15th July 2015
advertisement

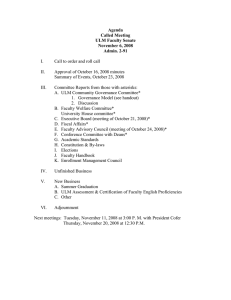
Meeting Notes Meeting Name: Wirral Drug & Therapeutics Panel Date: Wednesday 15th July 2015 Location: Under Grad Centre, APH Present: Dr M Van Miert (MVM) Dr S Jalan (SJ) Mrs M Charlton (MC) Mrs K Herbert (KH) Dr M George (MG) Dr F Newton (FN) Dr B Hammer (BH) Mrs R Pugh (RP) Mrs H Hurley (HH) Mr S Riley (SR) Mrs J Edwards (JE) Mrs L Ormson (LO) Consultant Anaesthetist, WUTH (Chair) GP, NHS Wirral (Vice Chair) Lead Pharmacist Medicines Management, WUTH (Secretary) Team Leader, Pharmacy Clinical Support Services, WUTH Consultant Rheumatologist, WUTH GP Partner, Wirral LMC Consultant Haematologist, WUTH (left the meeting @ 1.35pm) Prescribing Advisor, NHS Wirral Finance Dept, WUTH Senior Prescribing Advisor, NHS Wirral Trust Pharmacist, Wirral Community Trust Deputy Associate Director Nursing Surgery, Women & Children, WUTH Attending: Mrs Lin Miller Dr K Joseph (KJ) Dr A Jayachandran (AJ) Dr K S Leong (KSL) Mr L Jarvis Secretary, WUTH Acute Medicine Consultant (WUTH) Acute Medicine Consultant (WUTH) Consultant Physician (WUTH) Observer, Pharmacy Department Agenda Item 50/15 | Apologies Apologies received: Dr J Cunniffe, Dr E Sim, Mrs A Rowlands, Ms M Carroll, Mrs N Holder Not present no apology sent: Ms S Mwenechanya, Dr A Hughes Agenda Item 51/15 | Conflicts of Interest Omalizumab-Novartis Fondaparinux-Aspen Toujeo-Sanofi Empagliflozin-Boehringer No other conflicts of interest were declared Agenda Item 52/15 | Minutes of Previous Meeting Initials incorrect in items 39/15.02 and 39/15.03 and 39/15.04 DG changed to RD (Dr R Dasgupta). 37/15.02 - MVM raised concern regarding the difficulties caused by tramadol now being classed as a schedule 3 CD which means that it is now stored in CD cupboards in the Trust. This is causing delays in patients receiving tramadol due to it having to be signed out the CD cupboard by 2 trained staff. MC advised that he should raise his concerns with Pippa Roberts who is the Accountable Officer for CDs for WUTH. Noted Page 1 of 6 Agenda Item 53/15 | Matters arising Alteplase infusion for the treatment of blocked dialysis catheters. Additional information requested from Dr Banerjee for application presented at WDTP in March 2015. The Panel discussed the report sent by Dr Banerjee. The Panel felt that it was still unclear how many times a patient could receive an alteplase infusion and that it should be limited to 2. The Panel also discussed that they would like to see how successful the infusions are in practice so requested that Dr Banerjee should report back its impact in 6 months. Decision: To report back in 6 months further findings and to limit the treatment to 2 infusions per patient Agenda Item 54/15 | Medicines Management Policies & Procedures 54/15.01 – Clinical Trials Policy - Policy review. No change to practice. One sentence has changed in this policy in definitions - Principal investigator changed from ‘the investigator is the responsible leader of the team’ to ‘the principal investigator has overall responsibility as leader of the team’. KH had also asked author for clarification under section 4.1 Clinical trial initiation-The Lead Clinical trials Pharmacist can refuse to authorise a Clinical Trial if: ‘the arrangements for continuation of access to the medicine once the trial has finished are satisfactory’ to add ‘e.g. patient must be informed that medicines may not continue after trial has ended. Approved 54/15.02 – Unlicensed Medicines Policy – Amendments made by: Sarah Hulse, Team Leader, Pharmacy Clinical Support Services List of amendments to this Policy 1.Link to statement on use of ULM in paediatrics. Clarification of special clinical need. Hierarchy of ULM. 3 ‘Off- label’ medicines excluded from policy. 4. Consent/patient information updated Link to paediatric patient information leaflet 5 Requests and approval sections updated Only Requests >£5000 need Divisional sign off. Director of Pharmacy can approve ULM requests for supply problems with licensed products Weekend and out-of hour’s requests for new ULM 6. Risk assessment of new ULM -new process and section updated 7 Supply ULM updated 8 Duties/Responsibilities updated. Role change for Trust Designated Pharmacist. Clarification of eligible prescribers. Pharmacy procurement added 9 Monitoring and review updated 12 ADRs and defective products updated Appendix A Hierarchy of use of ULM added Appendix B New ULM patient information leaflet Appendix C Flow chart for requesting ULM added Appendix D ULM request form updated Appendix E New ULM risk assessment Appendix F Supply Instructions for GP/community pharmacist updated Following sections removed: -Definitions -Liabilities -Funding -Continuing supplies of ULMs MC stated that this policy had come to the meeting as it was due for review