Increased Expression of Inducible Nitric Oxide Synthase and
advertisement

ICANCER RESEARCH 58. 2929-2934.
July 15. 1998]
Advances in Brief
Increased Expression of Inducible Nitric Oxide Synthase and Cyclooxygenase-2 in
Barrett's Esophagus and Associated Adenocarcinomas1
Keith T. Wilson,2 Sidong Fu, Kalathur S. Ramanujam, and Stephen J. Meltzer
Department of Medicine, Division of Gastroenterologe ¡K.T. W., S. f., K. S. R., S. J. M.l, Greeiiebauni Cancer Center {K. T. W.. S. J. MJ. Graduate Program in Molecular and
Cell Biology ¡S.J. M.], and Department of Pathology ¡S.J.M.I. University of Maryland School of Medicine and Baltimore Veterans Affairs Maryland Health Care System.
Baltimore. Mailand 2I20I
Abstract
Barrett's esophagus is a premalignant
condition arising in response to
chronic reflux esophagitis. Inducible nitric oxide synthase (¡NOS;NOS-2)
and cyclooxygenase-2 (COX-2) are mediators of inflammation and regu
lators of epithelial cell growth. Expression levels of ¡NOSand COX-2 are
high in colorectal adenomas and carcinomas, and COX-2 expression is
elevated in gastric cancers. To determine the involvement of ¡NOSand
COX-2 in Barrett's-associated neoplasia, we measured expression of these
genes in metaplastic Barrett's and esophageal adenocarcinomas. We de
tected elevated ¡NOSand COX-2 niKNA levels in Barrett's mucosa com
pared with paired gastric control tissues in 16 of 21 (76%) and 17 of 21
(80%) patients, respectively (/' < 0.001 for both genes). In esophageal
adenocarcinomas, ¡NOSand COX-2 inKNA levels were increased in four
of five and five of five cases, respectively. Furthermore, in 10 of 10
Barrett's patients, immunohistochemical
staining for ¡NOSand COX-2
expression was strongly positive and higher than in matched gastric
controls. Increased COX-2 expression was confirmed by Western blotting.
These findings support the hypothesis that ¡NOSand COX-2 are involved
early and often in Barrett's-associated
neoplastic progression.
Introduction
Barrett's esophagus is the replacement of the normal squamous
esophageal epithelium by a specialized columnar lining in response to
chronic reflux esophagitis (1). This condition is highly premalignant,
being associated with a risk of esophageal adenocarcinoma up to
125-fold greater than the general population (2, 3). The molecular
basis of this increased risk is now being elucidated. Generalized
genetic instability, evidenced by aneuploidy and chromosomal abnor
malities, has been shown to occur early in this process (4, 5). Loss of
heterozygosity, inactivation of tumor suppressor genes, and microsat
ellite instability have all been identified in Barrett's metaplasia and
associated esophageal adenocarcinomas, but the frequency of
alterations in metaplastic mucosa is generally lower than in
esophageal adenocarcinomas (6). In any case, much remains
learned about the molecular pathogenesis of Barrett's-associated
these
frank
to be
neo
plastic progression.
iNOS3 is the enzyme that catalyzes the high output pathway of
production of NO from L-arginine, whereas COX-2 is the rate-limiting
enzyme for the high output production of prostanoids (prostaglandins
and thromboxanes) from arachidonic acid. Increased expression of
Received 4/3/98; accepted 6/1/98.
The costs of publication of this article were defrayed in part by the payment of page
charges. This article musi therefore be hereby marked advertisement in accordance with
18 U.S.C. Section 1734 solely to indicate this faci.
1 Supported by NIH Grants K08-DK02469. ROI-CA67497. ROI-DK47717. and R01DK53620: the Robert and Sally D. Funderburg Award in Gastric Cancer Biology; the
University of Maryland School of Medicine; and the Office of Medical Research.
Department of Veterans Affairs.
2 To whom requests for reprints should be addressed, at Baltimore Veterans Affairs
Medical Center. Room 5D-151. 10 North Greene Street. Baltimore. MD 21201. Phone:
(410) 605-7000. ext. 5211; Fax: (410) 605-7914; E-mail: kwilson@umaryland.edu.
3 The abbreviations used are: iNOS. induciblc nitric oxide synthase; NO. nitric oxide:
COX-2. cyclooxygenase-2: RT-PCR. reverse transcription PCR; Gl. gastrointestinal.
both iNOS and COX-2 has been demonstrated in intestinal inflam
mation, in both animal models (7-9) and human diseases (10, 11).
Furthermore, we and others have identified high levels of expression
of iNOS and COX-2 in Helicobacter pylori-associated gastritis ( 12,
13). Finally, in in vitro studies, both iNOS and COX-2 have been
shown to have mutagenic (14-16) and tumorigenic (17-19) activity.
