Types and Functions of Muscle Tissue
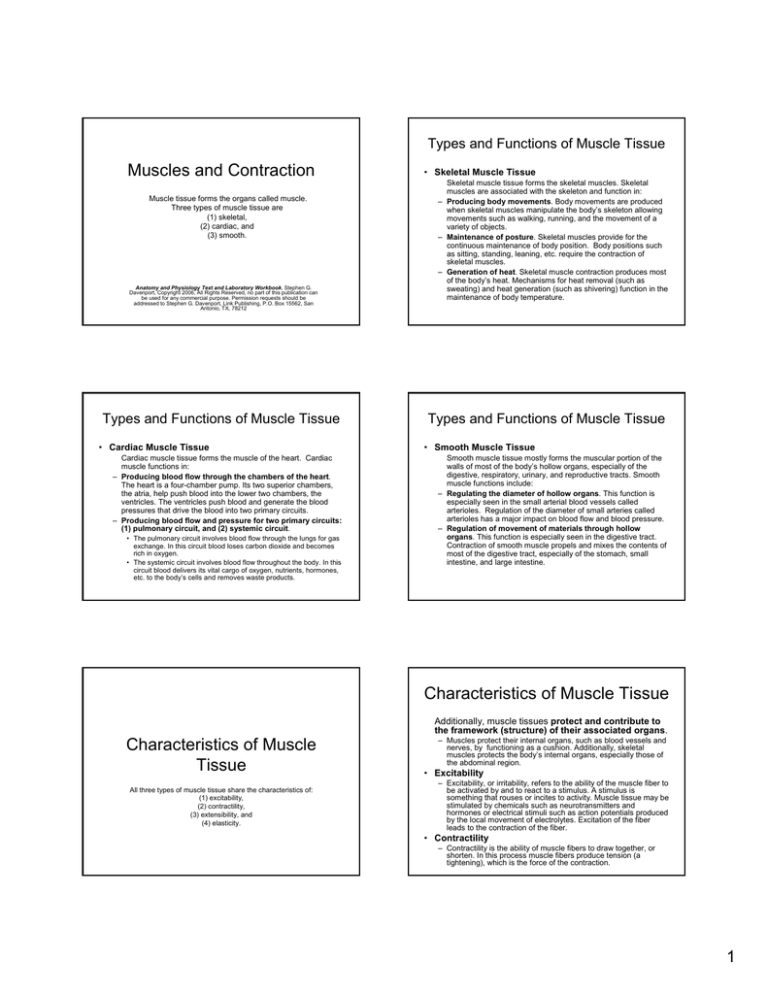
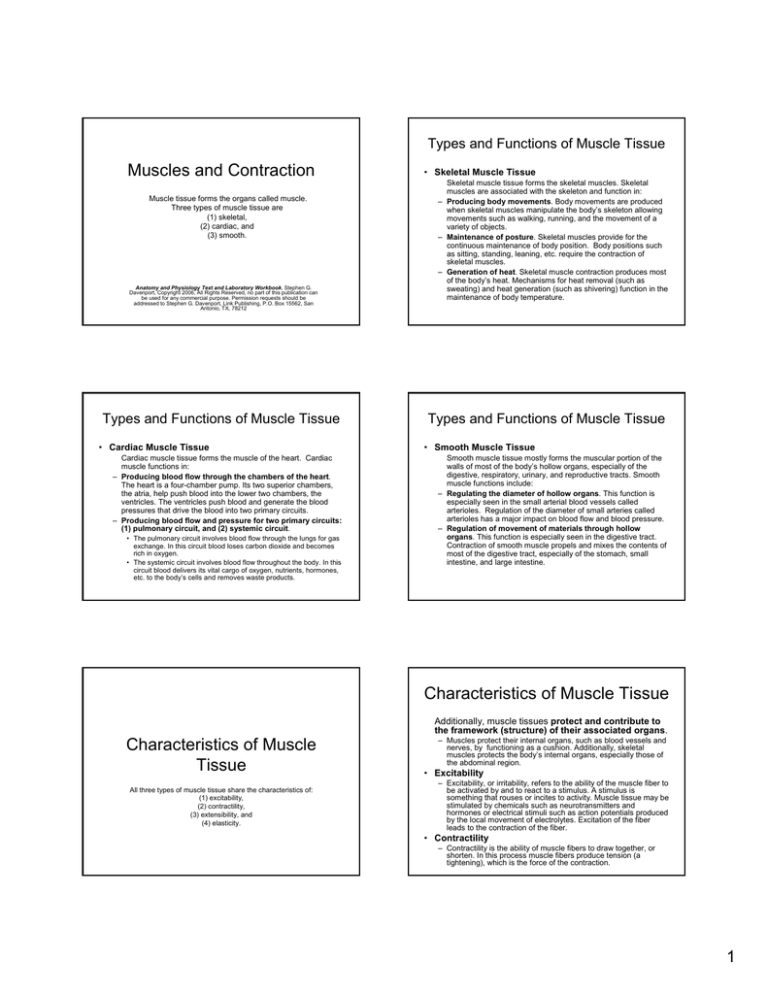
Muscles and Contraction
Muscle tissue forms the organs called muscle.
Three types of muscle tissue are
(1) skeletal,
(2) cardiac, and
(3) smooth.
Anatomy and Physiology Text and Laboratory Workbook, Stephen G.
Davenport, Copyright 2006, All Rights Reserved, no part of this publication can
be used for any commercial purpose. Permission requests should be
addressed to Stephen G. Davenport, Link Publishing, P.O. Box 15562, San
Antonio, TX, 78212
Types and Functions of Muscle Tissue
• Cardiac Muscle Tissue
Cardiac muscle tissue forms the muscle of the heart. Cardiac
muscle functions in:
– Producing blood flow through the chambers of the heart.
The heart is a four-chamber pump. Its two superior chambers,
the atria, help push blood into the lower two chambers, the
ventricles. The ventricles push blood and generate the blood
pressures that drive the blood into two primary circuits.
– Producing blood flow and pressure for two primary circuits:
(1) pulmonary circuit, and (2) systemic circuit.
• The pulmonary circuit involves blood flow through the lungs for gas
exchange. In this circuit blood loses carbon dioxide and becomes
rich in oxygen.
• The systemic circuit involves blood flow throughout the body. In this
circuit blood delivers its vital cargo of oxygen, nutrients, hormones,
etc. to the body’s cells and removes waste products.
• Skeletal Muscle Tissue
Skeletal muscle tissue forms the skeletal muscles. Skeletal
muscles are associated with the skeleton and function in:
– Producing body movements. Body movements are produced
when skeletal muscles manipulate the body’s skeleton allowing
movements such as walking, running, and the movement of a
variety of objects.
– Maintenance of posture. Skeletal muscles provide for the
continuous maintenance of body position. Body positions such
as sitting, standing, leaning, etc. require the contraction of
skeletal muscles.
– Generation of heat. Skeletal muscle contraction produces most
of the body’s heat. Mechanisms for heat removal (such as
sweating) and heat generation (such as shivering) function in the
maintenance of body temperature.
Types and Functions of Muscle Tissue
• Smooth Muscle Tissue
Smooth muscle tissue mostly forms the muscular portion of the
walls of most of the body’s hollow organs, especially of the
digestive, respiratory, urinary, and reproductive tracts. Smooth
muscle functions include:
– Regulating the diameter of hollow organs. This function is
especially seen in the small arterial blood vessels called
arterioles. Regulation of the diameter of small arteries called
arterioles has a major impact on blood flow and blood pressure.
– Regulation of movement of materials through hollow
organs. This function is especially seen in the digestive tract.
Contraction of smooth muscle propels and mixes the contents of
most of the digestive tract, especially of the stomach, small
intestine, and large intestine.
Characteristics of Muscle Tissue
Additionally, muscle tissues protect and contribute to
the framework (structure) of their associated organs.
Characteristics of Muscle
Tissue
All three types of muscle tissue share the characteristics of:
(1) excitability,
(2) contractility,
(3) extensibility, and
(4) elasticity.
– Muscles protect their internal organs, such as blood vessels and
nerves, by functioning as a cushion. Additionally, skeletal
muscles protects the body’s internal organs, especially those of
the abdominal region.
• Excitability
– Excitability, or irritability, refers to the ability of the muscle fiber to
be activated by and to react to a stimulus. A stimulus is
something that rouses or incites to activity. Muscle tissue may be
stimulated by chemicals such as neurotransmitters and
hormones or electrical stimuli such as action potentials produced
by the local movement of electrolytes. Excitation of the fiber
leads to the contraction of the fiber.
