609
Pleural Effusion as a Cause of Right Ventricular
Diastolic Collapse
Kevin Vaska, MD; L. Samuel Wann, MD; Kiran Sagar, MD; and H. Sidney Klopfenstein, MD, PhD
Background. We hypothesized, after seeing several suggestive clinical examples, that a
process
leading
to a large bilateral pleural effusion in the presence of an otherwise insignificant pericardial effusion could
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
result in right ventricular diastolic collapse (RVDC) as seen by two-dimensional echocardiography. This
noninvasive marker for hemodynamically significant cardiac tamponade occurs when pericardial fluid is
under pressure. Therefore, RVDC resulting from a large pleural effusion would represent a false-positive
indication of cardiac tamponade caused by excessive pericardial fluid.
Methods and Results. Seven spontaneously breathing dogs were chronically instrumented to measure
ascending aortic, right atrial, intrapericardial, intrapleural, left atrial, and pulmonary artery pressures
and cardiac output. Intravascular volume was adjusted before each experiment to the euvolemic range
with saline solution. The onset of RVDC was observed in each animal by two-dimensional echocardiography during seven paired episodes of tamponade induced by infusions of warm saline into the pericardial
space alone and, after drainage of the pericardial fluid and complete recovery, into the pleural space in
the presence of a small pericardial effusion. The onset of RVDC occurred at the same intrapericardial
(8.17 versus 9.47 mm Hg) and right atrial (7.41 versus 7.46 mm Hg) blood pressures regardless of whether
it was produced by an intrapericardial or an intrapleural effusion but began in expiration during the
former and in inspiration during the latter. Intrapericardial pressure increased in the same manner as
intrapleural pressure during intrapleural saline infusion. Nevertheless, cardiac output and aortic blood
pressure were better preserved, and at the onset of RVDC, the pulmonary artery systolic blood pressure
was higher (p<0.0001) and the degree of pulsus paradoxus lower (p<0.01) with intrapleural infusion.
Conclusions. These results indicate that a large bilateral pleural effusion can elevate intrapericardial
pressure sufficiently to cause RVDC and, perhaps, lead to misdirected therapy of an otherwise
insignificant pericardial effusion. (Circulation 1992;86:609-617)
KEY WoRDs * transmural pressure * pulsus paradoxus * intrathoracic pressure * pericardial
constraint * cardiac tamponade * pleural effusion * right ventricular collapse
C ardiac tamponade is a life-threatening hemodynamic abnormality caused by the accumulation of pericardial fluid under pressure. It is
not a discrete event, but encompasses a spectrum
ranging from pericardial effusions that produce trivial
hemodynamic abnormalities to those that result in
hemodynamic decompensation.1-3 At any point along
this progression, the severity of the hemodynamic
abnormality is believed to depend on the intrapericardial pressure, intracavitary filling pressures, and chamber compliances.4-7 It has been helpful to have twodimensional echocardiographic landmarks along this
progression to clinically assess the severity of the
compromised cardiac function and to aid in planning
therapeutic interventions before decompensation occurs. This is especially important because the treatFrom the Cardiology Section of the Department of Medicine,
The Bowman Gray School of Medicine, Winston-Salem, N.C., and
the Medical College of Wisconsin, Milwaukee, Wis.
Supported in part by National Institutes of Health grants R01
H13228, HL-40511, HL-42254, and T32 H107546 from the National Heart, Lung, and Blood Institute, Bethesda, Md. and by a
grant-in-aid from the American Heart Association (H.S.K.).
Address for correspondence: H. Sidney Klopfenstein, MD,
PhD, Cardiology Division, The Bowman-Gray School of Medicine,
Medical Center Boulevard, Winston-Salem, NC 27157-1045.
Received January 2, 1991; revision accepted April 21, 1992.
ment of hemodynamically significant cardiac tamponade (pericardiocentesis or surgery) is invasive and
associated with some risk.
Right atrial and right ventricular (RV) diastolic collapse (RVDC) have been shown to be sensitive and
specific markers for cardiac tamponade both in conscious
animals8-10 and in human studies.11,12 In euvolemic, nonconvalescent, conscious animals and humans without RV
hypertrophy or elevated RV diastolic pressures, the onset
of RVDC has been shown to be associated with a 15-20%
decline in cardiac output from baseline levels and a
preserved systemic blood pressure.
The echocardiographic observation of RVDC in several patients who had large pleural effusions and small
pericardial effusions led us to test the hypothesis that a
large bilateral pleural effusion may result in RVDC in
the presence of an otherwise insignificant pericardial
effusion. In such a situation, removal of the pleural
effusion and treatment of the process causing it, instead
of a pericardial drainage procedure, would seem to be
the appropriate course.
Methods
Seven healthy and acclimated adult mongrel dogs of
either sex (weight, 26-30 kg) were anesthetized with
thiamylal sodium (20 mg/kg i.v.), intubated, and venti-
610
Circulation Vol 86, No 2 August 1992
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
TABLE 1. Hemodynamic Data During Pericardial Effusion and Pleural Effusion
Pericardial effusion
End point (DCT)
Onset of RVDC
End
End
End
End
Mean
Mean
Baseline
inspiration
expiration
expiration
inspiration
17.39±0.25
8.88±0.24
17.00±0.37*
16.12±0.36
8.17±0.20*
6.91±0.17
0.45±0.09
IPP (mm HG)
-0.10±0.32
-0.57±0.13
-7.22±0.29
-7.86±0.37
-0.04±0.11
-0.96±0.29
IPIP (mm Hg)
-3.45±0.31
23.34±0.40
17.57±0.33
17.43±0.27
9.13±0.30
14.77±0.41
3.9±0.22
8.98+0.33
TMPIpp (mm Hg)
7.73±0.15
15.13±0.39*
15.01±0.30
15.37±0.21
7.06±0.19
7.41±0.1O
1.58±0.08
RABP (mm Hg)
-1.11±0.14
-2.02±0.19
0.15±0.11
-1.15±0.17
1.13±0.11
-1.88±0.06*
-0.76±0.13*
TMPRA (mm Hg)
3.6±0.3
1.2±0.1*
0.4±0.2
2.4±0.6
2.5±0.3
3.0±0.1§
3.5±0.2
CO (1/min)
79.2±1.3
88.7±1.5
69.5±0.4*
62.8±1.5
76.7±2.1
84.7±1.1§
102.9±1.1
AoBP (mm Hg)
126±7
135±6
128±5
170±5
104±4
131±51
HR (bpm)
159±40
9.58±0.24
14.07±0.27
14.73±0.41*
11.53±0.32
17.65±0.44
11.80±0.48*
6.72±0.25
LABP (mm Hg)
5.19±0.22
-2.27+0.35*
-4.59±0.41
0.26±0.39
2.67±0.20
3.63±0.24*
6.27±0.28
TMPLA (mm Hg)
14.07±0.56
21.84±0.69
25.11±0.77
13.45 ±0.80
12.02±0.44
23.29±0.94t
22.09±0.98
PASP (mm Hg)
14.02±0.77*
19.24±0.39
14.11±0.37
25.21±0.49
24.25 ±0.72t
29.70±0.55
25.54+0.72
TMPPASP (mm Hg)
...