Recently, the importance of COX-2 in GI carcinogenesis has been
recognized. Induction of COX-2 expression has been demonstrated in
human and rodent colorectal adenomas and carcinomas (20, 21) and,
importantly, COX inhibition results in both regression of neoplastic
polyps and prevention of their development in individuals with fa
milial adenomatous polyposis, as well as in the murine models of this
disease, the min mouse and APC knockout mouse (21-23). In humans,
gastric adenocarcinomas have shown increased COX-2 expression
with no alteration in levels of COX-1, the constitutive form of
cyclooxygenase (24, 25). In contrast, the role of NO and iNOS in
human Gì
neoplasia is more uncertain. Although NO can induce DNA
damage (14, 15) and angiogenesis (26), it has been shown to inhibit
the growth of epithelial tumor cells (26). NOS activity has been
reported to be decreased in colorectal adenomas and carcinomas (27).
However, a recent comprehensive study by Ambs et al. (28) demon
strated increased Ca-independent iNOS activity and protein expres
sion in both colorectal adenomas and carcinomas.
We and others have determined that iNOS expression in human GI
inflammation predominates in the epithelium, and that intestinal ep
ithelial cell lines abundantly express iNOS with cytokine stimulation
(10, 29, 30). Although COX-2 expression is abundant in lamina
propria mononuclear cells and fibroblasts, it is also readily induced in
intestinal epithelial cells in vitro (31). Because Barrett's epithelium is
an intestinoid metaplasia that arises in response to chronic injury (acid
reflux), we hypothesized that Barrett's mucosa would express in
creased levels of iNOS and COX-2. We also sought to determine
whether levels of these gene products would remain elevated in
adenocarcinomas arising in Barrett's esophagus. In this report, we
demonstrate frequent overexpression of iNOS and COX-2 mRNA and
protein in both Barrett's metaplastic tissues and frank esophageal
adenocarcinomas
relative to matching gastric control mucosa.
Materials and Methods
Tissue Samples.
All tissues in this study were obtained from endoscopie-
biopsies or surgical resections from patients at either the University of Mary
land or Baltimore Veterans Affairs Medical Centers. Twenty-one paired Bar
rett's esophagus and gastric body tissues were included in this study. All cases
had histologically confirmed specialized columnar epithelium of Barrett's
esophagus. In addition, five paired tissues from surgical resections for adeno
carcinoma arising in known Barrett's mucosa and adjacent normal esophageal
tissue were studied. Tissues were snap-frozen in liquid nitrogen for the mRNA
and immunoblotting analysis and fixed in 10% buffered formalin for immunohistochemistry.
RT-PCR Analysis for ¡NOSand COX-2. Total RNA was isolated using
Trizol reagent (Life Technologies. Inc.. Gaithersburg. MD) and 2 /ig of RNA
2929
¡NOSAND COX-2 EXPRESSION
A
M
SBSBSB
IN BARRETT'S
ESOPHAGUS
MSBSBSBSBSB
—¿
ß-actin
-¡NOS
—¿
ß-actin
—¿
COX-2
B
0.9
0.8
0.7
:~ 0.6
; e
CQ.£>
0.4-
0.20.1
O
Stomach
Barrett's
Stomach
Barrett's
MNTNTNTN
—¿
ß-actin
-¡NOS
-COX-2
—¿
ß-actin
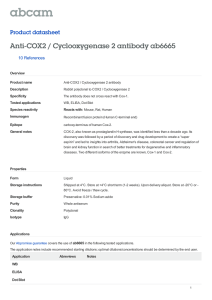
Fig. 1. RT-PCR analysis of ¡NOSand COX-2 mRNA expression in Barrett's esophagus tissues and in associated adenocarcinomas. A, representative gels of transcripts for ¡NOS
((op) and COX-2 (bottom). PCR product sizes in bp are ¡NOS,237; COX-2, 305; and ß-actin,496. M. DNA markers; S, stomach; B, Barrett's mucosa. B, densitometry of ¡NOSand
COX-2 transcripts, standardized to ß-actin,from control stomach and Barrett's mucosa for each patient. *** P < 0.001 versus stomach control by paired Student's / test. C, transcript
abundance of ¡NOSand COX-2 in esophageal adenocarcinomas. PCR product sizes (in bp) ¡NOS,237; COX-2, 756; and ß-actin,496. /V, normal esophagus; T, tumor.
