Ostomy care
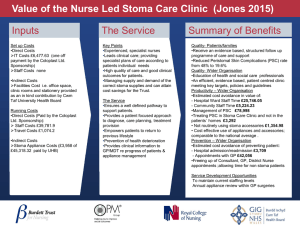
advertisement

TOPIC HEADER CLINICAL FOCUS Resuming a normal life: holistic care of the person with an ostomy Jennie Burch Jennie Burch is Enhanced Recovery Nurse Facilitator, St Marks Hospital, North West London NHS Trust. Email: jburch1@nhs.net C ommunity nurses regularly care for patients with a stoma and in order to provide holistic care to such patients, an understanding of stoma care is vital. This article briefly explores a variety of aspects of stoma care including why stomas are formed, what appliances can be used and issues that might affect the ostomate once they are discharged home from hospital. Stomas A stoma, also known as an ostomy, is an artificial, surgically created opening onto the abdominal wall to allow the exit of faeces and urine. There are three main types of stoma that the community nurse might encounter. The most common is the colostomy, with 11000 formed in the UK in 2006 (IMS, 2007). The least commonly seen is the urostomy; there is also the ileostomy, which is being increasingly formed due to surgical improvements and the reduced need for a permanent stoma. A colostomy is formed from the colon (large bowel) and will usually pass flatus and soft, formed faeces into a closed bag. An ileostomy is formed from the ileum (small bowel) and will often pass about 800 ml of loose, porridge-like stool and flatus throughout the day into a drainable pouch that requires emptying between four and six times daily. A urostomy is generally formed from a segment of ileum and this gives the name ileal conduit. A urostomy will pass urine and a small amount of mucous into a drainable bag with a bung or tap on it and requires emptying four to six times daily. Abstract A community nurse may often encounter an ostomate (person with a stoma) but may not be regularly involved in their stoma care. This article explains the main types of stoma, stoma appliances and indications for some operations. Explanations are provided on some of the stoma appliances and accessories and when these might be useful to the community nurse and the ostomate. Stoma care is explained, including how to undertake a basic stoma appliance change. Issues that community nurses might be questioned about, such as diet and driving, are explored to assist the community nurse in providing holistic care for ostomates. KEY WORDS Stoma w Colostomy w Ileostomy w Urostomy w Holistic care 366 A healthy stoma is red or pink in appearance and usually round or oval in shape. An ideal colostomy should be minimally raised above the level of the abdominal skin and is often 30–35 mm in diameter and is generally formed in the left iliac fossa. An ileostomy and a urostomy look similar (except for the output) they should ideally have a small spout of about 25 mm and be about 28–30 mm in diameter and they are formed in the right iliac fossa most commonly. A colostomy or an ileostomy can be temporary or permanent, depending on the type of operation performed and the indication for the operation, whereas a urostomy is permanent. A colostomy or ileostomy will be either an end or a loop stoma, again depending on the operation. A urostomy is always an end stoma. Colostomy There are many reasons to form a stoma. These include: wBladder cancer wBowel perforation wCrohn’s disease wColorectal cancer wDiverticular disease wHirschsprung’s diseases wImperforate anus wSpina bifida wTrauma wUlcerative colitis. A colostomy can be formed for a rectal cancer, diverticular disease, perforation or trauma. An operation that results in a permanent end colostomy is an abdominoperineal resection of the rectum. This operation involves the removal of the anus, anal canal, rectum and some of the distal colon. A loop colostomy might be formed, for example in the transverse colon; two ends are brought to the abdominal surface to protect or ‘defunction’ a lower anastomosis. Ileostomy An ileostomy is formed by bringing the end or loop of small intestine (the ileum) out on to the surface of the skin. An anterior resection involves the removal of some or most of the rectum but the anal canal and anus are retained. The two ends of the bowel that are left when the cancer is removed are joined (anastomosed). However, as the join is within the pelvis there is an increased chance of this join leaking, which can lead to a potentially life-threatening British Journal of Community Nursing Vol 16, No 8 TOPIC HEADER CLINICAL FOCUS An elderly colostomy patient with an abdominal wound being treated by a district nurse. peritonitis due to faeces leaking inside the abdomen. The surgeon may opt to perform a defunctioning ileostomy, also called a loop ileostomy. The anastomosis is then defunctioned so that faeces do