ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
120 Accommodation and Presbyopia
Sunday, May 05, 2013 10:30 AM-12:15 PM
TCC LL 4/5 Paper Session
Program #/Board # Range: 381-387
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 381
Presentation Time: 10:30 AM - 10:45 AM
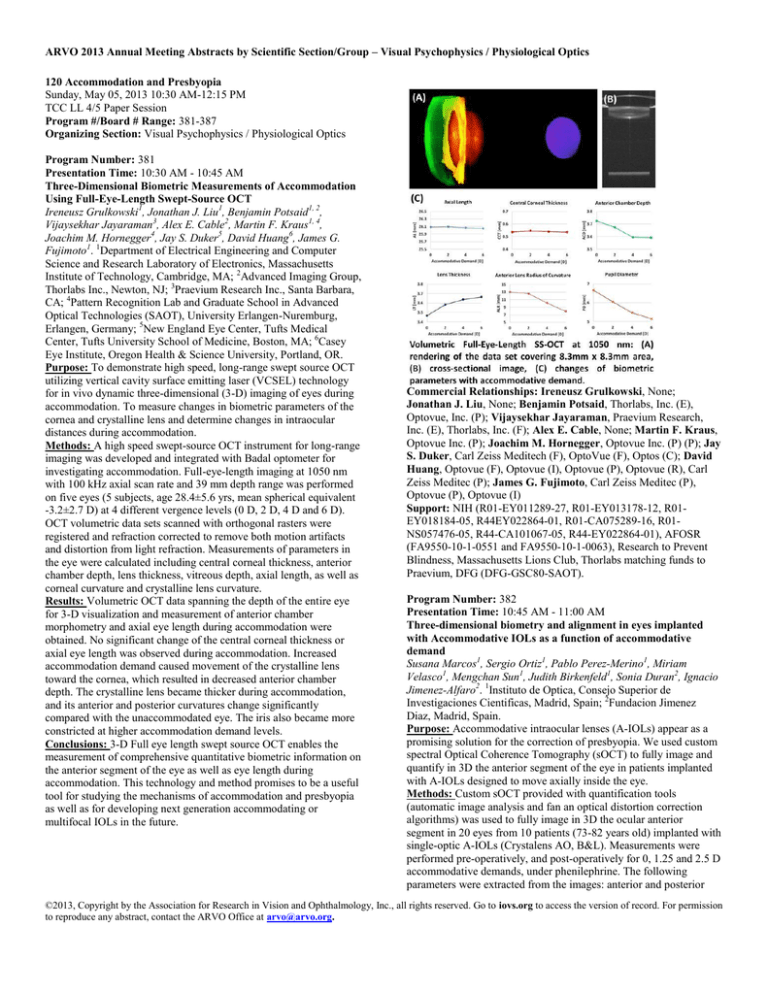
Three-Dimensional Biometric Measurements of Accommodation
Using Full-Eye-Length Swept-Source OCT
Ireneusz Grulkowski1, Jonathan J. Liu1, Benjamin Potsaid1, 2,
Vijaysekhar Jayaraman3, Alex E. Cable2, Martin F. Kraus1, 4,
Joachim M. Hornegger4, Jay S. Duker5, David Huang6, James G.
Fujimoto1. 1Department of Electrical Engineering and Computer
Science and Research Laboratory of Electronics, Massachusetts
Institute of Technology, Cambridge, MA; 2Advanced Imaging Group,
Thorlabs Inc., Newton, NJ; 3Praevium Research Inc., Santa Barbara,
CA; 4Pattern Recognition Lab and Graduate School in Advanced
Optical Technologies (SAOT), University Erlangen-Nuremburg,
Erlangen, Germany; 5New England Eye Center, Tufts Medical
Center, Tufts University School of Medicine, Boston, MA; 6Casey
Eye Institute, Oregon Health & Science University, Portland, OR.
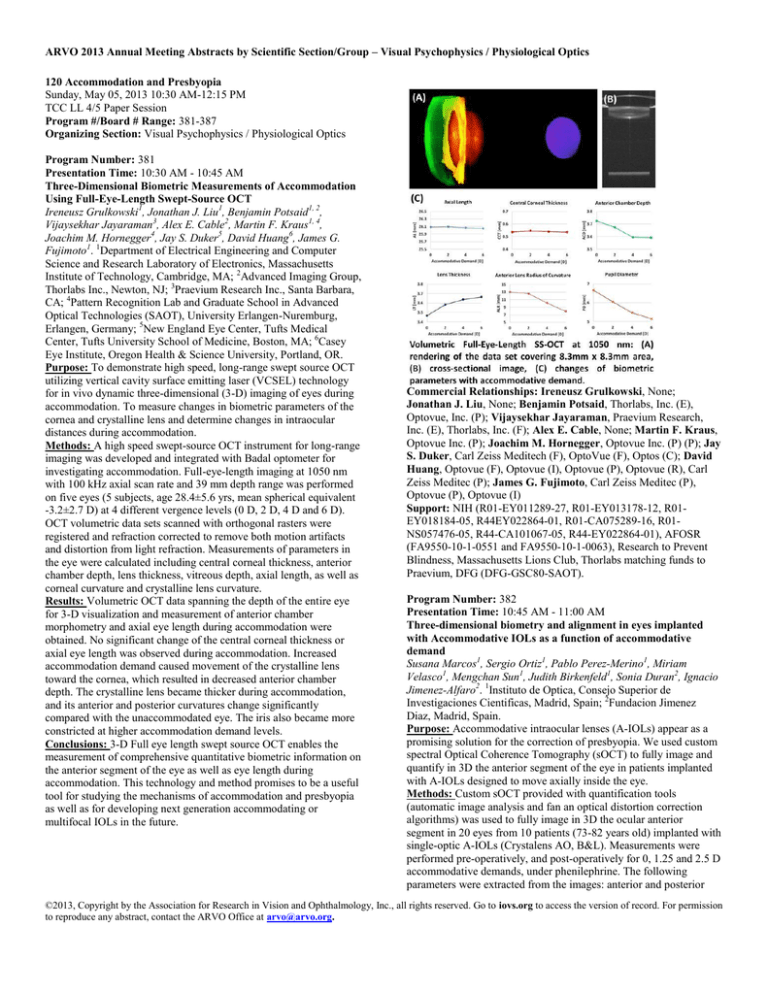
Purpose: To demonstrate high speed, long-range swept source OCT
utilizing vertical cavity surface emitting laser (VCSEL) technology
for in vivo dynamic three-dimensional (3-D) imaging of eyes during
accommodation. To measure changes in biometric parameters of the
cornea and crystalline lens and determine changes in intraocular
distances during accommodation.
Methods: A high speed swept-source OCT instrument for long-range
imaging was developed and integrated with Badal optometer for
investigating accommodation. Full-eye-length imaging at 1050 nm
with 100 kHz axial scan rate and 39 mm depth range was performed
on five eyes (5 subjects, age 28.4±5.6 yrs, mean spherical equivalent
-3.2±2.7 D) at 4 different vergence levels (0 D, 2 D, 4 D and 6 D).
OCT volumetric data sets scanned with orthogonal rasters were
registered and refraction corrected to remove both motion artifacts
and distortion from light refraction. Measurements of parameters in
the eye were calculated including central corneal thickness, anterior
chamber depth, lens thickness, vitreous depth, axial length, as well as
corneal curvature and crystalline lens curvature.
Results: Volumetric OCT data spanning the depth of the entire eye
for 3-D visualization and measurement of anterior chamber
morphometry and axial eye length during accommodation were
obtained. No significant change of the central corneal thickness or
axial eye length was observed during accommodation. Increased
accommodation demand caused movement of the crystalline lens
toward the cornea, which resulted in decreased anterior chamber
depth. The crystalline lens became thicker during accommodation,
and its anterior and posterior curvatures change significantly
compared with the unaccommodated eye. The iris also became more
constricted at higher accommodation demand levels.
Conclusions: 3-D Full eye length swept source OCT enables the
measurement of comprehensive quantitative biometric information on
the anterior segment of the eye as well as eye length during
accommodation. This technology and method promises to be a useful
tool for studying the mechanisms of accommodation and presbyopia
as well as for developing next generation accommodating or
multifocal IOLs in the future.
Commercial Relationships: Ireneusz Grulkowski, None;
Jonathan J. Liu, None; Benjamin Potsaid, Thorlabs, Inc. (E),
Optovue, Inc. (P); Vijaysekhar Jayaraman, Praevium Research,
Inc. (E), Thorlabs, Inc. (F); Alex E. Cable, None; Martin F. Kraus,
Optovue Inc. (P); Joachim M. Hornegger, Optovue Inc. (P) (P); Jay
S. Duker, Carl Zeiss Meditech (F), OptoVue (F), Optos (C); David
Huang, Optovue (F), Optovue (I), Optovue (P), Optovue (R), Carl
Zeiss Meditec (P); James G. Fujimoto, Carl Zeiss Meditec (P),
Optovue (P), Optovue (I)
Support: NIH (R01-EY011289-27, R01-EY013178-12, R01EY018184-05, R44EY022864-01, R01-CA075289-16, R01NS057476-05, R44-CA101067-05, R44-EY022864-01), AFOSR
(FA9550-10-1-0551 and FA9550-10-1-0063), Research to Prevent
Blindness, Massachusetts Lions Club, Thorlabs matching funds to
Praevium, DFG (DFG-GSC80-SAOT).
Program Number: 382
Presentation Time: 10:45 AM - 11:00 AM
Three-dimensional biometry and alignment in eyes implanted
with Accommodative IOLs as a function of accommodative
demand
Susana Marcos1, Sergio Ortiz1, Pablo Perez-Merino1, Miriam
Velasco1, Mengchan Sun1, Judith Birkenfeld1, Sonia Duran2, Ignacio
Jimenez-Alfaro2. 1Instituto de Optica, Consejo Superior de
Investigaciones Cientificas, Madrid, Spain; 2Fundacion Jimenez
Diaz, Madrid, Spain.
Purpose: Accommodative intraocular lenses (A-IOLs) appear as a
promising solution for the correction of presbyopia. We used custom
spectral Optical Coherence Tomography (sOCT) to fully image and
quantify in 3D the anterior segment of the eye in patients implanted
with A-IOLs designed to move axially inside the eye.
Methods: Custom sOCT provided with quantification tools
(automatic image analysis and fan an optical distortion correction
algorithms) was used to fully image in 3D the ocular anterior
segment in 20 eyes from 10 patients (73-82 years old) implanted with
single-optic A-IOLs (Crystalens AO, B&L). Measurements were
performed pre-operatively, and post-operatively for 0, 1.25 and 2.5 D
accommodative demands, under phenilephrine. The following
parameters were extracted from the images: anterior and posterior
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
corneal and lens (natural and A-IOL) surface 3D geometry, pre-and
post- anterior chamber depth (ACD), and lens and A-IOL tilt. ACD
and lens alignment were estimated from 3D data, from the distances
between surface apices, and from the vectors normal to the pupil and
lens planes, respectively.
Results: Data were obtained from fully registered pre/post-operative
images, and from images corresponding to different accommodative
demands (see Figure). The average ACD pre-op was 2.67±0.25 mm,
and post-op (relaxed accommodation) was 3.84±0.39 mm, with high
left/right eye symmetry. Most lenses moved axially backward upon
an accommodative demand (up to 0.4 mm), opposite from the
expected shift by design. Only five lenses moved forward (up to 0.11
mm). Natural lens tilt ranged from -2.14 to 1.84 (superior). The
absolute tilt of the implanted A-IOLs was on average higher than the
natural lens’ tilt; in 5 eyes the A-IOL tilt exceeded by more than x2.5
the pre-op tilt, and changed orientation. A-IOLs tilts generally
occurred in the superior/nasal orientation. Most lenses changed tilt
with accommodative demand (from 0 to 9 deg/D, on average across
eyes).
Conclusions: Quantitative sOCT imaging of the pre- and postoperative anterior segment of the eye appear essential to understand
the mechanisms by which current A-IOLs operate and advance
towards new developments. The tested A-IOL did not work as
expected in most eyes, indicating that potential improvements in near
vision are unlikely resulting from effective change in paraxial power,
but may be associated to induced lens tilt.
Program Number: 383
Presentation Time: 11:00 AM - 11:15 AM
Synchronized Real Time Imaging of Ocular Anterior Segment
Biometry and Ciliary Muscle during Accommodation
Aizhu Tao1, 2, Yilei Shao1, 2, Meixiao Shen2, Hong Jiang1, Jianguang
Zhong1, 3, Dexi Zhu2, Jianhua Wang1. 1University of Miami Miller
School of Medicine, Bascom Palmer Eye Institute, Miami, FL;
2
Wenzhou Medical College, School of Ophthalmology and
Optometry, Wenzhou, China; 3Hangzhou First People’s Hospital,
Hangzhou, China.
Purpose: To test the feasibility and repeatability of synchronized
real-time imaging of ocular anterior segment biometry and ciliary
muscle during accommodation using optical coherence tomography
(OCT).
Methods: An improved OCT system using CMOS camera for scan
speed improvement based on our previously reported ultra-long scan
depth OCT was used (Du et al., Ophthalmology, 2012). The scan
depth was 12.6 mm in air. A switchable reference arm was used to
sequentially acquire a set of two frames with the placement of the
zero delay lines on the top and the bottom of the anterior segment.
Semi-automatic software was used to register and overlap the two
frames and optical correction was performed before yielding
biometric measurements. Another OCT was used to image the ciliary
muscle and had a light source with the central wavelength of 1310
nm and the bandwidth of 75 nm. The two devices were combined and
synchronized. The full range of the anterior segment at horizontal
meridians with a frame rate of 8 fps, while the ciliary muscle at the
temporal side of 7 fps, were imaged for a total time of approximately
3.7 second. The 6.00 D accommodative stimulus was given 1 second
after the onset of acquisition. Four healthy subjects (age: 24.3 ± 2.1
yrs, refractive error: 4.4 ± 2.0 D) were enrolled and imaged in two
separate sessions.
Results: Dynamic alternation of both the anterior segment biometry
and ciliary muscle were successfully recorded and measurements
matched well between two imaging sessions (Fig. 1). During
accommodation, the ciliary muscle contracts as shown in the increase
of the maximal ciliary muscle thickness and the forward movement
of the ciliary apex. As expected, the crystalline lens became thicker
and steeper in the front surface. These changes appeared to be as a
function of time and the biometric alternation was almost parallel to
the ciliary muscle constriction. However, hysteresis (0.5 s) of the lens
reshaping (time to reach the maximal changes) compared to maximal
ciliary muscle contraction occurred in two cases.
Conclusions: This pilot study demonstrated for the first time that
combined OCT system is feasible to determine the dynamic
alternation of the anterior segment during accommodation. The realtime relationship between anterior segment biometry and ciliary
muscle contraction can be quantified reliably, which sets the stage for
studying the mechanism of accommodation.
Commercial Relationships: Susana Marcos, Essilor (F),
PCT/ES2012/070185 (P); Sergio Ortiz, PCT/ES2012/070185 (P);
Pablo Perez-Merino, None; Miriam Velasco, None; Mengchan
Sun, None; Judith Birkenfeld, None; Sonia Duran, None; Ignacio
Jimenez-Alfaro, None
Support: Spanish Government Grant FIS2011-25637; European
Research Council ERC-2011 AdG-294099; EU Marie Curie FP7PEOPLE-2010-ITN 264605; CSIC JAE-Program; Unidad Asociada
IO-CSIC/FJD
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
accommodate less, and thus presents a real accommodative lag for
near targets.
Commercial Relationships: Norberto Lopez-Gil, None; Paula
Bernal-Molina, None; Richard Legras, None; Teresa FerrerBlasco, None; Robert Montés-Micó, None
Support: European grant ERC-2012-StG 309416-SACCO and
Fundacion Seneca Grant 15312/PI/10
Commercial Relationships: Aizhu Tao, None; Yilei Shao, None;
Meixiao Shen, None; Hong Jiang, NIH (F); Jianguang Zhong,
None; Dexi Zhu, None; Jianhua Wang, NIH (F), RPB (F)
Support: Supported by research grants in part from the NIH
EY021012, EY021336 and R01EY020607S, NIH Center Grant P30
EY014801, Research to Prevent Blindness (RPB), Department of
Defense (DOD- Grant#W81XWH-09-1-0675).
Program Number: 384
Presentation Time: 11:15 AM - 11:30 AM
Depth-of-focus of the accommodating eye
Norberto Lopez-Gil1, Paula Bernal-Molina1, Richard Legras2, Teresa
Ferrer-Blasco3, Robert Montés-Micó3. 1Grupo de Investigación de
Ciencias de la Visión, Universidad de Murcia, Murcia, Spain;
2
Laboratoire Aimé Cotton, CNRS. University Paris-Sud, Orsay,
France; 3Optica, Universidad de Valencia, Burjassot, Spain.
Purpose: To obtain experimental values of the depth-of-focus (DoF)
of the human eye for different accommodative states.
Methods: In a first part of the experiment we measured the
aberrations of 7 young eyes (29.7 ± 7.7 years) during accommodation
at 8 different accommodative steps (from -1 to 6 D). Then, in a
second part, accommodation was paralyzed (cyclopentolate) and we
used an adaptive optics system with a deformable mirror (Imagine
Eyes, France) to correct the aberrations of the paralyzed eye and to
simulate the aberrations of the accommodated eye for each
accommodative state measured in the first part of the experiment. A
Badal system was used to modify the vergence of the stimulus in
order to obtain three-repeated measurements of the subjective DoF.
Equally in the second part of the experiment, an artificial pupil with a
similar diameter to the natural pupil measured in the first part was
used. The object stimulus used consisted on microdisplay showing
three lines of high contrast black letters of 0.4, 0.5 and 0.6 VA on a
white background. The criteria used for DoF was the objectionable
blur.
Results: All subjects presented a similar result of DoF (maximum
intra-subject SD = 0.23 D) with a mean value of DoF which
increased from 0.85 to 1.07 D during accommodation (0 to 6 D). This
increase can be explained in terms of pupil accommodative myosis
(mean pupil diameter decreased from 5.70 to 4.63 mm during the
accommodation range). Accommodative lag increased with
accommodation, and for large accommodation demands (4-6 D) the
refractive state of the eye was close to the extreme of the DoF, so, in
fact, accommodation was minimum. Results of DoF correlate with
the few measurements previously obtained using other methodologies
by other authors.
Conclusions: Under experimental conditions, DoF is close to 1 D.
Our results clearly indicate that, if the deterioration of the retinal
image quality is acceptable, the visual system uses DoF to
Program Number: 385
Presentation Time: 11:30 AM - 11:45 AM
Anatomical and accommodative changes in patients undergoing
cataract surgery with presbyopia accommodative lens placement
Diego Chavez. echography, Hospital Nuestra Señora de la Luz,
Mexico, Mexico.
Purpose: Document with UBM study the anatomical and
accommodative intraocular changes that occur with pharmacological
accommodative stimulus using 2% pilocarpine in eyes with
accommodative IOLs implantation.
Methods: METHODS patients undergoing cataract surgery with
intraocular accommodative lens placement during 2012.
Measurements in millimeters of the lens-corneal endothelium
distance (LCED) , irido-corneal angle (ICA) and trabecular ciliary
body distance (TCBD) were taken using UBM study, all of them with
superior and nasal orientation. Then we apply one drop of pilocarpine
2% every 15 minutes and measure the same variables.
Results: patients undergoing cataract surgery with accommodative
lens placement from January to September 2012. Three patients
attended the study, all with placement of accommodative IOLs in
both eyes, six eyes were analyzed. The average age was 60 years, the
average IOLs power was 22.9 diopters.
To analyze the data we search a significant difference between the
measurements obtained at baseline and after application of
pilocarpine. We calculate the mean, median and standard deviation.
Finally data was analyzed using F Fisher statistic method with 5
degrees of freedom and 95% interval confidence looking for a P
value less than 0.05.
Conclusions: Pilocarpine induced no significant changes in the
anterior displacement of the IOLs. Assuming the anterior
displacement of the IOLs provides accommodative capacity,
endothelium lens distance should decrease, however, in this study we
found no correlation between them. Also found no significant
difference between the distance trabecular ciliary body and
iridocorneal angle.
We conclude that pilocarpine does not induce any change in position
of the lens in spite of several studies that reported a change in lens
position using this method, the present study found no significant
difference in the measurement of anterior chamber depth,
iridocorneal angle and trabecular ciliary body distance.
More studies with a larger number of patients and long-term followup is needed to document the loss of motility of the lens over time,
whereas capsular fibrosis is an expected consequence of cataract
surgery, we assume that the accommodative IOLs analyzed in this
study have already presented some type of capsular fibrosis impeding
the proper functioning of the accommodative IOLs.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
eyes, respectively, and in the older eyes the posterior pole of the lens
moved forward during accommodation by -0.08 ± 0.04 mm (n=4).
Over the entire age range for the human subjects, the posterior lens
movement declined by 0.0049 ± 0.0008 mm/year (p=0.001, r=0.86).
Similar results were seen in the phakic monkey eyes. Following
ECLE the capsule bowed backward in all 6 monkeys during
accommodation. In the three monkey eyes in which measurements
were taken, the posterior capsule bowed backward during
accommodation by 0.70 ± 0.03 mm, 0.45 ± 0.02 mm, and 0.26 ± 0.03
mm in the 8-, 17-, and 22-year-old monkeys, respectively.
Conclusions: During accommodation, the vitreous allows a small
amount of posterior movement of the posterior pole of the lens and
allows pronounced backward movement of the capsule following
ECLE, but this posterior accommodative movement declines with
age. These findings may have implications for the mechanism of
accommodation and presbyopia and the function of accommodating
IOLs.
Commercial Relationships: Mary Ann Croft, Seros Medical (R),
Z-Lens LLC (R); Gregg A. Heatley, None; T Michael Nork, None;
Jared P. McDonald, None; Alex Katz, None; Julie Kiland, None;
Paul L. Kaufman, Alcon (C), Allergan (C), Altheos, Inc (C), Bausch
& Lomb (C), Amakem Therapeutics (C), Johnson & Johnson (C),
Lens AR, Inc (F), Merck (C), Pfizer (C), Santen (C), WARF (F), Z
Lens, LLC (F), Alcon (R), Allergan (R), Altheos, Inc (R), Bausch &
Lomb (R), Amakam Therapeutics (R), Merck (R), Pfizer (R), Santen
(F), Santen (R)
Support: Support: NEI (RO1 EY10213 & R21 EY018370 to PLK),
RPB, Grant # 5P51 RR 000167 to WNPRC, OPREF Core Grant for
Vision Research Grant # P30 EY016665.
Commercial Relationships: Diego Chavez, None
Program Number: 386
Presentation Time: 11:45 AM - 12:00 PM
Accommodative Movements of the Lens/Capsule in Relation to
the Vitreous Face and Aging
Mary Ann Croft, Gregg A. Heatley, T Michael Nork, Jared P.
McDonald, Alex Katz, Julie Kiland, Paul L. Kaufman.
Ophthalmology, Univ of Wisconsin-Madison, Madison, WI.
Purpose: To elucidate the accommodative movements of the
posterior lens/capsule in the human eye at various ages in comparison
to the monkey eye before and after extracapsular lens extraction
(ECLE).
Methods: The eyes of 6 rhesus monkeys (aged 8-22 yrs) and 12
human subjects (aged 19-65 yrs) were studied. Maximum
accommodative responses were induced in the human eyes by
pharmacological stimulation (2 drops 4% pilocarpine) and in the
monkey eyes by central electrical stimulation of the EdingerWestphal (E-W) nucleus. Ultrasound biomicroscopy (UBM; 50 MHz,
35 MHz) images were collected in the region of the lens/capsule,
ciliary body, and zonular attachments in both species.
Results: During accommodation in the human eyes, the posterior
pole of the lens moved posteriorly by 0.08 ± 0.01 [mean ± s.e.m.]
mm (n=4) and 0.01 ± 0.03 mm (n=4) in the young and middle-aged
Program Number: 387
Presentation Time: 12:00 PM - 12:15 PM
Accommodative-Disaccommodative IOL with Zonular Capture
Haptics
Paul M. Beer1, 2, Paul L. Kaufman3, Mary Ann Croft3, Gregg A.
Heatley3, Jared P. McDonald3, Alex Katz3. 1Ophthalmology, Z Lens
LLC, Slingerlands, NY; 2Ophthalmology, Albany Medical College,
Albany, NY; 3Ophthalmology, Univ of Wisconsin, Madison, WI.
Purpose: To determine if a single optic accommodativedisaccommodative IOL with Zonular Capture Haptics will exhibit
desirable axial shift and accommodation.
Methods: Single optic, accommodative IOL’s with Zonular Capture
Haptics were manufactured using a 5mm silicone optic from a
commercially available IOL and haptics made from Prolene® suture
material. Two such IOL’s were implanted into two Rhesus monkeys.
The capsular bag was sectioned three weeks post implantation. Two
weeks later UBM and plano perfusion lens imaging was performed in
each animal. One week later the experiments were repeated with
Visante OCT imaging. Accommodation was induced by
pharmacological stimulation with corneal iontophoresis of 40%
carbachol (CARB) in agar; a supramaximal dose for inducing
accommodation.
Results: Pharmacologically stimulated accommodation yielded a
maximum accommodation of 2 and 6 diopters in respectively. In both
animals maximum accommodation was reached 10 minutes after
CARB administration with a rapid return to near baseline refractions
at only 20 minutes.
Both animals had accommodative anterior chamber shallowing as
measured using UBM: 0.33mm(0.39-0.27) at two weeks post
sectioning and OCT 0.54mm(0.65-0.43mm) at three weeks post
sectioning.
Plano perfusion lens imaging revealed a decrease in capsule diameter
during accommodation in both animals of 0.59mm (0.52-0.65mm).
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Conclusions: Zonular Capture Haptic based accommodativedisaccommodative IOL’s demonstrate a useful range of
accommodation and significant axial shift in a first prototype, proof
of concept IOL model.
Conclusions: A significant difference in the number of patients with
high scattered light measurements were observed in the patients with
floaters and no PVD. The exact nature of this difference needs to be
further evaluated. It is possible that only floaters close to the retinal
surface are able to induce a measureable light scattering and be
responsible for the clinical manifestations.
Axial Shift
Commercial Relationships: Paul M. Beer, Z Lens LLC (I), Z Lens
LLC (P); Paul L. Kaufman, Alcon (C), Allergan (C), Altheos, Inc
(C), Bausch & Lomb (C), Amakem Therapeutics (C), Johnson &
Johnson (C), Lens AR, Inc (F), Merck (C), Pfizer (C), Santen (C),
WARF (F), Z Lens, LLC (F), Alcon (R), Allergan (R), Altheos, Inc
(R), Bausch & Lomb (R), Amakam Therapeutics (R), Merck (R),
Pfizer (R), Santen (F), Santen (R); Mary Ann Croft, Seros Medical
(R), Z-Lens LLC (R); Gregg A. Heatley, None; Jared P.
McDonald, None; Alex Katz, None
128 Spatial Vision, Visual Psychophysics and Aging I
Sunday, May 05, 2013 10:30 AM-12:15 PM
Exhibit Hall Poster Session
Program #/Board # Range: 568-586/C0179-C0197
Organizing Section: Visual Psychophysics / Physiological Optics
Contributing Section(s): Eye Movements / Strabismus / Amblyopia
/ Neuro-Ophthalmology
Program Number: 568 Poster Board Number: C0179
Presentation Time: 10:30 AM - 12:15 PM
The effect of posterior vitreous detachment or vitreous opacities
(floaters) on straylight measurements
Miguel Castilla, Marc D. de Smet. MIOS, Lausanne, Switzerland.
Purpose: To evaluate if straylight measures taken in patients with
complaints of floaters (and no posterior vitreous detachment [PVD])
are different from patients presenting with a PVD.
Methods: A retrospective review of patients having undergone a
straylight measurement with a C-Quant (Oculus, Germany) who
presented with a complaint of floaters or observed to have a PVD
when examined but who did not complain of floaters. Data was
collected on age, status of the lens, and only the initial C-Quant
measurement was analyzed if several were taken. Only patients with
intact vitreous were considered in the study. Straylight measurements
were considered significant if they were above 2 standard deviations
[SD] from a normative database, controlled for age.
Results: The mean age for both groups was 58.58 years with an SD
of 12.75 years. Thrity one eyes from 29 patients were included, 11
eyes with a diagnosis of PVD, and 20 eyes with floaters. In the PVD
group, only 5 eyes had measures above the 2 SD cutoff, while 14 of
20 eyes in the floaters group met this criterion. The mean straylight
value for the floaters group was 1.88 with an SD of 1.42 and for the
PVD group of 1.24 with an SD of 0.25. The differences between both
groups did not reach statistical significance (p=0.087).
Commercial Relationships: Miguel Castilla, None; Marc D. de
Smet, Thrombogenics (P), Thrombogenics (C), Sanofi (C), Bayer
(C), Regeneron (C), Preceyes (R), Allergan (C), Janssens (R), GSK
(C), CRL (C)
Program Number: 569 Poster Board Number: C0180
Presentation Time: 10:30 AM - 12:15 PM
Visual findings in children with Autistic Spectrum Disorder
Pamela M. Anketell1, Kathryn J. Saunders1, Stephen M. Gallagher2,
Clare Bailey3, Julie-Anne Little1. 1School of Biomedical Sciences,
University Of Ulster, Coleraine, United Kingdom; 2School of
Psychology, University of Ulster, Coleraine, United Kingdom;
3
Community Child Health, Northern Health & Social Care Trust,
Newtownabbey, United Kingdom.
Purpose: Anomalous visual findings have been described in Autistic
Spectrum Disorder (ASD) including both superior and reduced visual
acuity (VA) (Ashwin et al. 2009, Milne et al. 2009), an increased
prevalence of strabismus (Denis et al. 1997) and reduced near point
of convergence (NPC) (Milne et al. 2009). The aim of this study was
to investigate visual findings in a large population of children with
ASD.
Methods: Children with ASD (n=88, mean age 10.7 years ±3.1
years, range 5-16 years) were recruited from a regional populationbased register (n=67) and special education schools (n=21). ASD
diagnosis was available from the register and classified as; Autism
(AU) n=50, Asperger’s syndrome (AS) n=33, unspecified n=5. Agematched controls were recruited from mainstream schools (n=204,
mean age 11.5 years ±3.1 years).
Monocular recognition crowded VA, presence of strabismus, NPC,
fusional reserves (FR) and Frisby stereoacuity scores were assessed.
Results: Table 1 presents success rates and summary statistics for all
data.
Controls demonstrated slightly but significantly better VA than the
ASD group (Mann Whitney z=-2.49, p<0.05).
A statistically significant higher prevalence of strabismus was noted
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
for the ASD group (6.8%) [AU; 4%, AS; 12.1%] compared with the
control group (1.4%) (Chi-squared χ2(2, 287)=10.76, p<0.01).
NPC was significantly poorer for AU subgroup compared to controls
(Mann Whitney z=3.6, p<0.0005). There was no significant
difference between ASD and control groups in magnitude of FR
(Base out; Kruskal-Wallis=0.02, p=0.99, Base-in; KruskalWallis=1.83, p=0.40).
Analyses of stereoacuity scores identified that control and AS
subgroups achieved significantly better stereoacuity compared to the
AU group (Mann Whitney control; z=2.85 p<0.005, AS; z=3.22
p<0.005).
Conclusions: Children with ASD in the current study have a
different visual profile when compared to controls; including
increased prevalence of strabismus and reduced VA, NPC and
stereoacuity. Whilst statistically significant, these differences in VA,
NPC and stereoacuity may lack clinical relevance. However,
clinicians should be aware of the increased prevalence of strabismus
in this population.
Table 1; success rates and summary statistics for all data
Commercial Relationships: Pamela M. Anketell, None; Kathryn
J. Saunders, None; Stephen M. Gallagher, None; Clare Bailey,
None; Julie-Anne Little, None
Support: NHS R&D Fellowship Grant number EAT/4197/09
Program Number: 570 Poster Board Number: C0181
Presentation Time: 10:30 AM - 12:15 PM
Videogame Experience Enhances Temporal Visual Attention in
Adult Amblyopia: The Attentional Blink in Amblyopia
Charlie V. Ngo1, 2, Truyet Tran2, Calvin Nguyen2, Dennis M. Levi2,
Roger W. Li2. 1Optometry, Baltimore VA Medical Center, Baltimore,
MD; 2School of Optometry, University of California, Berkeley,
Berkeley, CA.
Purpose: Amblyopia causes deficits in spatial and temporal vision.
Our recent findings have shown that videogame training induces a
generalized recovery of spatial visual functions in amblyopic
patients. Here we investigated whether playing videogames enhances
temporal visual attention in adult amblyopia. When visual targets are
presented in rapid succession, correct identification of the first target
can interfere with identification of the second. This second-target
deficit is known as the attentional blink. This phenomenon has often
been explained on the basis of an “attentional bottleneck” (i.e., a
processing stage that can handle only one item at a time). Amblyopes
show an abnormal attentional blink with their amblyopic eye.
Methods: We measured the attentional blink in each eye of 11 adults
with amblyopia, before and after 40 hours of videogame play, using a
rapid serial visual presentation (RSVP) technique. The observer had
two tasks: (1) To identify a white letter (T1) randomly positioned in a
temporal sequence of black letters and (2) to detect the presence of a
black letter “X” (T2), which was presented in half of the trials at a
random temporal position after T1 (lag=1-8; lag 1: “X” was the first
letter to appear after T1; each letter frame was 100 ms). Additional
random letters were added to the end of the sequence.
Results: Prior to videogame play the shape of the mean baseline
attentional blink curve (probability of correct T2 report vs time after
T1) of the amblyopic eyes was slightly shallower than that of the
fellow preferred eyes, as reported by Popple & Levi, 2008). After 40
hours of videogame play, we observed a 22% improvement
(reduction) in the attentional blink (identifying T2 200 ms after T1)
seen through the amblyopic eye.
Conclusions: Our findings suggest that videogame play improves
temporal visual attention in adult amblyopia. Importantly, this
videogame training technique might be useful in combination with
other vision therapy regimens and induce visual plasticity in cortical
visual disorders.
Commercial Relationships: Charlie V. Ngo, None; Truyet Tran,
None; Calvin Nguyen, None; Dennis M. Levi, None; Roger W. Li,
None
Support: NIH Grant R01EY01728
Program Number: 571 Poster Board Number: C0182
Presentation Time: 10:30 AM - 12:15 PM
Suppression of the Implicit Surface
Susan Kelly, Yi Pang. Basic Science, Illinois College of Optometry,
Chicago, IL.
Purpose: A number of authors have reported that human observers
can accurately judge the physical distance of visual targets if they are
located on a flat ground surface. The correlation between distance
judgments measured with the blind-walking technique correlate
highly with a target’s physical distance in lighted conditions.
However distance judgments of self-illuminated targets in darkness
are very inaccurate.
Ooi and colleagues have proposed that in both darkness and light,
observers judge an object’s distance as the intersection between its
angle of declination and the perceived slant of the ground surface.
They report that in darkness the human visual system relies on a
default ground surface called the implicit surface that tilts upwards
towards the horizon with a slant of around 12 deg.
Our experiments have revealed another aspect of this implicit
surface; it is triggered by the absence of light in the visual field and
suppressed by the presence of light in the visual field.
Methods: Forty-five visually normal young adults observed a small
self-illuminated target in darkness. Subjects were instructed to blindwalk to the remembered location of the target under one of the
following conditions: 1) blind-walk in darkness (n=28); 2) blind-walk
in presence of white light (n=10) and 3) blind-walk in presence of red
light (n=7).
Results: The blind-walking estimates of a target’s distance are much
more accurate if the blind-walking takes place in a lighted room
versus a dark room (F=18.85, p<0.001) even though in both cases
subjects are blind-folded when walking; the only difference between
these conditions is the presence or absence of light in the visual field.
Pair-wise comparison showed no difference in estimates made in
white versus red room illumination (p=0.21) but both differed
significantly from the dark condition (p<0.01).
Conclusions: The distance perception of targets viewed in darkness
is dramatically affected by the presence or absence of room lighting;
when subjects blind-walk to the remembered target location in
darkness they rely on the implicit surface and their distance estimates
are inaccurate. However, if they blind-walk to the remembered target
location with room illumination present then there is no default to the
implicit surface and distance perceptions are accurate. Neither the
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
photoreceptors nor the neural pathway responsible for suppressing
the implicit surface are known.
Commercial Relationships: Susan Kelly, None; Yi Pang, None
Program Number: 572 Poster Board Number: C0183
Presentation Time: 10:30 AM - 12:15 PM
Postural adaptation to large optic flow fields
Guillaume L. Giraudet1, 2, Clementine Faron1, Jocelyn Faubert1.
1
Psychophysics & Visual Perception Lab, Universite de Montreal,
Montreal, QC, Canada; 2ESSILOR Canada, Montreal, QC, Canada.
Purpose: The aim of the current study was to determine the effect of
visual adaptation for contracting and expanding optic flow on
postural stability.
Methods: Twelve subjects participated in the experiment. They stood
in a fully immersive virtual reality environment. The stimulus was a
3D textured tunnel, either static or moving forward (expansion) or
backward (contraction) at 3 different speeds: 0.275, 1.1 and 4.4 m/s.
Each trial was composed of 3 stages. The first one was called
“Baseline”, during which the tunnel was static. It lasted 2 seconds.
Then the stimulus started to move forward or backward for 10, 20 or
40 seconds; “Adaptation” stage. For the third, “post-adaptation” stage
the stimulus suddenly halted and remained static for 15s. Optical
motion sensors, located on the stereoscopic goggles, were used to
track and register body movements. Behavioral reactions to the
various visual conditions were described by comparing postural
stability between the 3 different stages described above.
Results: Results showed that subjects get adapted to the expansion
optic flows by increasing their postural stability. The longer the
adaptation stage lasted, the more body movements were reduced. A
similar stabilization effect was observed when movement speed
increased. However, we did not measure any adaptation for the
contraction optic flow. In this direction, postural behavior remained
constant during the whole sequence, that is, during all 3 different
stages of presentation and for all moving scene speeds.
Conclusions: The current study confirms that expansion and
contraction optic flows are processed differently and have different
impacts on visuomotor systems. Several neurophysiological and
imaging studies reported an expanding motion bias represented as
greater activation in motion sensitive cortical areas than for
contraction optic flow (Ptito, Kupers, Faubert, Gjedde, 2001). Our
results highlight that, in the context of visually guided actions, the
control of body posture changes when the properties of the expanding
optic flow are modified but it does not respond to properties of
moving scenes in contraction.
Commercial Relationships: Guillaume L. Giraudet, ESSILOR
Canada (E); Clementine Faron, None; Jocelyn Faubert, Université
de Montréal (P)
Support: CRSNG-ESSILOR Industrial Chair
Program Number: 573 Poster Board Number: C0184
Presentation Time: 10:30 AM - 12:15 PM
Measurement of stimulus contrast and fading under natural and
manipulated motion trajectories
Nicole M. Putnam1, 2, Pavan Tiruveedhula2, Austin Roorda2. 1Arizona
College of Optometry, Midwestern University, Glendale, AZ;
2
School of Optometry, University of California, Berkeley, Berkeley,
CA.
Purpose: High-resolution imaging with Adaptive Optics Scanning
Laser Ophthalmoscopy (AOSLO) combined with real-time image
stabilization and targeted stimulus delivery allows simultaneous
imaging and psychophysical testing. We utilize this capability to
investigate the role of small fixational eye movements, or the lack
thereof, on stimulus contrast and fading.
Methods: Image stabilization and targeted stimulus delivery with
AOSLO facilitates the presentation of any stimulus motion including
natural, stabilized, amplified, rotated, or independent trajectories. We
first investigated the threshold for detection of a small grating that
increased in contrast over the course of a 6 second trial at the fovea
and 1 degree eccentricity. Subjects performed a 2 AFC judgment of
grating orientation as soon as they were able to make a judgment. We
recorded the contrast level at the time the decision was made under
natural, stabilized and manipulated eye motion conditions. We then
looked at the time-course of image fading for small stimuli near the
fovea. Subjects fixated the corner of the imaging raster and a small
100% contrast grating appeared at a random location within the field.
Subjects pressed one button when the stimulus was no longer visible
and pressed another if the 9 second trial concluded with no image
fading. We measured the time the stimulus was visible and the
percentage of trials where the stimulus was visible for the entire trial
for natural, stabilized, and manipulated eye motion conditions.
Results: We find that the contrast required to detect a stimulus that
was ramping up in contrast over a 6 second trial was the highest
under stabilized conditions at both locations tested. The conditions
under which thresholds were smallest, however, depended on the
retinal location. At the fovea, the thresholds were at a minimum for
natural stimulus motion whereas at 1 deg, the minimum threshold
occurred with amplified motion (double the retinal slip). For the
fading experiments, we found that the time required for an image to
fade was shortest under stabilized conditions and that there were no
instances where the stimulus did not fade in the 9-second trials for
three subjects.
Conclusions: Our results suggest that the sensitivity of foveal cones
is optimal for natural image motion caused by fixation. However, as
close as 1 degree, contrast sensitivity is improved when the retinal
image motion is amplified.
Commercial Relationships: Nicole M. Putnam, None; Pavan
Tiruveedhula, None; Austin Roorda, US Patent #6890076 (P), US
Patent #7118216 (P), UC Berkeley (P)
Support: EY014375 and AOF William C. Ezell Fellowship
Program Number: 574 Poster Board Number: C0185
Presentation Time: 10:30 AM - 12:15 PM
Dynamic stimulus presentation facilitates peripheral resolution
acuity
Peter R. Lewis, Victoria Holm, Karthikeyan Baskaran, Jorgen
Gustafsson. Section of Optometry and Vision Science, Linnaeus
University, Kalmar, Sweden.
Purpose: Peripheral high-contrast resolution is sampling limited; the
center to center spacing between ganglion cells ultimately limiting
visual performance (Thibos et al., 1987). Although retinal image
motion in the fovea has a detrimental effect on visual acuity, previous
studies have suggested that retinal image motion may be
advantageous in the peripheral visual field (Bex et al., 2003; Brown,
1972; Macedo et al., 2010). The aim of this study was to evaluate the
effect of drift motion on peripheral resolution acuity.
Methods: Peripheral high-contrast resolution acuity in a group of 26
subjects (age 23.5 ± 3.2 years) was initially determined using a 2alternative forced-choice Bayesian algorithm; the threshold value
defined as the spatial frequency resulting in a 75% correct response
rate. The stimuli used to measure static visual acuity were stationary
Gabor-patches with a visible diameter of 2° and were presented at
20° in the nasal visual field. We determined the percentage correct
response rate for varying velocities using drifting Gabor patches of
the same spatial frequency as determined during measurement of
static visual acuity. The sine-wave gratings drifted within the
Gaussian envelope at one of 10 angular velocities, varying from 0.2
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
to 2.0 degrees/second in 0.2 degrees/second steps.
Results: Results showed an overall improvement in the subjects’
performance for all velocities. There was a significant difference in
the percentage of correct responses between static stimulus
presentation and for velocities of between 0.4 to 1.2 degrees/second
(p < 0.05, One-way repeated measures ANOVA with Bonferroni post
hoc tests). The average “correct response” for static stimulus
presentation was 76 ± 2 %, improving to at least 85 % for velocities
between 0.4 to 1.2 degrees/second. At velocities greater than 1.2
degrees/second performance was still better than for static stimulus
presentation, but showed a gradual decline with increasing speed.
Conclusions: In line with previous studies stimulus motion has a
positive effect on peripheral high-contrast resolution acuity.
Presenting moving stimuli may benefit patients who rely on
peripheral visual function, such as those with central visual field loss
subsequent to AMD.
Commercial Relationships: Peter R. Lewis, None; Victoria Holm,
None; Karthikeyan Baskaran, None; Jorgen Gustafsson, None
Program Number: 575 Poster Board Number: C0186
Presentation Time: 10:30 AM - 12:15 PM
Distance Visual Acuity Screening of Preschoolers with Hyperopia
Marjean T. Kulp1, Gui-Shuang Ying2, Jiayan Huang2, Maureen G.
Maguire2, Graham E. Quinn3, Elise Ciner4, Deborah A. Orel-Bixler5,
Lynn A. Cyert6, Bruce Moore7. 1College of Optometry, Ohio State
University, Columbus, OH; 2University of Pennsylvania,
Philadelphia, PA; 3Children’s Hospital of Philadelphia, Philadelphia,
PA; 4Pennsylvania College of Optometry, Salus University, Elkins
Park, PA; 5School of Optometry, University of California, Berkeley,
CA; 6College of Optometry, Northeastern State University,
Tahlequah, OK; 7New England College of Optometry, Boston, MA.
Purpose: Hyperopia has been shown to be associated with an
increased risk of amblyopia and strabismus among preschoolers. The
purpose of this study is to compare uncorrected distance visual acuity
(VA) measured with the VIP Crowded Single LEA Symbols® VA
Test at 5 feet (VIP 5ft Lea) in 3- to 5-year-old Head Start children
with versus without hyperopia.
Methods: In VIP (Phase II), 1452 preschoolers were screened with
the VIP 5ft Lea test by lay screeners. All children underwent
comprehensive vision examination including threshold VA using the
ATS single-surround HOTV letter protocol, cover testing, and
cycloplegic retinoscopy by masked examiners. Hyperopia was
defined as >+3.25D in the most positive meridian in one or both eyes.
Uncorrected distance VA in the worse eye as measured by the VIP 5
ft Lea was compared for 1) children with hyperopia and those
without and 2) children with hyperopia plus other visual conditions
(amblyopia, strabismus, astigmatism, and/or anisometropia), those
with hyperopia alone, and those without hyperopia.
Results: Uncorrected distance VA measured with the VIP 5ft Lea
test was significantly different between children with hyperopia
(n=182, median VA 20/50) as compared to those without hyperopia
(n= 1270, median VA 20/40)(p<0.0001). Uncorrected distance VA
was also significantly different when compared among children with
hyperopia plus other visual conditions (n=111, median VA 20/200),
those with hyperopia alone (n=71, median VA 20/50), and those
without hyperopia (p<0.0001 for comparison among the 3 groups,
p=0.02 for comparison between children with hyperopia alone versus
no hyperopia).
Conclusions: Uncorrected distance visual acuity, measured with the
VIP 5ft Lea test, is significantly lower in children with versus without
hyperopia, even when not associated with other visual conditions.
Commercial Relationships: Marjean T. Kulp, None; Gui-Shuang
Ying, None; Jiayan Huang, None; Maureen G. Maguire, Inspire
Pharmaceuticals (F), Amakem (F), IDx LLC (F), Merck (C);
Graham E. Quinn, None; Elise Ciner, None; Deborah A. OrelBixler, None; Lynn A. Cyert, None; Bruce Moore, EyeNetra Inc.
(I)
Support: NEI/NIH, DHHS grants: U10EY12644; U10EY12547;
U10EY12545; U10EY12550; U10EY12534; U10EY12647;
U10EY12648 and R21EY018908
Program Number: 576 Poster Board Number: C0187
Presentation Time: 10:30 AM - 12:15 PM
Comparison of foveal and perifoveal acuity in myopia
Stephanie X. Shao, Nancy J. Coletta. New England College of
Optometry, Boston, MA.
Purpose: Visual acuity and cone density both decrease at parallel
rates with increasing myopia (Coletta and Watson, Vis. Res., 2006;
Chui et al., IOVS, 2008). Young adult eyes with refractions less than
3D are reported to have relatively lower perifoveal cone density when
the foveal cone density is high, implying that foveal specialization
involves greater migration of perifoveal cones to the foveal area
(Elsner et al., ARVO 2012). We compared perifoveal and foveal
acuity in a group of young adult subjects with the aim of determining
whether higher foveal acuity was associated with relatively lower
perifoveal acuity and if this relationship was affected by the degree of
myopia.
Methods: The subjects (n=33) had a mean age of 24.4 years +/- 1.8
s.d. Refractive errors ranged from +0.25 D to -8.88 D with a mean of
-3.04 D and axial lengths, measured with a Zeiss IOL Master, ranged
from 22.5 to 26.7 mm with a mean of 24.3 mm. Acuity was measured
with 543nm laser interference fringes displayed in a 2 deg patch at
the fovea and at 7° eccentricity in the temporal, nasal, superior and
inferior retinal meridians. Acuity was expressed in cycles per mm on
the retina, adjusted by the axial lengths.
Results: Foveal and perifoveal acuity both decreased with increasing
myopia, significantly at the fovea (p=0.0004). The perifoveal to
foveal acuity ratio was on average 0.40 on the horizontal meridian
and 0.28 on the vertical meridian. Perifoveal acuity in each retinal
meridian increased with foveal acuity when all subjects were
included. On the nasal retinal meridian, however, there was a
negative correlation between perifoveal acuity and foveal acuity that
was evident only for refractions in the range of -1.00 to -6.00 D.
Conclusions: A comparison of perifoveal and foveal acuity in young
adults over a range of refractive errors indicates that acuity in the
fovea and perifovea are generally positively correlated. However, in
subjects with low to moderate myopia, perifoveal acuity on the nasal
meridian decreased with increasing foveal acuity, implying that
myopia may affect the relative cone density distribution on the nasal
side of the fovea.
Commercial Relationships: Stephanie X. Shao, None; Nancy J.
Coletta, None
Support: NIH grants R24 EY014817 and T35 EY007149
Program Number: 577 Poster Board Number: C0188
Presentation Time: 10:30 AM - 12:15 PM
iPad-Based Quick CSF Implementation to Assess Effects of
Dioptric Blur on Contrast Sensitivity
Michael Dorr1, Luis A. Lesmes1, Zhong-Lin Lu2, Peter Bex1.
1
Schepens Eye Research Institute, Harvard Medical School, Boston,
MA; 2Department of Psychology, Ohio State University, Columbus,
OH.
Purpose: The quick CSF method is a novel adaptive method
developed to rapidly estimate features of the contrast sensitivity
function, including i) peak contrast sensitivity; and ii) CSF acuity, the
high-frequency cutoff that corresponds to a contrast threshold of 50%
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
(sensitivity=2). It has been demonstrated that CSF acuity estimates
correlate well with logMAR acuity (Lesmes LA, et al. IOVS
2012;52:ARVO E-Abstract 4358).
Because acuity is an important criterion for choosing optical
correction, we investigated how dioptric blur affects CSF acuity
estimates obtained with the quick CSF, implemented on an iPad for
convenience.
Methods: Six observers (21-46 yrs old; mean 27.5) were tested at a
viewing distance of 40cm. Tests were run at self-reported correction
and additional blur conditions (+1,+2,+3,+4D). Gratings of different
frequencies (.29-18.5cpd) and contrasts (.2-100%) were presented for
250ms at 3.4deg either left or right of fixation (spatial 2AFC) and
subjects used the touch screen to respond. Each test (120 trials) lasted
3-4 min. To estimate repeatability, all conditions were run again the
following day.
Results: As expected, dioptric blur primarily affected the CSF's highfrequency region, and not its peak height (Fig 1). When normalized
to the lens condition with maximum acuity, CSF acuities exhibited a
sharp decrease across lens conditions that was not demonstrated by
peak sensitivity (Fig 2). Although contrast thresholds measured on
digital displays often exhibit ceiling effects, we reliably obtained
peak thresholds <1% for 5 subjects.
Test reliability was calculated from the coefficient of variation for
difference scores between first and second tests; for peak sensitivity,
this was <12% after 30 trials, <6.2% after 60, and <3.8% after 90 and
120 trials. These values for CSF acuity are <16%, <14.4%, <10%,
and <7%, respectively.
Conclusions: These results confirm that dioptric blur affects high
frequencies more than the peak and lower frequency regions of the
CSF. The main contribution of the current study is the use of a
portable tablet device, and algorithms to extend contrast resolution
(>8bits), to rapidly and reliably measure features of the contrast
sensitivity function.
Example CSFs obtained from one subject; each curve describes the
average of two runs at a fixed dioptric blur.
Average relative CSF acuity and peak sensitivity, normalized to the
maximum acuity condition.
Commercial Relationships: Michael Dorr, Adaptive Sensory
Technology, LLC (S), Rapid Measurement of Visual Sensitivity (P);
Luis A. Lesmes, Adaptive Sensory Technology (S), 7938538 (P);
Zhong-Lin Lu, US Patent 7,938,538 (P); Peter Bex, Adaptive
Sensory Technology, LLC (S), Rapid Assessment of Visual
Sensitivity (P)
Support: Supported by NIH EY018664, EY019281 (MD, LAL, and
PB), and EY017491 (ZLL)
Program Number: 578 Poster Board Number: C0189
Presentation Time: 10:30 AM - 12:15 PM
Repeatability of Visual Acuity with a Chart Having Lines of
Equivalent Legibility
Lawrence R. Stark, Scot A. Class. Southern California College of
Optometry, Fullerton, CA.
Purpose: To determine if differences in legibility between the ten
letters of the British standard (BS) set contribute to variability in
visual acuity (VA).
Methods: Intra-session test-retest repeatability of best-corrected VA
was assessed in 68 visually-normal young adults under bright
photopic conditions. Threshold VA was determined with custom
Bailey-Lovie charts (five letters per line) in two conditions in random
order: (1) Non-Paired Condition. Presentation of two letter charts
having non-matched letter legibility across lines. The five letters on
each line in a single chart were chosen randomly without replacement
from the BS set; and (2) Paired Condition. Presentation of paired
letter charts having matched letter legibility across lines. In these
chart pairs, each of the ten BS letters appeared exactly once for a
given line size across the two charts of a pair.
Results: The 95% limits of agreement for test-retest repeatability
were ±0.053 log MAR for the Non-Paired condition, and ±0.075 log
MAR for the Paired condition. Repeatability was not significantly
better in the Paired condition (Brown-Forsythe test, one-tailed, p =
.97). When three outlying points were removed (> ±3 s.d.), the
finding did not change substantially (n = 65, p = .82).
Conclusions: When visual acuity is based on the average of two
chart presentations (each with five letters per line), differences in
letter legibility in the British Standard set do not have a significant
effect on the repeatability of visual acuity.
Commercial Relationships: Lawrence R. Stark, None; Scot A.
Class, Nationwide Vision Center (E)
Program Number: 579 Poster Board Number: C0190
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Presentation Time: 10:30 AM - 12:15 PM
The Effect of Exposure Duration on Visual Acuity for Letter
Optotypes Depends On How Visual Acuity is Defined
J Jason McAnany, Philip R. Nolan, Aimee Beluch. Ophthalmology
and Visual Sciences, University of Illinois at Chicago, Chicago, IL.
Purpose: Increasing exposure duration improves visual acuity (VA)
for letter optotypes, as defined by the standard logarithm of the
minimum angle of resolution (log MAR) scale. This study
determined the extent to which VA, expressed in terms of retinal
frequency (cycles per degree; cpd), improves with increasing
duration after accounting for the object frequency information
mediating performance (cycles per letter; cpl).
Methods: Log MAR VA of four visually-normal individuals (ages
25 to 35) was measured for a set of tumbling E optotypes presented
on a CRT display for presentation durations ranging from 0.02 to 1.0
s. The Es were either unblurred or blurred through convolution with
Gaussian functions of different widths (σstim), which permitted object
frequency to be derived. Log MAR values were plotted as a function
of log σstim and fit with the function: MAR = MAR0[1 + (σstim/
σint)2]0.5, where MAR0 and σint set the vertical and horizontal
positions of the function, respectively. The object frequencies
mediating VA were derived from MAR0 and σint as: cpl =
5*MAR0*1/(2π*σint). The retinal frequencies mediating VA were
derived from MAR0 and cpl as: cpd = 12*cpl/ MAR0.
Results: Log MAR for the unblurred E decreased (VA improved)
significantly (p < 0.05) by a factor of 1.6 as duration was increased
from 0.02 to 0.50 s, but log MAR was constant for durations longer
than approximately 0.50 s. These findings are consistent with
previous reports. Increasing the exposure duration had similar effects
on log cpl, a relationship that has not been reported previously. That
is, from 0.02 to 0.50 s, cpl decreased significantly (p < 0.05) by a
factor of approximately 1.6, and was constant for longer durations.
However, VA expressed in cpd was independent of exposure
duration. This constancy is due to the offsetting effects of the
decrease in letter size (increase in cpd) and the decrease in cpl
(decrease in cpd), as indicated in the definition of retinal frequency.
Conclusions: The extent to which VA for broadband optotypes
improves with increasing exposure duration depends on how VA is
defined. If it is assumed that object frequency is independent of
duration (i.e. the log MAR scale), then VA improves as duration is
increased up to approximately 0.50 s. However, if both size and
object frequency are included in the definition of VA (i.e. cpd), then
VA is approximately independent of duration.
Commercial Relationships: J Jason McAnany, None; Philip R.
Nolan, None; Aimee Beluch, None
Support: NIH research grant R00EY019510 (JM), NIH core grant
P30EY001792, and an unrestricted departmental grant from Research
to Prevent Blindness.
Program Number: 580 Poster Board Number: C0191
Presentation Time: 10:30 AM - 12:15 PM
Assessing the Quality of Functional Vision through AdSpecs
Nadine Solaka1, Hilary Gaiser1, Joshua Silver2, Bruce Moore1. 1New
England College of Optometry, Boston, MA; 2Center for Vision in
the Developing World, Oxford University, Oxford, United Kingdom.
Purpose: According to the RESC Studies, at least 10% of children in
the developing world could benefit from refractive correction. Lack
of professional eyecare limits access to refractive correction.
Adjustable glasses (AdSpecs) both measure and correct refractive
error. A previously published study showed that AdSpecs provide
clear vision when adjusted by myopic children. However, it remained
uncertain whether this complex lens system may adversely effect
visual function, especially at near. The purpose of this study was to
assess near visual function through AdSpecs.
Methods: 30 myopic adults 21-41 years of age were recruited from
New England College of Optometry. Near VA was measured in Munits using a Good-Lite (#251000) near card at 40 cm. Contrast
sensitivity (CS) was measured using a Mars Test (mars perceptrix) at
50 cm. Lateral and vertical phoria were measured with Modified
Thorington at 40 cm. All tests were done in down gaze (45° from
primary gaze) with both AdSpecs and habitual correction (HC).
Inclusion criteria were: Hyperopia +1.50 to +4.50 D, Myopia -0.75 to
-6.00 D, Astigmatism <2.00 D, Anisometropia <1.00 D and VAcc
≥20/25 in each eye.
Results: Near VA mean for OD was 1.08M ± 0.16M with HC and
0.99M ± 0.20M with AdSpecs (mean diff.: 0.09M, p-value: 0.02). CS
mean for OD was 1.76 ±0.07 with HC and 1.77 ±0.05 with AdSpecs
(mean diff.: -0.01, p-value: 0.62). Lateral phoria mean was -3.57PD
(Exo) ±4.74PD with HC and -3.48PD (Exo) ±5.15PD with AdSpecs
(mean diff.: -0.09PD (Exo), p-value: 0.79). Vertical phoria mean was
0.02PD (RHyper) ±0.43PD with HC and -0.08PD (RHypo) ±0.47PD
with AdSpecs (mean diff.: 0.1PD (RHyper), p-value: 0.25).
Conclusions: Near VA was slightly reduced through AdSpecs. This
may be due to the AdSpec's complex lens design. Multiple lens
surfaces result in reflection and reduced light transmission. CS and
phoria were similar between AdSpecs and HC . The small difference
in phoria is likely due to the preset pupillary distance on the
AdSpecs, resulting in some subjects with induced prismatic effect
exacerbated by the complex lens system. Future designs with reduced
lens thickness are underway.
Despite small statistical differences, the overall results of each of the
variables (near VA, contrast sensitivity and phoria) were not
clinically significantly different between the AdSpecs and HC. These
results help answer the question about the quality of functional vision
through these adjustable glasses.
Commercial Relationships: Nadine Solaka, None; Hilary Gaiser,
None; Joshua Silver, Centre for Vision in the Developing World (E),
Adaptive Eyecare Ltd (I), Adlens Ltd (I); Bruce Moore, EyeNetra
Inc. (I)
Program Number: 581 Poster Board Number: C0192
Presentation Time: 10:30 AM - 12:15 PM
Neural substrates of perceptual integration during bistable object
perception
Anastasia V. Flevaris1, 2, Antigona Martinez2, 3, Steven Hillyard2.
1
Department of Psychology, University of Washington, Seattle, WA;
2
Department of Neurosciences, University of California, San Diego,
San Diego, CA; 3Nathan Kline Institute, New York, NY.
Purpose: Object perception depends not only on physical stimulus
properties but also on endogenous, top-down factors that affect the
observer’s perceptual state. In this study we equated physical
properties to investigate the neural mechanisms of top-down
contributions in object perception.
Methods: We recorded EEG and compared neural activity elicited by
varying perceptions of the same physical image - a bistable moving
image in which perception spontaneously alternates between
dissociated fragments and a single, unified object.
Results: A time-frequency analysis of EEG changes associated with
the perceptual switch from object to fragment and vice versa revealed
a greater decrease in alpha band (8-12Hz) power accompanying the
switch to object-percept than to fragment-percept. Recordings of
event-related potentials elicited by irrelevant probe flashes
superimposed on the image revealed an enhanced positivity in the
latency range of the P2 component (~184-212ms) when the probes
were contained within the perceived unitary object. The topography
of this positivity elicited by probes during object- relative to
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
fragment-perception was distinct from the topography of the P2
elicited by probes during fragment perception, suggesting that neural
processing of probes differed as a function of perceptual state. Two
source localization algorithms estimated the neural generator of the
difference positivity to lie in the lateral occipital cortex (LOC), a
region associated with object perception.
Conclusions: These data suggest that objects attract attention and
modulate the processing of individual elements occurring within their
boundaries, perhaps reflecting the perceptual binding of the elements
into a unified object. Importantly, these effects were observed when
the perceived "object" in this case emerged as a function of the
fluctuating perceptual state of the viewer.
Commercial Relationships: Anastasia V. Flevaris, None;
Antigona Martinez, None; Steven Hillyard, None
Support: T32 MH 020002-11A1
Program Number: 582 Poster Board Number: C0193
Presentation Time: 10:30 AM - 12:15 PM
Digital precise remote near visual acuity evaluation using mobile
devices
Oren Yehezkel, Anna Sterkin, Maria Lev, Uri Polat. Ucansi Inc., New
York, NY.
Purpose: Our aim was to develop a tool for precise remote selfassessment of near visual acuity in order to accurately and remotely
estimate the functional reading acuity.
Methods: We used an application by Ucansi Inc., developed for iOSbased mobile devices (iPhone, iPad, iPod), based on the technology
tested both on mobile devices and PCs (electronic visual acuity,
eVA). Here we present part of the data, collected on 73 volunteers
that were tested on iPhone 4, operating the application by themselves.
The minimal measurable acuity is -0.18 logMAR, as determined by
the pixel size of 0.078 mm. The stimuli were matrices composed of
25 letters "E" (5×5), each with a randomly chosen orientation out of 4
possibilities (left, right, up or down). Two variations of inter-letter
spacing within the matrix were used (0.4 and 1 letter size). The task
was to report the orientation of the central letter. The evaluation was
performed using a staircase measuring the minimal detectable target
size. For each staircase, the duration of target presentation (ranging
between 240 to 30 msec) and the inter-letter spacing were changed.
The results were compared to the standard clinical near visual acuity
chart (ETDRS chart-based visual acuity, cVA) and to the required
reading addition (measured using the fused cross-cylinder test, FCC).
Results: There was a significant correlation between the eVA and the
cVA. Best correlation was found between monocular eVA and cVA
(R=0.85, p<0.01; eVA: mean of 0.34±0.02 logMar, ranging between
-0.09 and 0.73; mean of 0.32±0.02; cVA: ranging between -0.04 and
0.72). There was also a significant correlation with the FCC
measurement (R=0.73, p<0.01; mean of 1.58±0.07, ranging between
0 and 2.75).
Conclusions: The remote self-assessment of near visual acuity using
the iOS-based application is very accurate and may better predict the
functional visual acuity due to the brief stimuli presentation similar in
duration to a single fixation between saccades during reading.
Moreover, measurements under the conditions of letter crowding
induced by the letter matrix used by the application better estimate
the functional reading acuity as opposed to single letter detection
used in reading chart measurements. The assessment may be
performed both monocularly and binocularly. Finally, VA
improvement measured with eVA was highly correlated to the
improvement measured by cVA.
Commercial Relationships: Oren Yehezkel, Ucansi Inc. (E); Anna
Sterkin, Ucansi Inc. (E); Maria Lev, Ucansi Inc. (E); Uri Polat,
Ucansi Inc. (I)
Program Number: 583 Poster Board Number: C0194
Presentation Time: 10:30 AM - 12:15 PM
The Handy Eye CheckTM: A Mobile Medical Application for
Testing Vision in Children
Amy K. Hutchinson1, Keri Stalun1, Michael J. Lynn2, T R. Candy3.
1
Ophthalmology, Emory University School of Medicine, Atlanta,
GA; 2Biostatistics and Bioinformatics, Emory University School of
Medicine, Atlanta, GA; 3Indiana University School of Optometry,
Atlanta, GA.
Purpose: The Handy Eye ChartTM uses hand gesture symbols as
optotypes and is a valid test of visual acuity in children age 6 to 18
years.1 Modifications are needed to improve testability in younger
children. The goal of this study was to develop an electronic version
of the chart.
Methods: We developed an iPad application (the Handy Eye
CheckTM) to test visual acuity by presenting isolated Handy Eye
ChartTM optotypes with crowding bars according to the Amblyopia
Treatment Study (ATS) protocol. Validity and reliability of the
Handy Eye CheckTM were determined by comparing results with the
previously validated chart and assessing test-retest results.
Results: The poorest seeing eye of 61 children aged 6-18 years was
tested. Visual acuity ranged from -0.1 to 1.0 logarithm of the minimal
angle of resolution (logMAR). There was a strong linear correlation
(r = .92) and a mean difference in acuity of -0.005 (less than one
letter) (95% CI -0.03 to 0.02) logMAR, between the two tests. The
95% limits of agreement were ± 2 lines. Test-retest reliability was
high, with 81% of retest scores within 0.1 logMAR (5 letters) and
100% within 0.2 logMAR (10 letters), an intraclass correlation
coefficient of 0.93, and a standard error of measurement of 0.08.
Conclusions: : Validity and reliability testing of the Handy Eye
CheckTM compares favorably to other pediatric acuity tests2 and to
other studies of electronic testing protocols in children3The Handy
Eye CheckTM is a valid and reliable test of visual acuity in children
age 6-18 years.
References:
1. Cromelin CH, Candy RT, Lynn MJ, Harrington CL, Hutchinson
AK. The Handy Eye ChartTM: A New Visual Acuity Test for Use in
Children. Ophthalmology 2012;119(10):2009-2013.
2. Vision in Preschoolers (VIP) Study Group. Visual acuity results in
school-aged children and adults: Lea Symbols chart versus BaileyLovie chart. Optom Vis Sci 2003;80:650 - 4
3. Cotter S, Chu RH, Chandler DL et al. Reliability of the electronic
early treatment diabetic retinopathy study testing protocol in children
7 to < 13 years old. AJO 2003;134(4);655-661.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Isolated optotypes presented with crowding bars
The Handy Eye ChartTM
Commercial Relationships: Amy K. Hutchinson, Emory
University (P); Keri Stalun, None; Michael J. Lynn, None; T R.
Candy, None
Support: Atlanta Pediatric Device Consortium
Program Number: 584 Poster Board Number: C0195
Presentation Time: 10:30 AM - 12:15 PM
Influence of glare light on contrast sensitivity through absorptive
lenses
Hiroshi Uozato1, 2, Masatsugu Kanazawa1. 1Ophthalmology/Visual
Science, Kitasato Univ Grad Sch of Med Sci, Sagamihara, Japan;
2
Orthoptics and Visual Science, Kitasato University School of Allied
Health Sciences, Sagamihara, Japan.
Purpose: To investigate the influence of glare light in peripheral
visual field on the contrast sensitivity (CS) through absorptive lenses
under photopic and mesopic vision.
Methods: The subjects were 13 healthy volunteers and accepted CS
measurement. Its measurement was performed to use a contrast glare
tester, CGT-2000 (TAKAGI SEIKO), under photopic (background
brightness: 100 cd/m2) and mesopic vision (background brightness:
10 cd/m2). Intensities of glare light which was indicated on 12° were
glare M (brightness: 40,000 cd/m2) or glare H (brightness: 100,000
cd/m2). Binocular CS without glare light was compared with glare M
and glare H. The effect of absorptive lenses was analyzed for
wavelength component: cone’s peak wavelength value through
absorptive lenses. We defined S-, M- and L- cone’s peak wavelength
value as S-, M- and L- wavelength components and calculated
correlation coefficients between contrast sensitivity and wavelength
components. Absorptive lenses were RETINEX (HOYA, CO.,
JAPAN) with 5 colors: Orange - Brown (OB: luminous transmittance
(LT), 12%), Orange (OR: LT, 49%), Red (RE: LT, 33%), Yellow
(YE: LT, 77%), Yellow - Brown (YB: LT, 29%).
Results: Compared with CS without glare light, there was no change
between CS with glare light under photopic vision. CS, however,
decreased with glare H under mesopic vision (ANOVA, Scheffé, p <
0.05). In the analysis of a correlation coefficient, L and M
wavelength components effectively contribute to contrast sensitivity
under photopic vision. Correlation coefficients of each wavelength
component showed almost the same values under mesopic.
Conclusions: We suggest that binocular CS decreases in the case of
the highest intensity of glare light in peripheral visual field under
mesopic vision. Absorptive lenses are especially useful in daylight
because color lenses which absorb short-wavelength hardly affect CS
under photopic vision.
Commercial Relationships: Hiroshi Uozato, None; Masatsugu
Kanazawa, None
Support: Grant from Kitasato Univ. School of Allied Health
Sciences No.2012-1013
Program Number: 585 Poster Board Number: C0196
Presentation Time: 10:30 AM - 12:15 PM
Novel method to objectively evaluate visual comfort during
sunglass use
George A. Zikos, Samantha Slotnick, Rocco Robilotto, Arkady
Selenow, Steven R. Ali. Institute for Vision Research, Manhattan
Vision Associates, New York, NY.
Purpose: Several studies connect visual comfort with squinting, and
muscle tension (Nahar et al. 2007, Sheedy et al. 2005, Aaras et al.
2005). In a previous study we demonstrated that polarized lenses
improve CSF and reaction times in a simulated driving environment
(Zikos et al. 2009) We have further developed this method by adding
simultaneous evaluation of pupil size and squint amount during either
distance or a near task in the presence of glare, in order to further
evaluate objectively different sunglass types.
Methods: Four subjects were tested during simulated outdoor
distance and near activities: The distance task was similar to the 2009
investigation’s simulated driving environment (CSF and response
times tested with Cambridge Research Systems Ltd. ViSaGe system).
The near task included a reading task and FACT Near CSF in the
presence of glare. A modified ISCAN eye movement system with IR
cameras was used to track pupil and aperture size (squinting level)
during testing. Three types of lenses were tested: polarized, tinted and
clear.
Results: Both distance and near CSF results show increased contrast
sensitivity when using polarized lenses vs. tinted or clear lenses.
(mean increase 124% distance and 134% near). Pupil measurements
were similar between the two sunglasses (Mean pupil size 4.2mm)
Good correlation between measuring squint levels with ISCAN and
photographically was found. Mean squint levels were 0.8mm less on
average with the sunglasses.
Conclusions: The addition of measuring pupil size and squint levels
may prove useful in objectively measuring comfort levels with
different spectacle lenses.
Commercial Relationships: George A. Zikos, Essilor USA (F);
Samantha Slotnick, Optos, Inc. (F); Rocco Robilotto, Essilor (F);
Arkady Selenow, None; Steven R. Ali, None
Support: Essilor USA
Program Number: 586 Poster Board Number: C0197
Presentation Time: 10:30 AM - 12:15 PM
Influence of Thermal Lensing on Human Visual Function
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Erica L. Towle1, 2, Michelle T. Aaron1, Leon N. McLin1, Benjamin A.
Rockwell1. 1711 HPW/RHDO, Air Force Research Laboratory, Fort
Sam Houston, TX; 2Research Apprenticeship Program, National
Research Council, Washington, DC.
Purpose: It has been hypothesized that slight heating (1 - 3°C) of
ocular tissue with a near-infrared (NIR) laser could induce temporary
changes in visual function through an effect known as thermal
lensing. If these visual distortions could be safely induced and
controlled, this technology would have potential as a new form of
device that can temporarily alter the visual field of the observer. A
previously completed study concluded that it was possible to safely
and temporarily interrupt visual function using the thermal lensing
effect; however, little effort was made to measure the extent of the
blurring in terms of changes to a subject’s visual acuity and contrast
threshold.
Methods: Ten subjects were asked to identify the orientation of a
50% contrast Landolt ring while being exposed to various laser
sources co-aligned with the stimulus. Each exposure lasted 0.5
seconds and was within the safety limits set by the American
Conference of Government Industrial Hygienists. With each
exposure, the size of the target was increased (from 0 logMAR) until
the subject was able to correctly identify the location direction of the
Landolt ring. Once the target was correctly identified, the current and
previous acuity levels were repeated three times to refine the
threshold of acuity. This threshold under each laser condition (none,
visible only, NIR only, combined visible and NIR) was then averaged
across three sessions (days) to account for any subject variability.
Results: Results show that effects of a visible only exposures
significantly alter the subject’s ability to see targets smaller than 0.25
logMAR. NIR only exposures did not significantly change the
subject’s acuity. By combining two sources, the influence of the NIR
on the visible obscuration was also observed to be negligible. Several
subjects, however, were able to correctly identify when the NIR light
was included in the exposure by a distinct “graying” or “loss of
contrast” of the target.
Conclusions: While the blurring effect of the thermal lens was not
able to obscure the target on its own, evidence suggests that a distinct
loss of contrast was induced during the experiments as a result of the
thermal lens introduced in the eye. This loss of contrast has the
potential to reduce visual acuity of much finer targets (high resolution
Gabors), and therefore, future experiments are planned to investigate
the change in an individual’s contrast acuity in the presence of a
thermal lens.
Commercial Relationships: Erica L. Towle, None; Michelle T.
Aaron, None; Leon N. McLin, None; Benjamin A. Rockwell, None
136 IOL and Crystalline lens
Sunday, May 05, 2013 1:00 PM-2:45 PM
Exhibit Hall Poster Session
Program #/Board # Range: 826-856/B0050-B0080
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 826 Poster Board Number: B0050
Presentation Time: 1:00 PM - 2:45 PM
Straylight in Pseudophakes for Different Intraocular Lens Types
Luuk Franssen1, Marrie Van der Mooren1, Burkhard H. Dick2, Ulrich
Mester3, Patricia A. Piers1. 1R&D, AMO Groningen BV, Groningen,
Netherlands; 2Universitätsklinikum Knappschaftskrankenhaus
Bochum, Bochum, Germany; 3Augenzentrum im Medizeum,
Saarbrücken, Germany.
Purpose: To investigate the influence of intraocular lens (IOL)
design and material on straylight in pseudophakes, and to investigate
straylight in cataract patients and pseudophakes at different scatter
angles.
Methods: Seventy-one eyes diagnosed for cataract were implanted
with either a monofocal (spherical acrylic (N=16), aspheric acrylic
(N=17), aspheric silicone (N=13)) or multifocal (silicone diffractive
(N=13), acrylic diffractive (N=12)) IOL. Intraocular straylight was
measured preoperatively and 1 week and 3 months postoperatively
with the C-Quant (Oculus), which measures at an average straylight
angle of 7 degrees. In 29 eyes, straylight was also measured with an
adapted C-Quant, which measures at an average angle of 3.5 degrees.
Results: The average 3-month postoperative straylight values for the
3 monofocal groups were not statistically significantly different
(log(s) between 1.26 and 1.37 for 7 degrees, log(s) between 1.41 and
1.45 for 3.5 degrees). For 7 degrees, the average value for the
multifocal group (log(s)=1.32) was almost the same as for the
monofocal group (log(s)=1.31). Also for 7 degrees, 80% of the
patients had a lower straylight value at 3 months postoperatively
compared to preoperatively. The 3.5 degree average results were
higher than the 7 degree results postoperatively (pseudophakes), but
not preoperatively (cataract patients).
Conclusions: For the patients implanted with monofocal IOLs,
design and material did not influence the average straylight value
postoperatively. There was also no difference found between the
multifocal and monofocal groups. Cataract patients tend to have a
different angular straylight dependence than pseudophakes.
Commercial Relationships: Luuk Franssen, AMO Groningen BV
(E); Marrie Van der Mooren, AMO Groningen BV (E); Burkhard
H. Dick, None; Ulrich Mester, None; Patricia A. Piers, Abbott
Medical Optics (E)
Program Number: 827 Poster Board Number: B0051
Presentation Time: 1:00 PM - 2:45 PM
Binocular through-focus image quality with various
combinations of modified monovision
Guillaume Van Der Meer1, Pierre-Jean Pisella1, Richard Legras2.
1
Univ Hospital of Tours, France, Tours, France; 2CNRS, Orsay,
France.
Purpose: To evaluate the binocular through-focus (TF) subjective
vision with various combinations of modified monovision (ie
different profile of spherical (SA4) and secondary spherical (SA6)
aberration on each eye).
Methods: We used a numerical eye model to calculate the
appearance of an image (ie three 0.4 logMAR size high contrast
letters) viewed thought an eye taking into account of the variation of
pupil size as a function of proximity (ie 4.7mm at distance vision to
3.3mm at near vision). Images were calculated for various
combinations of SA4 and SA6 (ie SA4-0.4μm, SA4+0.4μm, SA40.4μm and SA6+0.2μm, SA4+0.4μm and SA6-0.2μm) and for all
proximities from -5-D to 5-D with a 0.125-D step. A 3D-NVIDIA
video device was used to simulated binocular vision by projecting a
different image on each eye with a 120Hz frequency. TF subjective
vision was evaluated by using a grading scale (ITU-R 500
recommendation) by three subjects under monocular and binocular
condition for each tested conditions (ie various combination of the
five multifocal profiles).
Results: Binocular TF curves followed the best monocular curve but
there was no binocular summation of quality of vision. Binocular
inhibition was greater when the difference in subjective vision
between each eye was important. Ocular dominance affected the level
of inhibition. We calculated area under the binocular curve (AUC) to
evaluate subjective quality of vision and depth-of-focus. AUC
increased when adding spherical aberrations and can even be
doubled, compared to naked eye, with reverse profile of SA4 and
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
SA6 between each eye (ie SA4-0.4μm and SA6+0.2μm on one eye
and SA4+0.4μm and SA6-0.2μm on the other eye). Pupil diameter
variations had to be taken into account when using simulated images.
The decrease of pupil size in near vision led to a better TF subjective
vision especially with combination of SA4 and SA6. Although we
distinguished two different optical performance profiles (ie (i) good
distance vision/acceptable intermediate vision/poor near vision, and
(ii) good distance vision/poor intermediate vision/good near vision)
there was a good correlation (r2=0.89) between AUC and mean
quality of vision at distance/intermediate and near vision.
Conclusions: There is no binocular summation of quality of vision.
However the use of different SA profiles on each eye especially
reverse profile of SA4 and SA6 profile involved a better binocular TF
subjective vision.
Commercial Relationships: Guillaume Van Der Meer, None;
Pierre-Jean Pisella, None; Richard Legras, None
Program Number: 828 Poster Board Number: B0052
Presentation Time: 1:00 PM - 2:45 PM
Influence of Pupil Diameter on Intraocular Scattering
Measurements Based on Double Pass Images in Patients with
Different Types of Cataracts
Jaume Pujol1, Juan Carlos Ondategui Parra2, Joan A. MartinezRoda2, Meritxell Vilaseca1, Mouafk Asaad Ammaar3. 1Centre for
Sensors, Instruments and Systems Development (CD6),, Universitat
Politecnica Catalunya, Terrassa, Spain; 2University Vision Center
(CUV), Universitat Politècnica Catalunya (UPC), Terrassa, Spain;
3
Ophthalmology, Hospital de Terrassa, Terrassa, Spain.
Purpose: To assess the influence of pupil diameter size on
intraocular scattering measurements obtained from double pass
images in patients with different type of cataracts.
Methods: Intraocular scattering was measured using a comercial
double-pass system (Optical Quality Analysis System, OQAS,
Visiometrics, Spain) (Güell et al. J Cataract Refr Surg 2004) and
quantified using Objective Scattering Index (OSI)(Artal et al. Plos
one 2011; Vilaseca et al Br. J. Ophthalmol. 2012) in four groups of
patients with cataracts (nuclear (NC), cortical (CC), posterior
subcapsular (PSC) and cortical-nuclear mixed (CNMC)). Cataracts
were classified using a LOCS III system. Measurements were
performed using two different pupil diameters: 4mm (with and
without cycloplegic drops) and 7mm (with cycloplegic drops), which
were obtained using the artificial pupil of OQAS system.
Results: 56,5% of the subjects were female where 48 eyes (of 55
patients with cataracts). Cataract classification showed: 29 NC, 12
PSC; 18 SPC and 26 CNMC). Mean ages (± SD [range]) were of
68.3±8.20 (47 to 85 yr.) There are not differences in OSI values
obtained for a pupil diameter of 4 mm either with or without
cyclopegia. The correlations between OSI (4mm) and OSI (7mm)
using cyclopegia were: NC r=0.804 (p=0.00); PSC r=0.608 (p=0.07);
CC r=0.957 (p=0.00) and CNMC r=0.769 (p=0.00). OSI parameter
showed a high correlation between both pupil diameters. Mean± SD
OSI results for 4mm and 7mm pupil were: NC 3.7±2.2 / 6.0±3.4;
PSC 3.1±1.7 / 4.8±2.0; CC 3.5±2.3 / 6.3±3.8 and CNMC 5.0±3.4 /
7.4±3.5. All OSI values presented a proportional increase for each
type of cataracts. Similar changes were obtained considering the
classification according LOCSIII system. The increase in OSI values
(lower in PSC and higher in CC) probably can be due to the
peripherical distribution of cataract in CC and to the central lens
opacity on PSC.
Conclusions: OSI results increase when pupil diameter is higher, but
we have not found difference to classify different types of cataracts.
We can conclude that OSI parameter provides useful information to
classify cataracts regardless of pupil diameter. Future work will be
focused on a larger number of patients with cortical and subcapsular
cataracts.
Commercial Relationships: Jaume Pujol, Visiometrics (P); Juan
Carlos Ondategui Parra, None; Joan A. Martinez-Roda, None;
Meritxell Vilaseca, None; Mouafk Asaad Ammaar, None
Support: “Ministerio de Educación y Ciencia”, Spain (grant n0
DPI2011-30090-C02-01 and European Union
Program Number: 829 Poster Board Number: B0053
Presentation Time: 1:00 PM - 2:45 PM
Capsular Adhesion to Intraocular Lens Evaluated In Vivo Using
Ultralong-scan-depth Optical Coherence Tomography
Yinying Zhao, Jin Li, Weilin Lu, Xiaoying Xing, Fan Lu, Yune Zhao.
wenzhou medical college, Wenzhou, China.
Purpose: A firm capsular apposition to the intraocular lens (IOL)
could inhibit lens epithelial cell proliferation and migration. Many
researchers have focused on the design and material of the IOL.
However, we found few studies evaluating the capsule-IOL
interaction in highly myopic eyes. This study was to evaluate the in
vivo capsular apposition to IOL in patients by ultralong-scan-depth
optical coherence tomography (OCT).
Methods: It is an observational case series research. Thirty eyes from
30 cataract patients were recruited at the Affiliated Eye Hospital,
Wenzhou Medical College, of which 15 eyes were highly myopic
(axial length >26 mm) and 15 eyes were emmetropic (22 mm<axial
length <24.5 mm). All eyes were examined with a custom-built
ultralong-scan-depth OCT at 4hours, 1 month, 3 month, 1 year after
surgery, as well as slit lamp examination.
Results: Most of posterior capsule started to adhere with the IOL
sectionally at 1 month after surgery. Complete apposition of the
posterior capsule with the IOL was significantly less among highly
myopic eyes than in emmetropic eyes at 1 year after surgery ( 10 vs
15 eyes; P<0.01). At 1-year follow-up, there are still 5 high myopia
eyes with uncompleted apposition of the posterior capsule with the
IOL. Posterior capsule adhesion to the IOL was inversely correlated
with axial length (r=0.491, P<0.001, nonparametric Spearman test).
The 6 types of adhesive capsular bend configurations observed were
classified as anterior adhesion, middle adhesion, and posterior
adhesion, funnel adhesion, parallel adhesion, and furcated adhesion
during the follow-up. Seven highly myopic eyes had PCO at the 1year follow-up, as did one emmetropic eye. Four of the eyes with
PCO presented opened capsular bends and uncompleted apposition of
the posterior capsule with the IOL, accompanied with proliferative
lens epithelial cells observed by ultralong-scan-depth OCT. While the
other three are presented closed capsular bends.
Conclusions: Ultralong-scan-depth OCT could be used to evaluate
capsular adhesion and different types of capsular bend of eyes.
Postoperatively, we found weak posterior capsule adhesion to the
IOL in myopic eyes, as well as various types of capsular bending.
These 2 weaknesses in the defense of highly myopic eyes could
increase the incidence of PCO. These features presumably increase
the likelihood of PCO during the early postoperative period.
Commercial Relationships: Yinying Zhao, None; Jin Li, None;
Weilin Lu, None; Xiaoying Xing, None; Fan Lu, None; Yune
Zhao, None
Support: the National Nature Science Foundation of China(Grant
No. 81170869)
Clinical Trial: NCT01605812
Program Number: 830 Poster Board Number: B0054
Presentation Time: 1:00 PM - 2:45 PM
Restoration of acrylic intraocular lens injected through cartridge
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Makoto Inoue1, Jiro Hidaka2, Akito Hirakata1. 1Ophthalmology,
Kyorin Eye Center, Mitaka, Japan; 2HOYA Corp., Tokyo, Japan.
Purpose: To evaluate the effect of temperature in restoration of
acrylic intraocular lenses (IOLs) after injection through a cartridge.
Methods: Acrylic IOLs (SA60AT; Alcon, 251; HOYA, YA-65BB;
HOYA, W-60, Santen, NX-70; Santen) were loaded or preloaded in a
cartridge with viscoelastic material and injected into a water chamber
under temperature control at 24 or 34 C°. Wavefront analyzer
(LAMBDA-X, NIMO TR0815) was used to measure the form of
IOLs. Time to restore the form of the IOLs was defined as Δcylinder
power (difference from the baseline) < 0.2 diopter.
Results: All IOLs restored within 2 minutes at 34 C°. At 24 C°,
SA60AT and 251 restored within 3 minutes but YA-65BB and W-60
(single-piece) required 3.5 minutes and NX-70 (three piece IOL with
same material of W-60) up to 6 minutes. The central optical thickness
of NX-70 (7.0 mm diameter) was 0.865 mm and was thicker than that
of W-60 (6.0 mm diameter) at 0.640 mm. The cross section of the
cartridge for NX-70 was round shape with mean diameter of 2.17 mm
and that for W-60 was oval shape with 1.65 mm of mean diameter.
Conclusions: Restoration of IOL was dependent on temperature.
However it may depend on the thickness of IOL and inner shape of
the cartridge.
Commercial Relationships: Makoto Inoue, None; Jiro Hidaka,
HOYA Corporation Medical Division (E); Akito Hirakata, None
Program Number: 831 Poster Board Number: B0055
Presentation Time: 1:00 PM - 2:45 PM
Stability of the human crystalline lens measured with a high
temporal resolution dynamic Purkinje-meter system
Juan Tabernero, Antonio Fernández, Pablo Artal. Laboratorio de
Optica, Universidad de Murcia, Murcia, Spain.
Purpose: To measure the dynamic stability of the human crystalline
lens by using a custom-made new instrument that tracks the lens
oscillations following a controlled saccadic eye movement (lens
wobbling effect)
Methods: We developed a modified prototype of a Purkinje-meter
that uses a high temporal resolution CMOS camera attached to a
telecentric lens and a semicircular ring of IR LEDs placed on the lens
aperture‘s rim. Saccadic eye movements of 9‘ amplitude were
induced by two flickering visible LEDs (1 Hz) placed in a central and
a peripheral position with respect to the objective-camera axis. Four
flickering orientations were possible (nasal, temporal, inferior and
superior). The wobbling effect is a quick oscillation of Purkinje
image PIV (posterior lens surface reflection) with respect to PI
(corneal reflection) that follows immediately after a change in the
direction of gaze and is captured at high speed (400 frames per
second).Stability is assessed by fitting the relative movement of PIV
with respect to PI to the solutions of a damped harmonic oscillator.
Four parameters are used to characterize the wobbling effect, i) the
amplitude (i.e., the overshooting effect with respect to the stable
position of PIV), ii) the oscillation frequency, iii) the damping ratio
and iv) the stationary time (the time constant of the wobbling effect).
Videos were recorded in eight subjects during a series of 15 saccadic
movements performed horizontally (center-temporal) and vertically
(center-up).
Results: The mean value of the oscillation frequency after a saccadic
was 19 Hz (standard deviation 6 Hz) and the mean damping ratio was
0.45 (SD 0.10). The average stationary time was 57 msec (SD 20
msec). Given that the mean post-saccadic suppression time is around
50 msec (Diamond et al, Journal of Neuroscience, 2000) the visual
effect of the lens wobbling in normal subjects will not be noticeable.
Comparing vertical and horizontal movement, we only observed
differences in the amplitude, larger in the case of the horizontal
movement (252 microns) than in the vertical upwards movement
(194 microns), which perhaps reveals some gravity effects or an
asymmetric distribution of tension on the lens zonule.
Conclusions: A new instrument to measure crystalline lens stability
has been developed and successfully tested in normal subjects. It may
be useful for a wide range of future studies involving lens stability.
Commercial Relationships: Juan Tabernero, None; Antonio
Fernández, None; Pablo Artal, AMO (C), Voptica SL (P), Voptica
SL (I), AMO (F), Calhoun Vision (F), Calhoun Vision (C), AcuFocus
(C)
Support: Ministerio de Ciencia e Innovación, Spain (grants
FIS2010-14926 and CSD2007-00013) and Fundación Séneca
(Region de Murcia, Spain), grant 4524/GERM/06
Program Number: 832 Poster Board Number: B0056
Presentation Time: 1:00 PM - 2:45 PM
Rotational stability of two single-piece toric acrylic intraocular
lenses
Gernot Steinwender, Navid Ardjomand. Dept of Ophthalmology,
Medical University Graz, Graz, Austria.
Purpose: To assess the rotational stability of two single-piece toric
acrylic intraocular lenses (IOL) during the first postoperative month.
Methods: This retrospective case series included 15 eyes (14
patients) with age-related cataract and corneal astigmatism ≥1.50
diopters [D]. Corneal astigmatism was measured using the Pentacam
Scheimpflug system (Oculus) and IOL biometry was performed with
laser interferometry (IOL Master). All eyes were analyzed after
uncomplicated phacoemulsification with in-the-bag implantation of
toric IOL (Hoya iSert 351; Rayner T-flex). Rotational stability of the
IOL was assessed by comparison of images taken by the microscope
video camera intraoperatively with retroillumination photographs at 1
month postoperatively.
Results: The overall mean absolute IOL rotation was 7.67 degrees ±
5.54 (SD). The mean absolute IOL rotation was 5.60 degrees ± 3.21
(SD) for Rayner T-flex IOL and 6.11 degrees ± 4.53 (SD) for Hoya
iSert 351 respectively.
Conclusions: Both investigated acrylic toric IOL seem to be
rotationally stable with just mild IOL rotation in the first
postoperative month and can be recommended for the correction of
astigmatism during cataract surgery.
Commercial Relationships: Gernot Steinwender, None; Navid
Ardjomand, None
Program Number: 833 Poster Board Number: B0057
Presentation Time: 1:00 PM - 2:45 PM
Multicenter clinical evaluation of an aspheric diffractive
multifocal one-piece IOL
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Daniel H. Chang1, Elizabeth A. Davis2. 1Empire Eye and Laser
Center, Bakersfield, CA; 2Minnesota Eye Consultants, Bloomington,
MN.
Purpose: To evaluate clinical outcomes, patient satisfaction, and
surgeon satisfaction following bilateral implantation of the
TECNIS® Multifocal 1-Piece IOL (ZMB00).
Methods: On-going, prospective, open-label observational trial from
surgeons performing cataract surgery and bilateral TECNIS®
Multifocal (TMF) 1-Piece IOL implantation in qualified subjects
aged 21 years or older. All eyes had preoperative corneal astigmatism
of < 1.0 D. Visual acuity (distance, intermediate, near) and patient
satisfaction questionnaires were collected at the 3-4 month
postoperative visit. Surgeon assessment questionnaires were taken at
3 months and at one year.
Results: Interim data were collected on 106 subjects with a mean age
of 66.0 ± 8.1 years. Mean postoperative sphere was 0.07 ± 0.47 D
with 0.40 ± 0.39 D of cylinder and a spherical equivalent of +0.05 ±
0.47 D. Mean binocular UCVA was 20/23 at distance, 20/30 at
intermediate and 20/22 at near. Mean binocular DCVA was 20/20 at
distance, 20/28 at intermediate, and 20/21 at near. The percentage of
subjects with UCVAs of 20/32 or better was 91.8% for distance,
67.7% for intermediate, and 93.8% for near. The percentage of
subjects with DCVAs of 20/32 or better was 98.8% for distance,
70.9% for intermediate, and 96.6% for near. At 3-4 months
postoperative, 86.9% of subjects never or hardly ever use glasses,
87.9% of subjects were either satisfied or very satisfied with their
overall vision without glasses, and 81.3% of subjects would most
likely choose this lens again. At the 3 months, 78.5% of surgeons felt
comfortable with the TMF after implanting ≤ 6 lenses, and 92.9% of
surgeons would recommend the TMF to family, friends, and
colleagues. At one year, 86% of top enrollers were still using the
TMF.
Conclusions: Subjects receiving the TECNIS® Multifocal 1-Piece
IOL showed high levels of satisfaction with good visual outcomes at
all distances and minimal postoperative refractive error. Surgeonreported experience and perception of the TMF were highly positive.
This experiential data further corroborates the U.S. FDA clinical
study results.
Commercial Relationships: Daniel H. Chang, Abbott Medical
Optics, Inc. (F), Abbott Medical Optics, Inc. (C), Abbott Medical
Optics, Inc. (R); Elizabeth A. Davis, None
Support: Abbott Medical Optics, Inc.
Program Number: 834 Poster Board Number: B0058
Presentation Time: 1:00 PM - 2:45 PM
Light Transmittance of Explanted Hydrophobic Acrylic
Intraocular Lenses with Surface Light Scattering
Liliana Werner1, Caleb Morris1, Shannon Stallings1, Erica Liu1, Anne
M. Floyd1, Andrew Ollerton1, Lisa Leishman1, Zachary Bodnar1,
Marcia Ong2, Ali Akinay2. 1Ophthalmology, John A. Moran Eye
Center, University of Utah, Salt Lake City, UT; 2Alcon Laboratories,
Fort Worth, TX.
Purpose: Surface light scattering on hydrophobic intraocular lenses
(IOLs) is caused by hydration-related subsurface nanoglistenings
within the acrylic IOL material. The aim of this study was to
investigate the potential effect of surface light scattering on the light
transmittance of single-piece hydrophobic acrylic IOLs made of
AcrySof material (Alcon) with or without blue light filter (BLF).
Methods: IOLs were obtained from human cadavers (49 lenses total;
36 with BLF), and from finished-goods inventory (controls). The
IOLs were explanted from the cadaver eyes and power/model
matched to unused control IOLs. After removing proteins, the IOLs
were allowed to hydrate for 24 hours at room temperature. Surface
light scattering was then measured with a Scheimpflug camera (EAS1000 Anterior Segment Analysis System, Nidek Ltd). Light
transmittance was measured with a Perkin Elmer Lambda 35 UV/Vis
spectrophotometer (single-beam configuration with RSA-PE-20
integrating sphere).
Results: Hydrated scatter values ranged from 4.8 to 202.5 CCT for
explanted IOLs with BLF and 1.5 to 11.8 CCT for controls; values
ranged from 6.0 to 137.5 CCT for explanted IOLs without BLF and
3.5 to 9.7 CCT for controls. In both groups, there was a tendency for
increasing scatter values with increasing postoperative time. No
differences in light transmittance were observed between explanted
IOLs and controls for both groups of lenses (BLF IOLs: P=0.407,
Paired T-Test; Non BLF IOLs: P=0.216, Wilcoxon Signed Rank Test
for Paired Data).
Conclusions: Although surface light scattering of explanted lenses
was significantly higher than that of controls and appeared to increase
with time, no effect was observed on the light transmittance of singlepiece hydrophobic acrylic lenses with or without blue light filter.
Commercial Relationships: Liliana Werner, Aaren Scientific (F),
Abbott Medical Optics (F), Advanced Vision Science (F), Alcon
Laboratories (F), Anew Optics (F), Bausch & Lomb Surgical (F),
Calhoun Vision (F), Innovia (F), MRI Research (C), Powervision
(C), Rayner Intraocular Lenses (F), Visiogen (C); Caleb Morris,
None; Shannon Stallings, None; Erica Liu, None; Anne M. Floyd,
None; Andrew Ollerton, None; Lisa Leishman, None; Zachary
Bodnar, None; Marcia Ong, Alcon Research (E); Ali Akinay,
Alcon Researh, Ltd (E)
Program Number: 835 Poster Board Number: B0059
Presentation Time: 1:00 PM - 2:45 PM
Visual Simulation of Retinal Images through a New Asymmetric
Refractive Multifocal Intraocular Lens with Two Spherical
Surfaces
Yuki Hidaka1, Kazuno Negishi1, Kazuhiko Ohnuma2, Kazuhiro
Watanabe1, Hidemasa Torii1, Megumi Saiki1, Kazuo Tsubota1.
1
Ophthalmology, Keio University School of Medicine, Shinjuku-ku,
Japan; 2Graduate School of Engineering, Chiba University, Chiba,
Japan.
Purpose: To evaluate optical performance of an asymmetric
refractive multifocal intraocular lens (MIOL) using a visual
simulation system.
Methods: The system consists of a lens that corresponds to a cornea,
an IOL in a water cell, and a charge-coupled device (CCD) camera.
The images formed by the lens can be detected by the CCD camera
and observed on the monitor of a personal computer. The aperture
diameter is exchangeable in the water cell. Using this system, visual
simulations of Landolt visual acuity (VA) charts at various distances
were performed using the MIOL (LENTIS® Mplus, Oculentis)
through a 3.5-mm aperture corresponding to photopic conditions or a
4.5-mm aperture corresponding to mesopic conditions. The contrasts
of the gaps of large (logarithm of the minimum angle of resolution
[logMAR] 0.7), medium (logMAR 0.4), and small (logMAR 0.0)
Landolt VA charts in the simulated images were analyzed using
Photoshop graphics editing software (Adobe).
Results: Using the 3.5-mm aperture, the contrasts of the gaps of the
large, medium, and small charts were 0.22, 0.1, and 0.08 at 5 meters
(m) and 0.08, 0.04, and 0.02 at 0.34 m, which was the best near
focus, respectively. Using the 4.5-mm aperture, the contrasts of the
gaps of the large, medium, and small charts were 0.14, 0.07, and 0.03
at 5 m and 0.07, 0.04, and 0.01 at 0.34 m, respectively. The large
charts maintained good contrast at all distances through the 3.5-mm
aperture. The contrast decreased with decreasing sizes of the Landolt
rings, especially at the intermediate distance (from 1-0.5 m). Through
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
the 4.5-mm aperture, the results showed a similar trend with degraded
contrasts compared to the 3.5-mm aperture. The typical simulated
image had an asymmetric blur probably due to the asymmetric MIOL
design.
Conclusions: The asymmetric refractive MIOL provides good
optical performance at all distances for large charts under photopic
conditions, although the optical performance degrades especially at
intermediate distance with medium and small charts or under
mesopic conditions.
Commercial Relationships: Yuki Hidaka, None; Kazuno Negishi,
Oculentis (F); Kazuhiko Ohnuma, None; Kazuhiro Watanabe,
None; Hidemasa Torii, None; Megumi Saiki, None; Kazuo
Tsubota, AcuFocus, Inc (C), Allergan (F), Bausch Lomb Surgical
(C), Functional visual acuity meter (P), JiNS (P), Kissei (F), Kowa
(F), Santen, Inc. (F), Otsuka (F), Pfizer (C), Thea (C), Echo Denki
(P), Nidek (F), Ophtecs (F), Wakasa Seikatsu (F), CEPT Company
(P)
Program Number: 836 Poster Board Number: B0060
Presentation Time: 1:00 PM - 2:45 PM
A novel hydrophilic intraocular lens with lateral walls to prevent
posterior capsular bag opacification
Hiroyuki Matsushima1, Koichiro Mukai1, Satoshi Watabiki1, Yoko
Katsuki1, Jiro Hidaka2, Senoo Tadashi1. 1Ophthalmology, Dokkyo
Medical University, Shimotsuga-Gun, Japan; 2Hoya Surgical Optics,
Tokyo, Japan.
Purpose: Previous studies show that equator ring and peripheral ring
prevented capsular bag opacification. And another study shows the
aqueous humor inhibit lens epithelial cells development. In this
study, we made a novel hydrophilic intraocular lense (IOL) with
lateral walls. And we evaluated the prevention of posterior capsular
bag opacification (PCO) by circulating aqueous humor in
experimental rabbit studies.
Methods: NY-60 (HOYA) was remodeled that having 4 lateral walls
(2.8mm height, Fig. 1) to expand posterior capsule after implanting
into the lens capsule. And 8 holes around the peripheral of intraocular
lens (IOL) optic and 1 each hole in center of the walls were made for
role of aqueous humor circulate into a capsular bag (aqueous humor
circulate IOL; AHC IOL). Eight weeks 6 albino rabbits weighting 2
kg were prepared and phacoemulsification in 2.65mm corneal
insertion were performed. Control IOL (NY-60, HOYA) was
implanted one eye and the AHC IOL was implanted another eye.
After 1, 2 and 4 weeks, the IOL and PCO were observed using slit
lump and tissue section was stained with hematoxylin-eosin and
observed under light microscope. The PCO was quantified on the
basis of the thickness of the lens epithelial cell layer on the central
subcapsular area and compared among two groups.
