DOI: 10.1161/CIRCULATIONAHA.115.016291
Arrhythmic Mitral Valve Prolapse and Sudden Cardiac Death
Running title: Basso et al.; Arrhythmic Mitral Valve Prolapse
Cristina Basso, MD, PhD1*; Martina Perazzolo Marra, MD, PhD1*; Stefania Rizzo, MD, PhD1;
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Manuel De Lazzari, MD, PhD1; Benedetta Giorgi, MD2; Alberto Cipriani, MD1; Anna Chiara
Frigo,
g MSc1; Ilaria Rigato,
g
MD, PhD1; Federico Migliore,
g
MD, PhD1; Kalliopi
p Pilichou, PhD1;
Emanuele Bertaglia, MD1; Luisa Cacciavillani, MD, PhD1; Barbara Bauce, M
MD,
D, P
PhD
hD1;
Domenico Corrado, MD, PhD1; Gaetano Thiene, MD1; Sabino Iliceto, MD1
1
Dept
Dep
De
pt of Ca
Cardiac, Thoracic, and Vascular Scienc
Sciences;
cess; 2Dept of Ra
Radiology,
adi
d ology, Azienda OspedalieraUniv
versity of Padua
Padua Medical
Pa
Mediicaal School,
Scho
Sc
hoool, Padua,
ho
Padu
dua, Italy
du
Itaaly
y
University
*contributed
*con
*c
ontr
on
trib
tr
ibut
ib
uted
ut
ed eequally
qual
qu
ally
al
ly
Address for Correspondence:
Cristina Basso, MD, PhD
Department of Cardiac, Thoracic, and Vascular Sciences
University of Padua Medical School
Via A. Gabelli, 61
35121 Padova-Italy
Tel: +39 0498272286
Fax: +39 0498272284
Email: cristina.basso@unipd.it
Journal Subject Codes: Diagnostic testing:[30] CT and MRI, Etiology:[5] Arrhythmias, clinical
electrophysiology, drugs
1
DOI: 10.1161/CIRCULATIONAHA.115.016291
Abstract
Background—Mitral valve prolapse (MVP) may present with ventricular arrhythmias and
sudden cardiac death (SCD) even in the absence of hemodynamic impairment. The structural
basis of ventricular electrical instability remains elusive.
Methods and Results—A) The Cardiac Registry of 650 young adults (40 yrs) with SCD was
reviewed and cases with MVP as the only cause of SCD were reexamined. Forty-three MVP
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
cases (26 female, age range 19-40, median 32 yrs) were identified (7% of all SCD, 13% of
women). Among 12 with available ECG, 10 (83%) had inverted T waves on inferior leads and all
right
found
ight bundle branch block ventricular arrhythmias. A bileaflet involvement was fo
oun
undd in 770%.
0%.
0%
LV fibrosis was detected at histology at the level of papillary muscles in all and infero-basal wal
wall
in
88%.
MVP
ventricular
n 88%
8%.. B) M
8%
VP
P ppatients
atients with complex ventricu
ula
larr arrhythmias (N=30)
0)) aand
nd without (controls,
N=14)
underwent
study
protocol
cardiac
magnetic
N=114) underwen
ent a st
en
stud
udyy pr
ud
prot
otoocol
ot
ocol
o iincluding
nclu
nc
luding
ng
g ccontrast-enhanced
ontra
rast-eenh
ra
nhan
ancced
an
ced ca
card
rdia
rd
iacc m
ia
agn
gnet
gn
etic
et
ic rresonance
eson
es
onnan
ance
ce ((CECECE
CMR).
Patients
with
arrhythmias
(22
age
28-43,
median
CM
MR)
R). Patien
ents w
en
ith ccomplex
om
mpleex ve
vventricular
nttri
ricu
ulaar ar
rrh
rhyt
ythm
mias (2
22 ffemale,
ema
male
ma
lee, ag
ge rrange
anngee 28
28-43
3, m
3,
ed
diaan 41
yrs),
either
branch
polymorphic,
yrrs)
yrs)
s), ei
eith
ther
th
er rright
ight
ig
ht bbundle
un
undl
ndl
dlee br
bran
anch
an
ch bblock-type
loc
ockk-ty
type
pe oorr po
poly
lymo
morp
mo
rphi
rp
hicc, sshowed
hi
howed
ho
ed a bbileaflet
ilea
il
eafl
ea
flet
fl
et iinvolvement
nvol
nv
olve
ol
veme
eme
ment
nt iin
n
70% of cases. LV late-enhancement was identified by CE-CMR in 93% vs. 14% of controls
(p<0.001), with a regional distribution overlapping the histopathology findings.
Conclusions—MVP is an under-estimated cause of arrhythmic SCD, mostly in young adult
women. Fibrosis of papillary muscles and infero-basal LV wall, suggesting a myocardial stretch
by the prolapsing leaflet, is the structural hallmark and correlates with ventricular arrhythmias
origin. CE-CMR may help to identify this concealed substrate for risk stratification.
Key words: arrhythmia (mechanisms), mitral valve, sudden cardiac death, arrhythmia,
pathology, cardiac magnetic resonance imaging, mitral valve prolapse
2
DOI: 10.1161/CIRCULATIONAHA.115.016291
Introduction
Mitral valve prolapse (MVP) is the most common valve disease with an estimated prevalence of
2-3% in the general population1. Although MVP is generally regarded as a benign condition2,3,
the outcome is widely heterogeneous and complications such as mitral regurgitation, atrial
fibrillation, congestive heart failure, endocarditis and stroke are well known. Ventricular
arrhythmias and sudden cardiac death (SCD) have been even reported4-7.
From a pathologic anatomy viewpoint, accumulation of proteoglycans (myxomatous
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
mitral valve) is the most common cause of MVP, accounting for leaflet thickening and
redundancy, chordal elongation, interchordal hoodings and anular dilatation8. While these valve
abnormalities well explain mitral regurgitation and mechanical complications duee tto
o en
enha
enhanced
hanc
ha
nced
nc
ed
extensibility, the pathogenesis of ventricular arrhythmias/SCD in MVP remains controversial.
The
The es
eestimated
tima
mate
ma
t d rate of SCD in MVP range
ranges
es fr
from 0.2% to 0.4% per
per year on the basis of
studies
pprospective
rosspective fo
ffollow-up
lllow-u
ow up stud
st
tud
udiies
ies4. Le
Left
ft ven
ventricular
enttricul
u ar (LV
(LV)
LV
V) dy
dysf
dysfunction
sfun
sf
fun
uncctio
ionn du
duee to sev
severe
ver
eree mi
mitr
mitral
tral
tr
al
regurgitation
egu
gurg
rgitatio
rg
on identifies
i en
id
e tifiees a patient
pattie
i nt
nt subgroup
suubg
b rooup
up at
at high
high
g risk
riisk off SCD
CD9. Ho
Howe
However,
w verr, lif
life-threatening
ifeif
e--threeat
ateenin
ng
veent
vent
ntri
ricu
ri
cula
larr ar
la
arrh
rhyt
rh
ythm
thm
hmia
iass oc
ia
occu
curr al
also
so iin
n MV
MVP
P pa
pati
tien
ti
entts with
en
wiith ttrivial
rivi
ri
vial
ial oorr ab
abse
sent
se
nt m
itra
it
rall re
ra
regu
gurg
rgit
rg
itat
it
atio
at
ionn10.
io
ventricular
arrhythmias
occur
patients
absent
mitral
regurgitation
Previous pathology studies of SCD mostly focused on the mitral valve or conduction system
abnormalities as cause of electrical instability8,11-17, while the demonstration of a myocardial
source of arrhythmias remained elusive18-20.
The aim of our report is to demonstrate that MVP is a significant cause of SCD and lifethreatening arrhythmias in young adults due to an underlying myocardial substrate, which is
detectable by contrast-enhanced cardiac magnetic resonance (CE-CMR) and may serve for risk
stratification and SCD prevention.
3
DOI: 10.1161/CIRCULATIONAHA.115.016291
Material and Methods
Study populations
A) SCD victims with MVP
In the time interval 1982-December 2013, all the hearts of SCD victims 40 years old occurring in
the Veneto Region, North East Italy (geographic area 18,368 km2, overall population 4.857.210
according to the Italian Census Bureau 2011), were collected, pathologically investigated and
preserved. SCD is herein defined as witnessed sudden and unexpected death occurring within 1
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
hour of the onset of symptoms or death of an individual who had been seen in stable condition <24
hours before being found dead21,22. Demographic, clinical and pathologic data were recorded in the
electronic database of the Registry of Cardio-cerebro-vascular pathology which act
acts
ts as rreferral
efer
ef
erra
er
rall
ra
center for SCD of the North-East of Italy.
