Molecular Psychiatry (2006) 11, 286–300
& 2006 Nature Publishing Group All rights reserved 1359-4184/06 $30.00
www.nature.com/mp
ORIGINAL ARTICLE
A neuronal nitric oxide synthase (NOS-I) haplotype
associated with schizophrenia modifies prefrontal cortex
function
A Reif1, S Herterich2, A Strobel3, A-C Ehlis1, D Saur5, CP Jacob1, T Wienker4, T Töpner1, S Fritzen1,
U Walter2, A Schmitt1, AJ Fallgatter1 and K-P Lesch1
1
Department of Psychiatry and Psychotherapy (Section for Clinical and Molecular Psychobiology and Laboratory for
Psychophysiology and Functional Imaging), Julius-Maximilians-University Würzburg, Würzburg, Germany; 2Central
Laboratory, Department of Clinical Biochemistry and Pathobiochemistry, University of Würzburg, Würzburg, Germany,
3
Department of Differential and Personality Psychology, Institute of Psychology II, Technische Universität Dresden, Dresden,
Germany; 4Institute of Medical Biometry, Informatics, and Epidemiology, University of Bonn, Bonn, Germany and 5Department
of Internal Medicine II, Technical University of München, München, Germany
Nitric oxide (NO) is a gaseous neurotransmitter thought to play important roles in several
behavioral domains. On a neurobiological level, NO acts as the second messenger of the Nmethyl-D-aspartate receptor and interacts with both the dopaminergic as well as the
serotonergic system. Thus, NO is a promising candidate molecule in the pathogenesis of
endogenous psychoses and a potential target in their treatment. Furthermore, the chromosomal locus of the gene for the NO-producing enzyme NOS-I, 12q24.2, represents a major
linkage hot spot for schizophrenic and bipolar disorder. To investigate whether the gene
encoding NOS-I (NOS1) conveys to the genetic risk for those diseases, five NOS1
polymorphisms as well as a NOS1 mini-haplotype, consisting of two functional polymorphisms located in the transcriptional control region of NOS1, were examined in 195 chronic
schizophrenic, 72 bipolar-I patients and 286 controls. Single-marker association analysis
showed that the exon 1c promoter polymorphism was linked to schizophrenia (SCZ), whereas
synonymous coding region polymorphisms were not associated with disease. Long promoter
alleles of the repeat polymorphism were associated with less severe psychopathology.
Analysis of the mini-haplotype also revealed a significant association with SCZ. Mutational
screening did not detect novel exonic polymorphisms in patients, suggesting that regulatory
rather than coding variants convey the genetic risk on psychosis. Finally, promoter
polymorphisms impacted on prefrontal functioning as assessed by neuropsychological
testing and electrophysiological parameters elicited by a Go-Nogo paradigm in 48 patients
(continuous performance test). Collectively these findings suggest that regulatory polymorphisms of NOS1 contribute to the genetic risk for SCZ, and modulate prefrontal brain functioning.
Molecular Psychiatry (2006) 11, 286–300. doi:10.1038/sj.mp.4001779; published online 3 January 2006
Keywords: polymorphism; neuronal NOS; promoter; electrophysiology; genomic imaging;
continuous performance test
Introduction
Schizophrenia (SCZ), one of the most devastating
mental illnesses, has a substantial genetic background
with a heritability of up to 81%;1 however, only risk
genes contributing with small odds ratios were
replicated in association studies. Furthermore, > 20
linkage analyses were conducted to date, including
> 1200 pedigrees with almost 3000 affected cases.
Correspondence: Dr A Reif, Section for Molecular and Clinical
Psychobiology, Department of Psychiatry and Psychotherapy,
University of Würzburg, Füchsleinstr. 15, D-97080 Würzburg,
Germany.
E-mail: a.reif@gmx.net
Received 28 July 2005; revised 1 November 2005; accepted 7
November 2005; published online 3 January 2006
Replicated loci include 1q, 6p24, 8p21, 13q32 and
22q11 and led to positional cloning approaches
resulting in haplotype analyses of candidate genes.
Among the most intensively studied, RGS4, dysbindin, neuregulin-1 and G72/G30 were replicated,2
although at-risk haplotypes showed substantial discrepancies between populations and only consisted
of probably non-functional, mostly intronic polymorphisms. Thus, no functional gene variant or
mutations were yet derived from linkage analyses.
Apparently the same is true for bipolar disorder
(BPD), which shows considerable overlap with SCZ
with regards to risk loci (13q, 22q).3,4 A further
consistently identified locus for endogenous psychoses, usually with Lod scores between 2 and 3, is
located on 12q22–24. BPD has been replicated 8
LOD-Score
NOS-I and psychotic disorders
A Reif et al
5
2
0
95.000.000
105.000.000
115.000.000
125.000.000
135.000.000
Chromosomal location (12q) built on Ensembl Freeze 04/04
DAAO
ATP2A2
NOS1
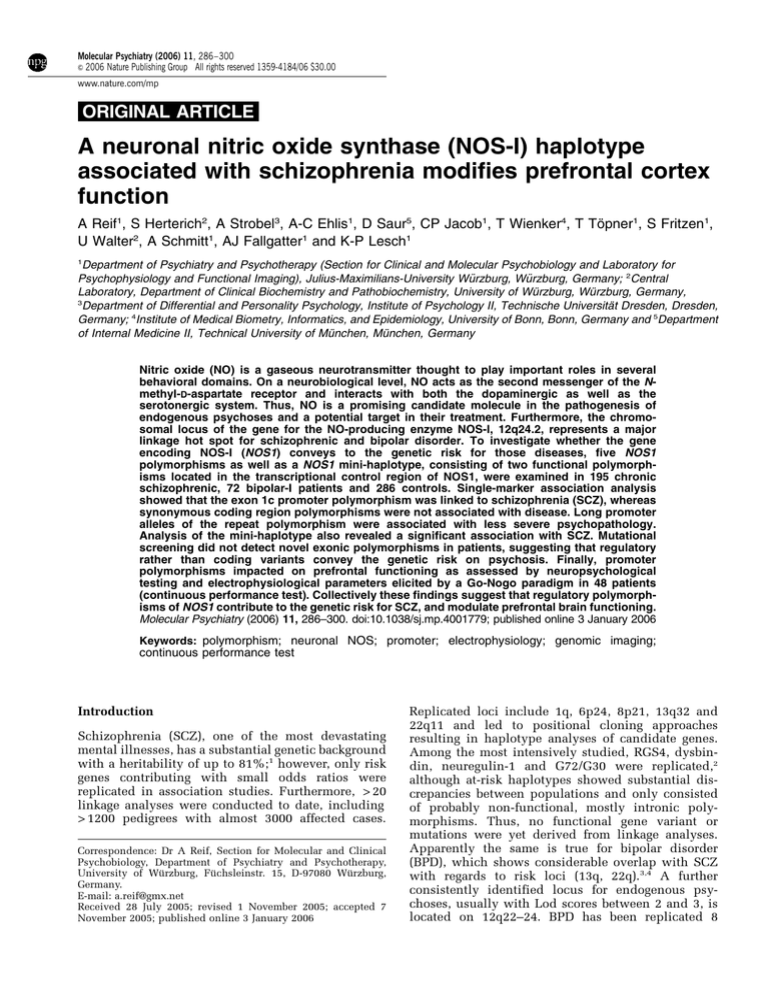
Figure 1 Based on the chromosomal location built on
Ensembl Freeze 04/04, Lod scores of markers on 12q24 are
given; the investigated phenotype was either SCZ,14–18,23
bipolar disorder5–12,19,22 or major depression.13 Highlighted
are the loci for DAAO, suggested as a candidate gene for
bipolar disorder and SCZ, ATP2A2 (the Darier’s disease
gene) and NOS1.
times,5–12 but also major depression (MD) was linked
to this locus with a very high Lod-score > 6, which
might be due to the homogeneity of the sample
consisting of 110 pedigrees from Utah.13 SCZ and
schizoaffective disorder14–17 and the marker ‘negative
symptoms’ in SCZ18 linked to 12q22–24 as well.
Furthermore, Darier’s disease, a dermatological disorder mapping to 12q24.2, co-segregates with BPD.19–22
Finally, obesity as a side-effect of neuroleptics maps
to this region.23 Figure 1 provides an overview on
linkage findings on 12q22–24 reported to date.
One intriguing candidate gene on 12q24 is the socalled neuronal isoform of nitric oxide synthase,
NOS-I. NOS-I is the main source of NO in excitable
tissue and can be found in up to 1% of all neurons.24
NO is a pleiotropic messenger molecule, which inter
alia functions as the second messenger of the Nmethyl-D-aspartate (NMDA) receptor.25 Furthermore,
the nitrinergic system is not only closely connected to
the dopamine system, but also to serotonergic
neurotransmission which provides a rationale for
the involvement of NO and its pathway in both
schizophrenic and affective disorders. Accordingly, a
rapidly increasing body of evidence coming from
pharmacological studies in animals argues in favour
of this hypothesis.26–35 Finally, a landmark study by
Akbarian et al.,36,37 followed by further histopathological investigations,38 argues that nitrinergic neurons
are pathologically altered in SCZ.
