Von Willebrand Disease - Department of Medicine
advertisement

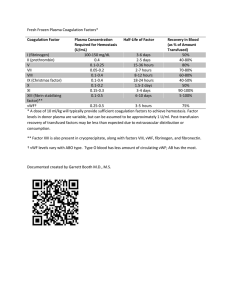
Von Willebrand Disease Diagnosis of type 1 VWD easy or difficult? Xiu Yan Jiang, MD Calgary Laboratory Services Objectives 1. Understand the current classification of von Willebrand disease variants and why diagnostic criteria for type 1 von Willebrand disease remain controversial. 2. Appreciate the influence of preanalytical variables upon the laboratory assessment of von Willebrand factor (VWF). 3. Understand the limitations of currently available assays of von Willebrand activity. 4. More skillfully interpret functional ratios such as the ratio of VWF activity to VWF antigen. Index case • 8 year-old male with severe epistaxis requiring cauterization and prolonged bleed from incision site. Questions • What historical information in this case is helpful in determining whether the patient has a hemostatic disorder? • Platelet-type vs coagulation-type bleeding ? • Based on the information described above, what would you recommend for initial tests? • What additional laboratory studies should be done? • What is the pathogenic mechanism for the likely diagnosis? Laboratory Tests - PT: 11.8 sec - INR 1.0 - PTT: 35.0 sec - Fibrinogen: 3.3 g/L - Ristocetin cofactor activity: 0.49 U/ml (0.41-1.44) - VWF antigen: 0.77 U/ml (0.40-1.85) - Factory VIII activity 1.09 U/ml (0.54-1.47) - CBC: normal - platelet: 337.4 10x9/L with normal morphology - Closure time: collagen/EPI >300 sec (84-176) collagen/ADP 262 sec (63-111) Discussion • Review von Willebrand Factor physiology • Review the classification of von Willebrand disease • Discuss the limitations of patient evaluation – Medical history and screening tests – Preanalytical variables – Review initial laboratory studies used in evaluation of VWD Von Willebrand Factor (VWF) • A large, multimeric blood glycoprotein • Gene located on chromosome 12 • Synthesized by – vascular endothelial cells and stores in WeibelPalade bodies – A small amount synthesized in megarkaryocytes and stored in the platelet α granules VON WILLEBRAND FACTOR Substructure of Human VWF Hemostatic Functions of VWF Two major roles in hemostasis • Supports platelet adhesion and activation at sites of vascular injury: – VWF binds extravascular collagen • Platelets adhere to bound VWF • Adherent platelets become activated • Supports coagulation mechanism: – VWF protects Factor VIII in circulation – VWF co-localizes Factor VIII at sites of vascular injury The Factor VIII/VWF Complex in Plasma Interaction between VWF, Platelets, and collagen of the subendothelium VWD: Definition NHLBI Expert Panel • “Von Willebrand disease is an inherited bleeding disorder that is caused by deficiency or dysfunction of von Willebrand factor (VWF), a plasma protein that mediates the initial adhesion of platelets at sites of vascular injury and also binds and stabilizes blood clotting factor VIII (FVIII) in the circulation.” The Diagnosis, Evaluation, and Management of von Willebrand Disease. NIH publication 08-5832. 2007 The Diagnosis, Evaluation, and Management of von Willebrand Disease NIH publication 08-5832. 2007 Classification of von Willebrand Disease ISTH 2006 • Inherited Quantitative Defects: – Type 1: Partial quantitative deficiency of VWF – Type 3: Virtual absence of VWF • Inherited Qualitative Defects: – Decreased VWF-dependent platelet adhesion: • Deficiency of High MW multimers: Type 2A • Defect not attributable to multimer abnormality: Type 2M – Increased affinity between VWF and Platelet: • Abnormal A1 loop of VWF: Type 2B • Abnormal platelet GP Ib: Platelet-type – Decreased Factor VIII Binding: Type 2N • Acquired VWD Type 1 VWD Mild quantitative deficiency of VWF Proposed ISTH Criteria 1. Significant bleeding history 2. Familial history of bleeding and 3. The bleeding is attributed to low levels of VWF ~80% of VWD cases are type 1: Bleeding attributed to “partial VWF deficiency” Why is the Diagnosis of Type 1VWD Difficult? • History: limitations of bleeding history – Mild bleeding symptoms are common – In surveys, healthy controls indicate that they have bleeding symptoms at a similar frequency as patients carrying a diagnosis of type 1 VWD • Incomplete penetrance of type 1 VWD Laboratory evaluation – Both inherited and acquired factors influence VWF levels – There is no single assay to definitely diagnose VWD – The correlation between laboratory and clinical phenotype varies with VWD type Laboratory Screening • Ideal screening test – Sensitive to presence of VWD – Low false positivity rate • NHLBI