Rehabilitation Guidelines for Type I and Type II Rotator
advertisement

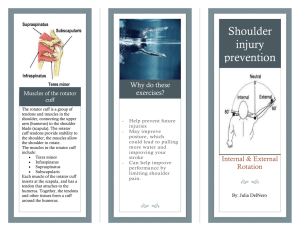
U W H e a lth S p o rts R e h a b i l it a ti o n Rehabilitation Guidelines for Type I and Type II Rotator Cuff Repair and Isolated Subscapularis Repair The anatomic configuration of the shoulder joint (glenohumeral joint) is often compared to that of a golf ball on a tee. This is because the articular surface of the round humeral head is approximately four times greater than that of the relatively flat shoulder blade face (glenoid fossa)1. This configuration provides less boney stability than a truer ball and socket joint, like the hip. The stability and movement of the shoulder is controlled primarily by the rotator cuff muscles, with assistance from the ligaments, glenoid labrum and capsule of the shoulder. The rotator cuff is a group of four muscles: subscapularis, supraspinatus, infraspinatus and teres minor (Figure 1). Rotator cuff tears can occur from repeated stress or from trauma. Throwing a baseball can create up to 750 newtons of distractive force on the shoulder2. This places a significant amount of stress on the rotator cuff while trying to dissipate this force. This stress and force may be even greater if there is improper form or mechanics while throwing. This repeated stress may lead to rotator cuff tears. Rotator cuff trauma also may result from falling on your arm, bracing your arm in an accident, arm tackling in football or any large sudden force applied to the arm. Most rotator cuff tears involve the supraspinatus and/ Back View Front View Supraspinatus Infraspinatus Teres Minor Subscapularis Figure 1Rotator cuff anatomy Image property of Primal Pictures, Ltd., primalpictures.com. Use of this image without authorization from Primal Pictures, Ltd. is prohibited. Bursal surface of the supraspinatus tendon Articular surface of the supraspinatus tendon Greater tuberosity Glenoid fossa Humeral head Figure 2. Coronal MRI Image of the Supraspinatus Note the black line of the bursal surface and articular surface. In this normal shoulder this tendon continues all the way to the greater tuberosity, the attachment site on the humerus. When there is a rotator cuff tear these black lines will become disrupted before reaching the greater tuberosity. or the infraspinatus. Occasionally isolated tears of the subscapularis can occur. This usually results from trauma rotating the shoulder outward. The rotator cuff tendons also undergo some degeneration with age. This process alone can lead to rotator cuff tears in older patients. Patients over The world-class health care team for the UW Badgers and proud sponsor of UW Athletics 6 2 1 S ci e n c e D ri v e • M a dis o n , W I 5 3 7 1 1 • u ws p o rtsm e dici n e . o rg Rehabilitation Guidelines for Rotator Cuff and Isolated Subscapularis Repair Figure 3Coronal MRI image of an articular surface tear of the supraspinatus. Note the top black line has maintained continuity but the undersurface black line is disrupted. Figure 4Coronal MRI image of a full thickness tear of the supraspinatus. Note the white fluid present where the dark tendon should be. 50 years of age are more susceptible to sustaining a significant rotator cuff tear from trauma3. 2 Rotator cuff tears can be classified in various ways. The first classification is a partial thickness or a full thickness tear. Normal tendon thickness is 9 to 12 mm. Partial thickness tears start on one surface of the tendon, but do not progress through the depth of the tendon. These can be bursal surface tears or articular sided tears . Figure 2 shows the normal anatomy of the bursal and articular side of the rotator cuff. Bursal surface tears occur on the outer surface of the tendon and may be caused by repetitive impingement. Articular sided tears (Figure 3) occur on the inner surface of the tendon, and are most often caused by internal impingement or tensile stresses related to overhead sports. Full thickness or complete tears (Figure 4) extend from one surface of the tendon all the way through to the other surface of the tendon. Full thickness tears are often caused by trauma, such as falling on the arm. Since a portion of the tendon is completely disrupted, there also will be some tendon retraction. Retraction is movement of the tendon away from its insertion point back toward the muscle.4 After determining the type of tear, a classification system is used to assess the size of the tear. Type I tears are tears less than 2 cm in width and Type II tears are greater than 2 cm. Surgical repair of a rotator cuff