Effects of Metoprolol CR in Patients With Ischemic and
Dilated Cardiomyopathy
The Randomized Evaluation of Strategies for Left Ventricular
Dysfunction Pilot Study
The RESOLVD Investigators*
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Background—Metoprolol provides clinical benefits in patients with congestive heart failure (CHF). In this study, we
investigated the effects of controlled-release metoprolol (metoprolol CR) on clinical status, on left ventricular (LV)
volumes and function, and on neurohumoral activation in a large number of patients with CHF of mixed causes.
Methods and Results—Four hundred twenty-six patients with symptomatic CHF were randomized to receive metoprolol
CR or placebo for 24 weeks. Metoprolol CR did not affect 6-minute walk distance, New York Heart Association
functional class, or quality of life. However, there was a significant improvement in measures of LV function with an
attenuation in the increase in LV end-diastolic (⫹23⫾65 mL [placebo] versus ⫹6⫾61 mL, P⫽0.01) and LV
end-systolic (⫹19⫾55 mL [placebo] versus ⫺2⫾51 mL, P⬍0.001) volumes after 24 weeks of therapy. LV ejection
fraction was unchanged (⫺0.05% or ⫺0.005) in the placebo group but increased by 2.4% in the metoprolol CR–treated
patients (P⫽0.001). Patients receiving metoprolol CR had a greater decrease in angiotensin II (P⫽0.036) and renin
(P⫽0.032) levels but an increase in N-terminal atrial natriuretic peptide and brain natriuretic peptide levels (P⬍0.01).
There were fewer deaths in the group receiving -blockers (3.4% versus 8.1%), and there was a similar number of
patients experiencing the composite outcomes of death or any hospitalization.
Conclusions—When added to ACE inhibitors, angiotensin II receptor antagonists, or both, the use of metoprolol CR
improves ventricular function, reduces activation of the renin-angiotensin systems, and results in fewer deaths.
(Circulation. 2000;101:378-384.)
Key Words: heart failure 䡲 receptors, adrenergic, beta 䡲 hormones 䡲 ventricles
dditional clinical benefits are provided by -adrenergic
blockers when administered in addition to ACE inhibitors.1–9 The recently presented Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERITHF) reported a significant beneficial effect of metoprolol CR
on survival rates in patients with congestive heart failure
(CHF) caused by both idiopathic dilated cardiomyopathy
(IDC) and ischemic cardiomyopathy. However, only 1 small
study evaluated the effects of metoprolol on left ventricular
(LV) volumes and function in patients with chronic ischemic
cardiomyopathy,10 and an extensive assessment of neurohormones has not been performed in any large trial of the use of
metoprolol in patients with CHF of mixed causes.
The Randomized Evaluation of Strategies for Left Ventricular Dysfunction (RESOLVD) Pilot Study represents one of
the largest studies conducted of the use of metoprolol in
patients with CHF of mixed causes who were receiving either
angiotensin receptor blockers (ARBs), ACE inhibitors, or a
combination. The objectives of stage II of the RESOLVD
Pilot Study were to comprehensively evaluate the effects of
A
the administration of metoprolol CR in addition to candesartan, enalapril, or the combination of candesartan and enalapril
on tolerability, 6-minute walk distance, ventricular volumes
and function, neurohumoral parameters, quality of life, and
New York Heart Association (NYHA) functional class in a
broad population of patients with CHF that included individuals with either ischemic or nonischemic cardiomyopathy.
Methods
The RESOLVD Pilot Study was a randomized double-blinded trial
of various therapeutic options in patients with CHF that consisted of
a 3⫻2 partial factorial design with a 2-stage randomization. In stage
I, patients were randomized to receive candesartan at 1 of 3 dosage
levels (4, 8, or 16 mg/d), 20 mg/d enalapril, or the combination of
candesartan (4 or 8 mg) and enalapril (20 mg) for a period of 17
weeks. In stage II, eligible patients were randomized to receive 200
mg/d metoprolol CR or placebo and followed for an additional 24
weeks.11
To be eligible for entry into the RESOLVD Pilot Study, patients
had to have symptomatic CHF (NYHA II to IV), a 6-minute walk
distance of ⬍500 m, and an LV ejection fraction (EF) of ⬍40%.
Received April 19, 1999; revision received August 25, 1999; accepted September 7, 1999.
*For a complete list of the members of the Writing Committee, please see the Appendix.
Correspondence to Project Office, Canadian Cardiovascular Collaboration, 2nd Floor, McMaster Clinic, 237 Barton St E, Hamilton, Ontario L8L 2X2,
Canada.
© 2000 American Heart Association, Inc.
Circulation is available at http://www.circulationaha.org
378
The RESOLVD Investigators
Metoprolol CR in Congestive Heart Failure
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Patients with chronic heart failure from any cause were allowed in
the trial. The cause of heart failure was determined by the investigators based on clinical judgment. The primary objective of stage II
of the RESOLVD Pilot Study was to determine the efficacy and
safety of the administration of the new controlled-release formulation of metoprolol (metoprolol CR) in addition to the stage I study
medication in terms of 6-minute walk distance and neurohumoral
parameters. The primary safety end point was a combination of
adverse events (defined as symptomatic hypotension, worsening of
CHF, and symptomatic bradycardia) and tolerability (proportion
of patients who did or did not reach their assigned target dose, plus
those who discontinued their assigned treatment). The secondary
objectives were to determine the effects of the combination of
metoprolol CR with stage I medications on ventricular volumes and
function, NYHA functional class, and quality of life. All patients
signed informed consent, and the protocol was approved by the
ethics committees of all of the investigators involved in the study.
