 Study Proposal 1411-77/1312-09 Study Title: Comparison of total body irradiation (TBI)-based with intravenous (i.v.) busulfan (Bu) containing chemotherapy-only myeloablative transplant conditioning regimens in adult patients with acute lymphoblastic leukemia (ALL) Partow Kebriaei, MD, MD Anderson Cancer Center, pkebriae@mdanderson.org Ibrahim Aldoss, MD, City of Hope Medical Center, ialdoss@coh.org Vinod Pullarkat, MD, City of Hope Medical Center, vpullarkat@coh.org Claudio Anasetti, MD, Moffitt Cancer Center, Claudio.Anasetti@moffitt.org David Marks, MD, University Hospitals Bristol Foundation Trust, David.Marks@UHBristol.nhs.uk Collaborators: Joseph Alvarnas, MD, City of Hope Medical Center, jalvarnas@coh.org Stephen Forman, MD, City of Hope Medical Center, sforman@coh.org Hypothesis: We hypothesise that i.v. Bu containing regimens will achieve similar survival to TBI based regimens in patients with ALL Specific Aims: Aim 1: To compare post-hematopoietic cell transplantation (HCT) outcomes [overall survival (OS), leukemia-free survival (LFS), relapse rate (RR) and non-relapse mortality (NRM)] between TBI- and nonTBI-, i.v. Bu-based myeloablative conditioning regimens in adults with ALL undergoing allogeneic HCT. Aim 2: To evaluate the influence of the conditioning regimen (TBI versus i.v. Bu) on post HCT outcomes among ALL risk subgroups (standard versus high) classified based on age, initial WBC and cytogenetics at diagnosis in adults with ALL undergoing allogeneic HCT. This aim will also address the effect of remission status (CR1 versus CR2) on the outcomes after TBI based versus Bu-based conditioning. Aim 3: To evaluate the impact on extramedullary relapse patterns, specifically central nervous system relapse, with the two different conditioning approaches. Aim 4: To evaluate the regimen related toxicity profile, and to compare graft versus host disease, of the two different conditioning approaches. Scientific Justification: Patient Eligibility Population: Inclusion criteria: Age 18-65 Patients with diagnosis of B or T-cell acute lymphoblastic leukemia (ALL) in CR1 or CR2 Patients who have undergone full-intensity conditioning regimen Definition of full-intensity regimen include: TBI: non-fractionated dose ≥ 5.5 Gy, fractionated ≥ 9 Gy Busulfan dose of ≥ 9 mg/kg First allogeneic HCT from an HLA-identical sibling or matched unrelated donor HCT beginning in 2000 and beyond 73 Not for publication or presentation Attachment 11 Exclusion criteria: Recipients of reduced-intensity conditioning (R) or nonmyeloablative conditioning (NMA) regimens Patients with active leukemia at the time HCT Umbilical Cord Blood or haploidentical HCT HCT from ≤ 7/8 unrelated donor Syngeneic donor HCT Ex vivo T-cell deplete Scientific Justification: TBI-based transplant conditioning regimens are considered the standard of care for patients undergoing HCT for ALL, with expected survival of 50% to 60% in first complete remission (CR1)(1, 2). However, TBI is associated with acute and long-term toxicity (including secondary malignancy), with non-relapse mortality (NRM) rates of 20%-45% following SCT (2-4). In efforts to minimize toxicity, the combination of oral Bu and cyclophosphamide (Cy) was developed. But a retrospective (5) and prospective analysis (6) in children comparing Cy-TBI with Bu-Cy demonstrated that although relapse rates were equivalent in the two groups, TRM was actually increased in the Bu-Cy group with greater rates of veno-occlusive disease and interstitial pneumonitis, and thus survival was better with Cy-TBI. Since these studies, the intravenous