tear can be done arthroscopically or with a miniopen procedure. A 2007 review published in The Journal of Bone and Joint Surgery stated that equally successful outcomes can be attained from either technique5. The primary goal of a rotator cuff repair is to restore the normal anatomy by approximating the rotator cuff tendon back to its normal attachment site on the greater tuberosity of the humerus. This is done by passing sutures through the tendon and then tying the tendon down to suture anchors that have been placed in the humerus. Prior to bringing the tendon back to its insertion, the edges of the tear may need to be brought together, referred to as side-to-side repair or convergence (Figure 5). Not all rotator cuff tears are repairable. A tear may be un-repairable if the tear is too large, there is too much retraction, or the tissue quality is too poor. The degree of success for tears that are repaired is related to various factors, including tear size, the number of tendons involved, patient age, associated injuries and post operative rehabilitation6, 7. 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Rotator Cuff and Isolated Subscapularis Repair A B C Figure 5Rotator cuff repair technique using anchors and sutures. The tear (A) is approximated. Then suture anchors are placed on both sides of the tear (B and C). Finally the tendon is approximated back to the bone with various suture patterns to decrease focal stress. Rehabilitation is vital to regaining motion, strength and function of the shoulder after surgery. Initially patients will use a sling to protect the repair site and allow healing of the tendon back to the bone. During this time, passive motion exercises are started to prevent the shoulder from getting stiff and losing mobility. The rehabilitation program will gradually progress to more strengthening and control type exercises. The rehabilitation guidelines will vary depending on the size of the 3 tear and quality of the tendon. The rehabilitation guidelines for Type I and Type II tears of the supraspinatus or infraspinatus and isolated subscapularis tears are presented below in a criterion based progression. General time frames are given for reference to the average, but individual patients will progress at different rates depending on their age, associated injuries, pre-injury health status, rehabilitation compliance and injury severity. 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Type I Rotator Cuff Repair TYPE I TEARS PHASE I (Surgery to 2 weeks after surgery) Appointments • Rehabilitation appointments begin within 1 week of surgery Rehabilitation Goals • Reduce pain and swelling in the post-surgical shoulder • Maintain active range of motion of the elbow, wrist and neck • Protect healing of repaired tissues Precautions • Use sling continuously except while doing therapy • Relative rest to reduce inflammation Suggested Therapeutic Exercise • Elbow, wrist and neck active range of motion • Ball squeezes • Passive range of motion for shoulder flexion and abduction (between 0° and 50°) Cardiovascular Fitness • Walking and/or stationary bike with sling on • No treadmill • Avoid running and jumping due to the forces that can occur at landing Progression Criteria • 14 days after surgery PHASE II (begin after meeting Phase I criteria, usually 2 weeks after surgery) 4 Appointments • Rehabilitation appointments are 2 times per week Rehabilitation Goals • Controlled restoration of passive and active assistive range of motion • Activate shoulder and scapular stabilizers in a protected position of 0° to 30° of shoulder abduction • Correct postural dysfunctions Precautions • Continue use of the sling for the first 4 weeks • Wean out of the sling slowly based on the safety of the environment during weeks 5 and 6 • Discontinue use of the sling by the end of week 6 • No active abduction for the first 8 weeks in order to protect the repair Suggested Therapeutic Exercise • Passive and active assistive range of motion for the shoulder in all cardinal planes (shoulder abduction should be passive only) • Begin active range of motion for shoulder flexion and rotation at 4 weeks • Gentle shoulder mobilizations as needed • Isometric internal and external rotator cuff strengthening in non-provocative positions with the shoulder in 0° to 30° of abduction • Scapular strengthening with the arm in neutral • Cervical spine and scapular active range of motion • Postural exercises • Core strengthening 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Rehabilitation Guidelines Guidelines for Rotatorfor