12.1±0.2*
...
...
8.0±0.2*
4.0±0.1
PP (mm Hg)
..
...
...
29.0±1.4
25.9±1.2'
47.4±4.0k
SVR (Woods)
4±1
13±2
8±1*
27±2
34±2
23±1*
20±2
SV (ml)
RVDC, right ventricular diastolic collapse; DCT, decompensated cardiac tamponade; IPP, change in intrapericardial pressure from
baseline; IPIP, change in intrapleural pressure from baseline; TMPIpp, calculated transmural pressure, change in intrapericardial pressure
from baseline; RABP, right atrial blood pressure; TMPRA, calculated transmural pressure, right atrial; CO, cardiac output; AoBP, aortic
blood pressure; HR, heart rate; bpm, beats per minute; LABP, left atrial blood pressure; TMPLA, calculated transmural pressure, left atrial;
PASP, pulmonary artery systolic blood pressure; TMPPASP, calculated transmural pressure, pulmonary artery systolic blood pressure; PP,
pulsus paradoxus; SVR, systemic vascular resistance; SV, stroke volume.
Data are mean±SEM.
*p<O.001 compared with baseline values.
tNot significant.
tp<O.O1 compared with baseline values
§p<0.05 compared with baseline values.
lated with a volume-cycled respirator (LKB Medical
AB, Engstrom 311). Anesthesia was maintained with an
in-line halothane vaporizer (1-1.5% by volume in oxygen). Arterial blood gases were monitored hourly, and
adequate oxygenation and acid-base status were maintained. A left thoracotomy was performed in the fifth
intercostal space using aseptic technique, and Tygon
fluid-filled catheters (Tygon microbore tubing, 0.05-in.
i.d. xO.09-in. o.d., Norton Plastics) were placed into the
ascending aorta (via the left internal mammary artery),
right atrium (via the right internal mammary vein),
main pulmonary artery (retrograde through an extrapericardial branch), and left atrium (retrograde through
an extrapericardial pulmonary vein).
The pericardial sac was entered through a 4-5 -cm
longitudinal incision beginning near the base of the
heart, and an electromagnetic flowprobe was placed
around the aortic root (Howell Instruments; used with a
Narcomatic flowmeter, Model RT 500, Healthdyne Cardiovascular, Inc.). Two fenestrated Tygon fluid-filled
catheters were positioned in the pericardial space over
the posterior and diaphragmatic surfaces of the left
ventricle (avoiding the RV free wall) and were secured
with purse-string sutures. The pericardium was closed
with a continuous locking suture, and a watertight seal
was verified by infusion of warm saline solution sufficient to cause a 30% reduction in mean aortic blood
pressure. The intrapericardial fluid was removed, and
20-25 ml of sterile saline was returned to the pericardial space. All catheters were passed individually
through the chest wall and exteriorized near the scapulae. The anterior mediastinum was opened wide to
allow communication of right and left pleural cavities. A
separate Tygon fluid-filled catheter was positioned in
the anterior thorax, and a 14F sump tube (Argyle,
Sherwood Medical Co.) was passed through the seventh
intercostal space and its tip positioned in the anterior
left pleural space. After brief hyperexpansion of the
lungs, the ribs were approximated with umbilical tape,
and the wound was closed in layers to provide an
airtight seal. All pleural fluid and air were evacuated,
and all intravascular catheters were aspirated, filled
with a heparin solution, and sealed.
The animal was extubated after spontaneous respirations and reflexes had returned and allowed to
recover overnight in an incubator with controlled
temperature and supplemental oxygen (5 1/min). Xylazine (1-2 mg/kg i.m. every 8 hours) was administered as needed for analgesia, and intramuscular
injections of penicillin and streptomycin were given
prophylactically. The pericardial space was irrigated
with saline after surgery and daily thereafter for 2 or
3 days; integrity of the space was confirmed by recovery of all irrigating fluid.
On day 2 or 3 after surgery, before thoracic adhesions
had formed between the parietal pericardium and visceral pleura, the conscious animal was returned to the
laboratory and allowed to stand comfortably in a sling.
The fluid-filled catheters were attached directly to pressure transducers (Deseret Medical, Inc.) with the zero-
Vaska et al Pleural Effusion
611
TABLE 1. Continued.
Pleural effusion
Baseline
1.73+0.14
-3.33±0.26
Mean
9.47+0.20*
4.69±0.16*
5.06±0.23
4.78±0.16*
7.46±0.11*
-2.01±0.57*
3.3±0.1t
109.0±2.0t
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
1.69±0.08
-0.04±0.18
3.6±0.1
105.1±1.7
123±2
6.82±0.28
5.09±0.16
21.31±0.90
19.58±0.86
4.1±0.1
29.2±1.2
29±1
141±4§
11.73±0.46*
2.26±0.29*
38.74±1.25*
34.05±0.64*
5.5±0.2t
31.0± 1.0t
23±1t
Onset of RVDC
End
inspiration
4.81+0.29
-0.37±0.19
5.18+0.32
0.95±0.33
-3.86±0
3.0±0.2
107.5±2.1
137±5
7.69±0.37
2.88±0.43
37.49±1.07
37.86±0.95
...
...
22±2
End
expiration
14.35+0.31
9.93±0.27
4.42±0.35
14.73±0.22
0.38±0.23
3.6±0.1
112.7±1.8
144±3
16.09±0.44
1.74±0.33
40.26±1.17
30.33±1.01
...
...