Interestingly, a single but not precisely described
marker within NOS1 (the gene encoding NOS-I)
reached a P < 0.05 for association with BPD.10
D12S366, located only 800 kb from NOS1, was found
to be associated with BPD and SCZ in three
studies.14,15,39 The human NOS1 gene is of outstanding complexity and features 12 alternative untrans-
lated first exons, termed exon 1a–1l, driven by
distinct promoters. The genomic region covering
these alternative promoter-exons units spans 130
kilobases; the coding regions, consisting of 28 exons,
extend over further 110 kilobases. Four association
studies were published investigating a synonymous,
exonic single nucleotide polymorphism (SNP) in
exon 29 (which codes for the last 4 amino acids of
the translated protein and the 30 -UTR), or an SNP in
intron 29 of NOS1 in SCZ and depression. The first
study, including 200 patients, reported an association
of NOS1 with SCZ,40 while a replication study
including 200 subjects was negative.41 Another
association study aiming at BPD failed to detect
association as well,42 as did another report on MD.43
In summarizing these conflicting findings, it needs to
be emphasized that all studies investigated only one
SNP, which by itself most likely is not functional, so
that the power to detect modest gene effects is
probably insufficient. Intriguingly, also proteins that
interact with NOS-I were suggested to play a role in
SCZ. Linkage of the disease to carboxy-terminal PDZ
ligand of neuronal NO synthase (CAPON) on chromosome 1q22 was demonstrated in two independent
studies:44,45 CAPON is an adaptor protein, regulating
the coupling of NOS-I to the NMDA receptor via the
enzyme’s PSD95 domain. PSD95 expression in turn is
decreased in SCZ and BPD.46
Based on genetic and functional findings, NOS1
thus represents a candidate gene of considerable
interest. Since studies conducted to date are ambiguous, we chose to perform a haplotype analysis of
NOS1 including four SNPs, one of which is a
functional promoter variant, and one promoter variable number of tandem repeat (VNTR) in SCZ and
BPD. We hypothesized that promoter variants with
functional impact, but not synonymous exonic SNPs
are associated with disease. To screen for novel
coding region variants, we also conducted a mutational analysis of protein coding exons. Finally, the
variants of NOS1’s transcriptional control region
thought to influence gene expression were investigated concerning their neurophysiological and
neuropsychological impact.
287
Materials and methods
Subjects
A total of 267 unrelated patients (mean age 44714
years; 125 male, 148 female) from the Lower Franconia area in Germany participated in this study, which
were ascertained at the Department of Psychiatry and
Psychotherapy, University of Würzburg. All patients
were inpatients at the Department of Psychiatry at
least once. One hundred and ninety-five patients
suffered from schizophrenic disorders according to
ICD-10 criteria (56, paranoid type; 39, hebephrenic
type; six, catatonic type; nine, undifferentiated type;
25, residual type; 7, SCZ simplex; 3, SCZ not
otherwise specified; 13, delusional disorder; 37,
schizoaffective disorder). None of the subjects
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
288
remitted completely during the course of the disease
and thus the sample consists entirely of patients
suffering from chronic SCZ, that is, it is selected for
severe cases. To test whether different classification
systems lead to more refined results, the Leonhard
classification47 was additionally applied and patients
were subdivided into two subgroups, the first comprising of highly heritable schizophrenic disorders
with bipolar course (group A SCZ; n = 147; so-called
‘unsystematic SCZ’) and the second covering less
heritable disorders leading to stable residual states
(group B SCZ; n = 48; ‘systematic SCZ’). Brief Psychiatric Rating Scale (BPRS) ratings were performed
by an experienced rater (AR) in 119 patients. The
mean Global Assessment of Functioning (GAF) score
of those patients was 52710, mean BPRS score was
4079. This relatively low BPRS score is explained by
the fact that all patients consented after the beginning
of neuroleptic treatment and according clinical
improvement.
Seventy-two inpatients suffered from BPD according to ICD-10 criteria. Only patients with at least one
manic and one depressive episode leading to treatment were classified as BPD (i.e., strict bipolar-I
criteria). While 82 SCZ spectrum disorder subjects
had a positive family history for psychosis in firstdegree relatives (corresponding to 42% of the total
sample; in systematic SCZ 9/48 patients had a
positive family history, in unsystematic SCZ 73/147;
w2 = 17.04, P < 0.0001), 66 BPD patients ( = 91%) had a
positive family history, in almost all cases for
depression or BPD.
None of the subjects showed significant neurological comorbidity, epilepsy, mental retardation or other
somatic disorders suggesting organic psychiatric
disorder. Patients with substance-induced psychotic
or affective episodes were excluded from the study as
well. Diagnoses were made by an extensive, semistructured interview analogous to the AMDP interview48 performed by an experienced psychiatrist (AR
or CPJ), along with chart reviews. If possible, further
information was retrieved from family informants and
case records from other hospitals to ensure consistent
diagnoses. Chart reviews of every patient were
performed by AR.
A sample of DNA probes derived from 284 control
subjects (150 males, 134 females) has been collected,
consisting of healthy blood donors stemming from the
same catchment area as the patient group. The sample
was not screened for psychiatric disorders; however,
all subjects were free of medication, and the study
was explained to them, so that the likelihood that
severe psychiatric disorders, especially chronic SCZ,
present in the control sample was low. Mean age of
controls was 35713 years. Both patients as well as
controls were of Caucasian origin. Only patients and
volunteers who gave written informed consent after
oral as well as written explanation about scope and
aim of the investigation were enrolled in the study.
The study was approved by the Ethics Committee of
the University of Würzburg.
Molecular Psychiatry
Genomic control
To control for ethnic stratification, five highly polymorphic short tandem repeat (STR) markers
(D2S2186, D3S1314, D4S2950, D22S420 and NOS1
VNTR1) were determined by PCR amplification and
size determination was as described below. STR
repeat frequencies can be obtained from the corresponding author on request. Thereafter, the CLUMP,49
CHECKHET,50 GENEPOP,51 POWERMARKER52 and
STRUCTURE53 software packages were used to
investigate for population stratification both between
as well as within the patient and the control sample.
Genotyping
For haplotype analysis, four SNPs and one VNTR54
were chosen as markers. (Nomenclature with regards
to NOS1 exon structure varies across different publications, as multiple exons 1 exist, which are not
translated, so that exon 2 represents the first translated exon. Therefore, this exon sometimes is designated as exon 1. In this paper, exon 1 refers to the
alternatively spliced UTR exons (in detail termed
exon 1a–1l), exon 2 is the first and exon 29 the last
translated exon.) Both the VNTR (hereafter termed
VNTR1) and one SNP (G-84A; hereafter termed SNP1;
Saur et al.55) are within the promoter region of NOS1
exons 1f (VNTR1) and 1c (SNP1), respectively, and
were suggested to be functional. Three further SNPs
were selected, which are located within the exons 13
(rs2293054, SNP2), 18 (rs1047735; SNP3) and 29
(rs2133681; SNP4). Another SNP (SNP5), originally
intended to be included in subsequent analysis
(located in exon 27; rs2293044), was not used
following genotyping, as only one patient and four
controls were heterozygous for this polymorphism,
contrary to database information giving a heterozygosity index of 0.162. All exonic SNPs are synonymous.
VNTR1 has been determined by PCR amplification
and product size determination. One of the primers,
VNTR1-Fw, was labeled with a fluorescent dye (cy-5;
TIB MolBiol, Berlin) enabling detection of the resulting PCR product. PCR was performed in a 50-ml
reaction mix containing 50 nM primers, 200 mM
dNTPs, 1.5 mM MgCl2 in PCR-buffer, 50 ng template
DNA, and 0.4 U Taq polymerase. Initial denaturation
for 3 min at 961C was followed by 33 cycles of 961C for
20 s, 581C for 20 s and 721C for 30 s. Electrophoretic
separation of the PCR products was performed using a
CEQ8000 DNA-sequencer (Beckman-Coulter, Krefeld,
Germany). An external standard allows size determination of the PCR products. Internal standards
contain previously sequenced DNA fragments of
known alleles. VNTR1 genotyping was accomplished
by comparing the allele sizes in each sample with the
sizes of known alleles. The STR markers D2S2186,
D3S1314, D4S2950, D22S420 were genotyped analogously except that touchdown PCR was performed
using all four primer pairs in one reaction. Cy 5 and
cy 5.5 fluorescent primers were used (TIB MolBiol,
Berlin). After initial denaturation for 3 min at 961C, 10
NOS-I and psychotic disorders
A Reif et al
cycles of 20 s denaturation at 961C, annealing for 20 s
at decreasing temperatures of 63–531C and elongation
for 30 s at 721C were followed by 30 cycles as above
with 531C annealing temperature. SNP2 (IVS13 þ 13
C-G) was determined by denaturing high performance liquid chromatography (dHPLC) analysis following routine PCR. Heteroduplexes were obtained
by denaturating for 2 min at 961C and cooling down to
41C at 21C s1. Genotype analysis was performed
on a Transgenomic WAVE system using the DNASept
column (Transgenomic, Elancourt, France). Melting
characteristics and separation method of the DNA
fragment were predicted by use of the wavemakert
software (version 4.1.44). Five microliters of the
PCR product were injected and separated at 631C.
Heteroduplexes appeared in two separated peaks in
the chromatogram and could reliably be differentiated
from homozygotes showing only one DNA peak.
Samples shown by dHPLC analysis to contain one
uniform sequence were mixed with equal amounts of
a wild-type PCR product (typically 10 ml of each),
denatured and re-annealed; 5 ml of this mixture were
separated on the WAVE system. SNP1, SNP3 and
SNP4 were genotyped by standard PCR and subsequent digest with Fnu4HI (SNP1), NlaIII (SNP3) and
Eco72I (SNP4) followed by gel electrophoresis. Primer
pairs for all polymorphisms and detailed PCR conditions are available on request.
Mutational analysis
In 205 patients (160, SCZ spectrum disorders; 45,
BPDs) of the above sample, coding regions critical for
the function of NOS-I (exon 2, containing the PSD-95
and PIN binding domains; exons 5 and 6, containing
the heme binding domain; exon 13 and 14, containing
the CaM binding site; and exon 27, contributing to the
NADPH binding site) were screened for mutations. To
do so, exons were amplified by PCR and sequenced.
For preparing the amplicons, the PCR Product PreSequencing Kit was used according to the instructions given by the supplier (USB, Cleveland, OH,
USA). The subsequent products were subjected to
cycle sequencing using the Quick Start Sequencing
Kit (Beckman, Krefeld, Germany). In brief, each
sequencing reaction contained 2 ml purified PCR
product, 2 ml reaction mix and 5 pmol primer in a
10 ml reaction. Cycle sequencing and subsequent
ethanol precipitation was performed according to
the manufacturer’s instructions. The sequencing
products were electrophoresed in a CEQ8000 DNAsequencer (Beckman, Krefeld, Germany). The remaining exons were screened by the same method in 20
selected patients (16, SCZ spectrum disorders; four,
bipolar affective disorders). Primer sequences are
available on request.