expert panel comment – There is no ideal screening test currently available – Panel suggests: • Initial history and physical • Laboratory screening with – Complete Blood Count and platelets – PT, PTT and fibrinogen – If bleeding history is strong: consider initial VWF assays Screening: Utility of PFA-100 Insufficient to either confirm or discard a diagnosis of VWD • Evaluation of patients with previously diagnosed VWD – Sensitivity of PFA: 95%, Sensitivity of BT: 65% • Performance in clinical practice – Normal closure time virtually excludes presence of severe VWD – Screening of with bleeding symptoms • Sensitivity: 62- 80% • Specificity: 84-89% • NHLBI Panel comment Initial Patient Evaluation in VWD VWD Guideline – NHLBI Expert Panel • Quantitative assays: – VWF ristocetin cofactor (VWF:RCo) activity: • Functional ability of VWF to bind and agglutinate platelets in presence of ristocetin – VWF antigen (VWF:Ag): • Immunoassay of VWF protein present – FVIII activity: • Coagulant activity of FVIII • Ratio of VWF:RCo/VWF:Ag Factors that Affect VWF Level • Physiologic stimuli elevate VWF level – Beta adrenergic stimulation • Stress, trauma, exercise, crying in a frightened child – Inflammation – Phase of menstrual cycle • Lowest during first 4 days of menses • Intra-individual variation is up to 40% • importance of timing of the testing with respect to the menstrual cycle is not clear – Pregnancy: 3~5 x increased by 3rd trimester – Thyroid status (Hyperthyroid have higher levels) • Blood Group (ABO, Lewis): – The rate of VWF synthesis probably is not affected by blood group; however, the survival of VWF appears to be reduced in individuals who have type O blood. – VWF levels are approximately 25-35% lower in people with blood group O (Gill JC, et al: Blood 1987; 69: 1689) Factors that Affect VWF Level Race: Africans and African Americans have higher average levels of VWF than the Caucasian population. Age: levels increase with age Importance of repeated testing Preanalytical Variables • Sample collection and handling: – Phlebotomy conditions, Patient stress level, sample processing, Sample storage • Refrigeration or storage of citrated blood for > 4 hours leads to artifactually low VWF levels (and loss of HMW multimers) • Multimeric analysis:may show abnormal Limitations of “screening Panel” • VWF Antigen – Lower limit of detection usually 1-2 IU/dL – CV data: Inter-lab usually ≥10%-20%, Intra-lab ~11% • VWF “activity” – Multiple assay methods – Lower limit of detection: Wide range ≤3-20 IU/dL – CV data*: Inter-lab ≥20%-40%, Intra-lab: ~20% (especially VWF:Rco), low in immunologic assay Initial Patient Evaluation in VWD VWD Guideline – NHLBI Expert Panel • Quantitative assays: – VWF ristocetin cofactor (VWF:RCo) activity: • Functional ability of VWF to bind and agglutinate platelets in presence of ristocetin – VWF antigen (VWF:Ag) – FVIII activity: • Coagulant activity of FVIII • Ratio of VWF activity/VWF:Ag Criteria for an abnormal Activity/Antigen ratio - 0.7 used in European MCMDM VWD1 study - 7% of 1166 controls had ratio < 0.7 - 0.6 used in Canadian VWD1 study - 0.5 is lower limit of range suggested by NHLBI panel - Individual labs may need to set their own criterion Prototype Laboratory data Condition VWF:Ac VWF:AG Low or 1 <50 <50 or NL NL 2A or 2M <30 <30-200 or NL <0.5-0.7 2B <30 <30-200 or NL < 0.5-0.7 2N 30-200 30-200 <3 <3 3 FVIII AC/AG NL <10 -- Type 1 VWD versus “Low VWF” JE Sadler, Annu Rev Med 2005; 56:173-191 • NHLBI consensus panel suggested reserving the diagnosis of VWD type 1 for patients with moderately low VWF levels (< 30 IU/dL) – Facilitates treatment and genetic counseling in this subgroup. • Suggested “low VWF” when VWF level 30 – 50 IU/dl – An epidemiological risk factor for bleeding • Statistics alone predict a high co-occurrence of bleeding symptoms, a positive family history of bleeding and low VWF level. • Using the descriptive term “Low VWF” avoids misdiagnosis of these patients as having an inherited bleeding disorder – Still allows appropriate “risk management” “Functional” VWF by Automated LIA Tange JI, et al: J Throm Haemost 2009; 7 (supp 2), 533 Tange JL et al: Mayo Clinic “Coagulation Testing Quality Conference 2009 • Automated latex particle-enhanced immunoturbidometric assay: – Particles coated with antibody to “functional epitope” – Modified procedure: Expand analytical range to 3 – 1400 IU/dL – Comparison of VWF-LIA to VWF:Rco – Decreased CV(%) VWF Collagen Binding Assay Another Quantitative VWF Functional Assay • Quantitates VWF binding to collagen coated