Cuff Type andI Rotator Isolated Cuff Subscapularis Repair Repair Cardiovascular Fitness • Walking and stationary bike • No treadmill or stairmaster • Avoid running and jumping until the athlete has full rotator cuff strength in a neutral position due to forces that can occur at landing Progression Criteria • The patient can progress to phase III when they have achieved full passive range of motion (equal to the uninvolved side) and normal (rated 5/5) strength for the shoulder internal rotators and external rotators at 0° of shoulder abduction • Usually 5 weeks after surgery PHASE III (begin after meeting Phase II criteria, usually 5-7 weeks after surgery) 5 Appointments • Rehabilitation appointments are 1 time per week Rehabilitation Goals • Full shoulder active range of motion in all planes • Normal (rated 5/5) strength for shoulder internal rotators and external rotators with the shoulder in 0° of abduction • Correct any postural dysfunction Precautions • No active shoulder abduction for the first 8 weeks after surgery • Dr. Orwin’s, Dr. Dunn’s and Dr. Baer’s patients should avoid external resistance (bands or weights) for shoulder abduction or supraspinatus strengthening for the first 9 to 10 weeks after surgery; Dr. Scerpella’s patients should avoid external resistance for 12 weeks. • Begin strengthening the supraspinatus very gradually by ensuring that the exercises are pain free and do not include long lever arms that will significantly change the torque throughout the motion Suggested Therapeutic Exercise • Shoulder internal rotation and external rotation with theraband or weights that begin at 0° of shoulder abduction - gradually increase shoulder abduction as strength improves • Open kinetic chain shoulder rhythmic stabilizations in supine at 90° of shoulder elevation (eg. stars or alphabet exercises) • Gentle closed kinetic chain shoulder and scapular stabilization drills • Proprioceptive neuromuscular facilitation patterns • Side lying shoulder flexion • Begin shoulder abduction in side lying (gravity eliminated) • Scapular strengthening • Active, active assistive, and passive range of motion at the shoulder as needed • Core strengthening • Begin trunk and hip mobility exercises 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Rehabilitation Guidelines Guidelines for Rotatorfor Cuff Type andI Rotator Isolated Cuff Subscapularis Repair Repair Cardiovascular Fitness • Walking and stationary bike • No treadmill, stairmaster or swimming • Avoid running and jumping until the athlete has full rotator cuff strength in a neutral position due to forces that can occur at landing Progression Criteria • Full shoulder active range of motion (equal to the uninvolved shoulder) and normal (rated 5/5) strength for shoulder internal rotators and external rotators at 30° of shoulder abduction PHASE IV (begin after meeting Phase III criteria, usually 12 weeks after surgery) 6 Appointments • Rehabilitation appointments are 1 time every 2 to 3 weeks Rehabilitation Goals • Normal (rated 5/5) rotator cuff strength and endurance at 90° of shoulder abduction and scaption • Advance proprioceptive and dynamic neuromuscular control retraining • Correct postural dysfunctions with work and sport specific tasks • Develop strength and control for movements required for work or sport Precautions • Post-rehabilitation soreness should alleviate within 12 hours of the activities Suggested Therapeutic Exercise • Multi-plane shoulder active range of motion with a gradual increase in the velocity of movement while making sure to assess scapular rhythm • Shoulder mobilizations as needed • Rotator cuff strengthening in 90° of shoulder abduction and overhead (beyond 90° of shoulder abduction) • Scapular strengthening and dynamic neuromuscular control in open kinetic chain and closed kinetic chain positions • Core and lower body strengthening • About 15 weeks after surgery, begin education in sport specific biomechanics with a very initial program for throwing that includes low velocity throws, focusing on movement control (air throws and light toss) Cardiovascular Fitness • Walking, stationary bike, and stairmaster • No treadmill or swimming • May begin light jogging and running if the patient has normal (rated 5/5) rotator cuff strength in neutral and normal shoulder active range of motion Progression Criteria • Full shoulder active range of motion in all planes and multi-plane movements • Normal (rated 5/5) strength at 90° of shoulder abduction • Negative impingement signs 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Rehabilitation