letters
EIF2AK4 mutations cause pulmonary veno-occlusive
disease, a recessive form of pulmonary hypertension
npg
© 2014 Nature America, Inc. All rights reserved.
Mélanie Eyries1–3, David Montani4–6, Barbara Girerd4–6, Claire Perret3,7, Anne Leroy2, Christine Lonjou8,
Nadjim Chelghoum8, Florence Coulet2,3, Damien Bonnet9,10, Peter Dorfmüller6,11, Elie Fadel6,12,
Olivier Sitbon4–6, Gérald Simonneau4–6, David-Alexandre Tregouët3,7, Marc Humbert4–6 & Florent Soubrier1–3
Pulmonary veno-occlusive disease (PVOD) is a rare and
devastating cause of pulmonary hypertension that is
characterized histologically by widespread fibrous intimal
proliferation of septal veins and preseptal venules and is
frequently associated with pulmonary capillary dilatation
and proliferation1,2. PVOD is categorized into a separate
pulmonary arterial hypertension–related group in the current
classification of pulmonary hypertension3. PVOD presents
either sporadically or as familial cases with a seemingly
recessive mode of transmission4. Using whole-exome
sequencing, we detected recessive mutations in EIF2AK4
(also called GCN2) that cosegregated with PVOD in all 13
families studied. We also found biallelic EIF2AK4 mutations in
5 of 20 histologically confirmed sporadic cases of PVOD. All
mutations, either in a homozygous or compound-heterozygous
state, disrupted the function of the gene. These findings
point to EIF2AK4 as the major gene that is linked to PVOD
development and contribute toward an understanding of the
complex genetic architecture of pulmonary hypertension.
PVOD was first recognized as a specific entity of pulmonary hypertension in the 1960s5. PVOD is characterized by a low diffusing capacity
for carbon monoxide, occult alveolar hemorrhage and high-resolution
computed tomography of the chest that shows patchy centrilobular
ground-glass opacities, septal lines and lymph node enlargement6. The
true incidence of PVOD remains unknown because many cases are
probably misclassified as idiopathic pulmonary arterial ­hypertension
(PAH). The proportion of idiopathic cases of PAH that in reality fulfill
the criteria for PVOD is likely around 10%1.
Mutations in BMPR2 are found in approximately 75% of familial
cases of PAH and in almost 20% of apparently sporadic cases of PAH.
Mutations in ACVRL1, which can complicate hereditary hemorrhagic
telangiectasia, have also been described in PAH7,8. PAH that is due
to BMPR2 mutations segregates as an autosomal-dominant trait with
incomplete penetrance9.
Familial cases of PVOD have been described in three different
studies, and the disease typically occurs in the young siblings of
one generation4,10,11. In the French referral center, we identified 13
PVOD families. In eight families (PVOD1, PVOD2, PVOD3, PVOD5,
PVOD6, PVOD7, PVOD8 and PVOD12), we confirmed the PVOD
diagnosis histologically after lung transplantation or lung biopsy in at
least one family member (Fig. 1 and Supplementary Tables 1 and 2).
In the five remaining PVOD families (PVOD4, PVOD9, PVOD10,
PVOD11 and PVOD13), we considered the diagnosis to be highly
likely on the basis of clinical and paraclinical data (Supplementary
Tables 1 and 2). All PVOD families were characterized by the
presence of at least two affected siblings and unaffected parents,
suggesting that the disease segregates as a recessive trait.
To identify the genetic basis of familial forms of PVOD, we
first adopted a genetic linkage mapping strategy in three families
(PVOD1, PVOD2 and PVOD3). We observed suggestive linkage signals at six regions, with a maximum log10 odds (LOD)-score peak
above 1.5 at each locus, but we detected no genome wide–significant linkage (LOD > 3) (Supplementary Fig. 1). We then performed
whole-exome sequencing on subjects from five families (PVOD1,
PVOD2, PVOD3, PVOD4 and PVOD5). We selected homozygous or
compound-­heterozygous variants that were rare (minor allele frequency (MAF) <0.1%) or unknown in either the National Heart,
Lung, and Blood Institute (NHLBI) Exome Sequencing Project Exome
Variant Server (EVS) or the 1000 Genomes Project and that were
shared by both affected subjects and were present in a heterozygous
state in the unaffected parents. We found that variants of a single gene,
EIF2AK4, met these criteria in two families, PVOD1 and PVOD4. In
PVOD1, the two affected siblings carried heterozygous frameshift and
1Unité
Mixte de Recherche en Santé (UMR_S 956), Université Pierre and Marie Curie Université Paris 06 (UPMC) and Institut National de la Santé et de la Recherche
Médicale (INSERM), Paris, France. 2Genetics Department, Hôpital Pitié-Salpêtrière, Assistance Publique–Hôpitaux de Paris (AP-HP), Paris, France. 3Institute for
Cardiometabolism and Nutrition (ICAN), Paris, France. 4Université Paris-Sud, Faculté de Médecine, Le Kremlin Bicêtre, France. 5Département Hospitalo-Universitaire
(DHU) Thorax Innovation (TORINO), Service de Pneumologie, Hôpital Bicêtre, AP-HP, Le Kremlin Bicêtre, France. 6INSERM UMR_S 999, Laboratoire d’Excellence
en Recherche sur le Médicament et l’Innovation Thérapeutique (LERMIT), Centre Chirurgical Marie Lannelongue, Le Plessis Robinson, France. 7UMR_S 937,
UPMC, INSERM, Paris, France. 8Post-Genomic Platform (P3S), UPMC, INSERM, Paris, France. 9Cardiac Surgery Department, Hôpital Necker-Enfants Malades,
AP-HP, Paris, France. 10UMR_S 765, INSERM and Université Paris Descartes, Paris, France. 11Department of Pathology, Centre Chirurgical Marie Lannelongue,
Le Plessis-Robinson, France. 12Thoracic Surgery Department, Centre Chirurgical Marie Lannelongue, Le Plessis-Robinson, France. Correspondence should be
addressed to F.S. (florent.soubrier@upmc.fr).
