Refugee Mental Health: Issues for the New Millennium - i
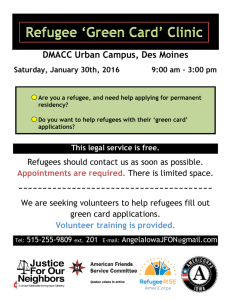
advertisement

i-counseling.net Refugee Mental Health Refugee Mental Health: Issues for the New Millennium Edited by the Center for Credentialing & Education CE Hours: 2 Course Introduction Many refugees leave their homes to escape life-threatening situations such as natural and man-made disasters, persecution, and human rights violations. Escaping these experiences might involve even further trauma. Refugees are at particular risk to resist treatment and are likely to not obtain services. Among refugees from group-oriented cultures, group-type interventions might be the treatment of choice. However, traumatized refugees may be reluctant to tell their stories due to shame, lack of trust, and fear. There is a pressing need for practitioners to be able to assist these people. This course summarizes the literature on refugee mental health. Learning Objectives Upon completion of this course, you will learn: • About issues and trends in forced migration • Aspects of U.S. policy regarding resettlement and asylum • About the implications for refugee mental health services • Cultural issues related to refugee mental health • About opportunities for refugee mental health and research priorities Course Content Article: Refugee Mental Health: Issures for the New Millennium Jaranson, J., Martin, S.F., and Ekblad, S. (2002). Refugee mental health: Issues of the millennium. In R.W. Manderscheid & M.J. Henderson (Eds). Mental Health, United States, 2002 (pp. 120-133). DHHS Pub. No. (SMA) 01-3537. Washington, DC: Supt. of Docs., U.S. Govt. Print. Off., 2001. 1 i-counseling.net Refugee Mental Health Refugee Mental Health: Issues for the New Millennium James Jaranson, M.D., M.A., M.P.H.; * Susan Forbes Martin, Ph.D.;* and Solvig Ekblad, D.M.Sc.* *University of Minnesota; Center for Victims of Torture; Regions Hospital/HealthPartners; * Institute for the Study of International Migration, Georgetown University;* National Institute for Psychosocial Factors and Health Ten years after exuberance about the end of the Cold War prompted the United Nations (U.N.) High Commissioner for Refugees (UNHCR) to declare a “decade of voluntary repatriation,” the international community is faced with a significant number of complex emergencies involving the forced movements of millions of persons. Forced migration has many causes and takes many forms. People leave because of persecution, human rights violations, repression, torture, conflict, and natural and human-made disasters. Many depart on their own initiative to escape these life-threatening situations; although, in a growing number of cases, people are driven from their homes by governments and insurgent groups intent on depopulating or shifting the ethnic, religious, or other composition of an area. Some manage to escape their countries and find temporary or permanent refuge abroad, while an alarmingly large number remain trapped inside or are forced to repatriate before the home country conditions change in any significant manner. Forced migrants often share a traumatic past, including “exposure to war-related violence, sexual assault, torture, incarceration, genocide and the threat of personal injury and annihilation” (Friedman & Jaranson, 1994). Escaping these experiences may involve still further trauma, including the physical danger of crossing borders, prolonged periods in refugee and displaced persons camps, malnutrition and disease, armed attacks, and sexual and other violence. Many forced migrants who reach the United States and other supposedly safe countries enter without authorization and continue to risk removal to their home countries. Even those who secure a legal status that permits them to remain may face chronic unemployment, poverty, racial discrimination, lack of access to medical care, difficulties in finding safe and affordable housing, high levels of crime, and an absence of family and community networks. Their adopted country, in some cases, may have supported the repressive regime that caused their original trauma (Quiroga & Gurr, 1998). The events of World War II produced a number of classic studies of refugee mental health, with particular focus on concentration camp survivors (Eitinger, 1959; Krupinski, Stoller, & Wallace, 1973). As humanitarian crises multiplied and grew in severity in the 1980’s, new interest in refugee mental health emerged, creating a new literature on the subject. Genocide in Rwanda; ethnic cleansing in Bosnia, Kosovo, and east Timor; savage conflicts in Liberia, Sierra Leone, and Chechnya— all of these events have shown the pressing need for even more attention to the traumas faced by the survivors of these calamities. Following a review of international and U.S. trends relating to forced migration, this article summarizes the scientific literature on refugee mental health, discusses challenges to address in improving responses, and presents recommendations for future research. 2 i-counseling.net Refugee Mental Health International Trends in Forced Migration The U.S. Committee for Refugees’ 1999 World Refugee Survey estimates that there were 13. 5 million refugees at the beginning of the year, down from almost 17 million at the beginning of the decade. Refugees have a special status in international law (USCR, 1999). The 1951 U. N. Convention Relating to the Status of Refugees defines a refugee as “a person who, owing to well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group or political opinion, is outside the country of his nationality and is unable or, owing to such fear, is unwilling to avail himself of the protection of that country.” Refugee status has been applied more broadly, however, to include other persons who are outside their country of origin because of armed conflict, generalized violence, foreign aggression, or other circumstances that have seriously disturbed public order, and who, therefore, require international protection. The largest number of refugees were in the Middle East (almost 6 million), followed by Africa (3 million), Europe and South Asia (1.7 million each), the Americas (750,000), and east Asia and the Pacific (500,000). Each of the following countries originated more than 250,000 persons who were still displaced in 1999: Afghanistan, the former Yugoslavia, Iraq, Somalia, Burundi, Liberia, Sudan, Sierra Leone, and Vietnam. In addition, more than 3 million Palestinians remained displaced and eligible for aid from the U. N. Relief and Works Administration. In some of these cases, the refugees had been uprooted for decades, whereas in others they had become refugees more recently. That the number of refugees— that is, persons outside of their home country— is at its lowest level in years does not mean that the number of persons in need of humanitarian aid and protection has reduced. There are growing numbers of conflicts in which civilians are targets of military activity as well as war crimes and crimes against humanity. Far too often, nationalism has turned rabid with ethnic group pitted against ethnic group in determining the national identity (e. g., Rwanda or the former Yugoslavia). In certain extreme cases, sovereignty itself has been compromised as no group can amass the strength or legitimacy to maintain order (e. g., Liberia or Somalia). Intense fighting erupts, with targeted attacks on civilians, massive population displacements, “ethnic cleansing” of opposing nationalities, and even genocide. Increasingly, people in these life-threatening situations are finding avenues of escape closed to them. Even when they are able to leave, an increasing number find no country willing to accept them as refugees. As a result, there has been a large increase in the number of internally displaced persons who in the late 1990’s outnumber refugees by as much as two to one. The 1999 World Refugee Survey lists more than 17 million internally displaced persons, but it warns that the total number may be much higher. Sudan leads the list with an estimated 4 million internally displaced persons. Angola and Colombia are estimated to have as many as 1.5 million internally displaced persons each, and Iraq, Afghanistan, Burma, and Turkey have as many as 1 million each. The decrease in the number of refugees reflects a second phenomenon as well: the repatriation of millions of refugees to their home countries. During the 1990’s, large-scale return occurred to a wide range of countries. In Africa alone, repatriation occurred in Angola, Burundi, Eritrea, Ethiopia, Liberia, Mali, Mozambique, Namibia, Rwanda, and Somalia. Other prominent repatriation destinations were Cambodia, Afghanistan, El Salvador, Nicaragua, Guatemala, and Bosnia-Herzegovina and Kosovo. In some cases, return is voluntary because hostilities have truly ended and with peace could come repatriation and reintegration. Too often during the decade, though, refugees along with their internally displaced cousins returned to communities still wracked by warfare and conflict. A range of factors induces such return. Countries of asylum may be weary from having hosted the refugees and place pressure on them to repatriate prematurely. 