25±1
pressure reference point adjusted to be one third of the
vertical distance between the sternum and spine. Respirations were measured with a Whitney gauge placed
around the thorax.
During each infusion, pressures in the right and left
atria, aorta, pulmonary artery, pericardial space, and
pleural space as well as cardiac output, heart rate, and
respirations were continuously recorded on an FM tape
recorder (A.R. Vetter Co.) and an eight-channel stripchart recorder (Gould series 2800). A maximum of one
pericardial infusion and one pleural infusion were performed in a single day, with sufficient time allowed for
recovery between runs. No animal underwent more
than two sets of infusion runs. Necropsy and in vitro
electromagnetic flowprobe calibration were performed
on all animals as previously described.13
Short-axis two-dimensional echocardiograms were
obtained with a hand-held transducer in the right
fourth or fifth intercostal space and an Irex HSP-1
phased-array ultrasonoscope (Johnson and Johnson)
and were recorded on videotape with a Sony Betamax
videocassette recorder (Sony Corp.). The echocardiograms were reviewed by two independent observers,
and RVDC was considered present if there was an
inward motion of the RV outflow tract or free wall
endocardial surface in diastole that varied with the
respiratory cycle. The reversal of curvature of the RV
wall always began after the mitral valve opened (as
judged in the left atrial pressure tracing) and was
sustained for at least 40% of the diastolic interval. It
has been shown in clinical studies that right and left
atrial collapse occur very early in the progression of
cardiac tamponade and are present before RV collapse. Unfortunately, we were not able to reliably
obtain a true apical four-chamber view of the heart in
this conscious canine model; therefore, we were unable to investigate these very early signs of increased
intrapericardial pressure.
The pericardial and pleural spaces were drained, and
30 ml of saline was instilled into the pericardial space so
Mean
18.88±0.50*
14.25±0.50*
4.63+0.61t
15.78±0.30*
-3.10±0.22*
2.9±0.1§
105.5±1.8t
168±3*
16.09±0.52*
-2.79+0.46*
53.52±2.61*
39.27±1.02*
8.1±0.1*
31.7±1.4t
17±1§
End point
End
inspiration
15.99±0.49
11.17±0.68
4.82+0.55
11.97±0.46
-4.02±0.31
2.4±0.2
101.2±2.3
160±4
15.78±0.42
-0.21 ±0.28
51.30±2.15
40.13±1.13
End
expiration
23.63 ±0.46
19.14±0.57
4.49±0.51
23.75±0.41
0.12+0.27
3.6±0.2
108.9±2.5
172±2
20.37+0.35
-3.26±0.31
55.35±1.92
36.21±1.78
...
...
15±2
21±2
that open-ended catheters would provide a valid measure of intrapericardial pressure.14 Mean right atrial
blood pressure was adjusted to between 1 and 2 mm Hg
by intravenous infusion of normal saline, and baseline
data were collected when a hemodynamic steady state
had been achieved. Warmed normal saline solution was
then continuously infused into the pericardial space at a
rate of 10 ml/min with a Masterflex infusion pump (Cole
Parmer Instrument Co.). The infusion continued until
the time of hemodynamic decompensation, which is
defined as a 30% decline in mean aortic blood pressure
from baseline levels. The pericardial fluid was immediately removed, and the mean right atrial blood pressure
was measured to ensure that intravascular volume had
remained stable. The volume infused and the pressures
present at the onset of RVDC and hemodynamic decompensation were noted.
The dog was allowed to recover for 1 hour. Absence
of fluid in the pleural space was confirmed, and a
volume of saline equal to 50% of the volume that
resulted in the onset of RVDC in the preceding pericardial infusion run was instilled into the pericardial
space. Therefore, each dog's individual physiology, size,
and pericardial compliance were able to influence the
specific volume of fluid chosen. The actual mean volume
of fluid instilled into the pericardium, 63+3 ml, resulted
in only a slightly elevated intrapericardial fluid pressure
(1.73+0.04 mm Hg). This method caused an equivalent
small, hemodynamically unimportant pericardial effusion in all dogs and allowed us to monitor the pericardial pressure with open catheters. Steady-state data
again were collected as the baseline for a pleural
effusion run. The pleural effusion was produced by
rapid manual instillation of 1.5 1 of warm saline into the
pleural space, which was followed by a continuous
intrapleural infusion at a rate of 50 ml/min with the
Masterflex infusion pump. Data were continuously recorded as before, and the intrapleural infusion was
stopped when the increase in intrapericardial pressure
equaled that present at the time of hemodynamic
Circulation Vol 86, No 2 August 1992
612
201
50
45
.3
15.
2 40
I
E
', 35
2
U
U
10
30
J
a)
L
U)5
(L)
D 25
0
SS i) ~~~~~~~~~~~~~~~0
11,1---
>20
a.
