2052
Intracoronary Urokinase for Intracoronary
Thrombus Accumulation Complicating
Percutaneous Transluminal Coronary
Angioplasty in Acute Ischemic Syndromes*
Gregory Schieman, MD, Barry M. Cohen, MD, Joseph Kozina, MD,
Joel S. Erickson, MD, Richard A. Podolin, MD, Kirk L. Peterson, MD,
John Ross Jr., MD, and Maurice Buchbinder, MD
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Intracoronary urokinase was used to treat flow-limiting intracoronary thrombus accumulation that
complicated successful percutaneous transluminal coronary angioplasty (PTCA) during acute
ischemic syndromes in 48 patients who were followed up through the acute phase of their illness.
The study group comprised 10 patients with unstable angina pectoris, 18 patients with an evolving
acute myocardial infarction, and 20 patients with postinfarction angina. The initial mean percent
coronary diameter stenosis for the entire population was 95+7% and decreased with initial PTCA
to 41+20%o (p<0.001), with improved corresponding coronary flow by Thrombolysis in Myocardial
Infarction trial (TIMI) grade. However, thrombus accumulation then resulted in a significant
increase in percent diameter stenosis to 83±17% (p<0.001); a corresponding significant reduction
in coronary flow also occurred by TIMI grade. After administration of intracoronary urokinase
(mean dose, 141,000 units; range, 100,000-250,000 units during an average period of 34 minutes),
with additional PTCA, mean percent diameter stenosis significantly decreased to 34±17%
(p<O.OOl); a correspondingly significant improvement in mean coronary flow by TIMI grade
occurred to 2.9±0.2. Overall, the angiographic success rate was 90%o. There were no ischemic events
requiring repeat PTCA and no procedure-related myocardial infarctions or deaths before hospital
discharge. One patient was referred for urgent coronary artery bypass graft surgery after a
successful PTCA. Plasma fibrinogen levels were obtained in 15 patients, and in no patient was the
level below normal for our laboratory. Angiographic follow-up was obtained in 79Y% of patients
(average time 30 days with 63% of all patients studied before discharge), and in no patient was there
angiographic evidence of reocclusion, although two patients showed angiographic evidence of
stenosis; improved vessel percent stenosis persisted, averaging 32±17%. In all patients studied, the
coronary flow was TIMI grade 3 at follow-up. Thus, in patients with acute ischemic syndromes with
flow-limiting intracoronary thrombus accumulation that complicated PTCA, intracoronary urokinase with repeated PTCA proved to be highly effective in restoring vessel patency and avoiding early
complications. (Circulation 1990;82:2052-2060)
T he acute ischemic syndromes of unstable angina pectoris, acute myocardial infarction,
and postinfarction angina often share a common pathogenesis, with atherosclerotic plaque rup*All editorial decisions for this article, including selection of
reviewers and the final decision, were made by a guest editor. This
procedure applies to all manuscripts with authors from the University of California San Diego or UCSD Medical Center.
From the Division of Cardiology, Department of Medicine,
University of California San Diego Medical Center.
Address for correspondence: Maurice Buchbinder, MD, UCSD
Medical Center, H-811A, 225 Dickinson Street, San Diego, CA
92103.
Received February 16, 1990; revision accepted August 7, 1990.
ture leading to platelet aggregation, activation of the
coagulation cascade, and formation of thrombus.1-6
Whether or not the thrombus becomes occlusive, the
duration of the occlusion and the extent of collateral
development determine whether or not myocardial
infarction develops and to what extent. Interventions
aimed at interrupting this sequence and salvaging
myocardium include thrombolytic therapy, percutaneous transluminal coronary angioplasty (PTCA),
and coronary artery bypass graft surgery (CABG).
Because the incidence of early acute myocardial
infarction and sudden cardiac death is relatively high
in patients with unstable angina pectoris,7-9 PTCA is
Schieman et al Intracoronary Urokinase With Repeated PTCA
2053
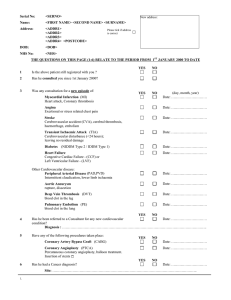
TABLE 1. Patient Characteristics
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Entire
Postinfarction
Evolving
Unstable
group
MI
angina
angina
Patients
248
86
35
126
Total (n)
With thrombus accumulation
48
20
10
18
(n)
19
23
51
8
Incidence (%)
77
74
89
70
Men (%)
Age (yr)
53
55
52
50
Mean
38-76
38-76
38-73
38-72
Range
13
0
17
30
Remote Q-wave MI (%)
11
15
28
0
Prior CABG/PTCA (%)
44
37
50
50
Currently smoking (%)
Pretreatment medication (%)
60
63
45
90
Aspirin
63
70
67
58
Heparin
46
0
42
78
Systemic lytic therapy
MI, myocardial infarction; CABG, coronary artery bypass graft surgery; PTCA, percutaneous transluminal coronary
angioplasty.
