Cell Stem Cell
Review
Tissue-Specific Stem Cells:
Lessons from the Skeletal Muscle Satellite Cell
Andrew S. Brack1,2,3,* and Thomas A. Rando4,5
1Center
of Regenerative Medicine, Massachusetts General Hospital, Boston, MA 02114, USA
Medical School, Boston, MA 02115, USA
3Harvard Stem Cell Institute, Cambridge, MA 02138, USA
4Paul F. Glenn Laboratories for the Biology of Aging and the Department of Neurology and Neurological Sciences, Stanford University School
of Medicine, Stanford, CA 94305, USA
5Neurology Service and Rehabilitation Research and Development Center of Excellence, Veterans Affairs Palo Alto Health Care System,
Palo Alto, CA 94304, USA
*Correspondence: abrack@partners.org
DOI 10.1016/j.stem.2012.04.001
2Harvard
In 1961, the satellite cell was first identified when electron microscopic examination of skeletal muscle
demonstrated a cell wedged between the plasma membrane of the muscle fiber and the basement
membrane. In recent years it has been conclusively demonstrated that the satellite cell is the primary cellular
source for muscle regeneration and is equipped with the potential to self renew, thus functioning as a bona
fide skeletal muscle stem cell (MuSC). As we move past the 50th anniversary of the satellite cell, we take this
opportunity to discuss the current state of the art and dissect the unknowns in the MuSC field.
Introduction
The observation that skeletal muscle has the capacity to regenerate after injury was well documented by microscopic examination in the mid-19th century, primarily in German literature
(Scharner and Zammit, 2011). Still, the cellular basis of this
regenerative potential remained elusive for a century until 50
years ago when Alexander Mauro detected a mononucleated
cell, which he termed a ‘‘satellite cell,’’ closely apposed to
mature myofibers in electron micrographs of skeletal muscle
(Mauro, 1961). Without any functional evidence, he hypothesized
that this could represent a kind of muscle progenitor cell akin to
those present in the developing embryo, capable of forming new
muscle in response to injury. This turned out to be a very accurate prediction: five decades of research on satellite cells have
demonstrated that they have the characteristics that Mauro
surmised. In modern parlance, the satellite cell is considered
a muscle stem cell distinguished from the plethora of adult
tissue-specific stem cells that have been described by the fact
that it was identified anatomically before it was characterized
functionally; most adult stem cells have been first demonstrated
to exist in functional assays, which are then followed by a hunt
for the cells histologically.
The history of the satellite cell has been the subject of several
recent reviews (Scharner and Zammit, 2011; Yablonka-Reuveni,
2011), and the regulation and contribution of satellite cell
progenitors during lineage progression, differentiation, and
contribution to muscle repair has also been extensively documented (Chargé and Rudnicki, 2004; Wang and Rudnicki,
2012; Zammit et al., 2006). In this review, we focus on the current
status of satellite cell research through the lens of stem cell
biology. We highlight recent studies illustrating that satellite
cells are essential for maintenance of the stem cell pool and
repair of the differentiated muscle tissue in which they reside.
In addition, we discuss the properties that satellite cells possess
in common with other stem cell populations and the mechanisms
that regulate satellite cell functions.
504 Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc.
Satellite Cell Identification and Stem Cell Properties
After anatomical identification of satellite cells in 1961, their
behavior in response to growth and regeneration was investigated. It was noted that in regenerating muscle, undifferentiated
cells increase in abundance and align with the periphery of
damaged fibers. As regeneration progresses, immature myogenic progenitors are replaced with more mature myoblasts
(Allbrook, 1962). At later stages of repair, undifferentiated cells
begin to appear in association with the regenerated fibers
(Shafiq and Gorycki, 1965). A series of studies using tritiated
thymidine confirmed that satellite cells were mitotically dormant
in mature muscle and the source for regenerating muscle (Reznik, 1969; Schultz et al., 1978; Snow, 1977) and that daughters
of satellite cells contributed to both the satellite cell compartment and differentiated nuclei in growing muscle (Lipton
and Schultz, 1979; Moss and Leblond, 1970, 1971; Schultz,
1996). Thus with the evidence that satellite cells were capable
of asymmetric divisions and endowed with self-renewal properties, a new era was born, in which satellite cells were considered
bona fide MuSCs.
Cell transplantation was becoming more commonplace in
regenerative biology to test cellular contribution to tissue repair
and renewal of progenitor populations. The grafting of committed satellite cell progeny (myoblasts) between mice with
different isoenzyme subtypes confirmed that donor cells could
fuse with host cells or myofibers (Partridge et al., 1978; Watt
et al., 1982), providing evidence of a renewable cell source
with regenerative capacity. However, identification and isolation
of the self-renewing cells, MuSCs, remained elusive for many
years.
Eventually, immunotypic analysis identified the paired box 7
transcription factor Pax7 as a uniform marker of satellite cells
(Seale et al., 2000). In response to injury, Pax7+ satellite cells
enter cycle and differentiate and a subset returns back to quiescence to replenish the dormant satellite cell pool (Abou-Khalil
and Brack, 2010). A body of work during the late 1980s and early
Cell Stem Cell
Review
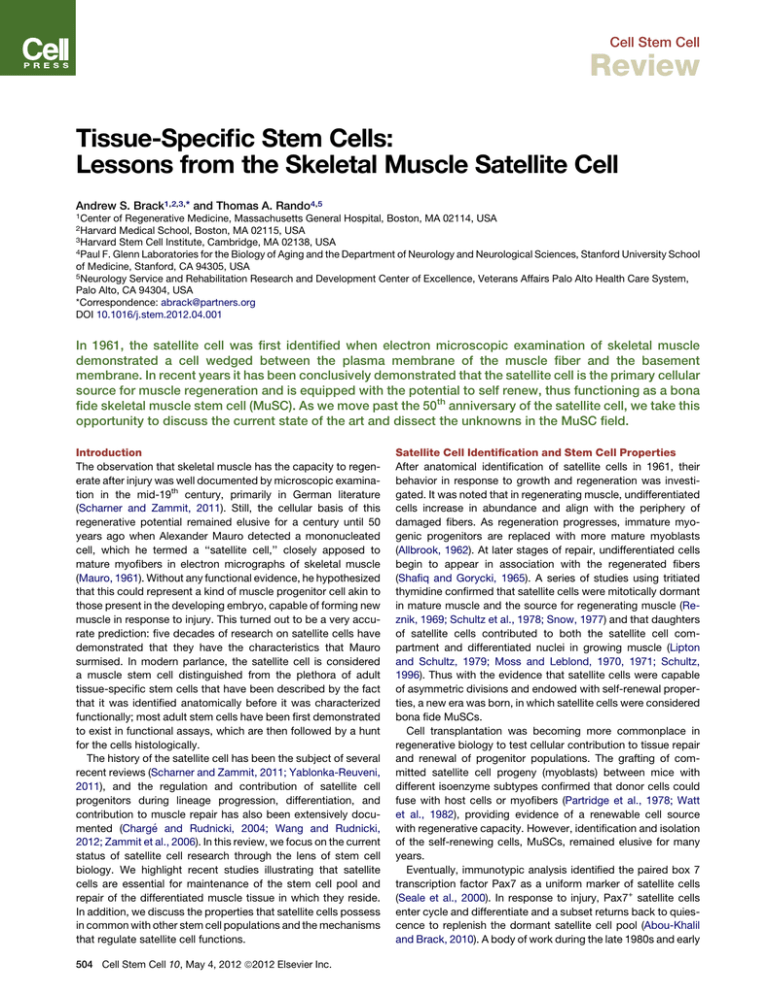
Figure 1. Satellite Cell Functions
(A) Adult single muscle fiber showing Pax7+ satellite cells (pink) located on individual multinucleated adult muscle fibers, myonuclei stained with DAPI (blue).
(B) An example of satellite cell contribution to muscle repair with Pax7CreERTM.R26Rb-gal is shown by X-gal reaction on an adult lower limb muscle prior to and after
injury (reproduced from Shea et al., 2010). Note the many X-gal+ muscle fibers running throughout the regenerating muscle.
(C) Pax7+ cells located in satellite cell position in uninjured muscle and their contribution to both myofiber repair and repopulation in the satellite cell position after
regeneration (reproduced from Shea et al., 2010).
(D) A schematic showing the participating roles of satellite cells. Pax7-expressing satellite cells (red) reside between the plasmalemma (brown line) of the muscle
fiber and the basal lamina (black line). A mature adult muscle contains thousands of differentiated nuclei (green) and 10 SCs (this number is highly dependent on
age, muscle length, and metabolic character). In response to injury, Pax7+ cells proliferate, most differentiate and fuse to regenerate myofibers (blue), whereas
a minority self renew and return back to quiescence to replenish the satellite cell pool (left). After genetic ablation of satellite cells, muscle regeneration is
prevented. During rapid hypertrophic stimuli, satellite cells fuse to add differentiated myonuclei. After genetic ablation of satellite cells, muscle hypertrophy
occurs without addition of myonuclei, suggesting that satellite cells are dispensable for protein accumulation and hypertrophy (center). During normal tissue
homeostasis, the contribution of satellite cells to maintenance of tissue or the satellite cell pool remains unknown (right).
1990s discovered the family of myogenic regulatory factors
(MRFs), including Myod, Myf5, Mrf44, and Myogenin, genes
that coordinate developmental myogenesis (Bentzinger et al.,
2012). In their quiescent state, adult satellite cells express, along
with Pax7, the Myf5 transcript but lack Myod. During activation
and lineage progression, satellite cells turn on Myod and
Myf5 protein, followed by the marker of terminal differentiation,
Myogenin (Chargé and Rudnicki, 2004).
Demonstration of a tractable muscle-resident cell that contributed to muscle fiber repair and repopulation of the niche
was achieved through transplantation of a FACS-isolated subset
of muscle-resident cells selected via cell surface receptor
expression (such as CD31 , CD45 , Sca1 , CXCR4+, CD31+,
Integrin b1+) (Montarras et al., 2005; Sherwood et al., 2004).
Engrafting a single myofiber with its satellite cells marked by
a nuclear Myf5lacZ reporter provided the first definitive demonstration that satellite cells possess stem cell activity (Collins
et al., 2005). In recent years, satellite cells have been proven to
self-renew at the single-cell level (Sacco et al., 2008) and to
retain stem cell function over seven rounds of serial transplantation and therefore function as MuSCs (Rocheteau et al., 2012).
With the advent of conditional Cre/lox systems, lineage tracing
of satellite cells has demonstrated that adult Pax7+ cells selfrenew and differentiate in their endogenous environment in
response to injury (Lepper et al., 2009; Shea et al., 2010), suggesting that adult Pax7+ satellite cells are sufficient for both
MuSC pool maintenance and myofiber repair. Moreover, studies
using inducible genetic strategies to ablate adult Pax7+ cells
have demonstrated that satellite cells are essential for muscle
repair and replenishment of the MuSC pool (Lepper et al.,
2011; McCarthy et al., 2011; Murphy et al., 2011; Sambasivan
et al., 2011). Cre/lox technology has also enabled the assessment of lineage potential of satellite cells. Based on studies
with Pax7CreERTM and MyodCre, it appears that most if not all
satellite cells are restricted to the myogenic lineage, arguing in
favor of unipotency of adult satellite cells (Lepper et al., 2009;
Shea et al., 2010; Starkey et al., 2011). However, it appears
that at least a subset of satellite cells are driven out of lineage,
becoming fibrogenic in pathological conditions or during aging
(Amini-Nik et al., 2011; Brack et al., 2007).
Although the contribution of satellite cells to tissue repair is
indisputable, their role in other aspects of skeletal muscle
biology is less certain (Figure 1). During normal daily activity,
muscle fiber size and myonuclear content remain relatively
constant throughout most of adult life (Hughes and Schiaffino,
1999), and satellite cells may exhibit a modest decline depending
upon the specific muscle and species examined (Brack and
Rando, 2007). Are satellite cells participating to maintain muscle
fibers during homeostasis? Indelible-marked adult satellite cells
chased over 6 weeks do not appear to undergo proliferation or
contribute to muscle fibers (Lepper et al., 2009; Shea et al.,
2010). Moreover, 2 weeks after ablation of the satellite cell
pool by a genetic strategy, muscle fiber size appears unaffected
(Lepper et al., 2011). Even 6 months after depletion of satellite
Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc. 505
Cell Stem Cell
Review
cells from a muscle, gross histological appearance is normal
and fiber size changes negligibly (Cheung et al., 2012). Together,
the data suggest that satellite cell contribution to myofiber
maintenance is minimal during homeostasis. It would be informative to determine whether ablation of the adult pool would
exacerbate muscle atrophy in contexts of higher cellular demand
such as exercise or aging.
Adult skeletal muscle is capable of hypertrophy, and the
question as to satellite cell participation in that process has
been debated for many years. Recent studies have provided
direct evidence of hypertrophy without any satellite cell contribution. Using a genetic strategy to ablate the adult Pax7+
cell pool, mice deficient in satellite cells were able to rapidly
increase muscle fiber size during a 2 week hypertrophic stimulus
(McCarthy et al., 2011). This occurred in the absence of satellite
cell-derived myonuclear accretion, suggesting that satellite cells
are dispensable for increase in muscle mass. However, it is
possible that over longer periods of time, additional differentiated nuclei, and hence a maintained myonuclear domain size
in hypertrophic muscle, would be required to maintain a larger
muscle fiber (Hughes and Schiaffino, 1999). This is supported
by the fact that loss of differentiated nuclei in aged muscle fibers
precedes muscle fiber atrophy (Brack et al., 2005).
Stem Cell Characteristics
Developmental Origins
Based on anatomical position and expression of Pax7, satellite
cell precursors first appear during late fetal stage (Relaix et al.,
2004, 2005). Lineage tracing approaches demonstrated that
the majority of adult Pax7+ satellite cells are formed from a
somitic origin of cells that transition through a Pax7+/Myod+ state
(Kanisicak et al., 2009; Lepper and Fan, 2010; Schienda et al.,
2006). It is clear that the number of Pax7+ cells declines during
development and postnatal growth (Schultz, 1989; White et al.,
2010). Therefore, not all embryonic Pax7+ cells will form the
self-renewing adult pool, but instead some will primarily
contribute to the growing myofiber. This suggests that some fetal
Pax7+/Myod+ cells differentiate and other Pax7+/Myod+ cells
form the adult satellite cell pool. Myod is considered a master
regulator of myogenesis (Weintraub et al., 1991). Based on
germline mutants, Myod is required for satellite cell differentiation but not for the formation of the satellite cell pool (Chargé
et al., 2008; Rudnicki et al., 1992). In vitro experiments demonstrate that subsets of myogenic progenitors lose Myod and
return to a quiescent state (Halevy et al., 2004; Olguin and Olwin,
2004; Yoshida et al., 1998; Zammit et al., 2004). Moreover, selfrenewing adult satellite cells transiently express Myod prior to
niche repopulation during repair (Shea et al., 2010). Therefore,
Pax7+/Myod+ precursors are able to form the satellite cell pool
providing that Myod is repressed. Based on studies with a
Myf5CreYFP reporter, it was demonstrated that the majority
(90%) of the adult satellite cell pool is formed from a Myf5+
precursor (Kuang et al., 2007). However, the formation of the
satellite cell pool in germline Myf5 nulls suggests that Myf5 is
not required for satellite cell formation; compensation by Myod
cannot be excluded (Gensch et al., 2008; Haldar et al., 2008).
While there are multiple caveats to consider when interpreting
these studies, including the contribution of non-Cre-recombined
cell populations, these results suggest that the adult satellite
506 Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc.
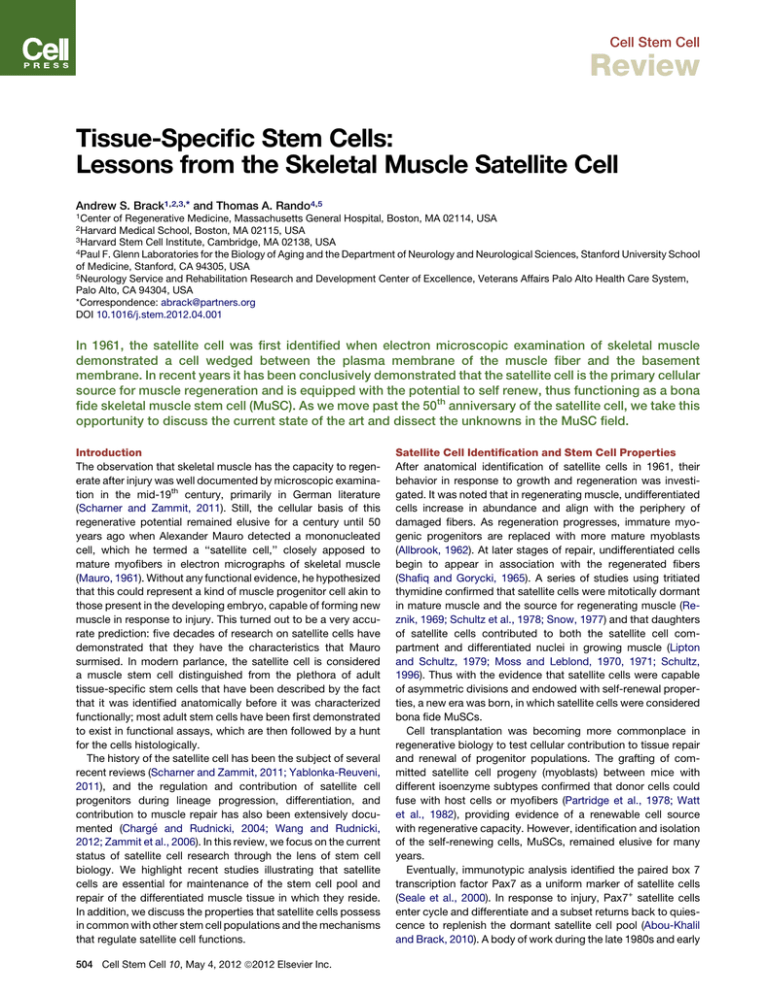
Figure 2. MuSC Heterogeneity
Origins of the MuSC pool. SC precursors (Pax7CreER+) located in the myotome
begin expressing Pax7 (red) at E10.5, and most express Myf5+ and Myod+
before occupancy into the niche. During early postnatal growth (P0–P7),
a subset of alkaline phosphatase (AP+)-derived pericytes as detected with
APCre (gray) express Pax7 (red) and occupy the MuSC niche (dark red). A
subset of AP+ pericytes is capable of contributing to myofiber differentiation
(dark red myonuclei). Whether pericytes that commit to myogenic fusion
express Pax7 during their lineage progression is unknown (thick red arrows).
cell pool is formed from precursors that are under different
transcriptional control. Contribution from the extrinsic environment may also participate in differential regulation of satellite
cell precursors.
While the adult satellite cell pool is formed from Pax7+ embryonic precursors, this does not preclude a model whereby an
alternative source of cells express Pax7 and home to the satellite
cell niche. Using immunotypic markers (CD34+/Sca1+) in combination with donor cell marking for transplantation studies, it
has been demonstrated that a subset of PICs (PW1+ Pax7
interstitial cells) self-renew and contribute to myofibers and
Pax7+ satellite cells in injured adult muscle (Mitchell et al.,
2010). Moreover, myogenic contribution of PICs was Pax7
dependent and temporally restricted to postnatal growing
muscle. Based on lineage tracking, a subset of alkaline phosphatase (AP)-expressing pericytes indelibly marked in postnatal
mice contributed to the formation of the adult Pax7+ satellite
cell compartment (Dellavalle et al., 2011). Therefore the origin
of the adult satellite cell pool may be heterogeneous (Figure 2).
In the future, it will be important to dissect the unique properties
and lineage relationship between pericytes and PICs that
express Pax7 relative to Pax7-derived satellite cells.
Asymmetric Cell Divisions
While asymmetric cell divisions are one of the fundamental characteristics of stem cells underlying the process of self-renewal,
stem cells may undergo self-renewal by virtue of symmetric
divisions (Tajbakhsh et al., 2009). As long as only one daughter
of a symmetric cell division is instructed to differentiate, the
stem cell pool can be maintained while differentiated progeny
are produced. Historically, there were no seminal observations
that provided evidence to either support or refute asymmetric
cell divisions in the satellite cell lineage, and it was only in the
past decade that this has been the focus of studies in the
MuSC field.
The first evidence of asymmetric cell divisions came from
studies of the role of Notch signaling during satellite cell activation and proliferative amplification. It was found that the Notch
inhibitory protein Numb was asymmetrically segregated in progenitors undergoing cell division and that Numb was localized
Cell Stem Cell
Review
Figure 3. Nonrandom Segregation of Chromosomes and
Asymmetric Fate Determination
The satellite cell pool is composed of primitive (Pax7hi, green) and lineage
primed (Pax7lo, gray) subsets. Pax7hi cells are in a dormant (less metabolically
active) state. Pax7lo satellite cells are lineage primed. After cytokinesis,
satellite cell daughters can each inherit some chromosomes bearing newer
(purple) or older (dark green) template strands. Pax7hi subsets undergo
nonrandom segregation of chromosomes, whereby one daughter contains
exclusively chromosomes bearing older template strands, while its sister
contains only chromosomes bearing newer template strands. In contrast,
Pax7lo cells undergo random segregation of chromosomes ensuring that each
daughter cell inherits an older and newer template strand. Subsets of Pax7hi
and Pax7lo are capable of multiple rounds of self-renewal (curved arrows) and
differentiation (blue cells), but Pax7hi cells are endowed with enhanced selfrenewal capability. Daughter cells containing newer template strands express
high levels of Numb, Myod, and Dek1 and are biased to differentiate (blue cell).
Pax7hi cells can give rise to Pax7lo, but not vice versa, suggesting a hierarchical relationship in the satellite cell pool based on Pax7 expression. In
addition to cell fate determination, nonrandom segregation of chromosomes
may act to protect genome integrity during cell proliferation. Because of low
metabolic output of primitive satellite cells, they may be protected from
oxidative damage. Lineage-primed satellite cells are capable of self-renewal
but may be acutely sensitive to proliferative demands and other forms of
genotoxic insults.
to one pole of dividing cells, perpendicular to the plane of cell
division (Conboy and Rando, 2002). This asymmetric Numb
localization is reminiscent of what had been previously
described in specific lineages during Drosophila development
(Petersen et al., 2002; Zhong et al., 1996). The result of such
an asymmetric segregation in the satellite cell lineage is the
inheritance of Numb by one daughter and not the other, the
former being destined to differentiate and the latter remaining
an undifferentiated progenitor (Conboy and Rando, 2002). The
asymmetric segregation of Numb was subsequently investigated during satellite cell activation, and asymmetric segregation of Numb was also detected in cells prior to the onset of
differentiation (Shinin et al., 2009). Other proteins, such as
Myod (Zammit et al., 2004) and Dek (Cheung et al., 2012), are
asymmetrically segregated in activated satellite cells, and those
proteins are more highly expressed in cells that have progressed
further along the myogenic lineage.
Asymmetric cell divisions have also been suggested in relation
to the aforementioned distinction of satellite cell subsets based
on developmental history of Myf5 expression (Kuang et al.,
2007). In this model, satellite cells undergo asymmetric cell divisions, giving rise to two daughters, one being another stem cell
(still with no history of Myf5 gene expression) and the other
becoming part of the larger pool of satellite cells (and expressing
the Myf5 transcript). In this case, there is no direct evidence as
yet of an asymmetric segregation of any specific protein or transcript in the mother cell, and the asymmetry may instead be
a divergent cell fate dictated by the different environments of
the two daughters. This is particularly likely given the observation
that daughters exhibiting divergent fates, one self-renewing and
the other committing toward differentiation, were much more
frequent when the plane of division was perpendicular to the
axis of the myofiber (Kuang et al., 2007). By contrast, divisions
that occurred parallel to the myofiber axis were much more likely
to give rise to two daughters with identical characteristics as
opposed to divergent fates, suggesting that the local environment of the satellite cell niche might be dictating the fate of
satellite cell progeny.
Yet another asymmetry that has been described is the asymmetric segregation of sister chromatids as satellite cells divide
and the population expands (Conboy et al., 2007; Shinin et al.,
2006). Recent evidence suggests that a subset of satellite cells,
in fact those with characteristics of long-term stem cells, are
more likely to exhibit nonrandom sister chromatid segregation
(Rocheteau et al., 2012). This further supports the notion that
asymmetric segregation of sister chromatids might be a property
of stem cells as originally proposed (Figure 3; Cairns, 1975).
Although the functional significance of this remains theoretical,
the proposed function is to segregate DNA strands that have
been damaged during replication to the more differentiated
daughter and reserve for the self-renewing stem cells those
strands that served as templates during the previous round of
cell division, thus acquiring few replication-induced errors (Charville and Rando, 2011). Although this teleological function has
not been demonstrated and there may be detrimental consequences of template strand segregation during aging (Charville
and Rando, 2011), it is supported by the fact that the oldest
template strands segregate with the less differentiated satellite
cell daughter (Conboy et al., 2007; Shinin et al., 2006).
Satellite Cell Heterogeneity
It is becoming more apparent that adult stem cell populations are
heterogeneous. Heterogeneity in the adult satellite cell pool
has been demonstrated based on multiple criteria, such as
expression profile (Beauchamp et al., 2000; Rocheteau et al.,
2012), proliferation kinetics in vitro (Day et al., 2009), self-renewal
potential (Kuang et al., 2007), and molecular regulation (Kitamoto
and Hanaoka, 2010; Kuang et al., 2007; Shea et al., 2010). Functional heterogeneity within a pool of adult stem cells can arise
from differentially specified subsets that retain distinct properties during cellular division or evolution of a subset of cells
derived from a single homogeneous cell population that will
emerge during cellular division.
It is widely accepted that Pax7 expression declines in differentiating progenitors (Zammit et al., 2004). Evidence for varied
Pax7 levels within the satellite cell pool was recently demonstrated via a transgenic GFP reporter of Pax7 transcript (Rocheteau et al., 2012). Functional analysis of satellite cells at extreme
ends of the Pax7 expression distribution demonstrated that
Pax7hi cells had reduced metabolic activity and slower cell cycle
entry kinetics, whereas Pax7lo cells were primed to differentiate
in vitro. Although cells with lower Pax7 expression appeared to
be more prone to differentiation, all Pax7+ cells could support
more than six serial transplantations, demonstrating that both
subsets of satellite cells possess remarkable regenerative
capacity and the ability to self-renew. Using an inducible Cre/
lox system, Pax7 was deleted from satellite cells in growing
postnatal muscle and adult muscle prior to injury. The results
Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc. 507
Cell Stem Cell
Review
demonstrated that Pax7 is essential for satellite cell function
during early postnatal growth and is dispensable for adult
muscle tissue repair (Lepper et al., 2009). Given that a subset
of postnatal Pax7+ cells seeds the adult Pax7+ pool, it supports
the hypothesis that there is a small subset of postnatal Pax7+
cells that evolve during the selective pressure of muscle growth
to propagate satellite cells that function independently of Pax7. It
raises the possibility that functionally distinct satellite cell
subsets can interconvert for selective advantage under conditions of high cellular demand as observed in spermatogonial
stem cells (Nakagawa et al., 2007, 2010).
Adult stem cells with limited proliferative history are endowed
with greater stem cell capability than more frequently dividing
counterparts (Foudi et al., 2009; Wilson et al., 2008), suggesting
that stem cell self-renewal capacity may decline in proportion
with the number of divisions a stem cell has undergone in its
history. Interestingly, subsets of presumptive satellite cells in
growing postnatal muscle divide with slower proliferation
kinetics, based on tritiated thymidine uptake (Schultz, 1996).
These data suggest that one level of functional heterogeneity
in the satellite cell pool may exist based on their proliferative
history. In dystrophic muscle, disease progression correlates
with proliferative capacity of satellite cells, suggesting that
restricting proliferative output of stem cells relative to their
downstream progeny may extend self-renewal capacity and
ameliorate disease pathogenesis (Sacco et al., 2010). Whether
functional heterogeneity across a pool of satellite cells is stable
once specified or adaptive based on cellular demand, it is clear
that the satellite cell pool is functionally heterogeneous. The
challenge in the future is to determine how molecular heterogeneity at the cell-intrinsic and -extrinsic levels instructs functional
diversity within the satellite cell pool.
Regulation of Satellite Cell Function
Stem Cell Niche
The stem cell niche refers to the microenvironment that maintains ‘‘stemness’’ (Schofield, 1978). The attributes of the niche
as originally conceptualized were (1) a defined anatomical site,
(2) a location where stem cells could reproduce, (3) a place
where differentiation is inhibited, and (4) a space that also limits
the numbers of stem cells. Therefore, the niche is a protector
of stem cell number and function, restraining proliferation
and differentiation of stem cells, and maintaining a quiescent
phenotype.
The location of the satellite cell, i.e., residing in a depression in
the plasmalemma and beneath the basal lamina of the muscle
fiber, provided a defined anatomical site of the putative MuSC
(Mauro, 1961). The hypothesis that the muscle fiber is a satellite
cell niche is supported by evidence generated from single
muscle fiber experiments. Removal of the myofiber plasmalemma drives quiescent satellite cells into cycle, suggesting
a role in inhibition of mitogen-induced cell cycle entry (Bischoff,
1986a). Quiescence is a conserved property of stem cells mediated by the niche (Orford and Scadden, 2008). Studies on freshly
isolated single muscle fibers have shown that a subset of quiescent satellite cells can proliferate and return back to quiescence
when in contact with the single muscle fiber, whereas a larger
subset commits to differentiation but their fusion is inhibited
(Bischoff, 1986a; Olguin and Olwin, 2004; Zammit et al., 2004).
508 Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc.
Therefore the muscle fiber fulfills three of Schoffield’s criteria
of a stem cell niche. Whether the muscle fiber constrains stem
cell numbers is to be determined.
In response to injury, the muscle fiber degenerates, which
probably leads to niche destruction and a loss of inhibitory
signals. Besides losing inhibitory factors that restrict proliferation
and differentiation from the degenerated niche, muscle injury
also promotes the release of stimulatory factors present at
the basal lamina of the muscle fiber that drive proliferation and
differentiation (Bischoff, 1986b; Sheehan and Allen, 1999). The
observation that microenvironment stiffness is a regulator of
stem cell potential and fate decisions suggests that maintenance
of stemness from the niche is regulated at many levels (Engler
et al., 2006; Gilbert et al., 2010). Resolving the signals that drive
self-renewal versus differentiation will require a careful characterization of the basal and apical aspects of the niche (Figure 4A).