formulation of Bu has been developed and increasingly used, and study results across disease types show a better safety profile (7, 8) (ref). Furthermore, PK- directed dosing of intravenous Bu affords even greater safety (9, 10) (Ansari EBMT 2012) and efficacy (Andersson ASH 2011). Interestingly, a recent CIBMTR multicenter cohort analysis in patients with acute myeloid leukemia (AML) receiving HCT following Cy-TBI or myeloablative, intravenous Bu-based conditioning regimens found superior survival for the Bu-based group (56% vs. 48%, p=.02) (11). Several phase II studies have reported excellent transplant outcomes with intravenous Bu combined with fludarabine (12, 13) and clofarabine(14) in patients receiving SCT for ALL. An updated analysis of MD Anderson data with Bu and clofarabine SCT conditioning for ALL patients in CR1 (n=44) and CR2 (n=21) revealed that 70% and 52%, respectively, of patients are alive and in remission with a median follow-up of 18 months. Thus, we would like to do a comparison of myeloablative TBI-based conditioning regimens versus intravenous Bu-based regimens in patients receiving allogeneic HCT for ALL. If we have sufficient numbers, we propose to evaluate the patients receiving i.v. Bu combined with a nucleoside analogue (Flu or Clo) separately from those receiving Bu combined with another alkylator, commonly cyclophosphamide, since the two approaches may not show similar results. We, and others, showed excellent disease control but increased toxicity in the form of interstitial pneumonia and hemorrhagic cystitis with the combination of Bu and the alkylator melphalan (15, 16). 74 Not for publication or presentation Attachment 11 Data Requirements: Data collection from standard CIBMTR forms. For i.v. Bu-based cases, data from MD Anderson and Moffitt Cancer Center, data readily available; both centers have published on these regimen results. MD Anderson (BuClo CR1 n=65, CR2 n=37; BuFlu CR1 n=6; BuMel CR1 n=28, CR2 n=15) Moffitt (BuFlu CR1 n=86, CR2 n=17) Sample Requirements: None Study Design: We propose a retrospective, case-controlled comparison of patients receiving radiation-based, myeloablative conditioning (TBI>5.5Gy in a single fraction or >9 Gy fractionated plus Cy >60 mg/kg or etoposide >30 mg/kg) compared with intravenous Bu >9 mg/kg plus cyclophosphamide, fludarabine or clofarabine for HCT in CR1 or CR2. Due to the relatively few cases of i.v. Bu-based regimens in the CIBMTR database, we will include data from the additional centers specified above. We plan to look at the i.v.-Bu or Clo cases separately from i.v. Bu combined with Cy if sufficient numbers exist. Primary outcomes: Overall survival, DFS, GVHD (acute and chronic), NRM at 2 years and relapse Study Variables: Patient-related: - Age (by decades, or as a continuous variable) - Gender (M vs F) - Karnofsky PS (<90% vs 90% or more) Disease-related: - Cytogenetic abnormalities: t(4;11), t(9;22), hypodiploidy or near triploidy, complex cytogenetics (>5 abnormalities) vs. diploid vs. other abnormalities vs. not known - Lineage (T vs. B vs. not known) - WBC at diagnosis <25, 25-100, 100-200, >200 - Time to achieve CR1: <4 weeks, >8 weeks, 4-8 weeks - Time from diagnosis to transplant for CR1 patients - Relapse on chemotherapy (yes/no) - Extramedullary disease at diagnosis: CNS (yes/no), testis (yes/no), other (yes/no) Transplant-related: - Time from remission to transplant (CR1 and CR2) - Duration of CR1 for CR2 transplants - Alemtuzamab vs ATG (dose to be collected) - GVHD prophylaxis for UD transplants: ex vivo T cell depletion vs. CsA+MTX vs. tacrolimus+MTX