Chapter 12 The Role of Fine Needle Aspiration Biopsy in the
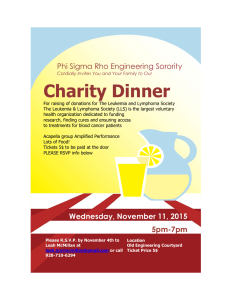
advertisement

Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms Rana S. Hoda FINE NEEDLE ASPIRATION Introduction Fine needle aspiration (FNA) is a well-established minimally invasive technique for the cytologic evaluation of suspicious mass lesions involving lymph nodes and other organs. The 2008 WHO classification of tumors of hematopoietic and lymphoid tissues utilizes a multiparametric approach based on cytomorphologic, immunophenotypic, and cytogenetic features to classify these tumors (1). This approach can be applied to FNA cytologic specimens (2–8), of both nodal and extranodal sites. About 25% to 40% of lymphoid neoplasms arise outside of the lymph node system, and dissemination of nodal neoplasms may occur to almost any anatomical site, presenting as an extranodal mass (8). FNA in conjunction with flow cytometry (FCM) has been shown to be useful for the diagnosis and subclassification of lymphoma (2–4,8–10). The use of FNA for in the initial workup of patients with hematolymphoid neoplasms, particularly for patients who present with lymphadenopathy, remains underutilized (Table 12.1). Lymphoma constitutes approximately 10% of cases diagnosed by FNA (2,7,9–11). Indications of FNA of Lymph Nodes The utility of FNA in lymphadenopathy varies with the clinical situation (Table 12.2). The majority of cases of lymphadenopathy are benign or reactive, and FNA can be particularly advantageous in the diagnosis and appropriate management thereof (12). Accuracy of Reporting FNA of Lymph Nodes Diagnostic accuracy of FNA for high-grade non-Hodgkin lymphoma (NHL) and Hodgkin lymphoma (HL) (with the exception of lymphocytic predominant variant) is high (70% to 90%) (2,13). However, FNA has significant limitations in Table 12.1 REASONS FOR UNDERUTILIZATION OF FNA FOR HEMATOLYMPHOID LESIONS • Relative ease of excisional biopsy • Ignorance of terminologies and classification • Limited experience • Limited availability of cytopathologists • Nonavailability of ancillary tests • Lack of histologic architecture • Morphologic difficulty in distinguishing reactive and low-grade lymphomas the assessment of low-grade B-cell lymphomas with a relatively low diagnostic accuracy (67%), inherent to the loss of architecture (14). False-negative rate of FNA for lymphoid lesions ranges from 5% to 15%, with low-grade lymphomas accounting for a significant percentage of the false-negative or indeterminate cases (14,15). The major strength of FNA in the workup of hematopoietic and lymphoid lesions is its high specificity (85% to 100%) even in extranodal sites. The diagnostic sensitivity of FNA in the initial workup of hematolymphoid lesions is enhanced when it is used in conjunction with FCM and/or needle core biopsy (16). A close interaction between cytopathologists and hematopathologists to coordinate the morphologic and immunophenotypic data is also required (7,8). Cytologic Preparations for FNA Specimens Aspirated material for evaluation of hematolymphoid lesions is first processed as direct smears, both air-dried and ­alcohol-fixed smears (Fig. 12.1). Air-dried smears are stained with a Romanowsky method. In this respect, Diff-Quik (DQ) stain, which provides better assessment of background and cytoplasmic features, is preferred. Alcohol-fixed smears are best stained with Papanicolaou (Pap) stain, which is useful for assessing nuclear features. Hematoxylin and eosin (H&E) stain can also be used for fixed smears. Residual material is rinsed for preparation of liquid-based preparations (LBPs), such as ThinPrep (TP [Hologic Inc., Bedford, MA]) or SurePath (SP [BD Diagnostics, Burlington, NC]), or for the preparation of cell block (17). LBPs are preferably not used as the sole preparation type for FNA of suspected lymphoma because of artifactual aggregation and clumping of lymphoid cells (Fig. 12.2), but are best suited for immunocytochemistry (ICC) and molecular analyses. FNA Technique and Triage Superficial FNA, by palpation only, is usually performed using thin needles, generally 22 to 27 gauge, and most often 1 to 1.5 inch in length attached to a 5 or 10 mL disposable Table 12.2 INDICATIONS OF FNA OF LYMPH NODES • Distinguish between benign and neoplastic lesions • Diagnosis of infection and to obtain material for bacterial or fungal cultures • Confirmation of suspected metastases • Diagnosis of hematolymphoid lesions and to obtain ancillary studies • Document disease extent, relapse, progression, or transformation of ­hematolymphoid neoplasm • Monitor effects of therapy in hematolymphoid neoplasms 293 Orazi9781609136826-ch12.indd 293 8/5/2013 12:01:45 PM 294 Knowles Neoplastic Hematopathology FIGURE 12.2. Both liquid-based techniques, TP and SP, produce artificial aggregations of lymphocytes that may be mistaken for epithelial cells (Pap stain, TP ×60 objective). performed by radiologists with CT guidance using a 21- and 22-gauge Chiba needle (20,21). EUS-FNA is considered the procedure of choice for tissue sampling of abdominal and mediastinal nodes that may be difficult to reach by percutaneous CT guidance. EUS-FNA combined with FCM has a reported accuracy of 70% to 90% in the diagnosis of intrathoracic and intra-abdominal lymphoma (14,22,23). EUS also has the ability to obtain biopsy for histologic evaluation (14,23). A cytologist should assess on-site adequacy at the time of FNA by the air-dried DQ-stained smears and perform proper specimen triage (24,25). When a hematolymphoid lesion is suspected, residual and additional specimen is rinsed in either a phosphate-buffered saline solution or RPMI (Roswell Park Memorial Institute) cell media for FCM. When an inflammatory/infectious etiology is suspected, microbiology studies can be obtained. Tables 12.3 to 12.5 outline the advantages and limitations of FNA. FIGURE 12.1. Gross appearance of various types of cytologic preparations. (Top row from left to right) Diff-Quik (DQ)-stained direct smear (DS), Papanicolaou (Pap)-stained DS, hematoxylin and eosin (H&E)-stained cell block section; (bottom row from left to right) ThinPrep (TP [20 mm diameter circle]), SurePath (SP [13 mm diameter circle]), and cytospin (CS [12 mm diameter circle]). plastic syringe that may be placed on a Cameco aspiration gun. Shorter gauge needles or “butterfly” needles may be used for superficial subcutaneous lesions (18). High-resolution ultrasound (US) technology is considered the “gold standard” for evaluation of superficially located targets. Pathologists are currently being trained and certified by the College of American Pathologists (CAP) in performing US-guided FNA (19). Image guidance enables anatomic localization of the target and its relationship to adjacent tissues. Specific features of the target including its size and shape can be visualized. Suspected lymphomas of deep-seated organs are sampled by the help of radiologic techniques including computed tomography (CT) or endoscopic ultrasound (EUS) techniques. Transthoracic and transabdominal FNA are generally Orazi9781609136826-ch12.indd 294 Strategies of FNA Interpretation Strategies for the evaluation of FNA of lymph nodes are outlined in Figure 12.3. Interpretive problems may result from improper FNA technique, faulty smearing technique, or lesional characteristics: (i) improper FNA technique fails to yield smears that are sufficiently cellular; (ii) faulty smearing Table 12.3 ADVANTAGES OF SUPERFICIAL FNA • Simple, easy, safe, rapid • Cost-effective • Noninvasive • Preserves native lymph node architecture • Ability to sample multiple lymph nodes • Can be combined with FCM • Fresh and pure tumor cells obtained for molecular tests • Easily repeated allowing serial (pretherapy and posttherapy) sampling • Complications are rare 8/5/2013 12:01:46 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms295 Table 12.4 ADVANTAGES OF RADIOLOGICALLY GUIDED FNA Table 12.5 • Small or deep-seated targets can be sampled • Nature of target (solid or cystic) can be assessed • Reduced number of nondiagnostic biopsies, after on-site cytologic a­ ssessment of adequacy • Follow-up of benign tumors for growth or change at defined intervals with US • No ionizing radiation exposure with US • Inability to subclassify lymphoma • Loss of important architectural patterns • Inability to reliably distinguish RHL from low-grade lymphomas • Inability to reliably distinguish between various types of low-grade lymphoma • False-negative results due to • Sampling error with inadequate sampling due to –– Poor biopsy technique –– Peripheral blood contamination –– Marked nodal fibrosis –– Partial involvement of lymph node by tumor –– Extensive necrosis or inflammation • Interpretive errors –– Faulty smearing techniques –– Paucity of diagnostic cells such as Reed-Sternberg cells • Rare, post-FNA changes in lymph nodes that may occur and interfere with histologic assessment • Total infarction • Hemorrhage • Granulation tissue Poorly-stained Artifacts Smear LIMITATIONS OF FNAB • Inability to subclassify lymphoma • Loss of important architectural patterns • Inability to reliably distinguish RHL from low-grade lymphomas • Inability to reliably distinguish between various types of low-grade lymphoma • False-negative results due to • Sampling error with inadequate sampling due toa –– Poor biopsy technique –– Peripheral blood contamination –– Marked nodal fibrosis –– Partial involvement of lymph node by tumor –– Extensive necrosis or inflammation • Interpretive errors –– Faulty smearing techniques –– Paucity of diagnostic cells such as Reed-Sternberg cells • Rare, post-FNA changes in lymph nodes that may occur and interfere with histologic assessment • Total infarction • Hemorrhage • Granulation tissue a Three or more passes with sampling from different parts of the lesion or lymph node will reduce sampling error. Sampling error may be reduced with the use of US guidance. Acellular/paucicellular Thick smears, bloody smears, “crush” artifact FIGURE 12.3. Strategies of FNA interpretation. Cystic squamous cell carcinoma congenital cysts, salivary gland lesions, stromal processes “Nodules” Cellular Dispersed Monotonous Polymorphous Polymorphous Carcinoma Melanoma ML, follicular, grades 1 and 2 Childhood round cell tumors Carcinoma Melanoma Nodular lymphoid hyperplasia ML, follicular grades 2 and 3 Diffuse lymphoid hyperplasia Hodgkin lymphoma ML, follicular, peripheral, T-cell lymphoma, Carcinoma, Melanoma Monotonous Suspect ML Rare events Granulomas Reed-Sternberg cells Small cells Large cells Round nuclei, clumped chromatin Round and/or irregular vesicular nuclei with multiple small nucleoli- ML, SLL/CLL Hodgkin lymphoma, lymphocyte predominant, Burkitt lymphoma, atrophic lymph node ML, diffuse large B-cell Irregular nuclei, creases/folds Round nuclei, coarsely reticulated chromatin with multiple nucleoli ML, follicular, grades 1 and 2 Burkitt lymphoma Convoluted nuclei, fine chromatin ML, lymphoblastic Orazi9781609136826-ch12.indd 295 8/5/2013 12:01:48 PM 296 Knowles Neoplastic Hematopathology FIGURE 12.4. Technical issues with lymph node aspirate preparation. A: A smear preparation with unevenly distributed cellular material that is too concentrated for proper staining. B: Excessive pressure during smear preparation showing “crush” artifact (A and B, DQ stain, DS ×20 objective). technique can result in concentration of the cellular material, resulting in poorly stained smears (Fig. 12.4A) or excessive pressure during smear preparation may result in “crush” artifact (Fig. 12.4B); or (iii) lesional characteristics—centrally necrotic masses are best sampled at the periphery or it may result in adequate sampling. Some lymphoid neoplasms are associated with marked sclerosis, such as nodular sclerosing Hodgkin lymphoma (NSCHL), and may yield paucicellular samples (26,27). Histologic evaluation of hematolymphoid processes is based on interpretation of architectural and cellular patterns that provide important clues in interpretation. Adopting the histopathologic approach to cytologic evaluation of lymph nodes enables the cytopathologist to discern vague architectural patterns on scanning magnification. Small cellular aggregates or dispersed cells pattern can be identified (Fig. 12.5A and B). Lymph nodes that display cellular patterns of an admixture of small, mediumsized, and large lymphocytes (polymorphous population) in addition to tingible body macrophages and histiocytes are usually associated with benign or reactive conditions (Fig. 12.6A–C). In contrast, a monotonous or monomorphous cell population generally implies a malignant condition (Fig. 12.7A–C). Several exceptions to this rule exist including HL and lymphoma with a high content of epithelioid histiocytes that may show polymorphous cells (Fig. 12.7D). Monotony in a lymph node aspirate also does not always indicate lymphoma. Carcinomas may appear discohesive and monotonous (Fig. 12.8). Examination of cytologic features at high magnification allows further separation into monomorphous and polymorphous lymphoid cell populations (Fig. 12.9A and B). Proliferative and apoptotic indices may also be used on FNA samples for subclassification and histologic grading of B-cell NHL (28,29). An increase in the mean Ki-67 proliferation index has been reported with tumor aggressiveness. The Ki-67 median percentages of 15% for indolent lymphomas and 50% for aggressive lymphomas have been reported that show good correlation with histologic samples (Fig. 12.9C) (28). Apoptotic index may be incorporated with other cytomorphologic criteria. An apoptotic index of more than 3.5% may indicate a highgrade lymphoma (Fig. 12.9D) (29). FIGURE 12.5. Architectural patterns on scanning magnification on cytologic smears. A: Small nodular aggregates indicating lymphoid follicles in reactive follicular hyperplasia. B: A dispersed cell pattern from a reactive lymph node (A and B, DQ stain, DS ×20 objective). Orazi9781609136826-ch12.indd 296 8/5/2013 12:01:51 PM FIGURE 12.6. Polymorphous lymphoid cells in a reactive lymph node FNA. A: Smear displays small, medium-sized, and large lymphocytes in addition to tingible body macrophages and histiocytes (A, DQ stain, DS ×40 objective). B,C: Higher magnification displays tingible