• Contractility
– Contractility is the ability of muscle fibers to draw together, or
shorten. In this process muscle fibers produce tension (a
tightening), which is the force of the contraction.
1
Characteristics of Muscle Tissue
• Extensibility
– Extensibility is the ability of muscle fibers to elongate, or stretch.
The extensibility of muscles is especially apparent in skeletal
muscle flexion and extension. As one muscle contracts and the
angle at the joint decreases (flexion), an opposing muscle is
extended, or stretched. Extensibility is also apparent in the
smooth muscle of the stomach, allowing filling of the stomach as
the muscle stretches.
Skeletal Muscles
Anatomy of a Skeletal Muscle
• Elasticity
– Elasticity is the ability of the muscle fibers to return to its normal
resting length after contraction or extension. Elasticity allows
muscle fibers to return their optimal working length.
Anatomy of a Skeletal Muscle
•
Anatomy of a Skeletal Muscle
Skeletal muscles are formed from muscle skeletal muscle fibers
(cells) and their associated connective tissues.
– The number of fibers and the amount of connective tissues in a muscle
varies from muscle to muscle.
– A muscle is well supplied with blood vessels and nerves. Blood
vessels are essential for the delivery of nutrients, oxygen, etc. and for
the removal of waste materials. Nerves associated with muscles
typically have both sensory and motor functions.
– Sensory endings (receptors) are found within the muscle (muscle
spindles) and in the muscle’s connective tissues. Additional receptors
are found within tendons and the connective tissues of the joints.
Sensory receptors monitor a muscle’s contraction and initiate nerve
impulses that are conducted along sensory fibers (axons) to the central
nervous system for integration.
– Motor fibers (axons) originate from motor neurons in the central
nervous system and terminate on muscle fibers at neuromuscular
junctions. Motor fibers conduct action potentials (nerve impulses) to the
muscle fiber. Acetylcholine (a neurotransmitter) released at the
neuromuscular junctions supplies the stimulus which initiates excitation
of the skeletal muscle fiber.
Skeletal Muscle Fiber
• The functional unit of a skeletal muscle is the
muscle fiber.
– An individual fiber is long, cylindrical,
multinucleate, striated, and typically lies parallel
to adjacent fibers.
– Each individual fiber has at least one connection
(synapse) with a motor neuron at a nerve-muscle site
called a neuromuscular junction.
– Each fiber is surrounded by a connective tissue
sheath called the endomysium.
– Fibers and their associated sheaths of endomysium
are arranged in groups and surround by connective
tissue, the perimysium, to form fascicles.
Figure 16.1
The anatomy of a typical skeletal muscle.
The functional unit of a muscle is the
muscle fiber (cell).
2
Connective Tissues of a Muscle
• Endomysium
Connective Tissues of a
Muscle
– Each muscle fiber is surrounded by and attached to a connective
tissue covering called the endomysium.
– The endomysium consists of short branching reticular fibers,
fibroblasts, and matrix. As the muscle fiber contracts, force is
transferred to the endomysium.
– The endomysium connects and transfers force to its associated
perimysium.
• Perimysium
– The perimysium is a layer of fibrous connective tissue that is
continuous with the endomysium and surrounds a group of
muscle fibers, a fascicle.
– The perimysium of the fascicles is continuous with the outer
layer of the muscle, the epimysium
Connective Tissues of a Muscle
• Epimysium
– The epimysium is the outer layer of dense irregular fibrous
connective tissue that surrounds the entire muscle.
– The epimysium is continuous with the perimysium and in most
muscles continues as dense regular connective tissue to form a
tendon. Tendons connect muscles to bones. A tendon connects
to the fibrous layer of a bone’s periosteum, where fibrous
extensions called Sharpey’s fibers enter into the bone’s matrix.
Lab Activity 1
Skeletal Muscle – l.s.
Skeletal Muscle in
longitudinal section
Lab Activity 1
Skeletal Muscle – l.s. (longitudinal section)
• Observe a tissue preparation labeled “Skeletal
Muscle, l.s.,” or “Muscle, three types.” A
nonparallel section makes the fibers appear
short and interwoven.
– Skeletal muscle fibers are characterized by having
distinctive cross bands called striations.
– The striations are produced by the alternating
arrangement of proteins in the rod-like contractile
elements called myofibrils.
Figure 16.2
Skeletal muscle consists of long
multinucleated fibers (cells).
3
Lab Activity 1
Skeletal Muscle – l.s. (longitudinal section)
• Fiber
– Because the muscle cell resembles the structure of a fiber,
(being long, thin, and cylindrical) the term fiber is substituted for
“cell.”
• Myofibril
Figure 16.3
Skeletal muscle (100x) consists of fibers (cells) that are long,
parallel, and striated. Long protein contractile elements, the
myofibrils, run the length of the fiber and contain thin and thick
protein filaments. The alternating arrangement of thin and thick
protein filaments produces the cross-bands called striations.
Lab Activity 1
Skeletal Muscle – l.s. (longitudinal section)
• Striations
– Striations are the cross bands produced by the alternating
pattern of thin and thick filaments along the length of the
myofibrils. The alignment of the striations of adjacent myofibrils
produces the striations of the fiber.
• Endomysium
– The endomysium is the layer of connective tissue that surrounds
each individual muscle fiber. It consists mostly of reticular fibers,
fibroblasts, matrix. The endomysium serves as a passageway for
capillaries and nerve fibers, and transmits the contractile force
from the fiber to adjacent connective tissues.
– Myofibrils are long parallel contractile elements that are mostly
composed of the contractile proteins actin and myosin.
Myofibrils are difficult to identify on most slide preparations. In
longitudinal sections of muscle, the myofibrils appear as
extremely thin parallel elements that have striations. The
alignment of the striations of adjacent myofibrils produces the
striations of the fiber.
Lab Activity 1
Skeletal Muscle – l.s. (longitudinal section)
• A band
– The A bands are the dark cross-bands and consist mostly of
protein filaments called thick filaments. The thick filaments are
associated with other proteins in two regions: (1) a region called
the zone of overlap, where thin filaments from the I bands
overlap the thick filaments, and (2) a central region called the M
line, where structural proteins align adjacent think filaments.
• I band
– The I bands are the light cross-bands. The I bands consist of
protein filaments called thin filaments. The thin filaments have a
central region called the Z lines (discs).
Lab Activity 1
Skeletal Muscle – l.s. (longitudinal section)
• Z lines (disks)
– Z lines are protein filaments located at the centers of
the I bands. The Z lines connect the thin filaments of
adjacent sarcomeres.
• Sarcomere
– The sarcomere is the region between two adjacent Z
lines (discs). The sarcomeres are the functional units
of contraction within the fiber.
Figure 16.4
Skeletal muscle fiber (1,000x) showing the
detail of the striations (bands) and the
sarcomere.
4
Lab Activity 2
Skeletal Muscle x.s.
Figure 16.5
Skeletal muscle fiber (1,500x) showing the
bands of the fiber.
Skeletal Muscle in
Cross Section
Lab Activity 2
Skeletal Muscle x.s. (cross section)
• Observe a tissue preparation labeled
“Skeletal Muscle, xs.”
– A preparation of a cross section of a muscle is
useful in showing the anatomy of the muscle.
Exceptionally good preparations show the
cross sectional detail of the individual fibers.
Figure 16.6
A cross section of a muscle (40x) showing
the general organization of the muscle.
Lab Activity 2
Skeletal Muscle x.s. (cross section)
• Fibers
– Because the cells of muscles are long, cylindrical, and threadlike, the cells are called fibers. In cross section each fiber is
seen surrounded by a thin light area of connective tissue called
the endomysium.
• Endomysium
– The endomysium is the connective tissue that surrounds the
muscle fibers. The endomysium merges into a layer of
connective tissue the perimysium.
• Perimysium
– The perimysium is the connective tissue that surrounds a group
of fibers and their associate connective tissue, the endomysium.
The perimysium merges into the outer connective tissue of the
muscle called the epimysium.
• Fascicles
Figure 16.7
Cross sections of muscle fibers as observed under oil
immersion (1,500x). The small dots are cross sections of
the fiber’s myofibrils. Myofibrils consist mostly of the
contractile proteins, actin and myosin. Regulatory and
organizational proteins are also present.
– Fascicles are groups of fibers surrounded by a layer of
connective tissue called the perimysium.
5
Lab Activity 2
Skeletal Muscle x.s. (cross section)
• Myofibril
– Myofibrils in cross section are difficult to identify on
most slide preparations. In a cross section of a
muscle fiber, the myofibrils appear as extremely small
dots.