vs. post SCT cytoxan - Donor age for unrelated donors (continuous variable) - Gender match (F-M vs M-F vs M-M vs F-F) - CMV status: -/- vs +/- vs _/+ vs +/+ - Year of transplant 75 Not for publication or presentation - Attachment 11 Matching of unrelated donors: well matched vs. partly matched vs. mismatched (CIBMTR criteria) Post-transplant therapy: DLI (yes/no); chemotherapy (yes/no); intrathecal chemotherapy (yes/no) PBSC vs. BM Busulfan PK monitoring, yes/no Daily Busulfan dose <130 mg/2 vs. > 130 or AUC <5000 vs. > 5000 Busulfan + nucleoside analogue (Fludarabine or Clofarabine) vs. others Dose of TBI <13 Gy vs. >13 Gy Cytoxan vs.VP16 vs. others + TBI cell dose data References: 1. Marks DI, Forman SJ, Blume KG, Perez WS, Weisdorf DJ, Keating A, et al. A comparison of cyclophosphamide and total body irradiation with etoposide and total body irradiation as conditioning regimens for patients undergoing sibling allografting for acute lymphoblastic leukemia in first or second complete remission. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2006;12(4):438-53. Epub 2006/03/21. 2. Goldstone AH, Richards SM, Lazarus HM, Tallman MS, Buck G, Fielding AK, et al. In adults with standard-risk acute lymphoblastic leukemia, the greatest benefit is achieved from a matched sibling allogeneic transplantation in first complete remission, and an autologous transplantation is less effective than conventional consolidation/maintenance chemotherapy in all patients: final results of the International ALL Trial (MRC UKALL XII/ECOG E2993). Blood. 2008;111(4):1827-33. Epub 2007/12/01. 3. Sutton L, Kuentz M, Cordonnier C, Blaise D, Devergie A, Guyotat D, et al. Allogeneic bone marrow transplantation for adult acute lymphoblastic leukemia in first complete remission: factors predictive of transplant-related mortality and influence of total body irradiation modalities. Bone marrow transplantation. 1993;12(6):583-9. Epub 1993/12/01. 4. Oliansky DM, Camitta B, Gaynon P, Nieder ML, Parsons SK, Pulsipher MA, et al. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the treatment of pediatric acute lymphoblastic leukemia: update of the 2005 evidence-based review. ASBMT Position Statement. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2012;18(7):979-81. Epub 2012/04/12. 5. Davies SM, Ramsay NK, Klein JP, Weisdorf DJ, Bolwell B, Cahn JY, et al. Comparison of preparative regimens in transplants for children with acute lymphoblastic leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2000;18(2):340-7. Epub 2000/01/19. 6. Bunin N, Aplenc R, Kamani N, Shaw K, Cnaan A, Simms S. Randomized trial of busulfan vs total body irradiation containing conditioning regimens for children with acute lymphoblastic leukemia: a Pediatric Blood and Marrow Transplant Consortium study. Bone marrow transplantation. 2003;32(6):543-8. Epub 2003/09/04. 7. Kashyap A, Wingard J, Cagnoni P, Roy J, Tarantolo S, Hu W, et al. Intravenous versus oral busulfan as part of a busulfan/cyclophosphamide preparative regimen for allogeneic hematopoietic stem cell transplantation: decreased incidence of hepatic venoocclusive disease (HVOD), HVOD-related mortality, and overall 100-day 76 Not for publication or presentation Attachment 11 mortality. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2002;8(9):493-500. Epub 2002/10/11. 8. Russell JA, Tran HT, Quinlan D, Chaudhry A, Duggan P, Brown C, et al. Once-daily intravenous busulfan given with fludarabine as conditioning for allogeneic stem cell transplantation: study of pharmacokinetics and early clinical outcomes. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2002;8(9):468-76. Epub 2002/10/11. 9. Andersson BS, Thall PF, Madden T, Couriel D, Wang X, Tran HT, et al. Busulfan systemic exposure relative to regimen-related toxicity and acute graft-versus-host disease: defining a therapeutic window for i.v. BuCy2 in chronic myelogenous leukemia. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2002;8(9):477-85. Epub 2002/10/11. 10. Geddes M, Kangarloo SB, Naveed F, Quinlan D, Chaudhry MA, Stewart D, et al. High busulfan exposure is associated with worse outcomes in a daily i.v. busulfan and fludarabine allogeneic transplant regimen. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2008;14(2):220-8. Epub 2008/01/25. 11. Bredeson C, LeRademacher J, Kato K, Dipersio JF, Agura E, Devine SM, Appelbaum FR, Tomblyn MR, Laport GG, Zhu X, McCarthy PL, Ho VT, Cooke KR, Armstrong E, Smith A, Rizzo JD, Burkart JM, Pasquini MC. Prospective cohort study comparing intravenous busulfan to total body irradiation in hematopoietic cell transplantation. Blood. 2013 Dec 5;122(24):3871-8. doi: 10.1182/blood-2013-08-519009. Epub 2013 Sep 30. 12. Russell JA, Savoie ML, Balogh A, Turner AR, Larratt L, Chaudhry MA, et al. Allogeneic transplantation for adult acute leukemia in first and second remission with a novel regimen incorporating daily intravenous busulfan, fludarabine, 400 CGY total-body irradiation, and thymoglobulin. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2007;13(7):81421. Epub 2007/06/21. 13. Santarone S, Pidala J, Di Nicola M, Field T, Alsina M, Ayala E, et al. Fludarabine and pharmacokinetictargeted busulfan before allografting for adults with acute lymphoid leukemia. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2011;17(10):1505-11. Epub 2011/03/10. 14. Kebriaei P, Basset R, Ledesma C, Ciurea S, Parmar S, Shpall EJ, et al. Clofarabine combined with busulfan provides excellent disease control in adult patients with acute lymphoblastic leukemia undergoing allogeneic hematopoietic stem cell transplantation. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2012;18(12):1819-26. Epub 2012/07/04. Kebriaei P, Madden T, Wang X, Thall PF, Ledesma C, de Lima M, et al. Intravenous BU plus Mel: an effective, chemotherapy-only transplant conditioning regimen in patients with ALL. Bone marrow transplantation. 2013;48(1):26-31. Epub 2012/06/27. 15. 16. Small TN, Young JW, Castro-Malaspina H, Prockop S, Wilton A, Heller G, et al. Intravenous busulfan and melphalan, tacrolimus, and short-course methotrexate followed by unmodified HLA-matched related or unrelated hematopoietic stem cell transplantation for the treatment of advanced hematologic malignancies. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2007;13(2):235-44. 77 Not for publication or presentation Attachment 11 Characteristics of Study Population from CIBMTR Database Variable CIBMTR MDACC MOFFITT Number of patients 1183 151 103 Number of centers 174 0 0 Median (range) 35 (18-65) 37 (19-64) 44 (20-65) 18-29 445 (38) 54 (36) 21 (21) 30-39 272 (23) 29 (19) 24 (23) 40-49 262 (22) 26 (17) 23 (22) 50-59 187 (16) 30 (20) 25 (24) 60-69 17 (1) 12 (8) 10 (10) Male 735 (62) N/A 56 (54) Female 448 (38) Age in decades Gender 47 (46) Karnofsky score <90% 298 (25) 35 (23) 19 (18) >=90% 828 (70) 116 (77) 83 (81) Missing 57 (5) 0 1 (1) Median (range) 12 (<1-8930) 14 (<1-3000) <= 30 654 (55) 83 (55) 30 - 100 175 (15) 25 (17) > 100 157 (13) 25 (17) Missing 197 (17) 18 (12) T-cell 199 (17) 24 (16) 7 (7) B-cell 698 (59) 119 (79) 89 (86) Unspecified 286 (24) 8 (5) 7 (7) CR1 838 (71) 99 (66) 86 (83) CR2 345 (29) 52 (34) 17 (17) Median (range) 