Received 6 August; accepted 6 November; published online 1 December 2013; doi:10.1038/ng.2844
Nature Genetics VOLUME 46 | NUMBER 1 | JANUARY 2014
65
© 2014 Nature America, Inc. All rights reserved.
letters
a
b
c
d
e
f
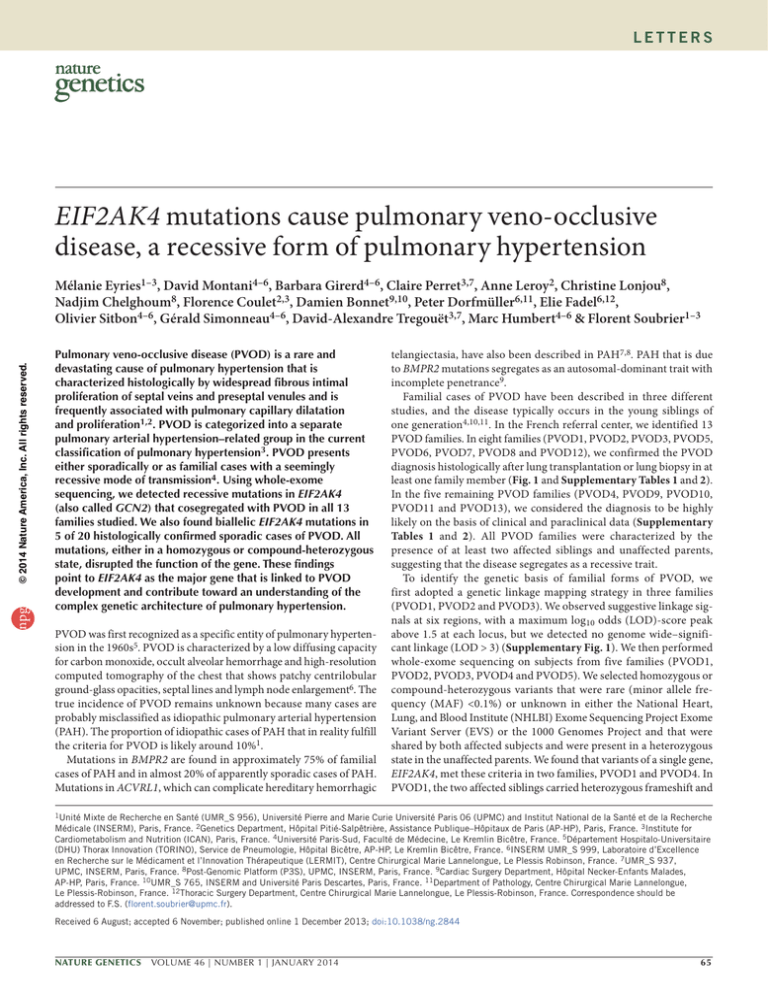
Figure 1 Pathology of heritable PVOD. (a) Septal vein displaying intimal fibrosis and overall thickening of the vessel wall. Scale bar, 500 µm. (b) Small vein
with occlusive intimal fibrosis. Scale bar, 100 µm. (c) Intimal remodeling of a pulmonary artery; the adjacent bronchiole is also visible (bottom). Scale bar,
100 µm. (d) Numerous patch-like foci of capillary hemangiomatosis; small veins with intimal remodeling are visible (left and bottom). Scale bar, 1,000 µm.
(e) PCH-like remodeling with a central muscularized arteriole or small artery. Scale bar, 100 µm. (f) Small artery displaying important concentric fibrosis of the
intima; the slender media is visible, which is delimited by the internal and external lamina elastica (highlighted in black). Scale bar, 100 µm. Hematoxylin and
eosin stains are shown in a–e, and orcein stain is shown in f.
­splicing mutations, and in PVOD4, the two affected siblings harbored
heterozygous nonsense and frameshift mutations. The genotypes
in PVOD2 and PVOD3 were not initially consistent with recessive
transmission in the affected subjects, but further Sanger sequencing of the corresponding EIF2AK4 coding sequences in these families showed that all affected subjects carried deleterious mutations
Table 1 Age at diagnosis of PVOD, gender and genotypes of subjects with EIF2AK4 mutations
Family number
npg
PVOD1
PVOD2
PVOD3
PVOD4
PVOD5
PVOD6
PVOD7
PVOD8
PVOD9
PVOD10
PVOD11
PVOD12
PVOD13
aShown
66
Individual
Gender
Age at diagnosis (years)
II-1
II-2
II-3
II-2
II-3
II-2
II-3
II-1
II-2
IV-2
IV-3
III-2
II-1
III-3
II-5
II-1
II-1
II-1
IV-3
112160
091769
05220
05498
06734
F
F
F
M
F
F
M
M
F
F
F
M
M
M
M
M
F
M
M
F
F
M
M
F
31
50
49
23
16
23
23
20
20
20
27
26
32
26
36
19
37
44
11
32
15
20
20
28
Mutationa
c.354_355del; c.1554-4C>A (p.Cys118Trpfs*7; p.Cys519Aspfs*17)
c.2319+1G>A; c.2319+1G>A (p.[?]; p.[?])
