Macro-creatine kinase syndrome as an
advertisement
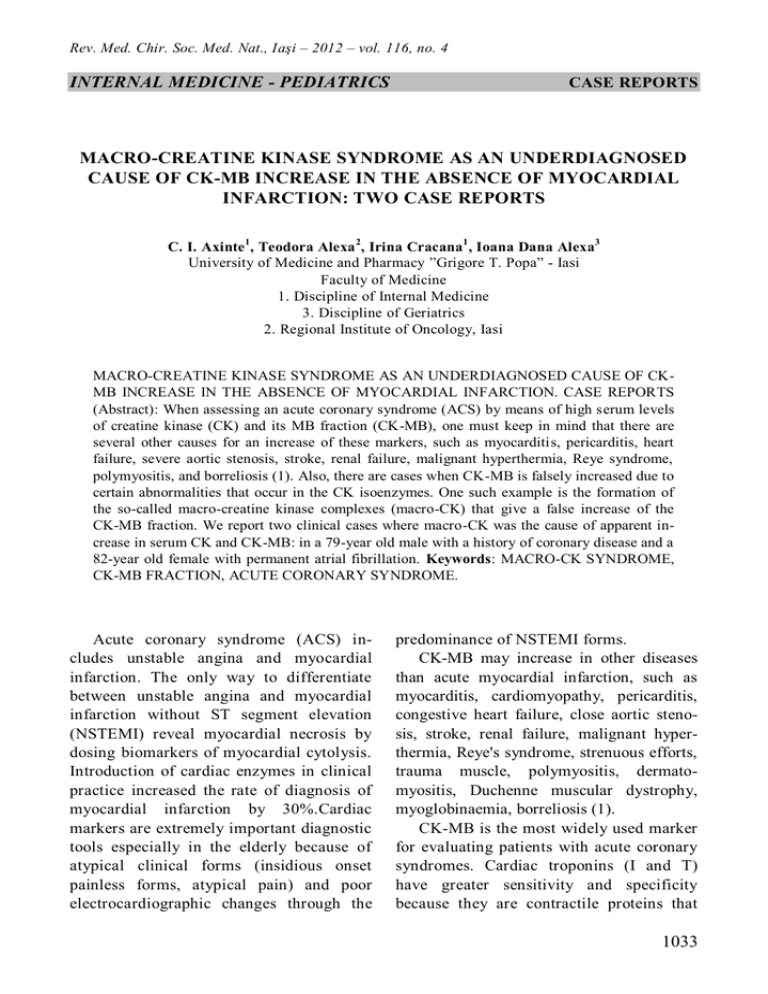
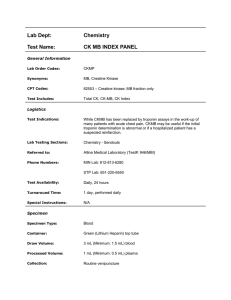
Rev. Med. Chir. Soc. Med. Nat., Iaşi – 2012 – vol. 116, no. 4 INTERNAL MEDICINE - PEDIATRICS CASE REPORTS MACRO-CREATINE KINASE SYNDROME AS AN UNDERDIAGNOSED CAUSE OF CK-MB INCREASE IN THE ABSENCE OF MYOCARDIAL INFARCTION: TWO CASE REPORTS C. I. Axinte 1, Teodora Alexa 2, Irina Cracana1 , Ioana Dana Alexa3 University of Medicine and Pharmacy ”Grigore T. Popa” - Iasi Faculty of Medicine 1. Discipline of Internal Medicine 3. Discipline of Geriatrics 2. Regional Institute of Oncology, Iasi MACRO-CREATINE KINASE SYNDROME AS AN UNDERDIAGNOSED CAUSE OF CKMB INCREASE IN THE ABSENCE OF MYOCARDIAL INFARCTION. CASE REPORTS (Abstract): When assessing an acute coronary syndrome (ACS) by means of high serum levels of creatine kinase (CK) and its MB fraction (CK-MB), one must keep in mind that there are several other causes for an increase of these markers, such as myocarditis, pericarditis, heart failure, severe aortic stenosis, stroke, renal failure, malignant hyperthermia, Reye syndrome, polymyositis, and borreliosis (1). Also, there are cases when CK-MB is falsely increased due to certain abnormalities that occur in the CK isoenzymes. One such example is the formation of the so-called macro-creatine kinase complexes (macro-CK) that give a false increase of the CK-MB fraction. We report two clinical cases where macro-CK was the cause of apparent increase in serum CK and CK-MB: in a 79-year old male with a history of coronary disease and a 82-year old female with permanent atrial fibrillation. Keywords: MACRO-CK SYNDROME, CK-MB FRACTION, ACUTE CORONARY SYNDROME. Acute coronary syndrome (ACS) includes unstable angina and myocardial infarction. The only way to differentiate between unstable angina and myocardial infarction without ST segment elevation (NSTEMI) reveal myocardial necrosis by dosing biomarkers of myocardial cytolysis. Introduction of cardiac enzymes in clinical practice increased the rate of diagnosis of myocardial infarction by 30%.Cardiac markers are extremely important diagnostic tools especially in the elderly because of atypical clinical forms (insidious onset painless forms, atypical pain) and poor electrocardiographic changes through the predominance of NSTEMI forms. CK-MB may increase in other diseases than acute myocardial infarction, such as myocarditis, cardiomyopathy, pericarditis, congestive heart failure, close aortic stenosis, stroke, renal failure, malignant hyperthermia, Reye's syndrome, strenuous efforts, trauma muscle, polymyositis, dermatomyositis, Duchenne muscular dystrophy, myoglobinaemia, borreliosis (1). CK-MB is the most widely used marker for evaluating patients with acute coronary syndromes. Cardiac troponins (I and T) have greater sensitivity and specificity because they are contractile proteins that 1033 C. I. Axinte et al. are found only in the cardiac myocytes (2). Serial measurements of total CK and CKMB, associated with troponin measurements may better indicate temporal evolution and infarct size (3, 4). Creatine kinase (CK) consists of 3 fractions (CK-MM, CK-MB, and CK-BB). A report of total CK / CK-MB> 50% is suggestive for the presence of macro CK complexes (type 1 or 2), resulting in a reaction type Ag-Ac. The occurrence of these immune complexes produces a false increase in CK-MB which can 't be differentiated except by electrophoresis (5). CASE REPORT Ι Patient 1 is known with significant coronary and hypertensive damage ; at the age of 76 years he was performed angioplasty with active pharmacologically on circumflex artery and at the age of 78 years a coronary angiography is carried out again because of prolonged chest pain and occurrence of electrocardiographic changes in dynamics. The coronary angiography revealed the following