Charts
Char
Ch
arts
ar
ts were
weere
ere evaluated for age, sex, sympto
symptoms
toms
to
m and clinical history
history.
y. Al
A
Alll the hearts were
reexamined
carefully
standardized
eex
xamined car
ref
efullly
y aaccording
cccor
ordding
ng tto
o a st
sta
anddard
rdizzed pprotocol
rd
ro
otoco
coll21. SCD
co
SCD ca
case
cases
sess w
were
ere selected
sel
elec
eccte
tedd inn whom
who
hom
m
MVP
MV
P due to
om
myxomatous
yx
xom
mattou
ous valve
vaalv
l e disease
dise
seaasee was
se
was the
th
he only
onnly
y cardiac
caarddiacc abnormality
abn
norma
mali
ma
l ty
y ffound
ou
und at au
auto
autopsy.
topssy..
to
Myxomatous
M
My
yxo
xoma
oma
mato
tous
to
uss val
valve
alve
al
vee ddisease
isea
is
ease
ea
se is
is defined
defi
de
fine
fi
nedd as increased
ne
inc
ncre
reas
re
aseed le
as
leaf
leaflet
afle
af
lett le
le
leng
length
ngth
ng
th and
and redundancy,
red
edun
und
ndan
ancy
cy, with
wiith interchordal
int
nter
erch
er
chor
ch
orda
or
dall
da
hoodings and leaflet billowing toward the left atrium and chordae tendineae elongation8. In the
absence of extracardiac (cerebral, respiratory) or mechanical cardiovascular explanations, the
cause of death was considered cardiac arrhythmic.
Exclusion criteria were clinical and/or pathologic evidence of more than mild mitral
regurgitation. Hearts from 15 sex and age-matched patients (10 females, mean age 30 years, range
18-40), who died suddenly for extracardiac causes (8 cerebral and 7 respiratory), served as controls.
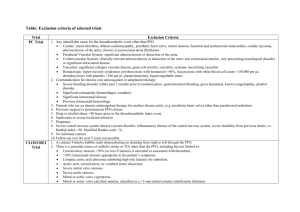
B) MVP patients with complex ventricular arrhythmias
The study included consecutive patients, referred to the Cardiology Clinic, from January 2010 to
4
DOI: 10.1161/CIRCULATIONAHA.115.016291
December 2013, with complex ventricular arrhythmias detected on the basis of 12-lead 24-hour
Holter monitoring and echocardiographic diagnosis of MVP, defined as >5 mm thickening and
>2-mm displacement of one or both mitral leaflets into the left atrium as viewed in the LV
outflow tract orientation23. Twelve-lead ECG 24 hours Holter was requested due to the presence
of either arrhythmic symptoms or 12-lead ECG changes. Complex ventricular arrhythmias
consisted of ventricular fibrillation (VF) and ventricular tachycardia (VT), either non-sustained
or sustained24. Complex ventricular arrhythmias patients were further sub-divided into two
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
groups, i.e. those with 3 ventricular premature beats (VPB) run and those >3 VPB run.
The control group consisted of MVP patients with minor ventricular arrhythmias, i.e.
solated VPB, couplets and bigeminal VPB.
isolated
Exclusion criteria were significant mitral regurgitation, tricuspid dysplasia or
eguurg
rgit
itat
it
atio
at
ion,
io
n, car
ardi
ar
d omyopathies orr congenital he
di
ear
artt abnormalities, hem
mod
odynamic unstable
regurgitation,
cardiomyopathies
heart
hemodynamic
conditions
con
nd
and ccontraindication
oon
ntrraind
ndic
dic
icaatio
ionn to C
io
MR. T
MR
he study
yw
as app
ppro
pp
r ve
ro
vedd by tthe
he ins
he
sti
titu
tuti
tu
tion
ti
onal
on
al rreview
evie
ev
iew
ie
w
conditions
CMR.
The
was
approved
institutional
booar
ard,
d and aall
ll pa
atieentss gave
ga iinformed
nffor
o me
medd co
cons
n en
nt..
board,
patients
consent.
Prot
Pr
otoc
ot
ocol
oc
olss of iinvestigation.
ol
nves
nv
esti
es
tiga
ti
gati
ga
tion
ti
on.
on
Protocols
A) Pathologic anatomy study
Formalin-fixed hearts were restudied according to a protocol previously reported21. Leaflet
involvement (whether anterior, posterior or bileaflet) and the presence of endocardial fibrous
plaque (friction lesion) on the LV infero-basal wall were assessed. Multiple samples of the LV
and right ventricular free walls and septum, including the papillary muscles (PMs), were
obtained for histology. Additional samples were taken in the LV infero-basal free wall,
underneath the posterior mitral leaflet. Five μm-thick sections were stained with HematoxylinEosin, Weigert-van Gieson, Heidenhain trichrome and Alcian-PAS. Morphometric analysis was
5
DOI: 10.1161/CIRCULATIONAHA.115.016291
performed using an Image-Pro Plus program (Version 4.0. Media Cybernetics, MD, USA) to
quantify the fibrous tissue percent area of LV myocardium on Heidenhain trichrome stained
sections at 25x magnification. Mean cardiomyocytes diameter was calculated on Haematoxylineosin stained sections at 400x magnification. Quantitative analysis was performed by two blind
expert pathologists (CB, SR) with an interobserver variability <5%.
B) Clinical study
All patients underwent cardiovascular evaluation including history, physical examination, 12Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
lead electrocardiogram (ECG), 2D-transthoracic echocardiography, 12-lead 24-hour Holter
monitoring and CE-CMR. Coronary angiography was performed in selected cases. The 12-lead
revi
re
viou
vi
ousl
ou
slyy
sl
ECG at rest and the 24-hour Holter monitoring were independently assessed as pre
previously
eported25 by two experienced observers (MDL and DC) who were blinded to patient data.
reported
NonNo
n-su
ns sttai
ainned VT was defined as 3 con
onnsec
secutive VPBs with a ra
ate > 100 bpm that lasted
Non-sustained
consecutive
rate
<
<30
300 seconds du
during
uri
rinng 224-hour
4-ho
4hour
ho
ur H
Holter
olte
ol
ter mo
te
mon
monitoring.
nitori
ring
ri
g. Su
Sustained
ustaine
nedd VT w
ne
was
as ddefined
efin
ef
ineed aass tachycardia
in
tach
ta
chyc
ch
ycarrdia
yc
dia
originating
orrig
igin
inatingg in thee ventricle
in
venttricle with
witth rate
ratte >100
>1
100 bbeats/minute
eats
ea
t /m
min
nutte an
aand
d la
lasting
astiing >
>30
30
0 seco
seconds
ondds orr re
requ
requiring
uiriing an
an
intervention
nte
terv
rven
enti
en
tion
ti
on ffor
or ttermination.
ermi
er
mina
mi
nati
na
tion
ti
on.
on
Cardiac magnetic resonance was performed on a 1.5-Tesla scanner (Magnetom Avanto,
Siemens Medical Solutions, Erlangen, Germany). All patients underwent detailed CE-CMR
study protocol as previously described25. The presence and location of late gadolinium
enhancement (LGE) were independently assessed by two experienced observers (MPM and BG)
who were blinded to clinical data. To exclude artifact, LGE was deemed present only if visible in
two orthogonal views (long-axis and short-axis). LGE was identified using a signal intensity
threshold of >5SD above a remote reference region and quantified according to a previously
reported method.
6
DOI: 10.1161/CIRCULATIONAHA.115.016291
Statistical Analysis
Data are expressed as mean value±standard deviation or median with 25 to 75 percentiles for
normally distributed and skewed variables, respectively. Normal distribution was assessed using
Shapiro-Wilk test. Categorical differences between groups were evaluated by the chi-square test
or the Fisher exact test as appropriate. Paired and unpaired t test were used to compare normally
distributed continuous variables respectively obtained from the same patient and different
patients; Wilcoxon signed rank test (same patient) and Wilcoxon rank sum test (independent
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
samples) were used for skewed continuous variables.
A p value <0.05 was considered significant. The minimal detectable effect at a
significance
ignificance level of 5% and power at 80% is equal to 1 (with non parametric test)
t) ffor
or
quantitative variables (Cohen’ Effect); for binary data an odds ratio of at least 10 can be detected
iff the
complex
hee proportion
pro
ropo
port
po
rtionn of the characteristic test is equal
rt
al tto
o 10% in the no com
mpl x ventricular
mple
arrhythmias
arrh
ar
hythmias group
grou
oupp (Fisher’s
ou
(F
Fishe
ishe
her’
r s exact
exaact
ex
act test).Statistics
test
te
stt).
) Stattis
i tiics were
we analyzed
analy
naly
lyzzedd with
with SPSS
SPS
PSS version
vers
ve
rsio
rs
ionn 19
io
1 (SPSS
(SP
SPSS
SS Inc,
Inc
Chicago,
IL).
Ch
hiccag
a o, IL)
L).
L)
Results
A) SCD victims with MVP
Among 650 consecutive young SCDs recorded in the Veneto Region Registry , 43 cases (26
females, median age 32 years, range 19-40) with MVP due to myxomatous valve disease were
identified. They represent 7% of all SCD cases and 13% of women who died suddenly, being the
first structural cause in the latter group. Main clinical and pathologic data are reported in Table
1. SCD occurred mostly at rest or during sleep (N=35, 81%). Twenty (47%) had an in vivo
diagnosis of MVP, with auscultatory click in 18 (90%) and palpitations in 14 (70%). Nine (21%)
7
DOI: 10.1161/CIRCULATIONAHA.115.016291
were under beta-blockers therapy due to non sustained ventricular arrhythmias. ECG was
available in 12 (28%), showing negative/isodiphasic T waves on inferior lead in 10/12 (83%)
(Figure 1A,B); all had right bundle branch block (RBBB) morphology (100%) ventricular
arrhythmias.