Guidelines Guidelines for Rotatorfor Cuff Type andI Rotator Isolated Cuff Subscapularis Repair Repair PHASE V (begin after meeting Phase IV criteria, usually 16 to 17 weeks after surgery) 7 Appointments • Rehabilitation appointments are once every 2 to 3 weeks Rehabilitation Goals • Normal (rated 5/5) rotator cuff strength at 90° of shoulder abduction • Normal (rated 5/5) supraspinatus strength • Advance proprioceptive and dynamic neuromuscular control retraining • Correct postural dysfunctions with work and sport specific tasks • Develop strength and control for movements required for work or sport • Develop work capacity cardiovascular endurance for work and/or sport Precautions • Post-rehabilitation soreness should alleviate within 12 hours of the activities Suggested Therapeutic Exercise • Multi-plane shoulder active range of motion with a gradual increase in the velocity of movement while making sure to assess scapular rhythm • Shoulder mobilizations as needed • Rotator cuff strengthening in 90° of shoulder abduction as well as in provocative positions and work/sport specific positions, including eccentric strengthening, endurance and velocity specific exercises • Scapular strengthening and dynamic neuromuscular control in overhead positions and work/sport specific positions • Work and Sport specific strengthening • Core and lower body strengthening • Throwing program, swimming program or overhead racquet program as needed Cardiovascular Fitness • Design to use work or sport specific energy systems Progression Criteria • The patient may return to sport after receiving clearance from the orthopedic surgeon and the sports rehabilitation provider. Return to sport decisions are based on meeting the goals of this phase 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Type II Rotator Cuff Repair TYPE II TEARS PHASE I (Surgery to 2 weeks after surgery) Appointments • Rehabilitation appointments begin within 7 to 10 days after surgery Rehabilitation Goals • Reduce pain and swelling in the post-surgical shoulder • Maintain active range of motion of the elbow, wrist and neck • Protect healing of repaired tissues Precautions • Use sling continuously • Relative rest to reduce inflammation Suggested Therapeutic Exercise • Elbow, wrist and neck active range of motion • Ball squeezes • Passive shoulder range of motion between 0° and 50° for flexion and abduction Cardiovascular Fitness • Walking and stationary bike with sling on • Avoid running and jumping due to the forces that can occur at landing Progression Criteria • 14 days after surgery PHASE II (begin after meeting Phase I criteria, usually 2 weeks after surgery) 8 Appointments • Rehabilitation appointments are 2 times per week Rehabilitation Goals • Controlled restoration of shoulder passive range of motion • Activate shoulder and scapular stabilizers in a protected position of 0° to 30° of shoulder abduction • Correct postural dysfunctions Precautions • Dr. Baer and Dr.Orwin’s patients may begin to wean out of the sling slowly during weeks 5 and 6, Discontinue the use of the sling by the end of week 6. • Dr. Dunn and Dr. Scerpella’s patients must wear the sling for at least 6 weeks and begin weaning out of the sling in week 7. • No active shoulder motion in order to protect repaired tissues Suggested Therapeutic Exercise • Codman’s exercises • Shoulder passive range of motion in all cardinal planes using a cane, pulleys, and/or table slides • Scapular squeezes • Cervical spine and scapular active range of motion • Postural exercises • Core strengthening Cardiovascular Fitness • Walking, stationary bike with sling on • No Treadmill Progression Criteria • The patient can progress to Phase III when they are at least 5 weeks after surgery 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Rehabilitation GuidelinesGuidelines for Rotatorfor Cuff Type andII Isolated Rotator Cuff Subscapularis Repair Repair PHASE III (begin after meeting Phase II criteria, usually 5-6 weeks after surgery) 9 Appointments • Rehabilitation appointments are 2 times per week Rehabilitation Goals • Full shoulder passive and active range of motion in all planes • Normal (rated 5/5) strength for shoulder internal rotators and external rotators at 30° of shoulder abduction • Correct postural dysfunction Precautions • No active abduction for the first 8 weeks after surgery • Dr. Baer and Dr. Orwin’s patients should avoid external resistance (bands or weights) for shoulder abduction or supraspinatus strengthening for the first 10 weeks; Dr. Scerpella’s and Dr. Dunn’s patients should avoid