Congenital Heart Diseases With Right-to
advertisement

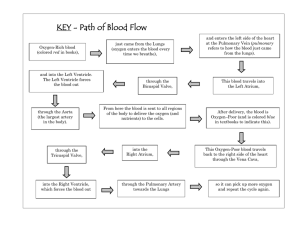
JOBNAME: iac 42#4 2004 PAGE: 1 OUTPUT: Wed September 15 11:05:00 2004 lww/iac/84488/V42N4-06 Congenital Heart Diseases With Right-to-Left Shunts Jason Z. Qu, MD There are 6 common types of congenital heart diseases with right-toleft lesions: tetralogy of Fallot (TOF), transposition of the great arteries, truncus arteriosus, tricuspid atresia, total anomalous pulmonary venous return, and pulmonary atresia with intact ventricular septum. Tetralogy of Fallot Tetralogy of Fallot is the most common intrinsic cyanotic congenital heart disease, which accounts for 5% to 10% of all congenital heart disease and has a prevalence of about 1 out of 2,000 live births.1 Anatomy and Pathophysiology Tetralogy of Fallot comprises a constellation of cardiac findings that share the following common anatomic abnormalities (Fig. 1): a large malaligned ventricular septal defect (VSD), overriding of the aorta over the septal defect, right ventricular outflow obstruction, and right ventricular hypertrophy. The anatomic spectrum of TOF is diverse and includes other variants such as pulmonary stenosis (TOF-PS), pulmonary atresia (TOF-PA), or absent pulmonary valve (TOF-APV). The pathophysiology of TOF depends, primarily, on the degree of right ventricular outflow tract obstruction (RVOTO) and, secondarily, on the status of the systemic vascular resistance relative to the degree of right ventricular obstruction. The patients can be fully saturated or severely cyanotic depending on the ratio of pulmonary to systemic blood flow. In a Tetralogy spell (tet spell), or hypoxic spell, the infants experience episodes of severe hypoxemia and acidemia. The responsible factors may be increase in RVOTO and increase in oxygen requirement, decrease in peripheral vascular resistance, contraction of the right ventricular infundibulum, closure of the ductus arteriosus, or development of physiologic anemia.2–4 59 JOBNAME: iac 42#4 2004 PAGE: 2 OUTPUT: Wed September 15 11:05:01 2004 lww/iac/84488/V42N4-06 60 n Qu Figure 1. The typical anomaly of tetralogy of Fallot: right ventricular outflow obstruction (pulmonary valvular and infundibular obstruction shown in the picture), ventricular septal defect, right ventricular hypertrophy, and dextroposition of the aorta. AO, aorta; LA, left atrium; LV, left ventricule; RA, right atrium; RV, right ventricle; PA, pulmonary artery. Erythrocytosis (increased blood cell mass) is the usual response of patients with TOF to hypoxia. Persistent hypoxemia results in increased blood erythropoietin, which stimulates bone marrow production of erythroid cells. Clinical Presentations Depending on the severity of RVOTO, the patients may present from no cyanosis to severe cyanosis. The tet spells frequently occur after crying. The child may appear normal between spells. Frequent and prolonged spells lead to cerebral injury. Hypoxia-induced erythrocytosis may result in cerebral venous thrombosis and further compromises neurologic function. Bacterial endocarditis and brain abscesses are not uncommon in this group of infants. Laboratory Studies Polycythemia is a common finding. The electrocardiogram shows right ventricular hypertrophy with or without right bundle branch block. A boot-shaped cardiac contour is very characteristic, and the pulmonary vascularity is diminished on chest x-ray. Echocardiography and color Doppler analysis provide data regarding hemodynamic characteristics as well as JOBNAME: iac 42#4 2004 PAGE: 3 OUTPUT: Wed September 15 11:05:04 2004 lww/iac/84488/V42N4-06 Right-to-Left Congenital Cardiac Lesions n 61 morphologic features of the anomaly. Cardiac catheterization and angiocardiography can provide additional important information such as major aortopulmonary collateral arteries (MAPCAs) or abnormal coronary arteries that cannot be imaged adequately with ultrasound. Surgical Management The goals of surgical management are to improve pulmonary blood flow and to correct pathologic anatomy. Blalock and Taussig initiated a procedure of connecting the right side subclavian artery to the right pulmonary artery by an end-to-side anastomosis.5 This procedure was later modified by interposing a tubular graft of Teflon or Gore-Tex between the subclavian and pulmonary arteries to preserve more blood flow to the arm. Total correction for TOF consists of closing the ventricular septal defect and relieving the right ventricular outflow obstruction.6 With refinements of surgical technique and