In SCD cases with MVP, valve leaflets were redundant, thick and elongated, with either
isolated posterior (N=13, 30%) or bileaflet (N=30, 70%) involvement (Figure 1C). The
involvement of the posterior leaflet was diffuse in 23 (53%) and confined to the medial scallop in
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
20 (47%). Endocardial fibrous plaques in the postero-lateral wall were found in 25 (58%).
Microscopic examination of the LV myocardium showed an increased endo-perimysial
and patchy replacement-type fibrosis at the level of PMs and adjacent free wall in
n aall
ll ((Figure
Figu
Fi
gure
gu
re
1D,E and Figure 2). Similar findings, with a subendocardial-midmural layer distribution, were
detected
infero-basal
leaflet,
deteect
cted
ed iin
n th
the in
nfe
fero-basal wall, underneath thee pposterior
o terior mitral valve le
os
leaf
a let, in 38 cases (88%).
The
Thee mean fibrous
fib
bro
ous tissue
tisssu
suee percent
perc
pe
rcen
rc
entt area
en
area in
in MVP
MV
VP SCD
D victims
vict
ctim
ct
imss was
im
wass 30.5%
30.5%
5% att thee level
level
evel of
of PMs
PMs and
and
33.1%
wall
myocardium
(vs.
and
controls,
p<0.001).
333.1
.1%
% in the
hee iinfero-basal
nffero-baasaal wa
alll m
yoca
yo
c rd
diu
ium
m (v
vs. 6.3% an
nd 66.4%
.4%
4% iin
n co
onttro
ols, p<
p<0.00
01).
1) In
n tthe
he
same
ame areas,
are
reas
as, the
as
the cardiomyocytes
card
ca
rdio
rd
iomy
io
myoc
ocyt
oc
ytes
tes showed
sho
howe
wed
ed increased
incr
in
crea
cr
ease
ea
sedd diameter
se
diam
di
amet
am
eter
et
er (19.2±6.0
(19.2±6
2±6.00 micron
mic
icro
ronn vs.
ro
vss 12.8±0.4,
12.8±0
8±0.4,
4
p<0.001) and dysmorphic and dysmetric nuclei.
B) MVP patients with complex ventricular arrhythmias
The baseline clinical and CMR findings are summarized in Table 2. Fourteen MVP patients with
or without minor ventricular arrhythmias (i.e. isolated VPB, couplets and bigeminal VPB) served
as controls.
Thirty MVP patients (22 female, median age 41) with complex ventricular arrhythmias,
i.e. 1 VF (N=2, who had also non-sustained VT) and VT (N=28) - either non-sustained (N=27)
or sustained (N=1)- were collected. VT of LV origin (RBBB morphology) was present in all,
8
DOI: 10.1161/CIRCULATIONAHA.115.016291
with either inferior (43%) or superior (87%) axis. Among the 27 patients with non-sustained
VT, the mean length was 4 beats (ranging 3-11 beats). Complex ventricular arrhythmias occurred
at rest in 26/30 (87%). All patients had normal QTc (mean 423, range 409-440). Exercise stress
test, performed in 20,was negative for effort-induced ventricular arrhythmias.
Bileaflet MVP was present in 21 (70%) patients with complex ventricular arrhythmias vs.
5 (36%) controls (p=0.031).
On post-contrast sequences, LV-LGE was identified in 28 (93%) vs. 2 (14%) (p<0.001).
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
By dividing the MVP population with complex ventricular arrhythmias into two sub-groups, 20
patients had 3 VPB run and 10 patients >3 VPB run (p>0.05). In MVP patients with complex
comparing
those
ventricular arrhythmias, no difference was found in terms of LV-LGE when comp
mp
par
arin
ingg th
in
thos
osee
os
with 3 VPB run and those >3 VPB run (p>0.05).
The
mid-apical
The LGE
L E was
LG
was localized on the PMs in 255 ppatients
a ients (83%), with a mi
at
m
d-apical distribution in
segment,
underneath
1166 and/or
and/or basall adjacent
adjjace
ad
cent
ntt free
fre
reee wall
w ll in
wa
in 24 cases;
casees;; andd on
on the
the LV
LV infero-basal
in
nfe
f ro-b
-bas
bas
asaal seg
egm
eg
ment
ment
nt, un
unde
dern
de
rnea
rn
eath
ea
th
the
3A-D).
focal
LGE
region,
he posterior
posterio
po
or leaflet,
l affleet, inn 22
le
22 (73%)
(73
73%)
73
%) (Figure
(Fi
Figu
uree 3A
A-D
D). A fo
ocaal eendocardial
ndo
doca
do
caardia
rdiaal LG
L
GE in the ssame
am re
ame
egionn,
featuring
fibrous
plaque,
found
patients
feat
fe
atur
at
urin
rin
ingg a fi
fibr
brou
br
ouss pl
plaq
aque
aq
ue,
e was
waas fo
foun
und
nd in 112
2 pa
pati
tien
ti
ents
en
ts ((40%).
40%)
40
%).
%)
The median LV LGE % was 1.2 in MVP with complex ventricular arrhythmias vs. 0 in
MVP without (p<0.01).
Two MVP patients experienced aborted SCD due to VF, despite beta-blocker therapy due
to previous sustained VT. Detailed invasive and non-invasive evaluation ruled out cardiac
causes other than MVP. Both had RBBB pattern ventricular arrhythmias with superior axis and T
waves abnormalities on inferior leads. CE-CMR, performed 6 and 10 months before aborted
SCD, revealed LV LGE of PMs and infero-basal wall (Figure 3 E,F). Both patients received an
implantable cardioverter defibrillator (ICD).
9
DOI: 10.1161/CIRCULATIONAHA.115.016291
One patient had pre-syncopal episodes despite bisoprolol therapy. She underwent
electrophysiological study with induction of sustained VT with the same RBBB morphology of
VPBs (Figure 4A-C). The CE-CMR showed a non-ischemic LGE pattern in the LV infero-basal
wall (Figure 4D). She also underwent ICD implantation.
Of the three patients with ICD (mean follow-up 10 months), two had non sustained-VT:
one patient with spontaneous interruption and the other requiring anti-tachycardia pacing.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Discussion
MVP is an under-recognized cause of SCD in young adults, accounting for 7% of total fatal
with
events and 13% of female victims in our large Cardiac Registry experience. The ppatient
atie
at
ient
ie
nt w
ithh
it
MVP and ventricular arrhythmias at risk of SCD is usually a young adult woman, with a midsystolic
auscultation,
involvement
ysttol
olic
ic cclick
lick
li
ck at au
ausc
s ultation, bileaflet involvem
men
entt of the mitral valve, T wave abnormalities on
inferior
RBBB-type
polymorphic
arrhythmias
ECG.
Clear-cut
nfeerior leads, RB
RBBB
BB
B-typ
ypee or po
yp
poly
lym
ly
morp
morp
rphhic vventricular
enntriccullar ar
arrh
rhyt
rh
ythm
yt
hmia
hm
i s on E
ia
CG. Cl
Clea
earea
r cu
rcutt ev
eevidence
iden
id
encee
en
electrical
instability
herein
provided
first
consists
off a ssubstrate
ubstraate off el
lectrriccal ins
nstaabi
ns
b liity inn MV
MVP
P iiss he
ereeinn pr
prov
vid
ded
d ffor
or tthe
or
h fi
he
irstt ttime
im
me an
andd co
onssistss ooff
myocardial
LV
wall,
underneath
myoc
my
ocar
oc
ardi
ar
dial
di
al scarring
sca
carr
rrin
rr
ingg targeting
in
targ
ta
rget
rg
etin
et
ingg the
in
the PMs
PMs and
and the
the infero-basal
infe
in
fero
fe
ro-bas
bas
asal
al L
V fr
free
ee wal
alll, und
al
nder
nd
erne
er
neat
ne
athh th
at
thee
posterior leaflet, well in keeping with the site of origin of RBBB-type ventricular arrhythmias.
The LV myocardial fibrosis observed at histology in SCD victims was then confirmed in the
clinical arm of the study, with evidence of LGE at CE-CMR in arrhythmic MVP patients, thus
pointing to a promising role of this non invasive technique for risk stratification beyond
traditional prognostic markers.