sometimes used in this setting for patients who have
failed to stabilize on medical therapy. The primary
success rate is similar to that after PTCA in patients
with stable angina, but the major complication rate is
higher in unstable patients, often because of the
development of abrupt thrombotic occlusion resulting in acute myocardial infarction or emergency
CABG.10-12
Direct PTCA has been used to treat acute myocardial infarction and has had high initial success rates,
but the incidence of abrupt thrombotic occlusion
during the procedure, or shortly afterward, is higher
than that for elective PTCA.13,14 When PTCA has
been used acutely to reduce the residual stenosis in
patients who initially received systemic thrombolytic
therapy, the complication rates of performing emergency CABG and of death also have been increased,
and the incidence of reocclusion in successfully dilated arteries has been 11-12.5%.15-17
Patients with early postinfarction ischemia are
known to be at high risk for reinfarction and death,'8,19
and PTCA has been used in this setting with high early
success rates. However, an increased incidence of
major procedure-related complications including
thrombotic coronary occlusion has been reported.20-22
These findings indicate that when PTCA is performed in patients with unstable angina pectoris,
early after acute myocardial infarction or during
postinfarction ischemia, high complication rates may
result from balloon-induced trauma to a highly
thrombogenic site, leading to intractable occlusive
thrombus. Because of these problems with the use of
PTCA in acute ischemic syndromes, this study was
designed to investigate the efficacy of intracoronary
thrombolysis with urokinase in conjunction with repeated PTCA for the treatment of flow-limiting
thrombus accumulation that complicates PTCA in
these settings. Urokinase was selected because it has
produced coronary reperfusion rates equivalent to
those produced by streptokinase in patients with
acute myocardial infarction when delivered by the
intracoronary route and has resulted in significantly
fewer bleeding complications and less systemic fibrinolysis.23 Moreover, it has a longer half-life than
recombinant tissue-type plasminogen activator, and
some patients had already received that agent.
Methods
Study Patients
Between July 1986 and October 1988, PTCA was
attempted in 248 consecutive patients with acute
ischemic syndromes (Table 1). For the purposes of
this study, acute ischemic syndromes included unstable angina pectoris, recurrent chest pain during the
evolving phase of an acute myocardial infarction, and
postinfarction angina. Of these 248 patients, 48 developed flow-limiting thrombus accumulation according to angiographic criteria (see below), and these 48
made up the study group.
Unstable angina pectoris was defined as the occurrence of ischemic pain at rest that lasted for at least
20 minutes and was associated with ST and T wave
changes, without evidence of myocardial necrosis
identified either by elevation of the total serum
creatine kinase to twice the normal value with greater
than 5% MB isoenzyme fraction or by the development of new pathological Q waves on the electrocardiogram. Angina pectoris during evolving acute myocardial infarction was defined as recurrent or
persistent symptoms of chest pain occurring within 72
hours of Q wave myocardial infarction, and this
definition applied to patients who had previously
received systemic thrombolytic therapy. Postinfarction angina was defined as the occurrence of angina
pectoris at rest with associated ST and T wave
2054
Circulation Vol 82, No 6, December 1990
changes occurring more than 72 hours after documented acute myocardial infarction but without evidence for additional myocardial necrosis (defined as
a second peak in creatinine kinase levels during a
documented decline, a lag or prolongation of the
return of the creatinine kinase to baseline or as the
development of new pathological Q waves).
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Management Before PTCA
All patients were intensively treated initially with
various combinations of /3-blockers, calcium channel
blockers, nitrates, aspirin, intravenous heparin, and
systemic thrombolytic agents. Patients who failed to
stabilize on an intensive medical regimen were referred for coronary angiography. Patients were selected for PTCA if the ischemia-related artery was
suitable for dilation. The stenotic artery was considered to be ischemia related in patients with singlevessel disease; in patients with multivessel disease,
the ischemia-related artery was defined by correlation with documented ST and T wave changes on the
electrocardiogram at rest.
PTCA Procedure
All PTCA procedures were performed by one of
three principal operators (M.B., K.L.P., or R.A.P.),
predominantly using the femoral approach. The procedure was performed with preformed guiding catheters, steerable dilating balloon catheters (usually
coaxial in design), and a pneumatic inflation device.
Ten thousand units of heparin were administered
intravenously after arterial cannulation followed by
an additional 1,000-1,500 units/hr in divided doses.
This dosage was chosen empirically because activated
clotting time measurements were not performed in
the catheterization laboratory at the time the study
was conducted. Preliminary angiography of the coronary artery was performed in at least two orthogonal projections. The balloon was positioned across
the stenosis, and sequential dilations were then performed with balloons of increasing size, and a final
balloon size was chosen that had an inflated diameter
approximately equal to the apparently disease-free
proximal lumen of the ischemia-related artery. As
many inflations as necessary were performed to produce acceptable angiographic results. Only the ischemia-related artery was dilated. All treated lesions
were observed by serial angiography in at least two
projections for a minimum period of 10 minutes after
the last dilation. Successful angioplasty was defined
as a reduction in the initial percent diameter stenosis
by at least 30%, with a final residual diameter
narrowing of 50% or less at the time of the patient's
departure from the cardiac catheterization laboratory. Cardiothoracic surgery and anesthesiology
teams were available during each dilation procedure.
Entry Criteria
The entry criteria for the study included an initially
successful PTCA of the ischemia-related artery, followed by angiographic documentation of flow-lim-
iting intracoronary thrombus accumulation. Flowlimiting intracoronary thrombus accumulation was
defined as angiographic evidence of at least a twofold
increase in the minimal percent diameter stenosis
obtained after PTCA, obliteration of the coronary
artery lumen at the site of a previously successful
angioplasty, or progressive reduction of antegrade
coronary flow to grade 0-1 as classified in the Thrombolysis in Myocardial Infarction (TIMI) study.24 Patients with evidence of coronary artery spasm or
occlusive subintimal dissection were excluded (see
definitions below).