The satellite cell niche may be composed of different cell
types, as observed for other stem cell compartments (Morrison
and Spradling, 2008). Besides the muscle fiber, there are other
muscle-resident cells in close proximity to the satellite cell,
such as Ang1-expresssing endothelial cells (Abou-Khalil et al.,
2009; Christov et al., 2007). It is becoming clear that other cell
types, such as fibro-adipogenic progenitors (FAPs) and TCF4+
fibroblasts, influence satellite cell behavior in contexts of
regeneration and growth (Joe et al., 2010; Murphy et al., 2011).
It remains to be determined whether such cell types constitute
the niche and therefore regulate stemness or function as
paracrine agents involved in proliferation and differentiation of
satellite cell progeny (Figure 4A). As cell-specific Cre drivers
become more readily available, it will be possible and essential
to determine the cell types and mode of regulation that
contribute to a functional satellite cell niche.
Signaling Pathway Regulation of Satellite Cell Function
A balance between extrinsic cues and intracellular signals
converge to preserve stem cell function. Over the past 50 years,
many excellent studies have demonstrated that multiple
extrinsic signaling pathways, such as IGF, FGF, Wnt, Notch,
BMP, and TGF-b, function in the activation of satellite cells, their
downstream progeny, and their lineage progression (Kuang
et al., 2008). More recently, the signaling pathways that modulate functions specific to stem cells, such as maintenance of
quiescence during homeostasis, reversible quiescence and
self-renewal after proliferation, asymmetric fate decisions, and
symmetric expansion of stem cells, are becoming more defined
(Figure 4B).
It was recently shown that active Notch signaling is required to
maintain satellite cells in the quiescent state, implying a role of
niche-derived Notch ligand that binds to a Notch receptor on
the quiescent satellite cell (Bjornson et al., 2011; Mourikis
et al., 2011). In these studies, Rbp-j, the downstream transcriptional coactivator in the Notch pathways, was deleted from adult
satellite cells in uninjured muscle. This led to activation and
ectopic differentiation of satellite cells, possibly in the absence
of cell cycle entry and therefore bypassing the transient amplifying (TA) progenitor stage (Bjornson et al., 2011; Mourikis
et al., 2011). Therefore, not only is RBP-J important for restricting
cell cycle entry, it also argues that in nonquiescent satellite
cells, RBP-J, possibly as a mediator of Notch1 signaling, may
be required for normal step-wise lineage progression (Conboy
Cell Stem Cell
Review
Figure 4. Regulation of MuSC Functions in Satellite
Cells
(A) The MuSC niche. The satellite cell (red) resides in
a quiescent state in contact with the plasmalemma (brown)
of the myofiber and basal lamina (black) in a milieu of
inhibitory (white arrows) and stimulatory (red arrows)
factors that retain satellite cells in a stem cell state and
inhibit their differentiation. Other cells in close proximity to
satellite cells in vivo such as TCF4+ fibroblasts, FAPs,
PICs, and pericytes may constitute components of the
MuSC niche and signal to the satellite cell and vice versa.
(B) Schematic of MuSC regulation. Satellite cells transition
from quiescence into a transient amplification stage; most
progress along a myogenic lineage to differentiate while
a subset self-renew and return back to quiescence (thick
blue arrows). Markers denoting each stage of lineage
progression are shown in black, and molecules required
for distinct satellite cell functions are shown in red.
Quiescent satellite cells express Spry1, Notch-3, and
miR-489. RBP-J and Myf5 are expressed in quiescent
and cycling satellite cells. RBP-J and miR-489 (red) are
required to retain satellite cells in quiescence. Spry1 and
Notch-3 are required in cycling satellite cells for their return
to quiescence and homeostasis of satellite cell pool after
injury. Myf5 is required for normal transient amplification of
progenitors. Myod, Myogenin, and Myosin Heavy Chain
(MyHC) are required for differentiation. Normal step-wise
lineage progression of satellite cells depends on RBP-J
(thin blue arrow), possibly through modulation of Notch-1
signaling.
and Rando, 2002). That the satellite cell pool is lost when the TA
stage is bypassed has implications for understanding the relationship between self-renewal and differentiation potential of
downstream progenitors within the stem cell hierarchy.
To replenish the satellite cell pool after injury, stem cells return
back to quiescence after proliferating. Our understanding of
reversion back to quiescence in vivo is limited. Based on
in vitro experiments it is becoming apparent that multiple
signaling pathways are actively involved in promoting satellite
cell quiescence. Activation of the Ang1/Tie2 signaling complex
promotes the return to quiescence of myoblasts in vitro (AbouKhalil et al., 2009). P38/MAPK pathway has also been implicated
in regulating quiescence of satellite cells (Jones et al., 2005).
Finally, Myostatin, a secreted growth factor belonging to the
TFG-b family, was shown to negatively regulate quiescence
and the return to quiescence of satellite cells in vitro (McCroskery
et al., 2003; McFarlane et al., 2008). Together these data illustrate a critical role of growth factor signaling in the return of
cycling satellite cell progenitors back to a quiescent state.
Further in vivo analysis and genetic approaches that directly
target satellite cells will clarify the signaling cascades that regulate the maintenance of quiescence and return to quiescence
after proliferation.
Recently, signaling through Notch-3 was found to negatively
regulate satellite cell pool size in regenerating muscle (Kitamoto
and Hanaoka, 2010). Whether this is regulated at the cellautonomous level of the satellite cell or by a niche-based
mechanism will require cell-specific genetic mutants. Using a
satellite cell-specific mutant for Spry1, it was demonstrated
that Spry1, an inhibitor of growth factor signaling, is required to
restore satellite cell pool size after injury (Shea et al., 2010).
This suggests that a balance between inhibitory and stimulatory
cues from the microenvironment is required for quiescence to be
achieved. One can theorize that Spry1 and other intracellular
growth factor inhibitors help to dampen the stimulatory factors
at the basal lamina to direct fate toward quiescence and the
repression of differentiation. The challenge in the future is to
identify niche-derived inhibitory signals that promote and retain
stemness after injury.
Stem cells possess a unique ability to divide symmetrically or
asymmetrically depending on tissue requirements (Tajbakhsh
et al., 2009). Noncanonical Wnt signaling through the Wnt7AFrz7-Vangl2 cascade was recently implicated in driving symmetric expansion of satellite cells located on single muscle fibers
in vitro (Le Grand et al., 2009). It will be interesting to unravel
the relationship between asymmetric divisions via Numb and
symmetric divisions via Wnt7A-Vangl2 that occur to control
stem cell expansion and differentiation.
In general, the cellular output within a pool of cells in response
to manipulation of signaling cascades is not equivalent. Through
loss-of-function approaches, it has been demonstrated that
satellite cells differentially respond to manipulation of signaling
molecules such as Spry1 and Notch-3 (Kitamoto and Hanaoka,
2010; Shea et al., 2010). It will be important to decipher whether
heterogeneous cell signaling requirements are due to extrinsic
differences, such as localization of satellite cells in discrete
niches, or to cell-intrinsic differences, based on lineage relationships.
While knowledge of the signaling cascades that regulate stem
cell properties of satellite cells is progressing, it is likely that more
Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc. 509
Cell Stem Cell
Review
pathways participate than have been identified. During cell
division and lineage progression, signaling molecules are used
reiteratively. For example, Numb is partitioned to initially allow
asymmetric fate of neural precursors and subsequently to
maintain progenitors (Petersen et al., 2004). Likewise, Numb
may be important for satellite cell self-renewal and also, at a
later stage of myogenic lineage progression, for regulating the
divergent fates of proliferating progenitors (Conboy and Rando,
2002; Jory et al., 2009; Shinin et al., 2006). Therefore, while
canonical Wnt, FGF, and BMP signaling cascades participate
in myogenic lineage progression and differentiation (Kuang
et al., 2008), it may be that they are also deployed in some
fashion to direct MuSC properties.
Epigenetic Regulation of Satellite Cell Function
Based on what we know about extrinsic cues controlling stem
cell function, the role of the stem cell niche cannot be underestimated. However, more stable modes of regulation may also
maintain key functions of satellite cells. Control of the function
of stem cells, particularly embryonic stem cells (ESCs), has
focused on regulatory mechanisms at the level of epigenetics,
namely the ensemble of heritable changes in gene function
that occur without modifications of the primary DNA sequence
(Bird, 2007). Such changes include DNA methylation and
chromatin structural modifications mediated by histone modifications and nucleosome positioning. Not too long after the
identification of the satellite cell, electron micrographs demonstrated that there are changes in chromatin organization in
satellite cells from adult muscle and growing muscle consistent
with their transition from a quiescent to a proliferative state
(Church, 1969). As our knowledge in the field of epigenetics
becomes more sophisticated, it is becoming appreciated that
the regulators of epigenetic states in stem cells include mediators of DNA methylation and demethylation, microRNAs and
other noncoding RNAs, and modifiers of histones, including
acetylases, deacetylases, methylases, and demethylases. This
field is redefining cellular states at a molecular level that are
much more varied and complex and probably reflect the
dynamic interaction of stem cells with their environment resulting in greater functional heterogeneity than was previously
envisioned.
It is likely that epigenetic states will better define such key
satellite cell features as prolonged quiescence and lineage
fidelity. It is also likely that DNA and histone modifications
will underlie many of the changes in aged satellite cells that
account for age-related declines in functionality and rejuvenation
through exposure to the systemic environment (Brack et al.,
2007; Conboy et al., 2005). Although there has been extensive
research on the epigenetic control of myogenesis, primarily
using the C2C12 myoblast cell line (Juan et al., 2011), studies
in satellite cells have been limited because of the need for
large numbers of cells for such analysis. Advances in both
satellite cell purification and methodologies for genome- and
epigenome-wide analyses of limited cell numbers will allow for
rapid advances in these areas in the coming years.
There have, however, been studies of regulators of epigenetic
states in satellite cells. It was shown that Pax7 functions with
the Wdr5-Ash2L-MLL2 histone methyltransferase (HMT) complex to direct methylation of histone H3 lysine 4 (H3K4). Binding
of the Pax7-HMT complex resulted in H3K4 trimethylation of
510 Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc.
chromatin at the Myf5 locus (McKinnell et al., 2008), suggesting
that Pax7 may act through chromatin modifications to stably
and hereditably maintain the myogenic program. Conversely,
the regulation of Pax7 expression may be determined by the
regulation of the repressive Polycomb repressive complex 2
(PRC2) and its enzymatic component, EZH2 (Palacios et al.,
2010), suggesting a network providing stability of the myogenic
program related to Pax7 expression.
The regulation of myogenesis by microRNAs has likewise
focused mainly on developmental myogenesis and the regulation of myogenic differentiation (Braun and Gautel, 2011). Recent
studies have also examined the role of miRNAs in the regulation
of quiescent satellite cells. miR-206 was recently shown to target
Pax3 in quiescent satellite cells, accounting for the differential
expression in Pax3 in cellular subsets (Boutet et al., 2012). This
study also revealed that alternate polyadenylation of the Pax3
transcript is an important determinant not only of satellite cell
heterogeneity but also of the susceptibility of the Pax3 transcript
to regulation by any miRNA (Boutet et al., 2012). Another microRNA, miR-489, was recently shown to be highly expressed in
quiescent satellite cells and to regulate specifically the quiescent
state by targeting the transcript of the Dek gene, a gene known to
be important for cell cycle regulation and alternative splicing
(Cheung et al., 2012). Knockdown of miR-489 in vivo led to
spontaneous activation of quiescent satellite cells, thus demonstrating the importance of a stable miRNA network for maintaining the quiescent state.
Conclusions and Perspectives
The last fifty years have led to a remarkable understanding of
the satellite cell. It is widely accepted that the satellite cell is
essential for regenerative myogenesis and can maintain itself
after injury. It has been demonstrated that the muscle fiber
constitutes a major functional component of the satellite cell
niche. More recently, experiments have illustrated the functional
heterogeneity within the satellite cell pool. As we move forward,
what will the next fifty years bring?
Remarkably, we do not know whether satellite cells maintain
themselves or differentiate to maintain muscle tissue during
normal daily wear and tear. This information is critical as biologists devise strategies to harness skeletal muscle strength of
the ever-expanding human aged population.
To date, direct experimental evidence is lacking to determine
whether stem cell number is limiting. If MuSCs have a finite
capacity, then a quorum will be required to functionally repair
muscle tissue and maintain homeostasis. In the context of
regenerating a tissue, such as skeletal muscle, it may be too
simplistic to consider MuSC number and function as independent entities. Rather, there is probably a cooperative relationship between MuSC number and function in response to
a regenerative insult. For example, in the presence of few
MuSCs, a greater functional demand will be imposed on those
rare cells, leading to their exhaustion. In contrast, increasing
the number of MuSCs in a muscle will lessen the burden on
each cell imposed by the regenerative insult. In scenarios of
limiting satellite cell number, other MuSCs may participate,
contributing as facultative stem cells. Other cell types such as
PICs, mesangioblasts, and pericytes are able to contribute to
muscle tissue repair (Péault et al., 2007). Further analysis is
Cell Stem Cell
Review
needed to determine whether such cell types function as
facultative stem cells that are dependent on cellular context.
Understanding whether their contribution is dependent on the
presence of a functional pool of satellite cells may reveal further
complexities of the regulation of skeletal muscle repair. Development of genetic tools to ablate fractions of satellite cells will
illustrate the intimate cooperative relationship between satellite
cell number and function and their interdependency with other
contributing cell types.
Technological advances in recent years have provided
greater resolution of stem cell heterogeneity. With the advent
of fluorescent reporters of proliferative history, it is now
possible to isolate and compare such heterogeneous cells to
dissect their function and molecular regulation (Foudi et al.,
2009; Tumbar et al., 2004). Marking satellite cells based on
Cre drivers has proven invaluable for tracking them and their
contribution to growth and repair (Lepper and Fan, 2010; Lepper et al., 2011; Shea et al., 2010). More recent advances
through the use of multicolor Cre reporters or genetic barcoding utilized in other stem cell compartments have provided
improved cellular resolution that facilitates the tracking of
clonally diverse cells in a population to be studied (Lu et al.,
2011; Snippert et al., 2010). Such techniques reveal that the
level of stem cell heterogeneity is more dynamic and context
dependent than previously appreciated (Lu et al., 2011). Information gleaned from such approaches will allow the relationship between molecular and functional heterogeneity to be
resolved.
The anatomical location of the satellite cell provides a landmark for the satellite cell niche. Based on its conceptual framework, although the niche impacts stem cell properties of the
satellite cell, the mechanism by which this is achieved remains
a mystery. In the future, functional components of the satellite
cell niche will be identified through technological advances in
live imaging, microdissection, and biochemical analysis. As
our understanding of satellite cell heterogeneity evolves, it will
be interesting to identify whether there are distinct niches that,
in some way, establish satellite cell heterogeneity. Advances in
our knowledge of cell-intrinsic mechanisms that regulate stem
cell function, such as epigenetic regulation of satellite cells,
will illustrate the communication between the extrinsic environment and intrinsic effectors to specify and maintain stem cell
states.
In conclusion, the seminal observations of the satellite cell in
its niche made by Alexander Mauro almost fifty years ago have
spawned many great advances in our understanding of this
tissue-specific stem cell. It is apparent that there is greater
heterogeneity in the satellite cell pool in terms of cellular subsets
that specify the pool, their function, and the signaling cascades
that regulate them. We are just beginning to unravel the microenvironmental influences that mediate stem cell properties and
how epigenetic regulation governs stable properties of satellite
cells during homeostasis and repair.
REFERENCES
Abou-Khalil, R., and Brack, A.S. (2010). Muscle stem cells and reversible
quiescence: the role of sprouty. Cell Cycle 9, 2575–2580.
Abou-Khalil, R., Le Grand, F., Pallafacchina, G., Valable, S., Authier, F.J., Rudnicki, M.A., Gherardi, R.K., Germain, S., Chretien, F., Sotiropoulos, A., et al.
(2009). Autocrine and paracrine angiopoietin 1/Tie-2 signaling promotes
muscle satellite cell self-renewal. Cell Stem Cell 5, 298–309.
Allbrook, D. (1962). An electron microscopic study of regenerating skeletal
muscle. J. Anat. 96, 137–152.
Amini-Nik, S., Glancy, D., Boimer, C., Whetstone, H., Keller, C., and Alman,
B.A. (2011). Pax7 expressing cells contribute to dermal wound repair, regulating scar size through a b-catenin mediated process. Stem Cells 29, 1371–
1379.
Beauchamp, J.R., Heslop, L., Yu, D.S., Tajbakhsh, S., Kelly, R.G., Wernig, A.,
Buckingham, M.E., Partridge, T.A., and Zammit, P.S. (2000). Expression of
CD34 and Myf5 defines the majority of quiescent adult skeletal muscle satellite
cells. J. Cell Biol. 151, 1221–1234.
Bentzinger, C.F., Wang, Y.X., and Rudnicki, M.A. (2012). Building muscle:
molecular regulation of myogenesis. Cold Spring Harb. Perspect. Biol. 4,
a008342.
Bird, A. (2007). Perceptions of epigenetics. Nature 447, 396–398.
Bischoff, R. (1986a). Proliferation of muscle satellite cells on intact myofibers in
culture. Dev. Biol. 115, 129–139.
Bischoff, R. (1986b). A satellite cell mitogen from crushed adult muscle. Dev.
Biol. 115, 140–147.
Bjornson, C.R., Cheung, T.H., Liu, L., Tripathi, P.V., Steeper, K.M., and Rando,
T.A. (2011). Notch signaling is necessary to maintain quiescence in adult
muscle stem cells. Stem Cells 30, 232–242.
Boutet, S.C., Cheung, T.H., Quach, N.L., Liu, L., Prescott, S., Edalati, A., Iori,
K., and Rando, T.A. (2012). Alternative polyadenylation mediates microRNA
regulation of muscle stem cell function. Cell Stem Cell 10, 327–336.
Brack, A.S., and Rando, T.A. (2007). Intrinsic changes and extrinsic influences
of myogenic stem cell function during aging. Stem Cell Rev. 3, 226–237.
Brack, A.S., Bildsoe, H., and Hughes, S.M. (2005). Evidence that satellite
cell decrement contributes to preferential decline in nuclear number from
large fibres during murine age-related muscle atrophy. J. Cell Sci. 118, 4813–
4821.
Brack, A.S., Conboy, M.J., Roy, S., Lee, M., Kuo, C.J., Keller, C., and Rando,
T.A. (2007). Increased Wnt signaling during aging alters muscle stem cell fate
and increases fibrosis. Science 317, 807–810.
Braun, T., and Gautel, M. (2011). Transcriptional mechanisms regulating
skeletal muscle differentiation, growth and homeostasis. Nat. Rev. Mol. Cell
Biol. 12, 349–361.
Cairns, J. (1975). Mutation selection and the natural history of cancer. Nature
255, 197–200.
Chargé, S.B., and Rudnicki, M.A. (2004). Cellular and molecular regulation of
muscle regeneration. Physiol. Rev. 84, 209–238.
Chargé, S.B., Brack, A.S., Bayol, S.A., and Hughes, S.M. (2008). MyoD- and
nerve-dependent maintenance of MyoD expression in mature muscle fibres
acts through the DRR/PRR element. BMC Dev. Biol. 8, 5.
Charville, G.W., and Rando, T.A. (2011). Stem cell ageing and non-random
chromosome segregation. Philos. Trans. R. Soc. Lond. B Biol. Sci. 366,
85–93.
ACKNOWLEDGMENTS
Cheung, T.H., Quach, N.L., Charville, G.W., Liu, L., Park, L., Edalati, A., Yoo,
B., Hoang, P., and Rando, T.A. (2012). Maintenance of muscle stem-cell quiescence by microRNA-489. Nature 482, 524–528.
This work was supported by grants from the NIH (R01 AR060868 to A.S.B. and
P01 AG036695, R37 AG23806, [MERIT Award], and R01 AR056849 to T.A.R.).
We thank Jenna Norton for artwork and Josef Christensen for critical reading of
the manuscript.
Christov, C., Chrétien, F., Abou-Khalil, R., Bassez, G., Vallet, G., Authier, F.J.,
Bassaglia, Y., Shinin, V., Tajbakhsh, S., Chazaud, B., and Gherardi, R.K.
(2007). Muscle satellite cells and endothelial cells: close neighbors and privileged partners. Mol. Biol. Cell 18, 1397–1409.
Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc. 511
Cell Stem Cell
Review
Church, J.C. (1969). Satellite cells and myogenesis; a study in the fruit-bat
web. J. Anat. 105, 419–438.
Collins, C.A., Olsen, I., Zammit, P.S., Heslop, L., Petrie, A., Partridge, T.A.,
and Morgan, J.E. (2005). Stem cell function, self-renewal, and behavioral
heterogeneity of cells from the adult muscle satellite cell niche. Cell 122,
289–301.
Conboy, I.M., and Rando, T.A. (2002). The regulation of Notch signaling
controls satellite cell activation and cell fate determination in postnatal
myogenesis. Dev. Cell 3, 397–409.
Conboy, I.M., Conboy, M.J., Wagers, A.J., Girma, E.R., Weissman, I.L., and
Rando, T.A. (2005). Rejuvenation of aged progenitor cells by exposure to
a young systemic environment. Nature 433, 760–764.
Conboy, M.J., Karasov, A.O., and Rando, T.A. (2007). High incidence of nonrandom template strand segregation and asymmetric fate determination in
dividing stem cells and their progeny. PLoS Biol. 5, e102.
Day, K., Paterson, B., and Yablonka-Reuveni, Z. (2009). A distinct profile of
myogenic regulatory factor detection within Pax7+ cells at S phase supports
a unique role of Myf5 during posthatch chicken myogenesis. Dev. Dyn. 238,
1001–1009.
Dellavalle, A., Maroli, G., Covarello, D., Azzoni, E., Innocenzi, A., Perani, L.,
Antonini, S., Sambasivan, R., Brunelli, S., Tajbakhsh, S., et al. (2011). Pericytes
resident in postnatal skeletal muscle differentiate into muscle fibres and
generate satellite cells. Nat. Comm. 2, 499.
Engler, A.J., Sen, S., Sweeney, H.L., and Discher, D.E. (2006). Matrix elasticity
directs stem cell lineage specification. Cell 126, 677–689.
Kitamoto, T., and Hanaoka, K. (2010). Notch3 null mutation in mice causes
muscle hyperplasia by repetitive muscle regeneration. Stem Cells 28, 2205–
2216.
Kuang, S., Kuroda, K., Le Grand, F., and Rudnicki, M.A. (2007). Asymmetric
self-renewal and commitment of satellite stem cells in muscle. Cell 129,
999–1010.
Kuang, S., Gillespie, M.A., and Rudnicki, M.A. (2008). Niche regulation of
muscle satellite cell self-renewal and differentiation. Cell Stem Cell 2, 22–31.
Le Grand, F., Jones, A.E., Seale, V., Scimè, A., and Rudnicki, M.A. (2009).
Wnt7a activates the planar cell polarity pathway to drive the symmetric expansion of satellite stem cells. Cell Stem Cell 4, 535–547.
Lepper, C., and Fan, C.M. (2010). Inducible lineage tracing of Pax7-descendant cells reveals embryonic origin of adult satellite cells. Genesis 48,
424–436.
Lepper, C., Conway, S.J., and Fan, C.M. (2009). Adult satellite cells and
embryonic muscle progenitors have distinct genetic requirements. Nature
460, 627–631.
Lepper, C., Partridge, T.A., and Fan, C.M. (2011). An absolute requirement for
Pax7-positive satellite cells in acute injury-induced skeletal muscle regeneration. Development 138, 3639–3646.
Lipton, B.H., and Schultz, E. (1979). Developmental fate of skeletal muscle
satellite cells. Science 205, 1292–1294.
Lu, R., Neff, N.F., Quake, S.R., and Weissman, I.L. (2011). Tracking single
hematopoietic stem cells in vivo using high-throughput sequencing in conjunction with viral genetic barcoding. Nat. Biotechnol. 29, 928–933.
Foudi, A., Hochedlinger, K., Van Buren, D., Schindler, J.W., Jaenisch, R.,
Carey, V., and Hock, H. (2009). Analysis of histone 2B-GFP retention reveals
slowly cycling hematopoietic stem cells. Nat. Biotechnol. 27, 84–90.
Mauro, A. (1961). Satellite cell of skeletal muscle fibers. J. Biophys. Biochem.
Cytol. 9, 493–495.
Gensch, N., Borchardt, T., Schneider, A., Riethmacher, D., and Braun, T.
(2008). Different autonomous myogenic cell populations revealed by ablation
of Myf5-expressing cells during mouse embryogenesis. Development 135,
1597–1604.
McCarthy, J.J., Mula, J., Miyazaki, M., Erfani, R., Garrison, K., Farooqui, A.B.,
Srikuea, R., Lawson, B.A., Grimes, B., Keller, C., et al. (2011). Effective fiber
hypertrophy in satellite cell-depleted skeletal muscle. Development 138,
3657–3666.
Gilbert, P.M., Havenstrite, K.L., Magnusson, K.E., Sacco, A., Leonardi, N.A.,
Kraft, P., Nguyen, N.K., Thrun, S., Lutolf, M.P., and Blau, H.M. (2010).
Substrate elasticity regulates skeletal muscle stem cell self-renewal in culture.
Science 329, 1078–1081.
McCroskery, S., Thomas, M., Maxwell, L., Sharma, M., and Kambadur, R.
(2003). Myostatin negatively regulates satellite cell activation and self-renewal.
J. Cell Biol. 162, 1135–1147.
Haldar, M., Karan, G., Tvrdik, P., and Capecchi, M.R. (2008). Two cell lineages,
myf5 and myf5-independent, participate in mouse skeletal myogenesis. Dev.
Cell 14, 437–445.
Halevy, O., Piestun, Y., Allouh, M.Z., Rosser, B.W., Rinkevich, Y., Reshef, R.,
Rozenboim, I., Wleklinski-Lee, M., and Yablonka-Reuveni, Z. (2004). Pattern
of Pax7 expression during myogenesis in the posthatch chicken establishes
a model for satellite cell differentiation and renewal. Dev. Dyn. 231, 489–502.
Hughes, S.M., and Schiaffino, S. (1999). Control of muscle fibre size: a crucial
factor in ageing. Acta Physiol. Scand. 167, 307–312.
Joe, A.W., Yi, L., Natarajan, A., Le Grand, F., So, L., Wang, J., Rudnicki, M.A.,
and Rossi, F.M. (2010). Muscle injury activates resident fibro/adipogenic
progenitors that facilitate myogenesis. Nat. Cell Biol. 12, 153–163.
Jones, N.C., Tyner, K.J., Nibarger, L., Stanley, H.M., Cornelison, D.D., Fedorov, Y.V., and Olwin, B.B. (2005). The p38alpha/beta MAPK functions as
a molecular switch to activate the quiescent satellite cell. J. Cell Biol. 169,
105–116.
Jory, A., Le Roux, I., Gayraud-Morel, B., Rocheteau, P., Cohen-Tannoudji, M.,
Cumano, A., and Tajbakhsh, S. (2009). Numb promotes an increase in skeletal
muscle progenitor cells in the embryonic somite. Stem Cells 27, 2769–2780.
McFarlane, C., Hennebry, A., Thomas, M., Plummer, E., Ling, N., Sharma, M.,
and Kambadur, R. (2008). Myostatin signals through Pax7 to regulate satellite
cell self-renewal. Exp. Cell Res. 314, 317–329.
McKinnell, I.W., Ishibashi, J., Le Grand, F., Punch, V.G., Addicks, G.C., Greenblatt, J.F., Dilworth, F.J., and Rudnicki, M.A. (2008). Pax7 activates myogenic
genes by recruitment of a histone methyltransferase complex. Nat. Cell Biol.
10, 77–84.
Mitchell, K.J., Pannérec, A., Cadot, B., Parlakian, A., Besson, V., Gomes, E.R.,
Marazzi, G., and Sassoon, D.A. (2010). Identification and characterization of
a non-satellite cell muscle resident progenitor during postnatal development.
Nat. Cell Biol. 12, 257–266.
Montarras, D., Morgan, J., Collins, C., Relaix, F., Zaffran, S., Cumano, A.,
Partridge, T., and Buckingham, M. (2005). Direct isolation of satellite cells for
skeletal muscle regeneration. Science 309, 2064–2067.
Morrison, S.J., and Spradling, A.C. (2008). Stem cells and niches: mechanisms
that promote stem cell maintenance throughout life. Cell 132, 598–611.
Moss, F.P., and Leblond, C.P. (1970). Nature of dividing nuclei in skeletal
muscle of growing rats. J. Cell Biol. 44, 459–462.
Moss, F.P., and Leblond, C.P. (1971). Satellite cells as the source of nuclei in
muscles of growing rats. Anat. Rec. 170, 421–435.
Juan, A.H., Derfoul, A., Feng, X., Ryall, J.G., Dell’Orso, S., Pasut, A., Zare, H.,
Simone, J.M., Rudnicki, M.A., and Sartorelli, V. (2011). Polycomb EZH2
controls self-renewal and safeguards the transcriptional identity of skeletal
muscle stem cells. Genes Dev. 25, 789–794.
Mourikis, P., Sambasivan, R., Castel, D., Rocheteau, P., Bizzarro, V., and Tajbakhsh, S. (2011). A critical requirement for Notch signaling in maintenance
of the quiescent skeletal muscle stem cell state. Stem Cells 30, 243–252.
Kanisicak, O., Mendez, J.J., Yamamoto, S., Yamamoto, M., and Goldhamer,
D.J. (2009). Progenitors of skeletal muscle satellite cells express the muscle
determination gene, MyoD. Dev. Biol. 332, 131–141.
Murphy, M.M., Lawson, J.A., Mathew, S.J., Hutcheson, D.A., and Kardon, G.
(2011). Satellite cells, connective tissue fibroblasts and their interactions are
crucial for muscle regeneration. Development 138, 3625–3637.
