220
Comments, Opinions, and Reviews
Stroke Prevention
An Opportunity for Efficient Utilization of Health Care
Resources During the Coming Decade
Philip B. Gorelick, MD, MPH, FACP
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Background Stroke is unique among neurological diseases,
since it has a high prevalence and burden of illness, high
economic cost, and is preventable. Epidemiological approaches to stroke prevention include the "high-risk" and
"mass" approaches. In this review we discuss these preventive
strategies, target host and discretionary risk factors that are
amenable to these measures, and discuss potential cost
savings.
Summary of Review Projected numbers of strokes prevented for specific stroke risk factors were estimated by using
the population-attributable risk estimation for hypertension,
cigarette smoking, atrial fibrillation, and heavy alcohol con-
sumption. The projected numbers of strokes that could be
prevented were substantial and highest for hypertension and
cigarette smoking. Projected yearly cost of stroke associated
with these two treatable factors was also substantial.
Conclusions The prevention of stroke can be accomplished
by the high-risk or mass approach or a combination of these
approaches. The high-risk approach prevents strokes but is
also expensive. The mass approach may be more cost-effective,
which could lead to substantial savings, but this needs to be
investigated. (Stroke. 1994;25:220-224.)
Key Words • costs and cost analysis • prevention, primary
• risk factors
S
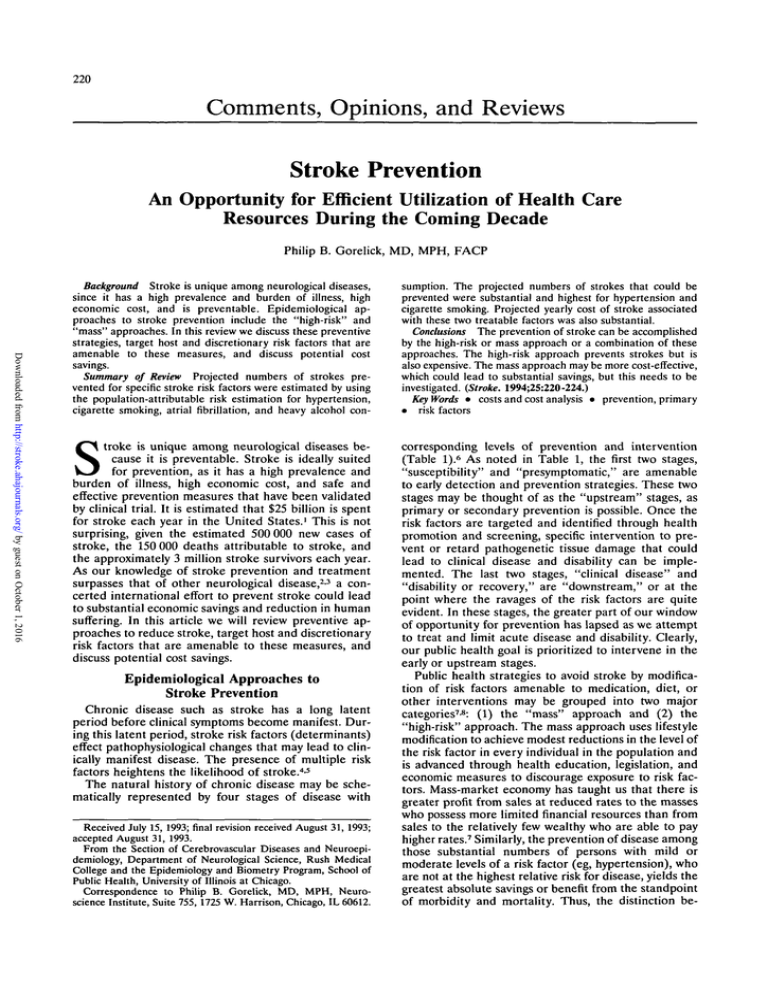
corresponding levels of prevention and intervention
(Table I). 6 As noted in Table 1, the first two stages,
"susceptibility" and "presymptomatic," are amenable
to early detection and prevention strategies. These two
stages may be thought of as the "upstream" stages, as
primary or secondary prevention is possible. Once the
risk factors are targeted and identified through health
promotion and screening, specific intervention to prevent or retard pathogenetic tissue damage that could
lead to clinical disease and disability can be implemented. The last two stages, "clinical disease" and
"disability or recovery," are "downstream," or at the
point where the ravages of the risk factors are quite
evident. In these stages, the greater part of our window
of opportunity for prevention has lapsed as we attempt
to treat and limit acute disease and disability. Clearly,
our public health goal is prioritized to intervene in the
early or upstream stages.