Treatment of Intracoronary Thrombus Accumulation
Patients who met the inclusion criteria received a
mean dose of 141,000 (range, 100,000-250,000) units
of intracoronary urokinase (Abbokinase; Abbott
Pharmaceuticals, North Chicago, Ill.) through the
guiding catheter during a mean period of 34 minutes.
Redilation was performed intermittently during the
urokinase infusion in all patients as deemed necessary by the operator to maintain coronary flow at
TIMI grade 2-3. Coronary angiograms of the involved vessel were repeated at 3-5-minute intervals
to assess patency. Intracoronary nitroglycerin was
administered in all patients to reduce the possibility
of coronary spasm. A minimum of 20 minutes of
angiographic observation in at least two projections
was performed on each patient meeting the above
inclusion criteria to ensure continued vessel patency
before the patient's departure from the catheterization laboratory.
Postprocedure Therapies
After successful recanalization, the femoral
sheaths were secured in place for overnight monitoring in the coronary care unit. Full anticoagulation
with heparin to achieve a partial thromboplastin time
2.5-3 times control was continued for 5 days after the
procedure unless a contraindication was present. All
patients received 80 mg aspirin twice daily during the
heparin infusion, and 325 mg aspirin twice daily after
discontinuation of heparin. Intravenous nitroglycerin
was continued for 24 hours after the procedure and
was discontinued after removal of the femoral
sheaths. All patients were asked to submit to follow-up limited coronary angiography before hospital
discharge, and patient refusal was the only reason for
lack of follow-up angiography. Patients studied after
discharge underwent follow-up angiography.
Complications
A procedure-related myocardial infarction was
diagnosed either by elevation of the total serum
creatine kinase to twice the normal value with
greater than 5% MB isoenzyme fraction or by the
development of new pathological Q waves on the
electrocardiogram. Infarct extension was diagnosed
when a second peak in the creatine kinase level
occurred during a documented decline or when new
pathological Q waves developed on the electrocar-
Schieman et al Intracoronary Urokinase With Repeated PTCA
diogram. Ischemic events in the hospital requiring
angiography and the number of patients requiring
transfusion were tabulated.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Definitions and Data Analysis
The coronary angiograms of all patients who developed acute progressive vessel reclosure after a
seemingly successful PTCA were reviewed in a
blinded fashion by two observers who independently
evaluated the stenosis site, its degree, and its morphology. Conclusions were reached by consensus.
Assessments were made before and after the initial
dilation, during reclosure, and after successful recanalization with urokinase. The evaluation was confined solely to the lesion that developed progressive
reclosure after PTCA and did not include lesions at
other sites in the same or other vessels. When more
than one lesion was present in an ischemia-related
vessel, only the lesion that developed flow-limiting
thrombus accumulation was assessed.
An intimal tear or dissection was considered to be
present after PTCA when there was a curvilinear or
linear intraluminal filling defect or vessel widening
with extraluminal contrast staining at the site of
dilation. Coronary artery spasm was defined as a
transient decrease in vessel diameter that could be
reversed by administration of intravenous, sublingual,
or intracoronary nitroglycerin. The presence of intracoronary thrombus was defined as a clearly localized
filling defect surrounded by contrast medium at the
site of a high-grade stenosis or as luminal staining at
the site of a high-grade stenosis or occlusion. Complete occlusion was defined as 100% coronary stenosis
according to angiography with TIMI grade 0 or 1 flow.
A peri-interventional myocardial infarction was diagnosed when new pathological Q waves developed or
when an abnormal cardiac enzyme elevation was
documented (see above definitions).
Statistical Analyses
Repeated measures analysis of variance was used
to assess the significance of sequential changes in
percent diameter stenosis and TIMI grade over time.
After obtaining an overall significant time effect,
multiple comparisons were made by Tukey's test.
Follow-up data were not included in the analysis of
variance because they were incomplete. Standard
deviations or ranges are presented for the mean
values in the tables and figures.
Results
Of the 248 patients undergoing PTCA for acute
ischemic syndromes during the period of study, 126
(51%) had unstable angina, 35 (14%) were being
treated for evolving myocardial infarction, and 86
(35%) had recurrent angina more than 72 hours after
acute myocardial infarction (Table 1).
Forty-eight of the 248 patients (19%) with ischemic syndromes underwent an initially successful
PTCA but developed flow-limiting intracoronary
thrombus accumulation in the dilated vessel and are
2055
the subject of this report. Of the 48 patients, 10
(21%) were in the unstable angina group, 18 (37%)
were being treated for evolving myocardial infarction, and 20 (43%) were in the postinfarction angina
group (Table 1). There was a significantly higher
incidence of flow-limiting thrombus accumulation in
the evolving myocardial infarction group than in
either the unstable angina or postinfarction angina
groups (p<0.001 and p<0.005, respectively, by x2
analysis). In the total group, 13 (27%) had complete
coronary occlusion.
In the entire group, the mean age of the patients
was 53 years (range, 38-76 years) (Table 1). Seventyseven percent of the patients were men, 13% had a
history of previous myocardial infarction, and 44%
were smokers at the time of hospital admission.
Among the patients in the evolving myocardial infarction group, 78% had received prior fibrinolytic
therapy with either recombinant tissue-type plasminogen activator or streptokinase (Table 1). Table 1
also shows these data for the treated patients with
each of the three types of ischemic syndromes.