not pass through the new join and thus eliminates the risk of peritonitis. A temporary ileostomy is then reversed or closed in a subsequent operation at a later date, often 3 months to a year later, depending upon the need for other treatments such as chemotherapy. This operation can be performed both open (with a large midline abdominal wound) or by laparoscopic or keyhole surgery with multiple small incisions. The community nurse might be requested to provide postoperative care for the wound(s) and again when giving holistic care, might also be requested to assist with any stoma-related issues at the same visit. Urostomy A urostomy can be formed for a bladder cancer when the bladder needs to be removed and the passage of urine diverted through the abdominal wall. The operation involves a cystectomy (bladder removal) with the ureters remaining attached to the kidneys; the other ends of the ureters are then joined to one end of a small segment of ileum (which is isolated from the rest of the small bowel). The end near the ureters is oversewn so that the urine does British 368 368 Journal of Community Nursing Vol ?, No not leak back into the abdominal cavity. The other end of the ileum is brought out as the stoma (Nazarko, 2008). The blood supply remains with the small segment (or conduit) and the two ends of the small bowel are re-joined or reanastomosed so that the ostomate passes bowel motion in the usual way. Appliances and accessories A stoma appliance – also known as a ‘bag’ or ‘pouch’ – is a device designed to attach around the stoma and collect the stomal output, i.e. faeces/flatus/urine, and contain any odours, but to also be secure and skin friendly. An appliance is made up from two parts, a flange and a pouch part. The flange can also be called the base plate, face plate or wafer and is the adhesive part that adheres to the skin around the stoma (peristomal skin). The pouch part is generally manufactured from plastic, covered in a cloth-type outer layer and is opaque, although appliances can also be clear. Stoma appliances can be closed, drainable or drainable with a bung. Each of these comes in a one-piece version and a two-piece version. A one-piece appliance has the flange and the pouch part joined and is removed in a single piece. A two-piece appliance has the flange and the pouch part separate and these are then joined (Williams, British BritishJournal JournalofofCommunity CommunityNursing Nursing Vol Vol 16, 368 ?, NoNo 8 CLINICAL FOCUS 2006). Historically, the two parts were joined by rings that clipped together. Since more recently, these two rings adhere together. The majority of stoma appliances have a flat adhesive flange, but for ostomates with problem stomas such as a retracted colostomy or a flush ileostomy/urostomy, a convex appliance might be necessary. These should not be used without a careful assessment as they can cause ulceration around the stoma from the pressure of the convexity, but are very useful in the appropriate situation (Cronin, 2008a). The stoma appliance is provided in hospital by the stoma care nurse and this might work well indefinitely. However, the appliance might actually become unsuitable very soon after discharge home owing to changes in the stoma or peristomal skin. There is also a wide range of stoma accessories used for a variety of different reasons. A stoma accessory is used with a stoma appliance. Accessories can help secure the appliance to the abdomen, might be used to remove the adhesive or to protect broken skin, for instance. These will be discussed later in the article. There are also available alternatives to conventional colostomy appliances including toilet disposable colostomy bags. These are specially designed to breakdown in the toilet system. To hold back faeces for short periods of time, stoma plugs (Cronin, 2008b) and other devices can be used. Alternatively the colostomy can be irrigated to wash out the faeces and then a small cap is required. Stoma education While in hospital (Colwell and Gray, 2007), a person with a newly formed stoma (ostomate) should be taught to care for their stoma and should have post-discharge followup by the stoma nurse (Fulham, 2008). Stoma training quickly enables the ostomate to gain independence with their stoma care and involves a number of simple steps. These steps are basically as follows (although can vary): wExplain the procedure to the patient and gain their consent wCollect all the stoma equipment (clean appliance, measuring guide (if needed), pen (if needed), scissors (if needed), cleaning/drying clothes or kitchen roll, warm tap water without soap and a disposal bag wEmpty the appliance if drainable wGently remove the old appliance, supporting the abdominal skin with one