At the end of stage I (week 17), all patients eligible for stage II
received 12.5 mg metoprolol CR once daily for 1 week (run-in
period). If they tolerated this dose, the patients were randomized to
receive either 25 mg metoprolol CR once daily or placebo. The dose
of metoprolol was increased gradually every 2 weeks to a maximum
dosage of 200 mg metoprolol CR daily in the following steps: 50, 75,
100, and 200 mg/d. Dosage reduction or delayed up-titration of
metoprolol CR was allowed at any time. The total follow-up from the
time of randomization into stage II until the end of the study was 24
weeks. Heart rate, blood pressure, biochemical and neurohumoral
parameters, 6-minute walk distance, quality of life (assessed with the
use of the Minnesota Living With Heart Failure questionnaire),
NYHA functional class, and quantitative radionuclide ventriculography were obtained during the week before the run-in period (end of
stage I) and at the end of the study.
TABLE 1.
379
Baseline Demographics and Patient Characteristics
Placebo
(n⫽212)
Age, y⫾SD
61⫾11
Metoprolol CR
(n⫽214)
62⫾12
Sex (male), n (%)
180 (85)
170 (79)
Ethnicity (white, European descent), n (%)
182 (86)
189 (88)
7–12 mo
26 (12)
27 (13)
⬎12 mo
185 (88)
188 (87)
132 (63)
139 (65)
Hypertension, n (%)
72 (34)
81 (38)
Diabetes, n (%)
50 (24)
58 (27)
Time with CHF, n (%)
Previous myocardial infarction, n (%)
Smoker, n (%)
Former
Never
Cause (ischemic), n (%)
34 (16)
30 (14)
126 (59)
134 (63)
52 (25)
50 (23)
146 (69)
149 (69)
NYHA class, n (%)
I
19 (9)
10 (5)
II
138 (65)
157 (73)
III
54 (26)
46 (21)
0 (0)
2 (1)
0.29⫾0.11
0.28⫾0.11
6-min walk, m
399⫾85
398⫾84
Digoxin, n (%)
146 (69)
139 (65)
Neurohumoral Analyses
Diuretics, n (%)
175 (83)
181 (84)
Blood samples were drawn after an overnight fast and 30 minutes of
rest in the supine position. Norepinephrine, epinephrine, and dopamine were measured with HPLC, whereas angiotensin II, aldosterone, and endothelin I were measured with radioimmunoassay.12,13
Both N-terminal proatrial natriuretic peptide (pro-ANP) and brain
natriuretic peptide (BNP) were measured in Oslo, Norway, with the
use of previously reported techniques.14,15 The neurohumoral data
for our study population were compared with those for aged-matched
healthy volunteers without cardiac disease, from whom blood samples were taken at 1 Italian center and 4 Canadian centers.
Nitrates, n (%)
66 (31)
83 (39)
Receiving candesartan, n (%)
84 (40)
96 (45)
Receiving enalapril, n (%)
41 (19)
30 (14)
Receiving combination, n (%)
86 (41)
89 (41)
Statistical Analyses
All analyses were performed on an intention-to-treat basis. ANOVA
was used to examine the efficacy of the administration of metoprolol
CR in addition to candesartan/enalapril on exercise tolerance, ventricular function, neurohormonal parameters, systolic and diastolic
blood pressures, and resting heart rate. Clinical events, NYHA
functional class, and quality of life were analyzed using the MantelHaenszel test. Data not distributed normally (eg, for neurohormones)
were log transformed before statistical comparisons were made. All
data are presented as mean⫾SD.
Results
Baseline Demographics and Patient Characteristics
Of the 768 patients randomized to stage I of the study, 426
were randomized to stage II. Four hundred sixty-eight patients were entered in the run-in period, but 52 (11%) were
not randomized because of poor adherence (n⫽7), patient
refusal (n⫽4), adverse events (n⫽24; 5%), and other exclusion reasons (n⫽17). Of the 24 patients who developed
adverse events and were not randomized into stage II, 7
patients experienced symptoms and signs of worsening heart
failure, 10 patients complained of nonspecific cardiac or
respiratory symptoms, 4 patients presented with abdominal or
IV
LVEF
n⫽426.
chest discomfort, 1 patient died suddenly, and 2 patients were
not randomized due to unknown reasons. The remaining 426
patients were randomized to receive metoprolol CR or to
placebo. Three hundred forty-two patients randomized in
stage I were not offered randomization into stage II because
of contraindication to -blocker, ongoing treatment with
-blockers, or unwillingness to pursue the second stage of the
trial. The 342 patients in stage I who were not offered
randomization into stage II were continually followed up at
8-week intervals. End point assessments were also made and
collected. Because of the early termination of the study, 29
(7%) patients were treated for ⬍24 weeks, and their duration
of follow-up was slightly reduced by a mean of 11⫾6 days.
For these patients, end point assessments were made at the
time of termination.