(D
]p~~~~~~~~~I
ro
-Y 15
L
4J
U) 10
(L)
-5,
a-
5
O
-100
2
0
A
a
6
4
10
12
14
16
18
20
Intrapericardial Pressure (mm Hg)
D
* X*
X X
0
2
6
4
B
10
12
14
ia
1B
20
1B
20
18
20
Intrapericardial Pressure (mm Hg)
70
=cl 60
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
E
50
a) 40
M
~~~~~.--1,"',
30
L
L 20
E
rt
D 10
0-
-1'
4
B
a
6
10
12
14
15
20
1B
Intrapericardial Pressure (mm Hg)
*
*
0
2
0
2
E
4
6
a
10
12
14
i6
Intrapericardial Pressure (mm Hg)
130
.a 120
10
L-100
0 100
to
01
80
-4
4
70
60 1*
0
C
,
2
4
6
0
1
8
10
12
14
16
18
20
F
2
4
6
a
o0
12
14
16
Intrapericardial Pressure (mm Hg)
Intrapericardial Pressure (mm Hg)
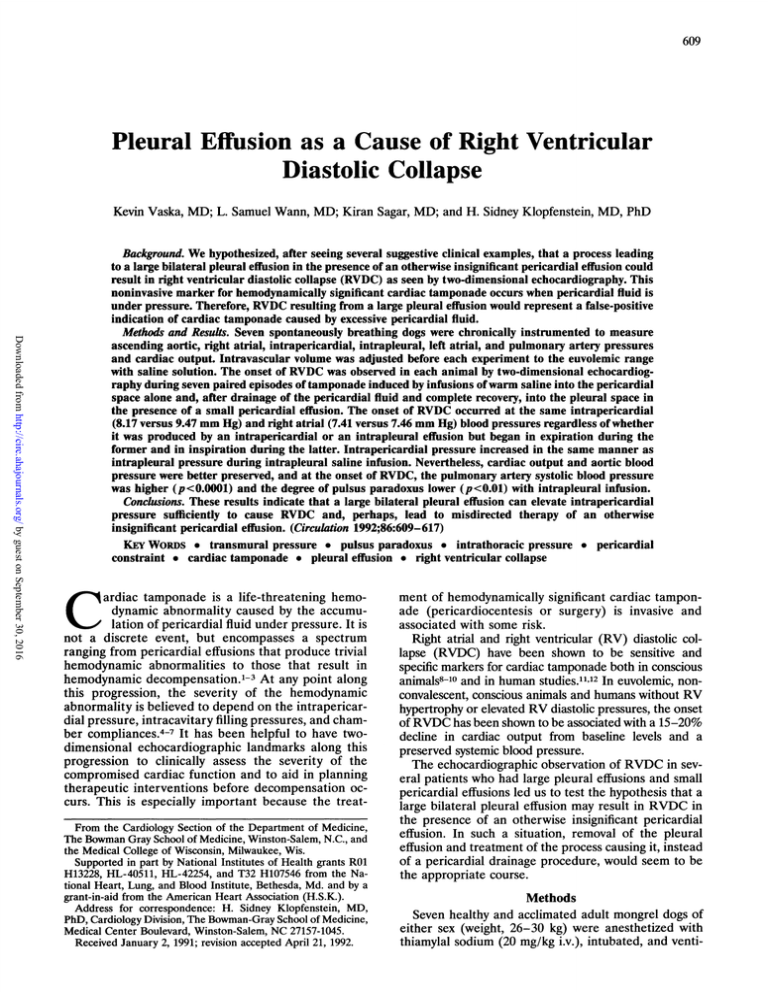
FIGURE 1. Graphs showing relations between mean intrapericardial pressure and hemodynamic indexes during intrapleural infusion
(dashed lines) and during intrapericardial infusion (solid lines). Panel A: The curves are significantly different from each other
(p<O.OOJ), but the point of onset (circle) of right ventricular diastolic collapse (RVDC) is the same. Panel B: The curves dffer
significantly from each other (p<O.OJ), but the cardiac output at the onset of RVDC (circle) during each infusion is the same. Panel
C: The curves are different from each other (p<O.OOl), and the aortic blood pressure is preserved during intrapleural infusion
(p<O.OOOJ). Panel D: The curves differ significantly from each other (p<O.Ol), but the stroke volume at the onset of RVDC (circle)
during each infusion is the same. Panel E: The curves are differentfrom each other (p<O.OO1), and the pulmonary artery systolc blood
pressure at the onset of RVDC (circle) is higher during intrapleural infusion (p<0.0001). Panel F: The curves differ significantly from
each other (p<O.Ol), and pulsus paradoxus at the onset of RVDC (circle) is greater during intrapericardisl infusion (p<O.Ol).
decompensation during the preceding pericardial infusion run. The pleural fluid was removed immediately,
and the mean right atrial blood pressure was checked to
stable intravascular volume. Arterial blood gas
samples were measured at baseline and at the completion of each type of infusion.
ensure a
Vaska et al Pleural Effusion
613
20
'PIP
0
20
IPP
'.AANVVW.1AMI
N.rM.4
0
20
~~~~~g~~~~~~~~~A~~~~~~~~~rAw~~~~~~~~~~~~
RABP
0
.
*.*.
*.
***.**.
*.
.
.
.
a
.
.
Baseline
.
.
a
.
A..A.A .
.
.
.--
.
.
.
.
.
.
.
.
.
.
.
.
.
RVDC During Intrapericardial Run
.
RDVC During Intrapleural Infuslon
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
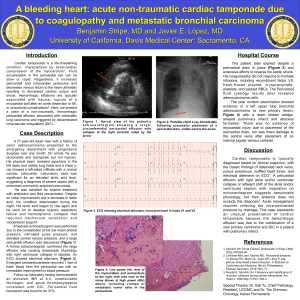
pressure data in a typical experiment during baseline (left panel), at RVDC during
intrapericardial infusion (middle panel), and at RVDC during intrapleural infusion (right panel). IPIP, intrapleural pressure;
IPP, intrapericardial pressure; RABP, right atrial blood pressure.
FIGURE 2. Graphs showing phasic
Data Analysis
All data were stored on analog magnetic tape and
transferred to a digital personal computer (Compaq, Inc.).
By use of sequential interactive programs, individual beats
in a 30-second file were defined at the baseline, at each
2-mm Hg increment in intrapericardial pressure above
baseline, at the onset of RVDC, and at the time of
decompensated cardiac tamponade or the termination of
the pleural infusion. Each file included several complete
respiratory cycles. Respiratory phases were noted, and
mean pressures for each data file were calculated. The
volumes infused into the pericardial or pleural spaces
were calculated by multiplying the time to the midpoint of
the 30-second data file by the infusion rate of the pump
and adding the baseline amount of pericardial fluid.
Statistical Analysis
Mean data recorded during each intrapericardial infusion were paired with data recorded during the pleural
infusion run that followed it. Paired t tests were used to
compare baseline values with values at the onset of RVDC
and at the termination of each run.15 Differences between
pericardial and pleural infusions at baseline, at the onset
of RVDC, and at termination were tested with a two-way
repeated-measures ANOVA with the dog as the block
effect. Multivariate regression analysis was used to analyze
the relation between increases in intrapericardial pressure
from baseline versus increases in intrapleural pressure
from baseline, calculated transmural pressure, mean aortic blood pressure, mean pulmonary artery systolic blood
pressure, left atrial blood pressure, mean cardiac output,
mean heart rate, and mean pulsus paradoxus. A multiple
comparison procedure was used to compare pleural infusion and pericardial infusion at baseline, at RVDC, and at
decompensation or the termination of the pleural infusion
as
defined previously.16
Results
Seven matched pairs of pericardial and pleural infusion runs were analyzed in seven conscious unanesthe-
tized dogs. Table 1 shows the mean, end-inspiration,
and end-expiration hemodynamic data (mean+ 1 SEM)
for each intervention at baseline, at the onset of RVDC,
and at the termination of each run.