MVP: an underappreciated cause of SCD
The absence of uniform diagnostic criteria of MVP in the general and forensic pathology practice
and the frequent consideration of this valve disease as an uncertain cause of SCD are major
10
DOI: 10.1161/CIRCULATIONAHA.115.016291
obstacles to provide data on the real burden of MVP based upon a metanalysis of published
studies21. With these shortcomings, the prevalence of MVP in pathology series of SCD in the
young ranges from 0 to 24%20,22,26,27. By adopting strict criteria for definition of myxomatous
mitral valve, in the Veneto Region SCD Registry MVP accounted for 7% of all cases in young
adults (<40 years) and 13% among women, representing the first structural cause in the latter
group. The diagnosis can be easily established at macroscopic examination and then confirmed
by routine histology, but it might be overlooked by superficial inspection, leading to discharge
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
the heart as normal. Our data are likely to change the current thinking about MVP as a benign
condition and point to the need to draw the attention of forensic pathologists to an entity that has
been largely underestimated so far.
Ventricular arrhythmias in MVP
nM
VP sseries
erie
er
ies wi
ie
with
th prolonged ECG recording, a vvariable
ar
ariable
prevalence off vventricular
entricular arrhythmias
In
MVP
ha been reported,
has
reporte
ted,
te
d, reflecting
ref
efllect
ef
lect
ctin
ingg the
in
the different
diff
di
fferren
ff
nt MVP
MV definition,
deefi
finiti
tion
ti
on, the
on
the population
popu
po
pula
pu
lattio
la
ionn studied
stud
udie
ud
iedd and
ie
an the
th
5,9,10,28-35
5,9,10,2
,28
28-3
-35
-3
co
omp
mplexity
y ooff ve
enttricu
ulaar ar
rrh
rhyt
ythm
yt
mia
ias co
onsid
ideered5,9
id
. In pparticular,
arrtiicu
ula
l r, tthe
hee cl
clinical
lin
i icaal eevidence
vide
deencee ooff
complexity
ventricular
arrhythmias
considered
hemo
he
mody
mo
dyna
nami
na
mica
mi
call
ca
lly im
ll
impo
port
po
rtan
rt
antt re
an
regu
gurg
rgit
rg
itat
it
atio
at
ionn gr
io
grea
eatl
ea
tly iimpacts
tl
mpac
mp
acts
ac
ts oon
n th
thee oc
occu
curr
rren
rr
ence
en
ce ooff vent
ve
ent
ntri
ricu
ri
cula
larr
la
hemodynamically
important
regurgitation
greatly
occurrence
ventricular
arrhythmias. However, the detection of MVP in survivors of life-threatening arrhythmias
suggests that a true association between hemodynamically uncomplicated MVP and arrhythmic
SCD may exist9. Thus, we decided to focus on "pure" MVP, excluding MVP associated with
valve incompetence and LV remodelling, not to defile the message by over-reporting ventricular
arrhythmias. Early electrophysiological studies demonstrated that the most common site of origin
of VPB is the infero-basal portion of the LV36. In the recent study of malignant MVP by Sriram
et al37, frequent VPBs originated from the outflow tract and PMs. Moreover, electrophysiology
mapped the site of origin to the PMs, the LV outflow tract and the mitral annulus, as to suggest
11
DOI: 10.1161/CIRCULATIONAHA.115.016291
that VPBs arising close to the prolapsing leaflet and adjacent structures are the arrhythmic
triggers.
From a pathophysiologic perspective, the mechanism of ventricular arrhythmias in MVP
patients with trivial or absent mitral regurgitation remains speculative9,38. MVP-related factors
have been first advocated, such as the excessive traction on the PMs by the prolapsing leaflets39;
the mechanical stimulation of the endocardium by the elongated chordae, with after
depolarization-induced triggered activity; the diastolic depolarisation of muscle fibres in
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
redundant leaflets with triggered repetitive automaticity40; and the endocardial friction lesions
with extension into the myocardium41. Moreover, the coexistence of extravalvular diseases has
been suggested, including autonomic nervous system dysfunction42, conduction ssystem
yste
ys
tem
te
m
abnormalities13, fibromuscular dysplasia of small coronary arteries19 and occult
10,43
1
10
43
card
dio
iomy
myop
my
opat
op
athiees10,
at
.
cardiomyopathies
T
The
hee myocardial
al ssubstrate
ub
bstra
rate
ra
te ooff el
elec
electrical
ectr
ec
tric
tr
icall ins
ic
instability
sta
abiliity
y in
n MV
MVP
P
Previous
pathology
studies
MVP
patients
mostly
Pr
rev
evio
i us pat
io
attho
h lo
ogy
y stu
udies iin
nM
VP
P pa
atieentss ddying
y ngg ssuddenly
yi
udddeenlyy mo
mos
stly
y ffocused
occussed
d onn mitral
mittraal valve
vaalvve
structural
tru
ruct
ctur
ct
ural
ral aalterations,
lter
lt
erat
er
atio
at
ions
io
ns, su
ns
ssuggesting
ugg
gges
gg
esti
es
ting
ti
ng a ro
role
le ffor
or aannular
nnul
nn
ular
lar ccircumference,
ircu
ir
cumf
mfer
mf
eren
er
ence
en
ce, le
ce
leaf
leaflets
afle
af
lets
le
ts llength
engt
en
gthh an
gt
andd th
thic
thickness
ickn
ic
knes
kn
esss
es
and presence and extent of endocardial plaques8,14-17. Surprisingly, no investigation did
systematically address the LV myocardium to search for the substrate of electrical instability,
except for few anecdotic cases11,13,14,44,45. For the first time, we extended the histopathology
investigation beyond the valve in all SCD cases and provided convincing evidence of fibrosis in
the LV myocardium, which is closely linked to the mitral valve, i.e. the PMs with adjacent free
wall and the infero-basal wall. The LV myocardial scarring is qualitatively different from that
observed in ischemic heart disease, where it is usually compact and confluent, being instead
patchy and interspersed within surviving, hypertrophic cardiomyocytes. Noteworthy, previous
12
DOI: 10.1161/CIRCULATIONAHA.115.016291
pathology studies addressed the so-called “idiopathic myocardial fibrosis” in SCD victims46. By
definition this entity is not associated with other structural heart diseases and remains without an
explanation. However, the LV fibrosis described in our MVP cases differ in terms of type (i.e.
scarring) and location (i.e. LV papillary muscles and basal postero-lateral wall).
Furthermore, we herein demonstrate that CE-CMR can detect LV-LGE in MVP patients
with complex ventricular arrhythmias, closely overlapping the histopathologic features observed
in SCD victims. At the level of PMs, two LGE sites have been found, i.e. the mid-apical portion
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
and the base/adjacent LV wall. Although PMs LGE has been reported by Han et al24 in MVP
patients with a history of arrhythmias, most of these patients had moderate to severe mitral
regurgitation.
egurgitation. While confirming
f
these data in purely arrhythmic MVP patients wi
without
ith
thou
outt
ou
hemodynamic impairment, we first provide convincing evidence of LGE in the infero-basal LV
wall.
wall
l. The
The arrhythmogenic
arrh
ar
rhythm
rh
hmogenic role of the LV myocardial
hm
myocaard
rdia
ial scarring is suppor
ia
supported
rte
tedd by the morphology of
arrhythmias
arrh
ar
hythmias andd byy eelectrophysiological
lect
le
ctro
ct
roph
ro
phys
ph
ysiiolo
ys
iolo
logi
giccall studies
gi
sttud
udiees inn MVP
MVP indicating
ind
ndic
icat
ic
atin
i g that
that the
thhe most
most
ost common
comm
co
mmon
mm
on site
sit
itee of
o
36,37
6,37
VPB
LV
wall
VP
B origin is
is the
th
he infero-basal
infeero
ro-bassal L
V wa
w
lll36
.
Most
Mo
st ooff CE
-CMR
CMR sstudies
tudi
tu
dies
di
es ffor
or aarrhythmic
rrhy
rr
hyth
thmi
th
micc ri
mi
risk
sk sstratification
trat
tr
atif
at
ific
if
icat
ic
atio
at
ionn ar
io
aree co
comi
ming
mi
ng ffrom
rom
ro
m ei
eith
ther
th
er
CE-CMR
coming
either
ischemic heart disease or cardiomyopathies, with the notion the larger the LGE burden the worse
the prognosis. Our quantitative data suggest that the volume of LV scarred tissue in MVP is
relatively small but still associated with SCD.. We should recognize that MVP differs from other
non-valvular diseases in terms of LGE distribution (“stretched areas”) and amount. Furthermore,
the mechanical stretch by the prolapsing leaflet and elongated chordae could act as a trigger of
electrical instability. Further studies with higher number of MVP patients are needed to confirm
these preliminary data of LV LGE.
Since the early descriptions, abnormal LV contraction pattern and ECG abnormalities
13
DOI: 10.1161/CIRCULATIONAHA.115.016291
suggested that MVP has a significant myocardial involvement47-51. The hypothesis that the socalled “MVP syndrome” is a cardiomyopathy, where regional hypercontractility acts as the
primum movens of mitral valve geometry disruption, with abnormal tension on the chordae and
leaflets and secondary increase in myxomatous tissue and leaflet thickening, has been even
advanced50,51. Our pathology and CE-CMR data support the theory that LV abnormalities are
rather the consequence of MVP, due to a systolic mechanical stretch of the myocardium closely
linked to the valve, i.e. PMs and infero-basal wall, by the prolapsing leaflets and elongated
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
chordae, accounting for a localized hyper-contractility, with myocyte hypertrophy and injury
leading eventually to fibrous tissue repair. The increased cardiomyocyte diameter, in the same
areas showing replacement-type fibrosis, is in keeping with this theory.
