Brain Atrophy Is Related to Lacunar Lesions and Tissue
Microstructural Changes in CADASIL
Eric Jouvent, MD; Anand Viswanathan, MD, PhD; Jean-François Mangin, PhD;
Mike O’Sullivan, MD, PhD; Jean-Pierre Guichard, MD; Andreas Gschwendtner, MD;
Rodica Cumurciuc, MD; Frédérique Buffon, MD; Nils Peters, MD; Chahin Pachaı̈, PhD;
Marie-Germaine Bousser, MD; Martin Dichgans, MD; Hugues Chabriat, MD, PhD
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Background and Purpose—Cerebral atrophy has been recently recognized as a key marker of disease progression in
cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). The
contribution of subcortical cerebral lesions in this process remains undetermined. The aim of this study was to
investigate the relationships between cerebral volume and different types of subcortical MRI lesions in CADASIL.
Methods—Demographic, clinical, and laboratory data from 147 patients with CADASIL recruited from a prospective
cohort study were analyzed. Validated methods were used to determine the ratio of brain volume to intracranial cavity
volume (brain parenchymal fraction [BPF]), volume of white matter hyperintensities, volume of lacunar lesions, number
of cerebral microhemorrhages, and mean apparent diffusion coefficient. Associations between BPF, clinical scales, and
the different subcortical MRI markers were tested.
Results—BPF obtained in 129 patients was significantly associated with the Mattis dementia rating scale (P⬍0.0001),
Mini-Mental State Examination (P⫽0.002), and modified Rankin scale (P⬍0.0001) after adjustment for age and sex.
Multiple linear regression modeling showed that BPF was independently associated with mean apparent diffusion
coefficient (P⬍0.0001), volume of lacunar lesions (P⫽0.004), and age (P⬍0.0001), accounting for 46% of the observed
variance in BPF but not with volume of white matter hyperintensities or number of microhemorrhages.
Conclusions—In association with age, mean apparent diffusion coefficient and volume of lacunar lesions are strong and
independent MRI predictors of BPF, a key marker of cognitive and motor disability in CADASIL. These results suggest
brain atrophy is related to remote and/or diffuse consequences of both lacunar lesions and widespread microstructural
alterations within the brain outside lacunar lesions. (Stroke. 2007;38:000-000.)
Key Words: CADASIL 䡲 cerebral atrophy 䡲 cerebral microhemorrhage 䡲 diffusion 䡲 lacune
䡲 white matter hyperintensities
C
bral microhemorrhages (CM) appear as rounded hypointense
foci on T2* or gradient echo images and are detected in
approximately one third of patients.8 Additionally, microstructural changes detected by diffusion imaging both inside
WMH and in normal-appearing white matter have been
previously reported to be strongly associated with motor and
cognitive decline.9,10
Recently, normalized brain volume was found to be
strongly correlated with cognitive and disability scales in
cerebral microangiopathies.11,12 These results, also reported
in CADASIL, both in cross-sectional and longitudinal analyses,13 suggest that brain atrophy may represent a “final
common pathway” in the pathophysiology of microangiopa-
erebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a
monogenic cerebral microangiopathy leading to disability
and dementia.1 It is caused by mutations in the Notch3 gene
on chromosome 192 and is considered a genetic model of
“pure” subcortical ischemic vascular dementia.
Three types of lesions are seen on conventional MRI
sequences. White matter hyperintensities (WMH) are detected on T2-weighted or fluid attenuated inversion recovery
images. They are commonly symmetrical, diffuse, and confluent3 and often involve the temporal poles.4 Lacunar lesions
(LL) are hypointense on T1-weighted images5 and appear of
various shapes and sizes6 as reported pathologically.7 Cere-
Received November 19, 2006; final revision received December 23, 2006; accepted January 4, 2007.
From the Department of Neurology (E.J., R.C., F.B., M.-G.B., H.C.), CHU Lariboisière, Assistance Publique des Hôpitaux de Paris, and Université
Paris VII, Paris, France; the Department of Neurology and Clinical Trials Unit (A.V.), Massachussets General Hospital and Harvard Medical School,
Boston, Mass.; Unité de NeuroAnatomie Fonctionelle (J.-F.M.), Service Hospitalier Frédéric Jolliot, CEA, Orsay, France; the Department of Neurology
(M.O., A.G., N.P., M.D.), Klinikum Grosshadern, Ludwig-Maximilians-University, Marchioninistrasse 15, Munich, Germany; the Department of
Neuroradiology (J.-P.G.), CHU Lariboisière, Assistance Publique des Hôpitaux de Paris, France; and Theralys, France (C.P.).