– Myofibrils are the contractile elements that are mostly
composed of the thin and thick filaments. The thin
filaments house the contractile protein actin, and the
thick filaments house the contractile protein myosin.
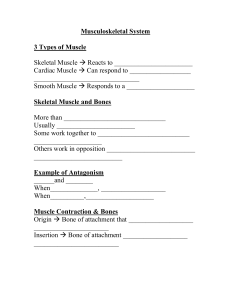
Attachments of a Muscle
Muscles typically have at two ends, each with one or more
sites of dense fibrous connective tissue that serves as points
of attachment. These points of attachment are either direct
or indirect attachments and serve either as the moveable or
immovable attachment sites.
Direct Attachments
• Direct attachments occur when the
epimysium of the muscle directly attaches
to the periosteum of the bone or
perichondrium of cartilage.
Figure 16.8
The connective tissues surrounding skeletal muscle
fibers are shown attached into the fibrous layer of
the periosteum.
Indirect Attachments
• Indirect attachments are more common
than direct attachments. Indirect
attachments occur when the epimysium of
the muscle continues as a rope-like dense
regular connective tissue strand called a
tendon or a sheet-like layer called an
aponeurosis.
Figure 16.9
The connective tissues surrounding skeletal muscle fibers are shown continuing
into a tendon. Tendons are rope-like structures formed of dense regular
connective tissue. Tendons connect muscles into the fibrous periosteum of
bone. Sharpey’s fibers connect the fibrous periosteum into the matrix of bone.
6
Attachments
• Insertion
– A muscle’s insertion is the site of attachment that
moves when the muscle contracts.
• Origin
Microanatomy of a Skeletal
Muscle Fiber
– A muscle’s origin is the site of attachment that does
not move when the muscle contracts.
Skeletal muscle fibers are characterized by
being long, cylindrical, striated, and
multinucleated
Neuromuscular Junction
• A neuromuscular junction is the synapse of an
axon of a motor neuron and a muscle fiber.
Figure 16.10
Microanatomy of a skeletal muscle fiber.
– Located at the neuromuscular junction are the
terminals of the axon. The axon terminals house the
presynaptic membrane.
– The presynaptic membrane releases a
neurotransmitter (acetylcholine).
– The region of the sarcolemma (plasma membrane) at
the neuromuscular junction that is responsive to the
neurotransmitter is called the postsynaptic
membrane.
– An action potential begins at the postsynaptic
membrane and spreads over the sarcolemma.
Sarcolemma
• The sarcolemma is the plasma membrane
of the muscle fiber.
– In addition to functioning as the boundary of
the fiber, the sarcolemma is excitable.
– Excitability means that the membrane can
generate and conduct a signal called an
action potential.
Figure 16.11
The neuromuscular junction is the union of an axon of a
motor neuron and the sarcolemma of a muscle fiber.
7
Sarcoplasm and T Tubules
• Sarcoplasm
– Sarcoplasm is the cytoplasm of the muscle fiber.
• Transverse tubules (T tubules)
– Transverse tubules (T tubules) are small excitable
tubules continuous with the sarcolemma and in close
association with the terminal cisternae of the
sarcoplasmic reticulum.
– Each T tubule is located between two terminal
cisternae forming a unit called a triad.
– T tubules wrap around the myofibrils and conduct
action potentials from the sarcolemma into the interior
of the fiber.
– T tubules contain extracellular fluid.
Figure 16.12
The sarcolemma is an excitable
membrane; it generates and conducts an
action potential.
Sarcoplasmic Reticulum
•
Figure 16.13
Transverse tubules (T tubules) are small excitable tubules
continuous with the sarcolemma and in close association
with the terminal cisternae of the sarcoplasmic reticulum.
The sarcoplasmic reticulum is a system of tubes and
membranes that wraps around each myofibril and is in
close association with the T tubules.
– On each side of a transverse tube the network of smaller tubules
of the sarcoplasmic reticulum merges into chambers called the
terminal cisternae. Thus, at the side of each T tubule there is a
terminal cisterna; the complex forming a unit called a triad.
– Similar to the endoplasmic reticulum of nucleated cells, in
muscle fibers the sarcoplasmic reticulum takes on an additional
role of calcium ion regulation.
– Calcium ion membrane pumps of the sarcoplasmic reticulum
actively remove calcium ions from the sarcoplasm for storage in
the terminal cisternae.
– Thus, resting muscle fibers have a low level of calcium ions in
their sarcoplasm. The arrival of an action potential by way of the
T tubules results in opening the terminal cisternae calcium ion
channels. Calcium ions then diffuse into the sarcoplasm and
initiate contraction.
Myofibrils
• Myofibrils are long parallel contractile elements
that are mostly composed of the contractile
proteins, myosin and actin, organized in the thick
and thin filaments, respectively.
Figure 16.14
The sarcoplasmic reticulum is a system of tubes and membranes that
wraps around each myofibril and is in close association with the
transverse tubules. At the side of each T tubule there is a terminal
cisterna; the complex forming a unit called a triad.
– The arrangement of the contractile proteins produces
cross-bands called striations. The dark bands are
called the A bands, and the light bands are called the
I bands.
– Also, associated with the myofibrils are regulatory
proteins, troponin and tropomyosin, and elastic
filaments called titin. Troponin and tropomyosin are
associated with the thin filaments are regulate
contraction by blocking the interaction of myosin with
actin. Titin filaments extend from the Z lines (discs)
into the thick filaments and function in the
organization and the alignment of the thin and thick
filaments.
8
A bands
• The A band is a dark band and is
organized into
– (1) thick filaments,
– (2) bare zone,
– (3) an M line,
– (4) a zone of overlap, and
– (5) H zone.
Figure 16.15
Microanatomy of myofibrils. Myofibrils are arranged into I bands and A bands.
A Bands - Thick filaments
• The thick filaments are composed of the contractile
protein myosin.
– A myosin molecule consists of two regions, a tail and a head.
The myosin head binds to the contractile protein actin, and
once bound pivots to produce contractile force. Many myosin
molecules are united to form a thick filament. The myosin
molecules of a thick filament are arranged so that the heads
occupy the end regions leaving a central bare zone.
– In the center of the thick filament a line called the M line joins
adjacent thick filaments.
– A portion of the A band additionally contains thin filaments. The
region where the thin filaments overlap the thick filaments is
called the zone of overlap.
– The region of the A band where the thin filaments are not located
is called the H zone.
I Bands
Figure 16.16
Thick filaments are composed of the contractile protein myosin. A
myosin molecule consists of two regions, a tail and a head. Many
myosin molecules are united to form a thick filament.
Troponin - I Bands
• The I band is the light band and is organized into
–
–
–
–
–
–
–
(1) thin filaments,
(2) G actin,
(3) F actin,
(4) troponin,
(5) tropomyosin,
(6) Z lines.
The thin filaments are composed of the contractile protein
actin. Actin molecules are globular in shape (G actin) and are
organized into filament strands (F actin). Each molecule of actin
has a myosin binding site (an active site).
– A portion of the thin filament extends into the A band forming the
region called the zone of overlap. In a resting fiber, the myosin
binding sites are covered by the troponin-tropomyosin
complex and the overlapping filaments are blocked from
interaction.
• Troponin consists of three subunits.
– One of the subunits binds troponin to tropomyosin
producing the troponin-tropomyosin complex.
– Another subunit binds the troponin-tropomyosin
complex to G actin in a position that causes the
troponin-tropomyosin complex to block the myosin
binding sites (active sites).
– The third subunit binds to calcium ions. In the resting
muscle fiber calcium ions are stored in the terminal
cisternae and this site is open.
9
I Bands
Movement of Troponin-Tropomyosin Complex
• When the terminal cisternae depolarize, calcium ions are
released into the sarcoplasm and bind to troponin.
• Binding of calcium ions to troponin results in a
movement of the troponin-tropomyosin complex
from its blocking position on the myosin binding site
(active site). This allows myosin to bind to actin and
contraction begins.
Figure 16.17
The I band is the light band and is organized into (1) thin filaments,
(2) G actin, (3) F actin, (4) troponin, (5) tropomyosin, (6) Z lines. The
myosin binding sites (active sites) are blocked by the troponintropomyosin complex due to the unavailability of ionic calcium.
Sarcomere
• The sarcomere is the functional unit of
contraction of the muscle fiber.
Figure 16.18
Ionic calcium bonds to troponin resulting the movement of the troponintropomyosin complex from the myosin binding sites (active sites).
Figure 16.19
Availability of ionic
calcium results in the
removal of the blocking
action of troponintropomyosin complexes.
