Detection of TEM-, SHV- and CTX-M-type b
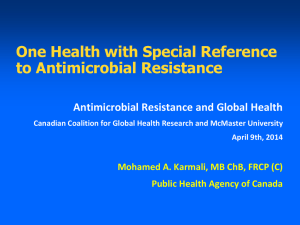
advertisement

Journal of Medical Microbiology (2014), 63, 962–967 DOI 10.1099/jmm.0.068486-0 Detection of TEM-, SHV- and CTX-M-type b-lactamase production among clinical isolates of Salmonella species Sathishkumar Elumalai,1 G. Muthu,2 R. Esther Mary Selvam3 and Srivani Ramesh1 Correspondence Srivani Ramesh srivani.ramesh@gmail.com 1 Department of Microbiology, Dr ALM Post Graduate Institute of Basic Medical Sciences, University of Madras, Taramani, Chennai 600 113, Tamil Nadu, India 2 Central Research Laboratory, Sri Manakula Vinayagar Medical College and Hospital, Madagadipet, Pondicherry 605 107, India 3 Department of Microbiology, ESIC Hospital, K. K. Nagar, Chennai 600078, Tamil Nadu, India Received 19 September 2013 Accepted 10 May 2014 Enteric fever is a major public health problem in developing countries. Due to the problem of resistance to first-line drugs and fluoroquinolone, cephalosporins are currently used for treatment of enteric fever. Cephalosporin resistance in Salmonella spp. is mainly due to production of extended-spectrum b-lactamases (ESBLs). The majority of ESBLs in Salmonella are derivatives of the TEM and SHV b-lactamase families. The objectives of this study were to detect antibiotic susceptibility patterns, ESBL production and TEM-, SHV- and CTX-M-encoding genes (blaTEM, blaSHV and blaCTX-M) among clinical isolates of Salmonella spp. A total of 134 Salmonella isolates [Salmonella Typhi (n5101), Salmonella Paratyphi A (n531), Salmonella Paratyphi B (n51) and Salmonella Typhimurium (n51)] were included in this study. Multidrug resistance was seen in 5/ 134 (3.73 %) isolates, all of which belonged to serotype S. Typhi. A better susceptibility profile was observed for first-line drugs (ampicillin, chloramphenicol, co-trimoxazole and tetracycline) and cephalosporins (cefotaxime, ceftazidime, ceftriaxone, cefixime and cefepime). However, 131 (97.76 %) of the 134 isolates were resistant to nalidixic acid and one (0.75 %) was resistant to ciprofloxacin. TEM-1-type b-lactamase (blaTEM-1) was detected in six (4.47 %) of the 134 isolates, which belonged to the serotype S. Typhi. All six TEM-positive isolates were negative for the blaSHV gene and none of the isolates was positive for the blaCTX-M gene. The presence of the blaTEM gene encoding TEM-1 b-lactamase is believed to confer resistance only to penicillins and early cephalosporins; however, the resistance spectrum of TEM-1 descendants may extend to second-, third- and fourth-generation cephalosporins. The ESBLs derived from TEM-1 differ from their progenitors by as few as 1 aa, and have the ability to hydrolyse third-generation cephalosporins. Therefore, appropriate selection and rotation of antibiotics as well as continuous monitoring of antibiotic susceptibility profiles could help to control the emergence and spread of resistant strains. INTRODUCTION Enteric fever includes typhoid and paratyphoid fever. It is an important public health problem caused by Salmonella enterica serovar Typhi and S. enterica serovars Paratyphi A, B and C respectively. Both serotypes are solely human pathogens. Infection occurs mainly due to ingestion of food or water contaminated with human waste (Scherer & Abbreviations: ESBL, extended-spectrum b-lactamase; MDR, multidrug resistant. The GenBank/EMBL/DDBJ accession number for the Salmonella enterica serovar Typhi strain determined in this study is KF551994. 