c.745C>T; c.2136_2139dup (p.Arg249*; p.Ser714Hisfs*21)
c.1392del; c.3802C>T (p.Arg465Valfs*38; p.Gln1268*)
c.567dup; c.567dup (p.Leu190Glufs*8; p.Leu190Glufs*8)
c.3159G>A; c.3159G>A (p.Lys975_Lys1053del; p.Lys975_Lys1053del)
c.3406C>T; c.3406C>T (p.Arg1136*; p.Arg1136*)
c.1754G>A; c.1754G>A (p.Arg585Gln; p.Arg585Gln)
c.4065+1G>C; c.4065+1G>C (p.[?]; p.[?])
c.1387C>T; p.1387C>T (p.Arg463*; p.Arg463*)
c.3448C>T; c.4728+1_4728+13delinsTTCT (p.Arg1150*; p.[?])
c.1387C>T; c.3244C>T (p.Arg463*; p.Gln1082*)
c.1928T>G; c.1928T>G (p.Leu643Arg; p.Leu643Arg)
c.560_564del; c.560_564del (p.Lys187Argfs*9; p.Lys187Argfs*9)
c.3159G>A; c.3159G>A (p.Lys975_Lys1053del; pLys975_Lys1053del)
c.2857C>T; c.3576+1G>T (p.Gln953*; p.[?])
c.4205dup; c.4205dup (p.Ser1403Lysfs*45; p.Ser1403Lysfs*45)
c. 2458C>T; c.2458C>T (p.Arg820*; p.Arg820*)
as the nucleotide changes with the respective protein effects in parentheses.
VOLUME 46 | NUMBER 1 | JANUARY 2014 Nature Genetics
letters
p.C118Wfs*7
p.L643R
p.R465Vfs*38
p.K190Efs*8
p.C519Dfs*17
p.R1150*
p.K975_K1053del
p.K975_K1053del
p.c.2319+1G>A
p.K187Rfs*9
p.R249*
NH2
1 25
p.R585Q
p.S714Hfs*21 p.R820*
Pseudokinase
RWD
137
p.R463*
p.R463*
296
Q958*
c.4065+1G>C
c.4728+1_4728+13delinsTTCT
p.Q1082* c.3576+1G>T
p.R1136*
p.Q1268*
p.S1403Kfs*45
His-tRNA synthase_like
Protein kinase
539 590
1001
1022
COOH
1493
1649 aa
npg
© 2014 Nature America, Inc. All rights reserved.
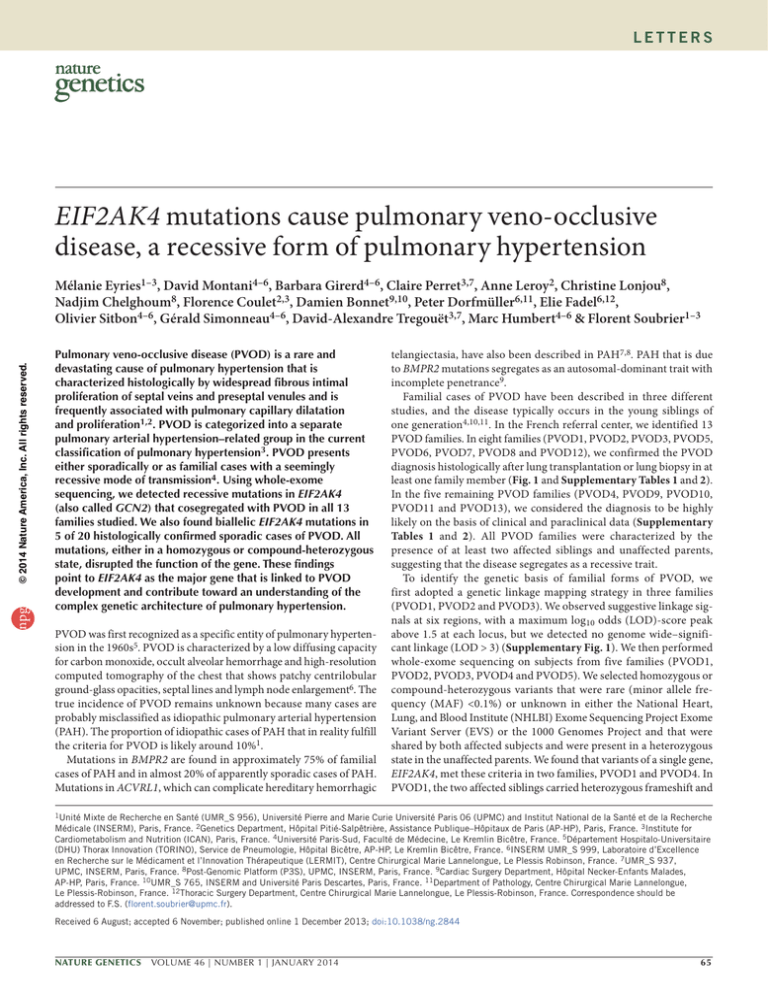
Figure 2 Location of the EIF2AK4 mutations detected in patients with PVOD. The locations and consequences of the recessive mutations in subjects
with familial PVOD (black) or sporadic PVOD (blue) are shown on a schematic of the EIF2AK4 protein 25. Mutations found in a homozygous state are
shown in bold; the other mutations were found in a heterozygous state. For nonsynonymous and frameshift mutations, the protein effects are shown,
and for splicing variants, the nucleotide changes are indicated. In the figure, amino acids are indicated by their one-letter abbreviations. aa, amino acid.
on both alleles and that each unaffected parent was heterozygous
for one of the two mutations (Table 1 and Supplementary Fig. 2a).