Public health strategies to avoid stroke by modification of risk factors amenable to medication, diet, or
other interventions may be grouped into two major
categories7-8: (1) the "mass" approach and (2) the
"high-risk" approach. The mass approach uses lifestyle
modification to achieve modest reductions in the level of
the risk factor in every individual in the population and
is advanced through health education, legislation, and
economic measures to discourage exposure to risk factors. Mass-market economy has taught us that there is
greater profit from sales at reduced rates to the masses
who possess more limited financial resources than from
sales to the relatively few wealthy who are able to pay
higher rates.7 Similarly, the prevention of disease among
those substantial numbers of persons with mild or
moderate levels of a risk factor (eg, hypertension), who
are not at the highest relative risk for disease, yields the
greatest absolute savings or benefit from the standpoint
of morbidity and mortality. Thus, the distinction be-
troke is unique among neurological diseases because it is preventable. Stroke is ideally suited
for prevention, as it has a high prevalence and
burden of illness, high economic cost, and safe and
effective prevention measures that have been validated
by clinical trial. It is estimated that $25 billion is spent
for stroke each year in the United States.1 This is not
surprising, given the estimated 500 000 new cases of
stroke, the 150 000 deaths attributable to stroke, and
the approximately 3 million stroke survivors each year.
As our knowledge of stroke prevention and treatment
surpasses that of other neurological disease,2-3 a concerted international effort to prevent stroke could lead
to substantial economic savings and reduction in human
suffering. In this article we will review preventive approaches to reduce stroke, target host and discretionary
risk factors that are amenable to these measures, and
discuss potential cost savings.
Epidemiological Approaches to
Stroke Prevention
Chronic disease such as stroke has a long latent
period before clinical symptoms become manifest. During this latent period, stroke risk factors (determinants)
effect pathophysiological changes that may lead to clinically manifest disease. The presence of multiple risk
factors heightens the likelihood of stroke. 45
The natural history of chronic disease may be schematically represented by four stages of disease with
Received July 15, 1993; final revision received August 31, 1993;
accepted August 31, 1993.
From the Section of Cerebrovascular Diseases and Neuroepidemiology, Department of Neurological Science, Rush Medical
College and the Epidemiology and Biometry Program, School of
Public Health, University of Illinois at Chicago.
Correspondence to Philip B. Gorelick, MD, MPH, Neuroscience Institute, Suite 755, 1725 W. Harrison, Chicago, IL 60612.
Gorelick
TABLE 1 .
Stroke Prevention and Economic Savings
221
Scheme for the Natural History of Chronic Disease and Levels of Prevention
Stage of disease*
Prevention level
Intervention
1: Susceptibility
2: Presymptomatic
1
Health promotion
Specific
intervention
3: Clinical
4: Disability or recovery
2
Early detection,
diagnosis, and
preventive
treatment
Acute treatment
Rehabilitation
*Stages 1 and 2 may be thought of as "upstream" and stages 3 and 4 as "downstream" (see text).
Reprinted with permission of WB Saunders Company.6
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
tween relative and absolute benefit must be kept in
mind when considering the mass approach.7 Furthermore, the "prevention paradox" (ie, a measure that
brings large benefits to the community may offer little to
the individual) must also be considered in this context.
The high-risk approach, on the other hand, identifies
individuals in the population with high levels of a risk
factor, and medication is usually administered to
achieve substantial reductions in that risk factor.8 This
approach is typically used by practicing physicians in
outpatient offices and clinics. When applied to a community or other large population, the high-risk approach can be a massive and expensive case-finding
procedure that still fails to prevent a high percentage of
the target disease (ie, among those in the community
with lower levels of the risk factor).