962 Miller, 2001). Typhoid fever is a major cause of morbidity and mortality, estimated to cause 21.7 million illnesses and 217 000 deaths per year, whereas paratyphoid fever causes illness in an estimated 5.4 million people per year worldwide (Crump et al., 2004). Appropriate treatment reduces the mortality rate as low as 0.5 % (Cooke & Wain, 2004). Multidrug-resistant (MDR) S. enterica (resistant to chloramphenicol, ampicillin and trimethoprim-sulfamethoxazole) has emerged worldwide in the last two decades (Madhulika et al., 2004). Invasive Salmonella infections can be treated with fluoroquinolones and b-lactam (cephalosporins) antibiotics (Rotimi et al., 2008). However, S. Downloaded from www.microbiologyresearch.org by 068486 G 2014 The Authors IP: 78.47.19.138 On: Sat, 01 Oct 2016 08:48:55 Printed in Great Britain TEM-, SHV- and CTX-M-type ESBLs in Salmonella spp. enterica isolates have developed resistance to fluoroquinolones in the Indian subcontinent and other regions (Effa & Bukirwa, 2008). In Salmonella, resistance to cephalosporins is largely due to the production of extended-spectrum b-lactamases (ESBLs) and is often plasmid mediated (Rotimi et al., 2008). The majority of ESBLs in Salmonella are derivatives of the TEM and SHV b-lactamase families. Other b-lactamases like CTX-M have also been described in Salmonella (Bradford, 2001; Bonnet, 2004). CTX-M-type ESBLs or cefotaximases are encoded by blaCTX-M genes located on a plasmid or on the chromosome (Rodriguez et al., 2004). Studies on ESBLproducing Salmonella strains have revealed the presence of insertion sequence ISEcp1 upstream of the blaCTX-M gene, which may contribute to the mobility and dissemination of these genes to other bacteria in the environment (Sjölund et al., 2008; Tamang et al., 2011). In this background, the present study was carried out to document recent antibiotic susceptibility profiles of ESBL production and to screen for the presence of TEM-, SHVand CTX-M-encoding genes (blaTEM, blaSHV and blaCTX-M) among clinical isolates of Salmonella spp. METHODS Bacterial isolates and serotyping. A total of 134 Salmonella isolates (98 isolates were collected in 2007–2009 and the remaining 36 were collected in 2011–2012) from blood samples of patients attending tertiary-care hospitals and other diagnostic laboratories in Chennai, India, were included in this study. Characterization and identification of the isolates were performed using a battery of biochemical tests (Old, 1996). Serotyping of the Salmonella isolates was performed using specific antisera procured from the King Institute of Preventive Medicine and Research, Chennai, India. Institutional ethical clearance was obtained to conduct this study. boiled suspension of bacterial cells as DNA template (Lim et al., 2009). The primers used were blaTEM: TEM-F, 59-ATGAGTATTCAACATTTCCG-39, and TEM-R, 59-CTGACAGTTACCAATGCTTA39; blaSHV: SHV-F, 59-GGTTATGCGTTATATTCGCC-39, and SHVR, 59- TTAGCGTTGCCAGTGCTC-39; and blaCTX-M: CTX-MU1, 59ATGTGCAGYACCAGTAARGT-39, and CTX-MU2, 59-TGGGTRAARTARGTSACCAGA-39. Reaction mixtures of 25 ml containing 1.5 U Taq DNA polymerase (New England BioLabs) in the reaction buffer provided by the manufacturer containing 1.5 mM MgCl2, 200 mM dNTPs, 0.2 mM selected primer and 2 ml DNA template were prepared in a thermal cycler (Eppendorf). The cycling parameters employed comprised one cycle of 5 min at 96 uC, followed by 35 cycles of 1 min at 96 uC, 