Mean Hemodynamic Measurements During
Pericardial and Pleural Infusions
By design, a small amount of pericardial fluid was
present at baseline for both pericardial infusion runs (30
ml saline) and pleural infusion runs (63+±3 ml saline).
Mean absolute intrapericardial pressures were similar
statistically at 0.45+0.09 and 1.73±0.14 mm Hg, respectively. Therefore, the animals were operating on the flat
portion of their pericardial pressure-volume curves in
both baseline situations.5 Furthermore, the mean absolute
intrapleural pressures (-3.45+0.31 versus -3.33+0.26
mm Hg, respectively) were not different at that time. At
baseline, the mean initial right atrial blood pressure,
cardiac output, aortic blood pressure, left atrial blood
pressure, pulmonary artery systolic blood pressure, calculated transmural pressure, degree of pulsus paradoxus,
systemic vascular resistance, and stroke volume did not
differ statistically between the two conditions. At the onset
of RV diastolic collapse, the mean absolute intrapericardial pressure was statistically the same regardless of treatment (8.17±0.20 mm Hg for pericardial infusion versus
9.47±0.20 mm Hg for pleural infusion). In addition, the
increase in intrapleural pressure paralleled that of intrapericardial pressure during the intrapleural fluid infusion.
At the time of onset of RVDC, the mean right atrial blood
pressure, cardiac output, heart rate, left atrial blood
pressure, calculated transmural pressures, systemic vascular resistance, and stroke volume were the same for both
types of infusion. Mean aortic blood pressure, however,
was 84.7±1.1 mm Hg during pericardial infusion and
109.0±2.0 mm Hg during pleural infusion (p<0.0001).
Similarly, mean pulmonary artery systolic blood pressure
varied by intervention (pericardial infusion, 23.29±0.94
mm Hg and pleural infusion, 38.74±1.25 mm Hg,
p<0.0001), as did calculated transmural pressure
(24.25±0.72 and 34.05±0.64 mm Hg, respectively;
614
Circulation Vol 86, No 2 August 1992
A
B
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
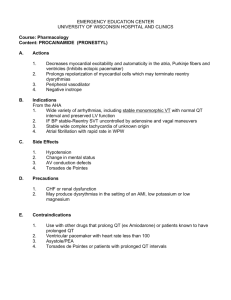
FIGURE 3. Two-dimensionalparasternal short-axis echocardiograms (early-diastolic frames) (panel A) after 1.5 liters of saline
has been instilled into the pleural space, and (panel B) at the onset of RVDC during the same pleural infusion. AV aortic valve;
LA, left atrium; PE, pericardial effusion; PlE, pleural effusion; RVO, right ventricular outflow tract; PA, pulmonary artery; L,
lung.
p<O.001). The magnitude of pulsus paradoxus at the onset
of RVDC also varied by intervention (p<O.O1). At the
termination of each type of infusion (i.e., hemodynamic
decompensation for pericardial infusion and an equivalent
increase in intrapericardial pressure during pleural infusion), the increase in intrapleural pressure continued to
parallel the increase in intrapericardial pressure only
during the intrapleural infusion. Figure 1A graphically
displays this continuous relation between mean intrapleural pressure and mean intrapericardial pressure for both
interventions. As for all values in this study, the curves
represent the mean±SEM (at 2-mm Hg increments in
intrapericardial pressure) for both intrapericardial (solid
curves) and intrapleural infusions (dashed curves) and
only extend to the end points of each condition. These two
curves differ significantly (p<0.001). Although not illustrated, the curves for mean right atrial blood pressure,
calculated mean transmural right atrial pressure, and
heart rate did not differ statistically between the two
treatments. Hemodynamic decompensation during pericardial infusion was marked by a reduction compared with
baseline in mean cardiac output (Figure 1B, curves significantly different; p<0.01), aortic blood pressure (Figure
1C, curves significantly different; p<0.001), and stroke
volume (Figure 1D, curves significantly different;p<O.01).
These values during decompensated cardiac tamponade
were significantly less than at the end point during pleural
infusion (p<0.0001 in all cases). At the same time, the
final systemic vascular resistance was higher during intrapericardial infusion (p<0.01). Therefore, at similar increases in intrapericardial pressure during each type of
infusion in these euvolemic animals, hemodynamic decompensation occurred only with intrapericardial infusion. Whereas the initial mean and calculated transmural
pulmonary artery systolic blood pressures were similar for
both treatments, they fell during decompensation because
of intrapericardial infusion and actually increased to hypertensive levels during pleural infusion (Table 1,
p<O.0001); the curves were significantly different (Figure
lE, p<O.001). The magnitude of pulsus paradoxus also
varied by intervention between the two end points
(p<0.0001), and the curves were significantly different
(Figure 1F, p<O0O1). Left atrial blood pressure had increased at the end point of both interventions but to a
lesser extent with intrapericardial infusion (p<O0.05 versus
pleural infusion); calculated transmural left atrial blood
pressures were similar.