and highlighted the important changes: Page 2 of 6 Added in that policy does not cover off-label use of medicines 4.1 consent-added that not necessary to document consent unless prescriber has reason to believe that consent may be disputed later Trust generic patient information leaflet regarding unlicensed medicines has been updated If an unlicensed medicine is classed as high risk then an unlicensed medicines request form is required each time a consultant wishes to start medicine in new patient Requests for use of new unlicensed medicine for supply problems with licensed medicines can be approved by the Director of Pharmacy Process of risk assessing unlicensed medicines has changed Approved 54/15.03 – Oxygen Therapy – 45g PCIS has been replaced throughout with ‘electronic prescribing system’ The Panel noted the minor change to this policy. Approved Agenda Item 55/15 | Reports back None Agenda Item 56/15 | New Medicine requests 56/15.01 – Omalizumab for urticarial NICE TA 339 Author: Dr S White, Consultant Dermatologist, WUTH Omalizumab (Xolair) is recommended as a possible treatment for people aged 12 years and over with severe chronic spontaneous urticaria if: a doctor has objectively diagnosed the condition as severe the condition has not improved with standard treatment with H1 antihistamines or leukotriene receptor antagonists the drug is stopped at or before the fourth dose if the condition has not responded the drug is stopped at the end of a course of treatment (6 doses) if the condition has responded, and is only restarted if the condition comes back the drug is given by a secondary care specialist in dermatology, immunology or allergy. Decision: Approved 56/15.02 – Fondaparinux for superficial vein thrombosis Author: Dr A Jayachandran & Dr K Joseph – Acute Medicine Consultants, WUTH KJ presented the application for fondaparinux as a treatment of intermediate risk superficial vein thrombosis (SVT) with fondapariunx for 45 days. KJ further explained that SVT was once considered to be a benign and self-limiting condition. However, it is now appreciated that a significant proportion of those presenting with superficial vein thrombosis will have concomitant deep vein thrombosis or pulmonary embolism, or are at significant risk of developing deep venous thromboembolism. KJ stated that currently these patients don’t receive any treatment. MVM did not feel that the application demonstrated the benefits of this treatment because the studies showed that you need to treat 88 patients to prevent one VTE. As the paper predicts they will treat 40-50 patients per year so it would take approximately 2 years to gain any benefits from this treatment at a cost of £17k per annum. The Panel discussed this application more fully and agreed that as patients currently don’t receive any treatment then this is a new treatment pathway. Therefore the approval and commissioning of the new pathway would have to be carried out before the Panel could consider the application. The proposed Page 3 of 6 pathway would also have an impact on District Nurses as they would need to administer fondapariunx after the patient has been discharged Decision: Not approved RAG Status: RED 56/15.03 – Insulin Glargine 300units/ml (high strength) Author: Dr K S Leong, Consultant Physician, WUTH Insulin glargine U300 (Toujeo®) is a new formulation based on the insulin glargine molecule, but with a reduced redissolution rate following subcutaneous administration, resulting in a flatter and more prolonged pharmacokinetic/dynamic profile than Lantus® (Insulin glargine U100). Toujeo and Lantus are not bioequivalent and are therefore not interchangeable without dose adjustments. It offers specific hypoglycaemia and insulin dose volume benefits. KSL presented the application for Insulin Glargine 300units/ml (high strength) to the Panel. KSL explained that patients with Type 2 diabetes can have nocturnal hypoglycaemic episodes, which most patients would be unaware they are experiencing. KSL stated that the incidence of nocturnal hypoglycaemia with Glargine 300units/ml was lower in the clinical trials. He also stated that as the volume injected was less this may benefit patients who suffer from injection site reactions. The lower volume is also useful in patients with limited manual dexterity as there is less resistance when injection smaller volumes. The Panel discussed KSL’s application at length and although evidence did not highlight any significant advantages over the insulins already on the formulary, they agreed that they could see the benefits in certain groups of patients. It has a lower acquisition cost to Tresiba and has been positioned 2nd line before Tresiba (insulin degludec) so is more cost effective. The panel also discussed the risks involved with introducing higher strength