Results: After 2 weeks, partial PCO was observed using slit lump in
control group; however, no significant PCO was observed in AHC
group. The thickness of developed lens epithelial cells in center of
IOL was 59.4±67.9μm in control group and 8.3±3.2μm in AHC
group at 4 weeks postoperatively. There is statistically significance
(unpaired t-test).
Conclusions: Novel AHC IOL prevents PCO in experimental rabbit
study. A device of IOL shape without well known sharp edge may
prevent PCO.
Commercial Relationships: Hiroyuki Matsushima, HOYA (C);
Koichiro Mukai, None; Satoshi Watabiki, None; Yoko Katsuki,
None; Jiro Hidaka, HOYA Corporation Medical Division (E);
Senoo Tadashi, None
Program Number: 837 Poster Board Number: B0061
Presentation Time: 1:00 PM - 2:45 PM
Curvature Changing Accommodating IOL
Jim Schwiegerling, Sean J. McCafferty, William Duncan. Optical
Sciences, University of Arizona, Tucson, AZ.
Purpose: To demonstrate the accommodative capabilities of a
curvature changing intraocular lens.
Methods: We previous demonstrated a concept for an
accommodating IOL in which an elastic material is sandwiched
between two rigid plates. One of the plates has a small aperture
through which the soft material can be partially extruded when the
plates are compressed. The extruded material takes on a roughly
parabolic shape and consequently imparts optical power to the
system. Here, we have fabricated a prototype lens consisting of a
silicone gel with refractive index of 1.38 and a durometer value of 12
units on the “00” scale. The rigid portion of the IOL is fabricated
from PMMA. To make the IOL increase in power in response to
constriction of the ciliary muscle, the soft material needs to extrude
into a higher index fluid. We evaluate a series of liquids, indexed
matched to the PMMA, as well as lower index fluids in the index
range of 1.44 to 1.48.
Results: Compression of 100 microns of the silicone gel over a 3 mm
aperture leads to a potential accommodative amplitude of 5.3 to 9.7 D
for the fluids examined. There is concern of the fluid diffusing into
the silicone gel and a membrane may be needed at this interface.
Conclusions: he feasibility of an accommodating IOL based on
curvature change of interface between a low index silicone gel and a
high index fluid is demonstrated. The power change of the lens model
works with the accommodation mechanism of the eye.
Commercial Relationships: Jim Schwiegerling, Alcon Research
(F), Wavetec (F), Visioneering (C); Sean J. McCafferty, None;
William Duncan, None
Support: NIH Grant EY021847
Program Number: 838 Poster Board Number: B0062
Presentation Time: 1:00 PM - 2:45 PM
A triplet optical design for a wide range accommodative IOL
Enrique-Josua Fernandez, Pablo Artal. Laboratorio de Optica,
Instituto Universitario de investigación en Óptica y Nanofísica
(IUiOyN), Universidad de Murcia, Murcia, Spain.
Purpose: Standard intraocular lenses (IOLs) are mostly designed for
far distance vision. Although accommodative IOLs have been
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
proposed, the current designs only provide a modest range of
accommodation in the best-case scenario. We describe here a new
optical design providing a wide-range of potential accommodation
change that could be incorporated in an IOL.
Methods: The mechanical properties of the capsule and the zonula
are known to solely slightly change as the eye ages. The ciliary
muscle essentially maintains its function during the life span.
Consequently, there is a possibility to use the accommodation
apparatus to eventually transmit the subtle mechanical changes into
an IOL able for modulating its optical power. A family of optical
designs with a variable power, sensitive to small compression forces
has been devised. If incorporated within an IOL, power would change
in response to small variations in their equatorial diameter. Regular
materials available for standard IOL have been employed, as acrylics
and silicones.
Results: The proposed design is a triplet-like optical structure that
produces unprecedented gains between the equatorial compression
and the subsequent change in lens power. Some of the generated IOL
models exhibit an increase in their power of up to 10 D once
implanted in the eye. The gain is approximately 1 D/µm of equatorial
compression. The proposed IOL also permits the incorporation of
aspheric or toric surfaces for optimizing ocular spherical aberration
or correcting astigmatism. Chromatic aberration and ghost images
analysis have been also accomplished showing a similar performance
to monofocal standard IOLs currently available. The typical central
thickness of the triplet is 1 mm, showing an optical zone of 6 mm of
diameter. These dimensions and the structure of the proposed haptics
might allow the implantation of the IOL through a corneal incision of
2-3 mm of diameter. The accurate control of the equatorial diameter
of the accommodative IOL and its changes during accommodative
efforts can be solved by using a special intracapsular ring. The
distribution of radial forces of the implanted IOL combined with the
ring showed an efficient mechanism to transmit the changes from the
ciliary muscle to the lens.
Conclusions: A new triplet-type optical design in combination with a
capsular ring for the precise control of its equatorial diameter may
have the potential to restore accommodation after cataract surgery.
Commercial Relationships: Enrique-Josua Fernandez, EP-101193
(P), VOPTICA SL (P), VOPTICA SL (P), VOPTICAL SL (I),
VOPTICAL SL (I); Pablo Artal, AMO (C), Voptica SL (P), Voptica
SL (I), AMO (F), Calhoun Vision (F), Calhoun Vision (C), AcuFocus
(C)
Support: Ministerio de Ciencia e Innovación, Spain (grants
FIS2010-14926 and CSD2007-00013) and Fundación Séneca
(Region de Murcia, Spain), grant 4524/GERM/06
Program Number: 839 Poster Board Number: B0063
Presentation Time: 1:00 PM - 2:45 PM
Optical Ensemble Analysis of the Potential Optical Performance
of Aspheric Multifocal Toric IOLs
Huawei Zhao. R & D, Abbott Medical Optics, Santa Ana, CA.
Purpose: Contrast transfer is an important link between
pseudophakic visual performance and intraocular lens (IOL) optical
performance. This study uses previously validated optical ensemble
analysis (OEA, Zhao, Optics Letters) to compute pseudophakic
optical performance for acrylic aspheric IOLs with diffractive
multifocal anterior or posterior and toric on the accordingly opposite
surfaces.
Methods: OEA is a Monte Carlo simulation using ZEMAX
(ZEMAX Corporation, Bellevue, WA, USA) and a clinically-oriented
eye model. MTF values are computed with different astigmatism,
asphericity, pupil size, and IOL decentration, tilt and astigmatic
orientation error. 600 eyes were simulated for two groups of aspheric
multifocal toric IOLs: Group1 [aspheric-toric anterior and 4D-add
diffractive multifocal posterior surface; low refractive index (1.47)
and chromatic dispersion (Abbe# = 55); full aspheric correction] and
Group 2 [aspheric apodized diffractive 3D-add anterior and toric
posterior surface; high refractive index (1.55) and chromatic
dispersion (Abbe# = 37); partial aspheric correction]. Three cylinder
powers were studied for each group (1.5, 2.25 and 3.0 D).
Results: Ocular parameters in Groups1 and 2 agreed well with
published clinical data and there were no statistically significant
differences between groups (p>0.05). Ocular spherical aberration for
Group1 was statistically significantly lower than Group2.
Pseudophakic optical performance declined consistently with
increasing astigmatic power in each of the two groups. Both IOLs
significantly reduced the ocular astigmatism (p<0.05) with no
statistically significant difference between the two groups in the
astigmatism (p>0.05) and MTFs of far vision (p>0.05). MTFs of near
vision for Group1 were statistically significantly better than Group2
(p<0.05).
Conclusions: Acrylic aspheric IOLs with diffractive multifocal
anterior and toric posterior or multifocal posterior and toric anterior
surfaces reduce refractive astigmatism effectively. Optical
performance is better at lower astigmatic corrections. Optical
performance of near vision is also better under all light conditions for
pseudophakic eyes with low chromatic dispersion IOLs that fully
correct ocular spherical aberration.
Commercial Relationships: Huawei Zhao, Abbott Medical Optics
inc. (E)
Program Number: 840 Poster Board Number: B0064
Presentation Time: 1:00 PM - 2:45 PM
Visual outcomes after implantation of a new trifocal intraocular
lens
Luis Izquierdo, Maria A. Henriquez, Mauricio Rodriguez.
Ophthalmology, Instituto Oftalmo Salud, Lima, Peru.
Purpose: To analyze the visual outcomes after cataract surgery with
a new trifocal intraocular lens (IOL) implantation
Methods: 30 eyes of 15 patients (age range 55-80 years) were
included in this prospective study. All subjects underwent a bilateral
cataract surgery with implantation of the new trifocal FineVision
(Physiol, Belgium) IOL. Distance (4m), intermediate (70cm) and
near (40cm) visual acuities (decimal scale, logMar and defocus ),
refractive outcomes, corneal topography, were evaluated 3 months
after surgery.
Results: the distance corrected visual acuity (DCVA) improvement
was observed after surgery (from 0.58 +/- 0.10 to 0.80 +/- 0.20; p <
0.01). 97% of eyes have a spherical equivalent within +/- 0.50D.
Postoperatively, the uncorrected near visual acuity was 0.76 +/- 0.15
and the uncorrected intermediate visual acuity was 0.69 +/- 0.28. The
efficacy and safety indexes incremented
Conclusions: The new trifocal intraocular lens FineVision IOL is
able to restore successfully the distance, intermadiate and near visual
acuity after cataract surgery.
Commercial Relationships: Luis Izquierdo, None; Maria A.
Henriquez, None; Mauricio Rodriguez, None
Program Number: 841 Poster Board Number: B0065
Presentation Time: 1:00 PM - 2:45 PM
Visual outcomes and patient satisfaction after cataract surgery
with a diffractive trifocal intraocular lens
Javier García Bella1, Jose Vazquez-Molinin2, Laura Valcarce1, Jesus
Carballo2, Juan Velez1, Juan Carlos Sanz2, Vicente Polo3, Jose M.
Martinez de la Casa1. 1HOSPITAL CLINICO SAN CARLOS,
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Madrid, Spain; 2Facultad de Óptica y Optometría, Madrid, Spain;
3
Hospital Universitario Miguel Servet, Zaragoza, Spain.
Purpose: To assess the visual and refractive outcomes after
implantation of the FineVision trifocal IOL (PhysIOL, Belgium).
Methods: Fifty eyes of twenty five patients were implanted
consecutively with the FineVision trifocal IOL. This IOL combine 2
diffractive profiles to achieve far, intermediate, and near correction.
Outcome measures recorded 3 months postoperatively were
uncorrected and distance-corrected (far, near, intermediate) visual
acuities, defocus curve, contrast sensitivity, reading speed (radner
vissum reading chart) and patients' quality of life (visual function
questionnaire VFQ-25, halos and glare presence, overall satisfaction).
Results: At the 3-month postoperative visit, the mean sphere was 0.16 ± 0.45 D and the mean cylinder -0.50 ± 0.55. Binocular
uncorrected and best corrected distance acuity were 0,10 ± 0.11 and
0.03 ± 0.07 logMAR respectively. The mean binocular uncorrected
best distance-corrected near acuity 0.11 ± 0.12 logMAR. The
photopic defocus curve showed similar performance in intermediate
and near distance with visual acuity around 0.1 logMAR. The speed
reading improved from 69,7 ± 13.8 words per minute preoperatively
to 94,7 ± 43,9 in the postoperative period. The photopic contrast
sensitivity was within the standard normal range. The rate of
spectacle independence for all the distances was higher than 85%. A
low percentage of patients referred significative halos or ghost
images.
Conclusions: The FineVision trifocal IOL provided a satisfactory
full range of vision with high optical quality and patient satisfaction.
Commercial Relationships: Javier García Bella, None; Jose
Vazquez-Molinin, None; Laura Valcarce, None; Jesus Carballo,
None; Juan Velez, None; Juan Carlos Sanz, None; Vicente Polo,
None; Jose M. Martinez de la Casa, None
Support: None in the Support field below
Program Number: 842 Poster Board Number: B0066
Presentation Time: 1:00 PM - 2:45 PM
Monochromatic Higher Order Aberrations in Patients
Undergoing Cataract Surgery with an Aspheric Intraocular Lens
Douglas A. Lyall1, 2, Sathish Srinivasan2, Lyle Gray1. 1Glasgow
Caledonian University, Glasgow, United Kingdom; 2Ophthalmology,
University Hospital Ayr, Ayr, United Kingdom.
Purpose: To evaluate the effectiveness of an aspheric intraocular
lens (IOL) in reducing monochromatic higher order aberrations
(MHOA) following routine phacoemulsification and IOL
implantation.
Methods: Prospective, observational study of 50 patients with
visually significant cataract who underwent uncomplicated cataract
extraction and aspheric IOL implantation. Whole eye, corneal and
internal MHOA were measured before, and four weeks after, surgery.
Pre and post-operative data was compared to 300 eyes of 167 agematched patients with no visually significant cataract. MHOAs were
measured over a 5 mm dilated pupil diameter using the iTrace
aberrometer (Tracey Technologies, Houston, TX). Zernike
coefficients were obtained to the 6th order.
Results: There was a significant reduction in total root mean square
(RMS) MHOA following cataract surgery (p<0.001). Whole eye
mean MHOA reduced from 0.729 µm to 0.484 µm (p<0.001) and
mean internal MHOA reduced from 0.681 µm to 0.475 µm
(p<0.001). The RMS of total internal 3rd (p<0.001), 4th (p<0.001),
5th (p=0.033) and 6th (p=0.006) orders also showed a significant
reduction post-operatively. Internal spherical aberration (SA; Z(4,0))
also showed a significant reduction from 0.172 µm to 0.071 µm
(p=0.004). Post-operative whole eye MHOAs (mean 0.484 µm) were
found to be significantly less (p<0.001) than age match controls
(mean 0.648 µm). Post-operative whole eye (mean 0.133 µm) and
internal SA (mean 0.071 µm) was found to be significantly less than
control cases (mean 0.223 µm; p<0.001 and mean 0.133; p=0.022
respectively).
Conclusions: Implantation of an aspheric IOL during cataract
surgery significantly reduces both internal and whole eye MHOA.
Post-operative MHOAs in patients with an aspheric IOL are
significantly less than age matched controls with clear optical media
and no visually significant cataract. These changes may contribute to
greater patient satisfaction and improved visual function following
cataract surgery.
Commercial Relationships: Douglas A. Lyall, None; Sathish
Srinivasan, Rayner (R); Lyle Gray, None
Clinical Trial: 11/AL/0067
Program Number: 843 Poster Board Number: B0067
Presentation Time: 1:00 PM - 2:45 PM
Non-invasive Evaluation of Intraocular Lens Performance
Patricia A. Piers1, Sanjeev Kasthurirangan2, Basilios Sideris1, 3.
1
Applied Research, Abbott Medical Optics Groningen, Groningen,
Netherlands; 2Clinical Research, Abbott Medical Optics, Milpitas,
CA; 3Biomedical Engineering, Delft Technical University, Delft,
Netherlands.
Purpose: Visual performance with intraocular lenses (IOLs) such as
multifocals is usually evaluated through human clinical trials with
surgical implantation. Development of a new type of IOL may need
multiple design iterations requiring multiple clinical trials, which
may prove costly and time consuming. A method is proposed to noninvasively evaluate IOLs in lieu of human clinical trials.
Methods: Photographic images of a miniature ETDRS chart in a
bench-top eye model (ACE) model) that has a cornea lens with the
same spherical aberration as the average human cornea were obtained
for a multifocal IOL (ZM900, Abbott Medical Optics, USA) and a
monofocal control lens (CeeOn, Abbott Medical Optics, USA).
Images were obtained in 12-bit grayscale at different defocus levels
from +0.75 to
-3.50D, in 0.25D steps, by adjusting the camera position, and for two
different entrance pupil diameters of the ACE model (3mm and
5mm). A central ‘S’ letter from the ETDRS chart was cropped and
scaled to different sizes for visual acuity testing using Matlab (The
Mathworks, USA), psychophysics toolbox and the QUEST procedure
with 4-alternative forced choice. The letter was presented on a CRT
monitor (NEC MultiSync FP2141SB, Mitsubishi Electronics,
Illinois) through a BITS# device (Cambridge Research Systems,
UK). Visual acuity testing was performed from 0D to 3D defocus (in
0.50D steps) binocularly in two observers with no prior ocular
surgery and 20/20 visual acuity. The results were compared to the
data from a FDA clinical trial on the two IOLs.
Results: Visual acuity for different defocus levels of the ‘S’ letter
was 20/20 at 0D for both IOLs (mean ± SD; 911A: -0.03 ± 0.0
logMAR, ZM900: 0.01 ± 0.01 logMAR) and declined with defocus
for both IOLs, but returned to 20/20 at 3D with the multifocal IOL
(ZM900: 0.0 ± 0.02 logMAR). The through focus visual acuities with
the multifocal IOL were similar for 3mm and 5mm apertures (all
differences were within 1-line or 0.1 logMAR). When compared to
clinical trial data, visual acuities with the multifocal IOL were within
1-line (or 0.1 logMAR) for all defocus levels. Data on more subjects
is being collected and will be presented at the meeting.
Conclusions: A non-invasive method for evaluating IOLs was
developed that provided visual outcomes similar to a previous human
clinical trial. The proposed methodology will be useful in quickly and
efficiently evaluating novel IOL designs prior to large-scale clinical
trials.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Patricia A. Piers, Abbott Medical
Optics (E); Sanjeev Kasthurirangan, Abbott Medical Optics (E);
Basilios Sideris, AMO Groningen BV (R)
Support: SNN Eoropean fund for Regional Development and the
Ministry of Economic Affairs, Peaks in the Delta grants 086 and 087
Program Number: 844 Poster Board Number: B0068
Presentation Time: 1:00 PM - 2:45 PM
Predicted changes in the cut surface and weight of colored acrylic
intraocular lenses in 20 years
Kenji Kawai. Ophthalmology, Tokai Univ School of Medicine,
Isehara, Japan.
Purpose: We previously reported that long-term immersion of
intraocular lenses (IOLs) in water at high temperature leads to their
opacification and deterioration, depending on differences in
materials. This study aimed to examine predicted changes in the cut
surface and weight of colored acrylic IOLs (colored IOLs) in 20
years.
Methods: Colored IOLs manufactured by various companies were
immersed in 50-mL screw-tube bottles containing ultrapure water at
100 degrees for 115 days (equivalent to 20 years). External
appearance and cut surfaces were observed before and after drying of
the IOLs, and then percent changes in weight before and after
treatment were determined.
IOLs used: We used 3 colored IOLs of each of the following 5 types
manufactured by different companies - SN60WF (Alcon) and AN6K
(KOWA) by the cast-molding method and NY-60 (HOYA), NX-60
(Santen), and NS-60YG (NIDEK) by the lathe-cut method.
Results: External appearance: Opacification was observed to a
varying degree in all IOLs except AN6K and NX-60. After drying at
a room temperature of 25 degrees for 48 hours, opacification
disappeared in all IOLs except SN60WF.
Cut surfaces: Opacification was observed to a varying degree for all
IOLs. After drying, opacification was observed in all except NS60YG.
Percent changes in weight: Percent changes in weight before drying
were unmeasurable for SN60WF, -3% for AN6K, -0.9% for NY-60,
+2.3% for NX-60, and +0.6% for NS-60YG. The changes after
drying were -1.5% for SN60WF, -9.8% for AN6K, -2.7% for NY-60,
-3.7% for NX-60, and -1.5% for NS-60YG.
Conclusions: There were differences in opacification among cut
surfaces of IOLs. Percent changes in weight before and after drying
differed by approximately 6% for AN6K and NX-60. These
differences may be attributable to different methods of manufacturing
acrylic resin.
Commercial Relationships: Kenji Kawai, Alcon (F), KOWA (F),
HOYA (F), Santen (F), NIDEK (F)
Program Number: 845 Poster Board Number: B0069
Presentation Time: 1:00 PM - 2:45 PM
Safety and clinical results of posterior chamber phakic
intraocular lens implantation in low anterior chamber depth
Min gyu Lee, Dong Hui Lim, Eui Sang Chung, Tae-Young Chung.
Ophthalmology, Samsung medical center, Seoul, Republic of Korea.
Purpose: To investigate the safety and present clinical experiences of
the Visian implantable Collamer lens (ICL) implantation in patients
with shallow anterior chamber.
Methods: This retrospective study included patients with anterior
chamber depth (ACD) lower than 2.8 mm who underwent ICL
implantation. Implanted ICL size, pre- and postoperative visual
acuity, refractive errors, postoperative central vault, intra- and
postoperative complications were recorded through a medical chart
review.
The implanted ICL size and vault at 6 months follow-up were
compared with a calculated ICL size and expected vault using a
regression formula reported by the same author previously.
Pneumatic tonometer, specular microscopy, and ultrasound
biomicroscopy (UBM) were performed before and after surgery to
evaluate the safety by measuring intraocular pressure (IOP),
endothelial cell count (ECC), ICL vault, angle opening distance at
500 μm from the scleral spur (AOD 500) and trabecular-iris angle
(TIA).
Results: The mean follow-up period of 16 eyes of 9 patients was
28.00 ± 15.03 months and preoperative ACD was 2.70 ± 0.08 mm.
Preoperative and postoperative spherical equivalent (SE) were -10.27
± 2.38 and -0.11 ± 0.51 diopters, respectively. Postoperative
uncorrected and best corrected visual acuity were 0.89 ± 0.24 and
0.98 ± 0.19, respectively.
The implanted ICL size revealed no significant difference with
calculated ICL size (independent t-test, p=.356). However,
postoperative vault was 0.346 ± 0.179 mm, which was lower than
expected vault of 0.531 ± 0.173 mm calculated by a regression
formula (independent t-test, p=.000).
The pre- and postoperative mean AOD 500 were 0.379 ± 0.088 and
0.267 ± 0.111 mm, and mean TIA were 33.68 ± 5.37 and 23.67 ±
8.33 degrees, respectively. There were significant differences
between preoperative and postoperative AOD500 and TIA
(independent t-test, p=.000). However, there was no severe
complication such as elevated IOP, ECC reduction, cataract
formation or angle closure glaucoma.
Conclusions: ICL implantation performed in the eyes with shallow
ACD showed good visual outcomes without severe complication
during relatively long follow-up period. The size of ICL which was
calculated to get ideal vault of 500 to 750 μm, but it resulted in lower
vault than expected. It suggests the necessity for modulation of ICL
sizing method in patients with low anterior chamber depth.
Commercial Relationships: Min gyu Lee, None; Dong Hui Lim,
None; Eui Sang Chung, None; Tae-Young Chung, None
Program Number: 846 Poster Board Number: B0070
Presentation Time: 1:00 PM - 2:45 PM
Comparative study of visual performance of two multifocal
intraocular lens : two-year follow-up
Balmitgère Thomas1, 2, Burillon Carole2, 1. 1Ophthalmology, Hôpital
Lyon Sud, Pierre-Bénite, France; 2Ophthalmology, Hôpital Edouard
Herriot, Lyon, France.
Purpose: To compare visual performance and functional tolerance of
two multifocal diffractive intraocular lens, AcrySof ReSTOR
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
SN60D3 (Alcon, Inc.) and Acri.LISA 376D (Carl Zeiss Meditec),
two years after cataract surgery.
Methods: This monocentric, prospective, comparative study was
conducted between March 2009 and September 2011. Inclusion
criteria were patients between 50 and 80 years, no longer willing to
wear glasses or contact lenses for distance and near vision, and
wanting a cataract surgery with bilateral implantation. Cataract
surgery was performed by the same surgeon using the same
phacoemulsification technique . The parameters analyzed were
biomicroscopic examination; monocular and binocular visual acuity
with and without spectacle correction using ETDRS charts, at a
distance of 4 meters for far vision, 66 centimeters for intermediate
vision, 33 centimeters for near vision; monocular contrast sensitivity
in photopic conditions ; glare sensitivity ; a quality of life
questionnaire, assessing visual disturbances and dependence on
glasses ; a macular OCT (Optical Coherence Tomography) analysis
to exclude a maculopathy.
Results: 20 eyes (10 patients) received the ReSTOR intraocular lens
(IOL) and 24 eyes (12 patients) received the Acri.LISA IOL in the
Edouard Herriot Hospital, Lyon. There was no statistically significant
difference (α=5%) between the two lens in terms of visual acuity for
far and near vision, for monocular and binocular vision, for contrast
sensitivity and glare test . There was a statistically significant
difference in favor of Acri.LISA group for intermediate visual acuity
specially for monocular uncorrected visual acuity (p = 0.03),
binocular uncorrected visual acuity(p = 0.041) and binocular
corrected visual acuity (p = 0.004) . The analysis of quality of life
questionnaire did not find any statistically significant difference
between the two groups and any correlation between visual
discomfort during night driving and glare test.
Conclusions: This study shows that both IOL have similar visual
performance (good level of satisfaction without eye glasses).
Intermediate vision is better in the Acri. LISA group. It could be
explained by the asphericity of the lens increasing the depth of field.
This study (2 years of follow-up) confirms the results of previous
studies reported in the literature (6 months and 1 year follow-up).
Commercial Relationships: Balmitgère Thomas, None; Burillon
Carole, None
images taken by the camera could be in focus with the target. In this
schematic eye, the target can be lowered, elevated or in a fixed
position, in the latter the images stay in focus while opening and
closing the diaphragm simulating a pupil, like that, the differences
from the same image taken with different diaphragm diameters can
be analyzed. Also at the lens position any kind of IOL can be placed.
For this study parallel or concentric line targets were used, and a
refractive - diffractive - apodized IOL was placed in the schematic
eye and images were recorded.
Results: ubjectively with 2 and 3 mm diaphragm diameters, the
images were clear in the central and peripheral areas of the image.
When the diaphragm was opened wider, the central image lost quality
and the peripheral image increased its sharpness. When elevating or
lowering the target a similar effect was found, with the peripheral and
central image changing in sharpness.
Conclusions: This novel schematic eye is an alternative to study the
images produced by different IOLs at variable diaphragm diameters.
Images can be analyzed qualitatively and in the future with the
appropriate software quantitatively. This schematic eye will help
clinicians and researchers to make better analysis of the behavior and
performance of optics systems related to cataract surgery, intraocular
lenses either focal or multifocal and it variations with pupil size.
Figure 1. Schematic eye and its components.
Program Number: 847 Poster Board Number: B0071
Presentation Time: 1:00 PM - 2:45 PM
Proposed novel schematic eye model for testing intraocular lens
performance
Cristina Mendoza1, 3, Anabel S. Sanchez-Sanchez2, Omar TeranJimenez2, David Rivera4, Claudia Palacio1, Laura Leticia ArroyoMuñoz1, Oscar Guerrero-Berger1, Ernesto Suaste Gomez2.
1
Fundacion Hospital Nuestra Senora de la Luz, Mexico, Mexico;
2
Centro de Investigación y de Estudios Avanzados del Instituto
Politécnico Nacional, Mexico, Mexico; 3Hospital General Manuel
Gea González, Mexico, Mexico; 4IDISA Instituto para el Desarrollo
Integral de la Salud, Mexico City, Mexico.
Purpose: How does a patient actually sees once he has been placed
an intraocular lens (IOL) is a subjective evaluation sometimes
difficult to understand by the clinicians. An objective way to know
how an IOL is performing would be to create a schematic eye that
could show us with real images how the patient is perceiving those
images. Here we present a proposed novel schematic eye where
different IOLs can be placed, and images of different targets can be
taken in order to objectively analyze them.
Methods: A schematic eye consisting of a optical microscope with a
camera, a platform holding the IOL, a diaphragm that simulates the
pupil with a range of aperture of 2-5mm, a pattern target (simulating
an optotype) and a light source (See figure 1) were arranged so the
Figure 2. Same image taken with different diaphragm diameters.
Commercial Relationships: Cristina Mendoza, None; Anabel S.
Sanchez-Sanchez, None; Omar Teran-Jimenez, None; David
Rivera, None; Claudia Palacio, None; Laura Leticia ArroyoMuñoz, None; Oscar Guerrero-Berger, None; Ernesto Suaste
Gomez, None
Program Number: 848 Poster Board Number: B0072
Presentation Time: 1:00 PM - 2:45 PM
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Schematic eye model based on the regression of age-dependent
changes of the crystalline lens
Takushi Kawamorita1, 2, Hiroshi Uozato1, 2, Hiroshi Sasaki3, Yuko
Shibata2, Masatsugu Kanazawa2, Masakazu Hirota2, yoona jang2,
Shinji Arai2, Kimiya Shimizu4, 2. 1Orthoptics and Visual Science,
Kitasato University School, Sagamihara-shi, Japan; 2Ophthalmology
and Visual Science, Kitasato University Graduate School of Medical
Sciences, Sagamihara, Japan; 3Ophthalmology, Kanazawa Medical
University, Kahokugun, Japan; 4Ophthalmology, Kitasato University
School of Medicine, Sagamihara, Japan.
Purpose: To construct a schematic eye model based on the
regression of age-dependent changes of the crystalline lens and
determine the effects on retinal image quality of refractive index,
transmittance, scattering, and lens shape.
Methods: Optical simulation was performed using the optical design
software CodeV. Three-dimensional eye models based on a modified
Navarro model eye were used for the simulation. We used a number
of published regression models in relation to the shape and optical
characteristics of crystalline lens used. Refractive error and
modulation transfer function (MTF) were calculated.
Results: With increasing refractive index of the lens nucleus (from 0
to +0.02), refractive errors showed a myopic shift (from 0 to -8.50
D). The amount of change increased in as the lens nucleus became
steeper. However, with increasing refractive index of the lens cortex,
refractive errors showed a hyperopic shift (from 0 to +2.33 D). As
scattering angle increased (from 0 to 30 min arc), MTF decreased
overall and the lens nucleus was affected the most. As transmittance
at the center of the lens decreased (from 100 to 10%), MTF was
increased at 250 c/mm and decreased at 100 c/mm, indicating the
effect of apodization.
Conclusions: This schematic eye model based on regression of agedependent changes of the crystalline lens should prove useful for the
comparative evaluation of refractive correction methods and the
development of new ophthalmic instruments.
Commercial Relationships: Takushi Kawamorita, None; Hiroshi
Uozato, None; Hiroshi Sasaki, None; Yuko Shibata, None;
Masatsugu Kanazawa, None; Masakazu Hirota, None; yoona
jang, None; Shinji Arai, None; Kimiya Shimizu, None
Support: JSPS KAKENHI Grant Number 24791872; Kitasato
University Research Grant for Young Researchers 2012
Program Number: 849 Poster Board Number: B0073
Presentation Time: 1:00 PM - 2:45 PM
Comparative Analysis of Residual Astigmatism Induced by a
Single-piece or Three-piece Intraocular Lens after Cataract
Surgery
Jin Kwon Chung1, Mee Kum Kim2, Won Ryang Wee2. 1Department of
Ophthalmology, Soonchunhyang University College of Medicine,
Seoul, Republic of Korea; 2Department of Ophthalmology, Seoul
National University College of Medicine, Seoul, Republic of Korea.
Purpose: To analyze comparatively lenticular astigmatism of singleand three-piece intraocular lenses (IOLs) after cataract surgery.
Methods: The medical records of the 397 patients who underwent
cataract surgery with IOL implantation were retrospectively
reviewed. Patients were divided into 4 groups depending on the
implanted IOLs (SN60WF, SN60AT, MA60BM, or AR40e). IOL
induced lenticular astigmatism was measured by differences between
refractive astigmatism and total corneal astigmatism as determined by
Fourier transformation. Vertical and horizontal astigmatic vectors
(J0), oblique astigmatic vectors (J45), and overall IOL induced
astigmatic strengths were compared. Coefficients of determination of
IOL J0 and J45 values were assessed using linear regression models.
Results: Mean (J0, J45) vectors were -0.19 diopters (D) and 0.06 D, -
0.20 D and 0.06 D, -0.17 D and 0.09D, and -0.22D and 0.06 D in the
SN60WF, SN60AT, MA60BM, and AR40e groups, respectively. No
significant intergroup differences were found for J0 or J45. Overall
IOL induced astigmatic strengths were 0.35 D, 0.37 D, 0.42 D, and
0.39 D in the SN60WF, SN60AT, MA60BM, and AR40e groups,
respectively, which were without statistical significance. Linear
regression analysis showed a highest R2 value for SN60AT and a
lowest R2 value for AR40e for the determination of refractive
astigmatism. The residual astigmatism induced by IOLs contributed
to refractive astigmatism by an average of 23.8%.
Conclusions: Single-piece IOLs with an aspheric optic seemed to be
comparable in terms of functional stability with three-piece IOLs in
terms of inducible residual astigmatism.
Commercial Relationships: Jin Kwon Chung, None; Mee Kum
Kim, None; Won Ryang Wee, None
Program Number: 850 Poster Board Number: B0074
Presentation Time: 1:00 PM - 2:45 PM
Impact of Ultrasound Biomicroscopy (UBM) versus White-toWhite (WTW) measurement on sizing of Visian Implantable
Collamer Lens (ICL) and Residual Postoperative Refraction
Puneet Panda1, Ann Ostrovsky2, Scott E. Brodie1, Mark Speaker2.
1
Ophthalmology, Mount Sinai Medical Center, New York, NY;
2
Laser and Corneal Surgery Associates, PC, New York, NY.
Purpose: The aim of this work is to compare residual postoperative
refractive error after implantation of Visian Implantable Collamer
Lens (ICL) in patients having the lenses sized with either Ultrasound
Biomicroscopy (UBM) or white-to-white (WTW) measurements, and
to determine if the residual refraction correlates with amount of
postoperative lens vault.
Methods: This cohort study included 33 eyes that underwent Visian
ICL implantation. Sulcus-to-sulcus (STS) distances were determined
using Ultrasound UBM in 23 eyes and with caliper assisted white-towhite (WTW) measurements in 10 eyes. Manifest refractions
(spherical equivalents) and central lens vaults were compared
between the two groups at the postoperative month 1 visit, using twosample t-tests.
Results: The pre-operative mean spherical equivalent (MSE) for all
33 patients was -10.97 diopters (D) (range: -5.37 D to -17.13 D). The
pre-operative MSE was -10.18D for the UBM group, and -12.78D for
the WTW group, respectively. The postoperative MSE was -0.43+/0.43D for the UBM group and -0.85 +/-0.53D for the WTW group
(p=0.02). Postoperative mean central vault height was 495 +/- 167um
in the UBM group and 710 +/- 250um in the WTW group (p>0.05).
Conclusions: This study suggests that UBM valuation of STS
distance results in more precise sizing of the ICL implant and
consequently in more accurate refractive outcomes. Effective lens
position, reflected by postoperative lens vault may be a factor in
postoperative refractive outcome. Residual refractive error was often
the result of astigmatism in some patients.
Commercial Relationships: Puneet Panda, None; Ann Ostrovsky,
None; Scott E. Brodie, None; Mark Speaker, None
Program Number: 851 Poster Board Number: B0075
Presentation Time: 1:00 PM - 2:45 PM
Measurement of the intraocular scattering in cataractous
patients, using different instruments and parameters.
Comparative study
Juan Carlos Ondategui Parra1, 2, Lorena Mateos-Pena1, 3, Joan A.
Martinez-Roda1, 2, Montserrat Arjona1, 3. 1Optics and Optometry,
Politechnical Univ of Catalonia, Terrassa, Spain; 2University Vision
Center (CUV), Terrassa, Spain; 3Center for Sensors, Instruments and
Systems Development (CD6), Terrassa, Spain.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Purpose: To perform clinical measurements of intraocular scattering
in cataractous patients by
means of different available commercial instruments that have
become common in clinical practice
Methods: Intraocular scattered light was measured by means of two
different available commercial instruments: the CQuant system
(Oculus), which provides an absolute intraocular scattering value
(log(s)) (Van der Berg et al Ophthal. Physiol Opt. 2009), and the
OQAS (Visiometrics), which uses the Objective Scatter Index (OSI)
parameter (Artal el al. Plos One 2011) obtained from the double-pass
retinal image.
78 cataractous eyes of 52 patients were included in the study (37 right
eyes, and 41 left eyes), 41 female and 37 male with a mean ± SD in
age of 68.24 ± 8.3 years (range: 47 to 85 years), spherical manifest
refraction ranged from -8.00 to +5.75D and the cylinder from 0.00 to
3.00D, best spectacle-corrected visual acuity in the logMAR scale of
0.17±0.27 (1.25 to -0.20). The grade and type of cataract was: 24
eyes of nuclear cataract (30.4%), 27 of mixed nuclear (34.2%), 9 eyes
of cortical (11.4%) and 18 of posterior subcapsular (24.1%). CSF was
also measured using CSV-1000 (Vector Vision
Results: Considering all types of cataract, the Pearson correlation
between log(s) and OSI is statistically significant (r=0.339 and
p=0.002). For high degree of cataract and high OSI values (OSI>8)
inconsistencies appear (normally low values of log(s)). Removing
this values a better correlation (r=0.559 and p<0.001) is obtained.
The correlation between log(s) and OSI values separate in nuclear
cataract group(r=0.654 and p=0.001) and mixed nuclear cataract
group (r=0.707 p<0.001), is statistically significant. There is no
statistically significant Pearson correlation for both cortical cataracts
group (r=0.524 and p=0.286), and for posterior subcapsular cataract
group (r=0.359 and p=0.144).
Pearson correlation r between CS (3, 6, 12, and 18 c/deg), LogMAR
log(s) and OSI is statistically significant in more cases with OSI than
with log (s)
Conclusions: C-Quant and OQAS are good predicting methods of
the gradation of different types of cataracts in the clinical practice,
although the OSI parameter has shown more statistically significant
results. Future work will be focused on a larger number of patients
with cortical and subcapsular cataracts.
Commercial Relationships: Juan Carlos Ondategui Parra, None;
Lorena Mateos-Pena, None; Joan A. Martinez-Roda, None;
Montserrat Arjona, None
Support: “Ministerio de Educación y Ciencia”, Spain (grant n0
DPI2011-30090-C02-01 and European Union
Program Number: 852 Poster Board Number: B0076
Presentation Time: 1:00 PM - 2:45 PM
Square-Edge IOLs and Epithelial Lens Cell Proliferation:
Implication on Posterior Capsule Opacification in an in Vitro
Model
Eleonora Favuzza, Iacopo Paladini, Ugo Menchini, Rita Mencucci.
Eye Clinic-University of Florence, Florence, Italy.
Purpose: To evaluate human Lens Epithelial Cell (hLEC)
proliferation comparing a 360-degree square-edge one-piece
Intraocular Lens (IOL) (TECNIS ONE Abbott Medical Optics) to a
square-edge three-piece IOL (AR40E, AMO) using an in vitro culture
model
Methods: An in vitro Posterior Capsule Opacification (PCO) model
was established: hLECs (104 from ATCC, USA) were seeded on
transwell cell culture inserts coated with a type I collagen membrane
on which an IOL (TECNIS ONE or AR40E) had been previously
placed. As control, cells were plated on the insert membrane without
an IOL and cultured at the same conditions. At day six (cells
confluent in controls) IOLs were removed and cell counting, viability
and cell density under and outside the IOLs were evaluated
Results: At day six the cell number in inserts containing IOLs was
significantly (P<0.05) lower than in controls. The inserts with
TECNIS ONE contained a similar number of cells to AR40e (P>0.05
); all the cells in each insert were viable. Cell density in the area
under each IOL was significantly lower either than the cell density
outside the IOL or in the control insert. Cell density under TECNIS
ONE was lower but not significantly different from that under
AR40E (P>0.05).
Conclusions: A 360-degree square edge is a key factor in PCO
formation. Probably also an haptic design able to increase IOL
capsular bag fixation is important in preventing PCO. Long term
clinical evaluation is necessary to estimate functional results.
Commercial Relationships: Eleonora Favuzza, None; Iacopo
Paladini, None; Ugo Menchini, None; Rita Mencucci, None
Program Number: 853 Poster Board Number: B0077
Presentation Time: 1:00 PM - 2:45 PM
visual impact of micro-vacuole defect in intraocular lenses
Marrie Van der Mooren1, Michelle Langeslag1, George Beiko2,
Patricia A. Piers1. 1Applied Research, AMO Groningen BV,
Groningen, Netherlands; 2McMaster, Univ of toronto, St. Catherines,
ON, Canada.
Purpose: The impact of micro vacuole defects in intraocular lenses
(IOL) on quality of vision is subject to scientific debate. The purpose
of this study is to estimate the visual effect of the micro vacuole
defect in IOLs based on in-vitro straylight measurements.
Methods: The straylight induced by the micro vacuole defect was
calculated by subtracting the straylight measurement results of an
IOL with and without inclusions. The micro vacuole defects were
induced by immersing IOLs in a saline solution and changing from
room to eye temperature overnight. The visual effect is estimated by
using the concept of equivalent veiling luminance introduced by
Stiles-Holladay. The additional induced luminance could be
calculated as function of visual angle and illuminance of the eye.
Confocal microscopy, dark field imaging and straylight
measurements were performed before and after the temperature
change on the IOLs. Four different hydrophobic acrylic lenses made
by respectively ALCON, B&L, AMO and HOYA were tested
including IOLs recently manufactured with an improved process.
Results: All lenses had straylight scatter less than a 20 yr old human
crystalline lens before temperature change. After change of
temperature in a water bath, micro vacuole formation was evident in
dark field imaging in ALCON and HOYA hydrophobic acrylic
lenses. The IOLs made with an improved process by the same
manufacturer had similar levels of micro vacuole formation as
previous IOLs. The straylight measurements results showed that
IOLs susceptible to micro vacuole formation produced two optical
fields arriving at different eccentric (retinal) locations. One field is
diffracted by the surfaces of the micro vacuoles creating a white halo
and the other field exists of colored fringes produced by the field
propagating through the micro vacuole. An average micro vacuole
size of 6 micrometer was obtained by confocal microscopy. For a
typical micro vacuole density the scatter level increased 5 deg2/sr at
10 degrees of visual angle. In this condition and for 20 lux of ocular
illuminance, a veiling retinal luminance of 1 cd/m2 is induced.
Conclusions: The angular straylight distribution induced by the
micro vacuole defect consists of two optical fields: white halo and
colored fringes. The visual effect was calculated in terms of veiling
retinal luminance predicting a potentially debilitating contrast loss.
Commercial Relationships: Marrie Van der Mooren, AMO
Groningen BV (E); Michelle Langeslag, AMO Groningen B.V. (E);
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
George Beiko, AMO (C); Patricia A. Piers, Abbott Medical Optics
(E)
Program Number: 854 Poster Board Number: B0078
Presentation Time: 1:00 PM - 2:45 PM
Evaluation of the Impact of Scatter in Pseudophakic Eyes with
Glistenings
Anand Doraiswamy1, Edward DeHoog2. 1Research and
Development, Advanced Vision Science Inc, Santa Barbara, CA;
2
Optical Engineering & Analysis LLC, Grants Pass, OR.
Purpose: To evaluate the impact of light scatter from glistenings in
pseudophakic eye models
Methods: A pseudophakic eye model is constructed in ZEMAX
using established eye models. The lens is optimized for a
polychromatic MTF for field angles 0, 1.4 and 2 Degrees
corresponding with Foveal vision. The modeling and evaluation of
scatter and image resolution (MTF) are performed for various
materials (hydrophobic acrylic, PMMA) for various size and grades
(density) of glistenings, all under scotopic and photopic conditions.
Results: Results from the evaluation demonstrate that light scatter
increases and MTF decreases with increase in glistening density for
both materials. The difference in index of refraction between the
cavitations filled with water and the IOL material causes the scatter.
As predicted by Mie theory as the relative difference between the
scatterer and media increases the amount of scatter will increase. Size
of glistenings/cavitations also plays a crucial role in the extent of
light scatter and loss of MTF. 2 micron sized glistenings were found
to more significant than 200 micron sized glistenings in influencing
resolution of image.
Conclusions: Incorporation of scatter metrics into a model eye
allows us to learn more about the impact of various phenomena on
quality of vision. Mathematical modeling demonstrated that
glistening can have a significant effect on scatter and resolution of
image. Smaller cavitations and larger density have a more
pronounced effect on the MTF than larger cavitations and smaller
density. The effect is more pronounce in higher index materials with
glistenings. Further evaluation will focus on the effect of surface
haze, and more importantly the role of neuroadaptation that may
depress the predicted outcomes in-vivo.
Commercial Relationships: Anand Doraiswamy, Advanced Vision
Science Inc. (E); Edward DeHoog, Advanced Vision Science (C)
Program Number: 855 Poster Board Number: B0079
Presentation Time: 1:00 PM - 2:45 PM
In vitro straylight levels for IOLs across forward scatter positions
up to 30 degrees
Michelle Langeslag, Marrie Van der Mooren, Patricia A. Piers, Luuk
Franssen. Research, AMO Groningen BV, Groningen, Netherlands.
Purpose: The purpose of the study is to combine the straylight levels
of IOLs measured with a method for small and a method for large
forward scatter position angles. The straylight levels were determined
for intraocular lenses (IOLs) with different designs and materials.
Methods: IOLs were measured on two different lab-based set-ups: 1)
for forward scatter positions between 0.6 and 2 degrees 2) for
forward scatter positions up to 30 degrees. In both cases the IOL was
placed in a saline filled cuvette on an optical bench set-up. A CCD
camera was used to measure the line spread functions from which the
angular dependent straylight parameters were then calculated. The
straylight measured using the two methods were then combined in
order to determine the magnitude over the entire angular range.
Using this method IOLs made from 4 different materials (2
hydrophobic and 2 hydrophilic acrylics) and 3 different designs
(spherical monofocal, aspheric monofocal and diffractive multifocal)
were measured and compared. Additionally, the measured straylight
levels were compared to the levels published for a 20 and 70 year old
human crystalline lens.
Results: All monofocal IOLs with the same type of optical design
show comparable straylight parameters, both for small and large
forward scatter angles.
At a forward scatter angle of 2° the average value for the straylight
parameter of diffractive multifocal lenses is 4.5. For an angle of 7.5°
the average value for the same type of lenses is 1.2.
Irrespective of material or design, the amount of straylight is reduced
for larger forward scatter angles. All IOLs have a straylight
parameter of approximately 1.0 for angles of 10° and larger. For an
angle larger than 7.5° all IOLs have a straylight level below that of a
20-year old human crystalline lens.
Conclusions: Straylight parameter results from both set-ups can be
combined to determine the straylight profile of an IOL over an
angular range from 0.6 to 30 degrees. IOL design has more influence
on the height of the straylight parameter than the IOL material does.
IOL straylight parameters get smaller as the measurement angles
increase. The straylight parameter of all IOLs measured is
independent of design parameters for angles larger than 10°.
Commercial Relationships: Michelle Langeslag, AMO Groningen
B.V. (E); Marrie Van der Mooren, AMO Groningen BV (E);
Patricia A. Piers, Abbott Medical Optics (E); Luuk Franssen,
AMO Groningen BV (E)
Program Number: 856 Poster Board Number: B0080
Presentation Time: 1:00 PM - 2:45 PM
Optical simulation for sub-surface nano glistening
Yoriko Takahashi1, Takushi Kawamorita2, Norihiro Mita1, Natsuko
Hatsusaka1, Eri Shibuya1, Eri Kubo1, Hiroshi Sasaki1.
1
ophthalmology, Kanazawa Medical University, Ishikawa, Japan;
2
Orthoptics and Visual Science, University School of Allied Health
Sciences, Sagamihara, Japan.
Purpose: To investigate the effect of sub-surface nano
glistening(SSNG)in hydrophobic acrylic intraocular lens (IOL) on
irradiance, forward light scattering and imaging characteristics of
retina by optical simulation.
Methods: To simulate the effect of SSNG we used optical design
software LightTools and CODE V (Synopsis) to evaluate the peak
value of irradiance on retina, forward light scattering, and the
modulation transfer function (MTF) with Liou-Brenann model eye
(JOSA, 1997). The physicality and shape of IOL was set as acrylic
IOL (SN60AT, Alcon). Ong et al (JCRS, 2012) found in explanted
acrylic IOLs with severe SSNG, particles of diameter 150 nm located
up to 60μm from the surface of the anterior and posterior side of the
IOL at a volume ratio of SSNG particle, which corresponds to the
density, of 0.05%. In the present optical simulation, particle diameter
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
and volume ratios were set at 100 nm, 150 nm and 200 nm and 0%,
0.05%, 0.1%, 0.2%, 0.5%,1.0%, 2.0%, 5.0% and 10.0%.
Results: Peak value irradiance reduced with increased volume ratio
and particle size of SSNG. At volume ratio 0.05%, peak values of
irradiance for SSNG particle diameters 100nm, 150nm and 200nm
reduced by 0.7%, 1.8% and 2.9%, respectively, compared with those
at volume ratio 0% (no SSNG). At volume ratio 0.1%, peak values of
irradiance for SSNG particle diameters 100nm, 150nm and 200nm
reduced by 1.5%, 3.6% and 5.7%, respectively. Forward light
scattering increased with increased size of SSNG particle and volume
ratio. MTF did not change with increased size of SSNG particle and
volume ratio.
Conclusions: Although SSNG in this condition setting slightly
increased forward scattering and reduced irradiance, there was no
effect on the characteristics of retinal imaging. These results suggest
that the effect of SSNG on visual function is very slight in eyes
without severe retinal diseases.
Commercial Relationships: Yoriko Takahashi, None; Takushi
Kawamorita, None; Norihiro Mita, None; Natsuko Hatsusaka,
None; Eri Shibuya, None; Eri Kubo, None; Hiroshi Sasaki, None
predicted vs. measured change of acuity did not differ significantly
from 1 (α=0.05) for 2 of the 3 metrics: logNS (p=0.28, Fig.2) and
logVSX (p=0.13, Fig.3).
Conclusions: One can confidently use logNS or logVSX to design
wavefront guided corrections that minimize the impact of registration
uncertainty on visual acuity.
218 Aberrations, Image Quality and Visual Performance
Monday, May 06, 2013 8:30 AM-10:15 AM
TCC LL 4/5 Paper Session
Program #/Board # Range: 1279-1285
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 1279
Presentation Time: 8:30 AM - 8:45 AM
Optical quality metrics predictive of visual acuity for the design
of wavefront guided corrections in the presence of dynamic
registration uncertainty
Yue Shi, Raymond A. Applegate, Ayeswarya Ravikumar, Harold E.
Bedell. College of Optometry, University of Houston, Houston, TX.
Purpose: When building a wavefront guided contact lens correction
for highly aberrated eyes we would like to achieve the best visual
acuity given dynamic registration uncertainty. To optimize the design
of such a lens correction, it is useful to have optical quality metrics
that are highly correlated with and predictive of visual acuity. The
purpose here is to find optical quality metrics that are highly
correlated with and predictive of acuity given the unusual aberration
structures generated by misalignment of wavefront guided
corrections.
Methods: Residual aberrations were generated by allowing 4
correction designs (3 wavefront guided and 1 sphero-cylinder for
each eye) to undergo horizontal, vertical and rotary motion with
respect to 3 keratoconic eyes (KC) for 2 pupil sizes (4 and 5mm).
Then 77 aberrations were selected based on their log visual Strehl
with the expectation that they would induce up to at least 5 lines loss
of acuity [JOV, 12:1-13, 2012]. The point spread functions of the
selected aberrations were convolved with unaberrated logMAR
acuity charts to generate blurred charts, which were presented
monocularly to 3 normal chart-readers with 20/15 best corrected
acuity. For each chart, visual acuity was measured up to 5th letter
missed through a 3 mm pupil placed conjugate and centered with the
chart-reader’s dilated pupil. The measured change of acuity with
respect to the unaberrated chart was regressed against the changes of
acuity predicted by 29 optical quality metrics [JOV, 12:1-13, 2012].
Results: Regression analysis revealed that only 3 of the 29 metrics
(Fig.1) predicted change of measured logMAR acuity with a
coefficient of determination (R2) of at least 0.9: logNS (R2=0.96),
logVSX (R2 =0.96), and logVSMTF (R2=0.90). The slopes of
Fig. 1: R2 values of 29 metrics in the regressions.
Fig. 2&3: Regressions of measured and predicted change of acuity by
logNS or logVSX. 3 data symbols: aberrations generated in 3 KC
eyes. Error bars: 1 standard deviaiton of measeured change of acuity
by 3 chart-readers.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Yue Shi, None; Raymond A.
Applegate, University of Houston (P); Ayeswarya Ravikumar,
None; Harold E. Bedell, None
Support: NEI 5R01EY008520; NIH/NEI 5R01EY019105; NIH/NEI
P30 EY 07551
Program Number: 1280
Presentation Time: 8:45 AM - 9:00 AM
Influence of aberration-induced blur on contrast sensitivity:
comparison of different optotype sizes
Jens Buehren1, Hendrik Jungnickel2, 3, Wolfgang Raab1, Daniel
Weigel3, Michael Gebhardt2, Richard Kowarschik3, Thomas Kohnen1.
1
Dept of Ophthalmology, Goethe University Frankfurt, Frankfurt am
Main, Germany; 2SciTec Department, Ernst Abbe University of
Applied Sciences, Jena, Germany; 3Institute for Apllied Optics,
Schiller University Jena, Jena, Germany.
Purpose: To compare the decrease of contrast sensitivity (CS) due to
defocus and higher-order aberration (HOA) blur measured with
optotypes of different size.
Methods: Thirty-three emmetropic healty volunteers were included.
In a first experiment (defocus blur), CS was measured in 31 eyes.
Experimental fogging was performed with spherical trial lenses of 0,
+0.25, +0.5 and +0.75 diopters (D). In a second experiment (HOA
blur), CS was measured in 3 eyes at an adaptive optics (AO) visual
simulator. Besides the correction of lower-order aberrations (LOA)
and full correction, subjects were presented 6 wavefront errors of
different blur strength and characteristics (3 keratoconus eyes, 3 postLASIK eyes). In total, 8 different wavefront errors with a VSOTF
(visual Strehl ratio based on the optical transfer function) range of 0.05 to -1.70 log units were presented. In both experiments, CS was
measured with Landolt rings of 1.3 and 0.3 logMAR using FrACT
software. The impact of defocus blur (D) or HOA blur (VSOTF) on
CS was assessed using linear regression analysis. The regression
coefficient b and the coefficient of determination R2 reflect the
sensitivity of the CS contrast test to aberration-induced blur.
Results: Experiment 1: Unfogged photopic CS was 1.93±0.06 logCS
(1.3 logMAR) and 1.56±0.05 logCS (0.3 logMAR). Regression
coefficients were higher for the 0.3 logMAR (b=-0.88, R2=0.70) than
for the 1.3 logMAR Landolt ring (b=-0.39, R2=0.28). Experiment 2:
CS was 1.98±0.17 (0.3 logMAR optotype: 0.95±0.14) log units with
full AO correction. Also in this experiment, CS was more sensitive to
optical blur if measured Landolt rings of 0.3 logMAR (b=0.63,
R2=0.74) compared to those of 1.3 logMAR (b=0.34, R2=0.34).
Conclusions: CS tests with large optotypes such as the Pelli-Robson
test may not pick up subtle, yet notable aberration-induced changes in
retinal image quality. Therefore, for the assessment of effects of
optical aberrations, CS testing should be performed at higher spatial
frequencies (e.g., 0.3 logMAR Landolt ring).
Commercial Relationships: Jens Buehren, None; Hendrik
Jungnickel, None; Wolfgang Raab, None; Daniel Weigel, None;
Michael Gebhardt, None; Richard Kowarschik, None; Thomas
Kohnen, None
Support: Federal Ministry for Education and Research (BMBF)
01EZ0608
Program Number: 1281
Presentation Time: 9:00 AM - 9:15 AM
Visual performance under natural, corrected and Adaptive
Optics induced astigmatism: meridional and adaptational effects
Maria Vinas1, Pablo De Gracia1, Carlos Dorronsoro1, Lucie
Sawides1, Gildas Marin2, Martha Hernandez2, Susana Marcos1.
1
Visual Optics & Biophotonics Lab, Instituto de Optica, CSIC,
Madrid, Spain; 2R&D, Vision Science Department, Essilor
International, Saint-Maur, France.
Purpose: To study the extent to what prior adaptation to astigmatism
affects visual performance, whether this effect is axis-dependent, and
the time-scale effect of potential changes in visual performance in the
presence of astigmatism following its correction. To study whether
the effect of possible positive interactions of aberrations (astigmatism
& coma) on visual performance might be altered after long-term
adaptation to correction of astigmatism.
Methods: Measurements of visual acuity (VA) were performed
under induction of astigmatism and a combination of astigmatism and
coma, while controlling the low and high order aberrations (HOA) of
the subject with an Adaptive Optics (AO) system, in 25 subjects
classified in 3 groups: non-astigmats, habitually-corrected and
uncorrected astigmats. Astigmatism (1.00D) was induced at 3
different orientations: at the natural axis, at the perpendicular
orientation, and at 45deg for astigmats, and at 0, 90 and 45deg for
non-astigmats. Experiments were also performed with coma (0.41µm
at a relative angle of 45deg) combined with the mentioned
amount/orientations of astigmatism. VA was measured in a total of
14 different conditions, using an 8-Alternative Forced Choice
(8AFC) procedure with tumbling E letters and a QUEST algorithm.
Uncorrected astigmats were provided with proper astigmatic
correction immediately after the first session. Measurements were
performed during 6 months following correction.
Results: In non-astigmats, inducing astigmatism at 90deg, under full
AO correction, produced a statistically (p<0.01) lower reduction in
VA (29%) than at 0 (40%) or 45deg (41%). In astigmats, the lower
decrease was for astigmatism induced at the natural axis (24% for
corrected astigmats, 28% for non-corrected astigmats). 6-months of
astigmatic correction wear did not reduce the insensitivity to
astigmatism induction along the natural axis. Visual benefit of adding
coma to astigmatism over astigmatism alone improved significantly
only in non-astigmats, and only for some orientations of astigmatism.
Conclusions: The impact of astigmatism on VA is greatly dependent
on the orientation of the induced astigmatism, even in non-astigmats.
Prior experience to astigmatism plays a significant role on visual
performance in the presence of both astigmatism and combinations of
astigmatism and coma, with a strong bias towards the axis of natural
astigmatism.
Commercial Relationships: Maria Vinas, Essilor International (F);
Pablo De Gracia, None; Carlos Dorronsoro, Essilor International
(F); Lucie Sawides, None; Gildas Marin, Essilor international (E);
Martha Hernandez, Essilor International (E); Susana Marcos,
Essilor (F), PCT/ES2012/070185 (P)
Support: Spanish Goverment FIS2008-02065, FIS2011-25637, and
FPU Programs; European Research Council ERC-2011-AdG294099; CSIC JAE Predoctoral Program ; Essilor International
Colaborative agreement
Program Number: 1282
Presentation Time: 9:15 AM - 9:30 AM
Perceptual learning after correcting the eye’s aberration with
adaptive optics
Ramkumar Sabesan1, 2, Geunyoung Yoon1, 2. 1Flaum Eye Institute,
University of Rochester, Rochester, NY; 2The Institute of Optics,
University of Rochester, Rochester, NY.
Purpose: Highly aberrated keratoconic (KC) eyes do not elicit the
maximum visual advantage immediately after a customized
correction. This is attributed to the neural insensitivity arising from
chronic visual experience with poor retinal image quality, dominated
by low spatial frequencies. The goal of this study was to investigate if
targeted perceptual learning with adaptive optics (AO) can stimulate
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
neural plasticity in these eyes, improving their visual benefit.
Methods: A large-stroke AO vision simulator was employed to train
the worse eye of 2 KC subjects in a contrast detection test under
complete aberration correction with AO. Prior to training, visual
acuity (VA) and contrast sensitivity (CS) at 4, 8, 12, 16, 20, 24 and
28 c/deg were measured in both eyes of subjects with AO correction
for a 6mm pupil. The spatial frequency requiring 50% contrast for
detection with AO correction was picked as the training frequency.
Subjects were required to train on a contrast threshold task with AO
correction for 1 hour each for 5 consecutive days. During each
training session, 800 trials of threshold CS measurement at the
training frequency with AO were conducted. The same pre-training
measurements were repeated after the 5 training sessions.
Results: Optical quality with AO was confirmed to be similar pre
and post-training and across training sessions. After training, CS with
AO improved by a factor of 1.91 (range: 1.77-2.04) and 1.75 (range:
1.22-2.34) on average over spatial frequencies in the two subjects. In
both subjects, the benefit in CS was measured across a broad range of
spatial frequencies, i.e. at frequencies lower and higher than the one
employed during training. In both subjects, this perceptual learning
effect with gratings transferred to letter VA, improving it by 1.5 lines
(0.04 to -0.1 logMAR) and 1.3 lines (-0.02 to -0.15 logMAR)
respectively. Inter-ocular transfer of training was also observed. The
untrained eye’s CS was improved by a factor of 1.57 on average
across spatial frequencies and VA by 0.8 lines (-0.01 to -0.09
logMAR) in one of the two subjects with AO.
Conclusions: The improvements in visual performance after training
with AO denote an improvement in neural sensitivity. Perceptual
learning with AO thus has the potential to enhance neural function in
abnormal corneal patients leading to improved visual benefit after a
customized correction.
Commercial Relationships: Ramkumar Sabesan, None;
Geunyoung Yoon, Bausch & Lomb (F), Johnson & Johnson (F),
Allergan (C), Staar Surgical (C), CIBA Vision (F), Acufocus (C)
Support: NIH/NEI grant RO1EY 014999, Research to Prevent
Blindness
Program Number: 1283
Presentation Time: 9:30 AM - 9:45 AM
What is the smallest change in visual acuity that is correlated
with a change in image quality?
Ayeswarya Ravikumar, Jason D. Marsack, Yue Shi, Raymond A.
Applegate. College of Optometry, University of Houston, Houston,
TX.
Purpose: The 95% confidence interval for logMAR acuity testing is
~ ±5 letters (±1 line)[ Optom Vis Sci, 1998. 75(5): 342]. Metrics of
image quality (IQ) can quantify 6 just noticeable differences in blur
before 1 line of acuity is lost [J Cataract Refract Surg, 2011. 37(8):
1523] and visual acuity (VA) is highly correlated (R2> 0.8) to change
in metrics of image quality when inducing several lines of change in
acuity. However, the correlation between acuity and metric values is
not known as the change in acuity approaches the test re-test
reliability of acuity. The purpose here is to determine how the
coefficient of determination (R2 ) between change in VA and change
in IQ metric/s value changes as the range is decreased from 8 lines to
the test re-test reliability of acuity measurement (1 line).
Methods: The Thibos virtual eye generator [Opththalmic Physiol
opt, 2009;29(3):288-291] was used to generate 60 WFEs whose log
visual Strehl ratio varied between 0.0 and -1.8 in approximately equal
steps. For each of the 60 WFEs, three unique logMAR acuity charts
were generated (0.8 to -0.3 logMAR). For each chart, VA was
measured up to the 5th letter missed for each of 3 normal subjects.
Change in visual acuity was linearly regressed against change in 29
IQ metrics to determine the coefficient of determination when the
change in visual acuity was decreased in 1 line steps from 8 lines to 1
line.
Results: See Figure. Extrapolation from the fitted line shows that R2
goes to zero at ~3 letters (0.6 of a line), which is below the test retest
reliability for acuity measurement (1 line). With a 2 line loss (or one
line above the 95% confidence level for the measurement of acuity),
42% of the variance in acuity is accounted for by the metrics. The
function begins to asymptote between 4 and 5 lines, and little
improvement in correlation is seen with additional lines of acuity
change.
Conclusions: Image quality metrics can detect blur prior to an acuity
loss (prior work), begin to be correlated with acuity below the re-test
reliability for acuity testing and reach a maximum R 2 > 0.8. These
two experimental observations suggest that IQ metrics can serve as
an objective tool for evaluating and designing therapy intended to
improve visual performance, and that correlations are primarily
limited by the acuity task and not by the IQ metrics.
Commercial Relationships: Ayeswarya Ravikumar, None; Jason
D. Marsack, University of Houston (P); Yue Shi, None; Raymond
A. Applegate, University of Houston (P)
Support: R01 EY08520 (RAA), R01 EY019105 (RAA), P30 EY
07551 (Core Grant), N0025910 P1354 (RAA)
Program Number: 1284
Presentation Time: 9:45 AM - 10:00 AM
Determination of Customized Aberration Thresholds
Carmen Canovas1, 2, Patricia A. Piers1, Silvestre Manzanera2,
Christina Schwarz2, Pedro M. Prieto2, Henk A. Weeber1, Pablo
Artal2. 1R&D, AMO Groningen B.V., Groningen, Netherlands;
2
Laboratorio de Optica, Unversidad de Murcia, Murcia, Spain.
Purpose: Different aberration terms may have lower or higher
impact on vision. This could be used to optimize correction
strategies. We studied the customized level of spherical aberration
(SA) and vertical coma (VC) that can be induced while maintaining
acceptable high contrast visual acuity (VA) and to then determine
whether these levels of aberration affect subjects’ through focus
vision.
Methods: An adaptive optics visual simulator (Fernández, et al. Opt.
Lett. 2001) was used to correct individual aberrations up to the fifth
order and to induce a common higher order aberration baseline (0.15
µm RMS for a 5mm pupil) corresponding to that of an average
pseudophakic eye, in five normal subjects. High contrast VA was
measured with SLOAN letters at the best focus position with a 4mm
physical pupil. Letter size was then increased to correspond to a
decrease in VA by 0.1LogMAR. Thresholds for SA (positive and
negative) and positive VC were then subjectively determined by
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
increasing its value in steps of 0.02 µm until the letter could not be
read.
Results: The threshold value for negative SA was the smallest (0.16±0.04 µm at 5mm pupil), followed by positive SA (0.25±0.05
µm). The custom threshold for VC was consistently the highest
(0.78±0.12 µms), ranging from 0.70 to 0.98 µms.
Monocular through focus VA was measured, both for the baseline
aberration level and after inducing the individual threshold for coma.
In this case, VA for the best focus position decreased by
0.16LogMAR with respect to the baseline, reaching an average
absolute VA of 0.04± 0.04LogMAR. VA decreased linearly as a
function of defocus in both cases, but has a flatter slope when the
individual threshold for VC was induced (0.17LogMAR per diopter
of defocus versus 0.40LogMAR, respectively).
Conclusions: Customized aberration thresholds for individual
Zernike modes were similar for the aberrations studied for all
subjects. The high contrast VA threshold for positive VC was
consistently higher than that for SA demonstrating the robustness of
our visual system to this aberration and indicating that disturbances
resulting in VC, such as decentration of optical surfaces that correct
spherical aberration, may play a less impact on vision than originally
believed. The induction of VC may be advantageous for extending
depth of focus.
Commercial Relationships: Carmen Canovas, AMO Groningen
B.V. (E); Patricia A. Piers, Abbott Medical Optics (E); Silvestre
Manzanera, AMO (F), CIBA Vision (F), CALHOUN (F),
VOPTICA (I); Christina Schwarz, AMO (F); Pedro M. Prieto,
AMO (F), AcuFocus (F), Voptica SL (I), Voptica SL (P); Henk A.
Weeber, AMO Groningen b.v. (E); Pablo Artal, AMO (C), Voptica
SL (P), Voptica SL (I), AMO (F), Calhoun Vision (F), Calhoun
Vision (C), AcuFocus (C)
Support: Ministerio de Ciencia e Innovación, Spain (grants
FIS2010-14926 and CSD2007-00013) and Fundación Séneca
(Region de Murcia, Spain), grant 4524/GERM/06 and AMO.
Program Number: 1285
Presentation Time: 10:00 AM - 10:15 AM
Impact of the Retinal Reflection on the Wide-Angle Point Spread
Function of the Human Eye
Harilaos S. Ginis1, 2, Guillermo M. Perez3, Alexandros Pennos1, Juan
M. Bueno1, Pablo Artal1. 1Laboratorio de Optica, UNIVERSIDAD
DE MURCIA, Murcia, Spain; 2Institute of Vision & Optics,
University of Crete, Heraklion, Greece; 3Voptica SL, Murcia, Spain.
Purpose: Objective measurements of scattered light in the living
human eye require the analysis of double-pass (DP) retinal images.
The inherent wavelength-dependent properties of the retinal
reflection may influence these measurements. The aim of this work
was to measure the wide-angle Point Spread Function (PSF) at
different wavelengths to better understand the role of the fundus
optical properties and to identify the optimal conditions for visually
relevant scattering measurements.
Methods: The instrument, based on the DP principle, used an
extended-source, and allowed the recording of the wide-angle PSF
for different wavelengths. A liquid-crystal wavelength tunable filter
was used to select six different wavelengths ranging from 500 to 650
nm. Series of uniformly illuminated disks with angular size up to 8.1
degrees in radius were sequentially projected onto the ocular fundus.
A technique previously reported (Ginis et al., J. Vision (2012)) was
employed to analyze the DP images and reconstruct the wide-angle
PSF for each wavelength. The complete series of measurements were
performed in 10 healthy Caucasian subjects with different
pigmentation. As an indication of the amount of measured scatter, we
obtained the value of the PSF for small (0.5 degrees) and large (7
degrees) angles.
Results: For small angles, there was a wavelength dependence that
matches the transmittance spectrum of oxy-hemoglobin, what
suggests that diffuse light from the fundus was part of the
reconstructed PSF at longer wavelengths. This contribution of the
fundus is more important for wavelengths longer than 600nm.There
was a different behavior depending on subjects’ pigmentation with
light-colored eyes exhibiting higher intensities of scattered light and
without dependence on wavelength. For larger angles, scatter was
nearly independent of wavelength and subjects’ pigmentation.
Conclusions: The central part of the wide-angle PSF in the eye is
affected by the wavelength dependent properties of the retinal
reflection, which are closely related to subject’s pigmentation. At
those small angles, measurements using wavelengths shorter than
600nm might be better correlated with scatter affecting vision.
However, the impact of the retinal reflection in the values of the PSF
at larger angles did not depend on the measuring wavelength.
Commercial Relationships: Harilaos S. Ginis, Universidad de
Murcia (P); Guillermo M. Perez, VOPTICA (E); Alexandros
Pennos, None; Juan M. Bueno, None; Pablo Artal, AMO (C),
Voptica SL (P), Voptica SL (I), AMO (F), Calhoun Vision (F),
Calhoun Vision (C), AcuFocus (C)
Support: Supported by the Ministerio de Ciencia e Innovación,
Spain (grants FIS2010-14926 and CSD2007-00013), Fundación
Séneca (Region de Murcia, Spain), grant 4524/GERM/06 and EU
ITN OpAL (PITN-GA-2010-264605).
233 Binocular Vision and Age Effects on Vision
Monday, May 06, 2013 8:30 AM-10:15 AM
Exhibit Hall Poster Session
Program #/Board # Range: 1517-1529/B0303-B0315
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 1517 Poster Board Number: B0303
Presentation Time: 8:30 AM - 10:15 AM
Oblique effects in V2 neurons of infant macaque monkeys
Xiaofeng Tao1, Bin Zhang1, 2, Guofu Shen1, Earl L. Smith1, Yuzo M.
Chino1. 1College of Optometry, Unitersity of Houston, Houston, TX;
2
College of Optometry, NOVA Southeastern University, Fort
Lauderdale, FL.
Purpose: The neural basis of oblique effects is elusive. We
previously reported that the spatial matrix of facilitatory subfields
(subunits) in the receptive fields of individual V2 neurons in adult
monkeys exhibits an orientation anisotropy; the homogeneity of the
subfields is greater if a neuron preferred the cardinal orientations
compared to oblique orientations (Tao et al, 2012). In this study, we
asked whether a similar orientation anisotropy (an oblique effect)
exists in V2 of infant monkeys shortly after birth. In addition we
asked whether or not we find an oblique effect if we analyze the
responses of a large number of adult V2 neurons (> 600 units) using
sine-wave grating stimuli.
Methods: Extracellular recording was made in individual V2 neurons
of anesthetized and paralyzed 4-, 8-, and 16-week-old macaque
monkeys. The results from infants were compared to those obtained
in adults. Standard sine-wave grating stimuli were initially used to
determine the preferred orientation, spatial frequency and size of
neuron’s receptive fields. Neurons were classified into vertically,
horizontally, or obliquely oriented units after we determined the
preferred orientation of each neuron. This was followed by the use of
dynamic two dimensional noise stimuli and a reverse correlation
(LSRC) method to obtain the spatial matrix of subfields with
facilitatory profiles.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Results: 1) Using grating stimuli, we found that V2 neurons in adult
monkeys show an oblique effect. 2) The oblique effect in the spatial
matrix of subfields was absent in V2 at 4 and 8 weeks of age but
emerged sometime between 8 and 16 weeks; the average maximal
orientation differences between adjacent subfields were smaller for
those neurons preferring the cardinal orientations.
Conclusions: 1) Our results with grating stimuli represent the first
demonstration of oblique effects in monkey extrastriate cortex. 2)
The oblique effect in the spatial matrix of facilitatory subfields may
not be present at birth, but appears to result from experiencedependent maturation of the connections between V1 and V2.
However, the effects of optical factors including higher-order
aberrations have not been ruled out.
Commercial Relationships: Xiaofeng Tao, None; Bin Zhang,
None; Guofu Shen, None; Earl L. Smith, Ziess (P); Yuzo M.
Chino, None
Support: NIH Grant R01-EY008128 (YMC), R01-EY003611 (ELS),
Core Grant P-30-EY007751
Program Number: 1518 Poster Board Number: B0304
Presentation Time: 8:30 AM - 10:15 AM
Interocular acuity differences alter the spatial frequency tuning
of stereopsis
Ashley Craven1, Truyet Tran1, Kevin Gustafson1, Thomas H. Wu1,
Kayee So1, Dennis M. Levi1, 2, Roger W. Li1, 2. 1School of Optometry,
University of California-Berkeley, Berkeley, CA; 2Helen Wills
Neuroscience Institute, University of California-Berkeley, Berkeley,
CA.
Purpose: It is well known that interocular acuity differences result in
reduced stereo acuity. However, previous studies have used tests that
are broadband in their spatial frequency content. The purpose of the
present study was to investigate the effects of interocular differences
in acuity on the spatial frequency tuning of stereoscopic depth
perception.
Methods: The visual stimulus consisted of two horizontally
separated square blocks, one presented to each eye. Each block
contained a Gabor target patch surrounded by four Gabor reference
patches. Binocular disparity was introduced by shifting the two
Gabor targets in opposite directions (controlled by 2 interleaved
staircases), and a haploscope was used to enable binocular fusion.
Stimulus spatial frequency ranged from 1-20 cyc/deg. The visual task
was to determine the stereoscopic depth of the Gabor target (crossed
disparity: in front of / uncrossed disparity: behind) relative to the four
references. Five adult observers with corrected-to-normal vision were
tested. Bangerter foils were used to reduce visual acuity in the
dominant eye. Stereothresholds were measured for a range of acuity
difference: from 1 to 8 letter-lines on a standard LogMAR letter
chart.
Results: The stereoacuity versus spatial frequency function is
basically the inverse of a typical contrast sensitivity function, with
the optimum spatial frequency at 5- 10 cyc/deg. Increasing the
interocular acuity difference degrades stereo thresholds selectively at
high spatial frequencies, gradually shifting the optimum frequency to
lower spatial frequencies. Interestingly, stereopsis for low frequency
targets was only mildly affected even with an acuity difference of as
much as eight letter-lines (0.8 LogMAR).
Conclusions: The current study shows that interocular acuity
differences result in spatial frequency specific losses of stereopsis.
These findings have important clinical implications for understanding
both the sparing of coarse stereopsis and the deficits in fine stereopsis
in anisometropic amblyopia.
Commercial Relationships: Ashley Craven, None; Truyet Tran,
None; Kevin Gustafson, None; Thomas H. Wu, None; Kayee So,
None; Dennis M. Levi, None; Roger W. Li, None
Support: NIH Grant R01EY01728
Program Number: 1519 Poster Board Number: B0305
Presentation Time: 8:30 AM - 10:15 AM
Enhancing stereoacuity through perceptual learning in normal
vision: Specificity for spatial frequency and orientation
Truyet Tran1, Kayee So1, Calvin Nguyen1, Tszwing Leung3, Sandy
Chat1, Dennis M. Levi1, 2, Roger W. Li1, 2. 1School of Optometry,
University of California-Berkeley, Berkeley, CA; 2Helen Wills
Neuroscience Institute, University of California-Berkeley, Berkeley,
CA; 3School of Optometry, The Hong Kong Polytechnic University,
Hung Hom, Hong Kong.
Purpose: To investigate whether practicing a stereoscopic depth
detection task enhances stereoacuity in adults with normal vision and
whether the learning effects, if any, transfer across target spatial
frequencies and carrier orientations.
Methods: The visual stimulus consisted of two horizontally
separated square blocks, one presented to each eye. Each block
contained a Gabor target patch surrounded by four Gabor reference
patches. A haploscope was used to enable binocular fusion. The
visual task was to determine the stereoscopic depth of the Gabor
target (in front / behind) relative to the four references. Ten adult
observers with corrected-to-normal vision participated. The training
protocol consisted of three training phases (each of 13 sessions). In
Phase 1 observers were trained with targets with a vertical carrier of 5
cyc/deg (V5, vertical). In Phase 2 they continued to train with the
same spatial frequency, but with an orthogonal carrier orientation
(H5, horizontal). They were subsequently required to practice with
targets with a vertical carrier at a higher spatial frequency (V10, 10
cyc/deg) in phase 3. Thresholds for each of the three stimulus
configurations were measured before and after each training phase.
Trial-by-trial feedback was provided.
Results: Our observers showed a substantial mean improvement of
64% in stereo thresholds after practicing with V5 stimuli in phase 1,
and the improvement transferred substantially to the other two
untrained stimulus configurations (H5: 46% and V10: 56%).
Additional significant improvements obtained with subsequent directtraining in phases 2 (H5: 29%) and 3 (V10: 19%) indicate that the
transfers observed in phase 1 were not complete.
Conclusions: Perceptual learning can induce functional plasticity for
enhancing stereovision in the mature visual system. Our findings
characterize the magnitude, time course and specificity of visual
learning. This technique might have important applications in
restoring impaired binocular vision in cortical visual disorders.
Commercial Relationships: Truyet Tran, None; Kayee So, None;
Calvin Nguyen, None; Tszwing Leung, None; Sandy Chat, None;
Dennis M. Levi, None; Roger W. Li, None
Support: NIH Grant R01EY01728
Program Number: 1520 Poster Board Number: B0306
Presentation Time: 8:30 AM - 10:15 AM
Factors influencing stereoacuity levels after surgery to correct
unilateral developmental cataracts in children
Soo Jung Lee1, Nam Eok Kim2, Jung Min Park2. 1Haeundae Paik
Hospital, Busan, Republic of Korea; 2Ophthalmology, Maryknoll
Medical Center, Busan, Republic of Korea.
Purpose: To evaluate factors influencing stereoacuity after surgery to
correct unilateral developmental pediatric cataracts.
Methods: We retrospectively surveyed 110 patients who had
undergone removal of unilateral acquired developmental cataracts
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
and primary posterior chamber intraocular lens implantation between
February 1992 and December 2009. In all patients, stereoacuity was
assessed using the Titmus test at the last follow-up period of
minimum 2 years after surgery. Patients were divided into two groups
according to the extent of stereoacuity: Group 1 (n=42) had
stereoacuity values ≤100 sec/arc and Group 2 (n=68) values >100
sec/arc. The values of ten parameters associated with stereoacuity
were measured in each group: Cataract types, preoperative best
corrected visual acuity (BCVA) of the affected eyes, between-eye
difference in BCVA, age at cataract surgery, operative method, aftercataracts, postoperative strabismus, postoperative BCVA of the
affected eyes, between-eye difference in BCVA, and anisometropia.
Results: The extent of stereoacuity was significantly associated with
both operative method and after-cataract (P=0.000 and P=0.016,
respectively). All patients in whom the posterior capsule was
preserved, had poor stereoacuity >100 sec/arc. Significant
correlations with the extent of stereoacuity were found with
postoperative strabismus (P=0.048), postoperative BCVA of the
affected eyes (P=0.002), anisometropia (P=0.034).
Conclusions: Postoperative stereoacuity was better in patients who
underwent either optic capture or anterior vitrectomy after posterior
continuous curvilinear capsulorhexis, and who didn’t develop aftercataracts or strabismus postoperatively. Furthermore, postoperative
BCVA of the affected eyes, and anisometropia influenced the
stereoacuity of the patients surgically treated for unilateral
developmental pediatric cataracts.
Commercial Relationships: Soo Jung Lee, None; Nam Eok Kim,
None; Jung Min Park, None
Program Number: 1521 Poster Board Number: B0307
Presentation Time: 8:30 AM - 10:15 AM
Do Bangerter filters promote binocular function in amblyopes?
Daming Deng1, Jinrong LI1, 2, Benjamin Thompson3, Minbin Yu1, 2,
Robert F. Hess4. 1State Key Laboratory of Ophthalmology,
Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou,
China; 2Department of Optometry and Vision Science, Sun Yat-sen
University, Guangzhou, China; 3Department of Optometry and
Vision Science, University of Auckland, Auckland, New Zealand;
4
Department of Ophthalmology, McGill University, Montreal, QC,
Canada.
Purpose: Bangerter foils have become an alternative treatment
regimen for amblyopia penalization. We have previously found that
while Bangerter foils can penalize the normal eye, they do so in a
manner that is not graded. In this study, we investigated whether
Bangerter foils promote binocular function within the amblyopic
visual system.
Methods: Suppression thresholds were measured for 17 amblyopes
using our previously established “balance point” protocol combined
with a Gabor direction discrimination task. We compared normal
binocular viewing with viewing conditions where the fellow fixing
eye was penalized with 0.8, 0.6, 0.4 and 0.2 strenght Bangerter foils.
In addition, the effect of Bangerter filters on suppression thresholds
for patients was compared to results from 10 control observers.
Results: The 0.8, 0.6 and 0.4 labeled foils did not influence
suppression in the amblyopic observers. The 0.2 Bangerter foil
reduced suppression thresholds and a binocular balance point was
obtained in 14 out of the 17 subjects.
Conclusions: Bangerter foils do not gradually induce binocular
facilitation. The 0.8 to 0.4 strength Bangerter foils did not predictably
shift the binocular status of amblyopes. Only the most extreme foil
tested, labeled 0.2, reduced suppression among the amblyopic
subjects. Care should be taken when prescribing Bangerter foils in
clinical practice.
Commercial Relationships: Daming Deng, None; Jinrong LI,
None; Benjamin Thompson, US12528934 (P), US8006372B2 (P);
Minbin Yu, None; Robert F. Hess, None
Support: JRL was supported by The Thrasher Research Fund for
Early Career Award, the Fundamental Research Funds of State Key
Laboratory of Ophthalmology, Sun Yat-sen University and the
Guangdong Province Medical Science Research Grant (B2011105).
DDM was supported by the Guangdong Province International
Collaboration Project Grant (2010B050100014).
Program Number: 1522 Poster Board Number: B0308
Presentation Time: 8:30 AM - 10:15 AM
Optimizing binocular vision of pseudophakes with uncorrected
astigmatism
Veerendranath Pesala1, Prashant Garg2, Shrikant R. Bharadwaj1.
1
Prof. Brien Holden Eye Research Centre, L V Prasad Eye Institute,
Hyderabad, India; 2Cornea and anterior segment services, L V Prasad
Eye Institute, Hyderabad, India.
Purpose: Uncorrected astigmatism improves monocular near acuity
of pseudophakes, but with an associated loss in distance vision. The
impact of uncorrected astigmatism on binocularity of these eyes
however remains unknown. This study determined combinations of
astigmatism in the two eyes that simultaneously optimize binocular
distance and near resolution acuity and stereoacuity of bilateral
pseudophakes with monofocal IOL implants.
Methods: Binocular distance (3m) and near (40cm) logMAR acuity
and random-dot stereoacuity (40cm) was measured in 13 emmetropic
pseudophakes with 10 different combinations of astigmatism induced
in random order before the two eyes. Three strategies were chosen
such that one eye had I) no astigmatism or II) 1D simple myopic or
III) 1D simple hyperopic astigmatism at 90° while the fellow eye had
a) the same error or that with b) orthogonal axis (180°) or c) different
magnitude (2.5D) or d) opposite polarity (-1D).
Results: For all combinations of induced astigmatism, the mean
(±1SEM) distance logMAR acuity (0.03±0.03) did not deteriorate
significantly from the best-corrected condition (-0.08±0.02) (p=0.32).
Near logMAR acuity and stereoacuity were in-between the
uncorrected (NVA: 0.59±0.05; Stereo: 232.9±33.9arc sec) and bestcorrected (NVA: 0.18±0.02; Stereo: 60.9±10.2arc sec) conditions for
all myopic astigmatic combinations (Ib & c and IIa - c) and same or
worse than the uncorrected condition for hyperopic astigmatic
combinations (Id, IId & IIIa - c) (p=0.003 to 0.36 for all). All
outcomes variables were closest to their respective best-corrected
values for combination IIc (OD: ±/+1.0x90°; OS: ±/+2.5x90°; DVA:
0.12±0.02; NVA: 0.38±0.03; Stereo: 82.6±8.05arc sec), followed by
IIa (OU: ±/+1.0x90; DVA: 0.04±0.02; NVA: 0.43±0.05; Stereo:
104.5±13.5arc sec) and Ib. Stereoacuity was worse with orthogonal
axes (IIb) than with parallel axes of myopic astigmatism (IIa) in the
two eyes (p=0.002).
Conclusions: Binocular near logMAR and stereo acuity of bilateral
pseudophakes can be simultaneously optimized without hindering
distance vision using combinations of myopic astigmatism in the two
eyes. Leaving such combinations uncorrected after cataract surgery
may be a viable alternative to sphero-cylindrical bifocals in
optimizing the overall binocular visual experience of the patient.
Combinations with astigmatism with orthogonal axes in the two eyes
or with hyperopia deteriorate near vision of pseudophakes.
Commercial Relationships: Veerendranath Pesala, None;
Prashant Garg, None; Shrikant R. Bharadwaj, None
Support: Department of BioTechnology Ramalingaswami
Fellowship, Govt. of India.
Program Number: 1523 Poster Board Number: B0309
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Presentation Time: 8:30 AM - 10:15 AM
Effects of refractive blur and clothing on night-time pedestrian
visibility
Joanne M. Wood, Ralph Marszalek, Trent Carberry, Philippe
Lacherez, Sumanth Virupaksha, Michael J. Collins. School of
Optometry and Vision Science, Queensland University of
Technology, Brisbane, QLD, Australia.
Purpose: To investigate the effects of refractive blur on night-time
pedestrian recognition and whether clothing that has been shown to
improve pedestrian conspicuity is robust to the effects of blur.
Methods: Twenty-four visually normal participants (12 younger
M=25.6 ± 5.2 years and 12 older adults M= 77.6 ± 5.5 years) drove
an instrumented vehicle around a 1.8 km closed road circuit at night
with 3 levels of binocular blur (+0.50 D, +1.00 D, +2.00 D)
compared to a baseline condition (optimal correction). A pedestrian
walked in place on the course and wore either normal clothing (gray
pants and top), black pants and top with a retroreflective vest, or the
same top and vest with retroreflective tape positioned on the
extremities in a configuration that conveyed biological motion
(known as “biomotion”). Participants pressed a vehicle-mounted
response pad when they were first confident that a pedestrian was
present; each participant drove around the track 13 times (4 vision
conditions x 3 pedestrian clothing conditions randomized + 1 practice
trial).
Results: Refractive blur and pedestrian clothing had a significant
effect on pedestrian recognition distances (p<0.05) and there was a
significant two-way interaction between these factors. Overall,
recognition distances were significantly reduced by all levels of blur
compared to the baseline. In all blur conditions, a pedestrian wearing
the “biomotion” clothing was more recognizable than either the
pedestrian wearing the retroreflective vest or normal clothing, and the
pedestrian wearing the retroreflective vest was more recognizable
than when wearing normal clothing, although the magnitude of the
difference became smaller with increasing levels of blur. These
effects were greater for younger adults, older adults showing
generally shorter recognition distances and therefore smaller effects
of either clothing or blur. In the absence of blur, the pedestrian
wearing biomotion clothing was recognized at an average distance of
173 m compared to 18 m in the normal-wear condition (almost 10X
the distance).
Conclusions: Even small amounts of blur have a significant
detrimental effect on night-time pedestrian recognition. Biomotion
configurations of retroreflective clothing represent a highly beneficial
visibility aid which are effective even under moderately degraded
visibility conditions, and improve the recognizability of pedestrians
for both older and younger drivers.
Commercial Relationships: Joanne M. Wood, None; Ralph
Marszalek, None; Trent Carberry, None; Philippe Lacherez,
None; Sumanth Virupaksha, None; Michael J. Collins, None
Support: ARC Linkage LP0990292
Program Number: 1524 Poster Board Number: B0310
Presentation Time: 8:30 AM - 10:15 AM
Pupil Changes under Scotopic and Photopic illumination
Li Chen, Dimitri Chernyak. AMO Development, LLC, Milpitas, CA.
Purpose: To investigate changes in pupil and iris diameter, location
of pupil center and non-circularity of pupil under scotopic and
photopic illumination.
Methods: Scotopic and photopic eye images of 98 eyes from 49
subjects (age range, 26 to 75 years) with normal eyes were captured
using the pupillometer of iDesign Wavefront Studio (AMO
Development, LLC). The pupillometer operated by capturing a pair
of images of the eye illuminated by a combination of IR and NIR
LEDs for scotopic illumination and a pair of green LEDs for scotopic
illumination. The scotopic image was captured first, then the green
LEDs were turned on and the photopic image was captured. The
scotopic and photopic eye images were then analyzed to locate pupil
and iris limbus boundary. Pupil boundary and iris boundary were
fitted with a best-fitting circle to locate the center and diameter. The
shift in pupil position relative to the cornea was calculated from the
pupil center and iris center from scotopic and photopic images. Pupil
boundary was also fitted with a best-fitting ellipse and the noncircularity of pupil was calculated from the major diameter and minor
diameter of the best-fitting ellipse.
Results: Under photopic illumination, the mean pupil diameter was
4.26 mm ± 0.95 (SD) (range 2.08 to 7.13 mm), and the mean iris
diameter was 12.03 mm ± 0.31 (SD) (range 11.22 to 12.67 mm);
Under scotopic illumination, the mean pupil diameter was 6.09mm ±
1.00 (SD) (range 3.43 to 8.13 mm), and the mean iris diameter was
12.03 mm ± 0.32 (SD) (range 11.45 to 12.69 mm). Pupil diameter
decreased as a function of age was observed both in photopic and
scotopic conditions. Iris diameter also showed a 0.24 mm average
decrease in aged eyes of the over 60s (unpaired t-test, p=0.002) both
under photopic and scotopic illumination. With changes of pupil
diameter from photopic and scotopic illumination, the mean pupil
center shifting toward temporal to cornea center was 0.064 mm ±
0.045 (SD) (range 0.004 to 0.293 mm). On average, the pupil noncircularity was 0.037 from the 98 photopic eyes and 0.046 from the
98 scotopic eyes.
Conclusions: This study not only confirmed pupil diameter decrease
with aged eyes, but also observed decreased iris diameter in aged
eyes. Pupil center shifted temporally from the cornea center with
changes of pupil diameter under scotopic illumination. Noncircularity of pupil increased on average with the increased pupil
diameters under scotopic illumination.
Commercial Relationships: Li Chen, Abbott Medical Optics Inc
(E); Dimitri Chernyak, Abbott Medical Optics (E)
Program Number: 1525 Poster Board Number: B0311
Presentation Time: 8:30 AM - 10:15 AM
The Correlation between Visual Acuity, Refraction and Cognitive
Function in the Elderly
Oriel Spierer1, Naomi Fischer1, Adiel Barak1, Michael Belkin2.
1
Ophthalmology, Tel Aviv Sourasky Medical Center, Tel Aviv,
Israel; 2Ophthalmic Technologies Laboratory, Goldschleger Eye
Research Institute, Tel Aviv University, Tel Hashomer, Israel.
Purpose: To study the correlation between visual acuity, refraction
and cognitive state in an elderly population, with no known dementia
or Alzheimer's disease.
Methods: A cross sectional study was conducted, comprising of 200
subjects age 75 and older from adult day care centers. Near visual
acuity was tested using the Jaeger chart and refraction was examined
by a portable auto-refractometer. Cognitive function was evaluated
with the mini-mental state examination (MMSE). The eye with better
visual acuity and no cataract or refractive surgery was used for
analysis. Patients that underwent cataract or refractive surgery in both
eyes were excluded. Correlation tests were used to find association
between visual acuity, refraction, wearing eyeglasses for near or far
vision and cognitive functions.
Results: One hundred and ninety five subjects (mean age 81.6 ± 5.1
years, 70.3% females) fulfilled the inclusion criteria and comprised
the study population. The mean period of education was 9.2 ± 4.6
years (range 0-25). Mean Jaeger near visual acuity was J3.3 ± 3.1
(range J1-J16). Mean refractive error was 0.52 ± 2.33 (range +4.625
to -5.625). Eyeglasses for near vision were used by 124 (63.6%)
participants and 128 (65.6%) participants used eyeglasses for
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
distance vision. Mean MMSE was 24.9 ± 4.0 points (range 15-30).
Good near visual acuity (J3 or lower) was found to be associated with
high MMSE score (>24) (OR=3.74, 95% CI=1.86-7.52, p<0.001) and
remained significant after adjustment for sex, age and years of
education. Wearing eyeglasses for near or far vision were found to be
correlated with high MMSE score after adjustment for sex and age
(OR=1.95, 95% CI=1.06-3.57, p=0.03, OR=1.94, 95% CI=1.05-3.59,
p=0.04, respectively) but did not after adjustment for years of
education. A trend was found toward correlation between myopia and
better MMSE score (r=-0.12, p=0.09, Pearson's correlation) although
it did not remain so after adjusting for sex, age or education.
Conclusions: Good near visual acuity and wearing eyeglasses for far
or near vision seem to be correlated with better cognitive function.
The nature of the relationship between visual and cognitive functions
and possible causality needs to be further investigated.
Commercial Relationships: Oriel Spierer, None; Naomi Fischer,
None; Adiel Barak, None; Michael Belkin, Alcon (C), Ellex (C),
PCT: IL2011/000373 Filed 9/5/2011 Published (P)
Program Number: 1526 Poster Board Number: B0312
Presentation Time: 8:30 AM - 10:15 AM
Relationship between dynamic vision and balance in older adults
Allen M. Cheong1, Kar Ho Siong1, William Tsang2, 3, Ho Lung Henry
Chan1, 3. 1School of Optometry, Hong Kong Polytechnic University,
Hung Hom, Kowloon, Hong Kong; 2Department of Rehabilitation
Sciences, The Hong Kong Polytechnic University, Hung Hom, Hong
Kong; 3Institute of Active Ageing, Faculty of Health and Social
Sciences, The Hong Kong Polytechnic University, Hung Hom, Hong
Kong.
Purpose: Deteriorated visual function is one important risk factor for
the detrimental balance control in older adults. Most studies
examined the relationship between static visual and balance
functions, largely ignoring that between dynamic vision and balance.
In this study, we examined dynamic visual function and its
interaction with balance in young and old people.
Methods: Fifteen younger (aged 21-40 years) and twelve
community-dwelling participants (60 years or above) with normal
vision were recruited. Visual acuity (VA) and contrast sensitivity
(CS) were measured by Psykinematix for stimuli of different
optotypes or gratings moving at 5 different speeds (0, 15, 30, 60 and
90 deg/sec). Static balance was measured by a force platform when
the participant stood on a firm or foam surface while fixating at
different targets. Dynamic balance was measured by limits of
stability test where the participants were asked to make a
corresponding weight shift as maximal as possible within their base
of support to 8 positions whenever individual stimulus representing
the weight shift at a particular position showed in the monitor.
Results: VA and CS significantly deteriorated for recognizing
moving objects as the speed increased. However, such deterioration
became plateau when the moving speed reached 30 deg/sec, where
the young group performed better (p<0.05). Age-related decline was
only found in CS (p<0.001), but not in VA. Standing on a compliant
foam surface imposed significant impediment on postural control
(p<0.05). Both static (in terms of total sway area) and dynamic
balance (in terms of averaged maximum excursion at 8 orientations)
were significantly impaired in the older group (p<0.05), however the
extent of deterioration was much stronger in the dynamic (rs=-0.682)
than static balance (rs=0.10). Multivariate analyses showed that
dynamic vision could weakly correlate with static balance (rs= 0.01),
but significantly correlate with dynamic balance (rs=-0.514).
Conclusions: As a consequence of aging, both visual and balance
functions were significantly deteriorated. However, stronger agerelated decline occurred when both vision and balance were
measured in dynamic perspective. In addition to age, a much stronger
relationship was established between dynamic vision and dynamic
balance, implying that a person with poorer dynamic vision has
weaker dynamic balance control.
Commercial Relationships: Allen M. Cheong, None; Kar Ho
Siong, None; William Tsang, None; Ho Lung Henry Chan, None
Support: PolyU Internal Grant - A-PJ67 & A-PL43
Program Number: 1527 Poster Board Number: B0313
Presentation Time: 8:30 AM - 10:15 AM
Effect of Visual Function on Giving and Receiving Help in an
Older Adult Population
Monique J. Leys1, Priyanka Jain1, Merideth Smith2, G. Jamie Miller1,
Kenneth B. Mitchell1, J V. Odom1. 1WVU Eye Institute, Morgantown,
WV; 2Psychology, WVU, Madison, WI.
Purpose: To determine the relationship of measures of visual
function and reported giving and receiving help in an older adult
population.
Methods: 100 persons participated in a telephone interview to
determine the relationship of volunteering or giving help, and help
received on depression and suicidal ideation in the elderly. The
specific measures of giving help were responses to the questionnaires
Volunteering (V) and Informal Support Provided (ISP); measures of
help received were Perception of Support Received (PSR) and
Informal Support Received (ISR). ISR had several subscales
Tangible Support (ISR-T), Instrumental Support (ISR-I), Emotional
Support (ISR-E) and Total (ISR-TOT). Patients were aged 60 years
or more (mean: 73.48 years; range 60-94) and passed standard
cognitive tests to rule out dementia. 55 were female and 45 were
male. Participants were patients at the WVU Eye Institute whose
vision ranged from normal to severe visual impairment. A chart
review determined the visual acuities, ocular disease, duration of
disease, and visual fields. Visual acuities of the better and worse
seeing eyes (VA-B and VA-W) were converted to LogMAR values.
The visual field (VF) information in the charts was converted to a 4point rating scale of binocular field loss severity. Disease duration
(DD) was expressed in years. Using correlation analyses and stepwise
regression, we determined which of the independent variables (IV)
predicted reports of giving or receiving help.
Results: Stepwise regression indicated a significant relationship of
visual variables to V (p < 0.00126; Multiple R-squared = 0.15 with
VA-B, VF, and DD as the significant IVs), to PSR (p<0.00052;
Multiple R-squared = 0.17 with VA-B, VA-W and VF as the IVs),
and ISR-T (p < 0.000697; Multiple R-squared = 0.14 with VA-B and
DD as the IVs). Measured visual functions did not predict ISP, ISR-I,
ISR-E and ISR-TOT significantly.
Conclusions: Our data provide additional support for the importance
of visual function as an influence on the prosocial behavior of older
adults. Better visual function is associated with more volunteering,
but influence the informal support that older adults provide others.
Poorer visual function is associated with the receipt of tangible
assistance, but does not influence receipt of other informal assistance.
Commercial Relationships: Monique J. Leys, None; Priyanka
Jain, None; Merideth Smith, None; G. Jamie Miller, None;
Kenneth B. Mitchell, None; J V. Odom, None
Support: Research to Prevent Blindness Challenge Grant
Program Number: 1528 Poster Board Number: B0314
Presentation Time: 8:30 AM - 10:15 AM
Online Assessment of Contrast Sensitivity and Hallucinations in
Parkinson’s Disease
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Mary Lou Jackson1, Jennifer Wallis1, Paul Wicks2, Peter Bex1.
1
Harvard Dept of Ophthalmology, Massachusetts Eye & Ear
Infirmary, Boston, MA; 2PatientsLikeMe Research, Boston, MA.
Purpose: To assess contrast sensitivity (CS) and visual hallucinations
(VH) in individuals with Parkinson’s disease. Patients with
Parkinson’s disease who experience hallucinations may show
impaired CS, a relationship previously reported in people with low
vision who experience Charles Bonnet Syndrome.
Methods: A total of 964 members of the online patient community
‘PatientsLikeMe’ were invited via email to participate in this study.
269 members completed the study; 153 of this group were patients
with Parkinson's disease, 116 were controls (other disorders).
Participants completed, online, a modified version of the University
of Miami Parkinson’s Disease Hallucinations Questionnaire (UMPDHQ) and a test of CS similar to the Pelli Robson chart.
Results: Results from the UM-PDHQ showed that 18% of people in
the Parkinson’s group currently experienced VH versus 9% in the
control group. Hallucinations reported by participants with
Parkinson’s disease included mice, cats, people, distorted faces,
furniture or complex patterns.
Both groups, participants with Parkinson’s disease (M: 1.85, SD: .36)
and the control group (M: 1.75, SD: .35) showed relatively good CS
as measured with the online letter test (F(1, 269)= 1.49, p=.22).
Individuals with current VH showed relatively low CS scores (M:
1.69, SD: .36) compared to individuals who had never had VH
(M:1.81, SD: .35), or had previously (M: 1.80, SD: .37) experienced
VH. This difference, however, did not reach statistical significance
(F(2, 263)= 1.55, p= .22). CS differences in the Parkinson’s disease
group between those with VH (M: 1.69, SD: .34) and those with no
current VH (never VH - M: 1.77, SD: .34, VH but not in past month M: 1.74, SD: .40) were small.
Conclusions: More patients with Parkinson’s disease reported visual
hallucinations than the control group, however, both groups showed
relatively good CS.
Interestingly, participants who reported VH, irrespective of disease
status, showed relatively low CS compared to participants who did
not. This difference is of clinical interest.
Contacting subjects via an online health social network is a novel
method of conducting vision research that allows large numbers of
individuals to be contacted quickly, including those in remote
communities.
Commercial Relationships: Mary Lou Jackson, None; Jennifer
Wallis, None; Paul Wicks, PatientsLikeMe (E), Abbott (F), Acorda
(F), Avanir (F), Biogen (F), Genzyme (F), Johnson & Johnson (F),
Merck (F), Novartis (F), Sanofi (F), UCB (F), PatientsLikeMe (I);
Peter Bex, Adaptive Sensory Technology, LLC (S), Rapid
Assessment of Visual Sensitivity (P)
Program Number: 1529 Poster Board Number: B0315
Presentation Time: 8:30 AM - 10:15 AM
Contrast acuity in Lewy Body Disease
Helene Kergoat1, 2, Guillaume Carcenac1, Mireille Parent1. 1School
of Optometry, University of Montreal, Montreal, QC, Canada;
2
Institut universitaire de gériatrie de Montréal, Montreal, QC,
Canada.