6 (2-229) 8 (2-129) 6 (2-196) <6 months 602 (51) 51 (34) 39 (38) 6 months - 1 year 268 (23) 41 (27) 48 (47) White blood count at diagnosis FAB classification Disease status prior to HCT Time from diagnosis to HCT 78 Not for publication or presentation Variable Attachment 11 CIBMTR MDACC MOFFITT 313 (26) 59 (39) 16 (15) Median (range) 17 (<1-164) N/A N/A <6 months 57 (5) 6 months - 1 year 49 (4) >1 year 171 (14) 88 838 (71) Missing 68 (6) N/A N/A >1 year Duration of CR1 for CR2 patients Time to achieve CR1 Median (range) 6 (<1-612) <4 weeks 158 (13) 4-8 weeks 479 (40) >=8 weeks 469 (40) Missing 77 (7) Extramedullary disease at diagnosis No 992 (84) 121 (80) Yes 184 (16) 24 (16) Missing 7 (<1) 6 (4) No 1115 (94) 136 (90) Yes 61 (5) 9 (6) Missing 7 (<1) 6 (4) No 1047 (89) 129 (85) Yes 129 (11) 16 (11) Missing 7 (<1) 6 (4) ATG alone 121 (10) 65 (43) 0 or 1 (double blind) CAMPATH alone 13 (1) 0 0 No ATG or CAMPATH 1049 (89) 86 (57) 102 or 103 (100) EMD at CNS at diagnosis EMD at other site at diagnosis ATG or campath Conditioning regimen for CIBMTR cases TBI + VP16 + Cy 60 (5) TBI + VP16 226 (19) TBI + Cy 792 (67) IV Bu + Fludara 58 (5) 79 Not for publication or presentation Variable Attachment 11 CIBMTR IV Bu + Cy 47 (4) Missing 0 MDACC MOFFITT Conditioning regimen for MDACC cases Bu+Clo 54 (36) Bu+Clo+ATG 48 (32) Flu+Bu 4 (3) Bu+Mel 28 (19) Bu+Mel+ATG 15 (10) Flu+Bu+Clo+ATG 2 (1) Missing 0 Conditioning regimen for Moffitt cases Flu+Bu (AUC 3500) Flu+Bu (AUC 5300) Flu+Bu (AUC 5300)+R Flu+Bu (AUC 5300) ATG-F/Placebo Flu+Bu (AUC 6000) Flu+Bu (AUC 7500) 1 (1) 87 (84) 1 (1) 1 (1) 5 (5) 8 (8) Total body irradiation No 89 (8) 151 103 Yes 1094 (92) 0 0 Median (range) 12 (4-55) N/A N/A <13 Gy 691 (58) >=13 Gy 403 (34) Not applicable 89 (8) N/A 23 (22) TBI dose Donor/Recipient CMV match -/- 322 (27) -/+ 280 (24) 28 (27) +/- 146 (12) 14 (14) +/+ 395 (33) 38 (37) Missing 40 (3) 0 Donor/Recipient sex match M/M 477 (40) N/A 30 (29) 80 Not for publication or presentation Variable Attachment 11 CIBMTR MDACC MOFFITT M/F 249 (21) 30 (29) F/M 258 (22) 26 (25) F/F 198 (17) 17 (17) Missing 1 (<1) 0 Type of donor HLA-identical sibling 655 (55) 85 (56) 52 (50) Well-matched unrelated 528 (45) 66 (44) 51 (50) Bone marrow 320 (27) 36 (24) 1 (1) Peripheral blood 863 (73) 115 (76) 102 (99) 2000 42 (4) 0 0 2001 53 (4) 0 0 2002 91 (8) 0 0 2003 97 (8) 0 0 2004 122 (10) 0 0 2005 154 (13) 2 (1) 5 (5) 2006 135 (11) 4 (3) 5 (5) 2007 109 (9) 9 (6) 7 (7) 2008 119 (10) 16 (11) 11 (11) 2009 82 (7) 15 (10) 15 (14) 2010 48 (4) 18 (12) 12 (12) 2011 74 (6) 25 (17) 16 (15) 2012 21 (2) 21 (14) 8 (8) 2013 36 (3) 28 (19) 15 (14) 2014 0 13 (9) 9 (9) 30 (1-93) 36 (1-97) Graft type Year of HCT Median follow-up of survivors (range), months 71 (3-173) 81 Not for publication or presentation Attachment 11 Crosstab of disease status by conditioning regimen group Conditioning 1 Bu+Clo 2 Bu+Clo+ATG 3 Flu+Bu 5 Bu+Mel 6 Bu+Mel+ATG 7 Flu+Bu+Clo+ATG Total Disease status 2 CR1 3 CR2 Total 36 18 54 29 19 48 4 0 4 18 10 28 10 5 15 2 0 2 99 52 151 82 Not for publication or presentation Attachment 12 Study Proposal 1411-85 Study Title: Allogeneic (allo) stem cell transplant (SCT) for AML: A comparison of three different reduced intensity conditioning (RIC) regimens in the CIBMTR data base. Rajneesh Nath, MD, UMass Memorial Medical Center, MA, neeshr@aol.com; Rajneesh.nath@umassmemorial.org Zheng (Frank) Zhou, MD, PhD, UMass Memorial Medical Center, MA, zheng.zhou@umassmemorial.org Jan Cerny, MD, PhD, UMass Memorial Medical Center, MA, jan.cerny@umassmemorial.org Hypothesis: Allo- SCT is a curative option in patients