hand wJoin the edges of the flange together to contain the stomal output and place in the disposable bag wGently but thoroughly clean and dry the peristomal skin (being gentle with the actual stoma, which will easily bleed, the stoma may also be active during this time) wMeasure the stoma (as the size can reduce in the first eight weeks or with weight loss and can conversely increase in diameter if weight is gained) wCut the appliance to the required shape and size (ideally 370 2-3 mm larger than the stoma) wRemove the flange backing wApply the flange to the peristomal skin wSecure the adhesive to the skin by pressing firmly (start at the stoma and work outwards) wIf a two-piece appliance is used attach the bag wHold the appliance onto the abdomen for 30-60 seconds to aid adhesion wEnsure the fastening is closed (if appropriate) wSeal the rubbish bag and dispose of it wWash hands wAvoid bending the abdomen for ten minutes after application to help adhesion (Trainor et al, 2003; Breckman, 2005; Rust, 2007). The ostomate is also taught what is normal in respect of their stoma, for example in appearance and stomal output. Ostomates should also be taught to contact the stoma specialist nurse in the case of problems with the stoma, but in practice, it is often the community nurse that is contacted for problems when the ostomate is reviewed for another reason. While still in hospital, ostomates are also instructed on diet, but this may require further clarification postdischarge home. Prior to discharge, the ostomate should be provided with stock of appliances and accessories. Further supplies are available on prescription and then collected from the chemist or delivered by the chemist or a specialist delivery firm. This is generally arranged by the stoma specialist nurse for ostomates on discharge home from hospital. To avoid wastage of expensive appliances, ostomates should not collect large stockpiles as the shape of the stoma changes post-discharge. In addition, supplies can be bulky and have a limited shelf life – although this is generally several years in length. Usually one to two months’ supplies are adequate to be kept at home and re-ordered each month. The prescription should be reviewed periodically to ensure that products are being used, and are useful and appropriate. Stoma care at home Once the ostomate is discharged home, the actual learningto-live-with-the-stoma process begins. All advice is general and may need to be specifically tailored for the individual ostomate. If in doubt, the stoma specialist nurse can be contacted for further advice by the community nurse or the ostomate. Some ostomates have problems adjusting to life with a stoma and the community nurse will possibly be the person contacted or who notices the problem. It is ideal when visiting and assessing an ostomate in the community to try and ensure that holistic care is provided. However, this is not always easily achieved when there are limited resources and a lack of familiarity with stoma care can result in caution on behalf of the nurse. In a study by Williams et al (2010), it was discovered that 54% of ostomates experienced at least two stoma problems on a regular basis. Areas that are likely to concern ostomates British British Journal Journal of Community of Community Nursing Nursing Vol Vol 16, ?, NoNo 8 CLINICAL FOCUS in the community are varied but may include: wAppliances and accessories wDiet wResuming normal life wSore skin wPsychological issues. Appliances and accessories: correct usage There are a multitude of stoma accessories that are used in conjunction with stoma appliances. These are available on prescription. Accessories can be used to prevent leaks, to remove adhesive and to protect the peristomal skin. The nurse needs to carefully assess the situation to ascertain whether accessories are necessary, and if so, that accessories are used correctly. While it is important not to waste products, as they are expensive, it is also necessary to provide the ostomate with a secure appliance that does not leak. Following a careful assessment by the community nurse, it still might be necessary to refer to the stoma specialist or stoma care nurse (available in the local district hospital), but it is possible to resolve some situations in the community setting. Often the community nurse can guide the ostomate on the correct usage of stoma products and educate them as necessary. Sore skin is a likely reason for the ostomate to contact the community nurse. For an example of a patient assessment, see Box 1. The assessment should include: wStoma type? wStomal output? wDoes the appliance leak? wWhere does the appliance leak? wWhat length of time have the leakages/problems been occurring? wIs there