body macrophages with round-to-oval nuclei, pale chromatin, small nucleoli, and cytoplasmic cellular debris; note the mature compact chromatin of polymorphous lymphoid cell nuclei (A, DQ stain, DS and B, Pap stain, DS ×100 objective with oil immersion). FIGURE 12.7. Nature of lymphoid cells in lymphoma. A,B: Smear from CLL depicts a monotonous small cell population that generally implies malignancy. Compare the size of neoplastic lymphoid cells with red blood cells (RBCs [A, DQ stain, DS and B, Pap stain, DS ×60 objective]). C: Smear from a case of DLBCL displaying monotonous population of large neoplastic lymphoid cells. Compare the nuclear size with scattered benign lymphoid cells (DQ stain, DS ×100 objective with oil immersion). D: HL and lymphoma with a high content of epithelioid histiocytes that may show polymorphous cells (DQ stain, DS ×60 objective). Orazi9781609136826-ch12.indd 297 8/5/2013 12:01:56 PM 298 Knowles Neoplastic Hematopathology ANCILLARY METHODS FOR DIAGNOSIS OF HEMATOPOIETIC AND LYMPHOID LESIONS The success of FNA in the diagnosis of hematolymphoid lesions relies on adopting a multidisciplinary approach, that is, analyzing cytomorphology, ICC, and FCM (2–8,27,30–35). Molecular studies further enhance diagnostic sensitivity and specificity of FNA (36). Immunochemistry FIGURE 12.8. Occasionally, carcinomas may appear discohesive and monotonous. In this case of metastatic urothelial carcinoma in lung, the smear shows monomorphic epithelial cells. Clinical history, review of urothelial carcinoma histology, and a cercariform cell (11 o’clock position) provide a helpful clue to the primary malignancy (DQ stain, DS ×60 objective). The application of ICC has enhanced the ability to diagnose and classify lymphomas. ICC can be successfully applied to FNA specimens. ICC is preferable in those cases where FCM has a high false-negative rate such as large cell lymphomas, HL, and metastases (37,38). An abbreviated antibody panel including leukocyte common antigen (CD45), cytokeratin (AE1/AE3), and S-100 protein can be applied initially. In suspected hematolymphoid lesions, an expanded battery of monoclonal antibodies can be employed including CD20, CD79a, and PAX5 (markers for B-cell lymphoma) (Figs. 12.9C and 12.10A and B). The presence of FIGURE 12.9. Evaluation of nuclear features. A: FNA smear from a case of DLBCL demonstrates monomorphic malignant cells. Note the large tumor cells size (compare with RBCs), nuclear contour irregularity, and nucleoli. Numerous lymphoglandular bodies (cytoplasmic fragments) are present close to bare nuclei. In comparison to (A), the smear in (B) is from a reactive lymph node showing polymorphous small lymphoid cells. Note the mature chromatin. Tingible body macrophage and a mitotic figure are also seen (A and B, DQ stain, DS ×100 objective with oil immersion). C: Cells from a case of DLBCL showing a Ki-67 index of 100% (DS ×60 objective). D: Increased apoptosis from a case of a high-grade lymphoma (Pap stain, DS ×60 objective). Orazi9781609136826-ch12.indd 298 8/5/2013 12:02:00 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms299 FIGURE 12.10. Immunocytochemistry. A: Cytoplasmic positivity for CD45 in a case of DLBCL. B: Strong nuclear positivity for Pax5 in a case of CLL/SLL (DS ×60 objective). light-chain restriction may be the most useful criterion for determining B-cell malignancy and can be applied to limited cytology sample or in cell block sections of adequate sample (31). Evaluation of antigen loss, crucial to the immunologic diagnosis of peripheral T-cell lymphoma (PTCL), may be more difficult to perform in FNA smears than in frozen sections, because assessment of antigen expression within specific regions of the lymph node is not possible. In cytology, ICC can be performed on additional LBP including TP or SP, cytospins, or cell block sections (37). The advantages of ICC over FCM are the requirement of a small sample, preservation of cellular morphology, use in cases of large cell lymphomas where FCM may be falsely negative, and ability to assess staining pattern and intensity of staining. The disadvantage of ICC is that evaluation of double antigen expression (e.g., CD5/CD23 or CD10/BCL2) is not possible. Flow Cytometry Immunophenotyping by FCM in the diagnosis of lymphoma is performed for the detection of clonality, which distinguishes lymphoma from reactive lymphoid hyperplasia (RLH). The utility of FNA in conjunction with FCM for definitive diagnosis of NHL is well documented (2,4,7,9,13,30,39–42). Several studies of FNA and FCM have used the REAL/WHO classification system for diagnosis and subclassification of NHL. Meda et al. (2) evaluated 290 aspirates from 275 patients. A definitive diagnosis of NHL was made in 76.7% on the basis of FNA and FCM, which resulted in a sensitivity of 95% and specificity of 85%. Dong et al. (4) diagnosed 67% of primary and recurrent lymphomas using FNA combined with FCM. In another reported series, all 74 cases of lymphoma on FNA were correctly diagnosed (9). In this study, correct classification was more accurate in 53 cases that were also subjected to concurrent FCM (84% vs. 33%). These studies indicate the importance of using FNA Table 12.6 FALSE-NEGATIVE FLOW CYTOMETRY • Sampling error • Partial involvement of lymph node by disease • Insufficient number of neoplastic cells • Few viable cells • Peripheral blood contamination • Large cell lymphoma • Primary T-cell lymphoma Orazi9781609136826-ch12.indd 299 in conjunction with FCM for diagnosis and subclassification of lymphoma. FCM is sensitive, provides quantitative results, and can detect a small abnormal cell population in a reactive background. FCM has the advantages of multiparametric analysis and objective interpretation. The panel of antibodies utilized in FCM depends on the amount of FNA material provided. The use of an FCM panel comprising of B- and T-cell counts, kappa and lambda, CD4/CD8 ratio, and proliferation index is effective in detection of NHL subtypes and distinguishing them from RLH. The ability to distinguish between monotypic and polytypic lymphoid cell population is considered a major advantage of FCM. The overall accuracy for diagnosis and subclassification of B-cell lymphomas by FCM performed on FNA samples is reported to be 88.4% with a sensitivity of 86% and specificity of 93% (39). Similar concordance (88%) has been reported for FCM performed from excised tissue and subsequent histopathologic diagnoses (2,4,9,10). The sensitivity of FCM for T-cell NHL is poor and reported to be 36.4% (39). FCM may be false negative in large cell NHL and HL. However, the cellular abnormalities in these lesions are easily appreciated on FNA smears and should prompt additional diagnostic studies. FCM may be misinterpreted as polyclonal due to a small fraction of tumor compared to a prominent component of benign/ reactive lymphocytes such as in T-cell lymphomas. When cellularity is limited because of fibrosis, extensive necrosis, or cellular damage, FCM results may be inconclusive (Table 12.6) (2,40). Molecular Analyses Molecular analyses in the diagnosis of lymphoma are performed for the detection of genetic abnormalities such as translocations, deletions or aneuploidy, and gene rearrangement. Sufficient DNA and RNA may be obtained from FNA-derived material for analysis by polymerase chain reaction (PCR), or fluorescence in situ hybridization (FISH) and nucleic acid microarrays/gene profiling techniques. For molecular analyses, specimen can be directly collected into RNA-preserving or extracting solutions or in PreservCyt solution (cell collection and preservation medium for TP [Hologic Inc., Bedford, MA]) that retains both cytologic features and RNA for assessment (36,43,44). These techniques can also be applied to archival cytologic material (TP, alcohol-fixed or formalin-fixed, paraffin-embedded). The results are comparable to those in excision biopsies (36). DNA obtained from FNA samples may be analyzed by PCR for the presence of specific chromosomal translocations, viral genomes, activated or amplified oncogenes, and gene rearrangements. For example, detection 8/5/2013 12:02:01 PM 300 Knowles Neoplastic Hematopathology of t(14;18) (q32;q21) on PCR may provide evidence of a follicular lymphoma (FL) and t(11;14)(q13;q32) evidence for mantle cell lymphoma (MCL) (36,43). In addition, PCR studies on cytology specimens may be used to determine viral load in patients infected with HIV. The pattern of gene rearrangements obtained on analysis of DNA from FNA cytology specimens is comparable to that obtained on excised lymph nodes (30). In an appropriate sample, interphase FISH can exploit intact interphase nuclei and detect structural and numerical chromosomal abnormalities (36,43). DNA microarrays can rapidly provide information on many genes at the mRNA level. It has been possible to use amplified RNA from small FNA samples for gene expression profiling in combination with morphology and immunophenotyping for subtyping of diffuse large B-cell lymphoma (DLBCL). The amount of RNA recovered from FNA has been shown to be comparable to that from a core biopsy (36,41). NON-HODGKIN LYMPHOMA Cytologic subclassification of NHL, particularly of small mature B-cell lymphomas, is controversial and underutilized (2,7,9–11). However, FNA in combination with ancillary tests including ICC, FCM, and/or molecular analyses can be used in the evaluation of NHL (2,4,7,9,13,27,30,36–44). Ninety percent of NHLs are B-cell type, with more than half representing either DLBCL or FL. Some lymphomas have characteristic cytologic appearances, and it may be possible in these cases to render a diagnosis of lymphoma based on cytomorphology alone, at least in general terms. On FNA of most NHL, a monotonous lymphoid cell population with uniform nuclear size and chromatin is evident (Figs. 12.7A–C and 12.9A). Once the monotony of the lymphoid population is appreciated, the initial subclassification into small and large lymphoid cells requires the comparison of the suspect neoplastic lymphoid cells to typical small mature lymphocytes, red blood cells, plasma cells (PCs), or histiocytes (Figs. 12.7A–C and 12.9A). Nuclei of histiocytes can be used as an internal reference to assess the relative size of the lymphoid cells and separate them into small- and large cell types (Figs. 12.6B, C and 12.9B). Careful evaluation of nuclear features including contour, chromatin pattern, and nucleolus aids in further subclassifying lymphoid cells on cytology (Figs. 12.6B, C, 12.7C, and 12.9A and B) (26,27). DIAGNOSTIC CATEGORIES OF FNA FOR HEMATOPOIETIC LESIONS Cytologic diagnostic categories for FNA of hematopoietic and ymphoproliferative lymphoid neoplasms include “atypical l­ lesion,” “atypical lymphoid infiltrate,” “suspicious for lymphoma,” “malignant lymphoma,” or “B-cell lymphoma” (the latter, if immunophenotyping has been performed) (7,25). ­Figure 12.11 outlines an algorithmic approach to evaluating FNA of lymph nodes for appropriate diagnostic categorization. B-Cell Neoplasms Lymphoblastic Lymphoma Lymphoblastic lymphoma (LBL) is of either precursor B- or T-cell differentiation (Table 12.7). It is discussed in the T-Cell and Natural Killer-Cell Lymphoma section. FIGURE 12.11. An algorithmic approach to evaluating FNA of lymph nodes. Enlarge Lymph Nodes FNA Lymphoid Cells Non-lymphoid cells Metastatic carcinoma Reactive Infectious Lymphoma Non-specific Granulomatous Hematolymphoid Non-hematolymphoid Non-granulomatous Primary Orazi9781609136826-ch12.indd 300 Others Lymphocytic component Non-Hodgkin Lymphoma Large cells Melanoma Mixed cell pattern Hodgkin Lymphoma Recurrent Primary Recurrent Small cells 8/5/2013 12:02:02 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms301 Table 12.7 2008 WHO NHL, B-CELL SUBTYPES REVIEWED IN THIS SECTION • Precursor B-cell lymphoblastic lymphoma • Mature B-cell neoplasms • SLL –– CLL/SLL –– LPL –– Plasmacytoma –– Extranodal MZL of MALTtype –– N-MZL –– FL –– MCL • Aggressive B-cell lymphomas –– DLBCL, not otherwise specified –– PBL –– BL Mature B-cell Neoplasms Chronic Lymphocytic Leukemia/ Small Lymphocytic Lymphoma Key Cytologic Features • Monomorphic small lymphocytes • Regular round nuclei, clumped chromatin, small to inconspicuous nucleoli • Scant cytoplasm • Promyelocytes and paraimmunoblasts Clinical Features. Chronic lymphocytic leukemia/small lympho­ cytic lymphoma (CLL/SLL) is a B-cell neoplasm that constitutes about 5% of all NHLs. SLL is regarded as a tissue manifestation of B-cell CLL and often involves lymph nodes. It predominantly occurs in older adults and is more common in men. Patients are usually asymptomatic, but anemia, hepatosplenomegaly, and generalized lymphadenopathy may be present. Patients also have peripheral blood and bone marrow involvement at the time of presentation. Although CLL/SLL is an indolent lymphoma, approximately 5% of cases can transform to a highergrade lymphoma clinically referred to as Richter syndrome or transformation. FNA can be used to evaluate patients with a history of CLL/SLL who are subsequently clinically suspected of having the Richter syndrome (45). Cytology. In CLL/SLL, a predominantly dispersed cell pattern of homogenous population of small lymphocytes that are the same size or slightly larger than a small, mature lymphocyte is evident on smears. The nuclei are round and regular or slightly irregular, with clumped chromatin, small to inconspicuous nucleoli, and scant pale to slightly basophilic cytoplasm (Fig. 12.12A and B). Occasionally, larger lymphocytes representing prolymphocytes and paraimmunoblasts are noted (Fig. 12.12C). These cells have centrally placed smooth nuclei and abundant pale cytoplasm. The prolymphocytes display single and central nucleoli while the paraimmunoblasts contain either multiple, peripherally located nucleoli or a single prominent nucleolus. Mitoses are rare and tingible body macrophages or lymphohistiocytic aggregates are not seen. FIGURE 12.12. Chronic lymphocytic leukemia/small lymphocytic lymphoma. A,B: Homogenous population of small lymphocytes (slightly larger than RBCs) is evident on smears (A, DQ stain, DS and B, Pap stain, DS ×60 objective). C: Nuclei are round and slightly irregular with coarse clumped chromatin, small-to-­inconspicuous nucleoli, and scant basophilic cytoplasm (C, DQ stain DS ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 301 8/5/2013 12:02:04 PM 302 Knowles Neoplastic Hematopathology Tingible (stainable) bodies are the phagocytosed apoptotic cells and cell debris in the macrophage cytoplasm. In cases of Richter syndrome, there are large numbers of blastic cells with round nuclei with vesicular chromatin and prominent nucleoli and scant basophilic cytoplasm (2,15). Phenotype. Positive for CD5, CD23, and Pax5 (Fig. 12.10B) and negative for CD10, FMC-7, and CD79b. CD20 and surface immunoglobulin (sIg), light-chain expression are typically dim. The proliferation index is usually low (<10%) with proliferation marker Ki-67. A proliferation index of >30% may indicate transformation (42). A newer marker LEF-1 is positive in approximately 100% of CLL/SLL (46). A subset of DLBCL and grade 3 FL are also positive for LEF-1 (46). Cytogenetics. Deletion 13q14 (50%), deletion 11q (20%), and trisomy 12 (10% to 15%). 