Ideally, risk factor modification is most effective when
the risk factor to be targeted is common in the population, there is a strong association between the risk factor
and disease, and there is a favorable effect of treatment
of the risk factor. Furthermore, valid, safe, and costeffective screening procedures and treatment are
necessary.9
Host and Discretionary Risk Factors to Target
for Stroke Prevention
There are two well-established risk factors, hypertension and cigarette smoking, and two less well-established risk factors, alcohol consumption and blood
lipids, that are amenable to the mass approach. Hypertension, whether systolic, diastolic, or combined, is a
well-documented risk factor for stroke, as seen in
observational and experimental epidemiological
study.4-5'10'14 Cigarette smoking has emerged more recently as a risk factor for ischemic stroke and some
forms of intracranial hemorrhage.15-18 Heavy alcohol
consumption may elevate the risk of ischemic and
hemorrhagic stroke.19'20 Among white populations, a
J-shaped epidemiological curve has been proposed to
explain the relation between the relative risk of ischemic
stroke and customary alcohol consumption, whereas a
positive direct linear association has been proposed for
the relative risk of hemorrhagic stroke with customary
alcohol consumption.20 There is mounting epidemiological evidence to link hypercholesterolemia or elevations
in low-density lipoproteins to ischemic stroke, although
blood lipids are not considered a well-established risk
factor for stroke.2125 Furthermore, these same four
factors play an important role in coronary heart disease
risk.26
There is substantial epidemiological evidence to advocate treatment of hypertension to reduce stroke.4-51014
Although controversial, it has been estimated that up to
70% of strokes could be eliminated by treatment of
hypertension.8 Furthermore, observational epidemiological study has shown that the stroke risk dramatically
reverses after abstinence from cigarette smoking for 2 to 5
years4 and after discontinuation of heavy alcohol consumption.19 Treatment of blood lipids reaps substantial
benefit for coronary heart disease, but there is controversy
about the benefit of treatment of hypercholesterolemia
and low-density lipoprotein cholesterol for stroke. However, it has been estimated that hypercholesterolemia
could account for up to 20% of strokes in Caucasians with
cholesterol levels >5.7 mmol/L.8
There are several other risk factors to consider for
stroke prevention. Atrial fibrillation may be responsible
for 75 000 strokes in the United States, and dramatic
risk reductions are noted when nonvalvular atrial fibrillation is treated with antithrombotic therapy.2730 Furthermore, clinical trials have shown that carotid endarterectomy is efficacious in the treatment of high-grade
(70% to 99%) carotid stenosis when there is mild stroke
or transient ischemic attack.3132 However, while the
absolute risk reduction for ipsilateral stroke is 17% in
the carotid endarterectomy treatment group compared
with medically treated patients,31 the absolute benefit of
carotid endarterectomy in stroke prevention is substantially lower, as there are relatively few individuals who
qualify for this operation based on accepted criteria.
Other risk factors such as coronary heart disease and
cardiac failure contribute to the attributable risk of
stroke,33 but it is uncertain at the present time to what
extent the treatment of these factors affects stroke
prevention.