In the consanguineous family (PVOD5), Sanger sequencing in both
affected siblings identified a deleterious homozygous mutation
located in exon 5 of EIF2AK4, which had not been captured by wholeexome sequencing. Of note, EIF2AK4 maps to the LOD-score peak
on chromosome 15 that had been detected by nonparametric linkage
(Supplementary Fig. 1).
We screened the index cases of eight additional PVOD families with
typical recessive transmission (PVOD6, PVOD7, PVOD8, PVOD9,
PVOD10, PVOD11, PVOD12 and PVOD13) and found biallelic
EIF2AK4 mutations in all of these families (Table 1 and Supplementary
Fig. 2b). In family PVOD13, we found a homozygous missense mutation encoding p.Leu643Arg, which is considered deleterious by
in silico analysis (Online Methods), in the 11-year-old index case, whose
brother and sister both died of pulmonary hypertension at the ages of
15 and 10 years, respectively. Histological aspects of the diagnostic lung
biopsy of the index case, a borderline value of mean pulmonary arterial
pressure, high-resolution computed tomography of the chest, substantial oxygen desaturation at exercise and familial context together argue
in favor of an incipient form of PVOD in this homozygous mutation
carrier (Supplementary Table 2). The rather high number of PVOD
families collected in our referral center could be explained by both a
long-term and careful search for the disease among patients studied
and referral to the center of patients originating from North Africa,
where recessive disease occurrence is favored by endogamy.
We also investigated the entire EIF2AK4 coding sequence in 20
apparently sporadic, histologically proven cases of PVOD, in which
a
Control
b
pulmonary tissue either after lung transplantation or lung biopsy or
at post-mortem was examined (Supplementary Table 3). We found
biallelic EIF2AK4 mutations in 5/20 cases (25%), suggesting that a
quarter of these sporadic cases could correspond to heritable PVOD
(Table 1). We also investigated an additional series of 26 patients with
pulmonary hypertension who had clinical and radiological signs that
were strongly suggestive of PVOD but in whom PVOD was not histo­
logically proven. No EIF2AK4 mutations were found in this series of
patients. We also analyzed nine index cases from PAH families without BMPR2 mutations, but we detected no EIF2AK4 mutations.
Collectively we identified a total of 22 distinct EIF2AK4 mutations
in this study. Most of these mutations are stop codons (n = 8) or
insertions/deletions (indels) (n = 6) that disrupt the function of the
gene. We identified two distinct missense mutations that resulted in
p.Arg585Gln in PVOD8 and p.Leu653Arg in PVOD13. Both of these
mutations are located in the kinase domain of EIF2AK4 (Fig. 2), alter
conserved residues and are predicted to be deleterious by in silico
tools (Online Methods). We also found six splice mutations, four
of which affect a consensus donor site and two of which are predicted to affect splicing by in silico analysis. In both cases, RT-PCR
experiments using RNA extracted from circulating blood cells from
the mutation carriers confirmed that mRNA splicing was defective
(Supplementary Fig. 3). Notably, we found two mutations (encoding p.Lys975_Lys1053del and p.Arg463*) in two patients from two
apparently unrelated families. In particular, we found the p.Lys975_
Lys1053del alteration in two native Algerian patients. To estimate the
frequency of this variant in the Algerian population, we performed
further genotyping in 278 Algerian control subjects. With a sample
Nonmutated PVOD
c
EIF2AK4-mutated PVOD
(p.L190Efs*8)
Figure 3 Immunohistochemical staining with an EIF2AK4 antibody in lungs from a control patient, a patient with PVOD not carrying mutations and a
patient with PVOD who is homozygous for a EIF2AK4 mutation encoding p.Leu190Glufs*8. (a) Control lung. The arrows indicate the slender venule
showing staining of the vessel wall (smooth muscle cells) and negative endothelial cells. Diffuse interstitial staining is indicated by arrowheads;
macrophages and some mononuclear cells are stained (triangles). (b) Nonmutated PVOD lung. Smooth muscle cells within the vessel wall of the
remodeled microvessel (arteriole or venule) are highlighted by the antibody (arrow). Again, diffuse interstitial staining is present (arrowhead).
(c) EIF2AK4-mutated PVOD lung. The remodeled microvessel (arteriole or venule; center) and the interstitium are not labeled. All scale bars, 100 µm.
Nature Genetics VOLUME 46 | NUMBER 1 | JANUARY 2014
67
npg
© 2014 Nature America, Inc. All rights reserved.
letters
of this size, we had 94% power to detect any variant with MAF as
low as 0.005. However, we did not detect any carriers in this group,
confirming that the p.Lys975_Lys1053del alteration is rare, even in
the Algerian population.
Using immunohistochemistry, the EIF2AK4 protein is detected
in smooth muscle cells of the vessel wall and interstitial tissue and
in macrophages in control lungs. We observed a similar pattern of
expression in a lung from a patient affected with PVOD that did
not have EIF2AK4 mutations, whereas we detected no expression of
EIF2AK4 in the lung from patient IV-3 of family PVOD5, who carries
the homozygous mutation encoding p.Lys190Glufs*8 (Fig. 3).