17p deletion is associated with disease progression and increased risk of death and is treated differently (47). Differential Diagnosis. Reactive lymphadenitis and other mature SLLs and large cell lymphomas when there is Richter transformation. Lymphoplasmacytic Lymphoma Key Cytologic Features • Small lymphocytes • Plasmacytoid lymphocytes • Mature PCs with Dutcher and Russell bodies • Mast cells • Epithelioid histiocytes Clinical Features. Lymphoplasmacytic lymphoma (LPL) is an uncommon low-grade B-cell malignancy comprising <2% of all NHL. The disease affects older men. LPL usually presents with bone marrow involvement, splenomegaly, and generalized lymphadenopathy. The clinical course is generally indolent, but transformation to large cell lymphoma occurs in 5% to 10% of cases (48). Cytology. Smears depict a mixed population of small lymphocytes (similar to CLL/SLL) and plasmacytoid lymphocytes. The latter have eccentric nuclei with coarse chromatin and inconspicuous nucleoli. The chromatin, however, is lymphocyte-like and does not demonstrate the “cartwheel” pattern as seen in PCs. Cytoplasm is moderate and basophilic with occasional paranuclear “hof” (large Golgi zone) (Fig. 12.13). Mature PCs containing Russell bodies (cytoplasmic globular eosinophilic immunoglobulin inclusions) and Dutcher bodies (intranuclear immunoglobulin inclusions) are also seen. Occasional multinucleated cells may be present. Mitoses are rare. Increased mast cells and epithelioid histiocytes may be seen (15,49,50). Phenotype. Positive for CD20, Ig light chains, and IgM and usually positive for BCL2 and negative for CD5 (usually), CD10, CD23, Cyclin D1, and BCL6. Lymphoplasmacytoid cells are positive for CD38, and mature PCs are positive for CD38 and CD138. Cytogenetics. Lacks a distinct molecular genetic hallmark. Deletion of 6q21-q23, a nonspecific finding, is the most common aberration reported in 40% to 70% of patients (50). Differential Diagnosis. Distinguishing the LPL from other small cell lymphomas, especially marginal zone lymphoma (MZL) with plasmacytic differentiation, may be problematic. PC neoplasms are also in the differential (50). Orazi9781609136826-ch12.indd 302 FIGURE 12.13. Lymphoplasmacytic lymphoma. Small lymphocytes (similar to CLL/SLL) and plasmacytoid lymphocytes. The latter has eccentric nuclei, lymphocyte-like coarse chromatin, and inconspicuous nucleoli. Cytoplasm shows occasional paranulear “hof” (DQ stain, DS ×60 objective). Plasmacytoma Key Cytologic Features • Mature and immature PCs • Eccentric nuclei, “cartwheel” chromatin • Basophilic cytoplasm, perinuclear “hof” • Some binucleated cells • Dutcher bodies and Russell bodies • Mitosis • Amyloid • Blastic morphology in plasmablastic form • Anaplastic morphology in anaplastic form Clinical Features. PC neoplasms encompass clonal PC pro­ liferations with a wide range of clinical manifestations and behavior. In most cases, PC neoplasms are associated with the production of a monoclonal immunoglobulin, or M protein which is detectable in the serum and urine. PC neoplasms constitute approximately 15% of all hematopoietic neoplasms and are rare before the age of 40. Plasmacytoma is a neoplasm of mature and immature PCs that presents as a discrete tumor mass. They can be multiple osteolytic tumors (multiple myeloma [MM]) or solitary. Solitary or extramedullary plasmacytomas (EMPs) are rare, constituting approximately 3% to 5% of all plasma cell neoplasms (PCN) and have no associated bone marrow or systemic disease. EMP can occur in any organ; however, approximately 90% are found in the head and neck region involving the upper aerodigestive tract. EMP may also present as a metastatic deposit from another soft tissue plasmacytoma or as a consequence of MM. Primary plasmacytoma of lymph nodes is uncommon, and metastasis should be excluded before making this diagnosis (51,52). Cytology. Smears are dominated by PCs, with varying degrees of maturity. These cells are arranged singly and in sheets and clusters. The mature PCs show monomorphic round and eccentric nuclei with condensed “cartwheel” chromatin and indistinct nucleoli. Cytoplasm is abundant and basophilic and shows a perinuclear “hof.” Binucleated cells are usually present (Fig. 12.14A and B). The plasmablastic form has a more blastic morphology with enlarged nuclei and bi- or multinucleation, open chromatin structure, prominent nucleoli, higher N:C ratio, and bare nuclei. Anaplastic plasmacytomas may 8/5/2013 12:02:05 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms303 FIGURE 12.14. Plasmacytoma. A,B: PCs with varying degrees of maturity. Mature PCs show condensed “cartwheel” chromatin. Occasional binucleated forms are seen. Note the crisp nuclear features in the Pap-stained smear (A, DQ stain, DS and B, Pap stain, DS ×100 objective with oil immersion). show considerable pleomorphism and need to be differentiated from DLBCL. Tumor cells may contain Dutcher bodies and Russell bodies. Mitotic rate is high in the pleomorphic types. Extracellular eosinophilic material representing amyloid may be seen in some cases and will show apple-green birefringence with Congo red stain on polarizing light microscopy (51,52). Phenotype. PCs lose many of the surface markers of mature B cells and are frequently negative for CD45 and CD20, but usually express CD79a, CD38, and CD138. The tumor cells synthesize Ig, most commonly of IgA and IgG isotype and show light-chain restriction. Cytogenetics. Translocations involving Ig genes. Many involve the switch region of the immunoglobulin heavy chain gene, consistent with the expression of IgA or IgG. The t(11;14) (q13;q32) occurs in 25% to 30% of myelomas, leading to overexpression of cyclin D1. Differential Diagnosis. MZL and LPL, both of which may have evidence of plasmacytic differentiation, should be considered in the differential diagnosis of PCN. Ancillary tests usually help with this differential. Reactive plasmacytosis is composed of a polymorphous collection of PCs and other inflammatory cells. Marginal Zone B-Cell Lymphoma Key Cytologic Features • Nodal MZL (N-MZL) and extranodal MZL of mucosa-­ associated lymphoid tissue (MALT lymphoma) are ­cytologically similar • Heterogeneous lymphoid cells • Monocytoid B cells • Small-to-intermediate centrocyte-like cells • Plasmacytoid cells (especially in MALT lymphoma) • Occasional immunoblasts • Few PCs • Occasional tingible body macrophages and lymphohistiocytic aggregates • Rare mitoses Clinical Features. MZL is a low-grade indolent B-cell lymphoma that is derived from monocytoid B cells. It is divided into two types, extranodal MZL (MALT lymphoma) and N-MZL. Both Orazi9781609136826-ch12.indd 303 types are morphologically and immunophenotypically similar. N-MZL is rare and has no extranodal or splenic disease. MALT lymphoma constitutes 7% to 8% of all B-cell lymphomas and is more common in older women, but may also occur in children. Up to half involve the gastrointestinal tract, with stomach being the most frequent site. However, other sites, not usually thought of as mucosa associated, can also be involved including salivary glands, thyroid, lung, breast, and urinary bladder. Most MALT lymphomas are associated with a predisposing infectious or autoimmune condition, such as Helicobacter pylori–associated chronic gastritis, Hashimoto thyroiditis, and Sjögren Syndrome (50). Cytology. Smears show a dispersed cell pattern comprising of various proportions of lymphocytes with monocytoid B cells and small-to-intermediate cells with centrocyte-like morphology. The monocytoid B cells are medium-sized lymphoid cells with round, reniform, or indented nuclei, with condensed chromatin and small indistinct nucleoli. Cytoplasm may be scant to abundant, and pale staining or clear. Small- to intermediatesized lymphoid cells contain slightly irregular nuclei and small nucleoli and are thus centrocyte-like (Fig. 12.15A and B). Plasmacytoid cells, scattered immunoblasts, and monoclonal PCs are also seen. The latter are most common in the MALT type. Lymphohistiocytic aggregates are common, while tingible body macrophages may be seen in some cases. Mitoses are rare. MZLs can transform to DLBCL in about 10% of the cases (53–55). Phenotype. Positive for CD19, CD20, CD79a (Fig. 12.15C), and bcl-2 and negative for CD5, CD10, CD23, BCL6, and cyclin D1. A subset is also positive for IgD (53). Cytogenetics. t(11;18) is seen in up to one third of low-grade extranodal MZL and trisomy 3 has been described in both nodal and extranodal MZL (50). Differential Diagnosis. Reactive lymphocyte proliferation and other small B-cell lymphomas should be considered in the differential diagnosis. Cytomorphology, specific phenotypic, and genetic features, such as absence of coexpression of CD19/CD5, seen in SLL/CLL and MCL, cyclin D1 expression in MCL, CD10 expression in FL, and the characteristic t(14;18) translocation involving the BCL2 locus in FL and the t(11:14) translocation in MCL may be helpful in this regard (53). 8/5/2013 12:02:07 PM 304 Knowles Neoplastic Hematopathology FIGURE 12.15. Nodal marginal zone lymphoma. A,B: Dispersed cell pattern comprising various proportions of lymphocytes with monocytoid B cells and small-to-intermediate cells with centrocyte-like morphology (A, DQ stain, DS ×100 objective with oil immersion and B, Pap stain, DS ×60 objective); C: Positive immunostain for CD20 (DS ×60 objective). Follicular Lymphoma Key Cytologic Features • Polymorphous lymphoid cells with centrocytes and ­centroblasts • Lymphoid cell aggregates in one third of cases • Centrocytes (cleaved cells) predominate • Approximately 10% centroblasts (large transformed ­noncleaved cells) • Lymphoglandular bodies (cytoplasmic fragments of ­lymphocytes) • Reactive T lymphocytes • Increasing number of centroblasts with increasing grade • Increased mitoses with increasing grade Clinical Features. FL is a B-cell neoplasm of follicular center cell origin, comprising of two cell types found in normal germinal centers, centrocytes (cleaved cells), and centroblasts (large transformed noncleaved cells). It is a common form of NHL in adults and accounts for about 20% to 40% of cases. Median age at presentation is 55 years with equal sex incidence. The vast majority of cases present with advanced disseminated disease with spleen, bone marrow, and lymph node involvement (33,56,57). Transformation to an aggressive large B-cell lym­ phoma may occur in 25% to 30% and is associated with rapid progression (34,58). The WHO recommends a three-tier grading system (grades 1 to 3) for FLs based on the absolute number of centroblasts Orazi9781609136826-ch12.indd 304 per high-power microscopic field (hpf) in 10 neoplastic follicles on histology (34). Grades 1 and 2 FLs, often combined together, are indolent tumors and may not be treated, whereas grade 3 FLs are aggressive but potentially curable with chemotherapy. Since FL may also have a diffuse growth pattern both The WHO 2008 and REAL classifications also recommend that the degree of follicle formation (predominantly follicular, follicular, diffuse, and predominantly diffuse) should also be reported. Grade 1 has an average of <6, grade 2, 6 to 15, and grade 3 >15 centroblasts/hpf counted in 10 neoplastic follicles. This method of grading system has prognostic implications (34). Cytology. On FNA smears, a loose follicular pattern or dense lymphoid aggregates suggest follicle formation in these lymphomas (Fig. 12.16A). Lymphoid cells are polymorphous and consist of two cell types, the centrocytes and centroblasts (Fig. 12.16B). The predominant cells are centrocytes. These are small- to intermediate-sized lymphocytes (slightly larger than benign lymphocytes) with cleaved nuclei with deep folds in the membrane, occasionally imparting a bilobed appearance. Chromatin is coarsely clumped and nucleoli are inconspicuous. Cytoplasm is scant and pale or lightly basophilic with poorly defined borders (Fig. 12.16C and D). The centroblasts, constituting about 10% of the cells, are large noncleaved lymphocytes (twice the size of benign lymphocytes), with round-to-oval nuclei, with occasional indentation. Chromatin is reticular and nucleoli may be single and central or multiple and peripheral. Cytoplasm is scant and dense basophilic or amphophilic. The nuclear membrane 8/5/2013 12:02:09 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms305 FIGURE 12.16. Follicular lymphoma. A: Loose clusters of small lymphoid cells indicating follicle formation (DQ stain, DS ×40 objective). B: Lymphoid cells are polymorphous with predominant centrocytes with occasional centroblasts (B, DQ stain, DS ×100 objective with oil immersion). C,D: Centrocytes are angulated or cleaved small lymphoid cells with deep nuclear folds (C, DQ stain. DS and D, Pap stain, TP ×100 objective with oil immersion). abnormalities are similar to those identified in histologic sections of small cleaved cell lymphoma, both follicular and diffuse. Small mature reactive T lymphocytes are also seen. Numerous lymphoglandular bodies (clumped cytoplasmic fragments) are present. There are few or no mitoses in low-grade FL (56,57,59). The relative lack of architecture in FNA remains a limitation in grading FL. Cytologic grading may be performed after a