3 i-counseling.net Refugee Mental Health Donors may also reduce their assistance in the expectation that return will soon take place. The refugees themselves may wish to restake their claim to residences and businesses before others take them, or they may wish to return in time to participate in elections. Families split by hostilities may be eager for reunification. Premature return, particularly when forced, is troubling for two reasons: (1) such repatriation can endanger the refugees who may move from one insecure situation into another; and (2) forced return undermines the entire concept of asylum, that is, a place where refugees can find protection from danger and persecution. In the post-Cold War era, the opportunities to respond to humanitarian tragedies are greater than ever before, though still difficult to seize. While the international community could provide aid and sometimes protection to those who left their countries in the decades after World War II, addressing root causes or bringing aid to victims still inside their countries was limited. Many humanitarian emergencies were triggered by surrogate Cold War conflicts, complicating matters. At the height of superpower rivalry, intervening in the internal affairs of a country allied with either the United States or the Soviet Union could have provoked a massive military response from the other. It was unlikely that the Security Council would authorize such actions. Today, humanitarian intervention has taken place in countries as diverse as the Sudan, Iraq, Bosnia, Somalia, Haiti, and now Kosovo and East Timor. The forms of intervention range from airlifted food drops to outright military action. The results have been mixed. Aid reached otherwise inaccessible people in many of these cases, and, in some cases, peace settlements lessened the immediate reasons for flight and permitted some repatriation to take place. The root causes of displacement have not generally been addressed, however, and internally displaced populations often still remain out of reach. And, safe havens established to protect civilians have too often been vulnerable to attack, leaving civilians still victimized by those committing war crimes and crimes against humanity. U.S. Policies Victims of persecution, human rights violations, and conflict come to the United States in numerous ways, with and without authorization from the Government. The United States offers resettlement to refugees who are processed abroad, as well as asylum to those arriving directly. Under the Refugee Act of 1980, these statuses apply only to individuals who have been persecuted or demonstrate a well-founded fear of future persecution. Persons admitted through the resettlement system or granted asylum may adjust to permanent resident status after 1 year, which puts them on the road to citizenship. The number of refugees resettled in the United States varies each year, determined annually by the President in consultation with Congress. Resettlement is available for refugees who are of special humanitarian concern to the United States. In the early years of the refugee program, resettlement generally was offered to refugees fleeing Communist countries, reflecting U.S. foreign policy. Since the end of the Cold War, however, the program reaches a broader segment of the refugee population, with an emphasis on protecting refugees at risk and providing durable solutions for those with no other alternatives. For fiscal year (FY) 2000, the President authorized admission of up to 90,000 refugees: 47,000 from Europe, divided among nationals of the former Yugoslavia and the former Soviet Union; 18,000 from Africa; 8,000 from east Asia; 8,000 from the near east/ south Asia; 3,000 from Latin America/Caribbean; and 6,000 geographically unallocated. Actual admissions in FY 1999 numbered 85,000, including humanitarian evacuees from Kosovo. Asylum applicants may apply directly through affirmative applications to the Immigration and Naturalization Service (INS) or through defensive applications during a removal hearing in immigration court when apprehended at a port of entry or in the interior of the United States. In affirmative cases, INS may grant asylum or refer the case to an immigration judge for further adjudication. Although there are no limits on the number 4 i-counseling.net Refugee Mental Health of persons who can obtain asylum (with the exception of those applying under a special program for Chinese protesting China’s coercive population control policies), the United States permits a maximum of 10,000 asylees to adjust to permanent residents each year. Preliminary statistics for FY 1999 indicate that about 40,000 asylum cases were filed with INS as affirmative cases. INS approved about 38 percent of the cases that reached final decisions in FY 1999. During the same period, the immigration court received almost 50,000 cases, some referred by the INS asylum office, and others applying as a result of apprehension. The immigration court approved almost 30 percent of all of the cases in which it made a final determination on the merits, granting asylum in about 6,500 cases. Individuals fleeing conflicts and other life-threatening situations, but who have not been granted asylum, may receive Temporary Protected Status (TPS), permitting them to remain within the United States until conditions change in their country of origin. TPS is now available to persons fleeing conflicts and natural disasters in such countries/areas as Nicaragua, Honduras, Kosovo, Sudan, Sierra Leone, and Burundi. Victims of torture who do not qualify for one of these other statuses (for example, because they have committed a crime) may apply for relief from removal if they would risk future torture. The process for obtaining such relief is relatively recent, adopted when the United States passed legislation implementing commitments under the U. N. Convention against Torture. Persons resettled in the United States or granted asylum have work authorization from the time of their admission/grant. By contrast, asylum applicants may not work legally unless the government fails to make an initial determination within 6 months of application. They are also ineligible for public assistance. Most rely on families, community members, or nonprofit agencies, or they work without authorization. Those granted TPS receive work authorization, but they are ineligible for public cash or medical assistance. Refugees and asylees are eligible for time-limited cash and medical assistance as well as social services aimed at assisting them in adjusting to their new homes. Funded by the Office of Refugee Resettlement (ORR) in the Department of Health and Human Services, these services include English language training, employment services, and job training. Assistance and services are provided by state refugee offices, private resettlement agencies, and mutual assistance associations organized by refugees themselves. In recognition of the traumas experienced by many refugees and asylees, ORR has an intraagency agreement with the Refugee Mental Health Program in the Substance Abuse and Mental Health Services Administration to provide refugee mental health consultation; advice and guidance to the refugee resettlement network, State governments, and resettlement agencies; and to serve as the focal point, in the Federal Government, on mental health issues and services for refugees and torture survivors. In addition to these programs, the United States plays an important role internationally in assisting and protecting forced migrants. The United States is one of the principal donors to the international humanitarian aid program, through its contributions to such agencies as the U. N. High Commissioner for Refugees and the U. N. Voluntary Fund for Torture Victims, as well as its support to the International Committee of the Red Cross and other nongovernmental organizations providing relief to the victims of humanitarian crises. In addition, the U.S. military has been actively involved in delivering assistance and participating in humanitarian interventions in such places as northern Iraq, Somalia, Haiti, Bosnia, and Kosovo. Regrettably, the United States has not yet signed the U. N. Convention on the Rights of the Child, which includes significant provisions that enhance protection of children caught in conflict situations. 