1 min at 58 uC for blaTEM or at 60 uC for blaSHV and 1 min at 72 uC, with a final extension of 10 min at 72 uC. The thermal cycling conditions for the CTX-M gene were one cycle of 7 min at 94 uC, followed by 35 cycles of 50 s at 94 uC, 40 s at 50 uC and 1 min at 72 uC, with a final extension of 5 min at 72 uC. The amplicon size for blaTEM and blaSHV was 867 bp, and for blaCTX-M was 593 bp. Aliquots (10 ml) of each PCR product were subjected to electrophoresis on a 1.5 % agarose gel. The amplified product was sequenced using an ABI 3730XL DNA Analyser (Applied Biosystems). Nucleotide sequences were analysed by searching GenBank using BLAST (http://www.ncbi.nlm.nih.gov/blast/). RESULTS Of the 134 isolates recovered from blood cultures of suspected cases of enteric fever, Salmonella Typhi was the predominant serotype (n5101, 75.4 %), followed by Salmonella Paratyphi A (n531, 23.12 %), Salmonella Paratyphi B (n51, 0.74 %) and Salmonella Typhimurium (n51, 0.74 %). Tables 1 and 2 show the antibiotic susceptibility pattern and resistance pattern for all the Salmonella isolates. Table 3 depicts the MICs of various antimicrobials for S. Typhi and S. Paratyphi A. Antibiotic susceptibility testing. Antibiotic susceptibility testing of the isolates was carried out by a standard Kirby–Bauer disk-diffusion method using Clinical and Laboratory Standards Institute guidelines (CLSI, 2011). The following antibiotics were tested: ampicillin (10 mg), chloramphenicol (30 mg), co-trimoxazole (1.25/23.75 mg), tetracycline (30 mg), cefotaxime (30 mg), ceftazidime (30 mg), ceftriaxone (30 mg), cefixime (5 mg), cefepime (30 mg), nalidixic acid (30 mg), ciprofloxacin (5 mg), ofloxacin (5 mg), levofloxacin (5 mg) and imipenem (10 mg). Antibiotic discs were obtained from HiMedia Laboratories. The MICs of ampicillin, cefotaxime and ceftazidime (HiMedia Laboratories) were determined by an agar dilution method (CLSI, 2011). Escherichia coli ATCC 25922 was used as the control strain. Detection of b-lactamase production. Isolates were screened for ESBL production by a combination disc method using cefotaxime (30 mg) and ceftazidime (30 mg) and a disc of cefotaxime+clavulanate (30+10 mg) and ceftazidime+clavulanate (30+10 mg) (HiMedia Laboratories). A ¢5 mm increase in diameter of the inhibition zone of the cefotaxime+clavulanate and ceftazidime+clavulanate disc compared with the cefotaxime and ceftazidime disc alone was interpreted as phenotypic evidence of ESBL production (CLSI, 2011). PCR for b-lactamase-encoding genes and nucleotide sequencing analysis. The b-lactamase genes blaTEM, blaSHV and blaCTX-M Table 1. Antibiotic susceptibility pattern of Salmonella isolates (n5134) to various antibiotics Results are shown as number of isolates (%). Antibiotics Ampicillin Chloramphenicol Co-trimoxazole Tetracycline Cefotaxime Ceftazidime Ceftriaxone Cefixime Cefepime Nalidixic acid Ciprofloxacin Ofloxacin Levofloxacin Imipenem Sensitive (%) 127 128 130 127 123 134 132 133 134 2 126 134 134 134 (94.78) (95.52) (97.10) (94.78) (91.8) (100) (98.5) (99.25) (100) (1.49) (94.03) (100) (100) (100) Intermediate (%) Resistant (%) 1 (0.75) 1 (0.75) 0 (0) 2 (1.49) 11 (8.2) 0 (0) 0 (0) 1 (0.75) 0 (0) 1 (0.75) 7 (5.22) 0 (0) 0 (0) 0 (0) 6 (4.47) 5 (3.73) 4 (2.9) 5 (3.73) 0 (0) 0 (0) 2 (1.5) 0 (0) 0 (0) 131 (97.76) 1 (0.75) 0 (0) 0 (0) 0 (0) were detected by PCR using forward and reverse primer pairs with a http://jmm.sgmjournals.org Downloaded from www.microbiologyresearch.org