NEWS &
FORUM
OCTOBER 2009
AMERICAN SOCIETY OF CLINICAL ONCOLOGY
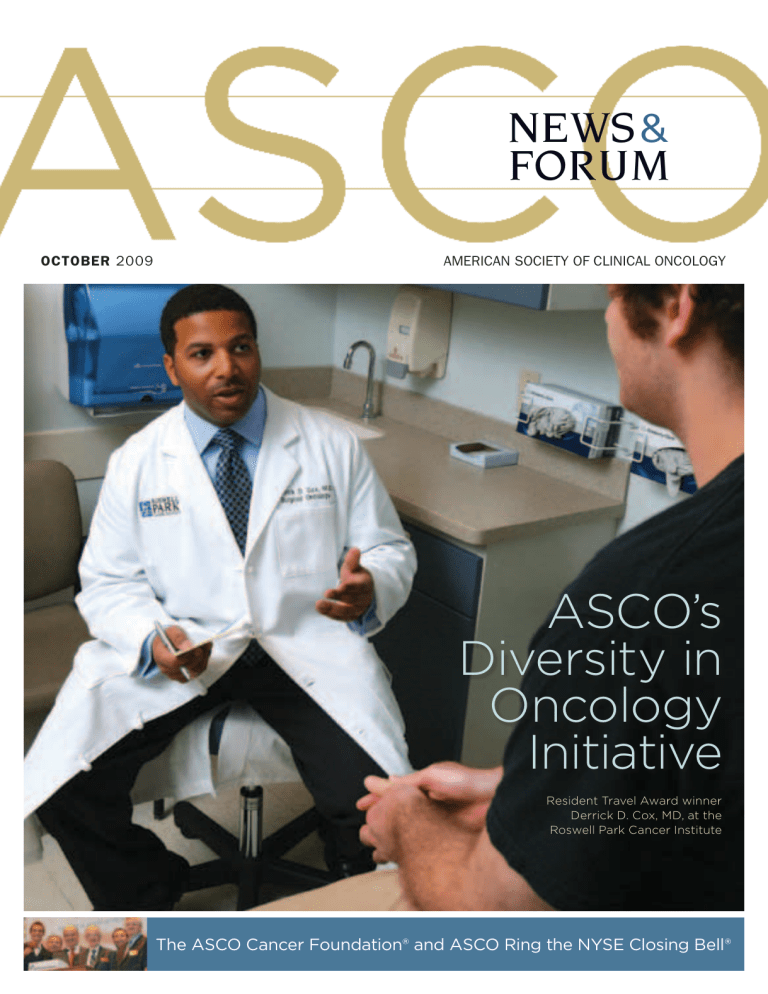
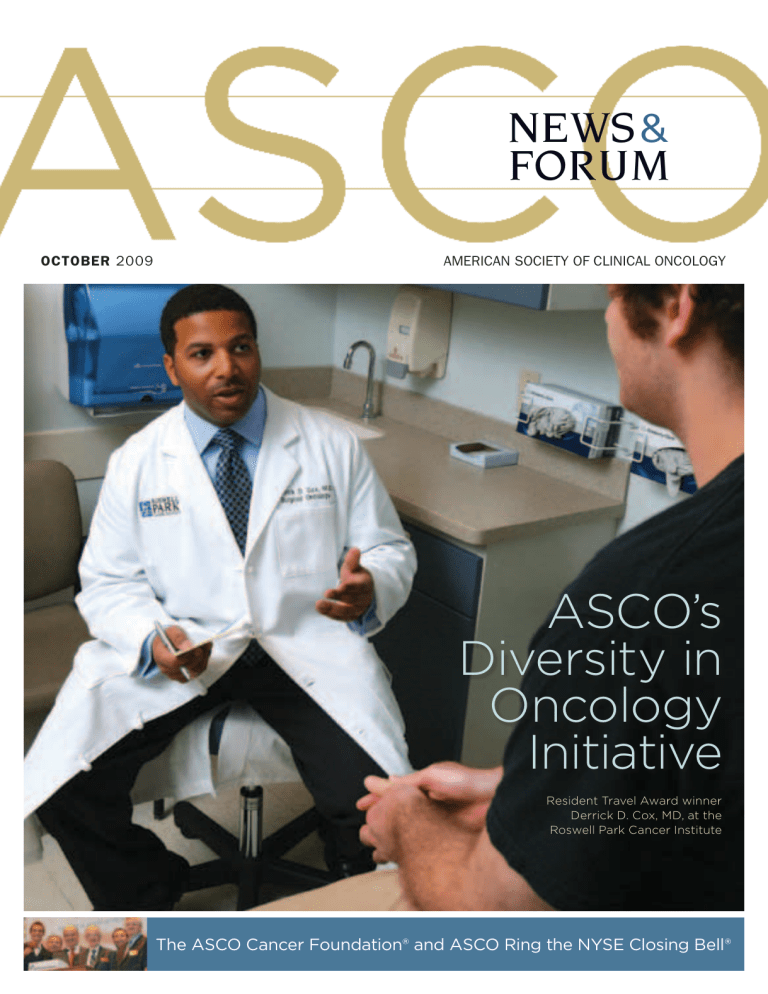
ASCO’s
Diversity in
Oncology
Initiative
Resident Travel Award winner
Derrick D. Cox, MD, at the
Roswell Park Cancer Institute
The ASCO Cancer Foundation® and ASCO Ring the NYSE Closing Bell®
In the adjuvant treatment of HER2+ breast cancer
Herceptin in combination
with Taxotere and
carboplatin (TCH), a
nonanthracycline
regimen, significantly
improved disease-free
survival (DFS) vs AC→T1
®
Adjuvant indications
Herceptin is indicated for adjuvant treatment of
HER2-overexpressing node-positive or node-negative
(ER/PR-negative or with one high-risk feature*)
breast cancer:
• As part of a treatment regimen containing doxorubicin,
cyclophosphamide, and either paclitaxel or docetaxel
• With docetaxel and carboplatin
• As a single agent following multi-modality
anthracycline-based therapy
Metastatic indications
Herceptin is indicated:
• In combination with paclitaxel for first-line
treatment of HER2-overexpressing
metastatic breast cancer
• As a single agent for treatment of
HER2-overexpressing breast cancer in patients
who have received one or more chemotherapy
regimens for metastatic disease
*High-risk features for patients with ER/PR+ breast cancer include: tumor size
>2 cm, age <35 years, and histologic and/or nuclear grade 2/3.
Please see accompanying brief summary of full Prescribing Information, including Boxed WARNINGS and additional
important safety information, on the following pages.
©2009 Genentech USA, Inc.
So. San Francisco, CA
All rights reserved.
9488201
7/09
TCH demonstrated DFS benefit consistent with AC→TH1
DFS at 3 years1,2 †
Absolute DFS
at 3 years
1.0
86.3% (TCH)
88.0% (AC→TH)
82.3% (AC→T)
Proportion event-free
0.8
TCH vs AC→T
HR=0.67
(95% CI: 0.54-0.84)‡
P=0.0006
0.6
0.4
AC→TH vs AC→T
HR=0.60
(95% CI: 0.48-0.76)
P<0.0001
0.2
AC→T (n=1073)
AC→TH (n=1074)
TCH (n=1075)
0.0
0.0
1.0
2.0
DFS (years)
3.0
4.0
971
1023
1018
802
885
877
417
457
447
103
126
126
Number at risk
AC→ T
AC→ TH
TCH
1073
1074
1075
AC=doxorubicin/cyclophosphamide
T=Taxotere
C=carboplatin
H=Herceptin
• 33% reduction in risk of recurrence with TCH (HR=0.67, CI: 0.54-0.84;
P=0.0006)
• 40% reduction in risk of recurrence with AC→TH (HR=0.60, CI: 0.48-0.76;
P<0.0001)
Reduced risk of congestive heart failure with TCH
vs AC→TH1
• 0.4% (TCH) vs 2% (AC →TH) and 0.3% (AC →T)
Boxed WARNINGS and Additional Important Safety Information
Herceptin administration can result in sub-clinical and clinical cardiac failure manifesting as congestive heart
failure and decreased left ventricular ejection fraction. Serious infusion reactions and pulmonary toxicity have
occurred; fatal infusion reactions have been reported. Exacerbation of chemotherapy-induced neutropenia has also
occurred. Herceptin can cause oligohydramnios and fetal harm when administered to a pregnant woman. The most common
adverse reactions associated with Herceptin use were fever, nausea, vomiting, infusion reactions, diarrhea, infections,
increased cough, headache, fatigue, dyspnea, rash, neutropenia, anemia, and myalgia.
Taxotere is a registered trademark of sanofi-aventis U.S. LLC.
† BCIRG
006 study design: Conducted by the Breast Cancer International Research Group (BCIRG), this clinical trial evaluated the efficacy and cardiac safety of
two regimens vs control in a 1:1:1 randomization. The TCH arm consisted of concurrent docetaxel, carboplatin, and Herceptin and the AC→TH arm consisted of
AC (doxorubicin and cyclophosphamide), followed by docetaxel and Herceptin.
Control did not include Herceptin. Hormonal and/or radiotherapy were given
as appropriate.
‡ HR = hazard ratio; CI = confidence interval.
References: 1. Herceptin Prescribing Information. Genentech, Inc. March 2009.
2. Data on file. Genentech, Inc.
www.herceptin.com
HERCEPTIN® (trastuzumab)
Brief Summary For full Prescribing Information, see
package insert.
WARNING: CARDIOMYOPATHY, INFUSION
REACTIONS, and PULMONARY TOXICITY
Cardiomyopathy
Herceptin can result in sub-clinical and clinical
cardiac failure manifesting as CHF and decreased
LVEF. The incidence and severity of left ventricular
cardiac dysfunction was highest in patients who
received Herceptin concurrently with anthracyclinecontaining chemotherapy regimens.
Evaluate left ventricular function in all patients prior
to and during treatment with Herceptin. Discontinue
Herceptin treatment in patients receiving adjuvant
therapy and strongly consider discontinuation of
Herceptin treatment in patients with metastatic breast
cancer for clinically significant decrease in left
ventricular function. [see Warnings and Precautions
and Dosage and Administration]
Infusion Reactions; Pulmonary Toxicity
Herceptin administration can result in serious
infusion reactions and pulmonary toxicity. Fatal
infusion reactions have been reported. In most cases,
symptoms occurred during or within 24 hours of
administration of Herceptin. Herceptin infusion should
be interrupted for patients experiencing dyspnea or
clinically significant hypotension. Patients should be
monitored until signs and symptoms completely
resolve. Discontinue Herceptin for infusion reactions
manifesting as anaphylaxis, angioedema, interstitial
pneumonitis, or acute respiratory distress syndrome.
[see Warnings and Precautions]
INDICATIONS AND USAGE Adjuvant Breast Cancer
Herceptin is indicated for adjuvant treatment of HER2
overexpressing node positive or node negative (ER/PR
negative or with one high risk feature [see Clinical Studies])
breast cancer • as part of a treatment regimen consisting
of doxorubicin, cyclophosphamide, and either paclitaxel or
docetaxel • with docetaxel and carboplatin • as a single
agent following multi-modality anthracycline based therapy.
Metastatic Breast Cancer Herceptin is indicated: • In
combination with paclitaxel for first-line treatment of HER2overexpressing metastatic breast cancer • As a single
agent for treatment of HER2-overexpressing breast cancer
in patients who have received one or more chemotherapy
regimens for metastatic disease. CONTRAINDICATIONS
None. WARNINGS AND PRECAUTIONS Cardiomyopathy
Herceptin can cause left ventricular cardiac dysfunction,
arrhythmias, hypertension, disabling cardiac failure,
cardiomyopathy, and cardiac death [see Boxed Warning:
Cardiomyopathy]. Herceptin can also cause asymptomatic
decline in left ventricular ejection fraction (LVEF). There is
a 4–6 fold increase in the incidence of symptomatic
myocardial dysfunction among patients receiving Herceptin
as a single agent or in combination therapy compared with
those not receiving Herceptin. The highest absolute
incidence occurs when Herceptin is administered with an
anthracycline. Withhold Herceptin for !16% absolute
decrease in LVEF from pre-treatment values or an LVEF
value below institutional limits of normal and !10%
absolute decrease in LVEF from pretreatment values. [see
Dosage and Administration] The safety of continuation or
resumption of Herceptin in patients with Herceptin-induced
left ventricular cardiac dysfunction has not been studied.
Cardiac Monitoring Conduct thorough cardiac assessment,
including history, physical examination, and determination
of LVEF by echocardiogram or MUGA scan. The following
schedule is recommended: • Baseline LVEF measurement
immediately prior to initiation of Herceptin • LVEF
measurements every 3 months during and upon completion
of Herceptin • Repeat LVEF measurement at 4 week
intervals if Herceptin is withheld for significant left
ventricular cardiac dysfunction [see Dosage and
Administration] • LVEF measurements every 6 months for
at least 2 years following completion of Herceptin as a
component of adjuvant therapy. In Study 1, 16% (136/844)
of patients discontinued Herceptin due to clinical evidence
of myocardial dysfunction or significant decline in LVEF. In
Study 3, the number of patients who discontinued Herceptin
due to cardiac toxicity was 2.6% (44/1678). In Study 4, a total
of 2.9% (31/1056) patients in the TCH arm (1.5% during the
chemotherapy phase and 1.4% during the monotherapy
phase) and 5.7% (61/1068) patients in the AC-TH arm (1.5%
during the chemotherapy phase and 4.2% during the
monotherapy phase) discontinued Herceptin due to cardiac
toxicity. Among 32 patients receiving adjuvant chemotherapy (Studies 1 and 2) who developed congestive heart
failure, one patient died of cardiomyopathy and all other
patients were receiving cardiac medication at last followup. Approximately half of the surviving patients had
recovery to a normal LVEF (defined as ! 50%) on continuing
medical management at the time of last follow-up.
Incidence of congestive heart failure is presented in
Table 1. The safety of continuation or resumption of
Herceptin in patients with Herceptin-induced left
ventricular cardiac dysfunction has not been studied.
Table 1 Incidence of Congestive Heart Failure in
Adjuvant Breast Cancer Studies
Study
Regimen
1 & 2a ACb!Paclitaxel+
Herceptin
3
Chemo!Herceptin
4
ACb!Docetaxel+
Herceptin
4
Docetaxel+Carbo+
Herceptin
Incidence of CHF
Herceptin
Control
2% (32/1677)
2% (30/1678)
0.4% (7/1600)
0.3% (5/1708)
2% (20/1068)
0.3% (3/1050)
0.4% (4/1056)
0.3% (3/1050)
Includes 1 patient with fatal cardiomyopathy.
b
Anthracycline (doxorubicin) and cyclophosphamide
a
Table 2 Incidence of Cardiac Dysfunctiona in Metastatic
Breast Cancer Studies
Study
5
(AC)b
5
(paclitaxel)
6
Incidence
NYHA I-IV
NYHA III-IV
Herceptin Control Herceptin Control
Event
Cardiac
Dysfunction 28%
Cardiac
Dysfunction 11%
Cardiac
Dysfunctionc 7%
7%
19%
3%
1%
4%
1%
N/A
5%
N/A
Congestive heart failure or significant asymptomatic
decrease in LVEF. b Anthracycline (doxorubicin or
epirubicin) and cyclophosphamide c Includes 1 patient
with fatal cardiomyopathy.
Infusion Reactions Infusion reactions consist of a
symptom complex characterized by fever and chills, and
on occasion included nausea, vomiting, pain (in some
cases at tumor sites), headache, dizziness, dyspnea,
hypotension, rash, and asthenia. [see Adverse Reactions].
In postmarketing reports, serious and fatal infusion
reactions have been reported. Severe reactions which
include bronchospasm, anaphylaxis, angioedema, hypoxia,
and severe hypotension, were usually reported during or
immediately following the initial infusion. However, the
onset and clinical course were variable including
progressive worsening, initial improvement followed by
clinical deterioration, or delayed post-infusion events with
rapid clinical deterioration. For fatal events, death
occurred within hours to days following a serious infusion
reaction. Interrupt Herceptin infusion in all patients
experiencing dyspnea, clinically significant hypotension,
and intervention of medical therapy administered, which
may include: epinephrine, corticosteroids, diphenhydramine, bronchodilators, and oxygen. Patients should
be evaluated and carefully monitored until complete
resolution of signs and symptoms. Permanent
discontinuation should be strongly considered in all
patients with severe infusion reactions. There are no data
regarding the most appropriate method of identification of
patients who may safely be retreated with Herceptin after
experiencing a severe infusion reaction. Prior to
resumption of Herceptin infusion, the majority of patients
who experienced a severe infusion reaction were premedicated with antihistamines and/or corticosteroids.
While some patients tolerated Herceptin infusions, others
had recurrent severe infusion reactions despite premedications. Exacerbation of Chemotherapy-Induced
Neutropenia In randomized, controlled clinical trials in
women with metastatic breast cancer, the per-patient
incidences of NCI CTC Grade 3-4 neutropenia and of febrile
neutropenia were higher in patients receiving Herceptin
in combination with myelosuppressive chemotherapy as
compared to those who received chemotherapy alone. The
incidence of septic death was not significantly increased.
[see Adverse Reactions]. Pulmonary Toxicity Herceptin
use can result in serious and fatal pulmonary toxicity.
Pulmonary toxicity includes dyspnea, interstitial
pneumonitis, pulmonary infiltrates, pleural effusions, noncardiogenic pulmonary edema, pulmonary insufficiency
and hypoxia, acute respiratory distress syndrome, and
pulmonary fibrosis. Such events can occur as sequelae of
infusion reactions [see Warnings and Precautions (5.2)].
a
Patients with symptomatic intrinsic lung disease or with
extensive tumor involvement of the lungs, resulting in
dyspnea at rest, appear to have more severe toxicity. HER2
Testing Detection of HER2 protein overexpression is
necessary for selection of patients appropriate for
Herceptin therapy because these are the only patients
studied and for whom benefit has been shown.
Assessment for HER2 overexpression and of HER2 gene
amplification should be performed by laboratories with
demonstrated proficiency in the specific technology being
utilized. Improper assay performance, including use of
suboptimally fixed tissue, failure to utilize specified
reagents, deviation from specific assay instructions, and
failure to include appropriate controls for assay validation,
can lead to unreliable results. Several FDA-approved
commercial assays are available to aid in the selection of
patients for Herceptin therapy. These include HercepTestTM
and Pathway® HER-2/neu (IHC assays) and PathVysion®
and HER2 FISH pharmDxTM (FISH assays). Users should
refer to the package inserts of specific assay kits for
information on the validation and performance of each
assay. Limitations in assay precision (particularly for the
IHC method) and in the direct linkage between assay result
and overexpression of the Herceptin target (for the FISH
method) make it inadvisable to rely on a single method to
rule out potential Herceptin benefit. A negative FISH result
does not rule out HER2 overexpression and potential
benefit from Herceptin. Treatment outcomes for metastatic
breast cancer (Study 5) as a function of IHC and FISH
testing are provided in Table 9. Treatment outcomes for
adjuvant breast cancer (Studies 2 and 3) as a function of
IHC and FISH testing are provided in Table 7. HER2 Protein
Overexpression Detection Methods HER2 protein
overexpression can be established by measuring HER2
protein using an IHC method. HercepTest®, one test
approved for this use, was assessed for concordance with
the Clinical Trial Assay (CTA), using tumor specimens
collected and stored independently from those obtained in
Herceptin clinical studies in women with metastatic breast
cancer. Data are provided in the package insert for
HercepTest®. HER2 Gene Amplification Detection Method
The presence of HER2 protein overexpression and gene
amplification are highly correlated, therefore the use of
FISH to detect gene amplification may be employed for
selection of patients appropriate for Herceptin therapy.
PathVysion®, one test approved for this use, was evaluated
in an exploratory, retrospective assessment of available
CTA 2+ or 3+ tumor specimens collected as part of patient
screening for clinical studies in metastatic breast cancer
(Studies 5 and 6). Data are provided in the package insert
for PathVysion®. Embryo-Fetal Toxicity (Pregnancy
Category D) Herceptin can cause fetal harm when
administered to a pregnant woman. Post-marketing case
reports suggest that Herceptin use during pregnancy
increases the risk of oligohydramnios during the second
and third trimesters. If Herceptin is used during pregnancy
or if a woman becomes pregnant while taking Herceptin,
she should be apprised of the potential hazard to a fetus.
[see Use in Specific Populations]. ADVERSE REACTIONS
The following adverse reactions are discussed in greater
detail in other sections of the label: • Cardiomyopathy
[see Warnings and Precautions] • Infusion reactions
[see Warnings and Precautions] • Exacerbation of
chemotherapy-induced neutropenia [see Warnings and
Precautions] • Pulmonary toxicity [see Warnings and
Precautions] The most common adverse reactions in
patients receiving Herceptin are fever, nausea, vomiting,
infusion reactions, diarrhea, infections, increased cough,
headache, fatigue, dyspnea, rash, neutropenia, anemia,
and myalgia. Adverse reactions requiring interruption or
discontinuation of Herceptin treatment include CHF,
significant decline in left ventricular cardiac function,
severe infusion reactions, and pulmonary toxicity [see
Dosage and Administration]. Clinical Trials Experience
Because clinical trials are conducted under widely varying
conditions, adverse reaction rates observed in the clinical
trials of a drug cannot be directly compared to rates in the
clinical trials of another drug and may not reflect the rates
observed in practice. Adjuvant Breast Cancer Studies The
data below reflect exposure to Herceptin across three
randomized, open-label studies, Studies 1, 2, and 3, with
(n= 3355) or without (n= 3308) trastuzumab in the adjuvant
treatment of breast cancer. The data summarized in Table
3 below, from Study 3, reflect exposure to Herceptin in 1678
patients; the median treatment duration was 51 weeks and
median number of infusions was 18. Among the 3386
patients enrolled in Study 3, the median age was 49 years
(range: 21 to 80 years), 83% of patients were Caucasian,
and 13% were Asian.
Table 3 Adverse Reactions for Study 3, All Gradesa:
MedDRA (v. 7.1)
1 Year Herceptin Observation
Adverse Event Preferred Term
(n= 1678)
(n= 1708)
Cardiac
Hypertension
64 (4%)
35 (2%)
Dizziness
60 (4%)
29 (2%)
Ejection Fraction Decreased
58 (3.5%)
11 (0.6%)
Palpitations
48 (3%)
12 (0.7%)
Cardiac Arrhythmiasb
40 (3%)
17 (1%)
Cardiac Failure Congestive
30 (2%)
5 (0.3%)
Cardiac Failure
9 (0.5%)
4 (0.2%)
Cardiac Disorder
5 (0.3%)
0 (0%)
Ventricular Dysfunction
4 (0.2%)
0 (0%)
Respiratory Thoracic Mediastinal Disorders
Nasopharyngitis
135 (8%)
43 (3%)
Cough
81 (5%)
34 (2%)
Influenza
70 (4%)
9 (0.5%)
Dyspnea
57 (3%)
26 (2%)
URI
46 (3%)
20 (1%)
Rhinitis
36 (2%)
6 (0.4%)
Pharyngolaryngeal Pain
32 (2%)
8 (0.5%)
Sinusitis
26 (2%)
5 (0.3%)
Epistaxis
25 (2%)
1 (0.06%)
Pulmonary Hypertension
4 (0.2%)
0 (0%)
Interstitial Pneumonitis
4 (0.2%)
0 (0%)
Gastrointestinal Disorders
Diarrhea
123 (7%)
16 (1%)
Nausea
108 (6%)
19 (1%)
Vomiting
58 (3.5%)
10 (0.6%)
Constipation
33 (2%)
17 (1%)
Dyspepsia
30 (2%)
9 (0.5%)
Upper Abdominal Pain
29 (2%)
15 (1%)
Musculoskeletal & Connective Tissue Disorders
Arthralgia
137 (8%)
98 (6%)
Back Pain
91 (5%)
58 (3%)
Myalgia
63 (4%)
17 (1%)
Bone Pain
49 (3%)
26 (2%)
Muscle Spasm
46 (3%)
3 (0.2%)
Nervous System Disorders
Headache
162 (10%)
49 (3%)
Paraesthesia
29 (2%)
11 (0.6%)
Skin & Subcutaneous Tissue Disorders
Rash
70 (4%)
10 (.6%)
Nail Disorders
43 (2%)
0 (0%)
Pruritis
40 (2%)
10 (0.6%)
General Disorders
Pyrexia
100 (6%)
6 (0.4%)
Edema Peripheral
79 (5%)
37 (2%)
Chills
85 (5%)
0 (0%)
Aesthenia
75 (4.5%)
30 (2%)
Influenza-like Illness
40 (2%)
3 (0.2%)
Sudden Death
1 (.06%)
0 (0%)
Infections
Nasopharyngitis
135 (8%)
43 (3%)
UTI
39 (3%)
13 (0.8%)
Immune System Disorders
Hypersensitivity
10 (0.6%)
1 (0.06%)
Autoimmune Thyroiditis
4 (0.3%)
0 (0%)
The incidence of Grade 3/4 adverse reactions was <1%
in both arms for each listed term. b Higher level grouping
term.
The data from Studies 1 and 2 were obtained from 3206
patients enrolled, of which 1635 patients received
Herceptin; the median treatment duration was
50 weeks. The median age was 49.0 years (range: 24-80);
84% of patients were White, and 7% were Black, 4% were
Hispanic, and 4% were Asian. In Study 1, only Grade 3-5
adverse events, treatment-related Grade 2 events, and
Grade 2-5 dyspnea were collected during and for up to 3
months following protocol-specified treatment. The
following non-cardiac adverse reactions of Grade 2-5
occurred at an incidence of at least 2% greater among
patients randomized to Herceptin plus chemotherapy as
compared to chemotherapy alone: arthralgia (31% vs.
28%), fatigue (28% vs. 22%), infection (22% vs. 14%),
hot flashes (17% vs. 15%), anemia (13% vs. 7%),
dyspnea (12% vs. 4%), rash/desquamation (11% vs. 7%),
neutropenia (7% vs. 5%), headache (6% vs. 4%), and
insomnia (3.7% vs. 1.5%). The majority of these events
were Grade 2 in severity. In Study 2, data collection
was limited to the following investigator-attributed
a
treatment-related adverse reactions NCI-CTC Grade 4
and 5 hematologic toxicities, Grade 3–5 non-hematologic
toxicities, selected Grade 2–5 toxicities associated
with taxanes (myalgia, arthralgias, nail changes, motor
neuropathy, sensory neuropathy) and Grade 1–5 cardiac
toxicities occurring during chemotherapy and/or
Herceptin treatment. The following non-cardiac adverse
reactions of Grade 2–5 occurred at an incidence of at
least 2% greater among patients randomized to Herceptin
plus chemotherapy as compared to chemotherapy alone:
arthralgia (11% vs. 8.4%), myalgia (10% vs. 8%), nail
changes (9% vs. 7%), and dyspnea (2.5% vs. 0.1%). The
majority of these events were Grade 2 in severity. Safety
data from Study 4 reflect exposure to Herceptin as part
of an adjuvant treatment regimen from 2124 patients
receiving at least one dose of study treatment [AC-TH:
n = 1068; TCH: n = 1056]. The overall median treatment
duration was 54 weeks in both the AC-TH and TCH arms.
The median number of infusions was 26 in the AC-TH arm
and 30 in the TCH arm, including weekly infusions during
the chemotherapy phase and every three week dosing in
the monotherapy period. Among these patients, the
median age was 49 years (range 22 to 74 years). In Study
4, the toxicity profile was similar to that reported in
Studies 1, 2, and 3 with the exception of a low incidence
of CHF in the TCH arm. Metastatic Breast Cancer Studies
The data below reflect exposure to Herceptin in one
randomized, open-label study, Study 5, of chemotherapy
with (n=235) or without (n=234) trastuzumab in patients
with metastatic breast cancer, and one single-arm study
(Study 6; n=222) in patients with metastatic breast cancer.
Data in Table 5 are based on Studies 5 and 6. Among the
464 patients treated in Study 5, the median age was 52
years (range: 25–77 years). Eighty-nine percent were
White, 5% Black, 1% Asian and 5% other racial/ethnic
groups. All patients received 4 mg/kg initial dose of
Herceptin followed by 2 mg/kg weekly. The percentages
of patients who received Herceptin treatment for
!6 months and !12 months were 58% and 9%,
respectively. Among the 352 patients treated in single
agent studies (213 patients from Study 6), the median age
was 50 years (range 28–86 years), 100% had breast
cancer, 86% were White, 3% were Black, 3% were Asian,
and 8% in other racial/ethnic groups. Most of the patients
received 4 mg/kg initial dose of Herceptin followed by
2 mg/kg weekly. The percentages of patients who
received Herceptin treatment for !6 months and
!12 months were 31% and 16%, respectively.