with AML. RIC conditioning is frequently employed for older patients and those with co morbidities. The three most commonly used RIC regimens are Buslfan (B) based (B oral dose < 9mg/kg or IV equivalent), Melphalan (M) based (M dose <150 mg/m2) or TBI based (TBI dose>200 cGy and <500cGYsingle dose or TBI dose < 800cGY fractionated). The relative organ toxicity and anti leukemia effect for these regimens is currently not known. The incidence of non-relapse mortality, relapse rate and overall survival of these three regimens in a large registry dataset of AML patients will help determine the relative efficacy of these regimens. Specific Aims: The aim of this study will be to evaluate from the CIBMTR database 1. The relative frequencies of three different RIC regimens for AML patients. 2. To compare the treatment related toxicity of the three RIC regimens in terms of non relapse mortality and incidence and severity of acute and chronic GVHD. 3. To compare the incidence of relapse and overall survival in the three groups Scientific Justification: RIC regimens are being increasingly used for allo SCT in AML. While several studies have compared the outcomes of conventional ablative with RIC regimens in AML, there is limited data about the relative toxicity and efficacy of the different RIC regimens. A single center analysis of 151 patients comparing M and B based RIC revealed that M based regimen was more myelosuppressive , had higher grade III-IV organ toxicity (53% versus 31%; P=0.005) and higher grade II-IV acute GVHD (53% versus 33%; P=0.01). M based RIC was also associated with higher non-relapse mortality (40% versus 16%; P=0.003). However, there was better disease control with M based RIC conditioning. CIBMTR database will provide a larger dataset to compare the relative toxicities and efficacy of these three RIC regimens in AML. Results will guide the development of future prospective RIC protocols in AML. Patient Eligibility Population: All patients over the age of 18 years who have undergone an allogeneic SCT for AML using related or unrelated donor and had data reported to the CIBMTR and had a minimum follow-up of 4 years. Data Requirements: Age Gender Donor-Recipient Sex Match 83 Not for publication or presentation Attachment 12 AML FAB subtype Therapy related/secondary AML Cytogenetics risk category Karnofsky HSCT-comorbidity index Disease Status at SCT Time from diagnosis to SCT Durations of prior CRs Bone marrow blast percentage Stem cell source (BM, PBSC, Cord blood) Donor age Donor recipient CMV status Prior auto SCT Conditioning regimen used Documented organ toxicity GVHD prophylaxis regimen T cell antibody use Date of SCT Time to Neutrophil engraftment time Time to Platelet engraftment time Immune recovery (objective measures, including CD4 counts recovery) Mixed chimerism at 30 days, 6 months and 1 year Post-transplant infection (bacteria, fungal and/or viral) Acute GVHD, organ involved and grade Chronic GVHD, organ involved and grade Relapse-free survival at different time points (day 100, 1 year, 3 and 5 years) Overall survival at different time points (day 100, 1 year, 3 and 5 years) Sample Requirements: This is a retrospective study from the CIBMTR database. No actual biological sample needed. Study Design: A retrospective cohort study of consecutive adult AML patients in the CIBMTR database, who underwent RIC based allogeneic stem cell transplantation using related or unrelated stem cell donor. Study endpoints: Primary endpoints: Overall mortality (OS) at Day +100, 1 year and 3 years Secondary endpoints: Treatment-related