changes: left coronary artery LAD stenosis 80% II, 80% ostial stenosis, stent re-stenosis minimum CX I, stenosis 80% GM I, GM II 90% ostial stenosis, right coronary artery - 80% stenosis CD I CD III 80% stenosis, 80% stenosis IVP with surgical myocardial revascularization indication that the patient has timed it. In April 2012, he was admitted in Geri- atric Hospital Clinic "Dr. C.I. Parhon " for precordial pain having angina character and worsening in the last 4 hours before addressing and which partially wakened after Nitroglycerin administration. Aim at internment: BP = 140/80 mm Hg, FC = 76 b / min, rhythmic, without signs of cardiac decompensation. Electrocardiogram: sinus rhythm, FC = 70/min, AQRS = -30 °, concentric left ventricular hypertrophy type, ISL = 40 mm Holter ECG: sinus rhythm throughout the recording Echocardiography: significant left ventricular wall hypertrophy, SIV = 16 mm, EF = 60%, without hypo-kinetic areas. Of laboratory results note: total CK = 245 U / l, CK-MB = 226 U / L, troponin T hs = 11 ng / ml (normal: 0-14 ng / ml), SGPT = 30 U / L, SGOT = 31 U / l, LDH = 175 U / l, glucose = 98 mg%. Because of increased CK-MB, troponin T hs normal, ratio CK / CK-MB> 50%, without significant electrocardiographic abnormalities dynamic and echocardiographic appearance's CK electrophoresis was performed (tab. I). Suspected a false increase in CK-MB. Macro CK Complex has been identified type 1 (1.56 micromol / SL), total CK = 2.5 (normal: 2.85 micromol / SL), CK-MB = 0 micromol / sL (normal: <0.1 micromol / SL), CK-MM = 0.94 micromol / sL (normal: <2.85 micromol / SL), CK-BB = 0 micromol / sL (normal: 0) (tab Ι, fig. 1, 2). TABLE Ι Results of CK izoenzyme electrophoresis in patient 1 Patient values Normal values CK 2,5 μmol/sl < 2,85 μmol/sl CK-MM 0,94 μmol/sl < 2,5 μmol/sl CK-BB 0 μmol/sl 0,00 μmol/sl CK-MB 0 μmol/sl < 0,1 μmol/sl Macro CK 1,56 μmol/sl (62% of CK) 0 μmol/sl 1034 Macro-creatine kinase syndrome as an underdiagnosed cause of CK-MB increase Fig. 1. CK and CK-MB values during previous hospital stay. Values in 2009 are previously recorded PTCA CASE REPORT ΙΙ Patient 2, well known hypertensive with permanent atrial fibrillation and heart failure NYHA class II left side is admitted for dyspnea at minor efforts occurred two days ago due to psycho-emotional stress. Associates prior atypical chest pain, with emphasis on compression onset 24 hours ago. Aim at internment: BP = 150/90 mm Hg, FC = 110 / min. Electrocardiography: Atrial fibrillation, FCM = 104/min, AQRS = 30°, negative T waves in V1, V2. Echocardiography: EF = 50%, SIV = 11 mm, without hypo-kinetic areas without pericardial fluid, VCI completely inspiratory collapse. From the laboratory results its is noted: total CK = 248 U / l, CK-MB = 274 U / L, troponin T hs = 17 ng / ml, SGPT = 36 U / l, ALT = 28 U /l. CK s electrophoresis was performed as in the case of the first patient. It has been identified macro CK complex type 1 (4.33 micromol / sL) = 4.79 total CK, CK-MB = 0 micromol / SL, CK-MM = 0.46 micromol / SL, CK-BB = 0 micromol / SL (tab ΙΙ, fig. 2). TABLE ΙΙ Results of CK izoenzyme electrophoresis in patient 2 Patient values Normal values 4,79 μmol/sl < 2,85 μmol/sl CK 0,46 μmol/sl < 2,5 μmol/sl CK-MM 0 μmol/sl 0,00 μmol/sl CK-BB 0 μmol/sl < 0,1 μmol/sl CK-MB 4,33 μmol/sl (90% of CK) 0 μmol/sl Macro CK 1035 C. I. Axinte et al. Fig. 2. CK and CK-MB values throughout hospital stay DISCUSSION In both cases one can notice a large increase in CK-MB values that could not be explained by acute myocardial ischemia or other common causes of this enzyme increase. Analyzing the previous documents of patient 1 reveals a constant value increase of CK-MB. The only normal value was recorded only in 2009 after stent angioplasty. On the internment in January 2011 and August 2011 the lowest CK-MB value was 125 U / l despite vigorous