from each sample were reverse transcribed using Superscript II RT (Life
Technologies, Inc.) in a total reaction volume of 20 fu. Reverse-transcription
product (cDNA; ! fj.\) was PCR-amplified with with Ampli-Taq DNA polymerase (Perkin-Elmer/Applied
Biosystems, Foster City, CA) and 0.5 pmol each
of ¡NOSor COX-2 forward and reverse primers, with ß-actinprimers included
in the same multiplex PCR reaction as an internal control for efficiency of RT
and amount of RNA. Each PCR cycle consisted of a denaturation step (94°C,
1 min), an annealing step (60°C, 1 min), and an elongation step (72°C, 1.5
min). There were a total of 35 cycles, followed by an additional extension step
(72°C,7 min). The primer sequences (F = forward, R = reverse primers) and
PCR product sizes were as follows: iNOS, 5'-TCTTGGTCAAAGC
TGTGCTC-3' (F) and 5'-CATTGCCAAACGTACTGGTC-3'
(R), 237 bp; two sets
of COX-2 primers, 5'-TTCAAATGAGATTGTGGGAAAATTGCT-3'
(F)
and S'-GATCATCTCTGCCTGAGTATCTT-S'
(R), 305 bp plus 5'-CAG-
CACTTCACGCATCAGTT-3'
(F) and 5'-TCTGGTCAATGGAAGCCTGT-3' (R), 756 bp; and, finally, ß-actin,5'-CCAGAGCAAGAGAGGTATCC-3' (F) and 5'-CTGTGGTGGTGAAGCTGTAG-3'
(R), 436 bp. PCR prod
ucts were run on 2% agarose gels with 0.5 /ig/ml ethidium bromide, and
stained bands were visualized under UV light, photographed, digitized with an
Agfa Arcus II scanner, and band intensity quantitated using NIH Image version
1.61.
Immunohistochemical
Analysis. Sections (5 jn.m) cut from paraffin-em
bedded tissues were deparaffmized, and endogenous peroxidase activity was
quenched by incubation in 0.3% H2O2 in methanol for 30 min. Sections were
then microwaved in citrate buffer, pH 6.1, for 30 min for antigen retrieval.
Nonspecific binding was blocked with 5% normal horse serum in PBS and the
tissue was incubated with monoclonal antibodies to ¡NOS(antimouse, 1:500
dilution; Transduction Labs, Lexington, KY) or COX-2 (antirat, 1:1000 dilu-
2930
¡NOSAND COX-2 EXPRESSION
feÎ^P^ï^VO'Al-'
IN BARRETT'S
ESOPHAGUS
F
?Ù
' j$>..i'~~^,
•¿-•rflPWiv
s---*•¿'
\
^*i
^K ^S&
¿^
'y<»M
/
¿
•¿.»'Sì-
|U|ïï ^£|$s
l •¿
^»».*
^_.
ft
fr*
*
*
-M
¿^
t
J^lÉ-
».T»
ÕLiSÎ*51*^
Fig. 2. Immunohistochemical detection of ¡NOS(A-D) and COX-2 (£-W)in tissues from gastric body (A and £").
Barrett's esophagus (ßand F), dysplasia (C and G), and carcinoma
(D and //). Staining was performed on formalin fixed tissues using specific monoclonal antibodies detected with peroxidase-3.3'-diaminobenzidine
(brownish pigment). iNOS staining
was absent in the normal gastric body (A) and squamous epithelium (B) in contrast to the staining of the metaplastic appearing glands of the Barrett's mucosa (B) which was especially
intense in areas of dysplasia (O and carcinoma (D). COX-2 protein is present at a low level in the normal gastric body (£")
and strongly increased in the lamina propria of Barrett's
mucosa (F) and in the epithelium of the dysplastic (C) and malignant glands (ff). Tissues incubated with mouse IgG rather than the primary antibodies had absent staining (data not
shown) verifying the specificity of the antibody staining.
tion; Transduction
Labs) overnight at 4°Cin 5% normal horse serum. As
controls, slides were incubated in the presence of 5% normal horse serum alone
or with the same concentration of mouse IgG (Vector Labs. Burlingame, CA)
as used for the primary antibody. Immunoreactivity was detected by the ABC
Method (Vectastain Elite ABC kit, Vector Labs). Slides were subsequently
incubated with a biotinylated secondary horse antimouse IgG antibody at 1:200
for 30 min. This was detected using avidin conjugated to horseradish peroxidase. The color was then developed using 3.3'-diaminobenzidine.
Mayer's
hematoxylin was then added as a counterstain for 5 min.
Western Blot Analysis. Tissues were homogenized in Tris-HCI pH
1.4 buffer containing 0.5% Triton X-100 and protease inhibitor cocktail
(Boehringer Mannheim, Indianapolis.