Table 4 Per-Patient Incidence of Adverse Reactions
Occurring in !5% of Patients in Uncontrolled Studies or
at Increased Incidence in the Herceptin Arm (Studies 5
and 6) (Percent of Patients)
Herceptin
Single
+
Paclitaxel Herceptin ACb
a
Agent Paclitaxel Alone + ACb Alone
n = 352 n = 91 n = 95 n = 143 n = 135
Body as a Whole
Pain
47
61
62
57
42
Asthenia
42
62
57
54
55
Fever
36
49
23
56
34
Chills
32
41
4
35
11
Headache
26
36
28
44
31
Abdominal pain 22
34
22
23
18
Back pain
22
34
30
27
15
Infection
20
47
27
47
31
Flu syndrome 10
12
5
12
6
Accidental
injury
6
13
3
9
4
Allergic
reaction
3
8
2
4
2
Cardiovascular
Tachycardia
5
12
4
10
5
Congestive
7
11
1
28
7
heart failure
Digestive
Nausea
33
51
9
76
77
Diarrhea
25
45
29
45
26
Vomiting
23
37
28
53
49
Nausea and
8
14
11
18
9
vomiting
Anorexia
14
24
16
31
26
Heme &
Lymphatic
Anemia
4
14
9
36
26
Leukopenia
3
24
17
52
34
Metabolic
Peripheral
edema
Edema
Musculoskeletal
Bone pain
Arthralgia
Nervous
Insomnia
Dizziness
Paresthesia
Depression
Peripheral
neuritis
Neuropathy
Respiratory
Cough
increased
Dyspnea
Rhinitis
Pharyngitis
Sinusitis
Skin
Rash
Herpes simplex
Acne
Urogenital
Urinary tract
infection
10
8
22
10
20
8
20
11
17
5
7
6
24
37
18
21
7
8
7
9
14
13
9
6
25
22
48
12
13
24
39
13
29
24
17
20
15
18
11
12
2
1
23
13
16
5
2
4
2
4
26
22
14
12
9
41
27
22
22
21
22
26
5
14
7
43
42
22
30
13
29
25
16
18
6
18
2
2
38
12
11
18
3
3
27
7
3
17
9
<1
5
18
14
13
7
a
Data for Herceptin single agent were from 4 studies,
including 213 patients from Study 6. b Anthracycline
(doxorubicin or epirubicin) and cyclophosphamide
The following subsections provide additional detail
regarding adverse reactions observed in clinical trials
of adjuvant breast, metastatic breast cancer, or
post-marketing experience. Cardiomyopathy Serial
measurement of cardiac function (LVEF) was obtained in
clinical trials in the adjuvant treatment of breast cancer. In
Study 3, the median duration of follow-up was 12.6 months
(12.4 months in the observation arm; 12.6 months in the
1-year Herceptin arm); and in Studies 1 and 2, 23 months
in the AC-T arm, 24 months in the AC-TH arm. In Studies 1
and 2, 6% of patients were not permitted to initiate
Herceptin following completion of AC chemotherapy due
to cardiac dysfunction (LVEF <50% or !15 point decline in
LVEF from baseline to end of AC). Following initiation of
Herceptin therapy, the incidence of new-onset doselimiting myocardial dysfunction was higher among patients
receiving Herceptin and paclitaxel as compared to those
receiving paclitaxel alone in Studies 1 and 2, and in
patients receiving Herceptin monotherapy compared to
observation in Study 3 (see Table 5, Figures 1 and 2).
Table 5a Per-patient Incidence of New Onset Myocardial
Dysfunction (by LVEF) Studies 1, 2, 3 and 4
LVEF <50%
and Absolute Decrease
from Baseline
Studies 1 & 2b
AC!TH
(n=1606)
AC!T
(n=1488)
Study 3
Herceptin
(n=1678)
Observation
(n=1708)
Study 4c
TCH
(n=1056)
AC!TH
(n=1068)
AC!T
(n=1050)
LVEF ≥10% ≥16%
<50% decrease decrease
Absolute LVEF
Decrease
<20%
and
≥10% ≥20%
22.8% 18.3%
(366) (294)
9.1% 5.4%
(136) (81)
11.7%
(188)
2.2%
(33)
33.4%
(536)
18.3%
(272)
9.2%
(148)
2.4%
(36)
8.6%
(144)
2.7%
(46)
7.0%
(118)
2.0%
(35)
3.8%
(64)
1.2%
(20)
22.4%
(376)
11.9%
(204)
3.5%
(59)
1.2%
(21)
8.5%
(90)
17%
(182)
9.5%
(100)
5.9%
(62)
13.3%
(142)
6.6%
(69)
3.3%
(35)
9.8%
(105)
3.3%
(35)
34.5%
(364)
44.3%
(473)
34%
(357)
6.3%
(67)
13.2%
(141)
5.5%
(58)
a
For Studies 1, 2 and 3, events are counted from the
beginning of Herceptin treatment. For Study 4, events are
counted from the date of randomization. b Studies 1 and 2
regimens: doxorubicin and cyclophosphamide followed by
paclitaxel (AC!T) or paclitaxel plus Herceptin (AC!TH)
c
Study 4 regimens: doxorubicin and cyclophosphamide
followed by docetaxel (AC!T) or docetaxel plus Herceptin
(AC!TH); docetaxel and carboplatin plus Herceptin (TCH)
Figure 1 Studies 1 and 2: Cumulative Incidence of Time to
First LVEF Decline of !10 Percentage Points from Baseline
and to Below 50% with Death as a Competing Risk Event
Time 0 is initiation of paclitaxel or Herceptin + paclitaxel
therapy.
Figure 2 Study 3: Cumulative Incidence of Time to First
LVEF Decline of!10 Percentage Points from Baseline and
to Below 50% with Death as a Competing Risk Event
Time 0 is the date of randomization.
Figure 3 Study 4: Cumulative Incidence of Time to First
LVEF Decline of !10 Percentage Points from Baseline
and to Below 50% with Death as a Competing Risk Event
Time 0 is the date of randomization.
The incidence of treatment emergent congestive heart
failure among patients in the metastatic breast cancer trials
was classified for severity using the New York Heart
Association classification system (I–IV, where IV is the most
severe level of cardiac failure) (see Table 2). In the
metastatic breast cancer trials the probability of cardiac
dysfunction was highest in patients who received
Herceptin concurrently with anthracyclines. Infusion
Reactions During the first infusion with Herceptin, the
symptoms most commonly reported were chills and fever,
occurring in approximately 40% of patients in clinical
trials. Symptoms were treated with acetaminophen,
diphenhydramine, and meperidine (with or without
reduction in the rate of Herceptin infusion); permanent
discontinuation of Herceptin for infusional toxicity was
required in <1% of patients. Other signs and/or symptoms
may include nausea, vomiting, pain (in some cases at tumor
sites), rigors, headache, dizziness, dyspnea, hypotension,
elevated blood pressure, rash, and asthenia. Infusional
toxicity occurred in 21% and 35% of patients, and was
severe in 1.4% and 9% of patients, on second or subsequent
Herceptin infusions administered as monotherapy or in
combination with chemotherapy, respectively. In the postmarketing setting, severe infusion reactions, including
hypersensitivity, anaphylaxis, and angioedema have been
reported. Anemia In randomized controlled clinical trials,
the overall incidence of anemia (30% vs. 21% [Study 5]), of
selected NCI-CTC Grade 2–5 anemia (12.5% vs. 6.6% [Study
1]), and of anemia requiring transfusions (0.1% vs. 0 patients
[Study 2]) were increased in patients receiving Herceptin
and chemotherapy compared with those receiving
chemotherapy alone. Following the administration of
Herceptin as a single agent (Study 6), the incidence of
NCI-CTC Grade 3 anemia was < 1%. Neutropenia In
randomized controlled clinical trials in the adjuvant setting,
the incidence of selected NCI-CTC Grade 4–5 neutropenia
(2% vs. 0.7% [Study 2]) and of selected Grade 2–5
neutropenia (7.1% vs. 4.5 % [Study 1]) were increased in
patients receiving Herceptin and chemotherapy compared
with those receiving chemotherapy alone. In a randomized,
controlled trial in patients with metastatic breast cancer,
the incidences of NCI-CTC Grade 3/4 neutropenia (32% vs.
22%) and of febrile neutropenia (23% vs. 17%) were also
increased in patients randomized to Herceptin in
combination with myelosuppressive chemotherapy as
compared to chemotherapy alone. Infection The overall
incidences of infection (46% vs. 30% [Study 5]), of selected
NCI-CTC Grade 2–5 infection/febrile neutropenia (22% vs.
14% [Study 1]) and of selected Grade 3–5 infection/febrile
neutropenia (3.3% vs. 1.4%) [Study 2]), were higher in
patients receiving Herceptin and chemotherapy compared
with those receiving chemotherapy alone. The most
common site of infections in the adjuvant setting involved
the upper respiratory tract, skin, and urinary tract. In study
4, the overall incidence of infection was higher with the
addition of Herceptin to AC-T but not to TCH [44% (AC-TH),
37% (TCH), 38% (AC-T)]. The incidences of NCI-CTC grade
3-4 infection were similar [25% (AC-TH), 21% (TCH), 23%
(AC-T)] across the three arms. In a randomized, controlled
trial in treatment of metastatic breast cancer, the reported
incidence of febrile neutropenia was higher (23% vs. 17%)
in patients receiving Herceptin in combination with
myelosuppressive chemotherapy as compared to chemotherapy alone. Pulmonary Toxicity Adjuvant Breast Cancer
Among women receiving adjuvant therapy for breast
cancer, the incidence of selected NCI-CTC Grade 2–5
pulmonary toxicity (14% vs. 5% [Study 1]) and of selected
NCI-CTC Grade 3–5 pulmonary toxicity and spontaneous
reported Grade 2 dyspnea (3.4 % vs. 1% [Study 2]) was
higher in patients receiving Herceptin and chemotherapy
compared with chemotherapy alone. The most common
pulmonary toxicity was dyspnea (NCI-CTC Grade 2–5: 12%
vs. 4% [Study 1]; NCI-CTC Grade 2–5: 2.5% vs. 0.1%
[Study 2]). Pneumonitis/pulmonary infiltrates occurred in
0.7% of patients receiving Herceptin compared with 0.3%
of those receiving chemotherapy alone. Fatal respiratory
failure occurred in 3 patients receiving Herceptin, one as a
component of multi-organ system failure, as compared to
1 patient receiving chemotherapy alone. In Study 3, there
were 4 cases of interstitial pneumonitis in Herceptin-treated
patients compared to none in the control arm. Metastatic
Breast Cancer Among women receiving Herceptin for
treatment of metastatic breast cancer, the incidence of
pulmonary toxicity was also increased. Pulmonary adverse
events have been reported in the post-marketing
experience as part of the symptom complex of infusion
reactions. Pulmonary events include bronchospasm,
hypoxia, dyspnea, pulmonary infiltrates, pleural effusions,
non-cardiogenic pulmonary edema, and acute respiratory
distress syndrome. For a detailed description, see Warnings
and Precautions. Thrombosis/Embolism In 4 randomized,
controlled clinical trials, the incidence of thrombotic
adverse events was higher in patients receiving Herceptin
and chemotherapy compared to chemotherapy alone in
three studies (3.0% vs. 1.3% [Study 1], 2.5% and 3.7% vs.
2.2% [Study 4] and 2.1% vs. 0% [Study 5]). Diarrhea Among
women receiving adjuvant therapy for breast cancer, the
incidence of NCI-CTC Grade 2–5 diarrhea (6.2% vs. 4.8%
[Study 1]) and of NCI-CTC Grade 3–5 diarrhea (1.6% vs. 0%
[Study 2]), and of grade 1-4 diarrhea (7% vs. 1% [Study 3])
were higher in patients receiving Herceptin as compared
to controls. In Study 4, the incidence of Grade 3–4 diarrhea
was higher [5.7% AC-TH, 5.5% TCH vs. 3.0% AC-T] and of
Grade 1–4 was higher [51% AC-TH, 63% TCH vs. 43% AC-T]
among women receiving Herceptin. Of patients receiving
Herceptin as a single agent for the treatment of metastatic
breast cancer, 25% experienced diarrhea. An increased
incidence of diarrhea was observed in patients receiving
Herceptin in combination with chemotherapy for treatment
of metastatic breast cancer. Glomerulopathy In the
postmarketing setting, rare cases of nephrotic syndrome
with pathologic evidence of glomerulopathy have been
reported. The time to onset ranged from 4 months to
approximately 18 months from initiation of Herceptin
therapy. Pathologic findings included membranous
glomerulonephritis, focal glomerulosclerosis, and fibrillary
glomerulonephritis. Complications included volume
overload and congestive heart failure. Immunogenicity As
with all therapeutic proteins, there is a potential for
immunogenicity. Among 903 women with metastatic breast
cancer, human anti-human antibody (HAHA) to Herceptin
was detected in one patient using an enzyme-linked
immunosorbent assay (ELISA). This patient did not
experience an allergic reaction. Samples for assessment
of HAHA were not collected in studies of adjuvant breast
cancer. The incidence of antibody formation is highly
dependent on the sensitivity and the specificity of the assay.
Additionally, the observed incidence of antibody (including
neutralizing antibody) positivity in an assay may be
influenced by several factors including assay methodology,
sample handling, timing of sample collection, concomitant
medications, and underlying disease. For these reasons,
comparison of the incidence of antibodies to Herceptin with
the incidence of antibodies to other products may be
misleading. USE IN SPECIFIC POPULATIONS Pregnancy
Teratogenic Effects: Category D [see Warnings and
Precautions] Herceptin can cause fetal harm when
administered to a pregnant woman. Post-marketing case
reports suggest that Herceptin use during pregnancy
increases the risk for oligohydramnios during the second
and third trimester. If Herceptin is used during pregnancy
or if a woman becomes pregnant while taking Herceptin,
she should be apprised of the potential hazard to a fetus. In
the postmarketing setting, oligohydramnios was reported
in women who received Herceptin during pregnancy, either
alone or in combination with chemotherapy. In half of these
women, amniotic fluid index increased after Herceptin
was stopped. In one case, Herceptin was resumed after
the amniotic fluid index improved, and oligohydramnios
recurred. Women using Herceptin during pregnancy should
be monitored for oligohydramnios. If oligohydramnios
occurs, fetal testing should be done that is appropriate for
gestational age and consistent with community standards
of care. Additional intravenous (IV) hydration has been
helpful when oligohydramnios has occurred following
administration of other chemotherapy agents, however the
effects of additional IV hydration with Herceptin treatment
are not known. Reproduction studies in cynomolgus
monkeys at doses up to 25 times the recommended weekly
human dose of 2 mg/kg trastuzumab have revealed no
evidence of harm to the fetus. However, HER2 protein
expression is high in many embryonic tissues including
cardiac and neural tissues; in mutant mice lacking HER2,
embryos died in early gestation. Placental transfer of
trastuzumab during the early (Days 20-50 of gestation) and
late (Days 120-150 of gestation) fetal development period
was observed in monkeys. [See Nonclinical Toxicology]
Because animal reproduction studies are not always
predictive of human response, Herceptin should be used
during pregnancy only if the potential benefit to the mother
justifies the potential risk to the fetus. Registry Pregnant
women with breast cancer who are using Herceptin are
encouraged to enroll in MotHER- the Herceptin Pregnancy
Registry: phone 1-800-690-6720. Nursing Mothers It is not
known whether Herceptin is excreted in human milk, but
human IgG is excreted in human milk. Published data
suggest that breast milk antibodies do not enter the
neonatal and infant circulation in substantial amounts.
Trastuzumab was present in the breast milk of lactating
cynomolgus monkeys given 12.5 times the recommended
weekly human dose of 2 mg/kg of Herceptin. Infant
monkeys with detectable serum levels of trastuzumab did
not have any adverse effects on growth or development
from birth to 3 months of age; however, trastuzumab levels
in animal breast milk may not accurately reflect human
breast milk levels. Because many drugs are secreted in
human milk and because of the potential for serious
adverse reactions in nursing infants from Herceptin, a
decision should be made whether to discontinue nursing,
or discontinue drug, taking into account the elimination halflife of trastuzumab and the importance of the drug to the
mother. Pediatric Use The safety and effectiveness of
Herceptin in pediatric patients has not been established.
Geriatric Use Herceptin has been administered to 386
patients who were 65 years of age or over (253 in the
adjuvant treatment and 133 in metastatic breast cancer
treatment settings). The risk of cardiac dysfunction was
increased in geriatric patients as compared to younger
patients in both those receiving treatment for metastatic
disease in Studies 5 and 6, or adjuvant therapy in Studies 1
and 2. Limitations in data collection and differences in study
design of the 4 studies of Herceptin in adjuvant treatment
of breast cancer preclude a determination of whether the
toxicity profile of Herceptin in older patients is different from
younger patients. The reported clinical experience is not
adequate to determine whether the efficacy improvements
(ORR, TTP, OS, DFS) of Herceptin treatment in older patients
is different from that observed in patients <65 years of
age for metastatic disease and adjuvant treatment.
OVERDOSAGE There is no experience with overdosage in
human clinical trials. Single doses higher than 8 mg/kg have
not been tested. PATIENT COUNSELING INFORMATION
• Advise patients to contact a health care professional
immediately for any of the following: new onset or
worsening shortness of breath, cough, swelling of the
ankles/legs, swelling of the face, palpitations, weight gain
of more than 5 pounds in 24 hours, dizziness or loss of
consciousness [see Boxed Warning: Cardiomyopathy].
• Advise women with reproductive potential to use
effective contraceptive methods during treatment and for
a minimum of six months following Herceptin [see
Pregnancy]. • Encourage pregnant women who are using
Herceptin to enroll in MotHER- the Herceptin Pregnancy
Registry [see Pregnancy].
HERCEPTIN® [trastuzumab]
Manufactured by:
4839803
Genentech, Inc.
Initial US Approval: Sept. 1998
1 DNA Way
Revision Date: March 2009
South San Francisco, CA
LK0726 7172911
94080-4990
7172713
©2009 Genentech, Inc.
Inside
OCTOBER 2009
NEWS&
FORUM
AMERICAN SOCIETY OF CLINICAL ONCOLOGY
FEATURES
COVER PHOTOGRAPH BY BILL WIPPERT
22
FORUM: CURRENT CONTROVERSIES IN ONCOLOGY
$EUDKDP+'DFKPDQ0'+HPDQW.5R\0'DQG0LFKDHO-*ROGEHUJ
0'GHEDWHWKHXVHRIRSWLFDOFRORQRVFRS\YHUVXV&7FRORQRJUDSK\WRGHWHFW
SUHFDQFHURXVDQGFDQFHURXVSRO\SV
26
BUILDING A DIVERSE WORKFORCE
32
ASCO RINGS THE NYSE BELL
34
MEMBERS ONLY
36
ASCO CONTINUES SUCCESSFUL LEADERSHIP
DEVELOPMENT PROGRAM
38
EXPERT ANALYSIS
40
SCIENTIFIC HIGHLIGHTS FROM OTHER MEETINGS
43
CLINICAL INVESTIGATOR TEAM LEADERSHIP AWARD
26
7KH$6&2'LYHUVLW\LQ2QFRORJ\,QLWLDWLYHLVGHVLJQHGWRKHOSUHFUXLWDQG
UHWDLQLQGLYLGXDOVIURPSRSXODWLRQVXQGHUUHSUHVHQWHGLQWKHILHOGRIRQFRORJ\
DQGHQFRXUDJHVRQFRORJLVWVWRSUDFWLFHLQXQGHUVHUYHGFRPPXQLWLHV
2Q$XJXVW7KH$6&2&DQFHU)RXQGDWLRQDQG$6&2MRLQHGWKHUDQNVRIWKH
PDQ\QRWDEOHEXVLQHVVHVRUJDQL]DWLRQVDQGFHOHEULWLHVWKDWKDYHUXQJWKH1HZ
<RUN6WRFN([FKDQJH·V&ORVLQJ%HOO
32
$6&21HZV )RUXPFRQWLQXHVLWVVHULHVDERXWWKHEHQHILWVRI$6&2
PHPEHUVKLSZLWKDIRFXVRQ$QQXDO0HHWLQJUHJLVWUDWLRQDQGKRXVLQJEHQHILWV
'HVLJQHGWRSURYLGHDQRULHQWDWLRQWR$6&2DVZHOODVOHDGHUVKLSWUDLQLQJVNLOOVWR
HPHUJLQJRQFRORJLVWVWKH/HDGHUVKLS'HYHORSPHQW3URJUDPSURYLGHVSDUWLFLSDQWV
ZLWKH[WHQVLYHH[SRVXUHWRWKHUROHVDQGPLVVLRQRI$6&2DQGWKH6RFLHW\·V
SRZHUIXOSODFHLQGHYHORSLQJWKHIXWXUHRIFDQFHUFDUH
8SGDWHIURPWKH$6&2$QQXDO0HHWLQJ
/%$(IILFDF\UHVXOWVIURPWKH7R*$WULDO$SKDVH,,,VWXG\RIWUDVWX]XPDE
DGGHGWRVWDQGDUGFKHPRWKHUDS\LQILUVWOLQHKXPDQHSLGHUPDOJURZWKIDFWRU
UHFHSWRU +(5 SRVLWLYHDGYDQFHGJDVWULFFDQFHU *& 36
7KH&DQFHUDQG/HXNHPLD*URXS% &$/*% KHOGLWV6XPPHU*URXS
0HHWLQJLQ&KLFDJR,OOLQRLVWKHWK,QWHUQDWLRQDO/XQJ&DQFHU&RQJUHVVWRRN
SODFHLQ.RKDOD&RDVW+DZDLL
$QHZDZDUGSURYLGHVIXQGLQJIRUDQGUHFRJQLWLRQRIFOLQLFDOLQYHVWLJDWRUVZKR
OHDGFDQFHUUHVHDUFKSURJUDPVDWDFDGHPLFFDQFHUFHQWHUV
ASCO NEWS & FORUM |
7
UP FRONT
9
10
17
18
19
20
NEWS&FORUM
OCTOBER 2009 VOLUME 4, NO. 4
Editorial
Letter to the Editor
EDITOR IN CHIEF
From the President
Jonathan S. Berek, MD, MMS
Call for Annual Meeting Abstracts
Stanford University School of Medicine
Stanford Cancer Center
Stanford, California
Leadership Perspectives
The ASCO Cancer Foundation®
44
48
53
EDITORIAL BOARD
Al B. Benson III, MD, FACP
Alan Sandler, MD
Robert H. Lurie Comprehensive Cancer
Center of Northwestern University
Vanderbilt University Medical Center
S. Gail Eckhardt, MD
Baylor University Medical Center
Marvin J. Stone, MD
University of Colorado Denver
Jamie H. Von Roenn, MD
Stuart A. Grossman, MD
Northwestern University
The Sidney Kimmel
Comprehensive Cancer Center
Antonio C. Wolff, MD, FACP
Melissa M. Hudson, MD
St. Jude Children’s Research Hospital
The Sidney Kimmel Comprehensive
Cancer Center at Johns Hopkins
Robert G. Mennel, MD
NEWS
44
45
46
48
50
51
52
53
54
Texas Oncology PA
ASSOCIATE EDITOR
What’s New in Policy & Practice
Joseph S. Bailes, MD
Houston, Texas
Inside JCO
JOP Outlook
What’s New in Policy & Practice
International Insight
Research Issues & Resources
Spotlight on Education
Focus on Fellows & Junior Faculty
For Your Patients
Membership Notes
PUBLISHER
GRAPHIC DESIGNER
MANAGING EDITOR
PRODUCTION COORDINATOR
ART DIRECTOR
ADVERTISING REPRESENTATIVE
Lisa G. Greaves
Lauren Evoy Davis
Leigh Hubbard
EDITORIAL STAFF
Virginia Anderson
Elyse Blye
Carrie Gann
Kirsten Sihlanick
John M. Otte
Kevin Dunn
Vice President
Cunningham Associates
201-767-4170
kdunn@cunnasso.com
ASCO News & Forum (ISSN 1931-7646) is published by the American Society of Clinical Oncology
and is issued quarterly. This magazine may not be reproduced, in whole or in part, without written
permission from the publisher. The American Society of Clinical Oncology assumes no responsibility for
errors or omissions in this publication. It is the responsibility of the treating physician or other health
care professional, relying on independent experience and knowledge of the patient, to determine drug
dosages and the best treatment for the patient.
ASCO News & Forum is indexed in the Cumulative Index to Nursing and Allied Health Literature®
(CINAHL®) print index and the CINAHL® database.
For reference purposes, articles herein may be cited in the following format:
“Article title.” ASCO News & Forum. Year; Volume, Number, Page.
ONLINE EXCLUSIVES
ASCO News & Forum is pleased to present
additional content online at asconews.org.
Recently Published Articles
Q Family of Websites: ASCO University™
Q Spotlight On: West Virginia Oncology Society
Q Tribute: William A. Knight, III, MD
8 | OCTOBER 2009
ASCO News & Forum is printed on recycled paper.
ASCO News & Forum received a 2009 APEX Award of Excellence.
© 2009 American Society of Clinical Oncology
ASCO News & Forum Mission Statement
ASCO News & Forum represents the interests and expertise of the members of the American Society
of Clinical Oncology and others in the oncology community. The publication, available in print and
electronic media, is the primary source of information about ASCO programs, benefits, and resources.
The publication also provides summaries of research from oncology-related meetings and the
literature (especially the Journal of Clinical Oncology), including commentary on controversial issues by
recognized experts in the field.
UP FRONT
(GLWRULDO
Lifesaving Legislation
By Jonathan S. Berek, MD, MMS
Editor, ASCO News & Forum
P
revention
is the best
medicine.
Oncologists would
be happy to see
fewer patients
being treated for
preventable illnesses, cancers
caused by tobacco use being chief among them. So it was
thrilling to see the United States Senate
approve the Family Smoking Prevention
and Tobacco Control Act on June 22,
2009. This legislation hampers the ability
of tobacco marketers to target children
and young adults in the places where they
learn and play, and prevents manufacturers from adding kid-friendly candy flavorings to mask the tobacco’s natural smoky
taste. It also prohibits misleading terms
such as “light” and “low-tar” that may
have led consumers to think one type of
cigarette was safer than another.
“The U.S. Senate has taken an important step forward in allowing the federal
government to counter Big Tobacco’s
100-year assault on public health,” said
ASCO President Douglas W. Blayney, MD,
in a statement about the historic vote.
Dr. Blayney attended the signing of the
legislation.
President Obama called the legislation
“change that has been decades in the
making.”
More than 400,000 Americans die
of tobacco-related illnesses each year,
making it the leading cause of preventable death in the United States. With
the passing of this legislation, we hope
to be leaders in ending needless death.
Oncologists can help accomplish this goal
by addressing tobacco usage with current patients and spreading the message
to young people before they pick up the
habit. By focusing on prevention, perhaps
the United States can use the $1 billion
per year that is currently being spent on
tobacco-related illness for research to
study cancers that are not currently preventable.
Change has been afoot for some years
but progress has been slow, even after
the U.S. Surgeon General declared cigarettes and tobacco products as harmful to
one’s health in 1964. This year, you won’t
see Santa Claus promoting Lucky Strikes
during the holiday season; the iconic cartoon Joe Camel has been retired for more
than a decade; and the Virginia Slims ads
informing the modern woman, “You’ve
come a long way, baby,” seem outdated,
if not outright condescending. With the
new legislation, the placement of tobacco
advertising that the U.S. Food & Drug
Administration (FDA) deems acceptable
will be more restricted than ever.
Although many people have quit, young
people continue to light up. Currently,
one in five high school students graduate
not only with a diploma but with a casual
cigarette habit that could blossom into
a full-blown addiction. As someone who
struggles to quit smoking cigarettes him-
self, President Obama knows firsthand
the difficulty in giving up tobacco.
Lung cancer is only one of 15 cancer types that is directly attributable to
tobacco usage.
Death from tobacco-related cancers is
preventable. If fewer people start smoking, fewer people will be later diagnosed
with tobacco-related illnesses and cancer.
This historic legislation is positive for
ASCO, oncologists, and the public.
ASCO has long been involved in ending tobacco usage. ASCO Past President
Paul A. Bunn, Jr., MD, (2002-2003)
spearheaded the development of ASCO’s
Statement on Tobacco Control, a policy
statement that promotes a comprehensive effort to address all elements of
the tobacco problem, including reducing
tobacco use among youth, requiring disclosure of ingredients in tobacco products, and increasing research on tobacco
addiction and prevention strategies, with
the ultimate goal of achieving a tobaccofree world.
This isn’t the end of the fight to end
tobacco usage but is one of many moves
to help improve the health of the American public.
President Obama concluded his June
22 speech with the apt aphorism previously quoted by Representative Henry
Waxman (D-CA), who introduced the legislation: A journey of 1,000 miles begins
with a single step.
ASCO NEWS & FORUM |
9
UP FRONT
/HWWHUWRWKH(GLWRU
The following letter was submitted to ASCO News & Forum in response to the U.S. presidential election and the changes in health
care that may result during the new administration. The views and opinions expressed are those of the authors alone and do not
necessarily reflect the views or positions of the Editor or of the American Society of Clinical Oncology.
Sixty Years of Free
Medical Care
In the United Kingdom (U.K.) we watch
with interest as President Obama works to
expand health care coverage while reducing costs. Last year our nation marked
the 60th anniversary of the creation of
the National Health Service (NHS). Its
purpose was to guarantee people of the
U.K. any type of health care they needed
at no immediate cost, irrespective of the
patient’s income.
Monies available to U.K. health care are
predetermined by Her Majesty’s Treasury.
The Department of Health in turn disburses its budget to the bodies that operate the NHS. The NHS relies on general
practitioners (GPs) to contain costs. GPs
are proud of their roles as gatekeepers.