Correspondence to Prof Hugues Chabriat, Service de Neurologie, Hôpital Lariboisière, 2 rue Ambroise Paré, 75010 Paris, France. E-mail
hugues.chabriat@lrb.ap-hop-paris.fr
© 2007 American Heart Association, Inc.
Stroke is available at http://www.strokeaha.org
DOI: 10.1161/STROKEAHA.106.478263
1
2
Stroke
June 2007
thies. Peters et al recently observed an atrophy rate 3 times
higher in 76 patients with CADASIL compared with rates in
normal aging independent from the extent of WMH. However, they did not investigate the potential impact of LL, CM,
or microstructural changes (assessed by diffusion imaging)
on this process.13
The aim of the present study was to investigate the
relationships between different MRI markers of subcortical
tissue lesions as assessed with routine MRI sequences (including apparent diffusion coefficient [ADC] measured with
diffusion-weighted imaging) and brain volume in a large
series of patients with CADASIL.
Materials and Methods
Subjects
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
One hundred forty-seven subjects (107 from Paris and 40 from
Munich) were recruited among consecutive CADASIL patients with
a positive genetic test and at least 18 years of age evaluated at
Lariboisière (Paris) or Ludwig-Maximilians-Universität (Munich)
hospitals between October 2003 and July 2005. Complete study
design has been detailed elsewhere.8 Clinical and demographic data
were collected, including age, sex, history of hypertension (defined
as diagnosis of hypertension or taking antihypertensive drugs),
systolic blood pressure, diastolic blood pressure, diabetes (1997
World Health Organization criteria), history of hypercholesterolemia
(diagnosis of hypercholesterolemia or taking lipid-lowering drugs),
smoking habits, alcohol intake, and body mass index. Laboratory
evaluation (which included complete blood count, glucose, hemoglobin A1c, homocysteine, high-density lipoprotein, low-density
lipoprotein, and total cholesterol levels) was performed in all
patients. All subjects underwent detailed baseline neurological examination during the 2 hours before MRI examination, including a
Mini-Mental State Examination, Mattis dementia rating scale, and
degree of disability based on the modified Rankin scale and Barthel
index. An independent ethics committee in both participating centers
approved this study.
MRI
MRI scans were obtained by the use of a 1.5-T system (Vision;
Siemens [Munich] or Signa General Electric Medical Systems
[Paris]). Three dimensional T1-weighted axial sequences (Munich:
TR/TE 11.4/4.4 ms, slice thickness 1.19 mm, no interslice gap,
256⫻256; Paris: TR/TE 9/2 ms, slice thickness 0.8 mm, no interslice
gap, 256⫻256), fluid-attenuated inversion recovery (FLAIR, Munich: TR/TE/TI 4284/110/1428, slice thickness 5 mm, no interslice
gap, 176⫻256; Paris: TR/TE/TI 8402/161/2002 ms, slice thickness
5.5 mm, no interslice gap, 256⫻160), T2*-weighted gradient echo
planar imaging (Munich: TR/TE 1056/22 ms, slice thickness 5 mm,
no interslice gap, 256⫻192; Paris: TR/TE 500/15 ms, slice thickness
5.5 mm, no interslice gap, 256⫻192), proton density (Munich:
TR/TE 3300/16 ms, slice thickness 5 mm, no interslice gap,
190⫻256; Paris: TR/TE 3300/15 ms, slice thickness 5.5 mm, no
interslice gap, 256⫻192), and diffusion-weighted imaging (Munich:
TR/TE 5100/137 ms, slice thickness 5 mm, interslice gap 1.5 mm,
128⫻128; Paris: TR/TE 8200/83 ms, slice thickness 5.5 mm,
interslice gap 1.5 mm, 128⫻128; b value⫽1000 s/mm2) were
performed. Diffusion-weighted imaging scans were acquired in the
X, Y, and Z directions and then averaged to make ADC measurements largely independent of the effects of anisotropic diffusion.
