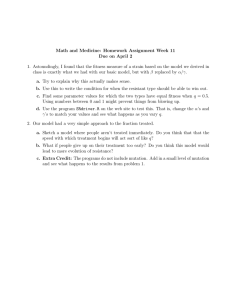
I560T
advertisement

Electrophysiological Characteris1cs and in-­‐silico Simula1ons of K Channel Muta1ons Responsible for Short QT Syndrome
Daniel Toshio Harrell1, Takashi Ashihara2, Ichiko Tominaga1, Keisuke Abe1, Naokata Sumitomo3,
Kikuya Uno4, Makoto Takano5, Naomasa Makita1
1) Nagasaki University, Department of Molecular Physiology, Nagasaki, Japan 2) Shiga University of Medical Science, Department of Cardiovascular and Respiratory Medicine, Heart Rhythm Center, Shiga, Japan 3) Nihon University, School of Medicine, Department of Pediatrics and Child Health, Tokyo, Japan 4) Tokyo Medical University, Hachioji Medical Center, Department of Cardiology, Hachioji, Japan 5) Kurume University School of Medicine, Department of Physiology, Kurume, Japan Disclosure: No Conflict of Interest for all Authors
Background
Methods
Short QT Syndrome is a rare inheritable arrhythmic
disease characterized by abnormally short QT intervals.
This disease can cause lethal ventricular fibrillation
ECG Diagnostic Criteria of SQT
QTc ≤370 ms
SimulaAons of KCNH2-­‐I560T 1. Patient Selection
• Found 3 probands diagnosed as having SQTS.
2. Mutation Screening
A
• Extraction of genomic DNA from patients’ blood
• PCR amplification of coding exons of KCNH2, KCNQ1, and KCNJ2.
• Direct sequencing using ABI Genetic Analyzer 3130
• Mutations verified by comparing probands with normal controls (n=200)
• Compared mutations to SNP data base
3. Whole-Cell Patch Clamp Recording of IKr
IKs
Markovian IKr
IKr = GKr · P(O) · (Vm – EK) (µA/µF)
• Site-directed mutagenesis were used to create plasmid
pCDNA3.1-KCNH2-WT or -I560T (1.5 µg) + pEGFP1(0.5µg)
• Transfection: Lipofectamine to COS-7 cells
IK r
P(O) = open probability of IKr
ααi
EK = (RT/F) · ln([K+]o / [K+]i) (mV)
4. Data Analysis
IK1
B
α
• Voltage dependence data was fit to the Boltzmann Equation:
Closed 3
αin
β
Inactivation
µ βi
αi
ααo
Closed 2
I / Imax = 1/ {1+exp [ ( V - V1/2) / k)] }
O’Hara-Rudy dynamic
Closed1
Open
βin
ββ
k= Slope factor, V1/2 = half-voltage potential
• Significance evaluated by Oneway ANOVA
Figure 1. (A) Used the Markov model to simulate the single channel gating
behavior of IKr. We simulated our mutation by changing the voltage dependence
of inactivation transition rates (βi and ββ). Also we increased the maximum
membrane conductance (GKr) by 45%. (B) The O’Hara-Rudy dynamic model
describes the cellular electrophysiology mechanisms of the human ventricular
myocytes. Using the Markov Model for IKr, the APDs were calculated for WT
and KCNH2-I560T.
5. APD and ECG Simulations of KCNH2-I560T
• Used Markov model for IKr to simulate channel properties of WT and I560T.
• Incorporated the Markovian IKr into the O’Hara-Rudy dynamic model
(PLoS Comput Biol 2011) to calculate the action potentials
to evaluate the effect of our mutation.
• Constructed the human ventricular transmural strand model based on the
modified O’Hara-Rudy dynamic model to calculate the QT interval
in the simulated ECG.
The increase in IKr, IKs, or IK1 abbreviates the action
potential duration (APD) which results in shortening of
the QT interval.
Results: Clinical
2. (A) Proband had palpitations
Case 1: 64 year-­‐old man (SQT1) Figure
and near syncope. He also suffered from
A Proband:
B
Palpitation
Near Syncope
Paroxysmal AF / AFL
QTc= 319 ms
SCD
ND
SCD
+
+
Case 2: 10 year-­‐old girl (SQT2)
A Proband:
paroxysmal AF and atrial flutter (AFL).
His QTc was 319 ms. (B) His brother and
father died from sudden cardiac death
(SCD). (C) Mutational screening showed
a novel missense mutation, I560T, at the
fifth transmembrane segment of KCNH2.