Contraction results in a
shortening of the
sarcomeres as the I
bands decrease in
length as the thin
filaments (actin) are
pulled toward the center
of the A band.
– A sarcomere is the region between adjacent Z
lines (discs).
– Structurally, a sarcomere includes one-half of
an I band, the A band, and one-half of the
adjacent I band. When a fiber contracts, the
myosin (thick filaments) pulls the actin (of the
thin filaments) inward. Thus, the sarcomeres
shorten as the I bands decrease in length.
Innervation of the Muscle
Fiber
Neuromuscular junctions
and
Muscle Spindles
10
Muscle Spindles - Proprioceptors
• Muscle contraction is controlled by the
central nervous system (the brain and
spinal cord) by motor neurons.
– To control muscle contraction the central
nervous system depends upon sensory input
from a class of receptors called
proprioceptors, receptors that receive stimuli
from within the body.
Proprioceptors
• For monitoring muscles, proprioceptors are
commonly located in within muscles, joints, and
in their associated connective tissues.
– Thus, these proprioceptors provide the central
nervous system with information as to the position of
the body’s parts in reference to neighboring parts.
The muscle spindles found scattered among a
muscle’s contractile fibers, in addition to monitoring
contraction, respond to muscle stretch and function in
reflex responses.
Figure 16.21
This preparation (40x) shows both muscle spindles (sensory) and
neuromuscular junctions (motor). Information from muscle spindles and other
proprioceptors is used to determine the position of the body’s parts. Motor
neurons of the central nervous system form unions with skeletal muscles, the
neuromuscular junctions, to control muscle contraction.
Figure 16.20
Muscle contraction is controlled by motor neurons in the central nervous
system, the brain and spinal cord. In order for the central nervous system to
control muscle contraction, it depends upon sensory input from a class of
receptors called proprioceptors.
Lab Activity -3
Proprioceptors – Muscle Spindle
• Observe a slide preparation labeled
“Muscle spindles.”
– Muscle spindles will be observed as small
sensory structures (“specialized fibers”)
located parallel to the long abundant
contractile muscle fibers.
Figure 16.22
A muscle spindle (430x) is shown located among the contractile
muscle fibers. Muscle spindles function as proprioceptors and
additionally respond to stretch and function in reflex responses.
11
Neuromuscular Junction –
Effector Site
• Axons of motor neurons leave the central
nervous system and terminate at muscle fibers
forming specialized unions called neuromuscular
junctions (NMJs).
Figure 16.23
Sensory information from proprioceptors is integrated within the central
nervous system and a response is initiated by motor neurons
Neuromuscular Junction –
Effector Site
• A neuromuscular junction is the union between a
motor neuron and a muscle fiber.
– As the axon from the motor neuron approaches the
plasma membrane (sarcolemma) of the muscle fiber it
forms many branches that end in knob-like structures
called axon terminals.
– Each axon terminal (presynaptic membrane) and its
associated region of the muscle fiber’s plasma
membrane (postsynaptic membrane) forms a
chemical synapse.
– The axon terminals release the neurotransmitter
acetylcholine.
– The postsynaptic membrane houses acetylcholine
receptors (and associated ion channels).
Lab Activity 4
Neuromuscular Junctions
• Observe a slide preparation labeled
“Neuromuscular junctions,” “Myoneural
junctions,” or “Motor end plates.” These
preparations are whole mounts of skeletal
muscle fibers with their associated motor
axons forming unions with the fibers at
neuromuscular junctions.
Figure 16.24
A neuromuscular junction is the union between a motor
neuron and a muscle fiber.
Neuromuscular Junctions
Chemical Synapse
• Neuromuscular junctions are the sites of
chemical synapses between the motor neuron
and the sarcolemma of the muscle fiber. A
synapse is the site of communication between
neurons or neurons and effector cells, such as
muscles and glands.
• A chemical synapse involves the following
components:
– Presynaptic neuron (membrane)
– Synaptic cleft
– Postsynaptic cell (membrane)
12
Neuromuscular Junctions
Chemical Synapse
• Presynaptic neuron (membrane)
– The presynaptic neuron houses a membrane that is
involved in the release of a neurotransmitter. At the
neuromuscular junction, the axon terminals house
presynaptic membrane that is involved in the release
of the neurotransmitter acetylcholine.
• Synaptic cleft
– The synaptic cleft is a space between the presynaptic
membrane and the postsynaptic cell (membrane).
The synaptic cleft is a minute cleft where the
neurotransmitter rapidly diffuses across to the
postsynaptic cell (membrane).
Neuromuscular Junctions
Chemical Synapse
• Postsynaptic cell (membrane)
– The postsynaptic cell (membrane) houses receptors
for the neurotransmitter. When bound with a
neurotransmitter, receptors allow the passage of ions,
thus, changing the transmembrane potential of the
postsynaptic cell. At the neuromuscular junction, the
receptors are located at the postsynaptic membrane.
The receptors bind acetylcholine, which results in the
opening of sodium ion channels. Once the sodium
channels open, sodium ions diffuse from the
extracellular fluid resulting in a depolarization at the
postsynaptic membrane.The depolarization results in
a wave of electrical excitation, an action potential,
that spreads over the sarcolemma.
Neuromuscular Junctions
• Neuromuscular junctions
– Neuromuscular junctions are the unions of the axons of motor
neurons and the muscle fibers. Each neuromuscular junction
consists of numerous synapses formed at each axon terminal
(presynaptic membrane) and its associated plasma membrane
(the sarcolemma of the muscle fiber) the postsynaptic
membrane.
• Axon of motor neuron
Figure 16.25
A neuromuscular junctions is the site of a chemical
synapse between a motor neuron and the
sarcolemma of the muscle fiber.
– Axons of motor neurons are long extensions from the body of the
motor neuron (in central nervous system) that forms unions with
muscle fibers called neuromuscular junctions.
• Axon terminals
– Axon terminals are the specialized ends of an axon. Each axon
terminal forms a portion of a synapse and houses the
presynaptic membrane. Presynaptic membrane releases a
neurotransmitter. At the neuromuscular junction, the
neurotransmitter is acetylcholine(ACh).
Contraction of
Skeletal Muscle Fiber
• Excitation
CONTRACTION OF SKELETAL
MUSCLE FIBER
– Excitation involves the events starting with the arrival
of a stimulus (nerve impulse) at the neuromuscular
junction and ends with the depolarization of the
terminal cisternae, which results in the release of
calcium ions.
• Contraction
Contraction of a skeletal muscle
fiber involves excitationcontraction coupling.
– Contraction begins with the exposure of the myosin
binding (active) sites of actin, the binding of myosin,
and the movement of the (thin filaments) inward
toward the centers of the A bands. This sliding of the
filaments, called the sliding filament theory, explains
how the thin filaments move inward along the thick
filaments.
13
Neuromuscular Junction
Excitation of Sarcolemma
• Motor neurons in the central nervous send
their axons by way of nerves to form
specialized unions with skeletal muscle
fibers called neuromuscular junctions (also
called myoneural junctions, or motor end
plates).
Figure 16.26
Sensory information from proprioceptors is integrated
and analyzed by the central nervous system. Motor
neurons send axons to muscle fibers and form unions
called neuromuscular junctions.
Events at the
Neuromuscular Junction
• Arrival of Action Potential (nerve impulse)
– The arrival of an action potential at an axon terminal
triggers the opening of calcium ion channels within
its plasma membrane.
– Calcium ions diffuse into the axon terminal and
promote the fusion of vesicles and the exocytosis of
the neurotransmitter acetylcholine (ACh).
– Acetylcholine released at the axon terminal’s
presynaptic membrane diffuses across the synaptic
cleft and binds to receptors on the postsynaptic
membrane (of the sarcolemma).
Events at the
Neuromuscular Junction
– The binding of acetylcholine to its receptors results in
the opening of sodium ion channels and the rapid
diffusion of sodium ions into the cell. The inward
movement of sodium ions causes a depolarization of
the postsynaptic membrane, which spreads along
the sarcolemma as an action potential.
– The excitation events at the neuromuscular junction
are rapid and brief. Acetylcholine is rapidly broken
down by the enzyme acetylcholinerase (AChE) and
the synapse is returned to its initial state, ready to
respond to the arrival of another action potential.
Depolarization of
Sarcolemma and T tubules
• Movement of troponin-tropomyosin complex
Figure 16.27
Excitation events begin at the neuromuscular junction with
the arrival of an action potential.