Statistical and haplotype analysis
Single association tests were performed by means of
w2 tests using SPSS for Windows 9.0. (SPSS Inc.,
Chicago, IL, USA). Pairwise linkage disequilibrium
(LD) between the polymorphisms was assessed using
2LD.56 Tests for global haplotype associations and for
significance of differences between controls and
patients in estimated frequencies of specific haplotypes were performed using the GENECOUNTING/
PERMUTE utility of the GENECOUNTING software.56
Both programs are available for download at:
http://web1.iop.kcl.ac.uk/iop/Departments/PsychMed/
GEpiBSt/software.shtml. GENECOUNTING implements
an expectation maximization algorithm to resolve
uncertain haplotypes and provides maximum-likelihood estimates of haplotype frequencies. It performs
permutation tests for global association/significance
of specific haplotypes by randomly reassigning case
and control labels in the actual data. The resulting
P-values reflect the proportion of replicates that
produce values of statistics at least as large as the
observed. In the current study, 10 000 permutations
were performed.
289
Semiquantitative real-time PCR of NOS1 exon 1c and
1f in human brain
Post-mortem adult human brain specimens of two
autopsy cases were obtained from the Austro–German
brain bank (Würzburg, Germany; Gsell et al.57).
Individuals had neither a history of neurological nor
of psychiatric disorders and lacked any neuropathological abnormalities. The following regions were
obtained: cortex frontalis, cortex frontoorbitalis, caput
nuclei caudate, corpus nuclei caudate, putamen pars
posterior and hippocampus. Dissection protocols and
sample preparations were described previously.57
Total RNA was isolated using the RNeasy RNA
isolation kit (Qiagen, Hilden, Germany) and the
RNase-free DNase Set (Qiagen) following the manufacturer’s protocols. Five hundred nanograms of total
RNA were reverse transcribed using the iScriptt
cDNA Synthesis Kit (BioRad, Cambridge, MA, USA).
Thereafter, expression of human NOS1 mRNA variants was quantified as described before55 using an
ABI Prism 7700 Sequence Detection System (Applied
Biosystems, Foster City, CA, USA), cDNAs corresponding to 12.5 ng of total RNA and the following
PCR conditions: one cycle 501C, 2 min; 951C, 10 min;
50 cycles 601C, 1 min; 951C, 15 s. Alternative NOS1
transcripts were amplified with primers and probes
complementary to the first exons 1c and 1f (forward
primers) and the common exon 2 (reverse primer,
probe) (for primer and probes see Saur et al.58). As
endogenous reference, the globally expressed housekeeping gene GAPDH (primers and probes were
purchased from Applied Biosystems, Foster City,
CA, USA) was used. For each amplicon, the amount
of target and endogenous reference was determined
from a standard curve generated by serial five-fold
dilutions of plasmids containing the respective target
sequence. The standard curve was amplified in
triplicate during every experiment and the amount
of target gene was normalized by the endogenous
reference. Signals were analyzed by the ABI Prism
Sequence Detection System software version 1.9
(Applied Biosystems, Foster City, CA, USA).
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
290
Electrophysiological and neuropsychological
examinations
Forty-eight acutely psychotic inpatients of the
Department of Psychiatry and Psychotherapy, University of Würzburg, were investigated. In these
patients, VNTR1, SNP1, SNP3 and SNP4 were
genotyped as described above (33 patients were also
included in the single SNP association and haplotype
analysis). For each of the polymorphisms, the different subgroups of patients were matched regarding
their mean age, gender and handedness distribution,
daily chlorpromazine equivalents of antipsychotic
medication, ICD-10 diagnosis, duration of the disease,
as well as number and duration of psychiatric
hospitalizations in the past. There were no significant
differences between the various groups of patients
concerning any of the above-mentioned parameters
(all t-values < 1.55, P > 0.13; all w2 < 4.7, P > 0.3).
All these patients suffered from SCZ spectrum
disorders according to ICD-10 criteria (12 paranoid
type; six hebephrenic type; three catatonic type;
seven undifferentiated type of SCZ; 16 acute polymorphic psychotic disorders or schizophreniform
disorders; five schizoaffective disorder). Eight
patients had a positive family history for SCZ with
an affected first-degree relative, whereas another 20
patients had first-degree relatives with non-psychotic
or unknown psychiatric conditions. Neuroleptic
treatment consisted of 4787385 mg (mean7s.d.)
chlorpromazine equivalents per day. Each patient
underwent an extensive psychopathological examination, consisting of the SCID-I-Interview, the BPRS, the
Positive and Negative Symptoms Scale (PANSS), and
the Hamilton Depression Rating Scale/24 Items
(HDRS). Neuropsychological assessment consisted of
the Verbal Fluency Test (VFT; letters and categories
version), the Stroop Color Word Task, and the Trail
Making Test (TMT; parts A and B).
Shortly after admittance, the patients were investigated electrophysiologically by means of a Continuous Performance Test (CPT) as published previously
(e.g. Reif et al.59). Briefly, 400 letters were presented
sequentially in a pseudo-randomized order; patients
were instructed to press a response button whenever
the primer condition ‘O’ (114 stimuli) was directly
followed by an ‘X’ (Go condition, n = 57). Nogo was
defined as ‘O’ followed by any other letter than ‘X’.
Each letter was presented for 200 ms with an interstimulus interval of 1650 ms. Parallel to this task, EEG
was recorded from 21 scalp electrodes. Data analysis
was performed offline with the program ‘Vision
Analyzer’ (Brain Products, Munich, Germany). The
data were segmented into the different conditions of
the CPT, and Go and Nogo epochs were further
analyzed. Segments were averaged to one Go and one
Nogo event-related potential (ERP) per subject,
whereby only trials with correct responses were
included in the ERP analysis. For the topographical
analysis, the global field power (GFP)60 peaks were
determined within a P300 time frame (275–530 ms).
At individual GFP peaks, amplitude, latency and
Molecular Psychiatry
anterior–posterior location of the positive centroid
were calculated. From these data, the Nogo-anteriorization (NGA),61–63 defined as the distance between
the individual Go and Nogo centroid, was determined. Furthermore, amplitudes and latencies as
traditional measures of the P300 component were
analyzed at electrode positions Fz, Cz and Pz.
For the topographical ERP analysis, 2 2 analyses
of variance (ANOVAs) for repeated measurements
were conducted for each of the four polymorphisms,
with the within-subject factor ‘condition’ (Go versus
Nogo) and the between-subject factor ‘group’. For the
traditional waveform ERP analysis, similar ANOVAs
were calculated for the amplitudes and latencies of
the P300 peaks, with the within-subjects factors
‘condition’ (Go versus Nogo) and ‘electrode position’
(Fz, Cz, Pz) and the between-subject factor ‘group’.
Post hoc analyses were conducted by means of
two-tailed t-tests for matched or independent
samples. T-tests were also used to compare the
psychopathological and neuropsychological data as
well as the behavioral performance during the CPT
between the different groups of patients, when two
genotypes were compared (e.g. SNP1 A/A and A/G
versus G/G). When more than two genotypes were
contrasted (e.g. VNTR1 SS, LS and LL), univariate
ANOVAs were applied, followed by post hoc t-tests if
indicated.
Results
Genomic control
Four highly polymorphic markers as well as the
NOS1 VNTR1 itself were used to evaluate whether the
patient and the control sample are genetically homogenous or not. Using the CHECKHET program, one
subject has been identified carrying an abnormal
genotype. Three software packages (GENEPOP,
POWERMARKER and STRUCTURE) were used to
investigate for population stratification both between
as well as within the patient and the control sample.
All calculations yielded negative results, that is, the
tested samples are genetically homogenous. Using the
CLUMP software, neither marker was found to be
associated with the phenotype ‘patient’ further
supporting the assumption of genetic homogeneity.
Allele and genotype frequencies
Four SNPs and one VNTR of the NOS1 locus were
determined and tested for association with disease, in
the first step of the study by means of a single-marker
association analysis. Several new alleles of VNTR1
were identified. VNTR1 alleles were distributed in a
bimodal fashion (Figure 2), with one peak for long
and two peaks for short alleles. Only eight out of the
15 VNTR1 alleles observed in the present sample had
a frequency greater than 1% and accounted for about
98% of the total variation (C, 17.4%; D, 5.4%; H,
18.7%; I, 2.4%; L, 13.5%; M, 7.9%; N, 30.7; O, 1.8%).
This may suggest functional relevance of and/or
evolutionary pressure on this polymorphism, and
NOS-I and psychotic disorders
A Reif et al
thus VNTR1 alleles were dichotomized in short (B–J)
and long (K–R) alleles in subsequent single association studies. Of the 49 VNTR1 genotypes observed in
the present sample, 21 had a frequency greater than
1% and accounted for 89% of the variation (the four
most frequent genotypes were: CN, 11.6%; HN,
11.5%; NN, 9.1% and LN, 8.9%).
The frequency of SNP1 A-allele was 10.5%. As
there were only five subjects with the A/A genotype
(0.9%), they were grouped together with the A/G
genotype (19.1%) and compared to the G/G genotype
(80.0%) in subsequent single-marker association
analyses. The allele and genotype frequencies of the
three other SNPs, all consisting of C/T transitions,
were comparable (alleles: C, B70%; T, B30%;
genotypes: C/C, B49%; C/T: B42%; T/T: B9%).
The genotypes of all four SNPs and VNTR1 were in
Hardy–Weinberg equilibrium (P = 0.135).
400
n (chromosomes)
350
300
250
Table 1 gives the pairwise LD between the five
NOS1 polymorphisms examined. Except for the
SNP1-SNP3, and SNP1-SNP4 pairs, respectively, the
polymorphisms were in significant LD. The comparably small D0 values are presumably due to the high
number of VNTR1 alleles, to the low frequency of the
rare SNP1 A allele, and to the fact that the NOS1
region examined spans about 240 kilobases.