morphologic and immunophenotypic diagnosis of FL (57). Methods include counting centroblasts only in clusters resembling follicular structures and evaluating the proliferation index by Ki-67 and DNA image analysis (60) or counting centroblasts, either in 300 lymphoid cells or per 10 hpf in TP slides (61). Grading can also be performed on cell blocks, which may better preserve follicular architecture (57). When the large cells/hpf approach 20% to 50%, the cases may be classified as grade II (mixed small cleaved and large cells) and when the large cells constitute more than 50% of the cells/hpf, the cases may be classified as grade III (variable mixture of large noncleaved cells, large cleaved cells, and occasional immunoblasts) (2,57,58,60). Phenotype. Positive for CD19, CD20, CD79a, CD10, and Bcl-6. Approximately 85% are positive for Bcl-2. CD5, CD23, and CD43 are negative. Cytogenetics. t(14;18)(q32;q21) occurs in 95% of FL (62,63). Orazi9781609136826-ch12.indd 305 Differential Diagnosis. RLH and MCL should be considered in the differential diagnosis of FL grades 1 and 2. Low-grade FL may be indistinguishable morphologically from normal or reactive lymph nodes because of a mixed pattern of small and large lymphocytes. This distinction between reactive hyperplasia and low-grade FL poses a serious obstacle to the use of FNA in the diagnosis of malignant lymphoma. FL must also be differentiated from other small or mixed small lymphomas including MCL. Morphologically, FL tends to be less monotonous and contains a mixture of small and large cleaved and large noncleaved cells, whereas MCL is composed of predominantly small irregular cells. The tumor cells of MCL are characteristically CD5 and cyclin D1 positive. FL-3 needs to be distinguished from DLBCL (62). Mantle Cell Lymphoma Key Cytologic Features • Monotonous small- to medium-sized lymphoid cells • Irregular (centrocyte-like) nuclei • Epithelioid histiocytes • Lymphoid cell aggregates • Rare plasmacytoid lymphocytes • Rare tingible body macrophages • Mitoses 8/5/2013 12:02:12 PM 306 Knowles Neoplastic Hematopathology • Blastoid variant has intermediate to large cells—resemble lymphoblasts • Pleomorphic type has large cells—resemble centroblasts Clinical Features. MCL is an aggressive B-cell lymphoma that is uncommon, constituting approximately 5% to 10% of all NHLs. These tumors mostly occur in older men. MCL is usually widespread at presentation, with generalized lymphadenopathy, hepatosplenomegaly, multiple lymphomatous polyposis within the gastrointestinal tract, and bone marrow involvement. Transformation to an aggressive blastoid variant is frequent (33,34). Cytology. Smears demonstrate a monotonous population of small- to medium-sized lymphoid cells, slightly larger than normal lymphocytes. Nuclei resemble centrocytes and are oval and irregular containing dispersed mature chromatin and inconspicuous nucleoli. Cytoplasm is scant and mildly basophilic (Fig. 12.17A and B). The cell proliferation is homogeneous, without the presence of larger cells with prominent nucleoli. Epithelioid histiocytes with large oval nuclei and abundant eosinophilic cytoplasm are commonly present. Lymphoid cell aggregates are seen in one third of the cases. Plasmacytoid lymphocytes and tingible body macrophages are rare. Mitoses may be identified (53,64). In the blastoid variant of MCL, the cells resemble lymphoblasts and are medium to large with irregular nuclei containing finely granular chromatin and multiple irregular nucleoli. The mitotic and apoptotic rate is high (Fig. 12.17C and D). Terminal deoxynucleotidyl transferase (TdT) is negative (65). The pleomorphic type has large cells which resemble centroblasts. Phenotype. Positive for pan B-cell antigens CD19, CD20, and PAX5. MCL is also positive for CD79a, CD5, and FMC7 and negative for CD10, BCL6, and CD23. The tumor cells express monotypic sIg, with lambda light-chain restriction being more common. Almost all show nuclear positivity for cyclin D1 that provides a specific marker for MCL (66). SOX11, a transcription factor for CNS development, is positive in >95% of MCL. It is also found in Burkitt lymphoma (BL) and LBL and some grade 3 FL. SOX11 is not found in other small B-cell lymphomas (67). Cytogenetics. MCL are characterized by t(11;14)(q13;q32) resulting in BCL1 gene rearrangement with characteristic overexpression of cyclin D1 in >95% of cases (47). In B-cell NHL, cyclin D1 overexpression is limited to MCL and provides a useful marker for this tumor (66). Differential Diagnosis. Includes other small cell lymphomas such as CLL/SLL, low-grade FL, and MZL. This differential is important since MCL has a relatively worse prognosis. Immunophenotyping may be critical in this differential. CLL/SLL is CD23 positive and FL is CD10 and BCL6 positive. Difficulty in diagnosing MCL can result from aberrant phenotypes. Positivity FIGURE 12.17. Mantle cell lymphoma. A,B: Homogeneous population of small to medium-sized lymphoid cells with oval and irregular nuclei, dispersed mature chromatin, inconspicuous nucleoli, and scant and mildly basophilic cytoplasm (A, DQ stain, DS and B, Pap stain, DS ×60 objective). C,D: Blastoid variant with lymphoblast-like cells showing open coarsely granular chromatin (C, DQ stain, DS and D, H&E-stained cell block ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 306 8/5/2013 12:02:16 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms307 for SOX11 may be helpful in the rare cases of CD5-negative/ equivocal or negative cyclin D1 MCL and CD5-positive MZL (67). Diffuse Large B-Cell Lymphoma, Not Otherwise Specified Key Cytologic Features • Monotonous population of large cells • Several morphologic subtypes • Centroblastic • Immunoblastic • T cell rich • Anaplastic • Epithelioid histiocytes and tingible body macrophages • Necrosis, mitoses • Artifacts of smearing Clinical Features. DLBCL is characterized by a variety of morphologic and clinical characteristics, suggesting an underlying pathogenetic heterogeneity. DLBCL is a common subtype of aggressive but potentially curable NHL that constitutes approximately 30% of adult lymphomas. It can occur at any age including childhood. Primary extranodal disease may be present. Lymph nodes are also frequently involved. Most cases of DCLBL arise de novo, while some cases represent transformation of a pre-existing low-grade lymphoma. DLBCL may also occur in patients with immunodeficiencies such as AIDS or may represent a post-transplant lymphoproliferative disorder (59,68). Cytology. DLBCL has a variable morphology. Smears of DLBCL show a dispersed pattern of monotonous cells (Fig. 12.9A). Usually, the smears are moderately cellular and recognizable as abnormal due to the presence of large atypical. Morphology may vary with the specific subtype—centroblastic, immunoblastic, or anaplastic. The centroblastic type is most common. It shows a preponderance of cells with medium-to-large cells with round-to-oval nuclei with distinct smooth or irregular contours, vesicular chromatin, and multiple prominent nucleoli, often peripheral. Cytoplasm is scant basophilic and may show vacuoles (Fig. 12.18A and B). There may be admixed immunoblasts. The immunoblastic type is composed predominantly of immunoblasts (>90%). Immunoblasts are larger than centroblasts, have smooth round or oval nuclei, and single central prominent nucleoli, a characteristic feature of this subtype. Cytoplasm is abundant pale or clear to intensely basophilic and may displace the nucleus eccentrically, imparting a plasmacytoid appearance (Fig. 12.18C and E). Cells of this type are seen in a large proportion of centroblastic lymphomas. Anaplastic type shows large, occasionally multinucleated pleomorphic cells (Fig. 12.18F and G). In the T-cell–rich type, small mature T cells dominate the smears with a variable FIGURE 12.18. Diffuse large B-cell lymphoma. A,B: Centroblastic type morphology with medium-to-large cells tumor cells, round-to-oval nuclei with smooth or irregular contours, and basophilic cytoplasm with small vacuoles. Nucleoli are more obvious in the Pap-stained DS (A, DQ stain, DS and B, Pap stain, DS ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 307 8/5/2013 12:02:19 PM 308 Knowles Neoplastic Hematopathology FIGURE 12.18. (Continued) C–E: Immunoblastic type with larger cells, smooth round or oval nuclei with single central nucleoli, and intensely basophilic cytoplasm. Note the nuclear features in the Pap-stained DS and TP (C, DQ stain DS; D, Pap stain, DS and E, Pap stain, TP ×100 objective with oil immersion). F,G: Anaplastic type showing pleomorphic cells (F, DQ stain, DS ×60 objective and G, Pap stain, TP ×100 objective with oil immersion). H: Smearing may induce cellular artifacts such as bare nuclei with many lymphoglandular bodies (cytoplasmic fragments) (DQ stain, DS ×60 objective). I: Poorly differentiated carcinoma may mimic DLBCL. Note the vague syncytial arrangement of tumor cells, nonhmatolymphoid chromatin, and absence of lymphoglandular bodies (DQ stain, DS ×60 objective). admixture of histiocytes. Large tumor cells are scattered and constitute <10% of all cells. All subtypes show variable numbers of epithelioid histiocytes and tingible body macrophages. Cells of DLBCL are fragile. Smearing may induce artifacts such as loss of cytoplasm, which appears as lymphoglandular bodies, and resultant distorted bare nuclei (Fig. 12.18H). Poorly differentiated carcinoma (PDCa) cells may mimic DLBCL (Fig. 12.18I). Phenotype. Cells of DLBCL express CD45 and B-cell markers CD20 and CD79a. Most DLBCL also express surface or Orazi9781609136826-ch12.indd 308 cytoplasmic Ig. The anaplastic variant expresses CD30. DLBCL of centroblastic morphology frequently express CD10, indicating a follicular center cell derivation. Expression for BCL6 may also be seen. Large cell lymphomas have a falsenegative or nondiagnostic rate of approximately 27% by FCM analyses. Possible causes of such a high rate include small sample size, necrosis, or cell fragility (7,69,70). Cytogenetics. Frequent molecular characteristics are 3q27 break involving BCL6 gene in 30%, BCL2 t(14;18) in 25%, and MYC rearrangement in 10%. The latter may make it difficult to 8/5/2013 12:02:22 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms309 distinguish DLBCL from Burkitt (34). Clonal rearrangement of Ig heavy- and light-chain genes is also seen. Differential Diagnosis. Tumor cells in the T-cell–rich subtype and the anaplastic subtypes of DLBCL may resemble RS cells. Other entities that should be considered in the differential diagnoses include FL-3, blastoid variant of MCL, BL, and PDCa (Fig. 12.18I). Immunophenotyping will aid in the differential (33,70,71). Primary Mediastinal (Thymic) Large B-Cell Lymphoma Key Cytologic Features • Monotonous large neoplastic cells • Enlarged irregular nuclei, granular chromatin, nucleoli • Pale blue cytoplasm with distinct outer border • High N:C • Lymphoglandular bodies • Mitoses Clinical Features. Primary mediastinal large B-cell lymphoma (PMBL), a unique subtype of DLBCL, is rare. It arises in the thymus, the cell of origin is most likely the CD19+/CD21− thymic B cell normally found clustering around Hassall corpuscles. The disease usually affects young women and displays a unique combination of clinical, histologic, immunologic, and cytogenetic features. Patients commonly present with a rapidly enlarging mass in the mediastinum that infiltrates surrounding structures and causes compression symptom including superior vena cava syndrome. It often involves the lungs and may eventually metastasize to other organs. Bone marrow involvement is uncommon at diagnosis. FNA is usually part of the initial workup of the patient. Cytology. Smears show singly dispersed, highly atypical large- to-intermediate, round-to-oval tumor cells. Nuclei are round and eccentrically located with prominent nucleoli (plasmablastic differentiation). The cytoplasm is scant to moderate in amount, densely basophilic with occasional fine vacuoles and distinct cell borders (Fig. 12.19A). Some cells are binucleated or multinucleated (Fig. 12.19B). Plasmacytoid morphology is more evident on air-dried DQ-stained slides (58,73,74). Phenotype. Plasmablastic differentiation is confirmed by diffuse and strong positivity for PC markers CD38, CD138, MUM1, and PRDM1/Blimp-1. Lymphocytic and B-cell marker CD79a is positive (50% to 85%), while others including CD45 and CD20 and PAX5 are negative. EBER is positive and EBV LMP1 (Latency Pattern 1) is negative. The proliferation index with Ki-67 immunochemistry approaches 100% (35). Cytogenetics. Clonal Ig kappa light-chain gene rearrangement (73). Differential Diagnosis. Plasmablastic myeloma must be distin­ guished from PBL because of the different clinical management pathways. Typically, the presence of serum paraprotein and/ or lytic bone lesions in older patients favors MM. However, widely disseminated bone disease and monoclonal serum Ig have been described in PBL and could lead to major confusion with MM. Although PBL and MM have nearly identical Cytology. Smears show a monotonous population of atypical lymphocytes, with predominance of large cells. The nuclei are enlarged (>5 times the size of a normal lymphocyte), irregular, cleaved or noncleaved, and lobulated, with coarsely granular chromatin and occasional prominent nucleoli. Cytoplasm is pale blue, scant to moderate in amount, and forms a narrow paleto-clear rim with a distinct cell border. Nuclear-to-cytoplasmic ratio is high. Lymphoglandular bodies and mitoses are present (72). FNA of primary DLBCL of the mediastinum may show low cellularity due to sclerosis (69,72). Phenotype. Distinct phenotype includes weak and nonhomogenous positivity for CD30 in 80% and CD23 positivity in 70% of cases. Expression of surface and cytoplasmic Ig is often absent as is CD21 expression. BCL6 mutations and BCL2 gene rearrangement are lacking. Differential Diagnosis. Includes mediastinal involvement with peripheral DLBCL, HL, anaplastic large cell lymphoma (ALCL), thymoma, and carcinoma. PMBL can be distinguished from these entities by ICC, FCM, and molecular features. Plasmablastic Lymphoma Key Cytologic Features • Large tumor cells • Round, eccentrically located nuclei, nucleoli • Occasional bi- or multinucleated cells • Basophilic or clear cytoplasm with distinct borders Clinical Features. Plasmablastic lymphoma (PBL) is an uncommon aggressive Epstein-Barr virus (EBV)–associated lymphoma of the oral cavity, which is usually but not always associated with HIV. Primary PBL may also occur at other extraoral sites, predominantly in the gastrointestinal tract and lung (73). Rarely, PBL may also occur in HIV-negative immunodeficient and immunocompetent individuals. Such cases are more common in lymph nodes. Orazi9781609136826-ch12.indd 309 FIGURE 12.19. Plasmablastic lymphoma. A,B: Singly dispersed atypical tumor cells with plasmablastic differentiation; some cells are bi- or multinucleated (A, DQ stain, DS ×100 objective with oil immersion and B, DQ stain, DS ×60 objective). 