– As the action potential spreads over the sarcolemma, the T
tubules are also depolarized. Depolarization of the T tubules
results in a rapid stimulation of the associated terminal
cisternae (a T tubule and two associated terminal cisternae are
a triad).
– The terminal cisternae respond by releasing calcium ions into
the sarcoplasm.
– Calcium ions bond to troponin, and troponin changes its shape.
– As a result, the troponin-tropomyosin complex moves from its
blocking position on the myosin binding sites (active sites) of
actin. Exposure of the myosin binding sites of actin allows
myosin to bind.
– The interaction of myosin with actin results in the inward sliding
of the thin filaments.
14
Contraction of the
Muscle Fiber
Sliding Filament Theory
Figure 16.28
Excitation results in the removal of the troponin-tropomyosin complex from
blocking the myosin binding sites (active sites) on actin. Exposure of the
myosin binding sites of actin allows myosin to bind. The interaction of
myosin with actin results in the inward sliding of the thin filaments.
Contraction of the Muscle Fiber
• Sliding Filament Theory
•
The sliding filament theory of muscle fiber
contraction states that the thin and thick filaments do not
shorten during contraction. Instead, the filaments slide
past one another. More specifically, the thin filaments
slide inward as the heads (cross-bridges) of the thick
filaments (myosin) pull actin inward.
• A molecule of myosin exists in either a high energy
configuration or a low energy configuration.
Contraction of the Muscle Fiber
Energy of Myosin
• High energy state of myosin
– In the high energy state, myosin has bound with the energy rich
molecule, ATP (ADP and phosphate remain bound at the head).
In this state, the head of myosin is in a position that extends
away from the center of the A band, the M line.
• Low energy state of myosin
– In the low energy state, myosin has reacted with actin, and the
head of myosin has moved (pivoted) to a position toward the
center of the A band, the M line. ADP and phosphate are
released from myosin. The pivoting of the head is an expression
of mechanical energy (derived from the chemical energy in the
breakdown of ATP).
Contraction of the Muscle Fiber
Figure 16.29
The heads (cross-bridges) of
myosin exist in either a high
energy configuration or a low
energy configurations.
• Binding of ATP produces the
high energy configuration, and
the myosin heads are
positioned away from the M
line.
• Binding of the myosin heads
to actin results in the pivoting of
the heads to the low energy
configuration. In this position
the myosin heads are
positioned toward the M line.
• Once the troponin-tropomyosin complex moves away
from its blocking position on actin, the high energy heads
of myosin (cross-bridges) bind to actin, and the process
of the inward sliding of the thin filaments initiated.
• The heads (cross-bridges) of myosin, now attached to
actin, pivot toward the M line (center of the A band). The
pivoting of a myosin head with the associated pulling of
actin (the thin filament) inward toward the M line is called
the power stroke.
• Upon completion of the power stroke and still attached to
actin, the myosin heads are in a low energy
configuration.
• The myosin heads now binds with ATP and capture its
chemical energy.
15
• Utilization of ATP has two results.
– The first result is the detachment of the low energy myosin
heads (cross-bridges) from actin.
– Once detached, the second event, the reactivation of the myosin
heads (cross-bridges) to their high energy state, occurs. The
reactivation of the myosin heads (cross-bridges) results in their
heads facing away from the M line, now ready to bind with actin
that has been pulled into position by the preceding power stroke.
• Binding of high energy myosin heads (cross-bridges),
power strokes, and reactivation of myosin heads (crossbridges) by ATP, will continue until the troponintropomyosin complex moves back to a blocking position
covering the myosin binding sites (active sites) of actin.
Figure 16.30
Contraction begins when high energy
myosin heads (cross-bridges) pull on
actin. Each head produces a power
stroke as it pivots and pulls its
associated actin (thin filament) inward
toward the M line (center of A band).
Binding of high energy myosin heads
(cross-bridges), power strokes, and
reactivation of myosin heads (crossbridges) by ATP, will continue until the
troponin-tropomyosin complex moves
back to a blocking position.
Filament Alignments
• The number of active cross-bridges and the position of
the thin filaments within the A band are two factors that
influence the tension that is produced by a contracting
fiber.
– Maximal tension is produced when a fiber begins contracting
from an alignment established at the normal resting length
(Figure A). This alignment allows maximal cross-bridge
interaction (thin filaments with thick filaments) along with the
maximal inward sliding of the thin filaments.
– When a fiber is in an alignment produced by a strong contraction
(Figure B), the Z lines (discs) contact the ends of the thick
filaments and the thin filaments touch at the M line. This
alignment results in a decrease of muscle tension. A decrease of
muscle tension is also seen when the fiber is in an overextended
alignment due to being stretched (Figure C). Stretching pulls the
thin filaments away from the A band resulting in reduction of
active cross-bridges.
Figure 16.31
Varying the alignment of the thin
filaments within the A bands results
in the production of different
amounts of tension. An alignment
of the thin filament that permits
maximal cross-bridge interaction
along with the maximal inward
sliding of the thin filaments
produces maximal tension. A
reduction in tension is seen in
fibers that are either stretched or
contracted beyond the ideal
operating length.
Relaxation
• Reabsorption of calcium ions into the
sarcoplasmic reticulum (SR), results in low
calcium levels in the sarcoplasm and the
return of the troponin-tropomyosin
complexes to their blocking position. Once
myosin binding sites are blocked, the
muscle fiber is in a state of relaxation.
Figure 16.32
Reabsorption of calcium ions into
the sarcoplasmic reticulum (SR),
results in low levels of calcium in
the sarcoplasm. This results in the
return of the troponin-tropomyosin
complex to its blocking position.
16
Twitch
• The regulation of the concentration of ionic calcium in
the sarcoplasm is essential for the control of muscle
contraction and relaxation. The sarcoplasmic reticulum
continually pumps ionic calcium out of the sarcoplasm
and maintains a low sarcoplasm level. Release of ionic
calcium into the sarcoplasm by stimulation of the
terminal cisternae triggers contraction as calcium ions
bind with troponin resulting in movement of the troponintropomyosin complex from its normal blocking position
on actin.
• Because calcium ions are continually being reabsorbed
by the sarcoplasmic reticulum, a single stimulus (nerve
impulse) produces a brief contractile event unless the
terminal cisternae are stimulated again. A single stimulus
producing a brief single contraction-relaxation of a
muscle fiber is called a twitch. Muscle activity can be
graphically recorded as a tracing called a myogram.
Figure 16.33
Myogram of a “typical” twitch. A twitch
results when a single stimulus produces a
brief single contraction-relaxation of a
muscle fiber.
Twitch – Latent Period
• Latent Period
– The latent period is the time from the arrival of the
nerve impulse at the synapse (a neuromuscular
junction) to the release of calcium from the
sarcoplasmic reticulum. Sequentially, the latent period
involves the following processes:
– (1) begins with the depolarization of the sarcolemma
at the synapse (a neuromuscular junction),
– (2) the spread of the depolarization over the
sarcolemma,
– (3) the depolarization of the T tubules, and the
– (4) stimulation of the terminal cisternae with the
release of calcium ions into the sarcoplasm.
Twitch Velocity
• Not all muscle fibers twitch at the same speed.
Depending upon the physiological aspects of the
fiber, especially the primary way the fiber
catabolizes fuel molecules (glycolysis vs.
aerobic metabolism), the speed of twitches
varies from fast (glycolysis) to slow (aerobic).
– Fast twitch fibers provide rapid movements and are
found, for example, in the extrinsic muscles of the eye
and in the eyelid.
– Intermediate and slow twitch fibers are more fatigue
resistant and are found, for example, in large leg
muscles such as the muscles of the calf (soleus and
gastrocnemius).
Twitch – Contraction Phase
• Contraction Phase
–
–
–
–
The contraction phase begins with the
(1) binding of calcium ions to troponin,
(2) the movement of the troponin-tropomyosin complex, and
(3) continues with the sliding of the thin filaments, which results
from power strokes at the cross-bridges.
• Power strokes are the pivoting of the high energy myosin
heads (cross-bridges) with the pulling of attached actin
molecules (thin filaments) inward toward the M line
(center of A band). Once the heads have pivoted and
pulled actin inward, they are in a low energy position and
binding of ATP to the myosin heads (cross-bridges)
occurs. The utilization of ATP results in the release of
myosin from actin and the reactivation of the myosin
head to its high energy position.
Twitch – Relaxation Phase
• Relaxation Phase
– The relaxation phase begins as calcium ion
reabsorption by the sarcoplasmic reticulum
starts to lower the availability of calcium ions
in the sarcoplasm. As calcium ions begin to
dissociate from troponin, the troponintropomyosin complexes begin to move back
into blocking the binding sites (the active
sites) on actin. The relaxation phase
continues until the blocking of the active sites
on actin returns the muscle fiber to its original
resting state.