by IP: 78.47.19.138 On: Sat, 01 Oct 2016 08:48:55 963 S. Elumalai and others Table 2. Resistance pattern of the S. Typhi and S. Paratyphi A isolates to various antibiotics Results are shown as number of isolates (%). The S. Paratyphi B (n51) and S. Typhimurium (n51) isolates were susceptible to all the antibiotics tested. Antibiotics S. Typhi (%) (n5101) Ampicillin Chloramphenicol Co-trimoxazole Tetracycline Cefotaxime Ceftazidime Ceftriaxone Cefixime Cefepime Nalidixic acid Ciprofloxacin Ofloxacin Levofloxacin Imipenem 5 5 4 5 0 0 2 0 0 100 1 0 0 0 S. Paratyphi A (%) (n531) (4.95) (4.95) (3.96) (4.95) (0) (0) (1.98) (0) (0) (99) (0.99) (0) (0) (0) 1 0 0 0 0 0 0 0 0 31 0 0 0 0 Of the 134 Salmonella isolates studied, 127 (94.78 %) were sensitive to ampicillin and tetracycline, 128 (95.52 %) were sensitive to chloramphenicol, 130 (97.10 %) were sensitive to co-trimoxazole, 123 (91.8 %) were sensitive to cefotaxime, 132 (98.5 %) were sensitive to ceftriaxone, 133 (99.25 %) were sensitive to cefixime and 126 (94.03 %) were sensitive to ciprofloxacin. Table 3. MICs of various antibiotics for the S. Typhi and S. Paratyphi A isolates The number of strains for each MIC is shown, –, No growth. The CLSI (2011) interpretive criteria for sensitive, intermediate and resistant strains, respectively, are (mg ml21): ampicillin (Amp), ¡8, 16, ¢32; cefotaxime (Ctx), ¡1, 2, ¢4; ceftazidime (Caz), ¡4, 8, ¢16. MIC (mg ml”1) ¡0.032 0.064 0.125 0.25 0.5 1 2 4 8 16 ¢32 Total *MIC90 values. 964 S. Typhi (n5101) S. Paratyphi A (n531) Amp Ctx Caz Amp Ctx Caz – – – – – 24 55 15* 1 1 5 101 – 4 24 51 22* – – – – – – 101 – – 7 8 84* 2 – – – – – 101 – – – – – 6 22 2* – – 1 31 3 3 9 14* 2 – – – – – – 31 – – – 1 30* – – – – – – 31 (3.22) (0) (0) (0) (0) (0) (0) (0) (0) (100) (0) (0) (0) (0) Total no. isolates (n5132) 6 (4.54) 5 (3.78) 4 (3.03) 5 (3.78) 0 (0) 0 (0) 2 (1.5) 0 (0) 0 (0) 131 (99.24) 1 (0.75) 0 (0) 0 (0) 0 (0) All 134 isolates were susceptible to ceftazidime, cefepime, ofloxacin, levofloxacin and imipenem. Multidrug resistance was seen in 5/134 (3.73 %) isolates, all of which belong to serotype S. Typhi. A better pattern of sensitivity was observed for first-line drugs (ampicillin, chloramphenicol, co-trimoxazole and tetracycline) and cephalosporins (cefotaxime, ceftazidime, ceftriaxone, cefixime and cefepime). However, 97.76 % (131/134) of isolates were resistant to nalidixic acid and 0.75 % (1/134) were resistant to ciprofloxacin. All the isolates were negative for ESBL production by the combination disc method. TEM-type b-lactamase (blaTEM) was detected in six (4.47 %) of the 134 isolates, which belonged to the serotype S. Typhi (Fig. 1), and nucleotide sequencing analysis revealed that the six isolates carried the blaTEM gene (TEM1-type b-lactamase). All the six TEM-positive isolates were negative for the blaSHV gene and showed resistance to ampicillin (MIC .32 mg ml21) but were sensitive to thirdand fourth-generation cephalosporins. None of the 134 isolates was positive for the blaCTX-M gene. DISCUSSION Enteric fever is a major systemic health problem in developing countries, including India. Various studies document S. Typhi as the predominant serotype and S. Paratyphi A as the second most common serotype (Hirose et al., 2001; Manchanda et al., 2006; Choudhary et al., 2013), which correlates well with our study result. The Salmonella Paratyphi A isolates showed a better susceptibility to routinely used antibiotics than