Baseline Angiographic Data
The baseline angiographic characteristics for all
study patients showed a preponderance of right
coronary artery (42%) and left anterior descending
artery lesions (48%). Eight percent had a circumflex
artery graft lesion, and one patient had dilation of a
saphenous vein graft to the distal right coronary
artery. The average percent stenosis before intervention was 95 +7% (SD), and coronary flow by average
TIMI grade was 2.0+1.1 Sixty-three percent of the
patients had angiographic evidence of intracoronary
thrombus at baseline.
Angiographic Data During and After
Initial Intervention
The interventional angiographic data on percent
stenosis in the entire group are summarized in Figure
1. The percent coronary stenosis after initial PTCA
was 41+20% and was significantly reduced compared
with baseline. Coronary flow by TIMI grade was also
significantly improved from 2.0±+ 1.1 to 2.8±0.6
(p <0.01).
After PTCA and before the administration of
urokinase, there was a significant increment in the
severity of the percent diameter stenosis due to
thrombus accumulation, and the average percent
diameter stenosis of the ischemia-related artery
increased to 83±17% (Figure 1). The corresponding TIMI grade for coronary flow decreased to
2.1±1.1 (p<0.01).
Angiographic Data After Urokinase Administration
and Repeated PTCA
The mean urokinase dose was 141,000 units
(range, 100,000-250,000 units), and the mean infusion period was 34 minutes (range, 20-65 minutes).
The final angiographic results obtained after the
2056
Circulation Vol 82, No 6, December 1990
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
A
B
C
D
administration of urokinase with repeated PTCA
before departure from the catheterization laboratory
showed significant improvement in the percent diameter stenosis, from 83+17% to 34-+-17%, with an
angiographic success rate of 90% for the entire group
(Figure 1). On departure from the catheterization
laboratory, the TIMI grade was 2.9±0.2 for coronary
flow, and 94% of patients had TIMI grade 3 flow.
graphic follow-up was 30 days (range, 4 days to 13
months). Reocclusion did not occur, although one
patient who was not studied before hospital discharge had an 80% stenosis when studied at 4
months, and another patient exhibited an 80% stenosis 10 days after treatment with persistent angiographic evidence of intraluminal thrombus. This latter patient was discharged on a Coumadin regimen
and had a negative thallium treadmill test 3 weeks
after hospital discharge. The mean percent diameter
stenosis was 32+17% for all patients with follow-up
studies and was similar to that obtained before
departure from the cardiac catheterization labora-
Angiographic Data From Follow-up Studies
Follow-up angiograms were obtained in 79% of the
total group, with 63% of the patients being studied
before hospital discharge. The mean time to angio-
Schieman et al Intracoronary Urokinase With Repeated PTCA
2057
E
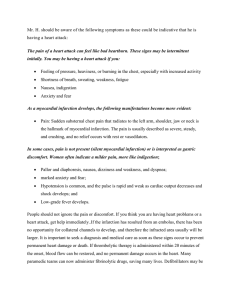
FIGURE 2. Sequential angiograms of the left anterior descending coronary artery in the right anterior oblique projection. Panel A: Before angioplasty. Panel B: Immediately after
angioplasty. Panel C: Several minutes after angioplasty, demonstrating thrombotic restenosis. Panel D: Immediately after
intracoronaty urokinase and repeated angioplasty. Panel E:
Follow-up 10 days after intracoronary urokinase and repeated
angioplasty.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
tory. In all of these patients, the coronary flow was
TIMI grade 3.0 at follow-up.
Sequential angiograms of the left anterior descending coronary artery in the right anterior oblique
100 r
75
F
(0
0
CD
ce
50
0
k
25 F
cx
Lp<0O01
0
I
rr
JL-p<0.1-iLapcO.O1o.i
I
I
A
Pre
Post
Post
Urokinase
Initial
and Repeat PTCA
PTCA
FIGURE 1. Plot of sequential changes in percent diameter
coronary stenosis of the ischemia-related artery in all treated
Initial
patients studied before the first angioplasty (Initial). A high
initial success rate is evident (Post Initial PTCA). Subsequently, flow-limiting intracoronary thrombus accumulation
occurred (Pre), with improvement after urokinase administration and repeated PTCA (Post). Mean ±SD shown. PTCA,
percutaneous transluminal coronary angioplasty.
projection from a representative patient are depicted
in Figure 2. The angiographic result after initial
PTCA was excellent (Figure 2B), but intracoronary
thrombus accumulation resulted in worsened stenosis and diminished antegrade flow (Figure 2C). After
the urokinase infusion and repeated PTCA, there
were luminal filling defects and haze indicative of
residual thrombus, but the stenosis severity was
decreased and coronary flow was TIMI grade 3
(Figure 2D). These abnormalities do not appear on
the follow-up angiogram (Figure 2E).
Complications
Only one patient was referred for urgent CABG.
This patient had an evolving acute myocardial infarction, and after successful restoration of flow in the
infarct-related artery (RCA), symptoms recurred because of a high-grade proximal stenosis in the left
anterior descending coronary artery.
In the entire group, there was no in-hospital
mortality and no procedure-related myocardial infarction or extension occurred. Also, no recurrent
ischemic events requiring repeated angiography or
PTCA occurred before hospital discharge in any
patient. The incidence of transfusion was 10%; one
of these patients bled after CABG surgery.
Plasma fibrinogen levels were determined in 15 patients, and in no patient was the measured level below
the normal range for our laboratory (200-400 mg/dl).