17
Muscle Responses
Varying the Contraction by Motor
Unit Recruitment
Figure 16.34
Myogram showing the relative speed of twitches
of different muscles. Depending upon the
physiological aspects of the fiber, especially the
amount and rate of enzyme activity, the speed of
twitches varies from slow to fast.
Varying the Contraction by Motor
Unit Recruitment
• Varying the degree of muscle contraction, called
a graded response, is important in producing
the required contraction for a movement. One
way a muscle’s response is graded is by the
nervous system recruiting more muscle fibers
into the contractile event (movement).
– The axon from the cell body of a motor neuron in the
central nervous system may branch and innervate
from a few to many muscle fibers. Each motor neuron
and the muscle fibers it innervates are called a motor
unit. In a contractile response of a muscle, increasing
the number of contracting motor units increases the
tension of the muscle.
Varying the Contraction by Motor
Unit Recruitment
•
The following myogram supports the relationship between
increasing the number of stimulated fibers and muscle tension. The
myogram shows the effect of stimulating a muscle with increasing
voltages.
– As voltage is increased from zero, a voltage is reached where the most
irritable fibers of the muscle contract.
– The voltage that produces the initial contraction is the threshold stimulus
(voltage). Any voltage stimuli that are less than threshold is a
subthreshold stimulus and does not produce a contraction.
– As the voltage of the stimuli is increased above the threshold, muscle
contractions show increasing tension. Increasing voltage stimulates
more and more of the muscle’s fibers until all fibers are stimulated.
– At the point of stimulation where all of the muscle’s fibers are stimulated
the muscle produces maximal tension. The voltage that produces
maximal tension is the maximal stimulus.
– Increasing the voltage beyond this point has no effect on the tension of
the muscle’s contraction as all fibers have already been stimulated.
Lab Activity 5
Neuromuscular Junctions
Figure 16.35
Myogram showing the relationship
between increasing the number of muscle
fibers and increased muscle tension.
• Observe a slide preparation labeled
“Neuromuscular junctions,” “Myoneural
junctions,” or “Motor end plates.” These
preparations are whole mounts of skeletal
muscle fibers with their associated motor
axons forming unions with muscle fibers at
neuromuscular junctions.
18
Lab Activity 5
Neuromuscular Junctions
• As the motor axons enter the muscle many
branches of the axons can be observed. Follow
an axon as it branches, each branch forming a
neuromuscular junctions with a different muscle
fiber.
Figure 16.36
A motor unit consists of a motor neuron and the
muscle fibers it innervates. Recruitment of motor
units increases the force of contraction.
– A motor neuron and the muscle fibers it innervates
are called a motor unit. Success with identification of
motor units depends upon the quality of the slide
preparation, especially, the presence of long
branching motor axons.
Treppe- Staircase Effect or
Staircase Phenomenon
Figure 16.37
Muscle fibers showing organization into motor units. Notice
that in this preparation, each fiber receives only one
neuromuscular junction and from only one motor unit.
• Treppe is a progressive series of increasing
stronger contractions of a resting muscle, where
each contraction results from a stimulus of the
same intensity.
• . Treppe results from the increased ability of the
muscle’s fibers to respond to subsequent stimuli
due to the (1) increased efficiency of enzyme
systems, (2) increased calcium ion availability,
and (3) increased heat.
Isotonic and Isometric
Contractions
Figure 16.38
Myogram of treppe showing the effect of stimulating a muscle with
stimuli of the same intensity and applying each stimulus immediately
after the muscle has completed each relaxation phase.
19
Isotonic Contraction
• An isotonic muscle contraction is a contraction
that results in a change of the length of the
muscle along with movement of the load. In an
isotonic contraction, once the muscle has
developed the tension required to move the load
(overcomes resistance), the tension remains
constant throughout the contraction.
• There are two types of isotonic contractions:
• (1) concentric and
• (2) eccentric.
Concentric Isotonic Contraction
• A concentric contraction is a contraction
that results in the shortening of the muscle
along with the movement of the load.
– An example of concentric contraction is seen
in an arm-wrestling match as the winning
person moves the opponent’s arm toward the
top of the table.
Eccentric Isotonic Contraction
• An eccentric contraction is a contraction that
occurs while a muscle lengthens. In an eccentric
contraction the muscle does not develop enough
tension to overcome the load (resistance). Thus,
even though the muscle is contracting, it is
lengthening because the load, such as a
stronger contracting muscle, is stretching the
muscle.
Figure 16.39
A concentric isotonic contraction produces tension that
overcomes the resistance (load). The muscle shortens with its
tension remaining constant throughout the contraction.
– An example of eccentric contraction is seen in an
arm-wrestling match as the losing person’s arm is
being pushed toward the table top. The losing person
cannot overcome the resistance (opponent) and their
contracting muscle lengthens as it moves toward the
table top.
Isometric Contraction
• An isometric contraction is a contraction
where the muscle does not change length
because it does not develop enough
tension to overcome the resistance (load).
– An example of concentric contraction is seen
in an arm-wrestling match when the arms of
the two opponents are locked in a fixed
position, as neither person can overcome the
opposing resistance.
Figure 16.40
A eccentric isotonic contraction produces tension but cannot
overcome the resistance (load). The muscle lengthens while its
tension remains constant throughout the contraction
20
Muscle Responses
Varying the Contraction by
Frequency of Stimulation
Figure 16.41
An isometric contraction is a contraction where the muscle
does not change length as it does not develop enough
tension to overcome the resistance (load).
Varying the Contraction by
Frequency of Stimulation
• In addition to motor unit recruitment,
another way muscle contraction can be
graded (varied) is to change the frequency
(rate) of muscle stimulation.
– The frequency (rate) of muscle stimulation
varies from producing a brief single
contraction to a sustained forceful contraction
called tetanus.
Wave Summation
• If another stimulus is applied in rapid succession
to a muscle (after the refractory period), the
muscle will immediately enter another phase of
contraction. The following contraction produces
more tension than the preceding contraction.
– Thus, the fiber is maintained in a state of contraction
for a longer period of time. This maintenance of
tension due to the rapid succession of stimuli is called
wave (temporal) summation.
Wave Summation (summation of
twitches) and Tetanus
• A twitch is the single brief contraction of a muscle fiber
(cell) that results from a single stimulus. Since the
functional units of whole muscles are muscle fibers
(cells) the term twitch can be expanded and used in
reference to the contraction of a whole muscle. This is
especially useful in laboratory studies when the
contractions of whole muscles are studied by applying
controlled (voltage and frequency) electrical stimuli.
Thus, in the following descriptions reference is to whole
muscles because whole muscles exhibit the contractile
characteristics of the individual fibers (cells).
Incomplete Tetanus
• Incomplete tetanus (incomplete wave
summation) is produced by rapid successive
contraction-relaxation phases of the muscle.
Incomplete tetanus is characterized by as
sustained contraction with the muscle quivering
as it rapidly undergoes contraction phases, each
followed by a brief relaxation phase.
– If the frequency of successive stimuli is increased, the
phases of relaxation continue to shorten and finally
disappear as the muscle enters complete tetanus, or
a sustained contraction.
21
Complete Tetanus
• Complete tetanus results when the stimuli
arrive at a frequency (rate) that does not
allow relaxation. In complete tetanus
stimuli are arriving so quickly that the
sarcoplasmic reticulum does not have time
to reabsorb calcium ions.
– Calcium levels remain high resulting in
maximal unblocking of actin and myosin
(cross-bridge) interactions.
Figure 16.42
Myograms showing
how a muscle can
be modified into a
sustained
contraction by
increasing the
frequency (rate) of
stimuli.
Lab Activity 6Increasing Frequency of Stimulation
• Frog Gastrocnemius Muscle
– Because laboratories are supplied with a
variety of instrumentation for the stimulation
and recording of muscle contraction, the topic
of instrumentation and setup is not covered.
This activity is limited to the interpretation of
typical myograms from muscle stimulation
and contraction exercises.
Figure 16.43
Myogram of a frog gastrocnemius muscle showing the
effect of increasing the frequency (rate) of stimulation.
MUSCLE ENERGETICS
Figure 16.44
Myogram from an isolated frog gastrocnemius muscle
showing the effect of increasing and the frequency of
stimulation and resulting muscle fatigue.
Muscle Fiber - Resting
The sources of energy for
resting muscle fibers include fatty
acids and glucose.