2931
IN). Protein concentration
of 14,000 g
iNOS AND COX-2 EXPRESSION
SBSB
IN BARRETT'S
ESOPHAGUS
NTNTNT
—¿
COX-2
70 kDa —¿
Fig. 3. Increased COX-2 protein levels (70 kDa band) by immunoblotting
in representative paired tissues from control stomach (.VIand Barrett's mucosa (ß:¡eftpanel}, and from
normal esophagus (AOand esophagcal tumors (T. righi). Equal concentrations of protein (100 ^g) were loaded in each lane. The nonspecific bands below 70 kDa on the n^lii are due
to some degradation of protein in surgical resections compared with an absence of such bands in endoscopie biopsies, which are more rapidly frozen.
soluble supernatants from each sample was measured by the method of
Bradford (32). Then 100 /ng of protein was loaded per lane, separated by
SDS-PAGE under reducing conditions, and transferred onto Hybond-PVDF
squamous epithelium (Fig. 2B). For COX-2 (Fig. IF), staining local
ized primarily to lamina propria mononuclear cells and myofibroblasts, with no detectable staining of the Barrett's epithelium or
membranes (Amersham Inc.. Arlington Heights. IL) by electroblotting. The
transfer of protein and equal loading in all lanes was verified using reversible
staining with Ponceau S. Membranes were blocked using 5% nonfat dry milk.
COX-2 protein was detected by incubation of blots with a monoclonal anti
body to a synthetic peptide from the human COX-2 sequence from Cayman
Chemical Company (Ann Arbor. MI ) at a dilution of 1:1(XX)overnight at 4°C,
adjacent squamous esophageal epithelium. Gastric mucosa showed
occasional low-level COX-2 staining in the lamina propria (Fig. 2E),
but of much less intensity than in the lamina propria of the Barrett's
followed by a sheep antimouse secondary antibody conjugated to horseradish
peroxidase and determination of enhanced chemiluminescence
(Amersham)
using exposure to Kodak BioMax MR film.
Results
Increased ¡NOSand COX-2 mRNA Expression
in Barrett's
Esophagus and Associated Adenocarcinorna. ¡NOSmRNA was
readily detectable by RT-PCR in 16of21 (76.2%) of Barrett's tissues,
and COX-2 mRNA was similarly expressed in 17of21 (81%)of these
tissues. As shown in Fig. 1, in all positive cases ¡NOSand COX-2
levels were increased above those in the gastric control tissues from
the same patients, and in no case were gastric levels greater than those
in Barrett's mucosa (P = 0.0004 for ¡NOSand P = 0.0003 for
COX-2; Fisher's exact test). Fig. \A demonstrates the increased iNOS
and COX-2 mRNA abundance in eight representative patient tissue
pairs. Gel densitometry of transcripts (standardized to constitutively
expressed ß-actin)illustrates the pattern of markedly increased ¡NOS
(P = 0.0002; Student's / test) and COX-2 (P < 0.0001) mRNA levels
in the Barrett's tissues compared with paired control stomach tissues.
Two of the 21 patients with Barrett's esophagus had dysplasia present
and both were positive for both iNOS and COX-2. As shown in Fig.
1C, increased iNOS and COX-2 mRNA expression also occurred in
adenocarcinomas arising in Barrett's mucosa. Expression of both
genes was very low to absent in adjacent normal esophagus but
readily detectable in four of five patients for ¡NOSand five of five for
COX-2.
We sought to compare the frequency of iNOS and COX-2 expres
sion with that of another growth-related gene previously shown to be
abundant in Barrett's esophagus, transforming growth factor-a (33).
The results were very similar: transforming growth factor-a mRNA
expression was increased in 17 of 21 cases (81.0%) of Barrett's
metaplasias and in 5 of 5 Barrett's-associated esophageal adenocar
cinomas versus matched gastric epithelium (data not shown). In
contrast, mRNA expression levels of the proinflammatory cytokines
tumor necrosis factor-a, interleukin-8, and monocyte chemotactic
protein-1 were not increased in Barrett's tissues compared with gastric
tissue. Particularly intense epithelial iNOS staining was discovered in
areas of esophageal dysplasia and adenocarcinoma (Fig. 2C and D). In
dysplastic and malignant esophageal glands, COX-2 uniquely local
ized to the epithelium, in addition to the lamina propria mononuclear
cell staining seen in gastric control and Barrett's tissues (Fig. 2G
and//).
Because we observed COX-2 protein expression in the gastric body
by irnmunohistochemistry,
we sought to confirm up-regulation of
COX-2 in Barrett's tissues by Western blot analysis. Fig. 3 demon
strates increased COX-2 protein abundance in Barrett's metaplasias
relative to paired stomach, as well as increased COX-2 protein ex
pression in Barrett's-associated carcinomas compared with adjacent
esophagus.
Discussion
These results suggest, for the first time, that iNOS and COX-2 are
involved in Barrett's-associated esophageal neoplasia. Furthermore,
our data suggest that overexpression of these proteins constitutes an
early event in the esophageal neoplastic transformation process which
occurs at the precancerous metaplastic stage. Overexpression of ¡NOS
and COX-2 was demonstrated in the great majority of metaplastic and
dysplastic or cancerous Barrett's specimens, suggesting that this ab
normality is involved in most cases of Barrett's lesions at diverse
stages of neoplastic development. Findings obtained at the mRNA
level (by RT-PCR) were strongly corroborated by similar findings at
the protein level (by immunoblotting or irnmunohistochemistry).