Discussion
PTCA has been used with high initial success rates
in the treatment of unstable angina pectoris, evolving
acute myocardial infarction, and postinfaretion angina, but the rates of coronary reocclusion, emergency CABG, and death have been increased compared with elective PTCA.
2058
Circulation Vol 82, No 6, December 1990
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
In patients with unstable angina, a major complication rate (myocardial infarction, CABG, or death)
of 10.5% was reported by de Feyter et a125 in a series
of 200 consecutive patients treated with PTCA.
These data are representative of a large experience
in patients with unstable angina approached with
steerable angioplasty systems.26-28 Angiographic evidence of intracoronary thrombus in patients with
unstable angina ranges from 1% to 53%, depending
on the criteria used for defining the presence of
thrombus and the time elapsed between the onset of
symptoms and angiography.29-34 In a preliminary
report, Suryapranata et a129 used intracoronary streptokinase to treat acute thrombotic closure that complicated PTCA for unstable angina in 200 consecutive patients; the initial success rate was 94%, but 21
patients developed acute vessel closure. Intracoronary streptokinase was administered in 12 of these
patients, and repeated PTCA was successful in restoring vessel patency in nine patients. In that study,
the patients were not restudied before discharge. In
the experience reported here with intracoronary
urokinase in 10 patients with unstable angina, we also
found a high incidence of angiographic evidence for
intracoronary thrombus in patients who developed
flow-limiting thrombus accumulation. Angiographic
success was obtained in nine of 10 patients, and all
patients had normal antegrade flow restored. Of
importance, our initial success was maintained
throughout the hospitalization with no mortality or
episodes of recurrent ischemia requiring repeated
PTCA, and 100% patency was present in those
patients who underwent angiography before discharge or as late as 13 months after discharge.
The experience with PTCA for the treatment of
acute myocardial infarction has been less encouraging. When direct angioplasty without prior systemic
thrombolytic therapy has been used, angiographic
success rates in selected patients have been high, but
reocclusion rates were 9-15%.35-41 When the strategy of PTCA after thrombolytic therapy has been
compared with thrombolysis alone, acute complication rates have been higher in the PTCA groups, and
infarct-related artery reocclusion rates were high and
not significantly different.15-17 Our experience in the
small number of such patients in the present pilot
study who were treated with PTCA during acute
myocardial infarction shows a significantly higher
incidence of intracoronary thrombus reaccumulation
but suggests that adjunctive intracoronary urokinase,
with repeated PTCA if needed, can successfully treat
acute thrombotic closure in this setting, thereby
avoiding the need for emergency CABG. Of the 35
patients treated with PTCA for evolving myocardial
infarction in the present study, the majority of whom
had received prior thrombolytic therapy, 18 were
treated with intracoronary urokinase for progressive
thrombus accumulation. Only one patient in this
group was referred for urgent CABG after successful
PTCA of the right coronary artery, but this was
because of a high-grade lesion in the proximal left
anterior descending coronary artery. As with our
experience in the unstable angina group, there were
no recurrent ischemic episodes, and the angiographic
infarct-related artery patency was 100% at follow-up
angiography in those patients studied. The very high
infarct-related artery patency rate suggests a role for
adjunctive intracoronary urokinase when PTCA is
complicated by flow-limiting thrombus accumulation
during acute myocardial infarction.
There have been a number of reports on the
treatment of early postinfarction angina with PTCA
in which initial recanalization rates were high (8191%), but the rates of major procedure-related com-
plications of myocardial infarction (1.5-8%) and
emergency CABG (1.5-12%) were increased compared with elective PTCA.20,21,42-45 To our knowledge, the efficacy of adjunctive intracoronary urokinase in patients with postinfarction angina who
developed thrombotic reclosure after a successful
PTCA has not been reported. In the present series,
the primary success rate with PTCA was high; intracoronary urokinase with repeated PTCA was successful in restoring normal antegrade flow in all patients;
no recurrent ischemic events requiring repeated
PTCA occurred before hospital discharge, and there
was no evidence for restenosis in the 65% of patients
undergoing predischarge angiography.
The results obtained by using adjunctive intracoronary urokinase with repeated PTCA for flow-limiting thrombus accumulation in the present study were
consistent: high angiographic success rates that were
maintained throughout the acute phase of their illness
without reocclusion. Thus, in addition to the immediate benefit of restoration of coronary flow, the use of
adjunctive intracoronary urokinase may result in
maintained vessel patency in patients undergoing
PTCA for acute ischemic syndromes. The benefit of
establishing and maintaining vessel patency has been
demonstrated in three separate trials in which a
significant correlation between survival 1 year after
acute myocardial infarction and patency of the infarctrelated artery was reported.46-48 Less late left ventricular dilation after infarction has been described in
patients with patent infarct-related arteries before
discharge,49 and it has been proposed that maintenance of successful reperfusion, even when it occurs
late, may lead to more favorable left ventricular
remodeling.50 Long-term follow-up of the patients in
the present study, and in additional patients subsequently treated with intracoronary urokinase, is currently underway to determine whether the favorable
initial results on vessel patency are maintained.
Limitations of the Study
This pilot study is limited by the lack of randomized design and the relatively small number of
patients in each group. Nonetheless, this represents
the largest experience reported on the efficacy of
intracoronary urokinase in the treatment of acute
ischemic syndromes. Although the angiographic follow-up is incomplete, 79% of patients underwent
Schieman et al Intracoronary Urokinase With Repeated PTCA
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
follow-up coronary angiography, and the lack of
recurrent ischemic events in the other patients suggests that a high patency rate was maintained
throughout the hospitalization. Quantitative angiography was not used, but the changes in percent
diameter stenosis were large and corresponded to
observed changes in TIMI grades of coronary flow.