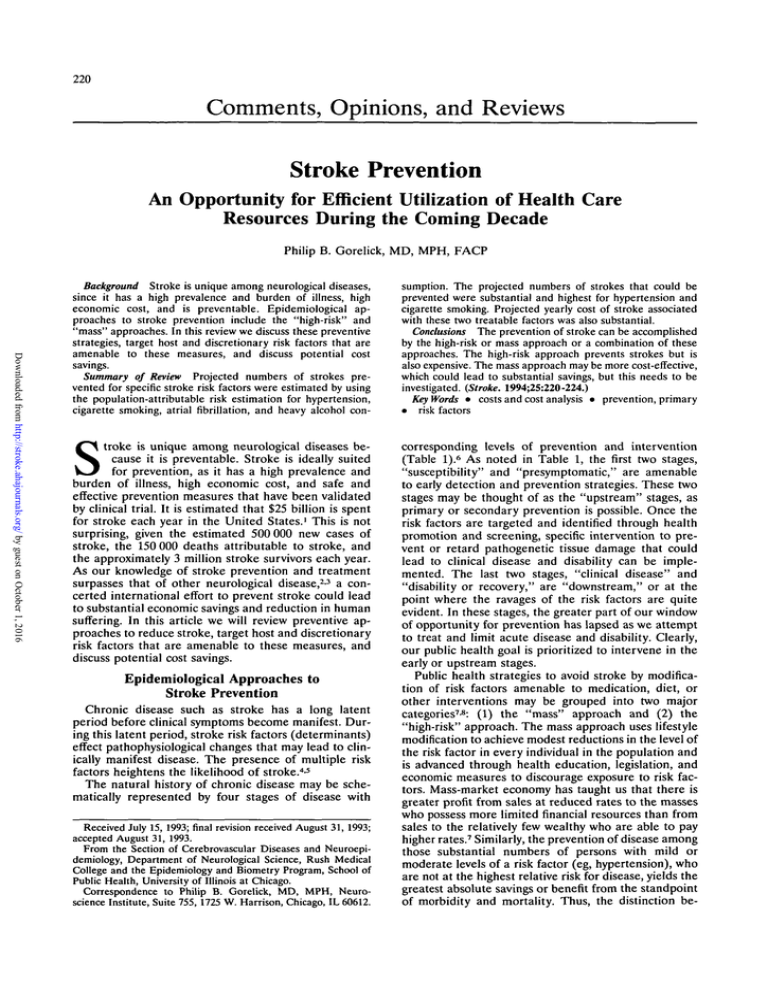
Illustrative Examples of Stroke Reduction
Through Risk Factor Modification
and Potential Cost Savings
Table 2 summarizes modifiable risk factors, population-attributable risk, and theoretical numbers of
strokes that could be prevented by successful treatment
of these risk factors. These calculations are estimates
and are based on the following assumptions that may
vary by population. (1) The overall population-attributable risks for hypertension and atrial fibrillation were
derived by averaging relative risk and prevalence data,
respectively, over age-specific categories (50 to 59, 60 to
69, 70 to 79, and 80 to 89 years) from the Framingham
Study.33 (2) The population-attributable risk of smoking
was calculated by averaging the given relative risks of
smoking for men and women from the Framingham
Study18 and using 27% as the estimate of the prevalence
of cigarette smoking in the population (data from
Morbidity and Mortality Weekly Report reprinted in
JAMA. 1987;258:1880). (3) As the population-attribut-
222
Stroke Vol 25, No 1 January 1994
TABLE 2. Modifiable Risk Factors, Population-Attributable Risk, and Projected Numbers of Strokes
Prevented in the United States*
Risk Factors
Estimated
Percentage
Exposed
Estimated
Relative
Risk
Estimated
Population-Attributable
Risk, %
Projected No.
of Strokes
Prevented
Hypertensiont
56.2
2.73
49.3
246 500
Cigarette smoking*
27.0
1.52
12.3
61 500
Atrial fibrillation!
3.98
3.60
9.4
47 000
Heavy alcohol consumption!
7.2
1.68
4.7
23 500
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
*Population-attributable risk was calculated from the following formula: A/1 +A, where A=prevalence multiplied by
(relative risk—1). The projected number of strokes prevented was calculated by multiplying the estimated 500 000
new stroke cases per year in the United States by the population-attributable risk.
tRelative risk and estimated percentage exposed were calculated by averaging the relative risks and prevalence
rates for a risk factor across the four given age strata, respectively, according to the Framingham data.33
^Relative risk was calculated by averaging the relative risks for men and women according to the Framingham
data,18 and the percentage exposed was estimated to be 27% according to national data sources (JAMA.
1987;258:1880).
§Relative risk for heavy drinkers was estimated to be 1.68 after Gorelick et al, 19 and the percentage exposed was
estimated by taking the ratio of "problem drinkers" to the total population in the United States (18 million to 250
million).
able risk of heavy alcohol consumption for stroke is
unknown, it was estimated by taking the ratio of "problem" drinkers in the United States (18 million persons)19 to total persons in the United States (250
million) and using an estimate of relative risk of stroke
of 1.68 for heavy alcohol consumption (after Gorelick et
al19). The population-attributable risk is an estimate of
the percentage of excess stroke in a population that is
attributable to a specific risk factor.