Referral of patients is reserved for situations in which a specialist’s diagnostic
expertise or more than the most minor of
surgical procedures is required. GPs are
contracted to Primary Care Trusts, which
control the bulk of NHS planning. Their
referral management offices vet all specialist referrals except for referrals made
when GPs suspect cancer.
Revised criteria for suspicion of cancer
were published in 2005.1 Patients with
obvious symptoms, for example, postmenopausal bleeding, will have their first
specialist appointment within two weeks.
GPs have successfully administered the
longest established screening service
for pathology of the uterine cervix. As
a result, the U.K.’s performance in the
diagnosis and treatment of cervical and
endometrial cancers is quite good. It is
not good for ovarian cancer where the
presenting symptoms are ambiguous and
capacity for their investigation is limited.
10 | JANUARY 2009
Patients’ socioeconomic status has a
great bearing on health outcomes. Access
to medical care is free at the point of use;
it does not depend on wealth. Wealthier
patients still receive diagnoses and
treatments for cancer much more effectively than other groups. If the U.K. is to
improve cancer survival, it must address
the recruitment of primary care staff in
deprived areas so that cancer in underserved patients can be diagnosed and
treated in a timely manner.
NHS doctors’ gatekeeping also diminishes the perception of demand. When I
started work in a District General Hospital
(DGH) two decades ago, the purpose of
my service was questioned. The visiting
radiotherapist and oncologist said that to
spend one day per week at the hospital
was “sufficient for the present rate of
referrals.” Unfortunately, the gatekeeping
attitude required of all services made this
perfectly true. As medical oncology and
clinical oncology (clinical oncologists practice radiotherapy) services have increased
in the last few years, more needs have
been recognized.
As the young NHS streamlined its
organization, three specific services were
centralized. Neurosurgery was already
centralized. Regional radiotherapy centers
were established and smaller units were
closed. Thoracic surgery was restricted
to a limited number of hospitals. The
distance between the patient’s residence
and the thoracic surgery or radiotherapy
facility affects one’s likelihood of receiving
such interventions for lung cancer.2 Yet
these facilities have insufficient capacity
to cope with their current patient loads.
While specialist services were centralized, the many small hospitals that the
NHS absorbed were condensed into a
smaller number of DGHs. The hospital
where I work opened in 1970. In its 650
beds and outpatient facilities, it then provided all the internal medicine, general
surgery, and obstetrics and gynecology
services for approximately 175,000 people. Over time, the number of beds available to the population has shrunk with
the closure of the outlying hospitals that
provided longer-term and convalescence
services. Currently, beds at the main hospital are being closed, but the number of
specialists is increasing. The hospital now
serves approximately 210,000 people
and functions in a very multidisciplinary
manner.
Current thinking at the NHS requires
more specialized services to be provided
in a few large centers with distribution
of other services to community facilities based around GPs, not specialists.
Gatekeeping is inherent in this system to
match demand for centralized specialized
services to capacity.
DGHs fit neither the commitment to
locate more services close to home nor
the pledge to centralize specialist services. Recent cancer planning strategies
envision satellite clinics delivering chemotherapy close to, or within, patients’
homes, while doctors who prescribe it are
based in the academic hospitals some
distance away, perhaps establishing visiting clinics in DGHs. Having a medical
oncology team based in a DGH is still very
unusual in the NHS, but the idea is now
finding favor.
Medicare data from U.S.-based
research showed that outcomes for ovarian cancer surgery are slightly superior
in the hospitals that were designated as
“large.”3 Comparable data for NHS DGHs
show that their workloads also would
categorize the majority of them as large.4
For economically challenged parts of
society, financial barriers to treatment are
absolute. Few within the U.K. doubt that
the “free at the point of need” NHS is the
best way to overcome these obstacles.
Such a service must be funded sufficiently to have the necessary capacity
or, as the NHS illustrates, its aims will be
defeated. Its facilities must be distributed
widely to facilitate access; the DGH is a
good starting point. If the Treasury balks
at the cost of this, I see no reason to
discourage wealthy patients from fund-
ing medical care privately, but the extra
benefit they gain must be similar to the
benefit of flying first class. The aircraft
takes off and lands at exactly the same
time but the circumstances in which one
travels are merely more comfortable than
economy class. So in cancer care, the
quality of the medicine must be the same
for all, but luxuries may differ.
Response: Reforming
Cancer Care: What
Can We Learn from the
United Kingdom?
specialists than is the case in the United
States. It appears that cancer prevention strategies that are of proven worth
are widely disseminated, and are to be
admired.
However, the regionalization of specialized services in the United Kingdom has
in some instances the effect of limiting
access to those services by reason of
geographical misdistribution. For example,
Dr. Crawford asserts that not all patients
with lung cancer can get to the specialized regional centers for radiation therapy
or thoracic surgery. Furthermore, these
regional facilities are of insufficient size,
so that over time they have become
overloaded and cannot effectively meet
the demand. He argues for a broader
distribution of cancer care services, both
in District General Hospitals (DGH) and in
satellite clinics. The latter are apparently
slow in coming. There is much for us to
learn from this.
The evolution of the U.S. health system
has led to far less reliance on primary
care physicians (PCPs) and far more use
of specialists, leading to escalating costs
and misdistribution of resources. This
is almost the opposite of the scenario
described in the U.K. Where do we go
from here? Clearly, for cancer care, the
answer is not that fewer oncologists are
needed; indeed, our aging population
causes us to project the need for an
enlarging labor force that must be broadly
distributed throughout the nation. However, we are obligated to make changes
in the system that provide for several
As the largest organization representing
U.S.-based oncologists, ASCO is vitally
interested in promoting changes in the
health system that support the goals of
ensuring equal access to high-quality
cost-effective cancer care for all patients.
It is a matter of record that the current
health care system in the United States
is more costly than those of most major
industrialized nations, and suffers from
great inequities in access to care.
Juxtaposed against these problems is
the reality that U.S. health care is second
to none in delivering highly technical care
for diseases such as cancer. The problem
we face is how to distribute the proper
care to the appropriate patient in a way
that is equitable, economically sound, and
uniform in quality.
Dr. Crawford, in his essay “Sixty Years
of Free Medical Care,” cites the obvious
and welcome achievement of the U.K.
National Health Service, which is universal availability of health care, independent
of an individual’s income. Not surprisingly,
he observes that the reliance on primary
care physicians as gatekeepers is at the
same time one of the great strengths of
the program and one of its weaknesses.
There is little doubt that this system has
facilitated broad access to care and has
done so with far more limited use of
—S. Michael Crawford, MD, FRCP
Consultant Medical Oncologist
Airedale General Hospital
United Kingdom
References
1. National Institute for Clinical Excellence. Clinical
Guideline 27, Referral guidelines for suspected
cancer. London, NICE 2005.
2. Jones AP, Haynes R, Sauerzapf V, et al. Travel
time to hospital and treatment for breast, colon,
rectum, lung, ovary and prostate cancer. Eur J
Cancer. 2008;44:992-9.
3. Schrag D, Earle C, Xu F, et al. Associations
between hospital and surgeon procedure volumes
and patient outcomes after ovarian cancer
resection. Natl Cancer Inst. 2006;98:163-71.
4. Cancer treatment policies and their effects on
survival – ovary. Key Sites Study 8. Northern &
Yorkshire Cancer Registry and Information Service,
Leeds, 2002. http://www.nycris.org.uk.
absolute goals. One is the oft-stated goal
of ASCO that every patient with cancer
must have ready access to state-of-theart cancer care regardless of the ability to
pay. A second is that cancer care must be
evidence-based, and reflect contemporary
assessments of the best available therapies defined in terms of clinical benefit,
quality of life, and cost. We have shied
away from defining value in cancer care,
but that luxury is no longer extant.
To achieve these aims, the system
for cancer care will have to change. The
oncology community represented by
ASCO must collaborate with like-minded
organizations, patient advocates, and
the government to develop policies that
assure optimal delivery of care in a clinical environment that supports high-quality
providers. Incentives for all the stakeholders in cancer care must become better
aligned. These include cancer clinicians,
our patients, the pharmaceutical industry,
and insurers. Instead of four occasionally
overlapping circles, these critical elements must be forged into a well-coordinated series of interwoven components
whose primary focus is the well-being of
the patient.
—Lowell E. Schnipper, MD
Theodore and Evelyn Berenson Professor
of Medicine
Harvard Medical School
Chief, Hematology/Oncology Division
Beth Israel Deaconess Medical Center
ASCO NEWS & FORUM |
11
""
!!""!""!%"
"!""!%" *(
##""
!!"
*(
Break Down
Down
Break
the Risk
Risk
the
*FRAGMIN is indicated for the extended treatment of symptomatic venous thromboembolism (VTE)
(proximal deep vein thrombosis [DVT] and/or pulmonary embolism [PE]), to reduce the recurrence
is
of VTE
inindicated
patients with
cancer.
*FRAGMIN
for the
extended treatment of symptomatic venous thromboembolism (VTE)
(proximal deep vein thrombosis [DVT] and/or pulmonary embolism [PE]), to reduce the recurrence
of VTE in patients with cancer.
Please see Important Safety Information, including the boxed warning
for spinal/epidural hematomas, on the third page of this ad.
Please see Important Safety Information, including the boxed warning
Please see briefhematomas,
summary of prescribing
information
for spinal/epidural
on the third
page of following
this ad. this ad.
References: 1.%%
%6).% !+%2%4!,&/24(%!.$/-):%$/-0!2)3/./&/7/,%#5,!2%)'(4%0!2).%23532!, .4)#/!'5,!.4(%2!09&/24(%
Please2%6%.4)/./&%#522%.4%./53(2/-"/%-"/,)3-).!4)%.437)4(!.#%2.6%34)'!4/23/7-/,%#5,!27%)'(4(%0!2).6%2353!#/5-!2).&/24(%02%6%.4)/.
see brief summary of prescribing information following this ad.
/&2%#522%.46%./534(2/-"/%-"/,)3-).0!4)%.437)4(#!.#%2N Engl J Med 2.!4!/.>,%)3!).#3. 2%3#2)").'.&/2-!4)/.
References:
%6).% !+%2%4!,&/24(%!.$/-):%$/-0!2)3/./&/7/,%#5,!2%)'(4%0!2).%23532!,
.4)#/!'5,!.4(%2!09&/24(%
1.%%
C/-0!2)3/./&L/7/,%#5,!2%)'(4%0!2).6%2353O2!,
.4)#/!'5,!.4(%2!09&/24(%2%6%.4)/./&%#522%.4%./53T(2/-"/%-"/,)3-).!4)%.437)4(
!.#%2 !2!.$/-):%$02/30%#4)6%-5,4)#%.4%2/0%.,!"%, -/.4(42)!,#/.3)34).'/& 0!4)%.437)4(!#4)6%#!.#%2!.$.%7,9$)!'./3%$4(2/-"/%-"/,)#$)3%!3%
2%6%.4)/./&%#522%.4%./53(2/-"/%-"/,)3-).!4)%.437)4(!.#%2.6%34)'!4/23/7-/,%#5,!27%)'(4(%0!2).6%2353!#/5-!2).&/24(%02%6%.4)/.
!*/2",%%$).'7!3$%>.%$!3!.9",%%$).'4(!47!3!##/-0!.)%$"9!$%#2%!3%).(%-/',/")./&≥'$).#/..%#4)/.7)4(#,).)#!,39-04/-3
/##522%$
/&2%#522%.46%./534(2/-"/%-"/,)3-).0!4)%.437)4(#!.#%2N
Engl J Med 2.!4!/.>,%)3!).#3. 2%3#2)").'.&/2-!4)/.
!4!#2)4)#!,3)4%).42!/#5,!230).!,%0)$52!,).42!#2!.)!,2%42/0%2)4/.%!,/20%2)#!2$)!,",%%$).' 2%15)2%$42!.3&53)/./&≥5.)43/&",//$ /2,%$4/$%!4(
C/-0!2)3/./&L/7/,%#5,!2%)'(4%0!2).6%2353O2!, .4)#/!'5,!.4(%2!09&/24(%2%6%.4)/./&%#522%.4%./53T(2/-"/%-"/,)3-).!4)%.437)4(
!.#%2 !2!.$/-):%$02/30%#4)6%-5,4)#%.4%2/0%.,!"%, -/.4(42)!,#/.3)34).'/& 0!4)%.437)4(!#4)6%#!.#%2!.$.%7,9$)!'./3%$4(2/-"/%-"/,)#$)3%!3%
!*/2",%%$).'7!3$%>.%$!3!.9",%%$).'4(!47!3!##/-0!.)%$"9!$%#2%!3%).(%-/',/")./&≥'$).#/..%#4)/.7)4(#,).)#!,39-04/-3 /##522%$
!4!#2)4)#!,3)4%).42!/#5,!230).!,%0)$52!,).42!#2!.)!,2%42/0%2)4/.%!,/20%2)#!2$)!,",%%$).' 2%15)2%$42!.3&53)/./&≥5.)43/&",//$ /2,%$4/$%!4(
#!./##5
FRAGM
#!./#
.!#,).
4/FRAGM
-/
/##522%
.!#,
4(!.
!.!$6%
4/ ).4(%/
/##522
0!4)%.43
4(!.
!.!$6
(2/-"
).4(%
4(2/-"/
0!4)%.
/&4()3#
4(2/-"/
(2/-
4(2//&4()3
4(2/-
*"'%)# %" $ "&"
*"'%)#
%" $ "&"
" ""!%"
"" ""!%"
" ""
(%,!.$-!2+
45$9 45$9
(%,!.$-!2+ Probability
VTE at months
(P=)
Probability of recurrent
VTE atof recurrent
months (P=)
&WFOUT5PUBMT
K
K
FRAGMIN
Warfarin
FRAGMIN
Warfarin
Patients
at risk
Patients
at risk
1SPCBCJMJUZPG
SFDVSSFOU75& 1SPCBCJMJUZPG
SFDVSSFOU75& &WFOUT5PUBMT
K
K
8BSGBSJO
'3"(.*/
8BSGBSJO
'3"(.*/
%BZTQPTUSBOEPNJ[BUJPO
%BZTQPTUSBOEPNJ[BUJPO
!""!"'!+" "$ ! #"$!% !""!"'!+" "$ ! #"$!% $+' $!% $ "!"#'
$+
'
$!% $ "!"#'
<Impressive reduction
in recurrent
VTE637!2&!2).).).4%.44/42%!40/05,!4)/.
).#)$%.#%2!4%7)4( 63 7)4(7!2&!2).
<Impressive reduction in recurrent VTE637!2&!2).).).4%.44/42%!40/05,!4)/.
).#)$%.#%2!4%7)4(
63
7)4(7!2&!2).
<Comparable incidence
/&!.9",%%$).'7)4( 637!2&!2).
/6%2 -/.4(3P <C
omparable incidence/&!.9",%%$).'7)4( 637!2&!2).
= .9",%%$).'!,3/).#,5$%$-!*/2",%%$).' 7)4( 63 7)4(7!2&!2).
/6%2 -/.4(3P =.%",%%$).'%6%.4(%-/0493)3).!0!4)%.4).4(% !2-!4$!9
7!3&!4!,
= .9",%%$).'!,3/).#,5$%$-!*/2",%%$).' 7)4( 63 7)4(7!2&!2).
=.%",%%$).'%6%.4(%-/0493)3).!0!4)%.4).4(% !2-!4$!9 7!3&!4!,
,)+%/4(%2!.4)#/!'5,!.433(/5,$"%53%$7)4(%842%-%#!54)/.).0!4)%.437(/(!6%!.).#2%!3%$2)3+/&(%-/22(!'% ",%%$).'
#52!4!.93)4%$52).'4(%2!09 .5.%80%#4%$$2/0).(%-!4/#2)4/2",//$02%3352%3(/5,$,%!$4/!3%!2#(&/2!",%%$).'3)4%
used
,)+%/4(%2!.4)#/!'5,!.433(/5,$"%53%$7)4(%842%-%#!54)/.).0!4)%.437(/(!6%!.).#2%!3%$2)3+/&(%-/22(!'%
",%%$).'
MIN should be
with
extreme caution in patients with history of heparin-induced thrombocytopenia.
#!./##52!4!.93)4%$52).'4(%2!09 .5.%80%#4%$$2/0).(%-!4/#2)4/2",//$02%3352%3(/5,$,%!$4/!3%!2#(&/2!",%%$).'3)4%
.)#!,42)!,/&0!4)%.437)4(#!.#%2!.$!#54%39-04/-!4)#42%!4%$&/250
/.4(3).4(%
42%!4-%.4!2-0,!4%,%4#/5.43/&<-FRAGMIN
should be used with extreme caution in patients
with history of heparin-induced thrombocytopenia.
%$). /&0!4)%.43).#,5$).' 7(/!,3/(!$0,!4%,%4#/5.43,%33
.!#,).)#!,42)!,/&0!4)%.437)4(#!.#%2!.$!#54%39-04/-!4)#42%!4%$&/250
-- .4(%3!-%#,).)#!,42)!,4(2/-"/#94/0%.)!7!32%0/24%$!3
42%!4-%.4!2-0,!4%,%4#/5.43/&<-
4/ -/.4(3).4(% %23%%6%.4)./&0!4)%.43).4(%
!2-!.$/&0!4)%.43
$/3%7!3$%#2%!3%$/2).4%22504%$).
/2!,!.4)#/!'5,!.4!2-
/##522%$). /&0!4)%.43).#,5$).'
7(/!,3/(!$0,!4%,%4#/5.43,%33
437(/3%0,!4%,%4#/5.43&%,,"%,/7-
4(!. -- .4(%3!-%#,).)#!,42)!,4(2/-"/#94/0%.)!7!32%0/24%$!3
!.!$6%23%%6%.4)./&0!4)%.43).4(% !2-!.$/&0!4)%.43
"/#94/0%.)!/&!.9$%'2%%3(/5,$"%-/.)4/2%$#,/3%,9%0!2).).$5#%$
).4(%/2!,!.4)#/!'5,!.4!2- $/3%7!3$%#2%!3%$/2).4%22504%$).
"/#94/0%.)!#!./##527)4(!$-).)342!4)/./&
(%).#)$%.#%
/.
0!4)%.437(/3%0,!4%,%4#/5.43&%,,"%,/7-#/-0,)#!4)/.)35.+./7.!402%3%.4.#,).)#!,02!#4)#%2!2%#!3%3/& "/#94/0%.)!7)4(4(2/-"/3)3(!6%!,3/"%%./"3%26%$
(2/-"/#94/0%.)!/&!.9$%'2%%3(/5,$"%-/.)4/2%$#,/3%,9%0!2).).$5#%$
(
!3%
(
4(2/-"/#94/0%.)!#!./##527)4(!$-).)342!4)/./& (%).#)$%.#%
/&4()3#/-0,)#!4)/.)35.+./7.!402%3%.4.#,).)#!,02!#4)#%2!2%#!3%3/&
4(2/-"/#94/0%.)!7)4(4(2/-"/3)3(!6%!,3/"%%./"3%26%$
B: 11.25 in
7/0!4)%.43).%!#('2/507%2%%8#,5$%$&2/-4(%%&>#!#9!.!,93)3"%#!53%4(%9$)$./4%80%2)%.#%!15!,)&9).'4(2/-"/4)#%6%.4
T: 10 in
S: 10 in
!0,!.%)%202/"!"),)49%34)-!4%!:!2$2!4)/ #/.>$%.#%).4%26!, 4/ ? .%6%.47!3$%>.%$!3!./"*%#4)6%,96%2)>
!0,!.%)%202/"!"),)49%34)-!4%!:!2$2!4)/
#/.>
$%.#%).4%26!,
4/ %$39-04/-!4)#%0)3/$%/&2%#522%.4,,
/2"/4($52).'4(%
-/.4(345$90%2)/$
;.4%.44/42%!40/05,!4)/.
? .%6%.47!3$%>.%$!3!./"*%#4)6%,96%2)>%$39-04/-!4)#%0)3/$%/&2%#522%.4,, /2"/4($52).'4(% -/.4(345$90%2)/$
7/0!4)%.43).%!#('2/507%2%%8#,5$%$&2/-4(%%&>
;.4%.44/42%!40/05,!4)/. #!#9!.!,93)3"%#!53%4(%9$)$./4%80%2)%.#%!15!,)&9).'4(2/-"/4)#%6%.4
Important Safety Information
SPINAL/EPIDURAL HEMATOMAS
%"++"2/5&)+"01%"0&"-&!2/)0-&+)+"01%"0&,/0-&+)-2+ 12/"&0"*-),6"!-1&"+10+1& ,$2)1"!,/0 %"!2)"!1,"
+1& ,$2)1"!4&1%),4*,)" 2)/4"&$%1%"-/&+0,/%"-/&+,&!0#,/-/"3"+1&,+,#1%/,*,"*,)& ,*-)& 1&,+0/"1/&0(,#!"3"),-&+$
+"-&!2/),/0-&+)%"*1,*4%& % +/"02)1&+),+$1"/*,/-"/*+"+1-/)60&0
%"/&0(,#1%"0""3"+10&0&+ /"0"!61%"20",#&+!4"))&+$"-&!2/) 1%"1"/0#,/!*&+&01/1&,+,#+)$"0&,/61%" ,+ ,*&1+1
20",#!/2$0##" 1&+$%"*,010&002 %0+,+01"/,&!)+1&&+>**1,/6!/2$0 0-)1")"1&+%&&1,/0,/,1%"/+1& ,$2)+10
%"/&0()0,--"/01,"&+ /"0"!61/2*1& ,//"-"1"!"-&!2/),/0-&+)-2+ 12/"
1&"+100%,2)!"#/".2"+1)6*,+&1,/"!#,/0&$+0+!06*-1,*0,#+"2/,),$& )&*-&/*"+1#+"2/,),$& ) ,*-/,*&0"&0+,1"!
2/$"+11/"1*"+1&0+" "00/6
%"-%60& &+0%,2)! ,+0&!"/1%"-,1"+1&)"+"=13"/020/&0("#,/"+"2/5&)&+1"/3"+1&,+&+-1&"+10+1& ,$2)1"!,/1,"
+1& ,$2)1"!#,/1%/,*,-/,-%6)5&0)0,0""WARNINGS, Hemorrhage +!PRECAUTIONS, Drug Interactions
8 &0 ,+1/&+!& 1"!&+-1&"+104&1% 1&3"*',/)""!&+$,/4&1%(+,4+%6-"/0"+0&1&3&161,1%"!/2$%"-/&+,/-,/(-/,!2 10
,/4&1%1%/,*, 61,-"+&00, &1"!4&1%-,0&1&3"+1&-)1")"1+1&,!61"01
81&"+102+!"/$,&+$/"$&,+)+"01%"0&0%,2)!+,1/" "&3" #,/2+01)"+$&+,/+,+:43"*6, /!&)&+#/ 1&,++!
-1&"+104&1% + "/2+!"/$,&+$/"$&,+)+"01%"0&0%,2)!+,1/" "&3" #,/"51"+!"!1/"1*"+1,#06*-1,*1& !2"1,+
&+ /"0"!/&0(,#)""!&+$00, &1"!4&1%1%"!,0$",# /" ,**"+!"!#,/1%"0"&+!& 1&,+0
8 +'" 1&,+&0+,1&+1"+!"!#,/&+1/*20 2)/!*&+&01/1&,+
8 ++,1"20"!&+1"/ %+$")62+&1#,/2+&14&1%2+#/ 1&,+1"!%"-/&+,/,1%"/),4:*,)" 2)/4"&$%1%"-/&+0
8 )&(",1%"/+1& ,$2)+100%,2)!"20"!4&1%"51/"*" 21&,+&+-1&"+104%,%3"+&+ /"0"!/&0(,#%"*,//%$" )""!&+$
+, 2/1+60&1"!2/&+$1%"/-6 +2+"5-" 1"!!/,-&+%"*1, /&1,/),,!-/"002/"0%,2)!)"!1,0"/ %#,/)""!&+$0&1"
8FRAGMIN should be used with extreme caution in patients with history of heparin-induced thrombocytopenia
8+ )&+& )1/&),#-1&"+104&1% + "/+! 21"06*-1,*1& 1/"1"!#,/2-1, *,+1%0&+1%" 1/"1*"+1/*-)1")"1
,2+10,#<**, 2//"!&+ ,#-1&"+10&+ )2!&+$ 4%,)0,%!-)1")"1 ,2+10)"001%+ **+1%"0*"
)&+& )1/&)1%/,*, 61,-"+&40/"-,/1"!0+!3"/0""3"+1&+ ,#-1&"+10&+1%" /*+! ,#-1&"+10&+1%",/)
+1& ,$2)+1/* !,0"40!" /"0"!,/&+1"//2-1"!&+-1&"+104%,0"-)1")"1 ,2+10#"))"),4**
8%/,*, 61,-"+&,#+6!"$/""0%,2)!"*,+&1,/"! ),0")6"-/&+&+!2 "!1%/,*, 61,-"+& +, 2/4&1%!*&+&01/1&,+,#
%"&+ &!"+ ",#1%&0 ,*-)& 1&,+&02+(+,4+1-/"0"+1+ )&+& )-/ 1& "//" 0"0,#1%/,*, 61,-"+&4&1%1%/,*,0&0
%3")0,""+,0"/3"!
8 0%,2)!"20"!4&1% 21&,+&+-1&"+104&1%)""!&+$!&1%"0&01%/,*, 61,-"+&,/-)1")"1!"#" 10 0"3"/")&3"/,/(&!+"6
&+02#= &"+ 6%6-"/1"+0&3",/!&"1& /"1&+,-1%6+!/" "+1$01/,&+1"01&+))""!&+$
8 %*2)1&-)"!,0"3&),# ,+1&+0"+76)) ,%,)0-/"0"/31&3"4%& %%0""+/"-,/1"!1,"00, &1"!4&1%#1)
;0-&+$6+!/,*"<&+-/"*12/"&+#+10 " 20""+76)) ,%,)*6 /,001%"-) "+1 -/"0"/3"!4&1%"+76)) ,%,)
0%,2)!"20"!4&1% 21&,+&+-/"$++14,*"++!,+)6&# )"/)6+""!"!#+1& ,$2)1&,+4&1% &0+""!"!!2/&+$-/"$++ 6
-/"0"/31&3"#/""#,/*2)1&,+00%,2)!"20"!4%"/"-,00&)"
8 0%,2)!"20"!4&1% /"&+-1&"+10/" "&3&+$,/)+1& ,$2)+10-)1")"1&+%&&1,/0+!1%/,*,)61& $"+10" 20",#
&+ /"0"!/&0(,#)""!&+$0""PRECAUTIONS, Laboratory Tests 0-&/&+2+)"00 ,+1/&+!& 1"!&0/" ,**"+!"!&+-1&"+101/"1"!#,/
2+01)"+$&+,/+,+:43"*6, /!&)&+#/ 1&,+0""DOSAGE AND ADMINISTRATION
8 ))"/$& /" 1&,+0&"-/2/&120/0%#"3"/&+'" 1&,+0&1"/" 1&,+2))",20"/2-1&,+
%3", 2//"!//")6 #"4 0"0,#+-%6) 1,&!/" 1&,+0%3"""+/"-,/1"!
8%"*,01 ,**,+)6/"-,/1"!0&!""##" 1&0%"*1,*11%"&+'" 1&,+0&1"
&0/"$&01"/"!1/!"*/(,#=7"/")1%
+!&0)& "+0"!1, &0&+ 9 &0&+ ))/&$%10/"0"/3"!/&+1"!&+ / % /("1"!6 &0&+ L ! ! ! )& # & 3
L )& # & * ! $
1- & ' * & J, ' .J, ( /"
& J, ) & $
K ! " #!
$
1- ) & # ) & * & !" * !" & +
) & * & 1-$ / ! ! ! & & * 1- ! +2+)* " ) & +
! ! ! & & * 1- ' J," # ! ) & & ! 1- & $ / ) & # ) & * & # & ) & 1-$
%& ' & ( & " ! & ! ) & ) ) !& &
& * & # * ! & )& & !+ $ ,& # & * & ) ! & ! & ! +
! & & + ! -. " & " & ! $ ,& #
$ / & 0 ! ! $ ! " ! $ ,&
& & & * # ' * ! +
! & &' !"$
1- $ 1- & ! ) &
& & ) ) !& & $ "%)(");!& !!#!";!
!"$ '#!*!) )( $#!$
1- & &' & ! +2+)* " )& ) & & #$%&!"'" !
#%! !"!"(%!)*+*,$ )!%' !$
1- & &' * & .J," )& & /
L ! ! & !3
- 1-" # & ! " & ) & ' )& &* # & &!" & & ) & * &
" " ! 0 ! +
" * ! ! " & &! #" & " &&+
! !$ #!%#!)%" ;!"" !)"'%;% %;!#!"
#!!)")&!%."#!% #!)%/""!"#!%# ;! "%!%*#
#%$"!"0!":'","!"!;!"'!);%%!#!)% " !"'))!!%
)"'' !""!"" " "."(&)) 1 !'$,!%% /0
) & & ! " ! ! & ) & 1-$ ' & & & ! $
( $#!- 1- !