external resistance for 12 weeks • Begin strengthening the supraspinatus very gradually by ensuring that the exercises are pain free and do not include long lever arms that will significantly change the torque throughout the motion Suggested Therapeutic Exercise • Shoulder internal rotation and external rotation isometrics, gradually progressing to isotonics with exercise bands or weights that begin at 30° of shoulder abduction as strength improves • Open kinetic chain shoulder rhythmic stabilizations in supine at 90° of shoulder elevation (eg. stars or alphabet exercises) • Gentle closed kinetic chain shoulder and scapular stabilization drills • Short arc proprioceptive neuromuscular facilitation patterns • Side lying shoulder flexion • Scapular strengthening • Shoulder active/active assistive/passive range of motion exercises as needed • Begin core strengthening • Begin trunk and hip mobility exercises Cardiovascular Fitness • Walking and stationary bike • No treadmill, swimming or running Progression Criteria • The patient can progress to phase IV when they have achieved full shoulder active range of motion (equal to the uninvolved side) and normal (rated 5/5) strength for the shoulder internal rotators and external rotators at 30° of shoulder abduction 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Rehabilitation GuidelinesGuidelines for Rotatorfor Cuff Type andII Isolated Rotator Cuff Subscapularis Repair Repair PHASE IV (begin after meeting Phase III criteria, usually 12 to 14 weeks after surgery) Appointments • Rehabilitation appointments are once every 1 to 2 weeks Rehabilitation Goals • Normal (rated 5/5) rotator cuff strength and endurance at 90° of shoulder abduction and scaption • Advance proprioceptive and dynamic neuromuscular control retraining • Correct postural dysfunctions with work and sport specific tasks • Develop strength and control for movements required for work or sport Precautions • Post-rehabilitation soreness should alleviate within 12 hours of the activities Suggested Therapeutic Exercise • Multi-plane shoulder active range of motion with gradual increase in the velocity of movement being sure to assess scapular rhythm • Shoulder mobilizations as needed • Rotator cuff strengthening in 90° of shoulder abduction, and overhead (beyond 90° of shoulder abduction) • Scapular strengthening and dynamic neuromuscular control in open kinetic chain and closed kinetic chain positions • Core and lower body strengthening Cardiovascular Fitness • Walking, stationary bike, and stairmaster • No treadmill or swimming • The patient may begin running if they have normal (rated 5/5) strength for the shoulder internal rotators and external rotators at 30° of shoulder abduction and normal shoulder active range of motion Progression Criteria • Full shoulder active range of motion in all planes and multi-plane movements • Normal (rated 5/5) strength at 90° of shoulder abduction • Negative impingement signs 10 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Type II Rotator Cuff Repair PHASE V (begin after meeting Phase IV criteria, usually 20 to 22 weeks after surgery) Appointments • Rehabilitation appointments are 1 time every 2 to 3 weeks Rehabilitation Goals • Normal (rated 5/5) rotator cuff strength at 90° abduction • Normal (rated 5/5) supraspinatus strength • Advance proprioceptive and dynamic neuromuscular control retraining • Correct postural dysfunctions with work and sport specific tasks • Develop strength and control for movements required for work or sport • Develop work capacity cardiovascular endurance for work and/or sport Precautions • Post-rehabilitation soreness should alleviate within 12 hours of the activities Suggested Therapeutic Exercise • Multi-plane shoulder active range of motion with a gradual increase in the velocity of movement being sure to assess scapular rhythm • Shoulder mobilizations as needed • Rotator cuff strengthening in 90° of shoulder abduction in provocative and/or work/sport specific positions, including eccentric strengthening, endurance and velocity specific exercises • Scapular strengthening and dynamic neuromuscular control in overhead positions and work/sport specific positions • Work and sport specific strengthening • Core and lower body strengthening • Begin education in sport specific biomechanics with an initial program for throwing, swimming or overhead racquet sports as needed • Transition to a specific throwing program or swimming program once the patient can demonstrate good control with the desired mechanics Cardiovascular Fitness • Use exercise