mortality (TRM) at Day +100, 1 year and 3 years Relapse free survival (RFS) at Day+100, 1 year and 3 years Engraftment rate and Time to engraftment (neutrophil, platelet and immunorecovery) Cumulative incidence and severity of GVHD (acute and chronic) Mixed Chimerism (%) at day 30, 6 months and 1 year TRM is defined as death during continuous disease remission after transplant; Relapse is defined as clinical or hematological recurrence; 84 Not for publication or presentation Attachment 12 RFS is defined as clinical or hematological relapses or deaths from any cause; OS is defined as death from any cause Surviving patients will be censored at the time of last clinic follow-up or the date of last contact, whichever is later. Methods of analysis: Comparison will be made for 3 different RIC condition regimens with respect to the study endpoints listed above. Descriptive Statistics Descriptive statistics for patient demographic, baseline clinical information and disease characteristics will be summarized among the RIC regimens. For continuous variables, mean, median, standard deviation (SD) and range of values will be provided; and for categorical variables, number in each category and proportion, % will be provided. Survival Analysis Multivariate Cox proportional hazard regression will be performed with adjustment for patient baseline clinical and disease characteristics to determine significance of difference in outcomes related to the RIC condition regimens. Hazard ratio with 95% confidence interval (CI) will be provided. Cumulative Incidence and Competing Risk Rates of relapse, TRM, success in engraftment (neutrophil, platelet and CD4) and GVHD (acute and chronic) will be estimated using cumulative incidence approach. In the analysis of the cumulative incidence of engraftments, early mortality will be considered as competing risk; In the analysis of GVHD, relapse and mortality will be considered a competing risk. Kaplan-Meier Curves OS, TRM and RFS will be compared with stratification by the 3 condition regimens using Kaplan-Meier curves. Log-rank P-value will be reported. References: 1. Luger SM, Ringden O, Zhang M-J et al . Similar outcomes using myeloablative vs reducedintensity allogeneic transplant preparative regimens for AML or MDS. Bone Marrow Transplantation (2012) 47, 203–211. 2. Russell NH, Kjeldsen L, Craddock C et al. A comparative assessment of the curative potential of reduced intensity allografts in acute myeloid leukaemia. Leukemia (2014) doi:10.1038/leu.2014.319. 3. Shimoni A, Hardan I, Shem-Tov V et al. Comparison between two fludarabine-based reducedintensity conditioning regimens before allogeneic hematopoietic stem-cell transplantation: fludarabine/Melphalan is associated with higher incidence of acute graft-versus-host disease and non-relapse mortality and lower incidence of relapse than fludarabine/busulfan. Leukemia (2007) 21, 2109–2116 85 Not for publication or presentation Attachment 12 Characteristics of Study Population Variable Number of patients Number of centers Age in decades TBI based 534 75 Bu based 729 94 Mel based 658 84 57 (19-76) 24 (4) 36 (7) 81 (15) 186 (35) 185 (35) 22 (4) 59 (18-79) 39 (5) 37 (5) 78 (11) 249 (34) 299 (41) 27 (4) 58 (18-77) 36 (5) 45 (7) 83 (13) 216 (33) 258 (39) 20 (3) Male Female Karnofsky score 286 (54) 248 (46) 419 (57) 310 (43) 364 (55) 294 (45) <90% >=90% Missing White blood count at diagnosis 169 (32) 350 (66) 15 (3) 242 (33) 431 (59) 56 (8) 255 (39) 380 (58) 23 (3) 6 (<1-801) 257 (48) 146 (27) 36 (7) 95 (18) 6 (<1-1300) 409 (56) 202 (28) 50 (7) 68 (9) 7 (<1-1105) 305 (46) 194 (29) 