Considering that performance of CE-CMR in all MVP patients would be an expensive
prop
pos
osit
itio
it
ion,
io
n, some
som
me clinical
c inical markers that could target
cl
targ
rget
rg
et a high-risk subgroup
subgrouup destined for screening
proposition,
by CE-CMR
by
CE-CMR are
arre needed.
need
eded
ed
ed.. ECG
ed
ECG depolarization
depol
epol
olar
arizzattio
ar
ionn abnormalities
abno
norrmal
alit
al
itie
it
iess on infero-lateral
ie
inffer
eroo latteraal leads,
olead
le
ads,
ad
s, complex
com
ompl
plex
pl
ex
ve
ent
ntri
r cular ar
ri
arrh
r ythmiaas ((
3 VPB
VPB
P run)
run
u ) with
with
h RBBB
RBBB
B morphology
morpphoology
mo
logy on
on 12-lead
122-lleaad ECG
EC Holter
Hollter
Ho
ventricular
arrhythmias
moni
mo
nito
ni
tori
to
ring
ri
ng and
and a hhistory
isto
is
tory
to
ry ooff pr
pre
e-sy
sync
ncop
nc
opee, syncope
op
sync
yn
ncop
opee an
andd ab
abor
orte
or
tedd SC
te
SCD
D se
seem
em tto
o re
repr
pres
pr
esen
es
entt an
en
monitoring
pre-syncope,
aborted
represent
indication for CE-CMR.
Finally, we recognize that our data support an association between anatomic substrate and
risk, in an entity that is underappreciated as a cause of SCD and also has a low enough incidence
that any marker of increased risk might be of significant value to the clinician.
Beta-blockers are commonly used to treat arrhythmias in MVP patients. The fact that
21% of young adult SCD victims and two living patients had aborted SCD despite beta-blocker
therapy is disappointing but not surprising10. Prospective multicenter studies are warranted to
support the role of CE-CMR and electrovoltage mapping for risk stratification and to assess the
14
DOI: 10.1161/CIRCULATIONAHA.115.016291
efficacy of antiarrhythmic therapy and targeted catheter ablation in selected cases.
Limitations of the study
While acknowledging the small number of MVP patients without complex ventricular
arrhythmias, we should recognize that it is difficult to collect “pure” MVP patients without either
valve incompetence or ventricular arrhythmias both clinically and at postmortem. Prospective
multicenter studies enrolling a higher number of MVP, with and without complex ventricular
arrhythmias, are warranted to evaluate the exact prevalence of LGE in the overall MVP
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
population.
Genetic data are not available in our SCD population. Noteworthy, in our series of SCD
(47%)
victims there was macroscopic evidence of myxomatous mitral valve and nearly half
hal
alff (4
(47%
7%)) ha
7%
had
a previous in vivo diagnosis of MVP, with a cardiological check-up ruling out channelopathies.
Moreover,
ECG,
revision
More
reov
re
over
ov
er,, the
er
the EC
CG,
G which was available for revi
visi
vi
sioon in 28%, did not sshow
si
how any evidence of
ho
long/short
MVP
ong
g/short QT or Brugada
Bru
uga
gada
da syndromes.
syn
yndr
drom
dr
omes
om
e . Of
Of the
the rremaining
emaain
nin
ng 31 M
VP ccases,
ases
as
es,, 225
es
5 ((80%)
80%)
80
%) hhad
a ffirstad
irst
st-st
degree
de
egr
gree
e family
famil
illy members
meemberrs referred
mem
refeerred
ed for
or cardiological
caarddiolog
ogiical screening,
og
sccreeening
ng, without
ng
wi ho
witho
hout
utt any
anny evidence
evi
vide
vi
deence of
channelopathies,
MVP
cases
(16%).
chan
ch
anne
an
nelo
ne
lopa
lo
path
pa
thie
th
iess, bbut
ie
utt M
VP iin
n 4 ca
case
sess (1
se
(16%
6%)).
6%
Although we are strong supporters of the relevance of molecular autopsy in the study of
SCD21,22, we follow the indication by the HRS/EHRA/APHRS expert consensus statement52.
According to these guidelines, an arrhythmia syndrome-focused postmortem genetic testing can
be useful for all sudden unexplained death syndrome victims as Class IIa indication; furthermore,
evaluation of first-degree blood relatives with resting ECG with high right ventricular leads,
exercise stress testing, and echocardiography is recommended as Class I.
Conclusions
This study suggests that MVP is a significant cause of SCD in young adults and is the leading
15
DOI: 10.1161/CIRCULATIONAHA.115.016291
one in women. Arrhythmic MVP patients are mostly female with ventricular arrhythmias of LV
origin and frequent repolarization abnormalities on inferior leads. The hallmark of arrhythmic
MVP is fibrosis of PMs and infero-basal LV free wall, which well correlates with arrhythmia
morphology, pointing to a myocardial stretch by the prolapsing leaflets and elongated chordae.
CE-CMR allows the identification of this arrhythmic substrate and is a promising non-invasive
tool for risk stratification and SCD prevention.
Funding Sources: This work was supported by the Registry of Cardio- Cerebro-Vascular
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Pathology, Veneto Region, Venice, Italy; Target Project “Sudden cardiac death in women”,
Regional Health System, Venice, Italy.
Conflict of Interest Disclosures: None.
References:
Re
efe
ferrences
re es
es::
11.. D
Delling
elling FN, V
Vasan
assan R
RS.
S. E
Epidemiology
pidemi
pid
mioolog
ol gy andd ppathophysiology
athopphys
ysiiolo
ys
ogy
y off m
mitral
itrall vvalve
alvve prola
prolapse:
laps
la
pse: ne
ps
new
ew
insights
molecular
basis.
Circulation.
nsiigh
g ts into disease
d seeasse progression,
di
progresssio
ion, genetics,
io
geene
neticcs, aand
ndd mo
oleecu
ula
larr ba
bas
sis. Ci
irculaatiionn. 22014;129:2158014;1229:21
211582170.
21
170
70.
22. Freed LA,
LA Levy D,
D Levine RA,
RA Larson MG,
MG Evans JC,
JC Fuller DL,
DL Lehman B,
B Benjamin EJ.
EJ
Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med. 1999;341:1–7.
3. Freed LA, Benjamin EJ, Levy D, Larson MG, Evans JC, Fuller DL, Lehman B, Levine RA.
Mitral valve prolapse in the general population: the benign nature of echocardiographic features
in the Framingham Heart Study. J Am Coll Cardiol. 2002;40:1298-1304.
4. Nishimura RA, McGoon MD, Shub C, Miller FA Jr, Ilstrup DM, Tajik AJ.
Echocardiographically documented mitral-valve prolapse. Long-term follow-up of 237 patients.
N Engl J Med. 1985;313:1305-1309.
5. Düren DR, Becker AE, Dunning AJ. Long-term follow-up of idiopathic mitral valve prolapse
in 300 patients: a prospective study. J Am Coll Cardiol. 1988;11:42-47.
6. Marks AR, Choong CY, Sanfilippo AJ, Ferré M, Weyman AE. Identification of high-risk and
low-risk subgroups of patients with mitral-valve prolapse. N Engl J Med. 1989;320:1031-1036.
7. Avierinos JF, Gersh BJ, Melton LJ III, Bailey KR, Shub C, Nishimura RA, Tajik AJ,
16
DOI: 10.1161/CIRCULATIONAHA.115.016291
Enriquez-Sarano M. Natural history of asymptomatic mitral valve prolapse in the community.
Circulation. 2002;106:1355-1361.
8. Davies MJ, Moore BP, Braimbridge MV. The floppy mitral valve. Study of incidence,
pathology, and complications in surgical, necropsy, and forensic material. Br Heart J.
1978;40:468-481.
9. Kligfield P, Levy D, Devereux RB, Savage DD. Arrhythmias and sudden death in mitral valve
prolapse. Am Heart J. 1987;113:1298-1307.
10. Vohra J, Sathe S, Warren R, Tatoulis J, Hunt D. Malignant ventricular arrhythmias in
patients with mitral valve prolapse and mild mitral regurgitation. Pacing Clin Electrophysiol.
1993;16:387-393.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
11. Jeresaty RM. The syndrome associated with mid-systolic click and-or late systolic murmur.
Analysis of 32 cases. Chest. 1971;59:643-647.
12. Shappell SD, Marshall CE, Brown RE, Bruce TA. Sudden death and the familiall occurrence
1973;48:1128-1134.
of mid-systolic click, late systolic murmur syndrome. Circulation. 1973;48:1128-11
1134
34..
34
13. Bharati S, Granston AS, Liebson PR, Loeb HS, Rosen KM, Lev M. The conduction system
in
n mitral valve prolapse syndrome with sudden death. Am Heart J. 1981;101:667-670.
14.
