Mapping England`s Health and Wellbeing Boards
advertisement

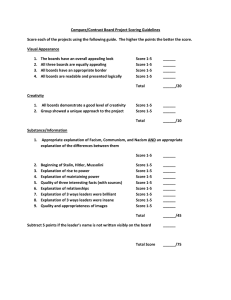
Mapping England’s Health and Wellbeing Boards’ vision for dying people What we did Hospice UK conducted research during April-May 2014 to assess the extent to which England’s 152 Health and Wellbeing Boards (hereafter ‘boards’) consider the needs of local people approaching the end of life in Joint Health and Wellbeing Strategies (JHWSs). Our research used methodology developed by the National Council for Palliative Care (NCPC) in its report published in 20121. The methodology included a red, amber and green (RAG) rating of boards based on the attention they gave to end of life care in their JHWSs. What we found2 Green – 43% (65/152) of boards have explicitly considered the needs of dying people. In 2012 25% (38/152) of boards had explicitly considered the needs of dying people. Amber – 26% (40/152) of boards have considered related issues to relevant groups without explicitly mentioning end of life care. In 2012 10% (15/152) of boards considered related issues without mentioning end of life care. Red – 24% (37/152) of boards failed to mention either directly or indirectly people approaching the end of life. In 2012 20% (30/152) of boards failed to mention people approaching the end of life. Unpublished – 7% (10/152) of boards failed to publish a strategy or make one publicly available. In 2012 45% (69/152) of boards failed to publish or make one publicly available. What we recommend All boards explicitly consider the needs of dying people in their JHWSs to bring health, social care and public health systems together in response to the increasingly complex comorbidities of our ageing population. All boards should utilise the data produced by Public Health England on end of life care needs and outcomes to inform their JHWSs. All boards should work with hospices and palliative care providers as well as with patient and community groups to co-produce JHWSs. All boards should make their JHWSs publicly available to foster local accountability and transparency. 1 Does dying matter to England’s new health and wellbeing boards? The National Council for Palliative Care [accessed 3 June 2014] http://www.ncpc.org.uk/news/half-new-nhs-boards-ignoring-end-life-care 2 The information was correct on the date of publication. Company Limited by Guarantee, Registered in England and Wales No. 2751549, Charity registered in England and Wales No. 1014851 and in Scotland No. SC041112. VAT No. 731 304476, registered office as above. Full report Introduction The Health and Social Care Act 2012 established Health and Wellbeing Boards (hereafter ‘boards’) as new statutory committees of upper-tier local authorities in England. The membership of boards must include representatives from Clinical Commissioning Groups, the local authority and local Healthwatch, but other people can be invited onto the board. Boards must undertake a Joint Strategic Needs Assessment (JSNA) to identify the needs of the local population. A Joint Health and Wellbeing Strategy (JHWS) is then developed by boards to set out recommendations for how the local population’s needs should be met by commissioners. Through these documents it is hoped boards will be able to shape commissioning and drive the integration of health, social care and public health services to better meet the needs of local people. What are JSNAs and JHWSs? Health and Wellbeing Boards are required to complete a Joint Strategic Needs Assessment (JSNA) – a comprehensive assessment of current and future needs of the local population relevant to health, social care and public health across the full life course, covering children, young people and adults. JSNAs provide a foundation for the production of a Joint Health and Wellbeing Strategy (JHWS) – a strategy to shape and support the decisions of local service leaders and commissioners to inform service planning across health, social care and public health. The Department of Health stated in its explanatory note that: “The joint health and wellbeing strategy is a unique opportunity for the health and wellbeing board members to explore together the local issues that they have not managed to tackle on their own.” End of life care Boards present an opportunity to secure an integrated approach to supporting people approaching the end of life. Hospice UK and the NCPC believe that all boards should have a concern for end of life care because: Evidence suggests that between 92,000 and 142,500 dying people have unmet care needs.3 Evidence suggests that the number of dying people is set to increase sharply over the next 30 years and that they will have more complex care needs.4 