5 i-counseling.net Refugee Mental Health Refugees and Mental Illness Refugees are at particular risk not only for developing mental disorders but also for failing to receive treatment for these illnesses. Premigration, migration, and postmigration experiences all contribute to the risk. Stressors include acculturation pressures, financial and employment disadvantages, dissonance between traditional sociocultural values and the host country, intergenerational stresses, and social isolation. Legal status can affect the reality of remaining in relative safety in the United States. Often the loss of family members or separation from them can affect mental well-being. Jablensky et al. (1994) have noted the following risk factors for determinants of poor mental health, and these factors occur throughout all phases of the refugee resettlement process. These factors are marginalization and minority factors, socioeconomic disadvantage, poor physical health, starvation and malnutrition, head trauma and injuries, collapse of social supports, mental trauma, and adaptation to host cultures. Psychological distress and impairment in psychosocial function are influenced by individual, family, cultural, and social variables (Ekblad, Ginsburg, Jansson, & Levi, 1994). It is useful to consider the major psychosocial systems that are affected by the refugee experience, both within the individual and across the community as a whole. Ekblad and Silove (1998) suggest the following simplified framework in which five fundamental systems are threatened or disrupted: (1) The attachment system: many refugees are affected by traumatic losses and separations from close attachment figures. (2) The security system: it is common for refugees to have witnessed or encountered successive threats to the physical safety and security of themselves and those close to them. (3) The identity/role system: the refugee experience poses a major threat to the sense of identity of the individual and the group as a whole. Loss of land, possessions, and professions divest individuals of a sense of purpose and status in society. (4) The human rights system: almost all refugees have been confronted with major challenges to their human rights. These include arbitrary and unjust treatment, persecution, brutality, and, in some instances, torture. (5) The existential-meaning system: the refugee experience poses a major threat to the sense of coherence and meaning that stable civilian life usually provides for most communities. According to Jablensky et al. (1994), the most common symptoms and signs that appear in refugees across different cultures include anxiety disorders (i. e., high levels of fear, tension, irritability, and panic), depressive disorders (i. e., sadness, anergia, anhedonia, withdrawal, apathy, guilt, and irritability), suicidal ideation and attempts, anger, aggression and violent behavior (which often finds expression in acts of spouse and child abuse), drug and alcohol abuse, paranoia, suspicion and distrust, somatization and hysteria, and sleeplessness. Boehnlein and Kinzie (1995) have reviewed biological, psychological, and sociocultural models for recognizing, conceptualizing, and treating the psychiatric problems of traumatized refugees. After World War II, a “concentration camp syndrome,” characterized by fatigue, irritability, restlessness, anxiety, and depression, was described in Jewish victims of the Nazi concentration camps (Krupinski et al., 1973). Higher rates of schizophrenia were also found (Eitinger, 1959; Krupinski et al., 1973). Since 1975, with the escape of Southeast Asian refugees to the United States from Vietnam at the end of the Vietnam War and from the killing fields of Pol Pot in Cambodia (1975–1979), the effects of severe trauma were studied in these populations. The most frequent psychiatric diagnoses have been identified as posttraumatic stress disorder (PTSD) and major depression (Boehnlein, Kinzie, Rath, & Fleck, 1985; Kinzie et al., 1990; Kinzie, Fredrickson, Rath, & Fleck, 1984; Kinzie & Jaranson, 1998; Kinzie, Sack, Angell, & Clarke, 1989; Kinzie, Sack, Angell, & Manson, 1986; Kinzie, Tran, Breckenridge, & Bloom, 1980; Krupinski et al., 1973). 6 i-counseling.net Refugee Mental Health In a study of Vietnamese refugees, severity of PTSD and related symptoms was directly correlated with the number of traumatic events (Smith-Fawzi et al., 1997). Although cognitive impairments are subjectively distressing and may be symptoms of PTSD, the increased frequency of head injury among victims of torture could account for some of this impairment (Goldfeld, Mollica, Pesavento, & Farone, 1988). Several other disorders and symptom complexes are common among refugees in general and especially prevalent among torture victims. One of these is the expression of emotional distress in psychological terms, or somatization (Turner & Goest-Unsworth, 1990; Westermeyer, Bouafuely, & Neider, 1989). Although PTSD is classified as an anxiety disorder in the U.S. and international diagnostic manuals, many clinicians do not consider torture survivors and other traumatized refugees as true psychiatric patients because they may be experiencing a normal reaction to an abnormal stressor. Labeling torture symptoms as a mental disorder is seen as a medicalization of a sociopolitical problem. From another perspective, one could speculate that the biological changes occurring in posttraumatic stress override this argument (Friedman & Jaranson, 1994). These changes include abnormal sleep patterns, increased arousal of the nervous system, elevated levels of adrenaline (as in the fight-or-flight response), decreased levels of serotonin (as in depression), lower cortisol levels (although they are higher in depression), and shrinkage of part of the brain, the hippocampus (Shalev &Yehuda, 1998). Among refugees seeking psychiatric care, damage to the central nervous system has been the most common type of biomedical condition (Begovac et al., 1992; Lunde, Rasmussen, Wagner, & Lindholm, 1981). Causes of biomedical illnesses include wounds and other physical assault; prolonged malnutrition; exposure to the elements; lack of medical care for infectious disease such as tuberculosis, HIV/AIDS, and other maladies; injury during refugee flight; and combat wounds (Walker & Jaranson, 1999). Malnutrition plus untreated medical conditions can be especially damaging (Thygesen, Herman, & Willanger, 1970). Refugee women, who with their children account for as much as 80 percent of the refugee population, may experience additional traumas (Martin, 1991). While men are usually the active participants in war, women are often left to respond to the increasing chaos and the breakdowns in their families and communities (Farhood, Zurayk, Chaya, Meshefedjian, & Sidani, 1993; Jensen, 1994; Kaler, 1997; Lifschitz, 1975; Lyons, 1979; Murphy, 1977). In war zones, women continue to be responsible for procuring and preparing food and for caring for children, the elderly, and the ill. They face survival issues every day with massive unemployment, dramatic price increases, lack of fuel, food shortages, shelling, and sniping (Ashford & Huet-Vaughn, 1997; Mann, Drucker, Tarantola, & McCabe, 1994). After women become refugees, they often live in poverty and feel powerless to reduce the stress in their families (D’Avanzo, Frye, & Froman, 1994; Mollica, Wyshak, & Lavelle, 1987). Both women living in war and refugee women are often left to wonder if their husbands or children are alive or dead, leaving them in a living limbo (Agger & Jensen, 1996; Boss, 1999). War-related stress, environmental factors, persistent grief, mourning, loneliness, and isolation tend to predispose women living in war and refugee women to sustained stress that leads to depression (Bryce, Walker, Ghorayeb, & Kanj, 1989; Bryce, Walker, & Peterson, 1989; Farhood et al., 1993; Fox, Cowell, & Johnson, 1995; Lipson, 1993). This is particularly relevant because mothers’ depression and their children’s adjustment are intrinsically linked (Downey, 1990; Field, 1995; Field et al., 1988; Field, Healy, Goldstein, & Guthertz, 1990; Murray, Kempton, Woolgar, & Hooper, 1993). There is evidence that children’s reactions to stress mirror their family’s responses. Symptoms related to trauma in mothers contribute to children’s vulnerability, and the mother’s level of depression has been shown to be the most important predictor of child morbidity (Apetkar & Boore, 1990; Chimienti & Abu Nasr, 1992–1993; Green et al., 1991; Punamaki, 1987). 