Apparent diffusion coefficient values were then calculated to generate ADC maps as described elsewhere.14
Image Processing and Analysis
Brain Volume Assessment
Determination of global brain volumes from 3-dimensional T1 sequences was performed using Brainvisa software (CEA, Orsay, France,
http://brainvisa.info). The first step consisted of a field inhomogeneity
bias correction with an algorithm detailed previously.15 Extraction of
nonbrain tissue and segmentation of images into gray matter, white
matter, and cerebrospinal fluid (CSF) were done using a validated
histogram analysis algorithm.16 Because of large amounts of signal
abnormalities in white matter, which can result in voxel misclassification, a manual correction was performed after visual examination
of the initial results based on the variance of intensity in gray matter
voxels. This correction was performed to obtain the minimal and best
matching of the external cerebral contours by visual inspection. To
assess validity and reliability of this method, two raters (E.J. and
A.V.) performed the task in a double-blind manner on a randomly
chosen subset of 20 scans. Intrarater and interrater correlations
coefficients were found to be excellent: 0.945 and 0.922. During the
segmentation process, all voxels containing CSF (including lacunar
cavities) were excluded from the brain volume. Segmentation was
performed from the vertex of the brain to the lowest axial slice,
including cerebellar tissue. Automated determination of the volume
of the intracranial cavity was done on proton density images from
base to top of the skull using a dedicated algorithm from Theralys
(Lyon, France). The corresponding mask was visually checked and
marginally corrected if necessary. Brain parenchymal fraction (BPF)
was defined as the ratio of brain tissue volume to total intracranial
cavity volume: BPF⫽brain tissue volume/intracranial cavity.
Determination of Mean Apparent Diffusion Coefficient
Histograms of ADC values from ADC maps were generated for each
patient using a bin width equal to 0.1 10⫺4 mm2s⫺1. Voxels
containing CSF were excluded in all patients before calculation using
a superior threshold value at 27 10⫺4 mm2s⫺1 (after careful visual
analysis of masks generated with different threshold values). To
correct for cross-subject differences in brain volume, each histogram
was normalized to the total number of brain tissue voxels. Only the
mean ADC derived from each histogram was used for analysis.
Lesions Quantification
Lesion quantification was made as previously described.8 Briefly,
WMH were analyzed on all axial FLAIR slices from the base of the
cerebellum to the vertex. LL were determined on 3-dimensional T1
scans. The total volume of WMH and LL were normalized to the
intracranial cavity in each patient [normalized volume⫽(volume/
volume intracranial cavity)⫻100]. The number of CM, defined as
rounded foci 5 mm or less in diameter hypointense on gradient echo
sequences and distinct from vascular flow voids, leptomeningeal
hemosiderosis, or nonhemorrhagic subcortical mineralization, was
recorded.
Statistical Methods
Correlations between clinical and MRI measures were calculated
using the Spearman’s rank correlation coefficient and partial correlation coefficient when needed. Linear regressions were performed
using Pearson’s product moment correlation to assess the relative
contribution of clinical and MRI variables on BPF. Variables were
selected on the basis of published epidemiological data: age, gender,
systolic and diastolic blood pressure, homocysteine levels, cholesterol levels, body mass index, fasting glucose, hemoglobin A1c, and
diabetes. Traditional cardiovascular risk factors such as smoking
habits and alcohol intake were also included. Both conventional MRI
markers and mean ADC values were analyzed in the models. A log
transformation was performed for normalized volume of WMH and
LL to obtain normal distributions, thus defining vWMH and vLL,
respectively. For analysis, number of CM values was divided into
tertiles (0, 1 to 3, or 4 or more).
Multivariable linear regression models were used to find
predictors of BPF. Candidate covariates were those associated
with BPF in univariate analysis (P⬍0.10). Center effect was
analyzed using a fixed-effects model. The final model variables
were selected by a stepwise regression analysis with entry and
removal values set to 0.05.