a specific occasion that leads to leakage, e.g. when in bed asleep? wThe appearance of the peristomal skin (skin around the stoma) wskin colour? wany breaks? wextent of skin damage? wAny recent changes that might have contributed to the problem? Leakage prevention The community nurse might assess the ostomate and discover a leaking appliance. In this situation, accessories that might be useful include seals (also termed washers; examples include Dansac GX-tra Seals, Coloplast mouldable rings or Salts Healthcare secuplast mouldable seals), filler paste (available in tubes or strips) and belts. Seals and filler paste can be used to ‘fill’ skin dips or creases and are used under the flange (Burch and Sica, 2008). A seal is circular in shape and this can be used directly around the stoma or broken into pieces to fill creases. Filler paste can be used in the same way. A belt can be used to more securely hold the appliance to the abdomen. There British Journal of Community Nursing Vol 16, No 8 Box 1. Stoma care case study A 70-year-old man with a temporary ileostomy formed 3 weeks ago is being reviewed by the community nurse for an unhealed surgical wound. He reports soreness around his stoma. On examination there is a 1cm ring of minimally red, broken skin directly around the ileostomy. On questioning the ileostomy output is a porridge-like in consistency, the appliance does not leak, the soreness has been felt for about one week, there is discomfort when changing the appliance and then again in the evening after the appliance is replaced. Nothing has changed that he can think of; in fact the faeces have thickened slightly as he is now eating more food. The community nurse when removing the appliance noticed that the hole in the middle of the flange was considerably larger than the ileostomy size. The community nurse assessed the problem to be due to cutting the flange aperture too large. The nurse planned to re-measure the stoma and re-size the aperture and re-teach as necessary and not to use any accessories in the first instance, with review in three days. On examination at the next visit the skin was healed and the ostomate reported feeling more comfortable. are often small loops on the edge of the flange and these belt hooks are used to attach the belt to the appliance. Adhesive removers Adhesive removers such as CliniMed Appeel, or Opus Healthcare’s Lift, which are available in wipes and sprays, can help remove appliances. Caution should be used with adhesive removers which contain alcohol as this can sting broken peristomal skin. For ostomates with fragile or damaged skin, an adhesive remover can reduce any trauma or pain associated with appliance removal. Another use for adhesive removers is to remove the adhesive left on the abdomen by the appliance.This can collect the fluff from clothes and leave an unsightly ring on the abdomen. For people with sensitive skin, it might be better to use a damp cloth to assist in appliance removal. Instead of an adhesive remover, a small amount of soap can be used to remove residual adhesive but this can dry the skin so it is not generally advocated and must be carefully cleaned off the skin (Burch and Sica, 2005). Skin protection Accessories can also be used to protect the peristomal skin. These are available as protective films such as Pelican protect and 3M Cavilon (Black, 2007), wipes or sprays and protective powder such as ConvaTec Orahesive powder, Hollister Premium powder. Peristomal skin might require a protective film if it is at risk of damage due to appliance leakage, for example, while the problem is in the process of being resolved. Broken peristomal skin might require protective powder to help to ‘dry’ and protect the skin prior to an appliance being adhered to the abdomen. Powder is most effective if minimally used, so that only a very fine coating is left on any broken areas of skin and none on the intact, healthy skin (Burch, 2008). Diet and stomas The community nurse is likely to be asked for advice regarding eating certain foods by an ostomate. In general, an ostomate can eat and drink as usual. However, in the 371 TOPIC HEA CLINICAL FOCUS first few months, foods may cause problems that might not occur subsequently. High fibre diets might not pass so simply through a newly formed, oedematous stoma for example. The general advice for all ostomates is to chew food well and to drink about 1.5-2 litres daily of fluids. Alcohol can be taken in moderation but might loosen the stomal output (Pearson, 2008). A colostomate (person with a colostomy) after an initial period can eat and drink anything. There is a risk of constipation so the community nurse can provide dietary advice to prevent this. It should be noted that oral