Vaska et al Pleural Effusion
-
R
40
PA
0
20
LABP
0
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
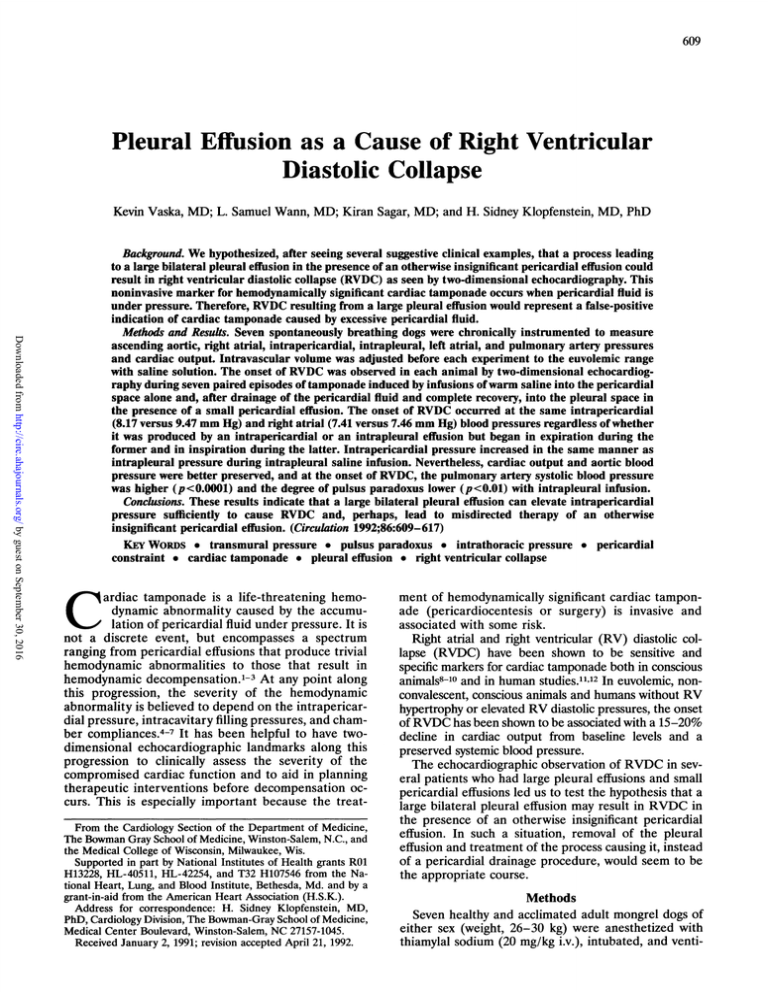
FIGuRE 4. Curves showing phasic pressure data at hemodynamic decompensation during intrapericardial infusion. R,
respiration (inspiration is indicated by a positive deflection);
PA, pulmonary artery blood pressure; LABP, left atrial blood
pressure.
Rfight Ventricular Diastolic Collapse
Adequate two-dimensional short-axis parasternal
echocardiograms were obtained in all infusion runs. No
dog failed to develop RVDC during any of the infusion
episodes. For both mechanisms, RVDC began in early
diastole and was equivalent in degree by criteria outlined above and became more pronounced and of
greater duration as the infusion progressed. RVDC,
however,, began during expiration with pericardial infusion and during inspiration with pleural infusion. Review of the phasic pressure data in a typical experiment
(Figure 2) revealed markedly diminished respiratory
fluctuations of intrapericardial and right atrial blood
pressures during intrapericardial infusion compared
with intrapleural infusion. With intrapericardial infusion during the inspiratory phase, both intrapericardial
pressure and right atrial blood pressure declined slightly
and to a similar extent. Intrapericardial pressure, however, slightly exceeded right atrial blood pressure during
the expiratory phase. In contrast, right atrial blood
pressure declined substantially and to a greater degree
than intrapericardial pressure with inspiration during
the intrapleural infusion. Figure 3 displays echocardiograms after 1.5 1 saline had been rapidly instilled into
the pleural space and at the onset of RVDC during the
same pleural infusion run.
Figure 4 illustrates phasic pressure data at the time of
hemodynamic decompensation during intrapericardial
infusion and reveals a vigorous respiratory excursion
and an apparent reversal of the pressure difference
across the pulmonary vascular bed.
Discussion
Cardiac tamponade is a continuum ranging from an
asymptomatic pericardial effusion with minimal hemodynamic derangement to severe cardiac compression
and hypotension.1"8 The onset of collapse of the RV free
wall in early diastole, as intrapericardial (extracardiac)
pressure exceeds RV diastolic pressure, identifies a
specific point in this progression of hemodynamic
events.2,3"7"18 In conscious, nonconvalescent, euvolemic
615
dogs without RV hypertrophy, this occurs when cardiac
output has declined about 20% from baseline but before
significant changes in aortic blood pressure have occurred. RVDC has been shown to be sensitive and
specific for the early detection of a hemodynamically
important pericardial effusion10 and has been used as an
indication that a pericardial drainage procedure is
needed. We have reported that RVDC may be absent
despite elevated intrapericardial pressures and significant hemodynamic impairment in the presence of RV
hypertrophy or during acute elevations of RV pressure.8'2 Conversely, we found RVDC to occur in the
presence of an otherwise insignificant pericardial effusion if cardiac size were abruptly increased.7 If the
process leading to the acute increase in cardiac size
were reversible, we would suggest that therapy be
directed to that end and RVDC be considered a falsepositive indication that a drainage procedure was
indicated.
In the present study, we have identified yet another
cause for RVDC in the absence of a hemodynamically
significant pericardial effusion. Although little has been
written about the hemodynamic significance of large
bilateral pleural effusions under pressure, this intervention would be expected to contribute to overall extracardiac pressure, given a compliant pericardium.14"518-21
Indeed, our data (Figure 1A, Table 1) show that intrapleural and intrapericardial pressures rise uniformly during intrapleural fluid infusion. Most importantly, the
onset of RVDC for both interventions occurred at similar intrapericardial pressures.
There were three unexpected and provocative findings. First, the same intrapericardial pressure is better
tolerated when caused by pleural effusion in the presence of a small pericardial effusion than when caused
solely by increased pericardial fluid. For example, the
same intrapericardial pressure that produced hemodynamic decompensation during isolated cardiac tamponade was associated with a smaller reduction in stroke
volume, no significant change from baseline in mean
aortic blood pressure, less pulsus paradoxus, and an
increase in pulmonary artery blood pressure during
intrapleural fluid infusion. Increasing intrapericardial
pressure during intrapericardial saline infusion in these
dogs was associated with a continuous decrease in mean
aortic blood pressure. This response is typical of convalescent conscious dogs and differs from that seen on
day 4 or 5 after surgery and thereafter, when mean
arterial blood pressure is well preserved during acute
cardiac tamponade until late in the progression.8'9 It was
necessary to study these dogs on day 2 or 3 after surgery
to ensure that the pleural surface overlying the parietal
pericardium was not affected by adhesions or fibrosis.
The major cause of hemodynamic deterioration during intrapericardial infusion appears to be the greater
fall in stroke volume at similar elevated heart rates. This
was associated with a greater elevation in systemic
vascular resistance than occurred during intrapleural
infusion. Perhaps the enhanced ability to tolerate increased intrapericardial pressure during intrapleural
infusion in these euvolemic convalescent dogs is related
to the better-preserved respiratory variation of intrapericardial pressure (as evidenced by comparison of the
end-inspiratory and end-expiratory pressures) with
brief inspiratory improvement in chamber compliance,
616
Circulation Vol 86, No 2 August 1992
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
left heart filling gradient,18'21-23 and reduced left ventricular afterload.4'21'24'25 As with the less severe extent
of pulsus paradoxus, a smaller degree of pulmonary
vascular pooling (caused by relatively smaller lung volumes) and adverse ventricular interactions may have
also played a role.2324 In addition, contractility may
have been supported more vigorously by neurohumoral
responses to this stress. The mechanism(s) responsible
for these observations and other possible reasons for
the smaller increase in pulsus paradoxus during intrapleural infusion require further study.