Table 2 summarizes the results of the single
association analyses with regard to the two presumably functional NOS1 promoter polymorphisms. w2
tests showed that schizophrenic patients did not
differ significantly from controls in dichotomized
VNTR1 genotype frequencies (w2 = 2.08, df = 2,
P = 0.335), whereas the SNP1 A/A and A/G genotypes
were significantly more frequent among schizophrenic patients than among controls (w2 = 5.42, df = 1,
P = 0.020). Subsequent analyses for subgroups of
schizophrenic patients divided into group A and B
SCZ (see Materials and methods), revealed that the
association between SNP1 and SCZ was mainly due
to considerably higher frequencies of the A/A and A/
G genotypes in the group B SCZ subgroup (w2 = 8.42,
df = 1, P = 0.004), whereas there was no significant
effect in the group A SCZ subgroup (w2 = 2.03, df = 1,
P = 0.154). There was no significant effect of VNTR1
with regard to the two SCZ subgroups. Similarly,
291
200
150
Table 1 Pairwise LD between NOS-I polymorphisms
100
50
0
B C D E F G H
I J K L M N O P Q
Allele
Figure 2 Allelic distribution of the NOS1 promoter VNTR
in 1088 chromosomes, determined as described in the
Materials and methods section. Alleles are arranged from
short (B) to long (Q).
Table 2
patients
VNTR1
SNP1
SNP2
SNP3
SNP4
VNTR1
SNP1
SNP2
SNP3
SNP4
—
0.003
< 0.001
< 0.001
< 0.001
0.281
—
0.031
0.077
0.525
0.411
0.293
—
< 0.001
< 0.001
0.465
0.238
0.569
—
< 0.001
0.310
0.085
0.386
0.552
—
Note: Above diagonal: D 0 , below diagonal: significance of
D 0.
NOS-I VNTR1 and SNP1 genotype frequencies (and percentages) in controls, schizophrenic patients and bipolar
NOS-I
Controls
SCZ
BPD
Total sample
Group B
Group A
VNTR1
SS
LS
LL
w2 (df = 2)
46 (0.16)
147 (0.52)
90 (0.32)
37 (0.20)
101 (0.54)
49 (0.26)
2.08, P = 0.353
7 (0.15)
29 (0.62)
11 (0.23)
1.70, P = 0.429
30 (0.21)
72 (0.52)
38 (0.27)
2.07, P = 0.355
13 (0.21)
36 (0.59)
12 (0.20)
3.71, P = 0.156
SNP1
A
Aþ
w2 (df = 1)
234 (0.83)
49 (0.17)
141 (0.74)
50 (0.26)
5.42, P = 0.020
31 (0.65)
17 (0.35)
8.42, P = 0.004
110 (0.77)
33 (0.23)
2.03, P = 0.154
51 (0.84)
10 (0.16)
0.03, P = 0.863
Note: Bold-faced: P < 0.05.
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
292
neither VNTR1 nor SNP1 were significantly associated with BPD (although the difference in VNTR1
LL genotype frequencies between controls and BPD
actually reached marginal significance when grouping together the SS and LS genotypes and comparing
them to LL; w2 = 3.54, df = 1, P = 0.060). No significant
association with SCZ or BPD were observed for all
three synonymous coding SNPs (w2 tests, df = 2, all
P > 0.5; data not shown). When applying a Bonferroni
correction considering all NOS1 variants and all four
groups examined (i.e., SCZ total, group A SCZ, group
B SCZ, and BPD), the association between SNP1 and
group B SCZ (which exactly had a significance of
P = 0.0037) failed to reach significance, the adjusted
level of significance of a0 = 0.05/(5 polymorphisms 4
patient groups) = 0.0025. It has to be noted, however,
that Bonferroni correction might be too conservative
for the current setting because Bonferroni correction
assumes independence of the statistical tests performed, which is certainly not the case in our
analyses.
Haplotype analyses
Haplotype analyses focused on the two putatively
functional NOS1 promoter polymorphisms. Twentyfour VNTR1-SNP1 haplotypes were observed in the
present sample. A test for global haplotype association with SCZ did not yield a significant result
(P = 0.149). However, when performing haplotype
association tests for SCZ subgroups as performed in
the single SNP association analyses, a significant
global haplotype association was found for group B
SCZ (P = 0.020), whereas for group A SCZ, there was
no association (P = 0.347). Table 3 shows the haplotype frequency estimates for controls and for schizophrenic patients (total sample, group A and B SCZ).
There were several frequency differences between
patients and controls being significant at the 5%
level, but in most cases these differences were found
for very rare haplotypes. One significant frequency
difference, however, was observed for a more common haplotype: the estimated VNTR1(N)-SNP1(A)
haplotype was present in 3.8% of the controls, but in
7.9% of patients with SCZ and even in 14.6% of the
patients with group B SCZ (P = 0.002). A haplotype
analysis for BPD did not yield significant results
(global P = 0.533).
Mutational analysis
In 205 patients (160, SCZ; 45, bipolar affective
disorder), exons critical for the catalytic function of
NOS-I (2,5,6,13,14, and 27) were screened for mutations by means of dHPLC to investigate for further
variants in coding regions, which could be in LD with
the examined polymorphisms. The remaining exons
likewise were analyzed in 20 selected patients (16,
SCZ; four, bipolar affective disorder). Table 4 provides
an overview on all detected mutations; variants were
more frequent in the reductase domain, while the
oxygenase region was highly conserved. No nonsynonymous mutations in the coding region were
found.
Neuropsychological investigations
Forty-eight schizophrenic patients were investigated
for an association of both neuropsychological and
Table 3 Estimated frequencies of NOS1 VNTR1 and SNP1 haplotypes in controls, schizophrenic patients and subgroups of
schizophrenic patients
VNTR1
SNP1
Controls
SCZ
Total sample
C
D
F
H
H
I
J
K
L
L
M
N
N
O
G
G
G
A
G
G
G
G
A
G
G
A
G
G
0.158
0.050
0.000
0.009
0.167
0.017
0.008
0.004
0.018
0.131
0.083
0.038
0.276
0.015
0.190
0.055
0.003
0.027
0.158
0.021
0.005
0.011
0.009
0.114
0.057
0.079
0.234
0.016
(0.234)
(0.380)
(0.338)
(0.021)
(0.600)
(0.611)
(0.652)
(0.237)
(0.298)
(0.513)
(0.151)
(0.009)
(0.115)
(0.496)
Global P = 0.136
Group B
0.189
0.044
0.011
0.031
0.136
0.011
0.022
0.033
0.000
0.144
0.044
0.146
0.165
0.022
(0.664)
(0.807)
(0.027)
(0.096)
(0.534)
(0.762)
(0.223)
(0.020)
(0.268)
(0.816)
(0.270)
(0.0004)
(0.047)
(0.382)
Global P = 0.020
Group A
0.182 (0.436)
0.059 (0.437)
—
0.026 (0.037)
0.167 (0.801)
0.021 (0.573)
0.000 (0.006)
0.004 (0.947)
0.007 (0.249)
0.107 (0.378)
0.062 (0.317)
0.060 (0.183)
0.258 (0.486)
0.014 (0.647)
Global P = 0.347
Notes: For reasons of simplicity, only those of the 24 observed haplotypes with a frequency of at least 1% in one of the groups
are shown (complete data available upon request); in parentheses: permutation-based significance of frequency differences
compared to controls (10,000 permutations); bold-faced: P < 0.05; italics: meaningful frequency differences.
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
Table 4
293
Mutations and SNPs detected in the mutational analysis
Exon
Position
Variant
Analysis
Known?
7
13
15
16
17
17
18
19
20
21
27
27
27
27
27
27
29
IVS715
SNP2
IVS15 þ 38
2607 (SNP)
2712 (SNP)
IVS17 þ 15 (SNP)
SNP3
IVS19 þ 13 (SNP)
137244
3258(SNP)
SNP5
4063 (mutation; detected in 2 from 488 subjects)
4065 (SNP)
4154 (private mutation)
IVS27 þ 14 (private mutation)
IVS27 þ 9 (private mutation)
SNP4
C-G
C-T (Ile/Ile)
C-T
C-T (Pro/Pro)
C-T (His/His)
A-G
C-T (His/His)
T-G
A-G
C-T (Asp/Asp)
C-A (Val/Val)
G-A (Val/Ile)
G-A (Val/Val)
G-A (Gly/Asp)
T-G
C-A
C-T (30 -UTR)
B
A
B
B
B
B
A
B
B
B
A
A
A
A
A
A
A
Yes
Yes
No
Yes
Yes
No
Yes
No
No
Yes
Yes
No
Yes
No
No
No
Yes
Exons 2–14 code for the oxygenase domain, exons 15–29 for the reductase domain of NOS-I.
Analysis: A, expanded analysis in at least 205 patients (exons critical for the catalytic function, i.e. 2, 5, 6, 13, 14, and 27) as
well as 283 controls (exons 5, 13, 27); B, analysis of the remaining exons in 20 patients. Known? Indicates whether the variant
is already described in the Ensembl database (June 2006). SNP2-5 refer to the SNPs investigated in the haplotype analysis as
described in the Materials and methods section.
electrophysiological measures with VNTR1 (dichotomized in short and long alleles), SNP1 (A/A and A/G
combined versus G/G), SNP3 and SNP4 genotype.
With respect to psychopathological scales, carriers of
SNP1 A-allele (A/A or A/G, n = 11) did not significantly differ from G/G-patients (n = 31), whereas
VNTR1 genotype (SS, n = 11 patients; LS, n = 20; LL,
n = 16) had a statistically significant influence on
PANSS positive, HDRS and GAF scores (F2,42 = 3.87,
3.82 and 3.49, respectively; P < 0.05). Post hoc tests
indicate that patients with an SS-genotype had higher
values for the PANSS positive scale (t23 = 3.14,
P < 0.01) and the HDRS (t23 = 2.56, P < 0.05) in comparison to LL-carriers (Table 5), which was mirrored
by an accordingly low GAF score (t23 = 2.62, P < 0.05).
Compared to the heterozygous genotype (LS), the SSgroup still had significantly lower GAF-scores
(t29 = 2.24, P < 0.05). However, due to the relatively
low number of SS-carriers these findings should
be interpreted cautiously. With most of the other
psychopathological test scores lying in-between the
two homozygous genotypes, the LS-group did not
differ significantly from either of them on any other
scale (cf. Table 5).