Purpose: Lewy Body Disease (LBD) is a neurodegenerative disease
affecting older individuals, that is characterized by visual
hallucinations, fluctuations in cognition and parkinsonism. It is
associated with deficits in both the dopaminergic and cholinergic
systems. These neurotransmitters play a role in the processing of
visual information. Therefore, the present study was undertaken to
verify if contrast acuity was altered in LBD.
Methods: Twelve participants with a confirmed diagnosis of LBD
(Avg: 76.0 yrs ± SD 6.1) and 12 age-matched controls (Avg: 75.1 yrs
± SD 6.5) were recruited for the study. All subjects received a
complete eye examination prior to testing to ensure that they had a
visual acuity better than 20/30 and good ocular health. The eye with
best corrected visual acuity was chosen for testing. Contrast
sensitivity and contrast acuity were measured at an 8 foot distance
with a retroilluminated CSV-1000 system (VectorVision) having a
mean luminance of 85 cd/m2. Contrast sensitivity was measured with
the CSV-1000E chart test face for 4 spatial frequencies: 3, 6, 12 and
18 cycles per degree (cpd). Contrast acuity was measured with the
CSV-1000CVA20/30 chart test face for 3 contrast levels: 100%, 9%
and 6%. Statistics consisted of ANOVAs for an alpha level of 0.05.
Results: Our results indicated that the contrast sensitivity was
significantly reduced in subjects with LBD for the 3, 12 and 18 cpd
gratings (p< 0.01). Contrast acuity was also reduced in subjects with
LBD, for all contrast levels tested (p< 0.01).
Conclusions: These results show that LBD is associated with a
reduction in contrast acuity for both gratings and letters. These
findings may be related to dopaminergic/cholinergic deficits, or to
structural anomalies known to occur in the retina of individuals with
LBD.
Commercial Relationships: Helene Kergoat, None; Guillaume
Carcenac, None; Mireille Parent, None
Support: Fondation Caroline-Durand, COETF
246 Cone Photoreceptors in Aging and Disease
Monday, May 06, 2013 11:00 AM-12:45 PM
TCC LL 4/5 Paper Session
Program #/Board # Range: 1740-1746
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 1740
Presentation Time: 11:00 AM - 11:15 AM
Cone Distribution Variations for Young Healthy Subjects vs.
Older Subjects
Ann E. Elsner1, Toco Y. Chui1, Lei Feng1, 2, Colleen M. McIntyre1,
Hongxin Song1, 3, Thomas Gast1, Stephen A. Burns1. 1Optometry,
Indiana University, Bloomington, IN; 2Second Affiliated Hospital,
College of Medicine, Zhejiang University, Zhejiang, China; 3Center
for Visual Science, University of Rochester, Rochester, NY.
Purpose: To compare the individual differences in cone distribution
with age, minimizing the effects of eye length and retinal disease. To
distinguish between cone density variations related to foveal
specialization, as opposed to more global factors or aging.
Methods: Subjects who had a normal fundus and axial length < 26
mm were divided into 2 groups, with age = 18 - 35 yr for the 47
subjects in the younger group and 50 - 70 yr for the 17 subjects in the
older group. Cone densities were quantified using a second
generation Adaptive Optics Scanning Laser Ophthalmoscope. Cones
were imaged using 820 to 840 nm +/- 20 nm at approximately 100
microwatts, illuminating 530 x 550 microns of the retina. Samples
collected in a + shape around the fovea were montaged. Cones were
counted at a nominal 270, 630, 1480, and 2070 microns from the
foveal center using custom software (Matlab, Mathworks). To reduce
shadowing from large retinal vessels, temporal meridian data were
used. Axial length measurements were used to correct the cone
sampling positions and retinal area in mm2 (IOL Master, Zeiss
Meditec). A subset of data were refit to a 2 parameter exponential
model.
Results: Cone density was greater on average for the younger group,
but had substantial variability and overlap with the older group. The
refit data from 36 younger subjects matched the 2 parameter
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
exponential model sufficiently well that 97% had R2 > 0.9; but the
parameters differed, and 92% of the data were slightly too steep.
These cone densities averaged 43,200, 27,500, 15,000, and 12,200
microns per mm2, for the 270, 630, 1440, and 2070 micron locations,
with a coefficient of variation of .14, .13, .10, and .10. Cone density
at 630 microns was negatively correlated with the ratio of cones at
2070: cones at 630, p < .0001 and p = .0008 for the younger and
older groups, respectively, and uncorrelated to the (unnormalized)
density at 2070 microns, p = 0.71 and 0.37. The ratio of cones at
2070: cones at 630 averaged 0.45 vs. 0.39, for younger vs. older eyes.
Conclusions: Cone density is not characterized by a scalar factor for
either eccentricity or age, nor a model with fixed exponents. Instead,
cones from outside the fovea migrate centrally to provide foveal
specialization, and aging further alters the distribution.
Commercial Relationships: Ann E. Elsner, Aeon Imaging, LLC
(I), Aeon Imaging, LLC (F), Aeon Imaging, LLC (P); Toco Y. Chui,
None; Lei Feng, None; Colleen M. McIntyre, None; Hongxin
Song, Canon (F); Thomas Gast, None; Stephen A. Burns, None
Support: NIH Grant EY007624, EY004395, P30EY019008
Program Number: 1741
Presentation Time: 11:15 AM - 11:30 AM
Longitudinal Cone Density Measurements using a Commercially
Available Flood-Illuminated Adaptive Optics Camera in
Japanese Macaque Monkeys with Dominantly Inherited Drusen
Mark E. Pennesi1, Keith V. Michaels1, Shu Feng1, Travis B. Smith1,
Anupam K. Garg1, Trevor J. McGill2, Laurie Renner2, Marvin
Sperling3, Kay D. Rittenhouse3, Martha Neuringer2. 1Ophthalmology,
Casey Eye Institute - OHSU, Portland, OR; 2Division of
Neuroscience, Oregon National Primate Center, Beaverton, OR;
3
External R&D Innovations, Pfizer Inc., San Diego, CA.
Purpose: To study the longitudinal changes in cone density in a line
of adult Japanese Macaque monkeys with dominantly inherited
drusen using a commercially available flood illuminated adaptive
optics camera.
Methods: Twenty male and female Japanese Macaques were sedated
and imaged on the RTx1 Adaptive Optics Camera (Imagine Eyes,
Orsay, France) at baseline and six months later. In each animal, a
series of overlapping AO images were obtained starting at the optic
nerve and extending temporally through the fovea. Individual images
were montaged using I2k Align (DualAlignTM). Cone profiles were
counted using a Matlab algorithm (generously provided by Dr.
Joseph Carroll) and axial lengths were measured to correct for
magnification. Macular drusen were identified with advanced Weka
segmentation (University of Waikato).
Results: Cone density plots revealed an anatomic distribution of cone
photoreceptors in the macula, but cones within 1.6° of the foveal
center could not be individually identified. The mean cone density
across 1.6-3.1° eccentricity was 28843 ± 5284 cones/mm2 after six
months. When broken into parafoveal quadrants, cone density was
highest in the nasal quadrant and lowest in the superior quadrant for
both time points. The mean baseline age for the animals was 10.8 ±
5.5 years. Age was not significantly associated with cone density (p =
0.46), nor was it associated with the change in cone density between
the time points (p = 0.75). The fraction of area occupied by drusen
was 8.8 ± 12.8 percent. Drusen area also was not significantly
associated with cone density (p = 0.55), nor was it associated with the
change in cone density between the time points (p = 0.70).
Conclusions: Commercially available flood illuminated adaptive
optics allows for longitudinal measurement of cone density in
macaques with drusen. Preliminary results indicate that age and
drusen load are not associated with a significant change in cone
density over the period studied. Further collections are planned every
six months to assess long-term changes in cone density.
Commercial Relationships: Mark E. Pennesi, Pfizer (F); Keith V.
Michaels, Pfizer, Inc. (F); Shu Feng, None; Travis B. Smith, Pfizer,
Inc. (F); Anupam K. Garg, None; Trevor J. McGill, StemCells,
Inc. (C), Pfizer (F), AGTC (F); Laurie Renner, Pfizer (F), Applied
Genetic Technologies Corporation (F); Marvin Sperling, Pfizer Inc.
(E); Kay D. Rittenhouse, Pfizer Inc. (E); Martha Neuringer, Pfizer
(F), Applied Genetic Technologies Corporation (F)
Support: Pfizer Ophthalmology External Research Unit, FFB CDCL-0808-0469-OHSU, RPB CDA (MEP), RPB Unrestricted - CEI,
NIH grant P51OD011092
Program Number: 1742
Presentation Time: 11:30 AM - 11:45 AM
Assessing the Mosaic of Cone Photoreceptors Overlying
Subretinal Drusenoid Deposits in vivo Using Adaptive Optics
Sarah Mrejen1, 2, Taku Sato1, 2, Richard F. Spaide1, 2. 1vitreous retina
macula consultants of New York, New York, NY; 2LuEsther T Mertz
Retinal Research Center, Manhattan Eye, Ear and Throat Hospital,
New York, NY.
Purpose: To investigate the cone photoreceptor mosaic in eyes with
pseudodrusen as evidenced by the presence of subretinal drusenoid
deposits (SDD) using adaptive optics (AO) imaging integrated into a
multimodal approach.
Methods: Consecutive patients with pseudodrusen were examined
using near-infra-red reflectance (IR) confocal scanning laser
ophthalmoscopy (SLO) and eye-tracked spectral-domain optical
coherence tomography (SD-OCT) and a flood-illuminated retinal AO
camera prototype (rtx-1, Imagine Eyes, Orsay, France). The AO
images were acquired between 1 and 5 degrees of retinal eccentricity
from the foveal center in the areas of SDD. Correlations were made
between the IR SLO, SD-OCT and the AO images. Cone packing
density analysis was performed on AO images within 50 x 50 µm
windows in 5 regions of interest overlying and in 5 located between
SDD. Five patients with soft drusen were evaluated as a comparison
group.
Results: The mean age of 5 patients, all female, with SDD was 71.8
years. The SDD identified by combined IR and eye-tracked SD-OCT
corresponded to well-defined areas darker than the surrounding
uninvolved areas in the AO images. The mean (±SD) cone packing
density was 1254 (± 673) cones/mm2 on SDD and 10818 (±1860)
cones/mm2 between SDD. Cone density on SDD was approximately
11% of cone density between SDD, whereas cone density on soft
drusen varied from 60 to 90% of cone density between soft drusen.
The cone density between SDD was not significantly different from
the cone density between soft drusen at the same degree of retinal
eccentricity. The lack of visualization of cones on SDD was
correlated with the disruption of the ellipsoid zone on corresponding
SD-OCT. The cone mosaic was well preserved on soft drusen when
the ellipsoid zone was preserved on corresponding SD-OCT.
Conclusions: The lack of visualization of cones on SDD in the AO
images can be due to several possible causes: a change in their
orientation, absence or shortening of their outer segments, or absence
of the cones. Whether the lack of detection of cones on SDD is due to
absent or shortened outer segment or absence of cones, all of these
explanations imply decreased cone function is possible. These
findings suggest these patients with pseudodrusen may experience
decreased retinal function independent of choroidal
neovascularization or retinal pigment epithelium atrophy.
Commercial Relationships: Sarah Mrejen, None; Taku Sato,
Alcon Japan Ltd. (F); Richard F. Spaide, Topcon (P),
Thrombogenics (C), Bausch and Lomb (C)
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 1743
Presentation Time: 11:45 AM - 12:00 PM
Adaptive Optics Scanning Laser Ophthalmoscopy in Stargardt
Disease Reveals Decreased Cone and Rod Densities
Hongxin Song1, Angela Pugliese2, Ethan A. Rossi1, Lisa R. Latchney2,
Edwin M. Stone3, Alfredo Dubra4, Jennifer J. Hunter1, 2, Mina M.
Chung1, 2. 1Center for Visual Science, University of Rochester,
Rochester, NY; 2Flaum Eye Institute, University of Rochester,
Rochester, NY; 3Ophthalmology and Visual Science, University of
Iowa, Iowa City, IA; 4Ophthalmology, University of Wisconsin,
Milwaukee, WI.
Purpose: Stargardt disease (SD) is defined clinically by its
ophthalmoscopic features including atrophy and lipofuscin deposition
in the retinal pigment epithelium (RPE). The causative ABCA4 gene
encodes a protein uniquely expressed in the cone and rod outer
segments. The pathologic steps by which mutations in ABCA4 lead
to the clinically detectable RPE changes remain unclear. We
investigated whether photoreceptor changes precede RPE loss in SD
using adaptive optics scanning laser ophthalmoscopy (AOSLO).
Methods: Two brothers with SD, aged 8 and 17 years, underwent a
comprehensive eye examination and conventional imaging including
fundus photography and optical coherence tomography (OCT).
Genetic testing was performed using a combination of allele-specific
testing and sequencing of the ABCA4 gene. AOSLO images were
obtained at the central fovea and along the inferior and temporal
meridians to generate 10x1.5 degree montages. The center of the
foveal avascular zone was used as the foveal center. Cones were
counted using custom semi-automated cone marking software.
Peripheral cones and rods were counted at 100 µm intervals in
100x100 µm and 50x50 µm windows respectively. At the foveal
center, cones were counted in a 50x50 µm window.
Results: Genetic testing showed the presence of three likely diseasecausing mutations: Gly863Ala, Gly1961Glu, and Arg2030Stop. The
older brother had visual acuity 20/150 with a central scotoma and
macular RPE atrophy with no peripheral flecks. His brother had
visual acuity 20/30 with subtle RPE stippling in the macula. In both
brothers, OCT confirmed central retinal thinning. AOSLO revealed
that rod density was decreased to ~30% of normal in the peripheral
macula; these areas appeared normal by ophthalmoscopy and OCT.
Cones in the peripheral macula showed a dark, low reflective
appearance with density 30% of normal. No cones were detectable in
the foveal center of the older brother. In the younger brother, foveal
cones were enlarged with low density.
Conclusions: This study provides the first in vivo images of both
rods and cones in SD. Although the primary clinical features of SD
are changes in the RPE, AOSLO reveals decreased density of both
cones and rods in areas that appear normal by conventional imaging
methods. These findings suggest that loss of cone and rod
photoreceptors precedes clinically detectable RPE disease in SD.
Commercial Relationships: Hongxin Song, Canon (F); Angela
Pugliese, None; Ethan A. Rossi, Canon Inc. (F); Lisa R. Latchney,
None; Edwin M. Stone, None; Alfredo Dubra, US Patent No:
8,226,236 (P); Jennifer J. Hunter, Polgenix, Inc. (F); Mina M.
Chung, Canon (F)
Support: NEI EY021786, EY014375, EY001319, Edward N. &
Della L. Thome Memorial Foundation to Mina Chung, Research to
Prevent Blindness Unrestricted/Challenge Grant, Burroughs
Wellcome Fund to Alfredo Dubra-Suarez
Program Number: 1744
Presentation Time: 12:00 PM - 12:15 PM
Cone structure imaged with Adaptive Optics Scanning Laser
Ophthalmoscopy in eyes with Non-Neovascular Age-related
Macular Degeneration
Shiri Zayit-Soudry1, Reema Syed1, Kavitha Ratnam1, Moreno
Menghini1, Austin Roorda2, Jacque L. Duncan1.
1
Ophthalmology/Retina Division, University of California, San
Francisco, San Francisco, CA; 2School of Optometry, University of
California, Berkeley, Berkeley, CA.
Purpose: To evaluate cone structure using Adaptive Optics Scanning
Laser Ophthalmoscopy (AOSLO) in eyes with non-neovascular age
related macular degeneration (AMD), and to correlate progression of
AOSLO-derived cone measures with standard measures of macular
structure. High resolution imaging of cone photoreceptor morphology
and quantitative measures of cone structure may enhance
understanding of the pathophysiology of vision loss in AMD and
provide a sensitive biomarker for disease progression.
Methods: AOSLO macular images were obtained over 12 to 21
months from 7 patients with non-neovascular AMD including 4 eyes
with geographic atrophy (GA) and 6 eyes with drusen. AOSLO
images were precisely superimposed onto color, infrared and
autofluorescence fundus photographs and spectral domain optical
coherence tomography (SD-OCT) images to allow direct correlation
of cone parameters with macular structure. Cone spacing was
measured for each visit in selected regions including areas over
drusen (n=29), at the margin of GA (n=14), and regions without
evidence of drusen or GA on fundus photos or SD-OCT (n=13) and
compared to normal, age-related values.
Results: AOSLO imaging revealed intact cones up to the GA edge
and overlying drusen, although subtle mosaic irregularity and
reduced reflectivity often resulted in a dark signal surrounding GA
margins and drusen. At baseline, cone spacing measures were normal
at all study locations but 2 GA margin locations and 4 drusen
locations. Although progression of GA was observed in most study
eyes with standard clinical measures, AOSLO longitudinal tracking
showed mild increases in cone spacing in 3 drusen locations, but
stable cone spacing measures in all other drusen and GA margin
locations.
Conclusions: AOSLO provides adequate resolution for quantitative
measurement of cone structure at the margin of GA and over drusen
in eyes with non-neovascular AMD, providing insight into the
pathophysiology of GA progression. Despite reflectivity changes
noted over drusen and at GA margins, cone spacing was often
preserved at these locations and remained stable over time,
suggesting changes in cone spacing may not represent a primary
structural change in AMD progression.
Commercial Relationships: Shiri Zayit-Soudry, None; Reema
Syed, None; Kavitha Ratnam, None; Moreno Menghini, None;
Austin Roorda, US Patent #6890076 (P), US Patent #7118216 (P),
UC Berkeley (P); Jacque L. Duncan, None
Support: NIH EY014375, Novartis Institutes for Biomedical
Research, NEI Core grant EY002162, American Health Assistance
Foundation (AHAF) Macular Degeneration Research Grant (MDR),
Foundation Fighting Blindness, Research To Prevent Blindness, That
Man May See
Program Number: 1745
Presentation Time: 12:15 PM - 12:30 PM
Adaptive Optics Imaging of Photoreceptors following Repair of
Rhegmatogenous Retinal Detachments
Meenakashi Gupta1, Michael Dubow1, 2, Alexander Pinhas1, 2, Nishit
Shah1, Patricia Garcia1, Gennady Landa1, Yusufu N. Sulai3, Alfredo
Dubra4, Richard B. Rosen1. 1New York Eye and Ear Infirmary, New
York, NY; 2Mount Sinai School of Medicine, Mount Sinai Hospital,
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
New York, NY; 3University of Rochester, Rochester, NY; 4Medical
College of Wisconsin, Madison, WI.
Purpose: Patients with macula-off rhegmatogenous retinal
detachments can have poor visual recovery or metamorphopsia
despite successful retinal reattachment. Subtle changes in the foveal
structure, causing such visual disturbances, can be difficult to identify
with standard examination and imaging tools. Adaptive Optics (AO)
allows in vivo imaging of individual photoreceptors. Using an AO
scanning laser ophthalmoscope, we evaluated the foveal
photoreceptor appearance following repair of macula-off retinal
detachments. AO images were compared with infrared and OCT
imaging. Visual acuity and microperimetry were obtained for
functional correlation.
Methods: Three patients who had previously undergone
anatomically successful repair of rhegmatogenous macula-off retinal
detachments were evaluated with AO following reattachment
surgery. AO videos were recorded using a 790 nm light source and 1
degree field of view. Motion contrast images from several videos
were used to create montages yielding a 2.5 degree field of view
centered around the foveal depression. Montages from the affected
eye were compared with corresponding montages from the unaffected
eye. Spectralis infrared imaging (870 nm), Spectralis OCT, visual
acuity and OCT/SLO microperimetry (Opko/OTI) were also
obtained.
Results: In reattached retina, the appearance of mottling of the
macula with infrared imaging (Fig 1A) and hyporeflectivity of the
foveal IS/OS junction using OCT (Fig 1B) corresponded to patchy
disruption of the foveal photoreceptor mosaic with AO imaging (Fig
1C). These findings were associated with reduced visual acuities and
threshold sensitivities on microperimetry (Fig 2).
Conclusions: AO imaging of repaired macula-off retinal
detachments demonstrated disruptions of the photoreceptor mosaic in
regions of abnormal fundus infrared signal, irregular IS/OS junction
and reduced visual function. Further AO studies will help us better
understand microstructural and pathophysiological changes following
retinal detachment repair.
Figure 1: A) Infrared imaging of a 43-year-old woman 6 weeks
following macula-off retinal detachment repair shows mottling of the
macula. B) OCT of the fovea with hyporeflective regions in the
IS/OS junction (Red). C) AO of foveal photoreceptors showing dark
patches interrupting the photoreceptor mosaic.
Figure 2: Microperimetry corresponding to Figure 1 showing
depressed sensitivity within the macula.
Commercial Relationships: Meenakashi Gupta, None; Michael
Dubow, None; Alexander Pinhas, None; Nishit Shah, None;
Patricia Garcia, None; Gennady Landa, None; Yusufu N. Sulai,
None; Alfredo Dubra, US Patent No: 8,226,236 (P); Richard B.
Rosen, Opko-OTI (C), Optos (C), Clarity (C), OD-OS (C), Topcon
(R), Zeavision (F), Genetech (F), Optovue (C)
Support: Marrus Family Foundation, Bendheim-Lowenstein Family
Foundation, Wise Family Foundation, Chairman's Research Fund of
the New York Eye and Ear Infirmary
Program Number: 1746
Presentation Time: 12:30 PM - 12:45 PM
Changes in Cone Reflectivity and Regularity Assessed by
Adaptive Optics Scanning Laser Ophthalmoscopy (AOSLO)
Correlate with Presence of Diabetic Retinopathy
Jan Lammer1, 2, Amel Ahmed5, Sonja G. Prager1, 2, Michael C.
Cheney1, Stephen A. Burns4, Paolo S. Silva1, 3, Lloyd P. Aiello1, 3,
Jennifer K. Sun1, 3. 1Beetham Eye Institute, Joslin Diabetes Center,
Boston, MA; 2Department of Opthalmology and Optometry, Medical
University of Vienna, Vienna, Austria; 3Department of
Ophthalmology, Harvard Medical School, Boston, MA; 4School of
Optometry, Indiana University, Bloomington, IN; 5Department of
Histology and Cell Biology, Faculty of Medicine, Assiut University,
Assiut, Egypt.
Purpose: To utilize high resolution AOSLO to evaluate differences
in cone density, reflectivity and regularity in eyes with and without
diabetes (DM) and across a range of diabetic retinopathy (DR)
severity.
Methods: Cone mosaics at the fovea and 4 macular quadrants
(1x1.2° area, mean+SD eccentricity = 4.2±0.4°) were imaged using
AOSLO (2.5µm resolution). Contrast of aligned and averaged images
was automatically standardized based on the 8-bit histogram. Cone
counting was performed semi-automatically using ImageJ and
manual correction by 2 independent graders masked to clinical data.
Count differences >20% were adjudicated. Parameters including
density, nearest neighbor (NN) and Voronoi tile measurements were
calculated as well as mean reflectivity of each Voronoi tile.
Results: Forty eyes of 40 subjects were assessed. For subjects,
mean±SD age was 44±12yrs, 57% (N=12) were male, 78% (31) had
DM, DM duration was 22±14yrs and 32% (10) had no DR, 19% (6)
mild nonproliferative DR (NPDR), 29% (9) moderate NPDR, 10%
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
(3) severe NPDR and 10% (3) PDR. No consistent relationship for
DM or DR was seen with absolute cone density, NN measurements,
or reflectivity. However, the reflectivity regularity index (RI)
(Voronoi tile reflectivity mean/SD) decreased in all 5 macular
regions with increasing DR severity and this decrease was
statistically significant in the inferior regions of the macula (No DR:
4.6±0.9, mild NPDR: 4.5±0.8, moderate NPDR: 4.5±0.7, severe
NPDR: 4.2±0.9, PDR: 3.8±0.9, p<0.05). A significantly lower NN RI
(NN mean/SD) was seen in macular quadrants in eyes with DM as
compared with no DM (4.7±1.0 vs. 5.4±1.5, p<0.04). Increasing age
correlated with a decrease in mean cone density (<35y:
11,567±2,848, 35-50y: 10,933±2,403, 50+y: 10,023±2,219
cones/mm2, p<0.05) as well as an increase in reflectivity RI (4.1±0.9,
4.3±0.8, 4.8±0.8, respectively, p=0.002) in all regions.
Conclusions: Although absolute cone density does not appear to
change substantially in diabetes, decreases in regularity of cone
spacing and reflectivity regularity are associated with presence of
DM and increasing DR severity, respectively. If future studies
demonstrate that these properties correlate with functional or
metabolic alterations of the retinal photoreceptors, these assessments
may provide novel predictors of visual or anatomic outcomes in the
diabetic eye.
Commercial Relationships: Jan Lammer, None; Amel Ahmed,
None; Sonja G. Prager, None; Michael C. Cheney, None; Stephen
A. Burns, None; Paolo S. Silva, Optos plc (F); Lloyd P. Aiello,
Genentech (C), Genzyme (C), Thrombogenetics (C), Ophthotech (C),
Kalvista (C), Pfizer (C), Proteostasis (C), Abbott (C), Vantia (C),
Optos, plc (F); Jennifer K. Sun, Boston Micromachines (F), Abbott
Laboratories (C), Novartis (C), Genentech (F)
Support: Eleanor Chesterman Beatson Childcare Ambassador
Program Foundation Grant, JDRF 17-2011-359, NIDDK 5 P30
DK036836-24 P&F Grant, Massachusetts Lions Eye Research Fund
281 Low Vision: Central Vision Loss
Monday, May 06, 2013 2:45 PM-4:30 PM
TCC LL 4/5 Paper Session
Program #/Board # Range: 2182-2188
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 2182
Presentation Time: 2:45 PM - 3:00 PM
Optical attachment for binocular imaging with the Scanning
Laser Ophthalmoscope (SLO)
George T. Timberlake1, Warren Ward2. 1Research, Kansas City VA
Medical Center, Kansas City, MO; 2Ward Electro-Optics, Inc.,
Gallatin, MO.
Purpose: Our objective was to develop a binocular optical system
that attaches to the SLO for imaging the retinas of both eyes. Such a
system may help answer questions as to how (or if) individuals with
bilateral macular scotomas use Preferred Retinal Loci (PRLs) in both
eyes when viewing an object.
Methods: We designed and constructed an electro-optical system
that alternately images the left and right retinas at 15 Hz. A linear
motor moves two small, offset orthogonal mirrors up and down,
reflecting the SLO light path left or right. The optical system is
adjusted in position so that the focal point of the converging laserbeam scan from the SLO is imaged at the intersection of the two
moving orthogonal mirrors. Additional mirrors reflect the left and
right beams toward the subject. Relay lens pairs mounted in rotating
eyepieces allow for inter-pupillary distance adjustment. Electronic
circuits synchronize the mirror movement with the SLO 30 Hz video
output. The retina is imaged in infrared (780 nm) and visual stimuli
are presented in the SLO’s HeNe (632 nm) laser-beam raster. Video
output can be recorded continuously and later separated into left and
right eye frames using standard software, or left and right retinas can
be presented on separate monitors.
Results: Initial tests with model eyes produced alternating video
images of the model eye “retinas” at 15 Hz. Analysis of recorded
SLO video showed the “retina” of each model eye imaged on every
other 30 Hz video frame. Retinas of two visually-normal subjects
were imaged in the same way. When following a moving disk in the
SLO raster, the image of the disk was placed on the fovea of both
eyes. The present binocular system has some loss of field due to
optical constraints. In addition, magnification is somewhat greater
than the SLO alone. The 15 Hz alternating rate produces noticeable
flicker for the observer, but it does not seriously interfere with
binocular viewing and tracking.
Conclusions: Presently, only eye-tracking techniques are available
for investigating how both eyes are used together by those with
macular scotomas. Such techniques cannot determine what retinal
area(s) are used to inspect visual stimuli. We believe that the
binocular SLO attachment will be useful for investigating how
individuals with bilateral macular scotomas use PRLs in both eyes to
look at objects.
Commercial Relationships: George T. Timberlake, None; Warren
Ward, None
Support: Department of Veterans Affairs Rehabilitation Research
and Development Service Grant C1000R
Program Number: 2183
Presentation Time: 3:00 PM - 3:15 PM
Does the location of the PRL correspond to the retinal location
with the best acuity?
Susana T. Chung, Jean-Baptiste Bernard. School of Optometry,
University of California, Berkeley, CA.
Purpose: Following the onset of central vision loss, most patients
develop a retinal location outside the central scotoma, the preferred
retinal locus (PRL), as the new reference for visual tasks. Little is
known as to how the PRL locations are selected. In this study, we
tested the hypothesis that the selection of the location for a PRL is
based on optimizing visual acuity, which predicts that acuity is the
best at the PRL, compared with other retinal locations.
Methods: Using a Rodenstock scanning laser ophthalmoscope (SLO)
as a gaze-contingent display, we first mapped out the absolute
scotoma for four observers with long-standing central vision loss
(age: 56-84, logMAR acuity: 0.52-1.04). We then measured acuity
using a 4-orientation Tumbling-E task presented using the SLO at the
PRL and at multiple locations around the scotoma. These locations
were positioned along 12 meridians (2-3 positions per meridian)
originating from the anatomical fovea (30° apart), straddling 1-5°
from the edge of the scotoma. The order of testing these 24-36
locations was random. A staircase procedure was used to track the
letter size threshold that corresponded to 71% correct. The thresholds
averaged across three staircases represented the acuity at each testing
location.
Results: Across observers, the acuity at the PRL was never the best
among all testing locations. Instead, acuities were better (up to 47%)
at 10-46% of the testing locations than at the PRL. These locations
with better acuities did not cluster around the PRL, and did not
necessarily lie at the same distance from the fovea or the edge of the
scotoma as the PRL. Except for the only observer who had foveal
sparing, acuities did not correlate with the eccentricities of the testing
locations. However, when acuities at different eccentricities along the
same meridian were averaged, the meridian with the best averaged
acuity was consistent with the meridian on which the PRL was
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
located.
Conclusions: The worse acuity found at the PRL than at other
locations around the scotoma implies that the selection of the PRL
location was unlikely to be based on optimizing acuity. Although our
measurements were made years after the development of the PRL,
perceptual learning suggests that with continuous usage, acuity at the
PRL should only get better and not worse, further affirming that the
initial selection of the PRL location was not based on optimizing
acuity at a specific location.
Commercial Relationships: Susana T. Chung, None; JeanBaptiste Bernard, None
Support: NIH Grant R01-EY012810
Program Number: 2184
Presentation Time: 3:15 PM - 3:30 PM
Retinal Fixation Locus in Patients with Bilateral Central
Scotomas: Letter Targets are Better Suited for Visual Testing
than Targets that Fill in
Joshua Pratt, Harold E. Bedell, Joy M. Ohara, Stanley Woo.
University of Houston College of Optometry, Houston, TX.
Purpose: Training eccentric viewing has been widely implemented
as a regular part of low vision services for patients with central
scotomas. In this experiment we investigated whether target type
affects the retinal fixation location and stability, and specifically
whether targets expected to perceptually fill in are imaged at the
vestigial fovea. If targets expected to fill in are imaged at or near the
vestigial fovea, then fixation on these targets would allow the
projected location of the vestigial fovea and the pathological scotoma
to be located accurately in visual space during eccentric viewing
training, even without the use of a fundus imaging device.
Methods: The retinal location and stability of fixation were
measured using the Nidek MP-1 microperimter in twelve patients
with bilateral central scotomas for six types of fixation target, three
expected to fill in and three that included letters. The approximate
position of the vestigial fovea was delineated either by using residual
retinal landmarks or by locating the residual foveal pit in a dense
macular scan, obtained with a Spectralis Optical Coherence
Tomographer. Fixation location and stability were compared for the
different target types and referenced to the position of the vestigial
fovea.
Results: All of the subjects except one fixated consistently on targets
that included a letter using peripheral retinal locations outside of the
central scotoma. Eleven of the twelve subjects used a retinal location
closer to the vestigial fovea to fixate targets expected to fill in,
compared to letters. Although four of the subjects imaged the fill-in
targets at or within a half degree of the vestigial fovea, six other
subjects imaged the fill-in targets at a retinal locus removed from the
vestigial fovea. Target type produced no overall significant difference
in fixation stability, specified in terms of bivariate contour ellipse
area. However, in some individual subjects fixation tended to be
more stable on letter targets than on fill-in targets.
Conclusions: In patients with central field loss, letter targets generate
more consistent fixation behavior than fill-in targets and should be
used for eccentric viewing training and perimetry.
Commercial Relationships: Joshua Pratt, None; Harold E. Bedell,
None; Joy M. Ohara, None; Stanley Woo, None
Support: NIH Core Grant P30 EY 07551, Beta Sigma Kappa
Student Research Grant
Program Number: 2185
Presentation Time: 3:30 PM - 3:45 PM
Qualitative and Quantitative Assessment of Metamorphopsia in
Retinopathy Patients
Emily K. Wiecek1, 2, Kameran Lashkari2, 3, Steven C. Dakin1, 4, Peter
Bex2, 3. 1Institute of Ophthalmology, University College London,
London, United Kingdom; 2Opthalmology, Harvard Medical, Boston,
MA; 3Opthalmology, Massachusetts Eye and Ear, Boston, MA;
4
NIHR Biomedical Research Centre for Ophthalmology, Moorfields
Eye Hospital, London, United Kingdom.
Purpose: Metamorphopsia (perceived distortion of visual space) is
commonly experienced by patients with retinal pathology. Although
this distortion is typically measured with Amsler charts, more
objective and quantitative assessments are desirable for effective
monitoring of the presence, progression, and remediation of visual
impairment. We compare qualitative assessments with novel
quantitative methods across a range of retinal pathologies.
Methods: An eleven-item questionnaire assessed metamorphopsia
symptoms in 80 patients with monocular distortion from
maculopathy. All patients completed an Amsler assessment
(presented on a computer screen with fixation compliance monitored
by an eye tracker), and 35 patients additionally completed two novel
objective measures of metamorphopsia in the central five degrees of
visual field. One task required participants to arrange dots in a square
(combining spatial bisection and Vernier hyperacuities), and the other
used spatial alignment of dichoptically-presented targets. A dichoptic
task was also used as a binary measure of inter-ocular suppression.
Results: Monocular distortions were suppressed by undistorted
vision in the better eye in 45% of patients. Questionnaire scores from
non-suppressing patients positively correlated with distortion
measures; however there was no relationship between subjective and
quantitative assessments for patients who experienced suppression (p
=.03). There was significant negative correlation in the overall
vertical direction of distortion between the two novel quantitative
distortion assessments (p = .05), as well as a positive correlation
between the directional displacement measured in the dichoptic task
and the gaze-contingent Amsler grid quantification (p = .01). There
were no significant correlations between localized measures of visual
distortion across all three measures.
Conclusions: The onset and progression of visual impairment may
be underreported in maculopathy due to the suppression of distorted
visual input from the more impaired eye. It is critical to assess
metamorphopsia monocularly, and we have introduced novel metrics
to quantify such visual distortion in central vision.
Commercial Relationships: Emily K. Wiecek, None; Kameran
Lashkari, Circadian Technologies (F), Regeneron (R); Steven C.
Dakin, None; Peter Bex, Adaptive Sensory Technology, LLC (S),
Rapid Assessment of Visual Sensitivity (P)
Support: R01EY019281, SCD is supported by NIHR Biomedical
Research Centre for Ophthalmology at Moorfields Eye Hospital
Program Number: 2186
Presentation Time: 3:45 PM - 4:00 PM
The effects of central and peripheral visual losses on reaching
and grasping
Aachal Kotecha1, 2, Rachel T. Fahy2, Gary S. Rubin2, 1. 1NIHR BRC
for Ophthalmology, UCL Institute of Ophthalmology & Moorfields
Eye Hospital, London, United Kingdom; 2Visual Neuroscience, UCL
Institute of Ophthalmology, London, United Kingdom.
Purpose: This study aims to evaluate the relative contributions of
central and peripheral vision to prehension in visually impaired
adults.
Methods: Reaching and grasping was quantified using motion
detection cameras (ProReflex, Qualisys AB, Sweden). Subjects
reached and grasped one of two cylindrical objects placed at 20cm or
40cm from the hand. Measures were repeated 8 times under each test
condition and the median used in subsequent analysis. Indices of
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
prehension planning [movement onset (MO ms); peak speed (V
mm/s), time to peak speed (ttV ms)], execution [movement duration
(MD ms); path deviation ratio (PD)] grasping [peak grip aperture
(PGA, angle), grip application time (GAT, ms)] and control
[deceleration time (DT ms)] were quantified. Analyses were
performed using repeated measures ANOVA.
Results: The results of 9 control (C), 11 age related macular
degeneration (AMD) and 12 glaucoma (G) patients during binocular
viewing are presented. There were significant group differences in
movement planning [MO: p < 0.01, V: p = 0.03, ttV: p < 0.01] and
grasping [GAT:p < 0.01] with aspects of execution and online control
approaching significance [MD: p = 0.06; PD, p = 0.1].
AMD and G patients had longer MO ('far,large' condition mean
[standard error]: C = 274 [46] ms; G = 378 [87] ms; AMD = 439
[104] ms), ttV (C = 594 [79] ms; G = 719 [103] ms; AMD = 766
[100] ms) and GAT (C = 411 [74] ms; G = 544 [126] ms; AMD =
644 [163] ms); however AMD reaching speed V was slower,
suggesting a deficiency in some aspects of movement planning (C =
1032 [122] mm/s; G = 918 [150] mm/s; AMD = 854 [94] mm/s). In
contrast, glaucoma patients displayed longer DT (C = 510 [109] ms;
G = 552 [79] ms; AMD = 528 [74] ms) , MD (C = 935 [113] ms; G =
1078 [192] ms; AMD = 1060 [156] ms) and higher PD (C = 1.14
[0.04]; G = 1.16 [0.05]; AMD = 1.12 [0.04]) suggesting difficulties
with online control.
Conclusions: This preliminary analysis suggests that whilst
glaucoma and AMD patients have deficits in reach to grasp
movements compared with controls, they display distinct differences
in movement planning and online control. Further work will explore
how these relate to their specific visual deficiency.
Commercial Relationships: Aachal Kotecha, None; Rachel T.
Fahy, None; Gary S. Rubin, None
Support: Special Trustees of Moorfields Eye Hospital
Program Number: 2187
Presentation Time: 4:00 PM - 4:15 PM
Effect of central vision loss on mutual gaze perception
Alexandra R. Bowers1, Sarah S. Sheldon1, Jessilin Quint2, Heiko
Hecht3. 1Schepens Eye Res Inst, Mass Eye and Ear, Ophthalmology,
Harvard Med School, Boston, MA; 2Indiana University School of
Optometry, Bloomington, IN; 3Psychologisches Institut, Johannes
Gutenberg-Universitat, Mainz, Germany.
Purpose: The ability to perceive mutual gaze (knowing whether
somebody else is looking at you) is an important nonverbal visual cue
that directs conversations and social interactions. Individuals with
central vision loss (CVL) have limited access to such cues, which
may cause difficulties in social situations. We evaluated perceived
difficulties with gaze perception and examined the relationship with
functional abilities quantified using a performance-based measure.
Methods: 18 persons with CVL (visual acuity 20/60 to 20/250) and
18 age-similar controls completed a battery of vision tests, a short
questionnaire rating perceived difficulties with gaze perception, face
recognition and social interactions, and a gaze perception task. They
adjusted the positions of the eyes of a life-size virtual head on a
monitor at a 1-m distance until the eyes appeared either to be looking
straight at them or were at the extreme lateral left or right position at
which they still appeared to be looking toward them. For each trial (n
= 48), the angular deviation of the final position of the virtual eyes
from the straight ahead gaze position was computed. The gaze cone
width was the difference between the extreme left and right positions.
Results: CVL participants reported moderate difficulty with knowing
when somebody was looking at them; moderate difficulty with seeing
how other people reacted in social situations; and a variety of coping
strategies. Controls reported no difficulties. The median gaze cone
widths were not significantly different for the two groups (CVL
11.5°, controls 13.2°; p = 0.9) neither were the mean judgments of
the straight ahead gaze direction (CVL 0.1 ± 0.9°, controls 0.2 ± 1.7°;
p = 0.82). However, CVL participants had significantly more
variability in their judgments (6.9 ± 2.4° and 4.6 ± 1.8°; p < 0.01).
Greater judgment variability correlated with higher levels of
perceived difficulties (r = 0.78, p < 0.001) but not with visual acuity
(r = 0.44, p = 0.07) or contrast sensitivity (r = -0.37, p = 0.13).
Conclusions: CVL increased the variability of mutual gaze
judgments suggesting that CVL participants had more difficulty with
the task than controls; however, the average estimate of gaze
direction was similar in the two groups. While traditional vision
measures did not predict the extent to which CVL affected the more
complex gaze judgment task, perceived difficulties were predictive of
increased judgment variability.
Commercial Relationships: Alexandra R. Bowers, None; Sarah S.
Sheldon, None; Jessilin Quint, None; Heiko Hecht, None
Support: NIH grant T35EY007149
Program Number: 2188
Presentation Time: 4:15 PM - 4:30 PM
Association of Self-Reported Task Difficulty with Binocular
Central Scotoma Locations
Nicole C. Ross, Judith E. Goldstein, Robert W. Massof.
Ophthalmology, Johns Hopkins Univeristy, School of Medicine,
Baltimore, MD.
Purpose: To determine if the location of binocular central scotomas
relative to fixation, predicts the difficulty that low vision patients are
likely to have with driving, reading, and mobility tasks.
Methods: This study was conducted in accordance with the tenets of
the Declaration of Helsinki and Johns Hopkins Institutional Review
Board.
Perimetry: Central scotomas were mapped with a video haploscope
tangent screen in 284 patients. The haploscope consisted of 2 flat
panel displays, one per eye, imaged at infinity through 9mm diameter
exit pupils centered on the patient’s pupils. The patient’s refractive
error corrections were incorporated into the optical paths. Infrared
video cameras where used to monitor ocular alignment and fixation
stability. The patient fused the two 50o h x 40o v displays and the
fixation cross was imaged at the center of both displays, thereby
providing binocular fixation, while test stimuli were presented
monocularly at 43 locations in a 25o square grid around fixation.
Self Reported Difficulty Ratings: Patients rated difficulty of a subset
of 120 reading, 50 mobility and 22 driving tasks in the Activity
Inventory on a five point scale. Rasch analysis was used to estimate
self-perceived ability for driving, reading and mobility for each
patient.
Analysis: Unpaired, two tailed t-tests were performed on distributions
of each ability measure for each test location in the central field
comparing patients who detected the stimulus to those who did not.
Results: Driving: Scotomas below and to the lower right of fixation
and a single point 10o above and to the right of fixation were
associated with significant decreases in self-perceived driving ability.
Reading: Scotomas from 7.5o left of fixation to 12.5o right of fixation
and scotomas below and to the lower right of fixation were associated
with significant decreases in self-perceived reading ability.
Mobility: Scotomas below and to the upper right of fixation were
most strongly associated with decreases in self-perceived mobility
function.
Conclusions: Driving difficulty is associated with scotomas that fall
on the instrument panel and rear view mirror when gazing straight
ahead. Reading difficulty is associated with scotomas that could
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
interfere with text preview and navigating to the next line. Mobility
difficulty is associated with scotomas that could interfere with
identifying information below the line of sight.
Commercial Relationships: Nicole C. Ross, None; Judith E.
Goldstein, None; Robert W. Massof, None
Support: NEI grant EY012045 and MD 22 Lions Vision Research
Foundation Postdoctoral Fellowship
288 Refractive Errors, Myopia I
Monday, May 06, 2013 2:45 PM-4:30 PM
Exhibit Hall Poster Session
Program #/Board # Range: 2327-2343/B0286-B0302
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 2327 Poster Board Number: B0286
Presentation Time: 2:45 PM - 4:30 PM
Daily interruptions to hyperopic defocus can reduce induced eye
growth in marmosets
Alexandra Benavente-Perez, Ann Nour, Luying Yan, Keisha Roden,
Kathleen Abarr, David Troilo. Biological Sciences, SUNY College
of Optometry, New York, NY.
Purpose: To assess the effect that short daily interruptions to
imposed hyperopic defocus have on the eye growth of marmosets,
and to measure the effective refractive state during the interruption
period.
Methods: A total of 20 marmosets were treated with -5D contact
lenses on their right eyes for 12 weeks from the age of 10 weeks of
age (left eyes wore plano controls). On-axis vitreous chamber depth
(VC) was measured after four (T4), eight (T8) and twelve weeks of
treatment (T12). Fifteen marmosets wore contact lenses continuously
for 9hrs/day and five had both contact lenses removed for 30mins
twice/day (mid morning and mid afternoon) during the first four and
last four weeks of treatment. Vision during the interruptions was
controlled by placing the marmoset in a primate chair at the center of
a 1m radius cylinder with videos of animal scenes projected on the
wall. Noncyloplegic Rx was measured at 5min intervals using an
infrared video photorefractor (Power Refractor, MultiChannel
System) while the marmosets were in the chair. Untreated marmosets
(N=25) were used as controls.
Results: At T4 the interocular difference in ocular growth rates in the
interrupted lens-reared group was smaller than in the continuous lens
reared group (mean±SE exp-con: -0.3±1.3 vs +3.6±1.0 µm/day,
p<0.05) and similar to the untreated group (-0.2±0.4 µm/day,
p=0.97). At T8, after both treatment groups worn -5D contact lenses
continuously for 4weeks, their growth rates were the same (+2.8±0.7
vs +1.8±1.2 µm/day, p=0.47). At T12, after the second period of lens
interruption, the growth rate in the interrupted lens-reared group was
again smaller than in the continuous lens reared group growth, but
did not reach significance (-0.07±0.8 vs +0.85±1.5 µm/day, p>0.05).
While inside the cylinder, the marmosets experienced an overall
relative myopic defocus of -2.07±0.63D during T4 that increased to 4.08±1.63 D during T12.
Conclusions: Daily brief interruptions to imposed hyperopic defocus
prevent the increased rate of ocular growth triggered by -5D contact
lenses in marmosets. The effects were stronger when the interruptions
happened early during treatment than when the interruptions were
applied to eyes that were already growing faster to compensate for
imposed hyperopia.
Commercial Relationships: Alexandra Benavente-Perez, None;
Ann Nour, None; Luying Yan, None; Keisha Roden, None;
Kathleen Abarr, None; David Troilo, None
Support: NIH R01 EY11228
Program Number: 2328 Poster Board Number: B0287
Presentation Time: 2:45 PM - 4:30 PM
Luminance and Color Changes with Defocus Provide Differential
Cues For Emmetropization
Molly Fellows1, Gagan Kaur2, Ashley Tang1, Frances J. Rucker1.
1
Biomedical Science & Disease, New England College of Optometry,
Boston, MA; 2Southern California College of Optometry, Fullerton,
CA.
Purpose: Factors that interfere with lens compensation are
considered to interfere with emmetropization. We examine the effects
of color and luminance changes on lens compensation.
Methods: Exp. 1: 5-7 day old chicks were exposed daily (9am-5pm)
for three days, on consecutive weeks, to 2Hz sinusoidal, in-phase
(LUM), modulated white light (619 nm + 515 nm + 460 nm; Mean
680 lux) or to counterphase-modulated red/green light (R/G). Chicks
wore either a negative or a positive 7 D lens on alternate weeks.
Exp. 2: 14 day old chicks were exposed daily (9am-5pm) for three
days to 2Hz sinusoidal, in-phase, modulated white light (619 nm +
515 nm + 460 nm; Mean 850 lux) either with (+B) or without blue
light (-B). Chicks wore either a negative or positive 7 D lens on one
eye. Chicks wore no lenses in a control, no flicker condition.
Chicks were kept in the dark overnight after exposures and otherwise
in a brooder on a 12/12 hr light cycle between experiments. Relative
changes in the ocular components were measured with ultrasound
(Exp.1) or with Lenstar (Exp. 2) and with a Hartinger refractometer.
Results: Exp. 1: LUM flicker, but not R/G flicker, interfered with
positive lens compensation. There was a change in refraction in R/G
(wk1: 4.93 ± 2.116 D; p=0.02) but not in LUM (wk1: 2.43 ± 2.68 D),
despite a reduction in eye growth in all conditions (R/G: -196 ± 30
μm; LUM: - 139 ± 24 μm; p<0.006) with choroidal thickening in R/G
but not in LUM (RG: 53 ± 18 μm; LUM: 14 ± 16 μm; p<0.01).
LUM flicker and R/G flicker both interfered with negative lens
compensation. There was no refractive (wk1: R/G: -1.76 ± 1.13 D;
LUM: -1.64 D), eye growth (RG: 24 ± 48 μm; LUM: -4 ± 23 μm), or
choroidal thickness change (-1 to -6 μm).
Exp. 2: There was no refractive change with or without blue light to
positive (+B: -0.47 ± 2.7 D: -B: 0.32 ± 3.03 D) or negative defocus
(+B: -0.77 ± 2.4 D; -B: -1.65 ± 1.19 D), compared to steady light/no
lens condition (+B: -0.25 D; -B: 0.51 D). However, with positive
lenses there were changes in eye length (+B: -219 ± 36 μm; -B: -228
± -28 μm; both p<0.001) and choroidal thickening (+B: 124 ± 14 μm;
-B: 132 ± 20 μm;both p<0.001) compared to the steady light/no lens
condition (+B: -50 µm; -B: -20 µm).
Conclusions: Luminance cues are important for lens compensation
with both signs of defocus, while color cues are only important with
negative defocus.
Commercial Relationships: Molly Fellows, None; Gagan Kaur,
None; Ashley Tang, None; Frances J. Rucker, None
Program Number: 2329 Poster Board Number: B0288
Presentation Time: 2:45 PM - 4:30 PM
Myelinated Retinal Nerve Fibers associated Local Scleral
Excavation and Induced Axial Myopia: Investigation using
Spectral-domain Optical Coherence Tomography
Baek-Lok Oh, Jeong-Min Hwang, Se Joon Woo. Ophthalmology,
Seoul National University College of Medicine, Seoul National
University Bundang Hospital, Seognam, Republic of Korea.
Purpose: To report findings of spectral domain optical coherent
tomography (SD-OCT) of myelinated nerve fibers (MNF) and
propose a mechanism for axial myopia associated with MNF.
Methods: In this retrospective observational case series, 12 eyes
from 12 patients (6 children and 6 adults) with MNF over 2 disc
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
diameters underwent a full ophthalmologic examination including
SD-OCT. The distribution of MNF in the fundus photography was
compared with the regional excavation of the scleral excavation in
vertical or horizontal scan and circular scan centered on the optic disc
of SD-OCT.
Results: In all cases, SD-OCT visualized MNF as hyperreflective
thickening of retinal nerve fibers and there were no morphologic
abnormalities in the photoreceptor layers in the fovea. In eyes with
temporally extended MNF, the tilting of Bruch’s membrane in
vertical scans of SD-OCT was significantly associated with the major
distribution of myelination (P < 0.001). The slope of Bruch’s
membrane was much smaller in the adult group than in the child
group (P = 0.008). The area of MNF in fundus photography and focal
scleral excavation in the peripapillary circular SD-OCT scan images
were significantly correlated (P <0.001).
Conclusions: Localized scleral excavation inducing axial myopia
was strongly associated with the distribution of MNF especially in
children, which indicates MNF itself or confined retinal areas with
visual deprivation by MNF may directly induce axial myopia via
local trophic effects on the underlying sclera in early life.
Fundus photography and reconstructed 3-dimensional images of
spectral domain optical coherence tomography of fundus with
myelinated nerve fibers. Sectioning planes are indicated with black
lines.
Examples of quantitative analysis of the association of the area of
myelinated nerve fibers measured by fundus photography (A, F) and
the depth of the internal limiting membrane or Bruch’s membrane
near the optic disc (B, G; white arrows) measured in circular 3.4 mm-
diameter scans centered on the optic disc of spectral domain optical
coherence tomography along clock-hours. E, J. The correlation
between the modified area of the myelinated nerve fibers (MNF
length) and the depth of the internal limiting membrane or Bruch’s
membrane (the scleral excavation) was statistically significant (P <
0.001).
Commercial Relationships: Baek-Lok Oh, None; Jeong-Min
Hwang, None; Se Joon Woo, None
Support: A grant from the Korea Health Technology R&D Project,
Ministry of Health and Welfare, Republic of Korea (Grant No.
A111161).
Program Number: 2330 Poster Board Number: B0289
Presentation Time: 2:45 PM - 4:30 PM
Comparing the Historical and Contemporary Ocular Biometry of
Emmetropes
Jos J. Rozema1, 2, David A. Atchison3, Marie-José B. Tassignon1, 2.
1
Dept of Ophthalmology, Antwerp University Hospital, Edegem,
Belgium; 2Dept of Medicine and Healthy Science, University of
Antwerp, Wilrijk, Belgium; 3School of Optometry & Institute of
Health and Biomedical Innovation, Queensland University of
Technology, Brisbane, QLD, Australia.
Purpose: To compare the historical emmetropic ocular biometry data
reported by Zeeman (Graefes Arch. Ophthal. 1911;78:93-128) and
Sorsby (Spec Rep Ser Med Res Counc 1957: 293) with data from
contemporary emmetropes published by Atchison et al. (J Vis.
2008;8:29, 1-20).
Methods: Zeeman and Sorsby published the ocular biometry for
Caucasian subjects using similar methods: retinoscopy for ocular
refraction, Javal keratometry for the corneal radius of curvature, a slit
lamp method for the anterior chamber depth and lens thickness, and
phakometry for the lens radii of curvature. In order to make sure that
the contemporary data are comparable with the historical data, it is
important that compatible biometry methods are used. Hence Placido
topography and ultrasound biometry were used (both of which have
been validated against the historical methods in the literature), as well
as autorefraction and phakometry. For all three datasets the axial
length was derived using a method proposed by Sorsby. As this
method does not take the aging of the crystalline lens into account,
only subjects aged between 18 and 38 were considered. This left 25
emmetropes from Zeeman (refraction within ±1 D), 38 from Sorsby
and 20 from Atchison et al. for analysis. Comparisons were done by
ANOVA, a t test after Fisher r-to-z transformation to compare
correlations, and Flury Hierarchy and random skewers to compare
covariance matrices.
Results: After Šidák correction to account for alpha inflation in case
of multiple comparisons, the posterior lens radius was found to be
significantly flatter for Atchison et al. (-6.88 ± 0.96 mm) than for
Zeeman (-6.02 ± 0.53 mm; P = 0.001), and the anterior chamber
depth was significantly shallower for Sorsby (3.55 ± 0.24 mm) than
for Zeeman (3.76 ± 0.29 mm; P = 0.004). No significant differences
were seen in the correlations between the parameters of the three
datasets. For the covariance matrices, considerable and significant
differences were seen between the Atchison et al. data on the one side
and the Zeeman and Sorsby data on the other side.
Conclusions: The average biometry and correlation between
biometric parameters of emmetropic subjects has remained similar
throughout the last hundred years. The significant differences
between the studies for the biometry and the covariance matrices may
reflect differences in methods or instrument calibration.
Commercial Relationships: Jos J. Rozema, None; David A.
Atchison, None; Marie-José B. Tassignon, None
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 2331 Poster Board Number: B0290
Presentation Time: 2:45 PM - 4:30 PM
Effects of Eyeglass Correction on Oral Reading Fluency in
Elementary and Middle School Children
Irene Campus1, Mabel Crescioni1, Tina K. Green1, John D. Twelker1,
2
, Joseph M. Miller1, 2, Erin M. Harvey1, 2. 1Ophthalmology and
Vision Science, University of Arizona, Tucson, AZ; 2College of
Public Health, University of Arizona, Tucson, AZ.
Purpose: To examine the influence of eyeglass correction on oral
reading fluency.
Methods: Eye examinations were conducted on students in grades 28 who failed a vision screening test. Exams included cycloplegic
refraction and subjective refinement. Glasses were prescribed for
children who met the following criteria: Astigmatism ≥ 1.00 D,
Myopia ≥ 1.00 D on any meridian, or Hyperopia ≥ 2.50 D spherical
equivalent (SE) in either eye, or anisometropia ≥ 1.50 D SE.
Eyeglasses were dispensed at a second testing session several weeks
after the exam for students meeting the criteria for eyeglass
correction (N=21). DIBELS Oral Reading Fluency (ORF) (a
standardized test of accuracy and fluency with connected text) was
measured at the eyeglass dispensing session, and children were tested
without correction (3 passages read). Several weeks later (average
6.31 weeks, SD 4.44), after students had adjusted to their eyeglasses,
DIBELS ORF was repeated while children were wearing their best
correction. Students in 7th and 8th grade completed DIBELS ORF
for the 6th grade level, the highest grade level available. DIBELS
ORF median raw score was determined for tests conducted while
uncorrected and corrected, and scores were converted to percentiles
Results: Most students were prescribed eyeglasses for astigmatism
(18) and/or myopia (14), with one meeting the criteria for hyperopia.
DIBELS ORF percentile scores increased significantly an average of
7.14 (SD 11.49, p < 0.02) with eyeglass correction. Amount of
improvement was not significantly correlated with time between tests
(duration of new eyeglass wear).
Conclusions: Students who meet common criteria for eyeglass
prescription show rapid improvement in reading fluency through
eyeglass wear. Due to the short follow-up interval and the fact that
improvement was not correlated with time from first to second test, it
is likely that this effect is a result of improved visual clarity, as
opposed to advances in reading skills resulting from instruction
(learning). There may be additional long-term effects on reading as a
result of improved visual clarity, but this study did not measure these
effects. These results indicate the importance of vision screening in
schools with follow-up to eye care professionals as needed.
Commercial Relationships: Irene Campus, None; Mabel
Crescioni, None; Tina K. Green, None; John D. Twelker, None;
Joseph M. Miller, None; Erin M. Harvey, None
Support: NIH/NEI 13153, Research to Prevent Blindness
Program Number: 2332 Poster Board Number: B0291
Presentation Time: 2:45 PM - 4:30 PM
Peripheral photoreceptor activity during accommodation and
emmetropization
Brian P. Schmidt1, Maureen Neitz2, Jay Neitz2. 1Graduate Program in
Neurobiology and Behavior, University of Washington, Seattle, WA;
2
Ophthalmology, University of Washington, Seattle, WA.
Purpose: Myopia results when the eye grows too long for its optics.
The importance of the peripheral retina in emmetropization has
recently been appreciated and our group has argued that the relative
activity of cone photoreceptors contributes as well. However, there
has not been a systematic analysis of how peripheral photoreceptor
activity might be stimulated by natural images during near
accommodation over the period of life which emmetropization
occurs. The present work uses mathematical modeling to develop a
theoretical framework of emmetropization based on the observation
that the peripheral retina is often exposed to distant scenes when the
fovea is accommodated to near objects.
Methods: The OSLO ray tracing software (Lambda Research) was
used to derive modulation transfer functions of a schematic eye
(Escudero-Sanz & Navarro 1999 J. Opt. Soc. Am. A. 16:1881-91) for
several eccentricities and accommodation states. The amplitude
spectrum of calibrated natural images (Tkačik et al. 2011 PLoS One
6:e20409) were computed with a fast Fourier transform and fit with a
1 / f power law. The activity of photoreceptors was modeled as a
difference of Gaussians. Finally, the transfer functions, amplitude
spectrum and photoreceptor model were combined to obtain the
response from the peripheral cone photoreceptor mosaic to the
average natural scene.
Results: Accommodation to near objects results in a significant loss
of medium and high spatial frequencies for images of distant objects
in the peripheral retina relative to the fovea reducing the relative
activity of photoreceptors there. This loss of frequency content is
partially ameliorated by accommodative lag that has been observed in
young children but decreases during emmetropization.
Conclusions: Considering the statistical environment and the optical
transfer functions characteristic of common accommodation states we
compute that the amount of information the peripheral retina receives
about the visual environment during near accommodation to small
centrally fixated targets changes systematically during
emmetropization. This change may regulate the signals that control
eye growth. The reason near work contributes to myopia may be
because the spatial frequency content of the images produced in the
periphery during such activity simulates the normal signals produced
by natural scenes in peripheral retina of a young hyperopic eye.
Commercial Relationships: Brian P. Schmidt, None; Maureen
Neitz, Genzyme (F), Alcon (F), Alcon (P); Jay Neitz, Alcon (F),
Alcon (P)
Program Number: 2333 Poster Board Number: B0292
Presentation Time: 2:45 PM - 4:30 PM
Relation between refractive astigmatism and change in spherical
equivalent with age in a sample of Native American children age
3 to 18 years of age
Erin M. Harvey1, 2, John D. Twelker1, 2, Joseph M. Miller1, 2.
1
Ophthalmology and Vision Science, University of Arizona, Tucson,
AZ; 2College of Public Health, University of Arizona, Tucson, AZ.
Purpose: To determine if presence of refractive astigmatism is
associated with change in spherical equivalent (SE) refractive error in
children age 3 to 18 years of age.
Methods: Subjects were participants one or more NIH/NEI funded
studies of visual development in Tohono O’odham children
(“Collaborative Longitudinal Evaluation of Ethnicity and Refractive
Error” (CLEERE, Tucson Site), “Astigmatism and Amblyopia
Among Native American Children”, “Amblyopia in Astigmatic
Children: Development and Treatment”). Previous research has
documented a high prevalence of with-the-rule astigmatism in this
population. A baseline exam was conducted and follow-up exams
were attempted at least yearly for each study. Data was combined
across studies. Cycloplegic autorefraction (Retinomax Autorefractor
(KPlus or KPlus2, Nikon Inc., Tokyo Japan)) was conducted at each
study exam. Subject exams that met the following criteria were
included in analyses: age 3 to < 19 years, right eye autorefraction
confidence ≥ 8. Only subjects with at least two study exams and a
minimum interval of 1 year between first and last exam were
included in analyses. Analyses included only right eye data, and only
data from each child’s baseline and final study exams. Linear
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
regression analysis was conducted to determine the relation between
baseline refractive astigmatism and change per year in SE refractive
error with age (change is SE/fu interval). The following variables
were also included: sex, baseline age, follow-up interval, baseline SE.
Results: For the 2,043 subjects who met inclusion criteria, mean age
was 6.13 years (SD 2.90) at baseline and 10.70 years (SD 3.56) at
follow-up, with a mean follow-up interval of 4.57 years (SD 3.28).
SE tended to shift towards less hyperopia/more myopia with age in
most children (Table 1). On average, there was a shift towards less
hyperopia/more myopia of 0.16 D/year (Table 2). Neither of these
trends varied significantly with amount of baseline astigmatism.
Regression analysis yielded significant effects of age, sex, length of
follow-up interval, and baseline SE on change per year in SE, but no
significant effect of baseline astigmatism magnitude.
Conclusions: The results of the present study indicate that highly
astigmatic children in this population are not at increased risk for
development or progression of myopia.
Sensor, the Pediatric Wavefront Evaluator (PeWE). Children ranged
in age from 6 mos to 9 yrs. Images were recorded while children
watched a cartoon at 50 cm (near, n) and 2 m (distant, d) viewing
distance. At least 7 focused and centered images were obtained at
both fixation distances, with undilated pupil diameters ranging from 3
to 5 mm. Zernike decomposition to 4th order was performed. Lower
order aberrations were converted to m, j0 and j45. Signed Zernike
terms Z(3,1) (y coma, yc), Z(3,-1) (x coma, xc) and Z(4, 0) (spherical
aberration, sa) were derived for the observed mm pupil diameter
(mmpd). Three different pupil scaling methods were used: (1) all
terms were scaled down to 3mmpd, (2) those greater than 4 mmpd
scaled down to 4 mmpd (data with pupil < 4 mm excluded), and (3)
all were scaled up to 5 mmpd. Within each subject, at least 3
observations were required at 4mmpd to be averaged, while 7 were
always averaged at 5 mmpd and 3 mmpd. Paired sample (d and n) ttests on the signed coefficients (micron) were compared at 3, 4, and 5
mmpd.
Results: As expected, accommodation produced a change in m from
n to d of -1.33 to -0.25D (p=0.000). A small (<0.1mm) but significant
decrease in d to n pd was also observed (p=0.000). J0 and J45 had
small but significant differences d to n (<0.1D, p=0.000. Coma (xc
and yc) did not change with accommodation (p>0.20). Spherical
Aberration became increasingly negative with accommodative effort
(p<0.05). Table summarizes d and n yc, xc and sa at 3 (n=545) , 4
(n=233), and 5 (n=545) mmpd.
Conclusions: In this population of Native American children, the
observed coma did not change with accommodation, suggesting a
non-lenticular or corneal origin. The increased negative spherical
aberration with accommodation enhances near vision, and suggests a
lenticular origin. Future work will compare these refractive
aberrations to corneal aberrations measured with surface topography.
Commercial Relationships: Joseph M. Miller, None; Erin M.
Harvey, None; Jim Schwiegerling, Alcon Research (F), Wavetec
(F), Visioneering (C)
Support: NIH/NEI 13153(EMH); RBP (JMM)
Commercial Relationships: Erin M. Harvey, None; John D.
Twelker, None; Joseph M. Miller, None
Support: NIH Grant EY13153, NIH/NEI EY08893, and Research to
Prevent Blindness
Program Number: 2334 Poster Board Number: B0293
Presentation Time: 2:45 PM - 4:30 PM
Change in coma and spherical aberration with accommodation in
Native American children of a tribe having elevated levels of
Corneal Astigmatism
Joseph M. Miller1, 2, Erin M. Harvey1, Jim Schwiegerling2, 1. 1Ophthal
& Vision Science, University of Arizona, Tucson, AZ; 2College of
Optical Sciences, University of Arizona, Tucson, AZ.
Purpose: Children from some Native American tribes are known to
have elevated levels of corneal astigmatism. We report
accommodation-induced changes in higher order refractive
aberrations (coma and spherical aberration) among children of one
such tribe, whose children participated in the tribally sponsored
Tohono O’odham Vision Screening Program (TOVSP).
Methods: Children were imaged with a hand-held Shack-Hartmann
Program Number: 2335 Poster Board Number: B0294
Presentation Time: 2:45 PM - 4:30 PM
Monochromatic Aberrations, Vision and Refractive Error in
Healthy Young Adults
David A. Mackey1, Seyhan Yazar1, Alex W. Hewitt1, Hannah
Forward1, Charlotte M. McKnight1, Alexander X. Tan1, Jenny A.
Mountain2. 1Centre for Ophthalmology and Visual Science,
University of Western Australia, Lions Eye Institute, Perth, WA,
Australia; 2Centre for Child Health Research, University of Western
Australia, Telethon Institute for Child Health Research, Perth, WA,
Australia.
Purpose: Understanding of monochromatic aberrations and their
associations with visual acuity and refractive error in a normal
population is crucial for applying customized intraocular lenses and
laser refractive surgery. In this study, we established the distribution
of monochromatic aberrations from a large cohort of healthy young
adults and investigated association of monochromatic aberrations
with visual acuity and refractive error.
Methods: Ophthalmic examination was conducted on the Western
Australian Pregnancy Cohort (Raine) Study at 20 years of age.
Monochromatic aberrations were measured in 2039 eyes of 1040
participants using Zywave II Wavefront Aberrometer (Bausch &
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Lomb, Inc., Rochester, NY) on natural pupils in a dark room. Bestcorrected logMAR visual acuity (BCVA) was measured monocularly
in normal room illumination. Cycloplegic autorefraction was
performed.
Results: Data from 1007 right eyes were analysed. Median (IQR)
BCVA and spherical equivalent were -0.06 (-0.10, 0) and +0.25 (0.38, 0.63) diopters (D), respectively. The median (IQR) 6mm higher
order aberrations (HOA) was 0.58 (0.44, 0.79) μm. Coma-like
aberrations, third, fourth and fifth HOAs were significantly different
between individuals with BCVA equal to or better than 6/4.8 and
worse than 6/4.8 Snellen score. Fourth order aberrations (Z4-4
p=0.024, Z4-2 p=0.029) and second order aberrations (Z20<0.001)
differed significantly between myopic, emmetropic and
hypermetropic eyes. Individuals with higher myopia had slightly
higher total HOAs.
Conclusions: HOAs in this population were marginally higher than
previously reported values. Our findings confirm that there is a
difference in monochromatic aberrations among different vision and
refractive groups. Results of this study will benefit decision-making
processes in the clinical setting.
Commercial Relationships: David A. Mackey, None; Seyhan
Yazar, None; Alex W. Hewitt, None; Hannah Forward, None;
Charlotte M. McKnight, None; Alexander X. Tan, None; Jenny A.
Mountain, None
Support: Lions Eye Institute, Australian Foundation for the
Prevention of Blindness, Alcon Research Institute
Program Number: 2336 Poster Board Number: B0295
Presentation Time: 2:45 PM - 4:30 PM
Refractive Astigmatism and the components of Astigmatism in
preschool children of China
Jia Huang, Xingtao Zhou, Xiaomei Qu. Ophthalmology, Eye Ear
Nose and Throat Hospital of Fudan University, Shanghai, China.
Purpose: To report the prevalence of refractive (RA), corneal (CA),
and internal astigmatism (IA) in a population of preschool children in
China, we also examine the contribution of corneal and internal
astigmatism components to total refractive astigmatism by power
vectors.
Methods: We examined refraction and eye health in 14116 cases of
3-6 years old children (7310 boys, 51.8%) in Yangpu District,
Shanghai, China. Cycloplegic refractive and keratometri measures
using autorefractor (Canon RK-F1,Japan) and IOL master( Carl
Zeiss, Germany). Of 13080 eligible children, all the data from right
eyes were analyzed. Measures of total and corneal cylinder were
transposed into J0 and J45 components, where positive and negative
J0 values quantified with-the-rule (WTR) and against-the-rule(ATR)
astigmatisms, respectively, and J45 quantified oblique astigmatism.
The difference of RA and CA is IA. We divided the sample into high
RA group (total cylinder≥1 D; mean, 1.56±0.73 D; n =2899) and
normal RA group (0.25D≤total cylinder≤0.75 D; mean, 0.54±0.20 D;
n= 4264).
Results: Overall prevalence of RA (≥1.0 diopter [D]) was 22.16%,
CA (≥1.0 D) 64.21%, IA (≥1.0 D) 40.28%. In high RA group, RA
axis was mainly WTR(81.54%), followed by oblique axis(17.00%),
then ATR(1.46%); in normal RA group, RA axis was also mainly
WTR(61.92%), then oblique axis(31.06%), ATR(7.02%). CA axis
was mainly with the rule (85.69%), while IA axis was mainly against
the rule (76.54%). Regression analysis showed J0 component of CA
was positively correlated with RA only in high WTR astigmats’
group(R2=0.684; P<0.001 ). In all groups, the mean J0 component of
CA were always positive; the mean J0 component of IA are always
negative.
Conclusions: In 3-6 years old preschool children of China,
astigmatism axis is mainly with the rule, especially in the high
astigmatism group, followed by the oblique axis astigmatism and
against the rule astigmatism. Corneal astigmatism is mainly with the
rule, while internal astigmatism is mainly against the rule. J0
components of CA and IA counteract each other in all groups, J45
components of CA and IA also counteract each other in high RA
group, however, J45 components of CA and IA are superimposed on
each other in normal RA group.
Commercial Relationships: Jia Huang, None; Xingtao Zhou,
None; Xiaomei Qu, None
Program Number: 2337 Poster Board Number: B0296
Presentation Time: 2:45 PM - 4:30 PM
Refractive and Corneal Astigmatism in Autistic Spectrum
Disorder
Julie-Anne Little1, Pamela M. anketell1, Stephen M. Gallagher2,
Kathryn J. Saunders1. 1Biomedical Sciences, University of Ulster,
Coleraine, United Kingdom; 2School of Psychology, University of
Ulster, Coleraine, United Kingdom.
Purpose: An increased prevalence of refractive error and increased
astigmatism has been reported in Autistic Spectrum Disorder (ASD)
(Haider et al. 2012). The present study investigated refractive error
and corneal keratometry in children with ASD.
Methods: 89 ASD participants (73 males) aged between 5-16 years,
(mean age 10.7+/-3.2 years) were recruited through a populationbased register and special educational schools. Age-matched controls
were recruited from mainstream schools (n=204). Refractive error
and corneal keratometry were measured using the Shin Nippon
NVision-K 5001 auto-refractor 30 minutes after instillation of
cyclopentolate HCl 1%. Where participants were not able to
cooperate for auto-refraction (AR), retinoscopy was performed.
Refractive errors and corneal powers were transformed into their M,
J0 and J45 vector components for analysis (Thibos et al. 1997).
Results: ASD Success rates: Cycloplegic AR was measured in n=74
children (83%), n=9 non-cycloplegic AR (10%) and n=5 cycloplegic
retinoscopy (6%). One participant did not cooperate for refractive
error measurement. Corneal keratometry was successful for n=63
(71%). Control success rates: Cycloplegic AR n=203 (99.5%).
Corneal keratometry was successful on 186 controls (92%). Table 1
includes summary statistics of the ASD and control data.
No significant difference in J0 data was found for right and left eyes,
so right eye data is presented. Mean refractive and corneal
astigmatism was significantly higher in the ASD group than controls
(one-way ANOVAs F(1,288)=22.6 and 24.1, p<0.00001). Refractive
J0 indicated that 54% of the ASD group had with-the-rule
astigmatism (44% controls), 29% against-the-rule (34% controls) and
18% no astigmatism (22% controls). In ASD, of those with refractive
astigmatism >/=1.50D (n=9), 44% did not wear glasses. Refractive J0
was significantly greater in ASD than controls (one way ANOVA
F(1,288)=3.99, p<0.05). No significant difference between ASD and
controls was found for corneal J0 (one way ANOVA F(1,288)=0.55,
p=0.46). The J45 component was small for both groups and no
significant difference was found between ASD and controls.
Conclusions: This study confirms that refractive astigmatism is
greater in ASD, and tends to be along the primary meridians;
however this is not fully accounted for by the profile of corneal
astigmatism.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
necessary to drive and can improve legally blind vision to a highly
functional level.
Commercial Relationships: Lloyd M. Cuzzo, None; Jesse L.
Berry, None; Peter A. Quiros, None
Table 1
Commercial Relationships: Julie-Anne Little, None; Pamela M.
anketell, None; Stephen M. Gallagher, None; Kathryn J.
Saunders, None
Support: HSC R&D Office Northern Ireland
Program Number: 2338 Poster Board Number: B0297
Presentation Time: 2:45 PM - 4:30 PM
Unmet Need for Corrective Eyeglasses: Follow-up Results from a
Los Angeles County Hospital Survey
Lloyd M. Cuzzo1, 2, Jesse L. Berry1, 2, Peter A. Quiros1, 2.
1
Ophthalmology, Doheny Eye Institute, Los Angeles, CA; 2Keck
School of Medicine, University of Southern California, Los Angeles,
CA.
Purpose: To demonstrate that donated eyeglasses can be used for
vision correction in settings where patients cannot afford to purchase
prescription glasses.
Methods: Patients at the Los Angeles County (LAC) Ophthalmology
clinic who were identified as having refractive error were manifest
refracted and prescribed glasses over a one-month period. Those who
could not afford glasses were given glasses from a donated glasses
collection in the clinic. Donated glasses with closest prescription to
their manifest refraction were given to the patients. Visual acuity
(VA) was recorded without glasses, with manifest refraction (MRx),
and with donated glasses. VA before and after glasses were converted
to logMAR. This study was approved by the University of Southern
California iSTAR Internal Review Board and the methods were in
accordance with the guidelines of Declaration of Helsinki.
Results: The results presented in this study come from the first
month of dispensing glasses from a donated eyeglasses program.
During the month, 7 patients (14 eyes) were refracted and then
provided recycled glasses. Two of the eyes had a VA of no light
perception and thus were excluded from the study. Of the 12 eyes
included in the study, the average logmar VA before glasses was 0.93
which correlates to a snellen VA of 20/170 (range 20/30-20/400).
The average best corrected logmar VA after MRx was 0.32,
correlating to snellen VA of 20/42 (range 20/25-20/100). With
donated glasses the average logmar was 0.41 correlating to a snellen
VA of 20/50 (range 20/30-20/100). Five of the 7 patients (71%) had a
VA less than the level required for driving (20/40 or better in at least
one eye) without glasses but were able to attain ‘driving’ vision with
donated glasses. Three of the 7 (43%) patients were previously
legally blind without corrective refractive lenses (20/200 or worse in
both eyes) but with donated lenses improved on average to 20/70.
Conclusions: Previously the authors have demonstrated that cost is a
major factor in preventing low-income, un- or under-insured patients
at LAC Hospital from obtaining prescription eyeglasses. Donated
eyeglasses are a functional, cost effective means for significantly
correcting refractive error. In many patients they can restore vision
Program Number: 2339 Poster Board Number: B0298
Presentation Time: 2:45 PM - 4:30 PM
Epidemiological profile of ophthalmological care in the Public
Service in Brazil
Marisa N. Figueiredo1, Larissa Rossana S. Stival1, Marcia L.
Machado1, Joao J. Nassaralla2. 1Cornea and Refractive Surgery,
Instituto de Olhos de Goiânia, Goiania, Brazil; 2Retina and Vitreous,
IOG, Goiania, Brazil.
Purpose: To improve health services it is necessary to know the
demand profile. This study was carried out with the 2 objectives: to
identify the main reasons to seek an ophthalmologic public care
service in Brazil (SUS - Brazilian National Health Care System) and
to analyze the frequency of the principal diagnoses, aiming to achieve
goals of loss in eyesight prevention.
Methods: This is an observational, retrospective, cross study
conducted from March to August 2012, at the Instituto de Olhos de
Goiânia (Goiânia Eye Institute), analyzing 1670 patients, therefore
representing a good share of the Goiás State and Mid-Western
Brazilian region. The data were obtained through the analysis of the
medical records with the ICD-10 registration. The studied variables
were age and sex of patient, origin, eye discomfort complaints,
comorbidities and diagnosis (ICD-10).
Results: The ages ranged from 0 to 99 years and the mean age was
56.9 years. There was a predominance of females (58.1%) and the
main origin of patients was Goiânia (61.5%) against 38.5% from
interior. It was detected a prevalence of 45.9% of patients with a
history of Systemic Arterial Hypertension, 16.8% of Diabetes
Mellitus and 5% of glaucoma. The main reason for the consultation
was low visual acuity (70%), followed by burning (26%) and
itchiness (24.4%), as shown in Figure 1. Among the abnormal tests
there was a high prevalence of refractive errors (73.4%) and
presbyopia (59.6%). The cause of refractive errors was astigmatism
(70.5%), hypertrophy (58.6%) and myopia (15.1%). Table 2 shows
other main diagnosis results.
Conclusions: The consequences of blindness are becoming an
important issue in public health. Primary care professionals play a
relevant role in prevention and control of ocular disabilities in their
communities. Understanding the main complaints and common
eyesight health problems in a particular region can help better
manage the public resources and make a better planning for strategic
action aiming to reduce and control visual impairment and blindness.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Marisa N. Figueiredo, None; Larissa
Rossana S. Stival, None; Marcia L. Machado, None; Joao J.
Nassaralla, None
Clinical Trial: NCT01740466
Program Number: 2340 Poster Board Number: B0299
Presentation Time: 2:45 PM - 4:30 PM
Comparison of a Novel Cell Phone-Based Refraction Technique
(Netra-G) with Subjective Refraction
Hilary Gaiser1, Bruce Moore1, Vitor Pamplona2, Nadine Solaka1,
David Schafran1, Dennis Merrill2, Nathaniel Sharpe2, Joe R.
Geringer2, Ramesh Raskar2. 1New England College of Optometry,
Boston, MA; 2EyeNetra Inc, Somerville, MA.
Purpose: To assess the performance of a cell phone based refracting
device (NETRA-G). This study determines the accuracy of this
prototype in determining refractive error in comparison to subjective
refraction (SR).
Methods: NETRA-G (NET) retrofits a high-resolution mobile phone
(Sony Xperia U) by adding a pinhole mask, a film and a lens onto the
display. The device is bi-ocular with the fellow eye viewing an object
at infinity. The subject aligns red and green lines with the translation
on screen proportional to refractive error. 27 subjects (mean + SD age
24.79 +/- 1.60) underwent SR, and NET refraction. Subjects
refractive error ranged from plano to -6.0D (mean + SD refraction 3.34 +/- 1.46D). Exclusion criteria included amblyopia, floaters,
divergent vertical deviation and any ocular pathology. The NET
result was used as a starting point for SR.
Results: For all 27 subjects (54 eyes), the average absolute difference
between NET and SR is 0.31 +/- 0.37D. The refraction determined by
NET is well correlated with that of SR r=0.96 and the two measures
were not statistically significantly different from each other
(p=0.36>0.05). Orthogonal linear regression fit presented a slope of
0.92 and a y-intercept of -0.36D. Average difference on visual acuity
between SR and NET 0.089 +/- 0.13 logMar and 77% received 20/25
or better vision directly from NET.
Conclusions: When compared to SR, NET slightly overestimated the
myopic refractive errors and had a small myopic offset of -0.36D. On
average, the visual acuity difference between SR and NET is less
then a line on the logMar chart. The results show that NET has
potential to be a used as an effective tool for rapidly estimating
refractive errors by non-eyecare professionals. Accuracy of this novel
technique is expected to increase as technology evolves.
Commercial Relationships: Hilary Gaiser, None; Bruce Moore,
EyeNetra Inc. (I); Vitor Pamplona, EyeNetra (E); Nadine Solaka,
None; David Schafran, EyeNetra Inc (R); Dennis Merrill, None;
Nathaniel Sharpe, Eyenetra (E); Joe R. Geringer, Impact Product
Development., LLC (C); Ramesh Raskar, EyeNetra Inc (I)
Program Number: 2341 Poster Board Number: B0300
Presentation Time: 2:45 PM - 4:30 PM
Comparison of Cycloplegic Handheld Autorefraction with
Conventional Cycloplegic Retinoscopy in a Pediatric Population
Smitha Inaganti1, Nisha Krishan-Dave2. 1Ophthalmology, New York
Medical College, New York, NY; 2Ophthalmology, Metropolitan
Hospital, New York, NY.
Purpose: Several studies have found that autorefraction under
cycloplegic conditions is accurate enough to substitute for
cycloplegic retinoscopy in children. The purpose of this study is to
analyze whether cycloplegic handheld autorefraction is accurate and
consistent with cycloplegic retinoscopy performed by ophthalmology
residents in a pediatric population.
Methods: A retrospective chart review was performed of pediatric
patients in an inner-city, resident eye clinic between November 2011
and November 2012. We identified 200 eyes of 100 patients between
the ages of 3 and 17 who underwent post cycloplegic handheld
autorefraction with the Righton Retinomax 3, followed by streak
retinoscopy and subjective manifest refraction, all performed by
second year ophthalmology residents. Spherical equivalence,
spherical power, cylindrical power and axis measurements were
compared.
Results: Spherical equivalence measured by autorefractor was
significantly different from both retinoscopy (p<0.0001) and final
subjective manifest refraction (p<0.0001). There was no significant
difference in spherical equivalence between retinoscopy and manifest
refraction (p= 0.41). Similar differences were found in spherical
power, with autorefractor measurements significantly different from
retinoscopy (p<0.0001) and manifest (p<0.0001) and no significant
difference between retinoscopy and manifest refraction (p=0.98). The
spherical power measured by autorefractor was within +/- 0.5 diopter
range of the manifest refraction in 26% of eyes compared to 84% by
retinoscopy. No significant difference was found between the
autorefractor and retinoscopy for cylindrical power (p=0.79) with
78% of autorefraction cylindrical power measurements within +/- 0.5
D of manifest. Measurement of axis, in 99 of 200 eyes, was
significantly different (p<0.0001), with retinoscopy measuring more
consistent with manifest. Only 63% of autorefractor measurements
were within ten degrees of manifest axis, compared with 98% of
retinoscopy measurements.
Conclusions: Under cycloplegic conditions, there remained a
significant difference between handheld autorefraction and standard
flash retinoscopy. The autorefractor had a tendency toward
overcorrecting spherical power for minus by a mean of 1.1 diopters.
The autorefractor was more consistent with retinoscopy when
measuring cylindrical power, although measurement of axis was
inconsistent.
Commercial Relationships: Smitha Inaganti, None; Nisha
Krishan-Dave, None
Program Number: 2342 Poster Board Number: B0301
Presentation Time: 2:45 PM - 4:30 PM
Evaluating Calibrated Retinoscopy
Clinton N. Sims. Self Employed, Self employed, Fort Myers, FL.
Purpose: To evaluate the accuracy of a 6-8° off axis mathematically
based retinoscopic technique using calibrated converging light to
produce a +0.50D retinoscopic endpoint, the retinoscopic
measurements were compared to those of a subjective refraction. The
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
optical clarity of the +0.50D retinoscopic endpoint was also
compared to an infinity endpoint using diverging light.
Methods: A Copeland Optec 360 Streak Retinoscope (Fig. 1) was
calibrated for a 65cm retinoscopic working distance (RWD) and
marked for a +0.50D retinoscopic endpoint using +1.00D converging
light (CCR+050D) and a infinity retinoscopic endpoint (∞) using 1.50D diverging light. Slide locks maintained the alignment of the
calibration line with the marked positions. The CCR+050D retinoscopic
technique uses the principles of conventional retinoscopy and doesn’t
require a fogging lens. With a phoropter, twenty-six normal and
abnormal eyes of patients aged 11-77 with undilated pupils were
retinoscoped using the CCR+050D technique as they read the Snellen
chart. The +0.50D endpoint was compared to the infinity endpoint by
adding a +1.50D sphere and elevating the calibration line from the
+0.50D position to the ∞ position with the thumb slide. A subjective
refraction was performed and the results compared to the CCR+050D
measurements.
Results: The mean differences and 95% confidence intervals
between the spherical equivalents (SE) and crossed cylinders (X/Cyl)
of the CCR+050D endpoints and subjective refractions were: 0.03(-0.21
to +0.21)DSE and 0.00(-0.21 to +0.21)DX/Cyl. The +0.50D pupillary
reflexes were brighter, sharper and easier to evaluate than the dull
infinity pupillary reflexes.
Conclusions: The results indicate a high degree of accuracy for the
CCR+050D technique in contrast to the accuracy/repeatability studies
of conventional retinoscopy. This is due to the calibrated visible
retinoscopic endpoint plus eliminating the fogging lens, the 0.50D
zone of doubt, the dull undetectable infinity endpoint, cycloplegics
and other disadvantages of conventional retinoscopy. Since
retinoscopes are the only uncalibrated instruments used to measure a
refractive error, they can produce different spherical measurements
and many cannot be calibrated. The clear CCR+050D endpoint should
improve the efficiency of the office and make retinoscopy easier to
perform and teach.
Ocular Refractive State In Fighting Bulls
Juan I Seva1, Manuel Sanes1, Francisco Martinez-Gomariz1, Matteo
Lo Sapio2, Juan M. Bueno2. 1Facultad de Veterinaria, Universidad de
Murcia, Murcia, Spain; 2Laboratorio de Optica, Universidad de
Murcia, Murcia, Spain.
Purpose: Fighting bulls are bred free range on extensive farms under
similar experimental conditions, well-defined manipulation
procedures and hardly human contact. Although they are genetically
selected for a certain combination physical energy and
aggressiveness, their behavior usually differs among animals during
bullfighting. It is believed that bulls present some lateral preferences
and sometimes they do not have a correct (near or far) vision. We
investigate whether differences in the ocular refractive state (RS)
might be part of this lateralized visual processing.
Methods: One-hundred and fifty eyes from 75 fighting bulls were
involved in the study. Animals were obtained from a local
bullfighting arena. They were raised in different farms distributed all
across the country and ages ranged from 48 to 70 months. Enrolment
was preceded by a veterinarian examination to rule out the presence
of any physical factor likely to interfere with the usual fighting. The
RS of each eye was assessed via streak retinoscopy with trial lenses
in the horizontal meridian immediately after the regular bullfighting
took place. Before assessment we ensured the eyes kept their optical
properties intact.
Results: RS values varied between -1.25 and 2.5 D, with a mean of
+0.65 D (SD=+/-0.80 D). Although both eyes were highly correlated
(R=0.79), left eyes tend to be less ametropic. 8% of eyes (12/150)
were myopic (refraction < -0.5 D). Anisometropia (difference in RS
in a pair of eyes > 0.5 D) was detected in 35 animals (23%). RS was
not correlated with either age or weight. No significant differences in
RS among the animals coming from different farms were found.
Conclusions: RS values of fighting bulls varied widely, although
they tend to be slightly hyperopic. This RS could explain their
behavior when stimuli are presented at different locations, especially
at short distances. Moreover, the existence of a certain degree of
anisometropy between pairs of eyes might be a factor contributing to
a possible visual lateralization, and might help to understand
differences in the behavior when the stimulus is presented in front of
an eye or the other.
Commercial Relationships: Juan I Seva, None; Manuel Sanes,
None; Francisco Martinez-Gomariz, None; Matteo Lo Sapio,
None; Juan M. Bueno, None
Support: Ministerio de Edicación y Ciencia, Spain (grants FIS200906234-E)
308 Binocular Vision and Stereopsis
Tuesday, May 07, 2013 8:30 AM-10:15 AM
TCC LL 4/5 Paper Session
Program #/Board # Range: 2658-2664
Organizing Section: Visual Psychophysics / Physiological Optics
Fig. 1 Retinoscope calibrated for CCR+050D and infinity pupillary
reflexes and the RWD.
Commercial Relationships: Clinton N. Sims, US 8,272,739 B2 (P),
US 8,272,740 B2 (P)
Program Number: 2343 Poster Board Number: B0302
Presentation Time: 2:45 PM - 4:30 PM
Program Number: 2658
Presentation Time: 8:30 AM - 8:45 AM
Mechanisms underlying global stereopsis in fovea and periphery
Robert F. Hess, Nirel Witz. Ophthalmology, McGill University,
Montreal, QC, Canada.
Purpose: To better understand the mechanisms underlying global
stereopsis we examined the relationship between carrier luminance
spatial frequency and modulator disparity spatial frequency.
Methods: Thresholds for detecting global sinusoidal disparity
corrugations of equi-detectable spatially band-pass noise were
measured as a function of modulator disparity spatial frequency for
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
both centrally and peripherally located stimuli using a standard 2-IFC
task.
Results: We found a characteristic relationship that depended on
modulator disparity spatial frequency. At high modulator disparity
spatial frequencies (>1 c/d), there is an optimal ratio of around 2.6,
whereas at low modulator disparity spatial frequencies, there is an
optimal absolute carrier luminance spatial frequency (i.e., 3 c/d). In
the periphery, vision is restricted to modulator disparity spatial
frequencies below 1 c/d and, as a consequence, follows the above
rule, there is an optimum absolute carrier luminance spatial frequency
that reduces in spatial frequency with increasing eccentricity.
Conclusions: This finding is consistent with there being more than
one channel processing global stereo. This is subsequently confirmed
using a 2x2 AFC detection/discrimination paradigm. Furthermore,
because of the different carrier/modulator relationships in central and
peripheral vision, peripheral global stereo cannot be simply related to
central global stereo by a scaling factor and thus cannot be simply
due to cortical magnification as previously proposed.
Commercial Relationships: Robert F. Hess, None; Nirel Witz,
None
Support: NSERC (#46528-11)
Program Number: 2659
Presentation Time: 8:45 AM - 9:00 AM
Effect of inter-ocular differences in blur on spatial and stereoresolution
Sowmya Ravikumar1, Bjorn Vlaskamp2, Martin S. Banks1. 1Vision
Science, University of California Berkeley, Berkeley, CA; 2Philips
Research, Eindhoven, Netherlands.
Purpose: Monovision—setting the refraction of one eye to a
different value than the other—is a procedure for dealing with
presbyopia. The difference in refractions for the two eyes should be
the appropriate value for maximizing visual performance, but there is
little research on what the appropriate value is. We know that both
visual acuity and stereoacuity worsen as blur increases. However,
visual-acuity tasks can in principle be performed when one eye is
suppressed, but stereo tasks cannot. Thus, visual acuity might be
limited by image quality in the better eye while stereoacuity might be
limited by the poorer eye. Some previous observations are consistent
with these expectations. Indeed, blur in one eye can be more
detrimental to stereoacuity than the same blur in both eyes (blur
paradox).
Methods: We compared visual acuity and stereoacuity in the same
observers with the same blur manipulations. Stimuli were displayed
binocularly using a custom stereoscope. Accommodation was
paralyzed with cyclopentolate. An artificial pupil set the effective
aperture to 4mm. Blur was introduced with ophthalmic lenses. We
measured visual acuity with a letter-identification task. We measured
stereoacuity using a random-dot stereogram that created sinusoidal
corrugations in depth oriented +/- 20 degrees about the horizontal;
subjects indicated which of two corrugation orientations was
presented.
Results: The results were consistent with our expectations. For
varying amounts of blur in the two eyes, visual acuity closely
conformed to the better eye’s performance while stereoacuity was
largely limited by the worse eye’s blur. Monocular blur had almost
no effect on visual acuity, with binocular visual acuity remaining
close to 20/20 with up to 1.5D blur in one eye. For the same amount
of blur, stereoacuity decreased by a factor of almost two. When the
blur was equal in the two eyes, stereoacuity was slightly better than
when the same blur was present in one eye only (e.g., In comparing
1.5D in both eyes to 1.5D of blur in one eye only, in one subject,
stereo-acuity was 1.98 cpd compared to 1.13 cpd and in another
subject, stereoacuity was 1.54 cpd compared to 1.37 cpd).
Conclusions: The results will help us design monovision protocols in
a way that is the best compromise between visual acuity and
stereoacuity for various viewing distances.
Commercial Relationships: Sowmya Ravikumar, None; Bjorn
Vlaskamp, Philips (E); Martin S. Banks, None
Support: RO1-EY 12851 to MSB
Program Number: 2660
Presentation Time: 9:00 AM - 9:15 AM
Binocular combination of optically-induced asymmetric
interocular blur
Aixa Alarcon1, Len Zheleznyak2, 1, Martin S. Banks3, Geunyoung
Yoon1, 2. 1Flaum Eye Institute, University of Rochester, Rochester,
NY; 2Institute of Optics, University of Rochester, Rochester, NY;
3
Vision Science Program, University of California Berkeley,
Berkeley, CA.
Purpose: It has been reported that interocular mirror symmetry in the
aberrations (or optical blur) is present in the normal population. The
goal of this study was to investigate the effects of interocular
differences of monocular blur orientation on binocular blur
perception.
Methods: Eight cyclopleged subjects were asked to binocularly view
a stimulus under 3 aberration conditions and to match the subjective
blur by inducing defocus to an unaberrated stimulus in 0.05D
increments. A binocular adaptive optics vision simulator was used to
correct subjects’ native aberrations, induce the 3 aberration
conditions and to induce defocus for the blur matching task for a
6mm pupil. A monochromatic (550nm) binary noise image with
random edge orientation served as the stimulus. The aberration
conditions consisted of 0.5 and 1D astigmatism and 1μm coma. The
aberration orientation of the right eye was rotated 0 and 90 degrees
(i.e. equivalent and orthogonal, respectively) in the case of
astigmatism and 0, 90 and 180 degrees in the case of coma while the
left eye’s aberration was held fixed at 0 degrees for all conditions. In
the coma condition, right eye orientations of 0 and 180 degrees
correspond to a binocular mirror asymmetry and symmetry of blur
orientation, respectively. Two subjects participated in the blur
matching experiment in the 0.5D astigmatism condition, and 8
subjects participated in the remaining conditions.
Results: Bilateral equivalent and orthogonal astigmatism of 0.5D
resulted in significantly different blur matches of 0.53±0.05 and
0.36±0.09D, respectively (p<0.01, Student’s t-test). However, the
blur matches for equivalent and orthogonal astigmatism of 1.0D did
not differ significantly (0.81±0.24 and 0.79±0.21D, respectively). In
the case of coma, as the right eye aberration rotated 0, 90 and 180
degrees with respect to the left eye with 0 degree, the blur match
decreased (0.93±0.42, 0.80±0.29 and 0.83±0.37D, respectively). The
perceived blur of coma with bilateral mirror symmetry (180-0
degree) was significantly less than the case of mirror asymmetry (0-0
degree) (p<0.01, Student’s t-test).
Conclusions: Binocular blur perception is reduced when interocular
blur orientations differ. This finding suggests a compensatory
mechanism of the binocular visual system to cope with different
interocular blur orientation, however its capacity likely depends on
the magnitude and relative orientation of blur between the eyes.
Commercial Relationships: Aixa Alarcon, None; Len Zheleznyak,
None; Martin S. Banks, None; Geunyoung Yoon, Bausch & Lomb
(F), Johnson & Johnson (F), Allergan (C), Staar Surgical (C), CIBA
Vision (F), Acufocus (C)
Support: NIH Grant EY014999, Unrestricted Grant from Research
to Prevent Blindness
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 2661
Presentation Time: 9:15 AM - 9:30 AM
The Effect of Unilateral Mean Luminance on Binocular
Combination in normal and amblyopic vision
Chang-Bing Huang1, Jiawei Zhou2, Robert F. Hess2. 1Key Laboratory
of Behavioral Science, Institute of Psychology, Chinese Academy of
Sciences, Beijing, China; 2Department of Ophthalmology, McGill
Vision Research, McGill University, Montreal, QC, Canada.
Purpose: We investigated the role of interocular luminance
difference on supra-threshold binocular phase combination, from
which we wanted to derive the functional balance index between the
two eyes, for both normals and amblyopes. We also attempted to
determine whether we can artificially simulate “amblyopic”
behaviour in normal subjects and recover “normal” response pattern
in amblyopic subjects by inducing luminance difference in the two
eyes, and to understand the theoretical basis of such effects.
Methods: Using a binocular combination paradigm developed by J.
Ding and G. Sperling (2006) and neutral density (ND) filters of
varied intensities, the effect of unilateral mean luminance on
binocular combination in 3 normal and 4 amblyopic observers were
quantified.
Results: In normal observers, attenuation of one eye’s stimulus
luminance with ND filters produces binocular combination similar to
those of amblyopic subjects. Correspondingly, in amblyopic
observers, reduction of the fellow eye’s stimulus luminance produces
binocular combination similar to those of normal subjects. These
results can be well explained by a modified contrast gain-control
model, which suggests that decreasing the mean luminance in one
eye reduces the efficiency of gain-control from that eye to the other
eye, thus lower its contribution in binocular combination.
Conclusions: Our manipulation of interocular luminance difference
provides a simple and effective way to modulate interocular
imbalances in amblyopia by reducing the effectiveness of the signal
originating from the fellow fixing eye, which might bear upon any
future binocular treatment of amblyopia.
Commercial Relationships: Chang-Bing Huang, None; Jiawei
Zhou, None; Robert F. Hess, None
Support: CIHR (# MOP53346) to RFH, and the Knowledge
Innovation Program of the Chinese Academy of Sciences, Institute of
Psychology (Grant No. Y1CX201006 to CBH)
Program Number: 2662
Presentation Time: 9:30 AM - 9:45 AM
The Contribution of Perspective, Blur and Disparity to Depth
Perception in Natural Vision
Guido Maiello1, 2, Manuela Chessa2, Fabio Solari2, Peter Bex1.
1
Department of Ophthalmology, Harvard Medical School, Boston,
MA; 2Department of Informatics, Bioengineering, Robotics and
System Engineering, University of Genoa, Genoa, Italy.
Purpose: Natural scenes contain multiple sources of depth
information. However, the relative contribution of these alternative
cues is not well understood under natural conditions. When these
cues are not accurately simulated in computer generated 3
dimensional scenes, observers can experience visual fatigue, nausea
and diplopia. We examine depth perception in real images with
natural variation in perspective, blur and binocular disparity.
Methods: Image patches subtending 8 degrees of visual angle were
extracted from light field photographs of natural scenes taken with a
Lytro camera that simultaneously captures up to 12 focal planes.
When accommodation at any given plane was simulated, the correct
defocus blur and stereoscopic disparity at other depth planes was
extracted from the stack of focal plane images. Depth information
from geometric cues, relative blur and stereoscopic disparity were
independently introduced into depth images. In a 2AFC paradigm
with feedback, four observers identified the closer of two stimuli
presented concurrently.
Results: Depth discrimination thresholds were lowest when
geometric and stereoscopic disparity cues were both present. Depth
order discrimination was not possible with defocus blur alone and the
addition of blur cues impaired geometric thresholds by reducing the
contrast of geometric information at high spatial frequencies. When
blur cues were introduced along with geometric and disparity cues,
they did not noticeably impair thresholds, and appeared to
compensate the perceptual bias towards the far plane previously
induced by disparity.
Conclusions: Light field photographs are a useful tool to quantify
how naturally-occurring cues contribute to depth perception. Correct
defocus blur diminishes visual fatigue while viewing stereoscopic
stimuli (Hoffman, et al (2008) JoV 8(3), 33,1-33,30) and should
therefore not be discarded in 3D images. Here we show that defocus
cues alone impair fine depth perception near the plane of fixation, but
might be beneficial if used in conjunction with stereoscopic disparity.
Commercial Relationships: Guido Maiello, None; Manuela
Chessa, None; Fabio Solari, None; Peter Bex, Adaptive Sensory
Technology, LLC (S), Rapid Assessment of Visual Sensitivity (P)
Support: NIH Grant R01EY019281
Program Number: 2663
Presentation Time: 9:45 AM - 10:00 AM
Rapid assessment of core visual deficits in amblyopia
MiYoung Kwon1, Luis A. Lesmes1, Alexandra Miller1, Melanie
Kazlas2, Michael Dorr1, David G. Hunter2, 1, Zhong-Lin Lu3, Peter
Bex1. 1Ophthalmology, Harvard Medical School, Boston, MA;
2
Ophthalmology, Boston Children’s Hospital, Boston, MA;
3
Psychology, Ohio State University, Columbus, OH.
Purpose: Amblyopia is the most common cause of monocular visual
loss in children, affecting approximately 3-5% of the population.
Although amblyopia is associated with a wide range of visual deficits
that include reduced visual acuity, loss of contrast sensitivity, spatial
distortion, and abnormal binocular interaction, outcomes for
amblyopia treatment currently monitor only visual acuity. A major
obstacle to broad characterization of the deficits has been inefficiency
of psychophysical assessments such as long testing time. The present
study aims to develop novel methods for rapidly assessing correlation
among these core deficits in amblyopic vision.