512 Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc.
Cell Stem Cell
Review
Nakagawa, T., Nabeshima, Y., and Yoshida, S. (2007). Functional identification
of the actual and potential stem cell compartments in mouse spermatogenesis. Dev. Cell 12, 195–206.
Nakagawa, T., Sharma, M., Nabeshima, Y., Braun, R.E., and Yoshida, S.
(2010). Functional hierarchy and reversibility within the murine spermatogenic
stem cell compartment. Science 328, 62–67.
Olguin, H.C., and Olwin, B.B. (2004). Pax-7 up-regulation inhibits myogenesis
and cell cycle progression in satellite cells: a potential mechanism for selfrenewal. Dev. Biol. 275, 375–388.
Schultz, E. (1996). Satellite cell proliferative compartments in growing skeletal
muscles. Dev. Biol. 175, 84–94.
Schultz, E., Gibson, M.C., and Champion, T. (1978). Satellite cells are mitotically quiescent in mature mouse muscle: an EM and radioautographic study.
J. Exp. Zool. 206, 451–456.
Seale, P., Sabourin, L.A., Girgis-Gabardo, A., Mansouri, A., Gruss, P., and
Rudnicki, M.A. (2000). Pax7 is required for the specification of myogenic
satellite cells. Cell 102, 777–786.
Orford, K.W., and Scadden, D.T. (2008). Deconstructing stem cell self-renewal:
genetic insights into cell-cycle regulation. Nat. Rev. Genet. 9, 115–128.
Shafiq, S.A., and Gorycki, M.A. (1965). Regeneration in skeletal muscle of
mouse: some electron-microscope observations. J. Pathol. Bacteriol. 90,
123–127.
Palacios, D., Mozzetta, C., Consalvi, S., Caretti, G., Saccone, V., Proserpio, V.,
Marquez, V.E., Valente, S., Mai, A., Forcales, S.V., et al. (2010). TNF/p38a/
polycomb signaling to Pax7 locus in satellite cells links inflammation to the
epigenetic control of muscle regeneration. Cell Stem Cell 7, 455–469.
Shea, K.L., Xiang, W., LaPorta, V.S., Licht, J.D., Keller, C., Basson, M.A., and
Brack, A.S. (2010). Sprouty1 regulates reversible quiescence of a selfrenewing adult muscle stem cell pool during regeneration. Cell Stem Cell
6, 117–129.
Partridge, T.A., Grounds, M., and Sloper, J.C. (1978). Evidence of fusion
between host and donor myoblasts in skeletal muscle grafts. Nature 273,
306–308.
Sheehan, S.M., and Allen, R.E. (1999). Skeletal muscle satellite cell proliferation in response to members of the fibroblast growth factor family and hepatocyte growth factor. J. Cell. Physiol. 181, 499–506.
Péault, B., Rudnicki, M., Torrente, Y., Cossu, G., Tremblay, J.P., Partridge, T.,
Gussoni, E., Kunkel, L.M., and Huard, J. (2007). Stem and progenitor cells in
skeletal muscle development, maintenance, and therapy. Mol. Ther. 15,
867–877.
Sherwood, R.I., Christensen, J.L., Conboy, I.M., Conboy, M.J., Rando, T.A.,
Weissman, I.L., and Wagers, A.J. (2004). Isolation of adult mouse myogenic
progenitors: functional heterogeneity of cells within and engrafting skeletal
muscle. Cell 119, 543–554.
Petersen, P.H., Zou, K., Hwang, J.K., Jan, Y.N., and Zhong, W. (2002). Progenitor cell maintenance requires numb and numblike during mouse neurogenesis. Nature 419, 929–934.
Shinin, V., Gayraud-Morel, B., Gomès, D., and Tajbakhsh, S. (2006). Asymmetric division and cosegregation of template DNA strands in adult muscle
satellite cells. Nat. Cell Biol. 8, 677–687.
Petersen, P.H., Zou, K., Krauss, S., and Zhong, W. (2004). Continuing role
for mouse Numb and Numbl in maintaining progenitor cells during cortical
neurogenesis. Nat. Neurosci. 7, 803–811.
Shinin, V., Gayraud-Morel, B., and Tajbakhsh, S. (2009). Template DNA-strand
co-segregation and asymmetric cell division in skeletal muscle stem cells.
Methods Mol. Biol. 482, 295–317.
Relaix, F., Rocancourt, D., Mansouri, A., and Buckingham, M. (2004). Divergent functions of murine Pax3 and Pax7 in limb muscle development. Genes
Dev. 18, 1088–1105.
Relaix, F., Rocancourt, D., Mansouri, A., and Buckingham, M. (2005). A Pax3/
Pax7-dependent population of skeletal muscle progenitor cells. Nature 435,
948–953.
Reznik, M. (1969). Thymidine-3H uptake by satellite cells of regenerating
skeletal muscle. J. Cell Biol. 40, 568–571.
Snippert, H.J., van der Flier, L.G., Sato, T., van Es, J.H., van den Born, M.,
Kroon-Veenboer, C., Barker, N., Klein, A.M., van Rheenen, J., Simons, B.D.,
and Clevers, H. (2010). Intestinal crypt homeostasis results from neutral
competition between symmetrically dividing Lgr5 stem cells. Cell 143,
134–144.
Snow, M.H. (1977). Myogenic cell formation in regenerating rat skeletal
muscle injured by mincing. II. An autoradiographic study. Anat. Rec. 188,
201–217.
Rocheteau, P., Gayraud-Morel, B., Siegl-Cachedenier, I., Blasco, M.A., and
Tajbakhsh, S. (2012). A subpopulation of adult skeletal muscle stem cells
retains all template DNA strands after cell division. Cell 148, 112–125.
Starkey, J.D., Yamamoto, M., Yamamoto, S., and Goldhamer, D.J. (2011).
Skeletal muscle satellite cells are committed to myogenesis and do not
spontaneously adopt nonmyogenic fates. J. Histochem. Cytochem. 59, 33–46.
Rudnicki, M.A., Braun, T., Hinuma, S., and Jaenisch, R. (1992). Inactivation of
MyoD in mice leads to up-regulation of the myogenic HLH gene Myf-5 and
results in apparently normal muscle development. Cell 71, 383–390.
Tajbakhsh, S., Rocheteau, P., and Le Roux, I. (2009). Asymmetric cell divisions
and asymmetric cell fates. Annu. Rev. Cell Dev. Biol. 25, 671–699.
Sacco, A., Doyonnas, R., Kraft, P., Vitorovic, S., and Blau, H.M. (2008). Selfrenewal and expansion of single transplanted muscle stem cells. Nature
456, 502–506.
Sacco, A., Mourkioti, F., Tran, R., Choi, J., Llewellyn, M., Kraft, P., Shkreli, M.,
Delp, S., Pomerantz, J.H., Artandi, S.E., and Blau, H.M. (2010). Short telomeres and stem cell exhaustion model Duchenne muscular dystrophy in
mdx/mTR mice. Cell 143, 1059–1071.
Sambasivan, R., Yao, R., Kissenpfennig, A., Van Wittenberghe, L., Paldi, A.,
Gayraud-Morel, B., Guenou, H., Malissen, B., Tajbakhsh, S., and Galy, A.
(2011). Pax7-expressing satellite cells are indispensable for adult skeletal
muscle regeneration. Development 138, 3647–3656.
Scharner, J., and Zammit, P.S. (2011). The muscle satellite cell at 50: the
formative years. Skeletal Muscle 1, 28.
Schienda, J., Engleka, K.A., Jun, S., Hansen, M.S., Epstein, J.A., Tabin, C.J.,
Kunkel, L.M., and Kardon, G. (2006). Somitic origin of limb muscle satellite and
side population cells. Proc. Natl. Acad. Sci. USA 103, 945–950.
Tumbar, T., Guasch, G., Greco, V., Blanpain, C., Lowry, W.E., Rendl, M., and
Fuchs, E. (2004). Defining the epithelial stem cell niche in skin. Science 303,
359–363.
Wang, Y.X., and Rudnicki, M.A. (2012). Satellite cells, the engines of muscle
repair. Nat. Rev. Mol. Cell Biol. 13, 127–133.
Watt, D.J., Lambert, K., Morgan, J.E., Partridge, T.A., and Sloper, J.C. (1982).
Incorporation of donor muscle precursor cells into an area of muscle regeneration in the host mouse. J. Neurol. Sci. 57, 319–331.
Weintraub, H., Davis, R., Tapscott, S., Thayer, M., Krause, M., Benezra, R.,
Blackwell, T.K., Turner, D., Rupp, R., Hollenberg, S., et al. (1991). The myoD
gene family: nodal point during specification of the muscle cell lineage.
Science 251, 761–766.
White, R.B., Biérinx, A.S., Gnocchi, V.F., and Zammit, P.S. (2010). Dynamics
of muscle fibre growth during postnatal mouse development. BMC Dev.
Biol. 10, 21.
Schofield, R. (1978). The relationship between the spleen colony-forming cell
and the haemopoietic stem cell. Blood Cells 4, 7–25.
Wilson, A., Laurenti, E., Oser, G., van der Wath, R.C., Blanco-Bose, W.,
Jaworski, M., Offner, S., Dunant, C.F., Eshkind, L., Bockamp, E., et al.
(2008). Hematopoietic stem cells reversibly switch from dormancy to selfrenewal during homeostasis and repair. Cell 135, 1118–1129.
Schultz, E. (1989). Satellite cell behavior during skeletal muscle growth and
regeneration. Med. Sci. Sports Exerc. 21 (5, Suppl), S181–S186.
Yablonka-Reuveni, Z. (2011). The skeletal muscle satellite cell: still young and
fascinating at 50. J. Histochem. Cytochem. 59, 1041–1059.
Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc. 513
Cell Stem Cell
Review
Yoshida, N., Yoshida, S., Koishi, K., Masuda, K., and Nabeshima, Y. (1998).
Cell heterogeneity upon myogenic differentiation: down-regulation of MyoD
and Myf-5 generates ‘reserve cells’. J. Cell Sci. 111, 769–779.
Zammit, P.S., Partridge, T.A., and Yablonka-Reuveni, Z. (2006). The skeletal
muscle satellite cell: the stem cell that came in from the cold. J. Histochem.
Cytochem. 54, 1177–1191.
Zammit, P.S., Golding, J.P., Nagata, Y., Hudon, V., Partridge, T.A., and Beauchamp, J.R. (2004). Muscle satellite cells adopt divergent fates: a mechanism
for self-renewal? J. Cell Biol. 166, 347–357.
Zhong, W., Feder, J.N., Jiang, M.M., Jan, L.Y., and Jan, Y.N. (1996). Asymmetric localization of a mammalian numb homolog during mouse cortical
neurogenesis. Neuron 17, 43–53.
514 Cell Stem Cell 10, May 4, 2012 ª2012 Elsevier Inc.
Review series
Repairing skeletal muscle: regenerative
potential of skeletal muscle stem cells
Francesco Saverio Tedesco,1,2 Arianna Dellavalle,1 Jordi Diaz-Manera,1,3,4
Graziella Messina,1,5 and Giulio Cossu1,5
1Division
of Regenerative Medicine, San Raffaele Scientific Institute, Milan, Italy. 2Vita-Salute San Raffaele and Open University, Milan, Italy.
Santa Creu i Sant Pau, Neuromuscular Diseases Unit, Barcelona, Spain. 4Centro de Investigación Biomédica en Red
sobre Enfermedades Neurodegenerativas (CIBERNED), Madrid, Spain. 5Department of Biology, University of Milan, Milan, Italy.
3Hospital
Skeletal muscle damaged by injury or by degenerative diseases such as muscular dystrophy is able to regenerate
new muscle fibers. Regeneration mainly depends upon satellite cells, myogenic progenitors localized between
the basal lamina and the muscle fiber membrane. However, other cell types outside the basal lamina, such as
pericytes, also have myogenic potency. Here, we discuss the main properties of satellite cells and other myogenic
progenitors as well as recent efforts to obtain myogenic cells from pluripotent stem cells for patient-tailored cell
therapy. Clinical trials utilizing these cells to treat muscular dystrophies, heart failure, and stress urinary incontinence are also briefly outlined.
Introduction
It has been known for more than a century that skeletal muscle,
the most abundant tissue of the body, has the ability to regenerate new muscle fibers after it has been damaged by injury or as
a consequence of diseases such as muscular dystrophy (1). Muscle fibers are syncytial cells that contain several hundred nuclei
within a continuous cytoplasm. Therefore, whether the process of
regeneration depends upon the fusion of mononucleated precursor cells or upon the fragmentation of dying muscle fibers, which
release new cells, remained controversial for a long time, even after
the demonstration by Beatrice Mintz and Wilber Baker (2) that
multinucleated fibers are formed by the fusion of single cells. In
1961, Alexander Mauro (3) observed mononuclear cells between
the basal lamina that surrounds each muscle fiber and the plasma
membrane of the muscle fiber and named them satellite cells (SCs)
(Figure 1). SCs were later accepted to be, and are still considered
today, the main players in skeletal muscle regeneration. SCs also
contribute to the postnatal growth of muscle fibers, which in
adults contain approximately 6–8 times more nuclei than in neonates, all of them being irreversibly postmitotic.
In addition to SCs, other progenitors located outside the basal
lamina, including pericytes, endothelial cells, and interstitial cells,
have been shown to have some myogenic potential in vitro or after
transplantation. The developmental origin of these progenitors is
unclear, as is their lineage relationship with SCs, even though they
may feed, to some extent, into the SC compartment (4).
There is much interest in understanding the cellular and molecular mechanisms underlying skeletal muscle regeneration in different contexts because such knowledge might help in the development of cell therapies for diseases characterized by skeletal muscle
degeneration. These diseases include muscular dystrophy, the term
for a group of inherited disorders characterized by progressive
muscle wasting and weakness leading to a variable degree of mobility limitation, including confinement to a wheelchair and, in the
most severe forms, heart and/or respiratory failure (5). Many muscular dystrophies arise from loss-of-function mutations in genes
encoding cytoskeletal and membrane proteins, the most common
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 120:11–19 (2010). doi:10.1172/JCI40373.
and severe being Duchenne muscular dystrophy (DMD), which is
caused by mutations in the gene encoding dystrophin, an integral
part of a complex that links the intracellular cytoskeleton with the
extracellular matrix in muscle. Muscular dystrophies are some of
the most difficult diseases to treat, as skeletal muscle is composed
of large multinucleated fibers whose nuclei cannot divide. Consequently, cell therapy has to restore proper gene expression in hundreds of millions of postmitotic nuclei (6).
In this Review, we discuss recent work indicating the possible existence of a stem/progenitor cell compartment in adult muscle (see
also ref. 7) as well as studies related to the derivation of myogenic
cells from embryonic and induced pluripotent stem cells (PSCs)
for the development of new cell therapy strategies for diseases of
skeletal muscle. An overview of clinical trials based upon transplantation of skeletal muscle stem cells is also provided. Neither the role
of SCs in aging skeletal muscle nor the SC niche are discussed here
due to space constraints, and readers are directed to excellent recent
reviews on these topics by Suchitra Gopinath and Thomas Rando
(8) and Michael Rudnicki and colleagues (9), respectively.
SCs
Identification and characterization. The most stringent way to classify
cells as SCs remains by determining their anatomical location: SCs
are found underneath the basal lamina of muscle fibers, closely juxtaposed to the plasma membrane (3). SCs originate from somites
(10, 11), spheres of paraxial mesoderm that generate skeletal muscle,
dermis, and axial skeleton, but the exact progenitor that gives rise
to SCs remains to be identified. SCs are present in healthy adult
mammalian muscle as quiescent cells and represent 2.5%–6% of all
nuclei of a given muscle fiber. However, when activated by muscle
injury, they can generate large numbers of new myofibers within just
a few days (12). Quiescent SCs (13) express characteristic (although
not unique) markers. In the mouse, the most widely used of these
markers is the transcription factor paired box 7 (Pax7) (14), which
is essential for SC specification and survival (15). In contrast, Pax3
is expressed only in quiescent SCs in a few specific muscle groups
such as the diaphragm (16). The basic helix-loop-helix (bHLH) gene
myogenic regulatory factor 5 (Myf5) is expressed in the large majority of quiescent SCs, and for this reason, mice expressing nuclear
LacZ under the control of the Myf5 promoter (Myf5nlacZ/+ mice) have
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
11
review series
Figure 1
Asymmetric cell division during activation of SCs. This is a drawing representing the anatomy of a muscle fiber with adjacent small vessels.
SCs and other myogenic cells (pericytes and hematopoietic, endothelial, and interstitial cells) are depicted. SC activation in vivo is followed by
an asymmetric division, with Pax7, MyoD, and Myf5 being expressed in differentiating cells and Pax7 in cells returning to quiescence in order
to maintain a pool of progenitors (25, 41).
been useful for identifying and characterizing SCs (17). Many other
markers (18–29) have been identified and are listed in Table 1.
Some of these surface markers are useful for isolating “purified” SC
populations by cell sorting, but since each marker is not exclusively
expressed on SCs, a combination of different markers must be used.
Alternatively, transgenic mice such as those expressing GFP under
the control of promoters that drive the expression of genes encoding SC markers — for example, the Pax3 promoter — can be used
to isolate SCs (29–31). In humans, markers of both quiescent and
activated SCs do not fully correspond to those in the mouse, and
relatively little is known about them due to the difficulty of obtaining human tissue. For example, although CD34 is a marker of SCs
in mice, it does not mark SCs in human muscle (32); and M-cadherin is not as consistent a marker of SCs in humans as it is in mice.
Among the more reliable markers of SCs in human muscle is CD56,
although it also marks natural killer lymphocytes (33).
Activation. In response to a muscle injury, SCs are activated
and start to proliferate; at this stage, they are often referred to
as either myogenic precursor cells (mpc) or myoblasts (34, 35).
Several signals, deriving both from damaged fibers and infiltrating cells, are involved in SC activation, including HGF (36), FGF
(37), IGF (38), and NO (39).
The progression of activated SCs toward myogenic differentiation is mainly controlled by Myf5 and myogenic differentiation 1 (MyoD) (17) and is followed by fusion into regenerating fibers.
The whole process takes approximately 7 days in the mouse (40),
during which time SCs undergo different fates, giving rise to a few
Pax7+MyoD– cells, which return to quiescence (to maintain the
progenitor pool), and many Pax7+MyoD+ cells, which are commit12
ted to differentiation (41) (Figure 1). Notch signaling is thought to
regulate this process through promotion of asymmetric divisions,
although there is not agreement on the role of Numb (a Notch
inhibitor and cell-fate determinant) in inducing differentiation (42)
and sustaining self renewal (43). The occurrence of asymmetric cell
division is also supported by the identification of a subpopulation
of SCs able to retain BrdU after pulse-chase labeling, with some
cells displaying selective template DNA strand segregation during
mitosis (43, 44). In addition, Rudnicki and colleagues validated
the label-retention model of SCs and demonstrated that approximately 10% of Pax7+ mouse SCs had never expressed Myf5 and that
these cells remain adherent to the basal lamina during asymmetric
mitosis, generating one Pax7+Myf5– satellite “stem cell” and one
Pax7+Myf5+ SC “progenitor,” eventually destined to differentiate
(25) (Figure 1). The same group also elegantly described Wnt7a as
regulating the symmetric expansion of Pax7+Myf5– SCs (45).
Transplantation. Because of their features, SCs were considered
obvious candidates for a cell-therapy approach to treating muscular
dystrophy. Pioneer studies demonstrated that intramuscular injection of normal myoblasts (46) into mdx mice, which lack dystrophin and are a model for DMD, resulted in fusion with host fibers
and extensive dystrophin production. These studies led to several
clinical trials in the early 1980s (see Muscular dystrophies section for
details) that failed for a number of reasons, including poor survival
and migration of donor cells after transplantation and rejection of
the donor cells due to an immune response by the patients (47).
Many subsequent preclinical studies aimed to improve the survival, proliferation, and differentiation of the SCs after engraftment. For example, transplantation in dystrophic mouse mus-
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
review series
Table 1
SC markers
Marker
SC expression
Localization
Function
Prospective isolationA
Pax7
100% of quiescent and Nucleus
Transcription Pax7-GFP activated SCs
factor
Pax3
Quiescent SCs Nucleus
Transcription Pax3-GFP (only in a subset of muscles)
factor
Myf5
Most quiescent SCs and all Nucleus
Transcription Myf5-nLacZ
proliferating SCs and myoblasts
factor
Syndecan-3 and -4
98% of quiescent Membrane
Transmembrane Cell and activated SCs
heparan sulfate sorting
proteoglycan
VCAM-1
Quiescent and activated SCs
Membrane
Adhesion Cell molecule
sorting
c-met
Quiescent and activated SCs
Membrane
HGF receptor
Not used
Foxk1
Quiescent and activated SCs
Nucleus
Nuclear factor
Not used
Cd34
Quiescent and activated SCs
Membrane
Membrane Cell protein
sorting
M-cadherin
Quiescent and activated SCs; Membrane
Adhesion Not used
myoblasts
protein
Caveolin-1
Quiescent and activated SCs; Membrane
Membrane Not used
myoblasts
protein
α7 Integrin
Quiescent and activated SCs; Membrane
Adhesion Cell myoblasts
protein
sorting
β1 Integrin
Quiescent and activated SCs
Membrane
Adhesion Cell protein
sorting
Cd56
Quiescent and activated SCs; Membrane Homophilic binding Cell myoblasts
glycoprotein
sorting
SM/C2.6B
Quiescent and activated SCs; Unknown
Unknown
Cell myoblasts
sorting
Cxcr4
Subset of quiescent SCs
Membrane
SDF1 Cell receptor
sorting
Nestin
Around 98% of quiescent SCs Intermediate Intermediate Nestin and myoblasts
filament
filament protein
GFP
Expression in other tissues/cells
Ref
Absent
14
Melanocyte stem cells
Absent
16
Brain, dermis, BM, bone, smooth
muscle, tumors
Activated endothelial cells
18
Many tissues and tumors
Neurons
Hematopoietic, endothelial, mast, and dendritic cells
Absent
Endothelial fibrous and adipose tissue
Vessel-associated cells
Many tissues
Glia, neurons, and natural killer cells
Unknown
HSCs, vascular endothelial cells, and neuronal cells
Neuronal precursor cells
17
19
20
21
13
22
23
24
25
26
27
28
29
AProspective
BNovel
isolation: direct isolation of cells from tissue, usually based upon cytofluorimetric sorting with antibodies directed against cell surface markers.
monoclonal antibody directed against an unknown antigen present on SCs. Foxk1, forkhead box k1.
cles of a single muscle fiber that contained as few as seven SCs
led to an increasing number of new SCs that in turn generated
more than 100 new muscle fibers and could also be activated
after injury (48). This is a much more efficient way to generate new muscle fibers than transplantation of cultured SCs, in
which normally the number of donor-derived new fibers that are
generated is several orders of magnitude less than the number of
injected cells. Unfortunately, this method would be difficult to
translate into clinical protocols.
In the past few years, several groups have succeeded in prospectively isolating “pure” populations of SCs by using a combination of
different markers (Table 1), such as Pax3-GFP (30), CXCR4 and β1
integrin (49), α7 integrin and CD34 (50), or syndecan-3 and -4 (51). It is still unknown whether the different protocols allow isolation of the same cell population, enriched to different extents for
a more primitive “stem-like” fraction. However, all these studies
revealed that freshly isolated cells have a much greater capacity to
generate dystrophin-expressing fibers in mdx mice than the same
cells after in vitro expansion (30); the simplest explanation for
this is that the “stem” fraction either dies in culture or generates
differentiation-committed SCs. Importantly, a short culture period of 3–4 days, without subculture, allowed lentiviral-mediated
transduction and thus genetic correction of SCs freshly isolated
from mdx mice, without compromising myogenic potency in vivo
(52). Despite these encouraging results, previous unsolved problems still prevent the use of SCs to systemically treat patients with
muscular dystrophy: in particular, the inability of these cells to
cross the endothelial wall makes systemic delivery impossible and
prevents possible healing of the diaphragm and cardiac muscles,
both critical for patient survival (34).
Other myogenic progenitors
The availability of cell-autonomous, tissue-specific transgenic markers allowed the unequivocal demonstration of the existence of myogenic progenitors originating from tissues other than skeletal muscle (53). Upon transplantation (either BM transplantation [BMT] or
direct injection into skeletal muscle), these cells, identified by transgene expression, participate in muscle regeneration in wild-type
and/or dystrophic mice (Figures 1 and 2; Table 2) and eventually
enter the SC pool. The possibility that myogenic differentiation may
depend upon fusion (and hence exposure to the dominant activity
of MyoD) remains, but for skeletal muscle, this would be part of the
physiological mechanism that creates the tissue. Below, we describe
briefly some examples of these unorthodox myogenic cells.
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
13
review series
cal β-gal–positive nuclei were detected in regenerated fibers, demonstrating that murine BM contains
transplantable progenitors that can be recruited to an
injured muscle through the circulation, where they
participate in muscle repair (56). This opened the
possibility of treating muscular dystrophy by BMT,
but work in mice indicated that, unfortunately, the
frequency of this event was too low, even in a chronically regenerating dystrophic muscle and even if the
side population (SP) progenitor–enriched fraction
was transplanted (57, 58). To address this issue, subsequent experiments were directed to identifying a rare,
potentially highly myogenic progenitor, but those
studies have so far had modest success. The hematopoietic, CD45+ fraction of the BM has been identified
as the cell population with myogenic potential (59),
and retrospective analysis in a DMD patient that had
undergone BMT confirmed the persistence of donorderived skeletal muscle cells over a period of many
years, again at very low frequency (60). Together, these
data suggested that HSCs or a yet-to-be-identified cell
that expresses several markers in common with true
HSCs has myogenic potential. More recent approaches confirmed that hematopoietic cells have myogenic
potential but disagreed on the stage at which myogenic differentiation would occur. One study reported
that the progeny of a single mouse hematopoietic progenitor cell can both reconstitute the hematopoietic
system and contribute, at low frequency, to muscle
regeneration (61). However, a similar study showed
that in response to injury, CD45+ hematopoietic progenitors contribute to regenerating mouse skeletal
muscle through fusion of mature myeloid cells rather
than fusion of the HSCs (62).
A subpopulation of circulating cells expressing CD133
(also known as Ac133), a well-characterized marker of
HSCs, also expresses early myogenic markers (63). When
injected into the circulation of dystrophic scid/mdx mice, CD133+ cells have been found to contribute to
muscle repair, recovery of force, and replenishment of
Figure 2
the SC pool. The group that discovered this also isolatDerivation of different stem cells for possible use in skeletal muscle regeneration.
The figure shows a flow chart with the sources of different myogenic stem cells. ed a population of muscle-derived stem cells (MDSCs)
+
The possibility of deriving the same cells from a reprogrammed cell of the dermis expressing CD133 (64). Furthermore, when CD133
is also outlined (blue boxes and arrows). Once obtained, the stem cells can be cells from DMD patients were genetically corrected by
lentivirus-mediated exon skipping for dystrophin exon
characterized, expanded, genetically corrected, and transplanted.
51, these cells were able to mediate morphological and
functional recovery in scid/mdx mice (64). Thus, differCells from ectoderm: neural stem cells. To date, neural stem cells ent subpopulations of hematopoietic cells, whose characterization
(both murine and human) are the only ectoderm-derived stem cells is still incomplete, seem to possess myogenic potency, but none of
that have been shown to differentiate into skeletal muscle when these exhibit this property at high frequency.
cocultured with skeletal myoblasts or transplanted into regeneratCells derived from mesoderm (other than hematopoietic cells). Many difing skeletal muscle (54). Interestingly, cells expressing Myf5 exist ferent types of mesoderm stem/progenitor cells have been shown
in the brain and spinal cord, suggesting a cryptic potency that to exhibit myogenic potential, usually after drug treatment, genetbecomes apparent in vitro (55).
ic modification, or coculture with SCs or myoblasts. In some cases,
Hematopoietic cells. The first evidence of in vivo generation of evidence of in vivo myogenesis has been documented. The list of
skeletal muscle from BM cells was reported in 1998 (56) in a such cells includes mesenchymal stem cells (MSCs), multipotent
study that used transgenic mice expressing a nuclear LacZ under adult progenitor cells (MAPCs), MDSCs, CD133+ cells, mesoanthe control of the striated muscle promoter myosin light chain gioblasts (MABs), endothelial progenitor cells (EPCs), and adi1/3 fast (MLC3f). After transplantation of BM from the trans- pose-derived stem cells, all of which are briefly described below or
genic mice and subsequent injury to the host muscle, unequivo- in Table 2. More details can be found in previous reviews (6, 32).
14
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
review series
Table 2
Properties of myogenic progenitors other than SCs
Cell type
CD133+
EPC
HSC
MAB
MADS
MAPC
MDSC
MEC
MSC
Origin
Proliferation
In vitro myogenic differentiation
Dystrophin expression in vivo
Systemic delivery
Ref
Blood/skeletal muscle
Vessel wall
BM
Vessel wall
Adipose tissue
Vessel wall
Skeletal muscle
Vessel wall
Vessel wall
Low/high
Low
Low
High
High
High
High
High
High
Induced by muscle cells /spontaneous
Induced by muscle cells
Induced by muscle cells
Induced by muscle cells/spontaneous
Spontaneous
Induced by Aza-cytidine
Induced by muscle cells
Spontaneous
Induced by Aza-cytidine
Yes
Not tested
Yes
Yes
Yes
Not tested
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Not done
Not done
Not done
Not done
Not done
64
71
56
68
74
32
32
73
65
MEC, myoendothelial cell.
MSCs have been shown to be capable of skeletal myogenesis (65).
However, recently, Perlingeiro and colleagues demonstrated that
although Pax3 activation enabled the in vitro differentiation of
murine and human MSCs into MyoD+ myogenic cells, these cells
failed to cause functional muscle recovery in mdx mice, despite good
engraftment (66). The reason for this failure remains unclear.