Our findings that iNOS and COX-2 were consistently up-regulated
in Barrett's tissues, in contrast to other pro-inflammatory cytokines,
suggest that this is a somewhat specific effect and not simply a
function of generalized inflammation, per se. Moreover, the persist
ence of increased iNOS and COX-2 expression in dysplasia and
carcinoma implies that induction of these genes may be necessary for
maintenance of the malignant phenotype as well. The hypothesis that
iNOS and COX-2 are involved in human neoplastic transformation
has been well supported by data obtained in tumors of other organ
systems. This evidence is particularly strong in the case of COX-2,
where up-regulation has been demonstrated in coloréela!and gastric
cancers (20, 21, 24, 25). Furthermore, pharmacological inhibition of
COX-2 activity has proven effective in reducing colonie polyp for
mation in humans and mouse models as well as in triggering polyp
regression (22, 23). Mice doubly null for the COX-2 and APC genes
show a marked reduction of polyp formation relative to APC-null
mice alone (21). In vitro data suggest that a key underlying mecha
nism for the proneoplastic effect of COX-2 is potent inhibition of
epithelial apoptosis coupled with stimulatory effects on epithelial
glands (Fig. 1A and B). There was also no iNOS protein in adjacent
proliferation (18, 34).
2932
controls (data not shown).
Increased iNOS and COX-2 Protein Expression. To confirm the
expression of iNOS and COX-2 at the protein level and to assess their
cellular sources, immunostaining for iNOS and COX-2 was per
formed in 10 of the patients, with the following pattern consistently
observed (Fig. 2). With iNOS, there was a lack of staining in the
gastric body compared with intense staining of metaplastic Barrett's
¡NOSAND COX-2 EXPRESSION
Our data implicate the involvement of iNOS in GI carcinogenesis.
Previous studies have demonstrated increased iNOS expression in
breast and gynecological malignancies (35, 36), but only recently has
iNOS induction been demonstrated in colorectal cancer (28). We and
others have identified increased iNOS expression in H. pylori gastritis
(12, 13, 37), but the present study is the first report, to our knowledge,
of iNOS expression in upper GI tract dysplasia or carcinoma. NO has
been shown to produce DNA damage and mutation in cell-free sys
IN BARRETT'S
References
Reid. B. J.. and Weinstein, W. M. Barrett's esophagus and adenocarcinoma.
Cancer Prev.. /: 323-325, 1992.
Williamson. W. A., Ellis. F. H.. Jr.. Gibb. S. P.. Shahian. D. M.. Aretz. H. T.. Heatley.
G. J., and Watkins, E., Jr. Barrett's esophagus. Prevalence and incidence of adeno
carcinoma. Arch. Intern. Med., 151: 2212-2216, 1991.
Rabinovitch. P. S.. Reid. B. J.. Haggitt. R. C.. Norwood, T. H., and Rubin. C. E.
Progression to cancer in Barrett's esophagus is associated with genomic instability.
Lab. Invest., 60: 65-71. 1989.
Reid. B. J.. Blount, P. L.. Rubin. C. E., Levine, D. S.. Haggitt, R. C., and Rabinovitch.
P. S. Flow-cytometric and histological progression to malignancy in Barrett's esoph
which then down-regulates iNOS transcription via a p53 binding site
agus: prospective endoscopie surveillance of a cohort. Gastroenterology. 102: 12121219. 1992.
Souza. R. F.. and Meltzer, S. J. The molecular basis for carcinogenesis in metaplastic
columnar-lined esophagus. Gastroenterol. Clin. N. Am., 26: 583-597. 1997.
Miller. M. J. S., Thompson. J. H.. Zhang. X-J., Sadowskakrowicka, H.. Kakkis, J. L.,
Munshi. U. K.. Sandoval. M., Rossi. J. L., Elobychildress, S.. Beckman. J. S., Ye,
Y. Z.. Rodi, C. P., Manning. P. T., Currie, M. G.. and Clark, D. A. Role of inducible
nitric oxide synthase expression and peroxynitrite formation in guinea pig ileitis.
Gastroenterology. 109: 1475-1483. 1995.
Chang, A. D.. Ramanujam. K. S.. and Wilson. K. T. Co-expression of inducible nitric
oxide synthase (iNOS), cyclooxygenase (COX-2). and TGF-/3 in rat models of colitis
(Abstract). Gastroenterology. 110: A881, 1996.