Regarding the neuropsychological tests (VFT,
Stroop Test, TMT), there was no difference in the
performance of SNP1 A-allele carriers and G/G
patients (Table 5). With respect to VNTR1, a respective ANOVA indicated a trend for a statistical
influence of the genotype on VFT performance
(F2,42 = 2.64, P < 0.1), with LS patients tending to
perform better than SS patients (t29 = 1.97, P < 0.1)
and LL (t32 = 1.84, P < 0.1) in the category version of
the task. Reaction times and error rates in the CPT are
also displayed in Table 5. Commission errors occurred whenever a patient responded to a non-target
stimulus, whereas omission errors consisted of Go
conditions the patient did not respond to. While there
were no significant differences between the VNTR
groups for any of the behavioral measures, carriers of
the SNP1 G/G-allele made significantly more omission errors than carriers of the A-allele, (t38 = 2.07,
P < 0.05), arguing for reduced attention in those
patients. With respect to SNP3 and SNP4, there were
neither differences in psychopathological or neuropsychological measures, nor in CPT performance (not
shown). Please note that no correction for multiple
testing was applied for the analysis of psychopathological and neuropsychological scores. Therefore, the
results have to be considered preliminary, until larger
patient samples are available that allow more conservative statistical analyses.
NGA and ERP data
Regarding the topographical ERP analysis, ANOVAs
revealed significant main effects of the factor ‘condition’ for each of the four SNPs (all F-values > 10,
P < 0.01), with no significant influence of any of the
genetic subgroups. The centroids of the positive
brain electrical field were always located more
anteriorly in CPT Nogo-trials as compared to the
Go-condition, which is a common topographical
pattern (‘Nogo anteriorization’) similarly observed in
healthy subjects. Accordingly, the NGA-values
did not differ between any of the genetic subgroups
(all t-values < 1, P > 0.3).
With respect to P300 latencies, the analysis of
VNTR1 revealed a significant main effect of the factor
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
294
Table 5 Psychopathological and neuropsychological data for subgroups of patients according to their SNP1 and VNTR1
genotype
SNP1
VNTR1
AA/AG (n = 11)
GG (n = 31)
SS (n = 11)
LS (n = 20)
LL (n = 14)
F-values
PANSS
Pos
Neg
Glob
Tot
12.675.6
13.974.2
25.974.3
52.5710.6
14.274.4
15.376.3
31.078.3
60.5716.4
16.774.0
16.173.9
32.478.5
65.2713.2
14.174.8
15.477.5
30.777.7
60.3716.8
11.973.7
13.374.1
28.277.3
53.4712.4
3.87*
0.87
0.91
2.06
BPRS
HDRS
GAF
32.576.7
7.878.9
43.876.9
38.6711.2
8.974.9
39.677.3
42.0710.4
11.976.0
35.675.0
37.7710.9
9.374.3
41.277.3
33.577.9
6.574.6
42.777.7
2.27
3.82*
3.49*
VFT
Letter
Categ
22.579.9
34.5713.4
21.379.4
29.379.6
24.2712.5
27.778.7
23.879.0
35.3710.8
19.178.9
28.2710.8
1.11
2.64w
TMT (B)
Stroop
57.5732.6
122.5757.3
62.0737.4
134.3743.7
59.9732.3
129.9738.4
59.8738.0
122.5736.4
60.2733.7
145.0761.2
0.001
0.91
RT
532.07109.9
600.07178.3
587.57150.8
560.37185.4
610.27147.7
0.38
1.971.9
4.374.2
1.872.5
8.879.9
1.872.9
7.1710.3
2.372.7
7.278.9
1.271.3
7.477.7
0.83
0.01
Errors
Com
Om
Between-group differences were analyzed by means of two-tailed t-tests for independent samples (SNP1) and univariate
ANOVAs followed by post hoc t-tests (VNTR1), respectively. Values that differed significantly between genotype subgroups
were printed in bold type. For the ANOVA analysis, F-values were given and significant results were indicated (*P < 0.05;
w
P < 0.1).
PANSS, Positive and Negative Symptom Scale; BPRS, Brief Psychiatric Rating Scale; HDRS, Hamilton depression rating
scale; GAF, global assessment of functioning; VFT, verbal fluency test; TMT (B), trail making test part B; RT, reaction time;
Com, commission errors; Om, omission errors.
‘genotype’ (F2,42 = 4.73, P < 0.05) due to overall shorter
latencies for the heterozygous genotype (LS). This
group of patients exhibited almost consistently shorter P300 latencies than the two homozygous genotypes, particularly in the Go condition of the CPT and
particularly compared to patients with two long
alleles of the NOS1 promoter (Table 6).
Regarding SNP1, an ANOVA for the P300 latencies
revealed significant main effects of the factors
‘electrode position’ (F2,80 = 6.81, P < 0.01) and ‘genotype’ (F1,40 = 8.87, P < 0.01), as well as a significant
interaction between these two factors (F2,80 = 10.64,
P < 0.001): patients with a G/G-genotype had overall
longer latencies than A/A and A/G patients,
which reached the level of significance for electrode
site Pz in Go trials (t40 = 2.62, P < 0.05) and for
electrode positions Cz and Pz, as well as the GFP, in
Nogo trials (t = 2.11, 4.15 and 2.02, respectively;
P < 0.05, 0.001 and 0.05, respectively). Averaged
across genotype subgroups, latencies were generally
longest at electrode position Fz, shorter at Cz and
shortest at Pz. The significant genotype electrode
position interaction resulted from the fact that
this pattern was reversed (Go trials) or not
Molecular Psychiatry
statistically present (Nogo trials) in the group of G/G
patients.
The analysis of the P300 amplitudes revealed a
significant main effect ‘electrode position’ (F2,84 =
41.67, P < 0.001), as well as significant interactions
‘CPT condition electrode position’ (F2,84 = 44.68,
P < 0.001) and ‘genotype group CPT condition’
(F2,42 = 3.84, P < 0.05) for the analysis of the VNTR1
polymorphism. The influence of the factor ‘genotype’
on P300 amplitudes resulted from the fact that only in
the heterozygous genotype group amplitudes tended
to be higher in Nogo as compared to Go trials, which
can be considered as the ‘normal’ finding. In a direct
comparison of the different genotype subgroups only
one significant difference occurred, with the LS group
exhibiting significantly higher Nogo amplitudes at Cz
than the SS group (t29 = 2.33, P < 0.05) (Table 6).
The same analysis of the P300 amplitudes for
SNP1 genotype subgroups revealed a significant
main effect ‘position’ (F2,80 = 34.08, P < 0.001) as well
as a significant interaction ‘position condition’
(F2,80 = 37.47, P < 0.001), with no other significant
results and in particular no significant influence of
SNP1 genotype on P300 amplitudes. Again, there
NOS-I and psychotic disorders
A Reif et al
Table 6
295
Electrophysiological data for subgroups of patients according to their SNP1 and VNTR1 genotype
SNP1
VNTR1
A/A and A/G (n = 11)
G/G (n = 31)
SS (n = 11)
LS (n = 20)
LL (n = 14)
Centroids
Go
Nogo
3.670.6
3.170.4
3.570.6
3.170.6
3.770.4
3.370.4
3.570.6
3.070.4
3.670.7
3.170.7
NGA
0.570.5
0.470.6
0.370.5
0.570.5
0.470.6
P300 Go amplitudes
Fz
Cz
Pz
1.270.9
2.871.4
3.971.2
1.170.9
2.671.3
3.571.4
1.370.6
2.870.8
3.471.4
1.171.0
2.571.4
3.671.2
0.770.9
2.771.4
3.871.6
P300 Nogo amplitudes
Fz
2.371.2
Cz
4.071.0
Pz
2.770.8
1.970.9
3.071.5
2.171.2
1.671.0
2.771.5
1.971.1
2.171.1
3.871.2
2.671.3
1.870.9
3.171.5
2.371.0
396.0755.9
365.1754.5
346.2756.0
377.4749.3
388.6744.2
396.2753.9
385.7764.6
386.0752.4
398.8759.4
383.0747.8
366.8747.3
361.7756.9
378.1748.7
399.6738.5
406.0750.7
P300 Nogo latencies
Fz
416.2733.3
Cz
372.5738.3
Pz
344.8727.3
404.5738.5
402.1740.6
399.1756.5
405.5742.5
389.2751.8
401.3750.5
393.8744.8
385.9730.6
379.9752.8
415.5736.1
409.3740.4
382.5758.0
P300 Go latencies
Fz
Cz
Pz
Values that differed significantly between genotype subgroups according to (post hoc) t-tests were printed in bold type.
Please refer to the text for the results of the respective ANOVAs.
NGA, Nogo anteriorization; Fz/Cz/Pz, frontal/central/parietal midline electrode positions according to the International
10–20 system of electrode placement.80
Expression of the alternative NOS1 exon 1c and 1f in
the human brain
As the exon 1c (G-84A; SNP1) and the exon 1f
(VNTR1) promoter polymorphisms were associated
with psychosis as well as prefrontal functioning, we
were interested whether these alternative first exons
are expressed in brain regions suggested to be
involved in SCZ (frontal cortex, caudate nucleus,
putamen, hippocampus). To do so, cDNA from two
control brains was prepared as described. Expression
of the alternative exon 1c and 1f was found in every
brain region examined, with relatively high expression levels of exon 1c in the putamen and the
hippocampus, whereas exon 1f was preferentially
expressed in the basal ganglia (Figure 3). Thus, the
expressional regulation exerted by SNP155 is active in
brain regions critically involved in the etiopathogenesis of SCZ, and also the presumably functional exon
1f promoter polymorphism is operational in crucial
brain regions.
0.01
relative mRNA expression
were no significant differences between different
SNP3- or SNP4-allele carriers for any of the electrophysiological variables (data not shown).
0.008
0.006
0.004
0.002
0
Cx
front.
conv.
Caput Corpus
f.-orb.
Put. Hippo.
Caudate
Figure 3 Expression of the alternative NOS-I exon 1c
(closed bars) and 1f (open bars) in the frontal cortex (Cx
front), the convexity of the frontal cortex (Cx conv), the
fronto-orbital cortex (Cx f.-orb), the caput and the corpus of
the caudate nucleus, the putamen (Put.) and the hippocampus (Hippo.). Expression values are normalized against
GADPH and represent means7s.d. of 2–4 measurements,
performed in duplicate.