7 i-counseling.net Refugee Mental Health Rape has a very high rate of acute PTSD and can lead to high rates of chronic PTSD, especially if left untreated (Foa, Rothbaum, Riggs, & Murdock, 1991). Female relatives of persecuted men are also at risk for psychological and health problems (Khamis, 1998). Children and adolescents also face special problems. They may be torture victims, either as a means of demeaning and demoralizing the children themselves or as a means of torturing their parents (Carlin, 1979; Krupinski & Burrows, 1986; Lonigan, Shannon, Taylor, Finch, & Sallee, 1994; consequences, despite having never been tortured themselves (Carlin, 1979; Danieli, 1998; Krupinski & Burrows, 1986; Lonigan et al., 1994; Solkoff, 1992; Westermeyer & Wahmanholm, 1996; Williams & Westermeyer, 1984). Prevalence of Mental Illnesses Among Refugees Since World War II, epidemiological studies and theoretical models of refugee trauma based on biomedical, sociopolitical, and ethnographic perspectives have been conducted in a variety of cultural and ethnic groups. Nonetheless, despite an increase of knowledge about the mental health problems and methods of intervention, the magnitude of the problems is not known. Recent epidemiological evidence indicates that PTSD can be identified across cultures, but it occurs in only a minority of persons exposed to mass conflict; prevalence rates vary between 4 and 20 percent, with higher rates among women (Silove, 1999). Previous studies in refugee clinic populations (Kinzie et al., 1986, 1989) and in refugee camps (Mollica et al., 1993) found a relatively high prevalence of PTSD (greater than 50 percent). More recently, studies among non-treatment-seeking populations have proliferated; however, they have continued to focus on symptoms rather than diagnoses or have not employed rigorous population-based sampling methodology. A controlled study comparing 526 Bhutanese refugee survivors of torture in Nepal with matched controls found that torture survivors had more PTSD symptoms and had higher anxiety and depression scores (Shrestha et al., 1998). In a retrospective cohort study, 35 refugee Tibetan nuns and lay students tortured in Tibet were compared with controls (Holtz, 1998). Torture survivors again had significantly higher anxiety scores than did the nontortured cohort. Similar increased symptom rates were found in tortured Burmese political dissidents in Thailand (Allden et al., 1996). A community sample of Afghan refugee adolescents and young adults living in the United States found high rates of depression (45 percent) and PTSD (13 percent) (Mghir, Freed, Raskin, & Katon, 1995). Amnesty International has estimated that over 150 countries around the world practice government-sponsored torture against their citizens. According to Baker (1992), between 5 percent and 35 percent of refugees have been tortured. It has been estimated that as many as 400,000 torture survivors live in the United States. The actual number of refugees in the United States who have been tortured or terrorized by their former governments is not known (Petersen, 1988), although it is clear from clinical reports and small surveys that the numbers are appreciable (Allodi & Stiasny, 1990; Eitinger, 1959; Westermeyer, 1989a). In the absence of adequate data, it is not possible to state with accuracy the total numbers of torture survivors or whether their needs are met. Coping and Resiliency Refugee mental health challenges may also be understood within the context of refugee resilience and coping capacity. The opportunity to freely practice traditions, beliefs, and customs and to recreate social institutions can serve as protection factors. The following protective factors have been identified (Jablensky et al., 1994): (1) availability of extended family; (2) access to employment; (3) participation in self-help groups; and (4) situational transcendence, or the ability of individuals and groups to frame their status and problems in terms 8 i-counseling.net Refugee Mental Health that transcend the immediate situation and give it meaning (e. g., ethnic identity, cultural history). Preexisting demographic and personality factors can also affect eventual functioning and mental health (McKelvey, Webb, & Mao, 1993). Mental health programs should stimulate these mechanisms of adaptation and foster self-help to minimize helplessness. Programs should help refugees develop coping mechanisms to replace or restore the lost protective factors offered by social networks, religion, and culture. Although it is important to initiate mental health programs during the emergency phase of the refugee crisis, this rarely happens. Cultural Issues According to Morris & Silove (1992), no single theory can adequately encompass the phenomenon of refugee trauma. According to Westermeyer (1987), understanding the larger sociocultural milieu in which the patient functions is crucial in distinguishing psychopathology from culture-bound responses. In assessment and treatment, excessive reliance on models of cultural determinism would be as unproductive, however, as totally disregarding cultural factors. Although survivors of traumatic life events have similar symptoms, cultures differ in the meaning ascribed to the key concepts of trauma and torture. In some cultures, there is reluctance to express emotions or to reveal traumatic experiences, including sexual torture, until trust has been established. Consequently, forcing refugees to tell their story may be counterproductive. In such situations, indirect methods may be more useful (Mollica, 1988). Cultural attitudes toward suffering also play an important role in help-seeking and treatment response (Boehnlein & Kinzie, 1995). For instance, beliefs that suffering is inevitable or that one’s life is predetermined may deter, for example, some Muslims or Buddhists from seeking health care. Cultures traditionally may use medications or religious/traditional ceremonies for treatment and be less familiar with Western mental health interventions. Western approaches tend to emphasize the individual and minimize the importance of the sociocultural context and social networks. Of the Western approaches, the authoritative view of the doctor is more active or directive and often more acceptable (Jaranson, 1991). In group-oriented cultures, intervention-based group activities may be more relevant than individual therapies. Symbolic interventions are particularly relevant, such as supporting the grieving process for lost family members when burial is impossible. Illnesses, tension, and conflicts are resolved in traditional societies through existing inbuilt cultural processes. Interventions that do not recognize these factors could be detrimental (Chakraborty, 1991). Social cohesion and solidarity act as protective forces. Establishing a specialized center may undermine local individual and community responses, except for those survivors who do not receive the social support they need. Over the past several decades, considerable attention has been devoted to matters of translation, including denotation, connotation, and semantic/technical/psychometric equivalence. This work began with Sapir and other linguists and anthropologists during the 1930’s to 1950’s (Hall, 1959), was continued by cultural psychologists in the 1970’s and 1980’s (Brislin, 1970; Butcher & Garcia, 1978; Hulin, 1987) and by psychiatrists doing cross-cultural work (Bravo, Woodbury, Canino, & Rubio-Stipec, 1993; Flaherty et al., 1988; Kinzie et al., 1982; Robins et al., 1988; Sabin, 1975; Westermeyer, 1990), and was developed further by psychiatric epidemiologists concerned with measuring and comparing psychiatric conditions in various populations during the 1980’s and 1990’s (Bravo, Woodbury, Canino, & Rubio-Stepic, 1993; Sartorius, 1989; Westermeyer & Janca, 1997). 9 i-counseling.net Refugee Mental Health Implications for Assessment and Treatment Mainstream professionals often do not wish to know the answers to, or do not know how to ask, the difficult questions. Therapists, especially those who have been traumatized themselves, need skilled supervision to help them deal with their own issues that arise while trying to help others. The sensitive personalities of people motivated to help traumatized refugees, especially torture survivors, can find the pain and suffering distressing. This is also true for interpreters, many of whom have been traumatized themselves as refugees. Since a trusting relationship must be developed for progress to be made, this has the highest priority beyond diagnosis or telling the trauma story. Cultural understanding is essential in choosing the methodology of the assessment. A standard Western psychiatric interview can be toxic (Mollica, 1989; Quiroga & Gurr, 1998). However, using structured interviews and diagnostic instruments as part of the assessment process can have several advantages, such as systematically recording symptoms in a way that elicits more than would otherwise be volunteered by survivors. Some can be self-administrated or administrated by even briefly trained non-professionals to make reasonably accurate diagnoses and to provide information for research purposes. However, there are still problems with diagnostic assessment tools, as has been shown with minor changes leading to major variations in prevalence in epidemiological surveys (Quiroga & Gurr, 1998; Regier et al., 1998), and this has important implications for assessing the need for services. Sensitivity also is required in the physical medical examination, as some survivors can find medical procedures reminiscent of torture experience and become highly anxious and frightened (Jaranson, 1995). The individual’s larger life experiences, personal values, current life situation, family situation, and external social supports are of equal importance to the medical assessments. There are problems if either the medical or the social assessment and actions dominate, as the diversity of the needs of survivors means that some will have medical treatment priorities, some psychological treatment priorities, and others practical assistance priorities. The best psychiatric care considers the multiple health and social service needs of refugees, as well as their other special needs (Kinzie & Jaranson, 1998). Interventions