+ " 4566"666(7 486"666(7 459 459 " *$ & ) & * & : &
& 1- " 4566"666(7 57$:9 " ! :$89 )& & & 86"666(7$ &
" & ) * * 56$;9 & 1- <$59
& = $ 1- ) )& )
566"666(7$ ,& ! & $ > + & ) & & 1-$ ,& & # ) $ "
& ) & & &* *$
!" %%"- & + * 1- ? & * *$ ? & & ) & @1 ! A $ ? & & "
1- * ) & ? & & ) & ! ) $ +
! ) & 1 ! ! " * *+ & " )& $$2 ! '' "$
& ' ) & & %-1- * & & ' !$ 1- & ) & ) & ! & " & +
3 * * # " & * &" ! +
!$ & * & &' " 1- & & $
!"-1- & ) & * ! ! " & " & ! # ! ($""$ " +
" ! +2+)* $
($""-/ " ! " & " ! & ) & 1-$ - ! ! $$"
/,, $ %& &' " ! & / & , /, * / ,& , /,, * * 1- * "
& " ! & ! 1-$ + B & +
! 1-" & ) & * ! ! & ! 1- &$
($" !"-*
, 1- !
+ )& & ) " * 1,(, 1/,(C, ! & & & & ! ) D$E9 D$F9"
*" ! ) & 1-$ & 1- ) & * & ) & 1- : & " +
* " , C," ! & & & & ! ) <$;9 ;$89 " *$ ,& 0 1 7 D , C," &
- = " = , ' = -=+=,= ! " ) 79 7$<9" *$ 1 F"
7 G D &* 5F9 5D9 " *$
!! !$"!"#!'!%!$-.
& ! !+ $ ) ! & , " & ) & & & & $ .
5F66 (#! E6<6 (F & * $
$- $$20, ! ) & * FD66 (#! 5D"5:6 (F ! D<66 (#! D6"<66 (F ! * & & $ ,& " & )*" 0 )+ !+
) $ ) * & " & ! & ! ! $
- ! = @1 ! A &* )& ! ? & &* ;;HD6D !(#!($ ,& ;$8 C & 7$< C + * 1- 5D !(C ? & $
"!"-C * '
& #$ 58 ! ) * ! & +B * #" 0 * #( 46$6F8+6$FFD$ C%> ' )" & " " &
! * & ! # ) $ =
& ' )& 1 ! ) $
)!! "- * &* &$
!! "- & 1-" 885: ) :8 ! FF7E ) E8 $ - * * ) * ) & ! +
$ !! & & # ! ) & !$ / # ! * &* * & 1- ) ! $ = ! * * " ! ) & ) ) !& 4D8 #! & *
3 % !" $
1 -,& & &! ! ) & 1- & )$ ,&
& & $ ,& ! ) & & !&
3 & )*" ! ) & ! "
! ! )
* )&
! 1- 8666 & 1- F866 ) & $ ! 1- 8666 1- F866 ! ! ! ! " & ! * ) D$:9 7$:9" * $ $$ ! 1- 8666 & 8666 ) "
& ! * ) 7$F9 F$E9" * $ $ & ! ! $
"(%!)*+*,$ )!%' !- , < ? ! * & ) &
1-" & " ! +2+)* $
(%7-92%)! ,"!"(%!)*+*,$ )!%' !
)! !
"!!
#!
% (
"(%!)
5
*+*,
5F6 (#!(5F &$ $$
$*$ $$F
* 5F & $$
9
9
9
! * 7"D
58(5D;E 5$6
E(E75 5$6
D(E:6 6$8
5, ) 8 < $
F> $*$ D< & " /,, 5$8 F " & 5F"866 $$ * 5F & 8 < $
7 E8 5:8 ! # & ) $
D ! * ) 5 & !
F !(C ) & 3 F ) 0 3 7 ! &3 D !$
!##% $- , ; ? 5 ! * " F & ! * ) & 1- * ! ! " )
" &
) & ! $
(%8-2%)! ,"%%;!!##% $
,"'!)!
,"#!
)! !
"!!
"!!
F
!#
'!
D
#!
#% 8666 5 8666 8666 &
$
$$
9
$$
$$
9
9
9
! * 7
E(FED F$:
5(FE; 6$D
6
7(:; D$7
& ! * 8
> <(FED F$;
8(FE; 5$<
6
6
% > :(FED F$F
6
6
6
> 7(FED 5$5
-
F(:; F$;
E(:; 56$5
5%
! ) & ' 5$D 5$8" ! - ? - ' F$8$
F & )& ! ! $
7 ! * ) 5 & &! ! * " F ) ) & & +
!
F !(C F " 7 !" D * * & &!$
D ) )& ! ! $
8 F9 & ! ) & 1- 8666 $
' & ) & 1- ' * ! * $ ,) & * ) ) & 0 ! " & ) ! & * " ) * ! * !"
) ! !$ - & ' & &! ! $ & & & ! " & ! * ) & ! 7$:9 5<(D;: )& 1- !3 F$89 5F(D<E )& 1- !3 7$59 58(D<; ) & )
$
()!%$- , 56 ? ! * & )& & 1- F866
8666 ! $
(%54-2%)! ,"%%;!()!%$
,"#!
," % ( ,"
)! !
"!!
"!!
"!!
#! #! % ( ()!%
F866 8666 8666 8666 F866 F866 8666 $
) ) $$
$$
$$
$$
$$
$$
$$
$$
9
9
9
9
9
9
9
9
/ *
F:(D8;
7:(D8D
<5(86<
:7(D;<
5D(5<F
57(5<F
<;(56F8 5F8(5677
, 8$E
E$;
58$;
5F$E
E$E
E$5
<$E
5F$5
% 5:(D:E
5<(D:E
5F(86<
:(D;<
F(E;
F(EE
5(5676
D(567;
> 7$D
7$;
F$D
5$F
F$8
F$:
6$5
6$D
F(7;F
7(7;F
D(86<
F(D;<
5(E;
5(E<
F(5676
57(567<
. !
6$8
6$<
6$<
6$D
5$7
5$7
6$F
5$7
5(D::
8(D:D
7:(86:
DE(D;7
<(5EF
F(5ED
7:(56F:
8E(5678
> 6$F
5$5
E$5
;$8
D$E
5$5
7$8
8$8
)! % !";!,%$"! )(!%!$ ! %%""-, 55 ? ! * & ) & * ! $
(%55-2%)! ,"!)! % !";!,%$"! )(!%!$ ! %%""
)! !
"!!
)! % !";!,%$
% (
"! )(!%!$
8666 $$
$$
9
9
! * 5 . 5D
<(5<D< 6$D
6(5<77 6
! * 5 . F5
;(5<D< 6$8
7(5<77 6$F
5 ! * ) 5 ) & !
F !(C ) & 3 F " ( " " !3 7 0 F 3 D 0 ! ! * 3 8 &$
,& & ! * & . F5 ) " ! & &! ) & ! ) & 1- & ! * ! $ ,) & . F5 & ! & & &! & . 88" E5 )
& * ! & 1- & $
!";! ) $#! 1"((%!"
, 5F ? & ) & ! * & & ) & * & $ ! * ) 5 ) & +
!
F !(C ) & 3 F " ( " "
" !3 7 0 F 3 D &$ !
) * ! & !$ & & '+ & " D: 57$:9 & 1- :F 5<$89 & = ' ! * $ !
* & & 1- . E5 ) $
(%56-2%)! ,".9)$/.")##%!/5
)$#!)
F66 (#! '$ 5<"666 $$
1- F66 (#! ' 5<"666 $$
' 5 &" & 586 (#!
' 8+E =
' 5<"666 $$ ' 8 &
: & ! - F+7
- / ) & / ) &
- / ) & / ) &
#
! !
#
! !
9
9
9
9
, ! 77<
5; 8$:
D: 57$:
778
5F 7$:
:F 5<$8
%# 5
77<
D 5$F
58 D$D
778
D 5$F
5F 7$:
%# F+D
77F
; F$E
5E 8$5
7F5
5 6$7
5F 7$E
%# 8+F<
F;E
; 7$6
F: <$<
F:E
< 7$6
D6 58$6
5/ ) & ! ) & * ) & *$ > )*" ) &
! & * ) & * )& & & * $
( $#!--( $#!0
-! ! $$" " &" *" " &* $ ) & &* $ C / & " & +
! * ) & 1- F9
& ! ) & 1-" ) D$89 ) & 1- 8666 * 55$<9 ) & & 8666 ) & ! $ & & " )
5F9 ) & 1- 8666 * 579 ) & & 8666 & $
! ! * # 5;<8" & &* & 58 & ) & ( & +
$ ,& & * ) ! & ! * !
! & $ & & !+ $ & * ) * # ) ?" 0 $
/ +# ! ' # & $ ,& &* & *
! $
1 $#" - ' * ! 1- & &! $ ,& ! & ) * 59 " 5 ! *
566 +B 1- ! * $ 6$8 ! 566 +B 1- +
& /,, F D & & !$ * ) & & +
" & /,, ! & ) ) ! * & $ " & + B * * ? ' :6 E89$ / & # * * ! ) & $ * & * & $ " ! &' " &* ) & " & ! *
)& & 0 & & # * $ " & ! / " /" $ ! 566"666 (#! 1- <9 5(5F )& 86"666 (#! ) +& $ ,& * ! ) & & $
&%$
$$ / D"767":85
* F66E
1-M
! # / ? >& $
# $" % C#" -I 6E:EE
6<6F75
/ F66<
NF66< $
9
0
'
PO
(
/
*
"*3
R
BE
M 4
E
OV %$
s . 0Y
$A G N
I
M
V
GI FRO
KS
8eXk`feXc\m\ekZfdY`e`e^k_\gfn\if]jgfik#jfe^
Xe[jlim`mfij_`gkfiX`j\ZXeZ\iXnXi\e\jjXe[`ejg`iXk`fe%
AN
4H
K_\8d\i`ZXeJfZ`\kpf]:c`e`ZXcFeZfcf^pËjgXk`\ek\[lZXk`fe
n\Yj`k\#:XeZ\i%E\k#`jgifl[kfY\k_\f]ÔZ`XcZc`e`ZXcZXeZ\i
`e]fidXk`fe i\jfliZ\ f] BXc\`[fjZfg\1 8 Z\c\YiXk`fe f]
jlim`mfij_`g# jfe^# Xe[ jgfik% BXc\`[fjZfg\ `j X _fc`[Xp
\ek\ikX`ed\ek mXi`\kp jg\Z`Xc ]\Xkli`e^ Fcpdg`Z jbXk`e^
Z_Xdg`fejXe[>iXddp8nXi[$n`ee`e^dlj`ZXik`jkj%
Gc\Xj\ _\cg lj kf `ejg`i\ k_\ glYc`Z kf c\Xie dfi\ XYflk
\Xicp[\k\Zk`fe#gi\m\ek`feXe[X[mXeZ\j`eZXeZ\iZXi\Yp
\eZfliX^`e^pfligXk`\ekj#]i`\e[jXe[cfm\[fe\jkfnXkZ_
BXc\`[fjZfg\feK_Xebj^`m`e^;Xp#K_lij[Xp#Efm\dY\i)-
]ifd+$,1*'GD<;Kfe=FO%
"DFMFCSBUJPOPGTVSWJWPSTIJQ TPOH BOETQPSU
nnn%ZXeZ\i%e\k
:XeZ\i%E\kYi`e^jk_\\og\ik`j\Xe[i\jfliZ\jf]8J:Fkfg\fgc\c`m`e^n`k_ZXeZ\iXe[
k_fj\n_fZXi\]fiXe[XYflkk_\d%:XeZ\i%E\k`jjlggfik\[YpK_\8J:F:XeZ\i=fle[Xk`fe#
n_`Z_]le[jZlkk`e^$\[^\i\j\XiZ_#gif]\jj`feXc\[lZXk`feXe[gXk`\ek`e]fidXk`fe%
Opt in to Receive the 2010 ASCO Membership Directory
New this year, members must opt in to receive a hard copy version of the 2010
Membership Directory. Members can opt in online by visiting their personalized
page on asco.org, or by indicating on the Membership Directory Update Form.
The 2010 print directories will be mailed in January only to those who opt in.
The online Membership Directory has undergone several enhancements that
make it much more convenient for members. Below are a few examples of the
exciting new additions available online:
Link to list of member’s articles and presentations
Ability to upload a photo
Ability to search by a zip code radius
Advanced search function that can help locate a colleague by specialty
or location, with the option to download his/her contact information to
Microsoft Outlook.
Practice location, academic rank, research involvement, other society
memberships, state/regional affiliate membership
Login today and test drive the new online Membership Directory features. If you have any questions regarding the
Membership Directory, please contact ASCO Member Services at membermail@asco.org.
UP FRONT
)URPWKH3UHVLGHQW
Working Together to Provide Quality Care
“A
dvancing
Quality
through
Innovation” is the
theme around
which we are
building the 2010
Annual Meeting, and which
will guide our
Douglas W. Blayney, MD
Society’s work in
2009-2010 ASCO President
the coming year.
This phrase captures much of what we do
in our professional lives: We start from
a sound base of quality cancer care and
46 years of experience as a professional
Society. Basic, translational, and clinical
research results enhance this care; our
clinical practice is enhanced by ASCO’s
efforts to assist us in measuring the quality of the care we provide; and constant
innovation has resulted in sustained
drops in the cancer death rates during the
last eight years.
Advancing quality is one of ASCO’s
signature programs. The Quality Oncology Practice Initiative (QOPI®), developed
under the leadership of Joseph V. Simone,
MD, is a unique, growing, voluntary program that reaches into both community
and academic practices. This is the only
wide-ranging quality measurement tool
that is oncologist-generated. Measurements can be made during defined
periods twice each year and include
core domains of care, disease-specific
domains, and process-of-care domains.
QOPI continues to grow as a selfassessment and benchmarking tool. As
of the latest measurement round, more
than 400 practices were registered participants and more than 12,000 patient
charts were measured. New this year is a
certification program that will recognize
practices for their quality enhancement
efforts and allow reduced regular chart
abstraction efforts, and concentration
improvement of the structural attributes
of their operation. (For more about QOPI
Certification, see page 46.)
Innovation leading to better care and
treatment of patients with cancer is a
feature of the Journal of Clinical Oncology
(JCO) and the Journal of Oncology Practice (JOP). Under the leadership of Editor
in Chief Daniel G. Haller, MD, JCO has
become the highest impact factor general
oncology journal. (Impact factor is a measure of how often articles in a journal are
cited by other publications). The print version of both Journals will be enhanced by
a growing variety of online and multimedia
offerings. We are committed to delivering timely and appropriate information to
where you deliver patient care, and to the
most convenient learning venues (in your
office, at your study at home, in your car,
at the airport, or wherever you prefer to
learn about the newest and best ways to
care for patients). (For more information
about the JCO impact factor and online
presence, see page 44.)
Our Annual Meeting remains the premier oncology scientific and educational
meeting. Planning for the 2010 meeting
in Chicago has already begun, and we will
continue to present practice-changing
results from clinical and translational
studies performed around the world. The
best, most clinically relevant abstracts
from this meeting will continue to be
reviewed at our Best of ASCO® meetings
in the United States and abroad, directed
toward clinicians who are unable to attend
the Annual Meeting in Chicago. Our popular thematic symposia, focusing on breast
cancer, gastrointestinal malignancies,
genitourinary malignancies, and biomarkers will continue, and will focus on those
of us whose professional efforts are concentrated in these fields. The educational
and scientific information presented is in
most cases available in print, in our popular Virtual Meeting web-based format, and
in a variety of other electronic platforms.
Quality cancer care and innovation will
not be possible unless we pay attention
to the proposals for change in the organization and financing of our health care
system. ASCO is committed to improving
access to oncologists for our current and
future patients, to maintaining the primacy of the oncologist–physician relationship in individual care decisions, ensuring
that any system-wide changes are
evidence-based, and allowing oncologists
the freedom to participate (or not participate) in any payment schemes based
on their own rational business decisions.
ASCO is also committed to addressing, in
a meaningful way, the cost–value calculus
in oncology care. We are using ASCO’s
well-developed policy apparatus to influence national and state legislative and
regulatory efforts on these issues.
We have a lot on our plate this year. I
look forward to renewing old friendships
and making new friends as we continue to
move our field forward together.
ASCO NEWS & FORUM |
17
UP FRONT
$QQXDO0HHWLQJ
Call for Abstracts
A
SCO will soon accept abstracts
to be considered for presentation
or publication at the 46th Annual
Meeting in Chicago, Illinois. This year’s
Meeting will focus on Advancing Quality
through Innovation and will provide an
opportunity to discuss the latest innovations in research, quality, practice, and
technology in cancer. ASCO encourages
the submission of abstracts of 300-350
words in several areas. Innovations in
research, which focus on new therapies
to prevent, detect, and manage cancer,
and innovations in quality, which highlight
methods to improve care, mitigate disparities, ensure access to treatments, and
maintain an adequate workforce for future
patients will be two strong areas of focus.
In addition, abstracts related to innovations in technology—the development of
new and novel technologies to enable the
entire oncology practice to operate more
efficiently—also are encouraged.
ASCO has created a new Call for
Abstracts website to provide authors with
detailed information regarding changes
to the submission process, submission
requirements, Annual Meeting abstract
policies, and the selection process. Visit
www.asco.org/callforabstracts for quick
links to the Abstract Submitter, Coauthor Disclosure Forms, Topic Categories,
Biostatistical Guidelines, and Frequently
Asked Questions.
All abstracts must be submitted
through the official Abstract Submitter
program at www.asco.org/callforabstracts
by January 12, 2010, 11:59 PM Eastern
Standard Time (EST).
Abstract Submission:
Changes in 2010
As you prepare to submit your abstract,
please keep in the mind the following
changes to the 2010 abstract submission
process:
Q ASCO has a new electronic abstract
submission system. Feedback is
welcome and can be sent to
abstracts@asco.org.
Q A $60 administrative fee, payable at
the time of submission, will be associated with all abstract submissions.
Q E-mail addresses are now required
for all Coauthors, as well as for the
First Author. A search feature will be
provided for ASCO member e-mail
addresses. Please note that any
changes to member information must
be completed through the member profile on ASCO.org.
Q First Authors of registered clinical trials
will be asked to enter the name of the
clinical trial registry and the trial registration number.
Q A separate Coauthor Disclosure Form
has been created for abstracts that
report on clinical trials. Coauthor Disclo-
Coming Soon: A Call for Abstracts Website
Visit www.asco.org/callforabstracts for quick links to the Abstract
Submitter and to downloadable disclosure forms, as well as for
detailed information about policies, guidelines, and frequently
asked questions. This site will launch early November 2009.
18 | OCTOBER 2009
Q
sure Forms can be downloaded at
www.asco.org/callforabstracts.
Late-breaking Abstract status has
been expanded to include randomized
phase II trials. For more detailed information on Late-breaking Abstracts, visit
www.asco.org/callforabstracts.
New Poster Session
The 2010 Annual Meeting will include
a new Trials in Progress Poster Session
designed exclusively to facilitate awareness of and dialogue about open, ongoing
clinical trials. This session will encourage
discussions of new clinical research and
the exchange of ideas on clinical trial
design.
Abstracts submitted to the Trials in
Progress Poster Session should not
include results. These abstracts will not
count as the author’s one allowed submission. The administrative fee will apply to
this abstract category, and sponsorship
must be attained from an ASCO Active
or Active-Junior member, if the author is
not an ASCO member. All conflict of interest policies apply. No CME credit will be
offered for this session.
Changes to the Conflict of
Interest Disclosure Process
If the First Author is employed by a
commercial interest as defined by the
Accreditation Council for Continuing Medical Education (ACCME) and the abstract
is selected for presentation in an oral
abstract session, an alternate presenter
who does not have a relevant employment
relationship must be named.
Clinical trial abstracts that do not identify a principal investigator will be asked
to answer additional questions.
UP FRONT
/HDGHUVKLS3HUVSHFWLYHV
Dr. Susan Lerner Cohn Represents Oncology’s Youngest
Patients on Board of Directors
S
usan Lerner Cohn,
MD, of the
University of Chicago, assumed
the role of Pediatric Oncology
representative to
the ASCO Board
of Directors at
Susan Lerner Cohn, MD
the 2009 Annual
Meeting.
“I’m absolutely delighted to be a part
of the Board. In addition to advocating
for children with cancer, I look forward
to working with my medical colleagues
to enhance the care of adolescents and
young adults,” Dr. Cohn said. “By working
together and sharing our experiences and
research we will be able to improve the
care of all of our patients with cancer.”
In the interview that follows, Dr. Cohn
speaks with ASCO News & Forum about
pediatric oncology and her goals for her
tenure in ASCO leadership.
AN&F: How did you choose pediatric
oncology as your specialty?
Dr. Cohn: After I worked with children
[during medical school rotations], it
became clear to me that I wanted to
devote my career to caring for children
with serious illnesses. During my pediatric
residency, I cared for several children with
different types of cancer. Despite having
devastating diseases, these kids managed to laugh and play while they were in
the hospital. During the past 20 years I
have cared for many children with cancer,
and I continue to be amazed by their courage and inspired by the strength of their
parents and caregivers. Although many
of the children I cared for during my resi-
dency and fellowship were cured of their
cancers, others were not as fortunate.
This experience significantly influenced
my decision to obtain further training in
translational and clinical research.
AN&F: Why is it important that pediatric oncologists are represented on the
Board of Directors?
Dr. Cohn: The needs of children with cancer and their families frequently are not
addressed in professional societies that
are largely focused on the more common
cancers that occur in adults. Therefore, it
is critical that the ASCO Board include a
strong advocate for pediatric patients and
their oncologists.
There are many genetic aberrations
that are common in many types of malignant tumors, and the study of pediatric
cancers has led to seminal discoveries
that have affected our understanding of
the biology of cancers that occur in children as well as adults. Pediatric clinical
trials also have demonstrated the efficacy
of pediatric treatment approaches in diseases like acute lymphocytic leukemia in
adolescents and young adults. Similarly,
pediatric patients have benefited from
the research that has been conducted by
our medical colleagues. ASCO provides an
ideal infrastructure to enhance communication between pediatric and medical
oncologists. In addition, this organization
can address the challenges associated
with adolescents and young adults with
cancer, because these patients may seek
care with either a pediatric or a medical
oncologist. Similarly, ASCO can be instrumental in educating medical colleagues
about the needs of our older long-term
survivors of pediatric cancer. As the sole
pediatric oncologist on the ASCO Board
of Directors, I will make sure that our
pediatric patients, adolescent and young
adult patients, and older long-term survivors have a voice and I will work hard to
enhance communication between pediatric and medical colleagues.
AN&F: What do you hope to accomplish
during your term?
Dr. Cohn: Clinical trials underlie the
progress that has been seen in cancer
treatment. This is especially true in pediatric oncology, where cooperative group
clinical trials have served as a paradigm.
Currently, more than 80% of children
diagnosed with a pediatric malignancy will
become five-year survivors of their cancer.
However, cancer remains a leading cause
of death in children. As a member of the
Board, I plan to raise awareness of the
significance clinical trials have on the survival and well-being of patients with cancer and advocate for additional funding to
support this research.
Our success in treating pediatric
cancers has resulted in a new and growing population of long-term survivors of
childhood cancer. Although this cohort of
patients is cured of their primary cancer,
many patients develop chronic diseases
that can involve multiple organ systems.
Numerous studies have shown that childhood cancer survivors are also likely to
experience more cancers as adults than
are individuals of similar age. Additional
survivorship research is needed to determine how the normal aging process will
influence the health of these patients. I
plan to work closely with my medical colleagues in ASCO to optimize the care of
adults who have survived childhood
cancer.
ASCO NEWS & FORUM |
19
UP FRONT
7KH$6&2&DQFHU)RXQGDWLRQ
Foundation Awards High-level Grants
to Support Clinical Research
20 | OCTOBER 2009
PHOTOGRAPH BY TODD BUCHANAN
T
he ASCO Cancer Foundation® continues its tradition of supporting the
best and most innovative cancer
research by awarding two Advanced Clinical Research Awards (ACRAs) and a Translational Research Professorship grant
in 2009, presented at the most recent
ASCO Annual Meeting.
Shanu Modi, MD, and Ingo Mellinghoff,
MD, both of Memorial Sloan-Kettering
Cancer Center (MSKCC), are the recipients of this year’s ACRAs, three-year
awards of $450,000 presented by the
Foundation for clinical or translational
research with a patient-oriented focus.
Dr. Modi received the ACRA for her work
in the field of breast cancer (supported
by The Breast Cancer Research Foundation®), and Dr. Mellinghoff received the
first ACRA dedicated to support glioma
research (supported by Genentech
BioOncology™).
Merrill J. Egorin, MD, FACP, received
the 2009 Translational Research Professorship for his significant contributions
to the direction of translational cancer
research and his dedication to mentoring.
The Translational Research Professorship,
a five-year grant totaling $500,000, is
intended to support qualified individuals
who are dedicated to bringing advances
in basic sciences into the clinical arena
and to mentoring other translational
researchers. The 2009 Translational
Research Professorship is supported by
Genentech BioOncology™.
Ingo Mellinghoff, MD, (left) and Shanu Modi, MD
ACRA Winners’ Research
Pursues Molecular Therapies
The most cutting-edge oncology research
zeroes in on the aspects of cancer that
have eluded current available treatments.
The two winners of ASCO’s 2009 ACRAs
are pursuing science of this nature, which
they hope will advance the treatment of
patients with breast cancer and glioma.
Dr. Modi’s research, “PU-H71: A Novel
HSP90 Inhibitor for the Treatment of
Breast Cancer,” is the latest development in a body of research conducted at
MSKCC on the action of HSP90, a protein
involved in the progression of breast
cancer and its resistance to treatment.
Although previous research has suggested
the viability of HSP90 inhibitors against
HER2-positive breast cancer, patients
with triple-negative breast cancer did not
seem to benefit from these treatments.
Dr. Modi’s investigation of PU-H71 shows
that this particular type of HSP90 inhibitor
could be beneficial for women with this
aggressive subtype of the disease.
“Unlike other breast cancer types for
which we have targeted therapies, there
are no specific targets identified for triplenegative breast cancers. Therefore we
rely on chemotherapy, which works very
well, but only for a proportion of patients.
It’s clear that we urgently need novel
agents and approaches,” Dr. Modi said. “I
think there’s such strong preclinical data
to support the development of PU-H71
that it has to be taken to the next step.”
Dr. Modi’s group will begin phase 0
clinical trials for PU-H71 in 2009, and
she hopes that the study will progress to
phase I trials before the end of the year.
Dr. Mellinghoff is the recipient of
ASCO’s first ACRA for glioma research.
His study, “Identification of Critical Signal Transduction Nodes during Glioma
Progression,” investigates the possibility
that gliomas may be more responsive to
therapy with signal transduction inhibitors
if they are treated earlier in the disease
process.
“Low-grade gliomas often afflict young
patients, and these patients are treated
with a combination of surgery, radiation,
and/or chemotherapy,” Dr. Mellinghoff
said. “We hope that our studies will point
toward new molecular targets to prevent
or at least delay the progression of these
tumors to high-grade gliomas.”
During his training, Dr. Mellinghoff saw
great potential in the cutting-edge science used in the study and treatment of
cancer.
“My interests in medical school always
gravitated toward the molecular basis of
human disease. I was impressed by how
quickly the combination of rigorous basic
science and its logical clinical application
transformed the treatment of HIV [human
immunodeficiency virus],” he said. “Based
on emerging insights into oncogenes and
tumor suppressor genes, cancer seemed
like a field with great opportunities for
similarly transformative science.”
As a previous recipient of a Young
Investigator Award (YIA) from the Foundation, he feels that ASCO has influenced
his career in a number of ways.
“In addition to the very generous
funding, the ACRA will provide me an
opportunity to exchange ideas and forge
collaborative efforts with colleagues working on related aspects of glioma biology,”
he said.
Pharmacology Expert Awarded
Translational Research
Professorship
Dr. Egorin, a mentor to five junior faculty
members, emphasized the mentorship
component of the Translational Research
Professorship.
“The people who were my mentors
were incredibly giving, and it’s nice to be
able to carry on that tradition and try to
inculcate the next generation of investigators,” he said. He added that the grant
will aid the development of his younger
colleagues just beginning a career in
translational research: “My job is to run a
greenhouse—to maintain an environment
in which really smart young people can
put down roots, grow, and flower.”
Dr. Egorin is a Professor of Medicine
and Pharmacology at the University of
Pittsburgh School of Medicine. He also
serves as Co-Director of the Molecular
Therapeutics/Drug Discovery Program,
and as Director of the Clinical Pharmacol-
PHOTOGRAPH BY LBJ IMAGES
UP FRONT
“My job is to run a greenhouse—to maintain an environment in which really smart young people can
put down roots, grow, and flower.” — Merrill J. Egorin, MD.
ogy Analytical Facility Core at the University of Pittsburgh Cancer Institute (UPCI).
Dr. Egorin and his colleagues study
different approaches to using poly (ADPribose) polymerase (PARP) inhibitors.
The grant will provide crucial funding to
increase the coordination and expansion
of the University of Pittsburgh’s program
on the studies of the PARP inhibitor ABT888 as a single agent in BRCA-mutated
or dysfunctional malignancies, or in
combination with cytotoxic chemotherapeutic agents against a broader range of
cancers.
“In the first case, these tumors—with
this one genetic defect—are exquisitely
sensitive to what this class of drugs does,
[so] you may not need to use anything
else,” Dr. Egorin explained. “In the other
case, you’re using [the inhibitor] to augment or enhance the activity of things
that are already known to have some
activity by modulating a potentially important resistance mechanism.”