perioperative management in recent years, early correction of tetralogy has been widely recommended and excellent results are now achievable in neonates and infants.7,8 Early correction can prevent or decrease complications (cerebral hypoxia, embolus, abscess, and myocardial hypertrophy) and avoid the complications of palliative procedures. Transposition of the Great Arteries Transposition of the great arteries (TGA) is a congenital heart lesion characterized by ventriculoarterial discordance. Transposition of the great arteries accounts for 5% to 7% of all congenital cardiac malformations.9 Anatomy and Pathophysiology In D-transposition of the great vessels, the aorta arises from the right ventricle (Fig. 2), and its route is anterior and rightward. The pulmonary artery originates from the left ventricle, and its route is posterior and leftward. Unlike in the normal heart, where the systemic and pulmonary circulations are in series, in TGA, the circulations are parallel. The deoxygenated blood returns to the right atrium and is pumped into the systemic circulation by the right ventricle via the aorta, whereas the oxygenated blood returns to the left atrium and is pumped into the pulmonary circulation by the left ventricle via the pulmonary artery. Therefore, there must be adequate mixing between the pulmonary and systemic circulation for survival. The mixing can occur at the levels of atrium (ASD), ventricle (VSD), or great vessels. L-transposition of the great arteries, also called corrected transposition, is less frequent. In this malformation, the arterial ventricle (anatomic JOBNAME: iac 42#4 2004 PAGE: 4 OUTPUT: Wed September 15 11:05:05 2004 lww/iac/84488/V42N4-06 62 n Qu Figure 2. Transposition of great arteries (D-transposition) with patent foramen ovale, patent ductus arteriosus, and intact interventricular septum. The atria and ventricles are concordant. The ventricles and arteries are discordant with the aorta arising from right ventricle and the pulmonary artery from the left ventricle. AO, aorta; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; PA, pulmonary artery. right ventricle) is displaced leftward and posteriorly and the venous ventricle (anatomic left ventricle) is displaced rightward and anteriorly. The right atrium empties blood into the anatomic left ventricle through the mitral valve, and the left atrium empties into the anatomic right ventricle via the tricuspid valve. The pulmonary artery originates from the venous ventricle, and the aorta originates from the arterial ventricle. About half of the patients with L-TGA are dextrocardiac. Patients with L-TGA lead normal lives if there are no other cardiac defects. Clinical Presentations In D-TGA, moderate to severe cyanosis is present after birth, and the infant is tachypneic. A systolic (regurgitant) murmur of VSD may be audible in less cyanotic infants with associated VSD. Congestive heart failure (CHF) develops in the first weeks of life. Without surgical intervention, death occurs in 90% of patients before they reach 6 months of age.10,11 Progressive hypoxia and acidosis result in death unless the mixing of the systemic and pulmonary blood improves. Many infants with TGA and a large VSD develop moderate pulmonary vascular obstructive disease by 3 to 4 months of age. Thus, early surgical procedures are recommended. JOBNAME: iac 42#4 2004 PAGE: 5 OUTPUT: Wed September 15 11:05:08 2004 lww/iac/84488/V42N4-06 Right-to-Left Congenital Cardiac Lesions n 63 Laboratory Studies Severe arterial hypoxemia with or without acidosis is present. Electrocardiography shows rightward QRS axis. Biventricular hypertrophy may be present in infants with large VSD, PDA, or pulmonary vascular obstructive disease. An egg-shaped cardiac silhouette with a narrow, superior mediastinum is characteristic. Echocardiography usually provides all the anatomic and functional information needed for the management of infants with D-TGA.11 Catheterization provides the delineated specifics such as great artery origin and coronary artery anomalies. Surgical Management Palliative procedures include pulmonary artery banding and atrial septostomy. Pulmonary artery banding is aimed to decrease pulmonary blood flow to control CHF and minimize pulmonary vascular obstructive disease. It is also performed in the neonatal period to prepare the LV for future definitive procedures. Atrial septostomy can be achieved by balloon dilation (Rashkind procedure)12 or excision of the posterior aspect of the atrial septum via a right thoracotomy (Blalock-Hannon operation).13 Intra-atrial physiological repairs (atrial switch) include the Mustard and Senning procedures, which result in physiologic correction of TGA. The Mustard operation redirects the pulmonary venous return to the right ventricle and the systemic venous return to the left ventricle by using a pericardial or prosthetic baffle.14 The Senning operation is a modification of the Mustard procedure.15 It creates the same discordant atrioventricular connections using the right atrial wall and interatrial septum instead of pericardium or prosthetic material. The Rastelli procedure is a method of anatomically correcting TGA with VSD and RVOTO.16 In this operation, the VSD is closed with an intraventricular patch-tunnel so that LV is directed to the aorta. The pulmonary artery is transected and ligated distal to the pulmonary valve. A right ventriculostomy is performed, and a prosthetic conduit or an aortic homograft is connected between the RV and PA. The Jatene (arterial switch) operation is the anatomic correction of TGA by switching the great arteries and retransplanting the coronary arteries.17,18 In this operation, the aorta and pulmonary artery are transected distal to their respective valves. The coronary arteries are explanted from the aortic root and then reimplanted into the proximal pulmonary artery (neoaorta). The great arteries are switched with the distal aorta, reanastomosed to the old proximal pulmonary artery, and the distal pulmonary artery brought anterior to be reanastomosed to the old proximal aorta. JOBNAME: iac 42#4 2004 PAGE: 6 OUTPUT: Wed September 15 11:05:09 2004 lww/iac/84488/V42N4-06 64 n Qu Truncus Arteriosus Truncus arteriosus accounts for 1% to 2% of congenital heart disease.19 There is a single semilunar valve and annulus with a common outflow trunk arising from the ventricles. Truncus arteriosus may be associated with DiGeorge syndrome.20 Anatomy and Pathophysiology A large and malaligned VSD is also part of the complex. There are 4 types of truncus arteriosus (Fig. 3). Because of the unrestricted VSD and Figure 3. The common types of truncus arteriosis (TA). In all types, TA arises from the base of the ventricles and straddles a VSD. In type I (A), a main pulmonary artery (PA) arises from the posterior left side of the TA and bifurcates into right (RPA) and left (LPA) pulmonary arteries. In type II (B) and III (C), there is no main PA, and the RPA and LPA arise separately from the posterior or lateral sides of the TA. In type IV (D), there is no pulmonary artery or its branches. Blood supplies to the lungs are derived entirely from major aortopulmonary collateral arteries (MAPCAs). AO, aorta; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; PA, pulmonary artery. JOBNAME: iac 42#4 2004 PAGE: 7 OUTPUT: Wed September 15 11:05:17 2004 lww/iac/84488/V42N4-06 Right-to-Left Congenital Cardiac Lesions n 65 the origin of the pulmonary arteries and the aorta from a single trunk, blood flow to the lungs and the systemic circulation is determined by the relative resistances in these circulations. In the infant with truncus arteriosus type I, II, and III who has no stenosis in the pulmonary arteries, the decreased pulmonary vascular resistance after birth will result in an increase in pulmonary blood flow, which will maintain the arterial oxygen saturation between 75% to 80%. The systemic arterial oxygen saturation may reach levels of 85% to 90% due to the increase in the pulmonary to systemic blood flow ratio. If the LV volume overload happens rapidly, the patient will develop cardiac failure within the first week of life. Ninety percent of patients die of heart failure during early infancy if left untreated.21 Truncal valve insufficiency or stenosis, pulmonary artery stenosis, and aortic arch anomalies may also be present with truncus arteriosus.22 Clinical Presentations The newborn with truncus arteriosus exhibits mild cyanosis right after birth. Cyanosis then deceases as pulmonary blood flow increases (type I and II), but the signs of heart failure become significant if the pulmonary blood flow is too large. Patients may have moderate to severe cyanosis if there is stenosis of pulmonary ostia or pulmonary arteries (type III). Laboratory Studies Chest x-ray reveals cardiomegaly, and the pulmonary vascular markings are increased within a week after birth. The electrocardiogram (ECG) can show the changes of left or right ventricular hypertrophy. Echocardiography can usually give diagnostic information in patients with truncus arteriosus. Cardiac