The reader should keep in mind that the populationattributable risk estimates as calculated above are rough
approximations and could be sharpened by making
calculations based on decade-specific estimates of prevalence and incidence of the various factors in the
population and expressing the result as a weighted
average. For example, the number of strokes prevented
may be overestimated in this analysis; a high percentage
of strokes occur in the elderly and the effect of antihypertensive therapy may be decreasing in those over 75
years of age,34 the relative risk of stroke for smoking
seems to be low above 75 years of age,17 and the
prevalence of heavy drinking may not apply to the
elderly. In addition, there may be residual relative risk
in treated hypertension and atrial fibrillation, for exam-
ple, that has not been accounted for in the analysis.
Furthermore, these estimates do not take into account
possible interactions among the risk factors.
The estimated number of preventable strokes in
Table 2 is substantial. This is especially true for hypertension and cigarette smoking. Let us now focus on
potential cost savings from prevention of these two
well-established and modifiable risk factors.
As the ideal is rarely achieved, Table 3 reviews (1)
cost savings at different levels of prevention success
based on a total of $25 billion spent for stroke per year
and (2) cost savings at different levels of prevention
success based on a theoretical 26-day hospital stay for
acute stroke that includes acute diagnosis, treatment,
and rehabilitation at a major private teaching hospital in
Chicago in fiscal year 1991 for ICD-9 diagnosis code
436. The sum of $25 billion spent for stroke each year is
an estimate of direct and indirect costs, the exactness of
which could vary and thus influence the calculated
savings.
The estimates in Table 3 suggest that substantial
economic savings could occur by successful modification
of stroke risk factors. Even if the effort were only 10%
efficient, the estimate of total yearly economic savings
TABLE 3. Projected Cost Savings at Different Levels of Stroke Prevention Success for
Hypertension and Cigarette Smoking
Level of Stroke Prevention Success
Cost Savings in Billions of Dollars
by Risk Factor
100%
75%
50%
25%
12.33
9.25
6.17
3.08
1.23
3.08
2.31
1.54
0.77
0.31
11.33
8.50
5.67
2.83
1.13
2.83
2.12
1.42
0.71
0.28
10%
Total yearly economic savings*
Hypertension
Cigarette smoking
Economic savings for acute stayt
Hypertension
Cigarette smoking
•Calculations are based on $25 billion spent per year on stroke and the prevention of a possible 246 500 strokes
among hypertensives and 61 500 strokes among US cigarette smokers, respectively.
tDiagnosis, treatment, and rehabilitation of 26 days at a major teaching hospital in Chicago in 1991 for ICD-9
diagnosis code 436. Calculations are based on a total of $46 000 spent per patient.
Gorelick Stroke Prevention and Economic Savings
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
could reach $1.23 billion for hypertension and $310
million for cigarette smoking. If medication is necessary
to control selected risk factors (eg, hypertension, atrial
fibrillation), these costs are then subtracted from the
projected savings, as are costs that are incurred due to
medication side effects or complications, to determine
the overall savings. A recent assessment of the costeffectiveness of primary stroke prevention in atrial
fibrillation in Sweden showed that after the direct and
indirect costs of "stroke saved," numbers of strokes
prevented, and cost of preventive treatment were calculated, primary stroke prevention with antithrombotics
resulted in a net savings.35-36 Table 3 also suggests that
the economic savings for acute hospitalization and
rehabilitation could be substantial as well.
An alternate approach to medication would be to
reduce the population's level of stroke risk factors (eg,
hypertension, cigarette smoking, heavy alcohol consumption, and hypercholesterolemia) by effecting lifestyle changes through behavioral modification using the
mass approach of economic and legislative measures
and education. The public needs to be educated about
healthy lifestyles, risk factors for stroke and other major
diseases, treatment of risk factors, and recognition of
early warning signs of stroke and other major causes of
mortality. Mass education to teach healthy lifestyles
through behavioral modification, targeted to groups at
risk for stroke and to the youth in our school systems,
could be the most cost-effective of all approaches.
Furthermore, even if risk-factor control were to delay
onset of stroke by only 5 years in a high proportion of
persons rather than eradicate stroke in those persons,
for example, substantial economic and human savings
could still be realized by postponing stroke onset.