MABs are vessel-associated progenitors (67) that express early
endothelial markers when isolated from the embryo and pericyte
markers when isolated from postnatal tissues. Since MABs are able
to cross the vessel wall and are easily transduced with lentiviral
vectors, they have been used in preclinical models of cell therapy
for muscular dystrophy. Intraarterial delivery of either wild-type
or genetically corrected MABs morphologically and functionally
ameliorated the dystrophic phenotype of mice lacking α-sarcoglycan (Sgca), which model limb-girdle muscular dystrophy 2D, a
muscular dystrophy caused by mutations in the SGCA gene (68). In
addition, intraarterial delivery of wild-type postnatal canine MABs
resulted in extensive recovery of dystrophin expression and ameliorated pathologic muscle morphology and function in golden
retriever dogs that model DMD (69). Similar cells have been isolated from human postnatal skeletal muscle and shown to represent
a subset of pericytes and to give rise to dystrophin-positive muscle
fibers when transplanted into scid/mdx mice (70). Based on these
studies, a phase I clinical trial with MAB allotransplantation in
DMD patients is planned for the near future.
Initially identified as circulating cells expressing CD34 and
fetal liver kinase-1 (Flk-1; also known as VEGFR2), EPCs (71)
were shown to be transplantable and to participate actively in
angiogenesis in various physiologic and pathologic conditions
(71). It was then shown that freshly isolated human cord blood
CD34+ cells injected into ischemic adductor muscles gave rise
not only to endothelial but also to skeletal muscle cells in mice
(72). Consistent with this, Péault and colleagues have identified
cells with high myogenic potential within the vascular endothelium of human adult skeletal muscle (73). These human myoendothelial cells, which represent less than 0.5% of the cells in
dissociated adult skeletal muscles, expressed both myogenic
and endothelial cell markers (CD56 +CD34 +CD144 +CD45 –),
exhibited long term proliferation, had a normal karyotype, and
when transplanted into scid mice, were able to regenerate fibers
in injured muscle (73).
Human multipotent adipose-derived stem (hMADS) cells, isolated from adipose tissue, differentiate into adipocytes, osteo
blasts, and myoblasts (74). Recently, the myogenic and muscle
repair capacities of hMADS cells have been enhanced by transient
expression of MyoD (75). The easy availability of their tissue
source, their strong capacity for expansion ex vivo, their multipotent differentiation, and their immune-privileged behavior suggest that hMADS cells could be an important tool for cell-mediated therapy for skeletal muscle disorders.
PSCs for muscle regeneration
PSCs can give rise to all cell types. Among the various PSCs, we
limit our discussion to ES cells (76, 77) and induced pluripotent
stem (iPS) cells (78), as they are, in practice, the two types of PSC
most commonly used to direct differentiation toward a given cell
type, skeletal muscle, for the purpose of this Review. PSCs hold
tremendous hopes for the cell therapy of degenerative diseases;
and iPS cells further offer the possibility of deriving patient-specific PSCs (79) to study diseases in vitro (80) and the potential for
genetic correction for autologous cell therapy.
Turning PSCs into skeletal muscle. A critical step in establishing
the potential of PSCs as a therapeutic for skeletal muscle diseases
is the development of techniques for the differentiation of these
cells into tissue-specific progenitors suitable for transplantation.
The most elegant way to obtain specific transplantable cell types
is by exposing them in vitro to the same molecules that control
their in vivo commitment during embryogenesis (reviewed in ref.
81), although the empirical testing of molecules and substrates
could generate equally useful cells.
Seminal studies from the mid-1990s described how ES cell–
derived embryoid bodies (EBs), tridimensional structures formed
when ES cells are grown in the absence of an embryonic fibroblast
feeder layer, contained multinucleated muscle fibers that express
skeletal muscle myosin heavy-chain genes (82, 83). Ten years later,
it was documented for the first time in vivo that intramuscular
injection of mouse EBs cocultured with mdx muscle–derived progenitors in mdx mice led to the production of a few clusters of
donor-derived dystrophin-positive fibers (84). Recently, Studer
and coworkers have derived transplantable myoblasts from
human ES cells (85), while Chang and colleagues have generated
transplantable satellite-like cells from mouse ES cells (86). Upon
transplantation into mdx mice, the latter cells have been found to
regenerate acutely and chronically injured muscle and could also
be secondarily transplanted (86). MyoD-mediated myogenic conversion of ES cell–derived cells is another intriguing approach,
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
15
review series
Table 3
Clinical trials of myoblast transplantation in DMD patients
Author
Year
Blind
Number Pt age
of pts
Drugs administered
Number of myoblasts (×106)
Expression of dystrophin
Law
1991
No
3
9–10
Cyclosporine
8
3/3 by IHC and WB at 3 months
Huard
1992
No
4
13–20
None
25
3/4 by IHC and WB at 4 months (up to
80% fibers positive)
Law
1992
No
21
6–14
Cyclosporine
5000
Not evaluated
Gussoni
1992
Yes
8
6–10
None
100
3/8 by PCR at 1 month
Karpati
1993
Yes
8
6–10 Cyclophosphamide
55
0/8 by IHC at 1-year follow-up
Tremblay 1993
Yes
5
4–9
None
100–240
3/4 by IHC at 1 month (up to 36% fibers positive);
1/4 by IHC at 6 months
Morandi
1995
Yes
3
6–9
Cyclosporine
55
0/3 by IHC or PCR
Mendell
1995
Yes
12
5–9
Cyclosporine
110
1/12 by IHCA
Miller
1997
Yes
10
5–10
Cyclosporine
100
3/10 by PCR at 1 month; 1/10 at 6 months
Neumeyer 1998
Yes
6B
>21
Cyclosporine
73-100
0/3, by IHCC
Skuk
2006
Yes
9
8–17
Tacrolimus
30 8/9 patients by IHCC 3.5%–26% fibers
expressed dystrophin
Improved strength
Ref
3/3 patients at 3 months
3/4 patients
95
43% muscles examined improved
Not evaluated
3/8
98
99
97
0/5
100
Not evaluated
0/12
0/10
101
102
103
0/3
Not evaluated
94
104
96
Pt, patient; IHC, immunohistochemistry; WB, Western blot. AMultiple injection site protocol. BStudy performed with Becker muscular dystrophy patients.
CIHC was performed using a peptide-specific antibody recognizing only donor dystrophin.
whose proof of principle dates to the early 1990s (87). On this
front, Perlingeiro and colleagues recently achieved in vivo skeletal muscle differentiation from purified PDGFRα+Flk1– progenitors isolated from EBs generated from mouse ES cells containing
an inducible Pax3 gene (88). At the time of writing, there are no
reports on the generation of myogenic cells from iPS cells, but
assuming that the present protocols for ES cells can be adapted
for iPS cells, we believe that in the next months, papers on this
topic are likely to appear.
Muscle regeneration from ES/iPS cells via mesodermal progenitors.
There is a large body of evidence indicating the existence of nonconventional muscle progenitors (see Other myogenic progenitors).
Thus, the possibility of deriving mesodermal myogenic progenitors (89) from ES/iPS cells offers an alternative route for cell therapy for skeletal muscle regeneration. This approach has the advantage of producing myogenic progenitors that could be delivered
systemically through the circulation.
In 2005, Studer and colleagues described the derivation from ES
cells of mesenchymal precursors (90) that differentiated in vitro into
different mesodermal lineages, including skeletal muscle. A recent
article described the derivation from mouse ES cells of PDGFRα+
mesodermal progenitors that, after in vivo transplantation, expressed
markers of SCs and contributed to muscle regeneration (91).
Issues to be solved. Despite the excitement for these novel strategies
for treating degenerative muscular conditions, a number of safety
and efficacy issues, some common to other cells (immunogenicity,
survival, and differentiation), some prominent for ES/iPS cells,
such as tumor formation, still need to be solved. For example, cytofluorimetric purification of committed progenitors (88) may dramatically decrease the possibility of transplanting undifferentiated
tumorigenic cells. The use of standardized protocols for generat16
ing iPS cells (92), together with stringent tumorigenic assays for
the derived cell types, will certainly be a fundamental step toward
their clinical application.
Skeletal muscle stem cells: past and
ongoing clinical trials
Until now only SCs, and, to a very minor extent, CD133+ cells have
been used in human clinical trials. The pathologies treated include
forms of muscular dystrophy, heart failure associated with myocardial infarction (HFMI), and stress urinary incontinence (SUI).
Muscular dystrophies. In 1990, Peter Law and collaborators reported the first SC transplant in a 9-year-old boy affected by DMD,
showing safety and dystrophin production (93). Soon after, 11
clinical trials in DMD patients were conducted using intramuscular injection of SCs (Table 3) (94–104). Although there were no
adverse effects, new dystrophin production was demonstrated in
many but not all cases and clinical benefit in none (6, 105). This
is not surprising considering that intramuscular injection in several locations of a single muscle (or at most a few muscles) cannot
elicit a general effect, although improved strength of the injected
muscles was detected in 15% of the patients treated. Treating muscular dystrophies by intramuscular injection of myoblasts presents
several problems that have not been solved yet. First, intramuscular injected cells distribute locally, implying that a huge number
of injections will have to be performed in order to treat a complete
muscle (96). Second, immune responses toward the injected SCs
have been described, even in the case of major histocompatibility locus coincidence. Finally, the rapid death of most of the SCs
in the first 72 hours after injection has been extensively reported (106, 107). Subsequent experimentation has been devoted to
solving these problems, and a phase I clinical trial has been com-
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
review series
pleted (104). Although encouraging results have been obtained,
this method is still limited by the impossibility of delivering myoblasts systemically through the circulation. Recently, Torrente and
colleagues reported the first CD133+ cell transplant (108). They
designed a phase I double-blind trial with an autologous transplant of unmodified, and thus still dystrophic, muscle-derived
CD133+ cells in 8 boys affected by DMD exclusively to test safety;
and indeed, no adverse events were reported.
Heart failure. Among different options to treat heart infarction,
skeletal muscle–derived myoblasts were considered an optimal
cell therapy, as they can be easily obtained from the same patient
(avoiding the need for long-term immune suppression), rapidly
expanded in vitro, and transplanted back in the patient heart. Preclinical experiments performed in animal models demonstrated
their ability to engraft correctly, survive in postinfarction scars,
differentiate into contractile skeletal muscle cells, and improve
heart function (109–111), possibly also because they release angiogenic factors. Unfortunately, in these models, myoblasts were not
able to differentiate into cardiomyocytes and did not integrate
electrically with the host cardiomyocytes (112, 113). Despite this
significant problem, several nonrandomized clinical trials using
myoblasts to treat the infarcted heart demonstrated thickening of
the LV, an increase in LV ejection fraction, and prevention of LV
dilatation, with clinical improvement in some patients (114–120). Histological analysis showed the presence of new myofibers in the
scar zone expressing skeletal muscle–specific myosin heavy chain
(121). In general, the transplantation procedure was clinically well
tolerated, but a high incidence of arrhythmias, some of which were
fatal, was reported. In 2007, the results of the MAGIC study, an
international phase II double-blind trial were published (122).
Ninety-seven patients affected by HFMI were randomized to receive
placebo, a low dose of myoblasts (400 × 106 cells), or a high dose
of myoblasts (800 × 106 cells). LV end-diastolic volumes decreased
substantially in patients receiving myoblasts, supporting a role
for myoblasts in remodeling of the heart muscle. The incidence
of secondary events, including arrhythmias, was not different
between the groups, although all patients received the antiarrhythmic agent amiodarone and were implanted with a cardioverter
defibrillator. The results of the CAuSMIC (123) and SEISMIC
trials (124) have demonstrated safety and some clinical improvement. Ongoing trials include the MARVEL study, a phase II/III randomized, double-blind, placebo-controlled trial for which
results are expected during the fall of 2009.
SUI. SC-derived myoblasts have also been used as cell therapy for
individuals with SUI, which is characterized by the loss of small
amounts of urine upon coughing, laughing, sneezing, exercising,
or other movements that increase intraabdominal pressure. Myoblasts may represent an interesting approach for the treatment of
this disease (125), as the main cause of SUI is impaired tone of the
urethral smooth and striated muscle, which is associated with atrophy of the supporting structures of the urethra, the mucosa, and
1.Carlson BM. The regeneration of skeletal muscle. A
review. Am J Anat. 1973;137(2):119–149.
2.Mintz B, Baker WW. Normal mammalian muscle
differentiation and gene control of isocitrate
dehydrogenase synthesis. Proc Natl Acad Sci U S A.
1967;58(2):592–598.
3.Mauro A. Satellite cells of skeletal muscle fibers. J Biophys Biochem Cytol. 1961;9:493–495.
4.Cossu G, Biressi S. Satellite cells, myoblasts and
other occasional myogenic progenitors: possible
vascular submucosa (126, 127). Treatment of SUI with SC-derived
myoblasts has been performed using two different strategies: injection of autologous myoblasts to improve the sphincter tone; and
injection of myoblasts together with fibroblasts (isolated by differential adhesion from the same muscle biopsy) to both improve
sphincter tone and treat mucosa atrophy. Until now, all published
studies have been nonrandomized, open studies, demonstrating a
remarkable clinical improvement in most of the patients treated
(127, 128). Moreover, structural and functional techniques have
demonstrated thickening of the urinary sphincter and an increase
in maximum urethral closure pressure. The onset of improvement
is not immediate and may be delayed up to six months after cell
injection; however, the benefit, once obtained, lasts for a long period of time, at least up to 12 months (126). Cystoscopic studies
have not demonstrated overgrowth of myoblasts nor obstruction
of the lower urinary tract (129). Unfortunately, these successful
results have not been confirmed yet in a randomized study.
Conclusions
This is an exciting period for those studying the biology of skeletal muscle stem cells and seeking to harness the information for
clinical applications. By learning more about SCs and other mesodermal skeletal muscle progenitors, we can learn how to better
use them to repair muscle. The main limitations of SCs are loss of
“stemness” upon culture and an inability to cross the vessel wall
for systemic delivery. Limitations for other cell types are incomplete characterization and their overall minor myogenic potency.
Nevertheless, a phase I clinical trial with donor-derived MABs is
planned for the end of 2010, given the fact that, because of extensive preclinical work, these cells appear at the moment as the best
candidates for the cell therapy of muscular dystrophy. Moreover,
the terrific prospective of deriving countless autologous, genetically corrected iPS cells from patients certainly will set the stage
for future cell therapies. Finally, we should remember that SCs
have already been used for clinical trials for DMD, myocardial
infarction, and SUI. The last seems to be a case of success for this
approach and a situation from which we may also learn in order
to redirect efforts toward therapies for myocardial infarction and
muscular dystrophies, which have thus far been less successful.
Acknowledgments
Work in the authors’ laboratory is supported by grants from the
European Community (OptiStem, Angioscaff, and MyoAmp),
European Research Council, Téléthon, Association Française contre les Myopathies, Duchenne Parent Project, CureDuchenne, and
the Italian Ministries of Research (FIRB) and Health.
Address correspondence to: Giulio Cossu, Division of Regenerative
Medicine, San Raffaele Scientific Institute, 58 via Olgettina, 20132
Milan, Italy. Phone: 39-02-2643-4954; Fax: 39-02-2643-4621; E-mail: cossu.giulio@hsr.it.
origin, phenotypic features and role in muscle
regeneration. Semin Cell Dev Biol. 2005;16(45):623–631.
5.Emery AE. The muscular dystrophies. Lancet.
2002;359(9307):687–695.
6.Cossu G, Sampaolesi M. New therapies for Duchenne muscular dystrophy: challenges, prospects and
clinical trials. Trends Mol Med. 2007;13(12):520–526.
7.Buckingham M, Montarras D. Skeletal muscle stem
cells. Curr Opin Genet Dev. 2008;18(4):330–336.
8.Gopinath SD, Rando TA. Stem cell review series:
aging of the skeletal muscle stem cell niche. Aging
Cell. 2008;7(4):590–598.
9.Kuang S, Gillespie MA, Rudnicki MA. Niche regulation of muscle satellite cell self-renewal and differentiation. Cell Stem Cell. 2008;2(1):22–31.
10.Shi X, Garry DJ. Muscle stem cells in development, regeneration, and disease. Genes Dev.
2006;20(13):1692–1708.
11.Sambasivan R, Tajbakhsh S. Skeletal muscle
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
17
review series
stem cell birth and properties. Semin Cell Dev Biol.
2007;18(6):870–882.
12.Whalen RG, Harris JB, Butler-Browne GS, Sesodia
S. Expression of myosin isoforms during notexininduced regeneration of rat soleus muscles. Dev
Biol. 1990;141(1):24–40.
13.Beauchamp JR, et al. Expression of CD34 and Myf5
defines the majority of quiescent adult skeletal muscle satellite cells. J Cell Biol. 2000;151(6):1221–1234.
14.Zammit PS, et al. Pax7 and myogenic progression in skeletal muscle satellite cells. J Cell Sci.
2006;119(pt 9):1824–1832.
15.Kuang S, Charge SB, Seale P, Huh M, Rudnicki MA.
Distinct roles for Pax7 and Pax3 in adult regenerative myogenesis. J Cell Biol. 2006;172(1):103–113.
16.Relaix F, et al. Pax3 and Pax7 have distinct and
overlapping functions in adult muscle progenitor
cells. J Cell Biol. 2006;172(1):91–102.
17.Tajbakhsh S, et al. Gene targeting the myf-5 locus
with nlacZ reveals expression of this myogenic factor in mature skeletal muscle fibres as well as early
embryonic muscle. Dev Dyn. 1996;206(3):291–300.
18.Cornelison DD, Filla MS, Stanley HM, Rapraeger
AC, Olwin BB. Syndecan-3 and syndecan-4 specifically mark skeletal muscle satellite cells and are
implicated in satellite cell maintenance and muscle
regeneration. Dev Biol. 2001;239(1):79–94.
19.Rosen GD, et al. Roles for the integrin VLA-4 and
its counter receptor VCAM-1 in myogenesis. Cell.
1992;69(7):1107–1119.
20.Cornelison DD, Wold BJ. Single-cell analysis of
regulatory gene expression in quiescent and activated mouse skeletal muscle satellite cells. Dev Biol.
1997;191(2):270–283.
21.Garry DJ, et al. Myogenic stem cell function is
impaired in mice lacking the forkhead/winged
helix protein MNF. Proc Natl Acad Sci U S A.
2000;97(10):5416–5421.
22.Irintchev A, Zeschnigk M, Starzinski-Powitz A,
Wernig A. Expression pattern of M-cadherin in
normal, denervated, and regenerating mouse muscles. Dev Dyn. 1994;199(4):326–337.
23.Gnocchi VF, White RB, Ono Y, Ellis JA, Zammit
PS. Further characterisation of the molecular signature of quiescent and activated mouse muscle
satellite cells. PLoS One. 2009;4(4):e5205.
24.Blanco-Bose WE, Yao CC, Kramer RH, Blau HM.
Purification of mouse primary myoblasts based
on alpha 7 integrin expression. Exp Cell Res.
2001;265(2):212–220.
25.Kuang S, Kuroda K, Le Grand F, Rudnicki MA.
Asymmetric self-renewal and commitment of satellite stem cells in muscle. Cell. 2007;129(5):999–1010.
26.Betsholtz C. Insight into the physiological functions of PDGF through genetic studies in mice.
Cytokine Growth Factor Rev. 2004;15(4):215–228.
27.Fukada S, Higuchi S, Segawa M, Koda K, Yamamoto Y, et al. Purification and cell-surface marker
characterization of quiescent satellite cells from
murine skeletal muscle by a novel monoclonal
antibody. Exp Cell Res. 2004;296(2):245–255.
28.Sherwood RI, et al. Isolation of adult mouse myogenic progenitors: functional heterogeneity of
cells within and engrafting skeletal muscle. Cell.
2004;119(4):543–554.
29.Day K, Shefer G, Richardson JB, Enikolopov G,
Yablonka-Reuveni Z. Nestin-GFP reporter expression defines the quiescent state of skeletal muscle
satellite cells. Dev Biol. 2007;304(1):246–259.
30.Montarras D, et al. Direct isolation of satellite
cells for skeletal muscle regeneration. Science.
2005;309(5743):2064–2067.
31.Bosnakovski D, et al. Prospective isolation of skeletal muscle stem cells with a Pax7 reporter. Stem
Cells. 2008;26(12):3194–3204.
32.Peault B, et al. Stem and progenitor cells in skeletal
muscle development, maintenance, and therapy.
Mol Ther. 2007;15(5):867–877.
18
33.Illa I, Leon-Monzon M, Dalakas MC. Regenerating
and denervated human muscle fibers and satellite
cells express neural cell adhesion molecule recognized by monoclonal antibodies to natural killer
cells. Ann Neurol. 1992;31(1):46–52.
34.Price FD, Kuroda K, Rudnicki MA. Stem cell based
therapies to treat muscular dystrophy. Biochim Biophys Acta. 2007;1772(2):272–283.
35.Dhawan J, Rando TA. Stem cells in postnatal myogenesis: molecular mechanisms of satellite cell quiescence, activation and replenishment. Trends Cell
Biol. 2005;15(12):666–673.
36.Tatsumi R, Anderson JE, Nevoret CJ, Halevy O,
Allen RE. HGF/SF is present in normal adult skeletal muscle and is capable of activating satellite
cells. Dev Biol. 1998;194(1):114–128.
37.Floss T, Arnold HH, Braun T. A role for FGF-6 in skeletal muscle regeneration. Genes Dev.
1997;11(16):2040–2051.
38.Musaro A. Growth factor enhancement of muscle
regeneration: a central role of IGF-1. Arch Ital Biol.
2005;143(3-4):243–248.
39.Wozniak AC, Anderson JE. Nitric oxide-dependence of satellite stem cell activation and quiescence on normal skeletal muscle fibers. Dev Dyn.
2007;236(1):240–250.
40.Zammit PS, et al. Kinetics of myoblast proliferation show that resident satellite cells are competent
to fully regenerate skeletal muscle fibers. Exp Cell
Res. 2002;281(1):39–49.
41.Zammit PS, et al. Muscle satellite cells adopt divergent fates: a mechanism for self-renewal? J Cell Biol.
2004;166(3):347–357.
42.Conboy IM, Rando TA. The regulation of Notch
signaling controls satellite cell activation and cell
fate determination in postnatal myogenesis. Dev
Cell. 2002;3(3):397–409.
43.Shinin V, Gayraud-Morel B, Gomes D, Tajbakhsh
S. Asymmetric division and cosegregation of template DNA strands in adult muscle satellite cells.
Nat Cell Biol. 2006;8(7):677–687.
44.Conboy MJ, Karasov AO, Rando TA. High incidence
of non-random template strand segregation and
asymmetric fate determination in dividing stem
cells and their progeny. PLoS Biol. 2007;5(5):e102.
45.Le Grand F, Jones AE, Seale V, Scime A, Rudnicki
MA. Wnt7a activates the planar cell polarity pathway to drive the symmetric expansion of satellite
stem cells. Cell Stem Cell. 2009;4(6):535–547.
46.Partridge TA, Morgan JE, Coulton GR, Hoffman
EP, Kunkel LM. Conversion of mdx myofibres from
dystrophin-negative to -positive by injection of normal myoblasts. Nature. 1989;337(6203):176–179.
47.Cossu G, Sampaolesi M. New therapies for muscular dystrophy: cautious optimism. Trends Mol Med.
2004;10(10):516–520.
48.Collins CA, et al. Stem cell function, self-renewal, and
behavioral heterogeneity of cells from the adult muscle satellite cell niche. Cell. 2005;122(2):289–301.
49.Cerletti M, et al. Highly efficient, functional
engraftment of skeletal muscle stem cells in dystrophic muscles. Cell. 2008;134(1):37–47.
50.Sacco A, Doyonnas R, Kraft P, Vitorovic S, Blau HM.
Self-renewal and expansion of single transplanted
muscle stem cells. Nature. 2008;456(7221):502–506.
51.Tanaka KK, et al. Syndecan-4-expressing muscle
progenitor cells in the SP engraft as satellite
cells during muscle regeneration. Cell Stem Cell.
2009;4(3):217–225.
52.Ikemoto M, et al. Autologous transplantation of
SM/C-2.6(+) satellite cells transduced with microdystrophin CS1 cDNA by lentiviral vector into mdx
mice. Mol Ther. 2007;15(12):2178–2185.
53.Cossu G. Unorthodox myogenesis: possible developmental significance and implications for tissue
histogenesis and regeneration. Histol Histopathol.
1997;12(3):755–760.
54.Galli R, et al. Skeletal myogenic potential of
human and mouse neural stem cells. Nat Neurosci.
2000;3(10):986–991.
55.Tajbakhsh S, et al. A population of myogenic
cells derived from the mouse neural tube. Neuron.
1994;13(4):813–821.
56.Ferrari G, et al. Muscle regeneration by bone
marrow-derived myogenic progenitors. Science.
1998;279(5356):1528–1530.
57.Gussoni E, et al. Dystrophin expression in the
mdx mouse restored by stem cell transplantation.
Nature. 1999;401(6751):390–394.
58.Ferrari G, Stornaiuolo A, Mavilio F. Failure to
correct murine muscular dystrophy. Nature.
2001;411(6841):1014–1015.
59.McKinney-Freeman SL, et al. Muscle-derived hematopoietic stem cells are hematopoietic in origin.
Proc Natl Acad Sci U S A. 2002;99(3):1341–1346.
60.Gussoni E, et al. Long-term persistence of donor
nuclei in a Duchenne muscular dystrophy patient
receiving bone marrow transplantation. J Clin
Invest. 2002;110(6):807–814.
61.Corbel SY, et al. Contribution of hematopoietic stem cells to skeletal muscle. Nat Med.
2003;9(12):1528–1532.
62.Camargo FD, Green R, Capetanaki Y, Jackson KA,
Goodell MA. Single hematopoietic stem cells generate skeletal muscle through myeloid intermediates. Nat Med. 2003;9(12):1520–1527.
63.Torrente Y, et al. Human circulating AC133(+) stem
cells restore dystrophin expression and ameliorate
function in dystrophic skeletal muscle. J Clin Invest.
2004;114(2):182–195.
64.Benchaouir R, et al. Restoration of human dystrophin following transplantation of exon-skippingengineered DMD patient stem cells into dystrophic
mice. Cell Stem Cell. 2007;1(6):646–657.
65.Dezawa M, et al. Bone marrow stromal cells generate muscle cells and repair muscle degeneration.
Science. 2005;309(5732):314–317.
66.Gang EJ, et al. Engraftment of mesenchymal
stem cells into dystrophin-deficient mice is not
accompanied by functional recovery. Exp Cell Res.
2009;315(15):2624–2636.
67.Minasi MG, et al. The meso-angioblast: a multipotent, self-renewing cell that originates from the dorsal aorta and differentiates into most mesodermal
tissues. Development. 2002;129(11):2773–2783.
68.Sampaolesi M, et al. Cell therapy of alpha-sarcoglycan null dystrophic mice through intraarterial delivery of mesoangioblasts. Science.
2003;301(5632):487–492.
69.Sampaolesi M, et al. Mesoangioblast stem cells
ameliorate muscle function in dystrophic dogs.
Nature. 2006;444(7119):574–579.
70.Dellavalle A, et al. Pericytes of human skeletal muscle are myogenic precursors distinct from satellite
cells. Nat Cell Biol. 2007;9(3):255–267.
71.Asahara T, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science.
1997;275(5302):964–967.
72.Pesce M, et al. Myoendothelial differentiation of
human umbilical cord blood-derived stem cells in
ischemic limb tissues. Circ Res. 2003;93(5):e51–e62.
73.Zheng B, et al. Prospective identification of myogenic endothelial cells in human skeletal muscle.
Nat Biotechnol. 2007;25(9):1025–1034.
74.Meliga E, Strem BM, Duckers HJ, Serruys
PW. Adipose-derived cells. Cell Transplant.
2007;16(9):963–970.
75.Goudenege S, et al. Enhancement of myogenic and
muscle repair capacities of human adipose-derived
stem cells with forced expression of MyoD. Mol
Ther. 2009;17(6):1064–1072.
76.Evans MJ, Kaufman MH. Establishment in culture of pluripotential cells from mouse embryos.
Nature. 1981;292(5819):154–156.
77.Thomson JA, et al. Embryonic stem cell lines
derived from human blastocysts. Science.
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
review series
1998;282(5391):1145–1147.
78.Yamanaka S. A fresh look at iPS cells. Cell.
2009;137(1):13–17.
79.Nishikawa S, Goldstein RA, Nierras CR. The
promise of human induced pluripotent stem cells
for research and therapy. Nat Rev Mol Cell Biol.
2008;9(9):725–729.
80.Park IH, et al. Disease-specific induced pluripotent
stem cells. Cell. 2008;134(5):877–886.
81.Murry CE, Keller G. Differentiation of embryonic stem cells to clinically relevant populations: lessons from embryonic development. Cell.
2008;132(4):661–680.
82.Robbins J, Gulick J, Sanchez A, Howles P, Doetschman
T. Mouse embryonic stem cells express the cardiac
myosin heavy chain genes during development in
vitro. J Biol Chem. 1990;265(20):11905–11909.
83.Sanchez A, Jones WK, Gulick J, Doetschman T,
Robbins J. Myosin heavy chain gene expression in
mouse embryoid bodies. An in vitro developmental
study. J Biol Chem. 1991;266(33):22419–22426.
84.Bhagavati S, Xu W. Generation of skeletal muscle from transplanted embryonic stem cells in
dystrophic mice. Biochem Biophys Res Commun.
2005;333(2):644–649.
85.Barberi T, et al. Derivation of engraftable skeletal
myoblasts from human embryonic stem cells. Nat
Med. 2007;13(5):642–648.
86.Chang H, et al. Generation of transplantable, functional satellite-like cells from mouse embryonic
stem cells. Faseb J. 2009;23(6):1907–1919.
87.Dekel I, Magal Y, Pearson-White S, Emerson CP,
Shani M. Conditional conversion of ES cells to
skeletal muscle by an exogenous MyoD1 gene. New
Biol. 1992;4(3):217–224.
88.Darabi R, et al. Functional skeletal muscle regeneration from differentiating embryonic stem cells.
Nat Med. 2008;14(2):134–143.
89.Bianco P, Cossu G. Uno, nessuno e centomila: searching for the identity of mesodermal progenitors. Exp Cell Res. 1999;251(2):257–263.