Methods: Contrast sensitivity, spatial distortion and binocular
interaction were assessed in subjects with strabismic amblyopia (546-yr-old; mean age =14.38 yrs; n=8), strabismus without amblyopia
(6-84-yr-old; mean age =34.4 yrs; n=15) and normal vision (5-32-yrold; mean age =18.71 yrs; n=24). The contrast sensitivity function
(CSF) was estimated in less than 30 trials with the quick CSF method
(Lesmes et al., 2010) on a handheld device (iPad). Local and global
spatial distortion was measured with a dichoptic pointing task
(Mcilreavy et al., 2010) in which subjects aligned a target dot
presented to their amblyopic eye with a cross-hair presented to their
fellow eye. Binocular interaction was measured with a dichoptic
matching task (Ding & Sperling, 2006) in which subjects matched the
phase of a binocular probe to the cyclopean percept of a dichoptic
pair of gratings whose ratios were systematically varied. Testing was
performed in an ophthalmology clinic with a total testing time of
approximately 20 minutes.
Results: Compared to subjects with normal vision or strabismus
without amblyopia, subjects with amblyopia had significantly
reduced contrast sensitivity (F(2,35) = 4.7, p = 0.015), significantly
larger spatial distortion (F(2,37) = 4.8, p = 0.014) and decreased
interocular contrast summation.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Conclusions: Amblyopia can be characterized by pronounced
deficits in contrast sensitivity, spatial distortion, and binocular
interaction suggesting a higher contrast requirement for the
amblyopic compared to the fellow eye. Despite the short testing time,
our novel methods are as effective as conventional laboratory
assessments for quantifying the core deficits in amblyopia.
Commercial Relationships: MiYoung Kwon, None; Luis A.
Lesmes, Adaptive Sensory Technology (S), 7938538 (P); Alexandra
Miller, None; Melanie Kazlas, None; Michael Dorr, Adaptive
Sensory Technology, LLC (S), Rapid Measurement of Visual
Sensitivity (P); David G. Hunter, REBIScan, Inc (I), Boston
Children's Hospital (P), Johns Hopkins University (P); Zhong-Lin
Lu, US Patent 7,938,538 (P); Peter Bex, Adaptive Sensory
Technology, LLC (S), Rapid Assessment of Visual Sensitivity (P)
Support: NIH Grant R01 EY021553
Program Number: 2664
Presentation Time: 10:00 AM - 10:15 AM
Binocular Visual Acuity with Combined Correction of Spherical
and Longitudinal Chromatic Aberrations
Christina Schwarz, Silvestre Manzanera, Pedro M. Prieto, Pablo
Artal. Laboratorio de Optica, Universidad de Murcia, Murcia, Spain.
Purpose: A previous study (Artal et al., Optics Express 2010)
showed that monocular visual acuity (VA) improved by correcting
spherical aberration (SA) and longitudinal chromatic aberration
(LCA). However, the effect of their combined correction on
binocular visual performance has not been investigated yet. Here, we
measured both monocular and binocular VA when correcting SA and
LCA separately or in combination.
Methods: We used a binocular adaptive optics visual analyzer to
measure binocular and monocular VA at an intermediate contrast of
letters (30%). The instrument (Schwarz et al., Optics Letters, 2011)
allows for modifying the magnitude and phase of the eye’s complex
pupil function. It incorporates two liquid-crystal spatial light
modulators for both wavefront shaping and to create the artificial
pupil. A micro-display presents letters through the controlled eye’s
optics to measure monocular and binocular VA for 4 different cases:
1) natural conditions (LCA and SA present), 2) LCA removed, 3) SA
corrected, 4) LCA removed and SA corrected. In the cases where SA
is present, the average SA value found in pseudophakic patients was
induced (0.149µm for a 4.8mm pupil). LCA was removed by using
monochromatic (532nm) instead of polychromatic light. The three
subjects that took part in this study had also participated in the
previous.
Results: The main tendencies of the previous monocular study were
reproduced, although a different instrument was used and the
technique to correct for LCA was different. Average monocular VA
increased gradually form condition 1) 0.68±0.05; 2) 0.75±0.05; 3)
0.82±0.06 and 4) 1.2±0.2. Average binocular VA for the three
subjects increased from 0.80±0.04 for the case when LCA and SA
were present to 1.2±0.1 for the case when LCA and SA were
corrected. The average binocular summation ratio ranged between
1.0±0.2 and 1.4±0.2, being the smallest in the all-corrected case.
Conclusions: We studied how binocular VA is affected by correcting
longitudinal chromatic aberration and spherical aberration in
combination. The best performance was attained binocularly when
both aberrations were removed. This result may indicates that
bilateral implantation of IOLs correcting both SA and LCA could
further improve binocular spatial vision.
Commercial Relationships: Christina Schwarz, AMO (F);
Silvestre Manzanera, AMO (F), CIBA Vision (F), CALHOUN (F),
VOPTICA (I); Pedro M. Prieto, AMO (F), AcuFocus (F), Voptica
SL (I), Voptica SL (P); Pablo Artal, AMO (C), Voptica SL (P),
Voptica SL (I), AMO (F), Calhoun Vision (F), Calhoun Vision (C),
AcuFocus (C)
Support: Ministerio de Ciencia e Inovación, Spain, FIS2010-14926
and CSD2007-00013; Fundación Seneca, Región de Murcia, Spain
4524/GERM/06; AMO
313 Low Vision Rehabilitation
Tuesday, May 07, 2013 8:30 AM-10:15 AM
Exhibit Hall Poster Session
Program #/Board # Range: 2747-2784/B0001-B0038
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 2747 Poster Board Number: B0001
Presentation Time: 8:30 AM - 10:15 AM
Measuring reading speed: a comparison of reading paragraphs
and single sentences
Susanne Trauzettel-Klosinski, Elke K. Altpeter, Tobias Marx, Nhung
Nguyen. Centre for Ophthalmology, University of Tuebingen,
Tuebingen, Germany.
Purpose: For measuring reading speed, the use of standardized texts
is crucial 2. Single sentences (MN-Read, Radner) are well suited for
assessing critical print size. We developed paragraphs (International
Reading Speed Texts IReST 2) for measuring reading speed, which
showed a high agreement within and between languages (17
languages, linguistically adapted). We hypothesize that paragraphs
are preferable to single sentences for more precise speed
measurement by stopwatch.
Methods: Reading speeds during reading standardized paragraphs of
text ( IReST, German version, texts 3,6,10; 132 words, SD 3.2) were
compared with standardized single sentences (Radner, German
version, texts 1-3; 14 words each). 30 normally sighted elderly native
German speakers (mean age = 64 years, SD 7 years) read the texts
aloud in random order. Reading time was measured by stop watch
and reading speed was calculated in correctly read words/minute
(wpm).
Results: Mean reading speed did not show a relevant difference
between IReST (167 wpm, SD 30.3) and Radner (170 wpm, SD
30.2), (highest mean difference: 7 WPM), when reading speeds of the
total cohort were compared. However, individual variation during
reading 3 texts of each type showed markedly higher standard
deviations for the Radner texts (SD 18.9) than for the IReST texts
(SD 5.2). A clinically relevant difference was defined as > 10 wpm 2.
Conclusions: For group comparisons, the kind and length of text
(IReST or Radner) did not have a relevant influence on reading
speed. For intra-individual measurement of reading speed, IReST
texts showed lower variation between the texts. For higher accuracy
we recommend to use them for repeated measurements, especially for
monitoring the course of a reading disorder and for assessing effects
of interventions.
References
1 Radner W et al (2002) Graefe`s Arch Clin Exp Ophthalmol 240:
461-46
2 Trauzettel-Klosinski S, Dietz K and the IReST Study Group (2012)
IOVS 53:5452-5461
Commercial Relationships: Susanne Trauzettel-Klosinski, None;
Elke K. Altpeter, None; Tobias Marx, None; Nhung Nguyen,
None
Program Number: 2748 Poster Board Number: B0002
Presentation Time: 8:30 AM - 10:15 AM
Properties of the Dutch Reading Charts
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Ger V. Van Rens, Tamara Verkerk Brussee, Edwin Klerkx, Ruth V.
Nispen. Ophthalmology, Free Univ Amsterdam Medical Ctr,
Amsterdam, Netherlands.
Purpose: To investigate some measurement properties of Dutch
reading charts.
Methods: 71 participants (mean age: 55 +/- 19.7 years) with normal
vision read 5 reading charts available in the Dutch language
(“Nederlanders”; LEO; IReST, Radner and Colenbrander). All
sentences and texts were printed at the same size and characters and
were read out loud and timed with a stopwatch. In order to compare
charts, the main outcomes were reading speed in syllables and
characters per minute (corrected for reading mistakes) and the mean
number of mistakes per character.
Results: The corrected reading speed in syllables per minute were in
ascending order of charts
Nederlanders 237/min, Colenbrander 246/min, Leo 269/min, IReST
278/min and Radner 299/min. The corrected reading speed in
characters per minute gave the same order of charts Nederlanders
713/min, Colenbrander 814/min, Leo 823/min, IReST 823/min and
Radner 923/min.
The number of mistakes made in the reading charts per character
were in descending order Nederlanders, Colenbrander, IReST, Leo
and Radner. A one tailed Pearson correlation of the number of
mistakes per character and reading speed per character revealed a
significant correlation for the reading charts that are based on longer
texts, 0.013 in Nederlanders and 0.008 in IReST. No significant
correlation was found in the other three reading charts that are based
on separate sentences.
The range of mistakes for the three reading charts with the highest
reading speeds was significantly lower than that of the Colenbrander
and Nederlanders. The reading speeds decreased from younger to
older age categories, aged 18-35 years (n=19) , 36-59 years (n=18)
and 60-86 years (n=34). This was also true for the number of
mistakes that were made.
Conclusions: Archaic language may have led to more mistakes in the
Nederlanders chart. The 5 Dutch reading charts revealed clear
differences in reading speed and difficulty (number of mistakes).
These findings have consequences for daily practice and for the
possibility to compare scientific outcomes. In the near future, we will
also study the charts with logarithmic progression of character size in
a population of visually impaired participants.
Commercial Relationships: Ger V. Van Rens, None; Tamara
Verkerk Brussee, None; Edwin Klerkx, None; Ruth V. Nispen,
None
Program Number: 2749 Poster Board Number: B0003
Presentation Time: 8:30 AM - 10:15 AM
iPad vs Closed Circuit Television Low Vision Reading Rates and
Preferences
Alex Zemke1, 2, Danielle Irvine1, 2, John Coalter1, Walter M. Jay3.
1
Spectrios Institute for Low Vision, Wheaton, IL; 2The Chicago
Lighthouse for People Who are Blind or Visually Impaired, Chicago,
IL; 3Loyola University Chicago, Maywood, IL.
Purpose: Accessibility features of tablets such as the Apple iPad
have revolutionized reading rehabilitation for low vision patients.
These features include system wide zoom and high reversible
contrast. We compared subjective preference as well as reading rates
on the Apple iPad and a closed circuit television (CCTV).
Methods: After IRB approval, fourteen low vision patients, 18 years
and older, were recruited with visual acuity ranging from 20/50 to
20/200 and minimal prior experience with an iPad or CCTV.
Objective data collection involved calculating reading rates from a
newspaper article and a book. Patients read both media for two
minutes on each device at their preferred zoom, and a third time on
the CCTV with the zoom matched to the iPad’s angle of resolution.
Physical copies were provided to be used on the 24 inch Optelec
Clearview CCTV and electronic copies were acquired for the third
generation iPad. Upon conclusion of the reading assignments,
patients were surveyed with a questionnaire concerning subjective
comfort, performance and preference. Paired t-test with Bonferroni
adjustment was used to compare reading rates. A chi squared analysis
was used for preference responses.
Results: The mean age of the subjects was 62.7 (Std Dev = 13.4)
years and the range was 35 to 91. There were 9 different diagnoses,
with proliferative diabetic retinopathy (5) and glaucoma (2) being the
most common. The mean acuity was 20/108 and the range was 20/50
to 20/200. Twelve of 14 subjects (85.7%) chose the iPad for overall
reading preference (mean age 59.3, mean acuity 20/110). The other
two subjects preferred the CCTV (mean age 83.5, mean acuity
20/100). Faster reading rates of the newspaper with the CCTV at both
the patient's preferred zoom and constant angle of resolution to the
iPad were statistically significant (p = 0.0047 and 0.0080
respectively), while there was no statistical significance between the
CCTV and iPad reading rates with the book.
Conclusions: Despite equal or slower reading rates with the iPad,
patients' subjective preference was in favor of the iPad. Patients'
primary reasons for preference of the iPad were portability, ease of
navigation, and added versatility. Considering these reasons in
addition to lower cost and improved social acceptance, tablets, such
as the iPad, should be considered in the reading rehabilitation of
visually impaired patients.
Commercial Relationships: Alex Zemke, None; Danielle Irvine,
None; John Coalter, None; Walter M. Jay, None
Support: 2012 Illinois Society for the Prevention of Blindness
Research Grant
Program Number: 2750 Poster Board Number: B0004
Presentation Time: 8:30 AM - 10:15 AM
Reading performance in low-vision patients using a low-cost
portable reading system prototype
Adriana Berezovsky, Vagner R. dos Santos, Nívea N. Cavascan,
Solange R. Salomao. Departamento de Oftalmologia, Universidade
Federal de Sao Paulo, Sao Paulo, Brazil.
Purpose: Reading performance is an important tool to evaluate
patients with impaired vision. Reading speed, reading acuity and
critical print size are factors that mainly influence reading
performance in normal and low-vision subjects. The aim of this study
was to investigate the impact of a recently developed low-cost
electronic portable magnifier reading system (PRS) in the reading
performance of low-vision subjects.
Methods: Ten adult subjects (ages ranging from 20 to 92 years) with
low vision and without any training for low vision devices were
included. Reading performance was assessed binocularly with best
optical correction with the Minnesota Reading Speed Chart version
for the Portuguese language (MNREAD Portuguese). PRS apparatus
is composed of a system of image capturing coupled with a 5.6 inch
monochromatic monitor, providing up to 15 x standard
magnification. Parameters of reading speed (words per minute),
reading acuity (logMAR), and critical print size (logMAR) were
determined without and with the PRS prototype. Paired t-test was
used to compare results with and without PRS prototype for reading
performance parameters. When normality test failed, Wilcoxon
signed rank test was used. Statistical significance was set at p≤0.05.
Results: Mean reading speed was 48.4 ± 30.5 words per minute
without PRS, decreasing to 45.0 ± 19.6 words per minute with PRS
utilization without any significance. All subjects showed
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
improvement in both reading acuity and critical print size with PRS
prototype. Mean reading acuity without PRS prototype (1.00 ± 0.23
logMAR) was statistically poorer (t=13.054, p≤0.001) than that
measured with it (-0.08 logMAR ± 0.25). The same trend was found
in mean critical print size, with 1.15 ± 0.18 logMAR without the PRS
prototype and for values significantly better (t=16.694, p≤0.001) with
prototype (0.13 ± 0.25 logMAR).
Conclusions: Considerable improvement in both reading acuity and
critical print size was provided by PRS prototype use. However,
reading speed results had no statistical differences with and without
PRS prototype in this small cohort of patients. Further studies with
large numbers of patients are recommendable to corroborate and
extend the findings with this new promising technology.
Commercial Relationships: Adriana Berezovsky, None; Vagner
R. dos Santos, None; Nívea N. Cavascan, None; Solange R.
Salomao, None
Program Number: 2751 Poster Board Number: B0005
Presentation Time: 8:30 AM - 10:15 AM
Improving reading speed in peripheral vision through a nontask-based training
Deyue Yu. College of Optometry, The Ohio State University,
Columbus, OH.
Purpose: People with central vision loss rely on their peripheral
vision for reading. Previous studies have shown that peripheral
reading can be improved with practice on character-based tasks. An
optimal training paradigm should require little effort from patients to
allow self-administration while providing efficient learning and
prominent improvements. Heretofore, such a paradigm has been
lacking. Here, we introduce a practical and effective training method
that utilizes priming of stimulus identity to facilitate learning in the
absence of a task.
Methods: Seven normally-sighted young adults were trained at 10°
in the lower visual field in a pre/post design. In the pre-test, we
measured reading speeds using Rapid Serial Visual Presentation,
visual-span profile (letter-recognition accuracy as a function of letter
position) with trigrams (strings of three random letters), the spatial
extent of crowding (letter separations yielding 80% recognition
accuracy for the middle letters of trigrams), and isolated-letter
recognition performance. To assess transfer of learning across print
sizes, reading speed was measured at two print sizes (2.5° (trained),
1°). Training consisted of five sessions of viewing trigrams presented
at various letter positions, a total of 7150 trials. Each training session
had 26 blocks. Within each block, the middle letter of the trigram was
always the same. The left and right letters were randomly selected
resulting in differences, across trials, in the perceived appearance of
the middle letter. The observer had no task, but rather was asked to
attend to each trial and learn the known target letter with the option
of repeating the same trigram stimulus for as many times as needed
(averaged 0.4 times). The post-test was identical to the pre-test but in
reversed order.
Results: Averaged across observers, the five-day training reduced the
spatial extent of crowding by 29% and enlarged the visual span by
1.6 characters. The improvements transferred to the untrained reading
task for both the trained print size (reading speed increased from 132
to 298wpm) and the untrained print size (from 68 to 171wpm), which
is beyond what is typically observed in traditional task-based
training.
Conclusions: Our findings demonstrate the effectiveness of utilizing
priming and stimulus exposure in training to improve peripheral
reading. Moreover, this non-task-based training is simple enough to
allow self-training at home.
Commercial Relationships: Deyue Yu, None
Program Number: 2752 Poster Board Number: B0006
Presentation Time: 8:30 AM - 10:15 AM
Effect of Decreased Lighting on Visual Acuity in Normal
Subjects Donald C. Fletcher MD; California Pacific Medical
Center Dept. of Ophthalmology and Smith-Kettlewell Eye
Research Institute. Laura Walker Renninger; Smith-Kettlewell
Eye Research Institute
David T. Hamilton. 1Low Vision Research, CPMC, San Francisco,
CA; 2Low Vision Research, Smith-Kettlewell Eye Research Institute,
San Francisco, CA.
Purpose: Central field loss patients anecdotally report that more light
improves their vision. In a recent study (Fletcher, Renninger, and
Schuchard, 2012), it was reported that indeed acuity declines with
lower light levels. The purpose of this study is to determine the extent
to which light conditions affect visual acuity in normally sighted
subjects.
Methods: Binocular Visual acuity was assessed on 20 normally
sighted volunteers using their habitual correction. Initially a Snellen
letter chart was viewed at one meter under ambient room light.
Participants were tested a second time while wearing 4%
transmission gray filter glasses (NOIR U23) over their spectacles or
contact lenses. The acuity difference is reported as lines difference
with decreased light.
Results: Participants ranged in age from 22-70 (with a mean of 44.85
years). All patients displayed diminished visual acuity when 4%
transmission glasses were worn. Lines difference ranged from 1 (31,
F) to 7 (60, F) with the majority of patients falling in the 2-5 line
range (mean: 2.95 lines, median: 2.5 lines). In Dr. Fletcher's patients,
he observes a mean drop of about two lines (ambient room light vs.
4% transmission gray filter glasses.) My results are slightly more
exaggerated, with almost a full additional mean line drop (2 vs. 2.95
lines.)
Conclusions: A significant reduction in visual acuity was noted with
reduced lighting in this population of normally sighted healthy
individuals. Providing adequate lighting conditions optimizes visual
acuity for tasks such as reading. This is an inexpensive and easily
administered test to evaluate visual performance under dim light
conditions. Pathological conditions are often felt to decrease
functional performance in subdued lighting. This data can serve as a
baseline for comparisons.
Commercial Relationships: David T. Hamilton, None
Program Number: 2753 Poster Board Number: B0007
Presentation Time: 8:30 AM - 10:15 AM
Luminance in Acuity and Reading Performance of Low Vision
Patients
Donald C. Fletcher1, 2, Laura Renninger2, Ronald A. Schuchard3.
1
Ophthalmology, California Pacific Medical Center, San Francisco,
CA; 2Smith-Kettlewell Eye Research Institute, San Francisco, CA;
3
VAPAHCS, Stanford University, Palo Alto, CA.
Purpose: To assess the role of luminance in low vision patients for
visual function tests.
Methods: 152 consecutive low vision patients had assessment of
visual acuity (VA) with habitual correction and with a 4%
transmission gray filter on the ETDRS chart at 1 meter. Reading
acuity on the MN Read was performed in room light and then with
125 (low) and 2070 Lux (high) additional lighting. Central visual
field (CCVFT) was also performed. All tests were done binocularly.
Results: Patient age median (range) was 82 (13 - 101) years with
63% female. All patients were referred for low vision rehabilitation
with 89% having the diagnosis of a maculopathy. Visual acuity with
habitual correction median (range) was 20/100 (20/20 - 20/1000).
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Visual acuity with a 4% transmission gray filter over habitual
correction median (range) was 20/220 (20/20 - 20/2000). Change in
visual acuity with the decreased luminance was median (range) 2
lines decrease (plus 2 - minus 10 lines). On the MN Read test the low
additional light gave no performance increase in 44% of patients, a
one block increase in 50% and a 2 block increase in 6%; the high
additional light gave no performance increase in 12% of patients, a
one block increase in 29% and a 2 block increase in 32% and a
greater than 2 block increase in 27% with up to an 8 block increase in
one patient. Ring scotoma patients (25) improved 1 block (range 0 2) on the MN Read with low additional light and 4 blocks (range 1 8) with high additional light. Non ring-scotoma patients (107)
improved 0 blocks (range 0 - 2) on the MN Read with low light and 2
blocks (range 0 - 5) with high light. There is a significant moderate
correlation between the lines lost with the filters and improvement
with additional lighting - 125 Lux (r = 0.30) and 2070 Lux (r = .49).
Of particular interest, patients with ring scotomas had the largest
improvements in reading with extra light.
Conclusions: There is a significant tendency for acuity to drop with
decreased luminance and this had some tendency to predict response
to extra light. There was a consistent positive improvement in reading
acuity with extra light and especially with very bright light. All
patients and particularly those with ring scotomas should have trials
with very bright illumination in their rehabilitation program.
Commercial Relationships: Donald C. Fletcher, Precision Vision
(R); Laura Renninger, None; Ronald A. Schuchard, QLT Inc. (C)
Program Number: 2754 Poster Board Number: B0008
Presentation Time: 8:30 AM - 10:15 AM
SK-Read performance as a predictor of handwriting difficulty in
low vision patients
Ken Downes1, 2, Donald C. Fletcher1, 2, Laura Renninger2.
1
Ophthalmology, California Pacific Medical Center, San Francisco,
CA; 2Smith-Kettlewell Eye Research Institute, San Francisco, CA.
Purpose: To assess whether performance on the Smith-Kettlewell
Reading (SK-Read) Test is a reliable predictor of handwriting in low
vision patients.
Methods: We performed a prospective cohort study of 31 low vision
patients at their initial low vision rehabilitation evaluation. The
patients completed all components of a routine low vision
appointment including logMAR acuity measurement, performed the
SK-Read Test (a non-conextual reading test), and performed a
handwriting task. Patients were timed while performing each task and
their accuracy was recorded. The handwriting task was performed by
having patients write five five-letter words into sets of boxes where
each letter is separated by a box. The boxes were 15mm x 15mm and
accuracy was scored with 50 points possible from 25 letters - one
point for each letter within the confines of a box and 1 point if the
letter was legible. The variables reported on are SK-Read errors per
block, SK-Read time per block, logMAR acuity, and handwriting
task time-to-accuracy ratio. Correlation analysis was performed to
examine the association between each pair of variables.
Results: 31 low vision patients participated in the study. Median age
was 81.5 years (range: 54-97). 27/31 patients (87%) had ARMD or
some other maculopathy while 3/31 patients (13%) had visual
impairment from media opacity or neurological impairment. Median
Snellen Acuity was 20/152 (range: 20/22-20/1000) and median
logMAR acuity was 0.88 (range: 0.04-1.70). SK-Read errors per
block correlated with logMAR acuity (r= 0.55, p<< 0.01) and SKRead time per block correlated with logMAR acuity (r=0.38, p=0.03).
SK-Read errors per block correlated with handwriting task time-toaccuracy ratio (r=0.68, p<< 0.01). SK-Read time per block correlated
with handwriting task time-to-accuracy ratio (r=0.84, p<<0.01).
LogMAR acuity score correlated with handwriting task time-toaccuracy ratio (r=0.35, p=0.053).
Conclusions: SK-Read may be a more reliable predictor of
handwriting performance than logMAR acuity in low vision patients.
SK Read difficulty has been associated with presence of central
scotomas which may also be associated with difficulty in visually
guided motor activity. Further study is warranted to examine the
implications of SK-Read performance on vision-related disability in
low vision patients.
Commercial Relationships: Ken Downes, None; Donald C.
Fletcher, Precision Vision (R); Laura Renninger, None
Program Number: 2755 Poster Board Number: B0009
Presentation Time: 8:30 AM - 10:15 AM
Using Mirametrix Eye Tracking Technology to Evaluate
Eccentric Reading
Joseph J. Zinkovich1, Erika Anderson2, Erin Doxtader2, Michelle
Nguyen2. 1School of Optometry, Massachusetts College of Pharmacy
and Health Sciences, Worcester, MA; 2Arizona College of
Optometry, Midwestern University, Glendale, AZ.
Purpose: The aims of the present study were two-fold: 1. To develop
and evaluate methods of utilizing a Mirametrix eye tracker to
evaluate eccentric reading. 2. To compare eccentric viewing results
with published anatomical descriptions of the fovea.
Methods: Using binocular point of gaze (POG) data captured on
Cartesian coordinates, eccentric viewing (EV) distances (by step
approach in four directions), and eccentric reading (ER; by
dynamically presenting and hiding words in the four directions), were
evaluated in 3 subjects.
Results: The average distances and standard deviations for EV were:
inferior: 27.3mm ±2.92; superior: 28.0 ±2.67; right: 43.25 ±2.55; left:
43.92 ±2.76. ANOVA analysis provides sufficient evidence to
suggest that the EV distances between three subjects are the same for
inferior (p=0.99), superior (p=0.40), right (p=0.98), however, for left,
it was the same for two of the three subjects (p=0.46). Analysis
suggests that ER difficulty is the same for inferior versus superior
(p=0.34), right versus left (p=0.65), but different for vertical versus
horizontal meridian (p<0.001).
Conclusions: EV was similar among subjects except when using left
retina for one subject, which we believe shows the identification of
the subject’s history of a binocular vision problem. The vertical to
horizontal ratio (0.634) of our findings is similar to the anatomical
ratio (0.667) of the fovea. The use of vertical directions during ER is
similar in terms of distance and difficulty, as is the horizontal
directions, but markedly differing between the two. Preliminary use
of the Mirametrix eye tracker along with our methodology proves to
be a useful research or clinical tool.
Commercial Relationships: Joseph J. Zinkovich, None; Erika
Anderson, None; Erin Doxtader, None; Michelle Nguyen, None
Program Number: 2756 Poster Board Number: B0010
Presentation Time: 8:30 AM - 10:15 AM
Search during Word Recognition in Visual Noise with the Laser
Scanning Digital Camera Stimulator
Elli J. Kollbaum1, Christopher A. Clark1, Bryan P. Haggerty1, Benno
L. Petrig1, 2, Ann E. Elsner1, 2. 1School of Optometry, Indiana
University, Bloomington, IN; 2Aeon Imaging, LLC, Bloomington,
IN.
Purpose: In this study we analyzed the visual search pattern of naive
subjects during a novel word recognition task. Varied levels of
contrast were presented by adding visual noise to word and
background in the Laser Scanning Digital Camera Stimulator (LSDCS). The stimuli were designed to simulate widespread internal visual
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
noise found in ocular and neurological disease, as opposed to focal
pathology.
Methods: The 11 subjects included 4 male and 7 female, ages 22 - 50
yr with visual acuity of 20/20. The stimulus was a 20/200 optotype, 2
- 3 syllable word in Arial font presented centrally in the LSDC-S. A
16 word list was generated from the Low Vision Training Manual
(Quillman). The LSDC-S is a slit scanning imager that provides a
high contrast, 11 Hz and 36 deg retinal image, 860 nm at 2 mW at the
cornea. The visual stimuli were projected by a digital light projector
in Maxwellian view, with linked stimulus and retinal image focus.
The background illuminance and the contrast for stimuli and
background matched Goldmann perimetry, 1.5 log units. Levels of
noise, at a fixed spatial frequency, were presented with the words,
starting with 9% and then lowered by 3% over 4 levels until the word
was recognized. The trial was stopped if recognition did not occur in
6 sec, and the time to recognition was recorded for the final trial.
Fixation and sample scan patterns were evaluated from the x, y
coordinates of a retinal image feature over time, plus the probability
of accuracy.
Results: Despite the large letter size, this task was difficult for all
subjects, who recognized no words with noise > 6% contrast. The
average jump in scanning on the x axis was 2.62X larger than for y
(p<0.0001). However, the jump size varied, 3.31X to 2.10X for the
highest vs. lowest contrasts. One prominent search pattern was to stay
at a specific point on the x axis, scan along the y axis, then jump to
the next x axis locus. In a subset of the data, the eye movements for
two hard words differed from two easy words, (p= 0.006). Smaller
jumps were typical for difficult words, “learned” than easier words,
“morning.”
Conclusions: The LSDC-S word recognition task is a novel visual
assessment method with varied noise contrast levels. Analysis of
fixation reveals both word difficulty and directional differences in
search patterns. These data may assist in reading assessment and
associated rehabilitation.
Commercial Relationships: Elli J. Kollbaum, None; Christopher
A. Clark, None; Bryan P. Haggerty, None; Benno L. Petrig, Aeon
Imaging LLC (E), Aeon Imaging LLC (P); Ann E. Elsner, Aeon
Imaging, LLC (I), Aeon Imaging, LLC (F), Aeon Imaging, LLC (P)
Support: NIH/NEI EY018772
Program Number: 2757 Poster Board Number: B0011
Presentation Time: 8:30 AM - 10:15 AM
Low-power Half Lens Prisms For The Rehabilitation Of
Hemianopia
Giovanni Sato1, Roberta Rizzo1, Gianfrancesco M. Villani2, 1. 1Centro
di Riabilitazione Visiva, Ulss16, Ospedale S. Antonio, Padova, Italy;
2
Ophthalmology, Centro Riabilitazione Ipovedenti e Microperimetria
- CRIM, Castel d'Azzano, Italy.
Purpose: To evaluate the expansion of visual fields in hemianopia
after binocular application of low-power prisms
Methods: Retrospective study of 26 patients with different types of
hemianopic defects secondary to cerebral lesions: 10 with right
homonymous hemianopia, 11 with left homonymous hemianopia, 2
with upper-right homonymous quadrantopsia, 1 with lower-right
homonymous quadrantopsia, 1 with bitemporal heteronymous
hemianopia, 1 with a complex type of hemianopic defect combined
with hemianopic macular scotoma. Evaluation included ETDRS
BCVA at 4m, Greene Test, Humphrey visual field test 30-2, and
Esterman binocular visual field test before and after application of
binocular correction with low-power half lens prisms (≤10 prismatic
diopters) with the base placed towards the blind site. Main outcome
measures were tolerance to prisms and expansion of Esterman
binocular grid. To measure personal satisfaction, a custom
questionnaire for visual adaptation to prism lenses and the
Environmental Social State test (ESS) were used
Results: Age median (range) was 54 (19-83) years, and BCVA was 0
(0-2) logMAR. Prismatic correction ranged from 8 to 2 prismatic
diopters (median 6 D). Esterman binocular visual field on the
meridian of greater involvement measured 80° median (range 40100°) before treatment, and 100° (50-120°) after the application of
prismatic lenses. The median of visual field expansion was 10°
(range 5-35°). Tolerance as reported by patients about the use of
prisms during the activities of daily living was high in all but 2
patients: so, 24 patients (92.3%) wore prisms all day. Among these,
only one patient complained about image displacement. Orientation
and mobility improvement was the most frequent achievement, and 7
patients regained their driving license. Patients also reported reading
with more ease
Conclusions: Low-power half lens prisms for the rehabilitation of
hemianopia resulted in an expansion of binocular visual fields and
were well tolerated by a great majority of patients, so that prisms
were worn all day in 92.3%. The highest satisfaction was reported
about the increase in orientation and mobility (7 patients had their
driving license back!), and in reading endurance
Commercial Relationships: Giovanni Sato, None; Roberta Rizzo,
None; Gianfrancesco M. Villani, Letter Scotometry/Marte srl ©
TX0007576130 / 2012-04-25 (P)
Program Number: 2758 Poster Board Number: B0012
Presentation Time: 8:30 AM - 10:15 AM
Peripheral Prisms Increase Blindside Eye And Head Scanning
Movements During Outdoor Walking In Hemianopes:
Preliminary Results
Matteo Tomasi, Jeffrey Churchill, Jean Paul Wiegand, Kevin
Houston, Eli Peli, Alexandra R. Bowers, Gang Luo. Schepens Eye
Research Institute, Boston, MA.
Purpose: Peripheral prism glasses are used as a field expansion
device for hemianopia. As the field expansion is always present at all
lateral gaze positions (unlike other designs), it should provide a
constant stimulus to initiate eye and/or head movements to the blind
side. We tested the hypothesis that peripheral prisms would increase
eye and head scanning movements toward the blind hemifield in an
outdoor walking task (as gaze behaviors in lab-based tasks may not
be representative of those in a natural environment).
Methods: To date 7 people with homonymous hemianopia walked
0.8-mile routes on busy downtown streets, with and without prism
glasses, on two occasions: immediately after receiving peripheral
prism glasses and 1.5 months later. Between the two visits, each
subject received 12 hours of in-lab perceptual-motor training with the
prism glasses and wore the device at home on a daily basis. During
the walks, their eye and head movements were recorded using a head
mounted eye tracker and inertial motion sensors, respectively. We
defined the neutral point as the most frequent sample of the
distribution for eye movements, and the standard anatomical position
for head movements. We analyzed the eye/head movements within
the blind and seeing sides (with respect to the neutral point) as the
sum of the amplitudes divided by the total number of samples. A 10°
range around the neutral point was excluded to minimize the impact
of random and less-meaningful fluctuations. A repeated-measures
ANOVA was used to evaluate the effects of prism (with/without),
side (seeing/blind) and training (pre/post).
Results: Patients had a trend to bias their eye-in-head position
towards the blind side when wearing the prisms but not when
walking without them (prism-by-side interaction p = 0.081). After
training, there was a trend for patients to increase their head turns
towards the blind side when wearing the prisms (prism-by-training
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
interaction p=0.070). However, the overall distribution (standard
deviation) of eye positions appeared to be narrower after training
(from 12.7° to 11.2°, p=0.081) suggesting that there might be an
environmental learning effect.
Conclusions: Preliminary results from this study suggest that
peripheral-prism glasses may increase scanning toward the blind side
in patients with hemianopia; recruitment is ongoing to increase the
sample size.
Commercial Relationships: Matteo Tomasi, None; Jeffrey
Churchill, None; Jean Paul Wiegand, None; Kevin Houston,
None; Eli Peli, Alcon Research , Ltd, Tx (C), Chadwick Optical (P),
Emerald Events (R), Google (C), Nintendo of America (C), ReVision
Optics, CA (C), SuperFocus (C), Trivisio Prototyping Gmbh (C),
VisionCare Inc (C), Butler Law Group (C), Dillon & Findley, P.C.
(C); Alexandra R. Bowers, None; Gang Luo, None
Support: NIH grant 2K12EY016335-06, DoD grant DM090420,
Harvard Milton Award
Program Number: 2759 Poster Board Number: B0013
Presentation Time: 8:30 AM - 10:15 AM
Perceptual-motor adaptation in hemianopes wearing peripheral
prisms is possible: Preliminary results
Kevin Houston1, 2, Jeffrey Churchill2, Jean Paul Wiegand2, Eli Peli2,
3
, Gang Luo2, 3, Robert B. Goldstein2, 3, Russell L. Woods2, 3,
Alexandra R. Bowers2, 3. 1Ophthalmology, Massachusetts Eye and
Ear, Boston, MA; 2Schepens Eye Research Institute, Massachusetts
Eye and Ear, Boston, MA; 3Ophthalmology, Harvard Medical
School, Cambridge, MA.
Purpose: For hemianopia, peripheral prism (p-prism) glasses are
used to optically shift peripheral areas of the blind hemifield 20°-30°
toward the seeing side. This improves detection immediately
however perceived location of prism side obstacles is incorrect. With
general wear, some hemianopes make cognitive corrections for the
displacement, but perceptual adaptation does not occur (Giorgi et al
2009). We are conducting a pilot study to evaluate whether intensive
perceptual-motor training improves adaptation and generalizes to
improved collision judgments in a walking simulator.
Methods: Seven hemianopes wearing 57Δ oblique p-prisms received
120 minutes of computerized training over 3 weeks consisting of
reaching out to touch peripheral stimuli presented on a touch screen
under fixed gaze conditions. Training included 5 levels of difficulty
starting with slow but accurate reaching to blind side stimuli (level
1), reaching to stimuli in both hemifields (level 2), increasing speed
(level 3), cognitive loading (level 4), and use of background visual
cues (level 5). Collision judgment data under fixed gaze conditions
were collected in a video walking simulator before and after training.
Results: Touch accuracy error to targets presented in prism areas
improved significantly (p=0.02) from median (x,y) (17°, 6°) to (1° ,
0.5°) (equivalent to seeing-side accuracy). The median difference
between seeing and prism side reaction times reduced significantly
(p=0.04) from 880ms to 110ms. Preliminary analyses of collision
judgment data suggest no or only modest improvements in
performance post-training.
Conclusions: These pilot data suggest that hemianopes wearing pprisms can be trained to perform similarly on the blind and seeing
side during a perceptual-motor task. We suspect the mechanism of
adaptation for most participants was realignment of the felt position
of the arm (as opposed to retinotopic coordinates), and so did not
generalize. We are developing pre- and post- test measures to
investigating this hypothesis by looking for transfer to the untrained
hand.
Commercial Relationships: Kevin Houston, None; Jeffrey
Churchill, None; Jean Paul Wiegand, None; Eli Peli, Alcon
Research , Ltd, Tx (C), Chadwick Optical (P), Emerald Events (R),
Google (C), Nintendo of America (C), ReVision Optics, CA (C),
SuperFocus (C), Trivisio Prototyping Gmbh (C), VisionCare Inc (C),
Butler Law Group (C), Dillon & Findley, P.C. (C); Gang Luo, None;
Robert B. Goldstein, None; Russell L. Woods, None; Alexandra
R. Bowers, None
Support: NIH grant 2K12EY016335-06, EY12890 and DoD grant
DM090420, W81WXH-07-2-0038
Program Number: 2760 Poster Board Number: B0014
Presentation Time: 8:30 AM - 10:15 AM
Contrast Sensitivity (CS) test-retest reliability and consistency
with Vector Vision CSV-1000LVand CSV-1000HGT in patients
with Albinism
Maria Cucuras1, Susan Kelly2, Faheemah Saeed3. 1Illinois College of
Optometry, Chicago, IL; 2Illinois College of Optometry, Chicago, IL;
3
Illinois College of Optometry, Chicago, IL.
Purpose: The ability to accurately monitor the disease status or
improve the visual function of low vision patients requires reliable
and repeatable vision tests. It is generally accepted that measures of
visual function in the low vision patient population are more variable
than normally sighted individuals. This may decrease the reliability
of standard visual tests when applied to a population such as
albinism. The purpose of our study is to determine whether one such
test of visual function, contrast sensitivity, could reliably be
measured in this population both in the presence of glare and without.
Methods: CS was tested with Vector Vision CSV-1000 LV which is
a low vision letter chart and the CSV-1000HGT (halogen glare test)
which tests CS in the presence of glare.
Thirteen subjects with albinism with best corrected logMAR visual
acuity (VA) ranging from 0.4 to 0.9, participated in this study.
LogMAR VA was tested using the EDTRS chart. Dependent
variables including CS under normal test condition and CS with
glare, were tested at two different visits, 3 months apart. The CSV1000LV chart was used to measure CS while the CSV1000HGT was
utilized to measure the effect of glare on CS. Test-retest reliability
was assessed with the intraclass correlation coefficient (ICC).
Results: A significant test-retest reliability was determined according
to the ICC values calculated for both CS measured without and with
glare (ICC=0.864, p<0.001; ICC=0.455, p= .048) respectively.
Conclusions: CS in patients with albinism, as tested with Vector
Vision CSV-1000LV and CSV-1000HG is repeatable and consistent,
indicating that this test is a reliable tool for measuring visual function
in this particular low vision population.
Commercial Relationships: Maria Cucuras, None; Susan Kelly,
None; Faheemah Saeed, None
Program Number: 2761 Poster Board Number: B0015
Presentation Time: 8:30 AM - 10:15 AM
Analyses of contrast sensitivity assessments over time: A pilot
study
Xi Chen, Luis A. Lesmes, Jennifer Wallis, Thomas S. Wallis, Mary
Lou Jackson, Peter Bex. Department of Ophthalmology,
Massachusetts Eye and Ear Infirmary, Boston, MA.
Purpose: The contrast sensitivity function (CSF) provides a useful
functional endpoint for development of ophthalmic drugs and
devices. Evaluation of CSF assessment over time is critical for
tracking the progression or remediation of CSF deficits. In this pilot
study, we examined a series of repeated CSF assessments, to evaluate
method reliability, and examine trends (such as learning) using a
time-based analysis that may be useful for future evaluation of
clinical therapies.
Methods: In 5 subjects with corrected-to-normal vision (ages ranging
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
from 20 to 57), we tested contrast sensitivity weekly over a 4-8-week
period with the novel quick CSF method (Lesmes et al, 2010) and
established contrast sensitivity charts (Pelli-Robson and Vistech). To
assess reliability, two runs of 20 quick CSF trials were collected at
each session, and each run lasted approximately 3 minutes. We
focused on the general contrast sensitivity assessment provided by
the area under the log CSF (AULCSF).
Results: The AULCSF values demonstrated excellent test-retest
reliability (r = 0.91) between runs, averaged across weeks. The
coefficient of variation (sd/mean) for within-session difference scores
<12%. We applied a Bayesian hierarchical linear model to analyze
the AULCSF values, with model terms that signified learning
patterns: either changes across weeks or across runs in the same
session. The significant differences observed between subjects were
expected age-related effects, though Pelli-Robson and Vistech
exhibited no difference across observers. The stability of CSF
assessments between and within repeated testing sessions was
confirmed by slope coefficient estimates that were not credibly
different from zero at the population level.
Conclusions: For clinical studies using contrast sensitivity endpoints,
it is critical to evaluate trends over time. The current study
demonstrated that the quick CSF method provides reliable contrast
sensitivity assessments using a statistical framework based on a
hierarchical analysis. Together, these tools demonstrate potential for
future studies that identify the progression of visual impairment, or
its remediation with therapeutic intervention.
Commercial Relationships: Xi Chen, None; Luis A. Lesmes,
Adaptive Sensory Technology (S), 7938538 (P); Jennifer Wallis,
None; Thomas S. Wallis, None; Mary Lou Jackson, None; Peter
Bex, Adaptive Sensory Technology, LLC (S), Rapid Assessment of
Visual Sensitivity (P)
Support: RO1EY01928
Program Number: 2762 Poster Board Number: B0016
Presentation Time: 8:30 AM - 10:15 AM
The Reliability of the quick CSF Method for Contrast Sensitivity
Assessment in Low Vision
Luis A. Lesmes, Jennifer Wallis, Mary Lou Jackson, Peter Bex. Dept
of Ophthalmology, Mass Eye and Ear Infirmary, Harvard Medical
School, Boston, MA.
Purpose: The contrast sensitivity function (CSF) presents a better
characteristic of functional vision than visual acuity. The quick CSF
is a novel adaptive method that greatly reduces CSF testing times,
using Bayesian adaptive inference and a trial-to-trial information gain
strategy. In an application of the quick CSF to assess low vision
(Lesmes et al, ARVO 2012), we reported that only 2-3 minutes (15
trials) were needed to obtain estimates of the area under the log CSF
(AULCSF), which were correlated with Pelli-Robson contrast
sensitivity. The current study was designed to complement the
previous demonstration of method accuracy, and assess method
reliability using repeated measurements in patients with normal and
impaired vision.
Methods: CSF assessments were obtained from people with normal
and impaired vision. Each observer completed two CSF tests (~3
minutes each). Reliability was assessed via the AULCSF difference
scores, calculated between estimates obtained from repeated CSF
assessments.
Results: Two important results were: (1) AULCSF estimates
obtained in normal vision were slightly more reliable than those in
impaired vision and (2) in both groups, AULCSF estimates
demonstrated greater reliability with increasing test length. For
normal vision, differences between repeated AULCSF estimates
exhibited a coefficient of variation (CV) of ~15% after 15 trials and
<10% after 20 trials. For impaired vision, CV values were ~20% after
15 trials and <15% after 20 trials. This level of variability, considered
between repeated measurements, is small when compared to the
individual differences (population variability) in sensitivity exhibited
in either the normal or impaired vision groups.
Conclusions: These results suggest that the quick CSF provides a
rapid and reliable contrast sensitivity assessment in normal and
impaired vision. The broad contrast sensitivity measure provided by
the AULCSF, which can be assessed in a short, clinically practical
testing time, demonstrates potential value as a functional endpoint for
clinical practice and clinical trials.
Commercial Relationships: Luis A. Lesmes, Adaptive Sensory
Technology (S), 7938538 (P); Jennifer Wallis, None; Mary Lou
Jackson, None; Peter Bex, Adaptive Sensory Technology, LLC (S),
Rapid Assessment of Visual Sensitivity (P)
Support: EY019281
Program Number: 2763 Poster Board Number: B0017
Presentation Time: 8:30 AM - 10:15 AM
Contrast Sensitivity Measurement in the Pediatric Low Vision
Setting
Gregory R. Hopkins, Angela M. Brown. College of Optometry, The
Ohio State University, Columbus, OH.
Purpose: A new test of contrast sensitivity (CS), the Stripe Cards of
Contrast Sensitivity (SCCS) test, can serve as a simple and efficient
means for estimating the maximum contrast sensitivity value of a
given patient without having to use multiple spatial frequency
gratings, and without knowing the spatial frequency at which
maximum sensitivity occurs. This test could be useful for a wide
range of patients with various levels of visual acuity (VA), ages, and
diagnoses.
Methods: We measured VA [Bailey-Lovie (BL), Teller Acuity Cards
(TAC)] and CS [Pelli-Robson (PR), SCCS] in counterbalanced order
of 26 subjects at the Ohio State School for the Blind. Thus, we tested
VA and CS using letter charts (BL, PR) and grating cards (TAC,
SCCS). Testing distance was 58 cm for the grating cards, and was
adjusted based upon nominal visual acuity for letter charts. Subjects
used the dominant or better eye only. Letter chart scoring was letterby-letter with no substitutions. Time of testing was recorded for each
test.
Results: Measurements were obtained on 24 (92%) subjects using all
four tests. Two additional subjects could not read letter charts, but
were able to complete the TAC and SCCS. Median acuity values
were: 1.09 [interquartile range (IQR)=0.71-1.41] for B-L, 0.59
[IQR=0.34-0.82] for TAC. Median log CS was 1.38 [IQR=0.81-1.75]
for P-R. The SCCS test showed a ceiling effect, with 65% of subjects
scoring the maximum CS (1.65); the upper quartile value was 1.35.
The subjects with impaired CS on the PR (according the WHO
standards, PR<1.65) showed reliably better sensitivity on the SCCS
test than the PR test (sign test, p= 0.002, 2-tailed; nonparametric test
required because of the ceiling effect on the SCCS). All subjects had
impaired VA, and they showed reliably better TAC acuity than
logMAR acuity (Paired t-test, p=0.001, 2-tailed, no ceiling effect).
Testing times averaged 54 ± 33 sec (B-L) and 96 ± 65 sec for TAC,
averaged 61 ± 42 sec for P-R and 58 ± 46 sec for SCCS.
Conclusions: Both of the grating tests (SCCS and TAC) gave better
sensitivity than the corresponding letter charts for subjects with
reduced vision. For measuring contrast sensitivity in those with
reduced vision, the simpler task and bolder patterns of the SCCS may
make it more likely to reveal the maximum performance that a given
patient can achieve.
Commercial Relationships: Gregory R. Hopkins, None; Angela
M. Brown, Precision-Vision (P)
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Support: NEI Grant: R41EY022545-01
Program Number: 2764 Poster Board Number: B0018
Presentation Time: 8:30 AM - 10:15 AM
Feedback measures for a wearable visual aid designed for the
visually impaired
Aminat Adebiyi1, James D. Weiland1, 2, Carey Zhang1, 3, Kaveri
Thakoor4. 1Biomedical Engineering, University of Southern
California, Los Angeles, CA; 2Ophthalmology, University of
Southern California, Los Angeles, CA; 3Electrical Engineering,
University of Southern California, Los Angeles, CA; 4Neuroscience
Graduate Program, University of Southern California, Los Angeles,
CA.
Purpose: To test the viability of a voice-driven feedback system to
assist low-vision subjects with mobility.
Methods: The audible feedback system consists of audio boneconduction headphones worn by the user behind the ear and a custom
Android application, which delivers commands to the user when a
researcher presses a button corresponding to that command on the
program. Two low-vision subjects were recruited from the Braille
Institute, Los Angeles. Wearing the audible feedback system,
subjects were steered around a three minute randomized course five
times by a researcher, who gave commands that were randomized by
trial. Commands included ‘forward’, ‘veer left’, ‘turn left’, ‘veer
right’, turn right’ and ‘stop’. The course measured 17ft X17ft and
was interspersed with one foot cones every five feet. Appropriate
response to commands, angle of turns and reaction time were
measured. Subjects were also given an exit survey that measured the
usability of the feedback system. The Android application recorded a
time stamp for each command and video footage was recorded for
each trial.
Results: Subject one had an average of 71.80% responses consistent
with commands, whereas subject two had an average of 53.18%
responses consistent with commands; although subject two showed a
higher range in improvement over the course of the trials. Both
subjects had an average of 95% positive compliance to the ‘forward’
and ‘stop’ commands, and less than 5% compliance to the ‘veer left’
and ‘veer right’ commands. Subject one had an average reaction time
of 1.5 seconds, whereas subject two had an average reaction time of
2.5 seconds. Both subjects had an average turning radius of
approximately 70 degrees for the ‘turn right and ‘turn left’
commands. Based on the system usability scale, the system was
determined to be 90% useable in its current condition.
Conclusions: Judging by the reactions times and the system usability
scale, the audible feedback system seems to be an intuitive solution
that will create a balanced connection between the user and the
feedback controller. However, significant training is needed to
maximize appropriate responses by its users to the commands
provided
Commercial Relationships: Aminat Adebiyi, None; James D.
Weiland, Second Sight Medical Products, Inc. (F); Carey Zhang,
None; Kaveri Thakoor, None
Support: Research to Prevent Blindness, W.M. Keck Foundation,
USAMRMC-W81XWH-10-2-0076
Program Number: 2765 Poster Board Number: B0019
Presentation Time: 8:30 AM - 10:15 AM
LOCOMOTION IN LOW LUMINANCE WITH NON
IMMERSIVE HEAD MOUNTED DEVICE FOR PATIENTS
WITH NIGHT BLINDNESS
Coen Cecilia1, Caroline Chauvire1, Guillaume Le Gall2, Arnaud
Koustanai1, Marion Swital2, Laurence Bernardini1, Philippe
Chaumet-Riffaud1, 3, Saddek Mohand-Said1, Jose A. Sahel1, Avinoam
B. Safran1. 1INSERM, U968; UPMC Univ Paris 06, UMR_S 968,
Institut de la Vision; CNRS, UMR_7210; CHNO des Quinze-Vingts,
INSERM-DHOS CIC 503, Paris, France; 2Essilor R&D
Internationnal, Paris, France; 3Univ Paris Sud, AP-HP, CHU Bicêtre,
EA 4046, Paris, France.
Purpose: Retinitis pigmentosa (RP) is characteristically associated
with reduced dark adaptation, which may lead to difficulties for
locomotion in dim light specially when lighting abruptly decreases.
We tested a non immersive Head Mounted Display (HMD) providing
a luminance-enhanced video image to determine its value for affected
individuals in dim light condition.
Methods: Nine RP patients were enrolled (age from 23 to 81 years,
mean 43). All patients complained of altered dark adaptation. We
evaluted visual acuity (VA), horizontal binocular visual field (VF)
and dark adaptometry (Goldmann-Weekers - GW). We tested a nonimmersive HMD (Essilor Int., Institut de la Vision, Paris, France;
Lumus, Rehovot, Israel), which provides a processed video image
displayed on transparent lenses. Image was a luminance-enhanced
view of the surrounding environment. Patients were asked to walk
along a straight corridor (white walls and floor, 30 meters long).
Five conditions were explored as follows: (1) in a clear corridor in
photopic condition (700 lux), and (2) in dim light (5 lux); (3) in a
corridor with 6 obstacles (white boxes 30x35x55cm) laid out on the
floor in photopic, (4) and dim light. The last condition (5) in a
corridor with 6 obstacles, in dim light, was tested using the HMD.
The walking speed was measured 3 times in each condition. Spatial
disposition of obstacles was modified between consecutive trials.
Patients were exposed to photopic lighting during 5 min before each
trial to prevent dark adaptation.
Results: Four of nine patients performed better using the HMD than
without: between-groups comparison showed that these four patients
increased their walking speed when obstacles were laid out in dim
light (mean walking speed without HMD = 0.35 m/s; SD = 0.07,
mean walking speed with HMD = 0.47 m/s; SD = 0.06) ;( F (4,152)
=12.1; p<.01). For these four subjects, alteration in dark adaptation
reduction in VA and VF were more pronounced than for the
remaining patients.
Conclusions: Significant HMD benefits were observed in patients
demonstrating severe handicap in dim light. However, in patients
suffering to a lesser degree from night-blindness, the device did not
prove to be invaluable.
Commercial Relationships: Coen Cecilia, None; Caroline
Chauvire, None; Guillaume Le Gall, Essilor International (E);
Arnaud Koustanai, None; Marion Swital, Essilor International (E);
Laurence Bernardini, None; Philippe Chaumet-Riffaud, None;
Saddek Mohand-Said, None; Jose A. Sahel, UPMC/Essilor (P),
Second Sight (F); Avinoam B. Safran, essilor (F)
Program Number: 2766 Poster Board Number: B0020
Presentation Time: 8:30 AM - 10:15 AM
Object identification by retinitis pigmentosa patients in dim light,
using a Head Mounted Display
Marion Swital2, Coen Cecilia1, Caroline Chauvire1, Arnaud
Koustanai1, Guillaume Le Gall2, Sihem Kime1, Philippe ChaumetRiffaud1, 3, Saddek Mohand-Said1, Jose A. Sahel1, Avinoam B.
Safran1. 1INSERM, U968; UPMC Univ Paris 06, UMR_S 968,
Institut de la Vision; CNRS, UMR_7210; CHNO des Quinze-Vingts,
INSERM-DHOS CIC 503, Paris, France; 2R&D, Essilor
International, Paris, France; 3Univ Paris Sud, AP-HP, CHU Bicêtre,
EA 4046, Paris, France.
Purpose: Retinitis pigmentosa (RP) results in peripheral vision loss
and reduced, delayed dark-adaptation. In this study we assessed with
affected individuals in dim light, the value of enhanced luminance
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
image processing using a Head Mounted Display (HMD), to locate
and identify objects.
Methods: We enrolled 12 patients with RP, complaining of night
blindness to various degrees, (23 to 81 years old, mean = 43; visual
acuity (VA) = -0.1 to +0.5 logMAR, mean = +0.15; horizontal visual
field = 20° to 180°, mean = 52°). Dark-adaptation threshold was
assessed with Goldmann-Weekers adaptometer.
We used a non-immersive HMD (Lumus, Israel; Essilor Int. and
Institut de la Vision, Paris) which provides a luminance-enhanced
video image, displayed through transparent lenses.
The experiment took place in a living room, including regular
furniture. Before starting the evaluation, the tested subject viewed the
furniture setting in photopic lighting condition (700 lux). Then, the
subject turned his back on the scene, and the experimenter placed
nine objects on various locations. Eventually lighting was abruptly
reduced to 3 lux, and the, subject was asked to identify all added
objects as quickly as possible. Trials were repeated three times, with
and without the HMD. Between two consecutive trials, object
locations were changed, and the subject was exposed to photopic
condition during 5 minutes to prevent dark adaptation. The number of
objects and the detection time were recorded.
Results: To identify the presented objects, four of 12 patients
performed better using the HMD than without it (F(1,54) = 8.05; p <
.01). In this group, three subjects had time-savings of mean 45.6 s
with the HMD and two subjects were able to recognize more objects
with the HMD (mean= 4.7). For these four subjects, alteration in dark
adaptation and reduction in VA were more pronounced than for the
remaining patients.
Conclusions: The luminance-enhanced image provided by the HMD
improved object identification, following sudden reduction in lighting
for patients with advanced RP. It may prove valuable in daily life, in
such lighting conditions. Less affected Individual might also benefit
from the HMD in dark environments if a more light-sensitive camera
is used.
Commercial Relationships: Marion Swital, Essilor International
(E); Coen Cecilia, None; Caroline Chauvire, None; Arnaud
Koustanai, None; Guillaume Le Gall, Essilor International (E);
Sihem Kime, ALTEN SA (E); Philippe Chaumet-Riffaud, None;
Saddek Mohand-Said, None; Jose A. Sahel, UPMC/Essilor (P),
Second Sight (F); Avinoam B. Safran, essilor (F)
Program Number: 2767 Poster Board Number: B0021
Presentation Time: 8:30 AM - 10:15 AM
Sensitivity recovery following a bleach; a dual “smiley” arc
stimulus technique for studying abnormal dark adaptation
Humza J. Tahir1, Ian J. Murray1, David Carden1, Neil R. Parry2.
1
Faculty of Life Sciences, University of Manchester, Manchester,
United Kingdom; 2University of Manchester Health Science
Research Centre and Vision Science Centre, Manchester Royal Eye
Hospital, Manchester, United Kingdom.
Purpose: There is much interest in sensitivity recovery under low
luminance conditions. The rate of recovery of rod-vision following a
bleach is important as it is slowed in the older eye and in many
clinical conditions, notably Age-Related Macular Degeneration. It is
not known for certain whether this is a pan-retinal effect or if there
are localised regions of impaired rod function. To address this a dual
arc stimulus was developed that simultaneously samples sensitivity
recovery in two retinal locations. Preliminary findings on normal
observers are presented.
Methods: Arc-shaped white “smiley” stimuli were presented on a
black CRT screen at two locations in the inferior visual field. They
were 75° segments of annuli with internal and external diameters 5°
and 7° (stim 1) or 10° and 12° deg (stim 2). The dynamic range of the
CRT was expanded by covering the left half of the screen with a 1.2
log unit neutral density (ND) filter, and the right half with 3.6 log
ND. The fixation/stimulus ensemble initially appeared in the left
window but shifted rightwards when screen stimulus intensity fell
below -1.5 log cd/m2, giving a total filtered luminance range of about
6.5 log units (0.8 to -5.7 log cd/m2). Recovery of sensitivity to the
two stimuli was measured simultaneously using method of
adjustment by alternately presenting them following a localised
bleach of at least 30% using a calibrated photographic flash.
Results: In normal observers the dark adaption process is composed
of a cone and a rod stage. When the stimuli are approximately
matched for photometric sensitivity their dark adaptation curves
coincide for the cone branch of the curve and remain separate for the
duration of the ‘S2’ stage which, due to the bleach intensity, can be
thought of as rate limited (Lamb and Pugh, IOVS, 2006;47;51385152). In some subjects the curves coalesce again for ‘S3’, the third
stage of the dark adaptation curve, but not in others indicating a
possible dissociation between S2 and S3.
Conclusions: This technique allows the measurement of dark
adaptation in multiple retinal locations simultaneously using a new
PC-based method. Preliminary results show differences in the tested
regions. As this new method places little additional demands on
subjects it allows for the easy investigation of potential regional
differences in impaired rod function in older and diseased eyes.
Commercial Relationships: Humza J. Tahir, None; Ian J.
Murray, None; David Carden, None; Neil R. Parry, None
Support: Nutricious R&D BV
Program Number: 2768 Poster Board Number: B0022
Presentation Time: 8:30 AM - 10:15 AM
Darks are detected faster and more accurately than lights in
normal subjects and patients with moderate glaucoma
Linxi Zhao, Mitchell W. Dul, Jose M. Alonso, Stanley J. Komban,
Qasim Zaidi. SUNY College of Optometry, New York, NY.
Purpose: Previous studies have shown that darks are detected faster
and more accurately than lights, when presented in noisy
backgrounds (Komban et al., 2011). We investigated how these
differences in detection time and accuracy are affected by age and
ganglion cell pathology caused by moderate glaucoma.
Methods: One eye of 8 glaucoma patients, 11 age-matched controls
(50-83 y/o) and 3 young control subjects (23-25 y/o) were tested.
Subjects were asked to count the number of light or dark targets
superimposed on a white noise background as fast as possible. Each
presentation contained 1-3 squared targets of 1° / side, located at
random positions within the central 30° of the visual field. A total of
600-800 measures were collected for per subject.
Results: We replicate previous findings (Komban et al., 2011) that
darks are detected more accurately and faster than lights. We extend
these findings by demonstrating that differences in detection time are
reliably found across different ages and are also present in subjects
with moderate glaucoma. In controls, we demonstrate that detection
times increase with age, both for lights (r=0.83, p<0.0001) and darks
(r=0.85, p<0.0001) but detection accuracy remains unchanged (lights:
r=0.37, p=0.18; darks: r=0.12, p=0.68). The difference in detection
time between lights and darks also increases with age (r=0.66,
p=0.99). When compared with controls, glaucoma patients showed a
significant reduction of 11-15% in detection accuracy
(normal/glaucoma, lights: 87.29% / 72.27%, p=0.008, darks: 94.42%
/ 83.02%, p=0.009, Wilcoxon tests) but not detection time
(normal/glaucoma, lights: 2.06 sec / 2.59 sec, p=0.13, darks: 1.47 sec
/ 1.87 sec, p=0.1, Wilcoxon tests). Differences in accuracy between
darks and lights were larger in glaucoma patients but the difference
was not large enough to reach significance (normal/glaucoma, 7.14%
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
/ 10.75%, p=0.06, Wilcoxon test).
Conclusions: Differences in the detection of darks and light are
robust, can be demonstrated over a wide range of ages and in patients
with retinal ganglion cell disease caused by glaucoma. The finding
that patients with glaucoma show a 15% reduction in detection
accuracy raises the question of whether a simple detection test could
be used to monitor disease progression.
Commercial Relationships: Linxi Zhao, None; Mitchell W. Dul,
None; Jose M. Alonso, None; Stanley J. Komban, None; Qasim
Zaidi, None
Support: EY007556, EY007716, EY013312, EY005253,
T35EY020481
Program Number: 2769 Poster Board Number: B0023
Presentation Time: 8:30 AM - 10:15 AM
Is visual exploration training beneficial in tunnel vision?
Iliya V. Ivanov, Annika F. Vollmer, Nhung Nguyen, Susanne
Trauzettel-Klosinski. University of Tuebingen, Tuebingen, Germany.
Purpose: Tunnel vision is a severe peripheral visual field loss
impairing mobility. It has been previously shown that normally
sighted subjects exhibit larger horizontal than vertical component of
eye position dispersions (standard deviations) while walking and
avoiding obstacles in daily life. However, for patients with tunnel
vision caused by retinitis pigmentosa (RP), horizontal and vertical
components were not found to be significantly different 1. In this
study we wanted to test whether visual exploration training is
beneficial for RP patients, as in patients with homonymous
hemianopia 2. Any efficient eye movement training in RP patients,
would result in change of eye-movement pattern- larger horizontal
than vertical dispersions.
Methods: Patients (n=33) were randomly assigned into three training
groups: saccadic (experimental), reading (placebo) or crossover
(placebo+experimental). In saccadic training condition, computerbased training extended eye-movement exploration outside of the
concentric constriction of the visual field (VF). In reading training
condition patients had to read a text that was presented at the center
of the screen, one word at time. To assess any effect of training,
mobile eye tracker was used to record eye positions while walking in
standardized environment (parkour), before and after training. We
compared horizontal and vertical eye dispersions of patients in the
different experimental groups with a control group of normals (n =
10).
Results: Comparable with previous findings, patients who had
residual VF < 15° (from fixation) showed equal horizontal and
vertical dispersions before training. After training however, patients
who received saccadic training showed significantly larger horizontal
dispersion (p<0.05). Patients with VF > 15° remained the same.
Regardless of their residual VF, patients in placebo group did not
show an effect of training: horizontal and vertical dispersions
remained unchanged after training.
Conclusions: These findings suggest that visual exploration training
is highly specific and resulted in significantly increased dynamic VF
for the RP patients with VF < 15°.
Commercial Relationships: Iliya V. Ivanov, None; Annika F.
Vollmer, None; Nhung Nguyen, None; Susanne TrauzettelKlosinski, None
Support: Kniese Foundation; Funke Foundation; Stiftung Auge
Program Number: 2770 Poster Board Number: B0024
Presentation Time: 8:30 AM - 10:15 AM
Is Vernier Acuity more Sensitive than Grating Acuity to Visual
Impairment in Adolescents?
Huizi Kelly Yin1, Barry S. Kran2, Darick Wright3, Donna D. Bent3, Li
Deng2, Dale L. Mayer2. 1Illinois College of Optometry, Chicago, IL;
2
New England College of Optometry, Boston, MA; 3Perkins School,
Watertown, MA.
Purpose: Vernier acuity, often referred to as a “hyperacuity”, may be
more sensitive than grating acuity in detecting visual deficits such as
amblyopia in young children. Thus, we compared vernier acuity
(VeA) and grating acuity (GA) tests to recognition acuity (RA) in
adolescents with visual impairment, hearing loss, and cognitive
disabilities.
Methods: 24 optometry students from the New England College of
Optometry and 10 adolescents (16 eyes) attending Perkins School for
the Blind were tested in each eye for RA (crowded letters), VeA
(Drover et al OVS 2010) and GA (Teller Acuity Cards) in 2 sessions.
Acuities were analyzed in logMAR. Test-retest reliabilities were
examined with Bland-Altman method (bias, 95% Limits of
agreement, LOA). To directly compare VeA and GA to RA in
adolescents, their raw data were normalized taking the difference
from the normal value for age (Delta-Normal, ΔN). ΔNs were
analyzed with correlations and means.
Results: Adult mean (SD) logMAR acuities (RE, session 1) were:
RA -0.11 (0.05) (20/16); VeA: -0.24 (0.15); GA: -0.09 (0.05). Testretest analyses of the adolescent data (in logMAR) showed minimal
bias and similar 95% LOA (0.66 for RA; 0.69 for VeA; 0.56 for GA).
For adults, test-retest 95% LOA for RA was 0.28 logMAR.
Correlations of adolescents’ ΔN for VeA and GA with RA (session1)
were significant and similar (VeA with RA, r=0.78; GA with RA,
r=0.83). Mean ΔNs were also similar and not significantly different
(RA: -0.79±0.34; VeA: -0.89 ± 0.44; GA: -0.76±0.31).
Conclusions: Test retest reliabilities are similar for RA, VeA and GA
tests in a small sample of adolescents with visual impairment and
other disabilities. Normalized VeA and GA acuities have a similar
relationship to normalized RA and are not significantly different on
average. Thus, vernier acuity may not have an advantage over grating
acuity in adolescents with visual impairments due to ocular and
neurological causes, who have other disabilities. However, for other
causes of visual deficits, for example, amblyopia, vernier acuity may
be more sensitive than grating acuity.
Vernier acuity cards with stimuli, forming a second-order shape of a
six-pointed star or a flower (Drover et al 2010). Acknowledgments:
Eileen E. Birch, PhD. and Yi-Zhong Wang, PhD. who provided the
stimuli.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
II is responsive to changes in VF resulting from LVR and has the
potential to be used as a measure of LVR outcomes in future studies.
Commercial Relationships: Vijaya K. Gothwal, None; Rebecca
Sumalini, None; Seelam Bharani, None
Photograph of examiner testing an adolescent participant with vernier
acuity cards.
Commercial Relationships: Huizi Kelly Yin, None; Barry S.
Kran, None; Darick Wright, None; Donna D. Bent, None; Li
Deng, None; Dale L. Mayer, None
Support: New England College of Optometry internal research grant
Program Number: 2771 Poster Board Number: B0025
Presentation Time: 8:30 AM - 10:15 AM
Evaluating the Effectiveness of Low Vision Rehabilitation in
Children
Vijaya K. Gothwal, Rebecca Sumalini, Seelam Bharani. Meera and L
B Deshpande Centre for Sight Enhancement, L V Prasad Eye
Institute, Hyderabad, India.
Purpose: Approximately 90% of patients with visual impairment
(VI) have adequate residual vision to benefit from low vision
rehabilitation (LVR). However, good evidence on LVR outcomes is
required to guide service development and improve the lives of
people with VI. Studies in adults with VI have demonstrated an
improvement in the overall visual functioning (VF) and quality of life
after LVR. Nonetheless, such effects are yet to be demonstrated in
children with VI. The aim of this study was to evaluate the
effectiveness of a multidisciplinary LVR program on VF using the
LV Prasad-Functional Vision Questionnaire II (LVP-FVQ II).
Methods: First-time referrals to the Centre for Sight Enhancement
were assessed before and after LVR (3-4 months). Children were
administered the LVP-FVQ II before low vision assessment and at 34 months follow-up to assess the outcomes of LVR. Recently, a
second version of the LVP-FVQ (LVP-FVQ II) was developed and
was demonstrated to be a reliable and valid measure of VF using
Rasch analysis. Rasch analysis was used to estimate the LVP-FVQ II
scores on an interval scale. Cohen d values were used to estimate the
magnitude of the change and the standardized response mean (SRM)
was selected to determine the clinical change of the LVR induced
changes.
Results: Sixty-three participants completed the rehabilitation (mean
age, 11.9 years; male, 62%). Approximately one-half had retinal
disorders (48%, 30) and most were moderately visually impaired
(<20/60-20/200, 74.6%, 47). Using the LVP-FVQ II, significant
improvement in VF was recorded (p<0.0001) after rehabilitation and
the increase in VF (SD) was 2.03 (1.68) logits (equivalent to an 8-line
improvement in visual acuity on an Early Treatment of Diabetic
Retinopathy Study chart). The magnitude of the improvement in LVR
intervention at follow-up was found to be relatively large (Cohen’s d
= 1.27, SRM = 1.21) indicating large treatment effects both
statistically and clinically. By comparison, there was no significant
change in VF for the control group (n=41).
Conclusions: This is the first study to provide strong evidence that
LVR services are effective in children with VI. Significant (both
statistically and clinically) improvements in the overall VF in
children with VI were found using the LVP-FVQ II. The LVP-FVQ
Program Number: 2772 Poster Board Number: B0026
Presentation Time: 8:30 AM - 10:15 AM
Quantification and evaluation of bivariate contour ellipse area
(BCEA) in different diseases after rehabilitation
Francesca Verboschi, Vittoria De Rosa, Chiara Di Crescenzo,
Gianmarco Rea, Marco Mafrici, Daniela Domanico, Enzo M.
Vingolo. University of Rome "La Sapienza", Latina (LT), Italy.
Purpose: To quantify BCEA in different diseases and to evaluate its
change after rehabilitation with microperimetric biofeedback.
Methods: 64 patients (38 female and 26 male, mean age 75.87 years)
were enrolled and 96 eyes were divided into different groups: 16 eyes
with dry age-related macular degeneration (group 1), 12 eyes with
advanced glaucoma (group 2), 11 eyes with central retinal vein
occlusion (group 3), 11 eyes after surgery for macula-off retinal
detachment (group 4), 11 eyes with amblyopia (group 5), 13 eyes
with myopic maculopathy (group 6), 12 eyes with diabetic
maculopathy (group 7), 10 eyes with retinitis pigmentosa (group 8).
All the patients underwent the same rehabilitative protocol:
microperimetry MP-1 (Nidek technologies, Padova, Italia), threshold
strategy 4-2, Goldmann III stimolus, with fixation study that was
quantified by calculating the BCEA; 10 training sessions, once a
week, 10 minutes for each eye, with microperimetric biofeedback,
repeated after 3 months. Statistical analysis was performed using ttest paired, p values less than 0.05 were considered statistically
significant. For statistical analysis, BCEA values (deg ) were
converted into their logarithms.
Results: After the training mean BCEA became from 7.51±2.48 deg
to 3.85±2.93 deg in group 1 (p=0.02); mean BCEA became from
4.02±2.83 deg to 0.84±0.48 deg in group 2 (p=0.14); mean BCEA
became from 3.72±4.85 deg to 2.18±2.22 deg in group 3 (p=0.42);
mean BCEA became from 3.31±2.53 deg to 2.15±1.59 deg in group 4
(p=0.03); mean BCEA became from 3.18±2.55 deg to 2.15±1.32 deg
in group 5 (p=0.06); mean BCEA became from 2.22±2.65 deg to
0.45±0.13 deg in group 6 (p=0.05); mean BCEA became from
3.38±3.42 deg to 1.72±1.72 deg in group 7 (p=0.02); mean BCEA
became from 1.89±1.40 deg to 0.77±0.26 deg in group 8 (p=0.14).
Conclusions: The largest BCEA reduction after the training indicates
a greater efficacy of microperimetric biofeedback especially in dry
age-related macular degeneration, after surgery for macula-off retinal
detachment, myopic maculopathy and diabetic maculopathy
compared to glaucoma, central retinal vein occlusion, amblyopia and
retinitis pigmentosa. The study of BCEA is useful and more sensitive
instrument than Fujii classification to evaluate the stability of fixation
especially in diseases with macular involvement.
Commercial Relationships: Francesca Verboschi, None; Vittoria
De Rosa, None; Chiara Di Crescenzo, None; Gianmarco Rea,
None; Marco Mafrici, None; Daniela Domanico, None; Enzo M.
Vingolo, None
Program Number: 2773 Poster Board Number: B0027
Presentation Time: 8:30 AM - 10:15 AM
Comparison of Fixation Stability Measured by Laser Scanning
Digital Camera and DLP-Cam
Benno L. Petrig1, 2, Jeff Clendenon2, Lisa Ensman1, Matthew S.
Muller2, Ann E. Elsner1, Glen Y. Ozawa3, Taras V. Litvin3, Jorge A.
Cuadros3, Tuhin Roy3, Danny Li3. 1School of Optometry, Indiana
University, Bloomington, IN; 2Aeon Imaging LLC, Bloomington, IN;
3
School of Optometry, UC Berkeley, Berkeley, CA.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Purpose: To compare fixation stability in diabetic patients measured
by the laser scanning digital camera (LSDC) and the digital light
projector camera (DLP-Cam), using standard deviation of Euclidean
distance (ED) and bivariate contour ellipse area (BCEA) as metrics.
Methods: Eight diabetic patients (5 male, 3 females, age 48±12 yr)
were imaged at the Eastmont Wellness Center, a diabetic retinopathy
screening site within the EyePACS telemedicine network, with both
the LSDC and the DLP-Cam. LSDC and DLP-Cam have 36 and 33
deg fields, respectively. Light levels at the cornea were 2 mW @ 850
nm, which appeared quite dim, for the LSDC and 42 uW from the
green LED, which was bright, for the DLP-Cam. Image buffers of 20
@ 11 fps (LSDC) and 16 @ 17 fps (DLPC) frames were acquired on
the same day by the same camera operator. One eye was chosen at
random for this analysis. Fixation stability was assessed using the
coordinates determined for image registration by the same alignment
algorithm. The measurements in pixels were converted to minArc
before comparing the LSDC and DLPC results by paired t-tests.
Results: The standard deviation of ED for this group of patients was
5.09±3.42 and 5.69±3.25 minArc for LSDC and DLP-Cam,
respectively. The BCEA, which typically decreases the effect of
outliers, was 2.43±0.41 and 2.43±0.44 log(minArc^2), for LSDC and
DLP-Cam, respectively. The differences in fixation stability were not
statistically significant by either metric.
Conclusions: Both imaging systems provide comparable fixation
stability measures, suggesting that the brighter fundus illumination of
the DLP-Cam compared to the LSDC does not affect fixation ability.
Our alignment algorithms are able to process images taken with
either visible or near infrared fundus illumination which are known to
emphasize different retinal structures.
Commercial Relationships: Benno L. Petrig, Aeon Imaging LLC
(E), Aeon Imaging LLC (P); Jeff Clendenon, Aeon Imaging, LLC
(E); Lisa Ensman, None; Matthew S. Muller, Aeon Imaging, LLC
(I), Aeon Imaging, LLC (P), Aeon Imaging, LLC (R), Aeon Imaging,
LLC (S), Indiana University Research and Technology Corporation
(P); Ann E. Elsner, Aeon Imaging, LLC (I), Aeon Imaging, LLC
(F), Aeon Imaging, LLC (P); Glen Y. Ozawa, None; Taras V.
Litvin, None; Jorge A. Cuadros, EyePACS LLC (I); Tuhin Roy,
None; Danny Li, None
Support: R44EY018772(BLP), R44EY020017(MSM)
Program Number: 2774 Poster Board Number: B0028
Presentation Time: 8:30 AM - 10:15 AM
Do visually impaired participants hear better? An evaluation of
self report using a modified version of Speech, Spatial and
Qualities of Hearing Scale
Shahina Pardhan1, Silvia Cirstea1, Andrew Kolarik2, 1, Brian Moore2.
1
Vision and Eye Research Unit (VERU), Anglia Ruskin University,
Cambridge, United Kingdom; 2Department of Psychology, University
of Cambridge, Cambridge, United Kingdom.
Purpose: Literature suggests that visually impaired participants may
perform better than sighted participants on auditory tasks. This is
more apparent in participants with severe visual impairment.
However, it is not known whether these participants perceive their
hearing to be better than normally sighted participants. We modified
the Speech, Spatial and Qualities of Hearing questionnaire for use by
visually impaired participants. Visual aspects were removed from ten
items, but modifications were kept minimal, so as to maintain the
meaning of the original items. The modified questionnaire addresses
a large variety of auditory scenarios and assesses situations which
visually-impaired participants find most demanding, and those which
present little difficulty.
Methods: The modified SSQ was administered to 8 participants with
severe visual impairment but who had normal hearing. Age-matched
sighted participants with normal hearing acted as controls. Items
assessed self report for speech comprehension in the presence or
absence of competing speech or noise, and spatial aspects of hearing
including judgements of direction and distance. Qualities of the
listening experience such as perceived effort and sound identification
were also assessed.
Results: In the speech domain, Mann-Whitney U tests showed that
participants with severe visual impairment reported significantly
more difficulties (p<0.05) than sighted participants in scenarios
where multiple sound sources were present, and the scenario required
noise or competing sound sources to be ignored. Significant
differences were not observed in the spatial or qualities domains.
Conclusions: Although there have been many reports of enhanced
auditory abilities of participants with severe visual impairment,
especially within the spatial domain, the present findings suggest that
sensory compensation is not perceived to confer benefit in their daily
lives. The self-reported increased difficulty for a subset of the speech
items is a consequence of the lack of visual cues, which, apart from
precluding lip-reading, may lead to increased difficulties in
separating objects in complex auditory scenes and to higher
susceptibility to informational masking.
Commercial Relationships: Shahina Pardhan, None; Silvia
Cirstea, None; Andrew Kolarik, None; Brian Moore, None
Support: Postdoctoral Fellowship, Postgraduate Medical Institute,
Anglia Ruskin University. MRC grant G0701870 to BCJM
Program Number: 2775 Poster Board Number: B0029
Presentation Time: 8:30 AM - 10:15 AM
An Object Localization and Feedback System
Nii Tete Mante1, 2, Gerard Medioni2, Armand R. Tanguay1, 4, Thang
Dinh2, Furkan E. Sahin4, Patrick J. Nasiatka4, James D. Weiland1, 3.
1
Department of Biomedical Engineering, University of Southern
California, Los Angeles, CA; 2Department of Computer Science,
University of Southern California, Los Angeles, CA; 3Department of
Opthamology, University of Southern California, Los Angeles, CA;
4
Department of Electrical Engineering, University of Southern
California, Los Angeles, CA.
Purpose: The goal of the project was to create a system which assists
blind/low vision subjects with reaching and grasping for objects. This
system is referred to as the 'Object Localization and Feedback
System' (OLFS). The OLFS aims to enhance the autonomy of blind
patients, by utilizing advanced algorithms and feedback mechanisms
for daily tasks.
Methods: The OLFS utilized a 100° wide-angle camera (Tanguay,
Sahin, Nasiatka), central processing unit (CPU) and bone conduction
headphones. Computer Vision algorithms (Context Tracker, Medioni
and Dinh) on the CPU parsed, and processed the camera input to
determine object(s) position. Bone conduction headphones produced
auditory feedback for the blind user based on object position. For
example, if the object is positioned left to the camera's center of
vision (COV), the computer would say “Left” to the test subject.
Once the object was centralized within the users/cameras center of
vision, test subjects were asked to reach out and touch the object.
Two blind test subjects evaluated the device. Subjects were trained to
use the system initially. Afterwards, autonomous testing was carried
out. In both stages, subjects were asked to reach and grasp for an
object with the aid of the OLF system. If test subjects were not able
to grasp the object within 45 seconds, the trial was stopped and
considered unsuccessful.
Results: In ten object localization trials, patient RS-2 was able to
grasp the desired object 6/10 times. The average time to grasp the
object for the 6 successful trials was 15.43 seconds. Patient NM was
able to grasp the object 10/10 times, and average the time to grasp the
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
object was 13.95 seconds. Both patients were given a System
Usability Scale (SUS) test. Patients RS-2 and NM gave the OLFS
system a score of 87.5% and 67.5%, respectively. A 100% score
symbolizes a perfectly usable system (as judged by the subject).
Object tracking path data within the FOV was also recorded for each
test and each test subject.
Conclusions: An initial system for assisting the blind in reaching and
grasping for objects was successfully designed, implemented and
tested. Test subjects were able to successfully grasp the object. Future
improvements to the system will include enhanced robustness of
vision algorithms, and new implementations of physical feedback.
These two improvements will act to make the use of the system more
intuitive for the patient.
Commercial Relationships: Nii Tete Mante, None; Gerard
Medioni, None; Armand R. Tanguay, University of Southern
California (P); Thang Dinh, None; Furkan E. Sahin, None; Patrick
J. Nasiatka, None; James D. Weiland, Second Sight Medical
Products, Inc. (F)
Support: Research to Prevent Blindness, W.M. Keck Foundation;
USAMRMC-W81XWH-10-2-0076
Program Number: 2776 Poster Board Number: B0030
Presentation Time: 8:30 AM - 10:15 AM
Magnification, Field of View and Depth of Field in Low Vision
Aids and Optical Instruments
Ian L. Bailey. School of Optometry, University of California,
Berkeley, Berkeley, CA.
Purpose: Clinicians prescribing low vision aids or using visual
instruments to examine eyes often need to understand what fine
details can be seen, how much of the object can be seen, and how
visual access depends of the viewing system. Some new simple
concepts can allow clinicians to estimate the magnitude of
magnification effects, fields of view and depths of field.
Methods: There are several different methods used to quantify
magnification effects at near and this often leads to erroneous
predictions of optical performance. As an alternative, we use
Equivalent Viewing Distance (EVD) which is the distance at which
the object would subtend the same angle that is being subtended by
the image. The size of just-resolvable detail is simply proportional to
the EVD. For collimating systems, the EVD is equal to the equivalent
focal length. For images at finite distances, the EVD is calculated by
dividing the eye-to-image distance by the enlargement ratio (ER) . To
understand such systems, the clinician needs to know the image
location and ER.
The Field of View (FoV) is determined by a “field cone’ whose angle
is determined by the field limiting aperture and its distance from the
eye. The Image Field Aspect Ratio (IFAR) is a diameter-to-distance
ratio defining this angle. The width of the FoV is equal to the product
of EVD and IFAR. Slit lamps, and most other microscope systems
are analogous to Kelperian telescopes and then, IFAR = approx. 1.0,
and the EVD and the FoV will be about equal.
A practical estimate of the Depth of Field is given by the square of
the EVD.
Results: These methods can provide an immediate and accurate
estimate of EVD, FoV and DoF in hand held magnifiers, stand
magnifiers, telescopes for distance or near. It is easy for clinician
observing a patient to mentally visualize the field cone and EVD
plane, and immediately estimate the FoV. The same approach can
easily be applied to the slit lamp and most other visual inspection
instruments. Once the geometric concepts are grasped, only minimal
calculation skills are required.
Conclusions: The concept of Equivalent Viewing Distance simplifies
the quantification of magnification effects and prediction of
resolvable detail. The image field cone concept when combined with
the EVD, directly and intuitively predicts the width of the FoV. Once
the EVD is known, the depth of field can be estimated by squaring
the EVD.
Commercial Relationships: Ian L. Bailey, None
Program Number: 2777 Poster Board Number: B0031
Presentation Time: 8:30 AM - 10:15 AM
Preference pattern of low vision aids in glaucoma-redefining
guidelines
Aparna Rao, Sirajum Monira, Mahasweta Chowdhury. Glaucoma
Services, LV Prasad Eye Institute, Patia, India, Bhubaneswar, India.
Purpose: To evaluate preference pattern of low vision devices
(LVD) in patients with glaucoma to arrive at specific guidelines for
prescribing these devices with regards to specific visual disabilities.
Methods: Retrospective review of records of glaucoma patients
attending low vision services. Criteria for low vision was defined as
best corrected distance visual acuity <20/80 in the better eye with
Log mar chart and/or near visual acuity <N10 binocularly with Bailey
Lovie word reading chart and/or visual field 20degrees or <20
degrees from the point of fixation. The data collected for each patient
included the age, gender, diagnosis, extent of visual field loss (mean
deviation and central residual field of vision), type of visual disability
and the type of low vision aid (optical vs electronic) preferred by the
patients for daily routine use.
Results: The mean age of the 51 patients was 51±23.4 (9-83 years)
which included 14 females (27.5%) and 37(72.5%) males, 14
developmental (27.5%), 8 PACG (15.7%) and 29 POAG (56.8%).
While 34 (77%) opted for optical devices, 17 opted for electronic
devices. There was no statistical difference in preference of LVD
among the two sexes or between patients with different level of
education (undergraduate or postgraduate or different distance or low
contrast visual acuity. On univariate analysis, younger age,
magnification>5x, color matching disabilities and glare were found to
significantly influence preference for electronic devices while on
multivariate regression, age <30 years (β=-0.04, p=0.005), color
matching disability (β=3.08, p=0.002), glare (β=2.04, p<0.001) were
significant influences for preference for electronic LVD. There was
no specific preference pattern for preference of optical magnifiers in
this study.
Conclusions: Younger patients <30 years with glare and color
contrast impairment may be prescribed electronic low vision devices
for optimal visual function as compared to optical devices. Glare
measurement and color matching disability may be added as
parameters for assessing visual functions routinely in patients with
advanced glaucoma.
Commercial Relationships: Aparna Rao, None; Sirajum Monira,
None; Mahasweta Chowdhury, None
Program Number: 2778 Poster Board Number: B0032
Presentation Time: 8:30 AM - 10:15 AM
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Sustained benefits of Therapeutic Tinted Contact Lenses (CL) in
patients with Albinism
Faheemah Saeed1, Darrell G. Schlange2, Tina Najafi3. 1Illinois
College of Optometry, Chicago, IL; 2Illinois College of Optometry,
Chicago, IL; 3Illinois College of Optometry, Chicago, IL.
Purpose: To determine whether the improvement in visual function
and nystagmus eye movements observed in patients with Albinism
using tinted CL correction is sustained after 6 months following the
initial dispense. Improved visual function and nystagmus eye
movements in 20 patients with Albinism resulting from tinted CL use
were reported last year. Results collected 6 months after the initial
CL dispense are now being reported on 13 returning patients.
Methods: 20 subjects were fitted with soft toric CL’s that were then
custom tinted to create an artificial iris. Dependent variables
including visual acuity (VA), contrast sensitivity (CS) with and
without glare, and nystagmus eye movement recordings were tested
again while wearing tinted CLs, 6 months following the initial
dispense of tinted CL. The EDTRS chart was used to measure visual
acuity. The CSV-1000HGT (halogen glare test) and 1000E (Contrast
Sensitivity chart) were used to measure the contrast sensitivity
function and effect of glare. Nystagmus eye movement characteristics
of intensity and foveation were recorded and analyzed with an
ISCAN system (RK 826PCI) that uses a video based dark pupil-tocornea reflection method.
Results: The improved logMar VA observed with tinted CLs was
still present at the 6 month follow up visit, as the difference obtained
at the two visits did not differ significantly (t= 1.72, p=0.11). Mean
CS under normal testing conditions was further improved at the 6
month follow up visit (t= 2.49, p=0.028) while the mean CS with
glare did not differ between the two visits (t= 1.17, P=0.266). ISCAN
recordings with 3 runs in each of 5 gaze positions showed that the
reduced intensity of nystagmus was also maintained with tinted CL
wear after 6 months (t= 0.61, p=0.557).
Conclusions: We previously reported that VA, Nystagmus intensity
and CS with and without glare were significantly improved with
tinted CL wear in patients with albinism. The current study indicates
that these significant improvements are maintained or even increased
for at least six months following initial dispensing of tinted CL’s.
Commercial Relationships: Faheemah Saeed, None; Darrell G.
Schlange, None; Tina Najafi, None
Program Number: 2779 Poster Board Number: B0033
Presentation Time: 8:30 AM - 10:15 AM
Evaluating center of pressure (CoP) measures of postural
stability in low and normal vision using the Nintendo Wii
Balance BoardTM (WBB)
Pamela E. Jeter1, Jialiang Gu2, Judith E. Goldstein1, Ava K. Bittner1,
Gislin Dagnelie1. 1Ophthalmology, Johns Hopkins University,
Baltimore, MD; 2Electrical & Computer Engineering, Carnegie
Mellon University, Pittsburgh, PA.
Purpose: To evaluate Center of Pressure measures obtained on a
commercially available Nintendo Wii Balance BoardTM (WBB) in a
group of low vision (LV) and normal participants.
Methods: Subjects with low vision (visual acuity worse than 20/70
and/or visual field less than 40°, in the better eye, N=7) and subjects
with corrected-to-normal vision (N=5), completed the modified
Clinical Test of Sensory Interaction on Balance (mCTSIB) which
includes four sensory conditions: double-leg standing on a firm
surface with eyes open (EO-firm); standing on a firm surface with
eyes closed (EC-firm); standing on an unstable (3” thick) surface
with EO (EO-foam); and standing on an unstable surface with EC
(EC-foam). Subjects performed each condition for 4 successive trials
for up to 30 seconds with a one-minute rest period in between. The
conditions were randomly ordered. Center of Pressure (COP)
outcomes were derived from data sent by the 4 force plate sensors in
the WBB to a laptop via Bluetooth. The COP measures include root
mean square (RMS) of the COP excursion (mm), RMS of velocity
(mm/s), mean total velocity (MTV, mm/s), and area (mm2).
Results: In the LV group, all COP measures differed significantly
between firm and foam conditions with EC and EO (all p<0.05) with
the exception of SD of velocity in the M-L direction. In both groups,
no significant differences across COP measures were found in an
independent samples t-test between the EO-firm and EC-firm
conditions (all p>0.05) and between the EO-foam and EC-foam
condition. No significant differences were found across all variables
when comparing LV participant COP measures to normal participants
with the exception of MTV and area in the EO-firm condition
(p=0.01 and p = 0.03, respectively).
Conclusions: This pilot study uses the WBB for determining postural
stability in a LV and normal group. As expected, differences were
found between the firm and foam conditions both with EO and EC in
the LV group suggesting that visual and sensorimotor challenges
exist. In comparison, the normal group performed well across all
conditions suggesting more stability. MTV and area measures
differed between the LV and normal group in the EO-firm condition
suggesting that these variables might by predictors of balance
impairment. A larger sample size is needed to determine test-retest
reliability of each COP measure.
Commercial Relationships: Pamela E. Jeter, None; Jialiang Gu,
None; Judith E. Goldstein, None; Ava K. Bittner, None; Gislin
Dagnelie, None
Support: Louise L. Sloan Research Grant Award, Lions Vision
Research Foundation, Wilmer Eye Institute
Program Number: 2780 Poster Board Number: B0034
Presentation Time: 8:30 AM - 10:15 AM
Low vision and work opportunities
Jørn Kalleberg1, Irene Langeggen2. 1NAV Buskerud, Drammen,
Norway; 2Buskerud University College, Kongsberg, Norway.
Purpose: The aim is to enhance routines around any working low
vision patients enrolled at The Norwegian Labour and Welfare
Association, Low vision clinic (NLW-LWC) and Kongberg
community, Buskerud, Norway. Data published by the Norwegian
Blind Association reports 25-40 % of visual impaired are working.
There is no literature referring to the role of NLW-LWC and
community cooperation to enhance low vision rehabilitation for these
patients.
Methods: Patients were recruited from a list of candidates given by
either the Kongsberg Community optometrist or the NLW-LWC
optometrist. The patients included were all eligible to low vision aids
according to Norwegian guidelines. All participants were asked and
signed the consent form.The interview of the subjects was based on a
questionnaire concerning general health, mobility, work situation, use
of visual aids and their experience with visual rehabilitation.
Results: Age ranged from 32 - 59 years. Of 13 participants, six males
and four females were interviewed. One of the subjects had a
congenital low vision condition. All subjects have completed
education at a high school level. One has a master degree. There is no
one working in health care profession. Eight of ten works daily on a
computer, but only one uses Zoomtext.
Visual acuity ranged from 0,15 - 1,2 (Snellen). Visual field was
reduced in nine of ten subjects. Six of ten used filter spectacles.
Magnifier (4), near and reading magnifying spectacles (7) and the
computer (7) were the prefered low vision aids. Seven subjects have a
full time position.
Neither had experienced a systematic approach to their low vision
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
situation. Follow ups where through the local optometrist (7/10).
They thought highly of the questionnaire and emphasized the need
for regular follow up of optometrists with low vision advices as a
health speciality.
Conclusions: To enhance better low vison rehabilitation and to
provide better work situationsis it necessary to look at the work and
the home situation together. There is a need for a systematic approach
towards this patient group. The optometrist is essential in optical low
vision follow up, the NLW-LWC needs to focus on technical support,
illumination, legal rights and the dialog with the work place. Our
questionnaire can be a tool of care. To improve the rehabilitation at
work you improve selfesteem and paricipation in the society.
Commercial Relationships: Jørn Kalleberg, None; Irene
Langeggen, None
Program Number: 2781 Poster Board Number: B0035
Presentation Time: 8:30 AM - 10:15 AM
The effect of an Adapted Day Centre on Physical and
Psychological Well-Being in Older Adults with Low Vision
Walter Wittich1, 2, Caitlin Murphy3, 2, Daphne Mulrooney1, 2.
1
Research, MAB-Mackay Rehabilitation Centre, Montreal, QC,
Canada; 2CRIR, Montreal, QC, Canada; 3School of Optometry,
University of Montreal, Montreal, QC, Canada.
Purpose: Older adults with visual impairment are vulnerable to
social isolation and associated health risks. The MAB-Mackay
Rehabilitation Centre runs a Day Centre program whose objectives
are to maintain or improve the seniors’ biological, psychological, and
social health, and foster a better quality of life, while delaying or
avoiding institutionalization. Activities include walking groups,
language courses, memory games, crafts and theme parties,
supervised by an interdisciplinary team, including a nurse, social
worker and occupational therapist. Services include medical and
rehabilitation follow-up and referrals to additional community
resources. The present study evaluates the impact the Day Centre has
on the holistic health of older adults with visual impairment.
Methods: Between September 2011 and October 2012, 16 newly
referred clients in the Day Centre (age 71 to 98, M = 85, VA 20/50 to
NLP, M = 20/126) were evaluated at intake, and after 6 months,
using the Visual Function Questionnaire-14, Hearing Handicap
Inventory for the Elderly, Geriatric Depression Scale (GDS),
Friendship Scale, Life-Space Questionnaire, Activity-specific
Balance Confidence scale, Timed-Up-and- Go Test, and the adapted
Montreal Cognitive Assessment (MoCA). Acuity, visual field, and
average decibel hearing loss were recorded.
Results: All participants continued to live independently in the
community 6 months after entering the Day Centre. Comorbid
conditions included high blood pressure, asthma, cardiac problems,
diabetes, stroke, arthritis, osteoporosis, and anxiety. Participants
reported statistically unchanged scores on all the measures, except for
increased GDS scores (p < .05) and a trend towards improvement on
the MoCA (p = .06).
Conclusions: Considering the fragility, vulnerability and age of this
population, the data indicate that the Day Centre fulfills its mandate
to prevent decline in its clients’ biological, psychological, and social
health. We speculate that the increase in depression scores is linked
to serious life events during the follow-up period for some of the
participants, such as loss of a spouse. Participation in adapted Day
Centre activities, as an integrated part of rehabilitation services,
seems to support independent living in older adults with vision loss.
Commercial Relationships: Walter Wittich, None; Caitlin
Murphy, None; Daphne Mulrooney, None
Program Number: 2782 Poster Board Number: B0036
Presentation Time: 8:30 AM - 10:15 AM
Vision, Demographic Factors, and Motor Vehicle Collisions in
Bioptic Drivers
Bradley E. Dougherty1, Roanne E. Flom1, Mark A. Bullimore2,
Thomas W. Raasch1. 1Optometry, Ohio State University, Columbus,
OH; 2Optometry, The University of Houston, Houston, TX.
Purpose: In approximately 40 US states, drivers who cannot meet
vision standards with conventional optical correction are permitted to
use bioptic telescopic spectacles to obtain licensure. Very few studies
of safety of bioptic driving have been conducted. This study
examined the relationships among visual and demographic factors
and motor vehicle collisions (MVC) in bioptic drivers in Ohio.
Methods: A retrospective study of patients identified as having
received an initial daylight bioptic examination at the College of
Optometry at the Ohio State University was conducted. Data were
collected on vision, including visual acuity (logMAR charts), contrast
sensitivity (Pelli Robson or Mars charts) and visual field (arc or
Goldmann perimeter). Driving records from the Ohio BMV were
obtained and demographics, ocular diagnoses, and licensure history
were also recorded. Relationships among vision, demography, and
BMV data including MVC were investigated using survival analysis
and the Cox proportional hazards regression model.
Results: 238 drivers (65% male) were identified. Age at initial exam
ranged from 16 to 81 years (mean = 39±15 years). Time since bioptic
licensure ranged from 1 to 22 years (mean = 10±5 years). Mean
logMAR visual acuity OU was 0.76±0.12 (approximately 20/115)
and mean log contrast sensitivity was 1.53±0.23. A total of 292 MVC
were documented in the BMV records for these drivers. The number
of MVC per driver ranged from 0 to 11, with 124 (52%) drivers
having had at least one MVC and 72 (30%) having had two or more.
Visual acuity, contrast sensitivity, and horizontal visual field were
not significant predictors of MVC (p = 0.81, 0.18, and 0.76,
respectively). Gender was not associated with MVC (p=0.28), but
age was associated with fewer MVC (p < 0.001). Previous (withoutbioptic) licensure status was associated with fewer MVC (p < 0.001),
with 41% of drivers with previous licensure involved in an MVC
versus 67% of drivers without previous licensure.
Conclusions: Age and previous non-bioptic licensure were inversely
associated with fewer MVC in this group of bioptic drivers. VA, CS,
horizontal VF, and gender did not predict MVC involvement.
Commercial Relationships: Bradley E. Dougherty, None; Roanne
E. Flom, None; Mark A. Bullimore, Alcon (C), Carl Zeiss Meditec
(C), DigitalVision Systems (C), Ridgevue (I); Thomas W. Raasch,
None
Support: NIH Grant 8TL1TR000091-05, Ohio Lions Eye Research
Foundation Grant
Program Number: 2783 Poster Board Number: B0037
Presentation Time: 8:30 AM - 10:15 AM
Effects of patient traits on physician-predicted low vision
outcomes
Tiffany L. Chan, Robert W. Massof, Judith E. Goldstein.
Ophthalmology, Johns Hopkins University School of Medicine,
Baltimore, MD.
Purpose: We reported that physicians’ ability to predict the success
of low vision rehabilitation (LVR), relative to patient-reported
outcomes, is no better than chance. This study determines if patients’
traits influence ratings physicians provide and if those traits affect
patient-reported outcomes.
Methods: The Activity Inventory (AI), a self-report visual function
questionnaire, was administered pre and post-LVR to 270 low vision
patients served by 28 LVR centers that participated in a collaborative
study. The physical component of the SF-36, GDS, and TICS also
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
were administered pre-LVR to measure physical capability,
depression and cognitive status. Following patient evaluation, 38
LVR physicians estimated the probability of outcome success (POS)
on a scale of 0 to 100% for each of their patients, using their own
criteria for success.The POS ratings and change in functional ability,
based on Rasch analysis of AI responses, were used to assess the
effects of patients’ baseline traits on predicted and patient-reported
outcomes. The distributions of SF-36 physical functioning, GDS, and
TICS measures were divided into quartiles and visual acuity (VA)
was categorized by severity. Analysis of variance was performed
with POS and change in functional ability as the dependent variables
and the quartiles for each trait serving as factors.
Results: Baseline traits with significant effects on POS are: physical
functioning (p=0.003), cognitive state (p=0.001), visual acuity
(p<0.001), and baseline functional ability (p= 0.005). Depressed
mood, age, gender, and number of symptomatic co-morbidities have
no significant effect on the POS. Only pre-LVR functional ability
(p=0.001) has a significant effect on changes in functional ability,
none of the other traits has a significant effect.
Conclusions: Physicians’ predictions of LVR outcomes appear to be
driven by patient’s physical ability, cognitive functioning, VA, and
baseline visual function - information physicians acquire from the
patient’s history and examination. However, none of these traits,
except baseline functional ability, is predictive of changes in
functional ability. Although physicians appear to be using reasonable
information about the patient’s state to estimate rehabilitation
potential, the baseline traits selected are not reliable predictors of
patient outcomes, therefore LVR physician predictions of successful
outcomes are no better than chance.
Commercial Relationships: Tiffany L. Chan, None; Robert W.