laxatives can be used with effect if dietary manipulation does not work. Although suppositories and enemas can be used, they are prone to leak out of the colostomy before being effective. Advice can be sought from the stoma care nurse. An ileostomate (person with an ileostomy) can after an initial period of about 6–8 weeks, also eat and drink most foods. Some ileostomates can tolerate all diet while others find they do not tolerate certain foods. Foods that tend to be less well-tolerated are those that are high in fibre, as these can cause loose stool for some ileostomates. Poorly chewed food can cause a food bolus blockage. This is reported by the ileostomate as abdominal discomfort and nil via the ileostomy. A blockage often simply resolves by stopping eating and increasing oral fluids until the blockage resolves and the ileostomy starts to function again. If this method does not resolve the blockage, intravenous fluids and a nasogastric tube in hospital are generally necessary. The stomal output is looser in general than it is prior to the operation, thus there is a loss of fluid in the loose stool, making it essential that ileostomates have at least 1.5 litres daily. There is also a loss of sodium, so a little bit of salt added to meals daily is often advocated, unless there is an already high dietary salt intake by the ileostomate (Pearson, 2008). Finally, a urostomate (person with a urostomy) is likely to have a bowel disturbance initially following surgery, as a segment of bowel is used to form the urostomy. This generally resolves in hospital but food should be well-chewed prior to swallowing for a few weeks post-discharge home. It is essential that urostomates drink well. Some find that a glass of cranberry juice taken each day can keep the urine clear and the mucous levels down. Resuming a normal lifestyle The community nurse may have several visits with a patient after discharge from hospital and in this period of recovery, it can be difficult for the ostomate to know how well they are recovering and when they can resume a normal lifestyle. In general, ostomates are encouraged to get up and dressed each day. They are encouraged to mobilize as their tolerance allows, but outside is ideal if the weather is good and there are no contraindications to this. It is normal to get easily tired in the initial post-discharge period and rest as needed. It is also advised not to undertake heavy lifting or activities for 3 months after surgery. Eating can often be better tolerated in the post-discharge 372 period if it is little and often, ensuring a balanced diet to aid healing. Long term, the advice is as above. Resuming driving is variable; patients who had laparoscopic surgery are likely to be able to start this sooner than ostomates with the larger laparotomy wounds. It is important to ensure the insurance company is in agreement then, it is usual to start driving once an ostomate is confident with walking and their strength has increased to allow them to perform an emergency stop if needed. This is usually a minimum of 2 weeks after discharge home but can be considerably longer. Sexual relationships can be resumed once the ostomate is comfortable. For men who have had a urostomy, there may be sexual problems such as erectile dysfunction and these need to be discussed with the urologist. For women that have had their rectum removed, there may be a change in the angle of the vagina, potentially making intercourse uncomfortable in certain positions. It is possible to have children, whichever partner has a stoma, and precautions need to be taken if this is not desired. Concerns of the ostomate can include embarrassment at potential sounds or worry about appliance leakage (Ayaz and Kubilay, 2008) and advice can be to ensure that the appliance is emptied (if appropriate) and secure before starting sexual relations. Interestingly, the support of having a good relationship is beneficial to recovery (Nichols and Riemer, 2008). Work and exercises can be resumed quickly after discharge home but not for all ostomates. Heavy jobs may not be resumed for up to 3 months to allow the wound to ‘mature’ and strengthen. Heavy exertion may result in an incisional or parastomal hernia (Thompson and Trainor, 2007). These are swellings on the incision sites or around the stoma respectively. Prevention can include the use of a hernia support belt in conjunction with abdominal exercises, which the stoma care nurse can advise upon. Walking is advised during hospitalization and therefore, from the day of discharge. Holidays in Britain or abroad can be taken. The general advice is to take more than the number of appliances used in the same period, twice as many as usual is advocated. Also, if the ostomate