8/5/2013 12:02:24 PM 310 Knowles Neoplastic Hematopathology immunophenotypic profiles, CD56 positivity, occasionally cyclin D1 positivity, and a relatively lower Ki-67 can help identify secondary extramedullary plasmablastic MM (58). Burkitt Lymphoma Key Features • Monomorphic medium-sized tumor cells • Round nuclei, clumped chromatin, small nucleoli • Deeply basophilic cytoplasm with small clear vacuoles • Tingible body macrophages in a “starry sky” pattern • Mitoses and apoptosis Clinical Features. BL is an aggressive mature B-cell lymphoma that may occur in extranodal sites. There are three major subtypes of BL—endemic, sporadic, and immunodeficiency associated. These subtypes of BL have similar morphology but differ clinically and biologically. Endemic BL occurs in equatorial Africa in areas of endemic malaria, strongly associated with the EBV (95%) (75). It commonly occurs in children, 4 to 7 years old, and affects mandible, gonads, and kidney. It is the most common childhood malignancy in Africa. Sporadic BL is the most common NHL in children and young adults in the developed countries. It commonly presents as an intra-abdominal tumor. Lymphoid tissue of Waldeyer ring may also be involved. Immunodeficiencyassociated BL is often associated with HIV infection and may present with nodal and extranodal disease with bone marrow involvement. BL is a fast-growing bulky disease. All types have a high risk of CNS, ovary, breast, and kidney involvement. The EBV genome is present in the neoplastic cells in all cases of endemic BL. EBV is detected in approximately 33% of sporadic and immunodeficiency-associated BL (75). Cytology. Smears show a largely monomorphic population of medium-to-large tumor cells. These cells bear round and uniform nuclei with occasional clefts or indentations, clumped chromatin, multiple small central nucleoli, and moderate amount of deeply basophilic and vacuolated cytoplasm (Fig. 12.20A). Similar cytoplasmic vacuoles can be seen in DLBCL (Fig. 12.18A). Numerous tingible body macrophages impart a “starry sky” pattern (Fig. 12.20B and C). Mitotic rate is brisk. Background looks “dirty” due to individual cell necrosis (apoptosis) (76). Some cases of BL may show tumor cells with plasmacytoid features, particularly in immunodeficiency-associated BL, or nuclear pleomorphism with more prominent nucleoli. Phenotype. Tumor cells express light-chain restriction and ger­minal center phenotype expressing CD10 and BCL6. Pro­ liferation index is high with nearly 100% positivity with Ki-67. Cells are negative for CD5, CD23, TdT, and bcl-2. Cytogenetics. t(8:14) in 90%. EBV genome can be demonstrated in all endemic BL and approximately 30% to 40% of other subtypes. Differential Diagnosis. Includes DLBCL and childhood small round blue cell tumors. These can be distinguished by immunostains and cytogenetic findings (77). T-Cell and Natural Killer–Cell Lymphoma T-cell lymphomas, which are more common in Asia, are a heterogeneous group of lymphomas with diverse morphology. In the United States, they are much less common than B-cell lymphomas and constitute about 10% to 20% of all NHL. T-cell lymphomas are derived from post-thymic or mature T cells at different FIGURE 12.20. Burkitt lymphoma. A: Monomorphic medium-to-large tumor cells with round nuclei with occasional clefts and clumped chromatin. Note the small clear lipid-containing cytoplasmic vacuoles (DQ stain, DS ×100 objective with oil immersion). B,C: Tingible body macrophages impart a “starry sky” pattern (B, DQ stain DS ×100 objective with oil immersion and C, Pap stain, TP ×60 objective). Orazi9781609136826-ch12.indd 310 8/5/2013 12:02:26 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms311 stages of differentiation and are divided into two broad categories in the WHO classification—precursor T-cell LBL and mature T-cell and natural killer-cell lymphomas. T-cell lymphomas have a poorer prognosis and response to treatment compared to B-cell lymphomas. The section will cover only those entities that may be encountered on FNA including precursor T-cell LBL/leukemia, PTCL (unspecified and angioimmunoblastic), and ALCL. rearrangements. T-LBL almost always has T-cell receptor gene rearrangements. Precursor B- and T-Cell Lymphoblastic Lymphoma/ Leukemia (B- and T-LBL) Peripheral T-Cell Lymphoma Unspecified (PTCL, NOS), Including Angioimmunoblastic T-Cell Lymphoma Key Cytologic Features in B- and T-LBL Key Cytologic Features • Small- or intermediate-sized blasts • Round or highly convoluted nuclei, distinct nucleoli, delicate blastlike chromatin • Scant-to-moderate amount of nongranular cytoplasm with frequent protrusions • Tingible body macrophages • Numerous mitoses Clinical Features. Precursor T-cell LBL/leukemia are composed of precursor B or T cells and involve the bone marrow and peripheral blood occasionally accompanied by primary nodal or extranodal site involvement. The neoplasm is rare. It occurs in all age groups, but has a relatively high incidence in children and young adults. B-LBL is most common in children and may present with skin nodules, bone lesions, and lymphadenopathy. T-LBL most frequently presents as symptomatic mediastinal mass with pleural and pericardial effusions and subdiaphragmatic lymphadenopathy. Both have coexistent leukemic involvement (78). Cytology. Smears contain small or intermediate-sized blasts with round-to-convoluted nuclei with delicate blastlike chromatin, distinct nucleoli, and scant-to-moderate weakly basophilic non­ granular cytoplasm (Fig. 12.21). Numerous mitoses are present. Tingible body macrophages may be present (79). Phenotype. Lymphoblasts in both B- and T-LBL are positive for TdT. The T-LBL is positive for T-cell antigens CD2, CD3, CD5, CD7, and CD1a and the B-LBL is positive for B-cell antigens CD19, CD79a, and PAX5. Cytogenetics. B-LBL show clonal but unmutated rearrange­ ments of Ig genes, two thirds show clonal Ig heavy-chain FIGURE 12.21. Precursor T-cell LBL displays intermediate-sized blasts with nuclear irregularities (DQ stain, DS ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 311 Differential Diagnoses. Include BL and blastoid variant of MCL. However, T-LBL is distinguished from B-cell lymphomas due to absent B-cell markers and positivity for CD7 and other T-cell markers. • Small, intermediate and large lymphocytes • Irregular nuclei, nucleoli • Pale-staining cytoplasm • Epithelioid histiocytes, PCs, and eosinophils • Mitoses • Reed-Sternberg (RS)–like cells Clinical Features. PTCL is rare and constitutes <10% of all NHL in the Western countries. It is primarily a disease of adults with no sex predilection. Clinically, PTCL is a more aggressive form of NHL. It is a heterogeneous group of tumors with variable clinical presentation, morphologic appearance, and prognosis. Patients commonly present with pruritus, lymphadenopathy, and extranodal disease (80,81). Cytology. PTCL most commonly shows a polymorphous pattern with variable admixture of small, intermediate, and large neoplastic cells. Percentage of large cells may range from 20% to 90%. Smears in PTCL appear to be monomorphous when one cell type predominates. The nuclei vary considerably in size and exhibit significant membrane irregularities with protrusions and indentations. Nucleoli may be present. Cytoplasm is scant to moderate in amount, pale to basophilic, and has well-defined borders (Fig. 12.22). Mitoses are numerous. Epithelioid histiocytes, eosinophils, and PCs may be seen. Occasionally, scattered large cells with vesicular nuclei and prominent nucleoli, resembling RS-like cells, may be observed (80,81). Phenotype. Neoplastic cells express T-cell phenotype including CD2, CD3, CD4, CD5, CD7, CD8, CD43 and CD45RO and are FIGURE 12.22. PTCL shows large neoplastic cells with variably-sized nuclei with membrane irregularities and scant cytoplasm (DQ stain, DS ×60 objective). 8/5/2013 12:02:28 PM 312 Knowles Neoplastic Hematopathology negative for B-cell antigens. The RS-like cells may have similar phenotype to RS-cells in HL with CD20, CD30 and occasionally CD15 positivity. Cytogenetics. Clonal rearrangement of T-cell receptor genes is seen. Differential Diagnoses. Includes reactive hyperplasia, HL, ALCL and DLBCL. A combination of cytomorphologic criteria, immun­ ophenotyping and molecular analyses are useful to distinguish PTCL from these entities. Anaplastic Large Cell Lymphoma Key Cytologic Features • Three variants: common, small cell and lymphohistiocytic types • “Hallmark” cells: large with irregular horseshoe-shaped nuclei, prominent nucleoli, • “Doughnut” cells: multiple nuclei arranged in a “wreathlike” pattern • RS-like cells • Histiocytes • PCs • Erythrophagocytosis • Necrosis and inflammation • Mitoses and apoptosis Clinical Features. Ki-1 (CD30)-positive ALCL is a rare T-cell lymphoma. ALCL can have diverse clinical, histologic and cytologic presentation. It is divided into morphologically indistinct but clinically distinct ALK-positive (ALK+) ALCL and ALK-negative (ALK−) ALCL according to the presence or absence of ALK protein. ALK+ ALCL is more common in children and young men. It involves both lymph nodes and extranodal sites (skin, bone, soft tissue, lungs, liver). ALK− ALCL tends to occur in older patients with a lower male to female ratio and exhibits immunophenotypic heterogeneity. Response to treatment and prognosis of ALK+ ALCL patients is comparatively better than in ALK− ALCL and other PTCL (82,83). Cytology. ALCL shows a broad morphologic spectrum which makes it difficult to make a definitive diagnosis on FNA (82). The three distinct morphologic variants are the common large cell and the less common lymphohistiocytic and small cell patterns. The “hallmark” cells, so-called because they constitute a hallmark of ALCL, are seen in all variants. These are large pleomorphic cells with eccentric lobulated (horseshoe-shaped or kidney-shaped) nuclei, finely granular chromatin, multiple basophilic nucleoli and abundant basophilic or clear cytoplasm. Usually a prominent perinuclear clear “hof,” corresponding to the Golgi region is evident (Fig. 12.23A) (83). The other notable cells are the “doughnut cells” which are multinucleated giant cells, with nuclei arranged in a wreathlike pattern close to the cytoplasmic border (Fig. 12.23B). RS-like cells are also present. Background shows reactive lymphocytes, histiocytes, and PCs (Fig. 12.23C). Erythrophagocytosis can occasionally be seen. Necrosis, mitoses, and apoptosis are frequent. The small cell variant shows medium-sized neoplastic cells with clear FIGURE 12.23. Anaplastic large cell lymphoma. A: “Hallmark” cell with eccentric lobulated, horseshoe-shaped, or kidney-shaped nucleus (Pap stain, DS ×100 objective with oil immersion). B: “Doughnut” cell with nuclei arranged in a wreathlike pattern (DQ stain, DS ×100 objective with oil immersion). C: Background shows reactive lymphocytes. Compare the size of the neoplastic cells with the benign lymphoid cells (Pap stain, DS ×60 objective). Orazi9781609136826-ch12.indd 312 8/5/2013 12:02:30 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms313 cytoplasm and distinct cell membranes. Nuclei are irregular with clumped chromatin resembling the horseshoe-shaped nuclei of the classical “hallmark” cells. The lymphohistiocytic variant contains similar small cells admixed with abundant pale histiocytes (82). Immunocytochemistry. Positive for ALK, CD30, EMA, CD45, and one or more T-cell markers including CD2 and CD5. Cytogenetics. T-cell receptor gene rearrangements, translocation in >80% of ALK+ ALCL cases. t(2;5) Differential Diagnosis. Includes other large cell lymphomas, anaplastic carcinoma, melanoma and HL. These tumors can be distinguished based on morphology and ICC. Caution should be exercised in interpreting positive EMA stain in a specimen with carcinoma-like features as EMA is also a characteristic marker for ALCL. ALCL and HL have overlapping morphologic and ICC features. Careful evaluation of the latter two features and clinical presentation would be helpful (84). HODGKIN LYMPHOMA WHO 2008 Classification of Hodgkin Lymphoma • Classical HL • Nodular sclerosis classical HL • Mixed cellularity classical HL • Lymphocyte-rich classical HL • Lymphocyte-depleted classical HL • Nodular lymphocytic predominant HL HL is a relatively uncommon form of lymphoma (∼10% to 20%). The two distinct groups are the classical (CHL) and the nodular lymphocytic predominant Hodgkin lymphoma (NLPHL) types. These two groups differ in their epidemiology, clinical features, phenotype, genetics, and association with EBV but share RS cells and its variants. CHL includes four subtypes: nodular sclerosis (NSCHL), mixed cellularity (MCCHL), lymphocyte rich (LRCHL) and lymphocyte depleted (LDCHL) (85). The role of FNA as a sole diagnostic modality in HL is controversial; however, FNA can be reliably used in the diagnosis of recurrent HL. A cytologic diagnosis of HL is dependent on the recognition of RS cells. Diagnostic RS cells may or may not be easy to identify on FNA, depending on the histopathologic type of HL. On FNA, the diagnostic accuracy of HL, not otherwise specified, is >90%, but the accuracy of subtyping the disease is lesser (86,87). However, accurate subtyping, as per WHO 2008, is not considered crucial for management purposes. Rarely, RS cells are seen in the absence of HL (88). FNA of HL may be false-negative due to sampling error or fibrosis. When the findings on FNA do not correlate with the clinical