90.Barberi T, Willis LM, Socci ND, Studer L. Derivation of multipotent mesenchymal precursors
from human embryonic stem cells. PLoS Med.
2005;2(6):e161.
91.Sakurai H, Okawa Y, Inami Y, Nishio N, Isobe K.
Paraxial mesodermal progenitors derived from
mouse embryonic stem cells contribute to muscle
regeneration via differentiation into muscle satellite cells. Stem Cells. 2008;26(7):1865–1873.
92.Maherali N, Hochedlinger K. Guidelines and techniques for the generation of induced pluripotent
stem cells. Cell Stem Cell. 2008;3(6):595–605.
93.Law PK, et al. Dystrophin production induced by
myoblast transfer therapy in Duchenne muscular
dystrophy. Lancet. 1990;336(8707):114–115.
94.Neumeyer AM, et al. Pilot study of myoblast transfer in the treatment of Becker muscular dystrophy.
Neurology. 1998;51(2):589–592.
95.Law PK, et al. Myoblast transfer therapy for
Duchenne muscular dystrophy. Acta Paediatr Jpn.
1991;33(2):206–215.
96.Huard J, et al. Human myoblast transplantation
between immunohistocompatible donors and
recipients produces immune reactions. Transplant
Proc. 1992;24(6):3049–3051.
97.Karpati G, et al. Myoblast transfer in Duchenne
muscular dystrophy. Ann Neurol. 1993;34(1):8–17.
98.Law PK, et al. Feasibility, safety, and efficacy of myoblast transfer therapy on Duchenne muscular dystrophy boys. Cell Transplant. 1992;1(2-3):235–244.
99.Gussoni E, et al. Normal dystrophin transcripts
detected in Duchenne muscular dystrophy
patients after myoblast transplantation. Nature.
1992;356(6368):435–438.
100.Tremblay JP, et al. Results of a triple blind clinical study of myoblast transplantations without
immunosuppressive treatment in young boys with
Duchenne muscular dystrophy. Cell Transplant.
1993;2(2):99–112.
101.M orandi L, et al. Lack of mRNA and dystrophin expression in DMD patients three months
after myoblast transfer. Neuromuscul Disord.
1995;5(4):291–295.
102.Mendell JR, et al. Myoblast transfer in the treatment of Duchenne’s muscular dystrophy. N Engl J
Med. 1995;333(13):832–838.
103.Miller RG, et al. Myoblast implantation in Duchenne muscular dystrophy: the San Francisco study.
Muscle Nerve. 1997;20(4):469–478.
104.Skuk D, Goulet M, Tremblay JP. Use of repeating
dispensers to increase the efficiency of the intramuscular myogenic cell injection procedure. Cell
Transplant. 2006;15(7):659–663.
105.Partridge T. The current status of myoblast transfer. Neurol Sci. 2000;21(suppl 5):S939–S942.
106.Fan Y, Maley M, Beilharz M, Grounds M. Rapid
death of injected myoblasts in myoblast transfer
therapy. Muscle Nerve. 1996;19(7):853–860.
107.Guerette B, et al. Prevention by anti-LFA-1 of acute
myoblast death following transplantation. J Immunol. 1997;159(5):2522–2531.
108.Torrente Y, et al. Autologous transplantation of muscle-derived CD133+ stem cells in Duchenne muscle
patients. Cell Transplant. 2007;16(6):563–577.
109.Atkins BZ, et al. Intracardiac transplantation of
skeletal myoblasts yields two populations of striated
cells in situ. Ann Thorac Surg. 1999;67(1):124–129.
110.Taylor DA, et al. Regenerating functional myocardium: improved performance after skeletal myoblast
transplantation. Nat Med. 1998;4(8):929–933.
111.Pouzet B, et al. Factors affecting functional outcome after autologous skeletal myoblast transplantation. Ann Thorac Surg. 2001;71(3):844–850;
discussion 850–851.
112.Reinecke H, Poppa V, Murry CE. Skeletal muscle
stem cells do not transdifferentiate into cardiomyocytes after cardiac grafting. J Mol Cell Cardiol.
2002;34(2):241–249.
113.L eobon B, et al. Myoblasts transplanted into
rat infarcted myocardium are functionally isolated from their host. Proc Natl Acad Sci U S A.
2003;100(13):7808–7811.
114.Smits PC, et al. Catheter-based intramyocardial
injection of autologous skeletal myoblasts as a
primary treatment of ischemic heart failure: clinical experience with six-month follow-up. J Am Coll
Cardiol. 2003;42(12):2063–2069.
115.Menasche P, et al. Myoblast transplantation for
heart failure. Lancet. 2001;357(9252):279–280.
116.M enasche P, et al. Autologous skeletal myoblast transplantation for severe postinfarction
left ventricular dysfunction. J Am Coll Cardiol.
2003;41(7):1078–1083.
117.Dib N, et al. Safety and feasibility of autologous
myoblast transplantation in patients with ischemic
cardiomyopathy: four-year follow-up. Circulation.
2005;112(12):1748–1755.
118.Hagege AA, et al. Skeletal myoblast transplantation in ischemic heart failure: long-term follow-up
of the first phase I cohort of patients. Circulation.
2006;114(suppl 1):I108–113.
119.Herreros J, et al. Autologous intramyocardial injection of cultured skeletal muscle-derived stem cells
in patients with non-acute myocardial infarction.
Eur Heart J. 2003;24(22):2012–2020.
120.Steendijk P, et al. Intramyocardial injection of
skeletal myoblasts: long-term follow-up with pressure-volume loops. Nat Clin Pract Cardiovasc Med.
2006;3(suppl 1):S94–S100.
121.Pagani FD, et al. Autologous skeletal myoblasts
transplanted to ischemia-damaged myocardium in humans. Histological analysis of cell
survival and differentiation. J Am Coll Cardiol.
2003;41(5):879–888.
122.M enasche P, et al. The Myoblast Autologous
Grafting in Ischemic Cardiomyopathy (MAGIC)
trial: first randomized placebo-controlled
study of myoblast transplantation. Circulation.
2008;117(9):1189–1200.
123.Dib N, et al. One-year follow-up of feasibility and
safety of the first U.S., randomized, controlled
study using 3-dimensional guided catheter-based
delivery of autologous skeletal myoblasts for ischemic cardiomyopathy (CAuSMIC study). JACC Cardiovasc Interv. 2009;2(1):9–16.
124.Serruys PW. Final results of a phase I/II randomized, open-label trial to evaluate intramyocardial
autologous skeletal myoblast transplantation in
congestive heart failure patients: The SEISMIC
Trial. Paper presented at: 57th Annual Scientific
Session of the American College of Cardiology;
March 29-April 1 2008; Chicago, IL, USA.
125.Smaldone MC, Chancellor MB. Muscle derived
stem cell therapy for stress urinary incontinence.
World J Urol. 2008;26(4):327–332.
126.Mitterberger M, et al. Adult stem cell therapy
of female stress urinary incontinence. Eur Urol.
2008;53(1):169–175.
127.Carr LK, et al. 1-year follow-up of autologous muscle-derived stem cell injection pilot study to treat
stress urinary incontinence. Int Urogynecol J Pelvic
Floor Dysfunct. 2008;19(6):881–883.
128.Strasser H, et al. Transurethral ultrasonographyguided injection of adult autologous stem cells versus transurethral endoscopic injection of collagen
in treatment of urinary incontinence. World J Urol.
2007;25(4):385–392.
129.M itterberger M, et al. Autologous myoblasts
and fibroblasts for female stress incontinence:
a 1-year follow-up in 123 patients. BJU Int.
2007;100(5):1081–1085.
The Journal of Clinical Investigation http://www.jci.org Volume 120 Number 1 January 2010
19
PERSPECTIVES
OPINION
Satellite cells, the engines of
muscle repair
Yu Xin Wang and Michael A. Rudnicki
Abstract | Satellite cells are a heterogeneous population of stem and progenitor
cells that are required for the growth, maintenance and regeneration of skeletal
muscle. The transcription factors paired-box 3 (PAX3) and PAX7 have essential and
overlapping roles in myogenesis. PAX3 acts to specify embryonic muscle
precursors, whereas PAX7 enforces the satellite cell myogenic programme while
maintaining the undifferentiated state. Recent experiments have suggested that
PAX7 is dispensable in adult satellite cells. However, these findings are
controversial, and the issue remains unresolved.
It has been 50 years since Mauro1 first postulated that satellite cells could be resident
progenitor cells involved in skeletal muscle
regeneration. Satellite cells were initially
characterized according to their anatomica­l
position as sublaminar mononuclear cells
‘wedged’ between the basal lamina and
the plasma membrane (also known as the
sarcolemma in this context) of myofibres.
Within this niche, satellite cells are commonly adjacent to a myonucleus of their host
myofibre and an endothelial cell of a nearby
capillary. The close proximity of satellite cells
to myofibres suggested that they may have
a role in muscle regeneration.
Since the discovery of satellite cells,
evidence has accumulated showing that
they are the primary contributors to the
postnatal growth, maintenance and repair
of skeletal muscle. In adult muscle, satellite
cells express the transcription factor pairedbox 7 (PAX7) (FIG. 1a) and remain quiescent
under normal physiological conditions2,3.
Readily responsive to molecular triggers
from exercise, injuries or disease, satellite
cells have a remarkable ability to self-renew,
expand, proliferate as myoblasts or undergo
myogenic differentiation to fuse and restore
damaged muscle4 (FIG. 1b). Most import­
antly, satellite cells are maintained through
repeated cycles of growth and regeneration, which supports the notion that they
are a heterogeneous population containing
stem cells that sustain their self-renewal.
Recent studies using transgenic mice
have further examined the role of satellite
cells during postnatal regeneration and in
hypertrophy. In this Opinion article, we
focus on the evidence that satellite cells are
essential during these processes, describe
the mechanisms maintaining their homeostasis through many rounds of regeneration
and discuss findings showing that PAX7 is
required to specify this lineage.
Myogenesis
Many similarities between the activation of
satellite cells and myogenesis in the somite
(BOX 1) have reinforced the idea that adult
muscle regeneration to a certain extent
re­capitulates embryonic development
through analogous, but not necessarily
identical, mechanisms. Below, we briefly
introduce the genetic networks involved in
myo­genesis — for recent, comprehensive
reviews on myogenesi­s, see REFS 4–7.
Myogenic regulatory factors. Similarly to the
establishment of embryonic progenitors in
the myotome (BOX 1), the activation of satellite cells into myoblasts involves the upregulation of the basic helix–loop–helix (bHLH)
transcription factors myogenic facto­r 5
(MYF5) and myoblast determination protein
NATURE REVIEWS | MOLECULAR CELL BIOLOGY
(MYOD) (FIG. 1b). Together with musclespecific regulatory factor 4 (MRF4; also
known as MYF6) and myogenin, which
are upregulated during myoblast differentiation, these myogenic regulatory factors
(MRFs) transcriptionally and epigenetically
determine the myogenic capacity of muscle
progenitors7.
Mice lacking MyoD have seemingly normal muscle but express about fourfold higher
levels of MYF5 (REF. 8). MYF5‑deficient animals also have normal muscle9,10. However,
mice lacking both Myf5 and MyoD are totally
devoid of myoblasts and myofibres11,12,
indicating that these genes are required for
the determination of myogenic precursors.
Although MRF4 has some capacity to function as a determination factor 12, it is has
not been established that it does so in the
presenc­e of MYF5 and MYOD.
As a downstream target of MYOD,
myogenin regulates the transition from
myoblasts into myocytes and myotubes
(FIG. 1b) and, although myogenin-knockout
mice show proper compartmentalization of
muscle groups, they almost completely lack
myofibres and accumulate undifferentiated
myoblasts13,14. Mice lacking both MyoD and
Mrf4 display a phenotype that is similar to
the myogenin-null phenotype, suggesting
that, for myoblasts only expressing MYF5,
the differentiation into myocytes requires
MRF4 (REF. 15). Thus, MYF5 and MYOD are
required for the determination of myogenic
precursors and act upstream of myogenin
and MRF4, which are required for terminal
differentiation11. Together, these findings
suggest that various overlapping regulatory
networks control myogenic differentiation.
PAX3 and PAX7 specify myogenic progeni­
tors. The expression of MRFs is regulated by
PAX3 and PAX7, both of which have been
shown to directly bind proximal promoters of MyoD and distal enhancer elements
of Myf5, thereby regulating their expression16–18. PAX3 and PAX7 play key parts in
maintaining the proliferation of progen­
itors and preventing early differentiation.
Moreover, ectopic expression of Pax3 or
Pax7 in mouse embryonic stem cells showed
that either one is sufficient to promote a
myogenic fate19.
VOLUME 13 | FEBRUARY 2012 | 127
© 2012 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
which requires the activation of hepatocyte
growth factor receptor (HGFR; also known
as MET) by PAX3 (REFS 21,25) (BOX 1). This
suggests that PAX3 is solely responsible for
the migration of progenitors to establish
myogenic compartments within the limb.
By contrast, PAX7 seems to be uniquely
required in satellite cells (discussed in detail
below). Indeed, PAX3 is downregulated postnatally in most muscle progenitors, except
for the satellite cells of a subset of muscle
groups such as the diaphragm25, whereas
PAX7 expression is maintained in all satellite
cells2. Furthermore, PAX7‑null mice have
normal embryonic myogenesis but lack functional satellite cells2. Together, these findings
argue that PAX3 and PAX7 have overlapping
but non-redundant roles in the myogenic
programme.
a Merge
PAX7
YFP
DAPI
b Quiescence
Basal lamina
Self-renewal
PAX7+MYF5–
Satellite
stem cell
Sarcolemma
Proliferation
Differentiation
MYOD–
Commitment
↑ MYF5 PAX7+MYF5+
↓ PAX7
↑ Myogenin
Activation
↑ MYOD
Commited
satellite cell
Myoblasts
PAX7+MYF5+MYOD+
↑ MRF4
↑ MYHC
Myocyte
MYOD+myogenin+
Figure 1 | Satellite cell fate in regeneration. a | Immunofluorescence
micrograph
of quiescent
satellite
Nature Reviews
| Molecular
Cell Biology
cells on a resting extensor digitorum longus muscle fibre isolated from a MYF5–Cre R26R–YFP trans‑
genic mouse, in which MYF5 expression is marked by yellow fluorescent protein (YFP; green): these
mice express MYF5–Cre (knock-in of the Cre coding region into the Myf5 coding region) and R26R–YFP
(loxP-based lineage reporter; loxP–tPA–loxP–EYFP knocked in at the Rosa locus coding region). Satellite
cells represent <5% of all nuclei (labelled with DAPI (4′,6‑diamidino-2‑phenylindole); blue) in skeletal
muscle and express the transcription f­actor paired-box 7 (PAX7; red). Although most satellite cells
(~90%) are committed to the muscle lineage and have expressed Myf5 at some point in their ancestry
(arrowhead), a subpopulation (~10%) has never expressed Myf5 and remains YFP negative (arrow). b | In
quiescence, satellite cells are a heterogeneous population residing between the basal lamina and the
sarcolemma of their host fibres; ~90% are committed satellite cells (PAX7+MYF5+), whereas ~10% are
satellite stem cells (PAX7+MYF5–). Following activation, committed satellite cells upregulate myoblast
determination protein (MYOD; PAX7+MYF5+MYOD+ cells), re-enter the cell cycle to proliferate as myo‑
blasts and then progress into differentiation by downregulating PAX7 and upregulating myogenin as
myocytes (MYOD+myogenin+ cells). Regeneration of myofibres requires the fusion of myocytes into new
myotubes or with host fibres (not shown). During proliferation, heterogeneity regarding MYOD expres‑
sion suggests that some MYOD– myoblasts are able to reverse into quiescence (dashed arrow). MRF4,
muscle-specific regulatory facto­r 4; MYHC, myosin heavy chain.
Belonging to the PAX family of transcription factors, PAX3 and PAX7 are paralogues
with conserved amino acid sequences and
have almost identical sequence-specific
DNA-binding motifs20. Despite this hom­
ology, studies using knockout mice suggest
that PAX3 and PAX7 have overlapping
roles only in myogenic specification; the
distinct phenotypes of these mice indicate
that PAX3 has unique functions during
embryonic development 21 and that PAX7 is
involved in the specification of satellite cells2.
PAX3‑null mice (also known as splotch
mice) have many developmental defects,
including a lack of limb muscles and reduced
MYOD expression in the myotome22 (BOX 1).
Interestingly, mice lacking both PAX3 and
Specification of satellite cells
It has long been postulated that satellite cells
are the remnants of embryonic muscle development1. Somitic progenitors that eventually
give rise to satellite cells express PAX3 and/or
PAX7 and do not express MRFs. These progenitor PAX3­­+PAX7+ cells upregulate MYF5
and MYOD when they enter the myogenic
differentiation programme, or remain as
satellite cells during late fetal myogenesis
without upregulating MRFs. PAX3­­+PAX7+
cells that do not express MRFs are first found
to align with nascent myotubes at embryonic
day 15.5 and then become satellite cells by
taking a sublaminar position24. Notably, once
they arrive at the nascent myotubes, most
satellite cells rapidly upregulate MYF5 and
downregulate PAX3 (REF. 26).
Lineage-tracing studies suggest that
PAX3+ cells contribute to embryonic myoblasts and the endothelial lineage, whereas
PAX7+ cells contribute to fetal myoblasts,
supporting the notion that these cells
rep­resent distinct myogenic lineages27.
Therefore, satellite stem cells (PAX7+MYF5–;
see below) in adult muscle may represent
a lineage continuum of the embryonic
PAX3+PAX7+MRF– progenitors28. However,
these studies have not conclusively ruled out
the possibility that satellite cells are a distinct
myogenic lineage, independent from those
that give rise to fetal myoblasts, or that they
arise from atypical myogenic stem cells in
postnatal muscle (BOX 2).
MYF5 cannot upregulate MYOD to compensate for the lack of MYF5 and thus lack
muscle23, which further indicates that PAX3
activates MYOD16. Even though PAX3 is
expressed at an earlier embryonic stage than
PAX7, PAX7 is upregulated in PAX3‑null
mice, presumably to compensate for the loss
of PAX3 (REF. 22). In fact, muscle formation
requires PAX3 or PAX7, as progenitor cell
populations from mice lacking both Pax3
and Pax7 undergo apoptosis, and these
mice do not form muscle24.
Although Pax7 knock-in at the Pax3 locus
can rescue the PAX3‑null phenotype during
somitogenesis, it does not fully rescue the
lack of delamination and long-range migration of muscle progenitors to the limb bud,
128 | FEBRUARY 2012 | VOLUME 13
Relative roles of PAX3 and PAX7 in satellit­e
cells. PAX7 expression is maintained in all
satellite cells and proliferating myoblasts but
is sharply downregulated before differentiation29. PAX3 and PAX7 co-expression in
adult satellite cells seems to be limited to
www.nature.com/reviews/molcellbio
© 2012 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
only a few muscle groups — mostly the diaphragm and body wall muscles25. Although
PAX3 expression is robust in the embryo,
its downregulation after birth suggests that
it has little function in most satellite cells.
Prolonged expression of PAX3, by preventing its proteosomal degradation, results in
the inhibition of terminal differentiation30,
consistent with the ability of ectopically
expressed PAX7 to inhibit differentiation29. This result has been used to argue
that PAX3 regulates satellite cell activation.
Although studies have indicated a role for
PAX3 in satellite cell development and
mainten­ance30,31,32,33, this currently remains
controversial.
By contrast, PAX7 is required for the
development and maintenance of satellite
cells. Indeed, cells found in the satellite cell
positions of PAX7‑null mice are not myogenic and do not express satellite cell markers
(such as syndecan 4 and CD34; see below)31.
Importantly, although rare PAX3+ myogenic
cells are observed in PAX7‑null mutants,
PAX3 cannot compensate for the loss of
PAX7 in the establishment of the satellite cell
lineage. Moreover, although satellite cells in
the diaphragm normally express abundant
PAX3, the phenotype of PAX7‑null satellite
cells that express PAX3 in the diaphragm is
identical to other muscle groups: they cannot
maintain the undifferentiated state, they fuse
into myofibres early or they have reduced
survival, ultimately compromising their
capacity for muscle growth and regeneration2,25,31,34,35. This suggests that PAX3 alone
is insufficient to rescue these cells2,32.
Two possible functions have been proposed for PAX7 in the specification of satel­
lite cells: the specification of the myogenic
identity and the maintenance of the undifferentiated state. Ectopic overexpression of
PAX7 in C2C12 myoblasts and primary myoblasts suggests that PAX7 drives the expression of Myf5 but not MyoD18,29. Furthermore,
PAX7 has been shown to directly activate
Myf5 by promoting the recruitment of the
ASH2‑like (ASH2L)–MLL2 histone methyltransferase complex at a regulatory element
57 kb upstream of the Myf5 coding region18,
which indicates that PAX7 can epigenetically
specify the myogenic identity of satellite cells.
However, PAX7 expression correlates with
an undifferentiated but committed myogenic
state36, which suggests that PAX7 in the early
postnatal period probably functions to prevent the transition into terminal differentiation while maintaining the myogenic identity
by promoting MYF5 expression. Both functions together allow PAX7 to specify the
satellite cell lineage.
Box 1 | Embryonic myogenesis
Early embryonic myogenic precursors giving rise to body wall muscles are marked by
paired-box 3 (PAX3) expression in the paraxial mesoderm67. At this early stage, PAX3+ progenitors
are multipotent and give rise to the dorsal dermis and vascular progenitors of the aorta68.
Morphogens expressed by surrounding embryonic structures eventually determine the cellular
commitment within the somites (mesodermal structures found on either side of the neural tube in
vertebrate embryos that eventually give rise to muscles, skin and vertebrae)69. Sonic hedgehog
signalling from the notochord acts on the ventral medial segment of the somite and leads to the
formation of the sclerotome, which contains precursors to bone and cartilage70. WNT signalling
in the dorsal portion of the somite leads to the retention of an epithelial morphology and the
formation of the dermomyotome71. Combined expression of PAX3 and PAX7 in the dermomyotome
further specifies progenitor cells towards the muscle lineage, but transient Notch activation from
neural crest cells is required before the expression of myogenic regulatory factors (MRFs; which
define muscle progenitors)22,24,72. Notch signalling is essential for retaining myogenic progenitors
in a proliferative state; however, its downregulation is required to allow progression into
terminal differentiation. MRF+ progenitors migrate and proliferate to give rise to the myotome,
in which cells downregulate PAX3 and PAX7 to undergo differentiation and form primitive
nascent myofibres21,24,26. These primitive myofibres act as templates for the formation of
additional myofibres during postnatal growth.
The development of limb muscles requires the establishment of myogenic compartments in
the limb bud. This process involves the delamination and migration of progenitors from the
dermomyotome73. Induction of hepatocyte growth factor (HGF) in the limb bud activates myogenic
progenitors expressing HGF receptor (HGFR; also known as MET), which delaminate from the
ventrolateral lip of the dermomyotome. PAX3, and not PAX7, is able to induce the expression of
HGFR in embryonic progenitors25. Thus, PAX3 is required to activate the long-range migration
of progenitors to the limb bud. This is consistent with the lack of limb muscles in PAX3‑null mice21.
Requirement for PAX7 in satellite cells.
Recently, a study by Lepper et al.35 using
an inducible knockout mouse strain lacking PAX7 specifically in satellite cells when
injected with tamoxifen challenged the
proposed requirement for PAX7 expression
in adult satellite cells. Interestingly, when
postnatal time points were examined, the
phenotype of mice in which Pax7 had been
deleted between postnatal day 7 (P7) and
P21 was the same as that of the previously
characterized PAX7‑null mice2,25,31,34,35. This
result confirms a crucial function for PAX7
during postnatal growth, and this is further
supported by the observed early fusion of
progenitors in PAX7‑null mice and the
conversion of fetal cells from conditional
PAX7‑knockout mice into fibroblasts35.
Surprisingly, induced ablation of both
Pax3 and Pax7 after P21 did not lead to any
deficiency in muscle regeneration, satellite
cell number or primary myoblast growth
or differentiation35. This suggests a rather
dramatic change in the genetic requirement of muscle regeneration around P21,
the time point when myonuclear accretion
is completed (see below) and when postnatal growth is thought to end and satellite
cell numbers to reach a steady state37. The
distinct regeneration phenotypes obtained
by PAX7 deletion between P7–P21 and
adulthood challenge the notion that PAX7
is required throughout adulthood to activate downstream MRFs. It remains unclear
NATURE REVIEWS | MOLECULAR CELL BIOLOGY
whether satellite cells are poised for activation and extrinsic signalling is sufficient
to initiate MRF expression or whether
temporal specification by PAX7 is sufficient
to maintain satellite cell identity after P21.
The temporal specification hypothesis is
supported by the finding that tamoxifeninduced knockout of Pax7 leads to loss of
myogenic identify in fetal cells but not adult
cells35. One possibility is that the epigenetic
function of PAX7 in recruiting ASH2L–
MLL2 to target genes has been completed
by P21 and that target genes that define
myogenic identity are capable of maintaining their epigenetic memory in the absence
of PAX7.
However, the ability of satellite cells to
function after P21 without PAX7 is difficult
to reconcile with the published literature.
For example, in vitro knockdown of Pax7
in any aged myoblast or satellite cell has
been shown to result in growth arrest and
marked reduction in MYF5 expression18,34.
Why would a knockdown of PAX7 but not
a deletion affect satellite cell maintenance?
The notion that proliferating myogenic cells
have become ‘addicted’ to PAX7 might be
considered; that is, that continued PAX7
expression might be required to keep the cells
in a proliferative state. Another interesting
possibility is that the floxed allele analysed by
Lepper et al. is a hypermorph that is expressing a truncated but functional PAX7 lacking
a paired domain.
VOLUME 13 | FEBRUARY 2012 | 129
© 2012 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
Box 2 | Atypical muscle stem cells
Several laboratories have observed that stem cell populations other than satellite cells also have
myogenic capacity. These include pericytes, mesangioblasts, side population cells, CD45+SCA1+
cells and even bone marrow-derived haematopoietic stem cells (HSCs)74–80. Their myogenic
specification requires activation by injury or co-culturing with myoblasts; however, even under
such conditions, only small fractions of these cells adopt myogenic fates. Paired-box 7 (PAX7) is
required for the myogenic specification of CD45+SCA1+ cells during regeneration79, whereas the
myogenic identity of pericytes, side population cells and HSCs can be activated by alternative
pathways. Limited engraftment of these cells to muscle is observed in transplantation experiments,
but the extent of their contribution during in vivo muscle regeneration will require further
lineage-tracing studies.
PW1+ interstitial cells (PICs) were recently described as non-satellite cell myogenic progenitors
during postnatal muscle growth that can also adopt either vascular or myogenic fates81.
The myogenic specification of PICs depends on PAX7 and is enhanced by the presence of satellite
cell-derived myoblasts, suggesting that the recruitment of PICs depends on community effects.
As most newly specified fetal satellite cells also express PW1, and because lineage-tracing
experiments suggest that PICs are not derived from satellite cells, it was speculated that PICs
could be a postnatal source of satellite cells.
However, in recent analyses of satellite cell-depleted muscle53,54, atypical muscle stem cells could
not promote muscle regeneration or replenish the satellite cell pool. This challenges the previous
evidence and suggests either that these atypical muscle stem cells have very limited myogenic
potential or that they are not recruited during regeneration in this model owing to a lack of
paracrine signals from satellite cells (FIG. 3). The functional participation of atypical myogenic
stem cells will need to be studied further. Moreover, the paracrine factors secreted by satellite
cells to induce the recruitment of atypical muscle stem cells could be an interesting therapeutic
target to modulate regeneration kinetics.
If PAX7 is required only in the specification of new satellite cells, such a defect would
become apparent only after several rounds of
regeneration, when satellite cell pools have
become exhausted. Moreover, this defect can
be masked by alternative mechanisms of selfrenewal in satellite cells, such as reversible
quiescence (see below).
Nevertheless, Lepper et al.35 challenged
the paradigm that PAX7 is crucial for satellite cells in adults. Thus, further analysis is
needed to elucidate the requirement and
function of PAX7 in adult satellite cells.
Satellite cells in postnatal life
After postnatal growth (~P21), maturation of
skeletal muscle slowly reaches a homeostasis
of rest and regeneration. Satellite cells also
enter quiescence as their numbers decrease
dramatically from ~30% of sublaminar nuclei
to <5% by 8 weeks, which reflects fusion into
myofibres, a process known as myonuclear
accretion37,38. This entry into quiescence was
recently shown to depend on Notch signalling, as mice lacking two Notch targets, Hairy
and Enhancer of Split-related 1 (HESR1) and
HESR3, fail to generate quiescent satellite
cells39. Inhibition or disruption of Notch signalling in quiescent satellite cells leads to their
early differentiation and fusion40,41, similarly
to what is observed in PAX7‑null mice.
Originally defined by their anatomica­l
position to the host myofibre1, quiescent
satellite cells are reliably identifiable
by the expression of molecular markers, such as PAX7, α7β1 integrin, CD34,
syndecan 3, syndecan 4, myotubule cadherin (M‑cadherin), caveolin 1 and CXC
chemokine receptor 4 (CXCR4; also known
as fusin and CD184)42. The identification
of these markers, as well as the generation of
transgenic reporter mouse lines, has only
recently allowed the prospective isolation
and characterization of satellite cells in their
quiescent state28,43.
Satellite cells are heterogeneous. All adult
satellite cells express PAX7, and this expression is conserved through evolution42.
However, subpopulations of satellite cells
express a mixture of different surface markers as well as altered expression levels of
MYF5 and MYOD44. Because satellite cells
are self-renewing, within this heterogeneity
there must be a stem cell-like population
that is resistant to differentiation and maintains the satellite cell pool through many
rounds of regeneration. Experiments have
shown that small fractions (~20%) of satellite cells have slower proliferation kinetics
and can resist differentiation45. Furthermore,
satellite cells from different muscle groups
also display differential engraftment
potential after transplantation46. In these
transplantation experiments, only a small
fraction of satellite cells shows stem cell-like
properties and engrafts into the satellite cell
compartment.