Dr. Egorin noted that the use of singleagent PARP inhibitors does not lead to
myelosuppression, nausea, vomiting,
hair loss, or immunosuppression. “[PARP
inhibitors] are a very interesting class of
compounds that can be used as adjuncts
to other forms of chemotherapy,” he said.
“Possibly the most exciting thing of all
would be to use them in this concept of
synthetic lethality, and to go after an Achilles heel of tumor cells.”
The UPCI phase I studies of ABT-888
will be translated into phase II studies in
a variety of malignancies including breast,
ovarian, pancreatic, and prostate cancers.
For more information on the grants and
awards offered by the Foundation, visit
www.ascocancerfoundation.com.
ASCO NEWS & FORUM |
21
Current
&RQWURYHUVLHV
in Oncology
The Controversy: CT Colonography for Colorectal
Cancer Screening vs. Optical Colonoscopy
Al B. Benson III, MD
Robert H. Lurie Comprehensive Cancer Center
Northwestern University
C
´&XUUHQW&RQWURYHUVLHVLQ2QFRORJ\µ
LVDIRUXPIRUWKHH[FKDQJHRI
YLHZVRQWRSLFDOLVVXHVLQWKH
ILHOGRIRQFRORJ\7KHYLHZVDQG
RSLQLRQVH[SUHVVHGWKHUHLQDUH
WKRVHRIWKHDXWKRUVDORQH7KH\
GRQRWQHFHVVDULO\UHIOHFWWKHYLHZV
RUSRVLWLRQVRIWKH(GLWRURURI
WKH$PHULFDQ6RFLHW\RI&OLQLFDO
2QFRORJ\
22 | OCTOBER 2009
olorectal cancer is a leading cause of cancer death that is also a potentially
preventable disease by applying screening strategies. The subject of colorectal
cancer screening has been one of significant interest with extensive efforts
undertaken to improve not only the rate of screening, but also to explore alternative
methods of screening.
Recent literature has emerged evaluating the optimal role of two important technologies, optical colonoscopy and computed tomographic (CT) colonography. Although the
Centers for Medicare & Medicaid Services (CMS) will reimburse optical colonoscopy for
the purposes of colorectal cancer screening, CMS denied reimbursement for CT colonography in its February 2009 Proposed Decision Memorandum.1 CMS stated that the
evidence was inadequate to justify the use of this screening modality, expressing concerns that it is not yet possible to generalize study results to support its use in an older
population of patients. In addition, the U.S. Preventative Services Task Force has not
endorsed CT colonography screening. The CMS decision has raised significant concerns
prompting the mailing of letters to the CMS Acting Administrator from Members of Congress, including the Congressional Black Caucus.
The following represents two independent points of view: the merits of CT colonography, presented by Abraham H. Dachman, MD, versus those of optical colonoscopy,
presented by Hemant K. Roy, MD, and Michael J. Goldberg, MD. Important areas
of discussion include the availability of gastroenterologists to perform colonoscopy
screening, cost, patient acceptance, bowel preparation, radiation exposure with CT
colonography, detection of small polyps and flat lesions, safety, avoidance of unnecessary biopsies, and colonoscopy as a “one-step” procedure for localization and biopsy
examples.
Reference
1. Centers for Medicare & Medicaid Services. Decision memo for screening computed tomography
colonography (CTC) for colorectal cancer (CAG-00396N). https://www.cms.hhs.gov/mcd/viewdecisionmemo.
asp?id=220. Accessed 17 July 2009.
PHOTOGRAPH BY OLIVIER VOISIN/PHOTO RESEARCHERS, INC.
PHOTOGRAPH BY PHANIE/PHOTO RESEARCHERS, INC.
A flexible fiber-optic endoscope (colonoscope) is inserted through the rectum to examine the interior of the colon and intestines. The virtual
colonoscopy permits the 3D reconstruction of the inner colon from computerized coloscanner images. Both techniques are used for screening of
colorectal cancer.
CT Colonography
Should Be Offered as a
Screening Test
Abraham H.
Dachman, MD
Department of
Radiology
University of Chicago
Medical Center
There is a critical
and immediate need
to improve screening for colorectal cancer (CRC)1 and the best option today is
acceptance of computed tomographic (CT)
colonography (CTC) in addition to optical
colonoscopy (OC).2 These alternatives provide synergistic alternatives for a diverse
population at risk for CRC, and together
provide benefits that exceed the sum of
their respective contributions.
The benefits accrue in cost, acceptance, utilization, and ultimately in overall survival. There is evidence that the
full approval of optical colonoscopy by
Medicare in 2002 played a major role in
improved compliance with American Can-
cer Society (ACS) screening guidelines.3
The approval of barium enema as a CRC
screening test was important, but its use,
while still representing a significant component of Medicare reimbursement costs,
continues to decline. The 43% sensitivity
for 10 mm polyps by barium enema4,5 was
not the problem. I believe the public did
not perceive barium enema as a desirable test. On the other hand, CTC has
developed since its introduction in 1993
to become a test known to the public.
Although only a few centers of excellence
perform high-volume screening CTC,
increasing numbers of radiologists have
introduced CTC into their practice.
The proliferation of CTC screening
exams into general radiology practice was
initially hampered by lack of endorsement
by the medical community and a lack
of widespread reimbursement. This has
gradually changed; with the publication of
the American College of Radiology Imaging Network (ACRIN) National Colonography Trial,6 CTC was endorsed by the ACS,
the Blue Cross/Blue Shield Technology
Assessment,7 and the U.S. Multi-Society
Task Force on CRC.2 CT scanner and
CTC interpretation software continue to
improve and the capacity to perform CTC
nationally has been realized. The ACR
developed standards,8 intensive hands-on
educational courses that can accommodate a large number of radiologists documented by a certificate of participation for
the interpretation of at least 50 carefully
selected teaching cases. Other educational opportunities have been developed
by the pharmaceutical industry, by universities, and through online resources, all
of which will facilitate the training of radiologists on a national scale. As of April
2008, at least partial reimbursement for
CTC existed in 43 states (often including
Medicare reimbursement for incomplete
OC done for a diagnostic indication).
Several recent studies have addressed
the cost effectiveness of CTC with favorable results. Pickhardt et al. used a Markov model and showed CTC to be cost
effective when used as recommended
(ignoring diminutive polyps smaller than 5
mm).9 CTC advocates do not suggest that
CTC should replace OC, but the comparison to OC should be fair and include the
false negative rate, cost of unnecessary
ASCO NEWS & FORUM |
23
biopsies, and complications. In a recent
comparison of more than 3,100 patients
in each arm of a screening program in
which patients chose between CTC or
OC screening, the detection and removal
of advanced neoplasia was comparable,
yet CTC resulted in only 561 polypectomies (and no CTC complications) versus
OC which had 2,434 polypectomies and
seven colonic perforations.9 The referral
rate to OC from the CTC screening arm
was 7.9%, consistent with a very costeffective program. The issue of polyp size
threshold and CTC sensitivity for diminutive lesions has also been addressed.10
The cost of additional workup incurred
as a result of potentially significant
extracolonic findings (not including surgical expenses) has been estimated to be
between a mean of $24 and $34 per
patient, and 0.2%-2% of asymptomatic
patients may be referred for surgery.11
Regarding radiation, the radiation doses
are less than those of a barium enema
and often less than the yearly ambient
population exposure to radiation.
Compliance would improve further if
CTC was fully reimbursed by Medicare
and private carriers. I am concerned that
the failure of the Centers for Medicare &
Medicaid Services (CMS) to endorse CTC
created a new misconception, by the public and by primary care physicians, that
CTC is rarely reimbursed. In our practice,
the percent of self-pay CTC patients has
dropped from 60% to 10% even though
our volume is steady.
Yes, I am a CTC enthusiast and I think
CTC is ready for prime time. My perspective is strongly endorsed by respected and
objective non-radiologists. In particular,
I quote from one documented eloquent
rebuttal of the CMS decision,12 that
states, “If the criteria applied by CMS
to CTC were re-applied universally to all
therapies, it is likely that no drug on the
market today would pass the test.”
References
1. Umar A, Greenwald P. Cancer Epidemiol
Biomarkers Prev. 2009;18:1672-73.
2. Levin B, Lieberman DA, McFarland B, et al. CA
Cancer J Clin. 2008;58:130-60.
3. Gross CP, Andersen MS, Krumholz HM, et al.
JAMA. 2006;296:2815-22.
4. Winawer SJ, Stewart ET, Zauber AG, et al. N Engl J
Med. 2000;342:766–72.
5. Rockey DC, Paulson, E, Davis W, et al. Lancet.
2005;365:305-11.
6. Johnson CD, Chen MH, Toledano AY, et al. N Engl
J Med. 2008;359:1207-17.
7. Blue Cross Blue Shield Technical Evaluation
Center. Technology evaluation center
assessments. www.bcbs.com/blueresources/
tec/press/ct-colonography-virtual.html. Accessed
July 17, 2009.
8. American College of Radiology. ACR practice
guideline for the performance of computed
tomography (CT) colonography in adults. ACR
Practice Guideline. 2005;Res.29:295-98.
9. Pickhardt PJ, Hassan C, Laghi A, et al. Cancer.
2007;109:2213-21.
10. Kim DH, Pickhardt PJ, Taylor AJ, et al. N Engl J
Med. 2007;357:1403-12.
11. Pickhardt PJ, Hanson ME, Vanness DJ, et al.
Radiology. 2008;249:151-59.
12. Pickhardt PJ, Kim DH. AJR Am J Roentgenol.
2009;193:40-6.
13. Lichtenfeld L. American Cancer Society. http://
www.cancer.org/aspx/blog/Comments.
aspx?id=307. Accessed June 25, 2009.
Share Your Thoughts and Opinions in a Letter to the Editor
Provide feedback about Current Controversies in Oncology. Letters should be
less than 250 words and may be edited for length, clarity, and accuracy. All
correspondence should include a daytime telephone number, current mailing
address, and e-mail address. ASCO News & Forum cannot acknowledge or
return letters. Letters become the property of ASCO and may be published in
all media.
To submit a letter, send an e-mail to asconews@asco.org; write to Letters to
the Editor, ASCO News & Forum, ASCO, 2318 Mill Road., Suite 800, Alexandria, VA
22314; or send a fax to 571-366-9550.
24 | OCTOBER 2009
An Argument for Optical
Colonoscopy
Hemant K. Roy, MD
Michael J. Goldberg,
MD
NorthShore University
HealthSystems
Department of Internal Medicine
University of Chicago
Pritzker School
of Medicine
The major focus for
colorectal cancer
(CRC) screening has
evolved from early
diagnosis to cancer
prevention through
the identification and removal of adenomas.1 Colonoscopic screening has been
documented to reduce risk for future
CRC by 75%-90% and thus has become
the “gold standard.”2 The multi-society
guidelines also recommended flexible
sigmoidoscopy and CT colonography (CTC)
for adenoma detection.1 Since flexible
sigmoidoscopy is limited by its inability
to assess the proximal two-thirds of the
colon, interest has turned to CTC as a less
intrusive option for pan-colonic evaluation. However, as detailed below, there
are significant challenges in implementing
CTC for CRC population screening.
The first issue for CTC is the ability to
detect adenomas and hence interrupt the
adenoma-carcinoma progression. There
are many widely divergent estimates of
performance characteristics. For instance,
in an observational single-center trial,
the detection rate for adenomas ≥10
mm was comparable to colonoscopy,
although this non-randomized study was
limited by potential selection bias and
lack of colonoscopic confirmation of most
CTC findings.3 On the other hand, previous randomized multicenter trials have
reported that CTC had poor sensitivity for
adenomas ≥10 mm (55%-59%), but has
been criticized for using earlier generation
technologies.4,5 Fortunately, there have
been two recently published, rigorously
conducted multicenter randomized trials.
These studies have yielded remarkably
similar sensitivities for clinically significant
adenomas (>9-10 mm) in average and
higher-risk cohorts (84% and 80%, respectively).6,7 For non-diminutive (≥5 mm) adenomas, the performance was even poorer
(65% and 72%).6,7 Even for CRCs, CTC miss
rate was not trivial (approximately 6%).6,7
Management of CTC-identified neoplasia represents one of the most vexing clinical challenges. Typically, during
colonoscopy all visualized lesions are
removed, reasoning that large polyps/
CRCs evolve from smaller lesions. For
CTC, referring every patient for polypectomy is impractical from both a cost and
patient satisfaction perspective (i.e., logistic constraints would probably necessitate
a second visit and bowel prep). Therefore,
the crux of these performance issues
centers on the consequences of lesions
either missed by CTC or identified but
left in situ. Most authorities consider it
reasonable to ignore adenomas <5 mm.8
Although one could argue that polyps
of 6-9 mm have a low risk of harboring
advanced features, this is not negligible
(6.6%)9 and may be higher in the subset
(approximately 10%) of lesions classified
as flat and depressed.10 Indeed, electing
to leave a potentially premalignant lesion
in place is unacceptable for most patients
and may have medico-legal ramifications.11 Even if one confined colonoscopy
to only patients with ≥10 mm lesions,
given the positive predictive value of CTC
is only 0.23, approximately one-fifth of the
average-risk population would require the
second test.6
An important consideration is patient
acceptability, as compliance is a major
obstacle in population screening. From
a patient perspective, CTC is less intrusive than colonoscopy but still requires a
bowel purge (the major reason for patient
non-compliance)12 and a rectal catheter
for air insufflation which is performed
without benefit of sedation. In fact, studies on CTC and colonoscopy have failed
to yield dramatic differences in patient
preferences.13 With regard to risks, colonoscopic complications are rare but not
insignificant (perforation, bleeding, sedation). CTC appears safer although concern
has been raised regarding neoplasia
occurring secondary to radiation exposure
from serial examinations.14
Another area that must be addressed
is the extra-intestinal lesions observed
on CTC. Superficially, this may appear to
be a “bonus.” However, these are extraordinarily common, seen in two-thirds
of cases with 16% deemed to require
further investigations.6 Although some
findings may benefit the patient (aortic
aneurysms, etc), the majority are simply
“incidentalomas” that still obligate followup testing that results in unnecessary
expense, patient anxiety, and potential
complications.15-17
In conclusion, CTC represents an important technological advance but in order
to make a significant contribution to the
average-risk screening armamentarium,
there are several critical issues that
still need to be resolved. Thus, at this
juncture, we believe that CTC’s numerous important limitations, especially the
lack of therapeutic ability, preclude its
designation as a preferred CRC screening strategy. We, therefore, concur with
the decisions not to endorse CTC by
the U.S. Preventive Services Task Force
(being particularly concerned about the
potential harms associated with “incidentalomas”)18 and the Centers for Medicare
& Medicaid Services.19 As the technology
and clinical paradigms mature, CTC may
have a role in screening a subgroup of
patients, including those with multiple
comorbidities, those refusing colonoscopy, and possibly patients at lowest risk
of CRC.20 However, at present, we believe
that the evidence strongly supports colonoscopy as the dominant CRC screening
strategy.
References
1. Levin B, Lieberman DA, McFarland B, et al.
Gastroenterology. 2008;134:1570-95.
2. Winawer SJ, Zauber AG, Ho MN, et al. N Engl J
Med. 2007;357:1403-12.
3. Kim DH, Pickhardt PJ, Taylor AJ, et al. N Engl J
Med. 2007;357:313-5.
4. Cotton PB, Durkalski VL, Pineau BC, et al. JAMA.
2004;291:1713-9.
5. Rockey DC, Paulson E, Niedzwiecki D, et al.
Lancet. 2005:365:305-11.
6. Johnson CD, Chen MH, Toledano AY, et al. N Engl
J Med. 2008:359:1207-17.
7. Regge D, Laudi C, Galatola G, et al. JAMA.
2009;301:2453-61.
8. Butterly LF, Chase MP, Pohl H, et al. Clin
Gastroenterol Hepatol. 2006;4:343-8.
9. Lieberman D, Moravec M, Holub J, et al.
Gastroenterology. 2008;135:1100-5.
10. Soetikno RM, Kaltenbach T, Rouse RV, et al.
JAMA, 2008;299:1027-35.
11. Shah JP, Hynan LS, and Rockey DC. Am J Med.
2009;122:687,e1-9.
12. Beebe TJ, Johnson CD, Stoner SM, et al. Mayo
Clin Proc. 2007;82:666-71.
13. Rockey DC. Gastroenterology. 2009;137:7-14.
14. Brenner DJ and Hall EJ. N Engl J Med.
2007;357:2277-84.
15. Fletcher RH, Pignone M. Arch Intern Med.
2008;168:685-6.
16. Kimberly JR, Phillips KC, Santago P, et al. J Gen
Intern Med. 2009;24:69-73.
17. Whitlock EP, Lin JS, Liles E, et al. Ann Intern Med.
2008;149:638-58.
18. Screening for colorectal cancer: U.S. Preventive
Services Task Force recommendation statement.
Ann Intern Med. 2008;149:627-37.
19. Mitka M. JAMA. 2009;301:1327-8.
20. Lin OS, Kozarek RA, Schembre DB, et al.
Gastroenterology. 2006;131:1011-9.
ASCO NEWS & FORUM |
25
ASCO’s
Diversity in Oncology
Initiative
Building a multicultural workforce
Recruiting the Best—and
Keeping Them
The Diversity in Oncology Initiative is
designed to facilitate the recruitment and
retention of individuals from populations
underrepresented in medicine to cancer
careers, with particular attention to the
development of clinical practitioners and
investigators. Three funding opportunities
were created to support the program’s
goals.
Q The Medical Student Rotation provides
8- to 10-week clinical or research oncology rotations for U.S. medical students
from underrepresented populations.
A mentoring component is included
whereby award recipients are paired
with a clinical oncologist who provides
ongoing academic and career guidance.
2009 Diversity in Oncology Initiative Award Recipients
ASCO and Susan G. Komen for the Cure® are pleased to recognize the following
participants in the 2009 Diversity in Oncology Initiative.*
Medical Student Rotation
Amanda Adeleye—Columbia University
College of Physicians and Surgeons
Frank Crespo—The Warren Alpert School of
Medicine, Brown University
Kimberly Lockhart—University of Arkansas
for Medical Sciences
Kenisha Pemberton—Florida State
University College of Medicine
Resident Travel Award
Andrew Aguirre, MD, PhD—Massachusetts
General Hospital
26 | OCTOBER 2009
David Chism, MD, MS—University of
Medicine and Dentistry of New Jersey/
Robert Wood Johnson Hospital
Derrick D. Cox, MD—Georgetown University
Hospital
Mitzie-Ann Davis, MD—University of
Pennsylvania
Renee Funches, MD—Emory University
Hospital
Lisa Garcia, MD—Boston Medical Center
Lourdes Mendez, MD, PhD—Cornell
University/New York-Presbyterian Hospital
Kelvin Moses, MD—Emory University
Q
Q
Award recipents receive a $5,000 stipend for the rotation plus $1,500 for
future travel to the ASCO Annual Meeting. An additional $2,000 is provided to
the student’s mentor.
The Resident Travel Award provides
financial support for residents from
underrepresented populations to attend
the ASCO Annual Meeting. The award
includes a $1,500 travel advance, complimentary meeting registration, and
access to the Annual Meeting housing
block and ASCO’s travel agency.
The Loan Repayment Program provides
repayment of qualifying educational
debt to oncologists or oncology fellows
who commit to practicing oncology in
a medically underserved region of the
United States (designated by the U.S.
Bridget Oppong, MD—University of Rochester
Rhoda Raji, MD—Temple University Hospital
Mayra Sanchez, MD—Kansas University
Medical Center
Zanetta Stewart-Lamar, MD—Wake Forest
Baptist Medical Center
Veronica Wilson, MD—Baylor University
Medical Center
Loan Repayment Program
Brooke Gillett, DO—Oncology-Hematology
Associates of Springfield, Montana
Boone W. Goodgame, MD—Washington
University School of Medicine, St. Louis
Derrick S. Haslem, MD—Intermountain
Medical Group, Utah
*Institutions as of the time of the recipient’s application.
PHOTOGRAPH BY MARINA MAKROPOULOS
A
SCO recognizes the value of
diversity with its many facets—
race, ethnicity, gender, socioeconomic background, geographic
location, interests, etc.—and has implemented a program to increase the diversity of physicians in the oncology workforce.
The ASCO Diversity in Oncology Initiative,
funded by Susan G. Komen for the Cure®,
consists of three unique awards that offer funding to physicians and medical
students with an interest in oncology who
self-identify as minorities or who commit
to practicing oncology in a medically underserved region of the United States. The
program supports the underrepresented
physicians establishing themselves in the
field of oncology and the underserved patients who desperately need care.
Amanda Adeleye’s
experience conducting
breast cancer research
inspired her to apply for the
Medical Student Rotation.
ASCO NEWS & FORUM |
27
PHOTOGRAPH BY RYAN T. CONATY
Frank Crespo looks forward to interacting with patients when he begins his Medical Student
Rotation in November 2009.
Q
Health Resources and Services Administration as a Health Professional Shortage Area or Medically Underserved
Area). The program will repay up to
$35,000 per year for two years (up to
$70,000 total) of qualifying education
debt.
The application for the ASCO Loan
Repayment program is currently open.
The application is due December 16,
2009.
Making a Difference in Lives of
Physicians, Patients
The recipients of these awards (see box
on page 26 for complete list of recipients)
represent a spectrum of backgrounds,
interests, and experiences, but all share
the same desire to improve the quality of
care of patients with cancer.
28 | OCTOBER 2009
“When I first read my acceptance
letter [to the Medical Student Rotation
program], I got chills,” Frank Crespo, of
The Warren Alpert School of Medicine at
Brown University, said. “I had to read the
letter three more times before it actually
sunk in. I couldn’t believe that I was about
to live one of my dreams.”
Mr. Crespo will start his oncology rotation in November 2009 in his hometown
at the University of Miami Sylvester Cancer Institute, and he is eager to meet his
patients. “I hope to affect their lives and
offer them guidance and support through
their battle with cancer,” he said. “I also
look forward to the abundance of knowledge my mentor, the institution staff, and
the patients will provide me.” He hopes
that his experiences will help him “to better appreciate how the intricacies of race,
nationality, and class affect illness.”
Amanda Adeleye, of Columbia University, had prior experience with oncology
when she applied for the Medical Student
Rotation, conducting research on an
aggressive subtype of breast cancer. “I
could see how what I was doing could
help someone down the road, and that
was thrilling to me,” she said. “There are
so many talented medical students interested in oncology. I’m still trying to figure
out how I was so lucky to be selected” for
the program.
Ms. Adeleye completed her oncology
rotation at Northwestern in summer
2009. “I was most excited to start my
research because it was my opportunity
to be able to make a difference in the
fight against cancer, no matter how small.
Great research takes time and I have
been working hard to make every minute
count,” she said.
Diversity includes a spectrum of attributes and experiences, and Ms. Adeleye
defines her own diversity in multiple ways:
as the daughter of a Nigerian father and
African-American mother; as a scientist
who also majored in Classics, which
“afforded me the experience of approaching some of the world’s most ancient
works with a scientific eye”; and as a
dancer and art lover who “appreciates
medicine in a unique way—the synchrony
in the steps of a procedure and the
beauty in the expression of a patient who
is a survivor.”
For Kimberly Lockhart, of the University
of Arkansas, diversity is about keeping an
open mind. “I strive to enrich my life with
the awareness, knowledge, and sensitivity
of other racial, ethnic, socioeconomic, and
cultural groups. I desire to interact and
serve people with different values, beliefs
and alternative perspectives,” she said.
Ms. Lockhart served her Medical Student
Rotation at the University of Arkansas for
Medical Science/Winthrop P. Rockefeller
Cancer Institute during summer 2009.
Ms. Lockhart knows firsthand what it
means to be an underserved patient. At
I hope, because I plan on being here forever, that I can break down some of those
barriers.”
Boone W. Goodgame, MD, of Washington University School of Medicine, St.
Louis, plans to practice in underserved
communities in Missouri as part of the
Loan Repayment Program. At Washington
University, the primary “safety-net” hospital in the region, he will treat the largest
uninsured and underinsured populations
in the state. He will also spend one day
each week at an outreach clinic in rural
Missouri, where patients frequently drive
one to two hours for treatment.
His desire to serve an underrepresented population was inspired by his
own life experiences. Dr. Goodgame spent
his childhood living in Uganda, where his
father taught at the nation’s only medical school. “Most of my childhood was
spent in a developing country, so I have
a balanced outlook on what it means to
be advantaged and disadvantaged,” he
said. He returned to East Africa during
his final year of medical school to work in
a hospital in rural Kenya, where he saw
“the profound devastation of cancer when
health care resources are essentially
unavailable.”
He is also guided by his spiritual faith,
which “shapes my approach to all areas of
life, including my patient interactions and
research.” He noted that, in his experience, strong religious beliefs are uncommon in academic medicine but they can
be “a common point of connection and
support with many of my patients.”
Experiences abroad also contribute to
Kenisha Pemberton’s understanding of
diversity. Ms. Pemberton, of Florida State
University College of Medicine and a recip-
PHOTOGRAPH BY PATRICK CUMMINGS
age 11, she was diagnosed with neurofibroma, a condition which left her “vulnerable, afraid, confused, and embarrassed”
for many years, she said. “By the time I
was a sophomore undergraduate, I managed to find two physicians willing to
carry out the daunting task of removing
the tumor and reconstructing my scalp
without compensation. I gained not only a
better quality of life, but also lifelong relationships with my physicians that inspire
me to help others just as I have been
helped.”
Derrick S. Haslem, MD, of Intermountain
Medical Group and a recipient of the Loan
Repayment Program, has experienced
multiple aspects of diversity. “My family is
composed of hardworking blue-collar farmers, ranchers, and construction workers.
I lived in the Dominican Republic for two
years among extreme poverty and need.
I feel like I can really relate to the people
who will become my patients,” he said.
Receiving funding from the Loan Repayment Program “was quite a relief to my
wife and me, that a substantial portion
of student loan debt would be taken care
of,” Dr. Haslem said. With the financial
burden of loan debt eased, he was able
to set up practice in a rural community in
St. George, Utah, where he grew up. The
coverage area for the practice includes
regions of Utah, Nevada, and Arizona.
“The population served includes Native
Americans from the Paiute and Navajo
tribes, Hispanic immigrants and rural
farmers and ranchers, as well as other
‘salt-of-the-earth’ people,” he explained.
“Currently, many travel 4.5 hours to Salt
Lake City or 1.5 hours to Las Vegas for
cancer care—imagine the drain that is
for people getting weekly chemotherapy.
Another challenge is overcoming some of
the distrust people have with the medical community,” exacerbated by the high
turnover of medical professionals in the
area, he noted. “Because it is somewhat
isolated, no one wants to come. I grew up
here and know the secrets to this great
place, so I was more than willing to return.
Derrick Haslem, MD, returned to his childhood home in rural Utah to provide oncology care to an
underserved community as part of the Loan Repayment Program.
ASCO NEWS & FORUM |
29
Why is it so important for the profession of oncology to represent people
with diverse origins and experiences?
understanding, which leads to positive
patient encounters in the health system
and, ultimately, improved outcomes.”
Amanda Adeleye: “In order to practice
with compassion, the oncology community must be able to appreciate and
incorporate the richness of differences
of its patient population. Having a
diverse group of health care professionals to provide care increases the probability that patients will be treated by
someone who is readily able to understand how the patient’s unique background may be beneficially weaved into
a plan to provide the best health care
possible. By interacting with people of
diverse backgrounds or bringing unique
experiences ourselves, we enhance the
relationships that we have with our colleagues and patients.”
Frank Crespo: “Different cultures have
varying ideas regarding cancer and life
after death. Having an appreciation and
respect for different cultures will allow
for a truly empathetic evaluation of
patients. By approaching patients in a
holistic fashion, we can overcome barriers to health care, which may include
mistrust of the medical community, fear
of dying, and disenfranchisement.”
Derrick D. Cox, MD: “Diversity promotes enhanced communication and
Renee Funches, MD: “People with
diverse backgrounds and experiences
often bring a unique perspective to
patients and their loved ones as they
cope with their diagnosis. They may
have a better appreciation of the things
that are culturally or spiritually important to the patient and their family,
which would influence their decision-
making and coping mechanisms.”
Boone W. Goodgame, MD: “When
patients see their physicians as real,
unique people, it helps them to trust
that you have their best interests at
heart. Whether experiences and origins are similar or different, they can
be used as a point to build common
ground. Patients may inherently trust
you because [they believe] ‘you’re like
me,’ or they might even trust you more
if they find that ‘you’re different from
me, but you care.’”
Derrick S. Haslem, MD: “Every person,
no matter what race, gender, or origin,
is different. They all have different life
experiences from which they base their
judgments. The more diverse experiences a provider has, the easier it is
for their patients to relate to them, feel
comfortable that they are getting genuinely good care, and trust that they will
be better off because of it.”
PHOTOGRAPH BY AMANDA NALLY
Kimberly Lockhart: “Diversity in the
profession of oncology provides for
an innovative workforce with a unique
knowledge base, fresh perspectives,
and alternative skills. This blend of characteristics equates to better medical
care for patients with cancer.”
30 | OCTOBER 2009
Kenisha Pemberton: “Cancer has
no regard for an individual; it afflicts
people from all walks of life. The oncology profession must include persons
with diverse origins and experiences to
provide superior patient-centered care
for an ever-increasing diverse patient
population.”