Jouvent et al
Demographic, Imaging, and Cognitive Features in 129 Patients
With CADASIL
Clinical variables
Age, years, mean⫾SD (range)
51.37⫾11.39 (26–78)
Male sex
56/129 (43%)
History of hypertension
20/128 (16%)
Body mass index, kg/m2
25.59⫾4.35
Current or previous smoking
62/129 (48%)
Any alcohol consumption
70/119 (59%)
History of hypercholesterolemia
64/128 (50%)
Diabetes
3/128 (2.3%)
Medications
Antiplatelet agent use
90/129 (70%)
Anticoagulant use
5/129 (3.9%)
Disability and cognitive scores
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Barthel index, mean, median (range)
89.2, 100 (0–100)
National Institutes of Health Stroke Scale,
mean, median (range)
1.9, 0 (0–25)
Rankin’s scale, mean, median (range)
1.1, 0 (0–5)
Mini-Mental State Examination, mean,
median (range)
26.1, 28 (7–30)
Mattis dementia rating scale, mean,
median (range)
131.8, 141 (35–144)
MRI markers
BPF, mean⫾SD
80.7⫾6.2
3
Absolute volume of LL, mm , median
(range)
Normalized volume of LL, median (range)
3
Absolute volume of WMH, mm , median
(range)
Normalized volume of WMH, median
(range)
No. of CM,* median (range)
524.3 (0–5708.07)
0.04 (0–0.41)
88921 (3819–334,289)
6.25 (0.27–22.69)
4 (0–26)
Mean ADC (10⫺4 mm2s⫺1), mean⫾SD
12.11⫾1.59
*Calculated only in patients with CM.
Results
Among the 147 patients from the cohort, 129 patients had full
sets of 3-dimensional T1, FLAIR, proton density, T2*, and
diffusion-weighted images of sufficient quality for postprocessing measurements. Their demographic, clinical, and main
MRI parameters are presented in Table 1.
After adjustment for age and sex, BPF was found to be
significantly correlated with Mattis dementia rating scale
(Spearman rank correlation coefficient, ⫽0.43, P⬍0.0001),
Mini-Mental State Examination score (⫽0.28, P⫽0.002),
Barthel index (⫽0.42, P⬍0.0001), modified Rankin score
(⫽⫺0.41, P⬍0.0001), and National Institutes of Health
Stroke Scale score (⫽⫺0.41, P⬍0.0001).
In univariate linear regression analyses for demographic
and clinical variables, BPF was inversely related to age
(Pearson’s correlation coefficient, r⫽⫺0.50, P⬍0.0001)
male gender (r⫽⫺0.27, P⫽0.002), and hypercholesterolemia
(r⫽⫺0.21, P⫽0.02). Conversely, no correlation was detected
between BPF and systolic blood pressure, diastolic blood
pressure, history of smoking, body mass index, alcohol
MRI Predictors of Brain Atrophy in CADASIL
3
intake, diabetes, homocysteine, hemoglobin A1c, or fasting
glucose levels.
Univariate analyses for MRI markers revealed that BPF
correlated with both mean ADC (r⫽⫺0.58, P⬍0.0001),
vLL (r⫽⫺0.43, P⬍0.0001), and number of CM
(r⫽⫺0.30, P⫽0.0005) but not with vWMH (r⫽⫺0.12,
P⫽0.19).
A stepwise multivariate analysis was performed with
significant clinical and MRI variables, including a potential
center effect. Three variables remained significantly related
to BPF: mean ADC (P⬍0.0001), vLL (P⫽0.0037), and age
(P⬍0.0001). In the statistical model, these three factors
explained 46% of the variance of BPF.
Discussion
In the present study, we found a strong correlation between
BPF and both cognitive and disability scales in a large series
of patients with CADASIL independent of age and sex. This
is in agreement with data recently obtained by Peters et al in
76 patients with CADASIL13 using a different method for
measurement of brain volume (SIENAX).17 They are also in
line with results observed in elderly populations having white
matter hyperintensities and/or lacunar infarctions.11,12
We detected a strong correlation between BPF and two
MRI markers of the disease, which was independent from the
age effect: the volume of LL and the mean ADC (measured
over the whole brain and after exclusion of tissue cavities
containing CSF). Although the negative impact of the load of
small deep infarcts on cognitive function has been repeatedly
demonstrated in various populations,19 only few studies have
examined the relationships between the brain volume and the
load of small deep infarcts using MRI. In a small study of 27
patients with cerebral microangiopathy, Preul et al recently
observed a significant correlation between the severity of T2
lesions (including LL) and both the cortical thickness and
ventricle index.20 Conversely, in the Atherosclerosis Risk in
Communities study, no association between LL and the
enlargement of cerebral ventricles or cortical atrophy was
detected.24 However, in this study, the volume of LL was not
evaluated and the degree of atrophy was assessed only by
visual scale. Additionally, the number of LL might be
significantly lower in this population, because individuals
with stroke or transient ischemic attack were excluded from
the cohort. It is noteworthy that the association between BPF
and LL in our study is unlikely to be related to direct tissue
loss caused by lacunar lesions because the results remained
unchanged when the volume of LL was included in BPF
estimation (data not shown). The results suggest that LL lead
to brain volume loss through remote and/or diffuse effects on
brain morphology. Apoptosis, recently described in cortical
neurons in patients with CADASIL, may participate in this
process.21
The strong association detected between the reduction of
BPF and the increase in mean cerebral ADC is another
important result of this study. It has been previously shown
that the mean diffusivity measured with diffusion tensor
imaging was of great value to assess the severity of microstructural tissue damage during the course of cerebral microangiopathies.10 The increase in diffusion in CADASIL as
4
Stroke
June 2007
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
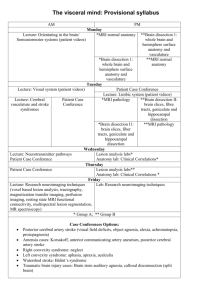
Registered axial MRI sequences of two
patients of similar age (65 and 66 years).