S. Typhi. In comparison with previous studies, which reported 11– 13 % multidrug-resistant Salmonella (Dutta et al., 2005; Downloaded from www.microbiologyresearch.org by IP: 78.47.19.138 On: Sat, 01 Oct 2016 08:48:55 Journal of Medical Microbiology 63 TEM-, SHV- and CTX-M-type ESBLs in Salmonella spp. M 1 2 3 4 5 1000 bp 800 bp 6 876 bp 500 bp 100 bp Fig. 1. PCR detection of blaTEM gene. Lanes: M, 100 bp ladder; 1–6, 876 bp PCR product from the six S. Typhi isolates carrying the blaTEM gene. Verma et al., 2010; Bhattacharya et al., 2011), we observed a significant decrease in MDR (3.73 %) among our study isolates. The majority of the isolates were resistant to nalidixic acid, whereas only one isolate showed resistance to ciprofloxacin. Several studies have shown that Salmonella spp. resistant to nalidixic acid may show reduced fluoroquinolone susceptibility in vivo, resulting in treatment failure (Crump et al., 2003; Kownhar et al., 2007; Choudhary et al., 2013). In our study, none of the isolates was found to be positive for ESBLs by a combination disc method. A possible reason for this result is that TEM-1 b-lactamase has the ability to hydrolyse only penicillins/early cephalosporins but not third- or fourth-generation cephalosporins, which could not be detected by the ESBL combination disc method. In Gram-negative pathogens, b-lactamase production remains the most important contributing factor to blactam resistance (Medeiros, 1997). The persistent exposure of bacterial strains to a multitude of b-lactams has led to overproduction and mutation of b-lactamases leading to their ability to hydrolyse penicillins and broad-spectrum cephalosporins (Bush, 2001). In addition to bacteria that have long been known to produce b-lactamase (such as Staphylococcus aureus and Enterobacteriaceae), these enzymes have spread to pathogens such as Haemophilus influenzae and Neisseria gonorrhoeae that previously lacked b-lactamase (Jacoby & Munoz-Price, 2005). Additionally, there are a few reports of ESBL production in pathogens such as Shigella flexneri, Shigella dysenteriae, Shigella sonnei and Vibrio cholerae (Ahamed & Kundu, 1999; Fortineau et al., 2001; Pai et al., 2001; Petroni et al., 2002). TEM-type b-lactamases are found mainly in Escherichia coli, Klebsiella pneumoniae and Proteus mirabilis. The first TEM variant with increased activity against extendedspectrum cephalosporins was TEM-3. In 1983, SHV-2 isolated from K. pneumoniae showed transferable resistance to cefotaxime as well as to other cephalosporins (Gupta, http://jmm.sgmjournals.org 2007). The ESBLs derived from TEM-1, TEM-2 and SHV-1 differ from their progenitors by as few as 1 aa, which results in the ability to hydrolyse third-generation cephalosporins (Paterson & Bonomo, 2005). The CTX-M-type b-lactamases, which differ from TEM- and SHV-type ESBLs, were initially reported in 1980s and are closely related to the b-lactamases of Kluyvera spp. (Bonnet 2004). Salmonella strains may acquire the gene encoding CTX-Mtype ESBLs from E. coli and Klebsiella spp. in the community and then spread it among the various serotypes of Salmonella (Rotimi et al., 2008). Although we found the blaTEM gene encoding TEM-1 blactamase in our isolates, which was shown to confer resistance only to penicillins and early cephalosporins, the resistance spectrum of its descendants may extend to second-, third- and fourth-generation cephalosporins (Salverda et al., 2010). This was supported by an