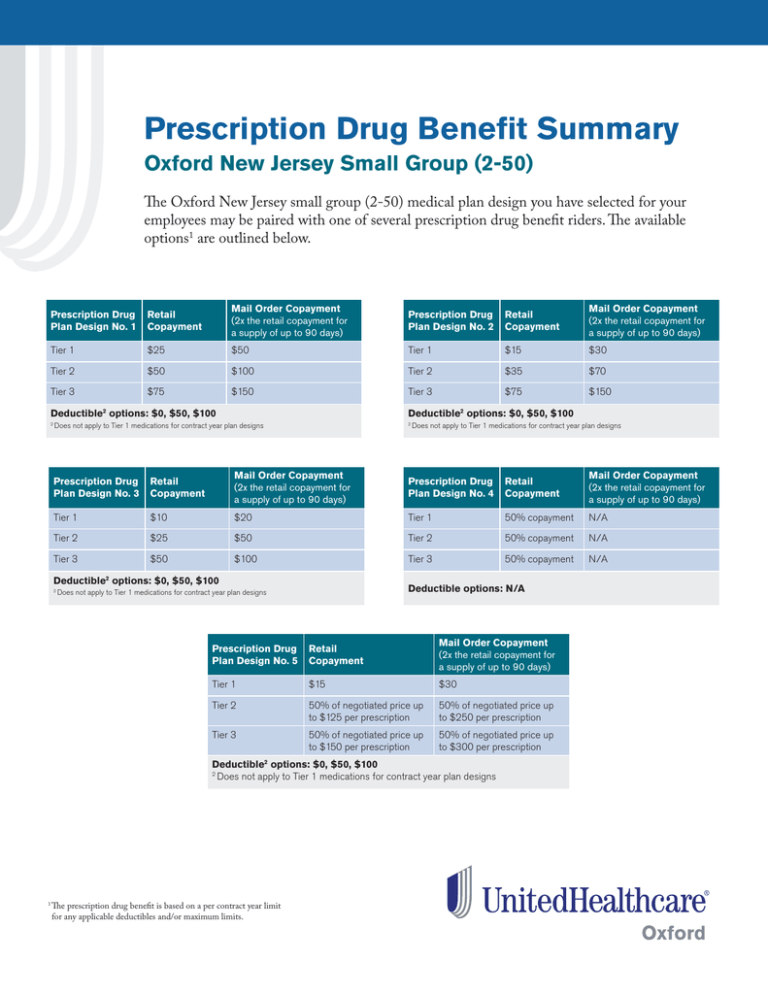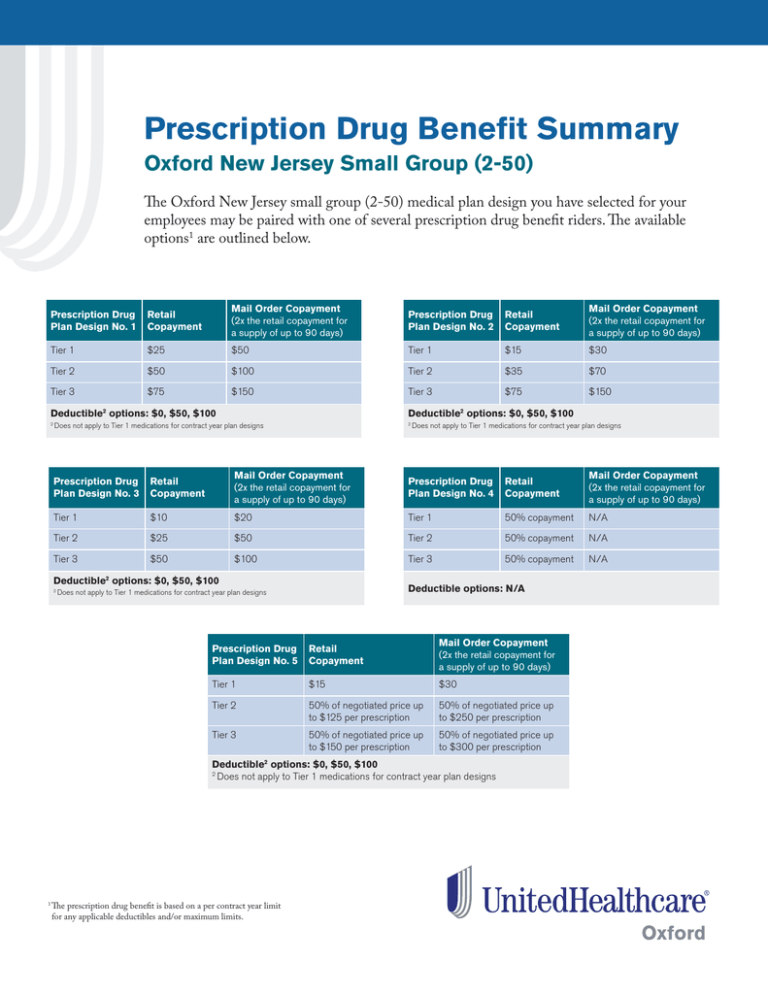
Prescription Drug Benefit Summary
Oxford New Jersey Small Group (2-50)
The Oxford New Jersey small group (2-50) medical plan design you have selected for your
employees may be paired with one of several prescription drug benefit riders. The available
options1 are outlined below.