Left: 3-dimensional T1 images, middle:
FLAIR images, right: ADC maps presented using a common color scale (unit:
10⫺4 mm2/s). Top: patient exhibiting high
load of WMH, low level of LL, low ADC
values, and high BPF. Bottom: patient
exhibiting high load of WMH and LL,
high ADC values, and low BPF (all lacunar lesions are not visible on the slice
selected from ADC maps attributable to
imperfect registration with FLAIR slices;
the lesions containing CSF were
excluded from ADC maps using a
threshold value). Note: the heterogenous
ADC changes detected both inside WMH
and within the normal-appearing white
matter indicating a large variability of
severity in local microstructural tissue
damage and the larger increase of ADC
in the white matter detected in the atrophic case (there was also a slight and
nonsignificant increase of ADC of the
brain related to cortical atrophy and partial volume effect).
well as in other cerebral microangiopathies was also found
strongly correlated with clinical severity.9 This increase in
diffusion (measured by mean diffusivity or ADC) is presumably related to the enlargement of the extracellular space
caused by demyelination and axonal loss.22 In the current
study, diffusion was measured over the whole brain after
masking LL. Thus, mean diffusivity was measured in noninfarcted tissue areas both inside and outside regions of WMH.
These results in addition to the lack of correlation between
brain atrophy and the extent of WMH (as recently reported in
a prospective study13) strongly suggest that the severity of
microstructural tissue damage has a much more potent impact
than the extent of WMH on brain atrophy in patients with
CADASIL. Of note, in the present study, we did not use
diffusion tensor imaging techniques to assess the microstructural tissue status but generated ADC maps from routine
diffusion-weighted images. The highly significant results
obtained using such a simple parameter suggest that this
measure may provide considerable prognostic and therapeutic
information in the evaluation of cerebral microangiopathies.
The comparison of these different diffusion MRI techniques
would be important for future studies.
The lack of association between BPF and the extent of
WMH in the present study is in contrast with data obtained in
the elderly showing that the extent of WMH is associated
with gray matter reduction23 and may even predict cerebral
atrophy.18 This discrepancy may be related to differences of
age, clinical presentation, MRI methods, and quantification
techniques in these studies. Also, the load of LL, CM, and the
severity of microstructural changes were not taken into
account in the previous studies. Altogether, the present data
further emphasize that although the extent of WMH (and
location) is of great diagnostic value3,4 at the initial phase of
CADASIL, its actual consequences on cerebral volume as
well as on clinical severity10 may be relatively limited when
other types of associated lesions are considered (Figure).
A significant association was detected between BPF and
the number of CM that did not remain significant in multivariate analysis. Although we cannot exclude a small effect of
CM on the cerebral volume, the inverse correlation with BPF
in univariate analysis may also reflect that these lesions are
mainly observed at the late stage of the disease when patients
have more extensive structural changes in the cerebral tissue.
There are potential limitations in the interpretation of our
results. First, we were unable to use our brain volume
segmentation algorithm in 18 patients attributable to insufficient image quality. Although this could introduce a potential
bias in our results, careful visual analysis of the data showed
that movement artifacts were mostly responsible for exclusion of these subjects from analysis. Additionally, because
our study was cross-sectional, we could not determine
whether the increase in the volume of LL or in cerebral
diffusion actually precedes the occurrence of cerebral atrophy. Prospective studies may help to understand the link
between the structural tissue changes observed at the subcortical level and the reduction of the whole brain volume.