treatment, properly administered. A report of total CK / CK-MB> 50% is suggestive for the presence of macro CK complexes. The occurrence of these immune complexes produces a false increase in CK-MB can t be differentiated except with electrophoresis. The presence of macro CK complex still doesn't have a precise use being possible to increase in many other diseases (6). There are two types of macro CK: type 1 and type 2. Macro CK type 1 occurs via 1036 antigen-antibody reaction type between CK-BB and IgG or, less commonly, between CK-MM and IgA (7, 8). Macro CK type 1 (incidence = 0.45% - 1.2%) occurs in hypothyroidism, autoimmune diseases, cancer, myositis, cardiovascular disease and even apparently healthy individuals. It is more common in women and in people over 70 years (9). Macro CK type 2 (incidence = 0.5 - 3.7%) is close to home and migrate mitochondrial CK-MM band. In more severe disease than type 1 appears: malignancy (most commonly colon or prostate cancer) and severe liver disease with a poor prognosis (10). Macro CK complex appearance does not determine great increase value of total CK (<500 U /l). It should be suspected a false increase in CK-MB in the presence of atypical symptoms of acute ischemia, lack of electrocardiographic changes, echocardiographic and persistent increases regardless of the therapeutic scheme administered (11). Macro-creatine kinase syndrome as an underdiagnosed cause of CK-MB increase Growth of these enzymes, with a total CK report /CK-MB under 5% is suggestive for non cardiac muscle damage. Troponin specificity and sensitivity is higher than CK-MB determination. Troponin T hs shows frequently increased values than CK-MB in the absence of acute coronary ischemia therefore it is important to determine its dynamics. Any significant increase in intraventricular pressure can lead to abnormal Troponin T hs without myocardial infarction. In patient 2, the slightest increase of Troponin T hs at interment with normalization in the next determination was interpreted in the context of heart failure and atrial fibrillation with fast frequency. There are few cases of this type reported in literature. Among these, some associate the presence of this syndrome with digestive disorders such as Crohn's disease or ulcerative colitis (12) or persistent diarrhea (13). In other reports it has been noticed associations with cancer (14) or myopathies (15). Rosa Jimenez & et al (16) presents a series of 7 cases with macro-CK type 1 syndrome, of which 3 cases had a history of cardiovascular disease and the rest were not known. Patients reported in this article are the first reported in Romania with macro-CK syndrome. CONCLUSIONS Highlighting cases of macro CK is useful for avoiding invasive investigations and unnecessary treatments. The particularity of the first patient case consists in a false increase of CK-MB at a patient with three-vessel lesions and indication for revascularization surgery. The systolic function is maintained within normal limits and poses no arrhythmia at ECG Holter monitoring, in significant myocardial ischemia. The particularity of the second case is the combination of a significant increase in CK-MB in the presence of a chest pain caused by musculoskeletal pain (possible intricate pain) and without electrocardiographic changes in dynamics and without echocardiographic hypo-kinetic areas. Electrophoresis Creatine is currently quite expansive investigation and can be suspected the presence of complex macro CK emergency when the total report CK / CK-MB> 50%. Discrepancy between the values of CKMB and troponin must raise a question mark for the diagnosis of acute myocardial infarction and the values of these biomarkers must be correlated with clinical examination, electrocardiographic and echocardiographic aspect. Guidelines for acute coronary syndrome should mention this false increase in CKMB as a variant of differential diagnosis. REFERENCES 1. Mannem SR, Ehtesham M, Praveen KN. Elevated CK-MB without myocardial infarction. Sci. med. 2009; 1(2): 120-122. 