Fibrinogen levels were measured in too few patients to state definitively that a systemic lytic state
was avoided with this approach. We have continued
to measure fibrinogen levels in all subsequent patients treated with intracoronary urokinase for
thrombotic closure complicating PTCA in acute ischemic syndromes (40 patients), and in none has the
fibrinogen level been abnormal. We believe this to be
an important advantage of this approach, and our
findings are consistent with the data from the only
randomized trial comparing intracoronary urokinase
with streptokinase in patients with acute myocardial
infarction.23 In that study, reperfusion rates were
equivalent for the two lytic agents, but fibrinogen
levels less than 100 g/dl were significantly more
frequent with streptokinase (66%) than with urokinase. Bleeding complications were also significantly
increased in the streptokinase group.
Implications
The exact role of PTCA in the treatment of acute
ischemic syndromes remains to be defined. In the
randomized trials on patients with acute myocardial
infarction treated with recombinant tissue-type plasminogen activator with or without immediate PTCA,
it can only be speculated whether or not the concomitant use of intracoronary urokinase could have diminished the rate of major complications in the
patient groups receiving immediate PTCA. Patients
with postinfarction ischemia, whether or not they
have received antecedent systemic thrombolytic therapy, often require emergency PTCA in the setting of
an acute ischemic syndrome, and our data suggest
that intracoronary urokinase may be helpful when
thrombus accumulation limits flow. Primary PTCA
has potential application in many patients in whom
thrombolytic therapy is contraindicated, and its usefulness may be enhanced with development of an
effective approach for treating flow-limiting intracoronary thrombus accumulation.
The conventional approach to patients with acute
ischemic syndromes involves medical therapy with
antianginal agents, systemic anticoagulants, and antiplatelet agents. If patients fail to stabilize early,
coronary angiography is indicated, and if suitable
coronary anatomy is present, PTCA may be attempted. If flow-limiting thrombus accumulation occurs in this setting, our data suggest that it can be
successfully managed with intracoronary urokinase
and repeated PTCA in most patients. However, the
high success rates in this pilot study will need to be
confirmed in randomized trials, and the late results
of this approach will also require assessment in such
trials and in ongoing follow-up studies.
2059
References
1. Davies MJ, Thomas AC: Plaque fissuring -The cause of acute
myocardial infarction, sudden ischemic death, and crescendo
angina. Br Heart J 1985;53:363-373
2. Mandelkorn JB, Wolf NM, Singh S, Schechter JA, Kersh RI,
Rodgers DM, Workman MB, Bentivaglio LG, LaPorte SM,
3.
4.
5.
6.
7.
8.
9.
Meister SG: Intracoronary thrombus in nontransmural myocardial infarction and in unstable angina pectoris. Am J
Cardiol 1983;52:1-6
DeWood MA, Spores J, Notske R, Mouser LT, Burroughs R,
Golden MS, Lang HT: Prevalence of total coronary occlusion
during the early hours of transmural myocardial infarction. N
Engl J Med 1980;303:897- 902
Ambrose JA, Winters SL, Stern A, Eng A, Teichholz LE,
Gorlin R, Fuster V: Angiographic morphology and the pathogenesis of unstable angina pectoris. JAm Coll Cardiol 1985;5:
609-616
Fuster V, Chesbro JH: Mechanisms of unstable angina. N Engl
JMed 1986;315:1023-1025
Sherman CT, Litvack F, Grundfest W, Lee M, Hickey A,
Chaux A, Koss R, Blanche C, Matloff J, Morgenstern L, Ganz
W, Swan HJC, Forrester J: Coronary angioscopy in patients
with unstable angina pectoris. N EnglJMed 1986;315:913- 919
Mulcahy R, Daly L, Graham I, Hickey N, O'Donoghue S,
Owens A, Ruane P, Tobin G: Unstable angina: Natural history
and determinants of prognosis. Am J Cardiol 1981;48:525-528
Mulcahy R: Natural history and prognosis of unstable angina.