The clinical characteristics of patients randomized into
stage II are presented in Table 1. There were no significant
differences between the 2 groups. The percentage of patients
receiving the target dose of ACE inhibitors, candesartan, or
both was ⱖ85% at the time of randomization into phase II,
with the highest group being the group treated with candesartan or enalapril alone (91% to 95%) and the lowest being
the group treated with high-dose enalapril and candesartan
(85%).
380
TABLE 2.
Circulation
February 1, 2000
Effects of Metoprolol CR and Placebo on Neurohumoral Activation
Placebo
Metoprolol CR
Control
Subjects
Baseline
24 wks
⌬
Baseline
24 wks
⌬
P ⌬ Placebo vs
⌬ Metoprolol
299⫾109
404⫾220
351⫾200
⫺54⫾189
411⫾211
341⫾209
⫺69⫾223
0.19
(42)
(175)
(161)
(175)
(n⫽168)
Epinephrine, pg/mL
42.3⫾24.0
50.5⫾49.4
41.7⫾28.5
⫺6.4⫾98.3
0.671
(42)
(137)
(126)
Dopamine, pg/mL
42.1⫾28.8
52.3⫾45.1
128⫾80
⫹67.2⫾69.7
0.62
(42)
(136)
(126)
Plasma renin, ng/mL
4.6⫾4.1
165⫾132
182⫾138
⫺54⫾137
0.032
(17)
(38)
(35)
Angiotensin II, pg/mL
21.2⫾11.1
35.9⫾38.7
39.9⫾44.7
⫺4⫾26.6
0.036
(40)
(177)
(159)
Aldosterone, pg/mL
60.7⫾36.3
105⫾110
128⫾121
(41)
(177)
(161)
Endothelin, pg/mL
1.16⫾0.32
2.4⫾2.7
2.5⫾3
(40)
(178)
(162)
Pro-ANP, pmol/mL
495⫾239
1320⫾1029
1311⫾936
(42)
(178)
(161)
BNP, pmol/mL
6.73⫾5.26
39.2⫾47.2
40.3⫾48.7
(42)
(178)
(161)
Norepinephrine, pg/mL
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
⫺8.3⫾55.9
57.6⫾76
(145)
(n⫽139)
⫹72⫾77
57.3⫾535
124⫾53
(145)
(n⫽139)
⫹5⫾69
147⫾132
99⫾114
(30)
(29)
⫹2.1⫾43.6
34.3⫾27.6
30.9⫾30.4
(174)
(n⫽168)
⫹23⫾104
113⫾127
129⫾132
(n⫽177)
(n⫽169)
⫹0.1⫾2.4
2.4⫾3.4
2.2⫾2.3
(n⫽176)
(n⫽168)
⫺17⫾657
1363⫾1104
1587⫾1151
(n⫽177)
(n⫽168)
⫹2.0⫾31.2
42.7⫾54.7
54.2⫾61.1
(n⫽178)
(n⫽168)
51.6⫾57.6
⫹15⫾122
0.57
⫺0.2⫾2.4
0.116
⫹208⫾696
0.001
⫹11.3⫾41.5
0.002
Values are mean⫾SD for analyses performed on neurohormones computed on log scale.
Six-Minute Walk Distance and
Neurohumoral Parameters
Long-term administration of metoprolol CR did not cause any
change in the 6-minute distance walked (metoprolol CR
398⫾84 to 397⫾95 m, placebo 399⫾85 to 396⫾102 m).
This was also true for the group treated with candesartan
alone (⫺4.8⫾64 m), enalapril alone (⫺7.6⫾57.6 m), or the
combination of enalapril and candesartan (⫺1.9⫾58 m). In
addition, these were no significant changes when only patients with lower exercise capacity (⬍400 m) were considered (metoprolol CR 332⫾61 to 342⫾81 m, placebo 325⫾52
to 321⫾64 m; NS).
The effects of metoprolol on neurohumoral activation are
presented in Table 2. Metoprolol CR provided an additional
reduction in plasma renin and angiotensin II levels but did not
decrease the other neurohormones. Renin and angiotensin II
levels decreased to a similar extent in patients receiving
candesartan alone or the combination of candesartan plus
enalapril before the administration of metoprolol. Metoprolol
CR–treated patients exhibited a significant increase in both
N-terminal ANP and BNP.
Tolerability and Clinical Events
Metoprolol CR was as well tolerated as placebo at all titration
visits, with an overall discontinuation rate of 11% for patients
treated with metoprolol versus 12% for those treated with
placebo. The mean dose of metoprolol was 156⫾70 mg, and
81% of patients were receiving the maximal dose of metoprolol CR (200 mg/d). The mean time to maximum titration
was 93 days for the metoprolol group versus 85 days for the
placebo group (P⬍0.05). The overall compliance was excel-
lent, with only 7% of patients who were randomized to
receive metoprolol CR taking ⬍80% of their study medication, a rate similar to that for placebo (8%).