and radiologic impression, repeat FNA or histologic biopsy should be performed (89,90). Key Cytologic Features • Classical HL • NSCHL may show low cellularity due to fibrosis • Characteristic cells are classic RS cells or its variants (Hodgkin cells) • Background of inflammatory cells in NSCHL and MCCHL • Nodular lymphocytic predominant HL • Characteristic cell are LP or “popcorn” cells • Background shows small and large lymphocytes • Histiocytes and PCs Orazi9781609136826-ch12.indd 313 Classical HL Clinical Features. Classical HL accounts for >95% of all HL and shows a bimodal age distribution—younger and older age groups with a male to female ratio of 2:1. Cervical lymph nodes are the commonest site of presentation followed by mediastinal, axillary, and inguinal lymph nodes. The spleen is involved in a minority of cases. Other extranodal sites are uncommon except in late stages. EBV infection is seen in 40% of CHL, with the highest incidence in patients with AIDS. NSCHL is the commonest subtype accounting for 70% of cases, primarily affects young people, and shows a female predominance. The mediastinum is involved in the majority of cases and more than one half of patients present with stage II disease (86,87). MCCHL constitutes about 20% of cases, while LRCHL and LDCHL types are rare; the former constitute <5% of all CHL and the latter <5% in the Western countries. MCCHL and LDCHL have overlapping epidemiologic, clinical, and biologic features; both are more common in developing countries, are most commonly associated with HIV infection, and commonly involve peripheral lymph nodes and bone marrow. MCCHL shows a bimodal age distribution while LDCHL is more common in the elderly. These three subtypes of CHL show a male ­predominance (85). Cytology. The smears often show low cellularity in NSCHL due to sclerosis. Small- to medium-sized lymphoid cells, eosinophils, and other inflammatory cells with scattered, RS cells or their mononuclear cell variants, the Hodgkin (H) cells, are present (Fig. 12.24A and B). Classic RS cells are large, three to four times the size of small lymphocytes and are binucleate or have a bilobed nucleus with prominent eosinophilic nucleoli (often occupying 25% of the nuclear diameter), giving the cells an “owl-eyed” appearance. Cytoplasm is moderate and basophilic (Fig. 12.24C–E). The RS variant, Hodgkin cell, has a large nucleus, distinct nucleolus, and abundant pale-blue cytoplasm (Fig. 12.24F). The nuclei may be irregular and polylobated. If diagnostic RS cells are identified in the appropriate polymorphous, dispersed population, the diagnosis of HL may be rendered (Fig. 12.24A). In MCCHL, H/RS cells are seen in a background of small- to medium-sized lymphoid cells, some centroblasts, eosinophils, PCs, neutrophils, and epithelioid histiocytes with occasionally granulomas. In some cases of MCCHL, granulomatous inflammation may dominate the smear and obscure the diagnostic cells. Smears of LRCHL show H/RS cells in a background showing a spectrum of lymphoid cells without eosinophils or histiocytes. In LDCHL, H/RS cells dominate the smear (35). Immunocytochemistry. CD15 and CD30 are positive (Fig. 12.24G and H) and EMA, CD45, and usually CD20 are negative. Positivity for EBV will be seen in EBV-associated cases. Differential Diagnosis. Difficulties encountered in the diagnosis of HL are attributable to overlapping features of RS cells and a variety of benign and malignant cells. These RS cell mimics or RS-like cells may be seen in large cell NHL (ALCL, T-cell– rich B-cell lymphoma, PTCL), carcinoma (breast, gastric, and nasopharyngeal), melanoma, sarcoma, germ cell tumor, infectious mononucleosis (IM), and RLH (86,87). ALCL and PTCL sometimes show large cells with large nuclei and prominent nucleoli that resemble RS cells. Nuclei in ALCL show prominent nuclear contour irregularities and cells are negative for CD15. p63 protein may be used as a potential tool in the differential diagnosis between ALCL and CHL. p63 is frequently expressed in a subset of ALCL cases while HL has shown to be negative (89). Gene rearrangement studies can be used to distinguish RS cells from T-cell lymphomas (90). The occasional bizarre cells of nasopharyngeal carcinoma (NPC) may mimic RS cells. Melanoma occasionally shows large, atypical cells that may mimic RS cells. MCCHL may be mistaken for RLH if diagnostic RS cells are sparse or not noticed (12). 8/5/2013 12:02:30 PM 314 Knowles Neoplastic Hematopathology A B C D E F G H I J FIGURE 12.24. Hodgkin lymphoma. Classical (CHL) in (A,B) shows a mixture of small and large lymphoid cells with scattered ReedSternberg (RS) cells (A, DQ stain, DS and B, Pap stain, DS ×60 objective). C,D: Diagnostic RS cells, also known as “owl-eyed” cell with “mirror image” nuclei (C, DQ stain, DS and D, Pap stain, DS ×100 objective with oil immersion). E: Classic binucleated RS cell in an inflammatory background (DQ stain, DS ×100 objective with oil immersion). F: Mononuclear variant of RS cell (Hodgkin cell). Note the eosinophil and benign lymphoid cells (DQ stain, DS ×100 objective with oil immersion). G,H: Positive ICC for CD15 and CD30 (G and H, TP ×100 objective with oil immersion). NLPHL in (I,J) shows LP (popcorn) cell with multilobed nucleus and prominent nucleoli (I, DQ stain, DS and J, Pap stain, DS ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 314 8/5/2013 12:02:40 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms315 Nodular Lymphocytic Predominant HL Clinical Features. NLPHL is rare accounting for <5% of all HL. It differs from CHL in its clinical, epidemiologic, pathologic, immunophenotype, and genetic features. It has a male predominance and peaks in the fourth decade. The majority of patients present with lymphadenopathy in the cervical, axillary, or inguinal regions. NLPHL is rarely associated with EBV. It is has a good prognosis even though recurrence is common (91). Cytology. The LP cells are sparse and may be difficult to find on FNA smears. The nuclei are folded or multilobated with fine chromatin and distinct nucleoli (Fig. 12.24I and J). Classical RS cells are not seen in NLPHL. The background shows small and large lymphocytes. Histiocytes, singly or in clusters, and PCs may be seen. Eosinophils and neutrophils are not present (91). Immunocytochemistry. The neoplastic cells of NLPHL are B cells and express CD45, CD20, CD79a, and BCL6. They are also positive for B-cell transcription factors PAX5, OCT2, and BOB-1 and negative for CD30 and CD15. Genetics. Monoclonal rearrangements of the Ig genes. Differential Diagnosis. Includes CHL and T-cell–rich B-cell lymphoma (TCRBCL). CHL shows positivity for CD30 and CD15. NLPHL is morphologically and immunophenotypically similar to TCRBCL, and the differential diagnosis between the two is controversial and a difficult task (97). Other entities such as PTCL may need molecular studies to distinguish from NLPHL (33). HISTIOCYTIC AND DENDRITIC CELL NEOPLASMS Dendritic cells are antigen-presenting cells. Their main function is to process antigen material and present it on the surface to other cells of the immune system. Dendritic cells include Langerhans cells (on the skin), interdigitating dendritic cells (IDDCs) (in the lymph node), and follicular dendritic cells (FDCs) (in lymph node follicle). Neoplasms of dendritic cells are rare. Langerhans cell histiocytosis (LCH) usually affects children between 1 and 15 years old and is traditionally divided into three groups: unifocal, multifocal unisystem, and multifocal multisystem. The key to diagnosing LCH is the identification of the characteristic nuclear features of Langerhans cells, FIGURE 12.25. A: Smear from a case of Langerhans histiocytosis showing large neoplastic cells with elongated grooved nuclei, prominent nucleoli, and light blue cytoplasm. Note the eosinophils in the background (DQ stain, DS ×100 objective with oil immersion). Courtesy of Stephan Papmbuccian, MD, Department of Pathology, University of Minnesota Medical Center, Minneapolis, MN. B: Dermatopathic lymphadenitis shows histiocytes containing melanin pigment, Langerhans cells, and scattered lymphocytes (Pap stain, DS ×60 objective). C: Rosai-Dorfman disease shows a histiocyte with engulfed PCs (Pap stain, DS ×60 objective). Both (B,C) courtesy of Ricardo Bardales, MD, Department of Pathology, Mercy General Hospital, Sacramento, CA. D: FDC sarcoma shows spiderweb-like network of thin, radiating, multipolar processes interconnecting single tumor cells (Ultrafast stain, DS ×60 objective). Courtesy of Grace Yang, MD, Department of Pathology & Laboratory Medicine, Weill Cornell Medical Center, New York, NY. Orazi9781609136826-ch12.indd 315 8/5/2013 12:02:43 PM 316 Knowles Neoplastic Hematopathology which usually are admixed with numerous eosinophils. Langerhans cell nuclei have a folded, indented, or grooved appearance, generally with a fine chromatin pattern, inconspicuous nucleoli, and a thin nuclear membrane (Fig. 12.25A). Dermatopathic lymph nodes may contain numerous Langerhans cells and eosinophils; therefore, dermatopathic lymphadenitis is in the cytologic differential diagnosis (Fig. 12.25B). FNA in sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) shows large histiocyte-like cells with abundant pale, eosinophilic cytoplasm containing well-preserved lymphocytes and occasional PCs and granulocytes. The diagnosis can be supported by the demonstration of S-100 protein in the large cells (Fig. 12.25C) (92). IDDCs sarcoma predominantly occurs in adults. Morphologically, IDDCs have a folded nucleus, in contrast to FDC sarcoma, which appear to have an elongated nucleus. On electron micro­scopy, IDDCs have long and fine cytoplasmic extensions that intermingle with similar cells. In contrast to FDCs, they lack desmosomes, and in contrast to Langerhans cells they lack Birbeck granules. Immunostains for S-100 and CD1a are p ­ ositive. FDC sarcoma also predominantly occurs in adults. On FNA, the smears are cellular and show cells in syncytial fragments in addition to a prominent single-cell population. The nuclei are round to oval and moderately pleomorphic with vesicular chromatin, small nucleoli, occasional grooves, and pseudoinclusions. Cytoplasm is abundant, eosinophilic, and shows spiderweb-like network of thin, radiating, multipolar processes interconnecting single tumor cells (Fig. 12.25D). Delicate cytoplasmic strands are also seen in the small syncytial fragments, sprinkled with small lymphocytes. Positive immunostaining for CD21, CD23, and CD35 confirms the diagnosis (93). Benign Conditions that Mimic Lymphoma Reactive Lymphoid Hyperplasia Key Cytologic Features • Dispersed polymorphous lymphoid cells • Predominantly small mature lymphocytes, centrocytes, and centroblasts • Immunoblasts • PCs, eosinophils, neutrophils • Tingible body macrophages, • Lymphohistiocytic aggregates • Mitoses Clinical Features. Nonspecific RLH is usually of unknown cause and frequently affects children and young adults. It is the most common cause of lymphadenopathy in children and largely attributed to the repeated antigenic stimulation encountered in early life. In adults, RLH is less common. The enlarged lymph nodes in RLH are usually < 3cm, soft, small, oval, mobile, and single or multiple. RLH commonly involves the cervical, axillary, or inguinal lymph nodes. The lymphadenopathy may last up to a few weeks to months. In the clinical setting of persistent or increasing lymphadenopathy, FNA may be warranted to exclude lymphoma. Cytology. FNA smears show a polymorphous population dom­ inated by small mature lymphocytes. The latter have round nuclei and condensed dark chromatin. Other cells include transformed lymphocytes including centrocytes, centroblasts, and immunoblasts, scattered histiocytes including tingible body macrophages, which are specialized histiocytes predominantly found in germinal centers and PCs (Figs. 12.6A–C, 12.9B, and 12.26). Lymphohistiocytic aggregates and mitoses are also present (12,38). Orazi9781609136826-ch12.indd 316 FIGURE 12.26. RHL shows a lymphohistiocytic aggregate comprising of small and large lymphoid cells and tingible body macrophages. The latter are present both within and at the periphery of the aggregate (Pap stain, DS ×60 objective). Figures 12.5A–C and 12.8B depict other characteristics of a reactive lymph node. Immunophenotype. Positive for pan-B-cell markers including CD19, CD20, CD22, CD79a, and PAX5 with no light-chain restriction nor any cytogenetic abnormalities, as well as panT-cell markers including CD3, CD2, and CD5. Cytogenetics. Absence of t(14;18) is helpful in distinguishing reactive from neoplastic proliferations. Differential Diagnosis. In some lymphoid malignancies, a heterogeneous lymphoid pattern may be seen. These include low-grade FL, MZL, HL, and PTCL. These malignant entities can be distinguished from RLH by FCM and molecular analyses and by finding large atypical cells with CD15 and CD30 positivity in HL (12,38). Granulomatous Processes Some infectious processes may incite a granulomatous response; however, clusters of epithelioid histiocytes, multinucleated giant cells, or a “sarcoid-like reaction” can be seen in some malignant conditions affecting the lymph node. These conditions include HL and NHL and metastatic tumors (94,95). Histiocytes typically seen in granulomas have elongated or curved nuclei with fine, evenly dispersed chromatin, small nucleoli, and moderate amount of finely vacuolated cytoplasm. Multinucleated histiocytic giant cells are commonly encountered (see specific types of granulomas in the Infectious Granulomatous Condition section below). When granulomatous inflammation is diagnosed on FNA, special stains for organisms, including acid-fast bacillus (AFB) and Grocott methenamine silver stains, should be obtained. Microbiology culture studies should be performed when ­possible. Infectious Granulomatous Condition Tuberculous Lymphadenitis Key Cytologic Features • Caseating granulomas • Histiocytes, reactive lymphocytes, central caseous necrosis • Langhans giant cells • Background of neutrophils and necrosis • Intracellular and extracellular “negative” images of bacilli on DQ stain in atypical mycobacteria (MAC) cases 8/5/2013 12:02:44 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms317 