Prescription Drug
Plan Design No. 1
Retail
Copayment
Mail Order Copayment
(2x the retail copayment for
a supply of up to 90 days)
Prescription Drug
Plan Design No. 2
Retail
Copayment
Mail Order Copayment
(2x the retail copayment for
a supply of up to 90 days)
Tier 1
$25
$50
Tier 1
$15
$30
Tier 2
$50
$100
Tier 2
$35
$70
Tier 3
$75
$150
Tier 3
$75
$150
Deductible2 options: $0, $50, $100
2
Deductible2 options: $0, $50, $100
Does not apply to Tier 1 medications for contract year plan designs
2
Does not apply to Tier 1 medications for contract year plan designs
Prescription Drug
Plan Design No. 3
Retail
Copayment
Mail Order Copayment
(2x the retail copayment for
a supply of up to 90 days)
Prescription Drug
Plan Design No. 4
Retail
Copayment
Mail Order Copayment
(2x the retail copayment for
a supply of up to 90 days)
Tier 1
$10
$20
Tier 1
50% copayment
N/A
Tier 2
$25
$50
Tier 2
50% copayment
N/A
$50
$100
Tier 3
50% copayment
N/A
Tier 3
Deductible options: $0, $50, $100
2
2
Deductible options: N/A
Does not apply to Tier 1 medications for contract year plan designs
Prescription Drug
Plan Design No. 5
Retail
Copayment
Mail Order Copayment
(2x the retail copayment for
a supply of up to 90 days)
Tier 1
$15
$30
Tier 2
50% of negotiated price up
to $125 per prescription
50% of negotiated price up
to $250 per prescription
Tier 3
50% of negotiated price up
to $150 per prescription
50% of negotiated price up
to $300 per prescription
Deductible2 options: $0, $50, $100
Does not apply to Tier 1 medications for contract year plan designs
2
The prescription drug benefit is based on a per contract year limit
for any applicable deductibles and/or maximum limits.
1
Understanding medication choices
Our Prescription Drug List (PDL) outlines the most commonly prescribed medications for certain conditions and divides them
into tiers. The PDL includes both brand-name and generic prescription medications approved by the U.S. Food and Drug
Administration (FDA).
The PDL is reviewed periodically and may change. Visit oxfordhealth.com for the most up-to-date listing.
Tiers
Tiers are the different cost levels a member will pay for a medication. Each tier is assigned a cost, which is determined by the
benefit plan you have selected for your employees. The assigned cost is how much a member will pay when filling a prescription.
The tier structuring is shown below:
Tier 1: Lowest-cost medications
Tier 2: Midrange-cost medications
Tier 3: Highest-cost medications
Tier placement decisions are made by our PDL Management Committee, which consists of senior level UnitedHealth Group
physicians and business leaders. The Committee’s goal is to help ensure access to a wide range of medications, while also helping
to control health care costs.
The PDL Management Committee uses several factors when determining tier placement:
• Clinical information from the UnitedHealthcare Pharmacy and Therapeutics Committee about the safety and effectiveness
of different medications1
• The medication’s costs and other economic factors
Specialty medications
Specialty medications treat some of the most complex and life threatening conditions. They can enhance quality of life and, for
some people, extend their life. These medications are often injected, infused or inhaled, as well as taken orally. That’s why it’s
important to provide the type of benefit coverage that best supports the member’s treatment needs. This flexibility is critical given
each medication’s unique requirements, the individual’s condition and cost management considerations.
To be the most effective, you must manage specialty medications under both the pharmacy and medical benefit. We choose where
a medication is covered based on a combined network, clinical and benefit model that is ideal for the particular medication.
Medications need to be covered under the medical benefit if they meet one or more of the following criteria; otherwise they are
covered under the pharmacy benefit:
• Physician or nurse assisted administration
• More intense physician oversight and support
• Faster access
• Less disruption to members and physicians
For more information on our prescription drug offerings,
please contact your broker or Oxford sales representative.
Please refer to your Outpatient Prescription Drug Rider for a description of how
economic factors are applied to New Jersey and Connecticut public sector plans.
1
Oxford HMO products are underwritten by Oxford Health Plans (NJ), Inc. Oxford insurance products are underwritten by Oxford Health Insurance, Inc.
© 2012 Oxford Health Plans LLC. All rights reserved. NJ-12-870