The second unexpected finding was that the onset of
RVDC occurred during expiration during intrapericardial infusion and inspiration during intrapleural infusion. During intrapericardial infusion, the cause of
RVDC, much like that of pulsus paradoxus, has been
related in part to the inspiratory augmentation of
venous return, RV volume, and right-sided pressures.',2,24-26 As a result, elevated intrapericardial pressure exceeded elevated RV diastolic pressure only in
expiration (i.e., transmural pressure became negative)
and led to the initiation of RVDC during this respiratory phase.12'27 In contrast to the observations of Shabetai et al,26 we found that the inspiratory augmentation
of RV volume in acute cardiac tamponade did not
further increase intrapericardial pressure, although the
transpericardial pressure did rise as a result of negative
intrathoracic pressure. This difference may have occurred because we used a chronically instrumented,
unanesthetized, convalescent canine model instead of
the acute model they studied. Our data are consistent
with theories on the changing relation of right-sided
diastolic and intrapericardial pressures.28'29 In the present study, intrapericardial infusion was associated with
minimal respiratory variation in both intrapericardial
and right atrial blood pressures (Figure 2), with a
constant and minimal varying difference between these
two pressures throughout the respiratory cycle. Intrapericardial pressure showed enough variation to exceed
right atrial blood pressure only in expiration, thereby
creating the negative RV transmural pressure that led
to RVDC. During intrapleural infusion, negative swings
in intrathoracic pressure were followed by both intrapericardial and right atrial blood pressures, but right
atrial blood pressure fell to a lower level, leading to a
negative transmural pressure and RVDC. Apparently,
the inspiratory augmentation of venous return was
insufficient to offset the fall in right atrial blood pressure
created by the negative intrathoracic pressure, perhaps
because of a reduced extrathoracic-to-intrathoracic
venous pressure gradient.4'6'21"30
During hemodynamic decompensation caused by intrapericardial saline infusion, pulmonary artery systolic
blood pressure fell below mean left atrial blood pressure
(Figure 4). Cardiac output at this time was 1.2 1/min.
This decline in pulmonary artery systolic pressure (i.e.,
narrowing of pulse pressure) has been described previously,12'3' as have the "reversed gradients" between
intrapericardial and extrapericardial structures,25,28,29,32
at least during inspiration. Furthermore, extreme cardiac tamponade has been characterized by pericardial
pressure exceeding pulmonary artery systolic blood
pressure, and it has been suggested that elastic recoil
(i.e., diastolic suction) associated with a negative transmural pressure gradient is responsible for left ventricu-
lar filling,33'34 as evidenced by the negative left atrial
transmural pressure. The reduction in left ventricular
filling gradient we observed could, at least in part,
represent a reason for the precipitous drop in stroke
volume seen with decompensation during intrapericardial infusion. This mechanism could not be effective if
the chambers of the heart function as Starling resistors
during cardiac tamponade. Another provocative theory
would be that blood flow through the pulmonary vascular bed during decompensated cardiac tamponade in
this conscious euvolemic model is dependent on
changes in pulmonary vascular capacitance induced by
respiratory activity instead of on energy derived from
right heart contraction. Therefore, there would be preservation of pulmonary venous-to-left atrial blood flow
only in expiration.25 The data in Figure 4 were recorded
during hemodynamic decompensation (same dog as
Figure 2) and demonstrate that inspiratory excursions
are present. More importantly, the intrapleural pressure at decompensation revealed markedly increased
respiratory excursions compared to baseline during the
intrapericardial infusion run. This suggests an increasing dependence on the mechanical energy of respiration
to transport blood from the right to the left heart and a
tight coupling of right and left heart function to the
phase of respiration. These observations are consistent
with those of Burwell,35 who noted that the loss of
effective RV pumping caused by excessive intrapericardial pressure did not signal the end of left ventricular
filling. The RV/pulmonary artery pressure was reduced
to a nonpulsatile curve that faithfully followed intrapleural pressure. In subsequent experiments using a
similar conscious canine model studied 5-14 days after
surgery when the dogs had completely recovered, we
found the pressure gradient across the pulmonary vascular bed to decrease to very low levels, but we never
observed a reversal of the gradient as we did in these
convalescent dogs.
Clinical Implications
We have seen several patients with large bilateral
pleural effusions and small pericardial effusions who
underwent echocardiography for evaluation of deteriorating hemodynamic status and were found to have
RVDC. A number of investigations have shown that
RVDC reflects a hemodynamically significant increase
in intrapericardial fluid pressure8'9"1217 and implies that
appropriate treatment strategies for pericardial tamponade should be undertaken. A previous study from
our laboratory has shown that RVDC occurs at a higher
intrapericardial pressure and lower intrapericardial
fluid volume in the presence of acute left ventricular
pressure overload, thus representing a potential falsepositive indication of significant pericardial effusion.7 In
our canine model, the onset of RVDC occurred at
similar intrapericardial and right atrial blood pressures
during both pericardial and pleural infusions. Therefore, large pleural effusions can cause cardiac chamber
compression in a manner analogous to that caused by
intrapericardial fluid infusion.
Conclusions
A process leading to a large bilateral pleural effusion,
in the presence of an otherwise unimportant pericardial
effusion, may increase intrapericardial fluid pressure
Vaska et al Pleural Effusion
sufficiently to cause RVDC. We suggest that in this
situation, RVDC is a false-positive indication of a
pericardial effusion in need of drainage and that the
appropriate therapeutic maneuver is drainage of the
pleural effusion(s).
Acknowledgments
We thank Hua Chen, MSEE, and Douglas Hettrick, BE, for
their technical assistance and Tina Burchette and Kathy
Hurdle for preparing the manuscript.