ELISA plates – More sensitive than VWF:RCo assay to loss of highest multimers – Lower limit of detection is similar to VWF:Ag – Has lower CV than VWF:RCo • Primary site for fibrillar collagen binding is A3 domain – Highly dependent on the source of collagen, as well as on whether type 1 collagen or a mixture of type 1/3 collagen is used. – Four families reported with VWD attributed to defect in A3 domain VWF Collagen Binding Assay Another Quantitative VWF Functional Assay • Role of VWF:CB – NHLBI panel: “The place of VWF:CB in the diagnosis of VWD has not been established” – Patients who have defects in collagen binding may have a normal VWF:RCo and thus escape clinical diagnosis unless a VWF:CB assay is performed • Availability • Most routine labs do not offer this assay • ~ 25% (CV 18-29%) Genetics of Type 1 VWD • Type 1 VWD with VWF < 30 IU/dL – Commonly found inheritable VWF gene defect (75%) – Most of the mutations: single amino acid substitutions in domain D3 • Milder Type 1 (“Low VWF”) with VWF 30 – 50 IU/dL: – Variable inheritance • VWF gene defect found in 50% of cases • Blood Group O is more common • Other genetic factors may play a role Index Case • 8 year-old male with severe epistaxis requiring cauterization and prolonged bleed from incision site – Closure time: collagen/Epi>300 sec (84-176) collagen/ADP 262 sec (63-111) – Ristocetin cofactor activity: 0.49 U/ml (0.41-1.44) – VWF antigen: 0.77 U/ml (0.40-1.85) – Factory VIII activity 1.09 U/ml (0.54-1.47) – VWF activity/Ag ratio: 0.64:1 – Platelet: 337.4 10E9/L Further Studies • Platelet aggregation study: slight disaggregation in 1.5 g/l ristocetin • Multimer study: – Initial test: relative decreased in high and intermediate molecular weight VWF – Repeated test: normal pattern • Platelet surface markers: CD36, CD41a, CD42a, CD29, CD31, CD62P, CD42b: normal • Desmopressin challenge test: good response but the VWF activity/antigen is still low (1.21:1.95=0.62:1) VWD genotype • Heterozygous A to G transition at nucleotide 4751 in exon 28 (TYR1584CYS) of the VWF gene. • This genetic changes is associated with type 1 VWD.This is the most frequent variant associated with type 1 VWD. Family Study • 13 year-old female (sister) with epistaxis – – – – VWF activity (GP1b): 0.60 U/ml (0.41-1.44) VWF antigen: 0.97 U/ml (0.40-1.85) Factory VIII activity 1.00 U/ml (0.54-1.47) VWF activity/Ag ratio: 0.61:1 • Heterozygous A to G transition at nucleotide 4751 in exon 28 (TYR1584CYS) of the VWF gene. Family Study (Mother) • 41 year-old with menorrhagia – – – – VWF activity (GP1b): 0.59 U/ml (0.41-1.44) VWF antigen: 0.83 U/ml (0.40-1.85) Factory VIII activity 0.94 U/ml (0.54-1.47) VWF activity/Ag ratio: 0.71:1 • VWF multimeric analysis: normal range • Closure time Collagen/EPI >250 seconds (84176) • Heterozygous A to G transition at nucleotide 4751 in exon 28 (TYR1584CYS) of the VWF gene. Specific Assays Used to Diagnose and Classify VWD: • Initial quantitative screening (NHLBI guideline) – VWF:RCo: Function of VWF to bind/agglutinate platelets – VWF antigen: Immunoassay of VWF protein – FVIII activity: Coagulant activity of FVIII • Ratio of VWF:RCo/VWF:Ag • Supplemental studies: Important to define Type 2 VWD – VWF multimer: Size distribution of VWF polymers – VWF:CB: Function of VWF to bind collagen – Other functional assays: LD-RIPA, VWF:FVIII binding – VWF gene analysis – Platelet-binding studies – Assays for antibodies to VWF Treatment • Desmopressin – – – – Treatment of choice in type 1 vWD Milder responses in type 2A and 2M In type 2B vWD, causes worsening of thrombocytopenia Ineffective in type 2N and 3 vWD • vWF/Factor VIII Concentrates – Indicated in type 2N and 3 vWD and in subtypes with more severe phenotype • Antifibrinolytic agents – Tranexamic acid – Adjunctive therapy or as sole therapy in mild bleeds Conclusions Diagnosis of type 1 VWD easy or difficult? • Screening tests such as the PFA-100 are insufficient to include or exclude von Willebrand disease – One should assay VWF:Ag, VWF:activity and F-VIII • Physiologic factors and sample processing are important pre-analytic variables that influence diagnostic value of clinical assays • The Panel emphasizes the importance of the timing of the phlebotomy for assays, with the patient at his/her optimal baseline as far as possible. • Type 1 VWF is a quantitative defect. – The distinction between diagnoses of “Low VWF” and Type 1 VWD is still being debated • VWF Activity and VWF:Ag ratio may be an important clue for diagnosis. • Supplemental test of VWF are useful to evaluate or exclude type 2 VWD