Kenisha Pemberton worked with pediatric
patients during her Medical Student
Rotation. She applied for the program
after witnessing her grandfather’s struggle
with cancer.
PHOTOGRAPH BY BILL WIPPERT
Derrick D. Cox, MD, chose to become an ASCO member after attending the 2009 Annual Meeting
on a Resident Travel Award.
ient of the Medical Student Rotation, has
been to England, Costa Rica, Jamaica,
and St. Kitts and Nevis. Her travels, along
with her study of public health, have
“equipped me with the necessary knowledge and skills for working with a diverse
oncology population,” she said.
“Witnessing firsthand how my grandfather fought and lost his battle with cancer
motivated me to apply for the Medical
Student Rotation,” she explained. “I was
ecstatic to discover that I was chosen
as a recipient.” Ms. Pemberton served
her rotation at All Children’s Specialty
Care of Tampa this past summer, where
she gained “a greater awareness of the
impact of cancer in pediatric patients and
how physicians and other members of the
health care team collaborate to maintain
some semblance of a normal childhood
for these unique patients.”
An interest in cancer health dispari-
ties led Derrick D. Cox, MD, a surgical
oncology fellow at Roswell Park Cancer
Institute, to apply for the Resident Travel
Award. As a recipient, “I feel a tremendous responsibility to make a difference
in populations disproportionally affected
by cancer,” he said. He applied for the
program during his chief resident year in
surgery at Georgetown University Hospital.
His experiences at the 2009 ASCO
Annual Meeting may help him to achieve
his goal. “It was awe-inspiring,” he said,
“to see so many people committed to the
care of patients with cancer. I enjoyed
going to a variety of lectures and presentations, as well as the scientific poster
sessions. In addition, I truly enjoyed the
Fellows and Active-Junior Lounge and
the access to pre-eminent speakers. The
knowledge and networking I gained while
at the Meeting motivated me to join ASCO
[as a member] at the conference.”
Renee Funches, MD, of Emory University Hospital, also attended the 2009
Annual Meeting as part of the Resident
Travel Award. “This was the first time I
had ever been to a conference like this
and it was very exciting. It was a great
opportunity to explore many areas in
oncology that I had not been exposed to
much before, such as neuro-oncology,
gynecologic oncology, survivor care,
and palliative care. My attendance has
strengthened my desire to learn all I can
in this field during my oncology fellowship
to provide my patients with the best and
most current treatment modalities,” Dr.
Funches said.
Ultimately, the experiences of these
medical students, residents, and practitioners will help to bring compassionate and
necessary treatment to the most underrepresented patient communities. “There
are a lot of areas in this great country
that are really lacking in access to care,”
Dr. Haslem said. For him, participating in
the Diversity in Oncology Initiative underscores “the commitment that ASCO is
making to bring quality care to the underserved.”
ASCO NEWS & FORUM |
31
The ASCO Cancer
Foundation®, ASCO Ring
NYSE Bell to Strengthen
Cancer Awareness
T
he ASCO Cancer Foundation® and
ASCO joined the ranks of many
notable businesses and organizations by ringing the New York
Stock Exchange (NYSE) Closing Bell on
Wednesday, August 19.
The official bell ringing, which is used
to signal the start or end of trading for the
business day, is a popular marketing platform, offering non-profit organizations like
ASCO an opportunity to raise awareness
of their mission and work. The bell ringing
marked the Foundation’s 10th anniversary and will raise awareness of the need
for cancer research funding, improving cancer prevention and patient care
)URPOHIWWRULJKW/DUU\1RUWRQ0'*HRUJH:6OHGJH0'(ULF6KDQWHDX
5LFKDUG$GDPRQLV6HQLRU9LFH3UHVLGHQW&RUSRUDWH&RPPXQLFDWLRQV1<6(
(XURQH[W'RXJODV:%OD\QH\0'/DZUHQFH+(LQKRUQ0'5LFKDUG/
6FKLOVN\0'-RVHSK6%DLOHV0'$OOHQ6/LFKWHU0'DQG1DQF\5'DO\
0603+ULQJLQJWKH&ORVLQJ%HOORQ$XJXVW
32 | OCTOBER 2009
1
through education, and giving patients the
best, most reliable cancer information.
Foundation Board of Directors member
Lawrence H. Einhorn, MD, rang the bell
alongside his patient, Olympic swimmer
and testicular cancer survivor Eric Shanteau. Dr. Einhorn is a world-renowned
testicular cancer expert who changed the
face of the disease through his research
and education efforts. In addition to
treating Mr. Shanteau, he also led the
team of oncologists who treated Lance
Armstrong when the celebrated cyclist
was diagnosed with testicular cancer.
´
7KLV>HYHQW@KDVDOORZHG$6&2³DQG
HVSHFLDOO\7KH$6&2&DQFHU)RXQGDWLRQ³WR
UHDOL]HDQHZOHYHORIQDWLRQDO
UHFRJQLWLRQIRURXUZRUN
µ
²$OOHQ6/LFKWHU0'$6&2&(2
PHOTOGRAPHS BY DANA HOWE
1. Eric Shanteau, Larry Norton, MD, and
Douglas W. Blayney, MD, (left to right)
inspect the NYSE gold medallion that was
given to all attendees of the bell ringing.
3
“This [event] has allowed ASCO—and
especially The ASCO Cancer Foundation—
to realize a new level of national recognition for our work,” said Dr. Lichter.
“Ringing the bell at the New York Stock
Exchange is something every organization covets and few will achieve. We
hope to build off this event to carry our
oncology messages to a broad audience
throughout the country. We are very
grateful to Foundation Board member
Larry Einhorn, MD, for opening the door
for us at the New York Stock Exchange,”
he added.
At a reception following the bell ringing,
the Honorable Michael Bloomberg, Mayor
of New York City, was presented with
the 2009 ASCO Public Service award.
“This award was established to recognize
individuals who, through their advocacy
at the legislative and community levels,
have increased public awareness about
cancer and have had a positive impact
on cancer-related policies and programs,”
said Dr. Blayney, who presented the
award with Dr. Schilsky.
Through his Bloomberg Initiative to
Reduce Tobacco Use partnerships, grants
are being awarded in low- and middleincome countries to deliver high-impact
tobacco control interventions. In 2006,
Mayor Bloomberg’s $125 million, twoyear contribution more than doubled the
global total of private and public donor
resources devoted to fighting tobacco
use in developing countries, where more
than two-thirds of the world’s smokers
live. Last year, Mayor Bloomberg and
the Bill & Melinda Gates Foundation
announced a commitment of $500 million to the global fight against tobacco
use—specifically, to focus on helping governments in developing countries implement proven policies and programs to
reduce the use of tobacco products.
“I would like to thank ASCO and The
ASCO Cancer Foundation for this honor,”
Mayor Bloomberg said. “Our Administration is doing its part by moving beyond
responding to illness and disease to actually preventing them. The Foundation,
2. ASCO founding member Jane C. Wright,
MD (seated) talks with NY City Council
Speaker Christine Quinn (background),
Larry Norton, MD, Mayor Bloomberg (far
right), and NYSE attendees.
3. Mayor Bloomberg is presented with the
2009 ASCO Public Service Award.
which continues to fund the efforts we
need to win this important fight, marked
its 10th anniversary today by ringing
the closing bell at the New York Stock
Exchange. I can’t wait for the day when
we ring the closing bell on cancer.”
Other notable speakers at the reception included New York City Council
Speaker Christine Quinn and Jane C.
Wright, MD, one of the seven founding
members of ASCO. In attendance were
Foundation Board of Directors sitting
members Michael Goldstein, MD; Martin J. Murphy, Jr., MD; Nora Janjan, MD,
MPSA; and Sandra Swain, MD; along with
Past Chair of the Foundation Board of
Directors Dr. Norton.
ASCO NEWS & FORUM |
33
Member Benefits Abound
at ASCO Meetings
T
he ASCO Annual Meeting and cosponsored thematic symposia offer
something of value for every oncology professional, regardless of the attendee’s affiliation with ASCO. But Society
members do receive special benefits at
the Annual Meeting and thematic symposia that can add significant value to their
experience there and beyond.
“When I walk away from the Annual
Meeting, I’ve brushed up on some things
that I don’t normally see, for example in
the Highlights of the Day session and
other Education Sessions. I feel like I’m a
stronger oncologist and I’m better able to
serve my patients when I leave the Annual
Meeting every year,” John E. Pippen, Jr.,
MD, of Sammons Cancer Center, said. For
Dr. Pippen, an ASCO member since 1999,
the Annual Meeting and thematic symposia are places where members can really
see their benefits at work.
“As a practicing oncologist, my membership in ASCO has been extremely valuable. The educational materials help me
help my patients. I feel like I’ve helped
my fellow oncologists through my service
on ASCO committees. I’ve made friends
throughout the world who are all working
together to help patients with cancer. I
recommend that every single person who’s
interested in oncology join ASCO,” he said.
Eliezer Robinson, MD, of the National
Council For Oncology and the Israeli Cancer Association, has attended the ASCO
Annual Meeting for the past 30 years.
“I hear the lectures, meet a lot friends,
make new friends, and exchange ideas,”
34 | OCTOBER 2009
he said. “I come back home with new
ideas, new energy, and hoping to give better care to my patients.”
Significant Savings on
Registration, Materials
As the global economy continues to be
unpredictable, discounts and savings are
more important than ever. ASCO members
save 30% to 60% off the nonmember registration rate at the ASCO Annual Meeting
and co-sponsored symposia—savings that
can reach hundreds of dollars per year.
Members also receive discounts on
educational products such as Virtual
Meeting and podcast presentations from
meeting sessions, which can enhance
their experience at the Meeting and serve
as reference and educational materials
after the event concludes. Members who
register before general registration opens
also get the first choice of ticketed Meet
the Professor and Clinical Problems in
Oncology sessions, and receive discounts
on these purchases as well, allowing
member attendees to maximize their educational opportunities during the meeting.
In addition, members receive many
meeting materials, including the Annual
Meeting Proceedings and ASCO Educational Book, at no charge.
“Once a person samples some of the
things that ASCO provides, they’ll want
more,” Dr. Pippen said. “Discounts for
attending the Annual Meeting, for me,
really encourage attendance. When people see how great the event and the materials are, they’ll want to come back.”
Exclusive Access to Lounges
Emerging oncologists who join ASCO also
have access to the Fellows and ActiveJunior Lounge, a private room with light
refreshments, computers, and quiet
space for networking, conversations, and
discussions with Meeting faculty. Dr.
Pippen, who participated in several presentations on topics of interest to earlycareer oncologists at the 2009 ASCO
Annual Meeting, noted that “I encourage
people to take advantage of ASCO membership starting as a fellow. You’re really
missing out if you wait to join.”
Sponsor Your Own Science
More than 2,200 abstracts were presented at the ASCO Annual Meeting in
2009—all of them were sponsored by
ASCO members. Clinical scientists and
translational researchers who are members of ASCO can sponsor their own
The Value of Membership
abstracts. Nonmembers must find an
Active or Active-Junior member to sponsor their abstract, spending time and
effort that could otherwise be devoted
to research or patient care. (Restrictions
apply based on membership category.)
A Sense of Belonging
MEMBERS: Register and Reserve
Housing Today
Member registration and housing reservations for the 2010 ASCO Annual
Meeting are now open. Members
have always enjoyed the benefit of
reserving their Annual Meeting housing before the housing block is made
available to nonmember attendees.
This year, as an added member benefit, ASCO members can streamline
their Annual Meeting experience by
reserving housing and registering
for the Meeting simultaneously. Visit
ASCO.org and type ascoannualmeeting to register and reserve housing.
Abstract submission for the Annual
Meeting opens in early November 2009
and closes on January 12, 2010, at
11:59 PM (EST). Visit www.asco.org/
callforabstracts to review the Call for
Abstracts submission information.
PHOTOGRAPH BY TODD BUCHANAN
ASCO members may observe an intangible benefit at the ASCO Annual Meeting or
thematic symposia: the sense that this is,
at heart, their meeting, executed by the
organization to which they belong.
“I have a sense of ownership when I’m
at the Annual Meeting, especially because
of some of the work we’ve done on ASCO
committees,” Dr. Pippen said. “When we
provide our input, the ASCO staff really
listens. I have enjoyed committee work
with ASCO for more than 10 consecutive
years and have found it to be a rewarding
part of my practice of oncology. We not
only improve the organization itself, but
through our committee work we improve
the care of the oncology patient. I feel like
I’ve had a part in that.”
And although the science presented at
the Annual Meeting is intended for all, it is
members who serve on the various Society committees who determine the scope,
breadth, and focus of the event.
“I’ve served on the Cancer Education
Committee and I’ve been actively involved
in the Career Development Subcommittee, so I take pride in the way that the
Meeting has shaped up. I feel like I’ve
contributed to its success. Being a member, where I am doing things to improve
the practice of oncology and improve the
Meeting itself, I think I’m getting something more out of the Meeting than a nonmember,” Dr. Pippen said.
Dr. Robinson, who serves as Chair of the
International Affairs Committee, considers his ASCO membership to be “so good
that I cannot describe it. [ASCO] brings so
much support to the oncology community
and to patients with cancer.”
2009 ASCO Annual Meeting attendees take a break for coffee and networking between sessions. ASCO members receive significant benefits at the event.
ASCO NEWS & FORUM |
35
3UHSDULQJ
WKH1H[W
*HQHUDWLRQRIM
$6&2/HDGHUV
3URJUDPRIIHUVOHDGHUVKLS
WUDLQLQJWRHPHUJLQJ
RQFRORJLVWV
embers interested in taking a larger role in ASCO have
a chance to gain extensive exposure to the Society’s
mission, leadership positions within the organization,
and ASCO’s role in improving cancer care and patient welfare by
participating in the organization’s formal Leadership Development Program.
The year-long program is designed to set early-career oncologists on the path to becoming future leaders within the Society.
The Leadership Development Program requires a time commitment for travel and training. Program participants are required
to attend all Leadership meetings/activities, including the 2010
ASCO Annual Meeting in Chicago, Illinois, and three visits to
workshops in Washington, DC. During this time, participants will
network with Society leaders, participate in a leadership boot
camp at ASCO Headquarters, and gain firsthand knowledge
about key ASCO research activities.
Members will also participate in an interactive learning
/HDGHUVKLS'HYHORSPHQW3URJUDP&ODVVRI
Anees B. Chagpar, MD
University of Louisville
School of Medicine
Quyen Chu, MD
Louisiana State University
Health Sciences Center
Christine H. Chung, MD
Vanderbilt University
School of Medicine
Gregg E. Franklin, MD,
PhD
New Mexico Cancer Center
Matthew D. Galsky, MD
Comprehensive Cancer
Centers of Nevada
project, allowing them to collaborate with both ASCO staff and
volunteers. The project will offer hands-on training that will further their leadership skills as well as benefit the Society.
Program participants will graduate from the Leadership
Development Program during the 2011 ASCO Annual Meeting
in Chicago. Upon completion of the program, graduates will
have opportunities to enter into roles in ASCO’s committees
and task forces.
Application materials are due October 13, 2009, and must be
submitted online. The application is available at www.asco.org.
Enter “leadership” in the search box. At the time of application,
36 | OCTOBER 2009
PHOTOGRAPH BY ANDREA SMILEY
Jill Gilbert, MD
Vanderbilt University
School of Medicine
Nasser H. Hanna, MD
Indiana University
Dawn L. Hershman, MD
Columbia University
College of Physicians and
Surgeons
the applicant must fulfill the following criteria:
Q Be a physician (MD, DO, or international equivalent with
explanation)
Q Have completed final subspecialty training between 2000
and 2005
Q Be currently licensed and residing in the United States
Q Be an active member of ASCO
Q Have a supervisor/senior member from one’s institution/practice provide a letter of support. If the supervisor/senior member is not an active ASCO Member, a supporting letter from an
active ASCO member must be included.
Amreen Husain, MD
Stanford University School
of Medicine
Jyoti D. Patel, MD
Northwestern University
Feinberg School of Medicine
For more information on ASCO’s Leadership Development
Program, please visit www.asco.org and type “leadership” in the
search box. Interested parties may send questions about the
program by e-mail to professionaldevelopment@asco.org.
Top: Participants in ASCO’s Leadership Development Program visited
ASCO headquarters August 12, 2009 as part of the year-long training
they will receive.
ASCO NEWS & FORUM |
37
Expert Analysis
Update from the 2009 ASCO Annual Meeting
The Treatment of Metastatic HER2-positive Gastric Cancer with
Chemotherapy and Trastuzumab
By David H. Ilson, MD, PhD, FACP
Memorial Sloan-Kettering Cancer Center
Weill Cornell Medical College
T
he late-breaking abstract LBA4509, “A phase III study of
trastuzumab added to standard chemotherapy in first-line
HER2-positive advanced gastric cancer,” presented by Eric
Van Cutsem, MD, PhD, of the University Hospital Gasthuisberg
and the University of Leuven, Belgium, is a landmark study in
metastatic gastric cancer that has the potential to change clinical practice.1 The study addressed two questions:
Q Can we screen and identify patients with gastric cancer whose
tumors overexpress HER2?
Q Does trastuzumab improve survival when added to chemotherapy in HER2-positive metastatic gastric cancer?
Dr. Van Cutsem’s study, the Trastuzumab in Gastric Cancer
(ToGA) trial, is an international collaboration conducted across
Europe, Asia, and Central and South America. The study included
3,807 patients with locally advanced unresectable or metastatic
gastric cancer who were screened for HER2 overexpression.
Central testing was performed using immunohistochemistry (IHC)
and fluorescent in situ hybridization (FISH). Positive patients
were defined as either IHC 3+ or FISH+. HER2 positivity was identified in 810 patients (22%) and 584 were treated on protocol.
The study treatment arms were:
1. Cisplatin 80 mg/m2 day 1, plus infusional 5-FU 800 mg/m2/
day for five days, or capecitabine 1000 mg/m2 BID for 14
days, cycled once every three weeks.
2. Chemotherapy plus trastuzumab 8 mg/kg loading dose followed by 6 mg/kg, every three weeks.
Chemotherapy with either 5-FU or capecitabine was selected
by the treating physician.
The primary endpoint was overall survival. Secondary endpoints included progression-free survival, response rate, and
safety. Half of the patients were treated in Asia and one-third
38 | OCTOBER 2009
in Europe, three-quarters had an intestinal histology, and onefifth had prior gastrectomy. The majority had metastatic disease
(97%) that was measurable (90%), and most had more distal
gastric primaries. The majority of patients were treated with
capecitabine (87%-88%).
Median overall survival was significantly improved for patients
receiving trastuzumab: 13.8 months compared to 11.1 months
for chemotherapy alone (HR 0.74, p=0.0046) (Figure 1). Progression-free survival was also improved with trastuzumab (6.7
months compared to 5.5 months, HR 0.71, p=0.0002) (Figure
2), and response was superior with trastuzumab (47% compared
to 35%, p=0.0017) (Figure 3). Nearly all subgroups of patients
benefited from the addition of trastuzumab, including gastric or
gastroesophageal (GE) junction primary, and patients treated
with capecitabine or 5-FU. Adverse events were comparable in
the treatment arms, with the exception of a greater incidence of
asymptomatic decline in left ventricular ejection fraction to less
than 50% (5.9% for trastuzumab compared to 1.1% for chemotherapy alone).
The Chemotherapy Question
Two-drug chemotherapy based on 5-FU and cisplatin is the
global standard of care for metastatic GE cancer. Toxicity varies
widely dependent on the dose and schedule of administered
5-FU, with a weekly or twice weekly infusion schedule2 or a
more protracted low-dose infusion3 tending to lessen toxicity
compared to bolus or 4-5 day infusions. Lowering the dose of
cisplatin to 60-80 mg/m2 also lessens gastrointestinal, renal,
and hematologic toxicity.3,4 Adding a third agent to 5-FU and
cisplatin—epirubicin on the ECF regimen3 and docetaxel on the
DCF regimen5 —may modestly improve response and survival;
however, toxicity is greater and three-drug regimens may not
be the ideal backbone for adding a targeted agent. The regimen most commonly used on the ToGA trial, capecitabine plus
cisplatin, performed well both as a control arm (median overall
survival: 11.8 months) and in combination with trastuzumab,
with acceptable rates of toxicity, consistent with other phase III
trials employing capecitabine.4,6 Whether or not more cumbersome and toxic three-drug regimens will permit the addition of
targeted agents remains to be established in ongoing phase II
and III trials.
Event
Figure 1. Primary endpoint: OS
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
OS
167
182
13.8
11.1
FC + T
FC
11.1 0
2
4
6
Median
HR
Events
0.74
95% CI
p value
0.60, 0.91
0.0046
13.8 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36
Time (months)
Number at Risk
294 277 246 209 173 147 113
90
71
56
43
30
21
13
12
6
4
1
0
290 266 223 185 143 117
64
47
32
24
16
14
7
6
5
0
0
0
90
Event
Figure 2. Secondary endpoint: PFS
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
Median
PFS HR
Events
FC + T
FC
5.5 0
2
6.7
5.5
226
235
0.71
95% CI
p value
0.59, 0.85
0.0002
6.7 4
6
8
10 12 14 16 18 20 22 24 26 28 30 32 34
Time (months)
Number at Risk
294 258
201
141
95
60
41
28
21
13
9
8
6
6
6
4
2
0
290 238
182
99
62
33
17
7
5
3
3
2
2
1
1
0
0
0
The Targeted Therapy Question
The trial by Dr. Van Cutsem and colleagues is the first trial to
validate the addition of a targeted agent to chemotherapy in
gastric cancer, in particular identifying a subpopulation of HER2positive patients likely to benefit most from the addition of a
new agent. Other targeted agents awaiting completion of phase
III trials include bevacizumab, cetuximab, panitumumab, and
lapatinib.
The conclusions of the study’s authors were:
Q Trastuzumab is the first biologic therapy to show a survival
benefit in advanced gastric cancer.
Q Trastuzumab in combination with chemotherapy is a new
treatment option for patients with HER2-positive advanced
gastric adenocarcinoma.
Analysis
The positive results of the ToGA trial establish trastuzumab as
a new and active therapy option in esophagogastric cancers
overexpressing HER2. As in breast cancer, oncologists will
now have to test esophagogastric cancer for overexpression
of HER2. Another landmark achieved on the ToGA trial is the
median survival exceeding one year, a first for a multinational
phase III trial in advanced esophagogastric cancer. The challenge is to move forward with trials of adjuvant trastuzumab in
HER2-positive esophageal and gastric cancers in the potentially
curative setting.
References
Figure 3. Secondary endpoint: tumor response rate
Intent to treat
p = 0.0017
60
p = 0.0145
Patients (%)
50
47.3%
40
41.8%
30
32.1%
34.5%
p = 0.0599
20
10
5.4%
2.4%
0
CR
ORR = CR + PR
CR, complete response; PR, partial response
PR
ORR
F+C + trastuzumab
F+C
1. Van Cutsem E, Kang YK, Chung HC, et al. Efficacy results from the ToGA trial:
a phase III study of trastuzumab added to standard chemotherapy in first-line
human epidermal growth factor receptor 2 (HER2)-positive advanced gastric
cancer. J Clin Oncol. 2009;27(Sup 15S):204.
2. Al Batran S, Hartmann J, Probst S, et al. Phase III trial in metastatic
gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either
oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische
Onkologie. J Clin Oncol. 2008;26:1435-42.
3. Webb A, Cunningham D, Scarffe JH, et al. A randomised trial comparing ECF
with FAMTX in advanced oesophago-gastric cancer. J Clin Oncol. 1997;15:2617.
4. Kang Y, Kang W, Shin D, et al. Capecitabine/cisplatin versus 5-fluorouracil/
cisplatin as first-line therapy in patients with advanced gastric cancer: a
randomised phase III noninferiority trial. Ann Oncol. 2009;20:605-8.
5. Van Cutsem E, Moiseyenko VM, Tjulandin S, et al. Phase III study of docetaxel
and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as firstline therapy for advanced gastric cancer: a report of the V325 Study Group. J
Clin Oncol. 2006;24:4991-7.
6. Cunningham D, Starling N, Rao S, et al. Capecitabine and oxaliplatin for
advanced gastric cancer. New Engl J Med. 2008;358:36-46.
ASCO NEWS & FORUM |
39
Scientific Highlights
from Other Meetings
Randeep Sangha, MD, of the University of Alberta, Canada, delivers a
presentation at the 10th International Lung Cancer Congress.
and case-based discussions. At afternoon workshops, renowned
oncology experts discussed novel therapeutic agents in the
pipeline and conducted a multidisciplinary tumor board. During
a special session, representatives from North American, European, and Japanese lung cancer cooperative groups presented
updates from ongoing clinical trials and discussed potential
intercontinental scientific collaborations.
Early-stage Non-small Cell Lung Cancer
10th International Lung Cancer
Congress
Kohala Coast, Hawaii
June 17-20, 2009
By David Gandara, MD
Co-chair, 10th International Lung Cancer Congress
University of California, Davis Cancer Center
Roy S. Herbst, MD, PhD
Co-chair, 10th International Lung Cancer Congress
The University of Texas M. D. Anderson Cancer Center
David J. Lee, PhD
Physicians’ Education Resource
T
he 10th Annual International Lung Cancer Congress, organized by David Gandara, MD, of the University of California,
Davis, and Roy Herbst, MD, PhD, of M. D. Anderson Cancer
Center, highlighted recent advances in the diagnosis and treatment of thoracic malignancies, including data presented at the
2009 ASCO Annual Meeting. Approximately 200 attendees gathered for the event, with significant representation of physicians
from European and Asian lung cancer cooperative groups. Morning sessions featured state-of-the-art didactic lectures followed
by the presentation of recent research results, expert debates,
40 | OCTOBER 2009
Heather Wakelee, MD, of Stanford University, discussed the
(Neo)Adjuvant Taxol/Carboplatin Hope (NATCH) trial evaluating
preoperative or postoperative carboplatin/paclitaxel or observation in patients with resected non-small cell lung cancer
(NSCLC).1 The results demonstrated no significant difference in
the primary endpoint of five-year disease-free survival between
the patients who were randomized to surgery alone, adjuvant,
or neoadjuvant chemotherapy. Of note is the fact that approximately 75% of the patients on this trial had clinical stage I disease, a patient subgroup that has been shown to receive the
least benefit from perioperative chemotherapy.
Maintenance Therapy
Karen Kelly, MD, of the University of Kansas, presented the
results of phase III studies on maintenance therapy, also referred
to as early second-line therapy, in patients with advanced
NSCLC. These studies investigated pemetrexed, single-agent
erlotinib (Sequential Tarceva® in Unresectable NSCLC [SATURN]
trial), and the addition of erlotinib to maintenance bevacizumab
(AVF3671g [ATLAS]) in patients who achieved a response or
stable disease after a frontline regimen.2-4 All three trials met the
primary endpoint of improved progression-free survival compared
to the placebo arm. Pemetrexed also demonstrated improved
overall survival compared to placebo; with regards to efficacy,
the benefit was restricted to patients with nonsquamous histology. In the SATURN trial, an overall survival benefit for erlotinib
versus placebo was announced in a press release, with details
PHOTOGRAPH BY SCOTT LEBLANC. © 2009, MEDICAL MEDIA HOLDINGS, LLC
/XQJ&DQFHU$GYDQFHVDQG&OLQLFDO7ULDOV
+LJKOLJKWHGDW5HFHQW0HHWLQJV
to be presented at the 13th World Conference on Lung Cancer.
Survival information from the ATLAS trial is still pending.
Epidermal Growth Factor Receptor Inhibitors
Paul A. Bunn, Jr., MD, of the University of Colorado, summarized
the use of epidermal growth factor receptor (EGFR) tyrosine
kinase inhibitors (TKIs) in patient populations selected for
response to this class of agents. This trial, known as the Iressa™
Pan-Asia Study (IPASS) study, was conducted in Asia and compared gefitinib to carboplatin/paclitaxel in never smokers or light
ex-smokers with adenocarcinoma.5 In this trial, gefitinib demonstrated superior progression-free survival compared to chemotherapy; however, biomarker analysis revealed that even in these
patients clinically selected to favor EGFR TKI therapy, only those
with EGFR mutations derived a significant progression-free survival benefit from gefitinib compared to chemotherapy.
Román Pérez-Soler, MD, from the Albert Einstein College of
Medicine, reviewed recent data on the use of EGFR antibodies in
patients with lung cancer. Biomarker analyses were performed
to examine correlations between efficacy and KRAS mutations or
EGFR status (mutations, gene copy number, protein expression).
Unlike what was observed in colorectal cancer, retrospective
analyses of the First-line in Lung Cancer with Erbitux® (FLEX) and
BMS-099 trials did not show KRAS mutations as a negative predictive marker for cetuximab in NSCLC.6,7 Additionally, EGFR gene
copy number by fluorescence in situ hybridization (FISH) did not
correlate with treatment outcomes with cetuximab in either trial.
However, these biomarker analyses were limited in statistical
power by the small sample size.
Multidisciplinary Tumor Board
A new activity that had its debut at the event was a multidisciplinary tumor board held during one of the afternoon workshops.