Reuter. B. K.. Asfaha. S.. Buret. A.. Sharkey. K. A., and Wallace. J. L. Exacerbation
of inflammation-associated colonie injury in rat through inhibition of cyclooxygenase-2. J. Clin. Invest.. 98: 2076-2085. 1996.
to. Singer. I. I., Kawka, D. W.. Scott, S.. Weidner. J. R.. Mutnford, R. A.. Riehl, T. E.,
and Stenson. W. F. Expression of inducible nitric oxide synthase and nitrotyrosine in
colonie epithelium in inflammatory bowel disease. Gastroenterology. ///: 871-885.
1996.
Fu. S., Ramanujam. K. S., Meltzer, S. J., and Wilson, K. T. Inducible nitric oxide
synthase (iNOS) and cyclooxygenase (COX-2) expression in ulcerative colitis and
Crohn's disease. Gastroenterology. 110: A910. 1996.
in the iNOS promoter (38). This suggests that regulation of iNOS
expression may be one important effect of p53, and that NO may be
capable of inducing p53 mutation with chronic stimulation (38, 39).
Recently, peroxynitrite, the reaction product of NO and Superoxide,
was shown to induce DNA strand breaks in gastric epithelial cells
whereas NO alone had no effect (40). In vivo, nitrosamines, which can
be formed from NO, have long been implicated in upper GI tract
carcinogenesis (41).
It should be noted that both NO and prostaglandins can have
important protective effects in the Gìmucosa. Although NOS inhibi
tion has been associated with amelioration of intestinal inflammation
in several chemically-induced models, iNOS null mice develop more
severe acetic acid colitis than wild-type controls (42). Moreover,
recent data from one of our laboratories (K. T. W.) indicate that
selective iNOS inhibition worsens the enterocolitis of IL-IO null mice
and acute colitis in rat models. Similarly, COX-2 inhibition exacer
bates rat models of colitis (9). It is likely that some of the antiinflammatory effects of NO and prostaglandins may ultimately prove
to be deleterious in the transformation to dysplasia and cancer, how
ever. For example, inhibition of cytokine production by NO and
prostaglandins (43, 44) and leukocyte adhesion to vascular endothelium by NO (45) may reduce immune response to tumors. Similarly,
induction of apoptosis by NO (39) may ultimately result in increased
epithelial turnover and proliferation as may the cytoprotective effects
of prostaglandins in the GI epithelium.
The localization of iNOS predominantly to the epithelium in the
Barrett's tissues is consistent with published findings in human in
flammatory bowel disease (10) and supports a potential role for NO in
the regulation of epithelial cell growth. This role now seems more
likely, in light of the particularly intense iNOS staining that we
observed in dysplastic and malignant Barrett's epithelium. Interest
ingly, in metaplastic Barrett's mucosa, COX-2 expression was ob
served primarily in the lamina propria, consistent with our findings in
intestinal inflammation and H. pylori gastritis; however, upon pro
gression to dysplasia and carcinoma, a shift of staining to the epithe
lium was observed, suggesting that COX-2 overexpression in these
cells may constitute a relatively late event.
Our findings in the present study have important clinical implica
tions. iNOS, COX-2, or both genes may prove valuable as biomarkers
of cancer risk for metaplastic and dysplastic Barrett's lesions, as well
iNOS or COX-2
may form the basis for future novel therapeutic and/or preventive
strategies using techniques to inhibit these genes, such as molecular
mimicry, pharmacological antagonism, or antisense gene therapy. In
addition, our findings suggest that the involvement of iNOS and
COX-2 should be investigated in other tumor types and premalignant
lesions such as cervical dysplasia, oral leukoplakia, gastric intestinal
metaplasia, ulcerative colitic dysplasia, pancreatic hyperplasia, or
early premalignant skin lesions.
4 K. T. Wilson and S. J. Meltzer. unpublished observations.
Annu.
Rev. Med.. 38: 477-492. 1987.
Bartlesman, J. F.. Hameeteman. W.. and Tytgat. G. N. Barrett's oesophagus. Eur. J.
tems (14, 15), but specific findings have been difficult to demonstrate
in cultured cells.4 NO can induce wild-type 53 protein expression,
as prognostic indicators for frank adenocarcinomas.
ESOPHAGI'S
Wong, A., Fu, S.. Varanasi. R. V., Ramanujam. K. S.. Fantry. G. T.. and Wilson. K. T.
Expression of inducible nitric oxide synthase and cyclooxygenase-2 and modulation
by omeprazole in Helicohacler pylori gastritis. Gastroenterology. 112: A332. 1997.
Mannick. E. F... Bravo. L. E.. Zarama. G.. Realpe. J. L., Zhang. X. J.. Ruiz. B.,
Fontham, E. T.. Mera. R.. Miller, M. J., and Correa. P. Inducible nitric oxide synthase.
nitrotyrosine. and apoptosis in Helicnbacler pylori gastritis: effect of antibiotics and
antioxidants. Cancer Res., 56: 3238-3243. 1996.