The tolerability and events related to metoprolol CR and
placebo are presented in Table 3. Patients receiving metoprolol CR had a trend toward fewer deaths (n⫽8, 3.7%)
compared with placebo (n⫽17, 8.1%). Sixteen patients died
suddenly without worsening CHF (metoprolol n⫽6, placebo
n⫽10), and 4 patients died suddenly with worsening CHF
(metoprolol n⫽1, placebo n⫽3). Other causes of death
included stroke (n⫽2), cancer (n⫽2), and myocardial infarction (n⫽1). The numbers of patients hospitalized or reporting
any serious adverse event were similar in the metoprolol CR
and placebo groups. There was an increase in hospitalization
rates for CHF in metoprolol CR–treated patients (n⫽15
[7.9%] versus n⫽5 [3.3%], 95% CI 1.01 to 5.63) that peaked
at 120 days. The hospitalized patients treated with metoprolol
CR exhibited similar clinical characteristics and LV volumes
and function at baseline as the other patients. However,
prerandomization angiotensin II levels were significantly
higher in patients who developed CHF while treated with
metoprolol (55.3⫾33.2 [CHF] versus 33.2⫹25 pg/mL [nonCHF], P⬍0.001). The number and profile of nonserious
adverse events, as well as the causes for the discontinuation
of study medication, were similar in the 2 groups.
Quality of Life, Functional Class, and
Hemodynamic and Cardiac Effects
Metoprolol CR caused no significant change in the quality of
life score or in NYHA functional class. Therapy with metoprolol CR caused no significant change in systolic or diastolic
The RESOLVD Investigators
TABLE 3. Deaths, Hospitalization, Serious Adverse Other Than
Clinical Events, Nonserious Adverse Events, Discontinuation,
Data on Symptomatic Hypotension, Worsening of CHF, and
Symptomatic Bradycardia in the Two Randomization Groups
Variable*
Deaths all-cause
Metoprolol CR
(n⫽214)
Placebo
(n⫽212)
95% CI for
Relative
Risk
8
17
34
36
0.60–1.42
CVD
25
19
0.73–2.27
CHF
15
5
1.09–7.96
7
16
0.18–1.02
Hospitalization all-cause
Non-CVD
0.20–1.05
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Other SAEs
31
31
0.62–5.34
Non-SAEs
137
134
0.62–1.55
Discontinuation
(tolerability)
24
22
䡠䡠䡠
Symptomatic
hypotension
4
1
䡠䡠䡠
Worsening of CHF
6
3
䡠䡠䡠
Symptomatic
bradycardia
0
0
䡠䡠䡠
Others
16
19
䡠䡠䡠
Back-titration
60
38
䡠䡠䡠
5
2
䡠䡠䡠
11
4
䡠䡠䡠
9
2
䡠䡠䡠
38
29
䡠䡠䡠
Permanent
discontinuation
24
25
䡠䡠䡠
Symptomatic
hypotension
4
2
䡠䡠䡠
Symptomatic
hypotension
Worsening of CHF
Symptomatic
bradycardia
Others
Worsening of CHF
7
5
䡠䡠䡠
Symptomatic
bradycardia
0
0
䡠䡠䡠
18
21
䡠䡠䡠
Others
CVD indicates cardiovascular disease; SAE, serious adverse event.
*Any report during the double-blind part of stage II.
blood pressure at the initiation of therapy or during the course
of the study. Metoprolol CR caused a decrease in heart rate of
⬇6 to 8 bpm once maximal doses were achieved. The
changes in blood pressure and heart rate were similar regardless of whether patients received candesartan, enalapril, or the
combination before randomization into phase II.
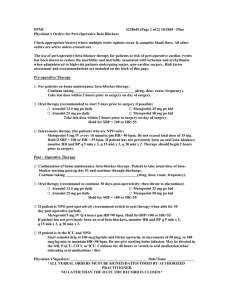
The effects of metoprolol and placebo on cardiac volume and function are presented in the Figure and Table 4.
Patients receiving placebo had no change in EF but
exhibited a significant increase in systolic and diastolic
ventricular volumes. In contrast, 24 weeks of treatment
with metoprolol CR significantly increased LVEF and
prevented the increase in end-systolic and end-diastolic
volumes. The effects of metoprolol on LV function and
volumes were significant and of similar magnitude in the
ischemic and nonischemic groups.
Metoprolol CR in Congestive Heart Failure
381
Discussion
Stage II of the RESOLVD Pilot Study is one of the largest
published randomized study of the use of metoprolol in
patients with CHF. The administration of metoprolol improved LV function and prevented LV dilatation but did not
result in significant improvements in symptoms, 6-minute
walk distance, or quality of life. In addition, despite the use of
an ACE inhibitor, ARB, or the combination in stage I,
metoprolol CR resulted in a further suppression of renin and
angiotensin II levels.