The arguments that support EIF2AK4 as a major causal gene for
PVOD are as follows: (i) the complete consistency between genotype
and phenotype of the affected patients, together with the segregation
of single-allele mutations from the parents to their progeny; (ii) the
unambiguous loss of gene function caused by the mutations identified; (iii) the presence of biallelic mutations in the same gene in all
families tested that share the same specific PVOD phenotype; (iv) the
presence of homozygous EIF2AK4 mutations in affected siblings of
consanguineous families; and (v) the low genetic burden of EIF2AK4,
as inspection of EVS showed only six loss-of-function mutations
among nearly 12,000 sequenced alleles.
We describe a genetic cause for PVOD, which is a particular form
of pulmonary hypertension whose recessive mode of transmission
differs from that of dominant-heritable forms of BMPR2-linked
PAH that have lower penetrance rates (14% and 42% in males and
females, respectively12). The penetrance of the EIF2AK4 mutations
is difficult to evaluate from our data because we genotyped only the
affected subjects from sibships, but the single unaffected sibling
tested from one family carries the mutation in the heterozygous state
(subject II-1 from PVOD2; Supplementary Fig. 2a). In the nonfamilial
but histologically proven cases of PVOD, we found a mutation rate of
25%, which indicates that these heritable-recessive forms are frequently
unrecognized, as is the case for sporadic PAH caused by BMPR2 mutations. The development of a genetic test will allow these heritable forms
to be recognized and genetic counseling to be performed.
The age of onset of PVOD in mutation carriers varies, with early
death seen in some families (at 10 years of age or earlier) and onset
delayed until the age of 50 years in others. The early occurrence suggests that additional genetic or environmental factors may accelerate
the disease process, as there is no detectable genotype-phenotype relationship in the families studied that could explain the variable age of
onset. Similar to previous observations in patients with PAH who carry
mutations in BMPR2 or ACVRL1 (ref. 8), we noted that patients with
PVOD carrying EIF2AK4 mutations (n = 24) were significantly younger
at the time of PVOD diagnosis compared to patients with PVOD who
do not carry such mutations (n = 15) (26.7 ± 10.4 years (mean ± s.d.)
compared to 44.3 ± 11.8 years, respectively; P < 0.0001).
Notably, patients II-1 and II-2 from family PVOD1 were initially
diagnosed as having pulmonary capillary hemangiomatosis (PCH)
on the basis of extensive precapillary proliferation with moderated
venous involvement that was seen in explanted lung samples from the
two siblings. In the current classification of pulmonary hypertension,
PCH is grouped with PVOD because PCH shares many similarities
with PVOD13,14. Researchers from a previous study demonstrated that
capillary proliferation could be identified in 73% of cases diagnosed
as having PVOD and that 80% of cases of PCH presented venous and
arterial changes that are typical of PVOD15. Our results reinforce the
hypothesis that PVOD and PCH may be two different histological
patterns of the same disease with a common genetic risk factor.
68
EIF2AK4 encodes a serine-threonine kinase present in all eukaryotes that can induce changes in gene expression in response to amino
acid deprivation. EIF2AK4 belongs to a family of four kinases
that phosphorylate the α-subunit of the eukaryotic initiation
factor 2 (eIF2α). eIF2 functions by directing the binding of initiator methionyl-tRNA to 40S ribosomal subunits in the early stages of
protein synthesis from a small number of specific mRNAs. EIF2AK4mediated phosphorylation of eIF2α inactivates the factor and leads
to preferential synthesis of stress proteins16.
The pathophysiological link between biallelic EIF2AK4 loss-offunction mutations and vascular cell proliferation and remodeling
of lung vessels remains elusive. Eif2ak4−/− mice on a C57BL/6J
background are less viable than wild-type mice, as a subset of the
mice lacking Eif2ak4 die shortly after birth; however, the lungs of
these mice have not yet been studied 17. EIF2AK4 has been shown
to prevent oxidative damage induced by an amino acid–imbalanced
diet, as Eif2ak4−/− mice show an increase in protein carbonylation,
which is a marker of oxidative stress that is important for pulmonary hypertension development18,19. The involvement of EIF2AK4
in PVOD could be related either directly to its amino acid starvation sensor function and subsequent translational changes secondary to its activation or to EIF2AK4 kinase activity, which might
have substrates other than eIF2α. Two series of experimental data
potentially connect EIF2AK4 to the bone morphogenetic protein
(BMP) pathway, which has been implicated in PAH pathogenesis
through mutations in BMPR2 and ACVRL1 (refs. 7,20). Notably, as
a result of an interaction screen performed with the ­luminescencebased mammalian interactome mapping technique, EIF2AK4
was found to interact with SMAD4 and SMAD1 (ref. 21) and also
with ALK-1, endoglin (ENG) and transforming growth factor-β
receptor-2 (TGFBR2) (M. Letarte, personal communication). These
proteins are receptors, co-receptors or signaling intermediates of the
TGF-β–BMP superfamily. Second, TRIB3, the Tribbles homolog 3
gene, is transcriptionally regulated by ATF4, a stress protein whose
translation is activated by EIF2AK4, as has been demonstrated in the
mouse liver22. Downregulation of TRIB3 has been shown to inhibit
BMP-mediated cellular responses23. One can speculate that EIF2AK4
inactivation would lead to TRIB3 downregulation and decreased
BMP signaling, this latter condition leading to PAH in the case of
BMPR2 haploinsufficiency24.
The identification of EIF2AK4 mutations as the major cause of
heritable PVOD confirms the hereditary origin of this particular type
of pulmonary hypertension and allows identification of heritable but
apparently sporadic cases. Mutation identification will allow genetic
counseling to be offered to families affected by this extremely severe
disease. These results also open new research avenues into the role
of EIF2AK4 in pulmonary vascular remodeling and pave the way for
innovative therapeutic strategies.