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
296
Discussion
Association of NOS1 with SCZ
A large proportion of SCZ association studies were
not replicated in subsequent studies. This may have
been due to a range of problems: ethnic stratification,
broad phenotype definition (thus, we chose to restrict
the SCZ phenotype in our study to severely ill, nonremitting cases) or restriction to one, often nonfunctional SNP. By using five highly polymorphic
STR markers, we undertook basic genomic control to
avoid stratification artefacts, and indeed our sample
proved to be genetically homogenous. One of our
candidate polymorphisms, VNTR1, was included in
the genomic control and found not to differ in its
distribution between patients and controls. This
seems counterintuitive at first sight; however, testing
for genomic stratification uses single alleles, whereas
for association with disease and neuropsychological
as well as psychophysiological data, the 15 VNTR1
alleles were dichotomized, reflecting a presumed
regulatory role of this polymorphism. Thus, functionality rather than allelic frequency likely accounts for
the association of NOS1 VNTR1 with psychological
and physiological parameters. That the VNTR1 has
been predicted to be functional by localization54 and
that the VNTR1-containing region was demonstrated to
influence gene expression64 further supports this view.
Of related interest is the fact that VNTR1 was not
directly linked to disease, yet SNP1 – a promoter
polymorphism with demonstrated functional significance, that is, 30% decrease in NOS1 exon 1c
expression levels55 – was significantly associated
with SCZ, even more so, when the phenotype was
restricted to less heritable disorders with stable
residual states (type B SCZ). As VNTR1 and SNP1
regulate transcription of different alternative exons,65
which have both previously66 and in the present
study been shown to be expressed in the human
brain, and as those polymorphism are in LD, this is
not contradictory but in fact strengthens the notion
that NOS-I plays a role both in brain function and
dysfunction as suggested by neuropsychological and
psychophysiological investigation (see below). Not
surprisingly, synonymous SNPs that were in LD with
VNTR1 and, in the case of SNP3, also with SNP1 were
neither associated with disease nor with dimensional
parameters, thus explaining the contradictory findings from previous studies investigating exclusively a
synonymous exon 29 and non-coding intron 29
SNP.40–43
The 12q24 ‘hot spot’ locus
Consideration of results from pertinent linkage and
association studies leads to the impression that the
12q24 locus is rather broad with no prominent single
linkage peak (Figure 1). This points to the presence of
several risk genes in this region, with relatively
modest influence of individual genes. NOS1 may
belong to this group of genes; DAAO (located also on
12q24), which has been linked to BPD4 as well as
Molecular Psychiatry
SCZ,67,68 could be another. It will be interesting to test
whether these two genes act independently or
whether they are in LD with each other, probably
causing false-positive association findings. Furthermore, there are several other outstanding candidate
genes at the 12q24 locus, in part presently investigated in our laboratory.
Role of NOS-I in SCZ and brain function
NOS-I is involved in several signaling cascades
apparently involved in the pathogenesis of SCZ. First,
it acts as the second messenger of the glutamatergic
NMDA receptor. As hypo-functionality of the glutamate system has consistently been suggested to be
implicated in SCZ, impaired NOS-I function may well
contribute to a dysregulated glutamate system present
in psychoses. This notion fits current conceptual
frameworks on SCZ candidate genes, which all can be
placed more or less convincingly in the glutamate
network.69 Furthermore, as the adaptor protein of
NOS-I to the NMDA receptor CAPON has been shown
to be associated with SCZ in two independent linkage
analyses,44,45 and as there are reports showing
association of NMDA receptor subunits with the
disease, a genetic basis for disturbed glutamate–NO
messaging gains further support. It would be a
worthwhile task to investigate for epistatic interactions, once functional SNPs of other genes of the
glutamatergic pathway are available.
Yet NOS-I is not only a part of the glutamatergic
system, but also influences the serotonergic and
dopaminergic tone in the brain by modulating
monoamine transporter function. Here NO does not
act by its specific receptor protein soluble G-cyclase,
but by direct chemical modification of protein
residues, that is, nitrosylation. By this mechanism,
NO has been shown to inhibit monoamine transporters – that is, serotonin transporter (5HTT), DAT and
NET – resulting in increased synaptic availability of
monoamine neurotransmitters.70 However, there are
conflicting data on direct NO effects on monoamine
transporters: Kilic et al.71 demonstrated that the NO
donor compound SNAP increased 5HTT function and
that a mutation of the transporter, cosegregating in a
large pedigree with broad phenotype serotonin-spectrum disorder,72 results in a constitutively activated
transporter. This indicates that impaired NO functioning might as well cause disturbance of serotonergic signaling. This notion is further supported by the
finding that NOS-I knockout mice feature marked
changes in serotonergic function: 5HT turnover is
impaired, 5HT receptors are desensitized, and 5HTT
expression in the brain stem neurons is decreased.73
Regarding dopaminergic signaling, it has been shown
that NO regulates striatal output by modulating the
firing pattern of striatal neurons.74 Taken together, NO
appears to be a link between glutamatergic transmission on the one hand and monoaminergic system on
the other, thus being centered in key pathways
previously shown to be involved in the pathophysiology of SCZ.
NOS-I and psychotic disorders
A Reif et al
The impact on the genetic disposition for SCZ
conveyed by NOS1 variation does not reflect a major
gene effect. This is, however, not expected for any
common, functional polymorphism but rather for rare
and potentially deleterious mutations. The fact that
we detected a low degree of genetic variation of NOS1
structure highlights the importance of integrity of NO
signaling. Genetic variation of NOS-I functioning
therefore seems to increase the risk to develop
psychosis in a non-specific mode, probably in concert
with other genes and/or environmental factors. The
present finding that the NOS1 VNTR1 polymorphism
is not only associated with psychosis, but also
influences disease severity with regards to several
psychopathological measures – with VNTR1 SS
carriers being more severely affected – supports this
notion.
How might NOS-I contribute to the pathogenesis of
SCZ at a functional level? Clues pertaining to answer
this question might be derived from electrophysiological examinations, as NOS1 polymorphisms
impacted significantly on P300 latency as well as
amplitude. The CPT, applied in the present study, is
regarded as a neuropsychological measure of sustained attention and thought to mirror prefrontal
brain functioning. Especially CPT errors are attributed
to anterior cingular gyrus dysfunctioning.75 Regarding
the NOS1 exon 1c promoter SNP1, the at-risk allele
(84A) interestingly was associated with less omission errors in the CPT, and with reduced P300
latencies in the both the Go and the Nogo condition.
Fewer omission errors in this group of patients
indicate that these subjects were more effectively
focused on the task at hand, whereas the overall
shorter latencies suggest an increased information
processing speed. The A-allele of SNP1 thus impacts
positively on both pace and accuracy of cognitive
processing. SNP1 is preferentially expressed in the
frontal cortex, the putamen and the hippocampus
(Figure 3); presence of the A-allele reduces the
transcriptional efficiency of NOS1 exon 1c by
approximately 30%.55 Thus, less nitrinergic neurotransmission can be assumed in the above brain
regions in carriers of the A-allele. This might be
especially important in (pre-)frontal cortical areas,
where almost no exon 1f expression can be found.
Here, lower NO levels will result in less activation of
neighboring neurons by a ‘NO cloud’,70 thereby
probably improving neuronal signal/noise ratio,
which might provide an explanation for better
attention in A-allele carriers. However, in the hippocampus, where NO functions as the second messenger
of the NMDA receptor, decreased NOS-I expression
might contribute to hypoglutamatergic states found in
schizophrenic disorders and thus further increase
susceptibility towards disease. This discrepancy in
NOS-I functioning might provide a rationale for the
finding that NOS1 exon 1c 84A enhances information processing, yet contributes to the genetic risk of
SCZ. Likewise, an SNP in the COMT gene (Val158),
which has repeatedly been associated with SCZ, has
at least some beneficial effect in that it results in
increased cognitive flexibility.76 The identification of
genes increasing the disposition toward disease, yet
also improving cognitive domains, could aid to
explain why SCZ, being a severe mental disorder,
persists in the population at a global 1% lifetime
prevalence.
With regards to VNTR1, the situation tends to be
more complicated, as this polymorphism affected
P300 amplitude as well as latency, yet neuropsychological function by and large remained unaffected.
Heterozygous subjects had significantly shortened
P300 latencies for conditions involving response
execution (Go), which indicates an increased information processing speed particularly during conditions that demand the execution of a prepared motor
response. At the same time, they showed increased
ERP amplitudes during response inhibition (Nogo)
over central scalp areas. This finding indicates an
enhanced cerebral activation within frontally located
structures that were suggested to be involved in
inhibitory control.77,78 The overall pattern of the
amplitude data (larger P300 amplitudes in Nogo as
compared to Go trials) was also closest to ‘normal’ in
this group of patients, which once again underlines a
positive influence of the heterozygous genotype on
basic mechanisms of response inhibition and cognitive response control. These findings are in line with
the concept of positive ‘molecular heterosis’, that
refers to situations in which subjects heterozygous for
a genetic polymorphism show a stronger effect for a
quantitative (phenotypic) trait than subjects homozygous for either allele (for a review on the subject see
Comings and MacMurray79). Interestingly, the SS
genotype was associated with significantly decreased
P300 Nogo amplitudes (Table 6). This might indicate
that both polymorphisms modulate the recruitment of
neuronal assemblies suppressing already initiated
motor responses. By ineffectively doing so, the atrisk alleles thus might contribute to defective
response control found in schizophrenic disorders.
The differing functional impact of both NOS1 polymorphisms can readily be explained by the fact that
both promoter variants code for distinct alternative
first exons, expressed in different spatial patterns
(Figure 3).
In conclusion, the key findings of the present
study are: (1) a functional SNP in the promoter
region of NOS1 is associated with SCZ, and is
related to worse (pre-)frontal brain functioning, (2) a
presumably functional promoter VNTR of NOS1
results in more severe psychopathology and influences response control, and (3) an NOS1 minihaplotype is associated with SCZ. Collectively,
three separate lines of evidence thus suggest that
NOS1 genotype is associated with SCZ and affects
brain functioning. Further research on the role of
these NOS1 variations in disease and normal brain
functioning are warranted, as NOS-I provides a novel
and innovative target in the treatment of mental
disorder.