Am Heart J 1985;109:753-759
Lewis HD, Davis JW, Archibald DG, Steinke WE, Smitherman TC, Doherty JE III, Schnaper HW, LeWinter MM,
Linares E, Pouget JM, Subharwal HC, Chester E, DeMots H:
Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. N Engl J Med
1983;309:396-403
10. de Feyter PJ, Suryapranata H, Serruys PW, Beatt K, van
Domburg R, van den Brand M, Tijssen JJ, Azar AJ, Hugenholtz PG: Coronary angioplasty for unstable angina: Immediate and late results in 200 consecutive patients with identification of risk factors for unfavorable early and late outcome. J
Am Coll Cardiol 1988;12:324-333
11. Faxon DP, Detre KM, McCabe CH, Fisher L, Holmes DR,
Cowley MJ, Bourassa MG, van Roden M, Ryan TJ: Role of
percutaneous transluminal coronary angioplasty in the treatment of unstable angina: Report from the National Heart,
Lung, and Blood Institute Percutaneous Transluminal Coronary Angioplasty and Coronary Artery Surgery Study Registries. Am J Cardiol 1984;53:131C-135C
12. Quiqley PJ, Erwin J, Maurer BJ, Walsh MJ, Gearty GF:
Percutaneous transluminal coronary angioplasty in unstable
angina: Comparison with stable angina. Br Heart J 1986;55:
227-230
13. Mabin TA, Holmes DR, Smith HC, Vlietstra RE, Bove AA,
Reeder GS, Chesebro JH, Bresnahan JF, Orszwlak TA:
Intracoronary thrombus: Role in coronary occlusion complicating percutaneous transluminal angioplasty. JAm Coll Cardiol 1985;5:198-202
14. Hartzler GO, McConahay DR, Johnson WL Jr: Direct balloon
angioplasty in acute myocardial infarction: Without prior use
of streptokinase. JAm Coll Cardiol 1986;7:149A
15. Topol EJ, Califf RM, George BS, Kereiakes DJ, Abbottsmith
CW, Candela RJ, Lee KL, Pitt B, Stack RS, O'Neill WM, and
the Thrombolysis and Angioplasty in Myocardial Infarction
Study Group: A randomized trial of immediate versus delayed
elective angioplasty after intravenous tissue plasminogen activator in acute myocardial infarction. N Engl J Med 1987;317:
581-588
16. Simoons ML, Arnold AE, Betriu A, deBono DP, Col J,
Dougherty FC, von Essen R, Lambertz H, Lubsen J, Meier B,
Michel P, Raynaud P, Rutsch W, Sanz GA, Schmidt W,
Serruys PW, Thery C, Uebis R, Vahanian A, van de Werf F,
Wilems GM, Wood D, Verstraete M, for the European
Cooperative Study Group for Recombinant Tissue-Type Plasminogen Activator (rTPA): Thrombolysis with tissue plasmin-
2060
Circulation Vol 82, No 6, December 1990
activator in acute myocardial infarction: No additional
benefit from immediate percutaneous transluminal coronary
angioplasty. Lancet 1988;1:197-203
17. The TIMI Research Group: Immediate versus delayed catheterization and angioplasty following thrombolytic therapy for
acute myocardial infarction: TIMI IIA Results. JAMA 1988;
260:2849-2858
18. Fraker TD, Wagner GS, Rosati RA: Extension of myocardial
infarction: Incidence and prognosis. Circulation 1979;60:
1126-1129
19. Ross J Jr, Gilpin EA, Madsen EB, Henning H, Nicod P,
Dittrich H, Engler R, Rittlemeyer J, Smith SC Jr, Viquerat C:
A decision scheme for coronary angiography after acute
myocardial infarction. Circulation 1989;79:292-303
20. Gottlieb SO, Brin KP, Walford GD, McGaughey M, Riegel
MB, Brinker JA: Percutaneous transluminal coronary angioplasty for early post-infarction unstable angina: Results and
follow-up (abstract). JAm Coll Cardiol 1986;7:20A
21. de Feyter PJ, Serruys PW, Soward A, van der Brand M, Bos E,
Hugenholtz PG: Coronary angioplasty for early post-infarction
unstable angina. Circulation 1986;74:1365-1370
22. Hopkins J, Savage M, Zalunski A, Dervan JP, Goldberg S:
Recurrent ischemia in the zone of prior myocardial infarction:
Results of coronary angioplasty of the infarct related artery.
Am Heart J 1988; 115:14-19
23. Tennant SN, Dixon J, Venable TC, Page HL Jr, Roach A,
Kaiser AB, Frederiksen R, Tacogue L, Kaplan P, Babu NS,
Anderson EE, Wooten E, Jennings HS III, Breinig J, Campbell WB: Intracoronary thrombolysis in patients with acute
myocardial infarction: Comparison of efficacy of urokinase
and streptokinase. Circulation 1984:69:756-760
24. The TIMI Study Group: The thrombolysis in myocardial
infarction (TIMI) trial: Phase I findings. N Engl J Med
1985;312:932-936
25. de Feyter PJ, Serruys PW, van der Brand M, Balakumaran K,
Mochtar B, Seward AL, Arnold AER, Hugenholtz PG: Emergency coronary angioplasty in refractory unstable angina. N
Engl J Med 1985;313:342-347
26. Meyer J, Schmitz HJ, Kiesslich T, Erbel R, Krebs W, Schulz
W, Bardos P, Minale C, Messmer BJ, Effert S: Percutaneous
transluminal coronary angioplasty in patients with stable and
unstable angina pectoris: Analysis of early and late results. Am
Heart J 1983;106:973-980
27. Williams DO, Riley RS, Singh AK, Gerwitz H, Most AS:
Evaluation of the role of coronary angioplasty in patients with
unstable angina pectoris. Am Heart J 1981;102:1-9
28. Plokker HWJ, Ernst SMPG, Bal ET, van den Berg ECJM,
Mast GEG, van der Feltz TA, Ascoop CAPL: Percutaneous
transluminal coronary angioplasty in patients with unstable
angina pectoris refractory to medical therapy. Cathet Cardiovasc Diagn 1988;14:15-18
29. Suryapranata H, de Feyter P, Serruys P: Coronary angioplasty
in patients with unstable angina pectoris: Is there a role for