14. Wink. D. A.. Kasprzak. K. S.. Maragos. C. M.. Elespuru. R. K.. Misra. M.. Dunams.
T. M.. Cebula. T. A.. Koch. W. H., Andrews, A. W.. Allen. J. S., and Keefer. L. K.
DNA deaminating ability and genotoxicity of nitric oxide and its progenitors. Science
(Washington DC), 254: 1001-1003. 1991.
Nguyen. T.. Brunson. D.. Crespi. C. L.. Penman, B. W.. Wishnok. J. S., and
Tannenbaum. S. R. DNA damage and mutation in human cells exposed to nitric oxide
in vitro. Proc. Nati. Acad. Sci. USA, 89: 3030-3034. 1992.
16. Plummer. S. M.. Hall. M.. and Faux. S. P. Oxidation and genotoxicity of fecapentaene-12 are potentiated by prostaglandin H synthase. Carcinogenesis (Lond.). 16:
1023-1028. 1995.
Mordan. L. J.. Burnett. T. S.. Zhang. L. X.. Tom. J.. and Cooney, R. V. Inhibitors of
endogenous nitrogen oxide formation block the promotion of neoplastic transforma
tion in C3H 10T1/2 fibroblasts. Carcinogenesis (Lond.). 14: 1555-1559, 1993.
Tsujii. M.. and DuBois, R. N. Alterations in cellular adhesion and apoptosis in
epithelial cells overexpressing prostaglandin endoperoxide synthase 2. Cell. 83:
493-501. 1995.
19. Boolbol. S. K.. Dannenberg, A. J.. Chadbum. A.. Martucci. C., Guo. X. J.. Ramonetti.
J. T.. Abreu-Goris. M., Newmark, H. L., Lipkin. M. L.. DeCosse. J. J.. and
Bertagnolli. M. M. Cyclooxygenase-2 overexpression and tumor formation are
blocked by sulindac in a murine model of familial adenomatous polyposis. Cancer
Res., 56: 2556-2560. 1996.
20 Eberhart, C. E., Coffey. R. J.. Radhika, A.. Giardiello, F. M.. Ferrenbach. S.. and
DuBois. R. N. Up-regulation of cyclooxygenase 2 gene expression in human colo
rectal adenomas and adenocarcinomas. Gastroenterology. 707: 1183-1188. 1994.
Oshima. M.. Dinchuk. J. E.. Kargman, S. L., Oshima. H.. Hancock. B.. Kwong. E..
Trzaskos, J. M.. Evans. J. F., and Taketo, M. M. Suppression of intestinal polyposis
in Ape delta716 knockout mice by inhibition of cyclooxygenase 2 (COX-2). Cell, 87:
803-809. 1996.
22. Giardiello. F. M.. Hamilton. S. R., Krush, A. J., Piantadosi. S.. Hylind. L. M.. Celano.
P.. Booker, S. V.. Robinson, C. R.. and Offerhaus. G. J. Treatment of colonie and
rectal adenomas with sulindac in familial adenomatous polyposis. N. Engl. J. Med..
328: 1313-1316. 1993.
23. Jacoby. R. F., Marshall. D. J., Newton. M. A., Novakovic, K., Tutsch. K., Cole, C. E.,
Lubet. R. A.. Kelloff. G. J.. Verma. A.. Moser. A. R.. and Dove, W. F. Chemoprevention of spontaneous intestinal adenomas in the Ape Min mouse model by the
nonsteroidal anti-inflammatory drug piroxicam. Cancer Res.. 56: 710-714. 1996.
Soydan, A. S.. Gaffen, J. D., Weech, P. K., Tremblay, N. M.. Kargman. S.. O'Neill.
24.
G.. Bennett. A., and Tavares. I. A. Cytosolic phospholipase A2, cyclo-oxygenases and
arachidonate in human stomach tumours. Eur. J. Cancer. 33: 1508-1512. 1997.
25 Rislimaki. A.. Honkanen. N.. Jankala. H.. Sipponen. P.. and Harkonen. M. Expression
of cyclooxygenase-2 in human gastric carcinoma. Cancer Res., 57: 1276-1280. 1997.
2933
¡NOSAND COX-2 EXPRESSION
26. Jenkins, D. C., Charles, I. G., Thomsen, L. L., Moss, D. W., Holmes, L. S., Baylis,
S.A., Rhodes, P., Westmore, K., Emson, P. C, and Moneada, S. Roles of nitric oxide
in tumor growth. Proc. Nati. Acad. Sci. USA, 92: 4392-4396, 1995.
27. Moochhala, S., Chhatwal, V. J., Chan, S. T., Ngoi, S. S., Chia, Y. W., and Rauff, A.
Nitric oxide synthase activity and expression in human colorectal cancer. Carcinogenesis (Lond.), 17: 1171-1174, 1996.