In summary, our results provide convincing evidence that
brain atrophy is strongly related to remote or diffuse consequences of both LL and cerebral tissue microstructural
damage. In association with age, volume of LL and mean
ADC may account for nearly half of the reduction of brain
volume in this disorder. Future prospective and pathological
studies may help to further elucidate the link between
subcortical structural changes and global cerebral atrophy in
CADASIL as well as in other cerebral microangiopathies.
Acknowledgments
We acknowledge E. Vicaut and C. Boutron for their help and support
in the building of the clinical and MRI database, and M. Boukobza
and D. Reizine who participated in the MRI examination of patients.
Jouvent et al
MRI Predictors of Brain Atrophy in CADASIL
Sources of Funding
This work was supported by PHRC grant AOR 02-001 (DRC/APHP)
and performed with the help of ARNEVA (Association de Recherche
en Neurologie VAsculaire), Hôpital Lariboisiere, France, the Deutsche Forschungsgemeinschaft (SFB596/TPA4), and a grant from
EISAI Medical Res. Inc (Germany). E.J. was supported by a grant
from the “Journées de Neurologie de Langue Française, France.”
R.C. was supported by a grant from the CADASIL Foundation of
America. M.O. is an Alexander von Humboldt Fellow and is also
supported by the European Neurological Society and the Peel
Medical Research Trust.
10.
11.
12.
Disclosures
None.
13.
References
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
1. Chabriat H, Vahedi K, Iba-Zizen MT, Joutel A, Nibbio A, Nagy TG,
Krebs MO, Julien J, Dubois B, Ducrocq X. Clinical spectrum of
CADASIL: a study of 7 families. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Lancet. 1995;
346:934 –939.
2. Joutel A, Corpechot C, Ducros A, Vahedi K, Chabriat H, Mouton P,
Alamowitch S, Domenga V, Cecillion M, Marechal E, Maciazek J,
Vayssiere C, Cruaud C, Cabanis EA, Ruchoux MM, Weissenbach J, Bach
JF, Bousser MG, Tournier-Lasserve E. Notch3 mutations in CADASIL, a
hereditary adult-onset condition causing stroke and dementia. Nature.
1996;383:707–710.
3. Chabriat H, Levy C, Taillia H, Iba-Zizen MT, Vahedi K, Joutel A,
Tournier-Lasserve E, Bousser MG. Patterns of MRI lesions in CADASIL.
Neurology. 1998;51:452– 457.
4. O’Sullivan M, Jarosz JM, Martin RJ, Deasy N, Powell JF, Markus HS.
MRI hyperintensities of the temporal lobe and external capsule in patients
with CADASIL. Neurology. 2001;56:628 – 634.
5. van Den Boom R, Lesnik Oberstein SA, van Duinen SG, Bornebroek M,
Ferrari MD, Haan J, van Buchem MA. Subcortical lacunar lesions: an MR
imaging finding in patients with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Radiology.
2002;224:791–796.
6. Herve D, Mangin JF, Molko N, Bousser MG, Chabriat H. Shape and
volume of lacunar infarcts: a 3D MRI study in cerebral autosomal
dominant arteriopathy with subcortical infarcts and leukoencephalopathy.
Stroke. 2005;36:2384 –2388.
7. Lammie GA. Hypertensive cerebral small vessel disease and stroke.
Brain Pathol. 2002;12:358 –370.
8. Viswanathan A, Guichard JP, Gschwendtner A, Buffon F, Cumurcuic R,
Boutron C, Vicaut E, Holtmannspotter M, Pachai C, Bousser MG,
Dichgans M, Chabriat H. Blood pressure and haemoglobin a1c are associated with microhaemorrhage in CADASIL: a two-centre cohort study.
Brain. 2006;129:2375–2383.
9. Chabriat H, Pappata S, Poupon C, Clark CA, Vahedi K, Poupon F,
Mangin JF, Pachot-Clouard M, Jobert A, Le Bihan D, Bousser MG.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
5
Clinical severity in CADASIL related to ultrastructural damage in white
matter: in vivo study with diffusion tensor MRI. Stroke. 1999;30:
2637–2643.