A key characteristic of a ‘good’ death is integrated care which can be achieved, in part, by giving priority to end of life care at a strategic level to send clear signals to commissioners and providers. Evidence suggests that improving end of life care can save commissioners and public money.5 6 3 Final Report, Palliative Care Funding Review [accessed 3 June 2014] https://www.gov.uk/government/publications/independent-palliativecare-funding-review 4 Current and Future Needs for Hospice Care: An Evidence Based Approach, Help the Hospices and King’s College London [accessed 3 June 2014] http://www.helpthehospices.org.uk/our-services/commission/resources/?entryid209=132678 2 Getting end of life care right continues to be a pressing issue, due to the country’s ageing population, and as boards have the potential to drive change Hospice UK decided to repeat research conducted by the NCPC in 2012. The research aims to track whether dying people and end of life care is a priority for boards, and to compare findings with those from 2012. What are Health and Wellbeing Boards (HWBs)? The Health and Social Care Act 2012 established local HWBs as a new statutory committee of every upper-tier local authority in England. They are designed to bring together key leaders from the health and care system to work together to improve the health and wellbeing of their local population, promote the integration of services, and reduce health inequalities. Methodology We used a list of 152 upper-tier local authorities which the NCPC established in 2012. The list was cross-referenced with The King’s Fund Health and Wellbeing Board Directory7 and the Local Government Association’s (LGA’s) Health and Wellbeing Board priority map 8. An internet search was carried out for the terms ‘health and wellbeing board’, ‘health and wellbeing board consultation’ and ‘health and wellbeing strategy’ for each of the identified upper-tier authorities. The search was conducted in August 2014. Each JHWS was searched for references to ‘end of life care’. Depending on the outcome local authorities were categorised using a traffic light system developed by NCPC in 2012. The ratings correspond to the extent end of life care is mentioned in the JSWBs: Green The strategy explicitly mentions people approaching the end of life or end of life care services. Strategies in this category may make brief or detailed mentions. Amber The strategy considers related issues or groups for whom end of life care is particularly relevant e.g. older people. Strategies in this category do not have to mention end of life care directly. Red The strategy does not directly or indirectly consider end of life care or end of life care services. Strategies in this category may make reference to the ageing population or older people but will not include further detail. 5 Understanding the Costs of End of Life Care in Different Settings, Marie Curie Cancer Care [accessed 3 June 2014] http://www.mariecurie.org.uk/en-gb/healthcare-professionals/commissioning-services/publications/?Tab=1 6 End of Life Care: Improving While Saving Money, Healthcare at Home [accessed 3 June 2014] http://www.hah.co.uk/media-centre/successstories/201 7 Health and Wellbeing Board Directory, The King’s Fund [accessed 3 June 2014] http://www.kingsfund.org.uk/projects/health-and-wellbeingboards/hwb-map 8 Health and Wellbeing Priority Map, the Local Government Association [accessed 3 June 2014] http://www.local.gov.uk/health-and-wellbeingboards/-/journal_content/56/10180/6111055/ARTICLE 3 Findings We found some positive trends in the attention that boards have given to the end of life care needs of local people in their JHWSs. Overall, we were able to find JHWSs for 142 boards out of 152 which we welcome, as almost half of all boards had failed to publish a strategy in 2012. We call on the 10 boards that have not published their strategies to do so at the earliest opportunity. The number of boards with a green-rated JHWS is now 65, up from 38 in 2012. The percentage of boards with a green-rated strategy now stands at 43% compared with 25% in 2012. The number of amber-rated strategies has also increased and now stands at 40 boards compared with only 15 in 2012. The percentage of boards with an amber strategy is 26% compared with 20% in 2012. Unfortunately, we found 37 boards with a red strategy, which is an increase on the 30 boards that were identified in this category in 2012. This means that 24% of boards have a red-rated strategy compared with 20% of boards in 2012. 