28. Ambs, S., Merriam, W. G., Bennett, W. P., Felley-Bosco, E., Ogunfusika, M. 0.,
Oser, S. M., Klein, S., Shields, P. G., Billiar, T. R., and Harris, C. C. Frequent nitric
oxide synthase-2 expression in human colon adenomas: implication for tumor angiogenesis and colon cancer progression. Cancer Res., 58: 334-341, 1998.
29. Ramanujam, K. S., Topczy, N., Fu, S., and Wilson, K. T. Expression and regulation
of inducible nitric oxide synthase (¡NOS)in intestinal epithelial cells. Gastroenterology, HO: A997, 1996.
30. Sherman, P. A., Laubach, V. E., Reep, B. R., and Wood, E. R. Purification and cDNA
sequence of an inducible nitric oxide synthase from a human tumor cell line.
Biochemistry, 32: 11600-11605, 1993.
31. DuBois, R. N., Tsujii, M., Bishop, P., Awad, J. A., Makita, K., and Lañaban, A.
Cloning and characterization of a growth factor-inducible cyclooxygenase gene from
rat intestinal epithelial cells. Am. J. Physiol., 266: G822-G827, 1994.
32. Bradford, M. M. A rapid and sensitive method for the quantitation of microgram
quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem.,
72: 248-254, 1976.
33. Brito, M. J., Filipe, M. I., Linchan, J., and Jankowski, J. Association of transforming
growth factor a (TGFa) and its precursors with malignant change in Barrett's
epithelium: biological and clinical variables. Int. J. Cancer, 60: 27-32, 1995.
34. Sheng, H., Shao, J.. Morrow, J. D., Beauchamp, R. D., and DuBois, R. N. Modulation
of apoptosis and Bcl-2 expression by prostaglandin E2 in human colon cancer cells.
Cancer Res., 58: 362-366, 1998.
35. Thomsen, L. L., Lawton, F. G., Knowles, R. G., Beesley, J. E., Riveros-Moreno, V.,
and Moneada, S. Nitric oxide synthase activity in human gynecological cancer.
Cancer Res., 54: 1352-1354, 1994.
IN BARRETT'S
ESOPHAGUS
36. Thomsen, L. L., Miles, D. W., Happerfield, L., Bobrow, L. G., Knowles, R. G., and
Moneada, S. Nitric oxide synthase activity in human breast cancer. Br. J. Cancer, 72:
41-44, 1995.
37. Wilson, K. T., Ramanujam, K. S., Mobley, H. L., Musselman, R. F., James, S. P., and
Meltzer, S. J. Helicobacter pylori stimulates inducible nitric oxide synthase expres
sion and activity in a murine macrophage cell line. Gastroenterology, ///: 15241533, 1996.
38. Forrester, K., Ambs, S., Lupold, S. E.. Kapust, R. B., Spillare, E. A., Weinberg,
W. C., Felley-Bosco, E., Wang, X. W., Geller, D. A., Tzeng, E., Billiar, T. R., and
Harris, C.C. Nitric oxide-induced p53 accumulation and regulation of inducible nitric
oxide synthase expression by wild-type p53. Proc. Nati. Acad. Sci. USA. 93:
2442-2447, 1996.
39. Brune, B., Gotz, C.. Messmer, U. K., Sandau, K., Hirvonen, M. R., and Lapetina,
E. G. Superoxide formation and macrophage resistance to nitric oxide-mediated
apoptosis. J. Biol. Chem., 272: 7253-7258, 1997.
40. Kennedy, M., Denenberg, A. G., Szabo, C., and Salzman, A. L. Poly(ADP-ribose)
synthetase activation mediates increased permeability induced by peroxynitrite in
Caco-2BBe cells. Gastroenterology, 114: 510-518, 1998.
41. Bartsch, H., Ohshima, H., Pignatelli, B., and Calméis,S. Endogenously formed
N-nitroso compounds and nitrosating agents in human cancer etiology. Pharmacogenetics, 2: 272-277, 1992.
42. McCafferty, D. M., Mudgett, J. S., Swain, M. G., and Kubes, P. Inducible nitric oxide
synthase plays a critical role in resolving intestinal inflammation. Gastroenterology,
112: 1022-1027, 1997.
43. Peng, H. B., Rajavashisth, T. B., Libby, P., and Liao, J. K. Nitric oxide inhibits
macrophage-colony stimulating factor gene transcription in vascular endothelial cells.
J. Biol. Chem., 270: 17050-17055, 1995.
44. Betz, M., and Fox, B. S. Prostaglandin E2 inhibits production of Thl lymphokines but
not of Th2 lymphokines. J. Immunol., 746: 108-113, 1991.
45. Kubes, P., Suzuki, M., and Granger, D. N. Nitric oxide: an endogenous modulator of
leukocyte adhesion. Proc. Nati. Acad. Sci. USA, 88: 4651-4655, 1991.
2934