45 (7) 114 (17) 375 (70) 128 (24) 31 (6) 495 (68) 187 (26) 47 (6) 417 (63) 193 (29) 48 (7) 107 (20) 27 (5) 32 (6) 71 (13) 288 (54) 9 (2) 98 (13) 54 (7) 30 (4) 90 (12) 452 (62) 5 (<1) 75 (11) 19 (3) 16 (2) 45 (7) 501 (76) 2 (<1) 66 (12) 257 (48) 111 (21) 79 (11) 420 (58) 156 (21) 161 (24) 262 (40) 96 (15) Median (range) 18-29 30-39 40-49 50-59 60-69 >=70 Gender Median (range) <= 10 10 - 100 > 100 Missing Type of AML De-novo Transformed from MDS/MPS Therapy linked HCT-CI 0 1 2 3+ N/A, earlier than 2007 Missing Disease status prior to HCT Primary induction failure CR1 CR2 86 Not for publication or presentation Variable >=CR3 Relapse Cytogenetics scoring Attachment 12 TBI based 18 (3) 82 (15) Bu based 10 (1) 64 (9) Mel based 4 (<1) 135 (21) 148 (28) 27 (5) 94 (18) 144 (27) 28 (5) 10 (2) 83 (16) 211 (29) 43 (6) 156 (21) 152 (21) 11 (2) 28 (4) 128 (18) 133 (20) 34 (5) 132 (20) 160 (24) 12 (2) 25 (4) 162 (25) 7 (<1-313) 234 (44) 149 (28) 151 (28) 7 (1-146) 325 (45) 218 (30) 186 (26) 6 (<1-185) 323 (49) 177 (27) 158 (24) TBI + Bu TBI + Cy + Flu +- other TBI + Cy +- other TBI + Flu +- other Other TBI based Bu + Flu Mel + Flu Mel + Flu + Nitro + BCNU Mel + Flu + other Graft type 112 (21) 308 (58) 11 (2) 56 (10) 47 (9) 0 0 0 0 0 0 0 0 0 729 0 0 0 0 0 0 0 0 0 535 (81) 94 (14) 29 (4) Bone marrow Peripheral blood Umbilical cord blood Type of donor HLA-identical sibling Other related Well-matched unrelated Partially matched unrelated Mismatched unrelated Unrelated TBD Cord blood Donor/Recipient sex match 75 (14) 256 (48) 203 (38) 82 (11) 636 (87) 11 (2) 104 (16) 507 (77) 47 (7) 76 (14) 53 (10) 81 (15) 63 (12) 16 (3) 42 (8) 203 (38) 243 (33) 24 (3) 297 (41) 85 (12) 15 (2) 54 (7) 11 (2) 131 (20) 16 (2) 287 (44) 107 (16) 28 (4) 42 (6) 47 (7) 181 (34) 130 (24) 283 (39) 175 (24) 241 (37) 183 (28) Normal Favorable Intermediate Poor TBD (needs review) Not tested Missing Time from diagnosis to HCT Median (range) <6 months 6 - 12 months >12 months Conditioning regimen M/M M/F 87 Not for publication or presentation Variable F/M F/F TBD Donor/Recipient CMV match Attachment 12 TBI based 104 (19) 116 (22) 3 (<1) Bu based 134 (18) 134 (18) 3 (<1) Mel based 122 (19) 110 (17) 2 (<1) -/-/+ +/+/+ TBD GVHD prophylaxis 101 (19) 145 (27) 50 (9) 148 (28) 90 (17) 143 (20) 220 (30) 68 (9) 266 (36) 32 (4) 118 (18) 215 (33) 64 (10) 216 (33) 45 (7) No GVHD prophylaxis Ex-vivo T-cell depletion CD34 selection Post-tx cy FK506 + MMF +- others FK506 + MTX +- others FK506 + others FK506 alone CSA + MMF +- others CSA + MTX +- others CSA + others CSA alone Other GVHD prophylaxis Missing In-vivo TCD 5 (<1) 19 (4) 10 (2) 20 (4) 114 (21) 36 (7) 10 (2) 19 (4) 235 (44) 32 (6) 10 (2) 7 (1) 14 (3) 3 (<1) 8 (1) 7 (<1) 4 (<1) 0 98 (13) 311 (43) 20 (3) 31 (4) 50 (7) 102 (14) 8 (1) 76 (10) 13 (2) 1 (<1) 13 (2) 4 (<1) 18 (3) 0 112 (17) 145 (22) 37 (6) 45 (7) 111 (17) 92 (14) 49 (7) 26 (4) 4 (<1) 2 (<1) No Yes Missing Year of HCT 371 (69) 154 (29) 9 (2) 279 (38) 440 (60) 10 (1) 283 (43) 331 (50) 44 (7) 13 (2) 21 (4) 42 (8) 55 (10) 44 (8) 55 (10) 58 (11) 83 (16) 102 (19) 61 (11) 68 (3-145) 38 (5) 41 (6) 43 (6) 53 (7) 79 (11) 93 (13) 105 (14) 121 (17) 101 (14) 55 (8) 68 (2-151) 26 (4) 44 (7) 72 (11) 84 (13) 104 (16) 86 (13) 85 (13) 83 (13) 52 (8) 22 (3) 73 (3-145) 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 Median follow-up of survivors (range), months 88 Not for publication or presentation Attachment 12 Selection: st 1 allo HCT for AML between 2001 to 2010 after CAP modeling Reduced intensity conditioning containing TBI/Bu/Mel Excluding syngeneic twin donor Complete research form Patient consent 89