insulin on to the formulary and agreed that KSL should provide a risk minimisation strategy to the panel prior to the introduction of Toujeo on to the formulary. Decision: Approved pending risk minimisation strategy RAG Status: AMBER 56/15.04 – Empagliflozin NICE TA 336 Author: Dr K S Leong, Consultant Physician, WUTH As per NICE TA336 Empagliflozin is recommended as a treatment for type 2 diabetes when taken with metformin, only if the person: cannot take sulfonylurea or is at significant risk of hypoglycaemia or its consequences. If a person needs to take 3 antidiabetic drugs, empagliflozin is recommended as a treatment for type 2 diabetes when taken with either metformin and a sulfonylurea, or with metformin and a thiazolidinedione. Empagliflozin is also recommended as a treatment for type 2 diabetes when taken with insulin, with or without other antidiabetic drugs. Decision: Approved Action: Guidelines to be updated RAG Status: GREEN Agenda Item 57/15 | Chairs Actions There were 3 ‘Chairs Actions’ for July: Dr Banerjee – alteplase injection Dr Hammer – Eltrombopag Dr Galvani – Eltrombopag MVM commented that if there are any further applications for ‘Chairs Action’ for eltrombopag a formal application would be required. Agenda Item 58/15 | Individual Funding Requests Page 4 of 6 MC reported one IFR for Everolimus for a patient with Tuberous Sclerosis Complex which has been approved by NHSE as a lifelong treatment. Agenda Item 59/15 | Unlicensed Medicine updates The Panel reviewed the list of ULM for July: Bupivacine 0.5% with adrenaline 1 in 200,000 injection – supply problem with licensed preparation Ketamine 500mg/10ml injection – supply problem with all licensed strengths of ketamine Pigmanorm cream (tretinoin, hydrocortisone, hydroquinone) – Previous unlicensed product no longer available Aspirin suppositories 300mg – Licensed product no longer available Approved Agenda Item 60/15 | NICE Guidance For information - noted Agenda Item 61/15 | Cancer Drug Fund For information - noted Agenda Item 62/15 | HIV Medicines For information - noted Agenda Item 63/15 | Clinical Trials For information - noted Agenda Item 64/15 | WDTP Gap Analysis Action Plan Update The Panel reviewed the data and noted that there is still work to do to close the remaining actions ongoing. Agenda Item 65/15 | Drug Safety Update None Agenda Item 66/15 | Minutes from other Committees – for noting 66/15.01 - Medicine Clinical Guidelines Team – None 66/15.02 - Wirral Wide Wound Formulary Group – None 66/15.03 - Chemotherapy Steering Group – None 66/15.04 - Medical Gas Team – None 66/15.05 - Non Medical Prescribing Team – March 2015 66/15.06 – Antimicrobial Stewardship Team – January 2015 & May 2015 Agenda Item 67/15| any other business 67/15.01 – Trust wide Patient Group Directions (PGDs) Page 5 of 6 KH informed the Panel that there is a robust system for PGDs within the Pharmacy Department but with the Trust wide PGDs it was difficult to ensure that nurses signed up to these as they rotate around wards and divisions. KH proposed that a nurse only needs to sign one copy to prove that they are working under its particular direction. Approved 68/15.02 – Prednisolone Switch Author: Karen Herbert – Team Leader Medicines Management, Pharmacy Department WUTH KH presented a paper outlining the savings that could be made if patients were switched from soluble prednisolone 5mg to prednisolone 5mg tablets which would then be dispersed in water in those patients with an NG tube or difficulty swallowing tablets. Anecdotal evidence suggests unfavourable palatability of the prednisolone 5mg soluble tablets leading to potential non-compliance, particularly in younger children. The taste of the prednisolone 5mg tablets dispersed in water has been reported to be more palatable. The switch to dispersing standard prednisolone 5mg tablets in place of using the soluble preparation has been completed, without incident, by other Trusts across the country. The other proposal is to replace the use of standard 25mg prednisolone tablets with 5mg tablets when there is no clinical justification for prescribing 25mg tablets. The potential saving would by approximately £14½k per annum. Approved 68/15.03 – Proposed change of set day for Wirral Drug & Therapeutics Panel meetings to Tuesday MVM asked the Panel members if changing the meeting day to a Tuesday would be suitable for the majority of members. The CCG members could not attend on Tuesday as they have a regular Board meeting on that day. MG also had clinical commitments each Tuesday so could not attend on that day. It was agreed to continue with Wednesday as the set day for the meeting. Future Meeting Dates 68/15 Next meeting 9th September 2015 @ 12.30 – 2.00pm in Maternity Conference Room, APH (papers for submission needed by 25th August 2015) Page 6 of 6