Conclusion
Stroke is a preventable disease that has a high
economic cost. As shown in this analysis, there is
potential for substantial human and economic savings.
The prevention of stroke can be accomplished by a
high-risk or mass approach. The high-risk approach is
effective in saving strokes but is also expensive and may
not save money, especially in lower-risk groups.37 The
mass approach, on the other hand, may be more costeffective, although this needs to be clarified.
How our health care resources will be allocated and
used in the coming decades has become a focus of major
public and presidential attention. Prudent use of these
resources is paramount. As concerned citizens we
should support economic and legislative measures to
educate the public about healthy lifestyles, at-risk behaviors, risk factors and warning signs of disease, and
the importance of standard treatments that reduce the
risk of disease. Now is the time to plan healthy lifestyles
to prevent disease in later life and to add "life to years."
We must become responsible health care partners in
this era of medical economic change.
Acknowledgment
Supported in part by National Institute on Aging grant No.
AG10102-03, the MR Bauer Foundation, and the Marjorie
and Herbert Fried Scholarship Fund.
223
References
1. American Heart Association. 1992 Heart and Stroke Facts. Dallas,
Texas, 1991, pp 1-48.
2. Gorelick PB. Epidemiologic contributions. In: Caplan LR, ed.
Scientific Basis of Stroke and Its Treatment. Springer-Verlag (in
press).
3. Gorelick PB. Degenerative diseases. Chicago Medicine. 1991;94:
14-18.
4. Wolf PA, Belanger AJ, D'Agostino RB. Management of risk
factors. Neurol Clin. 1992;10:177-191.
5. Wolf PA, D'Agostino RB, Belanger AJ. Predicting Stroke Risk.
Monograph. Phase Five Communications, Inc, August 1992,
pp 10-14.
6. Mausner JS, Kramer S. Mausner and Bahn Epidemiology—An
Introductory Text. Philadelphia, Pa: WB Saunders Company;
1985:1-42.
7. Rose G. Strategy of prevention: lessons from cardiovascular
disease. Br Med J. 1981;282:1847-1850.
8. Dunbabin DW, Sandercock PAG. Preventing stroke by modification of risk factors. Stroke. 1990;21(suppl IV):IV-36-IV-39.
9. Sox HC. Screening for lipid disorders under health system reform.
N EnglJ Med. 1993;328:1269-1271.
10. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic
hypertension: final results of the Systolic Hypertension in the
Elderly Program (SHEP). JAMA. 1991;256:3255-3264.
11. MacMahon SW, Cutler JA, Furberg CD, Payne GH. The effects of
drug treatment for hypertension on morbidity and mortality from
cardiovascular disease: a review of randomized controlled trials.
Prog Cardiovasc Dis. 1986;29(suppl 1):99-118.
12. MacMahon S, Peto R, Cutler JA, Collins R, Sorlie P, Neaton J,
Abbot R, Godwin J, Dyer A, Stamler J. Blood pressure, stroke and
coronary heart disease: part I. Effects of prolonged differences in
blood pressure — evidence from nine prospective observational
studies corrected for the regression dilution bias. Lancet. 1990;335:
765-774.
13. Collins R, Peto R, MacMahon S, Hebert P, Fiebach NH, Eberlein
KA, Godwin J, Qizilbash N, Taylor JD, Hennekens CH. Blood
pressure, stroke and coronary heart disease: part II. Effects of
short-term reductions in blood pressure and overview of the
unconfounded randomized drug trials in an epidemiologic context.
Lancet. 1990;335:827-838.
14. Bozzola FG, Gorelick PB, Jensen JM. Epidemiology of intracranial hemorrhage. Neuroimag Clin N Am. 1992;2:l-10.
15. Gorelick PB, Rodin MB, Lanzerberg P, Hier DB, Costigan J.
Weekly alcohol consumption, cigarette smoking, and the risk of
ischemic stroke: results of a case-control study at three urban
medical centers in Chicago, Illinois. Neurology. 1989;39:339-343.