Massof, None; Judith E. Goldstein, None
Support: NIH Grant EY018696
Program Number: 2784 Poster Board Number: B0038
Presentation Time: 8:30 AM - 10:15 AM
An Inventory of Visually Guided Activities Self-reported by
Individuals with Profound Visual Impairment
Gislin Dagnelie1, Pamela E. Jeter1, Lauren Dalvin2, Ellen R. Arnold1.
1
Ophthal-Lions Vision Cntr, Johns Hopkins Univ, Baltimore, MD;
2
NE Ohio Medical Univ, Rootstown, OH.
Purpose: Visual functioning questionnaires (VFQs) can assess
functional vision in individuals with mild to severe impairment, but
are uninformative if remaining vision is minimal. We performed a
systematic inventory of daily activities that require some, albeit
minimal, visual guidance or support. These activities can then be
assigned item difficulty scores through rating by profoundly impaired
individuals, with the eventual purpose of extending the range of
currently used VFQs.
Methods: Nine focus groups of 4-6 members with profound vision
loss met in person or conference call to discuss the role of vision in
their daily activities. The Massof Activity Inventory (Optom vis Sci
84:763-74;2007) was used as a template. Each group held 4-7
sessions of 60-90 min; audio recordings of the sessions were
abstracted and analyzed for content. Reported activities were
categorized into 4 domains - reading (R), mobility (M), visual motor
(V), and visual information (I) -- and into 10 aspects -- brightness,
contrast, lighting, movement, size, distance, depth, eccentricity,
familiarity, and other.
Results: Focus groups reported 760 activities, with 10%, 17%, 24%,
and 49% categorized in the R, M, V, and I domains, respectively. On
average, 1.58 aspects of visual function were involved in each
activity. Contrast (68%), brightness (27%), lighting (14%), size
(14%), and distance (12%) were the most prevalent aspects that were
critical in performing these activities, with eccentricity (8%),
movement (7%), familiarity (5%), depth (1%), and other (2%) critical
in smaller subsets of activities. A representative subset of these
activities spanning all domains and visual aspects was used to create
a set of 144 survey questions for a draft VFQ for ultra-low vision.
Conclusions: Even at these ultra-low vision levels visual activities in
all 4 domains, and spanning all 10 aspects, of vision continue to be of
critical importance. Following administration to a population of 100
profoundly impaired individuals and Rasch analysis, the resulting
survey questions will be reduced to a set of ~50 questions spanning
the lower end of the item difficulty scale largely untested by current
VFQs. The selected activities also form the basis for training and
assessment test in controlled environments, now being developed as
part of the prosthetic low vision rehabilitation (PLoVR) curriculum.
PLoVR: Prosthetic Low Vision Rehabilitation
Commercial Relationships: Gislin Dagnelie, None; Pamela E.
Jeter, None; Lauren Dalvin, None; Ellen R. Arnold, None
Support: R01EY021220(+-S1)
320 Color Vision, Photoreceptor Function, Adaptation
Tuesday, May 07, 2013 8:30 AM-10:15 AM
Exhibit Hall Poster Session
Program #/Board # Range: 3014-3030/C0177-C0193
Organizing Section: Visual Psychophysics / Physiological Optics
Contributing Section(s): Visual Neuroscience
Program Number: 3014 Poster Board Number: C0177
Presentation Time: 8:30 AM - 10:15 AM
Is dark-adapted cone detection optimized given noise and
uncertainty?
Darren E. Koenig, Heidi J. Hofer. College of Optometry, University
of Houston, Houston, TX.
Purpose: Spatial summation is important for understanding and
modeling the early stages of vision. Optimal summation is stimulusmatched; however our previous work in the dark-adapted fovea
suggests independent combination across multiple units of different
sizes within a zone of spatial uncertainty. By developing detection
models with different summation strategies and comparing predicted
behavior with experimental data we investigate the number of
different size units and whether detection is nearly optimal given both
uncertainty and noise.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Methods: Detection thresholds were previously measured in the
dark-adapted fovea for spots from 0.3' to 25' in diameter (550nm, 1030ms), viewed through either a 2 mm (conventional optics, 4
subjects) or 6 mm pupil (adaptive optics aberration correction, 5
subjects). Thresholds and psychometric function slopes were
compared with predictions from analytic and Monte-Carlo models
with different summation strategies given detection uncertainty,
Poisson noise, and cone mosaic granularity.
Results: Average change in log threshold with log stimulus area was
0.12±0.03 for stimuli up to 4-10' diameter, precluding both a single
unit size and the optimal stimulus-matched strategy. Data were
consistent with spatial uncertainty of at least 25'. Model comparison
suggests suboptimal combination across multiple-sized units, where
smaller units exhibit relatively more post-receptoral noise, with the
smallest unit no larger than the smallest stimulus (~0.5' retinal fullwidth half maximum), and the largest unit 4-10' in diameter. At least
two different unit sizes are required to describe the data. Although
many different unit sizes are required for performance approaching
optimal stimulus-matched summation, independent combination
across two sizes reduces efficiency by only ~0.1 log unit. With a 10'
largest unit (roughly parasol receptive field center size) and quantum
efficiency of 0.11-0.35, dark noise is estimated at 9-435
events/cone/s.
Conclusions: Dark-adapted foveal detection as a function of stimulus
size is consistent with independent combination across at least two
different sized units, the largest and smallest of which are consistent
with midget and parasol ganglion cell receptive field sizes. An
independent detection strategy across midget and parasol ganglion
cells is expected to perform only slightly worse than the optimal
stimulus-matched strategy, given noise and uncertainty constraints.
Commercial Relationships: Darren E. Koenig, None; Heidi J.
Hofer, None
Support: NIH ROI EY019069, P30 EY07551
Program Number: 3015 Poster Board Number: C0178
Presentation Time: 8:30 AM - 10:15 AM
Quick and easy light sensitivity assessment of the dark adapted
eye: The Tuebingen Scotopic Threshold Test (TSTT)
Torsten Strasser, Hana Langrová, Anne Kurtenbach, Ditta Zobor,
Dominic Hillerkuss, Eberhart Zrenner. Institute for Ophthalmic
Research, Centre for Ophthalmology, Tuebingen, Germany.
Purpose: Light sensitivity of the dark-adapted eye is a valuable
indicator of retinal function. Changes in light sensitivity are observed
in many retinal disorders like Retinitis pigmentosa, CSNB, or in
vitamin A deficiency. Light sensitivity is usually tested using dark
adaptometry: after transient exposition to bright light the darkadaptation curve and the final threshold are measured. This procedure
is time-consuming and uncomfortable, especially for children. Within
the EU-project TREATRUSH, we developed a test for assessing the
scotopic threshold for early detection of Usher's syndrome.
Methods: The TSTT has 2 panels for scotopic and photopic
stimulation. Each panel has a size of 7×10cm, consisting of 35
individually addressable LED bars, thus allowing to use various
stimulus shapes. The centerpiece of the TTST is a microcontroller
(ATmega8515, Atmel Corp.), running a self-developed software.
Stimulus luminance is tuned by pulse-width modulation and
adjustable in 100 steps between -3 to -1 log cd/m2. Using filters, this
can be extended from -8 to -1 log cd/m2. The luminance gradually
increases until a perception is indicated. The patient names the shape
and the examiner confirms or discards the response, thus
discriminating correct answers from false-positives. If confirmed, the
luminance is decreased and the procedure is repeated.
Feasibility and repeatability were tested in 11 subjects (10-68yrs).
Monocular and binocular presentation were compared, as well as
results obtained with natural or dilated pupil.
Results: All subjects completed the test successfully. Binocular
presentation reduced threshold by ~0.15 log units. Intra-subject
repeatability was >90%. We found no difference in the results
obtained with natural or dilated pupils. A flickering stimulus did not
show advantages over a constant presentation.
Conclusions: The Tuebingen Scotopic Threshold Test allows for
quick and easy assessment of the sensitivity of the dark-adapted eye.
The recording takes only 5 minutes (w/o dark adaptation), can be
done with natural pupils and is comfortable for the patient. Results
obtained with the TSTT show a high correlation to similar tests. This
makes the TSTT to a well suited tool for testing children.
This project and study is supported through TREATRUSH
(HEALTH-F2-2010-242013), a European Collaborative project supported by the European Commission under the 7th Framework
Program.
Commercial Relationships: Torsten Strasser, None; Hana
Langrová, None; Anne Kurtenbach, None; Ditta Zobor, None;
Dominic Hillerkuss, None; Eberhart Zrenner, Retina Implant AG
(F), Retina Implant AG (I), Retina Implant AG (C), Retina Implant
AG (P), QLT Inc (C), Servier, Paris (C), Steinbeis GmbH&CoKG,
Stuttgart (I), Steinbeis GmbH&CoKG, Stuttgart (C), Neurotech, USA
(C), Pfizer, USA (C)
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 3016 Poster Board Number: C0179
Presentation Time: 8:30 AM - 10:15 AM
Dark Adaptation and the effect of Oxygen Inhalation in Cystic
Fibrosis
Rachel Hiscox1, Christine Purslow2, Rachel V. North1, Ian Ketchell3,
Katharine Evans1. 1School of Optometry and Vision Sciences,
Cardiff University, Cardiff, United Kingdom; 2School of Health
Professions, Plymouth University, Plymouth, United Kingdom; 3All
Wales Adult Cystic Fibrosis Centre, University Hospital Wales,
Cardiff, United Kingdom.
Purpose: Previous research has shown impaired measures of dark
adaptation in cystic fibrosis (CF), with the cause generally attributed
to concomitant vitamin A deficiency. However, other factors
including CF-related diabetes (CFRD) may influence these results.
Impaired dark adaptation in Type 1 and 2 diabetics improves upon
oxygen inhalation and has therefore been attributed to retinal
hypoxia. The purpose of this preliminary study was to evaluate the
effect of oxygen inhalation on dark adaptation in CF, to determine the
underlying cause of impairment.
Methods: Dark adaptation was assessed in 9 CF (5 CFRD, 4 nonCFRD) and 9 age, gender and ethnicity-matched controls using a
custom made computerised dark adaptometer to present an 11°
achromatic stimulus centred on the fovea. All CF subjects were
vitamin A sufficient. Following pupil dilation, a Maxwellian view
optical system was used to administer an 82% cone and 75% rod
photopigment bleach. Subsequently, threshold was monitored for 25
minutes whilst the patient inhaled either medical air or 100% oxygen
(selected at random) through a 60% venti mask. This procedure was
repeated for the second gas following a 15 minute wash out period.
Threshold recovery parameters were modelled and the cone time
constant of recovery (τ), final cone and final rod thresholds
determined. Relationships were evaluated using paired and unpaired
T-tests as appropriate.
Results: Final rod threshold was significantly elevated in CF subjects
compared to controls when inhaling medical air, -4.54 and -4.64 log
cd/m2 respectively (p=0.03). Oxygen inhalation had no significant
effect on any parameter for controls. Oxygen inhalation in CF
subjects caused a significant decrease in final rod threshold compared
to medical air, -4.66 and -4.54 log cd/m2 respectively (p=0.04). When
analysed according to CFRD status, the CFRD group was found to
have a significantly elevated final rod threshold compared to the nonCFRD group when inhaling medical air, -4.47 and -4.64 log cd/m2
respectively (p=0.03). This difference was not present when inhaling
oxygen.
Conclusions: This study has shown final rod threshold to be
significantly elevated in CF, particularly in those with CFRD, with
recovery to normal levels upon inhalation of oxygen. For the first
time, this observation suggests that CFRD subjects experience
impaired dark adaptation secondary to retinal hypoxia, indicating
similarities to Type 1 and 2 diabetics.
Commercial Relationships: Rachel Hiscox, None; Christine
Purslow, None; Rachel V. North, None; Ian Ketchell, None;
Katharine Evans, None
Support: School of Optometry and Vision Sciences, Cardiff
University
Program Number: 3017 Poster Board Number: C0180
Presentation Time: 8:30 AM - 10:15 AM
Characteristics of Color Visual Acuity by Step Changes of
Background Luminance in Young Subjects of Normal Eyes
Yoshiki Tanaka1, Kiyoshi Tanaka1, Sho Yokoyama2, Hideki
Nakamura2, Kazuo Ichikawa2, Shoko Tanabe3. 1Faculty of
Engineering, Shinshu University, Nagano, Japan; 2Ophthalmology,
Social Insurance Chukyo Hosp., Nagoya, Japan; 3Chukyo Eye Clinic,
Nagoya, Japan.
Purpose: Color Visual Acuity (CVA) is the visual acuity that
measures from colored Landolt ring on the background of achromatic
color and that is the measure for evaluation of visual function for
colors in daily life. In our previous research, we measured CVA of
young normal subjects in the case of the background luminance of
the color 30 [cd/m2] (same luminance with Landolt ring’s color) and
100 [cd/m2]. In the result, for the background luminance of 100
[cd/m2], CVAs of all colors were almost the same value; and for the
background luminance of 30 [cd/m2], the CVAs of Blue-Yellow axis
of color were higher than the other colors. Then, we further examined
the changes of CVA for gradual changes of background luminance.
Methods: Four normal eyes of 4 subjects (4 males) were enrolled in
this study. The mean age was 21.8 years old (range 21-22 years).
They had no history of ocular disease (including color anomaly) or
surgery. All of them had best corrected visual acuity of 20/13. We set
the background color as white point of the standard light D65, and
Ladnolt ring was colored with four colors (“Red” and “Green” for the
Red-Green axis of color, “Green-Yellow” and “Blue-Purple” for the
Green-Yellow axis of color) used in New Color Test (Luneau
Ophtalmologie).The luminance value of Landolt ring was 30 [cd/m2]
as a fixed value, and background was from 50 to 30 [cd/m2] and from
15 to 30 [cd/m2].
Results: There was significant difference for the colors of G
(between 50 and 30 [cd/m2]), GY (between 50 and 30, 15 and 30
[cd/m2]), BP (between 50 and 30, 15 and 30, 15 and 28 [cd/m2])
(p<0.05, p<0.01, Friedman/Dunn test, shown in Figure)
Conclusions: In young subjects of normal eyes, it was confirmed that
the influence of luminance difference between background and
Landolt ring for the CVA of Blue-Yellow axis of color was
significant that in comparison with the CVA of Red-Green axis of
color. In addition, it was confirmed that there was a range of the
background luminance that could measure the CVA without the
influence of luminance difference between background and Landolt
ring in the area of 30 plus or minus 2 [cd/m2].
Measurement results of CVA by step changes of background
luminance in young subjects of normal eyes (CVA: Decimal Visual
Acuity).
Commercial Relationships: Yoshiki Tanaka, None; Kiyoshi
Tanaka, None; Sho Yokoyama, None; Hideki Nakamura, None;
Kazuo Ichikawa, None; Shoko Tanabe, None
Program Number: 3018 Poster Board Number: C0181
Presentation Time: 8:30 AM - 10:15 AM
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
A Color Visual Function Test to Evaluate the Age-Related
Changes in Good Visual Acuity of Normal Eyes
Sho Yokoyama1, Kazuo Ichikawa1, Hideki Nakamura1, Shoko
Tanabe2, Yoshiki Tanaka3, Kiyoshi Tanaka3, Rie Horai2.
1
Ophthalmology, Social Insurance Chukyo Hosp, Nagoya, Japan;
2
Chukyo Eye Clinic, nagoya, Japan; 3Faculty of Engineering, Shinshu
University, Matsumoto, Japan.
Purpose: Color Visual Acuity (CVA) is the visual acuity that
measured from colored Landolt ring on the background of achromatic
color and that is the measure for evaluation of visual function for
colors in daily life. From ARVO of 2012, we measured the subjects
of best corrected visual acuity (BCVA) 20/20 or better of normal
eyes in each generation to examine the CVA and we noticed
particularly in Red-Green axis color of CVA had negative correlation
with age. However, target group of BCVA has already accepted the
negative correlation with age, so that in comparison with the
conventional Landolt ring, we were not able to fully grasp the
significance correlation with CVA and age. Therefore, this time we
intended for only BCVA 20/13 of normal eyes and again to examine
the correlation of CVA and age-related changes.
Methods: One hundred thirteen normal eyes of 131 subjects were
enrolled in this study. The mean age was 39 years old (range 16-80
years). They had no history of ocular disease (including color
anomaly) or surgery. All of them had the BCVA 20/13. We set the
background color as white point of the standard light D65 and
Landolt ring colors with fifteen colors using the New Color Test
(Luneau Ophtalmologie, Paris). The luminance of background and
Landolt Ring is both set approximately at the same value of
30[cd/m2]).We measured all CVA of fifteen different colors for each
subjects (Figure).
Results: The results of the negative correlation with age are shown in
the descending orders GB, G, R, YR, YG, RY, BG, B, PR, P and RP.
In contrast the results of no correlation were Y, GY, PB and BP
(linear regression analysis: significance level P<0.05).
Conclusions: The subject group of the BCVA 20/13, even in the
normal subjects with good visual acuity, depending on colors, the
CVA decreased with increasing age.
Commercial Relationships: Sho Yokoyama, None; Kazuo
Ichikawa, None; Hideki Nakamura, None; Shoko Tanabe, None;
Yoshiki Tanaka, None; Kiyoshi Tanaka, None; Rie Horai, None
Program Number: 3019 Poster Board Number: C0182
Presentation Time: 8:30 AM - 10:15 AM
Training for Identification of Colors Altered by Colored Filters
Thomas Kuyk1, Alastair Smith1, Semih Kumru2. 1TASC, Inc, Ft Sam
Houston, TX; 2Air Force Research Laboratory, Ft Sam Houston, TX.
Purpose: Colored filters (CF) can alter the appearance of colored
stimuli because they selectively absorb visible light. Last year we
reported subjects can learn to rename narrow band (NB) hues
(generated on a CRT) that were altered in appearance by a CF. We
repeated last year’s experiment but with broad band (BB) reflective
hues and also determined if learning to identify altered BB hues had
any effect on identifying NB hues.
Methods: Six subjects were tested on a color naming (CN) task
wearing a CF that blocked short wavelengths. The CN stimulus set
consisted of 8 circular BB hues printed on a white background. One
hue was presented at a time using a color wheel (CW) format. Each
CW had 8 hues that differed in the set and order. One CW set had
colors labeled by name and another set had no labels. After
familiarization with the color set using labeled CWs, CN without a
CF was tested with the unlabeled CWs. Each color was presented 8
times in random order and subjects had a choice of 8 CNs. The test
was repeated with the CF. Then the CN test with NB hues was given
without and with the CF. Next a block of training trials with the CF
on was given using the labeled CWs. Subjects examined 64 colors (8
for each color in the set) at their own pace and were instructed to
learn to associate the CN with hues as they appeared through the CF.
No training with the NB hues was given. Immediately after the
training block, the BB CN test was re-administered. Subjects were
instructed to use what they had learned in training to name the colors.
Re-testing without further training occurred again 2 and 7 days later.
Also on day 7, the CN test with the NB hues was re-done. A control
group of 5 completed a similar sequence of CN testing with BB hues
but were never given any CN training. Data were CN error rates.
Results: CN without a CF was near 100% correct. With the CF, but
before training, errors increased to 33% incorrect. After training
errors decreased to 14% and stayed there at 2 days post training. At 7
days the error rate rose slightly to 20%. The initial error rate for the
NB colors with the CF was 71% and was unchanged at day 7. CN
performance for the control group showed little improvement with
repeated testing.
Conclusions: Subjects were able to learn to rename a set of BB hues
altered in appearance by a CF and retain that ability over a few days.
There was no evidence what was learned for BB hues transferred to
CN of NB hues.
Commercial Relationships: Thomas Kuyk, None; Alastair Smith,
None; Semih Kumru, None
Program Number: 3020 Poster Board Number: C0183
Presentation Time: 8:30 AM - 10:15 AM
Investigation of color vision defect among dental practitioners
Hani Alarify, Nasser Aldossari, Ahmed Alharbi, Ali Masmali, Turki
Almubrad. Cornea Research Chair, Optometry Department, College
of Applied Medical Sciences, King Saud University, Riyadh, Saudi
Arabia.
Purpose: Most of dental practitioners use the traditional method for
selecting shade which is based on the experience and the judgment of
the trained human eye of the operator. Dentists having defective color
vision may be unaware of their defect or may have problems in
perceiving color vision as normal dentists do. This study was aimed
to investigate color vision defect in adult dental practitioners.
Methods: 57 subjects (41 male, 16 Female) were recruited for the
study from Dentistry College at KSU & Dental Technology
Department at CAMS. The subjects were aged between 20 and 40
years (mean= 24.38), they were dentists, dental students and dental
technologist. Ishihara Color Test and Farnsworth dichotomous test D15 were used in this study. The Ishihara test was taken 1minute in
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
range. The Farnsworth dichotomous test D-15 was taken twice for
each subject with 6 minutes in range.
Results: 12.79% of subjects have color vision defect, 5 Males (8.7%)
have Protan and 2 Females (3.5%) have Protan during the first test of
Farnsworth D-15; but only 2 Males (3.5%) have Protan during the
retest of Farnsworth D-15.
Conclusions: The prevalence of color vision defect among dental
practitioners in this study is higher than the prevalence in a previous
study (12.3% of 160 subjects). Color vision test should be applied to
dental practitioners in order to avoid any defect for shade matching of
teeth.
Commercial Relationships: Hani Alarify, None; Nasser Aldossari,
None; Ahmed Alharbi, None; Ali Masmali, None; Turki
Almubrad, None
Program Number: 3021 Poster Board Number: C0184
Presentation Time: 8:30 AM - 10:15 AM
Dependence of the color brown on the spatial configuration of
high luminance surrounds
Tanner DeLawyer, Ariel Frederick, Simon Kaplan, Tracy Lin, Sophie
Shonka, Steven L. Buck. Psychology, University of Washington,
Seattle, WA.
Purpose: The same long-wavelength stimuli look brown when dim
and yellow-orange when bright, relative to surrounding stimuli.
Earlier research showed that the stimuli directly surrounding a brown
stimulus were most important in the perception of brown. We
confirmed these earlier results quantitatively and then tested the
dependence of brown on brighter surrounding stimuli by varying
their spatial configuration, to assess necessary and sufficient
conditions for perceiving brown.
Methods: Observers, under room-light adaptation, adjusted the
luminance of a constant-chromaticity 4°-diameter foveal test stimulus
to set both upper and lower luminance thresholds for perceiving
brown under the four possible combinations of white and black near
(4°x6° annulus) and far (6° and beyond) surrounds. The test stimulus
appeared yellow-orange when at a high luminance and brown at a
low luminance.
Observers also completed a set of trials with an otherwise identical
1°, 2°, 3°, 4°, 5°, 6°, or 7°-diameter foveal test stimulus with a 2°, 4°,
6°, and 8° white near surround and black far surround.
Results: Our results for the different combinations of near and far
surrounds indicated that the perception of brown occurred at
significantly higher luminance thresholds in the presence of a white
near surround regardless of far surround luminance. Subjects could
not perceive brown with a black near and far surround.
In our spatial configuration conditions we found a general trend that
as the size of the test stimulus increased, subjects had to adjust to
lower luminance values in order to perceive brown. The size of the
annulus did not have a significant effect on the subjects’ perception
of brown.
Conclusions: Our replication of earlier results established
quantitative light levels that are necessary for the perception of brown
under normal lighting conditions both with and without the presence
of a high luminance near surround.
Spatial results appear to indicate that as an object covers areas of the
retina outside of the fovea the perception of brownness begins to
fade, requiring a higher luminance contrast in order to perceive the
object as being brown. This agrees with observation that it is difficult
to perceive a stimulus as brown when it is viewed extra-foveally even
in the presence of a high luminance surround. This suggests the
neural mechanisms for perceiving a brown object are highly
dependent on foveal input.
Commercial Relationships: Tanner DeLawyer, None; Ariel
Frederick, None; Simon Kaplan, None; Tracy Lin, None; Sophie
Shonka, None; Steven L. Buck, None
Program Number: 3022 Poster Board Number: C0185
Presentation Time: 8:30 AM - 10:15 AM
Frequency of atypical genotypes associated with normal and
defective color vision
Candice Davidoff, Jay Neitz, Maureen Neitz. Ophthalmology,
University of Washington, Seattle, WA.
Purpose: The majority of red-green color vision deficiencies result
from gene rearrangements that cause the loss of normal L or M opsin
expression. This can be due to deletion of an L or M gene or insertion
of an extra L gene between the normal L and M genes, displacing the
M gene to a non-expressed position. Thus, characterizing the number
of L and M genes is a good predictor of the presence and type of
congenital red-green color vision defects. However, two atypical
types of mutations, missense mutations and extra L opsin genes
downstream of the expressed positions, would result in misdiagnoses
based on L and M gene stoichiometry. This study aims to estimate
the frequency of these types of mutations in the population.
Methods: For 803 males unselected for color vision deficiencies,
PCR was performed to selectively amplify L or M opsin genes. From
these products exons 3 and 4 were sequenced. The number and type
of opsin genes on the X-chromosome were determined by SNP
analysis using Sequenom's MassARRAY system. For samples found
to have extra L genes, long range PCR was performed to amplify the
most downstream gene and verify whether it encoded an L or M
opsin. For samples with missense mutations, parts of the last gene
were sequenced to determine if the mutation was in a gene in an
expressed position.
Results: 3 missense mutations were identified in L opsin genes:
R151T, V171L and V232L. 8 mutations were found in M opsin
genes: six C203R, one R163I and one synonymous mutation. No
C203R mutation was observed in any L opsin gene. 74 samples were
found to have extra L genes. Of these 25 were confirmed to have the
extra L in an expressed position, 20 were confirmed to have L genes
at the end of the array and thus are likely to have normal color vision,
and 29 had arrays too long to determine the position of the extra L
gene.
Conclusions: C203R mutations are unlikely to cause protan defects.
Missense mutations that may cause protan defects were present in
0.37% of the sample and those that may cause deutan defects were
detected in 1%. 9% of men in this sample have more than one L gene.
Of those, at least a quarter had the genetic basis for normal color
vision despite the presence of an extra L gene. 3.1% of men could be
confirmed to have an L gene in the second position and are presumed
to have deuteranomaly and another 3.6% may be deuteranomalous
depending on the location of the extra L gene(s) in arrays with > 3
genes.
Commercial Relationships: Candice Davidoff, None; Jay Neitz,
Alcon (F), Alcon (P); Maureen Neitz, Genzyme (F), Alcon (F),
Alcon (P)
Program Number: 3023 Poster Board Number: C0186
Presentation Time: 8:30 AM - 10:15 AM
Rod Hue Biases for Foveal Stimuli on CRT Displays
Katharina G. Foote, Steven L. Buck. Psychology, University of
Washington, Seattle, WA.
Purpose: Signals from rod photoreceptors bias (shift) the hues
determined by cone photoreceptors for extrafoveal mesopic stimuli creating green, blue, and red rod hue biases at long, middle, and short
wavelengths, respectively. The fovea contains far fewer rods and S
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
cones but may not be immune to rod hue biases. Here, we determine
which biases are found for foveal stimuli presented on a CRT display.
Methods: On a CRT display, a 1-s duration test disk of 0.5°, 1.0°, or
2.0° diameter alternated with a 3-s duration array of 0.25° fixation
dots placed 4° from fixation, all on a black background. Seven
observers adjusted the hue of the test disk around the RGB phosphor
mixture triangle, to yield each of the 4 unique hues, Ured, Ugreen,
Ublue, and Uyellow. Light levels ranged from 0.05 - 0.17 (CIE2°) or
0.08 - 0.03 (CIE10°) cd/m2.
Results: 1°-2°-diameter foveal test disks (a) produced rod green bias
at Uyellow for most observers, (b) favored rod green bias at Ublue
over the rod red biases shown in prior extrafoveal studies, and (c)
produced less consistent rod hue biases at Ured and Ugreen. 0.5°diameter foveal test disks produced no consistent rod hue biases
across observers. Remaining rod hue biases tended to be small but
some observers showed larger idiosyncratic effects for a specific
unique hue.
Conclusions: 1°-2°-diameter foveal disks on a CRT display
produced relatively strong rod green bias, mediated by rod interaction
with L & M cones, presumably in midget/parvo pathways. In
contrast, these foveal stimuli disadvantaged rod influence mediated
by S cones, presumably in small-bistratified/konio pathways,
producing only weak/inconsistent rod red bias at Ublue and rod blue
bias at Ured and Ugreen. 0.5°diameter disks disadvantaged all rod
hue biases, but with individually idiosyncratic exceptions for some
observers.
Commercial Relationships: Katharina G. Foote, None; Steven L.
Buck, None
Program Number: 3024 Poster Board Number: C0187
Presentation Time: 8:30 AM - 10:15 AM
Fundus-controlled two-color adaptometry with the
Microperimeter MP1
Wadim Bowl, Birgit Lorenz. Department of Ophthalmology, JustusLiebig-University, Giessen, Germany.
Purpose: To provide fundus-controlled two-color adaptometry of
mesopic vision with an existing device without modifying the CEmarked Microperimeter MP1 itself. Rod and cone sensitivity can be
measured and differentiated on defined retinal positions the examiner
is most interested in.
Methods: An external filter holder was imposed on the objective lens
of the MP1 (Nidek, Padova, Italy) and fitted with filters to modify
background and stimulus intensity. Light output of the MP1 was
reduced by Schott RG780 and BG3 filters outside the instrument to
create the stimulus colors red and blue, which were used alternating
in this examination. Absorption of infrared light by these filters is
low thereby minimizing problems with fundus observation by the
built-in infrared camera system. After bleaching with a Ganzfeld
ColorDome (Espion E2, Diagnosys LLC, Lowell, MA, USA) with a
luminous intensity of 3000 cd/m2 for 5 minutes, twenty normal
subjects were investigated with a pattern covering 3 spots at the
posterior pole of the retina (3 blue spots at 12° nasal; 3 red spots at 0°
and 1°). The test was repeated every 3 minutes during the first 15
minutes and every 5 minutes until 45 minutes of dark-adaptation.
Thresholds were determined using a 200 ms red Goldmann IV
stimulus and a blue Goldmann III stimulus employing the built-in 4-2
strategy in a dark room.
Results: In the first 5 minutes a slight increase of median light
increment sensitivity (LIS) was measured for the red stimulus. With
further dark-adaptation, LIS to red stimuli remained at about 7 dB.
For blue stimuli LIS increased considerably during the first ten
minutes. With processing time sensitivity to blue stimuli reached a
plateau at 15 dB. Both measurements showed typical characteristics
of dark-adaptation-curves.
Conclusions: Two-color fundus-controlled adaptometry with a
commercial MP1 without internal changes to the device provides a
quick and easy examination of rod and cone function during dark
adaptation at defined retinal loci. Under the mesopic lighting
conditions chosen, LIS for blue stimuli is determined by the rod
pathway. LIS for red stimuli is mediated by the cone pathway. The
method should be helpful to identify rod vs. cone function in the
posterior pole in early stages of retinal degenerations.
Commercial Relationships: Wadim Bowl, None; Birgit Lorenz,
Optos (F)
Support: German Research Counsil (DFG LO457/10-1)
Program Number: 3025 Poster Board Number: C0188
Presentation Time: 8:30 AM - 10:15 AM
Color Discrimination and Visual Perimetry Evaluation in
Multiple Sclerosis and Neuromyelitis Optica
Phelipe A. Paixao1, 2, Lorena B. Botelho Vergara1, 2, Lucas Daniel A.
Almeida Fernandes1, 2, Eliza Maria C. Lacerda1, 3, Givago S. Souza1,
3
, Hideraldo Luis Souza Cabeça5, Alexandre A. Rosa2, 4, Luiz Carlos
L. Silveira1, 3. 1Nucleo de Medicina Tropical, Universidade Federal
do Para, Belem, Brazil; 2Instituto de Ciencias da Saude, Universidade
Federal do Para, Belem, Brazil; 3Instituto de Ciencias da Biologicas,
Universidade Federal do Para, Belem, Brazil; 4Hospital Universitario
Bettina Ferro de Souza, Universidade Federal do Para, Belem, Brazil;
5
Neurologia, Hospital Ophir Loyola, Belem, Brazil.
Purpose: To compare visual performance in color discrimination and
visual perimetry of patients with multiple sclerosis (MS) and
neuromyelitis optica (NMO) with or without optic neuritis (ON).
Methods: Patients with MS (9 subjects, 17 eyes, 37±9.7 years old)
and with NMO (10 subjects, 18 eyes, 36.1±11.8 years old) were
studied with biomicroscopy, fundoscopy, and visual acuity
measurements. Color vision was evaluated with the full test protocol
of Colour Assesment and Diagnosis (CAD) Test. The diameter of the
circle with equivalent area of the color discrimination ellipses was
measured. Visual perimetry was evaluated by Central 30-2 Threshold
Test of the Humphrey Visual Field Analyzer. The two patient groups
were compared to each other and to an age- and gender-matched
control group. Statistical analyses used: tolerance intervals, binomial
test, two-way ANOVA, α=0.05.
Results: After the ophthalmologic evaluation, it was observed that 4
eyes from patients with MS and 6 eyes from patients with NMO had
ON. Color discrimination. 2/4 eyes from patients with MS and ON
and 4/10 eyes from patients with MS without ON had color
discrimination above the upper tolerance limit for controls. 1/6 eyes
from patients with NMO and ON and 1/9 eyes from patients with
NMO without ON had color discrimination above the upper tolerance
limit for controls. Regardless of ON presence, MS had significantly
more eyes with altered color discrimination results than NMO
(p<0.05). The MS group had statistically lower color discrimination
than the control group (p<0.05). Visual perimetry. There were no
statistical differences between the number of altered results across the
visual field between patients with MS with and without ON. The
group with MS and ON had significantly more altered results than
NMO with ON and, despite of the disease, there were more altered
results in patients with ON than without ON (p<0.05). There were no
altered results in the group of NMO without ON across the visual
field. The group of NMO with ON had significant lower sensitivity
than the control group at all eccentricities and had lower sensitivity
than the group of NMO without ON at eccentricity of 20° (p<0.05).
Conclusions: MS was more harmful to color discrimination than
NMO, while NMO patients had worse performance in visual
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
perimetry than MS patients. The ON presence impaired the visual
function mainly for visual perimetry and NMO patients.
Commercial Relationships: Phelipe A. Paixao, None; Lorena B.
Botelho Vergara, None; Lucas Daniel A. Almeida Fernandes,
None; Eliza Maria C. Lacerda, None; Givago S. Souza, None;
Hideraldo Luis Souza Cabeça, None; Alexandre A. Rosa, None;
Luiz Carlos L. Silveira, None
Support: CNPq, CAPES, FINEP, FAPESPA, UFPA
Program Number: 3026 Poster Board Number: C0189
Presentation Time: 8:30 AM - 10:15 AM
Psychophysical and electrophysiological evaluation of visual
function in type 1 diabetics
Valéria D. Garcia1, 3, Mirella Gualtieri3, 1, Mirella T. Barboni3, 1,
Daniela M. Bonci3, 1, Thiago L. Costa3, 1, Balázs V. Nagy1, 3, Sérgio T.
Rodrigues4, Ana L. Moura1, 3, Francisco Max Damico1, 2, Dora F.
Ventura1, 3. 1Neuroscience and bahavior, University of São Paulo,
São Paulo, Brazil; 2Ophthalmology, University of São Paulo, São
Paulo, Brazil; 3Experimental Psychology, University of São Paulo,
São Paulo, Brazil; 4Physical Education, Universidade Estadual
Paulista, Bauru, Brazil.
Purpose: Diabetes mellitus (DM) is a chronic disease that impairs
different aspects of health at different times during its progression.
One of the most prevalent complications associated with DM is
diabetic retinopathy (DR), which causes losses in visual functions
and can ultimately result in blindness. Visual loss can be detected
prior to the development of DR, potentially leading to improvement
in the blood sugar control, prevention, and treatment of DR. The
present work investigated color discrimination, contrast sensitivity
and the multifocal electroretinogram (mfERG) of type 1 DM patients
without DR.
Methods: Twenty patients with type 1 DM without DR (mean age =
28 ± 7 years old) were compared to 20 control subjects without
diabetes or ocular diseases (mean age = 28 ± 5). Color discrimination
was evaluated with the Cambridge Colour Test (CCT) and contrast
sensitivity with the Metropsis software (Cambridge Research System,
Ltd) using vertical sine wave gratings at seven spatial frequencies
(0.2; 0.5; 1; 2; 5; 10; 20 cpd). The Visual Evoked Response
Imagining System (VERIS) was used to record the mfERGs . Groups
were compared using ANOVA.
Results: Type 1 diabetic patients presented significantly elevated
values for all CCT parameters compared to control subjects. Protan,
deutan and tritan thresholds in u’v’ units were respectively 51.95 ±
23.81 (F1,40 = 5.384, p = 0.026); 53.45 ± 25.66 (F1,40 = 6.90, p =
0,012) and 93,90 ± 41,94 (F1,40 = 14.30, p = 0.001); elipse area was
1672 ± 1102 (F1,40 = 11.665, p = 0.002). Contrast sensitivity was
reduced in the diabetics at 0. 2 cpd (F1,40 = 4.67, p = 0.037) and 5 cpd
(F1,40 = 6.08, p = 0.004). mfERGs of DM patients showed increased
implicit time for N1 at 0° (F1,40 = 5.18, p = 0.03) and N2 at 5°(F1,40 =
4.15, p = 0.04) eccentricities. In addition, there was reduced
amplitude of N2 at the 20° (F1,40 = 4.40, p = 0.04) and 25° (F1,40 =
5.42, p = 0.02) eccentricities.
Conclusions: Non retinopathic type 1 diabetes mellitus patients
present significant visual loss detectable by psychophysical and
electrophysiological tests. Retinal hypoxia caused by chronic
hyperglycemia has been identified as the main reason for reduced
visual functions detected in the early DM, including color vision loss
and contrast sensitivity. These findings suggest that psychophysical
and electrophysiological tests should be routinely performed in
diabetic patients
Commercial Relationships: Valéria D. Garcia, FAPESP (F);
Mirella Gualtieri, None; Mirella T. Barboni, None; Daniela M.
Bonci, None; Thiago L. Costa, None; Balázs V. Nagy, None;
Sérgio T. Rodrigues, None; Ana L. Moura, None; Francisco Max
Damico, None; Dora F. Ventura, None
Program Number: 3027 Poster Board Number: C0190
Presentation Time: 8:30 AM - 10:15 AM
Psychophysical Measurement of Rod and Cone Thresholds in
Stargardt Disease with Full-Field Stimuli
Frederick T. Collison1, Gerald A. Fishman1, 2, J Jason McAnany2,
Jana Zernant3, Rando Allikmets3, 4. 1The Pangere Center for
Hereditary Retinal Diseases, The Chicago Lighthouse for People
Who Are Blind or Visually Impaired, Chicago, IL; 2Department of
Ophthalmology, University of Illinois Chicago, Chicago, IL;
3
Department of Ophthalmology, Columbia University, New York,
NY; 4Department of Pathology and Cell Biology, Columbia
University, New York, NY.
Purpose: To investigate rod and cone psychophysical thresholds in
Stargardt disease with the Diagnosys Full-Field Stimulus Test (DFST) using chromatic stimuli and a dark adaptation protocol.
Methods: Twenty-two patients with Stargardt disease (age range 2152) were categorized by fundus appearance as Stage 1 (flecks
confined to the macula, n=7), Stage 2 (flecks also outside the macula,
n=6), or Stage 3 (resorbed flecks, n=9). The better-seeing eye was
tested with ETDRS acuity charts, SD-OCT, and full-field ERG.
Using the D-FST, dark-adapted rod thresholds were measured with
short-wavelength stimuli and cone thresholds were obtained from the
cone plateau phase of dark adaptation using long-wavelength stimuli.
Four visually normal subjects (age range 28-38) also underwent the
D-FST with the same protocol.
For D-FST results zero dB = 0.1 photopic cd/m2. Correlation
coefficients were calculated for comparisons of D-FST thresholds to
other tests.
Results: Stargardt patient D-FST cone thresholds correlated with
ETDRS acuity (r=+0.56, p<0.01), ERG light-adapted single flash bwave (r=-0.78, p<0.001), and SD-OCT macular thickness (r=-0.62,
p<0.01).
For normal subjects D-FST mean rod threshold was -70.1 dB (SD
3.4), and mean cone threshold was -29.1 dB (SD 1.2).
Stage 1 D-FST cone and rod thresholds were all within 3 dB of
normal (mean rod and cone thresholds were -69.7 dB, SD 1.2 and 28.4 dB, SD 1.5, respectively). Stage 2 rod and cone thresholds
ranged from normal to well above normal by 7 dB for rods and 9 dB
for cones (rod mean -69.2 dB, SD 4.2; cone mean -25.6 dB, SD 4.5).
Stage 3 rod thresholds ranged from 1.3 to 13.8 dB above normal (rod
mean -63.8 dB, SD 4.9), whereas Stage 3 cone thresholds were all
elevated at least 6 dB above normal (cone mean -21.3 dB, SD 1.5).
Conclusions: D-FST may be useful as an efficient measure of visual
function in patients with macular dystrophies who have difficulty
fixating during visual field tests. Various levels of threshold elevation
were identified among three stages of Stargardt disease by measuring
thresholds with the D-FST both fully dark adapted (for rods) and
during dark-adaptation (for cones). Of particular importance, cone
thresholds in Stage 3 were consistently elevated, suggesting that fullfield cone thresholds may be a parameter that warrants monitoring in
this subset of Stargardt disease patients in treatment trials.
Commercial Relationships: Frederick T. Collison, None; Gerald
A. Fishman, None; J Jason McAnany, None; Jana Zernant, None;
Rando Allikmets, None
Support: Pangere Corporation, Grant Healthcare Foundation, Cless
Foundation, NIH #R00EY019510 (JM), NEI/NIH R01 EY021163
and NEI/NIH R24 EY019861 (RA)
Program Number: 3028 Poster Board Number: C0191
Presentation Time: 8:30 AM - 10:15 AM
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Laser Eye Protection and Visibility of Multi-Function Displays
Martin LaFrance1, Craig A. Williamson2, Leedjia Svec3, Thomas
Kuyk1. 1Air Force Research Laboratory, Fort Sam Houston, TX;
2
Defence Science and Technology Laboratory, Salisbury, United
Kingdom; 3Defense Equal Opportunity Management Institute, Patrick
AFB, FL.
Purpose: Handheld lasers have become commonplace, examples
include laser games and hobbyist targeting devices. Unfortunately
these lasers are at times used maliciously against commercial aircraft.
Misuse has risen at an alarming pace with the Federal Aviation
Administration reporting 3500+ events in 2011 alone; thus, laser eye
protection (LEP) for aircrew is a growing concern.
Aircrew LEP requires careful consideration for integration with
avionics and multifunction displays (MFD) which are heavily
dependent upon the accurate perception of color. The perception of
color, mediated by cone photoreceptors, is altered by conventional
LEP due to incongruent impact upon short, medium and longwavelength sensitive cones. The objective of this study is to compare
a color-balanced LEP design, one which preserves the weighting of
spectral transmission to cone subtypes, with conventional LEP on
tests of color discrimination used as predictors of MFD integration
and user acceptance.
Methods: 15 color-normal subjects completed color identification
tasks with the Farnsworth Munsell-100 and an 8-hue simulated MFD
color identification test without and with a color-balanced LEP and a
luminance matched neutral density (ND) filter. Results were
compared to predictive models of color identification errors (E94,
Color-Zone Border Analysis and ΔEu’v’) and like data collected
previously for two conventional LEP.
Results: FM-100 total error scores exceeded 80 for conventional and
color-balanced LEP designs, the threshold for impaired
discrimination, and were significantly higher than null and ND filter
conditions. Color identification was markedly improved on the 8-hue
MFD test for the color-balanced design vs. conventional LEP,
statistically outperforming on five hues and producing a minor
decrement for one. Global error rate across 8 hues was ~40% for
conventional designs and 7% for cone-balanced. E94 calculations
were ~10 for conventional vs. 8 for the cone balanced LEP design
also predicting improved hue discrimination.
Conclusions: A color-balanced LEP design demonstrates better
integration for key multi-function display hues when compare with
conventional LEP. Both conventional and color-balanced LEP, by
virtue of selectively blocked wavelengths, produce higher total error
scores with the Farnsworth Munsell-100; however, this test may not
be the best predictor of user acceptance for LEP in cockpit
integration.
Commercial Relationships: Martin LaFrance, None; Craig A.
Williamson, None; Leedjia Svec, None; Thomas Kuyk, None
Program Number: 3029 Poster Board Number: C0192
Presentation Time: 8:30 AM - 10:15 AM
Chromatic components in underwater targets do not affect Great
cormorants’ (Phalacrocorax carbo) visual resolution
Gadi Katzir1, 2, Ruth Almon1, Ido Izhaki1. 1Evolutionary and
Environmental Biology, University of Haifa, Haifa, Israel; 2Marine
Biology, University of Haifa, Haifa, Israel.
Purpose: The negative effects of scatter and absorption of light on
image formation impair vision underwater. Because scatter and
absorption are wavelength dependent, it is expected that visual
resolution for targets with different chromatic components, will
differ. Great cormorants pursue prey (fish) underwater, facing visual
constraints in their frequent transitions between air and water. Visual
resolution of cormorants for achromatic targets has been previously
established yet the effects of chromatic components have remained
open.
We aimed here to determine the underwater visual resolution of
cormorants for square wave gratings comprising chromatic and
achromatic components.
Methods: Hand-reared Great cormorants (N=6) were trained and
tested for their resolution, in an underwater Y-maze. The visual
targets comprised square-wave gratings that were achromatic (black
& white) or chromatic (black & color). Colors ranged from “reds”
through “yellow greens” to “blues”. Targets with vertically oriented
bars were “positive” and targets with horizontally oriented bars were
“negative”. Gratings ranged from 1.4 to 12 cpd. Illumination was
diffuse daylight and water turbidity ranged 0.3-5.6 NTU. The
cormorants’ choice was made at 1.4m from the targets. Each
individual provided results from ca. 30 tests on chromatic and ca. 7
tests on achromatic gratings. The proportion of correct choices was
used to determine resolution (at p=0.75 level).
Results: Over all cormorants (grouped) the mean maximal
underwater visual resolution for achromatic and chromatic gratings
was ca. 8cpd. Resolution for achromatic gratings was consistently
higher than for chromatic gratings yet the difference was not
significant. Chromatic components did not have a significant effect
while the effects of gratings frequency and of individual differences
on resolution were significant. Individuals showing high resolution
reached 6.1-12.2 cpd while individuals showing low resolution
reached 3.0 - 4.0 cpd.
Conclusions: Under the experimental conditions here, the chromatic
components in the targets did not affect visual resolution. It may well
indicate that color patterns of fishes, such as alternating black and
chromatic bars, may not significantly affect their detection by
foraging cormorants. Marked and consistent individual differences in
visual resolution must play a role in prey detection and capture
success.
Commercial Relationships: Gadi Katzir, None; Ruth Almon,
None; Ido Izhaki, None
Support: Israel Science Foundation - ISF
Program Number: 3030 Poster Board Number: C0193
Presentation Time: 8:30 AM - 10:15 AM
High Throughput Behavioral Estimates of Visual Thresholds in
Mice in a Watermaze with Cued Escape Platform
Arkady Lyubarsky, Muhammad Sheheryar Khan, Meera Sivalingam,
Jean Bennett. F.M. Kirby Center for Molecular Ophthalmology,
School of Medicine, University of Pennsylvania, Philadelphia, PA.
Purpose: To develop a quantitative, sensitive, cost-effective, noninvasive behavioral technique for evaluation of vision in mice with
emphasis on its suitability for the end point characterization in gene
therapy of retinal diseases.
Methods: The apparatus was a round (1.2 m diameter and 0.7 m
high) tub made of a dark blue plastic, and filled with water to a 20 cm
depth with a single submerged escape platform (8 cm diameter). A
plastic 20 cm high pole covered with a disposable aluminum foil
sleeve and standing at the platform center served as a visual cue
assisting animals in finding the platform. Four infrared sources
provided a uniform, invisible for mice, illumination of the tub, and a
video camera with an infrared filter was recording animal’s moves.
Four regulated visible light sources provided uniform illumination
inside the apparatus in a 1E-5 to 1E+2 scot cd m-2 range. Wild-type
(WT) and neural retina leucine zipper (NRL) knock-out (KO) mice
lacking rod photoreceptors were trained to escape to the platform at
the brightest level of illumination, and then were tested at 0.5 - 0.8
log-unit decrements of the illumination intensity. To determine the
threshold, we first evaluated the probability of reaching the platform
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
by chance per second of swimming time; to do this we measured the
frequency of platform encounter by mice swimming in dark with only
IR illumination on. In test runs an animal was considered as “seeing”
the pole if it reached the platform in 3 out of 3 consecutive trials, and
the probability of achieving this result by way of 3 random hits was
<1%.
Results: The thresholds for seeing the platform were ~1E-5 and ~5
scot cd m-2 for the WT and NRL KO mice, respectively; the value of
the threshold for the WT mice was somewhat lower than the one
determined by Hayes and Balkema (5E-5 scot cd m-2, Behavior
Genetics, VoI. 23, No. 4, 1993) in 6-way water maze experiments. In
contrast with their paradigm which required over 10 days of training
plus a comparable time for testing, our method needs only 6-8 hours
for training , 1-3 days for testing, and it does not require specialized
tracking software.
Conclusions: We suggest a quantitative behavioral test for evaluating
vision in mice which, as compared to analogous existing techniques,
offers 5-10 fold higher throughput at comparable or better sensitivity.
Commercial Relationships: Arkady Lyubarsky, None;
Muhammad Sheheryar Khan, None; Meera Sivalingam, Canon
Inc (F); Jean Bennett, Gensight Biologics (S)
Support: NIH P30EY001583, 8 DP1 EY023177, 1R24 EY019861,
Foundation Fighting Blindness, Research to Prevent Blindness,
Foundation for Retinal Research, EuroUsher Consortium, the
Grousbeck Family Foundation, The Mackall Foundation Trust.
334 Clinical Aspects of Motion Perception - Minisymposium
Tuesday, May 07, 2013 11:00 AM-12:45 PM
TCC LL 4/5 Minisymposium
Program #/Board # Range: 3210-3216
Organizing Section: Visual Psychophysics / Physiological Optics
Contributing Section(s): Eye Movements / Strabismus / Amblyopia
/ Neuro-Ophthalmology, Glaucoma
Program Number: 3210
Presentation Time: 11:00 AM - 11:15 AM
Motion perception in ocular disease and visual dysfunction
Peter Bex. Harvard Medical School, Boston, MA.
Commercial Relationships: Peter Bex, Adaptive Sensory
Technology, LLC (S), Rapid Assessment of Visual Sensitivity (P)
Program Number: 3211
Presentation Time: 11:15 AM - 11:30 AM
Motion perception in migraine
Allison M. McKendrick. Optometry & Vision Sciences, The
University of Melbourne, Parkville, VIC, Australia.
Commercial Relationships: Allison M. McKendrick, Heidelberg
Engineering GmbH (F)
Program Number: 3212
Presentation Time: 11:30 AM - 11:45 AM
Motion Perimetry
Michael Wall. Neurology & Ophthalmology, Univ of Iowa, Carver
Coll of Med, Iowa City, IA.
Commercial Relationships: Michael Wall, None
Program Number: 3213
Presentation Time: 11:45 AM - 12:00 PM
Moorfields Motion Displacement Test for Glaucoma
David F. Garway-Heath. Institute of Ophthalmology, University
College London, London, United Kingdom.
Commercial Relationships: David F. Garway-Heath, Moorfields
MDT (P), Carl Zeiss Meditec (F), Heidelberg Engineering (F),
Reichert Technoloies (F), Ziemer Ophthalmic Systems AG (F), Pfizer
Inc (F), Allergan (F), Allergan (C), Allergan (R), Alcon (C), Alcon
(R), Bausch & Lomb (R), Merck (R), Santen (R), Quark (C), Teva
(C), Topcon (F), OptoVue (F)
Program Number: 3214
Presentation Time: 12:00 PM - 12:15 PM
Global motion, suppression and amblyopia
Robert F. Hess. Ophthalmology, McGill University, Montreal, QC,
Canada.
Commercial Relationships: Robert F. Hess, None
Program Number: 3215
Presentation Time: 12:15 PM - 12:30 PM
Peripheral Motion Perception in Low Vision: Characterization of
Deficits and the Effects of Training
Duje Tadin. Brain & Cognitive Science, University of Rochester,
Rochester, NY.
Commercial Relationships: Duje Tadin, None
Program Number: 3216
Presentation Time: 12:30 PM - 12:45 PM
Motion Perception in Nystagmus
Magella M. Neveu. Electrophysiology, Moorfields Eye Hospital,
London, United Kingdom.
Commercial Relationships: Magella M. Neveu, None
344 Cones and Outer Retina
Tuesday, May 07, 2013 11:00 AM-12:45 PM
Exhibit Hall Poster Session
Program #/Board # Range: 3428-3455/C0149-C0176
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 3428 Poster Board Number: C0149
Presentation Time: 11:00 AM - 12:45 PM
Photoreceptor Pointing as a Function of Retinal Eccentricity in
Normal Human Eyes
Nathan Doble1, Rebecca Kivlin1, Johanan L. Codona2, Simone Li3,
Stacey S. Choi1. 1Vision Science, New England College of
Optometry, Boston, MA; 2Steward Observatory, University of
Arizona College of Optical Sciences, Tuscon, AZ; 3Retina
Foundation of the Southwest, Dallas, TX.
Purpose: The optical alignment of the cone photoreceptors with
respect to the pupil center is a potential metric to assess retinal health.
Roorda and Williams (JOV, 2002) first made measurements of the
directionality of single cone photoreceptors in normal human eyes.
Choi et al, (IOVS 2008) subsequently performed measurements on a
subject with retinal disease. We present work on a larger number of
normal subjects at several retinal eccentricities.
Methods: The adaptive optics (AO) fundus camera at the New
England College of Optometry was used to acquire retinal images on
three normal human subjects, N1, N2 and N3 (ages 23 to 26) at 2 and
4 degrees in the nasal retina. 2 degrees temporal eccentricity was also
measured in two of the subjects. At each location, a series of 1°
diameter retinal images (680nm light) were acquired for 9 different
entrance pupil positions. Images were then registered and a
centroiding algorithm applied to determine the alignment property of
individual cones at the pupil plane of the eye.
Results: After processing, the pointing of approximately 600 cones at
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
each retinal location could be measured. As an example, for subject
N1, the projection of the cone pointing at the pupil plane from all
retinal locations fell within an area of 0.25mm in diameter, located
slightly nasally (0.15mm) from the pupil center along the horizontal
meridian. The other subjects showed similar nasal bias in alignment
with respect to the pupil center.
Our disarray is smaller than that reported by previous studies
(Roorda, JOV, 2002) possibly due to choosing areas that did not
include retinal blood vessels.
Conclusions: For normal subjects, our results are in agreement with
previous reports (both psychophysical and imaging studies) that the
disarray of the photoreceptors is very small; which is to optimize the
efficiency of light capture within the photoreceptors. In diseased
eyes, larger variations in cone disarray were reported (Choi et al,
IOVS 2008).
Commercial Relationships: Nathan Doble, Iris AO Inc (I);
Rebecca Kivlin, None; Johanan L. Codona, None; Simone Li,
None; Stacey S. Choi, None
Support: EY020901
Program Number: 3429 Poster Board Number: C0150
Presentation Time: 11:00 AM - 12:45 PM
The role of defocus on photoreceptor light coupling analyzed
with a waveguide-based retinal simulator
Brian Vohnsen1, Diego Rativa Millan2, Carmen Vela1, Benjamin
Lochocki1, Philip B. Kruger3. 1School of Physics, University College
Dublin, Dublin, Ireland; 2Pós-Graduação em Engenharia de Sistemas
(PPGES), Universidade de Pernambuco, Recife, Brazil; 3College of
Optometry, State University of New York, New York, NY.
Purpose: Obliqueness of light at the retina diminishes the visual
response as a consequence of the Stiles-Crawford effect caused by
photoreceptor waveguiding. The aim of this study is to analyze the
sensitivity to defocus under waveguide conditions that resemble those
of the human eye retina using a retinal simulator consisting of an
array of photonic-crystal waveguides.
Methods: A liquid-filled photonic crystal fibre array has been used to
simulate waveguiding by retinal photoreceptors and the total fraction
of coupled light has been measured. Defocus is generated with a
Badal-system and monitored simultaneously with a Hartmann-Shack
wavefront sensor. Measurements are performed both at 633 nm and
at 543 nm wavelength to study a possible chromatic impact. The
results are compared with those of an analytical waveguide model
and Zemax-based eye models.
Results: Measurements show that the fraction of coupled light power
is sensitive to defocus as expected due to the wavefront curvature at
the entrance facet of the waveguides. This is in agreement with the
numerical models suggesting a possible role of light power for
accommodation and emmetropization of the eye.
Conclusions: We found that a photonic crystal fibre array is a
suitable experimental tool to analyze the role of defocus and more
generally aberrations and their possible role on vision and effective
retinal images. The fraction of light that couples to waveguide modes
may provide a clue for accommodation and emmetropization of the
eye. The sign of defocus is not determined but may relate to the
chromatic difference for a finite bandwidth or to photoreceptor
disarray though also other aberrations and other factors can provide
accommodative clues.
Commercial Relationships: Brian Vohnsen, None; Diego Rativa
Millan, None; Carmen Vela, None; Benjamin Lochocki, None;
Philip B. Kruger, None
Support: Science Foundation Ireland grants 07/SK/B1239a and
08/IN.1/B2053
Program Number: 3430 Poster Board Number: C0151
Presentation Time: 11:00 AM - 12:45 PM
Measurement of the Photoreceptor Pointing in the Living Chick
Eye
Maria Walker, Rebecca Kivlin, Nathan Doble. Vision Science, New
England College of Optometry, Boston, MA.
Purpose: The chick retina is a widely used animal model in the study
of eye growth, in particular for the study of emmetropization and
myopia. Like most eyes, the ability to image the fine retinal structure
is degraded by the aberrations in the lens and cornea. In previous
work, we showed in-vivo images of individual chick photoreceptors
taken with an adaptive optics (AO) fundus camera (Headington et al.
Current Eye Research, 2011). Here we utilize this imaging capability
to examine the individual cone directionality of the chick
photoreceptors.
Methods: Two White Leghorn chickens (Gallus gallus domesticus)
(age 30d, approx. 650g) were anesthetized with a combination of
Ketamine/Xylazine and dilated with Vecuronium Bromide
suspension prior to imaging. The AO fundus camera at the New
England College of Optometry was modified in order to image the
smaller 3mm pupil of the chick. Translating the entrance pupil
position of the imaging beam (650nm) allowed for the measurement
of the individual cone pointing. Thirteen entrance pupil positions
were tested to obtain 1-degree FOV retinal images; four retinal
images were registered for each position. Upon compensating for the
variation in incident light intensity due to light delivery optics, a
centroiding algorithm was used to determine the directionality of
individual cones.
Results: Upon projection of the cone pointing toward the pupil plane,
the degree of disarray was found to be slightly larger than that found
in the human eye. Interestingly, our initial results show an elliptical
pointing pattern in the pupil plane with major and minor axes of 0.5
and 0.2 mm respectively. The major axis was horizontal and the
center of the pattern lay on average 0.5 mm from the pupil center.
Conclusions: Similar to the human eye, the chick photoreceptor
disarray is small, implying that the receptors are aligned to maximize
the signal coming through the center of the pupil aperture.
Commercial Relationships: Maria Walker, None; Rebecca Kivlin,
None; Nathan Doble, Iris AO Inc (I)
Support: NH Grant EY020901
Program Number: 3431 Poster Board Number: C0152
Presentation Time: 11:00 AM - 12:45 PM
Reproducibility of the rtx1 adaptive optics retinal camera
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Dirk-Uwe G. Bartsch, Cheryl Arcinue, Feiyan Ma, Lingyun Cheng,
William Freeman. Ophthalmology-Shiley Eye Ctr, Univ of
California-San Diego, La Jolla, CA.
Purpose: To study the reproducibility of the flash-illumination
commercially available adaptive optics retinal camera rtx1
(ImagineEyes, Orsay, France) in a group of normal volunteers.
Methods: The rtx1 is an adaptive optical fundus camera using
flashed, non-coherent flood illumination centered at 850 nm to record
a series of 40 images. Each image covers an area of 4° x 4°. The
instrument is claimed to have a pixel resolution of 1.6 µm and resolve
250 line pairs per millimeter. The instrument uses a yellow fixation
cross to help the subject fixate. The location of the center of fixation
cross is stored by the instrument allowing the subject to fixate to the
same stimulus location.
After approval by the Institutional Review Board we recruited 6
subjects and imaged each subject in two different sessions. We
selected 5 regions of interest. One was at the center of the fovea, and
the other four regions were centered at 2 degrees from the foveal
center in the four principal directions (superior, inferior, nasal and
temporal). We selected a measurement area for each image pair that
was matching according to vessel landmarks. We used the adaptive
optics analysis software from ImagineEyes to measure density and
spacing for each image.
For statistical analysis we used concordance correlation coefficient
(Lin, 1989) with a 95.0% asymptotic confidence interval, and a 95%
BCa bootstrap confidence interval using SAS (Cary, NC).
Results: We found that the rtx1 was able to resolve the photoreceptor
cone mosaic in the parafoveal area. The instrument was not able to
resolve the cone mosaic in the center of the macula. The central 2.5°
of the fovea could not be resolved. For density means we found a
CCC of 0.767. For spacing means we found a CCC of 0.786.
Conclusions: The rtx1 adaptive optical camera allows reproducible
acquisition of the photoreceptor cone mosaic. The resolution limit of
the instrument does not allow imaging at the center of the fovea due
to the very dense spacing of the photoreceptors. The current software
does not allow to exclude blood vessels from the analysis. These two
areas might influence overall accuracy and should be excluded in
future versions of the software.
Commercial Relationships: Dirk-Uwe G. Bartsch, None; Cheryl
Arcinue, None; Feiyan Ma, None; Lingyun Cheng, Spinnaker
Biosciences (C); William Freeman, OD-OS, Inc. (C)
Support: NEI Grants R01EY016323, R01EY007366,
R01EY018589, P30EY022589
Program Number: 3432 Poster Board Number: C0153
Presentation Time: 11:00 AM - 12:45 PM
Test-Retest Reliability of Microperimetry Using the Optos OCT
SLO in Eyes With and Without Known Retinal Diseases
Hyun Soo Jang, Yasir J. Sepah, Millena G. Bittencourt, Mohammad
A. Sadiq, Owhofasa O. Agbedia, Hongting Liu, Mehreen Ansari,
Zubir S. Rentiya, Daniel A. Ferraz, Quan Dong Nguyen. Retinal
Imaging Research and Reading Center, Wilmer Eye Institute, Johns
Hopkins University, Baltimore, MD.
Purpose: To evaluate the test-retest reliability of Optos (Optos, Inc,
Scotland, UK) OCT SLO microperimetry (MP) device in eyes with
and without known retinal diseases.
Methods: Thirty six eyes of 19 subjects (ages 20-53, mean 29) with
no known retinal diseases and 10 eyes of 5 subjects (ages 29-76,
mean 52) with known retinal diseases were scanned. All tests were
performed using the Optos OCT SLO. For each eye, a fixation test
and spectral domain optical coherence tomography were obtained
before the MP. Three consecutive fundus-aligned MP sessions for
each eye with a maximum of 2-minute interval between the sessions
were performed using the following settings: a customized 9-point
pattern, 200 ms stimulus duration, Goldmann III size, 4-2-1 dB
staircase strategy, 10 dB initial brightness, and red cross as the
fixation target. The 9 points consisted of a 3x3 upright square lattice
centered at the fovea, having a 1.5° angle between the center and
every corner point (Figure). The point sensitivities were recorded.
Results: Sensitivities and variances are recorded in the Table.
Friedman Test showed no significant differences in the mean
sensitivities across the 3 sessions in both groups (p>0.7 for both). The
overall inter-session variances in normal (1.03 ± 0.07) and diseased
(2.43 ± 0.51) groups were significantly different (p=0.05, MannWhitney Test). The variances of 9 points were significantly different
in both groups (p<0.05, Friedman Test). The points with greatest
variances are highlighted in the Table.
Conclusions: The Optos OCT SLO microperimeter produces reliable
test results with no significant differences in mean sensitivities
among sessions.
Eyes with retinopathies were found to have greater inter-session
variance than those without. Therefore, interpretation of the changes
in retinal sensitivities among eyes with pathologies must take into
consideration the differences in test variances between normal and
diseased eyes.
Additional studies on the MP variances in different and larger
diseased groups are indicated.
Figure
Table
Commercial Relationships: Hyun Soo Jang, None; Yasir J.
Sepah, None; Millena G. Bittencourt, None; Mohammad A.
Sadiq, None; Owhofasa O. Agbedia, None; Hongting Liu, None;
Mehreen Ansari, None; Zubir S. Rentiya, None; Daniel A. Ferraz,
None; Quan Dong Nguyen, Genentech (F), Regeneron (F), Lux
Biosciences (F), Abbott (F), GSK (F), Santen (F), Santen (C), Bausch
and Lomb (C), Optos (F), Heidelberg Engineering (F)
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Support: Retinal Imaging Research and Reading Center Fund
Program Number: 3433 Poster Board Number: C0154
Presentation Time: 11:00 AM - 12:45 PM
Assessing retinal detailed structure in pathological myopia with
adaptive optics scanning laser ophthalmoscope
na liao, Chaohong Li, Yiyu Li, Hao Chen, Qinmei Wang. wenzhou
medical college, WenZhou, China.
Purpose: To examine the retinal detailed structure in pathological
myopia with adaptive optics scanning laser ophthalmoscope
(AOSLO).
Methods: The 20 eyes (10 emmetropias and 10 pathological
myopias) of 20 subjects, whose ages ranged from 18 to 30, were
enrolled. An AOSLO was used to obtain high resolution images of
the macular photoreceptor mosaic, the surface-level pores of the
lamina cribrosa and parafoveal capillary network of all participants.
Results: AOSLO can compensate living human eye’s optical
aberrations and get the retinal detailed histological image. Compared
with the emmetropic eyes, the pathological myopia subjects showed
an average lower cone packing densities in macular, greater lamina
cribrosa pore areas, bigger foveal avascular zone (FAZ) and lower
leukocyte speed.
Conclusions: AOSLO as a non-invasive technique is able to
visualize detail images in vivo retina which can assist in detecting
pathologic features and illuminating the reasons of the increased
glaucoma susceptibility in highly myopic eyes. This novel technique
provides opportunities to enhance the understanding of retinal
pathogenesis.
Commercial Relationships: na liao, None; Chaohong Li, None;
Yiyu Li, None; Hao Chen, None; Qinmei Wang, None
Program Number: 3434 Poster Board Number: C0155
Presentation Time: 11:00 AM - 12:45 PM
Variation of cone density assessed by Adaptive Optics Retinal
Camera with axial length
meillat mathieu, Perle TUMAHAI, Mélanie Bidaut-Garnier,
Guillaume Debellemaniere, Mathieu Flores, Michel Montard,
Bernard Y. Delbosc, Maher Saleh. ophthalmology, besancon hospital
jean minjoz, Besancon, France.
Purpose: To assess macular cone densities changes with axial length
(AL) and spherical equivalent (SE) using Adaptive Optics (AO).
Methods: Fifty-two eyes of 28 healthy adults under 50 years, with a
visual acuity of 20/20, were imaged. Group 1 included myopic and
group 2 non myopic eyes. All patients underwent a complete
ophthalmologic examination, spectral-domain optical coherence
tomography (SD OCT), and imaging with the RTX-1 Adaptive
Optics (AO) device from Imagine eyes™ (Orsay, France). Mean cone
density (cells/mm2) at a fixed distance from the fovea (1° nasally and
temporally), spacing between cells (µ) and percentage of hexagonal
cells calculated on Voronoi diagrams, were obtained by two masked
graders using AODetect v. 0.1, the proprietary software of the device.
Axial length was measured by using IOL Master® (Carl Zeiss.
Meditec. USA).
Results: In group 1 (n=22), AL was 25.17+-1.15 mm and SE -5+2.73 D. In group 2 (n=30), AL was 23.09+-0.87mm (p<0.05) and SE
1.23+-2.05 D (p<0.05). The mean age was 30.55 with no difference
between groups (p<0.05). Cone density was lower in group 1
(23251+-1845 cells/mm2 vs 25419 +-2443 cells mm2 in group 2, t
test, p=0.001). Spacing between photoreceptors was also higher in
myopic eyes (7.47 +-0.52 µ vs 7.06 +-0.36 µ,t test, p=0.001). There
was no difference in percentage of hexagonal cells between both
groups. The cone density was inversely proportional to the axial
length and the spherical equivalent (r2= 0.22,p=0.002 and r2=0.17
p=0.002, respectively). The multiple regression analysis showed that
AL but not age contributed to the change in cone density (p=0.001).
Conclusions: Myopic subjects with a good visual acuity showed a
lower cone density in the macular area and a higher spacing between
cells, correlated to the axial length. Adaptive Optics could help
understanding the pathological changes induced in the retina by the
myopia.
Commercial Relationships: meillat mathieu, None; Perle
TUMAHAI, None; Mélanie Bidaut-Garnier, None; Guillaume
Debellemaniere, None; Mathieu Flores, None; Michel Montard,
None; Bernard Y. Delbosc, None; Maher Saleh, None
Program Number: 3435 Poster Board Number: C0156
Presentation Time: 11:00 AM - 12:45 PM
Quantification and Comparison of Cone density, Outer Nuclear
Layer and Henle’s Fiber Layer Thickness Using High-Resolution
Imaging
Grace K. Han1, Jan Kristine T. Bayabo2, Brandon J. Lujan2, 3, Jessica
I. Morgan1. 1Scheie Eye Institute of Opthalmology, University of
Pennsylvania, Philadelphia, PA; 2Vision Science, University of
California, Berkeley, CA; 3West Coast Retina Medical Group, San
Francisco, CA.
Purpose: To quantify and compare cone photoreceptor density as
measured with adaptive optics scanning laser ophthalmoscopy
(AOSLO) to the thicknesses of the outer nuclear layer (ONL) and
Henle’s fiber layer (HFL) as measured by directional optical
coherence tomography (D-OCT).
Methods: Retinal images from 8 normal sighted subjects (age 15-22)
with no known retinal pathology were acquired along the nasaltemporal meridian with an AOSLO developed by Canon Inc.
Horizontal D-OCTs through the fovea were acquired using the
Heidelberg Spectralis OCT. During D-OCT imaging the entry
position of the beam was modified horizontally through the pupil to
reveal HFL. AOSLO cone images were registered using custom
software from Canon, and manually montaged for precise alignment
to the Spectralis fundus images and D-OCT sets. Cone density was
measured at precise locations along the horizontal meridian using a
semi-automated, custom Matlab program. D-OCTs were registered
and the ONL and HFL were manually segmented. The thicknesses of
these layers were measured at locations where cone density was
measured.
Results: Cone density was highest in the central most measured
location and decreased with increasing eccentricity. The cone
densities measured in this study agreed with previously reported
densities for normal controls. From ~0.75-1.5mm cone density
positively correlated with HFL thickness (R2=0.46). ONL thickness
was highest in the fovea and decreased with eccentricity until
reaching a local minimum at ~0.8mm. From ~ 0.8-1.3mm there was a
slight increase in ONL thickness, beyond which ONL thickness
leveled off. Cone density did not correlate with ONL thickness from
0.75-1.5mm (R2=0.02). The variability in cone density between
subjects was less than the variability of ONL and the variability of
HFL thickness at all locations measured between 0.75-1.5mm
eccentricities.
Conclusions: HFL can be imaged and quantified separate from the
ONL by using directional OCT. ONL thickness did not correlate with
cone density in the imaged regions, likely due to the increasing rod
contribution at these eccentricities. Cone density measurements show
less variability between subjects than ONL measurements, which
may be a reflection of variability in the contribution of rods. Further
studies will examine total photoreceptor densities in comparison with
ONL and HFL thicknesses.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Grace K. Han, Canon Inc. (F), Optos
PLC (F); Jan Kristine T. Bayabo, None; Brandon J. Lujan,
Genentech (C), Genentech (R), Genentech (F), Carl Zeiss Meditec,
Inc (C), Avalanche Biotech (C), Regeneron (R), UC Berkeley (P);
Jessica I. Morgan, Canon (F), Optos (F)
Support: Earl and Brenda Shapiro Leber's Congenital Amaurosis
Research Initiative, Foundation Fighting Blindness, NIH K12
EY017269, NIH EY019861, F.M. Kirby Foundation, Research to
Prevent Blindness, Mackall Trust, Canon Inc.
Berkeley (P); Shiri Zayit-Soudry, None; Reema Syed, None;
Travis Porco, NIH NEI (F); Jan Kristine T. Bayabo, None; Joseph
Carroll, Imagine Eyes, Inc. (S); Austin Roorda, US Patent
#6890076 (P), US Patent #7118216 (P), UC Berkeley (P); Jacque L.
Duncan, None
Support: Foundation Fighting Blindness, Research to Prevent
Blindess, That Man May See, NEI Core Grant EY002162, NIH K12
EY017269
Clinical Trial: NCT00254605
Program Number: 3436 Poster Board Number: C0157
Presentation Time: 11:00 AM - 12:45 PM
Correlation of outer nuclear layer thickness with cone density
values in patients with retinitis pigmentosa and healthy subjects
Moreno Menghini1, Brandon J. Lujan2, Shiri Zayit-Soudry1, Reema
Syed1, Travis Porco1, Jan Kristine T. Bayabo2, Joseph Carroll3,
Austin Roorda2, Jacque L. Duncan1. 1Ophthalmology, University of
California San Francisco, San Francisco, CA; 2School of Optometry,
University of California Berkeley, Berkeley, CA; 3Ophthalmology,
Medical College of Wisconsin, Milwaukee, MI.
Purpose: Outer nuclear layer thickness (ONL) has been widely used
as a marker for photoreceptor numbers. However, some studies have
not shown a consistent correlation between ONL thickness and cone
density. Variability in ONL thickness measurements may be
attributed to the inclusion of Henle’s fiber layer (HFL) when using
standard optical coherence tomography (OCT) imaging techniques.
The aim of our study is to compare ONL thickness using directional
OCT (D-OCT) with cone density values at identical retinal locations
in normals and retinitis pigmentosa (RP) patients.
Methods: Cross-sectional analysis of images acquired with D-OCT
and adaptive optics scanning laser ophthalmoscopy (AOSLO) from
normals and RP patients. The D-OCT data sets were obtained using a
previously described method of varying the pupil entry position of
the beam to reveal the HFL. Five retinal layers (ILM, OPL/HFL
junction, HFL/ONL junction, ELM and outer RPE border) were
segmented using Image J and MatLab® software. Multiple locations
along the central horizontal meridian were selected on the AOSLO
images and compared with ONL thicknesses at identical
eccentricities. Cone density was analyzed in areas where cone
mosaics could unambiguously be identified and expressed as
cones/degree2.
Results: Mean age in our population was 40.5 in patients and 42.0
years in normals. Average central retinal thickness was 240±25.0um
and 234±12.8um, with an average ONL thickness at 1° eccentricity of
47.2±8.8um and 46.0±3.7um in patients and in normals. Mean ONL
thickness at 2° eccentricity was also comparable with 33.7±6.7um in
RP patients and 33.7±7.1um in normals. Average cone densities
measured at 1° eccentricity were 3718±1287 and 4313±541 for
patients and normals, respectively. At more eccentric locations (2°
eccentricity) the values were 2646±531 and 2646±245. Combining
the normal and patient images, ONL thickness was significantly
correlated with cone density (Pearson’s correlation coefficient 0.74,
95% CI 0.67, 0.82). The correlation between ONL+HFL values and
cone density on the other hand was weaker (coefficient 0.59, 95% CI
0.46, 0.78).
Conclusions: ONL thickness measures correlated with cone density
measures in normals and RP patients, as measured using D-OCT.
ONL thickness could be an easily obtainable indirect parameter to
represent cone density values both in diseased and healthy
individuals.
Commercial Relationships: Moreno Menghini, None; Brandon J.
Lujan, Genentech (C), Genentech (R), Genentech (F), Carl Zeiss
Meditec, Inc (C), Avalanche Biotech (C), Regeneron (R), UC
Program Number: 3437 Poster Board Number: C0158
Presentation Time: 11:00 AM - 12:45 PM
Repeatability of Cone Density Measurements in Healthy Subjects
Using Commercially Available Flood-Illuminated Adaptive
Optics
Shu Feng, Anupam K. Garg, Ambar Faridi, Jonathan D. Fay, Hope
E. Titus, Travis B. Smith, Keith V. Michaels, Mark E. Pennesi. Casey
Eye Institute, Oregon Health & Sciences University, Portland, OR.
Purpose: To evaluate a commercially available flood-illuminated
adaptive optics camera for its repeatability in measuring the cone
mosaic and to determine average cone density among healthy
subjects
Methods: We used the RTX1 flood-illuminated adaptive optics
camera (Imagine Eyes: Orsay, France) to image the cone mosaic in
54 healthy subjects, ages 14 to 69 years. For each subject, a series of
25 4°x4° retinal images were obtained. Using MosaicJ, these images
were combined to create a retinal montage spanning a 12°x12° field
of the central macula. Retinal montages were analyzed for regional
differences in cone density. Images were post processed in ImageJ
and cone counting was performed with a MATLAB algorithm. To
determine repeatability of the device and montaging process, a subset
of 7 subjects ranging in age from 19 to 36 years were imaged on 3
separate occasions. To assess the validity of automated cone counting
for each montage, automated cone counts were compared to manual
counts in sample retinal areas 2° and 4° temporal to the foveal center.
Results: Image quality was excellent in most young subjects, but
increasingly variable in older subjects. Cones within 1.5° of the
foveal center could not be resolved with this camera. Angular density
of cones averaged 1587 ± 91 cones/degree2 at 1.6° - 4.3° eccentricity
and 1428 ± 64 cones/degree2 between 4.3° and 5.4° eccentricity.
When adjusted for axial length, cone density averaged 18,688 ± 2081
cones/mm2 between 1.6° and 4.3° and 16,763 ± 1669 cones/mm2
between 4.3° and 5.4°. Angular cone density between 1.6° and 4.3°
decreased with age, but between 4.3° and 5.4° increased. Repeated
measurements of cone density in the same subject from separate
imaging sessions resulted in an intraclass correlation coefficient of
0.98 (p < 0.001, 95% CI: 0.93-1.00) between 1.6° and 4.3° and 0.95
(p < 0.001, 95% CI: 0.83-0.99) between 4.3° and 5.4°. However,
validity of the automated cone counting algorithm depended on
image quality, with poor quality images producing higher variability.
Conclusions: Flood-illuminated adaptive optics provides
measurements of cone density that are consistent with anatomical
studies. Repeated measurements in a subset of younger subjects
resulted in very strong intraclass correction coefficients, which
indicate the system produced consistent measurements. However,
challenges remain with older subjects.
Commercial Relationships: Shu Feng, None; Anupam K. Garg,
None; Ambar Faridi, None; Jonathan D. Fay, None; Hope E.
Titus, None; Travis B. Smith, Pfizer, Inc. (F); Keith V. Michaels,
Pfizer, Inc. (F); Mark E. Pennesi, Pfizer (F)
Support: Research to Prevent Blindness (Unrestricted, CEI),
Foundation Fighting Blindness (Pennesi CDA, CD-CL-0808-0469-
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
OHSU), Foundation Fighting Blindness (Weleber, C-CL-0711-0534OHSU01)
Program Number: 3438 Poster Board Number: C0159
Presentation Time: 11:00 AM - 12:45 PM
High resolution imaging of photoreceptors in healthy humans of
different ages eyes using RTX-1 ™ Adaptive Optics Retinal
camera
Perle TUMAHAI, meillat mathieu, Melanie Bidaut-garnier,
Guillaume Debellemaniere, Mathieu Flores, Michel Montard,
Bernard Y. Delbosc, Maher Saleh. Ophthalmology, University
Hospital of Besançon, Besançon, France.
Purpose: To determine age-related macular photoreceptor density
changes in healthy patients of various ages.
Methods: Observational case series. Healthy subjects with no retinal
pathology or systemic affection were included. High myopic patients
were excluded. All patients underwent a full ophthalmologic
examination, SD-OCT imaging, and imaging with the RTX-1 ™
Adaptive Optics (AO) retinal camera from Imagine eyes® (Orsay,
France).
Mean cone density (cells/mm2) at a fixed distance from the fovea (1°
nasally and temporally), spacing between cells (µm) and % of
hexagonal cells calculated on Voronoi diagrams, were obtained using
AODetect v. 0.1, the proprietary software of the device.
Results: 58 normal eyes of 35 patients were studied. Mean age was
34.45±2.5 y (min-max: 10-78y). The mean cone density reached
24039±2914.5 cells/mm2. It decreased with age (R2=0.21, p<0.001).
Patients above 50 y lost 17.5% of the cone density compared to
patients under 15 y (t-test, p=0.003). Spacing between cells
(mean±SD: 7.31±0.56µm) increased with age (R2 =0.15, p=0.002),
while the percentage of hexagonal cells (mean±SD: 43.93±3.8 %)
moderately decreased (R2 =0.07, p=0.04). Cone density was slightly
correlated to the thickness of the photoreceptor layer on OCT
(distance between IS/OS and ELM hyperreflective lines) (R2= 0.08,
p=0.04) but neither with central macular thickness nor choroidal
thickness.
Conclusions: Macular cone density decreased with age. The
consequences of this finding on visual acuity as well as the meaning
of spacing between cells and rate of hexagonal cells in the macula are
not known yet.
Commercial Relationships: Perle TUMAHAI, None; meillat
mathieu, None; Melanie Bidaut-garnier, None; Guillaume
Debellemaniere, None; Mathieu Flores, None; Michel Montard,
None; Bernard Y. Delbosc, None; Maher Saleh, None
Program Number: 3439 Poster Board Number: C0160
Presentation Time: 11:00 AM - 12:45 PM
Quantitative analysis of cone photoreceptor distribution in aged
patients using an adaptive optics fundus camera
Ryo Obata1, Xue Tan1, Kayo Kure1, Frida Rosander2, Yasuo Yanagi1.
1
Department of Ophthalmology, The University of Tokyo, Tokyo,
Japan; 2Department of Biomedical Engineering, Medical Informatics,
Linköping University, Linköping, Sweden.
Purpose: Relationship between cone photoreceptor distribution and
aging is unclear. We used adaptive optics fundus camera to examine
cone photoreceptor distribution in the macular area of aged patients
and quantitatively analyzed its relationship with age, axial length, and
age-related maculopathy for the first time to our knowledge.
Methods: Sixty-three cases aged 50 or older with unilaterally
affected macular diseases were included. Thirty-five cases (54%)
were affected by neovascular age-related macular degeneration
(AMD). The unaffected eye was examined with adaptive optics
fundus camera (rtx1TM, Imagine Eyes, France) and high-resolution
retinal images with cone photoreceptor mosaic were obtained. After
excluding the eyes with any pathological findings within the area of
interest, averaged cone packing density and spacing at 2° superior
and 5° temporal to the fovea were calculated. Relationships between
these values and age, axial length, AMD or non-AMD in the affected
eye, drusen or pigment abnormality in the measured eye were
analyzed. Amongst 24 eyes were repeatedly examined for testing
repeatability.
Results: Patient age ranged 50 to 77, and axial length 21.7 to 27.5
mm. At 2° superior (n=51) and 5° temporal (n=53) to the fovea
average cone packing density were 19,200 ± 591 and 13,700 ± 386
(cells/mm2), and average cone spacing were 8.10 ± 0.14 and 9.56 ±
0.16 (μm), respectively. Axial length was significantly correlated
with the density and the spacing (-1,360 and -1,080 cells/mm2/mm,
0.32 and 0.42 μm/mm at 2° superior and 5° temporal, respectively).
Age was significantly correlated with the density at 5° temporal (-130
cells/ mm2/year), and this correlation was also observed when the
density was calculated as angular density (-9.4 cells/deg2/year). AMD
or non-AMD in the contralateral eye and degrees of drusen or
pigment abnormality in the measured eye was not significantly
associated with the density or the spacing. Intraclass correlation
coefficients (%) for the density and the spacing were 95 and 94 at 2°
superior, 90 and 91 at 5° temporal, respectively.
Conclusions: Axial length and age were significantly correlated with
cone photoreceptor distribution in aged patients. Patient’s
background disease or degrees of drusen or pigment abnormality
might not affect them. Influence of axial length and age should be
considered when analyzing cone distribution in aged patients.
Commercial Relationships: Ryo Obata, None; Xue Tan, None;
Kayo Kure, None; Frida Rosander, Imagine Eyes (R); Yasuo
Yanagi, None
Support: Grant-in-Aid for Young Scientists (B) 24791837 from
Ministry of Education,Culture,Sports,Science and Technology-Japan
Program Number: 3440 Poster Board Number: C0161
Presentation Time: 11:00 AM - 12:45 PM
Reproducibility of photoreceptor imaging by Adaptive Optics
Retinal Camera
Mélanie Bidaut-Garnier1, Mathieu Flores1, Perle TUMAHAI1,
meillat mathieu1, Guillaume Debellemaniere1, Marc Puyraveau2,
Bernard Y. Delbosc1, Michel Montard1, Maher Saleh1. 1Department
of Ophthalmology, University Hospital of Besançon, Besançon,
France; 2Methodology center, Besançon, France.
Purpose: To report the reproducibility and the repeatability of
photoreceptor imaging in healthy human eyes, using the RTx-1™
Adaptive Optics (AO) Retinal Camera, (Imagine Eyes, Orsay,
France) and AOdetect v0.1 cone counting software.
Methods: Three healthy emmetropic adults of 30, 42 and 42 years
old, were imaged. Mean cone density (cells/mm2) at a fixed distance
from the fovea (0.3 x 0.3 degree square located at 1° temporally),
spacing between cells (µ) and percentage of hexagonal cells
calculated on Voronoi diagrams, were also measured using the
proprietary software of the device. Intersession repeatability was
assessed by imaging both eyes of each subject, 5 consecutive days,
by the same operator. Intrassession repeatability was assessed by
comparing 10 consecutive acquisitions, obtained by the same
operator from the right eye of each subject. Inter-operator variability
was evaluated by comparing the images acquired by three different
operators. The cone counts were blind measured by 2 graders using
AOdetect v0.1. Pearson Coefficient (r) and coefficients of variation
(COVs) were calculated.
Results: The mean cone counts were 25475 ± 2983/mm2 and 26396
±3174 cells/mm2 for the first and the second grader, respectively (t
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
test, p <0.05). All the parameters evaluated were highly reproducible:
Pearson's r reached 0.90 (CI 95%: 0.84; 0.94) between both graders
and 0.96 (CI 95%:0.57 ; 0.96) for the inter-operator variability. The
intra-session and intersession COVs were 6% and 4%, respectively.
The measurements of percentage of hexagonal cells and spacing
between cells also varied in the same proportion (COV range from 3
to 9 %).
Conclusions: Photoreceptor counts using the RTx-1™ Adaptive
Optics Retinal Camera showed good reproducibility and repeatability
in normal human eyes. Further studies on the use of AO in the normal
clinical setting are needed.
Commercial Relationships: Mélanie Bidaut-Garnier, None;
Mathieu Flores, None; Perle TUMAHAI, None; meillat mathieu,
None; Guillaume Debellemaniere, None; Marc Puyraveau, None;
Bernard Y. Delbosc, None; Michel Montard, None; Maher Saleh,
None
Program Number: 3441 Poster Board Number: C0162
Presentation Time: 11:00 AM - 12:45 PM
Analysis of the Photoreceptor Mosaic in Patients with Each Stage
of Dry Age-Related Macular Degeneration (AMD): Cone Density
and Spacing as Image-Based Biomarkers
Adam Boretsky1, Faraz Khan1, Frederik J. van Kuijk2, Massoud
Motamedi1. 1Center for Biomedical Engineering, Univ of Texas
Medical Branch, Galveston, TX; 2Ophthalmology and Visual
Neuroscience, University of Minnesota, Minneapolis, MN.
Purpose: To use high resolution imaging to objectively measure
photoreceptor density and spacing in patients with dry age-related
macular degeneration (AMD).
Methods: A custom built adaptive optics confocal scanning laser
ophthalmoscope (AO-SLO) was used to acquire high resolution
reflectance images of the macular cone photoreceptor mosaic in 20
patients comprising each category of dry AMD. An 830 nm
Superluminescent diode (SLD) was used for both image acquisition
and wavefront sensing. Photoreceptor mosaics were generated by
automated registration and averaging of multiple images from video
sequences. Particular emphasis was placed on macular disruption
associated with the formation of drusen observed using fundus
photography and spectral domain optical coherence tomography (SDOCT). We used an automated algorithm to identify individual
photoreceptors and calculate local density values. Additionally, we
performed Delaunay triangulation to characterize the mean spacing
(center-to-center) of the cone photoreceptors within 0.25° x 0.25°
subsets of each mosaic.
Results: Photoreceptor density measurements varied greatly
depending on the retinal eccentricity and were heavily influenced by
the presence of vasculature and pathology. Segmenting the image
into small regions of interest (ROIs) enabled us to differentiate
between decreased photoreceptor density due to vasculature versus a
reduction in cones due to drusen or geographic atrophy. This data
was used to generate heatmaps of the local photoreceptor density.
Mean cone spacing was also measured for each ROI to identify areas
with increased spacing above one standard deviation from the mean.
Conclusions: Cone photoreceptor density and spacing have the
potential to be used as image-based biomarkers of AMD. Objective
analysis of the photoreceptor mosaic in patients with dry AMD may
provide an additional metric to assess disease progression and
establish a correlation between photoreceptor loss and a decline in
visual function. Additionally, AO-SLO may offer insight into the
efficacy of emerging dry AMD therapies.
Analysis of the local variations in the photoreceptor mosiac was
performed to help identify areas of decreased cone density and an
increase in photoreceptor spacing in patients with dry age-related
macular degeneration.
Commercial Relationships: Adam Boretsky, None; Faraz Khan,
None; Frederik J. van Kuijk, None; Massoud Motamedi, None
Support: The Wagner AMD Fund, Research to Prevent Blindness
(RPB), Beckman Initiative for Macular Research (BIMR)
Program Number: 3442 Poster Board Number: C0163
Presentation Time: 11:00 AM - 12:45 PM
High Resolution Imaging with Adaptive Optics in Patients with
Vogt-Koyanagi Harada Disease
Kiyoko Gocho, Sachiko Kikuchi, Takenori Kabuto, Hisatomo
Takahashi, Shuhei Kameya, Kunihiko Yamaki, Hiroshi Takahashi.
Ophthalmology, Nippon Med Univ, Chiba Hokusoh Hosp, Inzai,
Japan.
Purpose: To report the findings of en face adaptive optics (AO)
fundus imaging in eyes with Vogt-Koyanagi-Harada disease (VKH)
patients.
Methods: The macular region of five eyes from different stage of
four VKH patients with a mean age of 39 (range 21-60) were imaged
using both an infrared AO camera (rtx1™, Imagine Eyes, France)
and spectral-domain optical coherence tomography (SD-OCT Cirrus™, Carl Zeiss Meditec, Germany). AO images were analyzed
for cone density at 600μm and 1200μm nasal from the foveola. The
data acquired from the VKH patients was then compared to that
acquired from the eyes of 21 healthy volunteers with a mean age of
36 years (range 20-57) at the same eccentricities.
Results: The mean cone densities in healthy retinas were 2.11±0.37
x104 and 1.70±0.31 x104 cones/mm2 at eccentricities 600μm and
1200μm respectively.
One acute phase VHK patient was presented after 2 weeks from the
onset, diagnosed with serous retinal detachment (SRD) and treated
using steroid pulse treatment, underwent AO and SD-OCT at followup visits over 16th weeks. Analysis of the AO images enabled us to
determine that the cone density at the 4th, 5th, 13th and 16th week
from onset was 1.17x104, 0.78x104, 1.16x104 and 2.21x104
cones/mm2 at 600μm respectively, and 0.95 x104, 1.02 x104, 1.54
x104 and 1.61 x104 cones/mm2 at 1200μm respectively. At 16th
week, even the cone density of the patient was within the range of the
standard deviation of healthy volunteers, patchy dark areas with
decreased cone were observed. OCT showed recovery from SRD, but
hypo-reflectance in the cone outer segment tip (COST) line. Another
patient who was treated with steroid pulse treatment just after the
onset cured SRD, the COST line showed normal reflectance and AO
cone counting was within normal range of healthy volunteers at both
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
600μm and 1200μm. In two very late stage patients with sunset-glow
fundus at more than 2 years after the onset, analysis of AO showed an
irregularity in cone density at both 600μm and 1200μm eccentricities,
even though patients’ visual acuity were better than 20/20.
Conclusions: We have found that the photoreceptor damage remain
longer even after serous retinal detachment was resolved with OCT in
the convalescent and chronic stage VKH patients. Combined
examinations using AO and SD-OCT may be useful in better
understanding and managing the ophthalmic consequences of VHK
disease.
Commercial Relationships: Kiyoko Gocho, None; Sachiko
Kikuchi, None; Takenori Kabuto, None; Hisatomo Takahashi,
None; Shuhei Kameya, None; Kunihiko Yamaki, None; Hiroshi
Takahashi, None
Program Number: 3443 Poster Board Number: C0164
Presentation Time: 11:00 AM - 12:45 PM
Spectral-Domain Optical Coherence Tomographic Findings in
Acute Zonal Occult Outer Retinopathy (AZOOR)-complex at
Initial Visit to the Hospital
Yoshitsugu Matsui1, Mai Miyata1, Hisashi Matsubara1, Shinji Ueno2,
Shu Kachi2, Yasuki Ito2, Hiroko Terasaki2, Mineo Kondo1.
1
Opthalmology, Mie University Graduate School of Medicine, Tsu,
Japan; 2Opthalmology, Nagoya University Graduate School of
Medicine, Nagoya, Japan.
Purpose: To study outer retinal structural changes in acute zonal
occult outer retinopathy (AZOOR)-complex by using spectraldomain optical coherence tomography (SD-OCT) at the initial visit to
the hospital.
Methods: Twenty-two eyes of 22 patients (four male and 18 female;
age, 19-69) with AZOOR-complex, whose periods from symptom
onset to initial visit to the hospital were within six months, were
included in this study. The continuity of the external limiting
membrane (ELM), photoreceptor inner/outer segment (IS/OS)
junction, and cone outer segment tip (COST) were evaluated using
SD-OCT at their initial visit to the hospital. These three lines were
divided into three categories of “continuous”, “discontinuous” and
“absent”.
Results: At the retinal area of visual field defects, the ELM was
continuous in eight eyes, discontinuous in five eyes, and absent in
nine eyes. The IS/OS junction was continuous in one eye,
discontinuous in nine eyes, and absent in 12 eyes. The COST line
was absent in all 22 eyes. In thee of 22 eyes, well-demarcated hyperrefractive materials were present between the retinal pigment
epithelium (RPE) and ERM, and these materials gradually
disappeared within three months after the initial visit.
Conclusions: The SD-OCT findings in AZOOR-complex at the
initial visit were variable. The structure of ELM was most likely to be
preserved, and COST line most severely affected. Our findings
supported the idea that outer retinal structure was more vulnerable at
the early stages of AZOOR-complex.
Commercial Relationships: Yoshitsugu Matsui, None; Mai
Miyata, None; Hisashi Matsubara, None; Shinji Ueno, None; Shu
Kachi, None; Yasuki Ito, None; Hiroko Terasaki, None; Mineo
Kondo, None
SongEun Lee1, Sung Pyo Park1, 2, Eun Jin Bae2, Stephen H. Tsang1,
Stanley Chang1. 1Ophthalmology, Harkness Eye Institute, Columbia
University, New York, NY; 2Ophthalmology, Kangdong Sacred
Heart Hospital, Hallym University Medical Center, Seoul, Republic
of Korea.
Purpose: To evaluate structural damage of photoreceptors in a
patient with chloroquine/hydroxychloroquine maculopathy and the
role of adaptive optics scanning laser ophthalmoscopy in screening of
chloroquine/hydroxychloroquine maculopathy
Methods: A 53-year-old Asian woman who had been treated with
hydroxychloroquine and chloroquine for lupus erythematosus,
developed bull's eye retinopathy. Humphrey visual field, fundus
autofluorescence, and adaptive optics scanning laser ophthalmoscopy
were performed. The area with disrupted cone in AO-SLO images
were matched with visual field test results.
Results: Adaptive optics scanning laser ophthalmoscopy (AO-SLO)
showed patch cone mosaic lesions, where cones were missing or lost.
Additionally, cones that were present were asymmetrical in size and
shape and varied in brightness. Disrupted cone AO-SLO images were
matched with visual field test results, and functional deficits were
given a precise location on the montage. This allowed functional
changes (on HVF) to be correlated with histological findings.
Conclusions: In the present study, bull’s eye maculopathy developed
as a result of chronic use of antimalarial agents. The patient was
studied with various imaging techniques, including AO-SLO. We
demonstrated not only the disrupted microarchitecture of the
photoreceptors but also a correlation between functional and
structural defects associated with chloroquine retinopathy. The
adaptive optics scanning laser ophthalmoscopy will provide better
understanding of retinal damages in antimalarial agent-associated
retinopathy.
Program Number: 3444 Poster Board Number: C0165
Presentation Time: 11:00 AM - 12:45 PM
Evidence of Retinal Damage in Chloroquine/Hydroxychloroquine
Maculopathy as Revealed by High Resolution Imaging: A Case
Report Utilizing Adaptive Optics Scanning Laser
Ophthalmoscopy
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: SongEun Lee, None; Sung Pyo Park,
None; Eun Jin Bae, None; Stephen H. Tsang, None; Stanley
Chang, Alcon Laboratories (C), Alimera Sciences (C)
Program Number: 3445 Poster Board Number: C0166
Presentation Time: 11:00 AM - 12:45 PM
Adaptive Optics Scanning Laser Ophthalmoscopy and High
Resolution Imaging in Autosomal Dominant Retinitis Pigmentosa
Caused by a Novel PRPF31 Nonsense Mutation
Jessica I. Morgan1, 2, Meera Sivalingam1, Grace K. Han1, Albert M.
Maguire1, 2, Brian J. Forbes1, 2, Xiaowu Gai3, Eric A. Pierce4, Jean
Bennett1, 2, Daniel C. Chung1, 2. 1Ophthalmology, University of
Pennsylvania, Philadelphia, PA; 2Ophthalmology, Children's Hospital
of Philadelphia, Philadelphia, PA; 3Molecular Pharmacology and
Therapeutics, Loyola University Chicago, Chicago, IL; 4Ocular
Genomics Institute, Department of Ophthalmology, Massachusetts
Eye and Ear Infirmary, Harvard Medical School, Boston, MA.
Purpose: To study cone photoreceptor density and retinal
ultrastructure in autosomal dominant retinitis pigmentosa (adRP)
using adaptive optics scanning laser ophthalmoscopy (AOSLO) and
spectral domain optical coherence tomography (OCT) and to
compare the results with clinical findings and genetic
characterization.
Methods: Exome sequencing was carried out in individuals negative
for previously known mutations causing adRP. The DNA variants
were confirmed in CLIA labs. Patients underwent ophthalmic
examination, visual acuity (VA), Humphrey and Goldman visual
field testing. Retinal images at several locations within 1.5mm of
fixation were obtained using an AOSLO developed by Canon, Inc.
Infrared and color fundus photos, OCT and autofluorescence (AF)
images were also obtained.
Results: For all patients, peripheral pigmentary clumping and bone
spicule retinopathy were observed on ophthalmic examination. One
individual was followed in the clinic for over 35 years. His VA went
from 20/200 at age 36 to 20/500 OD and hand motion OS at age 73.
VA was reduced: 20/60, 20/40, 20/25 for patients aged 44, 16 and 11
respectively in the second family. Goldman visual fields showed
restricted peripheral fields with remaining central vision. Humphrey
visual field showed no reduction of visual threshold in the central
retina for the 16 and 11 y.o., but reduced sensitivity in the 44 y.o.
OCT for the 11 y.o. revealed central intact photoreceptors with
peripheral thinning. The 16 y.o. had macular edema OU. AF revealed
a hyper-AF ring within the macula region. As well, the 44 y.o.
exhibited clumps of hypo-AF in the periphery corresponding to
regions of degenerated retinal pigment epithelium. AOSLO imaging
of the central macula revealed intact cone photoreceptor mosaics, and
cone density fell within normal limits. Results of genetic testing (in
both families) revealed a PRPF31 c.1060 C>T mutation
(p.Arg354Stop) which segregated with the phenotype and was
consistent with the diagnosis of adRP.
Conclusions: Here we report a novel PRPF31 mutation causing
adRP in two apparently unrelated families. AOSLO imaging allows
visualization of the cone mosaic within the remaining central retina in
patients with adRP. AOSLO in combination with other imaging
modalities will be useful for studying the mechanisms of disease
progression for degenerations including adRP.
Commercial Relationships: Jessica I. Morgan, Canon (F), Optos
(F); Meera Sivalingam, Canon Inc (F); Grace K. Han, Canon Inc.
(F), Optos PLC (F); Albert M. Maguire, None; Brian J. Forbes,
None; Xiaowu Gai, None; Eric A. Pierce, None; Jean Bennett,
Gensight Biologics (S); Daniel C. Chung, None
Support: Earl and Brenda Shapiro Leber's Congenital Amaurosis
Research Initiative, Foundation Fighting Blindness, Penn Genome
Frontiers Institute, National Institute of Health EY019861,NIH
EY012910, F.M. Kirby Foundation, Mackall Trust, Reserach to
Prevent Blindness, Canon, Inc. Kathleen Marshall and Sarah
McCague.
Program Number: 3446 Poster Board Number: C0167
Presentation Time: 11:00 AM - 12:45 PM
Cone Abnormalities in Fundus Albipunctatus Associated with
RDH5 Mutation Using Adaptive Optics Scanning Laser
Ophthalmoscopy
Sotaro Ooto, Yukiko Makiyama, Masanori Hangai, Ken Ogino,
Norimoto Gotoh, Akio Oishi, Nagahisa Yoshimura. Ophthalmology
& Visual Sciences, Kyoto University Graduate School of Medicine,
Kyoto, Japan.
Purpose: To asses macular photoreceptor abnormalities in eyes with
fundus albipunctatus associated with RDH5 mutation using adaptive
optics scanning laser ophthalmoscopy (AO-SLO).