In TB, the most common finding, seen in about 50% of cases, is the presence of epithelioid clusters with or without Langhans giant cells (large cells with nuclei arranged in a horseshoe-shaped pattern in the cell periphery) with necrosis (Fig. 12.27A and B); necrosis is absent in about one third of cases. FNA shows a sensitivity of about 75% in the detection of tuberculous lymphadenitis (94). AFBs may be identified by AFB special stain (Fig. 12.27C). In AIDS patient, MAC appear as intracellular and extracellular “negative images” in air-dried DQ-stained smears. FIGURE 12.27. Granulomatous conditions. A–C: Necrotizing granulomatous lymphadenitis, secondary to tuberculosis: (A) A large, loose aggregate of epithelioid cells is accompanied by a multinucleated giant cell and mixture of background lymphocytes and neutrophils. (B) Note the necrotizing nature of the granuloma (A, Pap stain, DS ×40 objective and B, Pap stain, DS ×60 objective). (C) Positive special stain for acid-fast bacilli (DS ×60 objective). D,E: Granulomatous lymphadenitis, secondary to sarcoid: (D) Smear shows a loose aggregate of epithelioid histiocytes and (E) A multinucleated giant cell with “asteroid bodies” (D, DQ stain DS and E, Pap stain, DS ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 317 8/5/2013 12:02:48 PM 318 Knowles Neoplastic Hematopathology Noninfectious Granulomatous Condition Sarcoidosis Key Cytologic Features • Noncaseating granulomas • Epithelioid histiocytes, reactive lymphoid cells • Multinucleated giant cells • Cytoplasmic asteroid bodies or Schaumann bodies in sarcoid • No necrosis Sarcoidosis is a systemic disease of unknown cause characterized by noncaseating granulomas. The disease predominantly affects adult and middle-aged African American women. Although any organ can be affected, sarcoidosis frequently involves mediastinal lymph nodes and lungs. Cytologically, the main findings are well-formed noncaseating granulomas comprising of epithelioid histiocytes, multinucleated giant cells, and lymphocytes without necrosis (Fig. 12.27D). Asteroid bodies (star-shaped intracytoplasmic cytoskeletal elements) (Fig. 12.27E) and Schaumann bodies (calcium oxalate crystals) may be observed. Sarcoidosis is a diagnosis of exclusion; a foreign-body giant cell reaction, an infectious etiology, or a malignancy need to be excluded. Cytologic findings should be correlated with clinical and imaging features (95). Infectious Mononucleosis Key Cytologic Features • Polymorphous lymphocytes • Immunoblasts • Plasmacytoid lymphocytes • Tingible body macrophages • Occasional PCs • Mitosis and apoptosis IM is an acute self-limited disease caused by EBV. It is usually seen in adolescents and young adults. In the acute infection, the virus replicates in the perifollicular B cells, simulating a vigorous humoral and cellular immune response. Typically, patients present with fever, pharyngitis, and cervical lymphadenopathy (75). Cytologically, IM displays large and small lymphocytes and large numbers of immunoblastic cells than are usually seen in a reactive lymph node. Immunoblasts are large cells with a large nucleus and nucleolus and basophilic cytoplasm (Fig. 12.28). Occasionally binucleated immunoblasts resembling RS cells are seen, a feature more commonly noted in the tonsils. Plasmacytoid lymphocytes, tingible body macrophages, and PCs are also seen. Mitosis and apoptosis are evident. In FNA smears, a polymorphic immunoblastic proliferation is suggestive of IM (Fig. 12.18A). ICC shows that these are of both B- and T-lymphocyte phenotype. Serologic studies confirm the diagnosis. Primary and Metastatic Neoplasms Primary and metastatic neoplasms including carcinomas, melanomas, germ cell tumors and sarcomas can mimic lymphoma (38,96). Poorly Differentiated Carcinoma Key Cytologic Features • Loosely cohesive cell clusters and single cells • Cell crowding • High-grade nuclei • Less or no cytoplasmic differentiation Metastatic carcinoma represents about 50% of cases in FNA of lymph nodes. Well- to moderately differentiated carcinoma usually shows cohesive cell clusters with community cell borders (Fig. 12.29A) and can easily be recognized as being of epithelial origin on FNA. In adenocarcinomas, cytoplasmic differentiation such as mucinous vacuoles may be present. In squamous cell carcinomas, keratinized cytoplasm is usually seen. PDCa predominantly exhibit dispersed single cells or loosely cohesive cell clusters and may mimic lymphoma. Differential diagnosis of PDCa includes DLBCL (Fig. 12.29B). A history of a previous carcinoma is usually present. Epithelial markers including cytokeratin in conjunction with tumor-specific markers, such as thyroid-transcription factor (TTF-1) for lung and thyroid, PSMA for prostatic, and CDX2 for gastrointestinal adenocarcinomas, can be applied to various types of cytology preparations. Artifactual aggregation of cells in lymphoma may simulate carcinoma (Fig. 12.29C). Small cell carcinoma may also be mistaken for lymphomas (Fig. 12.30). Careful evaluation for the classic nuclear features of molding, “salt and pepper” chromatin with crush artifact, and ICC positivity for endocrine markers including chromogranin, synaptophysin, and CD56 help to distinguish it from lymphoma (97). FNA smears of metastatic NPC show neoplastic single cells and clusters in a reactive lymphoid background (mixed pattern). Most single neoplastic cells present as large, pleomorphic bare nuclei. Metastatic NPC and HL may have a similar reactive lymphoid background, with eosinophils, PCs, and sometimes epithelioid-cell granulomas, and can be distinguished by ICC (98). Melanoma FIGURE 12.28. Infectious mononucleosis. Smear shows immunoblasts, reactive lymphocytes, and rare PCs (DQ stain DS ×100 objective with oil immersion). Orazi9781609136826-ch12.indd 318 Melanoma demonstrates monomorphous mono- or binucleated cells in a dispersed cell pattern. Nuclei are large and round with smooth chromatin and prominent nucleoli. Cytoplasm is scanty and may contain melanin pigment (Fig. 12.31). The large binucleated melanoma cells with prominent nucleoli may mimic RS cells or cells of ALCL. Immunoreactivity for S-100 protein, HMB-45, and Melan A is characteristic. 8/5/2013 12:02:49 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms319 FIGURE 12.29. Carcinoma. A: Well-differentiated carcinoma of lung depicting columnar epithelial cells in a glandular architecture (DQ stain, DS ×60 objective). B: Poorly differentiated carcinoma may mimic DLBCL. In this case of poorly differentiated papillary thyroid carcinoma, cells are arranged in a vague follicular arrangement. Nuclei are round to oval with occasional intranuclear inclusions and grooves. Cytoplasm is pale and basophilic (Pap stain, DS ×60 objective). C: Cells of large cell lymphoma may artifactually aggregate and may need ICC for confirmation of lymphoid nature (DQ stain DS ×60 objective). FIGURE 12.30. Metastatic small cell undifferentiated carcinoma of the lung. Aggregate of cohesive tumor cells with nuclear molding, fine to coarse, evenly dispersed chromatin, and scant to absent cytoplasm is easily identified. Note occasional nuclear elongation indicating crush artifact and apoptotic bodies (DQ stain DS ×60). Orazi9781609136826-ch12.indd 319 FIGURE 12.31. Metastatic melanoma showing dispersed neoplastic cells with eccentrically placed nuclei, prominent nucleoli, and granular blue-to-purple staining cytoplasm. Bi- and multinucleation and intranuclear cytoplasmic inclusions were also noted (DQ stain DS ×100 oil immersion). 8/5/2013 12:02:53 PM 320 Knowles Neoplastic Hematopathology FIGURE 12.32. FNA of seminoma shows the characteristic “tigroid background” and monomorphic tumor cells with hyperchromatic round-to-oval nuclei and prominent nucleoli and lymphocytes (DQ stain DS ×100 oil immersion). Courtesy of Grace Yang, MD, Department of Pathology & Laboratory Medicine, Weill Cornell Medical Center, New York, NY. Small Round Blue Cell Tumors A group of undifferentiated malignancies known as the small round blue-cell tumors include neuroblastoma, Ewing family of tumors consisting of Ewing sarcoma and primitive neuroectodermal tumors, rhabdomyosarcoma, and lymphoblastic leukemia. These tumors share cytomorphologic similarities that can make them indistinguishable from each other and from lymphomas. On FNA, neuroblastoma, Ewing sarcoma, and rhabdomyosarcoma frequently form small cellular aggregates in addition to discohesive cells. Other specific architectural features may be evident such as pseudorosettes in Ewing sarcoma and neuroblastoma and neurophil-like material in neuroblastoma. Rhabdomyosarcoma nuclei tend to be round with a vesicular chromatin pattern, occasionally with prominent nucleoli and relatively abundant cytoplasm. Ewing sarcoma tends to have spherical to ellipsoid nuclei with faintly stippled chromatin and small nucleoli. ICC and cytogenetic studies can facilitate the distinction between lymphoma and other types of small round blue-cell tumors. Thus, for example, a panel composed of CD99 and TdT, lymphocytic markers (LCA, CD20, CD3), and vimentin appears to be sensitive and specific for distinguishing Ewing sarcoma from LBL (99). Ewing sarcoma also shows cytogenetic abnormality of t(11;22) in the majority of cases and t(21;22) in a small number of cases. Immunoreactivity for CD56 and chromogranin are effective in detecting neuroblastoma cells, and desmin and myogenin are useful in rhabdomyosarcoma. Seminoma Dispersed monomorphic cells with thick nuclear membranes, prominent nucleoli, and vacuolated cytoplasm with a lymphocytic component are characteristic for seminoma and may simulate lymphoma. The “tigroid background” of seminoma, produced by strands of cytoplasm and proteinaceous material, provides a helpful clue on DQ stain (Fig. 12.32). Immunoreactivity for nuclear OCT4, membranous c-kit, and new marker SALL4 and 12p abnormality by FISH are seen in seminoma (100). References 1. Swerdlow SH, Campo E, Harris NL, et al., eds. World Health Organization classification of tumors of the hematopoietic and lymphoid tissues. Lyon: IARC Press, 2008. Orazi9781609136826-ch12.indd 320 2.Meda BA, Buss DH, Woodruff RD, et al. Diagnosis and subclassification of ­primary and recurrent lymphoma. The usefulness and limitations of combined fine-needle aspiration cytomorphology and flowcytometry. Am J Clin Pathol 2000;113:688–699. 3.Wakely PE Jr. Fine-needle aspiration cytopathology in diagnosis and classification of malignant lymphoma: accurate and reliable? Diagn Cytopathol 2000;22:120–125. 4.Dong HY, Harris NL, Preffer FI, et al. Fine-needle aspiration biopsy in the diagnosis and classification of primary and recurrent lymphoma: a retrospective analysis of the utility of cytomorphology and flow cytometry. Mod Pathol 2001;14:472–481. 5. Landgren O, Porwit MacDonald A, et al. A prospective comparison of fine-needle aspiration cytology and histopathology in the diagnosis and classification of lymphomas. Hematol J 2004;5:69–76. 6. Katz RL. Modern approach to lymphoma diagnosis by fine-needle aspiration: restoring respect to a valuable procedure. Cancer 2005;105:429–431. 7. Wakely PE Jr. The diagnosis of non-Hodgkin lymphoma using fine-needle aspiration cytopathology: a work in progress. Cancer Cytopathol 2010;118:238–243. 8. Orucevic A, Reddy VB, Selvaggi SM, et al. Fine-needle aspiration of extranodal and extramedullary hematopoietic malignancies. Diagn Cytopathol 2000;23:318– 321. 9. Mourad WA, Tulbah A, Shoukri M, et al. Primary diagnosis and REAL/WHO classification of non-Hodgkin’s lymphoma by fine-needle aspiration: cytomorphologic and immunophenotypic approach. Diagn Cytopathol 2003;28:191–195. 10. Sigstad E, Dong HP, Davidson B, et al. The role of flow cytometric immunophenotyping in improving the diagnostic accuracy in referred fine-needle aspiration specimens. Diagn Cytopathol 2004;31:159–163. 11. Hehn ST, Grogan TM, Miller TP. Utility of fine-needle aspiration as a diagnostic technique in lymphoma. J Clin Oncol 2004;22:3046–3052. 12.Monaco SE, Khalbuss WE, Pantanowitz L. Benign non-infectious causes of lymphadenopathy: a review of cytomorphology and differential diagnosis. Diagn Cytopathol 2012;40(10):925–938. 13. Bangerter M, Brudler O, Heinrich B, et al. Fine needle aspiration cytology and flow cytometry in the diagnosis and subclassification of non-Hodgkin’s lymphoma based on the World Health Organization classification. Acta Cytol 2007;51:390– 398. 14. Ribeiro A, Pereira D, Escalón MP, et al. EUS-guided biopsy for the diagnosis and classification of lymphoma. Gastrointest Endosc 2010;71:851–855. 15. Chhieng DC, Cohen JM, Cangiarella JF. Cytology and immunophenotyping of lowand intermediate-grade B-cell non-Hodgkin’s lymphomas with a predominant small-cell component: a study of 56 cases. Diagn Cytopathol 2001;24:90–97. 16. Amador-Ortiz C, Chen L, Hassan A, et al. Combined core needle biopsy and fine-needle aspiration with ancillary studies correlate highly with traditional techniques in the diagnosis of nodal-based lymphoma. Am J Clin Pathol 2011;135:516–524. 17. Hoda RS. Non-gynecologic cytology on liquid-based preparations: a morphologic review of facts and artifacts. Diagn Cytopathol 2007;35:621–634. 18. Ljung BM. Techniques of fine needle aspiration, smear preparation and principles of interpretation. In: Koss G, Melamed MR, eds. Koss’ diagnostic cytology and its histopathologic bases, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2006:1056–1581. 19. Lieu D. Value of cytopathologist-performed ultrasound-guided fine needle aspiration as a screening test for ultrasound-guided core-needle biopsy in nonpalpable breast masses. Diagn Cytopathol 2009;37:262–269. 20. Gong JZ, Snyder MJ, Lagoo AS, et al. Diagnostic impact of core-needle biopsy on fine-needle aspiration of non-Hodgkin lymphoma. Diagn Cytopathol 2004;31: 23–30. 21. Assaad MW, Pantanowitz L, Otis CN. Diagnostic accuracy of image-guided percutaneous fine needle aspiration biopsy of the mediastinum. Diagn Cytopathol 2007;35:705–709. 22. Ko HM, da Cunha Santos G, Darling G, et al. Diagnosis and subclassification of lymphomas and non-neoplastic lesions involving mediastinal lymph nodes using endobronchial ultrasound-guided transbronchial needle aspiration. Diagn Cytopathol. Published online 2011 May 31. PubMed PMID: 21630485. 