may include not only standard Western treatments such as pharmacotherapy and psychotherapy, but also community approaches and traditional healing, such as cultural, religious, and political dimensions important to the refugee. Traumatized refugees may be reluctant to tell their stories due to shame, lack of trust, or fear of symptom exacerbation, and they should be allowed to reveal information at a pace that is comfortable for them (Jaranson, 1998; Jaranson et al., 1998). In addition to a complete mental status examination and symptom inventory, prior and postmigration experiences, adjustment, and disorders must be assessed (Westermeyer, 1989b). Judicious use of psychotropic medications can reduce symptoms, further the development of trust in the care-providers, and allow further assessment and psychotherapy to proceed (Jaranson, 1991). In many cultures, the medical model is more accepted or better understood than psychotherapy. Education about PTSD, depression, and psychotropic medications is important. A consistent, supportive, nonjudgmental, and culturally competent clinical approach is essential. Since the symptoms and other effects of torture and severe trauma are modulated by bio-psychosocial factors related to the individual, a comprehensive treatment and rehabilitative approach should provide long-term flexible involvement in order to cope with relapses (Kinzie & Jaranson, 1998; Quiroga & Gurr, 1998; Shalev, Bonne, & Eth, 1996). For instance, there is evidence of a chronic fluctuating course in PTSD, which can last a lifetime if untreated (Basoglu, 1993; Basoglu, Jaranson, Mollica, & Kastrup, 1998). There are fluctuations in the revelation of, and reaction to, the trauma experiences, as the survivor’s level of psychological security fluctuates with life events and life stages. Psychological treatment is very important for the more severely affected survivors, and evidence exists that social support may not be of much help unless the survivor is 10 i-counseling.net Refugee Mental Health psychologically healthy enough to access and use it (Basoglu, 1993; Kinzie & Jaranson, 1998; Quiroga & Gurr, 1998). The family is intimately involved and may need as much assistance for indirect trauma and for dealing with the survivor. In order for refugee mental health care to be effective, it is essential that primary health care serve as the main health service infrastructure. The challenge is to orient and train primary health care workers in mental health skills and services, including diagnosis and therapy. Mental health services should be closely coordinated with general health services, psychosocial services, and other relevant rehabilitation, social, educational, occupational, cultural, and recreational activities. Mental health services should be community based, and, wherever possible, focus on early intervention at the primary, secondary, and tertiary levels of prevention. Mental health services should be sensitive to gender and cultural issues and the needs of particular demographic groups, as well as to high-risk groups such as the physically injured and disabled, the severely mentally disabled, and survivors of extreme trauma, torture, and sexual abuse. In addition, the doctor must be sensitive to the differing ethnic responses to psychotropic medications in metabolism, nutritional status, age, smoking, and drug interactions. According to Shalev, Bonne, and Eth (1996), the main outcome goal for therapy is increased functionality to achieve personal goals, rather than symptom reduction. However, symptom reduction may also be a goal, particularly for high levels of the positive symptoms of PTSD, major depression, or other disorders that respond to medication. These disorders require a combination of medical, psychological, social, and legal intervention. However, the reality is that most refugees do not get formal help. It is important to train community members to recognize signs of torture and trauma and to inform torture survivors that they are not alone, that their reactions and symptoms are not unusual. The advantages of this approach, conducted by members of the community, include minimizing linguistic or cultural barriers and providing better capacity to screen people needing services. Disadvantages include the need for supervision and limited capacity for diagnosis or provision of psychotherapy. Challenges and Opportunities Despite the growth in expertise, experience, and knowledge about mental health issues affecting forced migrants, there are many barriers to use of this information to improve policy and programmatic responses. In part, the barriers reflect failures of communication between scientists, service providers, and policymakers. Research is not necessarily formulated or packaged in a manner that translates readily into new program designs or policy approaches. Service providers and policymakers, often moving quickly from one crisis to another, have little time to review the research literature to assess its implications for programs or policies. Moreover, issues raised by the refugee mental health literature cross many fields of expertise, but there is considerable fragmentation of responsibility for forced migration within the United States and, even more so, within the international community. The barriers also reflect basic realities in the delivery of services to forced migrants. Refugee and other forced movements tend to be defined as emergencies requiring emergency responses. These responses tend, in turn, to be defined in logistical terms: how many tents and how many tons of food, clothing, and medicines can be delivered in the shortest time possible. Failure to respond quickly and efficiently to these immediate needs may result in thousands of deaths. The emergency paradigm makes sense in some cases— for example, the rapid exodus and then repatriation of Kosovars— but many refugee situations would be described more properly as protracted crises, with displacement continuing for years. 11 i-counseling.net Refugee Mental Health Even in developed countries with the resources and expertise to respond to emergencies, large-scale forced migration presents logistical challenges. In many cases, the migrants arrive without authorization and are unwilling to present themselves to the authorities for fear of return to their home countries. Humanitarian evacuations, such as occurred from Southeast Asia in the late 1970’s and Macedonia during the height of the Kosovo crisis, present particular challenges as refugees arrive, having had little opportunity for planning or preparation. Often overlooked in responding to the emergency are the actual people who are in flight. Their non-material needs are much more difficult to quantify. The after-effects of rape and witnessing murder are far more difficult to address than are the after-effects of an empty stomach. Food and shelter may serve the most immediate needs of the small child separated from his or her parents, but the emotional and psychological effects of this loss also require attention. Even with the best will in the world to tackle these nonmaterial needs, budgets constrain options for services. In 2000, the United Nations issued a consolidated appeal for 17 complex emergencies, requesting almost $3 billion in assistance. The appeal covers all of the U. N. agencies that assist the victims of humanitarian crises— refugees, internally displaced persons, and other war-affected populations. It does not include resources for new emergencies that may occur during the course of the year. Generally, contributions fall short of the requested amount. UNHCR reported a shortfall of $185 million in its 1999 budget of $1.2 billion (which includes funds beyond what were requested in the consolidated appeals process). The situation is likely to be no better in 2000. In the United States, for example, Congress appropriated $625 million to support overseas refugee assistance programs as well as resettlement of refugees, $52.5 million less than the President requested. In a budgetary climate in which it is difficult to raise funds for basic food, shelter, and security needs, providing funding for mental health services may appear foolhardy. From a policymaker’s point of view, the literature on the psychosocial needs of refugees and other forced migrants presents a daunting picture. The prevalence of experiences that could trigger mental health problems appears staggeringly high. The potential client base for any programs could number in the millions. Further complicating the problem is access to those needing services. Many of the most vulnerable forced migrants are internally displaced, often trapped in conflict zones and out of reach by the international community. Refugees and displaced persons who reach relative safety may be able to avail themselves of services, but life remains highly insecure for them as well. Tending to basic needs, particularly for refugee women who are often responsible for water, food, and firewood collection in addition to other household and childcare duties, often precludes participation in programs. Even