22
Fatty Acids
Fatty Acids
Fatty acid catabolism provides most of the energy (about
95%) for the resting muscle cell. Fatty acids from the
blood enter the sarcoplasm (cytoplasm) of the muscle
cell. Then they enter into the mitochondria where their
energy is used in the TCA (tricarboxylic acid cycle), or
Krebs cycle, and the electron transport system to drive
the reaction ADP + Pi –> ATP. In the final step of
mitochondrial catabolism, oxygen is combined with
protons (hydrogen ions) and electrons to form water.
• Thus, because oxygen is used in this phase of
catabolism, it is aerobic metabolism. In this process of
ATP production carbon dioxide and water are produced
as waste products.
• A small quantity of ATP produced in a resting
muscle fiber remains in the sarcoplasm and is
considered “stored” ATP. Stored ATP is an
immediate source of energy, especially for a
quick response in muscle contraction.
• ATP is also used in the formation of energy rich
creatine phosphate (ATP + creatine –> ADP +
creatine phosphate).
– Creatine, a product formed from the amino acids
arginine and glycine, is phosphorylated (through the
action of the enzyme creatine phosphokinase) to
produce the high energy molecule creatine
phosphate.
Glucose
• Another source of energy for resting muscle
cells is glucose. However, the major utilization of
glucose is in the production of glycogen.
– Glycogen is produced by combining molecules of
glucose into long branching chains. Thus, glycogen is
a polysaccharide stored in the sarcoplasm of the
muscle cell, and is used as a source of energy during
a muscle fiber’s rapid response and in prolonged
exercise.
Figure 16.45
In a resting muscle fiber, the major source of energy for the
production of ATP is from the catabolism of fatty acids. A small
amount of ATP is stored. Additionally, ATP is used to form stored
sources of energy, glycogen and creatine phosphate.
Muscle Fiber - Moderate Prolonged
Activity
•
MUSCLE ENERGETICS
Muscle Fiber –
Moderate Prolonged Activity
As a muscle fiber begins contraction, any
stored ATP is immediately utilized. The
catabolism of fatty acids continues, but
cannot provide the required amount of ATP.
• Two other sources of energy are catabolized to
meet higher energy requirements
– creatine phosphate and
– glucose.
23
Moderate Prolonged Activity
Creatine Phosphate and Glucose
• Creatine Phosphate
– Creatine phosphate, found stored in the sarcoplasm, is broken
down to creatine with the transfer of phosphate to ADP, forming
energy rich ATP. Because the amount of stored creatine
phosphate is small, this source of energy is rapidly depleted.
Oxidation of glucose provides prolonged ATP production.
• Glucose
– Glucose is delivered by the blood and derived from the
catabolism of glycogen stored in the sarcoplasm. Glucose is
catabolized in two pathways, anaerobically in the cytoplasm by
glycolysis and aerobically in the mitochondria (TCA & ETS).
Glycolysis (anaerobic) produces pyruvic acid and a small
amount of ATP (2 ATP per glucose molecule). Pyruvic acid is
modified and enters into the mitochondria where its oxidation
produces considerable amounts of ATP (34 ATP per glucose
molecule) to sustain muscle contraction.
Figure 16.46
A muscle fiber in moderate activity relies first upon creatine
phosphate as a source of energy. As the contraction becomes more
prolonged, glucose is oxidized. Glucose is delivered by the blood and
from glycogen stored in the sarcoplasm.
Muscle Fiber - Peak Activity
• As increased energy demands are placed upon
the muscle, glucose remains the prime source
of energy. The difference between the fiber in
moderate prolonged activity and peak activity is
between the speeds of glycolysis (anaerobic)
and mitochondrial (aerobic) oxidation (TCA &
ETS).
– As energy demands increase the rate of glycolysis
can increase to about 100x faster than that of aerobic
oxidation. Thus, even though glycolysis produces only
2 ATP for each glucose molecule, the rate of
production produces a large amount of ATP. Pyruvic
acid that is not destined to enter the mitochondria for
oxidation is converted to lactic acid (or lactate).
MUSCLE ENERGETICS
Muscle Fiber –
Peak Activity
MUSCLE ENERGETICS and
TYPES OF FIBERS
Type I and Type II Fibers
Figure 16.47
Increased energy requirements shift the catabolism of
glucose to glycolysis. Even though glycolysis produces
only 2 ATP for each glucose molecule, the rate of
production produces a large amount of ATP.
24
TYPES OF FIBERS
• Muscle fibers are generally classified into two categories,
Type I and Type II. The primary source of fuel for both
types of fibers in moderate and peak contraction is
glucose. However, differences in glucose catabolism are
seen in number of mitochondria and the fiber’s
preference for either the aerobic or anaerobic pathway.
• Type I fibers
– Type I fibers are also called slow-twitch red fibers. They have
abundant mitochondria and depend mostly upon the aerobic
(mitochondrial) pathway of glucose oxidation. The fibers are rich
in myoglobin, which serves as an intracellular oxygen source.
Type I fibers are resistant to fatigue.
• Type II fibers
– Type II fibers are also called fast-twitch white fibers. They
have relatively few mitochondria and depend mostly upon the
anaerobic (glycolytic) pathway of glucose oxidation. Rich in
stored glycogen to provide glucose for glycolysis, they produce
abundant ATP rapidly. The fibers are low in myoglobin. Type II
fibers fatigue quickly.
Figure 16.48
This slide preparation of muscle fibers in cross section is stained for glycogen.
Glycogen is abundant in Type II fibers. Type II fibers depend mostly on glycolysis to
produce abundant ATP necessary for brief rapid movement. Type II fibers, low in
myoglobin, are also called fast-twitch white fibers. Type I fibers are low in glycogen
and are not darkly stained. Type I fibers mostly depend upon the aerobic oxidation of
glucose. Type I fibers, rich in myoglobin, are also called slow-twitch red fibers. Their
sustained contractions are resistant to fatigue.
SMOOTH MUSCLE TISSUE
•
SMOOTH MUSCLE TISSUE
Smooth muscle tissue is formed
from smooth muscle fibers.
Smooth muscle tissue is formed from smooth
muscle fibers. Its name, smooth muscle,
describes the muscle’s appearance;
– its fibers lack the striations (cross-bands) seen in both
skeletal and cardiac muscles.
– Smooth muscle fibers are spindle-shaped (round with
tapered ends), each fiber with a single central
nucleus.
Smooth Muscle
• Smooth muscle contains both thin and thick filaments.
– The thin filaments of actin overlap the thick filaments of myosin.
– The filaments are not organized into myofibrils as in skeletal and
cardiac muscle. In smooth muscle fibers, the thin filaments are
associated with intermediate filaments.
– The intermediate filaments are organized in a spiral-like network
within the cell. The intermediate filaments associate with the
sarcolemma at sites called dense bodies. Thus, when a smooth
muscle contracts, tension from the interaction of the thin and
thick filaments is transmitted from the thin filaments through the
intermediate fibers, to the dense bodies, to the surrounding
connective tissue (endomysium).
– During stretch the intermediate filaments are reorganized
(unspiral) and the thin and thick filaments are not separated
(within limits). This feature of reorganization gives smooth
muscle the ability to be increasingly stretched without greatly
reducing the ability to generate tension.
Figure 16.49
In smooth muscle fibers, the thin filaments are associated with
intermediate filaments. The intermediate fibers are organized in a
spiral-like network within the cell. The intermediate fibers associate
with the sarcolemma at sites called dense bodies.
25
Single-unit (Visceral)
Smooth Muscle
• In single-unit smooth muscle large groups of fibers are
organized to function as a single unit.
– This type of smooth muscle tissue is mostly found in the walls of
the body’s internal organs (except the heart). When found in this
location, the smooth muscle is called visceral (viscus, an internal
organ of the body) smooth muscle. In the walls of the internal
organs of most of the digestive, respiratory, urinary, and
reproductive tracts, smooth muscle forms muscular sheets.
– Usually, the walls contain two adjacent smooth muscle sheets
that are at right angles. One sheet of smooth muscle is called the
longitudinal layer as the cells are located parallel to the long axis
of the organ. Contraction of this layer shortens the organ and
causes a dilation of its internal cavity. The other sheet of smooth
muscle is called the circular layer as the cells are located around
the circumference of the organ. Contraction of this layer
lengthens the organ and causes a constriction of its internal
cavity.
Figure 16.50
Single-unit (visceral) smooth muscle is found in areas controlled by
single-unit contractions, such as shown in this photograph of a cross
section of the esophagus. The smooth muscle is organized into two
distinctive layers, an inner circular layer and an outer longitudinal layer.