URLs. The NHLBI Exome Sequencing Project EVS, http://
evs.gs.washington.edu/EVS/; 1000 Genome Projects, http://
www.1000genomes.org/; the Consensus Assessment of Sequence and
Variation (CASAVA) software, http://www.illumina.com/software/
genome_analyzer_software.ilmn; the Human Genome Variation
Society, www.hgvs.org/mutnomen; SIFT, http://sift.jcvi.org/; PolyPhen-2,
http://genetics.bwh.harvard.edu/pph2/; Align-GVGD, http://agvgd.
iarc.fr; Mutation Taster, http://www.mutationtaster.org/; MaxEntScan,
http://genes.mit.edu/burgelab/; NNsplice, http://www.fruitfly.org/seq_
tools/splice.html; GeneSplicer, http://ccb.jhu.edu/software/genesplicer/;
Human Splicing Finder, http://www.umd.be/HSF/.
VOLUME 46 | NUMBER 1 | JANUARY 2014 Nature Genetics
letters
Methods
Methods and any associated references are available in the online
version of the paper.
Note: Any Supplementary Information and Source Data files are available in the
online version of the paper.
AUTHOR CONTRIBUTIONS
F.S. initiated and supervised the study. M.E., D.-A.T., M.H. and F.S. conceived
and designed the experiments. D.M., B.G., D.B., O.S., G.S., E.F. and M.H.
performed clinical phenotyping. D.M., B.G. and M.H. analyzed clinical data of
collected patients. C.P. performed the whole-exome sequencing experiments.
N.C. performed bioinformatic analyses. D.-A.T. supervised bioinformatic and
biostatistical data. M.E. and F.S. analyzed whole-exome sequencing data.
C.L. performed linkage analysis. A.L. performed Sanger sequencing. M.E. and
F.C. analyzed Sanger sequencing data. E.F. collected lung sample specimens.
P.D. performed tissue imaging. M.E., D.M., B.G., D.-A.T., M.H. and F.S. wrote the
manuscript. All authors reviewed the manuscript.
COMPETING FINANCIAL INTERESTS
The authors declare no competing financial interests.
Reprints and permissions information is available online at http://www.nature.com/
reprints/index.html.
1. Mandel, J., Mark, E.J. & Hales, C.A. Pulmonary veno-occlusive disease. Am. J.
Respir. Crit. Care Med. 162, 1964–1973 (2000).
2. Montani, D. et al. Pulmonary veno-occlusive disease. Eur. Respir. J. 33, 189–200
(2009).
3. Simonneau, G. et al. Updated clinical classification of pulmonary hypertension.
J. Am. Coll. Cardiol. 54, S43–S54 (2009).
4. Davies, P. & Reid, L. Pulmonary veno-occlusive disease in siblings: case reports
and morphometric study. Hum. Pathol. 13, 911–915 (1982).
5. Heath, D., Segel, N. & Bishop, J. Pulmonary veno-occlusive disease. Circulation
34, 242–248 (1966).
npg
© 2014 Nature America, Inc. All rights reserved.
Acknowledgments
We thank F. Pires, A. Dion-Minière, S. Bakas, G. Legrand and N. Raymond
for technical assistance. We thank W. Carpentier for supervising SNP array
experiments. We thank R. Peat for kindly editing the manuscript. D.M. and
P.D. are supported by a grant from the Association Hypertension Artérielle
Pulmonaire (HTAP) France. This work was supported by Programme Hospitalier
de Recherche Clinique (PHRC) AOM07-041, INSERM and UPMC. The tissue
bank was supported in part by the Legs Poix, Chancellerie des Universités de Paris.
Bioinformatics analyses benefit from the C2BIG computing centre funded by the
Région Ile de France and UPMC.
6. Montani, D. et al. Pulmonary veno-occlusive disease: clinical, functional, radiologic,
and hemodynamic characteristics and outcome of 24 cases confirmed by histology.
Medicine 87, 220–233 (2008).
7. Trembath, R.C. et al. Clinical and molecular genetic features of pulmonary
hypertension in patients with hereditary hemorrhagic telangiectasia. N. Engl. J.
Med. 345, 325–334 (2001).
8. Girerd, B. et al. Clinical outcomes of pulmonary arterial hypertension in patients
carrying an ACVRL1 (ALK1) mutation. Am. J. Respir. Crit. Care Med. 181, 851–861
(2010).
9. Machado, R.D. et al. Genetics and genomics of pulmonary arterial hypertension.
J. Am. Coll. Cardiol. 54, S32–S42 (2009).
10.Rosenthal, A., Vawter, G. & Wagenvoort, C.A. Intrapulmonary veno-occlusive disease.
Am. J. Cardiol. 31, 78–83 (1973).
11.Voordes, C.G., Kuipers, J.R. & Elema, J.D. Familial pulmonary veno-occlusive
disease: a case report. Thorax 32, 763–766 (1977).
12.Larkin, E.K. et al. Longitudinal analysis casts doubt on the presence of genetic
anticipation in heritable pulmonary arterial hypertension. Am. J. Respir. Crit. Care
Med. 186, 892–896 (2012).
13.Humbert, M. et al. Pulmonary edema complicating continuous intravenous
prostacyclin in pulmonary capillary hemangiomatosis. Am. J. Respir. Crit. Care Med.
157, 1681–1685 (1998).
14.Langleben, D. et al. Familial pulmonary capillary hemangiomatosis resulting in
primary pulmonary hypertension. Ann. Intern. Med. 109, 106–109 (1988).