catheterization and angiography can reveal the precise origin of pulmonary arteries, severity of obstruction of pulmonary ostia or pulmonary arteries, and coronary anomalies. Surgical Management The palliative procedure for patients with truncus arteriosus is PA banding. Surgical repair can be accomplished with a relatively low mortality, even in small infants.23,24 The essentials of the surgical repair are to close VSD, divide the truncus using the truncal valve as the aortic valve, and place a conduit with or without a valve from the RV to the PA. Tricuspid Atresia Accounting for 1% to 3% of congenital heart defects, tricuspid atresia is a congenital heart lesion characterized by agenesis of the tricuspid valve.25 JOBNAME: iac 42#4 2004 PAGE: 8 OUTPUT: Wed September 15 11:05:17 2004 lww/iac/84488/V42N4-06 66 n Qu Anatomy and Pathophysiology Tricuspid atresia is commonly classified into 3 types.25 Type I tricuspid atresia is not associated with transposition of the great arteries. Type II is associated with D-transposition, and type III consists of L-transposition with tricuspid atresia. All patients with tricuspid atresia will need an ASD with right-to-left shunt to survive. More than 70% of patients with tricuspid atresia have pulmonary atresia or pulmonary or subpulmonary stenosis. An additional downstream shunt (PDA, bronchial collaterals) is necessary for survival if pulmonary atresia exists. Clinical Presentations Patients often show cyanosis on the first day of life. Squatting may be noted in older children. Physical examination will reveal cyanosis as well as clubbing of fingers and toes in children older than 1 year. A systolic thrill and loud systolic murmur along the sternal border can be appreciated if a VSD present. A systolic murmur of pulmonary stenosis and a machinery murmur of PDA may be heard. Symptoms and signs of heart failure may appear when the disease progresses into late stage. Laboratory Studies Arterial hypoxemia and polycythemia (hematocrit >56%) are revealed on blood tests. Electrocardiogram findings include LVH, LV strain pattern, and ST and T wave changes. Chest x-ray shows an elevated apex, left atrial enlargement, and absence of right ventricle. Echocardiography is often diagnostic for tricuspid atresia. Surgical Management Prostaglandin E1 should be used to maintain ductal patency after the diagnosis is confirmed. A balloon atrial septostomy or atrial septectomy may be urgently needed for patients with CHF and a large pressure gradient between the 2 atria. The most common palliative shunt performed early in tricuspid atresia is a modified Blalock-Taussig. A bidirectional Glenn shunt can provide pulmonary perfusion by anastomosing the upper end of divided superior vena cava (SVC) to the side of the right pulmonary artery. Both of these procedures allow adaptation to a Fontan correction at a later stage. The Fontan operation is based upon the realization that venous (or atrial) pressure alone is adequate to drive blood through the pulmonary circulation.26 By connecting SVC to right pulmonary artery and right atrium to left pulmonary artery, the Fontan operation successfully separates the pulmonary from systemic circulation. The blood returning from the SVC now perfuses the right pulmonary artery, and blood from the inferior JOBNAME: iac 42#4 2004 PAGE: 9 OUTPUT: Wed September 15 11:05:18 2004 lww/iac/84488/V42N4-06 Right-to-Left Congenital Cardiac Lesions n 67 vena cava (IVC) passes through the right atrium and then into the left pulmonary artery. The Fontan procedure has been modified into many variations such as anastomosing RA to the main PA, connecting RA to RV via homograft, and constructing a tunnel between the IVC and pulmonary artery.27 Total Anomalous Pulmonary Venous Return Total anomalous pulmonary venous return (TAPVR) accounts for 1% of all congenital heart lesions. The pulmonary veins connect to the systemic venous system instead of to the left atrium. Anatomy and Pathophysiology Total anomalous pulmonary venous return may be classified into 4 types28: supracardiac (45%), cardiac (25%), infracardiac (25%), and mixed (5%). In the supracardiac type, the common pulmonary vein confluence drains into the right atrium via left innominate vein or into the SVC. In the cardiac configuration, the common pulmonary vein connects to the coronary sinus or directly with the right atrium. In the infracardiac (subdiaphragmatic) pattern, the common pulmonary vein drains through diaphragm into the portal vein, ductus venosus, hepatic vein, or