Chesler
E,, King RA, Edwards JE. The myxoma
myxomatous
valve
14
4. C
hesler E
matous mitral va
ma
alv
lve and sudden death.
Circulation.
C
irc
rculation. 1983;67:632-639.
rc
198
983;
98
3;677:6
:632
32-6
32
-639
-6
39
9.
15.
WA,
Bosman
CK,
Chesler
Barlow
JB,
Edwards
JE.
Sudden
15
5. Pocock
Po
W
A,, B
osma
man CK
ma
K, Ch
C
esle
es
l r E,
E, Ba
arllow JB
B, Ed
Edwa
ard
rds JE
E. Su
udd
den ddeath
eath
ea
t inn pprimary
rim
mary
prolapse.
1984;107:378-382.
mitral
al vvalve
alvve
al
ve pro
ola
laps
pse.
se Am
m Heart
Hea
art J.
J. 1984;
4;10
4;
107:
10
7:37
7:
37837
8 382.
38
82
16. Dollar AL, Roberts WC. Morphologic comparison of patients with mitral valve prolapse who
died suddenly with patients who died from severe valvular dysfunction or other conditions. J Am
Coll Cardiol. 1991;17:921-931.
17. Farb A, Tang AL, Atkinson JB, McCarthy WF, Virmani R. Comparison of cardiac findings
in patients with mitral valve prolapse who die suddenly to those who have congestive heart
failure from mitral regurgitation and to those with fatal noncardiac conditions. Am J Cardiol.
1992 ;70:234-239.
18. Morales AR, Romanelli R, Boucek RJ, Tate LG, Alvarez RT, Davis JT. Myxoid heart
disease: an assessment of extravalvular cardiac pathology in severe mitral valve prolapse. Hum
Pathol. 1992;23:129-137.
19. Burke AP, Farb A, Tang A, Smialek J, Virmani R. Fibromuscular dysplasia of small
coronary arteries and fibrosis in the basilar ventricular septum in mitral valve prolapse. Am Heart
J.1997;134:282-291.
17
DOI: 10.1161/CIRCULATIONAHA.115.016291
20. Corrado D, Basso C, Nava A, Rossi L, Thiene G. Sudden death in young people with
apparently isolated mitral valve prolapse. G Ital Cardiol. 1997;27:1097-1105.
21. Basso C, Burke M, Fornes P, Gallagher PJ, de Gouveia RH, Sheppard M, Thiene G, van der
Wal A; Guidelines for autopsy investigation of sudden cardiac death. Association for European
Cardiovascular Pathology.Virchows Arch. 2008;452:11-18.
22. Basso C, Calabrese F, Corrado D, Thiene G. Postmortem diagnosis in sudden cardiac death
victims: macroscopic, microscopic and molecular findings. Cardiovasc Res. 2001;50:290-300.
23. Levine RA, Stathogiannis E, Newell JB, Harrigan P, Weyman AE. Reconsideration of
echocardiographic standards for mitral valve prolapse: lack of association between leaflet
displacement isolated to the apical four chamber view and independent echocardiographic
evidence of abnormality. J Am Coll Cardiol. 1988;11:1010-1019.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
24. Han Y, Peters DC, Salton CJ, Bzymek D, Nezafat R, Goddu B, Kissinger KV, Zimetbaum
PJ, Manning WJ, Yeon SB. Cardiovascular magnetic resonance characterization of mitral valve
prolapse. JACC Cardiovasc Imaging. 2008;1:294
2008;1:294-303.
303.
25. Perazzolo Marra M, De Lazzari M, Zorzi A, Migliore F, Zilio F, Calore C, Vettor
Vet
etto
et
torr G, Tona
to
Ton
onaa F,
Tarantini G, Cacciavillani L, Corbetti F, Giorgi B, Miotto D, Thiene G, Basso C, Iliceto S,
Corrado D. Impact of the presence and amount of myocardial fibrosis by cardiac magnetic
resonance
esoona
nanc
ncee on arrhythmic
nc
arrrhy
hythmic outcome and sudden cardiac
caard
rdia
i c death in non ischemic
ische
hemi
he
m c dilated
cardiomyopathy.
caard
rdiiomyopat
io
athy. Heart Rhythm.
at
Rhyt
y hm. 2014;11:856-863.
2014;11:856-863
3.
26.
Kelly
KL,
Titus
Sudden
with
apparently
normal
heart.
2 . Chugh SS, K
26
ellly KL
K
L, Ti
itu
tus JL. Sudd
dden ccardiac
arrdiaac ddeath
eath
th w
ithh ap
ppaarenttly
y no
orm
mal he
hea
ar
art.
Circulation.
Circ
Ci
rcul
rc
u ation.. 22000;102:649-654.
00
00;
0;1022:6649-66544.
4.
27.
27 Topaz
Topa
To
paz O,
pa
O, Edwards
Edw
dwar
ards
ar
ds JE.
JE. Pathologic
Pat
atho
holo
ho
logi
lo
gicc features
gi
feat
fe
atur
at
ures
res of
of sudden
sudde
ud
dde
denn death
deat
de
athh in children,
at
chi
hild
ldre
ld
renn, adolescents,
re
ado
dole
lesc
le
scen
sc
ents
en
ts, and
ts
and
young adults. Chest. 1985;87:476-482.
28. Campbell RW, Godman MG, Fiddler GI, Marquis RM, Julian DG. Ventricular arrhythmias
in syndrome of balloon deformity of mitral valve. Definition of possible high risk group. Br
Heart J. 1976;38:1053-1057.
29. De Maria AN, Amsterdam EA, Vismara LA, Neumann A, Mason DT. Arrhythmias in the
mitral valve prolapse syndrome. Ann Intern Med. 1976;84:656-660.
30. Winkle RA, Lopes MG, Popp RL, Hancock EW. Life-threatening arrhythmias in the mitral
valve prolapse syndrome. Am J Med. 1976;60:961-967.
31. Levy S. Arrhythmias in the mitral valve prolapse syndrome: clinical significance and
management. Pacing Clin Electrophysiol. 1992;15:1080-1088.
32. Morady F, Shen E, Bhandari A, Schwartz A, Scheinman MM. Programmed ventricular
stimulation in mitral valve prolapse: analysis of 36 patients. Am J Cardiol. 1984;53:135-138.
18
DOI: 10.1161/CIRCULATIONAHA.115.016291
33. Sanfilippo AJ, Abdollah H, Burggraf GW. Quantitation and significance of systolic mitral
leaflet displacement in mitral valve prolapse Am J Cardiol. 1989;64:1349-1355.
34. Kulan K, Komsuo÷lu B, Tuncer C, Kulan C. Significance of QT dispersion on ventricular
arrhythmias in mitral valve prolapse. Int J Cardiol. 1996;54:251-257.
35. Devereux RB, Kramer-Fox R, Shear MK, Kligfield P, Pini R, Savage DD. Diagnosis and
classification of severity of mitral valve prolapse: methodologic, biologic, and prognostic
considerations. Am Heart J. 1987;113:1265-1280.
36. Lichstein E. Site of origin of ventricular premature beats in patients with mitral valve
prolapse. Am Heart J. 1980;100:450-457.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
37. Sriram CS, Syed FF, Ferguson ME, Johnson JN, Enriquez-Sarano M, Cetta F, Cannon BC,
Asirvatham SJ, Ackerman MJ. Malignant bileaflet mitral valve prolapse syndrome in patients
with otherwise idiopathic out-of-hospital cardiac arrest. J Am Coll Cardiol. 2013;62:222-230.
Kramer-Fox
Natural
38. Zuppiroli A, Rinaldi M, Kramer
Fox R, Favilli S, Roman MJ, Devereux RB. Nat
tur
u al history
of mitral valve prolapse. Am J Cardiol. 1995;75:1028-1032.
39. Cobbs BW Jr, King SB 3rd. Ventricular buckling: a ffactor in the abnormal ventriculogram
and peculiar hemodynamics associated with mitral valve prolapse. Am Heart J. 1977;93:741758..
440.
0. Salazar AE,
AE
E, Edwards
Edwa
Ed
ward
wa
rdss JE.
rd
JE. Friction
Fric
Fr
icti
ic
tioon lesions
ti
lessionns of
of ventricular
veentricu
cula
cu
larr endocardium.
la
end
ndoc
o ar
ardi
dium
di
um. Relation
um
Reela
lati
tion
ti
on to
to chordae
chorrda
ch
daee
tendineae
mitral
valve.
Arch
Pathol.
enddineae of mitra
r l va
ra
alv
lve. Ar
rch
h Pathol
l. 11970;90:364-376.
9700;990:364
4-376
76..
76
Barlow
Bosman
leaflet
mitral
valve.
41. Ba
Barl
rlow
rl
ow JB, B
ossma
mann CK.
C . Aneurysmal
CK
Aneu
An
eurysm
eu
mal protrusion
pro
rotr
trus
tr
ussion
ion off tthe
he pposterior
osteri
rioor
ri
or le
eaf
afle
lett off tthe
le
he m
itra
rall valv
ra
va
alv
lvee.