The CR formulation of metoprolol16 was used in patients
with CHF of mixed causes. Compared with the conventional
metoprolol tablet, the CR formulation has ⬇30% less bioavailability17; however, a dose of 200 mg of the CR formulation caused more pronounced -blockade than 150 mg of
the immediate-release formulation in patients with heart
failure. Metoprolol CR caused the expected decrease in heart
rate but no significant changes in systolic or diastolic blood
pressure. These findings are consistent with previous studies
showing no change in blood pressure after the first month of
the initiation of metoprolol.2,18,19 Despite a mean daily dose
of 160 mg metoprolol, heart rate decreased by only 6 bpm by
the end of the titration phase. This moderate decrease in heart
rate is less striking than previously reported with the use of
metoprolol in patients with more severe CHF caused by
dilated cardiomyopathy.2,19 However, the magnitude of decrease in heart rate reported in this study is similar to the
6.8-bpm decrease obtained with carvedilol in the Australia/
New Zealand Trial, which is a study of patients with less
severe heart failure and ischemic cardiomyopathy.6
The administration of metoprolol CR produced a significant 0.024 improvement in LVEF after an average of 6
months of therapy compared with no change (⫺0.05) in
patients treated with a placebo. The increase in LVEF is
slightly less than that reported in other studies of the use of
metoprolol and other -blockers but more than that reported
by Woodley et al20 on the use of bucindolol in patients with
ischemic heart failure. The reasons for this are not clear, but
because of the small sample size in many of these trials, it is
difficult to make conclusions regarding a lesser effect on EF
in the present study population of patients with CHF for
which the cause is in large part ischemic cardiomyopathy. In
addition to its significant effect on EF, metoprolol CR
prevented the increase in LV end-diastolic and end-systolic
volumes. These observations are in agreement with those of
Hall et al,18 who reported a favorable effect on LV volumes
after 3 months of therapy with metoprolol in patients with
CHF caused by IDC. Similar decreases in volumes have been
reported in the Australia/New Zealand Trial6 and with the use
of bucindolol in patients with ischemic heart failure.20 Accordingly, our data extend the available data on the beneficial
effect of metoprolol on LV geometry from a population with
IDC to a population with heart failure largely caused by
ischemic heart disease.
Metoprolol CR produced no change in NYHA functional
class, quality of life, or 6-minute walk distance. These results
are consistent with the heterogenous results reported in
various randomized trials, with some trials reporting a favorable effect,10 some reporting positive effects but after a longer
382
Circulation
February 1, 2000
Changes in LVEF and LV volumes in response to metoprolol (F) versus placebo (E). Data are mean⫾SEM.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
duration of treatment,2,8,21 and others reporting no sustained
benefit.6 The reason for the absence of consistent improvement in submaximal exercise capacity with the use of a
-blocker is likely multifactorial, but it is possible that the
short follow-up period may have played a role in the lack of
exercise effect. In addition, the SD for the 6-minute walk test
in this trial was 84 m, as opposed to the expected 39 m used
for sample size calculation.11 Such discrepancy likely contributed to a lack of power to detect differences between the
2 treatment arms.
In this study, metoprolol therapy caused no significant
change in plasma catecholamine levels but did cause a
decrease in renin levels, which is in agreement with previous
reports.18,22,23 A decrease in angiotensin II levels by the use of
a -blocker has been reported in normotensive and hypertensive subjects but not in patients with CHF.24 In fact, the
magnitude of suppression of angiotensin II by the short-term
TABLE 4.
use of nonselective or selective -adrenergic blockers appears to be comparable to the suppression provided by an
ACE inhibitor. Thus, our data confirm the efficacy of
-adrenergic blockade to decrease renin activity and angiotensin II levels when administered on a long-term basis in
patients with CHF who have already been treated with an
ACE inhibitor or an ARB. Nevertheless, the absence of a
decrease in aldosterone levels emphasizes the multifactorial
control of aldosterone secretion in patients with CHF. The
metoprolol CR–treated group experienced an increase in
N-terminal ANP and BNP levels at 6 months. There are little
data available regarding the effect of -blockers on natriuretic peptide levels in CHF patients; however, a recent
population-based survey reported that the long-term administration of -blocking agents increases circulating levels of
ANP and BNP.25 The reasons for such an increase are not
readily apparent. One possibility is that metoprolol-increased
LVEF and Volumes for Patients Treated With Metoprolol CR Versus Placebo
Placebo All
Metoprolol All
Placebo Ischemic
Metoprolol Ischemic
Placebo Nonischemic
Metoprolol Nonischemic
28⫾11
28⫾11
28⫾10
28⫾11
29⫾13
28⫾11
LVEF, %
Baseline
n
24 wk
n
⌬
207
212
136
144
62
63
29⫾11
31⫾11
28⫾10
29⫾11
31⫾13
34⫾12
178
⫺0.5⫾6
191
⫹2.4⫾6*
118
⫺0.9⫾5
139
⫹1.4⫾5*
55
⫹0.6⫾7
52
⫹5⫾8*
LVDV, mL
Baseline
n
24 wk
264⫾125
268⫾117
245⫾101
260⫾113
302⫾158
204
212
136
145
60
62
273⫾133
271⫾118
254⫾107
268⫾115
311⫾171
274⫾125
n
181
197
119
⌬
⫹23⫾65
⫹6⫾61*
⫹17⫾44
⫹7⫾54†
138
200⫾107
182⫾95
194⫾104
287⫾125
55
53
⫹35⫾95
⫹4⫾76†
LVSV, mL
Baseline
n
24 wk
197⫾115
226⫾144
214⫾115
202
211
134
144
60
62
203⫾123
196⫾108
190⫾102
196⫾105
231⫾159
192⫾114
n
178
195
118
138
55
52
⌬
⫹19⫾55
⫺2⫾51*
⫹16⫾38
⫹0.4⫾44*
⫹28⫾80
⫺9⫾66*
LVDV indicates left ventricular diastolic volume; LVSV, left ventricular systolic volume.
*P⬍0.05, †0.10ⱖP⬎0.05 vs placebo for respective subgroups. The interaction with treatment group for ischemic vs nonischemic is not significant
for any of the parameters.
The RESOLVD Investigators
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
LV filling pressure is an effect that would be consistent with
the increased incidence of hospitalization for patients with
worsening heart failure with the use of metoprolol found in
this relatively short trial. Alternatively, -adrenergic blockade may decrease the excretion of natriuretic peptides or
directly block the inhibitory effect of adrenergic activation on
natriuretic peptides and result in a compensatory beneficial
increase in natriuretic peptides.