IVC. The mixed type is a combination of the other types. Clinical Presentations Clinical manifestations differ, depending on the degree of pulmonary vein obstruction. Neonates with obstructed TAPVR present with profound cyanosis, severe respiratory distress, and failure to thrive. The infant without pulmonary venous obstruction will have mild cyanosis, CHF, frequent pulmonary infection, and growth retardation. Laboratory Studies Right ventricle hypertrophy (RVH) is common on the EKG. X-ray studies reveal normal or slightly enlarged heart silhouette and pulmonary edema. Two-dimensional echocardiography delineates the anatomic connection of the pulmonary veins and the type of TAPVR. Surgical Management Corrective surgery is necessary for all patients with TAPVR. Balloon atrial septostomy may be done if immediate surgery cannot be performed. All procedures are performed under cardiopulmonary bypass and are intended to redirect the pulmonary venous return to the LA. JOBNAME: iac 42#4 2004 PAGE: 10 OUTPUT: Wed September 15 11:05:18 2004 lww/iac/84488/V42N4-06 68 n Qu Pulmonary Atresia With Intact Ventricular Septum Pulmonary atresia with intact ventricular septum (PAIVS) accounts for less than 1% of all congenital heart defects. The prevalence of this disorder is 4.1 per 100, 000 live births.29 Anatomy and Pathophysiology In the usual form of pulmonary atresia and intact ventricular septum, the pulmonary valve is atretic with a diaphragmlike membrane. The infundibulum is also atretic in some infants. Because there is no direct communication between the RV cavity and the PA, the pulmonary blood flow is usually entirely dependent on a PDA. The systemic venous return to the RA must flow to the LA via an ASD or a PFO. Systemic and pulmonary venous returns mix in the LA and go to the LV to supply the body and lungs. If the PDA closes after birth, the pulmonary blood flow is significantly decreased, and the infant becomes severely cyanotic. Tricuspid valve regurgitation is common due to the high pressure in the RV. The high RV pressure is also decompressed retrograde through the dilated coronary sinus and its microcirculation into the left or right coronary artery. If the proximal coronary artery obstruction is present, coronary circulation is perfused by desaturated blood causing myocardial ischemia. Clinical Presentations Cyanosis is usually apparent within hours of birth because of functional and anatomic closure of the PDA. Severe tachypnea, dyspnea, and hypoxia are seen in distressed infants. A tricuspid regurgitation murmur may be audible. Progressive hypoxia and metabolic acidosis indicate the poor prognosis. Laboratory Studies The ECG commonly shows sinus rhythm with LVH and right atrial enlargement. The ST-T abnormalities consistent with subendocardial ischemia are frequently seen. The chest x-ray may show an enlarged heart and reduced pulmonary vascular markings. Echocardiography reveals an atretic pulmonary valve with no blood flow through it, and a right-to-left interatrial shunt by color Doppler imaging. Cardiac catheterization and angiocardiography are required in infants with severe hypoplastic right ventricle and anticipated ventriculocoronary artery connections. Surgical Management Pharmacologic preservation of the PDA with prostaglandin E1 infusion should begin as soon as the diagnosis is suspected or confirmed. JOBNAME: iac 42#4 2004 PAGE: 11 OUTPUT: Wed September 15 11:05:18 2004 lww/iac/84488/V42N4-06 Right-to-Left Congenital Cardiac Lesions n 69 A balloon atrial septostomy may be performed to improve the right-to-left atrial shunt if RV sinusoids are confirmed. The goals of surgical procedures are to restore ‘‘normal’’ biventricular circulation and pulmonary blood flow. The initial operation is directed toward establishing pulmonary blood flow with modified Blalock-Taussig shunt and promoting normal RV development by relieving RVOTO with a pulmonary valvotomy or transannular path. Patients who have severe tricuspid regurgitation, right ventricle-dependent coronary circulation, or do not have appreciable right ventricular development at follow-up should be tracked to a Fontan procedure or cardiac transplantation. Anesthesia Management for Right-to-Left Congenital Heart Disease Preoperative assessment and preparation have been discussed in detail in the other part of this issue. Prior to induction of anesthesia, routine monitors should be applied including ECG, pulse oximetry, capnogram, and noninvasive blood pressure measurement. Warm ambient temperature and a quiet