References
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
1. Shabetai R, Mangiardi L, Bhargava V, Ross J, Higgins C: The
pericardium and cardiac function. Prog Cardiovasc Dis 1979;22:
107-134
2. Shabetai R, Fowler N, Guntheroth W: The hemodynamics of cardiac tamponade and constrictive pericarditis. Am J Cardiol 1970;
26:480-489
3. Fowler N: Physiology of cardiac tamponade and pulsus paradoxus.
Mod Concepts Cardiovasc Dis 1978;47:115-118
4. Morgan B, Guntheroth W, Dillard D: Relationship of pericardial
to pleural pressure during quiet respiration and cardiac tamponade. Circ Res 1965;16:493-498
5. Holt J, Rhode E, Kines H: Pericardial and ventricular pressure.
Circ Res 1960;8:1171-1181
6. Holt J: The normal pericardium. Am J Cardiol 1970;26:455-465
7. Cogswell T, Bernath G, Keelan M, Wann L, Klopfenstein H: The
shift in the relationship between intrapericardial fluid pressure and
volume induced by acute left ventricular pressure overload during
cardiac tamponade. Circulation 1986;74:173-180
8. Leimgruber P, Klopfenstein H, Wann L, Brooks H: The hemodynamic derangement associated with right ventricular diastolic collapse in cardiac tamponade: An experimental echocardiographic
study. Circulation 1983;68:612-620
9. Cogswell TL, Bernath GA, Raff H, Hoffman RG, Klopfenstein
HS: Total peripheral resistance during cardiac tamponade: Adrenergic and angiotensin roles. Am J Physiol 1986;251:R916-R922
10. Klopfenstein H, Cogswell T, Bernath G, Wann L, Tipton K, Hoffman R, Brooks H: Alterations in intravascular volume affect the
relation between right ventricular diastolic collapse and the hemodynamic severity of cardiac tamponade. JAm Coll Cardiol 1985;6:
1057-1063
11. Gillam L, Guyer D, Gibson T, King M, Marshall J, Weyman A:
Hydrodynamic compression of the right atrium: A new echocardiographic sign of cardiac tamponade. Circulation 1983;68:294-301
12. Singh S, Wann L, Schuchard G, Klopfenstein H, Leimgruber P,
Keelan M, Brooks H: Right ventricular and right atrial collapse in
patients with cardiac tamponade: A combined echocardiographic
and hemodynamic study. Circulation 1984;70:966-971
13. Case R, Roselle H, Nassar M: Simplified method for calibration of
electromagnetic flowmeters. Med Res Eng 1966;5:38-40
14. Smiseth 0, Frais M, Kingma I, Smith E, Tyberg E: Assessment of
pericardial constraint in dogs. Circulation 1985;71:158-164
617
15. Winer B: Statistical Principles in Experimental Design, ed 2. New
York, McGraw-Hill, 1971, pp 316-370
16. Glantz S: Primer of Biostatistics, ed 2. New York, McGraw-Hill,
1987, pp 191-245
17. Ditchey R, Engler R, LeWinter M, Pavelec R, Bhrgava V, Covell
J, Moores W, Shabetai R: The role of the right heart in acute
cardiac tamponade in dogs. Circ Res 1981;48:701-710
18. Isaacs J, Berglund E, Sarnoff S: Ventricular function: III. The
pathologic physiology of acute cardiac tamponade studied by
means of ventricular function curves. Am Heart J 1954;48:66-76
19. Guntheroth W, Morgan B, Mullins G: Effect of respiration on
venous return and stroke volume in cardiac tamponade: Mechanism of pulsus paradoxus. Circ Res 1967;20:381-390
20. Janicki J, Shroff S, Weber K: Extracardiac pressure and ventricular
hemodynamics: Contrasting effects of pericardial and pleural pressures. (abstract) Circulation 1981;64(suppl IV):IV-54
21. Weber K, Janicki J, Shroff S, Likoff M: The cardiopulmonary unit:
The body's gas transport system. Clin Chest Med 1983;4:101-110
22. Braunwald E: Regulation of the circulation. N Engl J Med 1974;
290:1124-1130
23. Refsum H, Junemann M, Lipton M, Skioldebrand C, Carlsson E,
Tyberg J: Ventricular diastolic pressure-volume relations and the
pericardium: Effects of changes in blood volume and pericardial
effusion in dogs. Circulation 1981;64:997-1004
24. McGregor M: Pulsus paradoxus. N Engl J Med 1979;301:480-482
25. Golinko R, Kaplan N, Rudolph A: The mechanism of pulsus
paradoxus during acute pericardial tamponade. J Clin Invest 1963;
42:249-257
26. Shabetai R, Fowler N, Fenton J, Masangkay M: Pulsus paradoxus.
J Clin Invest 1965;44:1882-1898
27. Schiller N, Botvinick E: Right ventricular compression as a sign of
cardiac tamponade: An analysis of echocardiographic ventricular
dimensions and their clinical implications. Circulation 1977;56:
774-779
28. Reddy P, Curtiss E, O'Toole J, Shaver J: Cardiac tamponade:
Hemodynamic observations in man. Circulation 1978;58:265-272
29. Reddy P: Hemodynamics of cardiac tamponade in man, in Reddy
PS, Leon DF, Shaver JA (eds): Pericardial Disease. New York,
Raven Press, 1982, pp 161-187
30. Spodick D: The normal and diseased pericardium: Current concepts of pericardial physiology, diagnosis and treatment. JAm Coll
Cardiol 1983;1:240-251
31. Metcalfe J, Woodbury J, Richards V, Burwell C: Studies in experimental pericardial tamponade: Effects in intravascular pressures
and cardiac output. Circulation 1952;5:518-523
32. Appleton C, Hatle L, Popp R: Cardiac tamponade and pericardial
effusion: Respiratory variation in transvalvular flow velocities studied by Doppler echocardiography. J Am Coll Cardiol 1988;11:
1020-1030
33. Fowler N, Shabetai R, Braunstein J: Transmural ventricular pressures in experimental cardiac tamponade. Circ Res 1959;7:733-739
34. Becher G: Critical review of recent work on ventricular diastolic
suction. Circ Res 1958;6:554-566
35. Burwell C: Some effects of pericardial disease on the pulmonary
circulation. Trans Assoc Am Physicians 1951;64:74-84
Pleural effusion as a cause of right ventricular diastolic collapse.
K Vaska, L S Wann, K Sagar and H S Klopfenstein
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Circulation. 1992;86:609-617
doi: 10.1161/01.CIR.86.2.609
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1992 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/86/2/609
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/