The distinguished panel included surgeon Harvey I. Pass, MD, of
the New York University School of Medicine, radiation oncologist
Walter Curran, Jr., MD, of Emory University School of Medicine,
and medical oncologist Martin Edelman, MD, of the University
of Maryland. Cases included resectable stage III disease, earlystage disease with poor pulmonary function, and prophylactic
cranial irradiation in stage III disease. This session fostered interaction between community physicians and the multidisciplinary
panel of lung cancer experts.
Cooperative Group Session
One of the unique features of the International Lung Cancer
Congress is the special session for cooperative groups from the
United States, Europe, and Asia to present current and planned
clinical studies. Senior representatives from each cooperative
group presented an overview of their group’s activities in various
disease settings, thereby stimulating interaction between the
different groups. The proceedings of this session will be summarized in a special peer-reviewed manuscript to be published in an
upcoming issue of Clinical Lung Cancer.
References
1. Felip E, Massuti B, Alonso G, et al. J Clin Oncol. 2009; 27(suppl): 382s (Abstract
7500).
2. Belani CP, Brodowicz T, Ciuleanu T, et al. J Clin Oncol. 2009; 27(suppl):806s
(Abstract CRA8000).
3. Cappuzzo F, Ciuleanu T, Stelmakh L, et al. J Clin Oncol. 2009; 27(suppl):407s
(Abstract 8001).
4. Miller VA, O’Connor P, Soh C, et al. J Clin Oncol. 2009; 27(suppl):799s (Abstract
LBA8002).
5. Fukuoka M, Wu Y, Thongprasert S, et al. J Clin Oncol. 2009; 27(suppl):408s
(Abstract 8006).
6. O’Byrne KJ, Bondarenko I, Barrios C, et al. J Clin Oncol. 2009; 27(suppl):408s
(Abstract 8007).
7. Khambata-Ford S, Harbison C, Woytowitz D, et al. J Clin Oncol. 2009;
27(suppl):412s (Abstract 8021).
CALGB Summer Group Meeting
The Role of Cooperative Groups in
Biomarker Studies
By Jeffrey Peppercorn, MD, MPH
Assistant Professor of Medicine
Division of Medical Oncology
Duke University Medical Center
During the Plenary Session, Dr. Schilsky presented a review of
CALGB involvement in the development of clinical biomarkers,
from exploratory studies to randomized trials using biomarkers
to guide therapy. He highlighted the work of Dr. Bertagnolli in
early stages of biomarker development. Dr. Bertagnolli and colleagues demonstrated that among patients with stage III colon
cancer and a DNA mismatch repair deficiency in the primary
tumor, outcomes were improved with the use of an adjuvant chemotherapy regimen containing irinotecan, moving the management of colorectal cancer further in the direction of personalized
therapy.1 In addition, Dr. Schilsky reviewed recently published
studies by Daniel F. Hayes, MD, of University of Michigan, and
colleagues that explored the role of endocrine receptor and
HER2 biomarkers in predicting benefit from sequential taxane
therapy after anthracyclines for adjuvant breast cancer management.2 Also discussed was the work of Martin J. Edelman, MD,
of Greenebaum Cancer Center, and colleagues in demonstrating
the negative prognostic impact of COX-2 in non-small cell lung
cancer, leading to development of a randomized trial of COX-2
inhibition, CALGB 30203, in select patients.3
The cooperative groups are also playing an important role in
T
he Cancer and Leukemia Group
B (CALGB) 2009 Summer Group
Meeting highlighted the role of cooperative groups in biomarker studies and
updated members on recent progress in
clinical trials. The new Group Chair-Elect
was announced: Monica Bertagnolli, MD,
Chief of Surgical Oncology at Brigham and
Women’s Hospital and a researcher into
the molecular biology of gastrointestinal
cancers at the Dana Farber Cancer Institute, will take on the
mantle of leadership from Richard L. Schilsky, MD, Professor
of Medicine and Associate Dean for Clinical Research at the
University of Chicago and ASCO Immediate Past President. Gini
Fleming, MD, of the University of Chicago, was announced as the
Group Vice Chair Designee.
ASCO NEWS & FORUM |
41
conducting large multi-group trials involving biomarker validation. These trials are
designed to demonstrate that a biomarker
can guide choice of therapy and improve
outcomes for patients on the basis of
more personalized treatment approaches.
One example is N0723, a study involving the North Central Cancer Treatment
Group (NCCTG), CALGB, the Eastern
Cooperative Oncology Group (ECOG),
the Southwest Oncology Group (SWOG),
the National Cancer Institute of Canada
(NCIC), and collaboration with partners in
industry to evaluate the role of erlotinib,
an epidermal growth factor receptor
(EGFR) inhibitor, in patients with and without overexpression of EGFR who receive
pemetrexed as second-line therapy for
metastatic non-small cell lung cancer.
Another example is CALGB 30506, a
randomized trial designed to evaluate the
ability of genomic prognostic model developed by Anil Potti, MD, of Duke University,
and colleagues to identify patients with
stage I non-small cell lung cancer as candidates for adjuvant chemotherapy.4
Dr. Schilsky noted the challenges
involved in biomarker studies, including
the adequacy of biospecimen collection,
sources of funding for research, regulatory
requirements, and developing contractual
agreements with commercial partners.
However, cooperative groups have demonstrated that they have the capacity to
conduct large biomarker studies, including
formal validation trials, which can translate the emerging understanding of molecular differences between cancers into
more personalized selection of therapy
that can improve outcomes for patients.
New Understanding of an
Old Drug
The theme of personalized medicine
continued in the Breast Cancer Session,
in which David Flockhart, MD, PhD, of
Indiana University School of Medicine,
spoke on the emerging evidence for the
importance of the CYP2D6 genotype in
tamoxifen metabolism for patients with
breast cancer. Tamoxifen is metabolized to endoxifen by a hepatic enzyme,
42 | OCTOBER 2009
CYP2D6, and patients have genetic differences that can lead to greater or lesser
degrees of metabolism. These differences have been shown to correlate with
outcomes, though much of the work to
date has been in small retrospective studies.5 Dr. Flockhart discussed two studies
presented at the 2009 ASCO Annual
Meeting that evaluated the impact of
concurrent use of tamoxifen and CYP2D6
inhibitors on breast cancer outcomes. In
a study conducted by Dr. Flockhart and
colleagues6 involving the Medco pharmaceutical claims database, patients
receiving tamoxifen and a CYP2D6 inhibitor (typically one of the serotonin-specific
reuptake inhibitors used for depression)
had a higher risk of breast cancer recurrence over two years compared to those
on tamoxifen alone (13.9% vs. 7.5%; HR
1.92, 95% CI 1.33–2.76, p<0.001).
Although a different group of investigators from the Netherlands conducted
a similar study involving a pharmacy
database and found no clear association
between concurrent prescriptions for
tamoxifen, CYP2D6 inhibitors, and differences in breast cancer outcomes, Dr.
Flockhart noted both that methodological
limitations restrict our ability to interpret
the second study, and that at this time the
potential for an adverse effect from the
use of strong CYP2D6 inhibitors among
patients taking tamoxifen for breast cancer suggests a reason to avoid overlap
of these drugs until the data becomes
more clear.7 In discussion, it was noted
that some oncologists are currently using
CYP2D6 testing to evaluate the potential
benefits of tamoxifen, but the majority
are waiting for the pending results of
large randomized trials that will allow us
to better determine if testing and alternative treatment strategies are appropriate
for women with breast cancer and poor
metabolism of tamoxifen.
Patient-reported Outcomes
Clinical trials are designed to test the
safety and efficacy of a drug, and the
severity, number, and frequency of
adverse events are carefully recorded in
all trials. However, some have questioned
whether the experience of the patients
participating in clinical trials is sufficiently
reported such that future clinicians and
patients can consider the tolerability
of therapy from the patient’s perspective when making treatment decisions.
Ethan Basch, MD, of Memorial SloanKettering Cancer Center and a leader in
the field of patient-reported outcomes
(PRO) research, presented an update on
national efforts to incorporate PRO into
clinical trials and clinical practice. Dr.
Basch reviewed data from his study published in Lancet Oncology demonstrating
that there may be differences in the perception of the frequency and severity of
symptoms among patients and physicians,
particularly for more subjective symptoms,
and that collection of PRO can improve
our understanding of the side effects of
treatment.8 Although there remains discussion of the value of adding PRO to the
U.S. Food and Drug Administration (FDA)
label of new drugs, which currently include
investigator-reported outcomes, Dr. Basch
argued that for many decisions we can
consider expert opinion and public opinion
and still draw meaningful conclusions.
Finally Dr. Basch presented the design
of CALGB 70501, a companion trial
linked to several CALGB randomized trials
designed to assess the feasibility of collecting patient-reported outcomes within
cooperative group trials and to compare
patient vs. clinician reporting of outcomes. Patients from any of eight trials
can participate in CALGB 70501.
References
1. Bertagnolli MM, Niedzwiecki D, Compton CC, et al.
J Clin Oncol. 2009;27:1814-1821.
2. Hayes DF, Thor AD, Dressler LG, et al. N Engl J
Med. 2007;357:1496-1506.
3. Edelman MJ, Watson D, Wang X, et al. J Clin Oncol.
2008;26:848-855.
4. Potti A, Mukherjee S, Petersen R, et al. N Engl J
Med. 2006;355:570-580.
5. Goetz MP, Rae JM, Suman VJ, et al. J Clin Oncol.
2005;23:9312-8.
6. Aubert RE, Stanek EJ, Yao J, et al. J Clin Oncol.
2009;27:18s (Abstract CRA508).
7. Dezentje V, Van Blijderveen NJ, Gelderblom H, et
al. J Clin Oncol. 2009;27:18s (Abstract CRA509).
8. Basch E, Iasonos A, McDonough T, et al. Lancet
Oncol. 2006;7:903-09.
New Award Supports, Recognizes
Crucial Clinical Investigators
A
t a time when a team science
approach to cancer research is
essential, the National Cancer
Institute (NCI) is providing funding
and recognition of clinical investigators
who lead cancer research programs at
academic cancer centers. ASCO’s Cancer
Research Committee (CRC) offered suggestions to NCI on how the award could be
shaped in order to make it most meaningful for investigators who serve in this role.
The new Clinical Investigator Team
Leadership Award will provide two years of
salary support for up to 10 clinical investigators who play leadership roles in clinical
trials at NCI-designated cancer centers.
The award recognizes outstanding clinical
investigators whose work fosters team
science and promotes retention of investigators in the academic setting, individuals
who are not principal investigators on a
National Institutes of Health grant but
who are participating extensively in NCIfunded collaborative clinical trials.
The award was engendered by “the
deliberations of the Clinical Trials Working Group [CTWG], a body convened by
the National Cancer Advisory Board of
NCI to examine methods to improve and
enhance the publicly funded clinical trials
enterprise,” Sheila Prindiville, MD, MPH,
of NCI, explained. “One idea was that NCI
could create new forms of funding support
and academic recognition to promote collaborative team science.”
Dr. Prindiville serves as Director of the
Coordinating Center for Clinical Trials, the
office that implements the recommendations of the CTWG. Her team recognized
that this particular award met a need
which was not being filled. If the program
is successful, the NCI may partner with private foundations to support future awards.
Because several ASCO volunteers
served on the CTWG, the CRC wanted
to offer ASCO recommendations for the
award structure. Theodore S. Lawrence,
MD, Immediate Past Chair of the committee, explained that the award supports
“that critical investigator who is very good
at accruing patients to studies, and is
the glue within the clinical trials group…
the kind of person who ‘makes it happen.’
This person may not be the first author
on the paper or may not have written the
grant, but without his or her efforts the
work never would have occurred.”
After reviewing the CTWG report, the
CRC discussed the potential goals of the
award and the needs of academic investigators. The committee agreed that it
would be critical to offer salary support to
reinforce the important work and provide
the protected time required for the leader
of an academic research program.
In addition to providing funding support, the award gives valuable recognition to investigators who may not have
received significant honors for their
crucial work. “We’re saying that this kind
of job is really valuable—you’re not kept
in the shadows, you’re recognized as a
key contributor in developing new clinical
research,” said Dr. Lawrence, who knows
firsthand the influence that such recognition can have on an oncologist’s career.
In 1987, he was one of the first radiation
oncologists to receive a Young Investigator Award from The ASCO Cancer
Foundation®.
The ASCO Cancer Research Committee
was grateful for the opportunity to provide
feedback to NCI on the development of
the award, as both organizations share
the desire to support, acknowledge, and
recognize outstanding clinical investiga-
tors whose participation and activities
promote successful clinical research
programs, which in turn lead to improved
therapies and outcomes for patients with
cancer. NCI, noted Dr. Lawrence, hopes to
drive investigator-initiated research, while
ASCO serves as the bridge to the practicing oncologists and their desire to implement new therapies.
This award, Joseph S. Bailes, MD, Chair
of the ASCO Government Relations Committee, believes comes at just the right
moment. “One of our big challenges in the
United States is going to be funding cancer research. You look at the health care
reform debate and clearly there’s a recognition that funding for cancer research
is needed. We have a big void between
where we are now and where we need to
be to continue to make advances. Federally-funded research plays a critical role in
answering important research questions.
This program is an innovative mechanism
to help ensure that NCI research fills that
void and is attractive to academic investigators,” he said.
Each award consists of $50,000 per
year for two years paid to the recipient’s
institution, which can be applied toward
the investigator’s salary, fringe benefits,
and associated facilities and administrative costs. Recipients are expected to
devote 10% to 15% of their time to the
activities associated with the award.
For more information on the eligibility
criteria and application process for 2010
Clinical Investigator Team Leadership
Awards, visit ccct.nci.nih.gov.
“We are truly excited to be able to recognize the crucial clinical investigators
without whom we couldn’t conduct these
trials,” Dr. Prindiville said.
ASCO NEWS & FORUM |
43
NEWS
,QVLGH-&2
JCO Reaches New Milestone, Implements Changes
T
he Journal of Clinical Oncology (JCO)
Impact Factor has increased for a
fourth consecutive year, as reported
by Thomson Reuters in its 2008 Journal
Citation Report. Furthermore, the publication has made several changes to its
publication procedures to better serve its
readers.
Impact Factor Increases
to 17.157
The impact factor represents a mean of
the number of papers published during
two years, divided by the total number of
citations in the following year, according
to JCO Editor in Chief Daniel G. Haller, MD.
In 2008, JCO articles were cited a total of
97,639 times—a 20% increase over the
previous year, according to the report. The
rise in the impact factor of nearly 50%
since 2005 is a reflection of the value
researchers find in JCO content.
“JCO is fortunate to receive thousands
of submissions from highly qualified
authors each year and to have outstanding Editors, Editorial Board members, and
peer reviewers who help select the best
articles for publication,” Dr. Haller said in
a statement.
By impact factor, the publication ranks:
Q Fourth of 144 oncology journals
Every six minutes research
published in JCO is
cited in other
peer-reviewed
journals.
44 | OCTOBER 2009
Q
Q
tracked worldwide
Forty-first among all scientific journals
surveyed, putting it in the top 1% of all
science, technology, and medical publications
Second in number of citations among
oncology journals, and 25th among all
6,598 scientific journals monitored
Former Print Columns
Re-launched as Exclusive
Online Content
To better accommodate the publication’s
growing number of submissions and to
meet the needs of a broader readership,
two article types have moved online: Diagnosis in Oncology and Correspondence.
The Diagnosis in Oncology section consists of oncology-specific case reports,
and the Correspondence section consists
of Letters to the Editor, responses from
authors, and short, freestanding pieces.
With JCO editors currently accepting
fewer than 20% of all manuscripts for
publication, “We felt that [these] sections
could be well served by being placed
online only, where there are fewer space
constraints,” Dr. Haller said. “Having
space available in the print version will
allow for the potential of placing more
high-quality original articles, both online
and in print,” he added.
Dr. Haller attributes the increase in the
number of JCO submissions during the
past few years to the Journal’s reputation
and broad international readership.
Placing content exclusively online, however, does not diminish the credibility or
importance of the content. In fact, the
JCO website (jco.ascopubs.org) serves
as the initial repository where readers
can access newly published material.
To get new content out to readers in the
timeliest manner, the online publication
date—not the print publication date—is
the official publication date of record.
“There are many measures of journalistic success [for the Journal] including
meeting readership needs by measures of
online usage and surveys, and by keeping
abreast of trends in medical journalism,”
Dr. Haller said.
The relocation of these sections is an
example of such successes, as these
changes improve the overall publication
and achieve its mission of disseminating
significant clinical oncology research in
both print and electronic formats.
Readers can identify exclusive online
materials by the “Online Only” logo that
accompanies article titles within the JCO
Table of Contents.
New Manuscript Guidelines
for Phase III Trials
Another change for JCO requires authors
to submit a redaction of the protocol for
all phase III studies, including the eligibility criteria, schema and dose modifications, and statistical section (including
endpoints).
Prior to this modification, “Many reviewers and the editors felt they could not
judge a manuscript adequately from the
limited information available in the manuscript, especially in regard to patientselection methodology and statistics,
including endpoints,” Dr. Haller said. “We
felt that phase III trials have the greatest
potential for affecting practice.”
NEWS
-232XWORRN
JOP Examines
the Cost of
Cancer Care
T
he cost of cancer care in the United
States is a critical subject for many
Americans and a topic of debate
within governmental, academic, and
industry groups. The September 2009
issue of the Journal of Oncology Practice
(JOP) focused on the cost of cancer care
and provided important insight on the
causes and potential solutions for the
problem.
In the interview that follows, Michael N.
Neuss, MD, Chair of the Clinical Practice
Committee, discusses important factors
surrounding the cost of cancer care.
AN&F: How is the cost of cancer care
different than the costs of care for other
major diseases?
Dr. Neuss: As is noted in the American
Society of Clinical Oncology Guidance
Statement: The Cost of Cancer Care,
drug costs are generally a greater proportion of the total cost burden for patients
with cancer than for patients with other
diseases. Additionally, the benefits of
using those drugs are not seen in every
patient; in order to help a small number of
patients realize benefit from these drugs,
we must treat a larger number of patients.
We all wear our seat belts, hoping, of
course, that we won’t need them, and
also that they won't somehow cause a
greater problem to us in some unusual
circumstance. Patients with colon cancer
who receive adjuvant therapy individually
may experience no benefit because they
happen to do well even without treatment
(like people who wear their seatbelts and
don't have an accident). Alternatively, in
a sadder circumstance, they might also
suffer a recurrence no matter what treatments they receive. And a few may actually suffer greatly from taking the drugs.
In the end, a treatment that may
include more than $50,000 in drug costs
may be given to 100 patients and only
help 20 of them. Even in a circumstance
where a drug may help a greater proportion of patients, for example the use of
imatinib in chronic myelogenous leukemia,
the daily drug costs of $130 may be too
much for patients to bear. Clearly, there
is a tipping point at which the drug, no
matter how good it is, is unaffordable to
individuals and society. Imagine a drug
that caused metastatic breast cancer to
go into a complete remission, but that
had to be taken every day to maintain the
remission. Would that circumstance be
reasonable if it was priced at $1,000 per
day? What about $5,000?
AN&F: What cost issues need the most
immediate attention or resolution?
Dr. Neuss: As a political issue, out-ofpocket expenses get more attention as
individuals experience the problem. This
is glaringly obvious in the Medicare Part
D “doughnut hole.” However, as a societal issue, total cost is probably more
important. A better understanding of
who benefits from expensive treatments
would go a long way toward helping us
expend resources more wisely, and basic
research is clearly going to be helpful in
this area.
Dr. Neuss: Research will help a lot in
approaching these issues. If we can
remove any questions of whether a particular treatment really helps an individual—
as opposed to a population of people in
similar circumstances—we can more easily understand and discuss the costs and
benefits of an intervention.
AN&F: Are there any ideal solutions?
Dr. Neuss: It is best to intervene only
with a clear understanding of the benefit.
Targeted therapies designed to approach
a specific identified molecular characteristic represent the most effective but also
the most expensive treatments available.
If we had a drug that could be guaranteed
to “cure” 90% of the patients who took it,
but they had to take it every day in order
to keep their otherwise fatal cancer in
remission, what would it be worth?
The definition of circumstances to
increase the likelihood of benefit to our
patients makes it easier to understand
the benefits relative to cost.
AN&F: What role does ASCO play in finding a solution to this problem?
Dr. Neuss: ASCO is a powerful public
voice in educating doctors, patients, and
other interested parties, including the
public at large and legislators. Promoting basic and clinical research, providing
many educational opportunities, and
keeping the discussion fact-based are
all factors in ASCO's approach, which is
exhibited in the guidance statement and
everything the Society does.
Read the full text of the September issue
online at jop.ascopubs.org.
AN&F: What needs to happen first to
make progress?
ASCO NEWS & FORUM |
45
NEWS
:KDW·V1HZLQ3ROLF\ 3UDFWLFH
QOPI® Certification Program Promotes Excellence in Cancer Care
A
SCO has launched the Quality
Oncology Practice Initiative (QOPI®)
Certification Program to recognize
oncology practices that achieve rigorous
standards for high-quality cancer care.
Through this program, ASCO hopes to:
Q Promote the highest quality cancer care
as defined by clinician experts;
Q Provide a trusted solution to satisfy
external demand for quality activities;
and
Q Reduce redundant programs or requirements for oncology practices.
“Increasingly, oncology practices are
being asked by payors, patients, and others to attest to the quality of care they
provide,” ASCO President Douglas W.
Blayney, MD, said. “QOPI Certification will
demonstrate a practice’s commitment to
delivering high-quality cancer care.”
Performance benchmarks can help
practitioners recognize areas for needed
improvement and work towards making
the necessary changes in those specific
areas. ASCO hopes that the process of
preparing for and completing the program will stimulate internal discussion
among practitioners about opportunities
for improvement and implementation of
improved systems.
Outpatient hematology-oncology practices that complete the program will be
certified for three years based on their
achievement in selected QOPI chart
abstraction measures and QOPI Certification Site Assessment. For practices that
do not achieve certification initially, ASCO
will provide improvement resources that
can help ensure success when the practices attempt the certification process
again.
QOPI participation is the first step to
achieving QOPI Certification. QOPI is a
voluntary, self-assessment program to
enable hematology-oncology and medical
oncology practices to assess the quality
of care they provide to patients. Participating practices abstract and submit data
from patient records twice a year. ASCO
analyzes these data for adherence to
more than 80 evidence-based and consensus quality measures and provides
feedback reports to participating practices. Individual practices can compare
their performance to aggregate data from
other practices across the country. Based
on these data, doctors can focus on specific areas for quality improvement. Currently, nearly 500 oncology practices are
enrolled in QOPI.
The QOPI Certification Program will be
available to all practices that meet specific performance requirements and that
pass a new site assessment. Practices
that participate in the fall 2009 QOPI data
collection process will be the first eligible
to receive certification in early 2010.
For more information on the QOPI
Certification Program, visit qopi.asco.org/
certification or send an e-mail to
qopicertification@asco.org.
Clinical Oncology Requirements for the EHR
(CORE): A Collaborative Project of ASCO and NCI
ASCO and the National Cancer Institute
(NCI) have formed a collaboration to
provide a clear understanding of the
electronic health record (EHR) functions
needed to support an oncologist in clinical practice, paving the way for development of oncology-specific products. The
Clinical Oncology Requirements for the
EHR (CORE) project supports ASCO’s goal
of increasing the use of EHRs by clinical
oncologists. Clinical oncology involves
many care processes, such as chemother-
46 | OCTOBER 2009
apy administration, that are not supported
by the EHR products currently on the market. Consequently, many oncologists are
reluctant to adopt them.
The CORE project comes at an opportune time, as the Medicare and Medicaid
programs will begin providing bonuses
to physicians who use EHRs beginning in
2011. In addition, with ASCO’s help, the
Certification Commission on Health Information Technology (CCHIT) plans to begin
certifying oncology-specific EHRs that year.
NEWS
QOPI® Certification Program FAQs
What is the first step to achieving
QOPI Certification?
QOPI participation is the first step to
achieving QOPI Certification. Practices
that meet the scoring requirements
in the fall 2009 QOPI data abstraction round will be the first eligible to
achieve Certification in early 2010.
What other steps are required to
achieve QOPI Certification?
All practices will have to meet a set of
structural quality standards regarding
safe chemotherapy administration.
Also, all Certification materials/data
submitted will be subject to audit.
When can I apply for QOPI Certification?
Practices may apply for Certification
after completion of any QOPI data
abstraction round, if scoring requirements are met. Practices must apply
prior to the initiation of the next QOPI
data collection round. Practices that
meet the scoring requirements during
the fall 2009 QOPI round will be the first
eligible to apply for Certification in January 2010.
What documentation is required to
apply for QOPI Certification?
To be reviewed for QOPI Certification,
a practice must submit the QOPI Certification online application, appropriate
practice fee, QOPI Certification Site
Assessment questionnaire and supportive documentation, and requested chart
audit information.
How long will it take to achieve Certification?
Once a practice has submitted the complete Certification program materials, the
practice will be awarded QOPI-Certification Pending status. Following successful review of submitted materials and
audit activities, QOPI Certification will be
Products
Process and Timeline
The CORE project will result in a white
paper and technical specifications that
EHR vendors and CCHIT can use to
develop and certify oncology-specific
EHRs.
The project has three components:
Q Describe the functions oncologists want
an EHR to perform;
Q Provide the structured data elements to
be used in oncology EHRs; and
Q Provide a common set of interoperability standards that will allow oncologyspecific data to be shared from one
EHR to another.
Dozens of ASCO volunteers, NCI staff,
and participants from the NCI Community
Cancer Centers Program (NCCCP) met
regularly in three work groups to come to
consensus on the detailed functionality,
data elements, and interoperability standards for an oncology-specific EHR. The
groups began meeting in the fall of 2008
and finished their work in summer 2009.
Hundreds of volunteer hours have made
the effort possible.
The discussion on functional requirements builds on previous work by ASCO’s
EHR Workgroup and the oncology commu-
awarded. The Certification review process
is expected to take about three months.
How much does QOPI cost?
QOPI is a free ASCO member benefit.
How much does QOPI Certification cost?
The cost of Certification is based on the
number of hematologist/oncologist fulltime equivalents at the practice. Introductory pricing will be in effect for 2010. For
full details, please visit qopi.asco.org/
application.
Why should I achieve QOPI Certification?
Participation in the QOPI Certification
process should provide the practice
with quality improvement goals, learning opportunities, and feedback. Also,
many payors, employers, and patients
are looking for meaningful indicators that
an oncology practice is achieving highquality care. QOPI Certification will be a
clear designation from ASCO that you can
refer to in your practice communications
and marketing materials.
nity to define an oncology-specific EHR.
The data elements and interoperability
portion of the project builds on previous work by NCI. Once the workgroups
have compiled their findings, they will
be circulated among clinical, technical,
and patient advocacy groups for review
and comment. A white paper and technical specifications will be released at the
ASCO EHR Symposium, which will be held
in San Francisco in October 2009.
ASCO NEWS & FORUM |
47
NEWS
,QWHUQDWLRQDO,QVLJKW
The IDEA Award Offers Travel Opportunities to
the Annual Meeting
T
he ASCO Cancer Foundation is
now accepting applications for the
International Development and Education Award (IDEA). The IDEA Program
enables oncologists in countries with limited resources to attend the ASCO Annual
Meeting and visit a cancer center in the
United States or Canada. The 2010 Annual Meeting will be held in Chicago, Illinois,
from June 4-10, 2010.
The IDEA Program is designed to help
early career oncologists from developing
countries expand their current knowledge,
earn continuing medical education, and
share their learning experience at the
Meeting with colleagues in their home
countries, ultimately enhancing the quality of cancer care around the world. The
grants help international physicians establish strong relationships with ASCO members who serve as scientific mentors. The
monetary award covers expenses associated with attending the Meeting (including
registration, airfare, hotel, and meals)
and the visit to a cancer center. Award
recipients also receive a complimentary
ASCO membership for three years, which
includes a subscription to the Journal of
Clinical Oncology.
The 2010 IDEA application will open
October 1, 2009. Grant criteria and the
application are available at www.asco.org.
Type the word “idea” in the search box.
Applications must be submitted by January 14, 2010.
2009 ASCO Cancer Foundation International Development and Education Award (IDEA) Recipients
Back row: Roxana Scheusan, MD, Susan Msadabwe, MBCHB, FC Rad Onc, Andréia Melo, MD, Naiyarat Prasongsook, MD, Timucin Cil, MD, Clement
Adebamowo, BM ChB Hons, FWACS, FACS, ScD (Chair, IDEA Working Group), Bijesh Ghimire, MD, Roman Shyyan, MD, Luis Ubillos, MD, Hua-Jun Chen,
MD, PhD, Kashif Iqbal, MBBS, MS. Front row: Ritwik Pandey, MBBS, MD, DM, Catherine Nyongesa, MBchB(Nbi), MMED Rad Onc, FC Rad Onc, Dauren
Adilbay, MD, Ilham Merad-Lahfa, MD, Leticia Arruda, MD, Yang Xu, MD, PhD, Cynthia Villarreal-Garza, MD, Raafat Abdel Malek, FRCR, Tabassum
Wadasadawala, MD, DNB. Not pictured: Parisa Karimi, MD.