after reaching resettlement countries, refugees engage in survival activities that may mask their need for psychosocial services while restricting their ability to access programs that are available to them. Resettled refugees, in fact, have a much wider array of services available than do other forced migrants arriving in the United States having had similar experiences. As discussed above, the Federal Government provides social service grants to private agencies and State governments and has an office specifically responsible for refugee mental health issues. By contrast, forced migrants who arrive in the United States other than through the resettlement program have access to few services. The U.S. Committee for Refugees (1999) has said: Psychological support for asylum seekers and survivors of torture who do not arrive under an organized resettlement program is particularly tenuous. Asylum seekers face legal uncertainty 12 i-counseling.net Refugee Mental Health and lack access to the social services afforded to resettled refugees, factors that compound problems associated with their lack of psychological support. Asylum seekers often require access to such services, not only to address their mental health problems but also to underscore the credibility of their asylum claims. Mental health professionals are often asked to certify the likelihood that an applicant experienced the torture or persecution alleged in the application. Improving responses requires actions at several different levels. The most effective responses would, of course, address the causes of forced migration through prevention strategies that protect human rights, avert conflicts, and improve economic development. Clearly, reducing the traumas that force people to migrate for safety will reduce the need for refugee mental health programs. Since such strategies require interventions far beyond the capacities of professionals working in the refugee or mental health fields, practical steps must be taken in the interim to increase access to appropriate services. Training and preparation of all staff with responsibilities for refugee assistance and protection will be necessary if significant improvement is to be made in addressing the psychosocial needs of refugees and other forced migrants. Since all decisions made in refugee emergencies hold the potential for increasing or reducing trauma, it is important that the mental health implications of decisions be taken into account. For example, human rights monitors who interview refugees to document war crimes may trigger posttraumatic stress responses as the refugees tell of their personal experiences. In addition, a cadre of specialists may be needed for quick responses, people who can get out at the start of an emergency to interview refugees, get an index of what the problems are, design low-cost responses, and train field staff as needed. Training of refugees themselves to take responsibility for problems as they arise is also a key element of a more effective response. Improving refugee mental health programs will also require changes in organizational roles and the deployment of institutional resources. At the international level, greater attention needs to be paid to determining which agencies among those responsible for refugees and forced migrants should take the lead regarding mental health issues. In addition to the UNHCR, the World Health Organization and UNICEF (U. N. International Children’s Emergency Fund) have mandates in this area. Ultimately, addressing more broadly the mental health and psychosocial needs of refugees will require financial resources. Through the consolidated appeal process, the U. N. agencies should determine what additional funding will be needed to respond more effectively. Within the United States, most programs designed to care for new Americans have faced overwhelming obstacles to survival. Although Federal law requires health care organizations to provide interpreters for nonEnglish-speaking patients, enforcement has been inconsistent. Interpretation increases the complexity and cost of providing health care services. Few programs have survived by depending solely upon third-party reimbursement, and local, State, Federal, or private foundation funding is usually required for sustainability. Realizing these obstacles, the U.S. Congress passed the Torture Victims Relief Act in October 1998, providing funding for torture rehabilitation programs both in the United States and abroad. However, no comparable Federal legislation to care for refugees and asylum seekers traumatized in other ways has been passed. Research Priorities According to Rosenheck and Fontana (1999), research on the delivery of health care services for PTSD can be thought of as addressing the following three goals: • Severity/Burden of Disease. Service use, along with epidemiological data on disease prevalence, is an indicator of the burden of disease on the general population and its economic consequences. Kessler et 13 i-counseling.net Refugee Mental Health al. (1999), in the National Comorbidity Survey, shows that PTSD is associated with nearly the highest rate of service use, and, by implication, the highest per-capita cost of any mental health disorder. This shows the central importance of PTSD for the public’s mental health. Rosenheck and Fontana also conclude that PTSD is also associated with high levels of use of non-mental health services. • Access to Care. Studies of service utilization provide information on the accessibility of services (i. e., the success or failure of the health care system to address the needs of its target population). Rosenheck and Fontana found that survivors of human-made disasters were reluctant to use mental health services because of the fear that painful memories would be aroused. • Outcome, Cost, and Value. Studies of service utilization are important to simultaneously evaluate the effectiveness and cost of services (i. e., their ultimate value to the public). Although medical care has traditionally focused its research efforts on individual patients and illnesses, new research methods and perspectives are increasingly operationalized to correct these deficiencies. Before starting a study, it is of crucial importance to consider theoretical dilemmas (i. e. emicetic perspectives regarding both diagnostic and outcome measures following severe but different traumatic life events). Researchers should also clarify the definitions of key concepts such as refugee versus immigrant; differences in ethnic, educational, religious, and socioeconomic backgrounds; and reasons for immigration. It must also be kept in mind that research conducted with refugees from countries where ethnic conflicts are still active can easily be affected by such conflicts. Further, from an ethical point of view it is important that the refugee who is to be interviewed does not have the feeling of being investigated by the police or courts. Time should be allowed for the necessary trust to develop. Before starting, the responsibility for various parts of the work should be clarified. The study site should be located close to the researchers, and a frequent dialogue of training and supervision take place between the researchers and practitioners, minimizing the need for gatekeepers. The cultural and language competence of the interviewer is important in the contact with the interviewees, but this competence is easily transformed into difficulties when transference/countertransference processes occur. Transcultural validity, the concept of equivalence, and appropriate methods, with their limitations, are of concern. An integration of quantitative and qualitative methods provides the best possibility for understanding the complex issues affecting the mental health of refugees. The study of methods to avoid burnout or vicarious traumatization among mental health providers is also relevant. Since funding is scarce, identifying effective rehabilitation models is essential. Controlled randomized clinical trials are needed in order to develop brief and cost-effective mental health programs for refugees. Of pressing importance are clinical outcome studies, few of which exist (Mollica et al., 1990) because of the lack of control groups, definitions of diagnostic criteria, validation of assessment instruments, and many other obstacles. A set of standards and measures of outcome should be included in research designs. International collaborative crosscultural studies would facilitate research on policy studies, methodological issues, technical issues in refugee health care, and the generic and culture-specific risk and resilience responses to traumatic life events and PTSD. 14 i-counseling.net Refugee Mental Health References Agger, I., & Jensen, S. (1996). Trauma and healing under state terrorism. London and New Jersey: Zed Books. Allden, K., Poole, C., Chantavanich, S., Ohmar, K., Aung, N. N., & Mollica, R. F. (1996). Burmese political dissidents in Thailand: Trauma and survival among young adults in exile. American Journal of Public Health, 86(11), 