to replicate energy systems needed for work or sport Progression Criteria • The patient may return to sport after receiving clearance from the orthopedic surgeon and the sports rehabilitation provider. Return to sport decisions are based on meeting the goals of this phase 11 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Isolated Subscapularis Repair Rehabilitation Guidelines for Isolated Subscapularis Repair PHASE I (Surgery to 2 weeks after surgery) Appointments • Rehabilitation appointments begin 7-10 days after surgery Rehabilitation Goals • Reduce pain and swelling in the post-surgical shoulder • Maintain active range of motion (AROM) of elbow, wrist and neck • Protect healing of repaired tissues Precautions • Use sling continuously except while doing therapy • Relative rest to reduce inflammation Suggested Therapeutic Exercise • Elbow, wrist and neck AROM • Ball squeezes • Completely passive range of motion (PROM) for flexion and abduction (0° - 50°) Cardiovascular Fitness • Walking, stationary bike with sling on. No Treadmill, Stairmaster or swimming • Avoid running and jumping due to the forces that can occur at landing Progression Criteria • 14 days after surgery PHASE II (begin after meeting Phase I criteria, usually 2 weeks after surgery) Appointments • Rehabilitation appointments are 1 to 2 times per week Rehabilitation Goals • Controlled restoration of PROM and/or AAROM • Correct postural dysfunctions Precautions • Continue use of sling for sleep and activities during the first 6 weeks, weaning out of the sling slowly based on the safety of the environment after 6 weeks • No external rotation motion beyond neutral for the first 6 weeks (protect repair) • No resisted internal rotation for the first 6 weeks (protect repair) Suggested Therapeutic Exercise • PROM and/or AAROM for the shoulder as tolerated for flexion and abduction • Gentle shoulder mobilizations as needed • Isometric rotator cuff strengthening in non-provocative positions. No internal rotator or subscapularis strengthening • Scapular strengthening with arm in neutral • Cervical spine and scapular AROM • Postural exercises • Core strengthening 12 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Isolated Subscapularis Repair Cardiovascular Fitness • Walking and stationary bike. No Treadmill, Stairmaster or swimming • Avoid running and jumping until athlete has full rotator cuff strength in a neutral position due to forces that can occur at landing Progression Criteria • 6 weeks after surgery PHASE III (begin after meeting Phase II criteria, usually 6 weeks after surgery) Appointments • Rehabilitation appointments are1 time every 1 to 2 weeks Rehabilitation Goals • Full AROM in all planes • Normal (rated 5/5) strength for internal rotation (IR)/external rotation (ER) at 0° abduction • Correct postural dysfunction Precautions • Begin external rotation range of motion past neutral and resisted internal rotation gradually to assess response and allow for progress adaptation Suggested Therapeutic Exercise • IR/ER isotonics with theraband or weights that begin at 0° abduction and gradually increases abduction as strength improves • Open kinetic chain (OKC) shoulder rhythmic stabilizations in supine at 90° elevation (stars or alphabet) • Gentle closed kinetic chain (CKC) shoulder and scapular stabilization drills • Proprioceptive neuromuscular facilitation(PNF) patterns • Side lying shoulder flexion • Scapular strengthening • AROM, AAROM and/or PROM as needed • Core strengthening • Begin trunk and hip mobility exercises Cardiovascular Fitness • Walking and stationary bike. No Treadmill, Stairmaster or swimming • Avoid running and jumping until athlete has full rotator cuff strength in a neutral position due to forces that can occur at landing 13 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Guidelines for Isolated Subscapularis Repair Progression Criteria • Full AROM (equal to uninvolved) and normal (rated 5/5) strength for IR/ER at 30° abduction PHASE IV (begin after meeting Phase III criteria, usually 12 to 14 weeks after surgery) Appointments • Rehabilitation appointments are 1 time every 2 to 3 weeks Rehabilitation Goals • Normal (rated 5/5) rotator cuff strength and endurance at 90° abduction and scaption • Advance proprioceptive and dynamic neuromuscular control retraining • Correct postural dysfunctions with work and sport specific tasks • Develop strength and control for movements required for work or sport Precautions • Post-rehab soreness should alleviate within 12 hours of the activities Suggested Therapeutic Exercise • Multi-plane AROM with gradual increase in velocity of movement - assessing scapular rhythm • Shoulder mobilizations as needed • Rotator cuff strengthening in at 90° abduction, and overhead • Scapular strengthening and dynamic neuromuscular control in OKC and CKC positions • Core and lower body strengthening • At about 16-18 weeks, begin education in sport specific biomechanics with initial program for throwing – low velocity, focusing on movement control (air throws and light toss) Cardiovascular Fitness • Walking, stationary bike, Stairmaster. No Treadmill or swimming • May begin light jogging and running if patient has full rotator cuff strength in neutral and normal AROM Progression Criteria • Full AROM in all planes and multi-plane movements • Normal (rated 5/5) strength at 90° abduction • Negative impingement signs PHASE V (begin after meeting phase IV criteria, usually 16 to18 weeks after surgery) Appointments • Rehabilitation appointments are 1 time per week every 2 to 3 weeks Rehabilitation Goals • Normal (rated 5/5) rotator cuff strength at 90° abduction and supraspinatus • Advance proprioceptive and dynamic neuromuscular control retraining • Correct postural dysfunctions with work and sport specific tasks • Develop strength and control for movements required for work or sport • Develop work capacity cardiovascular endurance for work and/or sport Precautions • Post-rehab soreness should alleviate within 12 hours of the activities 14 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g Rehabilitation Rehabilitation Guidelines Guidelines for Rotator for Cuff Isolated and Isolated Subscapularis Subscapularis Repair Repair Suggested Therapeutic Exercise • Multi-plane AROM with gradual increase in velocity of movement - assessing scapular rhythm • Shoulder mobilizations as needed • Rotator cuff strengthening in at 90° abduction, provocative positions and work/ sport specific positions - including eccentric strengthening, endurance and velocity specific exercises • Scapular strengthening and dynamic neuromuscular control in overhead positions and work/sport specific positions • Work and Sport specific strengthening • Core and lower body strengthening • Throwing program, swimming program or overhead racquet program as needed Cardiovascular Fitness • Design to use work or sport specific energy systems Progression Criteria • The patient may return to sport after receiving clearance from the orthopedic surgeon and the sports rehabilitation provider. This will be based on meeting the goals of this phase These rehabilitation guidelines were developed collaboratively by Marc Sherry, PT, DPT, LAT, CSCS (msherry@uwhealth.org) and the UW Health Sports Medicine physician group. Updated 12/2013 References 1.Wilk KE, Reinold MM, Dugas JR, Arrigo CA, Moser MW, Andrews JR. Current concepts in the recognition and treatment of superior labral (SLAP) lesions. J Orthop Sports Phys Ther. May 2005;35(5):273291. 2.Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The “dead arm” revisited. Clin Sports Med. Jan 2000;19(1):125-158. 3.Wolf BR, Dunn WR, Wright RW. Indications for repair of full-thickness rotator cuff tears. Am J Sports Med. Jun 2007;35(6):1007-1016. 4.Kuhn JE, Dunn WR, Ma B, et al. Interobserver agreement in the classification of rotator cuff tears. Am J Sports Med. Mar 2007;35(3):437-441. 7.Boes MT, McCann PD, Dines DM. Diagnosis and management of massive rotator cuff tears: the surgeon’s dilemma. Instr Course Lect. 2006;55:45-57. 5.Nho SJ, Shindle MK, Sherman SL, Freedman KB, Lyman S, MacGillivray JD. Systematic review of arthroscopic rotator cuff repair and mini-open rotator cuff repair. J Bone Joint Surg Am. Oct 2007;89 Suppl 3:127-136. 6.Abrams JS. Arthroscopic approach to massive rotator cuff tears. Instr Course Lect. 2006;55:59-66. Copyright 2013 UW Health Sports Medicine Center 15 6 2 1 S c i e n c e D r i v e • M a d i s o n , W I 5 3 7 1 1 • u ws p o r t sm e d i c i n e . o r g SM-38183-13 At UW Health, patients may have advanced diagnostic and /or treatment options, or may receive educational materials that vary from this information. Please be aware that this information is not intended to replace the care or advice given by your physician or health care provider. It is neither intended nor implied to be a substitute for professional advice. Call your health provider immediately if you think you may have a medical emergency. Always seek the advice of your physician or other qualified health provider prior to starting any new treatment or with any question you may have regarding a medical condition.