297
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
298
Abbreviations
5HTT, serotonin transporter; BPD, bipolar affective
disorder; BPRS, Brief Psychiatric Rating Scale; CPT,
continuous performance test; dHPLC, denaturing
high-performance liquid chromatography; ERP,
event-related potentials; GAF, global assessment of
functioning; GFP, global field power; HDRS, Hamilton
Depression Rating Scale/24 Items; LD, linkage disequilibrium; MD, major depression; NGA, Nogoanteriorization; NMDA, N-methyl-D-aspartate; NOS,
nitric oxide synthase; PANSS, Positive and Negative
Symptoms Scale; SCZ, schizophrenia; SNP, single
nucleotide polymorphism; STR, short tandem repeat;
TMT, trail making test; VFT, verbal fluency test;
VNTR, variable number of tandem repeats.
Acknowledgments
We gratefully acknowledge B Pfuhlmann, S Kamolz, B
Göwein, M Heine and C Leonhard for their kind help
in ascertaining patients and diagnostic assessment, as
well as M Herrmann for most helpful discussions of
the paper. We are indebted to the Austro–German
brain bank, courtesy of Professor P Riederer, for
providing post-mortem tissue. We thank S Schmidt
for excellent assistance in genotyping. This study
was supported by the Deutsche Forschungsgemeinschaft (Grant RE1632/1-1 and 1-3 to AR, KFO
125/1-1 to AR and KPL and SFB581 to KPL),
Bundesministerium für Bildung, Wissenschaft, Forschung und Technologie (IZKF Würzburg, 01KS9603)
and the European Commission (NEWMOOD LSHMCT-2003-503474).
References
1 Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex
trait: evidence from a meta-analysis of twin studies. Arch Gen
Psychiatry 2003; 60: 1187–1192.
2 Harrison PJ, Weinberger DR. Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol
Psychiatry 2005; 10: 420.
3 Berrettini WH. Genetics of psychiatric disease. Annu Rev Med
2000; 51: 465–479.
4 Schumacher J, Jamra RA, Freudenberg J, Becker T, Ohlraun S, Otte
AC et al. Examination of G72 and D-amino-acid oxidase as genetic
risk factors for schizophrenia and bipolar affective disorder. Mol
Psychiatry 2004; 9: 203–207.
5 Ewald H, Degn B, Mors O, Kruse TA. Significant linkage between
bipolar affective disorder and chromosome 12q24. Psychiatr Genet
1998; 8: 131–140.
6 Ewald H, Flint T, Kruse TA, Mors O. A genome-wide scan shows
significant linkage between bipolar disorder and chromosome
12q24.3 and suggestive linkage to chromosomes 1p22–21, 4p16,
6q14–22, 10q26 and 16p13.3. Mol Psychiatry 2002; 7: 734–744.
7 Curtis D, Kalsi G, Brynjolfsson J, McInnis M, O’Neill J, Smyth C et
al. Genome scan of pedigrees multiply affected with bipolar
disorder provides further support for the presence of a susceptibility locus on chromosome 12q23–q24, and suggests the presence
of additional loci on 1p and 1q. Psychiatr Genet 2003; 13: 77–84.
8 Degn B, Lundorf MD, Wang A, Vang M, Mors O, Kruse TA et al.
Further evidence for a bipolar risk gene on chromosome 12q24
suggested by investigation of haplotype sharing and allelic association
in patients from the Faroe Islands. Mol Psychiatry 2001; 6: 450–455.
Molecular Psychiatry
9 Detera-Wadleigh SD. Chromosomes 12 and 16 workshop. Am J
Med Genet 1999; 88: 255–259.
10 Morissette J, Villeneuve A, Bordeleau L, Rochette D, Laberge C,
Gagne B et al. Genome-wide search for linkage of bipolar
affective disorders in a very large pedigree derived from a
homogeneous population in quebec points to a locus of major
effect on chromosome 12q23–q24. Am J Med Genet 1999; 88:
567–587.
11 Shink E, Morissette J, Sherrington R, Barden N. A genome-wide
scan points to a susceptibility locus for bipolar disorder on
chromosome 12. Mol Psychiatry 2005; 10: 545–552.
12 Maziade M, Roy MA, Chagnon YC, Cliche D, Fournier JP,
Montgrain N et al. Shared and specific susceptibility loci for
schizophrenia and bipolar disorder: a dense genome scan in
Eastern Quebec families. Mol Psychiatry 2005; 10: 486–499.
13 Abkevich V, Camp NJ, Hensel CH, Neff CD, Russell DL, Hughes DC
et al. Predisposition locus for major depression at chromosome
12q22–12q23.2. Am J Hum Genet 2003; 73: 1271–1281.
14 Bailer U, Leisch F, Meszaros K, Lenzinger E, Willinger U, Strobl R
et al. Genome scan for susceptibility loci for schizophrenia and
bipolar disorder. Biol Psychiatry 2002; 52: 40–52.
15 Bailer U, Leisch F, Meszaros K, Lenzinger E, Willinger U, Strobl R
et al. Genome scan for susceptibility loci for schizophrenia.
Neuropsychobiology 2000; 42: 175–182.
16 DeLisi LE, Shaw SH, Crow TJ, Shields G, Smith AB, Larach VW et
al. A genome-wide scan for linkage to chromosomal regions in 382
sibling pairs with schizophrenia or schizoaffective disorder. Am J
Psychiatry 2002; 159: 803–812.
17 Brzustowicz LM, Hodgkinson KA, Chow EW, Honer WG, Bassett
AS. Location of a major susceptibility locus for familial schizophrenia on chromosome 1q21–q22. Science 2000; 288: 678–682.
18 Wilcox MA, Faraone SV, Su J, Van Eerdewegh P, Tsuang MT.
Genome scan of three quantitative traits in schizophrenia
pedigrees. Biol Psychiatry 2002; 52: 847–854.
19 Craddock N, Owen M, Burge S, Kurian B, Thomas P, McGuffin P.
Familial cosegregation of major affective disorder and Darier’s
disease (keratosis follicularis). Br J Psychiatry 1994; 164: 355–358.
20 Dawson E, Parfitt E, Roberts Q, Daniels J, Lim L, Sham P et al.
Linkage studies of bipolar disorder in the region of the Darier’s
disease gene on chromosome 12q23–24.1. Am J Med Genet 1995;
60: 94–102.
21 Jacobsen NJ, Franks EK, Elvidge G, Jones I, McCandless F,
O’Donovan MC et al. Exclusion of the Darier’s disease gene,
ATP2A2, as a common susceptibility gene for bipolar disorder.
Mol Psychiatry 2001; 6: 92–97.
22 Jones I, Jacobsen N, Green EK, Elvidge GP, Owen MJ, Craddock N.
Evidence for familial cosegregation of major affective disorder and
genetic markers flanking the gene for Darier’s disease. Mol
Psychiatry 2002; 7: 424–427.
23 Chagnon YC, Merette C, Bouchard RH, Emond C, Roy MA,
Maziade M. A genome wide linkage study of obesity as secondary
effect of antipsychotics in multigenerational families of
eastern Quebec affected by psychoses. Mol Psychiatry 2004; 9:
1067–1074.
24 Snyder SH, Ferris CD. Novel neurotransmitters and their neuropsychiatric relevance. Am J Psychiatry 2000; 157: 1738–1751.
25 Garthwaite J, Garthwaite G, Palmer RM, Moncada S. NMDA
receptor activation induces nitric oxide synthesis from arginine in
rat brain slices. Eur J Pharmacol 1989; 172: 413–416.
26 Bird DC, Bujas-Bobanovic M, Robertson HA, Dursun SM.
Lack of phencyclidine-induced effects in mice with reduced
neuronal nitric oxide synthase. Psychopharmacology 2001; 155:
299–309.
27 Bujas-Bobanovic M, Bird DC, Robertson HA, Dursun SM. Blockade
of phencyclidine-induced effects by a nitric oxide donor. Br J
Pharmacol 2000; 130: 1005–1012.
28 Bujas-Bobanovic M, Robertson HA, Dursun SM. Effects of nitric
oxide synthase inhibitor N(G)-nitro-L-arginine methyl ester on
phencyclidine-induced effects in rats. Eur J Pharmacol 2000; 409:
57–65.
29 Black MD, Selk DE, Hitchcock JM, Wettstein JG, Sorensen SM. On
the effect of neonatal nitric oxide synthase inhibition in rats: a
potential neurodevelopmental model of schizophrenia. Neuropharmacology 1999; 38: 1299–1306.
NOS-I and psychotic disorders
A Reif et al
30 da Silva GD, Matteussi AS, dos Santos AR, Calixto JB, Rodrigues
AL. Evidence for dual effects of nitric oxide in the forced
swimming test and in the tail suspension test in mice. Neuroreport
2000; 11: 3699–3702.
31 Yildiz F, Erden BF, Ulak G, Utkan T, Gacar N. Antidepressant-like
effect of 7-nitroindazole in the forced swimming test in rats.
Psychopharmacology (Berlin) 2000; 149: 41–44.
32 Harkin AJ, Bruce KH, Craft B, Paul IA. Nitric oxide synthase
inhibitors have antidepressant-like properties in mice. 1. Acute
treatments are active in the forced swim test. Eur J Pharmacol
1999; 372: 207–213.
33 Karolewicz B, Bruce KH, Lee B, Paul IA. Nitric oxide synthase
inhibitors have antidepressant-like properties in mice. 2. Chronic
treatment results in downregulation of cortical beta-adrenoceptors. Eur J Pharmacol 1999; 372: 215–220.
34 Klamer D, Engel JA, Svensson L. The nitric oxide synthase
inhibitor, L-NAME, block phencyclidine-induced disruption of
prepulse inhibition in mice. Psychopharmacology (Berlin) 2001;
156: 182–186.
35 Klamer D, Engel JA, Svensson L. The neuronal selective nitric
oxide synthase inhibitor, Nomega-propyl-L-arginine, blocks the
effects of phencyclidine on prepulse inhibition and locomotor
activity in mice. Eur J Pharmacol 2004; 503: 103–107.