Holtmannspotter M, Peters N, Opherk C, Martin D, Herzog J, Bruckmann
H, Samann P, Gschwendtner A, Dichgans M. Diffusion magnetic resonance histograms as a surrogate marker and predictor of disease progression in CADASIL: a two-year follow-up study. Stroke. 2005;36:
2559 –2565.
Seshadri S, Wolf PA, Beiser A, Elias MF, Au R, Kase CS, D’Agostino
RB, DeCarli C. Stroke risk profile, brain volume, and cognitive function:
the Framingham Offspring Study. Neurology. 2004;63:1591–1599.
Fein G, Di Sclafani V, Tanabe J, Cardenas V, Weiner MW, Jagust WJ,
Reed BR, Norman D, Schuff N, Kusdra L, Greenfield T, Chui H. Hippocampal and cortical atrophy predict dementia in subcortical ischemic
vascular disease. Neurology. 2000;55:1626 –1635.
Peters N, Holtmannspotter M, Opherk C, Gschwendtner A, Herzog J,
Samann P, Dichgans M. Brain volume changes in CADASIL: a serial
MRI study in pure subcortical ischemic vascular disease. Neurology.
2006;66:1517–1522.
Roberts TP, Rowley HA. Diffusion weighted magnetic resonance
imaging in stroke. Eur J Radiol. 2003;45:185–194.
Mangin J-F. Entropy minimization for automatic correction of intensity
non uniformity. Hilton Head Island, SC: IEEE Press; 2000:162–169.
Mangin J-F, Coulon O, Frouin V. Robust brain segmentation using
histogram scale-space analysis and mathematical morphology. In: Wells
WM, Colchester A, Delp S, eds. Proc 1st MICCAI, LNCS-1496, MIT,
Boston, pages 1230 –1241, October 1998. Springer Verlag.
Smith SM, Zhang Y, Jenkinson M, Chen J, Matthews PM, Federico A, De
Stefano N. Accurate, robust, and automated longitudinal and crosssectional brain change analysis. Neuroimage. 2002;17:479 – 489.
Schmidt R, Ropele S, Enzinger C, Petrovic K, Smith S, Schmidt H,
Matthews PM, Fazekas F. White matter lesion progression, brain atrophy,
and cognitive decline: the Austrian Stroke Prevention Study. Ann Neurol.
2005;58:610 – 616.
Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ, Breteler
MM. Silent brain infarcts and the risk of dementia and cognitive decline.
N Engl J Med. 2003;348:1215–1222.
Preul C, Lohmann G, Hund-Georgiadis M, Guthke T, von Cramon DY.
Morphometry demonstrates loss of cortical thickness in cerebral microangiopathy. J Neurol. 2005;252:441– 447.
Viswanathan A, Gray F, Bousser MG, Baudrimont M, Chabriat H.
Cortical neuronal apoptosis in CADASIL. Stroke. 2006;37:2690 –2695.
Molko N, Pappata S, Mangin JF, Poupon F, LeBihan D, Bousser MG,
Chabriat H. Monitoring disease progression in CADASIL with diffusion
magnetic resonance imaging: a study with whole brain histogram analysis. Stroke. 2002;33:2902–2908.
Wen W, Sachdev PS, Chen X, Anstey K. Gray matter reduction is
correlated with white matter hyperintensity volume: a voxel-based morphometric study in a large epidemiological sample. Neuroimage. 2006;
29:1031–1039.
Knopman DS, Mosley TH, Catellier DJ, Sharrett AR; Atherosclerosis
Risk in Communities (ARIC) Study. Cardiovascular risk factors and
cerebral atrophy in a middle-aged cohort. Neurology. 2005;65:876 – 881.
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Brain Atrophy Is Related to Lacunar Lesions and Tissue Microstructural Changes in
CADASIL
Eric Jouvent, Anand Viswanathan, Jean-François Mangin, Mike O'Sullivan, Jean-Pierre
Guichard, Andreas Gschwendtner, Rodica Cumurciuc, Frédérique Buffon, Nils Peters, Chahin
Pachaï, Marie-Germaine Bousser, Martin Dichgans and Hugues Chabriat
Stroke. published online April 19, 2007;
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2007 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/early/2007/04/19/STROKEAHA.106.478263.citation
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/