In the digestive tract, large groups of smooth muscle fibers contract as
single-units producing wave-like contractions called peristaltic waves.
Multi-unit Smooth Muscle
• Multi-unit smooth muscle is organized to function
individually as many multiple units.
– Multi-unit smooth muscle is commonly found in areas
where smooth muscle precisely controls contraction.
The locations of multi-unit smooth muscle include the
iris of the eye, large arteries, large airways, and the
arrector pili muscles (contraction produces goose
bumps).
– Multi-unit smooth muscle consists of groups of fibers
(multiple units) organized as motor units. Mostly
under direct controlled of the autonomic nervous
system, the recruitment of motor units is used to
control the amount of tension produced by the
muscle’s contraction.
Figure 16.51
Multi-unit smooth muscle is found in areas that require precise control,
such as shown in this photograph of a section of the iris of the eye.
Motor units of the iris adjust the pupil and precisely regulate the amount
of light entering the eyeball.
Lab Activity 7
Smooth Muscle (Single Unit)
•
Observe a slide preparation labeled “Smooth Muscle,”
or “Visceral Smooth Muscle.” Slides of smooth muscle
are usually made from preparations of the small intestine
(or other organ of the digestive tract). Smooth muscle
fibers from the digestive tract are usually organized into
two muscular sheets, an inner circular layer and an outer
longitudinal layer. In cross sections of organs, the inner
circular layer shows the muscle fibers exposed along
their long axis, and the outer longitudinal layer shows the
muscle fibers sectioned across their long axis (fibers are
cross sectioned).
Figure 16.52
Smooth muscle (100x) lacks striations and is organized into muscular sheets
that surround or enclose many of the body’s organs. This sketch shows the
details of smooth muscle fibers from the circular layer muscle layer of the
digestive tract. Preparations of “Teased Smooth Muscle” show the structure of
the individual fibers.
26
Figure 16.53
Smooth muscle from the circular layer of the small
intestine. The cells function in large single units to
produce wavelike contractions called peristaltic waves.
Figure 16.54
Preparations of teased smooth muscle show
the fibers to be long, spindle shaped,
uninucleate, and nonstriated.
Characteristics of Smooth Muscle
• Structurally and functionally smooth muscle fibers are
very different from skeletal muscle fibers.
Characteristics of Smooth
Muscle
– The most obvious difference between smooth muscle and
skeletal muscle is in the arrangement of the thin and thick
filaments. In smooth muscle the thin and thick filaments are not
organized into sarcomere containing myofibrils as in skeletal
muscle. Instead, the thin and thick filaments are arranged
diagonally to the long axis of the cell.
– Groups of thin filaments are anchored to noncontractile
cytoskeletal elements called intermediate filaments. Intermediate
filaments attach to areas called dense bodies that are associated
with the sarcolemma.
– Thus, tension produced by the interaction between the thin
(actin) and thick (myosin) filaments is transferred through
intermediate filaments to the sarcolemma, to the surrounding
connective tissue (endomysium).
Contraction of Smooth Muscle
Figure 16.55
Comparisons
between smooth
muscle and skeletal
muscle.
27
Contraction of Smooth Muscle
• Contraction of smooth muscle is similar to
contraction of skeletal muscle in that both
– (1) have the contractile proteins (actin and myosin),
– (2) increased levels of ionic calcium in the sarcoplasm
initiates contraction,
– (3) ATP provides the source of energy for energizing
the myosin heads (cross-bridges), and
– (4) low levels of ionic calcium terminates contraction.
Contraction of Smooth Muscle
• Calcium ions bind to the protein calmodulin and forms a
calcium-calmodulin complex. This complex activates an
enzyme called myosin light chain kinase (MLCK). This
enzyme catalyzes the transfer of phosphate from ATP to
the light chain region of the myosin head, thus,
producing high energy myosin.
• Contraction begins when high energy myosin binds with
actin and results in actin (thin filaments) sliding inward.
The concentration of intracellular calcium and, thus, the
degree of contraction is determined by the balance
between intracellular ionic calcium and its active
transport out of the sarcoplasm.
Contraction of Smooth Muscle
• Contraction of smooth muscle may be initiated
by
– (1) stretching of the fibers,
– (2) electrical depolarization, or
– (3) local chemical stimuli.
• All initiators of contraction lead to an increase of
intracellular calcium. Calcium is delivered mostly
by way of calcium channels from the
extracellular fluid. Additionally, some ionic
calcium is from intracellular delivery from the
sarcoplasmic reticulum.
Contraction of Smooth Muscle
• Active calcium ion pumps, which remove
calcium ions from the sarcoplasm, are
associated with both the sarcolemma and
sarcoplasmic reticulum. Each moves calcium
ions back into its respective locations.
• Contraction ends when calcium ions
concentration is reduced to its original level.
Features of Smooth Muscle
Figure 16.56
Sequence of events in the contraction of smooth muscle.
Most calcium ion delivery is from the extracellular
environment. Contraction ends when calcium ion
concentration is reduced to its original level.
28
Stress-relaxation Response
• Smooth muscle exhibits a stress-relaxation
response. This response is characterized by
relaxation of the muscle after being stretched.
– This response allows reduction of tension in organs
such as the stomach and urinary bladder that stretch
upon filling. Relaxation allows the organs to stretch
further and allows their contents to remain in storage
until the muscle is stimulated to contract. The stressrelaxation response is mostly mediated by the
diagonal and overlapping contractile filaments. During
stretch the filaments are rearranged allowing
reduction in tension with the maintenance of the
cross-bridges
Length and Tension Changes
• Because of the rearrangement (not separation)
of the thin and thick filaments during stretching
of the fiber, the thin and thick filaments maintain
their ability to interact.
– Smooth muscle can be stretched to about four times
its length and still produce considerable tension.
CARDIAC MUSCLE
• Cardiac fibers form the myocardium (heart
muscle).
CARDIAC MUSCLE
Cardiac fibers form the
myocardium (heart muscle).
– The rod-like fibers are short,
– striated,
– mostly uninucleate (some are binucleate),
– and form chains (as the individual fibers are
joined end-to-end at intercalated discs) that
branch.
Cardiac Muscle
Intercalated Discs
• Compared to skeletal muscle the T tubules are shorter
and do not form triads because the sarcoplasmic
reticulum does not have terminal cisternae. Like skeletal
muscle, contraction is dependent upon the presence of
calcium ions.
• Calcium ions bond to troponin resulting in exposure of
actin (thin filaments). Like skeletal muscle, depolarization
of the fiber triggers the release of calcium ions from the
sarcoplasmic reticulum. However, like smooth muscle
depolarization opens calcium ion channels in the
sarcolemma allowing a greater influx of calcium ions
than supplied by the sarcoplasmic reticulum. Like
smooth muscle, contraction is terminated by the removal
of calcium ions back into the sarcoplasmic reticulum and
the extracellular environment.
• Intercalated discs are unique to cardiac muscle.
They are formed at adjacent ends of cardiac
muscle fibers by the close association of the two
fibers plasma membranes. Intercalated discs
house gap junctions and desmosomes.
– Gap junctions allow the transmission of small ions
and function as a direct electrical connection.
– Desmosomes are junctions that provide mechanical
connections between adjacent fibers. Thus,
depolarization, contraction, and the transmission of
tension involve all of the junctioned fibers in the
myocardium.
29
Pacemaker Fibers
• The heart houses a group of self-excitable fibers
called the heart’s “pacemaker.” The pacemaker
cells undergo spontaneous depolarization.
– However, the rate of their depolarization is controlled
by the autonomic nervous system. Thus,
neuromuscular junctions are present only where
neural regulation occurs.
– Depolarization spreads from the pacemaker fibers to
adjacent cardiac fibers through gap junctions.
Figure 16.57
Cardiac muscle fibers form the myocardium (heart
muscle). The rod-like fibers are short, striated, and are
mostly uninucleate. Fibers are joined end-to-end at
specialized sites called intercalated discs. Intercalated
discs contain jap junctions and desmosomes and
organized the fibers into long chains that show
extensive branching.
Lab Activity 8
Cardiac Muscle
• Observe a tissue preparation labeled
“Cardiac Muscle,” or “Muscle, three types.”
Identify the branched cardiac fibers and
the darkly stained intercalated disks.
Figure 16.58
Comparisons
between cardiac
muscle and skeletal
muscle.
Figure 16.59
Cardiac muscle tissue consists of branching
cells that are joined at end-to-end junctions
called intercalated discs.
Figure 16.60
Cardiac muscle tissue consists of branching cells
that are joined at end-to-end junctions called
intercalated discs.
30