36 Akbarian S, Bunney Jr WE, Potkin SG, Wigal SB, Hagman JO,
Sandman CA et al. Altered distribution of nicotinamide-adenine
dinucleotide phosphate-diaphorase cells in frontal lobe of schizophrenics implies disturbances of cortical development. Arch Gen
Psychiatry 1993; 50: 169–177.
37 Akbarian S, Vinuela A, Kim JJ, Potkin SG, Bunney Jr WE, Jones EG.
Distorted distribution of nicotinamide-adenine dinucleotide phosphate-diaphorase neurons in temporal lobe of schizophrenics
implies anomalous cortical development. Arch Gen Psychiatry
1993; 50: 178–187.
38 Lauer M, Johannes S, Fritzen S, Senitz D, Riederer P, Reif A.
Morphological abnormalities in NO synthase positive striatal
interneurons of schizophrenic patients. Neuropsychobiology
2005; 52: 111–117.
39 Detera-Wadleigh SD, Badner JA, Berrettini WH, Yoshikawa T,
Goldin LR, Turner G et al. A high-density genome scan detects
evidence for a bipolar-disorder susceptibility locus on 13q32 and
other potential loci on 1q32 and 18p11.2. Proc Natl Acad Sci USA
1999; 96: 5604–5609.
40 Shinkai T, Ohmori O, Hori H, Nakamura J. Allelic association of
the neuronal nitric oxide synthase (NOS1) gene with schizophrenia. Mol Psychiatry 2002; 7: 560–563.
41 Liou YJ, Tsai SJ, Hong CJ, Liao DL. Association analysis for
the CA repeat polymorphism of the neuronal nitric oxide
synthase (NOS1) gene and schizophrenia. Schizophr Res 2003;
65: 57–59.
42 Buttenschon HN, Mors O, Ewald H, McQuillin A, Kalsi G,
Lawrence J et al. No association between a neuronal nitric oxide
synthase (NOS1) gene polymorphism on chromosome 12q24 and
bipolar disorder. Am J Med Genet 2004; 124B: 73–75.
43 Yu YW, Chen TJ, Wang YC, Liou YJ, Hong CJ, Tsai SJ. Association
analysis for neuronal nitric oxide synthase gene polymorphism
with major depression and fluoxetine response. Neuropsychobiology 2003; 47: 137–140.
44 Brzustowicz LM, Simone J, Mohseni P, Hayter JE, Hodgkinson KA,
Chow EW et al. Linkage disequilibrium mapping of schizophrenia
susceptibility to the CAPON region of chromosome 1q22. Am J
Hum Genet 2004; 74: 1057–1063.
45 Zheng Y, Li H, Qin W, Chen W, Duan Y, Xiao Y et al. Association of
the carboxyl-terminal PDZ ligand of neuronal nitric oxide
synthase gene with schizophrenia in the Chinese Han population.
Biochem Biophys Res Commun 2005; 328: 809–815.
46 Clinton SM, Meador-Woodruff JH. Abnormalities of the NMDA
receptor and associated intracellular molecules in the thalamus in
schizophrenia and bipolar disorder. Neuropsychopharmacology
2004; 29: 1353–1362.
47 Leonhard K. Classification of Endogenous Psychoses and Their
Differentiated Etiology, 2 edn. Springer: Wien, 1999.
48 Arbeitsgemeinschaft für Methodik und Dokumentation in der
Psychiatrie. Das AMDP-System. Manual zur Dokumentation
psychiatrischer Befunde. Hogrefe: Göttingen, Germany, 2000.
49 Sham PC, Curtis D. Monte Carlo tests for associations between
disease and alleles at highly polymorphic loci. Ann Hum Genet
1995; 59(Part 1): 97–105.
50 Curtis D, North BV, Gurling HM, Blaveri E, Sham PC. A quick and
simple method for detecting subjects with abnormal genetic
background in case-control samples. Ann Hum Genet 2002; 66:
235–244.
51 Bentounsi B, Cabaret J. Analysis of helminth genetic data:
comparative examples with Haemonchus contortus isozymes
using exact tests or resampling procedures. Parasitol Res 1999;
85: 855–857.
52 Liu K, Muse SV. PowerMarker: an integrated analysis environment
for genetic marker analysis. Bioinformatics 2005; 21: 2128–2129.
53 Pritchard JK, Stephens M, Donnelly P. Inference of population
structure using multilocus genotype data. Genetics 2000; 155:
945–959.
54 Hall AV, Antoniou H, Wang Y, Cheung AH, Arbus AM,
Olson SL et al. Structural organization of the human neuronal
nitric oxide synthase gene (NOS1). J Biol Chem 1994; 269:
33082–33090.
55 Saur D, Vanderwinden JM, Seidler B, Schmid RM, De Laet MH,
Allescher HD. Single-nucleotide promoter polymorphism alters
transcription of neuronal nitric oxide synthase exon 1c in infantile
hypertrophic pyloric stenosis. Proc Natl Acad Sci USA 2004; 101:
1662–1667.
56 Zhao JH. 2LD, GENECOUNTING and HAP: computer programs
for linkage disequilibrium analysis. Bioinformatics 2004; 20:
1325–1326.
57 Gsell W, Lange KW, Pfeuffer R, Heckers S, Heinsen H, Senitz D et
al. How to run a brain bank. A report from the Austro-German
brain bank. J Neural Transm (Suppl) 1993; 39: 31–70.
58 Saur D, Seidler B, Paehge H, Schusdziarra V, Allescher HD.
Complex regulation of human neuronal nitric-oxide synthase
exon 1c gene transcription. Essential role of Sp and ZNF
family members of transcription factors. J Biol Chem 2002; 277:
25798–25814.
59 Reif A, Fallgatter AJ, Ehlis AC, Lesch KP. Altered functioning of
the cingulate gyrus in two cases of chromosome 22q11 deletion
syndrome. Psychiatry Res 2004; 132: 273–278.
60 Lehmann D, Skrandies W. Reference-free identification of components of checkerboard-evoked multichannel potential fields.
Electroencephalogr Clin Neurophysiol 1980; 48: 609–621.
61 Fallgatter AJ, Brandeis D, Strik WK. A robust assessment of the
NoGo-anteriorisation of P300 microstates in a cued Continuous
Performance Test. Brain Topogr 1997; 9: 295–302.
62 Fallgatter AJ, Strik WK. The NoGo-anteriorization as a neurophysiological standard-index for cognitive response control. Int J
Psychophysiol 1999; 32: 233–238.
63 Fallgatter AJ, Esienack SS, Neuhauser B, Aranda D, Scheuerpflug
P, Herrmann MJ. Stability of late event-related potentials:
topographical descriptors of motor control compared with the
P300 amplitude. Brain Topogr 2000; 12: 255–261.
64 Rife TK, Xie J, Redman C, Young AP. The 50 2 promoter of the
neuronal nitric oxide synthase dual promoter complex mediates
inducibility by nerve growth factor. Brain Res Mol Brain Res 2000;
75: 225–236.
65 Zhang T, Haws P, Wu Q. Multiple variable first exons: a
mechanism for cell-and tissue-specific gene regulation. Genome
Res 2004; 14: 79–89.
66 Wang Y, Newton DC, Robb GB, Kau CL, Miller TL, Cheung AH et
al. RNA diversity has profound effects on the translation of
neuronal nitric oxide synthase. Proc Natl Acad Sci USA 1999; 96:
12150–12155.
67 Liu X, He G, Wang X, Chen Q, Qian X, Lin W et al. Association of
DAAO with schizophrenia in the Chinese population. Neurosci
Lett 2004; 369: 228–233.
68 Chumakov I, Blumenfeld M, Guerassimenko O, Cavarec L,
Palicio M, Abderrahim H et al. Genetic and physiological data
implicating the new human gene G72 and the gene for D-amino
acid oxidase in schizophrenia. Proc Natl Acad Sci USA 2002; 99:
13675–13680.
69 Harrison PJ, Owen MJ. Genes for schizophrenia? Recent findings
and their pathophysiological implications. Lancet 2003; 361:
417–419.
299
Molecular Psychiatry
NOS-I and psychotic disorders
A Reif et al
300
70 Kiss JP, Vizi ES. Nitric oxide: a novel link between synaptic
and nonsynaptic transmission. Trends Neurosci 2001; 24:
211–215.
71 Kilic F, Murphy DL, Rudnick G. A human serotonin transporter
mutation causes constitutive activation of transport activity. Mol
Pharmacol 2003; 64: 440–446.
72 Ozaki N, Goldman D, Kaye WH, Plotnicov K, Greenberg BD,
Lappalainen J et al. Serotonin transporter missense mutation
associated with a complex neuropsychiatric phenotype. Mol
Psychiatry 2003; 8: 895, 933–936.
73 Chiavegatto S, Dawson VL, Mamounas LA, Koliatsos VE, Dawson
TM, Nelson RJ. Brain serotonin dysfunction accounts for aggression in male mice lacking neuronal nitric oxide synthase. Proc
Natl Acad Sci USA 2001; 98: 1277–1281.
74 West AR, Galloway MP, Grace AA. Regulation of striatal dopamine
neurotransmission by nitric oxide: effector pathways and signaling mechanisms. Synapse 2002; 44: 227–245.
Molecular Psychiatry
75 Carter CS, Braver TS, Barch DM, Botvinick MM, Noll D, Cohen JD.
Anterior cingulate cortex, error detection, and the online monitoring of performance. Science 1998; 280: 747–749.
76 Nolan KA, Bilder RM, Lachman HM, Volavka J. Catechol
O-methyltransferase Val158Met polymorphism in schizophrenia:
differential effects of Val and Met alleles on cognitive stability and
flexibility. Am J Psychiatry 2004; 161: 359–361.
77 Fallgatter AJ, Bartsch AJ, Herrmann MJ. Electrophysiological
measurements of anterior cingulate function. J Neural Transm
2002; 109: 977–988.
78 Bokura H, Yamaguchi S, Kobayashi S. Electrophysiological
correlates for response inhibition in a Go/NoGo task. Clin
Neurophysiol 2001; 112: 2224–2232.
79 Comings DE, MacMurray JP. Molecular heterosis: a review. Mol
Genet Metab 2000; 71: 19–31.
80 Jasper H. Report of committee on methods of clinical exam in EEG.
Electroencephalogr Clin Neurophysiol 1958; 10: 370–375.