induction room can help peripheral circulation and facilitate intravenous (IV) access, which sometimes can be very challenging in younger infants. It is essential that all intravenous fluids be free of air bubbles. In children who come to the operating suite without an IV line in place, anesthesia is usually induced with sevoflurane by mask. Ketamine intramuscular (IM) injection is an alternative for infants without an IV line. Although, theoretically, a right-to-left shunt may slightly delay the induction time with inhaled anesthetics, the minor delay is of little practical concern in the clinical setting. In patients with existing intravenous access, IV induction of anesthesia is performed with propofol (1–2 mg/kg) or ketamine (1–2 mg/kg) and fentanyl (2 ^g/kg). Endotracheal intubation is facilitated with nondepolarizing muscle relaxant, such as pancuronium (0.1 mg/kg), vecuronium (0.1 mg/kg), or cisatracurium (0.2 mg/kg). Because of potential contraction of the PDA, succinylcholine is preferably avoided. In patients with right-to-left shunt, a decrease in SVR and/or increase PVR may further increase shunt. It is therefore crucial to provide adequate ventilation with oxygen and maintain systemic vascular resistance. Continuous monitoring of the oxygen saturation, blood pressure, ECG, and end-tidal capnography will help achieve these goals. Blood pressure cuff and radial artery cannulation should be avoided on the side where a Blalock-Taussig shunt will be performed, as flow will be diverted from the subclavian to the pulmonary artery. Placement of arterial and central venous pressure lines is performed after successful tracheal intubation. Body temperature should be monitored at 2 different sites JOBNAME: iac 42#4 2004 PAGE: 12 OUTPUT: Wed September 15 11:05:19 2004 lww/iac/84488/V42N4-06 70 n Qu (rectal and tympanic/esophageal/nasopharyngeal) for children who need CPB. Urine output is quantified. Left atrial pressure monitoring is useful in sick children or patients needing complex repairs. Intraoperative transesophageal echocardiography is being used more frequently to provide instant morphologic and hemodynamic information, especially during the early phase after CPB. Anesthesia is usually maintained with IV narcotic (fentanyl 50– 100 ^/kg), benzodiazepine (midazolam 50–100 ^/kg), and isoflurane. Patients should remain paralyzed throughout the case with nondepolarizing muscle relaxants (pancuronium or cisatracurium). Arterial blood gases, serum calcium and potassium, and hematocrit should be frequently monitored. Heparin is usually injected into the right atrium by the surgeon or through the central venous line before cannulation. Protamine is administered at the conclusion of extracorporeal circulation. In patients with poor ventricular function and prolonged CPB time, dopamine (3–10 ^g/kg/min) and milrinone (0.5 ^g/kg/min after 50 ^g/kg load) are commonly used. Perioperative fluid and ventilation management are very important in patients with right-to-left shunt lesions. Because these children have higher hematocrits to maintain oxygen delivery, packed red blood cells should be transfused to keep the hematocrit optimized. Some patients may benefit from the addition of slight positive end expiratory pressure because they have increased pulmonary blood flow (truncus arteriosus, TAPVC). However, in patients with decreased pulmonary blood flow (TOF, pulmonary atresia with intact ventricular septum, tricuspid atresia) and post-Fontan procedure, one should avoid using excessive positive airway pressure or positive end expiratory pressure during ventilation. Patients who have had a complicated repair, long CPB time, or unstable cardiopulmonary status are usually left intubated and mechanically ventilated postoperatively. Once the patient is awake, stable, rewarmed to a normal body temperature, and without metabolic imbalance, the endotracheal tube can be removed. In summary, understanding the general principles and pathophysiology of congenital heart lesions is essential for the management of a child with CHD for any type of surgery. Taking care of this group of patients in the operating room can be very challenging. The anesthesiologist should be able to predict the effects of various anesthetics and ventilation techniques on the hemodynamic stability of the patients. References 1. Siwik ES, Patel CR, Zahka KG, et al. Tetralogy of Fallot. In: Allen HD, Gutgesell HP, Clark EB, et al. Moss and Adam’s Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult, 6th ed. Philadelphia, PA: Lippincott; 2001: 880–881. JOBNAME: iac 42#4 2004 PAGE: 13 OUTPUT: Wed September 15 11:05:19 2004 lww/iac/84488/V42N4-06 Right-to-Left Congenital Cardiac Lesions n 71 2. Liberthson RR. Tetralolgy of Fallot. In: Congenital Heart Disease: Diagnosis and Management in Children and Adults. Boston, MA: Little, Brown; 1989:95–114. 