Methods: Ten eyes of 5 patients with fundus ablipunctatus
associated with RDH5 mutation (4 men and 1 woman from 4
families; mean age, 29.6 y; range, 15-64y) and 11 eyes of 11
volunteers underwent a full ophthalmologic examination, color
fundus photography, microperimetry, spectral-domain optical
coherence tomography (SD-OCT), and imaging with a prototype AOSLO system. Cone density and spatial organization of the cone
mosaic were assessed using AO-SLO images.
Results: Four patients from 3 families had the same mutation in
RDH5, (c.928delC/ insGAAG). One patient had another mutation in
RDH5 (c.718delG), which was the novel mutation of RDH5 gene.
AO-SLO revealed the presence of small patchy dark areas
representing cone loss in the macula of all eyes with fundus
albipunctatus, which was true even in eyes for which SD-OCT did
not reveal any visible defects in the photoreceptor layer. AO-SLO
and SD-OCT showed microhole-like photoreceptor defect in the
fovea in 1 eye. In eyes with fundus albipunctatus, cone density was
significantly lower in each area at 0.5 mm and 1.0 mm from the
center of the fovea compared to normal eyes (P = 0.014 for both). At
0.5 mm and 1.0 mm from the center of the fovea, a decreased number
of cones had 6 neighbors in eyes with fundus albipunctatus (P =
0.022 and 0.002). The ratio of observed mean nearest neighbor
distance (NND) for each subject divided by expected NND
(computed assuming a perfectly hexagonal lattice of cones with a
density equal to that observed for a given subject) was significantly
lower for eyes with fundus albipunctatus than for normal eyes at 0.5
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
mm and 1.0 mm from the center of the fovea (P=0.007 and 0.001).
Mean retinal sensitivity was significantly lower in the area with white
dots, compared with area without them (11.2 ± 2.6 dB and 13.9 ± 3.1
dB, P<0.001).
Conclusions: Macular cone density is decreased and the regularity of
the macular cone mosaic spatial arrangement is disrupted in eyes with
fundus albipunctatus, even when SD-OCT shows normal
photoreceptor layer. AO-SLO imaging is a sensitive quantitative tool
for detecting photoreceptor abnormalities in eyes with fundus
albipunctatus.
Commercial Relationships: Sotaro Ooto, None; Yukiko
Makiyama, None; Masanori Hangai, Topcon (F), Canon (F), Nidek
(C), Topcon (C); Ken Ogino, None; Norimoto Gotoh, None; Akio
Oishi, None; Nagahisa Yoshimura, Canon (C), Canon (F), Nidek
(C), Topcon (F), PCT/JP2011/073160 (P)
Support: Innovative Techno-Hub for Integrated Medical Bioimaging of the Project for Developing Innovation Systems, from the
Ministry of Education, Culture, Sports, Science and Technology
(MEXT), Japan, and Canon Inc.
Program Number: 3447 Poster Board Number: C0168
Presentation Time: 11:00 AM - 12:45 PM
Adaptive Optics Scanning Laser Ophthalmoscopy and MultiModality Clinical Imaging in a Patient with Gyrate Atrophy
Eva S. Klinman1, Albert M. Maguire2, Grace K. Han2, Jessica I.
Morgan2. 1Neuroscience, University of Pennsylvania School of
Medicine, Philadelphia, PA; 2Scheie Eye Institute Department of
Ophthalmology, University of Pennsylvania School of Medicine,
Philadelphia, PA.
Purpose: Characterize retinal structure and function in a patient with
gyrate atrophy using high resolution clinical imaging and adaptive
optics scanning laser ophthalmoscopy (AOSLO).
Methods: A patient with gyrate atrophy was imaged at several retinal
locations within 1.5mm of fixation using an AOSLO developed by
Canon Inc. Infrared (IR) fundus photography, spectral domain optical
coherence tomography (OCT), and autofluorescence (AF) images
were also obtained. Wide field SLO reflectance and AF images were
acquired using the Optos P200C SLO. Retinal sensitivity was
assessed by microperimetry at the locations corresponding to AOSLO
images.
Results: The patient had a peripheral ring of degenerated retina, with
central preservation of both retinal pigment epithelium (RPE) and
photoreceptors. Wide field SLO imaging also revealed retinal
preservation in the far periphery. Within the ring of degeneration, the
retina displayed hypo-AF with RPE disruption. Microperimetry
displayed vision loss in this region. Choroidal vessels were visible on
AOSLO in the region of degeneration; no cones were observed in
these areas. In contrast, the spared central retinal on fundus
photography corresponded to regions with preserved AF. AOSLO
imaging confirmed cones in this region, including near the border of
healthy and degenerated retina. Cone density was normal throughout
most of the preserved retina, with slightly lower density at regions
bordering degenerated retina. Photoreceptor and RPE cell layers
appeared intact on OCT in the region of the central macula, although
there were disruptions of the retinal architecture including cysts.
Abnormal hyper-reflective patches were observed at multiple levels
of retinal depth anterior to the photoreceptors, in multiple locations
including the fovea. At these locations, the patient had slightly
reduced light perception, as assessed by microperimetry.
Conclusions: This patient with gyrate atrophy maintained
photoreceptors and RPE cells centrally, although both are lost in a
ring pattern in the periphery. Cones are visible with AOSLO until the
point of RPE loss, as seen with AF. Gyrate atrophy is associated with
findings in multiple levels of the retina, visible by both AOSLO and
OCT. AOSLO imaging in combination with other imaging modalities
will be useful to monitor disease progression, and provide a measure
of cone loss over time in patients with gyrate atrophy.
Commercial Relationships: Eva S. Klinman, Canon Inc (F), Optos,
PLC (F); Albert M. Maguire, None; Grace K. Han, Canon Inc. (F),
Optos PLC (F); Jessica I. Morgan, Canon (F), Optos (F)
Support: Earl and Brenda Shapiro Leber's Congenital Amaurosis
Research Initiative, Foundation Fighting Blindness, Choroideremia
Research Foundation, NIH Grant EY019861, F.M. Kirby Foundation,
Research to Prevent Blindness, Mackall Trust, Canon Inc.
Program Number: 3448 Poster Board Number: C0169
Presentation Time: 11:00 AM - 12:45 PM
Cellular Imaging Demonstrates Genetic Mosaicism in
Heterozygous Carriers of an X-Linked Ciliopathy Gene
Sung Pyo Park1, 2, In Hwan Hong2, Winston Lee1, Marcela
Marsiglia1, Takeshi Kitamura4, Stephen H. Tsang1, 3, Stanley Chang1.
1
Ophthalmology, Columbia University Medical Center, New York,
NY; 2Ophthalmology, Kangdong Sacred Heart Hospital, Hallym
University Medical Center, Seoul, Republic of Korea; 3Pathology &
Cell Biology, Columbia University Medical Center, New York, NY;
4
Canon Inc., Tokyo, Japan.
Purpose: The purpose of this study was to evaluate structural
characteristics in 5 female obligate carriers of XLRP by using
multimodal non-invasive imaging methods, including AO-SLO.
Methods: Five patients and 18 controls having similar age and
refractive error with patients were investigated. The XLRP carrier
state was diagnosed by clinical and genetic analyses. All participants
underwent a complete ophthalmic examination that included fundus
color photography, IR and FAF imaing, SD-OCT and ERG. High
resolution image of cone cells and direct measurement of the number
of cones were investigated by AO-SLO equipped with a dual liquid
crystal on silicon modulator. For the number of cones, we acquired 2
kinds of parameters: cone count by manual estimation and cone
density by automated estimation.
Results: 3 patients were confirmed with mutations in RPGR gene
and the rest of the patients were diagnosed as carriers by clinical
investigation and pedigree analysis. Regarding AO-SLO
examination, compared to normal eyes, some images of each XLRP
patient showed normal appearance of cone cell with a compact
arrangement. However, cone cells in several areas showed irregular
pattern and were of variable asymmetrical sizes and shapes. There
were some dark areas where the cone cells were damaged or lost so
that less compact distribution of cone cells than controls was noted.
Statistical analysis between 5 carriers and controls revealed that the
number of cone cells in these images was significantly decreased.
When we compared the average number of cone cells counted using
either method, among total 60 areas obtained from 5 carriers, overall
29 areas showed cone counts or densities lower than 1 standard
deviation from the controls and the agreement between the 2 different
methods was up to 82.8%.
Conclusions: In all carriers, qualitative and quantitative analyses by
AO-SLO imaging revealed a mosaic pattern of cone disruption, even
in the absence of visual symptoms, normal visual acuity, normal
macular thickness and mildly subnormal full-field cone ERG
findings. Since the technique is sensitive to the level of a single cone,
the ability to visualize the cone cells in vivo should be especially
useful in other retinal diseases. Further investigation of XLRP
carriers may yield insight into how cone structures change over time
and ultimately enable understanding of the role of RPGR and RP2 in
live human patients.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Sung Pyo Park, None; In Hwan
Hong, None; Winston Lee, None; Marcela Marsiglia, None;
Takeshi Kitamura, Canon U.S.A., Inc. (E); Stephen H. Tsang,
None; Stanley Chang, Alcon Laboratories (C), Alimera Sciences (C)
Program Number: 3449 Poster Board Number: C0170
Presentation Time: 11:00 AM - 12:45 PM
Disruption of the Human Cone Photoreceptor Mosaic from a
Defect in NR2E3 Transcription Factor Function
Frank S. Siringo1, Sung Pyo Park1, 2, In Hwan Hong2, Stephen H.
Tsang1, 3, Winston Lee1, Jason Horowitz1, Rando Allikmets1, Stanley
Chang1, Suzanne Yzer4, 1. 1Ophthalmology, Columbia University
Medical Center, Fort Lee, NJ; 2Ophthalmology, Kangdong Sacred
Heart Hospital, Hallym University Medical Center, Seoul, Republic
of Korea; 3Pathology & Cell Biology, Columbia University Medical
Center, New York, NY; 4Ophthalmology, Rotterdam Eye Hospital,
Rotterdam, Netherlands.
Purpose: Enhanced S-cone syndrome is an orphan disease caused by
mutations in the NR2E3 gene, which results in an increased number
of S-cones overpopulating the retina. Although the characteristic
onset of enhanced S-cone syndrome can be well documented by
current ophthalmic imaging modalities, techniques such as spectral
domain optical coherence tomography (SD-OCT) and scanning laser
ophthalmoscopy (SLO) fail to provide sufficient details regarding the
microstructure of photoreceptors in retinal diseases. Adaptive optics
(AO) provides a unique opportunity to analyze the effects of genetic
mutations on photoreceptors by compensating for aberrations in the
human eye.
Methods: 3 eyes of 3 patients with enhanced S-cone syndrome were
studied by clinical examination, genetic screening, fundus
autofluorescence (FAF) imaging, SD-OCT, and electroretinography
(ERG). Cone mosaic imaging was accomplished by an AO-SLO
equipped with a dual crystal on silicon spatial light modulator.
Qualitative image analyses and genetic findings were investigated in
each patient.
Results: The diagnosis was confirmed by ERG and genetic analysis.
Two disease-causing mutations in the NR2E3 gene were identified on
2 study patients, as well as a novel mutation (202 A>G, S68G) in the
third. Fundus photograph, FAF and SD-OCT found a rosette-like
lesion within the mid-periphery along the vascular arcades of the
retina. In all AO-SLO images, sparse distribution and asymmetric
size of cone mosaic pattern were found within central retina. There
were regions of dark space between groups of photoreceptors,
distinguishable from shadowing and artifacts.
Conclusions: AO-SLO provided an in-depth window into the retina
of enhanced S-cone syndrome patients beyond the ability of other
current imaging modalities. Dark lesions within the central retina
contain structurally dysfunctional cones, which account for retinal
mosaic disorganization and may predispose affected areas to other
abnormalities such as rosettes. AO-SLO can be an efficient
diagnostic tool in clinics for examining cellular-level pathologies in
various retinal dystrophies.
Commercial Relationships: Frank S. Siringo, None; Sung Pyo
Park, None; In Hwan Hong, None; Stephen H. Tsang, None;
Winston Lee, None; Jason Horowitz, None; Rando Allikmets,
None; Stanley Chang, Alcon Laboratories (C), Alimera Sciences
(C); Suzanne Yzer, None
Program Number: 3450 Poster Board Number: C0171
Presentation Time: 11:00 AM - 12:45 PM
Cellular Imaging after Remission from Diabetic Macular Edema
Ching-Lung Chen1, 2, Sung Pyo Park1, 3, Takeshi Kitamura4, Stanley
Chang1. 1OPhthalmology, Columbia university medical center, New
york, NY; 2Department of Ophthalmology, Chang Gung Memorial
Hospital, Chiayi, Taiwan; 3Department of Ophthalmology, Hallym
University Medical Center, Seoul, Republic of Korea; 4Healthcare
Solutions Division, Canon, New york, NY.
Purpose: To evaluate structural differences in the patient recovered
from diabetic macular edema by using multimodal non-invasive
imaging methods, including adaptive optics scanning laser
ophthalmoscopy (AO-SLO).
Methods: An eighty-one year old Indian male suffered from diabetic
retinopathy with macular edema. Following resolution of the macular
edema in one eye, the visual acuity did not recover fully. The patient
underwent a complete ophthalmic examination that included fundus
color photography, IR imaging, OCT. High-resolution image of cone
structure and measurement of the number and shape of cones was
investigated by AO-SLO. After 14 months, the patient received the
same examination. For the accurate analysis of condition of cone
cells, we focused on the same portions of macula by manual
estimation.
Results: OCT revealed no macular edema with a central thickness of
231um in his right eye and central thickness of 289 um with inferior
0.5mm local edema of 352um in his left eye. 14 months later, OCT
showed no specific difference on the right eye with central thickness
of 229 um, but the central and inferior 0.5mm thickness had declined
to 275 um and 339 um. Central vision metamorphopsia had almost
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
subsided and the visual acuity had improved. At the 14-month follow
up visit, the density of cone photoreceptors, as measured by AO-SLO
examination, had only decreased slightly, but the cellular hexagon
rate declined remarkably in both eyes on average. Compared to the
initial inferior local edema of 0.5 mm in the left eye, the cellular
hexagon rate decreased from 36.4% to 22.8% at the 14-month followup exam.
Conclusions: The analyses by AO-SLO imaging revealed only a
slightly lower density of cone cells, but the cellular hexagon rate
decreased in both eyes as compared to the examination 14 months
prior. The cellular hexagon rate of previous edema area of left eye
showed marked decline. The macular edema from long-term diabetic
macular edema had subsided, based on the OCT image which showed
flatter retina. The visual acuity had also improved, but the detail
density and morphology still remained and even worsened. Longterm edema, diabetic retinopathy, or aging might be the risk factors.
However, AO-SLO is more sensitive to the level of a single cone cell,
and the ability to visualize the cone cells in vivo should be used in a
larger diabetic retinopathy survey and may also be useful for studying
other retinal diseases as well.
Commercial Relationships: Ching-Lung Chen, None; Sung Pyo
Park, None; Takeshi Kitamura, Canon U.S.A., Inc. (E); Stanley
Chang, Alcon Laboratories (C), Alimera Sciences (C)
Support: None in the Support field
Program Number: 3451 Poster Board Number: C0172
Presentation Time: 11:00 AM - 12:45 PM
Photoreceptor Structure in Presumed Non-Neoplastic
Autoimmune Retinopathy
David B. Kay1, Robert F. Cooper2, Drew H. Scoles3, Fouad R.
Zakka1, Vesper Williams1, Alfredo Dubra1, 4, Joseph Carroll1, 4,
Kimberly E. Stepien1. 1Department of Ophthalmology, Medical
College of Wisconsin, Milwaukee, WI; 2Department of Biomedical
Engineering, Marquette University, Milwaukee, WI; 3Department of
Biomedical Engineering, University of Rochester, Rochester, NY;
4
Department of Biophysics, Medical College of Wisconsin,
Milwaukee, WI.
Purpose: Autoimmune retinopathies (AIR) are rare diseases,
sometimes associated with systemic neoplasms, in which anti-retinal
antibodies lead to cone and rod dysfunction. Patients present with
progressive, bilateral, painless vision loss despite normal clinical
fundus appearance, making diagnosis difficult. SD-OCT has shown
outer retinal abnormalities and decreased macular thickness in AIR
patients. Adaptive optics scanning light ophthalmoscopy (AOSLO)
enables high-resolution imaging of the photoreceptor mosaic. This
study incorporates AOSLO into the comprehensive investigation of
individuals with AIR to evaluate its utility in improving the
characterization and management of AIR.
Methods: Three individuals with presumed non-neoplastic AIR who
presented with vision loss, normal fundus appearance and known
anti-retinal antibodies underwent a comprehensive ophthalmic
evaluation and multiple retinal imaging sessions over a 5 - 14 month
interval. Retinal appearance and lamination were assessed using
fundus photography and SD-OCT. The photoreceptor mosaic was
assessed using AOSLO.
Results: All three individuals had different anti-retinal antibody
combinations in serum, and presenting vision ranged from 20/40 to
20/100. Clinical and fundus photography evaluation confirmed
normal appearing fundus. SD-OCT revealed decreased central
macular thickness in two of the three patients, and focal disruption of
outer retinal lamination was seen at the fovea in all patients. This
disruption was also visible in the AOSLO images as a large
hyporeflective area at the fovea. In addition, AOSLO images
revealed significant reduction in parafoveal cone density in all three
subjects, with variable numbers of non-waveguiding cones
interspersed throughout the mosaic. This disruption was not
visualized on SD-OCT.
Conclusions: Both SD-OCT and AOSLO show outer retinal
structure changes associated with AIR not apparent on clinical
examination. However, AOSLO allows for assessment of
photoreceptor structure at a resolution not resolvable on SD-OCT.
AOSLO may prove to be a useful, noninvasive, highly accurate tool
to aid in diagnosis of AIR as well as monitoring progression and
treatment responses. Further study is needed to determine whether
AOSLO can be used to accurately track progression of photoreceptor
disruption in AIR over time.
Commercial Relationships: David B. Kay, None; Robert F.
Cooper, None; Drew H. Scoles, None; Fouad R. Zakka,
VitreoRetinal Surgery Foundation (F); Vesper Williams, None;
Alfredo Dubra, US Patent No: 8,226,236 (P); Joseph Carroll,
Imagine Eyes, Inc. (S); Kimberly E. Stepien, None
Support: VitreoRetinal Surgery Foundation, Research to Prevent
Blindness, NIH (UL1RR031973, EY017607, EY001931), Alcon
Research Institute, Burroughs Wellcome Fund
Program Number: 3452 Poster Board Number: C0173
Presentation Time: 11:00 AM - 12:45 PM
Cone photoreceptors at the fovea after serous retinal detachment
observed with adaptive optics fundus camera (rtx1)
Atsushi Hayashi, Tomoko Nakamura, Naoki Tojo, Tomoko Ueda,
Toshihiko Oiwake, Akio Miyakoshi, Hironori Ozaki. Ophthalmology,
University of Toyama, Toyama, Japan.
Purpose: Purpose: To examine recovery of cone photoreceptors in
the fovea after serous retinal detachment (SRD) in patients with
central serous chorioretinopathy (CSC) and Vogt-Koyanagi-Harada
disease (VKH) with an adaptive optics (AO) fundus camera and to
examine correlations between cone analyses and visual acuity.
Methods: Methods: Ten eyes of CSC and 4 eyes of VKH were
examined. After the SRD at the fovea was resolved with
photodynamic therapy or steroid therapy, photographs of cone
photoreceptors including the fovea were taken with an AO fundus
camera (rtx1, Imagine eyes, France). The area of 200µm X 200µm at
the fovea was chosen in the photograph of each eye and analyzed
with the manufacturer’s software. Analyses of cone density, cone
spacing, and voronoi domains were obtained and correlations
between visual acuity and cone analyses were examined. OCT was
obtained at the same time and length of the IS/OS line in the OCT
image was measured in the area of 200µm at the fovea.
Results: Results: Cone analyses showed that average cone density at
the fovea was 15363±4239, average cone spacing was 8.96±1.21μm,
and average voronoi domains was 36.9±4.1%. Average visual acuity
(logMAR) was 0.155±0.391. Average length of the IS/OS line in the
area of 200µm was 77.7±31.5%. Visual acuity and cone analyses
showed significant correlations. Cone density; rs= -0.698
(Spearman’s rank Correlation Coefficient), cone spacing; rs=0.663,
and voronoi domains; rs=-0.749. The length of IS/OS line and cone
density showed a significant correlation; rs=0.770.
Conclusions: Conclusions: Analyses of cone photoreceptors at the
fovea after SRD was resolved were significantly correlated with
visual acuity.
Commercial Relationships: Atsushi Hayashi, None; Tomoko
Nakamura, None; Naoki Tojo, None; Tomoko Ueda, None;
Toshihiko Oiwake, None; Akio Miyakoshi, None; Hironori Ozaki,
None
Program Number: 3453 Poster Board Number: C0174
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Presentation Time: 11:00 AM - 12:45 PM
Evaluation of cone density after retinal detachment surgery using
an Adaptive Optics camera
Maher Saleh, meillat mathieu, Mélanie Bidaut-Garnier, Perle
TUMAHAI, Guillaume Debellemaniere, Mathieu Flores, Michel
Montard, Bernard Y. Delbosc. Ophthalmology, University Hospital
of Besançon, Besançon, France.
Purpose: To assess macular cone photoreceptors density in human
eyes operated for retinal detachment (RD) and in contralateral
healthy eyes.
Methods: Patients operated for RD with macular involvement were
imaged using the RTX-1 Adaptive Optics (AO) device from Imagine
eyes™ (Orsay, France), 6 weeks after the surgery. Cone density
(cells/mm2) at a fixed distance from the fovea (1 °), spacing between
cells (µ) and percentage of hexagonal cells calculated on Voronoï
diagrams, were obtained using AO Detect v.0.1, the proprietary
software of the device. Group 1 represented the eyes with history of
RD and group 2 the contralateral eyes. Visual acuity (logMAR),
refraction, axial length (mm) and the thickness of the different
choroid and retinal layers (RPE, IS/OS, LME lines) imaged by SDOCT (Spectralis®, Heidelberg), were also compared to the cone
densities.
Results: Thirty eyes from 15 patients were studied. Visual acuities
decreased in group 1 (0.34 vs 0.1 in group 2, paired t test, p<0.05).
There was a reduction in cone density in group 1 (14368±4761/mm2)
compared to group 2 (19240±3894/mm2) (p=0.002). In group 1,
spacing between cones was increased (11.16±3.34 µ vs 8.65±1.95µ,
p=0.01), while the proportion of hexagonal cells was reduced
(36.11±5.29% vs. 42.08± 5.16 %, p=0.01). There was also a negative
correlation between overall cone densities and visual acuities
(R2=0.45). Cone density was also correlated to the thickness of the
RPE hyperreflective layer on OCT (R2= 0.21, p=0.02) but neither
with central macular thickness nor choroidal thickness.
Conclusions: Adaptive Optics allowed in vivo imaging of the
macular phoreceptors in eyes operated for RD. The cone density was
correlated to the visual acuity. OA could represent a valuable
prognostic tool after RD surgery.
Commercial Relationships: Maher Saleh, None; meillat mathieu,
None; Mélanie Bidaut-Garnier, None; Perle TUMAHAI, None;
Guillaume Debellemaniere, None; Mathieu Flores, None; Michel
Montard, None; Bernard Y. Delbosc, None
Program Number: 3454 Poster Board Number: C0175
Presentation Time: 11:00 AM - 12:45 PM
Recovery of photoreceptors in the macula of idiopathic choroidal
neovascularization observed with adaptive optics fundus camera
Tomoko Nakamura, Toshihiko Oiwake, Tomoko Ueda, Akio
Miyakoshi, Atsushi Hayashi. University of Toyama, Toyama, Japan.
Purpose: To observe recovery of photoreceptors in the macula of
idiopathic choroidal neovascularization (ICNV) patients and to assess
correlations between cone analyses and OCT images.
Methods: Three eyes of 3 patients with ICNV were studied. All
patient received intravitreal injections of 1.25mg bevacizumab (IVB).
After subretinal fluid was resolved, adaptive optics (AO) images
were obtained with rtx1TM (Imagine Eyes ,France) and cone
analyses were performed. Changes in OCT and visual acuity were
examined during the follow up.
Results: After subretinal fluid was resolved by IVB, decimal visual
acuity of all patients improved to 1.0. In AO images, cone
photoreceptors were not observed in the area with absent or disrupted
photoreceptor inner segment / outer segment (IS/OS) junction and
cone outer segment tips (COST) line in OCT images. In the area with
intact IS/OS junction and absent or disrupted COST line, cone
photoreceptors returned to be observed after IVB. Cone density, cone
spacing, and voronoi domains were improved with the recovery of
the COST line in OCT.
Conclusions: Recovery of cone photoreceptors in the macula of
ICNV patients after IVB was associated with changes in OCT
images.
Commercial Relationships: Tomoko Nakamura, None; Toshihiko
Oiwake, None; Tomoko Ueda, None; Akio Miyakoshi, None;
Atsushi Hayashi, None
Program Number: 3455 Poster Board Number: C0176
Presentation Time: 11:00 AM - 12:45 PM
High resolution cone photoreceptor imaging analysis of an occult
macular dystrophy patient with RP1L1 mutation
Shuhei Kameya1, Takenori Kabuto1, Sachiko Kikuchi1, Hisatomo
Takahashi1, Kiyoko Gocho1, Kunihiko Yamaki1, Hiroshi Takahashi2.
1
Ophthalmology, Chiba Hokusoh Hosp Nippon Med Sch, Inzai,
Japan; 2Ophthalmology, Nippon Medical School, Tokyo, Japan.
Purpose: To analyze cone photoreceptor degeneration by adaptive
optics (AO) fundus camera in a Japanese occult macular dystrophy
(OMD) patient with mutation in the RP1-like protein 1 (RP1L1)
gene.
Methods: An OMD patient with RP1L1 mutation (S1199C) and 20
normal volunteer underwent high resolution imaging analysis. Highresolution en face images were obtained using a flood-illumination
AO fundus camera (Imagine Eyes, Orsay, France). We have
statistically analyzed biomarker metrics (cone density, inter-cell
spacing) computed from the images. These metrics are analyzed from
the images obtained at 600 μm and 1200 μm from the fovea.
Results: The mean age of volunteers is 36.0±10.5 (range 20-57
years). The mean cone density of volunteers was 2.11±0.37 x 10 4
cones/mm2 at 600 μm from the fovea and 1.70±0.31 x 10 4 cones/mm2
at 1200 μm from the fovea. The mean inter-cell spacing of volunteers
was 7.73±0.81 μm at 600 μm from the fovea and 8.56±0.93 μm at
1200 μm from the fovea. The cone density of the right eye of the
patient was 4.72 x 103 cones/mm2 at 600 μm from the fovea and 3.04
x 103 cones/mm2 at 1200 μm from the fovea. The inter-cell spacing
of the right eye of the patient was 13.0 μm at 600 μm from the fovea
and 16.9 μm at 1200 μm from the fovea. The cone density and intercell spacing of the patient were outside the range of the both standard
deviation and 95% confidence intervals of normal volunteer.
Conclusions: We have analyzed high resolution images of a
Japanese OMD patient with RP1L1 mutation. An OMD patient
showed decreased cone density and increased inter-cell spacing at
both 600 μm and 1200 μm from the fovea. AO fundus camera and its
computed metrics analysis were useful to detect the changes in the
cone photoreceptors in OMD.
Commercial Relationships: Shuhei Kameya, None; Takenori
Kabuto, None; Sachiko Kikuchi, None; Hisatomo Takahashi,
None; Kiyoko Gocho, None; Kunihiko Yamaki, None; Hiroshi
Takahashi, None
370 Color Vision
Tuesday, May 07, 2013 2:45 PM-4:30 PM
TCC LL 4/5 Paper Session
Program #/Board # Range: 3705-3710
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 3705
Presentation Time: 2:45 PM - 3:00 PM
A psychophysical approach to spectral classification of single
cones in vivo
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
William S. Tuten1, Wolf M. Harmening2, Lawrence C. Sincich3,
Austin Roorda2. 1Vision Science, University of California, Berkeley,
Berkeley, CA; 2School of Optometry, University of California,
Berkeley, Berkeley, CA; 3Vision Sciences, University of Alabama at
Birmingham, Birmingham, AL.
Purpose: To distinguish L-cones from M- and S-cones
psychophysically in humans using an adaptive optics scanning laser
ophthalmoscope (AOSLO).
Methods: We used a multi-wavelength AOSLO to measure visual
sensitivity to cone-sized stimuli under L-cone isolating conditions in
two subjects with normal color vision. Increment thresholds were
measured at 1.5° eccentricity, and stimulus delivery to targeted cones
was achieved using high-speed retinal eye tracking. An image-based
measure of transverse chromatic aberration (TCA) was obtained and
used to ensure repeated stimulation of the cone of interest. The test
stimulus (λ = 711 nm) was a square which subtended 27 seconds of
arc (= 2.2 microns) on the retina. The background was comprised of
dim infrared light from the imaging beam, light leaking through the
acousto-optic modulator in the red stimulus channel, and an external
488 nm LED source viewed through a beam splitter. The luminances
of the red and blue backgrounds were 2.5 and 50 cd/m2, respectively.
Converting these luminances to cone contrasts, an L- versus M-cone
sensitivity ratio of 24-to-1 was expected. Stimulus intensity of the red
beam was controlled via 10-bit modulation and expressed as arbitrary
units (au) ranging from zero to 1. Thus, for L-cone thresholds greater
than 0.042 au, M- and S-cone thresholds would be predicted to lie
beyond the upper modulation limit of the stimulus beam (i.e., >1.0
au).
Results: Thresholds were measured for 88 cones in the two subjects.
The stimulus was readily visible in one group of cones (n = 59;
threshold = 0.55 ± 0.14SD au), and these were classified as candidate
L-cones. A second group of cones (n = 18) had thresholds above 1.0
au, with even the brightest stimulus being not visible. In these cones,
threshold values were normal when tested under achromatic
conditions, ruling out underlying dysfunction. In the remaining
cones, classification was ambiguous (n = 11). Finally, there were
multiple sites in each subject where thresholds from neighboring
cones yielded different spectral identities, supporting the notion that
the spatial accuracy of our psychophysical apparatus is on the order
of a single cone.
Conclusions: With combined retinal eye tracking, high-order
aberration correction, and TCA compensation, AOSLO can be used
to identify the spectral class of single cones in vivo with a
psychophysical approach.
Commercial Relationships: William S. Tuten, None; Wolf M.
Harmening, None; Lawrence C. Sincich, None; Austin Roorda,
US Patent #6890076 (P), US Patent #7118216 (P), UC Berkeley (P)
Support: EY007043; Irvin M. Borish-Essilor Ezell Fellowship; DFG
Ha 5323/2-1; EY021642; EY019566; Eyesight Foundation of
Alabama; EY014375
Program Number: 3706
Presentation Time: 3:00 PM - 3:15 PM
S-cone Electroretinograms in Old and New World Primates
Recorded Using Two Methods
James A. Kuchenbecker, Scott H. Greenwald, Maureen Neitz, Jay
Neitz. Ophthalmology, University of Washington, Seattle, WA.
Purpose: Using the exchange of two lights that lie along a tritan line
makes it possible to isolate pure S-cone electroretinogram (ERG)
signals. Here, we compare the pure S-cone ERG using silent
substitution with a method in which “S-cone ERGs” are obtained to
short wavelength flashes in the presence of intense long wavelength
adaptation. Results were compared in an Old World (OW) primate
(baboon) and a New World (NW) primate (squirrel monkey) to
evaluate the possibility of differences in S-cone circuitry between the
two primate groups that have been proposed to explain reported
neuroanatomical differences.
Methods: An LED Ganzfeld system was used (Q450; Roland
Consult, modified by replacing 450 with a 420 nm LED). A tritan
pair of lights was alternated at 1 Hz with a 50% duty cycle. A tritan
pair that completely isolated S-cone responses for each individual
animal was found by making small adjustments to the relative
intensities of the two lights while taking advantage of the striking
differences in the temporal characters of L/M vs. S-cone ERG
signals. For comparison, “S-cone ERGS” were recorded in response
to the 420 nm LED in the presence of steady adaption from an amber
LED (~590 nm peak).
Results: Compared to L/M, S-cone ERGs have very distinct temporal
characteristics. The component waves also have strikingly different
relative amplitudes including a much smaller a-wave and absent dwave which can be explained by the absence of S-cone specific offbipolar cells in primates. In comparison to the pure S-cone ERGs
obtained with silent substitution, long wavelength adaptation can
reduce but does not eliminate L/M contamination.
Conclusions: Using silent substitution we recorded pure S-cone
ERGs to investigate differences between S-cone and L/M cone
mediated signals very early in the visual pathway. The temporal peak
of both the S-cone a- and b-wave is slower indicating the
sluggishness of S-cone temporal responses observed in human
psychophysics has its origins in the outer retina and, at least, partly in
the cones themselves. The robust off-bipolar cells signals in both the
a- and d-waves elicited by L/M cone stimulation are absent in the
pure S-cone ERG with no evidence for the species differences
predicted from the anatomy in which off-midget bipolars have been
proposed to contact S-cones in OW but not NW primates.
Commercial Relationships: James A. Kuchenbecker, None; Scott
H. Greenwald, None; Maureen Neitz, Genzyme (F), Alcon (F),
Alcon (P); Jay Neitz, Alcon (F), Alcon (P)
Program Number: 3707
Presentation Time: 3:15 PM - 3:30 PM
Age-related decline in chromatic-spatial sensitivity
Elise W. Dees1, 2, Stuart J. Gilson1, Rigmor C. Baraas1. 1Optometry
& Visual Science, Buskerud University College, Kongsberg,
Norway; 2Mathematical Sciences & Technology, Norwegian
University of Life Sciences, Ås, Norway.
Purpose: The aim was to investigate the variation in chromatic
contrast sensitivity to low spatial frequencies for observers with
varying degrees of color discrimination at different age decades.
Methods: Twenty six normal trichromatic subjects (17 females and 9
males, aged 20-71 years), 2 female carriers of protan color vision
deficiencies (aged 20-39) and 6 female carriers of deutan color vision
deficiencies (aged 20-59) were included in the study. All observers
were healthy with no known ocular abnormalities. They were tested
with a battery of color vision tests and their statuses of either a
normal trichromat or a carrier were confirmed with genetic analysis
of the genes encoding L- and M-pigments. The observers were
corrected to best logMar visual acuity and viewed the stimulus
monocularly at a distance of either 114.6 cm (0.3-3.0 c/deg) or 229.2
cm (4.0-6.0 c/deg). The stimulus was a Gabor patch with a
pseudoisochromatic design. The chromatic contrast was varied along
either the L- or M-cone axis in the CIE 1931 chromaticity diagram.
The observers were tested with 9-16 different spatial frequencies
from 0.3-3.0 c/deg in all observers, and up to 6.0 c/deg in some.
Results: The sensitivity to chromatic spatial patterns declined with
age. Subjects aged 50 years and older had significantly lower
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
sensitivity [area under curve (ANOVA: f = 13.27, d.f. = 1, p = 0.01)]
and cut-off values (ANOVA: f = 6.33 , d.f. = 1, p = 0.038) than the
younger subjects. The protan carriers had similar sensitivity curves as
the age matched normal trichromatic subjects. The deutan carriers,
however, had on average lower chromatic sensitivity than both the
normal trichromatic subjects and the protan carriers (for all age
groups). The cut-off spatial frequencies were lower for the deutan
carriers than for the normal trichromatic subjects at all age groups.
Conclusions: The results show a decline in sensitivity to chromatic
spatial patterns with age, and that deutan carriers have lower
sensitivity to chromatic spatial patterns compared with age-matched
normal trichromatic subjects.
Commercial Relationships: Elise W. Dees, None; Stuart J. Gilson,
None; Rigmor C. Baraas, None
Support: Research Council of Norway Grant 176541/V10 and
182768/V10 (RCB)
Program Number: 3708
Presentation Time: 3:30 PM - 3:45 PM
Contrast Sensitivity (CS): Color CS is Decreased More than
Luminance CS at Low Light Levels
Jeff C. Rabin1, Michael Castro1, Daniel Ewing1, Hayley George1,
Paul Lau1, Shannon Leon1, Andrew Yoder1, John Gooch2, Steve
Wright2. 1Optometry, UIW Rosenberg School of Optometry, San
Antonio, TX; 2Ophthalmology, USAF School Aerospace Medicine,
Dayton, OH.
Purpose: It is well-known that spatial & temporal vision decrease
with decreasing luminance but less is known about the impact of
luminance on color vision. Our purpose was to compare the effect of
luminance on chromatic (color) & achromatic (luminance) CS.
Methods: Luminance CS was measured with the Pelli-Robson (PR)
chart which has large letters which decrease in contrast in 0.15 log
steps (0.05/letter). Color CS was measured with the cone contrast test
(CCT; Innova Systems, Inc.) which uses a Netbook computer & rapid
staircase to present colored letters on a grey background which
decrease in cone contrast to measure red (L), green (M) and blue (S)
cone contrast thresholds. PR & CCT were measured at photopic (85
cd/m2), low photopic (5.4 cd/m2) & mesopic (0.7 cd/m2) levels by
having subjects view monocularly through neutral density filters. 16
color vision normals (CVN) & 14 hereditary color vision deficients
(CVD) were tested.
Results: In CVN color (L & M cone) and luminance log CS were
equal at high luminance (1.95 log CS) but decreased linearly with log
luminance with color CS decreasing more rapidly (3.5X) vs.
luminance CS (2.5X) such that color CS was 0.2 log units (1.6X)
lower than luminance CS at the mesopic level (p<0.001). A linear
decrease with luminance also prevailed for L & M cone CVD but
both luminance & color CS decreased more rapidly in CVD for both
affected & unaffected cones (L for protans, M for deutans).
Suprisingly at the lowest light level achromatic luminance CS was
0.2 log units lower for CVD than for CVN (p<0.01). L & M CVD
also showed a more rapid decrease in S cone CS with luminance
(3.1X) vs. CVN (1.7X; p<0.01).
Conclusions: Foveal color CS deceases more rapidly than luminance
CS with decreasing light level in CVN & CVD. It is plausible that
color-sensitive parvo cells mediate both color & luminance CS. The
more rapid decline in color CS with decreasing luminance may
reflect the selective nature of cone CS (e.g., red on grey) which
stimulates fewer neurons at threshold (in this example mainly R+/Gopponent cells). The lack of redundant stimulation at low luminance
yields decreased CS, more pronounced in CVD. These results
indicate that cone CS may be more sensitive for detection of acquired
CVD early in eye disease. The finding that low luminance achromatic
CS can be decreased in hereditary CVD may have occupational
significance.
Commercial Relationships: Jeff C. Rabin, None; Michael Castro,
None; Daniel Ewing, None; Hayley George, None; Paul Lau,
None; Shannon Leon, None; Andrew Yoder, None; John Gooch,
None; Steve Wright, None
Program Number: 3709
Presentation Time: 3:45 PM - 4:00 PM
Rod and cone inputs differ to bright and dark colors
Steven L. Buck, Vina Hadyanto, Walker Short, Miaolu Tang, Joris
Vincent, Lauren Wilson. Dept of Psychology, University of
Washington, Seattle, WA.
Purpose: Long-wavelength light that looks yellow in a black
surround looks brown in a white surround. No other unique hue
(blue, green, red) shows such distinct hue change when seen on white
surrounds: they simply appear darker. We determined whether cone
and rod weights differ for yellow vs. brown, and what differences
occur for bright vs. dark versions of other hues.
Methods: Observers saw a 1-s duration 2°-diameter foveal disk
presented in a full-field surround that was either white (141 cd/m2,
CIE 10° x,y .29,.29) or black, and adjusted the disk hue around the
RGB-phosphor-mixture triangle of the CRT display at 21 cd/m2 in
both surrounds. To assess cone balances, observers adjusted the hue
to (a) red-green (RG) null for yellow, brown, and blue disks and (b)
blue-yellow (BY) null for red and green disks. To assess rod hue bias,
we reduced light levels by 2 log units to mesopic level, and compared
hue balances under dark adapted and bleached conditions.
Results: Cone balances. Yellow/brown: All 5 observers showed
different RG balances for yellow and brown, with balanced-brown
chromaticity shifted toward red compared to unique yellow at both
photopic and mesopic levels. Blue: 3 of 5 observers showed the same
direction of shift for bright/dark blue as for yellow/brown. Red and
green: Shifts in BY hue balances between bright/dark versions were
small or inconsistent across observers.
Rod hue biases. Yellow/brown: Rods exerted a green bias on yellow
for all 4 observers but a red bias on brown for 3 of 4 observers. Blue:
Rods also exerted a green bias on bright blue for 3 of 4 observers. 2
observers showed a red bias for both dark blue and brown. Red and
green: Rod effects were inconsistent across observers.
Conclusions: Both RG balance and rod hue biases differ when the
same test light appears yellow vs. brown. The different RG balances
suggest M cones have stronger weighting relative to L cones in the
portions of midget pathways mediating RG balance for brown
compared to those for yellow. The opposite rod hue biases can be
explained by rod and cone signals mixing with same sign in ON and
OFF midget pathways. While some observers showed similar effects
for light vs. dark blue, results were inconsistent for light vs. dark
green and red. Thus cone and rod input differences were not apparent
in S-cone pathways for light vs. dark colors, and may be exclusive to
midget pathways.
Commercial Relationships: Steven L. Buck, None; Vina
Hadyanto, None; Walker Short, None; Miaolu Tang, None; Joris
Vincent, None; Lauren Wilson, None
Program Number: 3710
Presentation Time: 4:00 PM - 4:15 PM
Cone signals feeding into luminance can exhibit large phase
delays and sign reversals: the effect of an inhibitory surround
network?
Andrew Stockman. Department of Visual Neuroscience, UCL
Institute of Ophthalmology, London, United Kingdom.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Purpose: The luminance flicker pathway is typically conceived of as
a simple additive combination of M- and L-cone signals. As we
reported before (ARVO, 2001), this simple picture is complicated by
the existence of multiple cone signals with different delays and signs,
which can be revealed by most conditions of chromatic adaptation.
Here, we extend these measurements and model the results in terms
of an inhibitory surround network.
Methods: Cone delays were measured by a flicker photometric
cancellation technique. Human subjects varied the relative delay
between two superimposed flickering lights (and their relative
modulation) in order to minimize or null the perception of flicker.
One flickering light was either an M-cone or an L-cone isolating
stimulus, and the other was a “standard” light that was of the same
wavelength as the background. Measurements were made as a
function of temporal frequency from 2.5 to about 25 Hz on a series of
adapting backgrounds with wavelengths between 410 and 658 nm
and at several background intensities.
Results: Under most conditions, sizeable delays or advances by as
much as 33 ms have to be introduced between the M- or L-cone
flickering light and the standard in order to null the perception of
flicker, particularly when M-cone flicker is used. In general, the
results are consistent with the L- and M-cone signals being made up
of faster components combined with delayed ones of the same or
opposite sign. For M-cone signals, the delayed components can be
larger than the fast, so that they predominate.
Conclusions: These results challenge the idea that the luminance
channel is made up of only additive M- and L-cone inputs. However,
these complexities may simply reflect the fact that the inhibitory
surround of each cone has both L- and M-cone inputs, and that there
are typically more L-cone inputs than M. We model the surround as a
network of direct and indirect inhibitory lateral connections across
which each step in the network inverts and delays the signal. Thus,
the effective sign and overall delay of the slow signal depend upon
the relative strengths of the inhibitory feedback at each step and upon
the number of steps.
Commercial Relationships: Andrew Stockman, None
Support: BBSRC
410 Spatial Vision, Visual Psychophysics and Aging II
Wednesday, May 08, 2013 8:30 AM-10:15 AM
TCC LL 4/5 Paper Session
Program #/Board # Range: 4063-4068
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 4063
Presentation Time: 8:30 AM - 8:45 AM
Two-point detection and appearance in the absence of higher
order aberrations
Heidi J. Hofer, Darren E. Koenig. College of Optometry, University
of Houston, Houston, TX.
Purpose: We investigated the impact of the cone mosaic on
spatiochromatic reconstruction of two-point stimuli by measuring
detection and appearance with stimuli made smaller than retinal
cones with adaptive optics. We sought to determine whether
detection and perception of these points are independent near the
fovea, as has been previously hypothesized, and if not the extent of
summation for detection and color. We also investigated whether
two-point resolution is consistent with a photoreceptor limit under
these conditions.
Methods: We performed two experiments in which subjects viewed
550nm two-point stimuli through a 6mm pupil with adaptive optics
aberration correction. Stimuli were viewed at ~1 degree eccentricity
under a rod bleaching protocol to isolate cone responses. In one
experiment two subjects were shown either one or two spots (25 ms,
0.5 arcmin estimated retinal full-width at half maximum (fwhm)) of
different intensities and reported the number seen and color
appearance. Separation was varied from 1.5 to 15 arcmin. In the
second experiment two subjects were shown either one or two dim,
yet suprathrehsold, spots (15 ms, 0.5 and 1.1 arcmin estimated fwhm)
and reported whether they believed one or two spots were present.
Separation was varied from 0.5 to 12 arcmin.
Results: Detection thresholds in the first experiment were consistent
with complete spatial summation up to 3-4 arcmin. Detection, but not
color appearance, was independent for separations of 8 arcmin or
more and consistent with at least 15 arcmin of spatial uncertainty. For
two-point stimuli color appearance was highly variable, as for single
points, but also highly coupled. Both points were reported to have the
same color appearance on over 97% of trials, regardless of
separation. Resolution thresholds were similar in both experiments,
2.5-5 arcmin, with a slight tendency towards lower thresholds with
the larger spots.
Conclusions: Cone detection at 1 degree is consistent with complete
spatial summation over an extent including at least a cone and its
nearest neighbors, creating challenges in recovering ‘single cone’
sensations from the responses to tiny stimuli. Despite this extent,
two-point resolution is roughly consistent with expectations based on
a photoreceptor limit. The large variation, but lack of independence,
in the color appearance of the two-point stimuli, implies nonlocality
in the color reconstruction mechanisms.
Commercial Relationships: Heidi J. Hofer, None; Darren E.
Koenig, None
Support: ROI EY019069, P30 EY07551
Program Number: 4064
Presentation Time: 8:45 AM - 9:00 AM
A Comparison of Acuity and Cone Density in the Temporal
Retina
Nancy J. Coletta1, Toco Y. Chui2, Ann E. Elsner2. 1Vision Science,
New England College of Optometry, Boston, MA; 2School of
Optometry, Indiana University, Bloomington, IN.
Purpose: Cone spacing has long been thought to set a limit on visual
acuity. While parafoveal acuity and cone density decrease at parallel
rates with increasing myopia (Coletta and Watson, Vis Res, 2006;
Chui et al., IOVS, 2008), parafoveal acuity has been reported to
exceed the limit estimated from histological measures of cone
spacing (Williams and Coletta, JOSA A, 1987). Recent advances in
retinal imaging allow a comparison of acuity and cone spacing in the
same eyes. We compared parafoveal acuity to cone density in several
young adult individuals to determine whether acuity is matched to the
limit estimated from cone density.
Methods: Measurements were made on five subjects with an average
age of 28 years +/- 4.30 s.d., average spherical equivalent refractive
error of -1.93 D +/- 3.32 s.d. and average axial length of 24.48 mm
+/- 1.38 s.d. (IOL Master, Zeiss Meditec). Acuity was measured on
the temporal retinal meridian using 543 nm laser interference fringes
at a retinal illumination of 100 td; fringes were displayed in a 1 deg
patch at 2 deg and a 2 deg patch at 7 deg eccentricity. Acuity was
estimated at the 75% correct level for a 2AFC vertical/horizontal
discrimination task. Cone densities in the temporal retinal meridian
were assessed using a second generation Adaptive Optics Scanning
Laser Ophthalmoscope. Densities were measured at a nominal 630
and 2070 microns from the foveal center with custom software
(Matlab, Mathworks). Axial lengths were used to correct the cone
sampling positions and retinal area, as well as to convert cone
densities to Nyquist frequencies (NF) in units of c/deg.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Results: The average acuity at 2 deg and 7 deg locations was 34.4
c/deg +/- 3.54 s.e.m. and 17.62 c/deg +/- 2.33 s.e.m., respectively,
while the average cone NFs at 2 deg and 7 deg locations were 26.97
c/deg +/- 1.02 s.e.m. and 18.79 c/deg +/- 0.73 s.e.m., respectively.
Individual ratios of acuity: cone NF ranged from 1.03 to 1.47 with a
mean of 1.26 at 2 deg and 0.75 to 1.18 with a mean of 0.93 at 7 deg.
A paired t-test of acuity and cone NF values at 7 deg was not
statistically significant.
Conclusions: Visual acuity exceeded the cone NF at 2 deg
eccentricity, confirming earlier studies that compared parafoveal
acuity and histological measures from different eyes. However our
results at 7 deg eccentricity suggest that interferometric acuity may
provide a good estimate of cone density in the perifoveal region.
Commercial Relationships: Nancy J. Coletta, None; Toco Y.
Chui, None; Ann E. Elsner, Aeon Imaging, LLC (I), Aeon Imaging,
LLC (F), Aeon Imaging, LLC (P)
Support: NIH Grants NEI EY007624 (AE Elsner), NEI EY004395
(SA Burns), NEI P30EY019008 at IU and NEI R24 EY014817 at
NECO
Program Number: 4065
Presentation Time: 9:00 AM - 9:15 AM
Age-related variation in foveal, parafoveal and peripheral spatial
suppression
Rigmor C. Baraas, Craig Aaen-Stockdale, Stuart J. Gilson.
Optometry & Visual Science, Buskerud University College,
Kongsberg, Norway.
Purpose: The study investigated motion-related spatial suppression
across different age groups and across different eccentricities, with
the stimuli scaled according to the size of MT receptive fields. The
aim was to test three alternative hypotheses: If spatial suppression (1)
is a perceptual correlate of center-surround antagonism in cortical
visual area V5 then the levels of spatial suppression should be
constant at all eccentricities; (2) reduces with increasing age, as a
result of a generalized weakening of inhibition then suppression
should be lower for older observers, but constant at all eccentricities;
(3) is related to contrast-related changes in receptive field size at a
retinal level then suppression should vary with eccentricity and
possibly vary with cone density.
Methods: Eleven normal, healthy subjects (7 females) with no
known ocular abnormalities, aged 21-71 yrs participated in the study.
Their left eye was patched and they fixated a fixation cross presented
on the screen at eccentricities of 0, 2, 5 or 10 deg, or a back-lit
fixation point at 25 or 40 deg. The stimulus was a 2 Hz drifting
sinusoidal grating with a peak contrast of 92%. Spatial frequency was
varied with eccentricity to keep it close to peak contrast sensitivity.
Stimulus duration was varied to derive a duration threshold. Highresolution images of the cone mosaic were obtained with the
Kongsberg Adaptive Optics Ophthalmoscope II.
Results: Older observers showed zero suppression for foveal vision
(0-2 deg), gradual increase in suppression in the parafovea (5-10 deg
eccentricity) and weaker suppression in the periphery (25-40 deg).
Contrary to this, young observers showed strong suppression for
foveal and parafoveal vision (0-5 deg) with a gradual decline in
suppression from 10 deg. There was between-individual variation in
both spatial suppression and cone density. Initial analyses indicate
that lower levels of suppression correlate with lower cone count.
Conclusions: The strength of suppression, in both young and old
observers, varied with eccentricity, despite the scaling of the stimulus
with average MT receptive field size. The results for older observers
imply that weaker suppression is not a generalizable result. The
results suggest that spatial suppression may be the result of low-level
stimulus characteristics and structural variation in the retina rather
than a direct result of center-surround antagonism in MT.
Commercial Relationships: Rigmor C. Baraas, None; Craig
Aaen-Stockdale, None; Stuart J. Gilson, None
Support: The Research Council of Norway Yggdrasil international
mobility grant #211313 (CAa-S); Research Council of Norway Grant
176541/V10 and 182768/V10 (RCB)
Program Number: 4066
Presentation Time: 9:15 AM - 9:30 AM
Heterochromatic Modulation Photometry can be used to measure
Macular Pigment Optical Density
Cord R. Huchzermeyer1, Juliane Schlomberg1, Ulrich Welge-Lüssen1,
Tos TJM Berendschot2, Jan J. Kremers1. 1Department of
Ophthalmology, University Erlangen-Nuremberg, Erlangen,
Germany; 2University Eye Clinic, Maastricht, Netherlands.
Purpose: Macular pigment optical density (MPOD) can be measured
psychophysically by comparing the luminance ratio between a shortwavelength and a long-wavelength light at a central and a peripheral
retinal locus using heterochromatic flicker photometry (HFP).
Heterochromatic modulation photometry (HMP) is a psychophysical
test that uses, in contrast to HFP, test fields with constant mean
luminance and chromaticity.
To study whether HMP is suitable for measuring MPOD, we
compared a custom made HMP protocol with measurements using
HFP and macular pigment reflectometry (MPR).
Methods: We developed a protocol for the measurement of MPOD
using a Maxwellian view LED stimulator. Two lights (B: 460nm and
R:660nm, retinal illuminance of 21 phot Td each) were modulated in
counterphase in a 2° center-field surrounded by a 12° white
background (587 phot Td). Flicker detection threshold contrasts were
determined for 9 different contrast ratios (B/R) of the two lights,
varying between 10-1 and 101. Thresholds were determined using two
randomly interleaved staircases and a 2AFC (flicker/no flicker)
procedure. The measurements were repeated with central and with 6°
nasal fixation.
For comparison, MPOD was also measured using an HFP-based
Macular Densitometer (Macular Metrics, USA) and the Macular
Pigment Reflectometer (Maastricht Instruments bv, The
Netherlands).
The right eyes of 14 normal subjects were measured.
Results: Log sensitivity (1/threshold) vs log B/R can be described by
a V-shaped curve with a minimum at log B/R = 0 for the standard
observer with Vλ-like spectral luminosity. A horizontal shift (along
the log B/R axis) of the minimum represents a deviation from the V λ.
The difference of the positions of the minima measured at central and
6°nasal fixation were used to estimate the MPOD.
MPOD measurements using HMP correlated with HFP (n=12,
r=0.79, p<0.01) and MPR (n=13, r=0.69, p<0.05).
Bland-Altman plots showed a marked systematic difference: HMP
yielded 0.27±0.19 lower values than MPR. Agreement with HFP was
much better (difference 0.02±0.13). HFP measured higher values in
eyes with low MPOD and lower values in eyes with high MPOD.
Conclusions: HMP measurements agree well with HFP, but HMP
has the advantage of using constant mean luminances and
chromaticities. HMP also correlates with MPR, but there are
systematic differences. This pilot study showed that the HMP method
can be used to measure MPOD.
Commercial Relationships: Cord R. Huchzermeyer, None;
Juliane Schlomberg, None; Ulrich Welge-Lüssen, None; Tos TJM
Berendschot, None; Jan J. Kremers, None
Support: ELAN Erlangen, IZKF Erlangen
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 4067
Presentation Time: 9:30 AM - 9:45 AM
Comparability of Visual Performance of Individuals with Low
Vision in Real and Virtual Street Intersections
Lei Liu, Ellen L. Bowman. School of Optometry, University of
Alabama at Birmingham, Birmingham, AL.
Purpose: Low Vision Orientation & Mobility (O&M) evaluation and
training are typically performed in streets and street intersections.
While effective, the efficiency of the practice can be greatly
improved by employing computer-generated virtual street scenarios.
To evaluate the feasibility of virtual O&M training, we compared
visual performance of low vision patients in real and virtual street
intersections.
Methods: A semi-CAVE virtual reality simulator was built. It
consisted of a game computer, 3 digital projectors, three 2.4x1.9 m
screens (>180o deg horizontal) and surrounding sound. Four virtual
street intersections were built based on 4 real intersections in an
urban environment. Google Street, Geographic Information System
and on-site photos/videos were used to match the physical layout and
surrounding, traffic controls, and vehicle and pedestrian traffic of the
real and virtual intersections. Multiple crossing scenarios were set at
each intersection. Ten legally blind subjects with adequate prior
O&M training performed 10 visual tasks in both real and virtual
intersections. These tasks included identifying traffic elements,
determining intersection layout and choosing the safest time to cross.
The performance was rated pass or fail by two certified O&M
specialists. Agreement between performance in corresponding real
and virtual intersections was compared.
Results: Data from corresponding real and virtual intersections was
organized into a 2x2 contingency table. The overall, positive and
negative agreements were 83.3%, 89.4% and 68.6%, respectively,
indicating that if a subject could perform a task in a real intersection,
it was highly likely that she could also perform the same task in a
virtual version of the intersection, and vice versa. The kappa
coefficient was 0.59, bordering moderate and substantial agreement.
A McNemar analysis of paired binary data showed an exact
significance of 0.824, indicating no difference in performance
between real and virtual intersections.
Conclusions: Persons with low vision exhibited similar abilities
while performing visual tasks in real and virtual street intersections.
The agreement suggested that computer-generated traffic scenes
provided sufficient visual and auditory information for low vision
patients to perform O&M tasks. Virtual reality has the potential to
become a useful supplement to tradition low vision rehabilitation
training.
Commercial Relationships: Lei Liu, None; Ellen L. Bowman,
None
Support: NIH Grant 1R21EY019549
Program Number: 4068
Presentation Time: 9:45 AM - 10:00 AM
Optical quality and subjective judgments of blur under pure
simultaneous vision
Carlos Dorronsoro, Aiswaryah Radhakrishnan, Lucie Sawides,
Susana Marcos. Instituto de Optica, CSIC, Madrid, Spain.
Purpose: To compare retinal image quality and subjective image
sharpness under pure bifocal simultaneous vision (PSV) across a
wide range of addition values.
Methods: Four subjects performed a weighted rank psychophysical
experiment to grade (from totally blurred to totally sharp, 0 to 5) the
perceptual quality of PSV images. As a control condition, the
perceptual quality of purely defocused (PD) images was also
assessed. Computer generated images of a face were observed, for
1.5s in random order, through adaptive optics to correct the
aberrations of the eye. The PSV images (50/50 energy content) were
obtained from the combination of a focused image superimposed to a
defocused version of the same image. At least 18 defocus conditions
(0-3D) were subjectively ranked (10 repetitions). In addition, optical
quality was evaluated as a function of defocus, from the PSV and PD
Point Spread Functions (PSF), using the Modulation Transfer
Function (MTF) at different frequencies as a metric.
Results: As expected, images without defocus were perceived as
sharp (score s=5) in all subjects and conditions. The perceptual
weighted rank systematically dropped for PD at a rate of 9.0±4.0 s/D,
with the images perceived as completely blurred (s=0) from 0.6 D
onwards. PSV images provided a similar decrease as their defocus
component increased, in the 0-0.3D range. However, in 3 subjects the
score reached a minimum at 0.5D (s=2.1±0.4) and then it was
partially recovered back towards sharpness (s=3.5 at 1.2D),
remaining stable afterwards. The 4th subject showed a similar trend
judging PSV images but without a minimum. The objective
simulations predicted the perceptual judgment trends, as well as the
differences between judgments of PD and PSV images. MTF@20
c/deg decreased sharply with defocus in PD, but reached a minimum
(0.42 at 0.5 D) and recovered a stable level (0.50 from 1.5D) in PSV.
Averaged MTFs (15-25 c/deg) provided the most accurate
predictions.
Conclusions: As opposed to the common idea that simultaneous
vision retinal images (as those found in multifocal contact or
intraocular lenses) are severely optically degraded, but later restored
in neural processes, we have found a good correspondence between
pure subjective perception experiments and pure optical simulations.
Although our findings do not preclude for possible effects of neural
adaptation, neural effects seem to be secondary in the perceptual
judgment of sharpness in PSV.
Commercial Relationships: Carlos Dorronsoro, Essilor
International (F); Aiswaryah Radhakrishnan, None; Lucie
Sawides, None; Susana Marcos, Essilor (F), PCT/ES2012/070185
(P)
Support: FIS2011-25637; ERC-2011-AdG-294099; EU Marie Curie
FP7-PEOPLE-2010-ITN #26405
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
417 Accommodation and Presbyopia Correction
Wednesday, May 08, 2013 8:30 AM-10:15 AM
Exhibit Hall Poster Session
Program #/Board # Range: 4250-4283/B0287-B0320
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 4250 Poster Board Number: B0287
Presentation Time: 8:30 AM - 10:15 AM
The Influence of Multifocal Lenses on Fine Motor Tasks
Rupal Lovell-Patel1, 2, Matthew A. Timmis2, Shahina Pardhan2, Paul
McCarthy1, 2. 1Vision and Hearing Sciences, Anglia Ruskin
University, Cambridge, United Kingdom; 2Vision and Eye Research
Unit, Anglia Ruskin University, Cambridge, United Kingdom.
Purpose: Literature suggests that multifocal lenses are associated
with a decreased performance for a variety of tasks including
negotiating steps, obstacles, driving and reading at certain distances,
when compared to single vision lenses. In daily life we regularly
perform other motor tasks, such as reaching and grasping an object.
Currently, there is no evidence based data on how multifocal lenses
affect the performance of such fine motor tasks when compared to
single vision lenses.
Methods: 12 presbyopic subjects who were habitual multifocal
spectacle wearers took part in the study. Performance was compared
for multifocal lenses and single vision lenses which were prescribed
following a comprehensive vision assessment and an analysis of the
distances at which the tasks were carried out. Subjects had a
minimum visual acuity of 0.00 LogMAR. Participants completed 3
different fine motor tasks wearing both types of correction; object
width estimation, reach-and-grasp and transport-and-placement.
Hand and head movements were captured by a 3-D motion capture
system.
Results: Data were analysed using ANOVA. Peak grip aperture was
significantly larger when grasping the large compared to small object
(p < .001). Participants also showed greater error when positioning
the large compared to small object (p < .001). For the reach-andgrasp task: onset time, overall movement time, peak velocity, peak
grip aperture, deceleration time and velocity corrections were not
significantly affected by spectacle type (p>0.05). Interestingly, head
flexion was also not affected by the spectacle type (p > .05). For the
object width estimation task: no significant difference was obtained
in the perceived aperture width between the spectacle types. For
transport-and-placement: movement time, peak velocity, deceleration
time, velocity corrections, head rotation and error in object placement
were unaffected by spectacle type (p > .05).
Conclusions: The type of spectacle lens did not affect the fine motor
tasks which encompassed a range of visual angles that would lie
outside the multifocal lenses’ intermediate corridor. Data
demonstrates that habitual multifocal spectacle wearers can carry out
fine motor tasks such as reaching and grasping just as competently as
they can with single-vision lenses.
Commercial Relationships: Rupal Lovell-Patel, None; Matthew
A. Timmis, None; Shahina Pardhan, None; Paul McCarthy, None
Program Number: 4251 Poster Board Number: B0288
Presentation Time: 8:30 AM - 10:15 AM
Accommodative Lag, Facility and Phoria with Multifocal Contact
Lenses
Jiyoon Chung1, Ravi C. Bakaraju1, Cathleen Fedtke1, Jerome Ozkan1,
Klaus Ehrmann1, 2, Darrin Falk1, Arthur Ho1, 2, Brien A. Holden1, 2.
1
Brien Holden Vision Institute, Sydney, NSW, Australia; 2School of
Optometry and Vision Science, University of New South Wales,
Sydney, NSW, Australia.
Purpose: To compare the accommodative lag, facility and phoria
measurements of myopic participants fitted with various commercial
contact lens designs.
Methods: Forty myopic, non-presbyopic, subjects were randomized
to be fitted bilaterally, with a single vision control lens (Air Optix
Aqua) and two of four multifocal (MF) lenses (Proclear Distance and
Near MF, Air Optix Aqua MF and PureVision MF) on a daily wear
basis. Subjects wore each lens type for a minimum of 8 days over 4
scheduled (baseline and 3 follow-up) visits with a 1-week wash-out
between lens types. Static accommodative responses were assessed
with the EyeMapper at all visits. Five repeats were performed in a
fogged state (+1D) and at four object vergences from -2 to -5D (1D
steps). Paraxial curvature matching of the wavefront aberration map
yielded the spherical equivalent. Accommodative facility and phoria
(at distance and near) were evaluated using ± 2D flippers and Howell
card, respectively. To reduce the effect of between-visit variability,
the data was averaged over the four visits.
Results: At +1D fogging, all lens types produced a myopic shift.
With the control lens, the accommodative response function was
relatively linear (slope = 0.82). Three centre-near MFs (Air Optix,
PureVision and Proclear Near) all demonstrated accommodative lead
at -2D, optimal response at -3D, and lag at -4 and -5D object
vergences. Proclear Distance produced lag over all test vergences. All
MFs produced lower accommodative facility compared to control
lens (19.2 cycles / min, p<0.05). The facility measures for Air Optix,
PureVision, Proclear Near and Proclear Distance were 15.8, 15.7,
14.4, and 16.5 cycles / min, respectively. There were no differences
for distance phoria between all lens types. Significant differences
were observed for near phoria with Proclear Near MF (5.6 exo, p<
0.05).
Conclusions: There were significant differences between measured
accommodative lag for different lens types with Proclear Distance
producing greater lag than the rest. This observation was more
pronounced at -3D, -4D and -5D accommodative states.
Commercial Relationships: Jiyoon Chung, None; Ravi C.
Bakaraju, None; Cathleen Fedtke, None; Jerome Ozkan, None;
Klaus Ehrmann, None; Darrin Falk, None; Arthur Ho, None;
Brien A. Holden, Allergan (F), AMO (I)
Clinical Trial: ACTRN12611001004954
Program Number: 4252 Poster Board Number: B0289
Presentation Time: 8:30 AM - 10:15 AM
The role of eye dominance on through-focus visual performance
in modified monovision presbyopic corrections
Len Zheleznyak1, 2, Aixa Alarcon2, Kevin C. Dieter3, Duje Tadin3, 2,
Geunyoung Yoon2, 1. 1The Institute of Optics, University of
Rochester, Rochester, NY; 2Flaum Eye Institute, University of
Rochester, Rochester, NY; 3Brain and Cognitive Sciences, University
of Rochester, Rochester, NY.
Purpose: To investigate the impact of the degree of sensory eye
dominance on through-focus visual performance in presbyopic
corrections with modified and traditional monovision.
Methods: The degree of sensory eye dominance was measured using
a binocular rivalry technique in which orthogonal sinusoidal gratings
(4cyc/deg) were presented to each eye. The proportion of exclusive
visibility of each grating was recorded as the right eye’s contrast
varied from 10-90% while the left eye remained fixed at 50%. The
degree of ocular dominance (DOD) was defined as the difference in
interocular contrast which resulted in perceiving the two gratings for
equal portions of time. A binocular adaptive optics vision simulator
was used to correct 9 cyclopleged subjects’ native aberrations and
induce modified monovision (1.5D anisometropia, spherical
aberration of +0.1 and -0.4μm in distance and near eyes,
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
respectively). To assess the impact of dominance on visual
performance, through-focus visual acuity (VA) from 0.0 to 3.0D at
0.5D step with a 4mm artificial pupil was measured under two
conditions by assigning dominant and non-dominant eye to distance
and near, respectively, and vice versa. Traditional monovision of
1.5D anisometropia was measured for comparison.
Results: Sensory eye dominance spanned from weak (DOD=4%) to
strong (DOD=23%) dominance with average DOD=9±8%. The
average difference in through-focus VA between switching eye
assignment for distance in modified and traditional monovision was 0.01±0.04 and 0.00±0.03 logMAR, respectively. The subject with the
strongest dominance experienced a loss in intermediate (0.5-1.5D)
VA of 0.16±0.09 and 0.05±0.01 logMAR with modified and
traditional monovision, respectively, when the non-dominant eye was
assigned to distance compared to assigning the non-dominant eye to
near.
Conclusions: For subjects with typical low and moderate levels of
sensory eye dominance, the degree of dominance did not have a
significant effect on through-focus VA in monovision regardless of
which eye was assigned to distance and near. However, it is
important for subjects with strong eye dominance to assign the
dominant eye to distance vision for optimal through-focus VA,
especially in modified monovision correction.
Commercial Relationships: Len Zheleznyak, None; Aixa Alarcon,
None; Kevin C. Dieter, None; Duje Tadin, None; Geunyoung
Yoon, Bausch & Lomb (F), Johnson & Johnson (F), Allergan (C),
Staar Surgical (C), CIBA Vision (F), Acufocus (C)
Support: NIH Grant EY014999, Research to Prevent Blindness
Unrestricted/Challenge Grant, NIH Training Grant T32 EY007125
Program Number: 4253 Poster Board Number: B0290
Presentation Time: 8:30 AM - 10:15 AM
Customizing depth of focus outcomes in Hyperopic Lasik using
an Adaptive Optics Vision Analyzer
Guillermo M. Perez1, Eloy A. Villegas2, Benjamin Leray3, Francois J.
Malecaze3, Pablo Artal2. 1Voptica S.L., Murcia, Spain; 2Laboratorio
de Optica, Universidad de Murcia, Murcia, Spain; 3Service
d'Ophtalmologie, CHU Toulouse-Purpan, Toulouse, France.
Purpose: LASIK allows not only to correct for the refractive error
but also to extend depth of focus by inducing controlled amounts of
spherical aberration (SA). However the success of the procedure may
depend on the particular SA values required by each patient. We
evaluate a customization procedure where the optimum values of SA
were determined for each patient using an adaptive optics vision
analyzer before the surgery.
Methods: A group of 38 hyperopic/presbyopic patients were
evaluated before and after surgery using the Adaptive Optics Vision
Analyzer (AOVA, Voptica SL, Murcia, Spain). This is a clinical
instrument to perform vision testing with full control of the optical
aberrations induced in the patient’s eye non-invasively. The AOVA
includes a wave-front sensor, a liquid crystal on silicon spatial light
modulator to induce any desired aberration profile on the patient’s
eye, and a micro-display to present the visual stimuli. Visual acuity
was measured for defined combinations of residual defocus and SA at
infinity, 60 cm and 40 cm. In each patient, the sets of optimized
values of defocus and SA required to maintain adequate near and far
VA were determined. Then, and taking into account the patient’s
corneal asphericity (Q-value), the LASIK procedure (WaveLight
Allegretto Wave Eye-Q Laser, Alcon) was settled to induce the
desired range of negative SA in one eye. The fellow dominant eye
was treated only to reach emmetropia without inducing SA. After the
surgery, through focus VA, residual refraction, and SA was measured
using the AOVA in each patient.
Results: The average Q-value changed from -0.1 to -0.6 in the
dominant eyes, and from -0.05 to -0.8 in the eyes treated for inducing
extra asphericity. The average value of SA providing an extended
depth of focus was around -0.2 microns for 4.5-mm pupil. In these
eyes, the required positive addition for intermediate and near vision
changed from +1.00D and +1.70D to +0.40D and +1.00D
respectively. In those eyes with no SA induced, the positive addition
required hardly changed.
Conclusions: Hyperopic presbyopic patients are ideal candidates for
customized LASIK to induce an extended depth of focus. This
procedure can be optimized when mediated with adaptive to predict
the right amount of SA to be induced. These results suggest that the
LASIK guided with and AOVA can provide improved visual
outcomes at all distances.
Commercial Relationships: Guillermo M. Perez, VOPTICA (E);
Eloy A. Villegas, Voptica, S.L. (I), Calhoun Vision (F); Benjamin
Leray, None; Francois J. Malecaze, None; Pablo Artal, AMO (C),
Voptica SL (P), Voptica SL (I), AMO (F), Calhoun Vision (F),
Calhoun Vision (C), AcuFocus (C)
Support: Ministerio de Ciencia e Innovación, Spain (grants
FIS2010-14926 and CSD2007-00013), Fundación Séneca (Region de
Murcia, Spain), grant 4524/GERM/06.
Program Number: 4254 Poster Board Number: B0291
Presentation Time: 8:30 AM - 10:15 AM
Effect of Age on Amplitude of Accommodation in Bolivia
Magnus Andersson, Baskar Theagarayan. Section of Optometry and
Vision Science, Linnaeus University, Kalmar, Sweden.
Purpose: The purpose of this study was to investigate the impact of
age on Amplitude of Accommodation (AA) in a Bolivian population
and compare it with previously published data. We were also
interested in finding out the age of onset of Presbyopia in this
population.
Methods: A sample of 197 Bolivian subjects aged between 8 to 60
years, attending three different field clinics provided by Vision For
All (non-profit organization, Sweden) was used in the study. All the
subjects were refracted binocularly and had at least best correction
Visual acuity of 20/25. None of the subjects had any visible
strabismus or ocular pathology. The AA was measured using the
push-up and push-down method with a Royal Air Force (RAF) ruler.
The ruler has both a metric scale in centimeters and a dioptric scale.
The subjects were asked to read letters of N5 print size and report
first sustained blur in push-up method and first sustained clear in the
push-down method. The subjects had their correction in place during
the measurements. Among the presbyopic subjects a +2.00D lens was
placed as an addition to bring the target within measurable limits. The
average of push-up and push-down readings was used as the
subjective AA.
Results: Independent samples t-test showed no statistically
significant difference between the present and the previous AA
studies (p > 0.05). The AA of the Bolivian population was generally
lower compared to previous investigations. Regression analysis
showed a significant correlation between age and the AA (r = 0.80, p
< 0.05). The onset of presbyopia among the Bolivian population was
found to be 38 years.
Conclusions: This result supports the theory that there is a lower AA
among people in tropical zones compared to those from temperate
zones. The onset of presbyopia for this Bolivian population was
seven years earlier than the Hofstetter formula would predict and five
years earlier compared to Duane’s (Duane A, Trans Am Ophthalmol
Soc, 1922; 20:132-157) values.
Commercial Relationships: Magnus Andersson, None; Baskar
Theagarayan, None
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 4255 Poster Board Number: B0292
Presentation Time: 8:30 AM - 10:15 AM
Influences of cycloplegia with topical cyclopentolate on higherorder aberrations in myopic children
Takahiro Hiraoka1, Kazunori Miyata2, Fumiki Okamoto1, Tetsuro
Oshika1. 1Dept of Ophthalmology, University of Tsukuba, Tsukuba,
Japan; 2Miyata Eye Hospital, Miyakonojo, Japan.
Purpose: It is little known about the effect of cycloplegia with
topical cyclopentolate on optical quality of the eye in myopic
children. We conducted this prospective study to investigate the
influence of topical cyclopentolate on higher-order aberrations
(HOAs) in myopic children.
Methods: Twenty-eight eyes of 28 myopic children (17 boys and 11
girls), ranging in age from 4 to 12 years (7.25 ± 2.55, mean ±
standard deviation), were enrolled in this study. We evaluated
refraction and wavefront aberrations before and after cycloplegia
with topical instillation of 1% cyclopentolate hydrochloride. Ocular
and corneal aberrations were simultaneously measured and compared
with each other. Individual Zernike components were also analyzed
for a 6-mm pupil up to the sixth order. All these parameters were
compared before and after cycloplegia. In addition, the obtained data
were compared with other 23 subjects with hyperopia.
Results: Cycloplegia with topical cyclopentolate induced significant
hyperopic changes from -3.07 ± 2.23 to -2.57 ± 2.15 D (P < 0.001,
paired t-test). Ocular higher-order aberrations (HOAs) increased
significantly from 0.243 ± 0.111 to 0.263 ± 0.105 μm for coma-like
aberrations (P = 0.042), from 0.124 ± 0.041 to 0.138 ± 0.037 μm for
spherical-like aberrations (P = 0.012), and from 0.279 ± 0.105 to
0.304 ± 0.096 μm for total HOAs (P = 0.015). Corneal HOAs did not
change by cycloplegia. When corneal and ocular HOAs were
compared, the ocular HOAs were significantly smaller than the
corneal HOAs in spherical-like aberrations (P < 0.001) and total
HOAs (P = 0.006). When compared between myopic and hyperopic
children, spherical-like aberrations and total HOAs were significantly
larger in hyperopia than in myopia (P = 0.001 and P = 0.042,
unpaired t-test). However, each Zernike component showed a large
standard deviation in both groups.
Conclusions: Internal optics compensate for corneal HOAs also in
myopic children, and paralysis of tonic accommodation with
cyclopentolate considerably affects ocular HOAs. It may be that
physiological tonic accommodation is done to improve retinal image
quality by reducing HOAs. In addition, HOAs tend to be smaller in
myopia than in hyperopia, but inter-individual variation in each
Zernike component is quite large in both myopic and hyperopic
children.
Commercial Relationships: Takahiro Hiraoka, None; Kazunori
Miyata, None; Fumiki Okamoto, None; Tetsuro Oshika, None
Program Number: 4256 Poster Board Number: B0293
Presentation Time: 8:30 AM - 10:15 AM
Five-year Incidence of Loss of Accommodative Ability in the
Beaver Dam Offspring Study
Dayna S. Dalton, Karen J. Cruickshanks, Mary E. Fischer, Barbara
E. Klein, Ronald Klein, Aaron A. Pinto. Ophthalmology and Visual
Sciences, University of Wisconsin, Madison, WI.
Purpose: To determine the 5-year incidence of loss of
accommodative ability in a large cohort of adults.
Methods: Subjects (n=2256, age 21-84 years at baseline) participated
in both the baseline (2005-2008) and 5-yr follow-up exam (2010 2012) of Beaver Dam Offspring Study. At each visit a Grand Seiko
Autorefractor was used to obtain three measures of refractive error;
distance correction and with correction focusing on two near targets;
one requiring 2 diopters (D) and the other 4.5D. Readings were
converted to spherical equivalent (sphere + ½ cylinder) (SE).
Participants were classified as myopic (SE ≤ -1.00), hyperopic (SE ≥
+1.00) or emmetropic (SE > -1.00 and < +1.00). At each of the two
near targets, the participant was considered to have lost
accommodative ability if the spherical equivalent was ≥ -0.50.
Subjects with cataract surgery were excluded.
Results: In preliminary analyses of right eyes, there were 741
participants in the baseline exam who were able to accommodate at
both targets. Of those, 333 (45%) were not accommodating at the 2D
target and 241 (33%) were not accommodating at the 4.5D target at
the 5-yr follow-up exam. Age was highly associated with the
incidence of loss of accommodative ability (mean age of
accommodating at 2D = 38.2 years; 4.5D = 38.7 years, not
accommodating at 2D = 44.7 years; 4.5D = 46.1 years) and risk of
losing accommodative ability increased with increasing age (OR
3.18, 95% CI 2.59-3.90 for each 5 years of age). Participants with
hyperopia were less likely to lose accommodative ability (OR 0.01,
95% CI 0.00 - 0.04) compared to those with emmetropia. There was
no association between myopia or sex with loss of accommodative
ability. Eight participants over the age of 55 years at the baseline
examination had accommodative ability at both distances at both
examinations.
Conclusions: Loss of accommodative ability is very common in
middle-age. These data show that adjusting for age, hyperopia was
associated with decreased risk. In spite of the strong age effect, a
small number of people retain accommodative ability beyond midlife. Further investigation is necessary to identify factors that are
associated with retention of accommodative ability. To the best of
our knowledge, this is the first longitudinal study using an objective
measure to investigate the loss of accommodative ability.
Commercial Relationships: Dayna S. Dalton, None; Karen J.
Cruickshanks, None; Mary E. Fischer, None; Barbara E. Klein,
None; Ronald Klein, None; Aaron A. Pinto, None
Support: NIH Grant AG021917
Program Number: 4257 Poster Board Number: B0294
Presentation Time: 8:30 AM - 10:15 AM
Effect of Unclean Display on Accommodative Response
Masakazu Hirota1, Hiroshi Uozato1, 2, Shinji Arai1, Yuko Shibata1.
1
Ophthalmology & Visual Sciences, Kitasato Univ Graduate School,
Minami-ku, Sagamihara-shi, Japan; 2Orthoptics & Visual Sciences,
Kitasato University School of Allied Health Science, Minami-ku,
Sagamihara-shi, Japan.
Purpose: To assess change of accommodative response when we
watched an unclean display.
Methods: Twenty volunteers (5 men and 15 women; mean ±
standard deviation age, 22.2 ± 3.4 years; range, 19 to 33 years)
participated in our study. All subjects had a visual acuity of 20/20 or
better. In addition, we confirmed that all subjects had enough
accommodation more than 7.00 D (mean ± standard deviation, 12.31
± 0.54 D) and their near reflex was normal. Each subject’s
accommodative response was measured by a target moving system
WMT-1 (Grand Seiko Co., Ltd, Hiroshima, Japan). WMT-1 can
move a target optionally from 0.2 to 1.0 m and it include a binocular
Autorefractor WAM-5500 (Grand Seiko Co., Ltd, Hiroshima, Japan)
that can measure refraction every 0.2 second in open field. We
adopted iPad (Apple Inc., Cupertino, CA) on WMT-1 as a target. As
an unclean display model, we covered closely to 3 pieces of tracing
paper upon the iPad’s display. We compared accommodative
response of a clean display and an unclean display in target distance
of 1 m, 0.5 m, and 0.2 m.
Results: The accommodative response of unclean display increased
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
larger than that of clean display (1.0 m: clean was -0.80 ± 0.24 D,
unclean was -1.03 ± 0.25 D.). When the target came near, the
difference of accommodative response between control and unclean
display increased (0.5 m: clean was -1.56 ± 0.25 D, unclean was 1.82 ± 0.24 D, 0.2 m: clean was -4.22 ± 0.38 D, unclean was -4.73 ±
0.74 D.). Statistical significant differences were found between the
accommodative response of unclean display and of clean display in
all target distances (Wilcoxon signed rank test, p < 0.001)
Conclusions: The accommodative response of unclean display was
larger than that of clean display. The increase in necessary
accommodative response may lead to asthenopia. We should keep a
display clean to prevent eye fatigue.
Commercial Relationships: Masakazu Hirota, None; Hiroshi
Uozato, None; Shinji Arai, None; Yuko Shibata, None
Program Number: 4258 Poster Board Number: B0295
Presentation Time: 8:30 AM - 10:15 AM
The effect of near addition lenses on the accuracy of the
accommodative response in myopic children during reading
Jinhua Bao, Zhili Zheng, Hao Chen. School of Optometry and
Ophthalmology, Wenzhou Medical College, Wenzhou, China.
Purpose: Addition lenses may play a role in the retardation of the
progression of myopia. The purpose of this study was to evaluate the
changes to accommodation and phoria when myopic children
perform near work with different near addition lenses.
Methods: We measured accommodative response and phoria in 18
children (14 myopic and 4 emmetropic) at 33cm through their
distance refractive correction alone or this correction combined with
multiple addition lenses (+0.50D, +1.00D, +1.50D, +2.00D, +2.50D,
and +3.00D). Accommodative response was measured using the
infrared optometer (WAM-5500) and near phoria was measured
using the modified Thorington technique.
Results: Myopic children had larger lags (1.35D) than emmetropic
children (0.86D) for a 33 cm reading target through the distance
correction, and significantly decreasing lags of accommodation with
larger addition lenses (P<0.01). A small lead of accommodation
(0.22D) was found with the addition of +3.0D lens . There were
obvious differences in the mean responses between the two refractive
groups across the multiple addition lenses (F=28.74, P<0.01). The
near phoria showed significant increases towards exophoria in both
groups with larger addition lenses during reading (P<0.01).
Conclusions: Near addition lenses may actually decrease the degree
of retinal defocus for myopic children who have large lag.
Accommodative lead to a +3.0D lens defocus to a near target (33cm)
may be associated with proximal accommodation.
Commercial Relationships: Jinhua Bao, None; Zhili Zheng, None;
Hao Chen, None
Program Number: 4259 Poster Board Number: B0296
Presentation Time: 8:30 AM - 10:15 AM
Tonic Accommodation Correlates with Accommodative
Amplitude-Scaled Facility Test for Symptomatic Graduate
Students
Chunming Liu1, Chris Chase1, Stefanie A. Drew3, Efrain
Castellanos1, Amy Escobar1, Eric Borsting2, Lawrence R. Stark2.
1
Optometry, Western University of Health Sciences College of
Optometry, Pomona, CA; 2Southern California College of
Optometry, Fullerton, CA; 3California State University, Northridge,
Northridge, CA.
Purpose: Among standard clinical measures of binocular function,
the accommodative amplitude-scaled facility (AsFac) test is the most
sensitive for predicting visual discomfort symptoms. The AsFac test
may be a better correlate due to its individual adjustment of the
accommodative stimulus (AS) based on amplitude. Another factor
that could affect stimulus demand is tonic accommodation (TA).
Higher TA could put the accommodation resting state closer to the
target demand, effectively reducing the AS. This study examined the
relationship between AsFac test and TA in symptomatic and
asymptomatic graduate students.
Methods: Visual symptoms were assessed by the Convergence
Insufficiency Symptom Survey (CISS). Based on the CISS adult cutoff score of 21, the sample was divided into High (N=22) and Low
(N=17) symptom groups. Assessment of binocular function was
made using standard clinical procedures. TA was recorded for 2 min
after 5 min of dark adaptation. From the AsFac test with the plus
lens, a TA-corrected AS was calculated based on testing distance,
lens power, and TA with the formula: [(100/distance in cm) - lens
power - TA].
Results: Among all clinical measures, including accommodative
amplitude/facility, and vergence facility (3BI/12BO), only the
binocular AsFac test showed a statistically significant correlation
with TA (r=0.48, p=0.004). A positive correlation was found in the
high symptom group (Y=6.989+2.812*X; R2=0.435; p=0.001), but
not in the low symptom group (Y=13.948+0.961*X; R2=0.169;
p=0.145) (Fig 1). A similar group effect was also found in the
relationship between TA-corrected AS and AsFac. A statistically
significant negative correlation only existed in the high symptom
group (Y=14.330-1.184*X; R2=0.336; p=0.006), not in the low
symptom group (Y=16.496-0.697*X; R2=0.064; p=0.406) (Fig 2).
Conclusions: Our results suggest a possible link between AsFac test
and the tonic accommodative adaptation state in graduate students
with significant visual discomfort. The sensitivity of the test for
predicting symptom might rely, at least partly, on this correlation. TA
might be utilized as compensatory mechanism for reducing AS
demand at near for this population. With lowered demand, subjects
would be more efficient at performing a facility test.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Fig 1. Regression plot for TA and AsFac test
were assessed by the Convergence Insufficiency Symptom Survey
(CISS).
The sample was divided into High (N=22) and Low (N=17) symptom
groups based on the CISS adult cut-off score of 21. The average AR
for each stimulus was compared between groups and correlated with
the average TA.
Results: Figure 1 shows the High and Low symptom groups had
similar AR for targets (F(4,132)=.54, p=.71). Groups also had the
same AR while reading (t(32)=.51, p=.61). TA values were the same
for both groups (t(37)=.11, p=.91), but the sample averaged a
significantly larger TA value (1.89 ± 1.09 D) than previously
reported for college students (t(38)=2.14, p=.04).
TA was significantly correlated with all AR measures for the High
symptom group but not for the Low Symptom group (see Table 1). A
linear regression between TA and accommodative error during
reading showed that error increased 0.4 D for every 1 D decrease in
TA below the text viewing distance of 3 D (Y = 1.5 - 0.4*X, R2 =
0.54, p=.0002).
Conclusions: These results suggest TA plays a significant role in the
AR of symptomatic graduate students. Those with more TA have
better accommodative focus at near work distances. Possible
weaknesses in the accommodation system of the symptomatic
students may be compensated for by tonic accommodation.
Fig 2. Regression plot for TA-corrected AS and AsFac test
Commercial Relationships: Chunming Liu, None; Chris Chase,
None; Stefanie A. Drew, None; Efrain Castellanos, None; Amy
Escobar, None; Eric Borsting, None; Lawrence R. Stark, None
Support: NIH Grant EY021021
Program Number: 4260 Poster Board Number: B0297
Presentation Time: 8:30 AM - 10:15 AM
Larger Tonic Accommodation Correlates with Better Focus at
Near for Symptomatic Graduate School Students
Chris Chase1, Stefanie A. Drew3, Amy Escobar1, Chunming Liu1,
Efrain Castellanos1, Lawrence R. Stark2, Eric Borsting2. 1College of
Optometry, Western University of Health Sciences, Pomona, CA;
2
Southern California College of Optometry, Fullerton, CA;
3
California State University, Northridge, Northridge, CA.
Purpose: Under stimulus-free conditions, tonic accommodation (TA)
adopts a resting posture of about 1.5 D, although studies have shown
considerable individual variability. Models developed in the 1980’s
suggested that TA contributes little to the closed-loop
accommodation response (AR), but empirical research on this issue
has been sparse. This study examines the relationship between TA
and AR in symptomatic and asymptomatic graduate students.
Methods: Students from Western University of Health Sciences
completed three tasks using an open-field WAM-5500 infrared
autorefractor under monocular viewing conditions. First, continuous
2-min recordings were made to assess AR at 0, 2, 3, 4, and 5 D.
Second, after 5-min of dark adaptation, TA was recorded for 2-min.
Third, continuous recordings were made while reading 20/50 text for
10-min at 3 D. Participants were screened for normal visual acuity,
no significant ocular pathology, no strabismus, normal stereopsis, and
no significant uncorrected refractive error. Near-work symptoms
Figure 1. Accommodation S-R Functions for High and Low
symptomatic groups.
Commercial Relationships: Chris Chase, None; Stefanie A. Drew,
None; Amy Escobar, None; Chunming Liu, None; Efrain
Castellanos, None; Lawrence R. Stark, None; Eric Borsting, None
Support: EY021021
Clinical Trial: NCT01329848
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Program Number: 4261 Poster Board Number: B0298
Presentation Time: 8:30 AM - 10:15 AM
The Dynamic Accommodative Response with the Binocular openfield autorefractor and a Movable Real Target
Shinji Arai1, Hiroshi Uozato1, 2, Masakazu Hirota1. 1Department of
Visual Science, Kitasato University Graduate School of Medical
Sciences, Kanagawa, Japan; 2Department Orthoptics and Visual
Sciences, Kitasato University School of Allied Health Science,
Kanagawa, Japan.
Purpose: To evaluate the dynamic characteristic of accommodation
in the open field and real target using new device WMT-1
Methods: Fourteen volunteers (6 men and 8 women; mean ±
standard deviation age, 23.9 ± 4.0 years; range, 19 to 33 years)
participated in our study. All subject had a visual acuity 20/20 or
better and normal ocular health. Each subject’s accommodative
response was measured by target moving system WMT-1 (Grand
Seiko Co., Ltd, Hiroshima, Japan) dynamically. The WMT-1 is a new
device that is connected to the WAM-5500 open-field autorefractor.
It can move a target optionally from 0.2 to 1.0 meter and measure
refraction every 0.2 second. We made shape of the cross as a visual
target, displayed it in iPad (Apple Inc., Cupertino, CA).
We evaluated three difference movements that had been programmed
on the WMT-1.
First, the constant diopter triangle drive. Second, constant velocity
triangle drive. Third, diopter sin drive. We measured dynamically
accommodative response in visual target distance from 1.0 meter to
0.2 meter. We compared maximum quantity of accommodative
response and among three movements.
Results: The maximum quantity of accommodative response of
Diopter Sin Drive became larger than Constant Velocity Triangle
Drive (p < 0.05, Scheffe test). However, statistical significantly
difference was not found to other comparison.
Accommodative response related to movement of visual target.
Conclusions: We could measure dynamic characteristic of
accommodation in the open field and real target using the WMT-1.
The accommodation is evaluated at a definite point conventionally.
The WMT-1 is useful to evaluate the dynamic characteristic of
accommodation, because it can measure not only maximum quantity
of accommodative response but also process of accommodative
response.
Commercial Relationships: Shinji Arai, None; Hiroshi Uozato,
None; Masakazu Hirota, None
Program Number: 4262 Poster Board Number: B0299
Presentation Time: 8:30 AM - 10:15 AM
Suppression in the accommodative response to short-duration
changes in dioptric stimulus
Alistair P. Curd, Karen M. Hampson, Edward Mallen. Bradford
School of Optometry and Vision Science, University of Bradford,
Bradford, United Kingdom.
Purpose: To investigate whether suppression of the accommodation
response (AR) would be observed when a dioptric stimulus
performed a step-change, followed by an inverted step-change within
the latency time for AR. Results would be relevant to models of
accommodation and nearwork.
Methods: A monocular adaptive optics apparatus displayed a target
to participants, and accommodation was recorded using a ShackHartmann wavefront sensor. A deformable mirror rapidly changed
the dioptric stimulus provided by the target. The baseline vergence of
the target was −2D at the eye. An initial step-change in the stimulus
was followed by a second, inverted step, before the stimulus returned
to the baseline. Initial steps were of 1D or 2D in either direction;
intervals between the steps ranged from 0.05s to 0.5s. The stimulus
settings were randomised in order. The six participants (aged 21-26)
observed every stimulus condition five times, through their dominant
eye. A Badal optometer arrangement was used to eliminate a size cue
and audible cues from the system were masked with auditory input
through headphones. Timings of the first change in the stimulus were
randomised.
Results: Whether accommodation was responding to the first or
second change in the stimulus affected the peak AR (p<0.05 with ttests, correcting for multiple comparisons).
For 0.2s intervals between the changes in stimulus, accommodation
and disaccommodation responses were suppressed when responding
to the first step change, relative to the second (p<0.05). These mean
decreases in the peak AR were 0.13D, 0.18D and 0.10D for 2D
disaccommodative (DS) and 1D and 2D accommodative stimuli
(AS), relative to the baseline (from peaks of 0.31D, 0.45D and 0.37D,
respectively).
1D DS from the baseline required a longer interval between steps
(0.25s) to elicit a response than did 2D DS, 1D AS and 2D AS.
Changes in stimulus with intervals between 0.4s and 0.5s also
significantly affected AR (p<0.05).
Conclusions: The accommodation system responds to changes that
occur and are subsequently inverted well within its latency
period.The response to the initial change in stimulus can be
suppressed by a second change well within the latency. Changes in
stimulus during onset may also affect the AR. During the latency,
information from 200ms from the first change in stimulus, onwards,
is used to determine the AR. Information prior to this is used, but less
influential.
Commercial Relationships: Alistair P. Curd, None; Karen M.
Hampson, None; Edward Mallen, None
Support: EPSRC grants EP/D036550/1 and EP/G015473/1
Program Number: 4263 Poster Board Number: B0300
Presentation Time: 8:30 AM - 10:15 AM
Accommodation induced variations of ocular axial length and
retinal thickness measured with SD-OCT
Chuanqing Zhou, Shanhui Fan, Zhe Chen, Xinyu Chai. Biomedical
Engineering, Shanghai Jiao Tong University, Shanghai, China.
Purpose: To measure and analyze the variations of the ocular axial
length and retinal thickness during ocular accommodation by spectral
domain optical coherence tomography (SD-OCT).
Methods: A custom-built dual channel SD-OCT was developed for
measurement of the ocular axial length and retinal imaging. The
scans were performed by the same experienced operator. All eyes
were studied in the relaxed and 5D accommodated states. During the
imaging, the subjects were asked to fixate on a Maltsecross visual
target and to see it clearly. The thickness between ILM and RPE and
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
its change caused by accommodation was calculated based on the
acquired image.
Results: Repeated measurements were taken in each accommodative
state. Compared with relaxed state (0D), the mean thickness variation
around the central fovea was 7.4957±8.3616 μm at 5D
accommodation. In further study, we will collect more data to
analyze the variations of axial length and retinal thickness.
Conclusions: Preliminary result showed that the thickness between
ILM and RPE in macular has a slight change during accommodation.
Commercial Relationships: Chuanqing Zhou, None; Shanhui
Fan, None; Zhe Chen, None; Xinyu Chai, None
Support: the National Basic Research Program of China
(2011CB707504), National Natural Science Foundation of China
(81171377)
Program Number: 4264 Poster Board Number: B0301
Presentation Time: 8:30 AM - 10:15 AM
The Effect Of Age On The Lens Ultrastructure During
Accommodation As Measured Using Slit Lamp Photos And
Wave Front Analysis
Rebecca K. Zoltoski1, Elizabeth Wyles1, Jennifer S. Harthan1, Jer R.
Kuszak2. 1Illinois College of Optometry, Chicago, IL; 2LensAR,
Orlando, FL.
Purpose: During dynamic focusing, the shape, as well as the ultrastructure of the lens is changed. We have hypothesized that unique
structural features and organization of fiber cells enables them to
interface at the sutures resulting in a change in surface curvature of
the lens, as well as an increase in thickness, allowing near focus to
occur. We are reporting extended data on lens slit lamp photos, OCT
of lens thickness changes, and sequential ray tracing analysis of the
patterns associated with the lens sutures to provide additional insight
into the importance of the ultra-structure of the lens in the
accommodative process.
Methods: OCT (Visante™), wavefront analysis (iTrace™), and slit
lamp photos (Haag Streit, 16X magnification, dilated eye) were
collected on the right eye of normal subjects, between the ages of 7 63 (n=30). Accommodation was stimulated using minus lenses in
front of the viewing eye in 2.5 D increments until the subject could
no longer clearly view the target. For the photos a prism system was
used to keep the eye appropriately oriented. The objective
accommodative response was calculated as the change from a
distance measurement refractive value. ImageJ (NIH) was used to
analyze the area of the sutural components. Data were analyzed using
Systat v11 to correlate accommodative response (AR) with total
HOA, SA and the foil patterns, as well as changes in slit lamp suture
areas. Spearman Rank Correlation coefficients and p values are
presented.
Results: Lens thickness increases by 0.13 ± 0.05 μm/D during
accommodation. The total foil aberration pattern was correlated with
AR (r2=0.5, p=0.04). There was a decrease in suture band thickness
that correlated with the AR (r2=-0.5, p<0.001).
Conclusions: Regardless of age, increase in accommodative response
results in changes in the ultra-structure of the lens, as evidenced by
the decrease in area of the dark central region of the suture and in the
total foil patterns. Further analysis of these changes will provide
further insight into the anatomical basis of accommodation.
Commercial Relationships: Rebecca K. Zoltoski, None; Elizabeth
Wyles, None; Jennifer S. Harthan, None; Jer R. Kuszak, LensAR,
Inc. (C)
Support: NIH Grant EY021015-01 and ICO RRC
Program Number: 4265 Poster Board Number: B0302
Presentation Time: 8:30 AM - 10:15 AM
Do Higher Order Aberrations Affect the Magnitude of Odd-error
Temporal Stimuli to Accommodation?
Sangeetha Metlapally1, Jianliang Tong2, Humza J. Tahir3, 1, Clifton
M. Schor1. 1School of Optometry, University of California at
Berkeley, Berkeley, CA; 2Brain Trauma Foundation, New York, NY;
3
University of Manchester, Manchester, United Kingdom.
Purpose: Fincham proposed that microfluctuations of
accommodation produced a temporal hunting cycle for detecting the
direction to accommodation (odd-error signal) for steps upto 2.5 D
(upper defocus limit). This notion assumes that accommodation is
performing contrast discrimination that is affected by spatial
frequency (SF), the magnitude of defocus (Green & Campbell, 1965)
and higher order aberrations (HOAs), which influence retinal image
quality. This study computes the impact of HOAs on signal strength
produced by microfluctuations (Weber fraction) for responding to
accommodative stimuli within the upper defocus limit.
Methods: We presented step-stimuli (1-3 D) for accommodation and
disaccommodation, at baseline accommodation of 3 D. The stimulus
was a maltese spoke. Wavefront aberrations were measured using a
Shack-Hartmann wavefront sensor using a 4 mm artificial pupil. The
direction of initial responses was noted and d-prime (d’) analysis
used to evaluate the detectability of the correct direction to
accommodate. We defined the upper defocus limit for each subject
where d’ was 1. The Modulation Transfer Function was derived from
Point Spread Functions computed from the wavefronts for 1 D and
2.5 D step-stimuli, at 2 and 4 cycles per degree (cpd), with and
without HOAs. Microfluctuations were estimated from the standard
deviation of the wavefronts at baseline. Weber fractions were derived
from retinal image contrast changes due to microfluctuations.
Results: As step defocus increased, accommodation only had
medium (4 cpd) and low (2 cpd) SF available to discriminate contrast
changes produced by microfluctuations. At 4 cpd, the Weber fraction
is higher but the overall contrast is low, and vice versa at 2 cpd.
HOAs generally reduced contrast changes from microfluctuations,
and to a greater extent at higher SF or defocus.
Conclusions: Empirical measures demonstrated that
microfluctuations of accommodation are potentially useful for
defocus values less than 2.5 D, where Weber fractions at 2 cpd and 4
cpd exceed detection thresholds. HOAs perhaps serve to marginally
diminish the effectiveness of microfluctuations in odd-error signal
detection under these conditions.
Commercial Relationships: Sangeetha Metlapally, None;
Jianliang Tong, None; Humza J. Tahir, None; Clifton M. Schor,
None
Support: NIH EY017678 to CMS and NEI K12EY017269 to SM
(BCSDP)
Program Number: 4266 Poster Board Number: B0303
Presentation Time: 8:30 AM - 10:15 AM
Impact of pupil amplitude apodization on through-focus image
quality with spherical aberration
Hae Won Jung1, 2, Len Zheleznyak1, 2, Geunyoung Yoon2, 1. 1The
Institute of Optics, University of Rochester, Rochester, NY; 2Flaum
Eye Institute, University of Rochester, Rochester, NY.
Purpose: It has long been known that the Stiles-Crawford effect, the
intrinsic pupil amplitude apodization of the eye, is effective for
enhancing retinal image quality. The goal of this study was to
investigate the impact on through-focus image quality (TFIQ) of
manipulating the pupil amplitude apodization function in
combination with multifocal presbyopic corrections with spherical
aberration (SA).
Methods: TFIQ with SA was evaluated by optical bench testing and
visual performance measurements in monochromatic light (550nm).
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
The optical bench system consisted of a model eye with phase-plate
induced SA, a liquid crystal spatial light modulator to control pupil
apodization, and a camera for imaging a tumbling E letter chart.
TFIQ was quantified by calculating the correlation coefficient
between a reference image (without SA and apodization) and
captured through-focus images (0 to 2.5D with 0.1D step). Pupil
apodization was modeled as a Gaussian function with various sigma
values (0.5 to 2.0mm). Through-focus visual acuity was measured in
2 cyclopleged subjects at distance, intermediate and near object
distances (0, 1 and 2D). Both optical bench testing and visual
performance were carried out with ±0.2µm SA over a 4mm artificial
pupil.