Neither arm of the RESOLVD Pilot Study was powered to
detect differences in clinical end points such as death.
However, despite a short follow-up duration, treatment with
metoprolol CR appears to be associated with a reduction in
mortality rates. In fact, the proportion of reduction in allcause mortality, sudden death, and pump failure death can be
superimposed on those recently reported in MERIT-HF.9
Interestingly, cause-specific analysis of hospitalizations
showed an increase in the diagnosis of hospitalizations for
CHF in the metoprolol CR group but a concomitant decrease
in hospitalizations for reasons other than CHF, leading to a
neutral effect on all-cause hospitalizations. The reasons for
the more common hospitalizations for CHF in the metoprolol
CR group may be related to the vigorous titration regimen
used in this trial. Although a similar mean dosage (159 mg/d
metoprolol CR) was reported in MERIT-HF,9 such a dosage
is higher than that (87 mg/d metoprolol) used by Fisher et al10
in patients with ischemic heart failure10 and the dosage (106
mg/d metoprolol) used in the Metoprolol in Dilated Cardiomyopathy Trial.2 Nevertheless, most patients who worsened
while receiving metoprolol were successfully managed with a
lowered dose of -blocker, which explains why, as reported
in MERIT-HF,9 no difference was observed in the percentage
of patients who stopped receiving the blinded medication.
In summary, treatment with metoprolol CR for ⬇6 months
in patients with moderately severe CHF is well tolerated and
improves LV function and some of the neurohormonal
profile, regardless of the cause of CHF. The trend toward
fewer deaths in this study was supported by the results of the
recently presented MERIT-HF Trial.
Appendix
Investigators and Committee Members
Clinical Centers
Brazil: W. Cirillo, R. Decanini, O. Rizzi Coelho,* Á. Avezum,*
M.S. Pacheco Peixoto, L.S. Piegas, J.M. Rossi Neto, M. Paiva, A.C.
Carvalho,* D.R. de Almeida, I.M. Ligori Fernandes, M.C. Malavasi,
R. Pavanello,* M. Canesin, S. Ishii, and A.C. Pereira Barretto.*
Canada: J. Imrie, R. Moore, K. Woo,* V. Bernstein,* H.F.
Mizgala, S. Mooney, D. Hilbich, R. Kuritzky, D.W. Rupka,* M.M.
Blackwell, L. Breakwell, J.M. Kornder, S.A. Pearce, P. Polasek,*
P.M. Richardson, J. Grant, D. Isaac,* P. Beresford, P. Giannoccaro,
D. Roth,* P. Greenwood,* T. Muzyka, A. Prosser, N. Brass, W.
Hui,* L. Kvill, M. Goeres, K. MacDonald, M. Senaratne,* L. Hill, D.
Humen,* K.K. Teo, N. Habib,* Mrs N. Habib, S. Teekasingh, J.
MacKenzie, B. McEwen, A. Morris,* A. Dhair, C. Lai,* K. Kwiatkowski, J. Brugos, S. Nawaz,* J. Andrews, G. Moe,* K. Freskiw, B.
Gilbert, C.D. Morgan,* B. Bozek, F. Halperin, A.J. Ricci,* N. Singh,
G. Cappelli, T. Boyne,* E. Fallen, A. Panju,* G. Woodcock, E. Kent,
A.D. Kitching,* H. Sullivan, D. Tomson, R.S. McKelvie,* R.T.
Tsuyuki, S. Yusuf, Y.K. Chan,* D. Thomson, J.M.O. Arnold,* G.
*Principal investigator.
Metoprolol CR in Congestive Heart Failure
383
Hurwitz, R. Miles, A. Baker, A. Haspect, S. Smith,* J. Bedard,* L.
Lavoie, L. Dufort, R. Harvey, S. Lepage,* E. Elstein, D. Fitchett,* A.
Serpa, L. Day, N. Racine, D. Savard, F. Sestier,* G. Gosselin, J.L.
Rouleau, M. White,* L. Whittom, G. Kiwan, S.M. Kouz,* M.
Laforest, H. Ouimet, P. Carmichael, J. Lenis,* P. Auger,* F.
Grondin, D. Saulnier, J. Campeau, R. Dupuis,* C. Lauzon, M.
Genest, N.M. Robitaille,* J. Beaudoin, N. Belanger, G. Houde, P.
Talbot,* J. Cossett, C. Koilpillai,* W.J. Sheridan, M. Tobin, and B.
Sussex.*
Italy: G. Ascoli, A. Fraticelli, E. Paciaroni,* Como, CO: R.
Belluschi,* F. Ruffa, F. Tettamanti, F. Cobelli,* F. Salvucci, R.
Arpesella, C. Campana, A. Gavazzi,* V. Cirrincione,* F. Ingrilli, E.
Sciortino, A. Boccanelli,* G. Cacciatore, M. Menichelli, E.
Bosimini, P. Giannuzzi,* C. Marcassa, M. Porcu, S. Salis, A.
Sanna,* G. Comerio, E. Gronda,* and M. Mangiavacchi.
Switzerland: T. Moccetti,* E. Pasotti, and F. Sessa.
United States: W.C. Levy, J. Probstfield,* J. Thompson, M.