1561–1569. Allodi, F., & Stiasny, S. (1990). Women as torture victims. Canadian Journal of Psychiatry, 35, 144–148. Anonymous. A cry for help: Refugee mental health in the United States. (1997). Refugee Reports, 18(9). Apetkar, L., & Boore, J. (1990). The emotional effects of disaster on children: A review of the literature. International Journal of Mental Health, 19(2), 77. Ashford, M., & Huet-Vaughn, Y. (1997). The impact of war on women. In B. Levy & V. Sidel (Eds.), War and public health (pp. 186–196). New York: Oxford University Press. Baker R. (1992). Psychosocial consequences for tortured refugees seeking asylum and refugee status in Europe. In M. Basoglu (Ed.), Torture and its consequences: Current treatment approaches (pp. 83–101). Cambridge: Cambridge University Press. Basoglu, M. (1993). Prevention of torture and care of survivors: An integrated approach. JAMA, 270, 606–611. Basoglu, M., Jaranson, J., Mollica, R., & Kastrup, M. (1998). Torture and its consequences. In T. Keane, E. Gerrity, & F. Tuma, (Eds.), Mental health consequences of torture and related violence and trauma. Preliminary report prepared for the Truth and Reconciliation Commission by a Working Group sponsored by the National Institute of Mental Health. Begovac, J., Jeren, T., Kuzman, I., Jukic, V., Ravlic, Z., & Andrasevic, S. (1992). Health status of 1458 Croatian prisoners of war. JAMA, 270( 5), 574–575. Boehnlein, J. K., & Kinzie, J. D. (1995). Refugee trauma. Overview. Transcultural Psychiatric Research Review, 32, 223–252. Boehnlein, J. K., Kinzie, J. D., Rath, B., & Fleck, J. (1985). One year follow-up study of posttraumatic stress disorder among survivors of Cambodian concentration camps. American Journal of Psychiatry, 142, 956–959. Boss, P. (1999). Ambiguous loss: Learning to live with unresolved grief. Cambridge, MA: Harvard University Press. Bravo, M., Woodbury, F. M., Canino, G., & Rubio-Stipec, M. (1993). The Spanish translation and cultural adaptation of the Diagnostic Interview Schedule for Children (DISC) in Puerto Rico. Culture, Medicine and Psychiatry, 17, 329–344. Brislin, R. (1970). Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology, 1, 185– 216. Bryce, J., Walker, N., Ghorayeb, F., & Kanj, M. (1989). Life experiences, response styles and mental health among mothers and children in Beirut, Lebanon. Social Science and Medicine, 28, 685–695. 15 i-counseling.net Refugee Mental Health Bryce, J., Walker, N., & Peterson, C. (1989). Predicting symptoms of depression among women in Beirut: The importance of daily life. International Journal of Mental Health, 18, 57–70. Butcher, J. N., & Garcia, R. (1978). Cross-national application of psychological tests. Personnel Guidance, 56, 472–475. Carlin, J. E. (1979). Southeast Asian refugee children. In J. D. Call, J. D. Noshpitz, R. L. Cohen, & I. N. Berlin, (Eds.), Basic handbook of child psychiatry. New York: Basic Books. Chakraborty, A. (1991). Culture, colonialism, and psychiatry. Lancet, 337, 1204–1207. Chimienti, G., & Abu Nasr, J. (1992–1993). Children’s reactions to war related stress II. The influence of gender, age, and the mother’s reaction. International Journal of Mental Health, 21(4), 72–86. Danieli, Y. (Ed.). (1998). International handbook of multi-generational legacies. D’Avanzo, C., Frye, B. & Froman, R. (1994). Stress in Cambodian refugee families. Image: The Journal of Nursing Scholarship, 26( 2), 101–105. Downey, G. (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108(1), 50–76. Eitinger, L. (1959). The incidence of mental disorders among refugees in Norway. Journal of Mental Science, 105, 326–338. Ekblad, S., Ginsburg, B.-E., Jansson, B., & Levi, L. (1994). Psychosocial and psychiatric aspects of refugee adaptation and care in Sweden. In A. J. Marsella, T. Bornemann, S. Ekblad, & J. Orley (Eds.), Amidst peril and pain. The mental health and well-being of the world’s refugees (pp. 275–292). Washington, DC: American Psychological Association. Ekblad, S., & Silove, D. (1998, August 18). Proposals for the development of mental health and psychosocial services in refugee camps. Geneva: Consultant Mission Report to UNHCR. Farhood, L., Zurayk, H., Chaya, S. F., Meshefedjian, G., & Sidani, T. (1993). The impact of war on the physical and mental health of the family: The Lebanese experience. Social Science and Medicine, 36( 12), 1555–1567. Field, T. Psychologically depressed parents. (1995). In M. Bornstein (Ed.), Handbook of parenting: Volume 4. Applied and practical parenting (pp. 85–99). Mahwah, NJ: Lawrence Erlbaum Associates. Field, T., Healy, B., Goldstein, S., & Guthertz, M. (1990). Behavior state matching in mother-infant interactions of nondepressed versus depressed mother-infant dyads. Developmental Psychology, 26, 7–14. Field, T., Healy, B., Goldstein, S., Perry, S., Bendell, D., Schanberg, S., Zimmerman, E., & Kuhn, C. (1988). Infants of depressed mothers show “depressed” behavior even with nondepressed adults. Child Development, 59, 1569–1579. Flaherty, J. A., Gaviria, F. M., Pathak, D., Mitchell, T., Wintrob, R., Richman, J. A., & Birz, S. (1988). Developing instruments for cross-cultural psychiatric research. Journal of Nervous and Mental Disease, 176(5), 257–263. 16 i-counseling.net Refugee Mental Health Foa, E. B., Rothbaum, B. O., Riggs, D. S., & Murdock, T. B. (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal Consulting Counseling Psychology, 59(5), 715–723. Fox, G., Cowell, J., & Johnson, M. (1995). Effects of family disruption on Southeast Asian refugee women. International Nursing Review, 42(1), 27–30. Friedman, M., & Jaranson, J. (1994). The Applicability of the Post-Traumatic Concept to Refugees In A. J. Marsella, T. Bornemann, S. Ekblad, & J. Orley (Eds.), Amidst peril and pain. The mental health and well-being of the world’s refugees (pp. 207–227). Washington, DC: American Psychological Association. Goldfeld, A. E., Mollica, R. F., Pesavento, B. H., & Farone, S. V. (1988). The physical and psychological sequelae of torture. JAMA, 259, 2725–2729. Green, B., Korol, M., Grace, M., Vary, M., Leonard, A., Gleser, G., & Smitson-Cohen, S. (1991). Children and disaster: Age, gender, and parental effects on PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 30(6), 945–951. Holtz, T. H. (1998). Refugee trauma versus torture trauma: a retrospective controlled cohort study of Tibetan refugees. Journal of Nervous and Mental Disease, 186(1), 24–34. Hulin, C. L. (1987). A psychometric theory of evaluations of item and scale translations: Fidelity across languages. Journal of Cross-Cultural Psychology, 18(2), 115–142. Jablensky, A., Marsella, A. J., Ekblad, S., Jansson, B., Levi, L., & Bornemann, T. (1994). Refugee mental health and well-being: Conclusions and recommendations. In A. J. Marsella, T. Bornemann, S. Ekblad, & J. Orley (Eds.), Amidst peril and pain. The mental health and well-being of the world’s refugees (pp. 327–339). Washington, DC: American Psychological Association. Jaranson, J. (1991). Psychotherapeutic medication. In J. Westermeyer et al. (Eds.), Mental health services for refugees (pp. 132–145). Washington, DC: National Institute of Mental Health, DHHS #(ADM) 91-1824. Jaranson, J. (1995). Governmental torture: Status of the rehabilitation movement. Transcultural Psychiatric Research Review, 32(3), 253–286. Jaranson, J. (1998). The science and politics of rehabilitating torture survivors. In J. Jaranson & M. Popkin (Eds.), Caring for victims of torture (pp. 15–40). Washington, DC: American Psychiatric Press. Jaranson, J., Kinzie, J. D., Friedman, M., et al. (1998). Assessment, diagnosis, and intervention. In T. Keane, E. Gerrity, & F. Tuma (Eds.), Mental health consequences of torture and related violence and trauma. A preliminary report prepared for the Truth and Reconciliation Commission (of South Africa) by a Working Group sponsored by the National Institute of Mental Health, Rockville, MD. Jensen, S. (1994). Psycho-social stresses and protective factors in families under war conditions and peace building in former Yugoslavia. In L. Arcel (Ed.), War victims and psychosocial care (pp. 72–80). Zagreb, Croatia: European Community Task Force. Kaler, A. (1997). Maternal identity and war in mothers of the revolution. NWSA Journal, 9(1), 1–21. 17 i-counseling.net Refugee Mental Health Kessler, R. C., Zhao, S., Katz, S. J., Kouzis, A. C., Frank, R. G., Edlund, M. J., & Leaf, P. (1999). Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry, 156, 115–123. Khamis, V. (1998). Psychological distress and well-being among traumatized Palestinian women during the Intifida. Social Science and Medicine, 46(8): 1033–1041. Kinzie, J. D., Boehnlein, J. K., Leung, P., Moore, L., Riley, C., & Smith, D. (1990). The high prevalence rate of PTSD and its clinical significance among Southeast Asian refugees. American Journal of Psychiatry, 147, 913–917. Kinzie, J. D., Fredrickson, R. H., Rath, B., & Fleck, J. (1984). Post-traumatic stress disorder among survivors of Cambodian concentration camps. American Journal of Psychiatry, 141, 645–650. Kinzie, J. D., & Jaranson, J. Refugees and asylum seekers. (1998). In T. Keane, E. Gerrity, & F. Tuma (Eds.), Mental health consequences of torture and related violence and trauma. A preliminary report prepared for the Truth and Reconciliation Commission (of South Africa) by a Working Group sponsored by the National Institute of Mental Health, Rockville, MD. Kinzie, J. D., Manson, S. M., Vinh, D. T., Nguyen, T., Bui, A., & Than, P. (1982). Development and validation of a Vietnamese language depression rating scale. American Journal of Psychiatry, 139(10), 1276–1281. Kinzie, J. D., Sack, W. H., Angell, R. H., & Clarke, G. (1989). A three-year follow-up of Cambodian young people traumatized as children. Journal of the American Academy of Child and Adolescent Psychiatry, 28, 501–504. Kinzie, J. D., Sack, W. H., Angell, R. H., & Manson, S. (1986). The psychiatric effects of massive trauma on Cambodian children: I. The children. Journal of the American Academy of Child Psychiatry, 25, 370–376. Kinzie, J. D., Tran, K. A., Breckenridge, A., & Bloom, J. D. (1980). An Indochinese refugee psychiatric clinic: Culturally accepted treatment approaches. American Journal of Psychiatry, 137, 1429–1432. Krupinski, J., & Burrows, G. (1986). The price of freedom: Young Indochinese refugees in Australia. Sydney: Pergamon Press. Krupinski, J., Stoller, A., & Wallace, L. (1973). Psychiatric disorders in East European refugees now in Australia. Social Science and Medicine, 7, 331–349. Lifschitz, M. (1975). Long-range effects of father’s loss: The cognitive complexity of bereaved children and their school adjustment. British Journal of Medical Psychology, 49, 187–197. Lipson, J. (1993). Afghan refugees in California: Mental health issues. Issues in Mental Health Nursing, 14, 411–423. Lonigan, C. J., Shannon, M. P., Taylor, C. M., Finch, A. J., & Sallee, F. R. (1994). Children exposed to disaster: II. Risk factors for the development of post-traumatic symptomatology. Journal of the American Academy of Child and Adolescent Psychiatry, 33(1), 94–105. Lunde, I., Rasmussen, O. V., Wagner, G., & Lindholm, J. (1981). Sexual and pituitary-testicular function in torture victims. Archives of Sexual Behavior, 10(1), 25–32. 18 i-counseling.net Refugee Mental Health Lyons, H. (1979). Civil violence. The psychological aspects. Journal of Psychosomatic Research, 23, 373–393. Mann, J., Drucker, E., Tarantola, D., & McCabe, M. (1994). Bosnia: The war against public health. Medicine and Global Survival, 1(3), 130–146. Martin, S. F. (1991). Refugee women. London: Zed Press. McKelvey, R. S., Webb, J. A., & Mao, A. R. (1993). Premigratory risk factors in Vietnamese Amerasians. American Journal of Psychiatry, 150(3), 470–473. Mghir, R., Freed, W., Raskin, A., & Katon, W. (1995). Depression and posttraumatic stress disorder among a community sample of adolescents and young adult Afghan refugees. Journal of Nervous and Mental Disease, 183, 24–30. Mollica, R. (1988). The trauma story: the psychiatric care of refugee survivors of violence and torture. In F. M. Ochberg (Ed.), Post-traumatic therapy and victims of violence. New York: Brunner/Mazel. Mollica, R. F., Donelan, K., Tor, S., Lavelle, J., Elias, C., Frankel, M., & Blendon, R. J. (1993). The effect of trauma and confinement on functional health and mental health status of Cambodians living in ThailandCambodia border camps. JAMA, 270, 581–586. Mollica, R. F., Wyshak, G., & Lavelle, J. (1987). The psychosocial impact of war trauma and torture on Southeast Asian refugees. American Journal of Psychiatry, 144(12), 1567–1572. Mollica, R. F., Wyshak, G., Lavelle, J., Troung, T., Tor, S., & Yang, T. (1990). Assessing symptoms change in South East Asian refugee survivors of mass violence and torture. American Journal of Psychiatry, 147, 83–88. Morris, P., & Silove, D. (1992). Cultural influences in psychotherapy with refugee survivors of torture and trauma. Hospital and Community Psychiatry, 43, 820–824. Murphy, J. (1977). War stress and civilian Vietnamese: A study of psychological effects. Acta Psychiatrica Scandinavica, 56, 92–108. Murray, C., & Lopes, A. (1996). Global burden of diseases. Geneva, Switzerland: World Health Organization. Murray, L., Kempton, C., Woolgar, M., & Hooper, R. (1993). Depressed mothers’ speech to their infants and its relation to infant gender and cognitive development. Journal of Child Psychology and Psychiatry, 34(7), 1083–1101. Petersen, H. D. (1988). The controlled study of torture victims: Epidemiological consideration and some future aspects. Scandinavian Journal of Social Medicine, 17, 13–20. Punamaki, R. (1987). Psychological stress responses of Palestinian mothers and their children in conditions of military occupation and political violence. Quarterly Newsletter of the Laboratory of Comparative Human Cognition, 9, 76. Quiroga, J., & Gurr, R. (1998, October). Approaches to torture rehabilitation. A desk study, covering effects, cost effectiveness, participation and sustainability. Manuscript commissioned by DANIDA, through Lars Adam Rehof, Human Rights Consultancy, Copenhagen, Denmark. 19 i-counseling.net Refugee Mental Health Regier, D. A., Kaelber, C. T., Rae, D. S., Farmer, M. E., Knauper, B., Kessler, R. C., & Norquiest, G. S. (1998). Limitations of diagnostic criteria and assessment instruments for mental disorders: Implications for research and policy. Archives of General Psychiatry, 55( 2), 109–115. Robins, L. N., Wing, J., Wittchen, H. U., Helzer, J. E., Babor, T. F., Burke, J., Farmer, A., Jablenski, A., Pickens, R., Regier, D. A., et al. (1988). The Composite International Diagnostic Interview: An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry, 45, 1069–1077. Rosenheck, R. A., & Fontana, A. (1999). Delivery of services for PTSD. The National Center for PostTraumatic Stress Disorder. PTSD Research Quarterly, 3. Sabin, J. E. (1975). Translating despair. American Journal of Psychiatry, 132, 197–199. Sartorius, N. (1989). Making of a common language for psychiatry: Development of the classification of mental, behavioral and developmental disorders in the 10th revision of the I. C. D. WPA Bulletin, 1(1): 3–6. Shalev, A. Y., Bonne, O., & Eth, S. (1996). Treatment of post traumatic stress disorder: A review. Psychosomatic Medicine, 58, 165–182. Shalev, A. Y., & Yehuda, R. (1998). Longitudinal development of traumatic stress disorders. In R. Yehuda (Ed.), Psychological trauma. Washington, DC: American Psychiatric Press. Shrestha, N. M., Sharma, B., Van Ommeren, M., Regmi, S., Makaju, R., Komproe, I., Shrestha, G. B., & deJong, J. T. V. M. (1998). Impact of torture on refugees displaced within the developing world: Symptomatology among Bhutanese refugees in Nepal. JAMA, 280(5), 443–8. Silove, D. (1999). The psychological effects of torture, mass human rights violations, and refugee trauma. Journal of Nervous and Mental Disease, 187, 200–207. Smith-Fawzi, M. C., Pham, T., Lin, L., Nguyen, T. V., Mur-phy, E., & Mollica, R. E. (1997). The validity of Post-traumatic Stress Disorder among Vietnamese refugees. Journal of Traumatic Stress, 10(1), 101–108. Solkoff, N. (1992). The Holocaust: survivors and their children. In M. Basoglu (Ed.), Torture and its consequences: Current treatment approaches (pp. 136–148). Cambridge: Cambridge University Press. Thygesen, P., Herman, K., & Willanger, R. (1970). Concentration camp survivors in Denmark. Danish Medical Bulletin, 17, 65–108. Turner, S., & Goest-Unsworth, C. (1990). Psychological sequelae of torture: A descriptive model. British Journal of Psychiatry, 157, 475–480. U.S. Committee for Refugees (USCR). (1999). World Refugee Survey. Washington, DC: U.S. Committee for Refugees. U.S. Department of Health and Human Services. (1999). Mental health: A report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health. 20 i-counseling.net Refugee Mental Health US reminder on mental health burden. (2000). Lancet, 355, 1. Walker, P. F., & Jaranson, J. (1999). Refugee and Immigrant Health Care. Medical clinics of North America, 83(4), 1103–1120. Westermeyer, J. (1987). Clinical considerations in cross-cultural diagnosis. Hospital and Community Psychiatry, 38, 160–165. Westermeyer, J. (1989a). Paranoid symptoms and disorders among 100 Hmong refugees: a longitudinal study. Acta Psychiatrica Scandanavica, 80(1), 47–59. Westermeyer, J. (1989b). In J. H. Gould (Ed.), Psychiatric care of migrants: A clinical guide. Washington, DC: American Psychiatric Press. Westermeyer, J. (1990). Working with an interpreter in psychiatric assessment and treatment. Journal of Nervous and Mental Disease, 178, 745–749. Westermeyer, J., Bouafuely, M., & Neider, J. (1989). Somatization among refugees: An epidemiological study. Psychosomatics, 30, 34–43. Westermeyer, J., & Janca, A. (1997). Language, culture, and psychopathology. Transcultural Psychiatry, 34(3), 291–311. Westermeyer, J., & Wahmanholm, K. (1996). Refugee children. In Children in war and communal violence: A mental health handbook. New Haven, CT: Yale University Press. Williams, C., & Westermeyer, J. (1984). Psychiatric problems among adolescent Southeast Asian refugees: A descriptive study. Journal of Nervous and Mental Disease, 171, 79–85. 21