Results: Introducing Gaussian apodization improved distance image
quality, regardless of sign of SA, by 7-12% for sigma ranging from
0.5 to 2.0mm. At intermediate (1D) image quality, the negative SA
case had a larger improvement (9-18%) than the positive SA case (711%) for sigma ranging 0.5 to 2.0mm. For near (2D), the
improvement with negative SA was even larger (14-33%) while
positive SA showed no improvement. Visual benefits with
apodization were also found. Pupil apodization with sigma=0.5 led to
a 1.0, 2.6 and 4.5 line improvement in visual acuity at 0, 1 and 2D,
respectively, in the presence of negative SA. For positive SA, visual
acuity improved by 1.0, 1.8 and 0.1 lines, respectively.
Conclusions: Pupil amplitude apodization led to a significant
improvement in through-focus image quality, especially with
negative SA. This finding suggests that halos and glare induced by
multifocal presbyopic corrections can be reduced with appropriate
pupil amplitude apodization.
Commercial Relationships: Hae Won Jung, None; Len
Zheleznyak, None; Geunyoung Yoon, Bausch & Lomb (F), Johnson
& Johnson (F), Allergan (C), Staar Surgical (C), CIBA Vision (F),
Acufocus (C)
Support: NIH Grant EY014999, Unrestricted Grant from Research
to Prevent Blindness, NYSTAR/CEIS, Bausch & Lomb
Program Number: 4267 Poster Board Number: B0304
Presentation Time: 8:30 AM - 10:15 AM
Contribution of shape and gradient index to the spherical
aberration of donor human lenses
Judith Birkenfeld, Alberto de Castro, Susana Marcos. CSIC-Instituto
de Optica, Madrid, Spain.
Purpose: The relative contribution of crystalline lens geometry and
gradient index (GRIN) to its spherical aberration (SA) and its agerelated changes is unknown. We investigated these relationship using
Optical Coherence Tomography (OCT) and Laser Ray Tracing
(LRT).
Methods: 11 ex vivo human lenses (22-71 years) from an eye bank
were imaged in 3D with a custom OCT to obtain optical path
differences. The shape of the lens surfaces was extracted from the
images using surface segmentation and Zernike polynomial fitting.
The lens power was measured using LRT for 2 and 4-mm pupil
diameters. The 3D GRIN was estimated by means of an optimization
method based on genetic algorithms (de Castro et al. OE 2010),
which searched for the parameters of a 4-variable GRIN model that
best fits the distorted posterior lens surface of the lens in 18 different
meridians. The SA of the lenses was estimated by computational ray
tracing, assuming both a homogeneous index and the estimated
GRIN.
Results: Geometrical data of all lenses were reconstructed using 3D
OCT images. Anterior radius of curvature and asphericity varied
widely across lenses (6.1 to 11.3 mm, and -9.9 to 5.6, respectively),
and were rather constant for the posterior surface (mean: 5 mm and 0.3, respectively). Lens power ranged from 34D (younger lens) to
24D (older lens). In 10/11 lens power decreased with pupil diameter,
revealing a negative spherical aberration. Lens thickness (ranging
from 3.8 to 5.2 mm) increased and mean group refractive index
(ranging from 1.392 to 1.407) decreased slightly with age. The
reconstructed GRIN showed surface refractive index values between
1.368 and 1.376, nucleus refractive index values between 1.403 and
1.415, and an exponential decay value ranging from 1.8 to 3.4 (axial)
and from 1.9 to 5.8 (meridional). The estimated SA (from lens
geometry and index) ranged from -0.8 to 0.3 µm for the equivalent
refractive index, and from -2.1 to -0.3 µm for the estimated GRIN.
SA shifted with age towards less negative values (slope=0.028 µm/yr
and 0.022 µm/yr assuming equivalent index or GRIN, respectively).
Conclusions: 3D OCT data and experimental power data of human
donor lenses of different ages allowed reconstruction of the lens
GRIN and evaluation of external geometry and GRIN contribution to
the lens spherical aberration. GRIN shifted the SA towards negative
values in all cases and played a role in the age-related shift of SA.
Commercial Relationships: Judith Birkenfeld, None; Alberto de
Castro, None; Susana Marcos, Essilor (F), PCT/ES2012/070185 (P)
Support: FIS2008-02065, FIS2011-25637 (Spanish Government)
and ERC 2011 Advanced Grant 294099 (European Research
Council) to SM, CSIC JAE Program Fellowship to JB.
Program Number: 4268 Poster Board Number: B0305
Presentation Time: 8:30 AM - 10:15 AM
Crystalline lens thickness determines transverse chromatic
aberration
Yun Chen, Frank Schaeffel. Section of neurobiology of the Eye,
Institute for Ophthalmic Research, Tuebingen, Germany.
Purpose: To describe the magnitude and variability of transverse
chromatic aberration (TCA) in the human eye, and to identify the
ocular parameters that might determine its magnitude.
Methods: Two different psychophysical procedures were used to
quantify TCA. First, a red and a blue square, presented on a black
screen, had to be matched in size by the subjects with their right eyes,
using the arrow keys on keyboard. Second, two filled red or blue
squares, flickering on top of each other at 2 Hz, had to be adjusted in
brightness and in size to minimize the perceived flicker by subjects.
Biometric ocular parameters in the right eyes were measured with a
commercially available low coherence interferometer, the Lenstar LS
900 (Haag Streit, Switzerland). Corneal power, thickness, anterior
chamber depth, lens thickness, vitreous chamber depth and axial
length were correlated to psychophysical date. Sixteen subjects with
no ocular pathologies other than refractive errors, with ages ranging
from 22 to 58 years, participated in the study.
Results: TCA varied widely among subjects, as was evident from the
perceived differences between the red and the blue square which
ranged from 0 to 3.2%. The two different psychophysical procedures
to measure TCA provided highly correlated results, suggesting that
no major confounders existed. The measurements of TCA were
affected neither by changes in brightness of the blue or red nor by
individual refractive errors. Comparing to optical parameters in the
subjects’ eyes, only lens thickness was significantly correlated to
TCA (p<0.01). However, since lens thickness and the gradient index
structure in the lens both change with age, inter-individual
differences in TCA could just be due to differences in age.
Conclusions: The high inter-individual variability in TCA is largely
determined by lens thickness. Since age is the major factor
determining lens thickness, TCA increases inevitably with age.
Commercial Relationships: Yun Chen, None; Frank Schaeffel,
None
Program Number: 4269 Poster Board Number: B0306
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Presentation Time: 8:30 AM - 10:15 AM
Prediction of human crystalline lens power and spherical
aberration using an anatomically-based discrete shell model
Fabrice Manns1, 2, Arthur Ho3, 4, Jean-Marie A. Parel1, 5.
1
Ophthalmic Biophysics Center, Bascom Palmer Eye Inst, Univ of
Miami, Miami, FL; 2Department of Biomedical Engineering,
University of Miami College of Engineering, Coral Gables, FL;
3
Brien Holden Vision Institute, Sydney, NSW, Australia; 4School of
Optometry and Vision Science, University of New South Wales,
Sydney, NSW, Australia; 5Vision Cooperative Research Centre,
Sydney, NSW, Australia.
Purpose: To develop an anatomically-correct aspheric discrete
model of the human crystalline lens that predicts power and spherical
aberration and the contribution of the refractive index gradient.
Methods: A continuous and a discrete model of a 30 year old relaxed
human lens were developed. The shape was modeled using data from
Dubbelman et al (Vis Res, 2001): Ant Radius=11.10mm; Ant
Asphericity=-3.05; Post Radius = -5.82mm; Post Asphericity=-0.795;
Thickness=3.69mm. In the continuous model, the refractive index
gradient is represented as a set of aspheric iso-indicial surfaces with
radius of curvature R(z) and asphericity Q(z) that vary linearly from
the lens equator to the value at the surface. The axial refractive index
follows a power-dependence in each half of the lens (Kasthurirangan
et al, IOVS 2008): n(z)=1.41-0.032×(z/t)4, where t is the anterior or
posterior half-thickness and z is the distance, both measured from the
equator. The discrete shell model was created by sampling isoindicial surfaces of the continuous model at regularly spaced
intervals. The ith shell of a model with K shells has thickness
tK=tlens/K, is located at position zi = i*tK, radius Ri=R(zi), asphericity
Qi=Q(zi), and is surrounded by refractive indices ni-1=n(zi-1) and
ni=n(zi). The number of shells ranged from K=6 to K=3000. The
contribution of each surface to lens power and Seidel primary
spherical aberration was calculated from a paraxial ray trace. The
contributions were plotted as a function of axial position and summed
to provide the Seidel wavefront aberration coefficient W040, and total
power contribution Psum. The power Psum was compared to the
effective power Peff.
Results: The spherical aberration coefficient and lens power
converge as the number of shell increases. The asymptotic values
were W040=0.053mm-3, Psum=22.2D, and Peff=22.3D. For lens power,
the number of shells required to reach 90%, 95% and 99% of the
asymptote are 20, 40, and 200. For spherical aberration the values are
160, 320, and approx. 1000. The contributions of the anterior and
posterior halves of the lens were -0.015mm-3 and 0.068mm-3.
Conclusions: The power and spherical aberration of the crystalline
lens can be predicted using a discrete model with tightly packed
shells.The discrete model allows calculation of contributions of
specific regions of the lens to total spherical aberration from a
paraxial ray trace.
Commercial Relationships: Fabrice Manns, None; Arthur Ho,
None; Jean-Marie A. Parel, CROMA (F), InnFocus (F), Abeamed
(F), University of Miami (P)
Support: NIH Grants R01EY14225, R01EY021834, and Center
Grant P30EY14801; Australian Government CRC Scheme (Vision
CRC); Florida Lions Eye Bank; an unrestricted grant from Research
to Prevent Blindness; Henri and Flore Lesieur Foundation (JMP).
Program Number: 4270 Poster Board Number: B0307
Presentation Time: 8:30 AM - 10:15 AM
Age-related Stiffening of Human Lens Measured by In Vivo
Brillouin Microscopy
Sebastien Besner1, 2, Giuliano Scarcelli1, 2, Roberto Pineda3, Seok H.
Yun1, 2. 1Department of Dermatology, Harvard Medical School,
Boston, MA; 2Wellman Center for Photomedicine, Massachusetts
General Hospital, Boston, MA; 3Department of Ophthalmology,
Massachusetts Eye and Ear Infirmary, Boston, MA.
Purpose: The loss of accommodation power with age is thought to
be related to the increase of the stiffness of the crystalline lens. More
recently, evidences have shown that the change in the stiffness
gradient may also play a dominant role in accommodation amplitude.
In order to investigate the contribution of lens sclerosis to loss of
accommodation with age, we present a novel optical, non-contact and
non-destructive method based on Brillouin scattering, which
measures the local elastic modulus of the crystalline lens in vivo with
micron size resolution.
Methods: Brillouin confocal microscopy was performed on 5 dilated
eyes (2.5% phenylephrine and 0.5% tropicamide) of 5 patients with
an age range of 23 to 47 years. The Brillouin spectral shift, which is
proportional to the longitudinal modulus of elasticity, was acquired
along the optical axis of the crystalline lens with an axial resolution
of about 60 microns and a lateral resolution of less than 10 microns.
Ongoing study will include 10 eyes from 10 patients with age ranging
between 20 and 60 years.
Results: At all ages, the elastic modulus was found to increase from
the lens cortex to the nucleus with a general steeper increase in the
posterior part of the lens. The overall lens stiffness was found to
increase with age (p<0.05). This is mainly due to the growth of the
stiffer nucleus portion of the lens (R=0.91) and by the increase of the
stiffness gradient from the cortex to the nucleus (R=0.65). Maximum
elastic modulus (in the nucleus) and minimal elastic modulus (in the
cortex) revealed no statistically significant age dependency.
Conclusions: Elastic modulus of the human crystalline lens was
measured for the first time in vivo by using confocal Brillouin
microscopy. For the age range of 23 to 47 years old, we found that
the lens nucleus was stiffer than the lens cortex. We also observed a
statistically significant increase of the stiffness of the lens with age.
However, the observed age-related stiffening was not due to an
increase of peak modulus with age, but rather to a variation of the
spatial distribution of the elastic modulus inside the aging lens, where
both nucleus thickness and stiffness gradient might play a role.
Total stiffness variation with age of the human crystalline lens along
the optical axis. Error bars represent the sum of elastic modulus
determination by Brillouin scattering and positioning errors.
Commercial Relationships: Sebastien Besner, None; Giuliano
Scarcelli, massachusetts general hospital (P); Roberto Pineda,
Amgen (C), Angiotech (C); Seok H. Yun, Massachusetts General
Hospital (P)
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Support: NIH grant P41-EB015903, NSF grant CBET-0853773 ,
Harvard Clinical and Translational Science Center (NIH UL1RR025758), American Society for Laser Medicine and Surgery
Program Number: 4271 Poster Board Number: B0308
Presentation Time: 8:30 AM - 10:15 AM
Effect of Temperature on Lens Power, Anterior and Posterior
Surface Lens Curvatures and Force during Simulated
Accommodation in Cynomolgus Monkeys
Jean-Marie A. Parel1, 3, Bianca M. Maceo1, 2, Cornelis J. Rowaan1,
Fabrice Manns1, 2, Esdras Arrieta1. 1Ophthalmic Biophysics Center,
Bascom Palmer Eye Institute, Univ. of Miami Miller School of
Medicine, Miami, FL; 2Biomedical Optics and Laser Laboratory,
Dept of Biomedical Engineering, College of Engineering, University
of Miami, Miami, FL; 3Vision Cooperative Research Centre, Sydney,
NSW, Australia.
Purpose: To determine whether temperature has an effect on the
accommodative response of primate lenses during simulated
accommodation in a lens stretcher.
Methods: Lens shape was measured during ex vivo simulated
accommodation on 4 cynomolgus monkey (4.5-6.9 years) lenses from
4 donors (PMT 9.5+/-11 hours). Tissue samples were mounted in the
EVASII lens stretching system (Ehrmann et al, Clin Exp Opt, 2008)
and stretched in a step-wise fashion (0.25mm/step up to 2.5mm
radially). In EVAS II, the tissue is immersed in preservation medium
(DMEM) throughout the experiment. A temperature controller with
thermocouple feedback was used to control the temperature of the
medium. For each lens, a stretching experiment was first performed
at 24°C (room temperature). At the end of the experiment, the
temperature of the medium was increased to 35°C (ocular
temperature). A second stretching experiment was then performed.
The power, anterior and posterior curvatures, and thickness of the
lens, and the force exerted to stretch the lens were measured at each
step at both temperatures. The change in lens power, thickness, radius
and the maximum force produced at the two temperatures were
compared.
Results: At 25°C, the average+/-SD of the change was 19.5+/-2.1D
for lens power, 0.58+/-0.09mm for lens thickness, -2.54+/-0.74 for
lens anterior radius; -0.94+/-0.12mm for lens posterior radius. The
maximum force was 1.50+/-0.22g. At 35°C, the average+/-SD of the
change was 18.1+/-2.7D for lens power, 0.57+/-0.09mm for lens
thickness, -2.46+/-0.86mm for lens anterior radius; -0.91+/-0.29mm
for lens posterior radius. The maximum force was 1.30+/-0.26g.
Conclusions: Within the range of temperatures tested in this study
(25-35°C), temperature does not have significant effect on the
changes in lens shape, power and force during simulated
accommodation in a lens stretcher.
Commercial Relationships: Jean-Marie A. Parel, CROMA (F),
InnFocus (F), Abeamed (F), University of Miami (P); Bianca M.
Maceo, None; Cornelis J. Rowaan, None; Fabrice Manns, None;
Esdras Arrieta, None
Support: NIH Grant R01EY14225, R01EY021834, F31EY021444
(NRSA Individual Predoctoral Fellowship [BM]), and Center Grant
P30EY14801; Australian Government CRC Scheme (Vision CRC);
FloridaLions Eye Bank; an unrestricted grant from Research to
Prevent Blindness; Henri and Flore LesieurFoundation (JMP)
Program Number: 4272 Poster Board Number: B0309
Presentation Time: 8:30 AM - 10:15 AM
Lens Spherical Aberration Changes in Cynomolgus Monkeys
during Simulated Accommodation in a Lens Stretcher
Bianca M. Maceo1, 2, Fabrice Manns1, 2, Alberto de Castro3, Stephen
Uhlhorn1, Esdras Arrieta1, Susana Marcos3, Jean-Marie A. Parel1, 4.
1
Ophthalmic Biophysics Center, Bascom Palmer Eye Institute,
Miami, FL; 2Biomedical Optics and Laser Laboratory, Department of
Biomedical Engineering, University of Miami College of
Engineering, Coral Gables, FL; 3Instituto de Óptica, Consejo
Superior de Investigaciones Científicas, Madrid, Spain; 4Vision
Cooperative Research Centre, Sydney, NSW, Australia.
Purpose: To quantify the difference in spherical aberration (SA) of
cynomolgus monkey lenses in the accommodated and
unaccommodated state.
Methods: A Laser Ray Tracing system (LRT) was used to obtain SA
measurements on 2 cynomolgus monkey lenses from 2 donors (4.5
and 6.9 years, PMT= 4 and 26 hours). The tissue was mounted in a
chamber filled with Dulbecco's Modified Eagle Medium inside a lens
stretcher (Ehrmann et al, Clin Exp Opt, 2008). The lens spherical
aberration was measured in the unstretched (accommodated) and
stretched (relaxed) state. The LRT delivered 51 equally-spaced
parallel rays along the vertical meridian of the lens over a total length
of 6mm. A camera mounted on a vertical position stage was placed
under the chamber containing the lens to sequentially record the spot
corresponding to each individual ray. Spot images were measured at
up 12 camera positions along the optical axis covering a range of up
to 22mm. The images were processed to determine the centroid of
each spot and calculate the corresponding ray height at each camera
position. For each camera position, the measured ray heights were
plotted as a function of entrance ray height and fit with a 3rd order
polynomial: y = A*x + B*x3. The A and B coefficients were then
plotted as a function of camera position and a linear fit was
performed. The effective focal length and Seidel spherical aberration
coefficient were extracted from the fits. A ray-trace analysis showed
that the posterior window of the chamber contributes less than 1%
error to the SA coefficient. Therefore the contribution of the window
to spherical aberration was not corrected for.
Results: The results for the two lenses are summarized in the table
below:
Conclusions: Spherical aberration in cynomolgus monkey lenses
increases in absolute value with accommodation, as found in human
and rhesus monkeys.
Commercial Relationships: Bianca M. Maceo, None; Fabrice
Manns, None; Alberto de Castro, None; Stephen Uhlhorn, None;
Esdras Arrieta, None; Susana Marcos, Essilor (F),
PCT/ES2012/070185 (P); Jean-Marie A. Parel, CROMA (F),
InnFocus (F), Abeamed (F), University of Miami (P)
Support: NIH Grant R01EY14225, R01EY021834, F31EY021444
(NRSA Individual Predoctoral Fellowship [BM]), and Center Grant
P30EY14801; Australian Government CRC Scheme (Vision CRC);
Florida Lions Eye Bank; an unrestricted grant from Research to
Prevent Blindness; Henri and Flore Lesieur Foundation (JMP),
Spanish Government FIS2011-25637, European Research Council
ERC-2011-AdG-294099; CSIC I3P Program.
Program Number: 4273 Poster Board Number: B0310
Presentation Time: 8:30 AM - 10:15 AM
Comparison between in vivo and in vitro age-related loss of
accommodation in rhesus monkeys
Mark Wendt, Adrian Glasser. College of Optometry, University of
Houston, Houston, TX.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Purpose: The progressive age related loss of accommodation in
rhesus monkeys has been studied in vivo or with in vitro mechanical
stretching to simulate disaccommodative changes in enucleated eyes
(in vitro accommodation). No prior study had directly compared the
two approaches with the same eyes. Here a direct comparison is made
between the age-related in vivo loss of accommodation in rhesus
monkeys and in vitro mechanical stretching induced
disaccommodative changes in the same eyes after enucleation.
Methods: Experiments were performed on 10 iridectomized
monkeys aged between 10 and 25 years. Accommodation was
stimulated with intravenous (i.v.) pilocarpine and refraction measured
statically with a Hartinger coincidence refractometer and dynamically
with infrared photorefraction. In one subsequent i.v. pilocarpine
experiment with each monkey, accommodative changes in lens
diameter were measured dynamically. Following euthanasia one eye
each from nine of the monkeys was dissected and stretched radially
step-wise while measuring changes in lens focal length and diameter
to attempt to achieve the largest changes possible.
Results: In vivo accommodative amplitudes decreased linearly with
age from 12.38 D to 3.38 D (n = 10; r2 = 0.9097; p < 0.0001) and
accommodative decrease in lens diameter decreased linearly with age
from 0.703 mm to 0.327 mm (n = 9; r2 = 0.8097; p = 0.0009). In vitro
accommodative change in lens power decreased linearly with age
from 16.9 D to 6.16 D (n = 9; r2 = 0.8805; p = 0.0001) and in vitro
accommodative change in lens diameter decreased linearly with age
from 1.43 mm to 0.73 mm (n = 9; r2 = 0.62; p < 0.0009). In vitro
accommodation with the maximum radial stretch overestimated in
vivo accommodation on average by 2.94 ±1.604 D without optical
compensation for ocular optical effects. In vitro accommodative
changes in lens diameter with the maximum radial stretch
overestimated the in vivo accommodative changes in lens diameter by
0.65 ± 0.083 mm.
Conclusions: Maximum change in power and diameter that lenses
undergo with stretching overestimates the in vivo accommodative
changes in optical power and lens diameter. Both in vivo and in vitro
accommodation in the same eyes of rhesus monkeys show a similar
progressive age-related loss of accommodation. Since in vitro
accommodation does not rely on ciliary muscle function, this
supports a lenticular basis for presbyopia in rhesus monkeys.
Commercial Relationships: Mark Wendt, None; Adrian Glasser,
None
Support: NEI Core Grant P30 EY007551 to UHCO
Program Number: 4274 Poster Board Number: B0311
Presentation Time: 8:30 AM - 10:15 AM
Age-related loss of accommodation in rhesus monkeys is
associated with an age-related increase in lens stiffness
Adrian Glasser, Mark Wendt. College of Optometry, University of
Houston, Houston, TX.
Purpose: It is generally agreed that presbyopia in humans is caused
by an age-related increase in lens stiffness. Rhesus monkeys develop
presbyopia with a similar relative age-course as humans and are used
as an animal model for human presbyopia, although prior studies
have suggested differences in the aetiology of presbyopia between
humans and monkeys. Here, the age-related loss of accommodation
from in vivo and in vitro experiments is correlated with the stiffness
of the same lenses to ascertain the relationship between presbyopia
and lens stiffness in rhesus monkeys.
Methods: Experiments were performed on 10 iridectomized rhesus
monkeys aged between 10 and 25 years. Accommodation was
stimulated with intravenous pilocarpine and refraction measured with
a Hartinger and infrared photorefraction and accommodative changes
in lens diameter measured with slit-lamp videography. After
euthanasia, one eye each from nine monkeys was used for
mechanical stretching experiments in which changes in lens focal
length and lens diameter were measured as a function of the applied
radial stretch. Lenses were then isolated and squeezed in six 100 µm
steps while measuring the applied force.
Results: In vivo accommodative amplitudes decreased linearly with
age (r2 = 0.9097; p < 0.001) and accommodative change in lens
diameter decreased linearly with age (r2 = 0.8097; p < 0.001). With
mechanical stretching the lens power and lens diameter curves for
each lens plateaued and the maximum changes in lens power and
diameter from all lenses decreased linearly with age (r2 = 0.8805; p <
0.001 and r2 = 0.62; p < 0.001, respectively). Maximum gram force
from squeezing lenses increased exponentially with age (f = 0.0408 *
1.1658age p < 0.001). In vivo accommodation, in vivo accommodative
change in lens diameter and in vitro change in lens focal length were
significantly exponentially related (p < 0.001) to the maximum gram
force from squeezing the lenses.
Conclusions: In rhesus monkeys accommodation is lost with
increasing age, lens stiffness increases exponentially with age, in
vitro accommodation is not limited by ciliary muscle function and the
magnitudes of in vivo ocular and in vitro lenticular accommodative
changes are related to lens stiffness. These results demonstrate that in
rhesus monkeys, as in humans, presbyopia is caused by a progressive
age-related increase in lens stiffness.
Commercial Relationships: Adrian Glasser, None; Mark Wendt,
None
Support: NEI Core Grant P30 EY007551 to UHCO
Program Number: 4275 Poster Board Number: B0312
Presentation Time: 8:30 AM - 10:15 AM
Dynamic wavefront measurement of accommodation and pupil
area in response to electric stimulation of ciliary nerve in cats
Suguru Miyagawa1, 2, Toshifumi Mihashi2, 4, Yoko Hirohara1, 2, Akira
Takada1, Takao Endo2, Hiroyuki Kanda2, Tomomitsu Miyoshi3,
Takashi Fujikado2. 1Optical Engineering Laboratory, Topcon
Corporation, Itabashi-Ku, Japan; 2Dept of Applied Visual Science,
Osaka University Graduate School of Medicine, Suita, Japan;
3
Integrative Physiology, Osaka University Graduate School of
Medicine, Suita, Japan; 4Innovative Research Initiatives, Tokyo
Institute of Technology, Yokohama, Japan.
Purpose: To investigate the changes of accommodation and pupil
area elicited by electrical stimulation of the ciliary nerve, we
analyzed the wavefront aberrations (WAs) and the pupil size with a
Shack-Hartmann wavefront aberrometer (SHWA) before, during, and
after the stimulation.
Methods: Six eyes of six cats were studied under general anesthesia.
Trains of monophasic pulse (current, 0.1 to 2.0 mA; duration, 0.5
ms/phase; frequency, 5 to 40 Hz) were applied to either the lateral or
medial branch of the short ciliary nerve (Kuchiiwa, 1990). Hookshaped bipolar stimulating electrodes were made of stainless steel
with a diameter of 0.3 mm and were hooked onto the short ciliary
nerve about 5 mm from the scleral surface. We measured the
wavefront aberration for 2 seconds before, 8 seconds during, and for
20 seconds after the electrical stimulation with a compact wavefront
aberrometer (Aston University and Topcon Co). The pupillary
images were simultaneously photographed during the wavefront
measurements. The wavefront aberrations and the pupil images were
recorded at 10 Hz.
Results: The pupil dilated asymmetrically when one side of the
ciliary nerve was stimulated and dilated symmetrically when both
sides of the ciliary nerves were stimulated. The pupil was never
constricted by any stimulating parameters. Although asymmetrical
pupil dilation occurred by unilateral ciliary nerve stimulation, no
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
asymmetrical terms of the WAs were found. The accommodative
responses had an implicit time of 2 to 6 sec and an amplitude of 1 to
2 diopters. The implicit times were slower than that in humans (0.4
second, F. W. Campbell, 1960) and the cat’s response to electrical
stimulation of the LS area (1.0 second, K. Ohtsuka, 1996). After the
stimulation, accommodation decreased slowly to the original state
taking >10 sec. The latencies of the accommodative responses were
always shorter than the detection limit (<100 ms).
Conclusions: The pupillary dilation was asymmetrical to the optical
axis following unilateral ciliary nerve stimulation but no
asymmetrical aberration change was found. The discrepancy may
stem from the fact that the crystalline lens has a viscoelastic property
and the asymmetric contraction of ciliary muscle might not cause the
optical asymmetry.
Commercial Relationships: Suguru Miyagawa, Topcon
Corporation (E); Toshifumi Mihashi, Topcon Corp. (F); Yoko
Hirohara, Topcon corp. (E); Akira Takada, None; Takao Endo,
None; Hiroyuki Kanda, Nidek Co., Ltd. (P); Tomomitsu Miyoshi,
None; Takashi Fujikado, Nidek (P)
Program Number: 4276 Poster Board Number: B0313
Presentation Time: 8:30 AM - 10:15 AM
Macular function contributes to the near vision performance in
the patients with monofocal intraocular lens: a functional
Multifocal ERG study
Xialin Liu, Yao Ni, Chang He, Li Wang, Yizhi Liu. Zhongshan
Ophthalmic Center, Sun Yat-sen University, Guangzhou, China.
Purpose: To investigate the relationship between macular function
and individual near vision performance in normal pseudophakic eyes
with monofocal intraocular lens (IOLs).
Methods: In this study, 36 eyes after standard phacoemulsification
with foldable monofocal IOLs implantation, and a postoperative
uncorrected distance visual acuity of 0.8 or better were enrolled. Best
corrected distance of visual acuity (BCVA), uncorrected near visual
acuity (UNVA) and distance corrected near visual acuity (DCNA)
were assessed. Macular function was measured by the multifocal
ERG system (VERIS; Electro-Diagnostic Imaging, Inc., Redwood
City, CA), with 103 scaled hexagons. The latencies and amplitude
densities were analyzed according to 6 concentric ring averages.
Results: All the pseudophakic eyes had a BCVA (logMAR) of 0.00
or better. Typical normal multifocal ERGs were obtained from these
eyes. There was a positive correlation between DCNA (logMAR) and
latencies of N1 in ring1(r=0.431, p=0.008). Except ring1, the other
measures of latencies and average amplitude densities (ring 2-6) from
multifocal ERG components were not correlation with DCNA.
Additionally, there were no correlations between UNVA (logMAR)
and all of the latencies and average amplitude densities.
Conclusions: Ring 1 (ranged from 0-1.5°) represented the fovea
which was responsible for sharp central vision.The data from the
bipolar cell-dominated multifocal ERG revealed slightly functional
differences between the enrolled individuals. A positive correlation
between DCNA and latencies of N1 in ring1 implied that the more
robust status of macular fovea may contribute to better DCNA. Our
finding may offer a new perspective to understand the phenomenon
of pseudo-accommodation.
Commercial Relationships: Xialin Liu, None; Yao Ni, None;
Chang He, None; Li Wang, None; Yizhi Liu, None
Program Number: 4277 Poster Board Number: B0314
Presentation Time: 8:30 AM - 10:15 AM
Changes in Add Power for Near Vision after Laser in Situ
Keratomileusis for Presbyopic High Myopia
Yukari Tsuneyoshi1, 3, Kazuno Negishi1, Miyuki Yoshida1, Megumi
Saiki1, Naoko Kato1, Ikuko Toda2, Kazuo Tsubota1. 1Ophthalmology,
Keio University School of medicine, Tokyo, Japan; 2Ophthalmology,
Minamiaoyama Eye Clinic, Tokyo, Japan; 3Ophthalmology,
Tachikawa Hospital, Tachikawa, Japan.
Purpose: To evaluate the changes in the minimal add power to attain
the best-corrected near visual acuity (add power) after laser in situ
keratomileusis (LASIK) for presbyopic high myopia.
Methods: We retrospectively analyzed 53 eyes of 41 patients who
were 45 years of age and older and had undergone LASIK for high
myopia (-6 diopters [D] and over). The add powers at 30 cm were
measured preoperatively and postoperatively.
Results: The mean patient age was 50.0 ± 4.1 years (standard
deviation [SD]); the mean power corrected by LASIK was -7.69 ±
1.10 D. The preoperative and postoperative add powers were 1.80 ±
0.60 D and 2.18 ± 0.69 D, respectively, which was a significant (P <
0.01) increase of 0.38 ± 0.60 D. In patients under 50 years (n=30), the
mean add power increased to 0.51±0.61 D, which is significantly (P <
0.01) greater than in patients 50 years and older (0.21±0.57 D),
although the powers corrected by LASIK did not differ significantly
between the groups.
Conclusions: The add power increases after LASIK performed to
treat presbyopic high myopia, especially in patients who are newly
presbyopic, probably due to the effect of the vertex distance. Our
results confirmed the importance of obtaining informed consent
regarding the apparent progression of presbyopia in such patients.
Commercial Relationships: Yukari Tsuneyoshi, None; Kazuno
Negishi, Oculentis (F); Miyuki Yoshida, None; Megumi Saiki,
None; Naoko Kato, None; Ikuko Toda, None; Kazuo Tsubota,
AcuFocus, Inc (C), Allergan (F), Bausch Lomb Surgical (C),
Functional visual acuity meter (P), JiNS (P), Kissei (F), Kowa (F),
Santen, Inc. (F), Otsuka (F), Pfizer (C), Thea (C), Echo Denki (P),
Nidek (F), Ophtecs (F), Wakasa Seikatsu (F), CEPT Company (P)
Program Number: 4278 Poster Board Number: B0315
Presentation Time: 8:30 AM - 10:15 AM
Subsurface Femto-Laser Photodisruption in the Sclera for the
Creation of Presbyopic Implant Tunnels
Aghapi mordovanakis1, 2, Larry Baitch3. 1Biomedical Engineering,
University of Michigan, Ann Arbor, MI; 2Center for Ultrafast Optical
Science, University of Michigan, Ann Arbor, MI; 3Research, Refocus
Group, Dallas, TX.
Purpose: The PresVIEWTM procedure (Refocus Group, Dallas, TX)
is a surgical ophthalmic procedure for the improvement of near visual
acuity in presbyopes. In that procedure, a precision bladed device,
scleratome, dissects the scleral tissue at a plane 400μm below the
surface of the perilimbal sclera, resulting in a tunnel into which each
of four PresVIEWTM Scleral Implants (PSI) are implanted per eye.
Our studies seek to determine the feasibility of using laser sources
similar to those used in currently-approved refractive femtolaser
platforms, for development of a laser-based method for the creation
of precise and predictable PSI tunnels.
Methods: Scleral tissue is highly scattering for the near-infrared
(NIR) wavelengths (1030-1065nm) employed by femtosecond
refractive lasers. Our approach was to focus femtosecond laser pulses
below the surface of porcine scleral sections to induce precise
disruption about the laser focal plane. We created tunnels by rasterscanning the focused laser beam while translating the tissue along the
tunnel length. We investigated the ablation efficacy at various depths
(down to 400μm) under different laser parameters (shot pattern, pulse
energy and repetition rate, lens numerical aperture). After laser
exposure, scleral tissue samples were subjected to: 1) histological
assessment to quantify uniformity of tunnel depth and collateral
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
damage to cells; 2) optical microscopy of the scleral tissue, cleared
with a 40% glucose solution after laser irradiation; and 3) mechanical
instrument probing to simulate the insertion of PSI implants.
Results: Optical microscopy of cleared sclera showed explicit
subsurface disruption when irradiated with microjoule-energy pulses
at 1030nm wavelength. The efficacy of tissue separation was
demonstrated by inserting a 1mm-wide blunt probe along tunnels of
3-4mm length. Histological assessment continued to show
improvement in accuracy and consistency of the ablated tissue plane
as the irradiation parameters were refined.
Conclusions: Given the challenges that scleral tissue presents as an
optical medium, our preliminary parametric trials of scleral
subsurface femtosecond laser ablation on ex-vivo porcine are
encouraging. These early results suggest that currently available
refractive femtolaser platforms might be adapted for the creation of
PSI tunnels. In-vivo animal experiments are necessary to assess the
clinical viability of the procedure.
Commercial Relationships: Aghapi mordovanakis, Refocus Group
(F); Larry Baitch, Refocus Group (E)
Support: Support from Refocus Group (Dallas, TX)
Program Number: 4279 Poster Board Number: B0316
Presentation Time: 8:30 AM - 10:15 AM
Electro-optic lens for correction of presbyopia
Guoqiang Li, Thomas F. Mauger. Depts of Ophthal and Vis Sci and
ECE, Ohio State University, Columbus, OH.
Purpose: A large population on the planet needs correction of near
vision with aging. To overcome the disadvantages of the existing
eyeglasses for correction of presbyopia based on area division, it is
very attractive to develop tunable electro-optic lens with high
imaging quality and large aperture. In this technique, the power can
be continuously adjusted by a small voltage across the whole
aperture.
Methods: By incorporating nanotechnology and cost-effective
microfabrication technology, we have designed and fabricated
tunable liquid crystal lenses with large aperture and large tunable
range needed for correction of presbyopia. To our knowledge, this is
the first demonstration of such a powerful device. The nanoparticles
doped in the liquid crystals provide excellent alignment of the liquid
crystals and this property eliminates the alignment layer on the
surface of the microsturctured element.
Results: We have designed and fabricated a tunable liquid crystal
lens with large aperture (over 20 mm), large tunable range (over 3
diopters) and low driving voltage. The lens shows high optical
quality. These lenses have been used to build the prototypes of
adaptive spectacles and visual simulator. Vision test results will be
shown.
Conclusions: The electro-optic tunable lenses with large aperture and
large tunable range are promising for vision correction and vision
assessment.
Model eye imaging. Left, adaptive lens off; right, adaptive lens on.
Commercial Relationships: Guoqiang Li, The Ohio State
University (E); Thomas F. Mauger, None
Support: NIH/NEI grant R01 EY020641
Program Number: 4280 Poster Board Number: B0317
Presentation Time: 8:30 AM - 10:15 AM
Tolerance to astigmatism with a small aperture corneal inlay
Abhiram S. Vilupuru1, Juan Tabernero2, Pablo Artal2. 1R&D,
AcuFocus, Inc, Irvine, CA; 2Universidad de Murcia, Murcia, Spain.
Purpose: Small aperture corneal inlays are used to extend depth of
focus in presbyopic patients. Visual outcomes depend on residual
refractive error. While the impact of defocus was already studied
(Tabernero & Artal, JCRS, 2011), we expanded their study to
investigate how much uncorrected astigmatism can be tolerated with
a small aperture corneal inlay.
Methods: We developed 20 computational eye models using data
from corneal topography, ocular axial lengths and wavefront
aberrations taken in 20 healthy presbyopic subjects (mean age 59
years, standard deviation 7 years). The axial length was adjusted to
render all eyes to be at best focus (emmetropia). A small aperture of
1.6 mm of diameter was placed at the corneal plane. The pupil of the
eye was set to 3 mm of diameter. Astigmatism was induced in steps
of 0.25 D (axis 90°) by placing a cylindrical lens at 15 mm from the
corneal axis and then the eye’s modulation transfer function (for
monochromatic light of 550 nm) was obtained for every eye from 0 D
up to 3 D of induced astigmatism. The spatial frequency that
corresponded to a modulation value of 0.2 (along the orthogonal
direction to the axis of the astigmatism) was used as an image quality
metric and calculated in every eye with and without the small
aperture.
Results: With the small aperture implanted in the cornea, the cut-off
frequencies increased significantly for all values of induced
astigmatism. On average for the 20 eyes, if 1 D of astigmatism
remained uncorrected for a pupil diameter of 3 mm (which
corresponds to a 0.2 cut-off frequency of 0.22 decimal visual acuity
units) then the equivalent value with the small aperture inlay
implanted is obtained at 1.9 D (i.e. an increasing of 0.9 D of tolerance
to astigmatism). For a different uncorrected threshold value of
astigmatism, for instance to 0.5 D, then the tolerance with the small
aperture would double up to 1 D. Since the inlay is actually an
annulus (external diameter of 3.8 mm), this tolerance would be lower
in those subjects with pupil diameters significantly larger than 4 mm.
Conclusions: The retinal image quality in eyes implanted with a
small aperture corneal inlay to extend depth of focus is affected by
the remaining uncorrected astigmatism. Although there is an
individual variability due to the particular eye’s aberrations, the
presence of the small aperture approximately doubles the typical
tolerance to astigmatism.
Commercial Relationships: Abhiram S. Vilupuru, AcuFocus (E);
Juan Tabernero, None; Pablo Artal, AMO (C), Voptica SL (P),
Voptica SL (I), AMO (F), Calhoun Vision (F), Calhoun Vision (C),
AcuFocus (C)
Support: FIS2010-14926 CSD2007-00013 4524/GERM/06
Program Number: 4281 Poster Board Number: B0318
Presentation Time: 8:30 AM - 10:15 AM
Distribution of Achromatizing Pupil Positions and First Purkinje
Reflections in a Normal Population
Silvestre Manzanera1, Juan Tabernero1, Antonio Benito1, Abhiram S.
Vilupuru2, Pedro M. Prieto1, Pablo Artal1. 1Laboratorio de Optica,
University of Murcia, Murcia, Spain; 2R&D, AcuFocus, Irvine, CA.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Purpose: Quality of vision in patients with small aperture corneal
inlays to correct for presbyopia depends on its proper centration. In
practice, the inlay is positioned on the 1st Purkinje image but if this
location is far from the foveal achromatic axis, a significant
transverse chromatic aberration could degrade retinal images. We
developed a new instrument to simultaneously measure both the 1 st
Purkinje image and the intersection of the achromatic axis with the
pupil plane.
Methods: The apparatus records images of the eye’s pupil and the 1 st
Purkinje reflection when illuminated with a semicircle of infrared
LEDs. In addition, a liquid crystal spatial light modulator produces a
small aperture conjugated to the subject’s pupil plane with a location
that can be controlled by the subject. Subjects perform a Vernier-type
alignment task by moving a 1-mm aperture over the eye’s natural
pupil to align a red target to a blue grid. Both the positions of the 1 st
Purkinje reflection and the achromatic axis intersection are
determined simultaneously. Series of data in 33 eyes with a range of
+/- 4 D refractive errors were obtained.
Results: For each subject the procedure was repeated 10 times. The
standard deviation in the measurements was below 0.18 and 0.04 mm
for the achromatic axis and 1st Purkinje positions respectively. The
average location of the achromatizing pupil, relative to the subject’s
natural pupil, was: x = 0.29 ± 0.19 mm (nasal); y = 0.09 ± 0.19 mm
(superior). These values should be compared to the average location
of the 1st Purkinje image: x = 0.34 ± 0.19 mm; y = 0.07 ± 0.07 mm.
Considered individually, the two positions were statistically different
in 8 and 16 eyes for the horizontal (x) and vertical (y) directions
respectively. The differences in the two locations were smaller than
0.4 mm for both directions in all the measured eyes.
Conclusions: We have designed and built a new instrument that
allows to measure simultaneously both the locations of the 1 st
Purkinje image and the achromatic axis intersection with the pupil
plane. On average, both locations coincide within the measurement
errors. Although there is individual variability, the maximum
differences in location did not exceed 0.4 mm in any eye. This value
should induce a modest amount of transverse chromatic aberration,
indicating that centration of the inlay on the 1st Purkinje image should
be adequate for most patients.
Commercial Relationships: Silvestre Manzanera, AMO (F), CIBA
Vision (F), CALHOUN (F), VOPTICA (I); Juan Tabernero, None;
Antonio Benito, None; Abhiram S. Vilupuru, AcuFocus (E); Pedro
M. Prieto, AMO (F), AcuFocus (F), Voptica SL (I), Voptica SL (P);
Pablo Artal, AMO (C), Voptica SL (P), Voptica SL (I), AMO (F),
Calhoun Vision (F), Calhoun Vision (C), AcuFocus (C)
Support: Supported by the Ministerio de Ciencia e Innovación,
Spain (grants FIS2010-14926 and CSD2007-00013) and Fundación
Séneca (Región de Murcia, Spain), grant 4524/GERM/06 &
AcuFocus.
Program Number: 4282 Poster Board Number: B0319
Presentation Time: 8:30 AM - 10:15 AM
Visual Simulation of Retinal Images with Various Designs of
Pinhole Contact Lenses using Ray Tracing Software
Kazuno Negishi1, Yasuyo Nishi1, Kazuhiko Ohnuma2, Kazuo
Tsubota1. 1Department of Ophthalmology, Keio Univ School of
Medicine, Shinjuku-Ku, Japan; 2Graduate School of Engineering,
Chiba Univesity, Chiba, Japan.
Purpose: To determine the optimal design of pinhole contact lenses
(PCLs) without refractive power to obtain a full range of vision from
far to near using ray tracing software.
Methods: We used five PCL designs in this study: design 1, a 2-mm
central clear zone with a 6-mm opaque zone; design 2, five randomly
positioned clear zones 2 mm in diameter in the 8-mm opaque zone;
design 3, eight randomly positioned clear zones 2 mm in diameter in
the 8-mm opaque zone. Simulated retinal images with the PCLs at 5
and 0.3 meter were obtained using an optical design software and a
Liou & Brennan eye model with an 8-mm corneal diameter, a 3-mm
pupil diameter, a -1.0-diopter refraction, and a 555-nm wavelength.
The modulation transfer functions (MTFs) also were calculated in
each condition.
Results: Among the three designs, design 3 performed the best.
Conclusions: Our results suggested that a PCL without refractive
power might be useful to obtain a full range of vision from far to near
if designed optimally, and the central clear zone may not always be
necessary for a PCL.
Commercial Relationships: Kazuno Negishi, Oculentis (F);
Yasuyo Nishi, None; Kazuhiko Ohnuma, None; Kazuo Tsubota,
AcuFocus, Inc (C), Allergan (F), Bausch Lomb Surgical (C),
Functional visual acuity meter (P), JiNS (P), Kissei (F), Kowa (F),
Santen, Inc. (F), Otsuka (F), Pfizer (C), Thea (C), Echo Denki (P),
Nidek (F), Ophtecs (F), Wakasa Seikatsu (F), CEPT Company (P)
Support: 2011FY NEDO Innovation Promotion Program 0822001
Program Number: 4283 Poster Board Number: B0320
Presentation Time: 8:30 AM - 10:15 AM
Visual Simulation of Retinal Images with Various Designs of
Pinhole Contact Lenses
Yasuyo Nishi, Kazuno Negishi, Kazuhiro Watanabe, Yuki Hidaka,
Hidemasa Torii, Megumi Saiki, Kazuo Tsubota. Ophthalmology,
Keio University School of Medicine, Tokyo, Japan.
Purpose: To determine the optimal design of pinhole contact lenses
(PCL) without refractive power to obtain a full range of vision from
far to near using a visual simulation system and to evaluate the
optical performance.
Methods: The PCL has a central clear zone in a 6.0-mm diameter
opaque zone with many minute clear zones. The total diameter and
the base curve of the PCL were 14.0 mm and 8.5 mm, respectively.
The visual simulation system consists of a model eye and a chargecoupled device camera. The different PCLs can be placed in front of
the model eye and evaluated. Visual simulations were performed
using this system at 5, 1, and 0.3 meters through a 3-mm aperture
using Landolt visual acuity (VA) charts with different PCLs
(different sized central clear zone, 2.0, 1.8, 1.6, 1.4, and 1.2 mm;
different sized minute clear zones in the opaque zone, 0.14, 0.17,
0.20, and 0.23 mm). The contrast levels of the gaps of the Landolt
VA charts in the simulated images were analyzed using Photoshop
software to determine the optimal PCL design.
Results: The PCL with a 1.4-mm central clear zone and 0.17-mm
clear zones in the opaque zone maintained the contrast of the
simulated images over 10% at all distances and had the best
performance among the tested designs.
Conclusions: Our results suggested that the PCL without refractive
power might be useful to obtain a full range of vision from far to near
if designed optimally.
Commercial Relationships: Yasuyo Nishi, None; Kazuno Negishi,
Oculentis (F); Kazuhiro Watanabe, None; Yuki Hidaka, None;
Hidemasa Torii, None; Megumi Saiki, None; Kazuo Tsubota,
AcuFocus, Inc (C), Allergan (F), Bausch Lomb Surgical (C),
Functional visual acuity meter (P), JiNS (P), Kissei (F), Kowa (F),
Santen, Inc. (F), Otsuka (F), Pfizer (C), Thea (C), Echo Denki (P),
Nidek (F), Ophtecs (F), Wakasa Seikatsu (F), CEPT Company (P)
Support: 2011FY NEDO Innovation Promotion
Program.0822001,Dated August 22nd,2011.
432 Refractive Errors, Myopia II
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Wednesday, May 08, 2013 11:00 AM-12:45 PM
TCC LL 4/5 Paper Session
Program #/Board # Range: 4549-4554
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 4549
Presentation Time: 11:00 AM - 11:15 AM
The impact of Spherical Aberration, Stiles Crawford Apodization
and Spatial Frequency on wavefront-based and subjective
refractions
Renfeng Xu1, Arthur Bradley1, Larry N. Thibos1, Gildas Marin2,
Martha Hernandez2. 1School of Optometry, Indiana University,
Bloomington, IN; 2Essilor International, Paris, France.
Purpose: Subjective refraction is independent of pupil size even for
eyes with spherical aberration (SA). We tested the popular
explanation that Stiles-Crawford apodization (SCA) biases subjective
refraction towards the pupil center by attenuating marginal rays.
Methods: Aberrometry data were used for objective wavefront
refractions that indentify the target vergence required to maximize
metrics of image quality for varying levels and signs of SA and
apodization, and a range of spatial frequencies (SFs). Subjective
refractions for a variety of test stimuli were measured with phase
plates that controlled SA levels, and apodization filters that controlled
the Stiles-Crawford effect.
Results: In the presence of SA, high SF image quality and subjective
appearance of best focus are both achieved with a near paraxial focus
irrespective of the presence or absence of pupil apodization.
Optimum low SF image quality is achieved by focusing more
marginal pupil regions, and thus best focus for low SFs changes with
SA levels and apodization. For letter charts used in clinical refraction,
optimum retinal image quality is achieved with a sphere lens that
focuses rays entering the eye 1- 1.5 mm from the pupil center.
Conclusions: Clinical subjective refractions are independent of pupil
size because retinal image quality is maximized when rays near the
pupil center are preferentially focused, independent of SCA.
Removing high spatial frequencies from the visual stimulus makes
subjective refractions more dependent on pupil size in the presence of
SA.
Commercial Relationships: Renfeng Xu, None; Arthur Bradley,
Essilor International (F); Larry N. Thibos, Essilor International (F),
Vistakon Inc. (F), Vistakon, Inc. (C), Self (P); Gildas Marin, Essilor
international (E); Martha Hernandez, Essilor International (E)
Support: NIH P30EY019008, Essilor International
Program Number: 4550
Presentation Time: 11:15 AM - 11:30 AM
Impact of Primary and Secondary Spherical Aberration on
Predicted Peripheral Image Quality
Amanda C. Kingston1, 2, Geunyoung Yoon2. 1BME, University of
Rochester, Rochester, NY; 2Flaum Eye Institute, University of
Rochester, Rochester, NY.
Purpose: To determine the impact of sign and magnitude of primary
and secondary spherical aberration (SA) on predicted image quality
at retinal eccentricities up to 20°.
Methods: An Arizona eye model was implemented in commercially
available optical design software (Zemax Bellevue, WA). Radii of
curvature, index and thicknesses were used from the model while
axial length and crystalline lens asphericity were varied to produce an
eye with zero defocus and SA. Zernike SA up to ±1.00μm over a
6mm diameter was added to the anterior cornea to induce different
signs and magnitudes of primary and secondary SA. Foveal retinal
image quality with each SA condition was optimized at distance by
adjusting defocus. Wavefronts were calculated for an elliptical pupil
with a 6mm long axis, at each retinal eccentricity, using Zemax.
Through-focus peripheral image quality, using an image-convolution
based image quality metric was done with a custom Matlab program.
Measured outcomes were retinal image quality, refractive error and
depth of focus (DOF) as a function of retinal eccentricity.
Results: For all eccentricities, negative primary SA induced
hyperopic defocus whereas positive primary SA and zero SA induced
myopic defocus. Peak image quality with zero SA was higher than all
eyes with SA, and maintained the same magnitude of myopic shift as
primary SA (0.25D and 1.50D at 10 and 20°, respectively). DOF was
extended with increasing magnitude of primary SA for all
eccentricities compared to the zero SA case. Positive secondary SA
induced hyperopic defocus at all eccentricities, whereas negative
secondary SA induced myopic defocus. Secondary SA gives a
secondary peak image quality instead of single focus found with
primary SA. This secondary peak is in the hyperopic direction for
positive SA and myopic direction for negative SA. Increasing the
magnitude of secondary SA degraded image quality by 26-35% for
all eccentricities. Decreasing the magnitude of secondary SA to 0.10μm increased image quality while still maintaining myopic
defocus.
Conclusions: Positive primary and negative secondary SA yield
acceptable foveal image quality while maintaining myopic defocus at
all eccentricities. Inducing optimal primary and secondary SA of the
eye with an advanced ophthalmic lens manipulates the amount of
refractive defocus and depth of focus in the peripheral retina,
potentially providing the ability to control myopia progression.
Commercial Relationships: Amanda C. Kingston, Bausch &
Lomb (E); Geunyoung Yoon, Bausch & Lomb (F), Johnson &
Johnson (F), Allergan (C), Staar Surgical (C), CIBA Vision (F),
Acufocus (C)
Support: Research to Prevent Blindness (RPB)
Program Number: 4551
Presentation Time: 11:30 AM - 11:45 AM
Peripheral Wavefront Aberrations of Accommodating Human
Eye
Tao Liu, Larry N. Thibos. School of Optometry, Indiana University,
Bloomington, Bloomington, IN.
Purpose: Retinal image quality in the peripheral visual field is
thought to contribute to visual control of eye growth and myopia
progression. The contribution of spherical aberration is of particular
interest because accommodation typically causes a sign reversal that
can have a large impact on accommodative lag and image quality.
Thus we aimed to measure spherical aberration in central and
peripheral visual field as a function of accommodative demand.
Methods: A scanning Shack-Hartmann wavefront aberrometer (Wei
& Thibos, 2010 Opt Express 18: 1134) was employed to measure
ocular aberrations along 37 different lines-of-sight over the central 26
degree visual field in 30 seconds. Aberrations were measured
sequentially using light reflected from a small spot produced on the
fundus by an incident probe beam that pivoted around the center of
the eye’s entrance pupil. Scanning mirrors that steered the incident
probe beam also de-scanned the reflected light into a fixed wavefront
sensor. Accommodation was stimulated over the range 0-6D by an
acuity target in a Badal configuration. Target and room illumination
was reduced to promote pupil dilation. Spherical aberration
coefficients C40 (primary) and C60 (secondary) for elliptically
foreshortened pupils (Wei & Thibos, 2010, Optom Vis Sci 87, E767777) describe ocular wavefront error over a fixed, 6mm circle
concentric with the eye’s pupil.
Results: Primary spherical aberration varied significantly in sign and
magnitude over the visual field but always changed in the negative
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
direction during accommodation. For 6D of accommodation, changes
in C40 ranged from 0.1 to 0.4 microns RMS, with larger values
occurring for larger eccentricities. These changes are much larger
than the population mean values reported previously (Mathur,
Atchison, & Charman, 2009. J Vis 9, 20 21-11). This discrepancy
may be due to several factors, including individual variation, duration
of measurement sequences, and the problematic interpretation of
aberration coefficients obtained over elliptical pupils. Unlike C40,
secondary spherical aberration C60 was typically positive and did not
vary significantly with accommodation
Conclusions: Spherical aberration in peripheral vision changes
significantly during accommodation, which may provide a potential
clue for visual control of eye growth.
Commercial Relationships: Tao Liu, None; Larry N. Thibos,
Essilor International (F), Vistakon Inc. (F), Vistakon, Inc. (C), Self
(P)
Support: NIH grant R01-EY05109
Program Number: 4552
Presentation Time: 11:45 AM - 12:00 PM
1 Changes in Ocular Biometrics and Refraction during Near
Work in Downward Gaze over Time
Atanu Ghosh, Michael J. Collins, Brett A. Davis, Scott A. Read, Fan
Yi, Payel Chatterjee. School of Optometry and Vision Science,
Queensland University of Technology, Brisbane, QLD, Australia.
Purpose: To investigate changes in the characteristics of the corneal
optics, total optics, anterior biometrics and axial length of the eye
during a near task, in downward gaze, over 10 min.
Methods: Ten emmetropes (mean - 0.14 ± 0.24 DS) and 10 myopes
(mean - 2.26 ± 1.42 DS) aged from 18 to 30 years were recruited. To
measure ocular biometrics and corneal topography in downward
gaze, an optical biometer (Lenstar LS900) and a rotating Scheimpflug
camera (Pentacam HR) were inclined on a custom built, height and
tilt adjustable table. The total optics of the eye were measured in
downward gaze with binocular fixation using a modified ShackHartmann wavefront sensor. Initially, subjects performed a distance
viewing task at primary gaze for 10 min to provide a “wash-out”
period for prior visual tasks. A distance task (watching video at 6 m)
in downward gaze (25°) and a near task (watching video on a
portable LCD screen with 2.5 D accommodation demand) in primary
gaze and 25°downward gaze were then carried out, each for 10 min
in a randomized order. During measurements, in dichoptic view, a
Maltese cross was fixated with the right (untested) eye and the
instrument’s fixation target was fixated with the subject’s tested left
eye. Immediately after (0 min), 5 and 10 min from the
commencement of each trial, measurements of ocular parameters
were acquired in downward gaze.
Results: Axial length exhibited a significant increase with downward
gaze and accommodation over time (p<0.05). The greatest axial
elongation was observed in downward gaze with 2.5 D
accommodation after 10 min (mean change from baseline 23±3 µm).
Downward gaze also caused greater changes in anterior chamber
depth (ACD) and lens thickness (LT) with accommodation (ACD
mean change -163±12µm at 10 min; LT mean change 173±17 µm at
10 min) compared to primary gaze with accommodation (ACD mean
change -138±12µm at 10 min; LT mean change 131±15 µm at 10
min). Both corneal power and total ocular power changed by a small
but significant amount with downward gaze (p<0.05), resulting in a
myopic shift (~0.10 D) in the spherical power of the eye compared
with primary gaze.
Conclusions: The axial length, anterior biometrics and ocular
refraction change significantly with accommodation in downward
gaze as a function of time. These findings provide new insights into
the optical and bio-mechanical changes of the eye during typical near
tasks.
Commercial Relationships: Atanu Ghosh, None; Michael J.
Collins, None; Brett A. Davis, None; Scott A. Read, None; Fan Yi,
None; Payel Chatterjee, None
Program Number: 4553
Presentation Time: 12:00 PM - 12:15 PM
Effect of Accommodation on Peripheral Refraction
Jason Shen, Frank Spors. College of Optometry, Western Univ of
Hlth Sciences, Pomona, CA.
Purpose: Both animal and human studies show that peripheral
refraction has an impact on the development of central refractive
error. Furthermore, there is evidence indicating the link between near
work and myopia progression. The purpose of this study is to
investigate the effect of accommodation during near work on
peripheral refraction.
Methods: Twenty six eyes (thirteen young subjects, 8 females and 5
males) with a narrow range of uncorrected refractive errors ranging
from -0.50 to +1.00 diopters, and astigmatism less than -1.00 diopters
were measured by a Grand Seiko WAM 5500 open field
autorefractor. The refractive error was measured in 10° steps up to
30° across both the temporal and the nasal horizontal visual fields.
The measurements were repeated with Maltese cross visual targets
displayed at 20 ft distance, 40 cm and 25 cm. The near targets were
arranged in an arc which allowed maintaining the same
accommodative demand throughout the different directions of gaze.
Central and peripheral refraction data were converted to power
vectors M, J0, and J45.
Results: Emmetropic eyes did have about 1.0 D myopic shift in 30°
periphery. Increasing Against-The-Rule astigmatism was presented in
the horizontal periphery. These results are in alignment with previous
literature. With stimulated accommodation, there were no statistically
significant differences of the peripheral spherical equivalents M and
J0 astigmatism. Right eyes showed a positive linear slope of J45
profile across the horizontal visual field which was negative for left
eyes. But with increasing accommodative demands, the slope of J 45
profiles changed signs. J45 values varied within a range of 0.6 D.
Conclusions: Near accommodation to 25 cm and 40 cm did not show
significant effects on M and J0 components of peripheral refraction in
emmetropic subjects. However, near accommodation had major
effects on the J45 component. It remains unclear why J45 changed
significantly. Further studies are needed to investigate the
relationships between J45 and the states of accommodation.
Commercial Relationships: Jason Shen, None; Frank Spors, None
Program Number: 4554
Presentation Time: 12:15 PM - 12:30 PM
School-Age Myopic Shift in Hyperopic Children with Infantile
Esotropia and Peripheral Myopia
Eileen E. Birch1, 2, Simone Li1, Sarah E. Morale1, Reed M. Jost1,
Vidhya Subramanian1, Donald O. Mutti3. 1Retina Foundation of the
Southwest, Dallas, TX; 2Ophthalmology, UT Southwestern Medical
Center, Dallas, TX; 3College of Optometry, The Ohio State
University, Columbus, OH.
Purpose: Children with infantile esotropia (IET) often fail to
emmetropize during the first year of life (Birch et al. Eye, 2010).
Nonetheless, after 5-6 years of persistent moderate hyperopia, many
children with IET experience a myopic shift of -0.50D/yr when they
are 7-12 years old (Birch et al Eye, 2010). Because eye shape and
peripheral retinal defocus are thought to play an important role in
controlling myopic progression, we examined foveal and peripheral
biometric and refractive data associated with the early hyperopia and
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
later myopic shift in 3- to 14-year-old children with IET.
Methods: Eye length (right eye) was measured with a Haag-Streit
Lenstar in 40 children with infantile ET. Five measurements were
obtained at the fovea and at 10° and 20° on the temporal retina. For
off-axis measurements, children fixated a dim mini-LED affixed to
the instrument. Distance refraction (right eye) was obtained for the
same 3 locations with a Grand Seiko binocular autorefractor with the
child fixating letter targets.
Results: At 3-4 and 5-6 years old, children with IET had mean±se
refractive error of +3.63±0.61D and +3.81±0.43D, respectively, and
axial length of 21.4±0.3mm and 21.2±0.2mm, respectively.
Peripheral eye length was 0.2-0.4 mm longer than axial length,
consistent with oblate ocular shape. Peripheral refraction was -0.84 to
-0.91D more myopic relative to foveal refraction. At 7-8 years, mean
hyperopia was lower (+2.66±0.67D) and axial length longer
(22.1±0.2mm). In this age group, peripheral eye length was shorter
than axial length by 0.1-0.3 mm; i.e., eyes were less oblate in shape.
By 9-14 years, mean hyperopia was again lower at +1.54±0.76D and
axial length longer at 23.1±0.5mm; eyes were even less oblate
(peripheral eye length was 0.2-0.4 mm shorter than axial length). In
the older age groups peripheral refraction remained slightly myopic (0.1 to -0.2D) relative to foveal refraction.
Conclusions: Hyperopia in IET is associated with oblate eye shape.
While the putative “stop” signal of relative peripheral myopia is
present in younger eyes, the older eyes are significantly longer and
significantly less oblate at 7-14 years of age, just as the children
experience a myopic shift. The possibility that some eyes can grow
rapidly to become less hyperopic despite inhibitory peripheral
defocus requires longitudinal confirmation.
Commercial Relationships: Eileen E. Birch, None; Simone Li,
None; Sarah E. Morale, None; Reed M. Jost, None; Vidhya
Subramanian, None; Donald O. Mutti, None
Support: NIH grant EY022313
467 Visual Functions in AMD
Wednesday, May 08, 2013 2:45 PM-4:30 PM
Exhibit Hall Poster Session
Program #/Board # Range: 5017-5042/A0179-A0204
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 5017 Poster Board Number: A0179
Presentation Time: 2:45 PM - 4:30 PM
Preliminary assessment of a new device to test potential visual
acuity when compared to gold standard PAM
Elizabeth R. Richter, Jan A. Kylstra. Storm Eye Institute, Medical
University of South Carolina, Charleston, SC.
Purpose: Assess a newly-developed potential visual acuity device
compared with the gold standard Guyton-Minkowski Potential
Acuity Meter (PAM)
Methods: The rationale for potential acuity assessment is to
determine if vision loss is due solely to cataract or due to other ocular
pathology. The current gold standard is the Guyton-Minkowski PAM.
This method has several problems, including high cost and difficulty
in use. The physician cannot see the projected chart on the retina and
has to rely on patient cooperation. When this method is unsuccessful,
the cause of failure may result from true retinal pathology or
difficulties with equipment use.
We have developed a new device (the SCALE) which combines
current indirect ophthalmoscopy with a 20 diopter lens and
transparent ETDRS-style eye chart. The virtual image of the retina is
formed 5cm in front of the lens, and in this same plane the eye chart
is held. This allows the physician to directly project the eye chart
onto the patient's retina while the practitioner also views the patient's
retina to make sure the image is directed on the macula. This is the
first comparison study to determine the ability of visual acuity
measurement when compared to the current gold standard in 23
patients with preoperative cataracts. After conversion to logMAR
acuity, paired t-test was used to compare differences amongst the
data. The goal of this study was to determine ease of use and
correlation with other accepted methods.
Results: Of 23 eyes, only one patient was unable to see letters on
either device. Another subject was unable to see anything on the
PAM device (>20/800), but could see one line (20/252) with the
SCALE. Analysis of the other patients yielded a significant
difference between the visual acuities measured by these two
potential acuity methods (t(20)=3.4916, p=0.00230). The mean PAM
logMAR acuity was 0.551 (SD=0.384), while the SCALE showed a
0.335 acuity (SD=0.246); this is approximately 2-line increase on the
ETDRS chart.
Conclusions: The SCALE is another method to assess potential
acuity. From preliminary study, it appears to overestimate visual
acuity when compared to the gold standard PAM. However, this new
device may be an excellent and inexpensive addition to the precataract toolkit to assess retinal function. Further studies are needed
to assess post-surgical acuity to determine if this is a good estimator
of prospective surgical outcome.
Commercial Relationships: Elizabeth R. Richter, US Provisional
Application No. 61/653,171 (P); Jan A. Kylstra, provisional
61/653,171 (P)
Clinical Trial: 00016836
Program Number: 5018 Poster Board Number: A0180
Presentation Time: 2:45 PM - 4:30 PM
Evaluation of vision auto-testing in patients with AMD using an
iPad App
Matthias G. Hartmann. Private Practice, Berlin, Germany.
Purpose: Patients with age-related macular degeneration (AMD)
need to undergo regular testing of their visual acuity. A tool for selfmeasurement to be run on an iPad was developed to enable patients
to have regular testing by themselves. It is available in German,
English, Spanish and Japanese. This project was designed to evaluate
whether iPad-based vision auto-testing is a feasible method for
patients with AMD compared to established instruments.
Methods: The project was run in 4 ophthalmologist’s offices. Target
sample size was 100 patients; only patients with an initial vision of at
least 0.05 were included. Patients had to consent to a threepart vision
test every 4 weeks for 6 months. Visual acuity was measured by a)
distance vision testing by projection of Landolt rings (EN ISO 8596)
b) near vision test charts (Oculus) with Landolt rings and c) automeasurement with Landolt rings using the iPad App “Eyetest Control your visual acuity”. Patients were initially advised how to
use the iPad App. All tests were performed in the office. Test results
were defined to be consistent when they differed to a maximum of
one line.
Results: 112 patients of 57 to 92 years of age (mean 77.2 yrs) were
included. Nearly all patients had never used an iPad before (96% vs.
4%). Results for vision tests by projection and iPad were consistent in
76% (right eye) and 83% (left eye) of the measurements. Near vision
test charts were used as a control. Results acquired by near vision test
charts frequently differed from projection results by 2 or more lines.
At the end of study, patients were asked for their preference. The
majority of patients (81.25%) chose the iPad App as their preferred
method to test visual acuity, only 12.5% chose the projection method,
6.25% preferred near distance test charts.
Conclusions: The fact that over 80% of the patients prefer the iPad
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
App for vision testing illustrates the feasibility of the method. It is
easy to use even for former iPad non-users and delivers results
consistent with established vision testing instruments. This suggests
that the iPad App is suitable to support patients and ophthalmologists
in the routine care of AMD. Features like an adjustable reminder and
a mail function contribute to its value. The Amsler grid will be
included and an automated distance adjustment will be implemented
to further improve feasibility and reliability of the tool. Home use of
the auto-vision App will be evaluated.
Commercial Relationships: Matthias G. Hartmann, Novartis (F)
Program Number: 5019 Poster Board Number: A0181
Presentation Time: 2:45 PM - 4:30 PM
A New Contour Integration Macular Perimetry (CIMP) on iPad
for Visual Function Evaluation in Maculopathy
Yi-Zhong Wang1, 2, Gina Mitzel1. 1Retina Foundation of the
Southwest, Dallas, TX; 2Ophthalmology, UT Southwestern Medical
Center, Dallas, TX.
Purpose: Patients with maculopathy often show early abnormalities
outside fovea. Such paracentral deficits may not be detected by visual
function tests for foveal vision. In this study, a new macular
perimetry based on contour integration was developed on iPad, and
the feasibility of using CIMP to detect paracentral vision loss in
maculopathy was assessed.
Methods: Thirty normal subjects (mean age 51 years ± 22SD, mean
visual acuity (VA) 0.04 logMAR ± 0.08SD) and 30 patients (mean
age 62±21, mean VA 0.36±0.35) with maculopathy (12 with
Stargardt disease, 7 diabetic maculopathy, and 11 age-related macular
degeneration) participated in the study. CIMP stimuli were circular
contour segments, and were generated on iPad screen that subtended
18x23.4 deg at a viewing distance of 18”. In each trial, 4 contour
segments, each a 30 deg circular arc, were evenly placed along the
center of the inner or outer ring of the ETDRS macular grid. Among
4 segments, one was distorted and others were smooth. The distortion
was introduced by radial modulation. The stimulus duration was 0.25
sec. The subject’s task was to indicate by touch which one of 4
locations had distorted contour. A spatial 4-alternative, forced-choice
(4AFC) staircase paradigm and a maximum likelihood fitting
procedure were employed to estimate the threshold for detecting
contour distortion in the inner or outer ring of the grid.
Results: Thirty-four diseased eyes (mean VA 0.19±0.20) were able
to perform the CIMP test. Their mean thresholds to detect distortion
in the inner and outer rings were -0.36±0.36 and -0.54±0.35
logMAR, respectively, significantly worse than normal controls (0.73±0.16 and -0.81±0.16, respectively, p<0.008). Furthermore, for
the diseased eyes with VA 0.20 or better (n=23, mean VA 0.08±0.11,
not significantly different from the normal control, p>0.16), the inner
and outer ring mean thresholds were -0.36±0.39 and -0.49±0.41,
respectively, also significantly worse than the normal controls
(p<0.0012). Twenty-six diseased eyes (mean VA 0.58±0.39) were
unable to perform CIMP due to severe damage to the macula.
Conclusions: These results suggest that the new CIMP test can detect
paracentral loss of visual function in patients having normal visual
acuity. CIMP implemented on iPad has the potential to be a new
remote monitoring tool for early detection of treatable disease
condition outside fovea in maculopathy.
Commercial Relationships: Yi-Zhong Wang, Vital Art and
Science, Inc. (I), Vital Art and Science, Inc. (C), Vital Art and
Science, Inc. (P); Gina Mitzel, None
Support: OneSight Research Foundation
Program Number: 5020 Poster Board Number: A0182
Presentation Time: 2:45 PM - 4:30 PM
myVisionTrack (mVT), a novel remote visual self-assessment,
correlates with clinical course of macular function
Yu-Guang He1, Johnathan D. Warminski1, Yi-Zhong Wang2.
1
Ophthalmology, Univ Texas Southwestern Med Ctr, Dallas, TX;
2
Retina Foundation of the Southwest, Dallas, TX.
Purpose: Reliable self-assessment of a patients’ visual function can
improve early detection of worsening macular function. mVT
provides patients with a handheld, electronic platform to assess visual
function based on shape discrimination.
Methods: Case series comparing mVT self-assessments to patients’
snellen acuity, central macular thickness and clinical course during
treatment for maculopathy.
Results: 36 patients were monitored for 180-550 days during
treatment of diabetic maculopathy (29) and age-related maculopathy
(7). Self-monitoring correlated well with the patients’ snellen visual
acuity and OCT measured central macular thickness.
Conclusions: mVT provided a reliable self-measure of visual
function in patients with macular edema.
Commercial Relationships: Yu-Guang He, None; Johnathan D.
Warminski, None; Yi-Zhong Wang, Vital Art and Science, Inc. (I),
Vital Art and Science, Inc. (C), Vital Art and Science, Inc. (P)
Program Number: 5021 Poster Board Number: A0183
Presentation Time: 2:45 PM - 4:30 PM
Visual Acuity Loss In Patients With AMD, Measured Using A
Vanishing Optotype Letter Chart
Nilpa Shah1, Roger S. Anderson1, 2, Adnan Tufail1, Catherine A.
Egan1, Steven Dakin1. 1NIHR Biomedical Research Centre for
Ophthalmology, Moorfields Eye Hospital & UCL Institute of
Ophthalmology, London, United Kingdom; 2Vision Science Research
Group, School of Biomedical Sciences, University of Ulster at
Coleraine, Northern Ireland, United Kingdom.
Purpose: Vanishing Optotype (VO) letters have a pseudo high-pass
design so that the mean luminance of the target is the same as the
background and the letters thus ‘vanish’ once the resolution threshold
is reached in the fovea. We wished to investigate how visual acuity
measurements using charts constructed from these letters compared
to charts of conventional letter design, in both normal subjects and
patients with differing levels of AMD.
Methods: 60 participants were recruited; 30 with no ocular
abnormalities and 30 with AMD and no other significant ocular
pathology. Following refractive error correction, each subject
underwent monocular (single letter scored) visual acuity
measurements using ETDRS charts 1 and 2, and charts of the same
layout but constructed using VO letters (VO1 and VO2). All tests
were performed in a random sequence. The methods of Bland and
Altman were employed with test-retest variability (TRV) expressed
as 95% confidence intervals for agreement.
Results: Visual acuity measurements with the VO chart were, on
average, approximately 3 logMAR lines ‘worse’ than those with
conventional letter design in subjects with AMD compared to a
difference of only 1.5 logMAR lines in normal subjects. This
difference between the two groups was statistically significant
(p<0.05, unpaired t-test). Similar TRV’s of approximately +/- 0.10
logMAR were found for both the ETDRS and VO charts in both
groups.
Conclusions: AMD patients display a measurably larger visual
acuity deficit using VO letter charts compared to conventional
ETDRS charts, with no significant difference in test-retest variability.
Commercial Relationships: Nilpa Shah, None; Roger S.
Anderson, None; Adnan Tufail, Allergan (C), Bayer (C), GSK (C),
Oculogics (C), Pfizer (C), Thrombogenics (C), Amakem (C),
Heidelberg Engineering (R), Novarits/Alcon (C), Sanofi/Genzyme
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
(C); Catherine A. Egan, Bayer (S), Oculogics (S), Novartis (S),
Allergan (S), Novartis (F); Steven Dakin, None
Support: Supported by a Fight for Sight studentship, by Moorfields
Special Trustees and by an award from the NIHR Biomedical
Research Centre for Ophthalmology, Moorfields Eye Hospital &
UCL Institute of Ophthalmology, London
Program Number: 5022 Poster Board Number: A0184
Presentation Time: 2:45 PM - 4:30 PM
Screening for AMD Using Psychophysical Correlates of Macular
Dysfunction
Han Li1, Susan M. Culican2. 1Washington University School of
Medicine, St. Louis, MO; 2Dept of Ophthalmology and Visual
Science, Washington University School of Medicine, St. Louis, MO.
Purpose: To assess the utility of our novel computerized vision task
as a screening tool for AMD and other macular disorders.
Methods: We developed a computerized task and administered it to
20 participants with AMD or other macular disorders, and 17
similarly aged control participants.
The task was based on participant identification of interruptions in
visual stimuli. Testing was conducted monocularly. Subject distance
to the video display was determined by empirical adjustment, by
positioning the physiological blind spot at the periphery of stimuli.
Stimuli consisted of a central fixation point surrounded by rotating
objects. Objective interruptions of some objects were programmed
into the stimuli, which the participant was instructed to report by
striking a key. We hypothesized that those with macular dysfunction
would subjectively perceive more interruptions than were
programmed, due to foveal and parafoveal scotomata.
Results: Our results show significantly different task performance
between those with and without macular disorders. Macular disorder
participants reported a higher number of subjective interruptions
(n=4.65 vs n=0.35, p<.001) as well as total errors, defined as sum of
missed objective interruptions and subjective interruptions, compared
to controls (n=6.3 vs n=1.24, p<.001). There was no significant
difference in the number of missed objective interruptions alone
(n=1.65 vs n=0.88, p=.158). Disease status correlates with test
performance, while controlling for near distance visual acuity
(p=.001).
Furthermore, interocular test performance was the same in control
participants, with no significant difference in subjective interruptions,
missed objective interruptions, and total errors.
Conclusions: Our visual task discriminates between macular disorder
and control group participants, independent of visual acuity.
Participant attention and instruction compliance were high, while
fatigue and interocular learning curve effects were negligible. These
results suggest that our novel computer task could be used as a rapid
and effective screening tool in detecting macular disorder. In
particular, the number of subjective interruptions could be used as a
reliable screening parameter. However, further testing in
demonstrating reliability and validity of our results must be done.
Commercial Relationships: Han Li, None; Susan M. Culican,
None
Program Number: 5023 Poster Board Number: A0185
Presentation Time: 2:45 PM - 4:30 PM
A New Method to Depict Central Scotomas: Automated
Sterocampimetry
Anthony P. Cappo1, Richard B. Rosen2, William H. Seiple3, Matthew
D. Orr1, michele arthurs4, Trisha Emborgo5. 1Opticology, Inc., New
York, NY; 2New York Eye & Ear Infirmary, New York, NY;
3
Lighthouse International, New York, NY; 4Universite de Montreal,
Montreal, QC, Canada; 5Hunter College, City University of New
York, New York, NY.
Purpose: Despite high prevalence of central and para-central
scotomas and the success of available treatments, no precise
automated means to measure the size or shape of the scotoma exists.
Such information would be useful for both early detection and
following treatment. Standard automated perimetry and
microperimetry present stimuli at various intensities to obtain
thresholds. The stimuli are typically in a preset grid pattern which
fails to give a detailed outline of scotomas. We describe a new
technique, Automated Stereocampimetery, that precisely defines the
size and shape of a scotoma, and compare the results to
Microperimetry and to the underlying image of the damaged retina
from SLO.
Methods: We tested 30 patients on the Automated Stereocampimeter
(AS) and an OCT SLO outfitted with a Microperimeter (MP) without
screening for the type of retinal pathology. Both devices require a
subjective response from the subject. The MP is part of an OCT SLO
which also gives retinal thickness and image of the retina. It is a
monocular test and ensures fixation by monitoring any movement of
landmarks in the retinal image. The MP presents stimuli in a regular
pattern over 30 degrees of visual field and the stimulus points are
repeated at various light intensities (full threshold). The AS does not
monitor fixation, but uses binocular fixation and animation of the
target to improve fixation. To compare the locations and extents of
loss, the AS results were superimposed on the MP results.
Results: Of 30 subjects tested on the AS, 12 were found to have
well-defined areas of scotomas. Eight of these 12 subjects were able
to complete MP Testing. In 6 of these 8 cases the MP result
confirmed the AS findings, with additional correspondence of the
probable defects identified in the SLO image to the AS-determined
scotoma outline. In 2 cases the relationship appeared weaker.
Conclusions: More than half of patients have been able to complete
an AS test successfully, and the comparison to the MP data suggests
that the AS produced meaningful results that may be useful in
following patients with centrally located pathology. Poor results were
usually easy to identify, which reduces the chance of false positive
tests. Further, the correspondence between discoloration in the retina
image and the shape of discovered defect was greater than expected.
MP results
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
AS superimposed on MP
Commercial Relationships: Anthony P. Cappo, Opticology, Inc.
(E), Centrofuse Technologies, LLC (I), LacriSciences, LLC (I);
Richard B. Rosen, Opko-OTI (C), Optos (C), Clarity (C), OD-OS
(C), Topcon (R), Zeavision (F), Genetech (F), Optovue (C); William
H. Seiple, None; Matthew D. Orr, Opticology, Inc. (C), Opticology,
Inc. (P); michele arthurs, None; Trisha Emborgo, None
Program Number: 5024 Poster Board Number: A0186
Presentation Time: 2:45 PM - 4:30 PM
Spaeth/Richman Contrast Sensitivity Test in Macular
Degeneration
Bruno M. Faria, Fulya Duman, Mohsin Ali, Camila Zangalli, Sheryl
S. Wizov, Lan Lu, Jesse Richman, Eric Spaeth, George L. Spaeth.
Glaucoma, Bruno Faria, Philadelphia, PA.
Purpose: To evaluate contrast sensitivity in age-related macular
degeneration (AMD) patients using a new contrast sensitivity
instrument.
Methods: Age-related Macular Degeneration patients and controls
were prospectively evaluated using the Spaeth-Richman Contrast
Sensitivity (SPARCS) method and the Pelli-Robson test. Testing was
performed monocularly in a standardized testing environment.
Contrast thresholds for the central, superonasal, superotemporal,
inferonasal and inferotemporal areas of vision were determined. The
contrast sensitivity scores for each area of vision and the cumulative
scores of AMD patients were compared with those of the controls.
The results were analyzed with Spearman coefficients for continuous
variables and the Kruskal-Wallis test for categorical variables.
Results: Fifty-four eyes with AMD and one-hundred and eighty
control eyes completed the study. The mean SPARCS scores were
54.6 for patients with AMD and 73.9 for controls (p<0.01). The
SPARCS scores were significantly lower in all five quadrants for
AMD patients (p<0.01).
Conclusions: SPARCS was able to discriminate well between
patients with AMD and controls. SPARCS may become a standard
technique to assess visual function in AMD patients.
Commercial Relationships: Bruno M. Faria, None; Fulya Duman,
None; Mohsin Ali, None; Camila Zangalli, None; Sheryl S. Wizov,
None; Lan Lu, None; Jesse Richman, none (P); Eric Spaeth,
SPARCS (C), SPARCS (S); George L. Spaeth, Merck (F), U.S.
Patent No. 8,042,946 (P), Pfizer (F)
Support: Pfizer, inc.
Clinical Trial: NCT01300949
Program Number: 5025 Poster Board Number: A0187
Presentation Time: 2:45 PM - 4:30 PM
Central And Paracentral Single-Letter Recognition In Eyes With
Macular Lesions
Gianfrancesco M. Villani1, Lorenzo Bertelli1, Giovanni Sato2, Marco
U. Morales3, August Colenbrander4. 1Ophthalmology, Centro
Riabilitazione Ipovedenti e Microperimetria - CRIM, Castel
d'Azzano, Verona, Italy; 2UO Oftalmologia, Centro Riabilitazione
Visiva, Ospedale S. Antonio, Ulss16, Padova, Italy; 3Ophthalmology
and Visual Sciences, School of Clinical Sciences, The University of
Nottingham, Nottingham, United Kingdom; 4Smith-Kettlewell Eye
Research Institute, San Francisco, CA.
Purpose: To investigate the size, location, and number of single
letters that can be recognized within 5° from fixation by patients with
central vision loss
Methods: 32 eyes (29 patients) with maculopathy (AMD, myopic
maculopathy, macular edema, cone dystrophy, toxo scar) were
enrolled. Lower-case single letters (TimesNewRoman) were
randomly projected on a 19” LCD monitor at a viewing distance from
10 to 60 cm with black-on-white contrast polarity, >90% contrast, by
custom software (“Letter Scotometry” [LS]). A two steps procedure
was followed: 1- central size threshold (“CST”): central projection of
a single letter at decreasing sizes from 0.63M to 25M in log steps
until the answer was correct (≥3/5 letters per size); 2- paracentral
span test (“PST”): random projection of single letters around a central
small fixation dot into a grid of adjoining cells proportional to letter
size. The letter size was set one log step bigger than CST, and not
scaled by eccentricity (it could be increased if the patient read no
letter, but then PST was restarted from the beginning). Stimuli stayed
on screen until an answer was given, and the response-time was
recorded. The only control of fixation was based on operator-patient
interaction. The examination included ETDRS BCVA at 1m,
MNREAD, SKREAD, and Microperimetry (MP) by Nidek MP1 or
OPKO. Digital overlapping of letter-grids and microperimetry maps
was done to compare scotoma borders in 8 directions from fixation
and to understand if correct letters matched with the scotoma-free
areas
Results: BCVA median (range) was 0.75 (0.2-1.6) logMAR, CST
was 0.84 (0.50-2.00) logMAR, MNREAD critical print size (CPS)
was 0.9 (0.5-1.3) logMAR and SKREAD CPS was 0.9 (0.4-1.4)
logMAR. Maximum Reading Speed (MRS) was 71.4 (2.4-162.2)
wpm on MNREAD, and 25.5 (1.2-49.6) wpm on SKREAD. When
the fixation dot was placed on the PRL the correspondence of
scotoma borders between letter-grids and microperimetry was 74%
(median 75%). CST on the LS test was strongly correlated with CPS
(r 0.71) and minimum print size (r -0.77) on the SKREAD
Conclusions: LS grids can be used clinically to display fixation/PRL
behavior in recognizing single-letters of the magnification needed for
the low-vision patient to read in the presence of central scotomas
Commercial Relationships: Gianfrancesco M. Villani, Letter
Scotometry/Marte srl © TX0007576130 / 2012-04-25 (P); Lorenzo
Bertelli, Letter Scotometry/Marte srl © TX0007576130 / 2012-04-25
(P); Giovanni Sato, None; Marco U. Morales, None; August
Colenbrander, None
Program Number: 5026 Poster Board Number: A0188
Presentation Time: 2:45 PM - 4:30 PM
Longitudinal Changes in Retinal Sensitivity among Patients with
Maculopathy
Hongting Liu, Millena G. Bittencourt, Owhofasa O. Agbedia,
Ahmadreza Moradi, Yasir J. Sepah, Daniel A. Ferraz, Mohamed A.
Ibrahim, Raafay Sophie, Mehreen Ansari, Quan Dong Nguyen.
Retinal Imaging Research and Reading Center, Wilmer Eye Institute
Johns Hopkins University, Baltimore, MD.
Purpose: To investigate longitudinal changes in retinal sensitivity
among patients with maculopathy with stable visual acuity (VA) and
central retinal thickness (CRT).
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Methods: In this prospective study,16 patients with maculopathy and
no change in VA (≤ 5 letters change in ETDRS score) and CRT (≤ 20
μm in spectral-domain optical coherence tomography (SD-OCT))
between 2 visits (interval: 2-6 months) were evaluated. Disease
entities included diabetic macular edema, age related macular
degeneration, central serous retinopathy, Stargardt's disease and
idiopathic macular hole.
Retinal sensitivity was assessed using the Spectral-OCT/SLO
microperimetry (MP) (Optos Inc, Scotland, UK) at both visits. The
test pattern was a standardized polar 3 grid which consists of 28
points within 11° from the fovea. The mean change and variance in
retinal sensitivity for all patients was compared to the MP intersession variation of 10 patients with retinopathies.
Results: A total of 700 points from 25 eyes (16 patients) with
maculopathy were analyzed. The mean age of subjects was 53 years
(SD ±16). The results are summarized in the table. The overall
variance between the two visits (6.0dB) was significantly greater than
the inter-session variance (2.4dB) (Mann Whitney Test, p=0.008).
Conclusions: Microperimetry may capture subtle functional changes
in maculopathy patients with stable visual acuity and no change in
central retinal thickness. Further studies with larger sample size are
indicated to validate the observed results.
decibels) was measured with fundus-tracking microperimetry. A
circular pattern of 28 test locations covering the central 11 degrees of
the macula was used. Stimulus duration was 200ms, at an average
interval of two seconds, and at a Goldmann III size. Fixation
locations were recorded during 20 seconds of viewing an “X.”
Fixation stability was calculated by fitting a Bivariate Contour
Ellipse Area to these data.
Results: Thickness remained stable post-treatment in half of the
patients whereas the other half demonstrated an initial drop after the
first injection and remained stable after subsequent visits. A
qualitative assessment of OCT suggests that the integrity of the IS/OS
layer did not improve if it appeared disrupted at baseline visit.
Sensitivity increased across all visits for one patient(12.5%),
increased for two patients in later visits(25%), remained stable in
three patients(37.5%), decreased slightly in one patient(12.5%), and
more importantly in the last patient(12.5%). While fixation location
was variable for all subjects, fixation stability (BCEA area) slightly
improved in one patient(12.5%), did not change in five
patients(62.5%), and was quite variable for two patients(25%).
Conclusions: Our data suggests that thickness and sensitivity were
predictors in evaluating outcome of anti-VEGF treatment. Fixation
did not show a significant improvement in stability post-treatment
and fixation location tended to vary between visits indicating the
possibility of more than one PRL.
Commercial Relationships: michele arthurs, None; Richard B.
Rosen, Opko-OTI (C), Optos (C), Clarity (C), OD-OS (C), Topcon
(R), Zeavision (F), Genetech (F), Optovue (C); Gennady Landa,
None; Rishard Weitz, None; William H. Seiple, None
Support: Genentech
Clinical Trial: nct01255774
Commercial Relationships: Hongting Liu, None; Millena G.
Bittencourt, None; Owhofasa O. Agbedia, None; Ahmadreza
Moradi, None; Yasir J. Sepah, None; Daniel A. Ferraz, None;
Mohamed A. Ibrahim, None; Raafay Sophie, None; Mehreen
Ansari, None; Quan Dong Nguyen, Genentech (F), Regeneron (F),
Lux Biosciences (F), Abbott (F), GSK (F), Santen (F), Santen (C),
Bausch and Lomb (C), Optos (F), Heidelberg Engineering (F)
Support: Wilmer Research Grant
Program Number: 5028 Poster Board Number: A0190
Presentation Time: 2:45 PM - 4:30 PM
Relationship between Visual Function and Optical Coherence
Tomography features in Early Age-related macular degeneration
(AMD)-Early Markers Observational Study
Ruth E. Hogg1, George Murphy1, Giovanni Staurenghi2, Chiara
Rosina2, Rufino Silva3, Ana Rita Santos3, Usha Chakravarthy1.
1
Center for Vision and Vascular Science, Queen's University Belfast,
Belfast, United Kingdom; 2Eye Clinic - Department of Clinical
Science, “Luigi Sacco”- Sacco Hospital, II School of Ophthalmology
- University of Milan, Milan, Italy; 3Faculty of Medicine., University
of Coimbra, Coimbra, Portugal.
Purpose: To investigate the relationship between visual function
parameters and tomographic metrics.
Methods: Study sample: 105 patients (53 males, 52 females) with
unilateral advanced AMD from 3 Centres (Milan, Coimbra and
Belfast) aged 52-93 years. Study Eye=Fellow eye without advanced
neovascular disease. Best corrected distance acuity (BCVA) and near
acuity (NVA), reading speed adjusted for print size (reading index;
RI) and low-luminance acuity (SKILL test) were measured. High
density macular raster scans on the Heidelberg were obtained.
Trained graders measured the neuroretinal thickness (NRT) and
choroidal thickness (CT) at the foveal centre and evaluated the
continuity of the following layers (ganglion cell layer GCL, inner
segment/outer segment junction IS/OS, external limiting membrane
ELM, photoreceptor layer PRL and retinal pigment epithelium RPE).
Univariate and logistic regression analyses were employed to
examine relationships between function and morphology.
Results: NRT was associated with BCVA (r=0.24 p=0.024); CT with
reduced (SKILL score) (r=-0.4 p<0.001). Retinal layer continuity
showed relationships with functional tests. External Limiting
Membrane continuity was associated with DVA (p=0.006), NVA
Program Number: 5027 Poster Board Number: A0189
Presentation Time: 2:45 PM - 4:30 PM
Monitoring the Progression of AMD post anti-VEGF treatment
using the OPKO OCT/SLO
michele arthurs1, Richard B. Rosen3, Gennady Landa3, Rishard
Weitz3, William H. Seiple2, 3. 1Université de Montréal, Montréal, QC,
Canada; 2New York Lighthouse, New York, NY; 3New York Eye &
Ear Infirmary, New York, NY.
Purpose: To evaluate the outcome of anti-VEGF treatment in
patients with exudative age-related macular degeneration (AMD)
using the optical coherence tomography-scanning light
ophthalmoscope (OCT/SLO), and to determine if predictors of an
individual patient’s responses to treatment can be identified.
Methods: Patients diagnosed with exudative AMD and having
received no prior AMD treatment were recruited. Eight subjects
between 58 and 85 years of age with visual acuities ranging between
20/16 and 20/200 were enrolled. Monthly treatments of ranibizumab
were given in the affected eye for up to 12 months. Three measures
of local retinal function were obtained monthly using the OPKO
OCT/SLO: retinal structure (OCT), psychophysical function
(microperimetry), and fixation location and stability. Integrity of
outer layers and retinal thickness were obtained with the OCT from
line scans and from 3D topographies. Psychophysical sensitivity (in
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
(p=0.021) and Reading index (p=0.020). IS/OS junction continuity
was associated with DVA (p=0.007), NVA (p=0.03) and SKILL
score (p=0.050). Photoreceptor layer continuity was associated with
Reading index (p=0.039). RPE layer continuity was associated with
SKILL score (p=0.003).
Conclusions: Significant associations exist between stressors of
macular visual function such as near acuity and low luminance acuity
and tomographic markers of retinal and choroidal morphology.
Commercial Relationships: Ruth E. Hogg, Novartis (F), Novartis
(C); George Murphy, None; Giovanni Staurenghi, Ocular
Instruments (P), GSK (C), Novartis (C), Alcon (C), Allergan (C),
Bayer (C), Roche (C), Heidelberg Engineering (C), OD-OS (C), QLT
(C), Optos (C); Chiara Rosina, None; Rufino Silva, Thea (C),
Novartis (C), Bayer (C), Allergan (C), Alimera (C); Ana Rita
Santos, None; Usha Chakravarthy, Bayer (C), Novartis (F),
Neovista (C), Oraya (F)
Program Number: 5029 Poster Board Number: A0191
Presentation Time: 2:45 PM - 4:30 PM
Relationship between retinal sensitivity and retinal thickness in
eyes with retinal disease
Srinivas R. Sadda, Muneeswar Nittala. Ophthalmology, Doheny Eye
Institute - USC, Los Angeles, CA.
Purpose: To evaluate the point-to-point relationship between local
retinal sensitivity as assessed by Optos SLO microperimetry and
retinal thickness and volume as determined by optical coherence
tomography (OCT).
Methods: Twenty four eyes of twenty four subjects with various
retinal diseases were enrolled in this IRB-approved prospective cross
sectional study. Microperimetry and spectral domain optical
coherence tomography (SD-OCT) were obtained on the study eye of
all enrolled subjects using an Optos Spectral OCT/SLO (Optos plc,
Dunfermline, UK). Microperimetry was performed with the using a
standard 45 stimuli pattern spread over the central 12 degrees of the
macula (foveal-centered), Goldmann III stimuli, and a 4-2-1
threshold strategy. The OCT-derived retinal thickness map was
registered to the microperimetry data by the OCT instrument
allowing point-to-point correlation between retinal sensitivity and
OCT thickness. Correlation analysis was performed using a total of
1080 loci.
Results: The mean age of the study cohort was 69 (SD; 13) years and
50 % were female. Retinal diseases in the study eyes included dry
and wet age related macular degeneration, diabetic retinopathy, vein
occlusions, macular telangiectasia and central serous
chorioretinopathy. The mean baseline best-corrected (log MAR)
visual acuity was 0.26 (Snellen ~ 20/30) and the mean (± SD) total
retinal sensitivity was 13.70 (± 2.74, range: 6.0 - 16.90) dB. The log
MAR visual acuity was significantly correlated with mean retinal
sensitivity (r= -0.43, p=0.05), with an expected stronger correlation
for foveal sensitivity (r= -0.74, p <0.001). Age was negatively
correlated with mean retinal sensitivity (r= -0.42, p=0.05). The mean
macular retinal thickness was 273.55 (± 32.31, range: 219 - 388) µm
and the mean total retinal volume was 7.70 (± 0.92, range: 6.18 10.94) cubic mm. There was no significant correlation between the
mean retinal sensitivity and mean retinal thickness (r=-0.06, p=0.79)
or total retinal volume (r=-0.06, p=0.78). The point retinal sensitivity
demonstrated a statistically significant, but weak correlation with
corresponding point retinal thickness (r=-0.095, p=0.002).
Conclusions: Local retinal sensitivity and retinal thickness are not
strongly correlated, suggesting that microperimetry can provide
independent, and potentially useful information regarding the effect
disease on the status of the retina.
Commercial Relationships: Srinivas R. Sadda, Regeneron (C),
Genentech (C), Allergan (C), Carl Zeiss Meditec (C), Optos (C), Carl
Zeiss Meditec (F), Optovue (F), Optos (F); Muneeswar Nittala,
None
Support: Research to Prevent Blindness
Program Number: 5030 Poster Board Number: A0192
Presentation Time: 2:45 PM - 4:30 PM
Multimodal Evaluation of Macular Function in Age-related
Macular Degeneration
Ken Ogino, Akitaka Tsujikawa, Kenji Yamashiro, Sotaro Ooto, Akio
Oishi, Isao Nakata, Masahiro Miyake, Ayako Takahashi, Abdallah A.
Ellabban, Nagahisa Yoshimura. Kyoto University Graduate School
of Medicine, Kyoto, Japan.
Purpose: To evaluate macular function using multimodality in eyes
with age-related macular degeneration (AMD) at various stages.
Methods: Macular function in 20 control eyes (20 subjects), 17 eyes
(17 patients) with large drusen, 18 eyes (18 patients) with drusenoid
pigment epithelial detachment (PED), and 19 eyes (19 patients) with
neovascular AMD were examined by a Landolt chart for visual
acuity; retinal sensitivity was measured by microperimetry, and focal
macular electroretinography (fmERG) was performed. In all of these
eyes, retinal morphology was examined using optical coherence
tomography.
Results: Eyes with neovascular AMD showed morphologic changes
in the neurosensory retina as well as marked deterioration of macular
function in all parameters measured with the Landolt chart, fmERG,
and microperimetry. Eyes with large drusen showed only minimal
morphologic changes in the neurosensory retina. In this large drusen
group, although retinal sensitivity at the central point was
significantly decreased (P = .0063), other parameters in macular
function were well preserved. In eyes with drusenoid PED, structure
of the neurosensory retina was well preserved while foveal thickness
was significantly increased (P = .013). Macular function of these eyes
was significantly deteriorated, with VA, amplitude of the a-wave and
b-wave, and the retinal sensitivity being markedly decreased. In
addition, the area of PED was correlated with amplitude of the
photopic negative response, latency of the a- and b-waves, and retinal
sensitivity within the central 4° or 8° region.
Conclusions: Multimodal evaluation demonstrates a significant
decrease in macular function in drusenoid PED and in neovascular
AMD.
Commercial Relationships: Ken Ogino, None; Akitaka
Tsujikawa, Pfizer (F); Kenji Yamashiro, None; Sotaro Ooto,
None; Akio Oishi, None; Isao Nakata, None; Masahiro Miyake,
None; Ayako Takahashi, None; Abdallah A. Ellabban, None;
Nagahisa Yoshimura, Canon (C), Canon (F), Nidek (C), Topcon
(F), PCT/JP2011/073160 (P)
Support: Grant-in-Aid for Scientific Research Japan 24791848
Program Number: 5031 Poster Board Number: A0193
Presentation Time: 2:45 PM - 4:30 PM
The functional impact of subfoveal SD-OCT characteristic on
reading acuity in neovascular age related macular degeneration
Florian Sulzbacher1, Christopher G. Kiss1, Stefan Sacu1, Marion R.
Munk1, Alexandra Kaider2, Tamara Mittermueller1, Philipp K.
Roberts1, Ursula Schmidt-Erfurth1. 1Ophthalmology, Medical
University Vienna, Vienna, Austria; 2Center for Medical Statistics,
Informatics, and Intelligent Systems; Section for Clinical
Biometrics;, Medical University of Vienna, Vienna, Austria.
Purpose: To correlate reading acuity in patients with neovascular
age-related macular degeneration (nAMD) to specific SD-OCT
characteristics of the subfoveal area.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Methods: Fourty four eyes showing untreated nAMD were examined
with the Heidelberg Spectralis-OCT. Pateints’ reading acuity
(logRAD) was assessed using a German language reading test
(Radner Lesetest), visual acuity (logMAR) was assessed using
EDTRS charts.
Reading- and visual performance was evaluated with respect to the
following OCT-findings in the subfoveal area 500x500µm:
neovascular complex (NVC), fibrovascular pigment epithelium
detachment (fPED), serous pigment epithelium detachment (sPED),
subretinal fluid (SRF), intraretinal fluid (IRF) and intraretinal cysts
(IRC).
Results: Of 44 eyes with nAMD mean reading acuity in logRAD was
0.72 ± 0.3 and mean visual acuity in logMAR was 0.59 ± 0.28
showing a strong correlation of r=0.821 spearmen (P=0,000).
In general, in subfoveal NVC, the mean logRAD score was 0.84 ±
0.24, whereas in NVC with additional cysts the mean logRAD score
was 1.0 ± 0.18.
With SRF, the mean logRAD was 0.58 ± 0.32, whereas with IRF the
mean logRAD was measured at 0.70 ± 0.35.
A SPED was associated with a mean logRAD score of 0.37 ± 0.10, a
FPED was associated with 0.83 ± 0.26 and FPED with additional cyst
revealed a mean logRAD score of 0.92 ± 0.28.
Conclusions: In nAMD, a severe deficiency in reading acuity was
observed especially with subfoveal NVC associated with additional
cysts and fibrovascular PED overlying cysts. Morphologic changes of
the central retina have a direct impact on reading ability.
Commercial Relationships: Florian Sulzbacher, None;
Christopher G. Kiss, None; Stefan Sacu, None; Marion R. Munk,
None; Alexandra Kaider, None; Tamara Mittermueller, None;
Philipp K. Roberts, Canon Inc. (F); Ursula Schmidt-Erfurth,
Alcon (C), Bayer Healthcare (C), Novartis (C)
Program Number: 5032 Poster Board Number: A0194
Presentation Time: 2:45 PM - 4:30 PM
Dark-adapted Microperimetry In Age-related Maculopathy And
Geographic Atrophy
Michael D. Crossland1, 2, Rola Ba-Abbad1, 2, Simona Degli Esposti2,
Adnan Tufail2, 3, Gary S. Rubin1, 3. 1UCL Institute of Ophthalmology,
London, United Kingdom; 2Moorfields Eye Hospital NHS
Foundation Trust, London, United Kingdom; 3NIHR Moorfields
Biomedical Research Centre for Ophthalmology, London, United
Kingdom.
Purpose: In order to evaluate the effectiveness of emerging
treatments for geographic atrophy, responsive metrics of visual
function are required. Histological, psychophysical and questionnaire
data indicate reduced rod function in age-related maculopathy (ARM)
and geographic atrophy (GA). In this study we use the new test of
dark-adapted microperimetry on a cohort of patients with ARM and
GA to determine the effectiveness of this test on identifying areas of
retinal abnormality.