2. Ginghina C. Mic tratat de cardiologie. Bucureşti: Editura Academiei, 2010. 3. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction : A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non -ST-Elevation Myocardial Infarction). Circulation 2007; 116: 148-304. 4. Alexa ID. Geriatrie clinică, ediţia a II-a. Iaşi: Editura “Gr. T. Popa”, 2006. 1037 C. I. Axinte et al. 5. Véronique L. Roger, Weston SA, et al. Trends in Incidence, Severity and Outcome of Hospitalized Myocardial Infarction. Circulation 2010; 121(7): 863–869. 6. Wallach J. Interpratation of diagnostic tests, Sixth edition. Philadelphia: Lippincott-Raven Publishers, 2000. 7. Etienne E, Hanser AM, Woehl-Kremer B, et al. Macroenzymes: macro-ASAT et macro-CPK. Deux observations et revue de la littérature. La Revue de Médecine Interne 2009; 30: 963-969. 8. Ruiz Ginés MA, Calafell Mas MF, Ruiz Ginés JA, et al. Macro creatine kinase: illness marker. Practical guide for the management. An Med Intern 2006; 23(6): 272-275. 9. Galarraga B, Sinclair D, Fahie-Wilson MN, et al. A rare but important cause for a raised serum creatine kinase concentration: two case reports and a literature review. Rheumatology 2003; 42(1): 186188. 10. Laureys M, Slon JP, Slabbynck H, et al. Macromolecular Creatine Kinase Type 1: a Serum Marker Associated with Disease. Clinical Chemistry 1991; 37(3): 430-434. 11. Benedikt G, Schoser H, Witt TN. Differential Diagnosis of Serum Creatine Kinase Elevation. In: Neuroacanthocytosis Syndromes ed. Danek, 2005, Part 2, 79-86, DOI: 10.1007/1-4020-2898-9_10. 12. Perez-Calle JL, Marin-Jimenez I, Lopez-Serrano P, et al. Prevalence of macrocreatinkinase type 1 in patients with inflammatory bowel disease. Dig Dis Sci. 2008; 53(2): 486-489. 13. Sztefko K, Grodzicki T, Strach M. Macro-CK in 82 year old woman. A case report. Intern. J. Cardiol. 2010; 141(3): e57-e58 14. Jap TS, Wu QC, Ho DM, Chiang H. Spuriously high CK-MB isoenzyme activity imicking acute myocardial infarction in a patient with adenocarcinoma of the rectum. Chin Med J (Taipei) 2000; 63: 413-417. 15. Hsiao JF, Ning HC, Gu PW, Lin WY, Chu PH. Clinical role of recurrently elevated macro creatine kinase type 1. J Clin Lab Anal. 2008; 22(3): 186-191. 16. Rosa-Jimenez F, Gasso de Campos M, Camacho Reina MV, et al. Macro creatine kinase type 1 as acause of increase of CK-MB isoenzyme. Apropos of 7 cases. Rev Esp Cardiol 1997; 50: 166-172. NEWS A NEW METHOD FOR DETECTION OF BACTERIAL PROTEIN SECRETION Bacteria interact with host cells through secretion systems which carry proteins through bact erial membrane. Developing methods to monitor bacterial protein secretion can bring new information for diagnostic of bacterial infections. Enzymatic or fluorescent marking of pr oteins to reveal genes involved in transmembrane export of bacterial proteins can used to study the i nteraction of bacteria with host cell. A recent study conducted by M. M. Champion and collab orators describe a modified form of bacterial proteomics using a MALDI-TOF mass spectrometer, which directly detects the proteins from whole colonies. This method is able to specifically monitor a special protein secretion system, which is a major virulence determinant in Mycobacterium tuberculosis, Bacillus and Staphylococcus species. Also this method can be applicable to study other bacterial protein export systems and for the identification of compounds that inhibit bacterial protein secretion (M. M. Champion, E. A. Williams, G. M. Kennedy, P. A. DiGiuseppe Champion. Direct Detection of Bacterial Protein Secretion Using Whole Colony Proteomics. Molecular & Cellular Proteomics, 2012; 11 (9): 596-604). Cătălina Luncă 1038