outbreak of TEM-1-producing Klebsiella oxytoca in a neonatal unit, which was reported in Liverpool, UK, in 1982. Initially, the isolate was sensitive to ceftazidime, and infected patients were treated with this drug, but subsequent isolation of K. oxytoca from the same unit found that they harboured the TEM-type ESBL (TEM-12) and showed resistance to ceftazidime (Du Bois et al., 1995). It was demonstrated that the ceftazidime resistance gene was transferrable and carried on a plasmid (Payne et al., 1990). ESBL production in Salmonella spp. was first identified in 1988 and is increasing in prevalence worldwide; it has been detected in Salmonella enterica strains of different serovars in a number of countries including Italy, France, Ireland and the Philippines (Morris et al., 2006; Al Naiemi et al., 2008). S. Paratyphi A and S. Typhi with high rates of MDR and ESBL production (SHV-12 and TEM-1) were reported in a study conducted in Nepal (Pokharel et al., 2006). Salmonella spp. co-producing CTX-M- and TEM-type blactamases have been documented in a few case reports from Bangladesh (Ahmed et al., 2012) and India (Karthikeyan et al., 2011). Plasmid analysis of the resistant isolate revealed that the blaCTX-M and blaTEM genes were Downloaded from www.microbiologyresearch.org by IP: 78.47.19.138 On: Sat, 01 Oct 2016 08:48:55 965 S. Elumalai and others located in the same plasmid, which carried the ISEcp1 element upstream of the blaCTX-M gene to facilitate mobilization and expression (Karthikeyan et al., 2011). The present study is important in understanding the mechanism of resistance operating in these common pathogens, which are also endemic in India. Crump, J. A., Luby, S. P. & Mintz, E. D. (2004). The global burden of Extended-spectrum cephalosporins are the drugs of choice for the treatment of infections due to fluoroquinoloneresistant Salmonella spp. The emergence of ESBLs in Salmonella constitutes a new challenge. ESBLs are the most evolving mechanism of antibiotic resistance among the family of Enterobacteriaceae due to the selective pressure imposed by inappropriate use of third-generation cephalosporins. This emergence may be due to the exchange of mobile genetic elements, such as plasmids and transposons, between enteric bacteria. Therefore, appropriate selection and rotation of antibiotics, as well as continuous monitoring of antibiotic susceptibility profiles, could help to control the emergence and spread of resistance strains. resistance to chloramphenicol and other antimicrobials in Kolkata, India. Antimicrob Agents Chemother 49, 1662–1663. typhoid fever. Bull World Health Organ 82, 346–353. Du Bois, S. K., Marriott, M. S. & Amyes, S. G. (1995). TEM- and SHVderived extended-spectrum b-lactamases: relationship between selec- tion, structure and function. J Antimicrob Chemother 35, 7–22. Dutta, S., Sur, D., Manna, B., Bhattacharya, S. K., Deen, J. L. & Clemens, J. D. (2005). Rollback of Salmonella enterica serotype Typhi Effa, E. E. & Bukirwa, H. (2008). Azithromycin for treating uncomplicated typhoid and paratyphoid fever (enteric fever). Cochrane Database Syst Rev 4, CD006083. Fortineau, N., Naas, T., Gaillot, O. & Nordmann, P. (2001). SHV-type extended-spectrum b-lactamase in a Shigella flexneri clinical isolate. J Antimicrob Chemother 47, 685–688. Gupta, V. (2007). An update on newer b-lactamases. Indian J Med Res 126, 417–427. Hirose, K., Tamura, K., Sagara, H. & Watanabe, H. (2001). Antibiotic