Heart
An aauscultatory-electrocardiographic
usscult
uscu
ltat
lt
ator
at
ory-el
or
elec
el
ectr
ec
troc
tr
ocar
oc
ardi
ar
diog
di
ogra
og
raph
ra
phic
ph
ic ssyndrome.
ynndr
yndr
drom
omee. Am
om
Am H
eart
rtt JJ.. 11966;71:166-178.
966;
96
6;71
6;
71:1
71
:166
:1
66-178
178
78.
42. Boudoulas H, Kolibash AJ, Baker P, King BD, Wooley CF. Mitral valve prolapse and the
mitral valve prolapse syndrome: a diagnostic classification and pathogenesis of symptoms. Am
Heart J. 1989;118:796-818.
43. Mason JW, Koch FH, Billingham ME, Winkle RA. Cardiac biopsy evidence for a
cardiomyopathy associated with symptomatic mitral valve prolapse. Am J Cardiol. 1978;42:557562.
44. Jeresaty RM. Sudden death in the mitral valve prolapse-click syndrome. Am J Cardiol.
1976;37:317-318.
45. Wilde AA, Düren DR, Hauer RN, deBakker JM, Bakker PF, Becker AE, Janse MJ. Mitral
valve prolapse and ventricular arrhythmias: observations in a patient with a 20-year history. J
Cardiovasc Electrophysiol. 1997;8:307-316.
46. John BT, Tamarappoo BK, Titus JL, Edwards WD, Shen WK, Chugh SS. Global remodeling
19
DOI: 10.1161/CIRCULATIONAHA.115.016291
of the ventricular interstitium in idiopathic myocardial fibrosis and sudden cardiac death. Heart
Rhythm. 2004;1:141-149.
47. Hancock EW, Cohn K. The syndrome associated with midsystolic click and late systolic
murmur. Am J Med. 1966;41:183-196.
48. Scampardonis G, Yang SS, Maranhão V, Goldberg H, Gooch AS. Left ventricular
abnormalities in prolapsed mitral leaflet syndrome. Review of eighty-seven cases. Circulation.
1973;48:287-297.
49. Rizzon P, Biasco G, Brindicci G, Mauro F. Familial syndrome of midsystolic click and late
systolic murmur. Br Heart J. 1973;35:245-259.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
50. Gulotta SJ, Gulco L, Padmanabhan V, Miller S. The syndrome of systolic click, murmur,
and mitral valve prolapse--a cardiomyopathy? Circulation. 1974;49:717-728.
51. Crawford MH, O'Rourke RA. Mitral valve prolapse: a cardiomyopathic state? Prog
1984;27:133-139.
Cardiovasc Dis. 1984;27:133
139.
52. Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, Blom N, Brugada J,
J, Chiang
Chia
Ch
iang
ia
ng CE,
CE,
Huikuri H, Kannankeril P, Krahn A, Leenhardt A, Moss A, Schwartz PJ, Shimizu W, Tomaselli
G, Tracy C. Executive summary: HRS/EHRA/APHRS expert consensus statement on the
diagnosis
management
inherited
arrhythmia
diag
gno
nosi
siss an
si
andd ma
anagement
na
of patients with inher
erit
er
ited
it
e primary arrhythmi
miaa syndromes. Heart
mi
Rhythm.
2013;10:e85-108.
Rh
hyt
ythhm. 201
0113;10:e85-108.
20
DOI: 10.1161/CIRCULATIONAHA.115.016291
Table 1. Clinical and pathologic features of 43 patients who died suddenly with MVP due to
myxomatous degeneration.
Variables
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Age, years median (range)
Female, n (%)
Athletes, n (%)
Marfan stigmata, n (%)
Pectus excavatum, n (%)
Pregnancy, n (%)
Circumstances of SCD, n (%)
- on emotion/effort
- at rest
- during sleep
12 lead ECG available, n (%)
nverted/biphasic T wave D2, D3, aVF n (%)
Inverted/biphasic
VAs, n (%)
VAs morphology, n (%)
- RBBB
- LBBB
Be
Beta-blocker
eta
ta-b
-blo
-b
lock
lo
cker
ck
er the
therapy,
era
rappy, n (%)
G
Gross
rooss featur
features
res
H
eart weight (g)
), m
eaan ±
SD
D*
Heart
(g),
mean
±SD*
LV w
all thickness
thicckn
k esss (mm)
m), me
ean
n±SD
D
wall
(mm),
mean±SD
VS
S thickness
thi
hick
ckne
ck
nesss (mm),
ne
(mm
mm),
) m
),
eaan SD
ean±
D
mean±SD
Pate
Pa
Patent
tent
te
nt foramen
for
oram
amen
am
en oovale,
vale
va
le, n (%
le
(%)*
)*
O
Ovall ffossa aneurysm, n (%)
Posterior MVP, n (%)
Bileaflet MVP, n (%)
Endocardial fibrous plaque, n (%)
Histology features
LV scar
- papillary muscles, n (%)
-infero-basal wall, n (%)
Fibrous tissue /myocardium (% area)
- papillary muscles, mean ± SD†
- infero-basal wall, mean ± SD†
Cardiomyocytes diameter (μm), mean± SD†
SCD due to MVP
43 patients
32 (19-40)
26 (61)
4 (9)
2 (5)
2 (5)
2/26 (8)
Control
15 patients
30 (18-40)
10 (67)
2 (13)
0
0
1/10
p
0.33
0.7
1.0
1.0
1.0
1.0
8 (19)
30 (70)
5 (12)
12 (28)
10 (83)
12 (28)
4 (27)
9 (60)
2 (13)
5 (33)
0
0
1.0
1.0
1.0
-
12 (100)
8 (67)
9 (21)
0
0
0
-
357±
35
7±
±53
3
357±53
12
.6±
6±1..3
12.6±1.3
13
.0±0
.0
0±0.88
13.0±0.8
25 ((58)
58))
58
10 (23)
13 (30)
30 (70)
25 (58)
323
23±
23
± 42
323±42
12.
.5±
±3.6
12.5±3.6
112.57±0.7
2 577±0
2.
±0.7
.7
4 (2
(27)
7)
1 (6)
0
0
0
00.02
.02
2
0.9
00.08
.008
00.04
.04
04
00.25
25
-
43 (100)
38 (88)
0
0
-
30.5±10.7
33.1±7.6
19.2±6.0
6.3±1.6
6.4±1.4
12.8±0.4
<0.0001
<0.0001
<0.0001
Abbreviations: LV= Left ventricle; MVP= mitral valve prolapse; RBBB= right bundle branch block; SCD= sudden
cardiac death; VAs= ventricular arrhythmias; VS= ventricular septum.
21
DOI: 10.1161/CIRCULATIONAHA.115.016291
Table 2. Clinical, ECG and CMR features of 44 patients with MVP.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Variables
Age, years median (range)
Female, n (%)
Symptoms, n (%)
- aborted SCD
- palpitations
tations
- syncope
ope
- chest pain
- dyspnea
nea
Therapy, n (%)
Beta-blockers
-blockers
Sotalol
lol
Otherr antiarrhythmic
anti
tiar
arrh
ar
rhyt
rh
ythm
yt
hmic
hm
ic
ICD
G
12 lead ECG
Inverted/biphasic
pha
h sic
ic T wave, n (%)
D , aV
D3
aaVF
F
- D2, D3,
- D1, aV
aVL
V
QTc duration,
n, msec
se
onit
on
itor
it
orin
or
ingg
in
ECG-Holterr m
monitoring
VPB,, n (%)
- Bigeminal
mina
mi
nall VP
na
VPB
B
- NSVT,
T n (%)
SVT, n (%)
VF, n (%)
CVAs morphology, n (%)
- LBBB inferior axis
- LBBB superior axis
- RBBB inferior axis
- RBBB superior axis
CMR Morpho-functional
Findings
LV EDV, ml/m2
LV EF, %
MVP
with
Complex VA
30 pts
Complex
VA
>3 VPB run
10 pts
Complex
VA
=3 VPB run
20 pts
MVP
without
Complex VA
14 pts
41 (28-43)
22 (73)
37 (32-43)
9 (90)
44 (36-52)
13 (65)
51 (24-64)
7 (50)
3VPB
vs
without
Complex VA
0.44
0.18
2 ((7))
15 (50)
2 (7)
2 (7)
2 (7)
2 (20)
( )
7 (70)
2 (20)
0
1 (10)
0
8 (40)
0
2 (10)
1 (5)
0
5 (36)
0
1 (7)
1 (7)
0.52
1.00
1.00
1.00
0.21
1.63
1.00
1.00
1.00
1.00
1.00
1.00
1.00
0.24
0.10
0.54
1.00
13 (43)
3 (10)
1 (3)
3 (10)
5 (50)
1 (10)
1 (10)
3 (100)
8 (40)
2 (10)
0
0
6 (43)
0
1 (7)
0
1.00
0.54
0.54
-
1.00
0.42
1.00
-
1.00
0.50
0.41
-
0.71
1.00
0.33
-
100 (33)
(33
3 )
9 (30)
0
2 (7)
7)
4423
23
3 (409(409-440)
9 440)
4
5 (50)
50
4 (40)
0)
2 (20)
4439
39
9 ((420-446)
420-44
446)
44
5
5 (25)
5
5 (25)
0
420 ((409-431)
4 940
9 431)
( 1))
(2
3 (21)
( 4)
(1
2 (14)
(7)
1 (7)
4412
12
2 (39
(394-432)
3 4-43
4 2))
0.55
0.5
0.46
1.00
0.19
0.220
0.