48 | OCTOBER 2009
NEWS
Cancer in Japan
By Nagahiro Saijo, MD, PhD
Kinki University School of Medicine
Osaka, Japan
I
t is an exciting time for oncology in
Japan. A law to help promote prevention and early detection of cancer
was enacted on June 16, 2006, and
took effect on April 1, 2007. The basic
policies of this law also promote the full
equality in medical care for all cases
of cancer, and the support of cancer
research. Because there is no subspecialty of oncology in Japan, medical
and radiation oncology capabilities lag
far behind those of Western countries.
There are very few well-trained medical
and radiation oncologists. To improve
the situation, the Ministry of Health,
Labor, and Welfare (MHLW) nominated
core and hub hospitals and provided
$60-65 million per year to equip them
with essential resources for taking care
of patients with cancer. The Ministry
of Education, Culture, Sports, Science,
and Technology (MEXT) began the
Gan(Cancer) Professional Educational
Plan to increase the number of medical
and radiation oncologists in the country. MEXT provides $20 million per year
to activate this plan and also mandated
that each university must establish an
oncology department. We hope that
this increased support will provide for
more positions for medical and radiation oncology in universities.
In addition to the action of the
government, the Japanese Society of
Medical Oncology (JSMO) began certifying specialists in medical oncology.
For that purpose, JSMO used the ASCO/
European Society of Medical Oncology (ESMO) core curriculum. Based on
this model, JSMO offered educational
seminars two or three times per year
for oncologists seeking this certification. Also, the Best of ASCO® meeting
in Japan has been organized as an
advanced course. After completing oral
and written examinations, the number of certified medical oncologists
increased to 306 at the end of April
2009. Although the pace of certification
is slow, the field of medical oncology has
steadily improved.
Another part of Japan’s recent cancerfighting law aims to provide full medical
care for patients with cancer living all
over Japan. It also recognizes the importance of palliative care for patients in the
late stages of disease. It is still difficult
to determine what kind of palliative care
is best for these patients. There are very
few quantitative and universally understandable methods of this kind of care.
In Japan, the government covers
the cost of medical care equally for all
patients. This is quite a different situation from other countries. As a result,
it is rather difficult to attract patients
for clinical trials. On the other hand,
patients need new drugs to continue
to improve cancer care for all. Government agencies, including the Cabinet
Office, MEXT, MHLW, and the Ministry
of Economy, Trade, and Industry (METI)
provided a Five-year Strategy for the
Development of Innovative Pharmaceuticals and Medical Devices in April
2009. The report stressed the importance of cooperation among industrial,
governmental, and academic groups. To
improve the infrastructure for clinical
research and to promote such endeavors, the government has nominated 10
core and 30 hub hospitals for clinical
trial promotion and offers $60 million
per year for funding. MEXT started the
Bridging Research Support Program
to facilitate translational research.
Seven universities have been nominated for this program. In addition, the
Pharmaceuticals and Medical Devices
Agency (PMDA) has been reformed and
consolidated. The number of reviewers
in PMDA has increased significantly. A
new guideline on methods for the clinical evaluation of oncology drugs was
activated on November 1, 2008. The
guideline is almost equivalent to those
of the U.S. Food and Drug Administration (FDA) and the European Medicines
Agency (EMEA). The Highly Advanced
Medical Technology Assessment system was introduced to facilitate use of
new drugs and treatment modalities.
A revised Japanese trial guideline for
clinical research was implemented in
April 2009. The guideline coincided
with global guidelines.
By these efforts, I am sure that cancer care in Japan will improve.
ASCO NEWS & FORUM |
49
NEWS
5HVHDUFK,VVXHV 5HVRXUFHV
Trial Explores Lung Cancer Biomarkers and
Demonstrates Improved Efficiency
By Laurence H. Baker, DO
Chair, Southwest Oncology Group
Laurence H. Baker, DO, is the Chair of the Southwest Oncology
Group (SWOG). Leading this cooperative group since 2005, Dr.
Baker is dedicated to clinical investigations of innovative treatments for cancer, but also to improving the efficiency and quality
of the clinical trial process. In the article that follows, he discusses an actively recruiting phase III trial (S0819) that not only
explores the efficacy of treatments for advanced non-small cell
lung cancer (NSCLC), but also showcases a new methodology for
making clinical investigation more efficient.
L
ung cancer takes a devastating toll in the United States.
Only 15% of patients with the disease survive five years
after their diagnosis. It is the most frequent cause of cancer death in the country, a fact that is largely due to the high
numbers of patients who present in the advanced stages of disease when effective therapies are limited. One emerging method
that holds promise for improving the grim toll of NSCLC is the
use of biomarkers to detect expression of increased copy number of the epidermal growth factor receptor (EGFR) gene, identified through fluorescent in situ hybridization (FISH).
EGFR FISH assays are a part of oncology’s advance into
Enrolling Patients in SWOG S0819
Title: A randomized, phase III study comparing carboplatin/paclitaxel or
carboplatin/paclitaxel/bevacizumab with or without concurrent cetuximab in
patients with advanced non-small cell lung cancer (NSCLC).
Endpoints: The primary endpoints of this trial are overall survival of the
entire study population and progression-free survival of patients who are
EGFR FISH-positive.
Inclusion Criteria: Entry criteria include, but are not limited to, the following:
Q Histologically or cytologically confirmed stage IV advanced primary NSCLC
Q No prior chemotherapy, cetuximab, gefitinib, erlotinib, or other investigational agents that target the EGFR pathway
Q Patients must have recovered from all associated toxicities of radiation
therapy at the time of registration
Q Zubrod Performance Status of 0-1
Contact Information:
Roy S. Herbst, MD, PhD, Study Coordinator
Phone: 713-792-6363
For more information on S0819, visit www.swog.org.
50 | OCTOBER 2009
smarter medicine. These biomarkers allow us to identify which
patients with NSCLC will benefit the most from a particular drug
regimen. Such identification helps eliminate the trial-and-error
aspect of chemotherapy and saves valuable time and resources
in the lives of these patients.
In this phase III trial, S0819, patients will begin chemotherapy
regimens with carboplatin and paclitaxel with or without bevacizumab, depending on their suitability for that drug. Patients
will be randomly assigned to continue that treatment alone or to
receive concurrent cetuximab. Although the primary endpoints
of the trial will examine the efficacy of these treatments, more
importantly, we are critically examining the value of EGFR FISH in
determining which patients will derive the greatest benefit from
these drugs.
S0819 also represents an important change for SWOG and the
general conduct of clinical trials. In 2006, a group led by David
Dilts, PhD, of Oregon Health and Science University, reported that
the average length of time for a phase III trial to move from initial
conception to activation in a cooperative group system was nearly
800 days (J Clin Oncol. 2006:24;4553-7.). This unfortunate number is frequently cited by critics of cooperative groups and cancer
centers. Although there has been much discussion of this study,
few efforts have been made to try to change the system. This trial
represents SWOG’s first attempt to start making such a change.
We developed a mechanism called SWAT (the Southwest
Oncology Group Action Team), a group composed of all of the
trial’s key players. Since the trial’s conception in October 2008,
all members of the SWAT team convened weekly for a conference call to discuss progress and to move the trial past any
unnecessary delays. This kind of vigilance and a little healthy
peer pressure made the team members work more efficiently
than they normally might have. As a result, the time required
from the conception of this trial to its date of accrual is approximately 270 days—nearly one-third of the original length observed
by Dr. Dilts. Now that we have evidence that the method works,
we plan to implement it in future SWOG trials.
For many reasons, we are very excited about this trial. Not only
will it test the potential of a chemotherapy regimen, but it will
shed light on the efficacy of a promising biomarker for patients
with NSCLC. It also represents a tremendous success in SWOG’s
development of new methods to conduct studies more efficiently. We hope this success will ultimately benefit our patients
in their fight against cancer.
NEWS
6SRWOLJKWRQ(GXFDWLRQ
Explore Latest Science at GI and GU Cancer Symposia
J
oin ASCO and its co-sponsoring societies at the 2010 Gastrointestinal
Cancers Symposium and the 2010
Genitourinary Cancers Symposium. Registration for both events is now open.
2010 Gastrointestinal
Cancers Symposium
January 22-24, 2010
World Center Marriott
Orlando, Florida
For the seventh year, experts in the field
of gastrointestinal (GI) malignancies will
convene to discuss the latest research
on cancers of the GI tract. The three-day
symposium will explore cutting-edge
science, educational forums, and discussions on each type of GI cancer, including:
Q Cancers of the esophagus and stomach
Q Cancers of the pancreas, small bowel,
and hepatobiliary tract
Q Cancers of the colon and rectum
The content offered in general sessions
will be augmented by oral and poster presentations throughout the symposium.
New this year, the symposium will feature a tumor board session on metastatic
endocrine tumors to the liver.
Attendees also can attend several tick-
eted sessions throughout the symposium,
including Meet the Professor sessions
and Translational Research Topic Forums.
Fellows, residents, and junior faculty can
interact with faculty and committee members at the Fellows Luncheon.
ASCO, the American Gastroenterological Association (AGA) Institute, the
American Society for Radiation Oncology (ASTRO), and the Society of Surgical
Oncology (SSO) are proud to again offer
a forum for cutting-edge research on GI
cancers.
For more information visit
www.gicasymposium.org.
2010 Genitourinary
Cancers Symposium
March 5-7, 2010
San Francisco Marriott
San Francisco, California
At the 2010 Genitourinary Cancers Symposium, attendees will learn about recent
advances in the multidisciplinary management of genitourinary tract malignancies,
including:
Q Prostate cancer
Q Cancers of the urothelium
Q Renal cell cancer
Q Rare tumors of the GU tract
Fellows and Junior Faculty: Many Reasons to Attend
At its thematic symposia, ASCO and its co-sponsoring organizations offer many
unique opportunities for fellows, residents, and junior faculty to make the most of
their experiences at these events.
Q The ASCO Cancer Foundation® grants Merit Awards to selected fellows and
junior faculty who submit abstracts to the GI, GU, and Breast Cancer Symposia.
Q At the GU Symposium, poster walks are open to fellows and junior faculty
exclusively and allow them to engage with experts about the latest science
presented at the meeting.
Q Fellows, Residents, and Junior Faculty Luncheons provide intimate settings for
young oncology professionals to meet faculty and leaders of their fields, as
well as a chance to network with colleagues and peers.
The three-day event will provide educational sessions and oral abstract and
poster presentations discussing the state
of progress against these diseases and
highlighting developments in prevention,
screening, and diagnosis; multidisciplinary
treatment; and translational research.
Several sessions at the symposium
offer attendees interaction with colleagues and explore the science.
Q The Best of Journals sessions offer a
dynamic review of published science
on prostate and renal cancers (ticketed
session).
Q The Tumor Board Discussion on Rare
Tumors of the GU Tract allows attendees to discuss the many aspects of
these diseases.
Q Poster walks give fellows and junior
faculty a chance to take part in discussions of GU cancer research with
faculty and presenters.
The 2010 Genitourinary Cancers
Symposium is sponsored by ASCO,
ASTRO, and the Society of Urologic
Oncology (SUO).
For more information visit
www.gucasymposium.org.
Mark Your Calendar
Q
Q
Q
Q
Late October 2009—Registration
and housing open for the 2010
GU Symposium
October 30, 2009—Abstract
submission deadline for the 2010
GU Symposium
Mid-December 2009—Early
registration ends for the 2010 GI
Symposium
January 2010—Early registration
ends for the 2010 GU Symposium
ASCO NEWS & FORUM |
51
NEWS
)RFXVRQ)HOORZV -XQLRU)DFXOW\
The First Year of
Faculty Appointment
By Colin D. Weekes, MD, PhD
Assistant Professor of Medicine
University of Colorado Denver
M
y first day as a junior faculty
member was filled with joy and
anxiety. I had attained my first
real job in my chosen field after completing 15 years of training. As I sat at my
desk looking out at Pike’s Peak in the
distance, I wondered if I would actually
be able to accomplish the goals I had set
for myself. Not only was I starting my first
academic position, but I also had moved
my family from the east coast to Colorado.
It was an exciting but apprehensive time.
However, I was fortunate to join a wellestablished team of investigators who
have facilitated my professional growth.
My career focus is on the application of
developmental therapeutics to gastrointestinal oncology with an emphasis in pancreatic cancer. As such, I have a translational
research lab, and I also attend a combined
developmental therapeutics and gastrointestinal oncology clinic once per week.
My clinical research focuses on phase I/II
clinical trials. The ultimate goal of my laboratory research is to develop molecularly
based strategies to be implemented into
early-phase clinical trials for pancreatic
cancer.
Given the complex nature of my career
goals, my program leader suggested that
I develop a timeline of milestones that I
should aim to reach in the first three years
of my faculty appointment. Part of her
52 | OCTOBER 2009
intent with this exercise was to help me
organize my laboratory endeavors compared with my clinical research efforts.
The other component was to ensure that
I would be in an appropriate position for
a promotion if I met my goals in a timely
manner. At first, I was a little overwhelmed
with the thought of working for a promotion within the first month of my new position. However, in hindsight, this was some
of the most beneficial time that I spent in
the first weeks of my appointment. I routinely refer to this template to make sure
that I am on track to achieve my long-term
career goals.
Time management has been a challenge
when balancing my responsibilities as a
clinical investigator and managing a laboratory. I am privileged to be part of a program that has an extensive, well-trained
clinical research support team that helps
me conduct clinical research efficiently.
However, even with this support team in
place, I find myself doing some clinically
related work on a daily basis. Establishing
daily, weekly, and monthly to-do lists helps
me stay focused and on target with the
completion of necessary tasks.
My role as a manager has been one of
the most difficult challenges that I have
faced during this transition. People-management skills are clearly not a part of the
standard medical school curriculum. I had
managed a group of interns as a senior
resident, but somehow this was different.
Creating a setting for folks with different
mindsets to come together for a common
goal is demanding. Balancing different
personalities and remaining on good terms
with everyone can be difficult at times. I
also have had the opportunity to hire and
fire people during this initial year. It was at
that moment that the initial timeline that
I created for myself became quite useful.
It enabled me to remove myself from the
emotional aspects of the situation and
focus on what was necessary to attain
my goals and ultimately support the livelihoods of those individuals working in my
lab. I also am thankful that I was able to
discuss these challenges with my program
manager, who assisted me in handling the
situation as amicably as possible. Prior to
this appointment, I had little experience in
a managerial role. It has been tricky finding a balance between directing the individuals in my lab and still giving them an
appropriate amount of autonomy. Providing
clear expectations and setting reasonable
goals while fostering individual thought is
paramount to developing a pleasurable
and productive laboratory environment.
Overall, I believe my transition from
fellowship to junior faculty has been successful. There were a few unforeseen
challenges to overcome, but I am looking
forward to seeing what the future holds.
I have experienced some unusual events
during the first year of my faculty appointment, but I feel that such experiences
are fairly standard. I have found that persistence, communication, a clear focus,
and laughter help me through the difficult
times.
NEWS
)RU<RXU3DWLHQWV
Help Your Patients
Learn About Managing
the Cost of Cancer Care
ASCO and
Cancer.Net Partner
with Kaleidoscope
Patient Information
from the 2009 Breast
Cancer Symposium
Do your patients have questions about
the cost of cancer care? Cancer.Net’s
Managing the Cost of Cancer Care booklet, developed by ASCO’s Cost of Care
Task Force Patient Resources Subcommittee, provides tools and resources that can
help your patients answer their questions
and plan for costs before, during, and
after treatment.
To order copies for your patients,
contact the ASCO Communications
and Patient Information Department at
888-651-3038, or send an e-mail to contactus@cancer.net. The booklet is also
available as a free, downloadable PDF at
www.cancer.net/managingcostofcare, and
in Spanish at www.cancer.net/spanish.
For the second year, ASCO is part of a
national campaign to raise awareness of
cancers that affect women. Kaleidoscope,
formerly known as Frosted Pink with a
Twist, is a televised music and figure
skating event and education campaign
hosted by cancer survivors Olivia Newton
John and Scott Hamilton. The event will
air nationwide on Fox on November 26
(Thanksgiving Day) from 4:30 PM–6:00
PM EST.
Cancer.Net is the official clinical cancer
information resource for Kaleidoscope,
making it an extraordinary opportunity
for ASCO and Cancer.Net to reach a large
audience. For more information, visit
www.cancer.net.
Help your patients learn about the
research highlighted at the 2009 Breast
Cancer Symposium, to be held October
8–10 in San Francisco, California, with
the special online newsletter, Cancer
Advances: News for Patients from the
2009 Breast Cancer Symposium.
In addition, Cancer.Net provides more
information about breast cancer research
and treatment in a question-and-answer
article that taps into the expertise of
ASCO’s membership. Your patients can
also listen online to a podcast of the
symposium highlights or download it free
of charge.
Direct your patients to www.cancer.net/
breastsymposium for these materials.
ASCO ANSWER S
PA N C R E AT I C C A N C E R
ASCO ANSWER S
Pancreatic cancer begins when cells in the pancreas grow
without control and form a tumor. The most common
type of pancreatic cancer, called ductal adenocarcinoma,
begins in the cells lining the pancreatic ducts. Because
pancreatic cancer often does not cause specific symptoms,
it may not be detected until the cancer has spread to other
areas of the body.
S TO M AC H C A N C E R
Stomach cancer, also called gastric cancer, can begin in
any part of the stomach. It may spread to nearby lymph
nodes and other areas of the body, such as the liver,
pancreas, colon, lungs, and a woman’s ovaries.
Most types of stomach cancer are adenocarcinoma. Other,
rare types of cancerous tumors that form in the stomach
include lymphoma, gastric sarcoma, and carcinoid tumor.
WHAT IS THE FUNCTION OF THE STOMACH?
WHAT IS THE FUNCTION OF THE PANCREAS?
The pancreas is a pear-shaped gland located in the
abdomen between the stomach and the spine that is
composed of two major components: exocrine and
endocrine. The exocrine component, made up of ducts
and acini (small sacs on the end of the ducts), produces
enzymes (specialized proteins) that help the body digest
and break down food. The endocrine component is
made up of cells clustered together, called the islets of
Langerhans, and produces hormones, the most critical one
being insulin, which helps control blood sugar.
WHAT DOES STAGE MEAN?
ASCO ANSWER S
E S O P H AG E A L C A N C E R
WHAT IS ESOPHAGEAL CANCER?
ASCO ANSWER S
Esophageal cancer begins when cells in the lining of
the esophagus grow uncontrollably and eventually form
a tumor. There are two types of esophageal cancer.
Squamous cell carcinoma develops in the upper and
middle part of the esophagus. Adenocarcinoma begins in
the glandular tissue in the lower part of the esophagus.
Rare cancers can also arise in neuroendocrine, muscle, or
lymphatic tissue.
N O N - H O D G K I N LY M P H O M A
Find additional cancer information at www.cancer.net.
WHAT IS NON-HODGKIN LYMPHOMA?
Non-Hodgkin lymphoma (NHL) is a disease of the
WHAT IS THE FUNCTION OF THE
ESOPHAGUS?
ASCO ANSWER S
The esophagus is a 10-inch long, hollow, muscular tube
that connects the throat to the stomach. When a person
swallows, the walls of the esophagus contract to push
food down into the stomach.
WHAT DOES STAGE MEAN?
Answers for
Your Patients
BL ADDER CANCER
Find additional cancer information at www.cancer.net.
The stage is a way of describing the cancer, such as where
it isIS
located,
if or where
it has spread, and if it is affecting the
WHAT
BLADDER
CANCER?
functions of other organs in the body. There are four stages for esophageal cancer: stages I through IV (one through four).
Bladder cancer begins when cells lining the bladder
Illustrations for these stages are available at www.cancer.net/esophageal.
grow uncontrollably and eventually form a tumor.
Illustration by Robert Morreale/Visual Explanations, LLC. © 2004 American Society of Clinical Oncology.
lymph
system,
in which
lymphatic
begin
to spread,
change,and if it is affecting the
The stage is a way of describing the cancer,
such
as where
it is located,
if orcells
where
it has
grow
uncontrollably,
and form
can becancer places the cancer into
functions of other organs in the body. The
most
common method
usedtumors.
to stage NHL
pancreatic
indolent
(slower
aggressive
(faster which
growing),
or
three categories: resectable, which can be
removed
usinggrowing),
surgery; locally
advanced,
is limited
to the area around the
have
of both
types.
pancreas; and metastatic, which has spread
tofeatures
other areas
of the
body.B-cell lymphoma is the most
common type of NHL; T-cell lymphoma is less common.
Find additional cancer information at www.cancer.net.
Because of the many types and subtypes of NHL, it is
important
to
know
the
diagnosis.
More
information
HOW IS PANCREATIC CANCER TREATED?
WHAT DOES STAGE MEAN?
about subtypes can be found at www.cancer.net/nhl.
The stage is a way of describing the cancer, such as where it is located, if or where it has spread, and if it is affecting theThe treatment of pancreatic cancer depends on the size and location of the tumor, whether the cancer has spread, and the
person’s overall health. There are three basic ways to treat pancreatic cancer: surgery, radiation therapy, and chemotherapy.
functions of other organs in the body. There are five stages for stomach cancer: stage 0 (zero) and stages I through IV (one
Surgery may involve removing all or part
of the pancreas,
depending on the
WHAT
IS THE FUNCTION
OFlocation
THE and size of the cancer. Radiation
through four).
therapy and/or chemotherapy may be used before surgery to reduce the size of a tumor, but they are used most often after
Illustration by Robert Morreale/Visual Explanations, LLC. © 2004 American Society of Clinical Oncology.
The stomach is located in the upper abdomen and plays a
central role in digesting food. When food is swallowed,
it runs down the esophagus, or throat, and enters the
stomach. The muscles in the stomach mix the food and
release gastric juices that help digest and break down the
food. The food then moves into the small intestine for
further digestion.
Illustration by Robert Morreale/Visual Explanations, LLC. © 2004 American Society of Clinical Oncology.
WHAT IS STOMACH CANCER?
Illustration by Robert Morreale/Visual Explanations, LLC. © 2004 American Society of Clinical Oncology.
Illustration by Robert Morreale/Visual Explanations, LLC. © 2004 American Society of Clinical Oncology.
WHAT IS PANCREATIC CANCER?
ASCO NEWS & FORUM |
53
NEWS
0HPEHUVKLS1RWHV
Experience the Value of Your ASCO Membership
Did you know?
ASCO is committed to helping you connect with colleagues and stay current
on important issues.
ASCO members have many ways to get
the latest news from the Society and the
field of oncology.
Q Discuss research presented at ASCO
meetings by joining the ASCO group on
LinkedIn.
Q Follow the latest oncology information
by using ASCO’s customized iGoogle
page.
Q Never miss an important ASCO deadline, such as members-only housing for
the Annual Meeting, by following ASCO
updates on Twitter.
Q Easily refer your patients to a colleague
by using the enhanced online Membership Directory.
Q Receive FDA news and off-label drug
alerts by e-mail.
Q Utilize new online Medicare coverage
tools like CAC (Contractor Advisory Committee) E-News.
Q Get the latest oncology updates from
Daily Cancer News and ASCO Express.
ASCO offers three easy ways to pay your
membership dues.
Q Automatic Dues Renewal: We keep your
credit card number secure and renew
your membership automatically each
year.
Q Discounted Multiple Year Dues: Lock
in at today’s dues rates and receive a
$75 discount by paying for three years
at one time.
Q Annual Renewals: Pay online at ASCO.
org or by phone, fax, or mail.
View all of your ASCO information on
your personalized ASCO.org page.
Q Upload your photo for the online Mem-
54 | OCTOBER 2009
www.asco.org/usernamereminder or
www.asco.org/passwordreminder.
ASCO on the Road
At the ASCO Booth, the Society provides
services to members while they are
attending oncology meetings around the
world. Members who visit the ASCO Booth
may update their professional information, make a dues payment, sign up for a
new dues payment option, and purchase
ASCO publications. Please visit us at the
following meetings:
Breast Cancer Symposium
October 8-10, 2009
San Francisco Marriott
San Francisco, California
Q
Q
Q
Q
bership Directory.
Update your contact information, including board certification and professional
activities.
See the ASCO meetings for which you
have registered and view other upcoming ASCO meetings.
View CME credits earned at ASCO
meetings.
Sign up for a new payment option or
pay your membership dues.
Our members’ security is important to us.
ASCO treats usernames and passwords
with the highest security and confidentiality. Member usernames and passwords
may not be communicated over the phone
or through unsolicited e-mail. If you forget your username or password, you can
request that your login information be
sent to the primary e-mail address that
ASCO has on record by visiting
American Society of Hematology
Annual Meeting
December 5-8, 2009
Ernest N. Morial Convention Center
New Orleans, Louisiana
Gastrointestinal Cancers Symposium
January 22-24, 2010
Orlando World Center Marriott
Orlando, Florida
In Memoriam
Heinrich Baust, MD
David J. Emanuel, MD
Chandra M. Jha, MD
William A. Knight III, MD
Barry J. Kobrin, PhD
Tetsuro Kubota, MD
Walter John Miller, MD
W. P. Laird Myers, MD
K_\8J:FCfXeI\gXpd\ekGif^iXd#
]le[\[YpJljXe>%Bfd\e]fik_\:li\
GXikf]k_\JljXe>%Bfd\e]fik_\:li\&8J:FHlXc`kpf]:Xi\@e`k`Xk`m\
<C@>@9@C@KP
KfhlXc`]pXggc`ZXekjdljkd\\kk_\]fccfn`e^
Zi`k\i`XXkk_\k`d\f]k_\XnXi[1
?Xm\Zfdgc\k\[XeXggifm\[feZfcf^p
]\ccfnj_`gkiX`e`e^gif^iXd`ek_\Le`k\[JkXk\j%
?Xm\flkjkXe[`e^hlXc`]p`e^cfXejfYkX`e\[]fi
d\[`ZXc\[lZXk`fec\X[`e^
kfX[\^i\\fi[`gcfdX`ed\[`Z`e\%
9\XL%J%Z`k`q\e#L%J%eXk`feXcfig\idXe\ek
i\j`[\ek%
K_\8J:F;`m\ij`kp`eFeZfcf^p@e`k`Xk`m\#]le[\[Yp
JljXe>%Bfd\e]fik_\:li\#`j[\j`^e\[kf`eZi\Xj\
[`m\ij`kp`ek_\feZfcf^pnfib]fiZ\Xe[XZZ\jjkf
hlXc`kpZXi\]file[\ij\im\[Zfddle`k`\j%
8nXi[KfkXc1lgkf.'#'''
lgkf*,#'''g\ip\Xi]fiknfp\Xij
8ggc`ZXk`feFg\ej1J\gk\dY\i(-#)''0
8ggc`ZXk`fe;l\1;\Z\dY\i(-#)''0
9\Xg_pj`Z`Xe_Xm\XeD;#;Ffi\hl`mXc\ek
d\[`ZXc[fZkfiXc[\^i\\
]ifdXeXZZi\[`k\[`ejk`klk`fe %
?Xm\XZlii\ekg\idXe\eklei\jki`Zk\[c`Z\ej\
XjXg_pj`Z`XekfgiXZk`Z\`ek_\[\j`^eXk\[
JkXk\%
9\YfXi[$Z\ik`Ô\[`eXefeZfcf^pjg\Z`Xckp`%\%
d\[&feZ#_\d&feZ#iX[&feZ %
:fdd`kkfgiXZk`Z`e^Zc`e`ZXcfeZfcf^p]lcc$k`d\
]fiknfp\Xij`eXd\[`ZXccple[\ij\im\[
Zfddle`kpf]k_\Le`k\[JkXk\jXjjg\Z`Ô\[Yp
k_\gif^iXdZi`k\i`X%
9\Xe8J:Fd\dY\ifiY\Zfd\Xe
8J:Fd\dY\i%
KfXggcp#^fkfnnn%XjZfZXeZ\i]fle[Xk`fe%fi^&CIG
:Xcc]fi
8YjkiXZkj
)'('>\e`kfli`eXip:XeZ\ijJpdgfj`ld
Gif^i\jj`eDlck`[`jZ`gc`eXipDXeX^\d\ek
DXiZ_,$.#)'('
JXe=iXeZ`jZfDXii`fkk
JXe=iXeZ`jZf#:Xc`]fie`X
nnn%^lZXjpdgfj`ld%fi^
8YjkiXZkJlYd`jj`fe;\X[c`e\1
FZkfY\i*'#)''0Xk((1,0GD<Xjk\ieK`d\
K_`jXZk`m`kp_XjY\\eXggifm\[]fi8D8GI8:Xk\^fip(:i\[`k%
TARG E T I NG
C A NC E R
C A RE
Every day, cancer treatment is becoming
a more accurate science. Which is why at
Yale-New Haven Hospital, you will be seen
by one of 12 teams of specialists. They are
among the country’s leading diagnosticians,
oncologists, surgeons and radiation
With all we know
about cancer today,
it takes a team to know
how to treat yours.
oncologists. They work collaboratively to
more accurately diagnose and treat your
specific type of cancer. That not only means
fewer appointments and less stress for you,
it also means less pain, fewer side effects
and a brighter outlook for your future. To
learn more, visit xxx/tnjmpxdbodfs/psh/
Yale-New Haven Hospital is the primary teaching hospital of Yale School of Medicine and is
ranked among the nation’s best hospitals by U.S.News & World Report. Smilow Cancer Hospital
at Yale-New Haven works in partnership with Yale Cancer Center – A National Cancer
Institute-designated Comprehensive Cancer Center.
Opening October 2009