Gramberg, J. Grover,* D. Towery, K. Ogunyankin, B.N. Singh,*
J. Celano, S. Graham, R.M. Kohn,* P. Pande,* A. Sass, R.S. Wiener,
S. Rydzinski, R.C. Starling, J. Young,* L. Hays, A. Naftilan,* A.
Miller,* A. Varga, and R. Wofford.
Regional Monitors
S. Barnhill, R. de Paula Brito, L. Harris, A. Haspect, T. Cristina, M.
Jarosz, J. Kellen, C. Kingry, R. Letterer, D. La Forge, C. Liuni, J.
MacKenzie, A. Magi, K. Stevens, and P. Squires.
Steering Committee
S. Yusuf (chair); J.L. Rouleau (cochair); A. Maggioni (cochair);
J.M.O. Arnold, Á. Avezum, R. Burns, J. Floras, A. Gavazzi, P. Held,
Å. Hjalmarson, D. Isaac, R. Latini, E. Lindgren, R.S. McKelvie, L.S.
Piegas, D. Pericak, J. Pogue, J. Probstfield, S. Smith, K. Swedberg,
K.K. Teo, R.T. Tsuyuki, C. Vint-Reed, Y. Wang, M. White, E.M.
Wiecek, and J. Young.
External Safety and Efficacy Monitoring Committee
D. Johnstone (chair); P.W. Armstrong; M. Packer, and H. Wedel.
Substudies Committee
K.K. Teo (chair); A. Gavazzi, R.T. Tsuyuki, M. White, and R.
McKelvie.
Canadian Cardiovascular Collaboration Project Office
(Hamilton, Ontario)
M. Anderson, I. Holadyk-Gris, K. Kucemba, J. MacKay, R.S.
McKelvie, M. Micks, D. Pericak, J. Pogue, S. Reeve, L. Robinson,
R.T. Tsuyuki, J. Tucker, E.M. Wiecek, Y. Wang, and S. Yusuf.
Core Laboratories
Neurohormones: P. Cernacek, M. Joyal, N. Poitras, J.L. Rouleau, M.
White, P. Sirois, Montréal; M. Bevilacqua, R. Latini (coordinator), S.
Masson, M. Torri, Milano; C. Hall, Norway; Nuclear Cardiology:
R.J. Burns, T. Heeney, S. Tadros, Toronto.
Manuscript Writing Committee
Michel White, MD (leader); Salim Yusuf, FRCP, DPhil; Robert S.
McKelvie, MD, PhD; Danny Pericak, MD; James Young, MD;
Roberto Latini, MD; Janice Pogue, MA, MSc; Robert J. Burns, MD;
Jeffrey Probstfield, MD; Ross T. Tsuyuki, PharmD, MSc; Aldo P.
Maggioni, MD; Álvaro Avezum Jr, MD; and Jean L. Rouleau, MD.
References
1. Heidenreich PA, Lee TT, Massie BM. Effect of beta-blockade on mortality in patients with heart failure: a meta-analysis of randomized clinical
trials. J Am Coll Cardiol. 1997;30:27–34.
2. Waagstein F, Bristow MR, Swedberg K, Camerini F, Fowler MB, Silver
MA, Gilbert EM, Johnson MR, Goss FG, Hjalmarson A, for the Metoprolol in Dilated Cardiomyopathy (MDC) Trial Study Group. Beneficial
effects of metoprolol in idiopathic dilated cardiomyopathy. Lancet. 1993;
342:1441–1446.
384
Circulation
February 1, 2000
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
3. The Metoprolol in Dilated Cardiomyopathy (MDC) Trial Study Group.
Three-year follow-up of patients randomised in the Metoprolol in Dilated
Cardiomyopathy Trial. Lancet. 1998;351:1180 –1181.
4. Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM,
Shusterman NH, for the US Carvedilol Heart Failure Study Group. The
effect of carvedilol on morbidity and mortality in patients with chronic
heart failure. N Engl J Med. 1996;334:1349 –1355.
5. Vantrimpont P, Rouleau JL, Wun CC, Ciampi A, Klein M, Sussex B,
Arnold JM, Moye L, Pfeffer M, for the SAVE Investigators. Additive
beneficial effects of beta-blockers to angiotensin-converting enzyme inhibitors in the Survival And Ventricular Enlargement (SAVE) Study.
J Am Coll Cardiol. 1997;29:229 –236.
6. Australia/New Zealand Heart Failure Research Collaborative Group.
Randomised, placebo-controlled trial of carvedilol in patients with congestive heart failure due to ischaemic heart disease. Lancet. 1997;349:
375–380.
7. Doughty RN, Rodgers A, Sharpe N, MacMahon S. Effects of betablocker therapy on mortality in patients with heart failure. Eur Heart J.
1997;18:560 –565.
8. CIBIS-II Investigators and Committees. The Cardiac Insufficiency Bisoprolol Study II. (CIBIS-II): a randomised trial. Lancet. 1999;353:9 –13.
9. MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart
failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive
Heart Failure (MERIT-HF). Lancet. 1999;353:2001–2007.
10. Fisher ML, Gottlieb SS, Plotnick GD, Greenberg NL, Patten RD, Bennett
SK, Hamilton BP. Beneficial effects of metoprolol in heart failure associated with coronary artery disease: a randomized trial. J Am Coll
Cardiol. 1994;23:943–950.