0.20
0 19
0.
0.19
0 55
0.
0.55
00.15
0.
15
00
1.00
0.67
0.41
00.34
.34
0.23
0.43
0.10
0.18
30 (100)
11 ((37)
37))
37
27 (90)
1 (3)
2 (7)
100 ((100)
100)
5 (5
(50)
0)
7 (70)
1 (10)
2 (20)
20 (1
((100)
00)
6 ((30)
30))
30
20 (100)
0
0
8 (57)
3 (2
(21)
1)
0
0
0
<0.01
00.49
.49
49
-
0.022
00.20
.20
20
-
<0.01
00.70
.70
70
-
0.43
-
0
1 (3)
13 (43)
26 (87)
0
0
7 (70)
10 (100)
0
1 (5)
5 (25)
16 (80)
0
0
0
0
-
-
-
1.00
0.05
0.27
91 (89-103)
64 (60-65)
91 (91-94)
63 (59-65)
91 (89-108)
64 (59-65)
91 (83-91)
66 (64-69)
0.13
<0.01
0.24
<0.01
0.18
0.01
0.91
0.68
22
p Value
> 3VBP
=3VPB
vs
vs
without
without
Complex VA Complex VA
0.40
0.59
0.08
0.49
>3VPB
vs
= 3 VPB
0.27
0.21
DOI: 10.1161/CIRCULATIONAHA.115.016291
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
LV mass, gr/m2
RV EDV, ml/m2
RV EF, %
Posterior MVP, n (%)
Bileaflet MVP, n (%)
Lengths MV leaflets, mm
- Anterior
- Posterior
Prolapse distance, mm
- Anterior leaflet
- Posterior leaflet
contrast Findings
CMR Post-contrast
LV LGE
- papillary
lary muscles
- infero-basal
o-basal wall
mount (%)
LV LGE amount
62 (60-63)
77 (71-79)
64 (61-66)
9 (30)
21 (70)
62 (59-74)
77 (71-79)
65 (62-69)
5 (50)
5 (50)
62 (60-63)
77 (75-81)
64 (62-65)
4 (20)
16 (80)
63 (49-63)
77 (76-78)
64 (64-66)
9 (64)
5 (36)
20.7 (19.3-26.0) 20.1 (18.5-28.0) 22.1 (20.0-25.0) 20.0 (17.0-25.0)
16.0 (12.6-18.0) 14.0 (11.0-17.7) 16.3 (13.0-19.7) 11.4 (9.5-14.0)
0.48
0.35
0.43
0.05
0.05
0.55
0.51
0.93
0.68
0.68
0.57
0.39
0.27
0.01
0.01
0.75
0.91
0.31
0.12
0.12
0.32
0.02
0.51
0.26
0.34
0.01
0.65
0.27
5.1 (1.7-8.0)
7.8 (4.0-11.8)
3.3 (0-7.0)
4.5 (2.7-7.5)
5.6 (3.9-8.0)
10 (5.5-12.9)
1.3 (0-3.0)
2.1 (2.0-3.5)
0.01
<0.01
0.47
0.11
<0.01
<0.01
0.12
<0.01
28 (93)
25 (83)
22 (73)
1.2 (0.8-2.1)
10 (100)
10 (100)
7 (70)
1.1 (0.9-2.7)
18 (90)
15 (75)
15 (75)
1.4 (0.7-2.1)
2 (14)
2 (14)
1 (7)
0
<0.01
<0.01
<0.01
<0.01
<0.01
<0.01
<0.01
<0.01
<0.01
<0.0
<0
.01
01
<0.01
<0.0
<0
.011
.0
01
<0.01
<0
<0.01
0.54
0.14
1.00
0.96
Abbreviations:
s: CMR=cardiac magnetic resonance; VA= ventricular arrhythmias; EDV = End-Diastolic Volume; EF= Ejection Fraction; ICD = Implantable cardioverter defibrillator;
defibrillat LGE=
late gadolinium
corrected;
um enhancement; LBBB= left bundle branch block; LV= Left Ventricle;MVP= mitral valve prolapse; NSVT = non-sustained ventricular tachycardia; QTc = QT corre
RBBB= right bundle branch block; RV= right
rig
ight ventricle; SCD= sudden cardiac death; SVT= sustaine
sustained
ned ventricular tachycardia; VPB=ve
ne
VPB=ventricular
ent
n ricular premature beats; VF = ventricular fibrillation.
Categorical variables
ariab
ble
less ar
aree pr
pres
presented
esen
es
ente
en
tedd as num
te
number
u be
b r of patients (%). Continuous values are express
expressed
ed
d aass me
m
median
dian with 25% and 75%-iles.
23
DOI: 10.1161/CIRCULATIONAHA.115.016291
Figure Legends:
Figure 1. SCD in a 36 years old woman with in vivo diagnosis of MVP. A,B) 12-lead basal ECG
at the time of emergency department admission for palpitations. Single and coupled VPBs with
RBBB morphology are present; note the negative T wave on the inferior leads. At 24 hour
Holter-ECG (B) NSVT is also recorded; C) At gross examination, myxomatous degeneration of
both leaflets of the mitral valve with elongated chordae is visible; D, E). At histology, severe
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
myxoid thickening of the posterior mitral valve leaflet and myocardial fibrosis of the LV inferobasal wall (D) and PM (E).
Figure 2.Histology of three representative SCD cases with MVP. Myocardial scarring is visible
underneath
mitral
at the
hee level
lev
evel
el ooff thee in
iinfero-basal
fero-basal LV free wall, unde
dern
de
rneath the posterior m
rn
itra
it
r l valve leaflet (A,B,C)
and
and of the PMss plus
plu
us adjacent
adja
ad
jace
ace
cent
nt free
freee wall
wal
alll (D,E,F).
(D
D,E
E,F
,F)). Close-up
Clo
ose-u
-u
up of the
t e scarring
th
s ar
sc
arri
ring
ri
ng aareas
reas
as sshowing
howi
ho
wing
wi
ng eendondond
operimysial
replacement-type
fibrosis
with
cardiomyocytes
peeri
r mysial
my
aand
n ppatchy
nd
attchyy re
eplaccem
mentt-ttyppe fib
tbrossis w
itth iinterspersed
nterssper
nt
erse
er
seed ca
ard
r io
iomy
myoc
my
ocyt
oc
y ess ((G,H,I).
G,H
H,II).
Figure 3. CMR post-contrast sequences findings in MVP patients with complex ventricular
arrhythmias and aborted SCD. A,B) A30 years old woman with MVP and complex ventricular
arrhythmias. LGE of the PM is visible on mid-short axis view (A). The 12 lead ECG (B) shows
the presence of NSVT with RBBB morphology originating from the posterior PM (superior
axis). C,D) A 33 years old woman with MVP and complex ventricular arrhythmias. LGE of the
LV infero-basal region, underneath the posterior valve leaflet, with endocardial-midmural
extension, is visible on 3-chamber long axis view (C). The 12 lead ECG demonstrates NSVT
with RBBB morphology originating from the LV infero-basal wall near the mitral annulus
24
DOI: 10.1161/CIRCULATIONAHA.115.016291
(inferior axis) (D). E, F) A 38 years old man with MVP and aborted SCD. CMR, performed 6
months before cardiac arrest, shows LGE in the infero-basal region of the LV on long-axis view
(E). ECG recording of polymorphic SVT degenerating into VF (F).
Figure 4. A 34 year old woman with pre-syncopal episodes despite antiarrhythmic drug therapy.
A) Basal ECG shows isolated VPBs with two RBBB morphologies, indicating a LV origin from
the PMs and the infero-basal wall close to the mitral anulus. B,C) Electro-physiologic study
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
with programmed stimulation and induction of sustained VT with the same morphology of VPBs
originating from the posterior mitral annulus, terminated by electrical cardioversion. D) On CECMR, LGE at the level of the LV infero-basal wall is visible.
25
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Figure 1
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Figure 2
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Figure 3
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Figure 4
Arrhythmic Mitral Valve Prolapse and Sudden Cardiac Death
Cristina Basso, Martina Perazzolo Marra, Stefania Rizzo, Manuel De Lazzari, Benedetta Giorgi,
Alberto Cipriani, Anna Chiara Frigo, Ilaria Rigato, Federico Migliore, Kalliopi Pilichou, Emanuele
Bertaglia, Luisa Cacciavillani, Barbara Bauce, Domenico Corrado, Gaetano Thiene and Sabino Iliceto
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Circulation. published online July 9, 2015;
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2015 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circ.ahajournals.org/content/early/2015/07/09/CIRCULATIONAHA.115.016291
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click Request
Permissions in the middle column of the Web page under Services. Further information about this process is
available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/