16. Longstreth WT, Nelson L, Koespel TD, vanBelle G. Risk factors
for subarachnoid hemorrhage. Stroke. 1991;22:149.
17. Shinton R, Beevers G. Meta-analysis of relation between cigarette
smoking and stroke. Br Med J. 1989;298:787-794.
18. Wolf PA, D'Agostino RB, Kannel WB, Bonita R, Belanger AJ.
Cigarette smoking as a risk factor for stroke: the Framingham
Study. JAMA. 1988;259:1025-1029.
19. Gorelick PB. The status of alcohol as a risk factor for stroke.
Stroke. 1989;20:1607-1610.
20. Camargo CA. Moderate alcohol consumption and stroke: the epidemiologic evidence. Stroke. 1989;20:1611-1626.
21. Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD. Serum
cholesterol levels and six-year mortality from stroke in 350,977
men screened for the Multiple Risk Factor Intervention Trial.
N EnglJ Med. 1989;320:904-910.
22. Salonen R, Seppanen K, Rauramaa R, Salonen JT. Prevalence of
carotid atherosclerosis and serum lipid levels in eastern Finland.
Atherosclerosis. 1988;8:788-792.
23. Tell GS, Gouse JR, Furberg CD. Relation between blood lipids,
lipoproteins and cerebrovascular atherosclerosis: a review. Stroke.
1988;19:423-430.
24. Qizibash N, Duffy SW, Warlow CP, Mann J. Lipids are risk factors
for ischemic stroke. Cerebrovasc Dis. 1992;2:127-136.
25. Dennis MS, Warlow CP. Stroke: incidence, risk factors and
outcome. BrJ Hosp Med. 1987;37:194-198.
26. Sytkowski PA, Kannel WB, D'Agostino RB. Changes in risk factors
and decline in mortality from cardiovascular disease. N Engl J Med.
1990;322:1635-1641.
27. Anderson DC, the SPAF Investigators. Progress report of the
Stroke Prevention in Atrial Fibrillation Study. Stroke. 1990;
21(suppl III):III-12-III-17.
224
Stroke Vol 25, No 1 January 1994
28. SPAF Investigators. Preliminary report of the Stroke Prevention in
Atrial Fibrillation Study. N Engl J Med. 1990;322:863-868.
29. Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. The effects of low dose warfarin on the risk of stroke in
patients with nonrheumatic atrial fibrillation. N Engl J Med. 1990;
323:1505-1511.
30. Petersen P, Godtfredsen J, Boysen G, Andersen ED, Andersen B.
Placebo-controlled, randomized trial of warfarin and aspirin for
prevention of thromboembolic complications of chronic atrial
fibrillation: the Copenhagen AFASAK Study. Lancet. 1989;1:
175-179.
31. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade stenosis. N Engl J Med. 1911;325:
445-453.
32. European Carotid Surgery Trialists' Collaborative Group. MRC
European Carotid Surgery Trial: interim results for symptomatic
patients with severe (70-99%) or with mild (0-29%) carotid
stenosis. Lancet. 1991;337:1235-1243.
33. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke.
1991;22:983-988.
34. Dahlof B, Lindholm LH, Hansson L, Schersten B, Ekbom T,
Wester P-O. Morbidity and mortality in the Swedish Trial in Old
Patients with Hypertension (STOP-Hypertension). Lancet. 1991;
338:1281-1285.
35. Gustafsson C, Asplund K, Britton M, Norrving B, Olsson B, Marke
L-A. Cost effectiveness of primary stroke prevention in atrial
fibrillation: Swedish national perspective. BMJ. 1992;305:
1457-1460.
36. Laupacis A, Feeny D, Detsky AS, Tegwell PX. How attractive
does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Can MedAssocJ. 1992;146:473-481.
37. Alderman MH. Blood pressure management: individualized
treatment based on absolute risk and the potential for benefit. Ann
Intern Med. 1993;119:329-335.
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Stroke prevention. An opportunity for efficient utilization of health care resources during
the coming decade.
P B Gorelick
Stroke. 1994;25:220-224
doi: 10.1161/01.STR.25.1.220
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1994 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/25/1/220
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click Request
Permissions in the middle column of the Web page under Services. Further information about this process is
available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/