B
Fetal bradycardia with
congenital SSS
PPM after 12 days-old
QTc= 268 ms
C
Exon 6 ND
: Mutation Carrier
ND : Not Determined
: Suspected SQTS
: Short QT ECG
C
-
+
+
+
KCNQ1 Exon 1 I560T
ATC> ACC (Isoleucine-> Threonine)
ND
Chronic AF
Bradycardia
QTc= 375ms
: Mutation Carrier
ND : Not Determined
: Suspected SQTS
: Short QT ECG
KCNH2 PPM
at 50 yr
V141M
GTG-> ATG (Valine -> Methionine)
A New KCNH2 Mutation
Mutation previously reported by Hong, 2005
Figure 3. (A) Proband had fetal bradycardia and
diagnosed with congenital Sick Sinus Syndrome
(SSS). At 12 days-old, she was implanted with a
permanent pacemaker (PPM). Her QTc was 268
ms. (B) Her grandfather was given a PPM at 50
years old. Her father has suffered from chronic
atrial fibrillation (AF) bradycardia since he was 3
years old. His QTc was 375 ms. The proband and
her father were genetically positive for the
mutation. Though her father has the mutation,
he showed a QTc interval outside the ECG
diagnostic criteria for SQTS. This implies that
some mutation carriers may not manifest short
QT rather other ECG abnormalities such as AF.
(C) Mutation screening showed a missense
mutation, V141M, located in the first
transmembrane segment of the KCNQ1.This
mutation results in a gain of function of IKs. This
mutation was previously reported by Hong et al.
Results: Channel Proper1es of KCNH2 -­‐ I560T Transmural Strand Model
2.5-fold
increase
2
1
t
0.06
I560T
WT
I560T
30
WT
0
–80
–60
–40
–20
0
20
40
60
0.6
2.5-fold
increase
B
IV relationship
3
Endo
B
A
M
A
Markovian SimulaAon of KCNH2 MutaAon Current density (pA/pF)
Current-­‐voltage RelaAonship and Voltage-­‐dependence of AcAvaAon 0
–30
–60
Test pulse (mV)
80
I560T
60
WT
40
20
No significant shift
0
–80
–60
–40
–20
0
20
40
60
Test pulse (mV)
No significant shift
1.0
Steady-state inactivation
A
Steady-­‐State InacAvaAon B
14 mV
positive shift Figure 5 (A) Tail currents after a brief repolarization pulse was measured. (B)
Steady-State Inactivation of I560T showed a significant 14 mV positive shift of
V1/2. (WT: -27.3 ± 2.4 mV; I560T: -13.2 ± 4.1 mV; p≤0.005) This is an
characteristic of a gain of function of IKr, whereas the slope factors were nearly
identical. (WT: -25.4 ±1.08; I560T: -26.5 ±1.2; NS)
Availability
Figure 4. (A) Representative current traces of wild type(WT) and I560T. (B)
I560T showed a 2.5-fold increase in current density (WT: 40.6 ± 10.4 pA/pF;
I560T: 99.7± 10.2 pA/pF; p≤ 0.005). This is a characteristic of a gain of function
of IKr. (C) Voltage-dependence of WT and I560T were nearly identical. (WT: 18.5
± 1.6 mV; I560T: -19.7 ± 3.2 mV; NS)
0.6
0.4
0.2
WT
0
–50
50
M
Endo
Epi
0
M
Endo
–50
–100
Epi
Simulated
ECG
14 mV
positive shift
0
–80 –60 –40 –20
50
–100
I560T
0.8
ECG
Recording
Electrode
–90
(mV)
200 ms
Vm (mV)
C
Epi
Relative tail current (%)
100
0.24 (cm)
2 cm
Voltage-dependence of activation
0
20
40
60
80
QT = 388 ms
QT = 287 ms
Prepulse potential (mV)
Figure 6. (A) Current-voltage relationship, voltage-dependence of activation, and steady-state inactivation curves of the
Markovian IKr model, based on our experimental data. (B) We calculated the action potentials of the endocardium (Endo),
midmyocardium (M), and epicardium (Epi) by using the human ventricular transmural strand model, which was based on
the modified O’Hara-Rudy dynamic model. Our simulations also showed a shortening of QT interval for KCNH2-I560T in
the simulated ECG. (WT: 388 ms; I560T: 287 ms). The KCNH2-I560T’s QT interval also falls within the diagnostic criteria
for SQTS.
Conclusions
1. We found one novel Gain of Function mutation, I560T, in KCNH2 associated with
Short QT Syndrome.
2. We were able to demonstrate in-silico that KCNH2-I560T channel properties do
cause an abbreviation of the action potential duration resulting in a shorter QT
interval.