susceptibilities of Salmonella enterica serovar Typhi and S. enterica serovar Paratyphi A isolated from patients in Japan. Antimicrob Agents Chemother 45, 956–958. Jacoby, G. A. & Munoz-Price, L. S. (2005). The new b-lactamases. REFERENCES N Engl J Med 352, 380–391. Karthikeyan, K., Thirunarayan, M. & Krishnan, P. (2011). CTX-M15 Ahamed, J. & Kundu, M. (1999). Molecular characterization of the SHV-11 b-lactamase of Shigella dysenteriae. Antimicrob Agents Chemother 43, 2081–2083. Kownhar, H., Shankar, E. M., Rajan, R. & Rao, U. A. (2007). Ahmed, D., Hoque, A., Mazumder, R., Nahar, K., Islam, N., Gazi, S. A. & Hossain, M. A. (2012). Salmonella enterica serovar Typhi strain producing extended-spectrum b-lactamases in Dhaka, Bangladesh. J Med Microbiol 61, 1032–1033. Al Naiemi, N., Zwart, B., Rijnsburger, M. C., Roosendaal, R., DebetsOssenkopp, Y. J., Mulder, J. A., Fijen, C. A., Maten, W., Vandenbroucke-Grauls, C. M. & Savelkoul, P. H. (2008). Extendedspectrum-b-lactamase production in a Salmonella enterica serotype Typhi strain from the Philippines. J Clin Microbiol 46, 2794–2795. Bhattacharya, S. S., Das, U. & Choudhury, B. K. (2011). Occurrence & antibiogram of Salmonella Typhi & S. Paratyphi A isolated from Rourkela, Orissa. Indian J Med Res 133, 431–433. Bonnet, R. (2004). Growing group of extended-spectrum b- lactamases: the CTX-M enzymes. Antimicrob Agents Chemother 48, 1–14. Bradford, P. A. (2001). Extended-spectrum b-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 14, 933–951. Bush, K. (2001). New b-lactamases in Gram-negative bacteria: diversity and impact on the selection of antimicrobial therapy. Clin Infect Dis 32, 1085–1089. Choudhary, A., Gopalakrishnan, R., Nambi, P. S., Ramasubramanian, V., Ghafur, K. A. & Thirunarayan, M. A. (2013). Antimicrobial susceptibility of Salmonella enterica serovars in a tertiary care hospital in southern India. Indian J Med Res 137, 800–802. CLSI (2011). Performance Standards for Antimicrobial Susceptibility Testing; 21st Informational Supplement. CLSI Document M100-S21. Wayne, PA: Clinical and Laboratory Standards Institute. Cooke, F. J. & Wain, J. (2004). The emergence of antibiotic resistance in typhoid fever. Travel Med Infect Dis 2, 67–74. Crump, J. A., Barrett, T. J., Nelson, J. T. & Angulo, F. J. (2003). Reevaluating fluoroquinolone breakpoints for Salmonella enterica serotype Typhi and for non-Typhi salmonellae. Clin Infect Dis 37, 75– 81. 966 type ESBL producing Salmonella from a paediatric patient in Chennai, India. Indian J Med Res 134, 487–489. Emergence of nalidixic acid-resistant Salmonella enterica serovar Typhi resistant to ciprofloxacin in India. J Med Microbiol 56, 136–137. Lim, K. T., Yasin, R., Yeo, C. C., Puthucheary, S. & Thong, K. L. (2009). Characterization of multidrug resistant ESBL-producing Escherichia coli isolates from hospitals in Malaysia. J Biomed Biotechnol 2009, 165637. Madhulika, U., Harish, B. N. & Parija, S. C. (2004). Current pattern in antimicrobial susceptibility of Salmonella Typhi isolates in Pondicherry. Indian J Med Res 120, 111–114. Manchanda, V., Bhalla, P., Sethi, M. & Sharma, V. K. (2006). Treatment of enteric fever in children on the basis of current trends of antimicrobial susceptibility of Salmonella enterica serovar Typhi and Paratyphi A. Indian J Med Microbiol 24, 101–106. Medeiros, A. A. (1997). Evolution and dissemination of b-lactamases accelerated by generations of b-lactam antibiotics. Clin Infect Dis 24 (Suppl 