130 | FEBRUARY 2012 | VOLUME 13
PAX7+MYF5– satellite stem cells. Using lin­
eage tracing in a mouse strain in which cells
that have expressed MYF5 are permanently
labelled with yellow fluorescent protein
(YFP), we identified that ~10% of adult satellite cells express PAX7 but not YFP, indicating that they have never expressed MYF5
(PAX7+MYF5– cells)28 (FIG. 1a). Compared
with their committed YFP+ counterparts,
PAX7+MYF5– satellite cells were able to
engraft as satellite cells, self-renew more
efficiently, give rise to committed YFP+
(PAX7+MYF5+) satellite cells and better
resist differentiation. Because of these stem
cell characteristics and their uncommitted
status, we concluded that these PAX7+MYF5–
satellit­e cells were in fact satellite stem cells.
Similarly to other adult stem cells
(reviewed in REF. 47), satellite stem cells follow traditional stochastic (symmetric) and
asymmetric paradigms of self-renewal28
(FIG. 2a). The asymmetric nature of the satellite cell niche, with the basal lamina acting
as the basement membrane and the sarcolemma of the host myofibre as the apical
surface, determines the cell fate of stem cell
divisions according to the orientation of
the mitotic axis in relation to the host fibre.
During in vivo regeneration, satellite stem
cell divisions in the apicobasal orientation
give rise to a committed MYF5+ satellite cell,
which is pushed into the apical surface, and
a daughter cell, which remains attached to
basal lamina and retains the satellite stem
cell identity. By contrast, planar divisions
of satellite stem cells occur along the host
myofibre, after which both daughter cells
remain in contact with the basal lamina,
symmetrically expand, giving rise to two
PAX7+MYF5– cells.
It remains unclear what intrinsic mech­
anism is responsible for the orientation of
divisions and how subsequent events lead
to commitment of the apical daughter cell.
However, insights into extrinsic regulators
revealed that satellite stem cells are similar
to embryonic PAX7+MYF5– cells in the
dermomyotome (BOX 1), in that inhibition
of Notch signalling drives satellite stem cells
to commit­ment and differentiation28,33.
Furthermore, WNT signalling is thought
to promote symmetric cell divisions by acting
through the planar cell polarity pathway 48.
Specifically, WNT7A signalling through
Frizzled 7 markedly stimulates the symmetric
expansion of satellite stem cells but does not
affect the growth of myoblasts or the kinetics
of their differentiation (FIG. 2b). This induces
the polarized distribution of the planar cell
polarity effector VANG-like 2 (VANGL2),
promoting a planar division plane and
www.nature.com/reviews/molcellbio
© 2012 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
therefore symmetric division of the daughter
cells. This pathway is thought to regulate the
regenerative potential of muscle. In support
of this, WNT7A is upregulated during regen­­
eration and increases both the number of
satel­lite cells and the muscle mass, and muscle
lacking WNT7A exhibits a decrease in
satellit­e cell number following regeneration.
Reversible quiescence. Replenishment of the
satellite cell pool requires stem cells to expand
but then return to quiescence, a common
feature of adult stem cells. This process is very
elusive and only applies to a subpopulation of
satellite cells, so our current understanding is
minimal. In vitro observations of satellite cells
on cultured myofibres suggest that a population of MYOD– reserve cells appear in late
regeneration and can return to quiescence
by sustaining PAX7 expression and resisting
differentiation49,50. This could arise from the
expansion of a MYOD– population of uncommitted satellite cells or the downregulation
of MYOD in proliferating myoblasts. Most
PAX7+MYF5– satellite stem cells correlate
with this population and do not express
MYOD or myogenin in fibre culture28. One
known mechanism regulating the reversible
quiescence of satellite stem cells is mediated
by the receptor Tyr kinase TIE2 (also known
as TEK)51. TIE2 activation by binding of the
hormone angiopoietin 1, which is secreted
from neighbouring fibroblasts and vascular
cells, activates extracellular signal-regulated
kinase (ERK) signalling downstream of TIE2.
This enhances PAX7 expression and thereby
sustains the undifferentiated state, ultimately
increasing the number of stem cells reverting
to quiescence.
Reversible quiescence of committed
myoblast­s challenges the paradigm that
MYOD, as a determination factor, is an
irreversible epigenetic checkpoint in the
myogenic programme. For a subpopulation
of myoblasts, this reversion was reported
to require the activation of Sprouty hom­
ologue 1 (SPRY1), a negative regulator
of ERK signalling 52. However, myoblasts
un­affected in SPRY1 deletion can maintain
a reduced, but homeostatic, number of satellite cells through subsequent injuries. This
indicates that alternative mechanisms of
reversion into quiescence exist. Although
contradictory, TIE2–ERK and SPRY1–ERK
signalling apply to two distinct cell types at
different time points during regeneration.
This suggests that temporal regulation of the
ERK signalling pathway controls the number
of satellite cells returning to quiescence and
reveals the possibility of modulating this
homeostasis with extrinsic factors.
a Self-renewal
b
PAX7+MYF5–
WNT7A
Basal lamina
Sarcolemma
Satellite
stem cell
Reverse into
quiescence
WNT7A
Asymmetric division
Symmetric expansion
PAX7+MYF5–
PAX7+MYF5–
FZD7
VANGL2
Planar cell polarity
pathway
PAX7+MYF5+
Figure 2 | Schematic of satellite stem cell fate in self-renewal. a | During regeneration, satellite stem
Nature
Reviewsdepending
| Molecular
Biology
cells expand and undergo stochastic (symmetric) or asymmetric
self-renewal,
onCell
the orienta‑
tion of divisions with respect to the basal lamina (basal surface) and the sarcolemma of the host fibre
(apical surface). In the stochastic paradigm, divisions parallel to the muscle fibre (planar) result in the
symmetric expansion of satellite stem cells. Divisions that are oriented perpendicular to the host fibre
(apicobasal) follow the asymmetric paradigm and give rise to two distinct fates: one daughter cell is
pushed into the apical surface, upregulates myogenic factor 5 (MYF5) and becomes PAX7+MYF5+; and
the other daughter cell remains adhered to the basal lamina and retains its stem cell identity
(PAX7+MYF5–). WNT7A, which is upregulated late in regeneration, promotes the symmetric expansion of
satellite stem cells to replenish the stem cell pool and maintain a homeostatic level of stem cells through
rounds of regeneration. b | WNT7A signals through its receptor Frizzled 7 (FZD7) to mediate the polarized
distribution of its effector VANG-like 2 (VANGL2). Acting through the planar cell polarity pathway to
induce cytoskeletal changes and orientation of spindles during division, WNT7A promotes satellite stem
cells to divide in a planar orientation, ultimately enhancing symmetric expansion. PAX7, paired-box 7.
Satellite cells in regeneration
The main function of satellite cells is to proliferate and differentiate into muscle cells to
regenerate muscle during exercise or injury.
Satellite cells are integral to regeneration.
The ability for satellite cells to contribute to
myogenesis has been demonstrated in vitro
and in vivo. In a series of diphtheria toxininduced ablation experiments, it was revealed
that muscle failed to regenerate when PAX7+
satellite cells were depleted53–55. Two different transgenic alleles were used to eliminate
PAX7+ satellite cells from muscle, and both
led to the same conclusion: no other cell types
can rescue the myogenic function of PAX7+
cells during exercise or injury 53,54 (BOX 2).
Instead of the formation of myofibres, adipocyte infiltrates expanded in place of muscle54.
This genetic ablation result resembles the
phenotypes of PAX7‑null mice and supports
the notion that satellite cells are the primary, if not the sole, contributors to muscle
regeneration.
Healthy adult muscle has a slow turnover
rate, so satellite cells remain mostly quiescent
(see above) unless activated by exercise or
injury 3. Consistent with this, ablation of satellite cells in resting conditions does not result
in progressive muscle mass loss54. However,
in degenerative muscle diseases, such as
Duchenne muscular dystrophy, chronic
regeneration of muscle triggers higher proliferative demand on satellite cells, leading to
NATURE REVIEWS | MOLECULAR CELL BIOLOGY
their eventual depletion56. Interfering with the
function of satellite cells in a mouse model for
Duchenne muscular dystrophy (mdx mice),
by either inducing reduced myogenic differ­
entiation (for example, in MYOD-null mice)
or reducing the telomere lengths (for example,
in mice lacking telomerase mRNA), results in
an exaggerated dystrophic phenotype57,58.
Together, these experiments suggest that satellite cells are absolutely necessary for regeneration and that satellite cells lost in disease are
not replaced by other stem cell sources.
Interactions with other cell types during regen­­
eration. Although satellite cells are the main
players in repairing muscle, various other cells
types are also recruited during regeneration
and can modulate the behaviour of satellite
cells by secreting cytokines (FIG. 3). During
the initial phase of regeneration, secretion of
pro-inflammatory cytokines by macrophages
can induce myoblast entry into terminal differentiation through the p38 kinase-mediated
repression of the Pax7 locus59. Expansion of
resident fibroadipogenic progenitors (FAPs)
during regeneration also promotes the
termin­al differentiation of myoblasts60.
However, not all signals during regeneration are pro-myogenic. The presence of
muscle connective tissue (MCT) fibroblasts
expressing T cell factor 4 (TCF4) seems to
prevent early differentiation of myoblasts by
creating a transitional niche. Reciprocally,
myoblasts promote MCT fibroblast
VOLUME 13 | FEBRUARY 2012 | 131
© 2012 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
Recruitment
Atypical myogenic
stem cell
Proliferation
Fibroblast
Macrophage
Factors?
Angiopoietin 1
TNF
IL-6
TGFβ
p38 activation
Proliferation
Quiescent
satellite cell
Reversal
Myoblast
Differentiation
Activation
FAPs
Regeneration
Damaged
myofibre
Figure 3 | Schematic of the cell interactions during regeneration. During regeneration, paracrine
signals (bold arrows) between necrotic fibres, infiltrating macrophages,
fibroblasts
and proliferating
Nature Reviews
| Molecular
Cell Biology
fibroadipogenic progenitors (FAPs) modulate satellite cell activation, proliferation and differentiation
(grey arrows). Secretion of angiopoietin 1 by fibroblasts and vascular cells has also been found to
promote satellite cell reversal into quiescence by activating extracellular signal-regulated kinase (ERK)
signalling. Signals coming from myoblasts also affect fibroblast proliferation. The lack in regenerative
capacity of atypical myogenic stem cells in satellite cell-depleted muscles suggests a possible require‑
ment for satellite cell- or myoblast-secreted factors in their recruitment. IL‑6, interleukin‑6; TGFβ,
transforming growth factor‑β; TNF, tumour necrosis factor.
proliferation55. Late in regeneration, newly
formed myotubes prevent the adipogenic
differentiation of mesenchymal progenitors
expressing platelet-derived growth factor
receptor-α (PDGFRα)61. These interactions
give rise to a complex interaction network
between satellite cells and other cell types,
which allows the extrinsic regulation
of satellite cells in regeneration.
Satellite cell requirement in hypertrophy.
Hypertrophy of muscle (that is, an increase in
myofibre size resulting from the production
of additional contractile proteins) caused by
overloading or exercise requires additional
myonuclei for protein synthesis. Because
myo­nuclei are mitotically arrested and cannot
replicate within the myofibre to meet such a
demand, hypertrophy is commonly associated
with the activation of satellite cells62, which
are thought to proliferate and fuse into existing myofibres. Indeed, classic studies using
γ‑radiation to inhibit the proliferation of
sate­llite cells found a dependence on satellite
cell, activation in overloading-induced hyper­
trophy 63. However, controversy over the specificity of γ‑radiation to satellite cells, as well as
a better understanding of intrinsic pathways
leading to the hypertrophy of myotubes, such
as calcineurin and AKT signalling, indicated
that further examination is needed64.
A recent study 65 provided evidence that
satellite cells are not required for overloadinginduced hypertrophy and that intrinsic
mechanisms within the myofibres can
compensate for protein synthesis without
additional myonuclei. Specifically, significant hyper­trophy was observed in satellite
cell-depleted muscles that were exposed to
overloading conditions. However, in controls, activation of satellite cells and fusion
into myofibres were observed. This indicates
that, in a physiological context, satellite
cells indeed participate in hypertrophy. It is
not surprising that myofibres can undergo
short-term hypertrophy without additional
myonuclei, but the addition of myonuclei
should reduce the ‘workload’ placed on the
existing myonuclei. Importantly, productive
hyper­trophy resulting from the participation
of sate­llite cells would be expected to couple
tissue mass with appropriate numbers of stem
and progenitor cells. Thus, satellite cells are
essential to achieve tissue homeostasis and
allow growth and repair over the long term.
Concluding remarks
50 years after their discovery, we have solidified the absolute requirement for muscle
satellite cells during muscle regeneration and
in hypertrophy. Composed primarily of a
nucleus and very little cytoplasm, the rege­n­
erative capacity of satellite cells can only be
described as remarkable. Indeed, whereas the
requirement for satellite cells has been questioned for short-term hypertrophy, it is clear
that maintenance of muscle and productive
hypertrophy absolutely require satellite cells.
132 | FEBRUARY 2012 | VOLUME 13
We have only scratched the surface of
a complex genetic network that requires
intrinsic and extrinsic activation to regulate
the myogenic fate of satellite cells. We know
that PAX3 and PAX7 regulate the expression
of MRFs and are crucial for muscle development, and that early postnatal specification
of the satellite cell lineage requires PAX7 to
establish an undifferentiated but myogenic
state. However, further work is needed
to definitively confirm whether PAX7 is
required in adult satellite cells.
Within the past two decades, our understanding of satellite cell biology has formed
new paradigms for the maintenance and
genetic regulation of adult stem cells in general. Without question, our advancing know­l­
edge of satellite cell biology has opened new
doors for the development of therapeutics targeting stem cell growth48, in vitro expansion
of satellite cells66 and even induction of embryonic stem cells for transplantation19 as promising avenues for the treatment of patients
suffering from degenerative muscle diseases.
Yu Xin Wang and Michael A. Rudnicki are at the
Sprott Centre for Stem Cell Research,
Ottawa Hospital Research Institute Ottawa,
501 Smyth Road Ottawa, Ontario K1H 8L6, Canada.
Yu Xin Wang and Michael A. Rudnicki are also at the
Faculty of Medicine, Department of Cellular and
Molecular Medicine, University of Ottawa, Ottawa,
Ontario K1H 8M5, Canada.
Correspondence to M.A.R. e‑mail: mrudnicki@ohri.ca
doi:10.1038/nrm3265
Published online 21 December 2011
Mauro, A. Satellite cell of skeletal muscle fibers.
J. Biophys. Biochem. Cytol. 9, 493–495 (1961).
Seale, P. et al. Pax7 is required for the specification
of myogenic satellite cells. Cell 102, 777–786
(2000).
3. Schultz, E., Gibson, M. C. & Champion, T. Satellite cells
are mitotically quiescent in mature mouse muscle:
an EM and radioautographic study. J. Exp. Zool. 206,
451–456 (1978).
4. Bentzinger, C. F., von Maltzahn, J. & Rudnicki, M. A.
Extrinsic regulation of satellite cell specification.
Stem Cell Res. Ther. 1, 27 (2010).
5. Braun, T. & Gautel, M. Transcriptional mechanisms
regulating skeletal muscle differentiation, growth and
homeostasis. Nature Rev. Mol. Cell Biol. 12, 349–361
(2011).
6. Buckingham, M. & Vincent, S. D. Distinct and dynamic
myogenic populations in the vertebrate embryo.
Curr. Opin. Genet. Dev. 19, 444–453 (2009).
7. Punch, V. G., Jones, A. E. & Rudnicki, M. A.
Transcriptional networks that regulate muscle stem cell
function. Wiley Interdiscip. Rev. Syst. Biol. Med. 1,
128–140 (2009).
8. Rudnicki, M. A., Braun, T., Hinuma, S. & Jaenisch, R.
Inactivation of MyoD in mice leads to up-regulation of
the myogenic HLH gene Myf‑5 and results in apparently
normal muscle development. Cell 71, 383–390 (1992).
9. Braun, T., Rudnicki, M. A., Arnold, H. H. & Jaenisch, R.
Targeted inactivation of the muscle regulatory gene
Myf‑5 results in abnormal rib development and
perinatal death. Cell 71, 369–382 (1992).
10. Kaul, A., Köster, M., Neuhaus, H. & Braun, T. Myf‑5
revisited: loss of early myotome formation does not
lead to a rib phenotype in homozygous Myf‑5 mutant
mice. Cell 102, 17–19 (2000).
11. Rudnicki, M. A. et al. MyoD or Myf‑5 is required for the
formation of skeletal muscle. Cell 75, 1351–1359
(1993).
1.
2.
www.nature.com/reviews/molcellbio
© 2012 Macmillan Publishers Limited. All rights reserved
PERSPECTIVES
12. Kassar-Duchossoy, L. et al. Mrf4 determines skeletal
muscle identity in Myf5:Myod double-mutant mice.
Nature 431, 466–471 (2004).
13. Hasty, P. et al. Muscle deficiency and neonatal death in
mice with a targeted mutation in the myogenin gene.
Nature 364, 501–506 (1993).
14. Nabeshima, Y. et al. Myogenin gene disruption results
in perinatal lethality because of severe muscle defect.
Nature 364, 532–535 (1993).
15. Rawls, A. et al. Overlapping functions of the myogenic
bHLH genes MRF4 and MyoD revealed in double
mutant mice. Development 125, 2349–2358 (1998).
16. Hu, P., Geles, K. G., Paik, J.‑H., DePinho, R. A. &
Tjian, R. Codependent activators direct myoblast
specific MyoD transcription. Dev. Cell 15, 534–546
(2008).
17. Bajard, L. et al. A novel genetic hierarchy functions
during hypaxial myogenesis: Pax3 directly activates
Myf5 in muscle progenitor cells in the limb. Genes Dev.
20, 2450–2464 (2006).
18. McKinnell, I. W. et al. Pax7 activates myogenic genes
by recruitment of a histone methyltransferase complex.
Nature Cell Biol. 10, 77–84 (2008).
19. Darabi, R. et al. Assessment of the myogenic stem cell
compartment following transplantation of Pax3/Pax7‑
induced embryonic stem cell-derived progenitors. Stem
Cells 29, 777–790 (2011).
20. Schäfer, B. W., Czerny, T., Bernasconi, M., Genini, M. &
Busslinger, M. Molecular cloning and characterization
of a human PAX‑7 cDNA expressed in normal and
neoplastic myocytes. Nucleic Acids Res. 22,
4574–4582 (1994).
21. Bober, E., Franz, T., Arnold, H. H., Gruss, P. &
Tremblay, P. Pax‑3 is required for the development
of limb muscles: a possible role for the migration of
dermomyotomal muscle progenitor cells. Development
120, 603–612 (1994).
22. Borycki, A. G., Li, J., Jin, F., Emerson, C. P. &
Epstein, J. A. Pax3 functions in cell survival and in pax7
regulation. Development 126, 1665–1674 (1999).
23. Tajbakhsh, S., Rocancourt, D., Cossu, G. &
Buckingham, M. Redefining the genetic hierarchies
controlling skeletal myogenesis: Pax‑3 and Myf‑5 act
upstream of MyoD. Cell 89, 127–138 (1997).
24. Relaix, F., Rocancourt, D., Mansouri, A. &
Buckingham, M. A Pax3/Pax7‑dependent population of
skeletal muscle progenitor cells. Nature 435, 948–953
(2005).
25. Relaix, F., Rocancourt, D., Mansouri, A. &
Buckingham, M. Divergent functions of murine Pax3 and
Pax7 in limb muscle development. Genes Dev. 18,
1088–1105 (2004).
26. Kassar-Duchossoy, L. et al. Pax3/Pax7 mark a novel
population of primitive myogenic cells during
development. Genes Dev. 19, 1426–1431 (2005).
27. Hutcheson, D. A., Zhao, J., Merrell, A., Haldar, M. &
Kardon, G. Embryonic and fetal limb myogenic cells are
derived from developmentally distinct progenitors and
have different requirements for β-catenin. Genes Dev.
23, 997–1013 (2009).
28. Kuang, S., Kuroda, K., Le Grand, F. & Rudnicki, M. A.
Asymmetric self-renewal and commitment of satellite
stem cells in muscle. Cell 129, 999–1010 (2007).
29. Olguin, H. C. & Olwin, B. B. Pax‑7 up-regulation inhibits
myogenesis and cell cycle progression in satellite cells:
a potential mechanism for self-renewal. Dev. Biol. 275,
375–388 (2004).
30. Boutet, S. C., Disatnik, M.‑H., Chan, L. S., Iori, K. &
Rando, T. A. Regulation of Pax3 by proteasomal
degradation of monoubiquitinated protein in skeletal
muscle progenitors. Cell 130, 349–362 (2007).
31. Kuang, S., Chargé, S. B., Seale, P., Huh, M. &
Rudnicki, M. A. Distinct roles for Pax7 and Pax3 in
adult regenerative myogenesis. J. Cell Biol. 172,
103–113 (2006).
32. Relaix, F. et al. Pax3 and Pax7 have distinct and
overlapping functions in adult muscle progenitor cells.
J. Cell Biol. 172, 91–102 (2006).
33. Conboy, I. M. & Rando, T. A. The regulation of Notch
signaling controls satellite cell activation and cell fate
determination in postnatal myogenesis. Dev. Cell 3,
397–409 (2002).
34. Oustanina, S., Hause, G. & Braun, T. Pax7 directs
postnatal renewal and propagation of myogenic
satellite cells but not their specification. EMBO J. 23,
3430–3439 (2004).
35. Lepper, C., Conway, S. J. & Fan, C.‑M. Adult satellite
cells and embryonic muscle progenitors have distinct
genetic requirements. Nature 460, 627–631 (2009).
36. Olguin, H. C., Yang, Z., Tapscott, S. J. & Olwin, B. B.
Reciprocal inhibition between Pax7 and muscle
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
regulatory factors modulates myogenic cell fate
determination. J. Cell Biol. 177, 769–779 (2007).
White, R., Bierinx, A.‑S., Gnocchi, V. & Zammit, P.
Dynamics of muscle fibre growth during postnatal
mouse development. BMC Dev. Biol. 10, 21 (2010).
Bischoff, R. in Myogenesis (eds Engel, A. G. &
Franszini-Armstrong, C.) 97–118 (McGraw-Hill,
New York,1994).
Fukada, S. et al. Hesr1 and Hesr3 are essential to
generate undifferentiated quiescent satellite cells and
to maintain satellite cell numbers. Development 138,
4609–4619 (2011).
Bjornson, C. R. R. et al. Notch signaling is necessary
to maintain quiescence in adult muscle stem cells.
Stem Cells 1 Nov 2011 (doi:10.1002/stem.773).
Mourikis, P. et al. A critical requirement for Notch
signaling in maintenance of the quiescent skeletal
muscle stem cell state. Stem Cells 8 Nov 2011
(doi:10.1002/stem.775).
Kuang, S. & Rudnicki, M. A. The emerging biology
of satellite cells and their therapeutic potential.
Trends Mol. Med. 14, 82–91 (2008).
Bosnakovski, D. et al. Prospective isolation of skeletal
muscle stem cells with a Pax7 reporter. Stem Cells 26,
3194–3204 (2008).
Sherwood, R. I. et al. Isolation of adult mouse
myogenic progenitors: functional heterogeneity of
cells within and engrafting skeletal muscle. Cell 119,
543–554 (2004).
Schultz, E. Satellite cell proliferative compartments in
growing skeletal muscles. Dev. Biol. 175, 84–94 (1996).
Collins, C. A. et al. Stem cell function, self-renewal, and
behavioral heterogeneity of cells from the adult muscle
satellite cell niche. Cell 122, 289–301 (2005).
Yamashita, Y. M. Cell adhesion in regulation of
asymmetric stem cell division. Curr. Opin. Cell Biol. 22,
605–610 (2010).
Le Grand, F., Jones, A. E., Seale, V., Scimè, A. &
Rudnicki, M. A. Wnt7a activates the planar cell polarity
pathway to drive the symmetric expansion of satellite
stem cells. Cell Stem Cell 4, 535–547 (2009).
Yoshida, N., Yoshida, S., Koishi, K., Masuda, K. &
Nabeshima, Y. Cell heterogeneity upon myogenic
differentiation: down-regulation of MyoD and Myf‑5
generates ‘reserve cells’. J. Cell Sci. 111, 769–779
(1998).
Zammit, P. S. et al. Muscle satellite cells adopt divergent
fates: a mechanism for self-renewal? J. Cell Biol. 166,
347–357 (2004).
Abou-Khalil, R. et al. Autocrine and paracrine
angiopoietin 1/Tie‑2 signaling promotes muscle satellite
cell self-renewal. Cell Stem Cell 5, 298–309 (2009).
Shea, K. L. et al. Sprouty1 regulates reversible
quiescence of a self-renewing adult muscle stem cell
pool during regeneration. Cell Stem Cell 6, 117–129
(2010).
Lepper, C., Partridge, T. A. & Fan, C.‑M. An absolute
requirement for Pax7‑positive satellite cells in acute
injury-induced skeletal muscle regeneration.
Development 138, 3639–3646 (2011).
Sambasivan, R. et al. Pax7‑expressing satellite cells are
indispensable for adult skeletal muscle regeneration.
Development 138, 3647–3656 (2011).
Murphy, M. M., Lawson, J. A., Mathew, S. J.,
Hutcheson, D. A. & Kardon, G. Satellite cells, connective
tissue fibroblasts and their interactions are crucial for
muscle regeneration. Development 138, 3625–3637
(2011).
Jejurikar, S. S. & Kuzon, W. M. Jr. Satellite cell depletion
in degenerative skeletal muscle. Apoptosis 8, 573–578
(2003).
Megeney, L. A., Kablar, B., Garrett, K., Anderson, J. E.
& Rudnicki, M. A. MyoD is required for myogenic stem
cell function in adult skeletal muscle. Genes Dev. 10,
1173–1183 (1996).
Sacco, A. et al. Short telomeres and stem cell
exhaustion model Duchenne muscular dystrophy in
mdx/mTR mice. Cell 143, 1059–1071 (2010).
Palacios, D. et al. TNF/p38α/polycomb signaling to
Pax7 locus in satellite cells links inflammation to the
epigenetic control of muscle regeneration. Cell Stem
Cell 7, 455–469 (2010).
Joe, A. W. B. et al. Muscle injury activates resident
fibro/adipogenic progenitors that facilitate myogenesis.
Nature Cell Biol. 12, 153–163 (2010).
Uezumi, A., Fukada, S., Yamamoto, N., Takeda, S. &
Tsuchida, K. Mesenchymal progenitors distinct from
satellite cells contribute to ectopic fat cell formation in
skeletal muscle. Nature Cell Biol. 12, 143–152 (2010).
Salleo, A., La Spada, G., Falzea, G., Denaro, M. G. &
Cicciarello, R. Response of satellite cells and muscle
NATURE REVIEWS | MOLECULAR CELL BIOLOGY
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
fibers to long-term compensatory hypertrophy.
J. Submicrosc. Cytol. 15, 929–940 (1983).
Rosenblatt, J. D. & Parry, D. J. Gamma irradiation
prevents compensatory hypertrophy of overloaded
mouse extensor digitorum longus muscle.
J. Appl. Physiol. 73, 2538–2543 (1992).
McCarthy, J. J. & Esser, K. A. Counterpoint: satellite cell
addition is not obligatory for skeletal muscle
hypertrophy. J. Appl. Physiol. 103, 1100–1102 (2007).
McCarthy, J. J. et al. Effective fiber hypertrophy in
satellite cell-depleted skeletal muscle. Development
138, 3657–3666 (2011).
Gilbert, P. M. et al. Substrate elasticity regulates
skeletal muscle stem cell self-renewal in culture.
Science 329, 1078–1081 (2010).
Williams, B. A. & Ordahl, C. P. Pax‑3 expression in
segmental mesoderm marks early stages in myogenic
cell specification. Development 120, 785–796 (1994).
Lagha, M. et al. Pax3:Foxc2 reciprocal repression in
the somite modulates muscular versus vascular cell fate
choice in multipotent progenitors. Dev. Cell 17,
892–899 (2009).
Aoyama, H. & Asamoto, K. Determination of somite
cells: independence of cell differentiation and
morphogenesis. Development 104, 15–28 (1988).
Borycki, A. G., Mendham, L. & Emerson, C. P. Jr.
Control of somite patterning by Sonic hedgehog and its
downstream signal response genes. Development 125,
777–790 (1998).
Tajbakhsh, S. et al. Differential activation of Myf5 and
MyoD by different Wnts in explants of mouse paraxial
mesoderm and the later activation of myogenesis in the
absence of Myf5. Development 125, 4155–4162 (1998).
Rios, A. C., Serralbo, O., Salgado, D. & Marcelle, C.
Neural crest regulates myogenesis through the
transient activation of NOTCH. Nature 473, 532–535
(2011).
Heymann, S., Koudrova, M., Arnold, H., Köster, M. &
Braun, T. Regulation and function of SF/HGF during
migration of limb muscle precursor cells in chicken.
Dev. Biol. 180, 566–578 (1996).
Dellavalle, A. et al. Pericytes of human skeletal muscle
are myogenic precursors distinct from satellite cells.
Nature Cell Biol. 9, 255–267 (2007).
Dellavalle, A. et al. Pericytes resident in postnatal skeletal
muscle differentiate into muscle fibres and generate
satellite cells. Nature Commun. 2, 499 (2011).
Sampaolesi, M. et al. Mesoangioblast stem cells
ameliorate muscle function in dystrophic dogs.
Nature 444, 574–579 (2006).
Asakura, A., Seale, P., Girgis-Gabardo, A. &
Rudnicki, M. A. Myogenic specification of side
population cells in skeletal muscle. J. Cell Biol. 159,
123–134 (2002).
Tanaka, K. K. et al. Syndecan-4‑expressing muscle
progenitor cells in the SP engraft as satellite cells
during muscle regeneration. Cell Stem Cell 4, 217–225
(2009).
Seale, P., Ishibashi, J., Scimè, A. & Rudnicki, M. A.
Pax7 is necessary and sufficient for the myogenic
specification of CD45+:Sca1+ stem cells from injured
muscle. PLoS Biol. 2, e130 (2004).
Xynos, A. et al. Bone marrow-derived hematopoietic
cells undergo myogenic differentiation following a Pax‑7
independent pathway. Stem Cells 28, 965–973 (2010).