15.Lantuéjoul, S., Sheppard, M.N., Corrin, B., Burke, M.M. & Nicholson, A.G.
Pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis:
a clinicopathologic study of 35 cases. Am. J. Surg. Pathol. 30, 850–857 (2006).
16.Donnelly, N., Gorman, A.M., Gupta, S. & Samali, A. The eIF2α kinases: their
structures and functions. Cell. Mol. Life Sci. 70, 3493–3511 (2013).
17.Anthony, T.G. et al. Preservation of liver protein synthesis during dietary leucine
deprivation occurs at the expense of skeletal muscle mass in mice deleted for eIF2
kinase GCN2. J. Biol. Chem. 279, 36553–36561 (2004).
18.Chaveroux, C. et al. Identification of GCN2 as new redox regulator for oxidative stress
prevention in vivo. Biochem. Biophys. Res. Commun. 415, 120–124 (2011).
19.Fessel, J.P. et al. Hyperoxia synergizes with mutant BMPR2 to cause metabolic
stress, oxidant injury, and pulmonary hypertension. Am. J. Respir. Cell Mol. Biol.
49, 778–787 (2013).
20.Machado, R.D. et al. BMPR2 haploinsufficiency as the inherited molecular
mechanism for primary pulmonary hypertension. Am. J. Hum. Genet. 68, 92–102
(2001).
21.Barrios-Rodiles, M. et al. High-throughput mapping of a dynamic signaling network
in mammalian cells. Science 307, 1621–1625 (2005).
22.Carraro, V. et al. Amino acid availability controls TRB3 transcription in liver through
the GCN2/eIF2α/ATF4 pathway. PLoS ONE 5, e15716 (2010).
23.Chan, M.C. et al. A novel regulatory mechanism of the bone morphogenetic protein
(BMP) signaling pathway involving the carboxyl-terminal tail domain of BMP type
II receptor. Mol. Cell. Biol. 27, 5776–5789 (2007).
24.Davies, R.J. et al. BMP type II receptor deficiency confers resistance to growth
inhibition by TGF-β in pulmonary artery smooth muscle cells: role of proinflammatory
cytokines. Am. J. Physiol. Lung Cell. Mol. Physiol. 302, L604–L615 (2012).
25.Sattlegger, E. & Hinnebusch, A.G. Separate domains in GCN1 for binding protein
kinase GCN2 and ribosomes are required for GCN2 activation in amino acid–starved
cells. EMBO J. 19, 6622–6633 (2000).
Nature Genetics VOLUME 46 | NUMBER 1 | JANUARY 2014
69
npg
© 2014 Nature America, Inc. All rights reserved.
ONLINE METHODS
Subjects. Patients were studied at the French referral center for severe
­pulmonary hypertension (Université Paris-Sud, AP-HP, Le Kremlin-Bicêtre),
and patient IV-3 from family PVOD 13 was studied at the Cardiopediatrics
Department of the Necker-Enfants Malades hospital (AP-HP). All clinical
characteristics at PVOD diagnosis and follow-up were stored in the Registry
of the French PAH Network. This registry was set up in agreement with
French bioethics laws (French Commission Nationale de l’Informatique et
des Libertés), and patients gave their consent to be included26. All patients and
relatives gave their informed consent for genetic research, which was approved
by the Comité de Protection des Personnes Ile de France-VI, decision ID
RCB2007-AO1347-46. The diagnosis of precapillary pulmonary hypertension
was defined by hemodynamic measurement during right-heart catheterization
of all patients included in the study. Precapillary pulmonary hypertension was
defined as a mean pulmonary arterial pressure ≥25 mm Hg (where normal
values are 14 ± 3 mm Hg (mean ± s.d.)) associated with normal pulmonary
capillary wedge pressure (≤15 mm Hg). In an early pediatric familial case
(PVOD13), an abnormal borderline value was observed (mean pulmonary
artery pressure of 23 mm Hg). Hemodynamic evaluation by right-heart
catheterization was performed at baseline in all subjects according to
previously described protocols27.
The diagnosis of PVOD was considered as confirmed when histological
proof of veno-occlusive disease was available. Histological proof of veno­occlusive disease was based on hematoxylin-eosin-safran staining of lung
biopsies, post-mortem lung samples or lungs obtained after lung transplantation. The pathologic hallmark of PVOD is defined as an extensive and
diffuse obstruction of pulmonary veins and venules by intimal fibrosis, cellular
proliferation and muscularization.
The diagnosis of PVOD was considered as highly probable if patients
fulfilled the following characteristics: precapillary pulmonary hypertension, presence of two or more radiological abnormalities on high-resolution
computed tomography of the chest (including lymph node enlargement,
­centrilobular ground-glass opacities and septal lines), low diffusing capacity
for carbon monoxide or occult alveolar hemorrhage. The diagnosis was even
more strongly supported when patients with signs of highly probable PVOD
developed pulmonary edema after the initiation of specific PAH therapy.
Genetic analysis. All patients were screened for BMPR2 mutations, and those
with a family history of precapillary pulmonary hypertension were further
screened for ACVRL1 mutations. Screening for point mutations and large
rearrangements was performed as previously reported28,29.