80 70 Comparison of Board attention to end of life care in JHWSs # of Boards 60 50 Green 40 Amber Red 30 Unpublished 20 10 0 2014 2012 Year research conducted 4 Green – 65 Barnet, Barnsley, Barking and Dagenham, Bath and North East Somerset, Bedford, Bolton, Bristol, Bromley, Bury, Cambridgeshire, Cheshire and West Chester, Croydon, Cumbria, Derby, Derbyshire, Devon, Doncaster, Dorset, Durham, East Riding of Yorkshire, East Sussex, Essex, Haringey, Harrow, Havering, Hertfordshire, Hillingdon, Hounslow, Kent, Kingston, Knowsley, Leicester City, Leicestershire, Merton, Milton Keynes, Northamptonshire, Portsmouth, Redbridge, Rutland, Salford, Sandwell, Sefton, Solihull, Southampton, Southendon-Sea, South Gloucestershire, Staffordshire, Stockport, Stockton-On-Tees, St Helens, Swindon, Tameside, Thurrock, Torbay, Tower Hamlets, Trafford, Waltham Forest, Warrington, Warwickshire, West Berkshire, Westminster, Wiltshire, Wolverhampton, Worcestershire, York. Amber – 40 Blackburn and Darwen, Blackpool, Bournemouth and Poole, Brighton and Hove, Calderdale, Central Bedfordshire, Cheshire East, Coventry, Ealing, Gateshead, Hampshire, Hartlepool, Hull, Isle of Wight, Islington, Lancashire, Leeds, Lincolnshire, Luton, Manchester, Medway, Newham, Norfolk, North Tyneside, Northumberland, North Yorkshire, Nottingham City, Nottinghamshire, Oldham, Richmond, South Tyneside, Shropshire, Southwark, Stoke on Trent, Suffolk, Surrey, Wakefield, Walsall, Windsor and Maidenhead, Wokingham. Red – 37 Bradford, Brent, Buckinghamshire, Camden, City of London, Cornwall, Darlington, Dudley, Enfield, Gloucestershire, Hackney, Halton, Hammersmith and Fulham, Isles of Scilly, Kensington and Chelsea, Kirklees, Lambeth, Lewisham, Liverpool, Middlesbrough, Newcastle, North East Lincolnshire, North Lincolnshire, Oxfordshire, Peterborough, Reading, Redcar and Cleveland, Rochdale, Rotherham, North Somerset, Sheffield, Slough, Sutton, Telford and Wrekin, Wandsworth, West Lindsey, West Sussex. Unpublished – 10 Bexley, Birmingham, Bracknell and Ascot, Greenwich, Herefordshire, Plymouth, Somerset, South Kent Coast, St Albans, Wigan. 5 Conclusions The trends that we have uncovered in our research are promising, with more strategies published and much greater attention given to the end of life care needs of people by boards across England. However, more needs to be done to by boards to secure strategies that are can be used as robust tools to support local service leaders and commissioners to inform service planning. This is an essential step as the hallmark of great end of life care and a ‘good’ death is integrated care. Boards and strategies have a role to play in securing improvements in end of life care for people across England and providing dying people with greater choice and control over their place of care and death. Recommendations All boards explicitly consider the needs of dying people in their JHWSs to bring health, social care and public health systems together in response the increasingly complex comorbidities of our ageing population All boards should utilise the data produced by Public Health England on end of life care needs and outcomes to inform their JHWSs. All boards should work with hospices and palliative care providers as well as with patient and community groups to co-produce JHWSs. All boards should make their JHWSs publicly available to foster local accountability and transparency. About us Hospice UK is the national charity for hospice care. We champion and support the work of more than 220 member organisations, which provide hospice care across the UK, so that they can deliver the highest quality of care to people with terminal or life limiting conditions, and support their families. Hospice UK is a registered charity in England and Wales number 1014851 and a company limited by guarantee number 2751549. Visit www.hospiceuk.org for more information. The National Council for Palliative Care (NCPC) is the umbrella charity for all those involved in palliative, end of life and hospice care in England, Wales and Northern Ireland. We believe that everyone approaching the end of life has the right to the highest quality care and support, wherever they live, and whatever their condition. NCPC is a registered charity number 1005671 and a company limited by guarantee number 2644430. Visit www.ncpc.org.uk for more information. Acknowledgements This report was written by Robert Melnitschuk, Policy and Advocacy Manager at Hospice UK, with help from Rob Micklewright and Katy Corner who contributed to the production of this report as policy and advocacy interns at Hospice UK. We are also indebted to the earlier work of our colleagues at NCPC who established the methodology and benchmark data in their 2012 report. For further information For further information about this work please email policy@hospiceuk.org or call 020 7520 8200. 6