Personal Protective Equipment PPE
advertisement

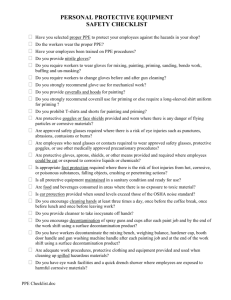
Trainer notes for personal protection equipment (PPE) presentation Personal Protective Equipment PPE A short presentation on the principles of infection control in social care 1|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme Different types of PPE? • Gloves • Aprons • Face and eye protection Why use these? Gloves • To reduce the number of micro-organisms getting on the skin of the carer during certain situations where there may be high numbers present, e.g. incontinence, wound discharge, blood spills • To reduce the chance of micro-organisms getting onto other patients or surfaces from the carer’s hands • To protect the carer’s hands from chemicals, medications and cleaning fluids Aprons • to protect uniform from becoming soiled with body fluids • to reduce the number of micro-organisms getting on to uniforms, particularly from the waist to knees area, when giving care • to reduce chance of transfer of micro-organisms to other patients and to carers’ hands from contact with the uniform Face/eye protection • To prevent micro-organisms, present in aerosols and sprays of body fluids, from having contact with mucous membranes - includes eyes and mouth 2|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme Heavy duty - reusable What gloves to use • Cleaning and environment • Handling laundry Thin polythene disposable • Food preparation • Food handling Single-use non-sterile vinyl gloves • Carer or service user is latex sensitive • When carers skin is damaged Single use powder free latex gloves • When dexterity is important or lengthy procedure likely • When contact with blood is likely Nitrile gloves • Food preparation • Food handling Sterile • Aseptic and invasive procedures • Manipulation of central lines and catheterisation Heavy duty – reusable e.g., Marigolds for general cleaning of environment and equipment washing up handling laundry Wash on hands, dry and hang up ready for next use Never use for patient care! Thin polythene disposable gloves for food preparation and food handling never use for patient care split easily and leak slip off hands easily Single use non sterile vinyl gloves When carer or patient is latex sensitive contact with spilt body fluids likely ( not as protective as latex with blood contact) changing pads, wiping bottoms, etc. dressing dirty wounds, leg ulcers, etc. when carer’s skin is damaged Single use powder free latex gloves When dexterity is important manipulation or lengthy procedure likely contact with blood is likely Nitrile gloves use as for latex gloves when carer or patient is latex sensitive better than vinyl when manipulation or dexterity important 3|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme more protective than vinyl for blood contact Sterile/surgical gloves Sterile gloves should be used for aseptic and invasive procedures. – manipulation of central lines – catheterisation 4|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme Aprons For use when your uniform is likely to have contact with body fluids and discharges. Eye/face protection When carrying out procedures where spray or aerosols may be created Aprons When your uniform is likely to have contact with body fluids and discharges : dressing wounds dealing with incontinence giving personal care cleaning equipment cleaning up spills Eye/face protection When carrying out procedures where spray or aerosols may be created : intubation using suction catheters scrubbing instruments emptying body fluids down sluices, toilets, etc. What types Eyes goggles visor glasses with side protection Mouth and face visor mask 5|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme Considerations for storage and disposal Who is going to be wearing these? Does the storage present a risk to vulnerable people? Does the storage present an infection risk? • The storage of PPE should be in a place that is easy for people to collect it and put it on. If a service user is isolated and relatives and friends are required to use PPE to prevent the spread of infection then PPE should be supplied in an obvious way to tell people they are required to use it, such as outside the isolated persons room. • Plastic gloves and aprons can present a significant choking and/or suffocation risk to certain vulnerable groups. They can also be placed in drainage pipes and toilets and cause damage or flooding problems. Is the personal protective equipment stored in a place where members of these vulnerable groups are unable to access it without supervision? • Staff should also be aware of methods of breaking the chain of infection. Putting on gloves and aprons in one aea such as a central PPE trolley then opening doors and touching contaminated surfaces between putting on the PPE and handling the service user, food and equipment can spread infection. Consideration should also be given to the way the PPE is removed and disposed of after a task or procedure. In this section it is important to allow colleagues to consider how they currently use PPE. Without asking colleagues to admit personal bad practices ask delegates to think about these three issues: 1. When should you use each of the following a) latex gloves b) plastic aprons and c) protective eye wear. 2. Can you identify anyone who might fall into the category of a vulnerable person when it comes to storing PPE close by 3. Can you think about any opportunity where you might pick up micro-organisms between collecting PPE and disposing of it following a task. Some answers to the above might be 1. You should have policy and procedures to indicate when each of these items of PPE are to be used. This is a good opportunity to check that staff are aware of the organisations 6|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme policies. This is also a good opportunity to check colleagues understanding of the key messages in the course. 2. People at risk from choking and/or suffocation are visiting children, people prone to placing foreign objects in their mouth or people prone to pick up foreign objects and handle them inappropriately. These could be people with dementia or learning disabilities. 3. Colleagues should be encouraged to walk through tasks and procedures highlighting points when they could potentially touch contaminated areas. Things such as sitting on service users beds during procedures, touching door handles, table tops and draw handles with clean PPE during aseptic procedures such as changing dressings or following a procedure. The more realistic the examples colleagues produce the closer to recognising the key messages they will be during their daily role 7|Page Trainer notes for personal protective equipment presentation Infection control supported learning programme