Mitchell, K. J. et al. Identification and characterization
of a non-satellite cell muscle resident progenitor during
postnatal development. Nature Cell Biol. 12, 257–266
(2010).
Acknowledgements
We thank F. Bentzinger and H. Yin for critical reading of the
manuscript. Y.X.W. is supported by a fellowship from the
Ontario Research Fund and by the Canadian Institutes of
Health Research (CIHR) Training Program in Regenerative
Medicine. M.A.R. holds the Canada Research Chair in
Molecular Genetics and is an International Research Scholar
of the Howard Hughes Medical Institute. The work from the
laboratory of M.A.R. is supported by grants from the US
National Institutes of Health, the Howard Hughes Medical
Institute, the CIHR, the Muscular Dystrophy Association and
the Canada Research Chair Program.
Competing interests statement
The authors declare no competing financial interests.
FURTHER INFORMATION
Michael A. Rudnicki’s homepage: http://www.rudnickilab.ca
ALL LINKS ARE ACTIVE IN THE ONLINE PDF
VOLUME 13 | FEBRUARY 2012 | 133
© 2012 Macmillan Publishers Limited. All rights reserved
Cell, Vol. 122, 659–667, September 9, 2005, Copyright ©2005 by Elsevier Inc. DOI 10.1016/j.cell.2005.08.021
Cellular and Molecular Signatures
Review
of Muscle Regeneration: Current
Concepts and Controversies in Adult Myogenesis
Amy J. Wagers1,2,* and Irina M. Conboy3,*
1
Section on Developmental and Stem Cell Biology
Joslin Diabetes Center and Department of Pathology
Harvard Medical School
Boston, Massachusetts 02215
2
Harvard Stem Cell Institute
Cambridge, Massachusetts 02138
3
Department of Bioengineering
University of California, Berkeley
Berkeley, California 94702
Adult skeletal muscle generates force in a controlled
and directed manner through the contraction of highly
specialized, postmitotic, multinucleated myofibers. Lifelong muscle function relies on maintenance and regeneration of myofibers through a highly regulated process
beginning with activation of normally quiescent muscle
precursor cells and proceeding with formation of proliferating progenitors that fuse to generate differentiated
myofibers. In this review, we describe the historical
basis and current evidence for the identification of
satellite cells as adult muscle stem cells, critically
evaluate contributions of other cells to adult myogenesis, and summarize existing data regarding the origins, genetic markers, and molecular regulation of
satellite cells in normal, diseased, and aged muscle.
Satellite Cells as Adult Muscle Precursor Cells
and Candidate Muscle Stem Cells
Adult skeletal muscle possesses remarkable regenerative capacity, and large numbers of new myotubes normally are formed in only a few days after acute muscle
damage (Bintliff and Walker, 1960; LeGros Clark, 1946;
Walton and Adams, 1956; Weber, 1863). Early hypotheses proposed that new myofibers were generated via
budding of myotubes from existing, injured fibers (LeGros
Clark, 1946; Volkmann, 1893); however, further study has
demonstrated instead that this rapid repair occurs
through the differentiation and subsequent cell fusion
of myogenically specified mononuclear precursor cells
contained within a population of “satellite cells” positioned between the plasma membrane and the surrounding basal lamina of mature, differentiated muscle
fibers (Mauro, 1961; Snow, 1978). Alexander Mauro first
proposed in 1961 that satellite cells might represent
“dormant myoblasts” left over from embryonic muscle
development and capable of recapitulating the developmental program of skeletal myogenesis in response
to muscle damage (Mauro, 1961). Subsequent studies,
in both the chick (Konigsberg, 1963) and mouse (Yaffe,
1969), demonstrated that multinucleated myotubes
could indeed be generated in vitro from single myo*Correspondence: amy.wagers@joslin.harvard.edu (A.J.W.); iconboy@
berkeley.edu (I.M.C.)
genic precursor cells, and that these precursors ultimately derived from muscle satellite cells (Bischoff,
1975). Furthermore, in vivo-labeled (Snow, 1978), and
clonally cultured in vitro-labeled (Lipton and Schultz,
1979), satellite cells were shown to participate in the
regeneration of damaged muscle when transplanted
in vivo, contributing almost exclusively via fusion with
pre-existing myofibers. Pulse-chase experiments using
a single dose of tritiated thymidine to label dividing
cells indicated that DNA synthesis among sublaminar
nuclei was limited to satellite cell nuclei, and that true
muscle nuclei do not undergo mitosis (Moss and
Leblond, 1970). Although these methods labeled satellite cells relatively infrequently, indicating the relative
quiescence of satellite cells (Schultz et al., 1978), in
some cases DNA label from satellite cells marked during the pulse phase eventually appeared in myonuclei
during the chase phase, demonstrating the capacity of
at least some satellite cell progeny to incorporate into
existing myofibers, even in the absence of acute tissue
injury (Moss and Leblond, 1970). Such studies formed
the basis for our current view of muscle satellite cells
as the primary mediators of postnatal muscle growth
and repair. These cells respond to regenerative cues,
such as injury or exercise, by proliferating to form myoblasts, which divide a limited number of times before
terminally differentiating and fusing to form multinucleated myotubes (reviewed in Morgan and Partridge,
2003; Sloper and Partridge, 1980) (see Figure 1A). The
life-long regenerative capacity of satellite cells implies
that they can be robustly and perpetually renewed
while maintaining the ability to generate differentiated
progeny and suggests that they may represent an adult
stem cell population for skeletal muscle.
Stem cells are thought to exist in many adult tissues
capable of regeneration and are defined by their unique
capacity to both self-renew and differentiate. Adult
stem cells have been best characterized in the mammalian blood-forming system, where clonogenic, multipotent hematopoietic stem cells (HSC) have been prospectively isolated from bone marrow and demonstrate
at the single-cell level the capacity to regenerate the
entire hematopoietic system (reviewed in Kondo et al.,
2003). While it is clear that satellite cells likewise contain unspecified precursor cells capable of extensive
proliferation and differentiation to generate mature
myofibers, to formally establish that they indeed function as adult stem cells, it will be necessary to demonstrate that individual cells within the satellite cell pool
maintain both self-renewal and differentiation potential
in vivo. Although this clonal analysis is still lacking, as
outlined below, multiple lines of evidence from in vitro
and in vivo studies do suggest that muscle stem cells
are contained within at least a subset of satellite cells.
First, as noted above, satellite cell number and regenerative capacity normally remain nearly constant
through multiple cycles of injury and repair, suggesting
satellite cell self-renewal. In addition, studies of isolated single myofibers and primary satellite cells maintained in culture have revealed that some cultured sat-
Cell
660
Taken together, these data strongly suggest that satellite cells represent self-renewing adult muscle stem
cells and alone are sufficient for muscle repair. This
conclusion likely will be strengthened by ongoing
studies of the capacity for and regulation of satellite
cell self-renewal, particularly those testing the continued regenerative potential of single or clonally marked
satellite cells in serial transplantations.
Figure 1. Regeneration of Skeletal Muscle via Cell-Cell Fusion
(A) Repair by endogenous myogenic satellite cells occurs in two
phases. First, a subset of differentiated myoblasts (Mb) fuse together to form a nascent myotube (Mt). Next, the Mt attracts and
fuses with additional Mb and, with further accretion of nuclei,
eventually forms a mature myofiber (Mf).
(B) Contributions from hematopoietic cells. The stage at which heterotypic fusion of myelomonocytic blood-lineage cells with muscle-lineage cells may occur in regenerating muscle has not been
defined but could involve interactions with damaged Mf, proliferating Mb, nascent Mt, or newly formed Mf.
ellite cells form clusters that contain both differentiated
progeny and cells that regain a phenotype characteristic of quiescent satellite cells (Pax-7+ and MyoD− or
myogenin−) (Olguin and Olwin, 2004; Zammit et al., 2004).
Furthermore, populations of neonatal, satellite cellderived myoblasts have been shown to generate both
differentiated myofibers and functional satellite cells
in vivo following intramuscular transplantation (Blaveri
et al., 1999; Heslop et al., 2001). In ex vivo explant cultures, satellite cells activated by muscle injury give rise
to intermediate progenitor cells expressing the myogenic transcription factor Pax-3, which divide asymmetrically and differentiate into Pax-3−, Myf-5hi, desminhi myoblasts (Conboy and Rando, 2002). This
progression along a myogenic lineage in adult muscle
resembles embryonic myogenesis, where Pax-3 induces the expression of Myf-5 and MyoD (Maroto et
al., 1997), and Pax-3+ pre-myoblast progenitor cells delaminate from somites and migrate into the limb buds
to generate fusion-competent myoblasts (Goulding et
al., 1994). Finally, the most compelling evidence for the
stem cell nature of satellite cells comes from recent
studies in which rigorously purified, single, intact myofibers, containing an average of only 7–22 associated
satellite cells, were transplanted into the radiationablated muscle of immunocompromised, dystrophic
(mdx-nude) hosts (Collins et al., 2005). The grafted fibers could give rise to over 100 new myofibers, contributing an estimated 25,000–30,000 differentiated myonuclei and, moreover, could regenerate substantially
expanded (up to 10-fold) numbers of functional Pax-7+
satellite cells in vivo. These donor-derived satellite cells
persisted in the skeletal muscle for at least several
weeks and could be reactivated and expanded in response to additional muscle injury (Collins et al., 2005).
Developmental Origins of Skeletal Muscle
and Satellite Cells
Myogenic precursors are specified during development
by signals emanating from neighboring cells of the notochord, neural tube, and dorsal ectoderm. This specification depends critically on the function of myogenic
transcription factors, such as Pax-3 and Pax-7 (Borycki
et al., 1999; Cossu et al., 1996a, 1996b; Goulding et al.,
1994). Once committed, somite-derived cells migrate to
multiple sites of embryonic myogenesis, begin to express the myogenic basic helix-loop-helix transcription
factors Myf-5 and MyoD (Birchmeier and Brohmann,
2000), and differentiate into muscle fibers. Somitederived myogenic progenitors that do not differentiate
into myofibers at this time have been suggested instead to be retained into adulthood as muscle satellite
cells (Armand et al., 1983; Mauro, 1961; Yablonka-Reuveni et al., 1987). This concept recently has been confirmed in two papers in which myogenic reporter strains
and cell-lineage tracing experiments demonstrated that
avian (Gros et al., 2005) and mouse (Relaix et al., 2005)
embryonic and fetal myogenic progenitor cells arise
from the central dermomyotome, following generation
of the primary myotome. Importantly, neonatal Pax-7+
progenitor cells found in the satellite cell position were
shown to originate also from the avian embryonic dermomyotome, indicating that some of the precursor
cells that contribute to embryonic and fetal muscle are
retained after birth as satellite cells (Gros et al., 2005).
In rapidly growing neonatal muscle, nuclei of satellite
cells and myoblasts comprise w30% of myofiber-associated nuclei, but after cessation of muscle growth, quiescent satellite cells represent only w5% of adult myofiber nuclei (Cardasis and Cooper, 1975). It remains to
be determined, however, whether the quiescent satellite cells in adult muscle have the same developmental
origin as embryonic, fetal, and neonatal cells, or, alternatively, if proliferating dermomyotome-derived myofibers-associated progenitors are exhausted during the
muscle growth, and subsequent regeneration of the
adult muscle invokes a distinct lineage of precursor
cells. Additional analysis of myogenic reporter markers
(Relaix et al., 2005) in older animals, and after repeated
rounds of muscle injury and regeneration, will be particularly informative to address this issue and also may
give further insight into the self-renewal potential of
embryonically specified dermomyotome-derived satellite cells.
Phenotypic and Functional Heterogeneity
of Satellite Cells
Satellite cells are classically defined by their position
beneath the basal lamina and by their ability to undergo
myogenic differentiation (Beauchamp et al., 2000; Mauro,
Review
661
1961). However, accumulating evidence suggests that
the satellite cell compartment contains cells of distinct
ontogeny and function. First, although several markers
have been associated with satellite cells, no single
marker defines all satellite cells. For example, while
most satellite cells express the surface protein CD34
(Beauchamp et al., 2000; Conboy and Rando, 2002;
Sherwood et al., 2004a), they can variably express
other surface markers (Sherwood et al., 2004a), as well
as myogenic transcription factors, such as Pax-7,
MyoD, and Myf-5 (Beauchamp et al., 2000; Cornelison
and Wold, 1997; Zammit et al., 2004). CD34 and Pax-7
identify quiescent satellite cells, and Pax-7, M-Cadherin, MyoD, and Myf-5 are actually upregulated with
differentiation of satellite cells into myoblasts (Morgan
and Partridge, 2003; Seale et al., 2000, 2004). This
heterogeneity of marker expression may reflect functional differences among satellite cells or distinct
stages of myogenic lineage specification or may distinguish myogenic from nonmyogenic cell types within
myofiber compartment. In this regard, it is interesting
that in vitro studies have shown that some cells emerging from explanted single myofibers can express markers of osteocytes or adipocytes, rather than myogenic
markers (Asakura et al., 2001; Csete et al., 2001). Recent studies from our group (Sherwood et al., 2004a)
and others (Shefer et al., 2004) have indicated that single cells from within the satellite-cell compartment exhibit mutually exclusive abilities to generate either myogenic or fibroblastic and adipogenic colonies in clonal
in vitro assays. Importantly, activated immune or inflammatory cells may also populate the satellite-cell
compartment, infiltrating beneath the basal lamina of
damaged muscle fibers (Stauber et al., 1988), although
such infiltrating hematopoietic cells display no myogenic activity (Sherwood et al., 2004a). Finally, intrinsic
differences in proliferation (Beauchamp et al., 1999;
Rantanen et al., 1995; Rouger et al., 2004; YablonkaReuveni et al., 1987), differentiation (Rantanen et al.,
1995; Zammit et al., 2004), and fusogenic capacity
(Rouger et al., 2004) among individual satellite cells
have been reported. More detailed studies employing
prospective isolation and/or clonal marking to further
delineate the precise lineage relationships, cellular interaction, and myogenic capacities of these distinct
populations of myofiber-associated cells will greatly
enhance our understanding of their normal roles and
relative importance during muscle regeneration.
Adult Myogenic Cells Distinct from Satellite Cells
Recent reports have suggested that adult skeletal muscle progenitors distinct from satellite cells may function
in some models of muscle injury and repair. For example, muscle-resident side population (muSP) cells, defined by their ability to exclude Hoechst 33342 (Asakura
et al., 2002), have been shown to contribute to myofibers when injected intramuscularly (McKinney-Freeman et al., 2002) or when cocultured with myoblasts
(Asakura et al., 2002), although these cells lack myogenic activity when cultured alone (Asakura et al.,
2002). Similarly, although they do not generate myogenic cells when cultured alone, interstitial muscle-resident CD45+Sca-1+ cells reportedly acquire myogenic
activity when cocultured with primary myoblasts or in
response to muscle injury or Wnt signaling (Polesskaya
et al., 2003). Finally, cells with high proliferative potential and surprisingly broad differentiation capacity, and
thus termed “muscle-derived stem cells” (MDSC) or
“multipotent adult progenitor cells” (MAPC), have been
isolated following prolonged culture of cells from muscle (Cao et al., 2003; Jiang et al., 2002; Qu-Petersen et
al., 2002).
Descriptions of these distinct subsets of myogenic
cells have raised the possibility that multiple mechanisms may support adult skeletal muscle regeneration.
Yet, as compared to conventional satellite cells, many
of these populations, with the notable exception of cultured MDSC (Qu-Petersen et al., 2002), display vanishingly small myogenic potential. In addition, in all cases,
the contribution of these cells to the maintenance or
repair of skeletal muscle under physiologic conditions
is uncertain, and their therapeutic potential has not
been clearly established. Moreover, recent data suggest that satellite cells are alone sufficient to mediate
extensive regeneration of damaged adult skeletal muscle in vivo (Collins et al., 2005). Thus, in further assessing the intrinsic myogenic function of these populations, it will be essential to exclude the possibility that
their activity derives from “contamination” with a small
subset of highly myogenic satellite cells or their progeny or from a change in developmental potential induced by cell culture. The use of lineage-tracing methods (Gros et al., 2005; Relaix et al., 2005) and single
myofiber transplantation (Collins et al., 2005) will be a
key first step in determining the myogenicity of these
populations in relationship to conventional satellite cells.
Bone marrow cells (Ferrari et al., 1998; Fukada et al.,
2002; Gussoni et al., 1999; LaBarge and Blau, 2002),
and even single hematopoietic stem cells (Camargo et
al., 2003; Corbel et al., 2003; Sherwood et al., 2004b),
also have been reported to contribute to myofibers
when injected directly into injured muscle or intravenously into irradiated injured or dystrophic animals. The
frequency with which these unexpected contributions
to skeletal muscle have been detected has varied
widely and, while generally quite low (<1% of total myofibers; Camargo et al., 2003; Corbel et al., 2003; Ferrari
et al., 1998; Gussoni et al., 1999; Sherwood et al.,
2004b), has been reported in some cases to reach
levels of 5%–12% of differentiated cells (Abedi et al.,
2004; LaBarge and Blau, 2002). In this regard, it is worth
noting that the method of detection of donor-derived
myofibers can significantly influence the estimation of
donor contributions, and assay systems employing
highly diffusible markers, such as GFP (Jockusch and
Voigt, 2003), cannot accurately quantify the numbers
of donor myonuclei incorporated due to spread of the
marker throughout the myofiber. In any case, such observations initially generated a great deal of excitement, suggesting that bone marrow could represent a
reasonably accessible, novel source of regenerative
cells for muscle repair; however, as with other nonsatellite cell populations, the physiological significance of
bone marrow contributions to skeletal muscle remains
uncertain (Ferrari et al., 2001; Gussoni et al., 2002), and
accumulating evidence suggests that these events may
in fact represent an accidental or even pathological re-
Cell
662
sponse elicited by severe muscle damage and inflammation (see below).
Interestingly, while early efforts aimed at eliciting
myogenic activity from bone marrow cells focused
largely on the hematopoietic lineages, recent studies
have suggested that nonhematopoietic elements isolated from adult bone marrow or from embryonic sites
of hematopoietic development might eventually be
harnessed for therapeutic skeletal muscle regeneration. For instance, cultured “mesangioblasts” (Minasi et
al., 2002), a subset of blood vessel-associated cells
originating from the embryonic dorsal aorta region,
which have been shown to generate multiple mesodermal cell types following in vivo transplantation, can,
when injected intra-arterially into dystrophic α-sarcoglycan knockout mice, contribute to myofiber formation
and significantly improve muscle function (Sampaolesi
et al., 2003). In addition, clonal, cultured marrow-derived
stromal cells, lacking expression of CD34, c-Kit, and
CD45, have been shown to participate in myogenesis
in vitro and in vivo, regenerating myofibers and sublaminar Pax-7+ satellite cells in immunocompromised dystrophic mice (Dezawa et al., 2005). Significantly, the
myogenic contributions from marrow stromal cells observed in this study were much more robust than those
typical of BM-derived HSC or hematopoietic progenitor
cell subsets; however, it is important to note that the
activation of a myogenic program by these stromal
cells absolutely required in vitro induction, first by culturing the cells with certain growth factors and then by
ectopic expression of constitutively active Notch-1 (Dezawa et al., 2005). Thus, while this work suggests a
promising therapeutic potential of marrow stromal
cells, these data do not necessarily suggest that analogous populations of marrow cells normally contribute
to physiologic muscle regeneration.
In summary, while under particular conditions some
cells apparently distinct from satellite cells can contribute to muscle tissue, the preponderance of evidence
indicates that the myogenic activity normally responsible for robust adult muscle regeneration is largely restricted to sublaminar CD34+ satellite cells.
Mechanisms of Bone Marrow Contribution to Skeletal
Muscle: Cell Fusion or Transdifferentiation?
In most studies in which hematopoietic or bone marrow-derived contributions to skeletal muscle have been
detected, significant muscle injury has been necessary,
except in particular muscles (e.g., panniculus carnosus)
(Corbel et al., 2003; Sherwood et al., 2004b). The mechanisms underlying these contributions have been an
area of intense research. While initial reports appeared
to favor the direct “transdifferentiation” of transplanted
BM cells to generate satellite cells (Fukada et al., 2002;
LaBarge and Blau, 2002), more recent studies have indicated that donor-marker-expressing myofibers arise
via fusion of donor hematopoietic cells with host muscle cells (Camargo et al., 2003; Doyonnas et al., 2004;
Sherwood et al., 2004b) (Figure 1B). While the precise
cell types involved in these fusion events have not been
fully defined, transplantation of BM cells from transgenic mice expressing Cre in a hematopoietic lineagerestricted manner suggests that at least one of the fu-
sion partners is likely to be a committed blood myeloid
cell (Camargo et al., 2003; Doyonnas et al., 2004). The
stage of differentiation at which muscle-lineage cells
participate in heterotypic cell fusions with infiltrating
hematopoietic cells remains unknown (Figure 1B). However, when considering the mechanism by which
hematopoietic cells fuse with muscle cells, it is important to remember that normally muscle is repaired by
fusion of myoblasts with each other, with nascent myotubes, and/or with damaged multinucleated fibers.
Thus, macrophages and other inflammatory cells known
to infiltrate injured muscle fibers (Stauber et al., 1988)
almost certainly are exposed to physiologic fusogenic
signals. Significantly, macrophages themselves are
known to undergo cell-cell fusion both physiologically,
to generate osteoclasts, and pathologically, to generate
multinucleated giant cells (Vignery, 2000). Therefore,
heterotypic cell fusion between endogenous muscle
cells and infiltrating blood cells may occur via mechanisms that normally allow the homotypic fusion of these
cells in the context of tissue maintenance and repair. At
present the molecular mediators, as well as the overall
significance, of these rare events remain unclear. Future
studies using coculture or transplantation models will
be required to identify the secreted factors, cell-surface
receptors, and signaling pathways involved in bloodcell/muscle-cell fusion. Knowledge of these mechanisms ultimately should allow experiments to block its
occurrence and thereby test its physiologic importance.
Prospective Isolation of Muscle Precursor Cells
We recently reported a methodology that permits the
prospective isolation by fluorescence-activated cell
sorting (FACS) of highly myogenic muscle precursor
cells from other cell populations contained within the
satellite-cell compartment (Sherwood et al., 2004a).
Combinatorial analysis of multiple cell-surface markers
indicated that autonomously myogenic colony-forming
cells (CFC) were highly enriched among the CD45−Sca1−Mac-1−CXCR4+β1-integrin+ (CSM4B) subset of myofiber-associated satellite cells, and that individual
CSM4B cells efficiently form myogenic colonies, which
express myosin heavy chain (MyHC) upon induction of
myogenic differentiation in vitro. CSM4B cells are contained within a population of cells (CD45−Sca-1−CD34+)
that also generates myofibers in vivo upon intramuscular injection and expresses mRNA encoding the myogenic transcription factors MyoD, Myf-5, and Pax-7
(Sherwood et al., 2004a).
The precise relationship of the CSM4B subset of myofiber-associated cells to previously described satellite
cells is clearly of interest in synthesizing recent literature and developing a further understanding of skeletal
muscle biology and regeneration. These cells coexpress
CD34 and c-met, previously reported satellite-cell surface
markers (Beauchamp et al., 2000; Cornelison et al., 2001),
but are not contained in c-kit+, CD13+, CD71+, Flk-1+,
CD105+, CD44+, α1-integrin+, or α6-integrin+ populations of myofiber-associated cells. They also fail to express the pan-hematopoietic marker CD45 and the surface protein Sca-1, in either resting or regenerating (2
days following cardiotoxin injection) muscle; both CD45
and Sca-1 have been reported by others (Polesskaya
Review
663
et al., 2003) to identify a subset of Wnt-responsive muscle-regenerative cells distinct from satellite cells and
likely residing in the muscle interstitium. Finally, CSM4B
cells are not derived from transplanted bone marrow
cells and are not repopulated from the circulation at
detectable levels, indicating that they likely arise from
and are maintained by a lineage of cells distinct from
bone marrow-derived, hematopoietic, and fibroblastic
cells also present in muscle. These data are consistent
with previous studies in muscle transplantation systems indicating that muscle repair does not generally
involve the recruitment of regenerative cells from a distance (Jockusch and Voigt, 2003; Washabaugh et al.,
2004).
Other groups similarly have undertaken phenotypic
analysis and prospective isolation of myogenic satellite-cell populations. Using Pax-3/GFP “knockin” mice,
in which a GFP marker reports transcriptional activity
of the Pax-3 locus, Montarras and colleagues also isolated a highly regenerative population of myogenic precursor cells. Like CSM4B cells, these Pax-3+ cells are
largely CD34+, CD45−, and Sca-1− (Montarras et al.,
2005). In these studies, intramuscular delivery of only a
few thousand freshly sorted CD34+CD45−Sca-1− cells
yielded substantial regeneration of normal myofibers in
irradiated mdx-nude recipients; however, strikingly, cell
culture prior to transplant dramatically reduced the efficiency of muscle engraftment (by as much as 10-fold).
Biochemical Pathways Regulating
Muscle Regeneration
Muscle remodeling involves myogenesis, reinnervation,
and revascularization and is regulated by multiple
biochemical pathways, including those initiated by inflammatory cytokines, growth factors, and the evolutionarily conserved Notch, Wnt, and Sonic Hedgehog
(Shh) signaling pathways (Conboy and Rando, 2002;
Husmann et al., 1996; Pola et al., 2003; Polesskaya et
al., 2003; Tidball, 2005). Muscle repair coincides with
injury-induced inflammation, and some inflammatory
cytokines, such as IL-4, LIF, TGF-β, IL-6, and TNF-α
regulate myogenic potential (Tidball, 2005). Damaged
muscle produces monocyte and macrophage chemoattractants, and blockade of inflammatory cell infiltration impairs muscle regeneration (Chazaud et al., 2003;
Jejurikar and Kuzon, 2003; Lescaudron et al., 1999),
possibly due to a reduction in macrophage-secreted
factors inducing myoblast proliferation (Bondesen et
al., 2004; Robertson et al., 1993).
In addition to initiating the inflammatory response, injury promotes the release of growth factors that bind to
extracellular matrix (ECM) proteins, such as proteoheparan sulfates (Husmann et al., 1996). This process involves the activity of matrix metalloproteinases, recently shown to play a role in muscle repair (Carmeli et
al., 2004). The most studied growth factors participating in muscle maintenance and regeneration are FGFs,
HGF, IGF-1, and GDF8/myostatin (Heszele and Price,
2004; Husmann et al., 1996; Lee, 2004; Miller et al., 2000).
FGF-2 and HGF promote proliferation of myogenic progenitors and delay their differentiation, in part by inhibiting the expression of myogenic regulatory factors,
such as MyoD (Maley et al., 1994; Miller et al., 2000).
Both growth factors require heparan sulfate proteoglycans for signaling via their receptors, and syndecan-3
and -4 have been identified as the relevant cell-surface
proteoglycans expressed by satellite cells (Cornelison
et al., 2001). IGF-1 promotes myogenic differentiation
and enhances protein synthesis in differentiated myofibers by activating the translation factor 4E-BP and the
ribosomal protein S6 kinase (p70S5K) and by inhibiting
muscle-specific E3 ligases that promote protein degradation (reviewed in Heszele and Price, 2004). These
mechanisms and the antiapoptotic effects of IGF-1 via
the suppression of caspases and activation of Akt
(Downward, 2004; Lawlor and Rotwein, 2000) likely explain why IGF-1 attenuates experimentally induced
muscle wasting (Shavlakadze et al., 2005). On the other
end of the proliferative spectrum, the muscle-specific
TGF-β family member, GDF8, inhibits cell-cycle progression in myogenic progenitors during embryonic development and in adult muscle via induction of p21 and
suppression of the cyclin-dependent kinase CDK25
(McCroskery et al., 2003; McPherron et al., 1997;
Thomas et al., 2000; Zimmers et al., 2002).
The appropriate expansion followed by the timely differentiation of myogenic progenitor cells during muscle
repair appear to be regulated by the same conserved
mechanisms that orchestrate embryonic organogenesis. Namely, proliferation of satellite cells in response
to muscle injury is positively regulated by the Notch
pathway, while terminal myogenic differentiation of
these cells requires the inhibition of Notch by its intracellular antagonist Numb (Conboy and Rando, 2002).
Notch receptor is expressed in quiescent satellite cells,
and Notch signal transduction responsible for satellitecell activation is initiated by the upregulation of Notch
ligand, Delta, on the fibers adjacent to the damaged
muscle and on the satellite cells themselves (Conboy
et al., 2003; Conboy and Rando, 2002). The recent demonstration that BM-derived stromal cells become myogenic after stable expression of constitutively active
Notch-1 (Dezawa et al., 2005) may suggest that activation of the Notch pathway generally regulates specification of organ precursor cells toward a myogenic lineage when other myogenic factors, such as FGF-2,
are present.
In addition to Notch, Shh mRNA and protein, as well
as the Patched receptor, become upregulated in regenerating skeletal muscle (Pola et al., 2003). Moreover, ectopic Shh appears to ameliorate experimentally induced muscle atrophy (Alzghoul et al., 2004), thus
demonstrating that yet another classic regulator of embryonic development likely also participates in adult
myogenesis. Additionally, Wnt signaling has been reported to be important for the presence of CD45+ cells
in regenerating adult muscle, although the physiologic
myogenic potential of these cells remains unclear
(Polesskaya et al., 2003; Sherwood et al., 2004a). Future
experiments that decipher how muscle regulates its
own inflammatory response and clarify the temporal
and spatial crosstalk between Notch, Shh, and Wnt
pathways will be instrumental for providing a better understanding of how cell fate is determined during muscle repair.