is flying, they should have their appliances in their hand luggage in case of lost luggage. It is recommended to see the stoma specialist nurse for travel advice. Psychological issues Although in general most ostomates seem to cope well with their stoma, some can have problems adjusting to it. It has been suggested that the initial phase of adjustment is very important (Bossom and Beard, 2009). Issues can include problems with the way the individual perceives what they look like to others, although many ostomates wear tight-fitting clothes without the stoma being visible. Others worry about issues such as sex (Simmons, 2008). On some rare occasions, ostomates require more intensive treatment for these issues such as sessions with a counsellor. There are also support groups available nationally and often locally (Hulme and Brierley, 2007). The community nurse can alert the general practitioner if psychological issues are suspected to be a problem. British Journal of Community Nursing Vol 16, No 8 CLINICAL FOCUS ADER Conclusion In summary, the community nurse should provide holistic care to ostomates, even if the primary reason for the contact is not the stoma. There can be a number of ways in which the community nurse can assist; this can include advice about stoma appliances or accessories and their correct usage. Nurses can also give advice on postoperative recovery including normal expectations, which include resumption of activities following discharge home from hospital. Although advice in general works for all ostomates, a young person is likely to regain strength faster than an older one. If further assistance is necessary by the nurse or the ostomate, the stoma specialist nurse can be contacted in the local hospital for advice. BJCN Ayaz S, Kubilay G (2008) Effectiveness of the PLISSIT model for solving the sexual problems of patients with stoma. J Clin Nurs 18: 89–98 Black P (2007) Peristomal skin care: an overview of available products. Br J Nurs 16(17): 1048–56 Bossom C, Beard J (2009) Two approaches to sharing stoma care expertise with non-specialist nursing staff. Gastrointest Nurs 7(2): 42–7 Breckman B (2005) Stoma care and rehabilitation. Elsevier Churchill Livingstone, London Burch J (2008) Complications. In: Burch J (ed) Stoma care. Wiley-Blackwell, West Sussex Burch J, Sica J (2008) Common peristomal skin problems and potential treatment options. Br J Nurs 17(17): S4–S11 Colwell JC, Gray M (2007) Does preoperative teaching and stoma site marking affect surgical outcomes in patients undergoing ostomy surgery? J Wound Ostomy Continence Nurs 34(5): 492–6 Cronin E (2008a) A guide to the appropriate use of convex stoma care products. Gastrointest Nurs 6(2): 12–16 Cronin E (2008b) Colostomies and the use of colostomy appliances. Br J Nurs 17(17): S12–S19 British Journal of Community Nursing Vol 16, No 8 LEARNING points w A colostomy is the most common type of stoma, followed by ileostomy and urostomy w Stoma appliances are varied but essentially closed for a colostomy, drainable for an ileostomy and drainable with a tap or bung for a urostomy w Community nurses should aim to give holistic care when with their stoma patients w Concerns about diet, sore skin and resuming lifestyles are common for people with a stoma once discharged home from hospital Fulham J (2008) A guide to caring for patients with a newly formed stoma in the acute hospital setting. Gastrointest Nurs 6(8): 14–23 Hulme E, Brierley R (2007) Living with a colostomy. Gastrointest Nurs 5(2): 22–4 IMS (2007) New Stoma Patient Audit GB – August 2007 Nazarko L (2008) Caring for a patient with a urostomy in a community setting. Br J Community Nurs 13(8): 354–61 Nichols TR, Riemer M (2008) The impact of stabilizing forces on postsurgical recovery in ostomy patients. J Wound Ostomy Continence Nurs 35(3): 316–20 Pearson M (2008) Nutrition. In: Burch J (ed) Stoma care. Wiley-Blackwell, West Sussex Rust J (2007) Care of patients with stomas: the pouch change procedure. Nurs Stand 22(6): 43–7 Simmons KL (2008) Improving stoma surgery outcomes: more patient choice, more psychological support. Gastrointest Nurs 6(4): 21–5 Thompson MJ, Trainor B (2007) Prevention of parastomal hernia: a comparison of result 3 years on. Gastrointest Nurs 5(3): 22–8 Trainor B, Thompson MJ, Boyd-Carson W, Boyd K (2003) Changing an appliance. Nurs Stand 18(13): 41–2 Williams J, Gwillam B, Sutherland et al (2010) evaluating skin care problems in people with stomas. Br J Nurs 19(17): S6–S15 Williams J (2006) Stoma care part 1: choosing the right appliance. Gastrointest Nurs 4(6): 16–19 373 Copyright of British Journal of Community Nursing is the property of Mark Allen Publishing Ltd and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.