3. Sun LS, Du F, Quaegebeur JM. Right ventricular infundibular beta-adrenoceptor complex in tetralogy of Fallot patients. Pediatr Res. 1997;42:12–16. 4. Garson A Jr, Gellettee PC, McNamara DG. Propranolol: the preferred palliation for tetralogy of Fallot. Am J Cardiol. 1981;47:1098–1104. 5. Blalock A, Taussig HB. The surgical treatment of malformations of the heart in which there is pulmonary stenosis or pulmonary atresia. JAMA. 1945;128:189–202. 6. Lillehei CW, Cohen M, Warden HE, et al. Direct vision intracardiac surgical correction of the tetralogy of Fallot, pentalogy of Fallot and pulmonary atresia defects. Report of first ten cases. Ann Surg. 1955;142:418–445. 7. Van Arsdell GS, Maharaj GS, Tom J, et al. What is the optimal age for repair of tetralogy of Fallot? Circulation. 2000;102(suppl 3):123–129. 8. Hirsch JC, Mosca RS, Bove EL. Complete repair of tetralogy of Fallot in the neonate: results in the modern era. Ann Surg. 2000;232:508–514. 9. Wernovsky G. Transposition of the great arteries. In: Allen HD, Gutgesell HP, Clark EB, et al. Moss and Adam’s Heart Disease in Infants, Children, and Adolescents: Including the Fetus and Young Adult. 6th ed. Philadelphia, PA: Lippincott; 2001:1027–1084. 10. Liebman J, Cullum L, Belloc NB. Natural history of transposition of the great arteries. Anatomy and birth and death characteristics. Circulation. 1969;40:237–262. 11. Rudolph AM. Transposition of the great arteries. In: Congenital Disease of the Heart: Clinical-Physiological Considerations, 2nd ed. Armonk: Futura; 2001:675–736. 12. Rashkind WJ, Miller WW. Creation of an atrial septal defect without thoracotomy: A palliative approach to complete transposition of the great arteries. JAMA. 1966;196: 991–992. 13. Blalock A, Hanlon CR. The surgical treatment of complete transposition of the aorta and pulmonary artery. Surg Gynecol Obstet. 1950;90:1–15. 14. Mustard WT. Successful two-stage correction of transposition of the great vessels. Surgery. 1964;55:469–472. 15. Senning A. Surgical correction of transposition of the great vessels. Surgery. 1959;45: 966–980. 16. Rastelli GC, McGoon DC, Wallace RG. Anatomic correction of transposition of the great arteries with ventricular septal defect and subpulmonary stenosis. J Thorac Cardiovasc Surg. 1969;58:545–552. 17. Jatene AD, Fontes VF, Paulista PP, et al. Anatomic correction of transposition of the great vessels. J Thorac Cardiovasc Surg. 1976;72:364–370. 18. Pasquali Sk, Hasselblad V, Li JS, et al. Coronary artery pattern and outcome of arterial switch operation for transposition of the great arteries: a meta-analysis. Circulation. 2002;106:2572–2580. 19. Mitchell SC, Korones SB, Berendes HW. Congenital heart disease in 56,109 births: incidence and natural history. Circulation. 1971;43:323–332. 20. Lupski JR, Langston C, Friedman R, et al. DiGorge anomaly associated with a de novo Y; 22 translocation resulting in monosomy del(22)(q11.2). Am J Med Genet. 1991;40: 196–198. 21. Marcelletti C, McGoon DC, Mair DC. The natural history of truncus arteriosus. Circulation. 1976;54:108–111. 22. William JM, De Leeuw M, Black MD, et al. Factors associated with outcomes of persistent truncus arteriosus. J Am Coll Cardiol. 1999;34:545–553. 23. Imamura M, Drummond-Webb JJ, Sarris GE, et al. Improving early and intermediate results of truncus arteriosus repair: a new technique of truncal valve repair. Ann Thorac Surg. 1999;67:1142–1146. 24. Anderson RH. Repair of truncus arteriosus. Eur J Cardiothorac Surg. 2001;20:1080– 1081. JOBNAME: iac 42#4 2004 PAGE: 14 OUTPUT: Wed September 15 11:05:19 2004 lww/iac/84488/V42N4-06 72 n Qu 25. 26. 27. 28. Rashkind WJ. Tricuspid atresia: a historical review. Pediatr Cardiol. 1982;2:85–88. Fontan F, Baudet E. Surgical repair of tricuspid atresia. Thorax. 1971;26:240–248. Berggren H. The Fontan procedure: a bad operation? Scand Cardiol J. 2002;36:69–70. Healy JE Jr. An anatomic survey of anomalous pulmonary veins: their clinical significance. J Thorac Cardiovasc Surg. 1952;23:433–444. 29. Daubeny PEF, Sharland GK, Cook AC, et al. Pulmonary atresia with intact ventricular septum: impact of fetal echocardiography on incidence at birth and postnatal outcome. Circulation. 1998;98:562–566.