Cell
664
Satellite-Cell Activity in Diseased Muscle
In certain pathological states, including congenital myopathies, denervation, and muscle atrophy, satellitecell numbers and proliferative potential may decrease
(Jejurikar and Kuzon, 2003). In muscular dystrophy
(MD), repeated cycles of muscle regeneration, brought
on by repeated loss of differentiated tissue, may lead
to an early loss of the proliferative potential of satellite
cells in these patients, and a subsequent failure to
maintain muscle homeostasis (Luz et al., 2002). Although the underlying mechanism for this loss of satellite-cell responsiveness in diseased muscle has not
been fully elucidated, these findings indicate that under
particular circumstances satellite cells may be functionally exhausted. Satellite-cell exhaustion may relate,
at least in part, to shortening of telomere ends after
repeated rounds of DNA replication (Collins et al., 2003;
Di Donna et al., 2003), to recurrent exposure to inflammatory conditions and/or oxidative stress (Renault et
al., 2002), to an accumulation of mutations in key satellite-cell regulatory genes, introduced during repeated
rounds of proliferation, or to a combination of these and
other factors. Nonmyogenic cells in the muscle may
also contribute to failed muscle regeneration, as fibroblasts in dystrophic patients have been shown to
secrete increased levels of IGF-1 binding proteins,
which could sequester this cytokine away from myogenic cells (Melone et al., 2000). A better understanding
of the dynamic interplay among distinct populations of
cells resident in the muscle and recruited by muscle
damage will aid in developing a full picture of the complex cellular networks responsible for myogenesis in
healthy and diseased muscle and for designing therapeutic strategies to promote muscle repair.
Age-Related Changes in the Molecular Regulation
of Satellite Cell Activity
One characteristic of aging is a decline in the ability of
organ stem cells to repair damaged tissues. Adult skeletal muscle is a perfect example of a tissue that robustly regenerates throughout adult life but fails to do
so in old age (Grounds, 1998). The reason for this decline in regenerative potential is not completely understood and may involve both intrinsic molecular changes
in the stem cells themselves and/or alterations in their
aged environment.
As mentioned above, muscle repair relies on Notch
activity, which is necessary and sufficient for the activation of satellite cells (Artavanis-Tsakonas et al., 1999;
Conboy et al., 2003; Conboy and Rando, 2002). Importantly, Notch receptor continues to be expressed in
aged satellite cells, while injury-specific induction of
the Notch ligand Delta, and therefore subsequent signal transduction, fail with age, resulting in grossly inefficient regeneration of old muscle tissue (Conboy et al.,
2003). Strikingly, productive tissue repair can be restored to old muscle by enforced activation of Notch,
while the repair of young muscle is severely perturbed
when Notch signaling is inhibited (Conboy et al., 2003).
Therefore, it seems that Notch is the key age-related
determinant of muscle regenerative potential.
Is the age-related decline in satellite cell regenerative
potential intrinsic or dependent on the cell environ-
ment? In early muscle transplantation studies, small
minced or intact muscle from young or old rodents was
transplanted into either young or old muscle beds, and
the ability of donor muscle pieces to regenerate in the
middle of either young or old host limbs was examined.
Amazingly, the efficiency of muscle regeneration was
clearly determined in these experiments by the age of
the host environment, rather than by the age of the
muscle donor (Carlson and Faulkner, 1989; Zacks and
Sheff, 1982). In these important studies, the small transplanted muscle was physically isolated from the host
satellite cells, revealing the effects of prevalent local
and organismal environments on the regenerative potential of the donor satellite cells.
In more recent studies, the age of the systemic environment likewise dominated over the intrinsic agerelated regenerative properties of satellite cells when
the efficiency of muscle repair was examined in young
and old mice with a shared blood circulation (Conboy
et al., 2005). Significantly, regeneration-specific DeltaNotch signaling, appropriate activation of satellite cells,
and general success in muscle repair were all rejuvenated by the exposure of aged tissue to a young systemic milieu (Conboy et al., 2005). In concert with the
above-mentioned pivotal role of satellite cells as muscle stem cells, the aged satellite cells endogenous to
the old muscle successfully engaged in tissue repair
without any recruitment of young cells from the shared
circulation (Conboy et al., 2005). These data strongly
suggest that the molecular pathways responsible for
muscle repair are regulated by systemic factors and
that these factors change with age in ways precluding
the activation of satellite cells.
Multiple lines of evidence suggest that many cellintrinsic changes occur with tissue aging, including the
accumulation of oxidative damage, a decline in genome
maintenance, and diminished mitochondrial function
(Ames, 2004; Golden et al., 2002; Hasty et al., 2003).
The rejuvenation of aged stem and progenitor cells by
the young extrinsic milieu, even in the presence of
these age-related changes, suggests the intriguing
possibility that the aging of organ stem cells might be
regulated extrinsically and that the molecular changes
underlying the loss of the tissue-regenerative potential
with age can be reversed or overcome if the stem cell
niche is young. Future identification of the relevant extrinsic age-related components will be instrumental for
therapies aimed at enhancing the regenerative potential of organ stem cells in aged individuals.
Future Avenues and Perspectives
It is quite clear that endogenous skeletal muscle satellite cells associated with myofibers account for most, if
not all, physiologic muscle-regenerative potential and
likely represent muscle stem cells. Recent advances
have allowed a more refined determination of their origin, position in the myogenic cell lineage, and molecular pathways regulating their function. Other avenues of
muscle repair, e.g., by bone marrow-derived cells, may
exist; however, unambiguous determination of the precise cell types and specific fusion and reprogramming
mechanisms involved in this process will be needed in
order to establish whether such cells form muscle tis-
Review
665
sue under physiologic conditions or can be used therapeutically. Current advances in our understanding of
the cellular and molecular mechanisms regulating cellfate determination and tissue specification during adult
muscle repair have indicated a remarkable conservation of developmentally regulated signal transduction
pathways, and age-related analysis of these pathways
indicates that at least some of them deteriorate in old
muscle, causing ineffective tissue repair. The identification of age-related systemic factors that regulate the
regenerative capacity of organ stem cells will improve
our understanding of aging as a conserved biological
process and will help to develop therapies for the enhancement of the regenerative potential often lost in
old age or disease.
Acknowledgments
We thank T. Partridge and D. Montarras for communication of unpublished data and for helpful discussions. This work was supported in part by a Burroughs Wellcome Fund Career Award and a
Harvard Stem Cell Institute Seed Funding Grant to A.J.W. and NIA
KO-1 AG25652 to I.M.C.
References
Abedi, M., Greer, D.A., Colvin, G.A., Demers, D.A., Dooner, M.S.,
Harpel, J.A., Weier, H.U., Lambert, J.F., and Quesenberry, P.J.
(2004). Robust conversion of marrow cells to skeletal muscle with
formation of marrow-derived muscle cell colonies: a multifactorial
process. Exp. Hematol. 32, 426–434.
Alzghoul, M.B., Gerrard, D., Watkins, B.A., and Hannon, K. (2004).
Ectopic expression of IGF-I and Shh by skeletal muscle inhibits
disuse-mediated skeletal muscle atrophy and bone osteopenia
in vivo. FASEB J. 18, 221–223.
phic mouse muscle: studies on isolated fibers. Dev. Dyn. 216,
244–256.
Bondesen, B.A., Mills, S.T., Kegley, K.M., and Pavlath, G.K. (2004).
The COX-2 pathway is essential during early stages of skeletal
muscle regeneration. Am. J. Physiol. Cell Physiol. 287, C475–C483.
Borycki, A.G., Li, J., Jin, F., Emerson, C.P., and Epstein, J.A. (1999).
Pax3 functions in cell survival and in pax7 regulation. Development
126, 1665–1674.
Camargo, F.D., Green, R., Capetenaki, Y., Jackson, K.A., and
Goodell, M.A. (2003). Single hematopoietic stem cells generate
skeletal muscle through myeloid intermediates. Nat. Med. 9,
1520–1527.
Cao, B., Zheng, B., Jankowski, R.J., Kimura, S., Ikezawa, M., Deasy,
B., Cummins, J., Epperly, M., Qu-Petersen, Z., and Huard, J. (2003).
Muscle stem cells differentiate into haematopoietic lineages but
retain myogenic potential. Nat. Cell Biol. 5, 640–646.
Cardasis, C.A., and Cooper, G.W. (1975). An analysis of nuclear
numbers in individual muscle fibers during differentiation and
growth: a satellite cell-muscle fiber growth unit. J. Exp. Zool. 191,
347–358.
Carlson, B.M., and Faulkner, J.A. (1989). Muscle transplantation between young and old rats: age of host determines recovery. Am. J.
Physiol. 256, C1262–C1266.
Carmeli, E., Moas, M., Reznick, A.Z., and Coleman, R. (2004). Matrix metalloproteinases and skeletal muscle: a brief review. Muscle
Nerve 29, 191–197.
Chazaud, B., Sonnet, C., Lafuste, P., Bassez, G., Rimaniol, A.C.,
Poron, F., Authier, F.J., Dreyfus, P.A., and Gherardi, R.K. (2003). Satellite cells attract monocytes and use macrophages as a support
to escape apoptosis and enhance muscle growth. J. Cell Biol. 163,
1133–1143.
Collins, C.A., Olsen, I., Zammit, P.S., Heslop, L., Petrie, A., Partridge, T.A., and Morgan, J.E. (2005). Stem cell function, selfrenewal, and behavioral heterogeneity of cells from the adult muscle satellite cell niche. Cell 122, 1–13.
Ames, B.N. (2004). Delaying the mitochondrial decay of aging. Ann.
N Y Acad. Sci. 1019, 406–411.
Collins, M., Renault, V., Grobler, L.A., St Clair Gibson, A., Lambert,
M.I., Wayne Derman, E., Butler-Browne, G.S., Noakes, T.D., and
Mouly, V. (2003). Athletes with exercise-associated fatigue have abnormally short muscle DNA telomeres. Med. Sci. Sports Exerc. 35,
1524–1528.
Armand, O., Boutineau, A.M., Mauger, A., Pautou, M.P., and Kieny,
M. (1983). Origin of satellite cells in avian skeletal muscles. Arch.
Anat. Microsc. Morphol. Exp. 72, 163–181.
Conboy, I.M., and Rando, T.A. (2002). The regulation of Notch signaling controls satellite cell activation and cell fate determination
in postnatal myogenesis. Dev. Cell 3, 397–409.
Artavanis-Tsakonas, S., Rand, M.D., and Lake, R.J. (1999). Notch
signaling: cell fate control and signal integration in development.
Science 284, 770–776.
Conboy, I.M., Conboy, M.J., Smythe, G.M., and Rando, T.A. (2003).
Notch-mediated restoration of regenerative potential to aged muscle. Science 302, 1575–1577.
Asakura, A., Komaki, M., and Rudnicki, M. (2001). Muscle satellite
cells are multipotential stem cells that exhibit myogenic, osteogenic, and adipogenic differentiation. Differentiation 68, 245–253.
Conboy, I.M., Conboy, M.J., Wagers, A.J., Girma, E.R., Weissman,
I.L., and Rando, T.A. (2005). Rejuvenation of aged progenitor cells
by exposure to a young systemic environment. Nature 433, 760–
764.
Asakura, A., Seale, P., Girgis-Gabardo, A., and Rudnicki, M.A.
(2002). Myogenic specification of side population cells in skeletal
muscle. J. Cell Biol. 159, 123–134.
Beauchamp, J.R., Morgan, J.E., Pagel, C.N., and Partridge, T.A.
(1999). Dynamics of myoblast transplantation reveal a discrete minority of precursors with stem cell-like properties as the myogenic
source. J. Cell Biol. 144, 1113–1122.
Beauchamp, J.R., Heslop, L., Yu, D.S., Tajbakhsh, S., Kelly, R.G., Wernig, A., Buckingham, M.E., Partridge, T.A., and Zammit, P.S. (2000).
Expression of CD34 and Myf5 defines the majority of quiescent adult
skeletal muscle satellite cells. J. Cell Biol. 151, 1221–1234.
Bintliff, S., and Walker, B.E. (1960). Radioautographic study of skeletal muscle regeneration. Am. J. Anat. 106, 233.
Corbel, S.Y., Lee, A., Yi, L., Duenas, J., Brazelton, T.R., Blau, H.M.,
and Rossi, F.M. (2003). Contribution of hematopoietic stem cells to
skeletal muscle. Nat. Med. 9, 1528–1532.
Cornelison, D.D., Filla, M.S., Stanley, H.M., Rapraeger, A.C., and
Olwin, B.B. (2001). Syndecan-3 and syndecan-4 specifically mark
skeletal muscle satellite cells and are implicated in satellite cell
maintenance and muscle regeneration. Dev. Biol. 239, 79–94.
Cornelison, D.D., and Wold, B.J. (1997). Single-cell analysis of regulatory gene expression in quiescent and activated mouse skeletal
muscle satellite cells. Dev. Biol. 191, 270–283.
Birchmeier, C., and Brohmann, H. (2000). Genes that control the
development of migrating muscle precursor cells. Curr. Opin. Cell
Biol. 12, 725–730.
Cossu, G., Kelly, R., Tajbakhsh, S., Di Donna, S., Vivarelli, E., and
Buckingham, M. (1996a). Activation of different myogenic pathways: myf-5 is induced by the neural tube and MyoD by the dorsal
ectoderm in mouse paraxial mesoderm. Development 122, 429–
437.
Bischoff, R. (1975). Regeneration of single skeletal muscle fibers
in vitro. Anat. Rec. 182, 215–235.
Cossu, G., Tajbakhsh, S., and Buckingham, M. (1996b). How is
myogenesis initiated in the embryo? Trends Genet. 12, 218–223.
Blaveri, K., Heslop, L., Yu, D.S., Rosenblatt, J.D., Gross, J.G., Partridge, T.A., and Morgan, J.E. (1999). Patterns of repair of dystro-
Csete, M., Walikonis, J., Slawny, N., Wei, Y., Korsnes, S., Doyle,
J.C., and Wold, B. (2001). Oxygen-mediated regulation of skeletal
Cell
666
muscle satellite cell proliferation and adipogenesis in culture. J.
Cell. Physiol. 189, 189–196.
Dezawa, M., Ishikawa, H., Itokazu, Y., Yoshihara, T., Hoshino, M.,
Takeda, S., Ide, C., and Nabeshima, Y. (2005). Bone marrow stromal
cells generate muscle cells and repair muscle degeneration. Science 309, 314–317.
Di Donna, S., Mamchaoui, K., Cooper, R.N., Seigneurin-Venin, S.,
Tremblay, J., Butler-Browne, G.S., and Mouly, V. (2003). Telomerase
can extend the proliferative capacity of human myoblasts, but does
not lead to their immortalization. Mol. Cancer Res. 1, 643–653.
Downward, J. (2004). PI 3-kinase, Akt and cell survival. Semin. Cell
Dev. Biol. 15, 177–182.
Doyonnas, R., LaBarge, M.A., Sacco, A., Charlton, C., and Blau,
H.M. (2004). Hematopoietic contribution to skeletal muscle regeneration by myelomonocytic precursors. Proc. Natl. Acad. Sci. USA
101, 13507–13512.
Ferrari, G., Cusella-De Angelis, G., Coletta, M., Paolucci, E., Stornaiuolo, A., Cossu, G., and Mavilio, F. (1998). Muscle regeneration
by bone marrow-derived myogenic progenitors. Science 279,
1528–1530.
Ferrari, G., Stornaiuolo, A., and Mavilio, F. (2001). Failure to correct
murine muscular dystrophy. Nature 411, 1014–1015.
Fukada, S., Miyagoe-Suzuki, Y., Tsukihara, H., Yuasa, K., Higuchi,
S., Ono, S., Tsujikawa, K., Takeda, S., and Yamamoto, H. (2002).
Muscle regeneration by reconstitution with bone marrow or fetal
liver cells from green fluorescent protein-gene transgenic mice. J.
Cell Sci. 115, 1285–1293.
Golden, T.R., Hinerfeld, D.A., and Melov, S. (2002). Oxidative stress
and aging: beyond correlation. Aging Cell 1, 117–123.
Goulding, M., Lumsden, A., and Paquette, A.J. (1994). Regulation
of Pax-3 expression in the dermomyotome and its role in muscle
development. Development 120, 957–971.
Gros, J., Manceau, M., Thome, V., and Marcelle, C. (2005). A common somitic origin for embryonic muscle progenitors and satellite
cells. Nature 435, 954–958.
Beilhack, G.F., Shizuru, J.A., and Weissman, I.L. (2003). Biology of
hematopoietic stem cells and progenitors: implications for clinical
application. Annu. Rev. Immunol. 21, 759–806.
Konigsberg, I.R. (1963). Clonal analysis of myogenesis. Science
140, 1273–1284.
LaBarge, M.A., and Blau, H.M. (2002). Biological progression from
adult bone marrow to mononucleate muscle stem cell to multinucleate muscle fiber in response to injury. Cell 111, 589–601.
Lawlor, M.A., and Rotwein, P. (2000). Coordinate control of muscle
cell survival by distinct insulin-like growth factor activated signaling
pathways. J. Cell Biol. 151, 1131–1140.
Lee, S.J. (2004). Regulation of muscle mass by myostatin. Annu.
Rev. Cell Dev. Biol. 20, 61–86.
LeGros Clark, W.E. (1946). An experimental study of regeneration
of mammalian striped muscle. J. Anat. 80, 24–36.
Lescaudron, L., Peltekian, E., Fontaine-Perus, J., Paulin, D., Zampieri, M., Garcia, L., and Parrish, E. (1999). Blood borne macrophages are essential for the triggering of muscle regeneration following muscle transplant. Neuromuscul. Disord. 9, 72–80.
Lipton, B.H., and Schultz, E. (1979). Developmental fate of skeletal
muscle satellite cells. Science 205, 1292–1294.
Luz, M.A., Marques, M.J., and Santo Neto, H. (2002). Impaired regeneration of dystrophin-deficient muscle fibers is caused by exhaustion of myogenic cells. Braz. J. Med. Biol. Res. 35, 691–695.
Maley, M.A., Fan, Y., Beilharz, M.W., and Grounds, M.D. (1994). Intrinsic differences in MyoD and myogenin expression between primary cultures of SJL/J and BALB/C skeletal muscle. Exp. Cell Res.
211, 99–107.
Maroto, M., Reshef, R., Munsterberg, A.E., Koester, S., Goulding,
M., and Lassar, A.B. (1997). Ectopic Pax-3 activates MyoD and
Myf-5 expression in embryonic mesoderm and neural tissue. Cell
89, 139–148.
Mauro, A. (1961). Satellite cells of muscle skeletal fibers. J. Biophys. Biochem. 9, 493–495.
Grounds, M.D. (1998). Age-associated changes in the response of
skeletal muscle cells to exercise and regeneration. Ann. N Y Acad.
Sci. 854, 78–91.
McCroskery, S., Thomas, M., Maxwell, L., Sharma, M., and Kambadur, R. (2003). Myostatin negatively regulates satellite cell activation and self-renewal. J. Cell Biol. 162, 1135–1147.
Gussoni, E., Soneoka, Y., Strickland, C.D., Buzney, E.A., Khan,
M.K., Flint, A.F., Kunkel, L.M., and Mulligan, R.C. (1999). Dystrophin
expression in the mdx mouse restored by stem cell transplantation.
Nature 401, 390–394.
McKinney-Freeman, S.L., Jackson, K.A., Camargo, F.D., Ferrari, G.,
Mavilio, F., and Goodell, M.A. (2002). Muscle-derived hematopoietic
stem cells are hematopoietic in origin. Proc. Natl. Acad. Sci. USA
99, 1341–1346.
Gussoni, E., Bennett, R.R., Muskiewicz, K.R., Meyerrose, T., Nolta,
J.A., Gilgoff, I., Stein, J., Chan, Y.M., Lidov, H.G., Bonnemann, C.G.,
et al. (2002). Long-term persistence of donor nuclei in a Duchenne
muscular dystrophy patient receiving bone marrow transplantation.
J. Clin. Invest. 110, 807–814.
McPherron, A.C., Lawler, A.M., and Lee, S.J. (1997). Regulation of
skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature 387, 83–90.
Hasty, P., Campisi, J., Hoeijmakers, J., van Steeg, H., and Vijg, J.
(2003). Aging and genome maintenance: lessons from the mouse?
Science 299, 1355–1359.
Melone, M.A., Peluso, G., Galderisi, U., Petillo, O., and Cotrufo, R.
(2000). Increased expression of IGF-binding protein-5 in Duchenne
muscular dystrophy (DMD) fibroblasts correlates with the fibroblast-induced downregulation of DMD myoblast growth: An in vitro
analysis. J. Cell. Physiol. 185, 143–153.
Heslop, L., Beauchamp, J.R., Tajbakhsh, S., Buckingham, M.E.,
Partridge, T.A., and Zammit, P.S. (2001). Transplanted primary neonatal myoblasts can give rise to functional satellite cells as identified using the Myf5nlacZl+ mouse. Gene Ther. 8, 778–783.
Miller, K.J., Thaloor, D., Matteson, S., and Pavlath, G.K. (2000). Hepatocyte growth factor affects satellite cell activation and differentiation in regenerating skeletal muscle. Am. J. Physiol. Cell Physiol.
278, C174–C181.
Heszele, M.F., and Price, S.R. (2004). Insulin-like growth factor I:
the yin and yang of muscle atrophy. Endocrinology 145, 4803–4805.
Minasi, M.G., Riminucci, M., De Angelis, L., Borello, U., Berarducci,
B., Innocenzi, A., Caprioli, A., Sirabella, D., Baiocchi, M., De Maria,
R., et al. (2002). The meso-angioblast: a multipotent, self-renewing
cell that originates from the dorsal aorta and differentiates into
most mesodermal tissues. Development 129, 2773–2783.
Husmann, I., Soulet, L., Gautron, J., Martelly, I., and Barritault, D.
(1996). Growth factors in skeletal muscle regeneration. Cytokine
Growth Factor Rev. 7, 249–258.
Jejurikar, S.S., and Kuzon, W.M., Jr. (2003). Satellite cell depletion
in degenerative skeletal muscle. Apoptosis 8, 573–578.
Jiang, Y., Jahagirdar, B.N., Reinhardt, R.L., Schwartz, R.E., Keene,
C.D., Ortiz-Gonzalez, X.R., Reyes, M., Lenvik, T., Lund, T., Blackstad, M., et al. (2002). Pluripotency of mesenchymal stem cells derived from adult marrow. Nature 418, 41–49.
Jockusch, H., and Voigt, S. (2003). Migration of adult myogenic precursor cells as revealed by GFP/nLacZ labelling of mouse transplantation chimeras. J. Cell Sci. 116, 1611–1616.
Kondo, M., Wagers, A.J., Manz, M.G., Prohaska, S.S., Scherer, D.C.,
Montarras, D., Morgan, J., Collins, C., Relaix, F., Zaffran, S., Cumano, A., Partridge, T., and Buckingham, M. (2005). Direct isolation
of muscle satellite cells demonstrates their major role in skeletal
muscle self renewal. Science. Published online September 1, 2005.
10.1126/science.1114758.
Morgan, J.E., and Partridge, T.A. (2003). Muscle satellite cells. Int.
J. Biochem. Cell Biol. 35, 1151–1156.
Moss, F.P., and Leblond, C.P. (1970). Nature of dividing nuclei in
skeletal muscle of growing rats. J. Cell Biol. 44, 459–462.
Olguin, H.C., and Olwin, B.B. (2004). Pax-7 up-regulation inhibits
Review
667
myogenesis and cell cycle progression in satellite cells: a potential
mechanism for self-renewal. Dev. Biol. 275, 375–388.
Pola, R., Ling, L.E., Aprahamian, T.R., Barban, E., Bosch-Marce, M.,
Curry, C., Corbley, M., Kearney, M., Isner, J.M., and Losordo, D.W.
(2003). Postnatal recapitulation of embryonic hedgehog pathway in
response to skeletal muscle ischemia. Circulation 108, 479–485.
Polesskaya, A., Seale, P., and Rudnicki, M.A. (2003). Wnt signaling
induces the myogenic specification of resident CD45+ adult stem
cells during muscle regeneration. Cell 113, 841–852.
Qu-Petersen, Z., Deasy, B., Jankowski, R., Ikezawa, M., Cummins,
J., Pruchnic, R., Mytinger, J., Cao, B., Gates, C., Wernig, A., and
Huard, J. (2002). Identification of a novel population of muscle stem
cells in mice: potential for muscle regeneration. J. Cell Biol. 157,
851–864.
Rantanen, J., Hurme, T., Lukka, R., Heino, J., and Kalimo, H. (1995).
Satellite cell proliferation and the expression of myogenin and desmin in regenerating skeletal muscle: evidence for two different populations of satellite cells. Lab. Invest. 72, 341–347.
Relaix, F., Rocancourt, D., Mansouri, A., and Buckingham, M.
(2005). A Pax3/Pax7-dependent population of skeletal muscle progenitor cells. Nature 435, 948–953.
Renault, V., Thornell, L.E., Butler-Browne, G., and Mouly, V. (2002).
Human skeletal muscle satellite cells: aging, oxidative stress and
the mitotic clock. Exp. Gerontol. 37, 1229–1236.
Robertson, T.A., Maley, M.A., Grounds, M.D., and Papadimitriou,
J.M. (1993). The role of macrophages in skeletal muscle regeneration with particular reference to chemotaxis. Exp. Cell Res. 207,
321–331.
Rouger, K., Brault, M., Daval, N., Leroux, I., Guigand, L., Lesoeur,
J., Fernandez, B., and Cherel, Y. (2004). Muscle satellite cell heterogeneity: in vitro and in vivo evidences for populations that fuse
differently. Cell Tissue Res. 317, 319–326.
Sampaolesi, M., Torrente, Y., Innocenzi, A., Tonlorenzi, R., D’Antona, G., Pellegrino, M.A., Barresi, R., Bresolin, N., De Angelis,
M.G., Campbell, K.P., et al. (2003). Cell therapy of alpha-sarcoglycan null dystrophic mice through intra-arterial delivery of mesoangioblasts. Science 301, 487–492.
Shavlakadze, T., White, J.D., Davies, M., Hoh, J.F., and Grounds,
M.D. (2005). Insulin-like growth factor I slows the rate of denervation induced skeletal muscle atrophy. Neuromuscul. Disord. 15,
139–146.
Schultz, E., Gibson, M.C., and Champion, T. (1978). Satellite cells
are mitotically quiescent in mature mouse muscle: an EM and radioautographic study. J. Exp. Zool. 206, 451–456.
Seale, P., Sabourin, L.A., Girgis-Gabardo, A., Mansouri, A., Gruss,
P., and Rudnicki, M.A. (2000). Pax7 is required for the specification
of myogenic satellite cells. Cell 102, 777–786.
Seale, P., Ishibashi, J., Holterman, C., and Rudnicki, M.A. (2004).
Muscle satellite cell-specific genes identified by genetic profiling
of MyoD-deficient myogenic cell. Dev. Biol. 275, 287–300.
Shefer, G., Wleklinski-Lee, M., and Yablonka-Reuveni, Z. (2004).
Skeletal muscle satellite cells can spontaneously enter an alternative mesenchymal pathway. J. Cell Sci. 117, 5393–5404.
Sherwood, R.I., Christensen, J.L., Conboy, I.M., Conboy, M.J.,
Rando, T.A., Weissman, I.L., and Wagers, A.J. (2004a). Isolation of
adult mouse myogenic progenitors; functional heterogeneity of
cells within and engrafting skeletal muscle. Cell 119, 543–554.
Sherwood, R.I., Christensen, J.L., Weissman, I.L., and Wagers, A.J.
(2004b). Determinants of skeletal muscle contribution from circulating cells, bone marrow cells, and hematopoietic stem cells. Stem
Cells 22, 1292–1304.
Sloper, J.C., and Partridge, T.A. (1980). Skeletal muscle: regeneration and transplantation studies. Br. Med. Bull. 36, 153–158.
Snow, M.H. (1978). An autoradiographic study of satellite cell differentiation into regenerating myotubes following transplantation of
muscles in young rats. Cell Tissue Res. 186, 535–540.
Stauber, W.T., Fritz, V.K., Vogelbach, D.W., and Dahlmann, B. (1988).
Characterization of muscles injured by forced lengthening. I. Cellular infiltrates. Med. Sci. Sports Exerc. 20, 345–353.
Thomas, M., Langley, B., Berry, C., Sharma, M., Kirk, S., Bass, J.,
and Kambadur, R. (2000). Myostatin, a negative regulator of muscle
growth, functions by inhibiting myoblast proliferation. J. Biol.
Chem. 275, 40235–40243.
Tidball, J.G. (2005). Inflammatory processes in muscle injury and
repair. Am. J. Physiol. Regul. Integr. Comp. Physiol. 288, R345–
R353.
Vignery, A. (2000). Osteoclasts and giant cells: macrophage-macrophage fusion mechanism. Int. J. Exp. Pathol. 81, 291–304.
Volkmann, R. (1893). Uber die regeneration des quergestrieften
muskelgewebes beim menschen und saugetier. Bieitr. Path. Anat.
12, 233–332.
Walton, J.N., and Adams, R.D. (1956). The response of the normal,
the denervated and the dystrophic muscle-cell to injury. J. Pathol.
Bacterol. 72, 273–298.
Washabaugh, C.H., Ontell, M.P., and Ontell, M. (2004). Nonmuscle
stem cells fail to significantly contribute to regeneration of normal
muscle. Gene Ther. 11, 1724–1728.
Weber, C.O. (1863). Ueber die regeneration quergestreifter muskelfasern. Zentrabl. Med. Wis. 1, 529–531.
Yablonka-Reuveni, Z., Quinn, L.S., and Nameroff, M. (1987). Isolation and clonal analysis of satellite cells from chicken pectoralis
muscle. Dev. Biol. 119, 252–259.
Yaffe, D. (1969). Cellular aspects of muscle differentiation in vitro.
Curr. Top. Dev. Biol. 4, 37–77.
Zacks, S.I., and Sheff, M.F. (1982). Age-related impeded regeneration of mouse minced anterior tibial muscle. Muscle Nerve 5, 152–
161.
Zammit, P.S., Golding, J.P., Nagata, Y., Hudon, V., Partridge, T.A.,
and Beauchamp, J.R. (2004). Muscle satellite cells adopt divergent
fates: a mechanism for self-renewal? J. Cell Biol. 166, 347–357.
Zimmers, T.A., Davies, M.V., Koniaris, L.G., Haynes, P., Esquela,
A.F., Tomkinson, K.N., McPherron, A.C., Wolfman, N.M., and Lee,
S.J. (2002). Induction of cachexia in mice by systemically administered myostatin. Science 296, 1486–1488.