Methods: 20 patients with ARM or GA were recruited. Conventional
and dark-adapted microperimetry were performed on a modified
microperimeter (MP-1S, Nidek Technologies, Italy). Perimetry maps
were registered with autofluorescence images (obtained using
Spectralis, Heidelberg Engineering, Germany; superimposed using
Navis software (Nidek Technologies, Italy)). Areas of abnormality on
the autofluorescence image were identified by an ophthalmologist
masked to microperimetry results.
Results: On average, more points were not seen at the highest
intensity on dark-adapted than conventional microperimetry (mean
number of points missed: conventional: 4.45, dark-adapted: 12.2;
matched pairs t-test, p<0.01). Dark-adapted sensitivity was poorer
over areas of abnormality identified on autofluorescence imaging
than over healthy retina (p<0.001). A significant relationship was
identified between abnormal autofluorescence and missed points on
dark-adapted microperimetry (Cochran-Mantel-Haenszel test,
stratified by patient, p<0.0001).
Conclusions: Performance on dark-adapted microperimetry was
poorer than performance on conventional (mesopic) microperimetry
testing in our patients with ARM and GA. Failure to detect a test
point on dark-adapted microperimetry was significantly associated
with the corresponding retinal location being identified as unhealthy
on autofluorescence imaging. These results suggest that dark-adapted
microperimetry may be a useful outcome measure in studies of
geographic atrophy.
Commercial Relationships: Michael D. Crossland, None; Rola
Ba-Abbad, None; Simona Degli Esposti, None; Adnan Tufail,
Allergan (C), Bayer (C), GSK (C), Oculogics (C), Pfizer (C),
Thrombogenics (C), Amakem (C), Heidelberg Engineering (R),
Novarits/Alcon (C), Sanofi/Genzyme (C); Gary S. Rubin, None
Support: National Institute for Health Research grant
PDF/01/2008/011
Program Number: 5033 Poster Board Number: A0195
Presentation Time: 2:45 PM - 4:30 PM
Development of a Dark Adaptation Protocol for Use in AMD
Clinical Trials
Gregory R. Jackson1, John G. Edwards2. 1Ophthalmology, Penn State
College of Medicine, Hershey, PA; 2MacuLogix, Hershey, PA.
Purpose: About 20% of AMD patients exhibit significant worsening
of dark adaptation (DA) over 12 months. This finding supports the
potential use of DA as an endpoint in AMD clinical trials. To
increase acceptance of DA, it is desirable to reduce the test duration
for patients with AMD. The purpose of this project was to develop a
new protocol that reduces test duration by 50% compared with our
previous standard protocol.
Methods: Eleven patients with AMD had their DA measured with
three different dark protocols. Each measurement occurred on a
different day. Protocol #1 was the previous standard. It utilized a
58,000 scotopic cd/m2 sec bleaching flash at a test location of 5o
inferior visual field (VF). Protocol #2 used an 18,000 scotopic cd/m2
sec bleaching flash located at 12o inferior VF. Protocol #3 used a
4,500 scotopic cd/m2 sec bleaching flash located at 12o inferior VF.
Results: Protocol #1 (previous standard) produced the slowest DA
and longest test duration. Protocol #3 produced the fastest DA and
shortest test duration. Protocol #2 produced an intermediate DA
speed and test duration. On average, participants exhibited a ~55%
reduction in test duration for protocol #2 compared with protocol #1.
For a typical AMD patient, protocol #1 produced a rod intercept of
17.5 minutes which was reduced to 7.8 minutes by Protocol #2.
Protocol #3 produced a very fast recovery of dark adaptation
consistent with a rod intercept of 3.1 minutes. For Protocol #3, four
of 11 participants had rod intercepts less than 3.1 minutes. It was
concluded that Protocol #3’s DA functions were too fast to allow for
the possibility of a significant improvement in DA performance in
response to intervention. Thus, Protocol #2 was selected as the
preferred new protocol.
Conclusions: DA measurement in response to a moderate 18,000
scotopic cd/m2 sec bleaching flash located at 12o inferior to the
fixation light produces a wide range of rod intercept values from
about five minutes to 35 minutes across the range of AMD severity
from early AMD to high-risk AMD. This protocol is under further
evaluation in a natural history study and an intervention study.
Further test duration reduction may be possible if the population of
interest is restricted to high-risk AMD patients.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Gregory R. Jackson, MacuLogix (F),
MacuLogix (I), MacuLogix (E), Genentech (R); John G. Edwards,
MacuLogix, Inc (I), MacuLogix, Inc (E), MacuLogix, Inc (P),
MacuLogix, Inc (S)
Support: NIH Grant EY019593
Program Number: 5034 Poster Board Number: A0196
Presentation Time: 2:45 PM - 4:30 PM
High Angular Resolution Peripheral Refraction in Patients with
Age Related Macular Degeneration
Bart Jaeken2, 1, Encarna Alcón1, 3, Jose María Marín3, Pablo Artal1.
1
Laboratorio de Optica, Universidad de Murcia, Murcia, Spain;
2
R&D, Voptica, Murcia, Spain; 3Oftalmología, Hospital Virgen de la
Arrixaca, Murcia, Spain.
Purpose: The Hartmann-Shack (HS) wavefront sensor was used to
determine the peripheral refraction (PR) at specific angles in subjects
with age related macular degeneration (AMD) (Lundström et al.,
Optom Vis Sci 2007). The correction of the PR in those subjects
could improve their visual acuity at eccentric locations. However,
instrumentation specifically designed for accurate and fast measuring
PR was never tested in those patients. Easy determination of PR
could provide those patients with customized corrections.
Methods: We adapted a fast scanning peripheral HS wavefront
sensor previously developed (Jaeken et al., Opt Exp 2011). Its design
makes it possible to measure fast (order of seconds) and with a high
angular resolution (1 measurement/°) a large part of a horizontal
meridian of the visual field (50°). Two fixation methods were tested:
placing the target in the patient’s preferred retinal location (PRL) and
having the PRL aligned to the center of the measuring system. For
both applications a red laser beacon was projected on a wall at 2
meter from the patient. The stability of fixation while scanning was
determined looking at the position of the pupil in each frame of a
scan. PR (sphere and cylinder) was determined from the series of
recorded HS images. The repeatability of 4 consecutive scans was
compared with that in normal elderly eyes. The light distribution
within the HS spots was evaluated intra-patient between the different
retinal areas.
Results: No variation in the quality of the HS images was observed
between the areas with and without retinal damage. Small
displacements of the centre of the pupil were registered, although this
did not affect the refraction results. The repeatability of the 4 scans in
eyes with AMD was not different from that in normal elderly eyes. In
some subjects anomalies were observed in the HS images which are
presumed to come from a plane close to the pupil plane. Since some
of the patients did not undergo cataract surgery, it probably comes
from crystalline lens opacities. The measured PR of PRL varied
among subjects.
Conclusions: An adapted scanning peripheral wavefront sensor was
found to be a functional tool for measuring fast and accurately the PR
in AMD patients. This refractive information can be useful for
customized corrections. For example, they could benefit from a
custom designed intraocular lens adjusted to their exact PR at their
PRL.
Commercial Relationships: Bart Jaeken, PCT/ES2011/070640 (P);
Encarna Alcón, None; Jose María Marín, None; Pablo Artal,
AMO (C), Voptica SL (P), Voptica SL (I), AMO (F), Calhoun Vision
(F), Calhoun Vision (C), AcuFocus (C)
Support: Ministerio de Ciencia e Innovación, Spain (grants
FIS2010-14926 and CSD2007-00013) and Fundación Séneca, Region
de Murcia, Spain (grant 4524/GERM/06)
Program Number: 5035 Poster Board Number: A0197
Presentation Time: 2:45 PM - 4:30 PM
Compensation of fixational instability by the NIDEK MP-1
micro-perimeter
Arunkumar Krishnan, Harold E. Bedell. University of Houston College of Optometry, Houston, TX.
Purpose: Micro-perimeters are used increasingly to assess patients
with central field loss, because of the reported capability of these
instruments to compensate for fixational eye movements and present
test stimuli repeatably at an intended retinal location. In this study we
investigated the precision of eye-movement compensation by the
NIDEK MP-1, when the fixation instability of normal subjects is
increased by changing the size of the fixation target.
Methods: Retinal sensitivity for horizontal (H) and vertical (V)
traverses across one edge of the optic disc were assessed in one eye
of 7 normal subjects, aged 25-35 years. Two fixation targets were
chosen to promote ‘more’ and ‘less’ stable foveal fixation,
respectively: a 1 deg cross and a 10 deg circle. A customized 15 x 2
element array of Goldmann size II test stimuli, each separated by 0.1
deg, was positioned horizontally across the temporal disc margin or
vertically across the inferior or superior disc margin. An in-built 4-21 strategy determined the detection threshold for each stimulus
element in the array. The MP-1 recorded the distribution of fixation
positions during testing, from which the standard deviation (SD) of
fixation was computed in both the H and V directions. Cumulative
Gaussians were fit to the threshold profiles obtained during fixation
on the cross and circle and the fitted SD for the circle fixation target
was compared to the expected value based on an additive-variance
model. Percent compensation during fixation on the circle target was
defined as (expected SD - observed SD) / (expected SD).
Results: Average fixational SDs increased from 0.20 to 0.65 deg (H)
and 0.20 to 0.72 deg (V) for fixation on the cross and circle targets,
respectively. Best-fit Gaussians to the perimetric profiles had SDs
that were not significantly shallower during fixation on the circle
compared to the cross (P = 0.11 [H]; P = 0.68 [V]). The average
percent compensation for the increase in fixation instability on the
circle target, was 91.7% (H) and 86.6% (V), corresponding to an
increase in the SD of retinal image scatter of 2.2 (H) and 3.8 (V) min
arc.
Conclusions: The NIDEK MP-1 compensates well for an increase in
fixational instability in the horizontal and vertical directions. This
compensation ensures that, even in subjects with unstable fixation,
perimetric test stimuli are presented close to the intended retinal
locations.
Commercial Relationships: Arunkumar Krishnan, None; Harold
E. Bedell, None
Support: Minnie flaura turner fund for impaired vision research,
University of Houston sVGR.
Program Number: 5036 Poster Board Number: A0198
Presentation Time: 2:45 PM - 4:30 PM
BCEA evaluation after pattern stimulation in wet AMD patients
Enzo M. Vingolo, Paolo G. Limoli, Serena Fragiotta, Vittoria De
Rosa, Daniela Domanico. UOC Ophthal Hosp "SM Goretti" LT,
University La Sapienza of Rome, Roma, Italy.
Purpose: age related macular degeneration is one of the main cause
of visual impairment in elderly people. We studied and compared the
efficacy of rehabilitation by means of two different type of
biofeedback techniques with MP-1 microperimeter in patients with
evoluted AMD.
Methods: We enrolled 30 patients, mean age 76,38yrs (8,77SD)
bilaterally affected by wet AMD. Patients were randomly divided in
two groups: A was treated with an acoustic biofeedback, group B was
treated with a luminous biofeedback constituted by a black and white
checkerboard flickering during the examination. All patients
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
underwent a complete ophthalmological examination including: best
distance and near visual acuity assessment, reading speed test, MP-1
microperimetry evaluating BCEA. Low vision rehabilitation
consisted in 12 training sessions of 10 minutes for each eye
performed once a week with MP-1 for both groups. Statistical
analysis was performed using Student’s t- test.
Results: After training all patients displayed an improvement in
visual acuity, fixation behaviuor, retinal sensitivity and reading
speed.
Group A: visual acuity was not statistically improved (p=0.054),
reading speed showed statistically significant improvement
(p=0.031), and a statistically significant reduction in average BCEA
fixation (p=0.0023) was evidenced and a mean single point retinal
sensitivity value was also improved (p=0.044).
Group B: visual acuity was statistically higher (p=0.048), reading
speed showed statistically significant improvement (p=0.024), a
statistically significant high reduction in BCEA (p=0.0012) was
evidenced and a mean single point retinal sensitivity value was also
improved (p=0.027).
Conclusions: Our results show that biofeedback techniques can
improve fixation stability. Audio feedback and pattern stimulus
facilites transmission between intraretinal neurons as well as between
the retina and the brain, thereby probably facilitating a remapping
phenomenon.
Furthermore, highly informative and contrast rich pattern stimulus
showed a statistically significant difference towards uninformative
plain exercise limited to train the PRL as obtained with older
software, thus indicating that it is possible with more informative
tasks to reach a wider involvement of cell populations and recruit
more and more efficient ganglion cell receptive fields so to better
utilize the residual retinal function.
Commercial Relationships: Enzo M. Vingolo, None; Paolo G.
Limoli, None; Serena Fragiotta, None; Vittoria De Rosa, None;
Daniela Domanico, None
Support: Sapienza C26A10NRES/2010
Program Number: 5037 Poster Board Number: A0199
Presentation Time: 2:45 PM - 4:30 PM
The Influence of Fixation Stability on Balance in Patients with a
Central Scotoma
Caitlin Murphy1, 4, Janette Chu2, Eoghan Landy2, Jean-Christophe
Campbell2, Amy Phan2, Olga Overbury1, 3. 1School of Optometry,
University of Montreal, Montreal, QC, Canada; 2Physiotherapy,
McGill University, Montreal, QC, Canada; 3Ophthalmology, McGill
University, Montreal, QC, Canada; 4Centre for Interdisciplinary
Research in Rehabilitation (CRIR), Montreal, QC, Canada.
Purpose: Vision is second only to the vestibular system in terms of
its contribution to balance. Research has shown that visually impaired
people (VIPs) often have problems in this domain. Some major visual
disorders damage the central retina. To compensate for the loss of a
functioning fovea, those affected use their remaining peripheral retina
to accomplish daily tasks. This sometimes results in the formation of
an unstable, non-central fixation point. The purpose of this study was
to determine if reduced balance in VIPs is related to unstable fixation.
Methods: Individuals with a visual acuity of 20/200 or better and a
diagnosis of a retinal disorder, were recruited for this study. There
were 44 participants (23 M and 21 F) ranging in age from 47 to 89
years. Fixation stability was determined using the Mirametrix Eye
Tracker and participants were then divided into two groups: stable
fixation and poor fixation. Functional balance was measured using
the Timed Get-Up-and-Go (TUG) and the Berg Balance Scale (BBS).
Balance confidence was assessed using the Activities-Specific
Balance (ABC) Scale. The examiners conducting the balance tests
were masked to the fixation status of the participants.
Results: Performance on the TUG test was significantly different
between the groups, with the poor-fixation group having a slower
TUG time than the stable-fixation group, t (42) = 1.7263, p < .05.
Clinically, taking more than 13.5 seconds to complete the task
indicates an increased risk of falls. The poor fixation stability group
had a mean score of 14.3 seconds. There was no significant
difference in functional balance between the stable- and unstablefixation groups as determined by the BBS. Subjects with poor
fixation stability scored lower on the ABC scale compared to the
stable fixation group, t (42) = -1.856, p < .05. However, their scores
were not low enough to have any clinical significance.
Conclusions: Based on the TUG, VIPs with unstable fixation are at a
higher risk of falls compared to those with stable fixation. Although
there is a statistically significant difference between the two groups
on the ABC scale, it is not great enough to conclude that those with
poor fixation are at risk of falls.
Commercial Relationships: Caitlin Murphy, None; Janette Chu,
None; Eoghan Landy, None; Jean-Christophe Campbell, None;
Amy Phan, None; Olga Overbury, None
Program Number: 5038 Poster Board Number: A0200
Presentation Time: 2:45 PM - 4:30 PM
Impact of Visual Motion Displayed in a Non-Immersive HeadMounted Device on the Balance of Patients with Age-Related
Macular Degeneration
Caroline Chauvire1, Coen Cecilia1, Arnaud Koustanai1, Johan Le
Brun1, Samuel Pineau1, Thierry Villette2, Philippe Chaumet-Riffaud1,
3
, Saddek Mohand-Said1, Jose A. Sahel1, Avinoam B. Safran1.
1
INSERM, U968; UPMC Univ Paris 06, UMR_S 968, Institut de la
Vision; CNRS, UMR_7210; CHNO des Quinze-Vingts, INSERMDHOS CIC 503, Paris, France; 2Essilor R&D International, Paris,
France; 3Univ Paris Sud, AP-HP, CHU Bicêtre, Paris, France.
Purpose: Age-related Macular Degeneration (AMD) results in a
reduced visual acuity (VA). Head-Mounted Displays (HMD) may be
useful for affected individuals, by magnifying, freezing and dragging
the view, vertically or horizontally, to relieve from reduced field of
vision due to magnification. However, changes in image (size and
movements) are susceptible to disturb visuomotor coordination and
thus to disrupt postural control. The aim of this study was to evaluate
the impact of changes in image on the balance of AMD patients,
when using a non-immersive HMD.
Methods: Three groups were included: 12 patients with atrophic
AMD (AMDs: age between 62 and 81 years, mean 70; VA between
+1.22 and +0.28 logMAR , mean +0.62), 6 older healthy subjects
(OH: age between 65 and 75 years, mean 70; VA between 0 and -0.2
logMAR, mean -0.04), and 5 young healthy subjects (YH: age
between 30 and 48 years, mean 37 ; VA between +0 and -0.1
logMAR, mean -0,01).
Subjects stood in the dark on a stable force plate. A virtual street was
projected onto a wall-screen. For comparison, subjects were tested
without HMD eyes closed (EC) and eyes open (EO). When tested
with HMD, subjects wore a non-immersive binocular opto-electronic
device, displaying an image through transparent lenses. They viewed
the scene moving successively in vertical and horizontal directions
and from one size to another. In non-immersive mode, subjects
viewed the scene both onto the wall-screen and in-motion through the
HMD. In immersive mode, they only viewed the scene in-motion
through HMD.
Average velocity of center of pressure (V) was recorded. Each trial
lasted 51.2 s and was repeated 3 consecutive times.
Results: Difference between EO and EC was greater in OH than in
AMDs and YH (p<.03). V was higher in immersive than in non-
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
immersive mode (p<.01). There was no significant difference
between AMDs and OH (p=.7). The postural effects generated by the
HMD image did not differ according to groups or modes of
presentation. (p=.4).
Conclusions: AMD patients demonstrated a smaller visual
contribution to postural control than age-matched healthy subjects.
Visual motion generated by the HMD did not induce stronger balance
disruption in AMD patients than in healthy subjects, and never
exceed sway in EC. Furthermore, immersive condition generated
more instability than non-immersive condition for all subjects.
Commercial Relationships: Caroline Chauvire, None; Coen
Cecilia, None; Arnaud Koustanai, None; Johan Le Brun, None;
Samuel Pineau, None; Thierry Villette, ESSILOR (E), ESSILOR
(P); Philippe Chaumet-Riffaud, None; Saddek Mohand-Said,
None; Jose A. Sahel, UPMC/Essilor (P), Second Sight (F); Avinoam
B. Safran, essilor (F)
Program Number: 5039 Poster Board Number: A0201
Presentation Time: 2:45 PM - 4:30 PM
Comparing the fixational and functional preferred retinal locus
Brian Sullivan, Laura Renninger. Smith-Kettlewell Eye Research
Institute, San Francisco, CA.
Purpose: Individuals with central vision loss (CVL) may adopt a
preferred retinal locus (PRL) to eccentrically view stimuli in
peripheral retina. PRLs are often defined by measuring the location
and extent of peripheral retinal subtended by a small fixation stimulus
viewed monocularly with the head stabilized. It is not known if this
‘fixational’ PRL is representative of situations where binocular vision
and head movements are allowed, or when stimulus properties are
varied.
Methods: Monocular visual fields were recording by having subjects
detect small suprathreshold stimuli using a scanning laser
ophthalmoscope (SLO). Fixational PRLs were measured by having
subjects fixate a stimulus for 10s and fitting a bivariate contour
ellipse to this data. Using a similar methodology, a second setup
using a binocular eye tracker, chin rest and monitor was used to
record monocular and binocular visual fields and fixational PRLs.
Subjects then participated in a reaching task where their functional
PRLs could be evaluated and compared to the fixational PRLs
described above. Subjects performed unspeeded reaches to targets
presented on a LCD touch screen at a one of eight of positions
presented at three eccentricities (5,10 and 15°). Trials were blocked
so that subject made reaches with or without head movements,
monocularly and binocularly. ‘Functional’ PRLs were measured by
using the location of the reach target in the visual field at the reach
endpoint.
Results: We have established means to measure monocular visual
fields in the SLO and on a computer monitor, with reasonable
agreement. Additionally, binocular visual fields may be predicted
from the monocular SLO data and compared to measured binocular
fields assessed with the eye tracker setup. We present fixational and
functional PRL data, including location and extent, using the
bivariate contour ellipse area. Preliminary results give evidence that
the fixational PRL is not always representative of the functional PRL.
Subject reach duration and accuracy data are also presented.
Conclusions: Although an ongoing study, our data thus far suggest
that the PRL is flexible under task changing stimulus conditions
during a reaching task. Further study is needed to better delineate the
circumstances in which this flexibility occurs.
Commercial Relationships: Brian Sullivan, None; Laura
Renninger, None
Program Number: 5040 Poster Board Number: A0202
Presentation Time: 2:45 PM - 4:30 PM
Maximum Reading Speed and Binocular Summation in Patients
with Central Vision Loss
Luminita Tarita-Nistor1, 2, Esther G. Gonzalez1, 2, Michael H. Brent3,
4
, Samuel N. Markowitz3, 4, Martin J. Steinbach1, 2. 1Vision Science
Research Program, Toronto Western Hospital, Toronto, ON, Canada;
2
Centre for Vision Research, York University, Toronto, ON, Canada;
3
Ophthalmology and Vision Sciences, University of Toronto,
Toronto, ON, Canada; 4Ophthalmology, Toronto Western Hospital,
Toronto, ON, Canada.
Purpose: Visual acuity is a poor predictor of the maximum reading
speed of patients with central vision loss. We hypothesized that the
maximum reading speed is a function of binocular summation of
acuity for these patients.
Methods: Maximum reading speed of 20 patients with central vision
loss (mean age = 77 ± 13 years) was measured binocularly using the
MNRead charts. Monocular and binocular acuities were measured
with the ETDRS chart. Binocular summation was evaluated with a
binocular ratio (BR) calculated as the ratio between the acuity of the
better eye to binocular acuity. Fixation stability and PRL distance
from the former fovea were evaluated with the MP-1 microperimeter.
Results: Six patients experienced acuity summation (BR > 1.05), 5
experienced acuity inhibition (BR < 1.05), and 9 showed equality
(BR = 1 ± .05). There were no differences in the mean acuity of the
better eye, fixation stability, or PRL distance from the fovea of the
three groups. Maximum reading speed was significantly slower (p <
.05) for patients who experienced binocular inhibition (mean 42 ± 27
wpm, median 40 wpm) than for those who experienced binocular
summation (mean 107 ± 39 wpm, median 108 wpm), or equality
(mean 111 ± 62 wpm, median 90 wpm). BR correlated with the
maximum reading speed for the overall sample (r(18) = .49, p = .03).
BR together with PRL distance from the former fovea in the better
eye explained 45% of the variance in maximum reading speed.
Conclusions: Binocular summation of acuity rather than visual
acuity alone predicts maximum reading speed of patients with central
vision loss. Patients with binocular inhibition read significantly
slower than those with binocular summation or equality. Assessment
of binocular summation is important when devising reading
rehabilitation techniques.
Commercial Relationships: Luminita Tarita-Nistor, None; Esther
G. Gonzalez, None; Michael H. Brent, None; Samuel N.
Markowitz, None; Martin J. Steinbach, None
Support: Milton Harris Fund for Adult Macular Degeneration
(MHB); Natural Sciences and Engineering Research Council of
Canada (NSERC) grant A7664 (MJS); Vision Science Research
Program, Toronto Western Hospital; Sandra and David Smith
postdoctoral fellowship; and an anonymous donor.
Program Number: 5041 Poster Board Number: A0203
Presentation Time: 2:45 PM - 4:30 PM
Predictive Factors of Reading Performance Post Reading
Rehabilitation Program in Central Field Loss Patients
Salvatore Di Lauro, Maria B. Coco, Alberto López-Miguel, Rubén
Cuadrado, Agustin Mayo, José Alberto De Lázaro, Miguel J.
Maldonado, Joaquín Herrera, Laura Mena, Jose-Carlos Pastor.
Retina- Low Vision, IOBA Eye Institute, University of Valladolid,
Valladolid, Spain.
Purpose: Reading is the main complaint of central field loss (CFL)
patients. Reading fluency might depend on visual and psychosocial
factors, thus this study assesses whether visual and psychosocial
variables can predict reading performance (RP) after a reading
rehabilitation program (IOBA-RRP).
Methods: Seventy-six CFL patients were recruited at IOBA-Eye
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Institute from the vision rehabilitation unit. Patients without previous
experience of low vision optical aids use underwent a vision
rehabilitation program (the IOBA-RRP). Visual (reading speed and
duration, visual acuity and magnification) and psychosocial
questionnaire outcomes were recorded before and after undergoing
the 6-week training. Odds ratios (ORs) were calculated to assess the
predictive value of these variables.
Results: Contrast sensitivity (OR’s: 2.94, 95% confidence intervals
(CI): 0.99-8.33), age (OR’s: 0.21, 95% CI: 0.06-0.74) and Geriatric
Depression Scale (GDS) score (OR’s: -2.33, 95% CI: 1.16-4.76) were
associated with improvement in reading speed.
Conclusions: Better contrast sensitivity, older age and lower GDS
scores can predict success on reading fluency in CFL patients after
reading rehabilitation training.
Commercial Relationships: Salvatore Di Lauro, None; Maria B.
Coco, None; Alberto López-Miguel, VISIÓN I+D, SL (E); Rubén
Cuadrado, None; Agustin Mayo, None; José Alberto De Lázaro,
None; Miguel J. Maldonado, None; Joaquín Herrera, None;
Laura Mena, None; Jose-Carlos Pastor, None
Support: RD 12/0034/0001
Program Number: 5042 Poster Board Number: A0204
Presentation Time: 2:45 PM - 4:30 PM
Do Pedestrians Make Safe Street-Crossing Decisions?
Shirin E. Hassan. School of Optometry, Indiana University,
Bloomington, IN.
Purpose: The aim of this study was to determine whether the streetcrossing decisions of subjects with Age-related Macular
Degeneration (AMD) are as safe as those made by young and older
subjects with normal vision.
Methods: Street-crossing decisions and crossing times in 12 AMD
subjects, 20 young and 20 older control subjects with normal vision
were measured along an unsignalized street for nine different gap
time categories. Using their habitual vision and hearing, subjects
observed an approaching vehicle for two seconds. At the end of the
two second period, subjects were required to make a crossing
decision of whether or not they thought it was safe to cross the street.
Subjects’ crossing decisions were then objectively classified as being
“safe” when the measured gap time was longer than the subject’s
street-crossing time. The converse was true for objectively
classifying crossing decisions as being “unsafe”. The proportion of
safe crossing decisions (ie. subjects reporting it was safe to cross for
objectively safe gap times) and unsafe crossing decisions (ie. subjects
reporting it was safe to cross for objectively unsafe gap times) was
determined for each subject group and gap time category. A
hierarchical logistic regression, with repeated measures for subject,
was used to determine if the proportion of safe and unsafe decisions
changed as a function of subject group and gap time category.
Results: We observed that the older normally-sighted subjects made
more unsafe crossing decisions compared to the AMD subjects for
gap times that were between four and one second shorter than the
time they needed to cross the street. However, the differences
between these two groups were only marginally significant (p=0.06,
p=0.05, p=0.04 and p=0.05 for gap times that were four, three, two
and one second shorter than subjects’ crossing times, respectively).
No significant difference in the proportion of unsafe decisions were
found between the young and older normally-sighted subjects
(p>0.05) and between the young normally-sighted and AMD subjects
(p>0.05). No significant differences in the proportion of safe crossing
decisions were also found between the different subject groups for
gap times that were longer than subjects’ crossing times (p>0.05).
Conclusions: Our data suggests that older pedestrians with normal
vision have a tendency to adopt a more risky crossing strategy than
either the young normally-sighted or AMD pedestrians.
Commercial Relationships: Shirin E. Hassan, None
508 Improving Imaging and Ophthalmic Instrumentation
Thursday, May 09, 2013 8:30 AM-10:15 AM
Exhibit Hall Poster Session
Program #/Board # Range: 5543-5554/B0053-B0064
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 5543 Poster Board Number: B0053
Presentation Time: 8:30 AM - 10:15 AM
Stabilized cone imaging with adaptive optics optical coherence
tomography
Omer P. Kocaoglu1, R. D. Ferguson2, Zhuolin Liu1, Ravi S. Jonnal1,
Qiang Wang1, Daniel X. Hammer3, Donald T. Miller1. 1School of
Optometry, Indiana University, Bloomington, IN; 2Physical Sciences
Inc., Andover, MA; 3Office of Science and Engineering Laboratories,
Center for Devices and Radiological Health, Food and Drug
Administration, Silver Spring, MD.
Purpose: Cone photoreceptors exhibit a complex optical signature
that has become increasingly valuable in ophthalmologic
examination. Adaptive optics optical coherence tomography (AOOCT) is a highly sensitive method that is particularly well suited for
3D imaging the cone signature. Like all in vivo retinal imaging
methods, however, AO-OCT suffers from the effects of involuntary
eye movements that blur and distort the image, especially at the cone
level. Compensation of movement can be realized with registration
algorithms in post processing or dynamic retinal tracking in
hardware. Tracking is particularly attractive for AO-OCT as it can
compensate for eye motion larger than the imaging field of view and
permits repeated imaging of the same retinal patch. In light of these
advantages, this study examines the efficacy of an active retinal
tracker integrated into AO-OCT for cone imaging.
Methods: The 2nd-generation Indiana AO-OCT system was
integrated with a customized retina tracker module. Key AO-OCT
components included a broadband light source (λc=800nm,
Δλ=160nm, bandpassed to Δλ=80nm), an astigmatism-free sample
arm, and a high-speed linescan camera operating at 100K Alines/s.
The tracker module was designed to stabilize the location of the AOOCT beam relative to a specific retinal landmark tracked at 1060nm,
and to provide a 35° field of view SLO image at 950 nm. Closed-loop
tracking performance was assessed by comparing cone motion in
1.8°x1.8° volume videos acquired with and without dynamic retinal
tracking. Videos were obtained at 4° nasal and 3° superior to the
fovea of a normal subject (30 yrs). Five sessions of volume videos
were collected, each consisting of five volumes (1 vol/s). En face
projections of the AO-OCT volumes were assessed for lateral cone
motion. To avoid masking tracker performance, no post-processing
registration was applied to the videos.
Results: The average maximum cone displacement was 18±5μm
with tracking compared to 150±107μm without tracking, a factor of
eight improvement. The corresponding contrast improvement in the
averaged en face cone image was 38% (p=0.008). Tracking was
sufficiently robust to find repeatedly the same cone patch across
sessions.
Conclusions: Dynamic tracking stabilized AO-OCT cone images,
sufficiently so for monitoring the same cones over time.
Commercial Relationships: Omer P. Kocaoglu, None; R. D.
Ferguson, Physical Sciences Inc (E), Physical Sciences Inc (P);
Zhuolin Liu, None; Ravi S. Jonnal, 7,364,296 (P); Qiang Wang,
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
None; Daniel X. Hammer, Physical Sciences Inc. (C), Physical
Sciences Inc. (P); Donald T. Miller, n/a (P)
Support: NEI Grants 5R01 EY014743, 1R01 EY018339,
P30EY019008
Program Number: 5544 Poster Board Number: B0054
Presentation Time: 8:30 AM - 10:15 AM
In vivo Imaging of the Human Retinal Pigment Epithelium Cell
Mosaic using Short-wavelength Autofluorescence and
achromatizing lenses
Alfredo Dubra1, 2, Drew H. Scoles3, Yusufu N. Sulai4.
1
Ophthalmology, Medical College of Wisconsin, Milwaukee, WI;
2
Biophysics, Medical College of Wisconsin, Milwaukee, WI;
3
Biomedical Engineering, University of Rochester, Rochester, NY;
4
The Institute of Optics, University of Rochester, Rochester, NY.
Purpose: Although adaptive optics (AO) imaging of the human
retinal pigment epithelium (RPE) cell mosaic using intrinsic
fluorescence has been recently demonstrated, it remains difficult to
perform. This is mostly due to light safety limitations, the presence of
longitudinal chromatic aberration (LCA) in the eye and more
importantly, its variation across individuals. This last point
complicates the focusing of the illumination (excitation) and the
imaging (emission) channels, as they need to be adjusted for each
individual. Here we explore the use of achromatizing lenses to
mitigate this problem by compensating for the LCA that would be
found in an average eye, thus bringing to closer focus the excitation
and emission wavelength ranges.
Methods: An AO scanning light ophthalmoscope (AOSLO) that
allows simultaneous near-infrared (NIR) and visible imaging was
modified with achromatizing lenses in the pupil planes of the
illumination and imaging paths. Images were recorded in four
subjects using a 2° field of view, 30 μW of 850 nm light for
wavefront sensing, 92 μW of 790 nm light for reflectance imaging
and 60 μW of 560-570 nm light for fluorescence excitation. At each
retinal location, the excitation was first brought into focus onto the
photoreceptor layer in reflectance, and then shifted towards the RPE.
This was followed by simultaneous NIR reflectance and fluorescence
imaging during 60-120 seconds using a 2.5 Airy disk confocal
aperture and a 625 nm central wavelength (90 nm bandwidth) in the
visible channel.
Results: Imaging the photoreceptor mosaic using a broadband
excitation light source (10 nm bandwidth) in reflectance greatly
facilitates the focusing of the RPE imaging in fluorescence. The
contiguous RPE cell mosaic can be visualized using safe light levels
in human subjects after recording images at multiple foci.
Conclusions: RPE imaging at the cellular scale is facilitated by the
use of achromatizing lenses, although further improvement to this
method requires accounting for inter-subject variations of LCA. The
ability to visualize the RPE mosaic holds promise for studying and
diagnosing retinal degenerations such as age related macular
degeneration, as well as evaluating new therapies.
RPE cell mosaic in two different human subjects, with the fluorescent
signal originating from lipofuscin containing granules (scale bars are
50 μm across).
Commercial Relationships: Alfredo Dubra, US Patent No:
8,226,236 (P); Drew H. Scoles, None; Yusufu N. Sulai, None
Support: Glaucoma Research Foundation Grant Catalyst for a Cure
grant, Research to Prevent Blindness Career Development Award and
Burroughs Wellcome Fund CASI award.
Program Number: 5545 Poster Board Number: B0055
Presentation Time: 8:30 AM - 10:15 AM
A novel compact optical instrument for the clinical measurement
of intraocular light scattering
Onurcan Sahin1, Harilaos S. Ginis2, 1, Guillermo M. Perez3, Juan M.
Bueno2, Pablo Artal2. 1Institute of Vision & Optics, University of
Crete, Heraklion, Greece; 2Laboratorio de Optica, Universidad de
Murcia, Murcia, Spain; 3Voptica SL, Murcia, Spain.
Purpose: To develop a compact instrument to measure light
scattering in the human eye for angles in the range between 3 and 9
degrees of visual angle.
Methods: The instrument is based on a previous laboratory setup
using extended light sources in a double-pass (DP) configuration
(Ginis et al., J of Vision, 2012). The light source is an array of green
(528±10 nm) light emitting diodes (LEDs) spatially homogenized by
light shaping diffusers. The field is separated in 2 zones: a central
area (corresponding to visual angles from 0 to 3 degrees (in radius)
and an annular area (3 to 9 degrees). In both zones LEDs are squarewave temporally modulated at 483 Hz and 769 Hz for the central and
peripheral areas respectively. Two annular diaphragms conjugated
with the cornea and the lens allow the projection of the source on to
the retina while leaving the central part of the pupil free of back
scattered light and reflections. Light reflected from the fundus is
sensed through a circular diaphragm conjugated with the center of the
pupil with no overlapping of the illumination and measurement paths.
A pupil camera controls the alignment. The light reflected from the
central retinal area (15-arcmin) is selected through a circular
diaphragm and a pinhole by a photodiode. The Fourier transform of
the signal reveals the contribution of each annulus and therefore the
average intensity of scattered light for the corresponding angles. The
total measurement time is 200 msec.
Results: Functionality, sensitivity and repeatability of the method
were demonstrated with an artificial eye and two different previously
characterized diffusers. The equivalent logarithm of the straylight
parameter measured for the diffusers were 0.67 (SD=0.005) and 0.84
(SD=0.003), values not statistically significantly different than the
anticipated. Pilot measurements in human eyes were also obtained. A
careful analysis of the artifacts associated to alignment and refractive
errors was also performed.
Conclusions: A new compact instrument suitable for routine or
clinical measurements of light scattering in the eye was developed. It
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
builds on previous experience with multi-wavelength, highsensitivity, imaging double-pass system for the measurement the
wide-angle point-spread function of the eye.
Commercial Relationships: Onurcan Sahin, None; Harilaos S.
Ginis, Universidad de Murcia (P); Guillermo M. Perez, VOPTICA
(E); Juan M. Bueno, None; Pablo Artal, AMO (C), Voptica SL (P),
Voptica SL (I), AMO (F), Calhoun Vision (F), Calhoun Vision (C),
AcuFocus (C)
Support: ITN OpAL (PITN-GA-2010-264605), Ministerio de
Ciencia e Innovación, Spain (grants FIS2010-14926 and CSD200700013), Fundación Séneca (Region de Murcia, Spain), grant
4524/GERM/06.
Program Number: 5546 Poster Board Number: B0056
Presentation Time: 8:30 AM - 10:15 AM
The Effect of AOSLO Image Distortion on Metrics of Mosaic
Geometry
Robert F. Cooper1, Zachary Harvey2, Michael Dubow3, 4, Yusufu N.
Sulai5, Alexander Pinhas3, 4, Drew H. Scoles6, Nishit Shah3, Richard
B. Rosen3, Alfredo Dubra2, 7, Joseph Carroll2, 8. 1Biomedical
Engineering, Marquette University, Milwaukee, WI;
2
Ophthalmology, Medical College of Wisconsin, Milwaukee, WI;
3
New York Eye and Ear Infirmary, New York, NY; 4Mount Sinai
School of Medicine, Mount Sinai Hospital, New York, NY; 5The
Institute of Optics, University of Rochester, Rochester, NY;
6
Biomedical Engineering, University of Rochester, Rochester, NY;
7
Biophysics, Medical College of Wisconsin, Milwaukee, WI; 8Cell
Biology, Medical College of Wisconsin, Milwaukee, WI.
Purpose: Adaptive Optics Scanning Light Ophthalmoscopes
(AOSLOs) permit near diffraction-limited imaging of the human
photoreceptor mosaic, though intraframe eye movements lead to
image distortion. Here, we explore the impact of these distortions on
a number of metrics commonly used to characterize the
photoreceptor mosaic.
Methods: We acquired 9 image sequences of the parafoveal cone
mosaic from 7 subjects on 3 similar AOSLOs. In another subject, we
acquired an AOSLO and flood-illuminated AO image sequences of
the same retinal location. To assess the effect of distortions within
AOSLO images, ten averaged images were produced by registering
against different reference frames using a previously described
algorithm. The images were then registered with the same software
while tracking the distortion applied to each image. The
photoreceptor coordinates from the reference frame were transformed
using this distortion. Voronoi geometry, cone density, nearestneighbor distance (NND), inter-cell spacing (ICS), and regularity
index (RI) were calculated for each set of images. Repeatability was
calculated to assess the effect of intraframe distortion on these
metrics.
Results: Across the AOSLO images, we analyzed 17,942 cones, 75%
of which retained the number of sides in the corresponding Voronoi
domains across the 10 images (range 56%-90%). Cone density was
found to have a repeatability of 1.8% (i.e., the difference between any
2 measurements on the same subject would be less than 1.8% for
95% of observations). NND and ICS had even better repeatability, at
1.4% and 0.95%, respectively. In contrast, the NND RI and ICS RI
had a repeatability of 11% and 31%, respectively. Comparing an
AOSLO image set to a flood-illuminated AO image, we found
similar repeatability (density: 2.7%, NND: 0.7%, ICS: 0.83%, NND
RI: 8.9%, ICS RI: 20.3%) and 83% of cells had retained Voronoi
geometry.
Conclusions: Global metrics (density and cell spacing) are minimally
affected by intraframe distortions, whereas local metrics (regularity
index and Voronoi geometry) are more significantly affected.
Intraframe distortion in AO scanning instruments limits the
measurement accuracy of mosaic geometry, thus every effort should
be made to choose minimally distorted reference frames.
Commercial Relationships: Robert F. Cooper, None; Zachary
Harvey, None; Michael Dubow, None; Yusufu N. Sulai, None;
Alexander Pinhas, None; Drew H. Scoles, None; Nishit Shah,
None; Richard B. Rosen, Opko-OTI (C), Optos (C), Clarity (C),
OD-OS (C), Topcon (R), Zeavision (F), Genetech (F), Optovue (C);
Alfredo Dubra, US Patent No: 8,226,236 (P); Joseph Carroll,
Imagine Eyes, Inc. (S)
Support: RPB, NIH (UL1RR031973, EY017607, EY001931),
Foundation Fighting Blindness, Alcon Research Institute, Burroughs
Wellcome Fund
Program Number: 5547 Poster Board Number: B0057
Presentation Time: 8:30 AM - 10:15 AM
Photoreceptor imaging with in-the-plane adaptive optics optical
coherence tomography using toroidal mirrors
Zhuolin Liu, Omer P. Kocaoglu, Qiang Wang, Donald T. Miller.
School of Optometry, Indiana University, Bloomington, IN.
Purpose: Recent technological advances in adaptive optics (AO) and
high-resolution ophthalmoscopy have resulted in sharper images of
the cellular retina than previously possible. As part of these ongoing
developments, we have re-engineered the Indiana AO-OCT system to
improve imaging performance. In this study, we assessed system
performance for imaging the 3D structure of photoreceptors.
Methods: The 2nd generation Indiana AO-OCT system is based on a
novel in-the-plane design of an off-axis ophthalmic AO system
realized with toroidal mirrors. Unlike conventional designs that rely
on all spherical mirrors, the inclusion of toroidal mirrors avoids
accumulation of system astigmatism and unwanted beam
displacement at pupil conjugate planes. As part of the new design, the
AO system was upgraded with a 97-magnetic-actuator ALPAO
wavefront corrector to improve stroke and fidelity, and a ShackHartmann wavefront sensor configured with an Andor Neo scientific
CMOS camera to improve sensitivity and speed. To assess
performance, volume images of the retina with focus at the
photoreceptor layer were acquired at retinal eccentricities ranging
from the fovea to 6 degrees in human subjects. Power spectra were
computed of en face images at different depths in the photoreceptor
layer. Each spectrum was radially averaged to increase signal to
noise.
Results: Ray trace analysis of the in-the-plane design predicts
diffraction-limited imaging across the entire 3.6°x3.6° field of view
of the AO-OCT system. Beam displacement of less than the pitch of
the SHWS lenslet array is also predicted, thus enabling the full
sensitivity of the SHWS to high spatial frequencies. Measured beam
displacement and wavefront root-mean-square error of the system
confirmed the theoretical predictions. Cone photoreceptors were
routinely observed at retinal eccentricities as small as 0.2 degrees.
This corresponds to cones narrower than that detected with the
previous Indiana AO-OCT system. Analysis of power spectra at the
inner segment / outer segment junction, and posterior tip of the outer
segment revealed more energy at high spatial frequencies.
Conclusions: The 2nd-generation Indiana AO-OCT system provides
a more detailed view of the photoreceptor optical signature than the
previous generation system.
Commercial Relationships: Zhuolin Liu, None; Omer P.
Kocaoglu, None; Qiang Wang, None; Donald T. Miller, n/a (P)
Support: NIH R01EY018339, NIH R01EY014743, NIH
P30EY019008
Program Number: 5548 Poster Board Number: B0058
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Presentation Time: 8:30 AM - 10:15 AM
Evaluation of a Dual-Conjugate Adaptive Optics Clinical
Prototype for Retinal Imaging
Zoran Popovic1, Jörgen Thaung1, Bengt Svensson2, Mette OwnerPetersen1. 1Department of Ophthalmology, University of
Gothenburg, Mölndal, Sweden; 2Exomed AB, Sollentuna, Sweden.
Purpose: To investigate the applicability of a new dual-conjugate
adaptive optics clinical prototype for wide-field high-resolution
adaptive optics retinal imaging in healthy volunteers and patients
with early stages of retinal disease.
Methods: A new design of a compact dual-conjugate adaptive optics
clinical prototype has been built and used to image healthy volunteers
and patients with early stages of retinal disease such as age-related
macular degeneration (AMD) and diabetic retinopathy (DR).
The clinical prototype, based on the concept of dual-conjugate
adaptive optics, employs five spatially separated retinal probe
beacons, two magnetic deformable mirrors (DM) (ALPAO,
Grenoble, France), and a multi-channel Shack-Hartmann wavefront
sensor.
Monochromatic aberrations are measured and corrected over a 6 mm
pupil. The five probe beacons are generated using light at a
wavelength of 830±10 nm from a superluminescent diode (Superlum,
Cork, Ireland). A 52 actuator DM positioned in a plane conjugate to
the pupil of the eye will apply an identical correction for all fieldpoints in the field of view (FOV). A 97 actuator DM positioned in a
plane conjugated to a plane inside the eye will contribute with
partially individual corrections for the five angular directions and
thus compensate for non-uniform (anisoplanatic) or field-dependent
aberrations. Imaging is performed over a 7x7 deg FOV using a
spectrally filtered Xenon flash at a wavelength of 575±10 nm.
Results: The dual-conjugate adaptive optics clinical prototype
features a 7x7 degree FOV and allows retinal features down to 2 μm
to be resolved. A narrow depth of field of approximately 9 µm in the
retina enables tomographic imaging of separate retinal layers, such as
the cone photoreceptor layer deep within the retina in AMD patients,
and superficial retinal capillary layers in DR patients.
Conclusions: High resolution adaptive optics retinal imaging has
enabled the vision research community to gain deeper insight into the
development and progression of retinal diseases. We believe that the
dual-conjugate adaptive optics clinical prototype has a future
potential for clinical imaging with an impact particularly important
for early diagnosis of retinal diseases, follow-up of treatment effects,
and follow-up of disease progression.
Commercial Relationships: Zoran Popovic, US7639369 (P),
PCT/EP2012/069620 (P), EP12165365 (P); Jörgen Thaung,
US7639369 (P), PCT/EP2012/069620 (P), EP12165365 (P); Bengt
Svensson, Exomed AB (E), PCT/EP2012/069620 (P), EP12165365
(P); Mette Owner-Petersen, US7639369 (P), PCT/EP2012/069620
(P), EP12165365 (P)
Support: Marcus and Amalia Wallenberg's Memorial Fund Grant
MAW 2009.0053, Vinnova Grant 2010-00518
Program Number: 5549 Poster Board Number: B0059
Presentation Time: 8:30 AM - 10:15 AM
AO-OCT Retinal Imaging with 163-Segment Deformable Mirror
Susanna C. Finn1, Cherry Greiner1, Nathan Doble1, Robert J.
Zawadzki2, John S. Werner2, Stacey S. Choi1. 1Vision Science, New
England College of Optometry, Boston, MA; 2Ophthalmology &
Vision Science, University of California Davis, Davis, CA.
Purpose: Adaptive Optics (AO) has enabled vision scientists to
directly image single retinal cells in vivo. We have constructed an
AO Fourier-domain Optical Coherence Tomography (AO-FD-OCT)
system utilizing a high segment count microelectromechanical
systems (MEMS) deformable mirror (DM). This DM provides much
higher spatial correction over a 7.5mm dilated pupil (Doble et al.
Applied Optics 2007), providing diffraction-limited imaging. We
describe retinal imaging results obtained on a range of human
subjects.
Methods: An AO-FD-OCT was designed and constructed at the New
England College of Optometry. The AO-OCT system acquires Bscans made up of 600 A-scans at a frame rate of 60 Hz. A Superlum
broadband superluminescent diode (SLD) light source is used with a
central wavelength of 860nm and a full bandwidth of 135nm.
Imaging data are post-processed and analyzed with custom Matlab
software. The AO system consists of a Hartmann-Shack wavefront
sensor and a 163-segment, 489-actuator Iris AO MEMS DM. The
AO-OCT is designed for a 7.5mm pupil, with 13 discrete mirror
segments across the pupil diameter.
Retinal images were obtained on normal human subjects at 4 and 10
degrees in the nasal retina. The scan size for each B-scan was 0.5°,
corresponding to approximately 150µm at the retina.
Results: Distinct retinal layers were visible from the nerve fiber
layer, to the inner and outer photoreceptor segments, through to the
retinal pigment epithelium. Moreover, individual cone photoreceptors
were clearly visible in images at 4 and 10 degrees eccentricity. The
lateral spacing of the cones was measured to be 6.4±1.5 microns at 4°
nasal, and 10.4±3.8 microns at 10°. The inner segment length of the
cones was found to be 32.9±5.7 microns at 4°, and 24.5±3.0 microns
at 10°. The outer segment length was correspondingly found to be
26.2±1.9 microns at 4°, and 27.8±1.4 microns at 10°. These results
are in good agreement with histology.
Conclusions: The combination of AO with the use of a higher
segment MEMS DM with established OCT technology has enabled
us to resolve fine retinal structure unseen with conventional OCT
technologies and promises to be highly valuable in the study of
retinal disease and injury.
Commercial Relationships: Susanna C. Finn, None; Cherry
Greiner, None; Nathan Doble, Iris AO Inc (I); Robert J.
Zawadzki, None; John S. Werner, None; Stacey S. Choi, None
Support: DoD Grant W81XWH-10-1-0738
Program Number: 5550 Poster Board Number: B0060
Presentation Time: 8:30 AM - 10:15 AM
Use of multiple metrics to describe the parafoveal cone mosaic
Marco Lombardo1, Sebastiano Serrao1, Pietro Ducoli1, Giuseppe
Lombardo2, 3. 1Fondazione GB Bietti IRCCS, Rome, Italy; 2CNRIPCF Unit of Support Cosenza, Rende, Italy; 3Vision Engineering,
Rome, Italy.
Purpose: To investigate the distribution of cone density and spacing
as well as the preferred packing arrangement of the cone mosaic as a
function of retinal eccentricity.
Methods: A flood-illumination adaptive optics retinal camera was
used to obtain images of the parafoveal cone mosaic in nineteen
healthy volunteers. Cone density and spacing were estimated for each
subject using a sampling window of 80 x 80 pixels, at 250-, 450-,
650- and 1100-um eccentricities from the fovea along the nasal and
temporal retina of both eyes. The inter-subject and intra-subject
variation of cone density and spacing were calculated via Coefficient
of Variation (CoV). Cone packing arrangement was assessed using
Voronoi analysis; calculations were done over 1024x128 pixels
image sections of the cone mosaic across the horizontal meridian
from 200- to 1050-um eccentricities.
Results: The inter-subject variation of parafoveal cone density
ranged between 10% and 15% (P<0.001) and the intra-subject
variation of cone density was lower than 8% in all subjects, except
for two. The cone spacing values showed a moderate inter-subject
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
(CoV<7%; P<0.001) and a low intra-subject variation (CoV<4% in
all subjects, except for two cases). In the parafoveal region, 40% to
50% of cones were hexagonally arranged; the percentage of nonhexagonal Voronoi tiles increased at greater eccentricities.
Conclusions: The use of multiple and complementary metric
descriptors allows for a more detailed description of packing
distribution and preferred arrangement of cone photoreceptors across
the parafoveal retina.
Commercial Relationships: Marco Lombardo, None; Sebastiano
Serrao, None; Pietro Ducoli, None; Giuseppe Lombardo, None
Program Number: 5551 Poster Board Number: B0061
Presentation Time: 8:30 AM - 10:15 AM
Improved Sensitivity of Automated Cone Identification in Images
of Adaptive Optics Scanning Laser Ophthalmoscope (AOSLO)
Keiko Yonezawa1, Hiraku Sonobe1, Akihito Uji2, Sotaro Ooto2,
Masanori Hangai2, Nagahisa Yoshimura2. 1Medical Imaging Project,
Canon Inc.,, Tokyo, Japan; 2Ophthalmology, Kyoto University
Graduate School of Medicine, Kyoto, Japan.
Purpose: To provide an automated, highly sensitive cone detection
algorithm even in the region where some cones are undetectable by
the conventional local maximum detection algorithm previously
proposed by Li and Roorda.
Methods: In retinal images taken by our AOSLO, some cones were
not detected by the conventional algorithm because those cones did
not have local max intensity profile by the effect of high intensity
neighboring cones. The undetected cones were precisely picked up
with our newly developed technique which combined a filter to
analyze local convex profile with the conventional local max filter.
Retinal images of healthy subjects were acquired with our AOSLO,
all with resolution of 400 x 400 pixels and 340μm x 340μm in size.
Total six images at eccentricities of 0.5mm (3 images) and 1.0mm (3
images) were selected for analysis. Cones in the images were first
detected by the conventional algorithm, and undetected cones were
manually labeled by two engineers. A pair of cones labeled manually
by the different engineer was considered the same when they were
located within 1.2μm for 0.5mm and 1.7μm for 1.0mm of each other.
Comparisons were made between the result of detection using our
algorithm and manually labeled result combined with conventional
algorithm.
Results: Total cone counts manually labeled by at least one engineer
were 3946±172 for 0.5mm and 2441±268 for 1.0mm. Agreement
between two manual labeling was 96.0±1.8% for 0.5mm and
97.4±0.2% for 1.0mm. Among the manually labeled cones by at least
one engineer, 97.5±0.9% for 0.5mm and 99.4±0.1% for 1.0mm of
cones were detected by our method, whereas 90.9±3.0% for 0.5mm
and 95.0±0.2% for 1.0mm of cones were detected by the
conventional method. This means 261±87 for 0.5mm and 107±9 for
1.0mm additional cones were labeled correctly with our algorithm.
Ratio of hexagon was also improved for all six images, in average
51.6±2.3 % to 54.4±2.2% for 0.5mm and 51.8±2.7 % to 53.4±2.4%
for 1.0mm.
Conclusions: Newly developed cone detection algorithm detected
more cones correctly when some cones did not have local maximum
intensity profile. As these effects were stronger in the region where
the cone density was higher, improved capability of detecting cones
of our algorithm was more evident at eccentricities of 0.5mm than
1.0mm.
Commercial Relationships: Keiko Yonezawa, Canon Inc., (E);
Hiraku Sonobe, Canon Inc (E); Akihito Uji, None; Sotaro Ooto,
None; Masanori Hangai, Topcon (F), Canon (F), Nidek (C), Topcon
(C); Nagahisa Yoshimura, Canon (C), Canon (F), Nidek (C),
Topcon (F), PCT/JP2011/073160 (P)
Support: the Innovative Techno-Hub for Integrated Medical Bioimaging Project of the Special Coordination Funds for Promoting
Science and Technology
Program Number: 5552 Poster Board Number: B0062
Presentation Time: 8:30 AM - 10:15 AM
Photoreceptors, Retinal Nerve Fibers and Retinal Blood Flow
Observation by AOSLO Applied to Wide Diopter Range
Takashi Yuasa1, Futoshi Hirose1, Kenichi Saito1, Kazuhiro
Matsumoto1, Hiraku Sonobe1, Akihito Uji2, Sotaro Ooto2, Masanori
Hangai2, Nagahisa Yoshimura2. 1Medical Imaging Project, Canon
Inc., Ohta-ku, Japan; 2Ophthalmology, Kyoto University Graduate
School of Medicine, Kyoto City, Japan.
Purpose: To construct a high contrast image of photoreceptors,
retinal nerve fibers (RNF), and capillaries by using adaptive optics
scanning laser ophthalmoscope (AOSLO) which is applied to wide
diopter range.
Methods: We have newly developed an AOSLO prototype equipped
with two liquid-crystal-on-silicon spacial light modulators and
optimized its optical system to cover a wide diopter range. The
prototype covered spherical diopter range from -10D to +5D and
cylindrical diopter range from -5D to 0D. Using the AOSLO
prototype, we took images of healthy eyes and diseased eyes.
Changing the position of in-line fixation target, we selected an
imaging position in a 6 x 6mm square area on the retina. We also
changed a focus position in the retina from retinal pigment epithelium
(RPE) layer to RNF layer.
Results: We took AOSLO images of 16 patients (27 eyes), whose
spherical diopter ranged from -10.75D to +2.25D and whose
cylindrical diopter ranged from -3.75D to 0D. We also took AOSLO
images of two healthy eyes (spherical -3.50D, -4.25D; cylindrical 4.75D, -4.00D respectively) and selected imaging positions at
eccentricities of 0.5, 1.0, 1.5, 2.0, 2.5, 3.0mm respectively, and
acquired reliable images of good quality sufficient for analysis. When
we selected a position nasal 2.0mm from the fovea, we changed focus
positions and we observed photoreceptors, blood flow in capillaries,
and retinal nerve fibers.
Conclusions: We observed high contrast images of photoreceptors,
RNF, and capillaries by using our AOSLO prototype. The instrument
is useful to research on retinal diseases due to its capability of
imaging the retina over a wide diopter range.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Commercial Relationships: Takashi Yuasa, Canon Inc. (E);
Futoshi Hirose, Canon Inc. (E); Kenichi Saito, Canon Inc. (E);
Kazuhiro Matsumoto, CANON INC. (E); Hiraku Sonobe, Canon
Inc (E); Akihito Uji, None; Sotaro Ooto, None; Masanori Hangai,
Topcon (F), Canon (F), Nidek (C), Topcon (C); Nagahisa
Yoshimura, Canon (C), Canon (F), Nidek (C), Topcon (F),
PCT/JP2011/073160 (P)
Support: the Innovative Techno-Hub for Integrated Medical Bioimaging Project of the Special Coordination Funds for Promoting
Science and Technology
Program Number: 5553 Poster Board Number: B0063
Presentation Time: 8:30 AM - 10:15 AM
Compact multimodal adaptive optics imager (MAOI)
R. D. Ferguson, Mircea Mujat, Ankit Patel, Nicusor Iftimia.
Biomedical Imaging Group, Physical Sciences Inc, Andover, MA.
Purpose: To demonstrate the imaging capabilities of a new multimodal version of the compact Adaptive Optics Line Scanning
Ophthalmoscope (AOLSO). High-resolution AO imaging of the
retina, capable of resolving photoreceptors and other cells and
structures in the eye, is an important new window on ocular health
and disease. A new design of the compact multi-modal AOLSO lineconfocal imager combines advantages of AOSLO with those of the
AO fundus cameras for routine mapping of photoreceptor density..
Methods: The new multimodal adaptive optics imager (MAOI)
incorporates a number of improvements in the optical design and the
AO/focus control algorithms. The AOLSO uses <500μw of SLD
illumination centered at 780nm (50nm FWHM) wih a cylindrical lens
to generate line illumination, and AO-SDOCTuses SLD ~700 μW at
850nm (110nm FWHM). The system is currently configured for
high-stroke DMs, a custom Shack-Hartman wavefront sensor, and an
SDOCT spectrometer (Basler Sprint camera). MAOI has a compact
footprint suitable for clinical application. The optical head measures
~30×45×20cm and is mounted to a standard slit lamp stand with
chin/forehead rests. A field of up to ~3.5x5deg (1000x1500 pixels) is
user-configurable with automated overlapping scan patterns in a
30deg field of regard for rapid montage. An integrated color LCD
fixation display is included. LSO-based design allows video-rate (15
to 70 fps) high resolution retinal imaging with improved retinal
navigation. Four normal adult volunteers ranging in age from 30 to
56 years, were imaged with a standard protocol (New England IRBapproved), and AOSLO image resolution was compared to that of
prior designs.
Results: New multimodal system design and AO control
significantly enhanced the capabilities and resolution of the AOLSO
portion of the MAOI imager. Based on images acquired in resolution
targets, optical resolution in the MAOI was measured to be ~1.8μm
(referenced to the retina); currently somewhat more in the eye
(~2.5μm), due to sampling at ~1μm/pixel to preserve light collection-a more than 50% improvement over the previous system. A small
region within a single, unprocessed image is shown below (512x
716μm with fovea ~100μm off the lower right corner of the image).
Conclusions: The new compact MAOI resolves cones very near the
fovea and can be used for automated AO montaging and
photoreceptor density mapping in the macula.
Portion of a MAOI image (AOLSO) of photoreceptors near the
fovea.
Commercial Relationships: R. D. Ferguson, Physical Sciences Inc
(E), Physical Sciences Inc (P); Mircea Mujat, Physical Sciences,
Inc. (E), Physical Sciences, Inc. (P); Ankit Patel, Physical Sciences
Inc. (E); Nicusor Iftimia, None
Support: NIH 5R44EY018509-03
Program Number: 5554 Poster Board Number: B0064
Presentation Time: 8:30 AM - 10:15 AM
Use of variable Field Size in AOSLO retinal imaging to improve
post-processing
Ting Luo, Gang Huang, Toco Y. Chui, Stephen A. Burns. School of
Optometry, Indiana University Blooomington, Bloomington, IN.
Purpose: To test the use of variable scan sizes to generate variable
field sizes giving low resolution images over a wider region of retina,
which then provide references for image alignment even in the
presence of modest sized saccades.
Methods: Three normal subjects participated in this experiment. The
Indiana AOSLO was used to generate both larger size (3.4 deg x3.3
deg) and standard size (typically either 1.9 deg x 1.8 deg or 1.3 deg
x1.2 deg) fields. These smaller field sizes, which provide pixel sizes
of approximately 1 micron per pixel or 0.66 microns per pixel, are
desirable for capturing small features but in patients with poor
fixation can be difficult to align and average due to eye movements.
The steering capability of the AOSLO was used to make a rapid set
of measurements on the eyes that covered 10x10 degrees. Subjects
were also imaged using the normal fields sizes within the same
session. In post-processing a montage of the large field size image
was first generated and resized to the same number of pixels per
degree as the small field images. Next each frame of the small field
video sequences was cross-correlated with the large field montage
and the location within the larger field identified. The location of the
peak of the cross-correlation was used to determine the best template
location within the larger field for each frame.
Results: The larger field data acquisition required about 3 minutes
additional time within a session. As expected the peak locations for
the cross correlation were stable when fixation was stable. However,
during eye movements between frames which cause problems for our
standard alignment approach, the new approach was able to find a
corresponding retinal location. Overall, the normalized crosscorrelation was lower, presumable due to a drop in image quality for
the large field template, due to both decreased AO control over the
wider field size, but also due to under sampling of the images.
Conclusions: The Multi-resolution approach holds promise for
increasing the yield of usable frames in subject with relatively poor
fixation. It adds only a slight amount to the total imaging time
required per patient. The major limitations are that improvements
may not extend to subjects with very bad fixation because in those
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
cases acceptable frames of even the large field size may be difficult
to obtain.
Commercial Relationships: Ting Luo, None; Gang Huang, None;
Toco Y. Chui, None; Stephen A. Burns, None
536 Inner Retina and Blood Vessels
Thursday, May 09, 2013 10:30 AM-12:15 PM
Exhibit Hall Poster Session
Program #/Board # Range: 6054-6066/B0065-B0077
Organizing Section: Visual Psychophysics / Physiological Optics
Program Number: 6054 Poster Board Number: B0065
Presentation Time: 10:30 AM - 12:15 PM
Future Insights on an Ocular Hypertension Model in the White
Leghorn Chicken
Jennifer L. Choi1, Radouil T. Tzekov2, 3, Stacey S. Choi1. 1New
England College of Optometry, Boston, MA; 2The Roskamp
Institute, Sarasota, FL; 3Department of Ophthalmology, University of
South Florida, Tampa, FL.
Purpose: While White Leghorn chicken (Gallus gallus domesticus)
have been used to study physiological optical properties of the eye
and conditions such as myopia, there is a lack of in vivo studies that
look at the potential of chicken as a model of ocular hypertension or
glaucoma. When advanced imaging techniques are to be used in such
models, chicken have an advantage over rodents, having bigger eyes
with less optical aberrations. The induction of elevated IOP in
chicken via anterior chamber injections of microbeads has thus been
investigated.
Methods: Animals of both genders and varying ages (n=15:12-124
days old) were subject to one of 12 combinations of anterior chamber
injections of microbeads: magnetic (4.5 µm) or non-magnetic (12
µm) in one or both eyes with saline as a control. Intraocular pressure
(IOP) was monitored frequently before and after injections with
Tonopen. In 4 out of the 17 animals A-scan ultrasound was used to
measure ocular parameters including anterior chamber depth (ACD),
lens thickness (LT), vitreous chamber depth (VCD), retinal thickness
(RT) and choroidal thickness (ChT) pre and post all injections. All
birds had isofluorane anesthesia prior to injections and ultrasound.
Results: Elevation of IOP with maintenance of a clear visual axis
was successful in 2 out of 17 animals after two 70µL injections of
magnetic microbeads (concentration 20x108beads/mL). Animal
#1943 was injected with 140x106 beads at age 51 days and with the
same amount two weeks later; 5 days later IOP was elevated 5 mm
Hg greater than the fellow eye for a period of 7 days. Animal #1975
received an injection of 140x106 beads at age 99 days and 160x106
beads at age of 110 days and an average elevation of 8mm Hg greater
than the fellow eye was noted from day 4 to day 7 post second
injection. In other animals injection of 98x106 magnetic beads at day
40 and again at day 51 blocked the visual axis. Non-magnetic
microbeads (125x108 to 875x108 beads) did not elevate the IOP. One
to 3 saline injections did not influence the growth rate of ocular
parameters measured via ultrasound biometry.
Conclusions: The White Leghorn chicken has potential for in vivo
studies of ocular hypertension and/or glaucoma via magnetic
microbead anterior chamber injections. Studying the effects of
elevated IOP on the chicken retina over a longer time period is
indicated. SD-OCT and Adaptive Optics imaging may shed further
insights.
Commercial Relationships: Jennifer L. Choi, None; Radouil T.
Tzekov, None; Stacey S. Choi, None
Support: NIH Grant EY007149
Program Number: 6055 Poster Board Number: B0066
Presentation Time: 10:30 AM - 12:15 PM
Detection of flow velocity fluctuations associated with erythrocyte
aggregation in diabetic retinopathy by using adaptive optics
scanning laser ophthalmoscopy
Akihito Uji, Masanori Hangai, Sotaro Ooto, Shigeta Arichika,
Tomoaki Murakami, Nagahisa Yoshimura. Ophthalmology, Kyoto
Univ Graduate Sch of Med, Kyoto City, Japan.
Purpose: Adaptive Optics Scanning Laser Ophthalmoscopy (AOSLO) has enabled noninvasive and direct monitoring of erythrocyte
aggregates in the retinal capillaries. In this study, we quantified the
blood flow velocity in the parafoveal capillaries of patients with
diabetic retinopathy (DR) by using the AO-SLO system prototype
developed by Canon Inc.
Methods: Ten patients (mean age ± standard deviation [SD], 45.8 ±
16.7 years) diagnosed with DR at Kyoto University Hospital (8
patients with mild nonproliferative DR [NPDR], 2 patients with
moderate NPDR) and 8 control subjects without any history of ocular
or systemic diseases (mean age, 34.6 ± 8.6 years) were recruited for
this study. AO-SLO videos were acquired from the temporal and
nasal areas located 0.5° from the foveal center. The scan area of the
retina was 1.4 × 2.8°, and scans were recorded for 4 seconds per area
at a frame rate of 64 Hz. Erythrocyte aggregates were detected as
“dark tails” that were darker than the vessel shadows, and the
velocities of all the dark tails observed in both temporal and nasal
areas were measured. In subjects whose pulse was measured
simultaneously during the AO-SLO video recording, a relative
cardiac cycle was assigned to each dark tail velocity in order to
investigate the effect of cardiac pulsation on the velocities.
Results: Vessels showing rapid changes in dark tail flow velocity
were noted in 6 DR patients, but these vessels were not detected in
normal subjects. In these vessels, dark tail flow velocity was
extremely low and deformation of the trajectory of the dark tail flow
was depicted in the spatiotemporal image. Two such vessels were
found in 3 patients and 1 vessel was found in each of the remaining 3
patients. The average velocity change in these vessels was 0.95 ±
0.53 mm/s. Pulse was measured in 6 DR patients and 8 normal
subjects, and 220 dark tails were analyzed in total. The velocity of the
dark tail in DR patients (1.45 ± 0.52 mm/s) was significantly higher
than that in normal subjects (1.33 ± 0.40 mm/s) (P < 0.05).
Conclusions: The velocity of the dark tail in NPDR patients was
higher than that in normal subjects. However, at the same time, there
were some vessels with extremely slow dark tail flow.
Spatiotemporal images were useful in detecting rapid changes in dark
tail flow.
Commercial Relationships: Akihito Uji, None; Masanori Hangai,
Topcon (F), Canon (F), Nidek (C), Topcon (C); Sotaro Ooto, None;
Shigeta Arichika, None; Tomoaki Murakami, None; Nagahisa
Yoshimura, Canon (C), Canon (F), Nidek (C), Topcon (F),
PCT/JP2011/073160 (P)
Support: Innovative Techno-Hub for Integrated Medical Bioimaging
Program Number: 6056 Poster Board Number: B0067
Presentation Time: 10:30 AM - 12:15 PM
Adaptive contrast enhancement in capillary shadow region of
AOSLO images using blood cell flow information
Hiroshi Imamura1, Takashi Yuasa1, Hiraku Sonobe1, Akihito Uji2,
Sotaro Ooto2, Masanori Hangai2, Nagahisa Yoshimura2. 1Canon Inc,
Ohta-ku, Japan; 2Ophthalmology, Kyoto University Graduate School
of Medicine, Kyoto City, Japan.
Purpose: To improve visibility of photoreceptors in capillary shadow
region of AOSLO images using characteristics of temporal intensity
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
variation caused by blood cell flow.
Methods: Our capillary shadow correction method consists of
detecting abnormal frames in an AOSLO video, calculating statistical
values of temporal intensity variation in each pixel except the
abnormal frames, and allocating the pixel value based on the
statistical values in each pixel position for producing the resultant
contrast enhanced AOSLO image. In this study, we recorded AOSLO
videos using Canon prototype AOSLO system with a high wavefront
correction efficiency using dual liquid crystal phase modulators. The
imaging light wavelength was 840 nm and the frame rate was 32 Hz.
The scan area at the parafovea was 1.1 × 1.1° and was sampled at 400
× 400 pixels. The videos were recorded for 2-5 seconds. The
proposed adaptive contrast enhancement method was applied to 15
AOSLO videos for 5 healthy subjects including parafoveal capillary
regions (leukocyte preferred paths (LPPs) and plasma-gap capillaries
(PGCs)) and macular arteriolovenous region. We calculated the
spectral power ratio as a function of frequency between the adaptive
contrast enhanced images and conventional frame averaged images
particularly in LPPs, PGCs and macular arteriolovenous regions.
Results: The spectral power ratio at a given frequency in LPPs and
PGCs of the adaptive contrast enhanced AOSLO images were 1.62
and 1.09 on average respectively, because capillary shadows were
corrected by using intensity values when leukocyte or plasma-gap
passes. On the other hand, shadows in macular arteriolovenous
regions were not corrected because pixel intensity was low in all
frames of AOSLO video as the result of erythrocytes next to a
leukocyte blocking the imaging light.
Conclusions: Our method improved contrast of photoreceptors in
retinal capillary shadow region of AOSLO images using blood cell
flow information.
Commercial Relationships: Hiroshi Imamura, Canon Inc. (E);
Takashi Yuasa, Canon Inc. (E); Hiraku Sonobe, Canon Inc (E);
Akihito Uji, None; Sotaro Ooto, None; Masanori Hangai, Topcon
(F), Canon (F), Nidek (C), Topcon (C); Nagahisa Yoshimura,
Canon (C), Canon (F), Nidek (C), Topcon (F), PCT/JP2011/073160
(P)
Support: the Innovative Techno-Hub for Integrated Medical Bioimaging Project of the Special Coordination Funds for Promoting
Science and Technology
Program Number: 6057 Poster Board Number: B0068
Presentation Time: 10:30 AM - 12:15 PM
Study of epimacular membranes using adaptative optics high
resolution imaging
Hassiba Bouakkaz1, Sarah Ayello-Scheer1, Alexandre Leseigneur1,
Celine Devisme1, Jose A. Sahel1, 2, Michel Paques1, 2. 1Centre
Hospitalier National d'Ophtalmologie des Quinze Vingts, Paris,
France; 2Institut de la Vision, Paris, France.
Purpose: High resolution imaging using adaptative optics (AO)
allows an improved viewing of retinal microstructures. Here, we
analyzed the AO features of epimacular membranes (ERMs) before
and after surgery.
Methods: Seven eyes with ERM were included. For each patient, a
complete ophthalmological examination including measurement of
visual acuity, optical coherence tomography and AO infrared flood
imaging (rtx1, ImagineEye, Orsay, France) was performed. In four
patients these exams were repeated after surgical ablation of the
membrane.
Results: A very precise viewing of the ERMs and of the underlying
retinal wrinkling was obtained. The ERM surface showed a myriad of
highly reflective dots, whose reflectance varied with the light
incidence. Around ERMs, radial retinal folds were seen. The peculiar
aspect of ERMs at their very beginning, which seemed to develop
around vessels, could be identified. By changing focus, it was
possible in three cases to distinguish the ERM itself from the
underlying retinal wrinkling. After surgery, retinal unfolding could be
documented.
Conclusions: Specific interests of AO imaging in ERM patients
comprise the ability to identify the earliest stages of ERMs, which
seem to develop primarily around vessels, and the characterization of
the optical properties of the ERM surface. The strong dependence of
reflectance to the angle of the incident light suggested that ERMs
have a bumpy mosaic-like surface.
Commercial Relationships: Hassiba Bouakkaz, None; Sarah
Ayello-Scheer, None; Alexandre Leseigneur, None; Celine
Devisme, None; Jose A. Sahel, UPMC/Essilor (P), Second Sight (F);
Michel Paques, MerckSerono (C), Roche (C), Sanofi (C)
Support: ANR_09_TECS_009_01_IPHOT
Program Number: 6058 Poster Board Number: B0069
Presentation Time: 10:30 AM - 12:15 PM
Parietal morphometry of retinal arterioles in health and
hypertension using adaptive optics
Edouard Koch1, 2, David Rosenbaumm3, Xavier Girerd3, Florence
Rossant4, Michel Paques1. 1Clinial Investigation Center, QuinzeVingts Hospital-INSERM, Paris, France; 2Ophthalmology, Versailles
Hospital, Versailles, France; 3Cardiology, Pitié Salpétrière Hospital,
Paris, France; 4Institut Supérieur d'Electronique de Paris, ISEP, Paris,
France.
Purpose: Morphological changes affecting the wall of small retinal
arteries are recognized surrogates of end-organ damage secondary to
aging and/or arterial hypertension. However, direct observation of the
microvascular wall is not feasible with routine imaging techniques.
We report here the quantitative analysis of the structure of retinal
arterioles (~ 50-150 µm diameter) using adaptive optics (AO) near
infrared (NIR) imaging (rtx1 camera; ImagineEyes, France) in normo
and hypertensive humans.
Methods: From OA images, the wall-to-lumen ratio (WLR) was
calculated using a dedicated software. We compared the WLR
between a control group (n = 20; 30.2 ± 6 years) and a group of
hypertensive subjects (n = 30, 48.1 ± 13 years). Focal lesions
(arteriolar narrowing and arteriovenous nickings) were also analyzed.
These data were compared to the carotid intima-media thickness
(IMT).
Results: The WLR was significantly higher in the hypertensive
group than in controls (0.35 ± 0.071 vs 0.26 ± 0.035, respectively;
p=0.017) after correcting for age. The WLR of retinal arterioles was
also positively correlated to current arterial pressure (r=0.36; p=0.03)
and to IMT (p=0.028). Arteriolar narrowing, but not arteriovenous
nickings, showed locally increased WLR. Follow-up of patients
under hypotensive treatment (n=7; mean follow-up 6 months) could
document progressive vasodilation in two.
Conclusions: Past history of arterial hypertension and current arterial
pressure are both associated with increased WLR. Arteriovenous
narrowing and arteriovenous nicking show distinct parietal
abnormalities and hence are probably due to distinct pathological
processes. Thickening of large and small arteries are correlated,
suggesting some degree of parallelism of the evolution of macro and
microcirculatory damage. We conclude that AO imaging enables to
phenotype the microcirculation with an unprecedented precision and
may improve the understanding and the management of arterial
hypertension.
Commercial Relationships: Edouard Koch, None; David
Rosenbaumm, None; Xavier Girerd, None; Florence Rossant,
None; Michel Paques, MerckSerono (C), Roche (C), Sanofi (C)
Support: ANR_09_TECS_009_01_iPhot
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Clinical Trial: C10-03
Program Number: 6059 Poster Board Number: B0070
Presentation Time: 10:30 AM - 12:15 PM
Investigation of the correlation among diameter of retinal vessel
and arteriosclerosis risk factors including hypoadiponectinemia
Kei Homma1, Ryo Kawasaki2, Yusuke Tanabe1, Koko Saito1, Akira
Sugano1, Atsushi Hozawa3, Katou Takeo4, Isao Kubota5, Takamasa
Kayama6, Hidetoshi Yamashita1. 1Ophthalmology, Yamagata Univ
Sch of Medicine, Yamagata, Japan; 2Public Health, Yamagata Univ
Sch of Medicine, Yamagata, Japan; 3Tohoku Univ Sch of Medicine,
Sendai, Japan; 4Neurology,Hematology,Metabolism,Endocrinology
and Diabetology, Yamagata Univ Sch of Medicine, Yamagata, Japan;
5
Cardiology,Pulmonology,and Nephrology, Yamagata Univ Sch of
Medicine, Sendai, Japan; 6Neurosurgery, Yamagata Univ Sch of
Medicine, Yamagata, Japan.
Purpose: Hypoadiponectinemia caused by visceral fat accumulation
is related to hypertension, diabetes, and hyperlipidemia, and is an
independent risk factor for the arteriosclerosis.
In this research, the correlation among diameter of retinal vessel and
arteriosclerosis risk factors including hypoadiponectinemia was
investigated in the population based epidemiological study.
Methods: This research was approved by the Ethics committee of
Yamgatata University School of Medicine. Fundus photographs were
taken in the subjects who participated in the Takahata study and
analyzed after securing written permission from the subjects. In
total,1473 subjects were investigated.
The estimated retinal artery(CRAE:centaral retinal artery equivalent,
the estimated retinal vein(CRVE:central retinal vein equivalent),and
AVR (arteliole to venule ratio) were measured from the fundus
photographs used by the vessel diameter measurement dedicated
software (Retinal Analysis,University of Wisconsin,
Wisconsin).Characteristics to be inspected were divided into about 4
groups, and the vessel diameter of an each part was analyzed.
Results: Multiple linear regression analysis showed that CRAE
decreased along with systolic arterial pressure increased(0.067μm;p=0.039).CRAE increased along with adiponectin level
increased(0.153μm;p=0.049).CRVE increase was also associated
with HbA1c,smoking index,and body mass
index(3.333μm;p=0.004,0.004μm;p=0.023,0.412μm;p=0.007
respectively).
Conclusions: Hypoadiponectinemia was an independent risk factor
for CRAE decrease.The results suggest that measurement of retinal
blood vessels are a good clinical marker to detect macrovascular
diseases.
Commercial Relationships: Kei Homma, None; Ryo Kawasaki,
None; Yusuke Tanabe, None; Koko Saito, None; Akira Sugano,
None; Atsushi Hozawa, None; Katou Takeo, None; Isao Kubota,
None; Takamasa Kayama, None; Hidetoshi Yamashita, Senju (C),
Senju (P)
Program Number: 6060 Poster Board Number: B0071
Presentation Time: 10:30 AM - 12:15 PM
Noninvasive Imaging of Retinal Pericytes and Endothelial Cells
in Living Human Eyes
Toco Y. Chui, Thomas Gast, Stephen A. Burns. Optometry, Indiana
University, Bloomington, IN.
Purpose: To image the retinal vascular pericytes and endothelial
cells in living human retina using an adaptive optics scanning laser
ophthalmoscope (AOSLO).
Methods: In vivo arteriolar wall imaging was performed on 8 healthy
subjects using the Indiana AOSLO (Ferguson et al, 2010). Vessel
wall imaging was performed using systematic control of the position
of a large confocal aperture (Chui et al, 2012). Peripapillary arteries
and arterioles were divided into 4 groups based on their lumen
diameters (Gr 1: ≥100µm; Gr 2: 50-99µm; Gr 3: 10-49µm; Gr 4:
retinal capillaries).
Results: The retinal microvasculature and scattering behavior of
erythrocytes were clearly visualized in all 8 subjects. On the smaller
vessels the pericytes were visualized as distinct cells laying along the
lumen of the blood vessel. The smaller vessel pericytes bulged
outward from the vessel wall resulting in a wall of irregular
thickness. For the larger Gr 1 vessels the pericytes were much flatter
and formed the outer corrugated layer of a two (or more) layered
vascular wall. While pericytes were readily seen in vessel groups 1,
2, and 3, endothelial cells were only visible in Gr 1 vessels - the
largest retinal arteries. Fig 1A shows the fine structure of arteriolar
wall in a Gr 1 and Gr 3 vessel. The ratio of pericytes to endothelial
cells was approximately 1:1 in the Gr 1 arteries (Fig 1B). Vascular
wall components were not identified in the smallest retinal capillaries
(Gr 4).
Conclusions: Our results show that retinal pericytes can be readily
resolved in normal subjects for arterioles with a lumen diameter
>10µm. Our noninvasive imaging approach allows direct assessment
of the cellular structure of the vascular wall in vivo with potential
applications in retinal vasculopathies such as diabetic retinopathy.
Fig1 A) Fine structure of vessel wall in peripapillary arterioles.
Asterisks indicate the vessel lumen of a 100µm diameter and 14µm
diameter arteriole. The inner and outer vessel wall linings of the
larger arteriole are indicated by the white arrows. Pericytes (black
arrows) are observed in a precapillary arteriole with a lumen diameter
of 14µm. B) Magnified region of the white box on A. Endothelial
cells (white arrows) and pericytes (black arrows) are readily seen
along the inner and outer vessel wall linings. Note the one to one
ratio of endothelial cells and pericytes.
Commercial Relationships: Toco Y. Chui, None; Thomas Gast,
None; Stephen A. Burns, None
Support: NIH grants R01-EY14375, R01-EY04395, and
P30EY019008
Program Number: 6061 Poster Board Number: B0072
Presentation Time: 10:30 AM - 12:15 PM
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Adaptive Optics Measurements of Retinal Arterial Wall
Thickness in both Normotensive and Hypertensive Subjects
Jake Hillard1, Toco Y. Chui1, Dan A. Sapir2, Thomas Gast1, Stephen
A. Burns1. 1School of Optometry, Indiana University, Bloomington,
IN; 2Medical School, Indiana University, Bloomington, IN.
Purpose: To make precise measurements of vascular wall thickness
in the retinas of both systemically normotensive and hypertensive
individuals using an adaptive optics scanning laser ophthalmoscope
(AOSLO).
Methods: We used the Indiana AOSLO, operated with a relatively
large (10x the Airy disc) confocal aperture, displaced by more than
the Airy disc radius. This imaging approach provides excellent
imaging of the retinal vasculature, and gives a better visualization of
the walls (Chui et al 2012). Images of retinal blood vessels ranging
from capillaries to the largest retinal vessels were obtained in a group
of 6 normal subjects and 16 subjects with a history of hypertension.
Vessels ranging in size from an inner diameter of 9 to 171 microns
were measured. Measurements were made using an image editing
program and were repeated on each vessel 5 times. The lumens of the
vessels were differentiated from the vessel walls by the motion of
erythrocytes, within the lumens, readily seen on aligned video
sequences.
Results: Arterial walls and lumens were able to be measured in all
subjects and in almost all of the vessels chosen for analysis. Venous
walls were occasionally measurable in hypertensive but not in normal
subjects. Some arteries could not be measured due to shadowing or
focusing in a different plane although all tested individuals had at
least some measurable arteries. For both small arteries and arterioles
(lumen diameters < 50 microns) and larger ones, the hypertensive
subjects had higher wall to lumen ratios (p< 0.02 , p<0.03 )
respectively. The highest ratios occurred for the smallest vessels in
the hypertensive subjects (Figure 2).
Conclusions: We have been able to measure arterial wall thickness in
vessels with lumen diameters as small as 9 microns using an AOSLO.
The imaging technique used allows clear visualization of the vessel
walls which can be used to precisely measure arterial wall thickness
non-invasively in subjects with a history of hypertension.
Commercial Relationships: Jake Hillard, None; Toco Y. Chui,
None; Dan A. Sapir, None; Thomas Gast, None; Stephen A.
Burns, None
Support: This work was supported by NIH grants R01-EY14375,
R01-EY04395, and P30EY019008 to S.A.B.
Program Number: 6062 Poster Board Number: B0073
Presentation Time: 10:30 AM - 12:15 PM
Distribution of vessels with dark tails in the parafoveal capillary
network monitored by adaptive optics scanning laser
ophthalmoscopy
Shigeta Arichika, Akihito Uji, Masanori Hangai, Sotaro Ooto,
Nagahisa Yoshimura. Kyoto University, Kyoto, Japan.
Purpose: Adaptive optics scanning laser ophthalmoscopy (AOSLO)
provides a unique opportunity for objective and noninvasive study of
vessels with dark tails, which correspond to erythrocyte aggregation.
In this study, we investigated the distribution of vessels with dark
tails in the parafoveal capillary network using our prototype AOSLO
system developed by Canon Inc.
Methods: The imaging light wavelength of AOSLO was 840 nm,
and the frame rate was 32 or 64 Hz. The scan area at the retina was
either 1.4 × 1.4° or 1.4 × 2.8°, and this was sampled at 200 × 200
pixels or 200 × 400 pixels, respectively. The AOSLO videos were
recorded for 2-4 seconds per scan area, and 10-25 scan areas were
obtained for each of 3 healthy subjects (aged 23-38 years) who had
no ocular or systemic diseases to ensure total coverage of the
parafoveal area. After the capillary images were constructed as
projections of the sequential division images, those covering an area
ranging from 0 to 0.15 mm peripheral to the edge of the foveal
avascular zone (FAZ) and in which most of the capillary network
appeared as a single layer were cropped and used for analyses.
Vessels with and without dark tails were identified and their entire
lengths were measured independently. Moreover, the boundary of the
FAZ was divided into 2 categories based on the presence or absence
of vessels with dark tails.
Results: In all 3 subjects, the vessels could be divided into 2
categories based on the presence or absence of dark tails. No timedependent change was observed in distribution of vessels with dark
tails. The total length of vessels with and without a dark tail was 3.01
mm and 5.44 mm, respectively. The lengths of vessels with and
without a dark tail at the boundary of the FAZ were 0.70 mm and
1.42 mm, respectively. The average ratio of the length of a vessel
with a dark tail relative to the length of a vessel without a dark tail
was 0.55 in the parafoveal area and 0.54 on the boundary of the FAZ.
Conclusions: AOSLO imaging revealed the existence of 2 pathways
of dark tail flow in the parafoveal capillary network. Vessels with
dark tails tended to be shorter than those without dark tails.
Commercial Relationships: Shigeta Arichika, None; Akihito Uji,
None; Masanori Hangai, Topcon (F), Canon (F), Nidek (C), Topcon
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
(C); Sotaro Ooto, None; Nagahisa Yoshimura, Canon (C), Canon
(F), Nidek (C), Topcon (F), PCT/JP2011/073160 (P)
Program Number: 6063 Poster Board Number: B0074
Presentation Time: 10:30 AM - 12:15 PM
In vivo imaging of Hypertensive Retinopathy using Fluorescence
Adaptive Optics Scanning Light Ophthalmoscopy
Michael Dubow1, 2, Alexander Pinhas1, 2, Nishit Shah1, Yusufu N.
Sulai3, Patricia Garcia1, Nicole K. Scripsema4, Joseph Carroll5,
Alfredo Dubra5, Richard B. Rosen1. 1New York Eye and Ear
Infirmary, New York City, NY; 2Mount Sinai School of Medicine,
Mount Sinai Hospital, New York City, NY; 3University of Rochester,
Rochester, NY; 4New York Medical College, Valhalla, NY; 5Medical
College of Wisconsin, Milwaukee, WI.
Purpose: While hypertension affects 1 in 3 adults and 2 in 3 adults
over age 60, hypertensive retinopathy is often overlooked as an
important indicator of systemic disease. Previous studies have
explored the relationship between hypertensive retinopathy and
diabetes, nephropathy, heart disease and cerebrovascular events.
Reflectance adaptive optics scanning light ophthalmoscopy
(RAOSLO) is a powerful tool in our exploration of the retina,
providing access to retinal microstructure previously unavailable in
vivo. However, the technology has not yet been optimized to study
the microvasculature. Our group has combined AOSLO with
fluorescein angiography (FAOSLO) to image patients with
hypertensive retinopathy.
Methods: 12 adult patients with vascular disease were recruited.
Baseline RAOSLO images were collected using a 790 nm light
source and 1° FOV. Patients then ingested 1g of fluorescein sodium
mixed with juice. Starting at 15 minutes post ingestion, reflectance
and fluorescence (488nm excitation emission; emission filter
centered at 525nm; 45nm bandwidth) 1° FOV image sequences were
recorded simultaneously. Conventional fundus photography with and
without intravenous fluorescein was performed.
Results: FAOSLO revealed fine changes in the retinal
microvasculature not seen with traditional imaging modalities and
RAOSLO in all patients. We successfully imaged features of
hypertensive retinopathy present in larger vessels on the microscopic
scale, including microaneurysms, hemorrhages, intravascular lesions,
focal arteriolar narrowing, and vessel tortuosity.
Conclusions: FAOSLO represents a promising new technology to
image features of hypertensive retinopathy with resolution previously
attainable only through biopsy. New quantitative classification
schemas will need to be developed to describe and categorize these
abnormalities. Following patients over time will capture the evolution
of the disease, giving invaluable insight into the onset and
progression of hypertensive changes, both in the eye and throughout
the body.
Figure 1: A tortuous tertiary artery imaged on both fundus photo (A)
and IV fluorescein (B). While the artery was visible on RAOSLO
(C), FAOSLO revealed a focal filling defect (D, E), suggesting local
constriction or intravascular lesion.
Figure 2: Variable vessel tortuosity was seen in all levels in
hypertensive retinopathy.
Commercial Relationships: Michael Dubow, None; Alexander
Pinhas, None; Nishit Shah, None; Yusufu N. Sulai, None; Patricia
Garcia, None; Nicole K. Scripsema, None; Joseph Carroll,
Imagine Eyes, Inc. (S); Alfredo Dubra, US Patent No: 8,226,236
(P); Richard B. Rosen, Opko-OTI (C), Optos (C), Clarity (C), ODOS (C), Topcon (R), Zeavision (F), Genetech (F), Optovue (C)
Support: Marrus Family Foundation, Bendheim-Lowenstein Family
Foundation, Wise Family Foundation, Chairman's Research Fund of
the NYEEI, Research to Prevent Blindness, Burroughs Wellcome
Fund, Glaucoma Research Foundation
Program Number: 6064 Poster Board Number: B0075
Presentation Time: 10:30 AM - 12:15 PM
Normal retinal vasculature imaged using fluorescence adaptive
optics scanning light ophthalmoscopy (FAOSLO)
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Nishit Shah1, Michael Dubow1, 2, Alexander Pinhas1, 2, Nicole K.
Scripsema1, Alfredo Dubra3, 4, Yusufu N. Sulai6, 3, Drew H. Scoles5, 3,
Richard B. Rosen1. 1Ophthalmology, New York Eye and Ear
Infirmary, New York, NY; 2Mount Sinai Hospital, Mount Sinai
School of Medicine, New York, NY; 3Ophthalmology, Medical
College of Wisconsin, Milwaukee, WI; 4Biophysics, Medical College
of Wisconsin, Milwaukee, WI; 5Biomedical Engineering, University
of Rochester, Rochester, NY; 6The Institute of Optics, University of
Rochester, Rochester, NY.
Purpose: To report high resolution images of retinal vasculature
using Fluorescein Angiography (FA) with the Adaptive Optics
Scanning Light Ophthalmoscope (AOSLO).
Methods: 5 subjects with no retinal pathology or evidence of eye
disease were identified prior to imaging. Reflectance imaging with a
790nm super luminescent diode was used to identify the vascular
structures of interest. One gram of fluorescein mixed with 4oz of
orange juice was administered orally. Single-photon fluorescence
images were then collected at the previously identified areas using a
488nm solid state laser for excitation and an emission filter centered
at 525nm with a 45nm bandwidth over a 1° field of view. Imaging
was repeated at 15 minute intervals until signal extinction. 3 subjects
were also imaged after IV fluorescein administration.
Results: Averaging 120 fluorescence images revealed the retinal
microvasculature. Measurable fluorescence signal was observed as
early as 8 minutes and as late as 2 hours after administering
fluorescein orally. Although absolute fluorescence signal varied
across patients, the best images were obtained between 15 and 45
minutes after administration. On the AOSLO, oral fluorescein
provided comparable image quality to that of IV fluorescein. Time to
signal extinction with IV fluorescein was shorter, probably due to
quicker redistribution of the dye. No side effects from either oral or
IV administration of fluorescein were observed.
Conclusions: Fluorescein angiography is an invaluable tool in the
management of ocular disease. Coupled with AOSLO, it permits a
detailed examination of the capillary bed of the inner nuclear layer
when compared to conventional IV FA. Furthermore, FAOSLO with
oral fluorescein is a safer alternative to IV angiography and provides
a longer imaging time window. High resolution imaging of the retinal
microvasculature with FAOSLO will not only help to further
understand vascular micropathology but will also guide early
intervention in management of vascular diseases.
Fig 1. Retinal vasculature as seen on: A.fundus photography B.with
IV Fluorescein C.magnified view of a vessel (top arrow in B)
D.FAOSLO image with IV fluorescein corresponding to frame C
E.magnified view of a vessel (bottom arrow in B) F.FAOSLO image
with oral fluorescein corresponding to frame E
Fig 2. Comparison of mean intensity over time on averaged
fluorescence images
Commercial Relationships: Nishit Shah, None; Michael Dubow,
None; Alexander Pinhas, None; Nicole K. Scripsema, None;
Alfredo Dubra, US Patent No: 8,226,236 (P); Yusufu N. Sulai,
None; Drew H. Scoles, None; Richard B. Rosen, Opko-OTI (C),
Optos (C), Clarity (C), OD-OS (C), Topcon (R), Zeavision (F),
Genetech (F), Optovue (C)
Support: Marrus Family Foundation, Bendheim-Lowenstein Family
Foundation, Wise Family Foundation, Chairman's Research Fund of
the NYEEI, Research to Prevent Blindness, The Burroughs
Wellcome Fund and the Glaucoma Research Foundation
Program Number: 6065 Poster Board Number: B0076
Presentation Time: 10:30 AM - 12:15 PM
Histopathologic Features of Diabetic Microangiopathy Imaged
Using an Adaptive Optics Scanning Laser Fluorescein
Angiography
Richard B. Rosen1, 2, Alfredo Dubra3, Rishard Weitz1, Joseph
Carroll3, Michael Dubow1, 4, Alexander Pinhas1, 4, Nishit Shah1,
Yusufu N. Sulai3, 5, Nicole K. Scripsema1, 2, Joseph B. Walsh1, 2.
1
Ophthalmology, New York Eye & Ear Infirmary, New York, NY;
2
Ophthalmology, New York Medical College, Valhalla, NY;
3
Ophthalmology, Medical College of Wisconsin, Milwaukee, WI;
4
Ophthalmology, Mount Sinai School of Medicine, New York, NY;
5
Ophthalmology, University of Rochester, Rochester, NY.
Purpose: To describe the fluorescein angiographic features of
diabetic microangiopathy lesions imaged with an adaptive optics
scanning light ophthalmoscope (AOSLO) compared to their
appearance on conventional fundus photography and spectral domain
optical coherence tomography (SDOCT).
Methods: AOSLO images (790nm; 1° degree field of view) without
fluorescein dye were collected in 15 adult diabetic retinopathy
patients to identify microvascular points of interest. Patients then
ingested 1gm fluorescein dye mixed in 4oz of orange juice.
Simultaneous reflectance (790 nm) and fluorescence (488 nm
excitation, 503-548 nm emission) AOSLO images (1° field of view)
were collected between 15 and 60 minutes post-ingestion. For
comparison with conventional imaging techniques, fundus imaging
with and without intravenous fluorescein were performed.
Results: In the fluorescence AOSLO channel we were able to
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
visualize microangiopathic features of diabetic microangiopathy in
vivo at the level of the retinal capillary bed. A number of lesions
were clearly delineated, including a variety of microaneurysms,
capillary loops, IRMA, and neovascularization, which could not be
seen well in the 790nm channel. These lesions typically appeared as
red dots on fundus photography or bright spots on clinical fluorescein
angiography. OCT appearances were typically less distinct.
Conclusions: Micro fluorescein angiography can by successfully and
safely achieved using AOSLO in diabetic patients revealing anatomic
features previously seen only on pathology slides. This level of
clinical imaging may prove useful for evaluating the impact of
treatment at a the microscopic scale.
Figure 1. A:Segment of wide field fundus photograph demonstrating
microaneurysms, tortuosity, and neovascularization. B:Standard wide
field fluorescein angiogram with color coded frames corresponding to
micro angiographic images in figure 2. C:Corresponding SD-OCT
slice through the red frame revealing microaneurysms
Figure 2. AOSLO FA images corresponding to frames in figure 1
revealing details of microangiopathy including vascular loops
(A,B,C) microaneurysms(A,B,C), and capillary dropout( A, B,C).
Commercial Relationships: Richard B. Rosen, Opko-OTI (C),
Optos (C), Clarity (C), OD-OS (C), Topcon (R), Zeavision (F),
Genetech (F), Optovue (C); Alfredo Dubra, US Patent No:
8,226,236 (P); Rishard Weitz, None; Joseph Carroll, Imagine Eyes,
Inc. (S); Michael Dubow, None; Alexander Pinhas, None; Nishit
Shah, None; Yusufu N. Sulai, None; Nicole K. Scripsema, None;
Joseph B. Walsh, None
Support: Marrus Family Foundation, Chairman's Research Fund of
the New York Eye and Ear Infirmary, Bendheim-Lowenstein Family
Foundation, Wise Family Foundation
Program Number: 6066 Poster Board Number: B0077
Presentation Time: 10:30 AM - 12:15 PM
Microangiopathic Features of Central Retinal Vein Occlusion
Imaged Using Fluorescence Adaptive Optics Scanning Light
Ophthalmoscopy
Alexander Pinhas1, 2, Nishit Shah1, Michael Dubow1, 2, Mitul Mehta1,
Patricia Garcia1, Nicole K. Scripsema1, 3, Joseph Carroll4, 5, Yusufu
N. Sulai6, Alfredo Dubra4, 7, Richard B. Rosen1. 1Ophthalmology,
New York Eye and Ear Infirmary, New York, NY; 2Mount Sinai
School of Medicine, New York, NY; 3New York Medical College,
Valhalla, NY; 4Ophthalmology, Medical College of Wisconsin,
Milwaukee, WI; 5Cell Biology, Neurology and Anatomy, Medical
College of Wisconsin, Milwaukee, WI; 6The Institute of Optics,
University of Rochester, Rochester, NY; 7Biophysics, Medical
College of Wisconsin, Milwaukee, WI.
Purpose: Central retinal vein occlusion (CRVO) remains a common
cause of vision loss in retinal vascular disease, second only to
diabetic retinopathy. Fluorescein angiography (FA) has remained the
gold standard for confirming its diagnosis and assessing the degree of
retinal nonperfusion, macroangiopathic change and macroscopic
response to treatment. The high transverse resolution of adaptive
optics scanning light ophthalmoscopy (AOSLO) has allowed for in
vivo study of retinal micropathology, but has been limited in its
capability to image retinal microvasculature. Here, we demonstrate
the use of fluorescence AOSLO (FAOSLO) for imaging microscopic
angiopathic features of CRVO.
Methods: Reflectance AOSLO (RAOSLO) images (790nm; 1° field
of view) were collected in five adult CRVO patients to identify
microvascular points of interest. Patients then ingested 1g fluorescein
dye. Simultaneous RAOSLO and FAOSLO images were then
collected between 15 and 60 minutes post-ingestion. The
fluorescence channel used a 488nm light for excitation; and, an
emission filter centered at 525nm with a 45nm bandwidth. For
comparison with conventional imaging techniques, Topcon fundus
imaging with and without IV fluorescein was performed.
Results: The combination of RAOSLO and FAOSLO enabled us to
visualize CRVO microangiopathic features in vivo in the finest
capillaries of the retinal inner nuclear layer. Among the features
visualized were vessel wall thickening, microaneurysms,
neovascularization and hemorrhage. FAOSLO showed the full extent
and detail of microangiopathy, as opposed to RAOSLO and
conventional fundus photography.
Conclusions: We believe that the clinical role of FAOSLO has
significant potential. Comparison with motion contrast-based
techniques remains to be evaluated. We believe that coupled with
RAOSLO and a method to analyze microangiopathic features
quantitatively, FAOSLO will lead to a better understanding of CRVO
pathophysiology, disease progression and a more comprehensive
method in monitoring tissue response to different treatment
modalities.
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.
ARVO 2013 Annual Meeting Abstracts by Scientific Section/Group – Visual Psychophysics / Physiological Optics
Fig 1. Fine capillary microaneurysms were seen (C, D) that were not
appreciated on either conventional imaging (A, B) or RAOSLO.
Fig 2. RAOSLO was better at visualizing hemorrhage (B) and vessel
wall thickening (D), whereas FAOSLO was better at outlining the
intravascular space and visualizing capillaries of finest caliber (C, E).
Commercial Relationships: Alexander Pinhas, None; Nishit Shah,
None; Michael Dubow, None; Mitul Mehta, None; Patricia
Garcia, None; Nicole K. Scripsema, None; Joseph Carroll,
Imagine Eyes, Inc. (S); Yusufu N. Sulai, None; Alfredo Dubra, US
Patent No: 8,226,236 (P); Richard B. Rosen, Opko-OTI (C), Optos
(C), Clarity (C), OD-OS (C), Topcon (R), Zeavision (F), Genetech
(F), Optovue (C)
Support: Marrus Family Foundation, Bendheim-Lowenstein Family
Foundation, Wise Family Foundation, Chairman's Research Fund of
the NYEEI, Research to Prevent Blindness, the Burroughs Wellcome
Fund and the Glaucoma Research Foundation
©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at arvo@arvo.org.