11. Tsuyuki RT, Yusuf S, Rouleau JL, Maggioni AP, McKelvie RS, Wiecek
EM, Wang Y, Pogue J, Teo KK, White M, Avezum A Jr, Latini R, Held
P, Lindgren E, Probstfield J, for the RESOLVD Pilot Study Investigators.
Combination neurohormonal blockade with ACE inhibitors, angiotensin
II. antagonists and beta-blockers in patients with congestive heart failure:
design of the Randomized Evaluation of Strategies for Left Ventricular
Dysfunction (RESOLVD) Pilot Study. Can J Cardiol. 1997;13:
1166 –1174.
12. Mayes D, Furuyama S, Kem DC, Nugent CA. A radioimmunoassay for
plasma aldosterone. J Clin Endocrinol Metab. 1970;30:682– 685.
13. Cernacek P, Stewart DJ. Immunoreactive endothelin in human plasma:
marked elevations in patients in cardiogenic shock. Biochem Biophys Res
Commun. 1989;161:562–567.
14. Sundsfjord JA, Thibault G, Larochelle P, Cantin M. Identification and
plasma concentrations of the N-terminal fragment of proatrial natriuretic
factor in man. J Clin Endocrinol Metab. 1988;66:605– 610.
15. Yasue H, Yoshimura M, Sumida H, Kikuta K, Kugiyama K, Jougasaki M,
Ogawa H, Okumura K, Mukoyama M, Nakao K. Localization and
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
mechanism of secretion of B-type natriuretic peptide in comparison with
those of A-type natriuretic peptide in normal subjects and patients with
heart failure. Circulation. 1994;90:195–203.
Sandberg A, Ragnarsson G, Jonsson UE, Sjögren J. Design of a new
multiple-unit controlled-release formulation of metoprolol-metoprolol
CR. Eur J Clin Pharmacol. 1988;33(suppl):S3–S7.
Sandberg A, Blomqvist I, Jonsson UE, Lundborg P. Pharmacokinetic and
pharmacodynamic properties of a new controlled-release formulation of
metoprolol: a comparison with conventional tablets. Eur J Clin
Pharmacol. 1988;33(suppl):S9 –S14.
Hall SA, Cigarroa CG, Marcoux L, Risser RC, Grayburn PA, Eichhorn
EJ. Time course of improvement in left ventricular function, mass and
geometry in patients with congestive heart failure treated with betaadrenergic blockade. J Am Coll Cardiol. 1995;25:1154 –1161.
Gilbert EM, Abraham WT, Olsen S, Hattler B, White M, Mealy P,
Larrabee P, Bristow MR. Comparative hemodynamic, left ventricular
functional, and antiadrenergic effects of chronic treatment with metoprolol versus carvedilol in the failing heart. Circulation. 1996;94:
2817–2825.
Woodley SL, Gilbert EM, Anderson JL, O’Connell JB, Deitchman D,
Yanowitz FG, Mealey PC, Volkman K, Renlund DG, Menlove R.
-Blockade with bucindolol in heart failure caused by ischemic versus
idiopathic dilated cardiomyopathy. Circulation. 1991;84:2426 –2441.
Colucci WS, Packer M, Bristow MR, Gilbert EM, Cohn JN, Fowler MB,
Krueger SK, Hershberger R, Uretsky BF, Bowers JA, Sackner-Bernstein
JD, Young ST, Holcslaw TL, Lukas MA, for the US Carvedilol Heart
Failure Study Group. Carvedilol inhibits clinical progression in patients
with mild symptoms of heart failure. Circulation. 1996;94:2800 –2806.
Eichhorn EJ, Heesch CM, Barnett JH, Alvarez LG, Fass SM, Grayburn
PA, Hatfield BA, Marcoux LG, Malloy CR. Effect of metoprolol on
myocardial function and energetics in patients with nonischemic dilated
cardiomyopathy: a randomized, double-blind, placebo-controlled study.
J Am Coll Cardiol. 1994;24:1310 –1320.
Currie PJ, Kelly MJ, McKenzie A, Harper RW, Lim YL, Federman J,
Anderson ST, Pitt A. Oral beta-adrenergic blockade with metoprolol in
chronic severe dilated cardiomyopathy. J Am Coll Cardiol. 1984;3:
203–209.
Blumenfeld JD, Sealey JE, Mann SJ, Bragat A, Marion R, Pecker MS,
Sotelo J, August P, Pickering TG, Laragh JH. -Adrenergic receptor
blockade as a therapeutic approach for suppressing the renin-angiotensin-aldosterone system in normotensive and hypertensive subjects. Am J
Hypertens. 1999;12:451– 459.
Luchner A, Burnett JC Jr, Jougasaki M, Hense HW, Riegger GA,
Schunkert H. Augmentation of the cardiac natriuretic peptides by betareceptor antagonism: evidence from a population-based study. J Am Coll
Cardiol. 1998;32:1839 –1844.
Effects of Metoprolol CR in Patients With Ischemic and Dilated Cardiomyopathy: The
Randomized Evaluation of Strategies for Left Ventricular Dysfunction Pilot Study
The RESOLVD Investigators
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Circulation. 2000;101:378-384
doi: 10.1161/01.CIR.101.4.378
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2000 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circ.ahajournals.org/content/101/4/378
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/