Linkage analysis. Three pedigrees (PVOD1, PVOD2 and PVOD3) were initially used for linkage analysis. In each of these pedigrees, two affected ­siblings
and their unaffected parents were genotyped for genome-wide SNPs by the
Illumina HumanOmniExpress_12v1 DNA beadchip. Genotyping quality
controls, including Mendelian errors, were conducted using Pedcheck 30 and
Merlin31 software. Nonparametric linkage analysis was performed using the
exponential model proposed by Kong and Cox32, which is particularly adapted
to studies with few families where a strong genetic effect is anticipated, as in
our project. Multipoint analyses were also performed. Because the presence of
linkage disequilibrium (LD) between SNPs can introduce bias in multipoint
linkage analysis, before the analysis, we eliminated strong LD between SNPs
and selected SNPs regularly spaced every ~250 kb. The absence of LD between
selected SNPs was further confirmed using the Haploview program33.
Exome sequencing and sequence analysis. All sequencing experiments were
conducted at the Post-Genomic Platform of the Pitié-Salpêtrière (P3S) campus.
Genomic DNA from selected individuals was prepared and subjected to exome
capture using the Truseq Exome Enrichment kit (Illumina) followed by nextgeneration sequencing on the HiSeq2000 platform (Illumina). Sequence reads
were aligned to the human genome reference sequence (hg19 build) using the
Consensus Assessment of Sequence and Variation (CASAVA) software. PCR
or optical duplicates were discarded, as were nonpaired reads and reads with
low-quality mapping (Q score < 20). Variant calling was performed using the
Nature Genetics
SAMtools program34, and Annovar35 software was used to annotate the identified variants. Variants reported with MAF > 0.1% in the 1000 Genomes Project
or in the EVS, as well as variants in intronic (except variants considered to be
splicing variants and located at exon-intron junctions ranging from −5 to +5)
and intergenic regions, were filtered out. The analysis prioritized homozygous
or compound-heterozygous protein-altering variants. Variants of interest were
verified by Sanger sequencing.
To search for EIF2AK4 mutations in additional subjects, the entire coding sequence and intronic junctions of EIF2AK4 were PCR amplified using
specific oligonucleotide primer pairs and subjected to bidirectional Sanger
sequencing. The EIF2AK4 primer sequences used are listed in Supplementary
Table 4. The resulting sequence data were analyzed with the SeqScape software, version 2.5 (Applied Biosystems), in comparison with the EIF2AK4
reference sequence (NM_001013703). Nucleotide numbering reflects cDNA
numbering, with +1 corresponding to the A of the ATG translation initiation
codon in the reference sequence according to the Human Genome Variation
Society (HGVS) recommendations.
In silico tools for variant interpretation. The missense mutations identified
were analyzed by the prediction programs SIFT, Polyphen-2, Align-GVGD
and Mutation Taster to predict the putative functional role of the amino acid
sequence alteration. Potential splice variants identified were analyzed by five
splice-site predictions programs, Splice Site Finder, MaxEntScan, NNsplice,
GeneSplicer and Human Splicing Finder, to predict the potential effect on
mRNA splicing. All these tools are available through Alamut v2.2 software
(Interactive Biosoftware).
cDNA analysis. Total RNA from whole-blood samples was extracted with
the PAXGene Blood RNA system (Qiagen), and 500 ng of RNA was used for
RT-PCR according to the manufacturer’s recommendations (Superscript II,
random primers, Invitrogen). PCR products were analyzed by bidirectional
Sanger sequencing.
Immunohistochemical studies. Lung specimens were obtained at the time of
lung transplantation from patients with PVOD. Control lung specimens were
obtained from patients without any evidence of pulmonary vascular disease
who underwent lobectomy or pneumonectomy for localized lung cancer, with
normal tissue collected at a distance from the tumors. Immunohistochemical
analysis was performed on formalin-fixed samples. Paraffin-embedded
sections were stained with polyclonal rabbit anti-human primary antibody
against EIF2AK4 (Abcam, reference ab137543; dilution, 1:100). Biotinylated
horse anti-rabbit IgG (Vector, reference BA-1100) was used for primary antibody detection, streptavidin-bound alkaline phosphatase (Vector, reference
SA-5100) was used for amplification and Vector Red alkaline phosphatase
substrate (Vector, reference SK-5100) was the chromogen.
26.Humbert, M. et al. Pulmonary arterial hypertension in France: results from a national
registry. Am. J. Respir. Crit. Care Med. 173, 1023–1030 (2006).
27.Sitbon, O. et al. Long-term response to calcium channel blockers in idiopathic
pulmonary arterial hypertension. Circulation 111, 3105–3111 (2005).
28.Sztrymf, B. et al. Clinical outcomes of pulmonary arterial hypertension in carriers
of BMPR2 mutation. Am. J. Respir. Crit. Care Med. 177, 1377–1383 (2008).
29.Eyries, M. et al. ACVRL1 germinal mosaic with two mutant alleles in hereditary
hemorrhagic telangiectasia associated with pulmonary arterial hypertension. Clin.
Genet. 82, 173–179 (2012).
30.O’Connell, J.R. & Weeks, D.E. PedCheck: a program for identification of genotype
incompatibilities in linkage analysis. Am. J. Hum. Genet. 63, 259–266 (1998).
31.Abecasis, G.R., Cherny, S.S., Cookson, W.O. & Cardon, L.R. Merlin—rapid analysis
of dense genetic maps using sparse gene flow trees. Nat. Genet. 30, 97–101
(2002).
32.Kong, A. & Cox, N.J. Allele-sharing models: LOD scores and accurate linkage tests.
Am. J. Hum. Genet. 61, 1179–1188 (1997).
33.Barrett, J.C., Fry, B., Maller, J. & Daly, M.J. Haploview: analysis and visualization
of LD and haplotype maps. Bioinformatics 21, 263–265 (2005).
34.Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics
25, 2078–2079 (2009).
35.Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic
variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164
(2010).
doi:10.1038/ng.2844