1), S19–S45. Morris, D., Whelan, M., Corbett-Feeney, G., Cormican, M., Hawkey, P., Li, X. & Doran, G. (2006). First report of extended-spectrumb-lactamase-producing Salmonella enterica isolates in Ireland. Antimicrob Agents Chemother 50, 1608–1609. Old, D. C. (1996). Salmonella. In Mackie and McCartney Practical Medical Microbiology, 14th edn, pp. 385–404. Edited by J. G. Collee, A. G. Fraser, B. P. Marmion & A. Simmons. Edinburgh: Churchill Livingstone. Pai, H., Choi, E. H., Lee, H. J., Hong, J. Y. & Jacoby, G. A. (2001). Identification of CTX-M-14 extended-spectrum b-lactamase in clinical isolates of Shigella sonnei, Escherichia coli, and Klebsiella pneumoniae in Korea. J Clin Microbiol 39, 3747–3749. Paterson, D. L. & Bonomo, R. A. (2005). Extended-spectrum b- lactamases: a clinical update. Clin Microbiol Rev 18, 657–686. Payne, D. J., Marriott, M. S. & Amyes, S. G. (1990). Characterisation of a unique ceftazidime-hydrolysing b-lactamase, TEM-E2. J Med Microbiol 32, 131–134. Downloaded from www.microbiologyresearch.org by IP: 78.47.19.138 On: Sat, 01 Oct 2016 08:48:55 Journal of Medical Microbiology 63 TEM-, SHV- and CTX-M-type ESBLs in Salmonella spp. Petroni, A., Corso, A., Melano, R., Cacace, M. L., Bru, A. M., Rossi, A. & Galas, M. (2002). Plasmidic extended-spectrum b-lactamases in Salverda, M. L., De Visser, J. A. & Barlow, M. (2010). Natural evolution of TEM-1 b-lactamase: experimental reconstruction and Vibrio cholerae O1 El Tor isolates in Argentina. Antimicrob Agents Chemother 46, 1462–1468. Scherer, C. A. & Miller, S. I. (2001). Molecular pathogenesis of Pokharel, B. M., Koirala, J., Dahal, R. K., Mishra, S. K., Khadga, P. K. & Tuladhar, N. R. (2006). Multidrug-resistant and extended-spectrum b- Salmonellae. In Principles of Bacterial Pathogenesis, pp. 265–316. Edited by E. A. Groisman. United States of America: Academic Press. lactamase (ESBL)-producing Salmonella enterica (serotypes Typhi and Paratyphi A) from blood isolates in Nepal: surveillance of resistance and a search for newer alternatives. Int J Infect Dis 10, 434–438. Sjölund, M., Yam, J., Schwenk, J., Joyce, K., Medalla, F., Barzilay, E. & Whichard, J. M. (2008). Human Salmonella infection yielding CTX-M b-lactamase, United States. Emerg Infect Dis 14, 1957–1959. Rodrı́guez, M. M., Power, P., Radice, M., Vay, C., Famiglietti, A., Galleni, M., Ayala, J. A. & Gutkind, G. (2004). Chromosome-encoded Tamang, M. D., Nam, H. M., Kim, T. S., Jang, G. C., Jung, S. C. & Lim, S. K. (2011). Emergence of extended-spectrum b-lactamase (CTX-M- CTX-M-3 from Kluyvera ascorbata: a possible origin of plasmidborne CTX-M-1-derived cefotaximases. Antimicrob Agents Chemother 48, 4895–4897. 15 and CTX-M-14)-producing nontyphoid Salmonella with reduced susceptibility to ciprofloxacin among food animals and humans in Korea. J Clin Microbiol 49, 2671–2675. Rotimi, V. O., Jamal, W., Pal, T., Sovenned, A. & Albert, M. J. (2008). Emergence of CTX-M-15 type extended-spectrum b-lactamase- Verma, S., Thakur, S., Kanga, A., Singh, G. & Gupta, P. (2010). producing Salmonella spp. in Kuwait and the United Arab Emirates. J Med Microbiol 57, 881–886. http://jmm.sgmjournals.org clinical relevance. FEMS Microbiol Rev 34, 1015–1036. Emerging Salmonella Paratyphi A enteric fever and changing trends in antimicrobial resistance pattern of salmonella in Shimla. Indian J Med Microbiol 28, 51–53. Downloaded from www.microbiologyresearch.org by IP: 78.47.19.138 On: Sat, 01 Oct 2016 08:48:55 967