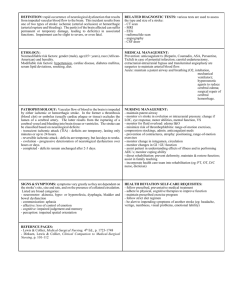
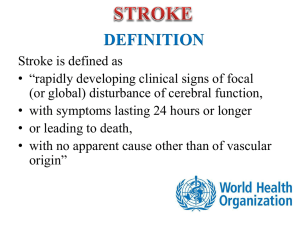
STROKE DEFINITION 1. Neurological deficit of cerebrovascular cause that persists beyond... interrupted by death within 24 hours.

STROKE
DEFINITION
1.
Neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours.
2.
Rapidly developed clinical sign of focal disturbance of cerebral function of presumed vascular origin and of more than 24 hours
Stroke-in-evolution describes progression during the first 24 hours.
Transient ischemic attack (TIA). This means a focal deficit, such as a weak limb, aphasia or loss of vision lasting from a few seconds to 24 hours. There is complete recovery. The attack is usually sudden
EPIDEMIOLOGY
1.
Third leading cause of the dead.
2.
Black people are more prone than white people.
3.
Male are more prone than female.
4.
Incidence of stroke increases with age.
SUB-TYPES OF STROKE
1.
Ischaemic – obstruction to one of major cerebral arteries, brainstem strokes are less common.
2.
Haemorrhage – 9% are caused by haemorrhage to the deep parts of the brain.
Patients are usually hypertensive.
PATHOPHYSIOLOGY OF COMPLETE STROKE
One of three mechanisms is usual:
1.
arterial embolism from a distant site
2.
arterial thrombosis
3.
haemorrhage into the brain (intracerebral or subarachnoid).
Less commonly:
1.
venous infarction
2.
carotid or vertebral artery dissection
3.
polycythaemia (hyperviscosity syndromes)
4.
fat and air embolism
5.
multiple sclerosis
6.
mass lesions (e.g. brain tumour, abscess, subdural haematoma)
7.
rarities: arteritis, neurosyphilis, systemic lupus erythematosus, mitochondrial disease.
PATHOPHYSIOLOGY OF TRANSIENT ISCHEMIC ATTACK
1.
TIAs are usually the result of microemboli.
2.
Principal sources of emboli to the brain are cardiac thrombi and atheromatous plaques/thrombi within the great vessels, and carotid and vertebral systems
RISK FACTORS
1.
Cardiovascular Disease a) Hypertension b) CAD.
2.
Diabetes
3.
Dyslipidemia a) High total Cholesterol b) and/or Low HDL
4.
Atrial Fibrillation
5.
Asymptomatic Carotid Artery Stenosis
6.
Bleeding disorders
7.
Pre-existing cerebral aneurysm
8.
Anticoagulant and antiplatelet drug therapy
CLINICAL FEATURES:
1.
The most common stroke is caused by infarction in the internal capsule following thromboembolism in a middle cerebral artery branch. A similar picture is caused by internal carotid occlusion.
2.
Limb weakness on the opposite side to the infarct develops over seconds, minutes or hours.
3.
There is a contralateral hemiplegia or hemiparesis with facial weakness.
4.
Aphasia is usual when the dominant hemisphere is affected.
5.
Weak limbs are at first flaccid and areflexic.
6.
Headache is unusual. Consciousness is usually preserved.
7.
After a variable interval, usually several days, reflexes return, becoming exaggerated. An extensor plantar response appears.