23. Marshall CB, Jacob B, Patel S, et al. The utility of endobronchial ultrasoundguided transbronchial needle aspiration biopsy in the diagnosis of mediastinal lymphoproliferative disorders. Cancer Cytopathol 2011;119:118–126. 24. Griffin AC, Schwartz LE, Baloch ZW. Utility of on-site evaluation of endobronchial ultrasound-guided transbronchial needle aspiration specimens. Cytojournal 2011;8:20. 25. Florentine BD, Staymates B, Rabadi M, et al. Cancer Committee of the Henry Mayo Newhall Memorial Hospital. The reliability of fine-needle aspiration biopsy as the initial diagnostic procedure for palpable masses: a 4-year experience of 730 patients from a community hospital-based outpatient aspiration biopsy clinic. Cancer 2006;107:406–416. 26. Punia RS, Dhingra N, Chopra R, et al. Lymph node infarction and its association with lymphoma: a short series and literature review. N Z Med J 2009;122: 40–44. 27. Caraway NP. Strategies to diagnose lymphoproliferative disorders by fine-needle aspiration by using ancillary studies. Cancer 2005;105:432–442. 28. Ali AE, Morgen EK, Geddie WR, et al. Classifying B-cell non-Hodgkin lymphoma by using MIB-1 proliferative index in fine-needle aspirates. Cancer Cytopathol 2010;118:166–172. 29. Symmans WF, Cangiarella JF, Symmans PJ, et al. Apoptotic index from fine needle aspiration cytology as a criterion to predict histologic grade of non-Hodgkin’s lymphoma. Acta Cytol 2000;44:194–204. 30. Dey P. Role of ancillary techniques in diagnosing and subclassifying non-Hodgkin’s lymphomas on fine needle aspiration cytology. Cytopathology 2006;17: 275–287. 31. Weiss LM, Loera S, Bacchi CE. Immunoglobulin light chain immunohistochemistry revisited, with emphasis on reactive follicular hyperplasia versus follicular lymphoma. Appl Immunohistochem Mol Morphol 2010;18:199–205. 32.Theodossiou C, Schwarzenberger P. Non-Hodgkin’s lymphomas. Clin Obstet Gynecol 2002;45:820–829. 33. Pambuccian SE, Bardales RH. Lymph node cytopathology. Essentials in cytopathology. New York: Springer, 2011. 34. Wright DH, Leong A S-Y, Addis BJ. Diagnostic lymph node pathology, 2nd ed. Canada: Hodder Arnold Publishers, 2011. 8/5/2013 12:02:54 PM Chapter 12 The Role of Fine Needle Aspiration Biopsy in the Diagnosis and Management of Hematopoietic Neoplasms321 35. Skooj L, Tani E. FNA cytology in the diagnosis of lymphoma. Basel, Switzerland: Karger, 2009. 36. Kocjan G. Best Practice No 185. Cytological and molecular diagnosis of lymphoma. J Clin Pathol 2005;58:561–567. 37. Rossi ED, Larghi A, Verna EC, et al. Endoscopic ultrasound-guided fine-needle aspiration with liquid-based cytologic preparation in the diagnosis of primary pancreatic lymphoma. Pancreas 2010;39:1299–1302. 38. Gupta RK, Naran S, Lallu S, et al. The diagnostic value of fine needle aspiration cytology (FNAC) in the assessment of palpable supraclavicular lymph nodes: a study of 218 cases. Cytopathology 2003;14:201–207. 39. Savage EC, Vanderheyden AD, Bell AM, et al. Independent diagnostic accuracy of flow cytometry obtained from fine-needle aspirates: a 10-year experience with 451 cases. Am J Clin Pathol 2011;135:304–309. 40. Zeppa P, Vigliar E, Cozzolino I, et al. Fine needle aspiration cytology and flow cytometry immunophenotyping of non-Hodgkin lymphoma: can we do better? Cytopathology 2010;21:300–310. 41. Barrena S, Almeida J, Del Carmen García-Macias M, et al. Flow cytometry immunophenotyping of fine-needle aspiration specimens: utility in the diagnosis and classification of non-Hodgkin lymphomas. Histopathology 2011;58:906–918. 42. Schmid S, Tinguely M, Cione P, et al. Flow cytometry as an accurate tool to complement fine needle aspiration cytology in the diagnosis of low grade malignant lymphomas. Cytopathology 2011;22:397–406. 43. Zhang S, Abreo F, Lowery-Nordberg M, et al. The role of fluorescence in situ hybridization and polymerase chain reaction in the diagnosis and classification of lymphoproliferative disorders on fine-needle aspiration. Cancer Cytopathol 2010;118:105–112. 44. Goy A, Stewart J, Barkoh BA, et al. The feasibility of gene expression profiling generated in fine-needle aspiration specimens from patients with follicular ­lymphoma and diffuse large B-cell lymphoma. Cancer 2006;108:10–20. 45. Reading CF, Schlette EJ, Stewart JM, et al. Fine-needle aspiration biopsy ­findings in patients with small lymphocytic lymphoma transformed to Hodgkin lymphoma. Am J Clin Pathol 2007;128:571–578. 46.Tandon B, Peterson L, Gao J, et al. Nuclear overexpression of lymphoidenhancer-binding factor 1 identifies chronic lymphocytic leukemia/small lymphocytic ­lymphoma in small B-cell lymphomas. Mod Pathol 2011;24:1433–1443. 47. Caraway NP, Thomas E, Khanna A, et al. Chromosomal abnormalities detected by multicolor fluorescence in situ hybridization in fine-needle aspirates from patients with small lymphocytic lymphoma are useful for predicting survival. Cancer 2008;114:315–322. 48. Lin P, Medeiros LJ. Lymphoplasmacytic lymphoma/waldenstrom macroglobulinemia: an evolving concept. Adv Anat Pathol 2005;12:246–255. 49. Vitolo U, Ferreri AJ, Montoto S. Lymphoplasmacytic lymphoma-Waldenstrom’s macroglobulinemia. Crit Rev Oncol Hematol 2008;67:172–185. 50.Berger F, Traverse-Glehen A, Felman P, et al. Clinicopathologic features of Waldenstrom’s macroglobulinemia and marginal zone lymphoma: are they distinct or the same entity? Clin Lymphoma 2005;5:220–224. 51. Goel G, Rai S, Naik R, et al. Cytodiagnosis of extramedullary plasmacytomas. Acta Cytol 2010;54:255–258. 52. Sarin H, Manucha V, Verma K. Extramedullary plasmacytoma, a report of five cases diagnosed by FNAC. Cytopathology 2009;20:328–231. 53. Murphy BA, Meda BA, Buss DH, et al. Marginal zone and mantle cell lymphomas: assessment of cytomorphology in subtyping small B-cell lymphomas. Diagn Cytopathol 2003;28:126–130. 54. Kaba S, Tokoro Y, Washiya K, et al. Cytology of pulmonary marginal zone B-cell lymphoma of MALT type: lessons learned for intra-operative diagnosis. Cytopathology 2011;22:346–349. 55. Crapanzano JP, Lin O. Cytologic findings of marginal zone lymphoma. Cancer 2003;99:301–309. 56. Saikia UN, Dey P, Saikia B, et al. Fine-needle aspiration biopsy in diagnosis of follicular lymphoma: cytomorphologic and immunohistochemical analysis. Diagn Cytopathol 2002;26:251–256. 57. Young NA. Grading follicular lymphoma on fine-needle aspiration specimens—a practical approach. Cancer 2006;108:1–9. 58.Ouansafi I, He B, Fraser C, et al. Transformation of follicular lymphoma to plasmablastic lymphoma with c-myc gene rearrangement. Am J Clin Pathol 2010;134:972–981. 59. Cibas ES, Ducatman BS. Cytology: diagnostic principals and clinical correlates, 3rd ed. Philadelphia: Elsevier Health Sciences, 2009. 60. Sun W, Caraway NP, Zhang HZ, et al. Grading follicular lymphoma on fine needle aspiration specimens. Comparison with proliferative index by DNA image analysis and Ki-67 labeling index. Acta Cytol 2004;48:119–126. 61. Brandao GD, Rose R, McKenzie S, et al. Grading follicular lymphomas in fineneedle aspiration biopsies: the role of ThinPrep slides and flowcytometry. Cancer 2006;108:319–323. 62. da Cunha Santos G, Ko HM, Geddie WR, et al. Targeted use of fluorescence in situ hybridization (FISH) in cytospin preparations: results of 298 fine needle aspirates of B-cell non-Hodgkin lymphoma. Cancer Cytopathol 2010;118:250–258. 63.Richmond J, Bryant R, Trotman W, et al. FISH detection of t(14;18) in follicular lymphoma on Papanicolaou-stained archival cytology slides. Cancer 2006;108:198–204. 64. Bangerter M, Brudler O, Heinrich B, et al. Fine needle aspiration cytology and flow cytometry in the diagnosis and subclassification of non-Hodgkin’s lymphoma based on the World Health Organization classification. Acta Cytol 2007;51: 390–398. 65. Parrens M, Belaud-Rotureau MA, Fitoussi O, et al. Blastoid and common variants of mantle cell lymphoma exhibit distinct immunophenotypic and interphase FISH features. Histopathology 2006;48:353–362. 66. Athanasiou E, Kotoula V, Hytiroglou P, et al. In situ hybridization and reverse transcription-polymerase chain reaction for cyclin D1 mRNA in the diagnosis of mantle cell lymphoma in paraffin-embedded tissues. Mod Pathol 2001;14: 62–71. Orazi9781609136826-ch12.indd 321 67. Zeng W, Fu K, Quintanilla-Fend L, et al. Cyclin D1-negative blastoid mantle cell lymphoma identified by SOX11 expression. Am J Surg Pathol 2012;36:214–219. 68. de Leval L, Hasserjian RP. Diffuse large B-cell lymphomas and burkitt lymphoma. Hematol Oncol Clin North Am 2009;23:791–827. 69. Verstovsek G, Chakraborty S, Ramzy I, et al. Large B-cell lymphomas: fine-needle aspiration plays an important role in initial diagnosis of cases which are falsely negative by flow cytometry. Diagn Cytopathol 2002;27:282–285. 70. Desouki MM, Post GR, Cherry D, et al. PAX-5: a valuable immunohistochemical marker in the differential diagnosis of lymphoid neoplasms. Clin Med Res 2010;8:84–88. 71. Daneshbod Y, Omidvari S, Daneshbod K, et al. Diffuse large B cell lymphoma of thyroid as a masquerader of anaplastic carcinoma of thyroid diagnosed by FNA: a case report. Cytojournal 2006;3:23. 72. Hoda RS, Picklesimer L, Green KM, et al. Fine-needle aspiration of a primary mediastinal large B-cell lymphoma: a case report with cytologic, histologic, and flow cytometric considerations. Diagn Cytopathol 2005;32:370–337 73. Rafaniello Raviele P, Pruneri G, et al. Plasmablastic lymphoma: a review. Oral Dis 2009;15:38–45. 74. Reid-Nicholson M, Kavuri S, Ustun C, et al. Plasmablastic lymphoma: cytologic findings in 5 cases with unusual presentation. Cancer 2008;114(5):333–341. 75. Rezk SA, Weiss LM. Epstein-Barr virus-associated lymphoproliferative disorders [Review]. Hum Pathol 2007;38:1293–304. 76. Troxell ML, Bangs CD, Cherry AM, et al. Cytologic diagnosis of Burkitt lymphoma. Cancer 2005;105:310–318. 77. Bellan C, Stefano L, Giulia de F, et al. Burkitt lymphoma versus diffuse large B-cell lymphoma: a practical approach. Hematol Oncol 2009;27:182–185. 78.Mann G, Attarbaschi A, Steiner M, et al. Austrian Berlin-Frankfurt-Münster (BFM) group. Early and reliable diagnosis of non-Hodgkin lymphoma in childhood and adolescence: contribution of cytomorphology and flow cytometric immunophenotyping. Pediatr Hematol Oncol 2006;23:167–176. 79. Wakely P Jr, Frable WJ, Kneisl JS. Soft tissue aspiration cytopathology of malignant lymphoma and leukemia. Cancer 2001;93:35–39. 80. Yao JL, Cangiarella JF, Cohen JM, et al. Fine-needle aspiration biopsy of peripheral T-cell lymphomas. A cytologic and immunophenotypic study of 33 cases. Cancer 2001;93:151–159. 81. Mathur S, Verm K. Peripheral T-cell lymphoma not otherwise specified vs. Hodgkin’s lymphoma on fine needle aspiration cytology. Acta Cytol 2005;49:373–377. 82. Das P, Iyer VK, Mathur SR, et al. Anaplastic large cell lymphoma: a critical evaluation of cytomorphological features in seven cases. Cytopathology 2010;21: 251–258. 83. McEvoy JR, Cady FM, Hoda RS. “Wreath cell” in recurrent anaplastic large cell lymphoma. Diagn Cytopathol 2006;34:112–113. 84. Buxton D, Bacchi CE, Gualco G, et al. Frequent expression of CD99 in anaplastic large cell lymphoma: a clinicopathologic and immunohistochemical study of 160 cases. Am J Clin Pathol 2009;131:574–579. 85. Eberle FC, Mani H, Jaffe ES. Histopathology of Hodgkin’s lymphoma. Cancer J 2009;15:129–137. 86. Das DK, Francis IM, Sharma PN, et al. Hodgkin’s lymphoma: diagnostic difficulties in fine-needle aspiration cytology. Diagn Cytopathol 2009;37:564–573. 87. Jiménez-Heffernan JA, Vicandi B, López-Ferrer P, et al. Value of fine needle aspiration cytology in the initial diagnosis of Hodgkin’s disease. Analysis of 188 cases with an emphasis on diagnostic pitfalls. Acta Cytol 2001;45:300–306. 88. Iacobuzio-Donahue CA, Clark DP, Ali SZ. Reed-Sternberg-like cells in lymph node aspirates in the absence of Hodgkin’s disease: pathologic significance and differential diagnosis. Diagn Cytopathol 2002;27:335–339. 89.Gualco G, Weiss LM, Bacchi CE. Expression of p63 in anaplastic large cell lymphoma but not in classical Hodgkin’s lymphoma. Hum Pathol 2008;39: 1505–1510. 90. Mourad WA, al Nazer M, Tulbah A. Cytomorphologic differentiation of Hodgkin’s lymphoma and Ki−1+ anaplastic large cell lymphoma in fine needle aspirates. Acta Cytol 2003;47:744–748. 91. Subhawong AP, Ali SZ, Tatsas AD. Nodular lymphocyte-predominant Hodgkin lymphoma: cytopathologic correlates on fine-needle aspiration. Cancer Cytopathol 2012;120(4):254–260. 92. Kumar PV, Mousavi A, Karimi M, et al. Fine needle aspiration of Langerhans cell histiocytosis of the lymph nodes. A report of six cases. Acta Cytol 2002;46:753– 756. 93. Yang GC, Wang J, Yee HT. Interwoven dendritic processes of follicular dendritic cell sarcoma demonstrated on ultrafast papanicolaou-stained smears: a case report. Acta Cytol 2006;50:534–538. 94. Mittal P, Handa U, Mohan H, et al. Comparative evaluation of fine needle aspiration cytology, culture, and PCR in diagnosis of tuberculous lymphadenitis. Diagn Cytopathol 2011;39:822–826. 95. Mehrotra R, Dhingra V. Cytological diagnosis of sarcoidosis revisited: a state of the art review. Diagn Cytopathol 2011;39:541–548. 96. Anderson GG, Weiss LM. Determining tissue of origin for metastatic cancers: meta-analysis and literature review of immunohistochemistry performance. Appl Immunohistochem Mol Morphol 2010;18:3–8. Review. 97. De Las Casas LE, Gokden M, Mukunyadzi P, et al. A morphologic and statistical comparative study of small-cell carcinoma and non-Hodgkin’s lymphoma in fine-needle aspiration biopsy material from lymph nodes. Diagn Cytopathol 2004;31:229–234. 98. Kollur SM, El Hag IA. Fine-needle aspiration cytology of metastatic nasopharyngeal carcinoma in cervical lymph nodes: comparison with metastatic squamouscell carcinoma, and Hodgkin’s and non-Hodgkin’s lymphoma. Diagn Cytopathol 2003;28:18–22. 99. Lucas DR, Bentley G, Dan ME, et al. Ewing sarcoma vs lymphoblastic lymphoma. A comparative immunohistochemical study. Am J Clin Pathol 2001;115:11–17. 100. Iwamoto N, Ishida M, Yoshida K, et al. Mediastinal seminoma: a case report with special emphasis on sall4 as a new immunocytochemical marker. Diagn Cytopathol. Published online 2012 Feb 1. Pubmed PMID: 22298374. 8/5/2013 12:02:54 PM