thrombolysis? JAm Coll Cardiol 1988;12:69A-77A
30. Capone G, Wolf NM, Meyer B, Meister SG: Frequency of
intracoronary filling defects by angiography in angina pectoris
at rest. Am J Cardiol 1985;56:403-406
31. Vetrovec GW, Cowley MJ, Overton H, Richardson DW:
Intracoronary thrombus in syndromes of unstable myocardial
ischemia. Am Heart J 1981;102:1202-1208
32. Zack PM, Ischinger T, Aker VT, Dineer B, Kennedy HL: The
occurrence of angiographically detected intracoronary thrombus in patients with unstable angina pectoris. Am Heart J
1984;108:1408-1412
33. Holmes DR, Hartzler GO, Smith HC, Fuster V: Coronary
artery thrombus in patients with unstable angina. Br Heart J
1981;45:411-416
34. Freeman MR, Williams AE, Chisholm RJ, Armstrong RW:
Intracoronary thrombus and complex morphology in unstable
angina: Relation to timing of angiography and in-hospital
cardiac events. Circulation 1989;80:17-23
ogen
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
35. O'Neill WM, Timmis GC, Bourdillon P, Lai P, Ganghadarhan
V, Walton J Jr, Ramos R, Laufer N, Gordon S, Schork MA,
Pitt B: A prospective randomized clinical trial of intracoronary
streptokinase versus coronary angioplasty therapy of acute
myocardial infarction. N Engl J Med 1986;314:812- 828
36. Hartzler GO, Rutherford BD, McConahay DR, Johnson Wl,
McCallister BD, Gura GM Jr, Conn RC, Crockett JE: Percutaneous transluminal coronary angioplasty with and without
thrombolytic therapy for treatment of acute myocardial infarction. Am Heart J 1983;106:965 -973
37. Kimura T, Nosaka H, Veno K, Nobuyoshi M: Role of coronary
angioplasty in acute myocardial infarction (abstract). Circulation 1986;74(suppl II):I1-22
38. Rothbaum DA, Linnemeier TJ, Laudin RJ, Steinmetz EF,
Hillis JS, Hallman CC, Noble RJ, See MR: Emergency
percutaneous transluminal coronary angioplasty in acute myocardial infarction: A 3 year experience. J Am Coll Cardiol
1987;10:264-272
39. Marco J, Caster L, Szatmary LJ, Fajadet J: Emergency percutaneous transluminal coronary angioplasty without thrombolysis as initial therapy in acute myocardial infarction. Int J
Cardiol 1987;15:55-63
40. Topol EJ: Direct or sequential PTCA, in Topol EJ (ed): Acute
Coronary Intervention. New York, Alan R. Liss, Inc, 1988, pp
77-84
41. Topol EJ: Coronary angioplasty for acute myocardial infarction. Ann Intem Med 1988;109:970-980
42. Holt GW, Gersh BJ, Holmes DR, Vliestra RE, Reeder GS,
Bresnahan JF, Smith HC: The results of percutaneous transluminal coronary angioplasty in post-infarction angina pectoris
(abstract). J Am Coll Cardiol 1986;7:62A
43. Safian RD, Snijder L, Snyder BA, McKay RG, Lorell BH,
Aroesty JM, Pasternak RC, Bradley AB, Monrad ES, Baim
DS: Usefulness of percutaneous transluminal coronary angioplasty for unstable angina pectoris after non-Q wave acute
myocardial infarction. Am J Cardiol 1987;59:263-266
44. Suryapranata H, Beatt K, de Feyter PJ, Verrostte J, van den
Brand M, Zijlstra F, Serruys PW: Percutaneous transluminal
coronary angioplasty for angina pectoris after a non-Q wave
acute myocardial infarction. Am J Cardiol 1988;61:240-243
45. Hopkins J, Savage M, Zaluwski A, Dervan JP, Goldberg S:
Recurrent ischemia in the zone of prior myocardial infarction:
Results of coronary angioplasty of the infarct related artery.
Am Heart J 1988;115:14-19
46. Stadius ML, Davis K, Maynard C, Ritchie JL, Kennedy JW:
Risk stratification for one year survival based on characteristics identified in the early hours of acute myocardial infarction.
Circulation 1986;74:703-711
47. Dalen JE, Gore JM, Braunwald E, Borer J, Goldberg RJ,
Passamani ER, Forman S, Knatterud G, the TIMI Investigators: Six- and twelve-month follow-up of the phase I thrombolysis in myocardial infarction (TIMI) trial. Am J Cardiol
1988;62:179-185
48. Stack RS, Califf RM, Hinohasa T, Phillips HR, Pryor DB,
Simanton CA, Carlson EB, Morris KG, Behar VS, Kong Y,
Peter RH, Hlatky MA, O'Connor CM, Mark DB: Survival and
cardiac event rates in the first year after emergency coronary
angioplasty for acute myocardial infarction. J Am Coll Cardiol
1988;11:1141-1149
49. Jeremy RW, Heickworth RA, Bautovich G, Hutton BF, Harris
PJ: Infarct artery perfusion and changes in left ventricular
volume in the month after acute myocardial infarction. J Am
Coll Cardiol 1987;9:989-995
50. Braunwald E: Myocardial reperfusion, limitation of infarct
size, reduction of left ventricular dysfunction, and improved
survival -Should the paradigm be expanded? Circulation 1989;
79:441-444
KEY WORDS * percutaneous transluminal coronaiy angioplasty
ischemia * thrombus
*
Intracoronary urokinase for intracoronary thrombus accumulation complicating
percutaneous transluminal coronary angioplasty in acute ischemic syndromes.
G Schieman, B M Cohen, J Kozina, J S Erickson, R A Podolin, K L Peterson, J Ross, Jr and M
Buchbinder
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Circulation. 1990;82:2052-2060
doi: 10.1161/01.CIR.82.6.2052
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1990 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/82/6/2052
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/