Required CMS Contract Clauses
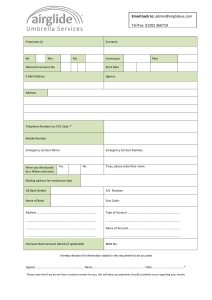
advertisement

Required CMS Contract Clauses Revised 8/28/14 – CMS MCM Guidance Chapter 21 The following provisions are required to be incorporated into all contracts with first tier, downstream, or related entities as defined in 42 CFR 422 and 423 et seq.: 1. Independent Contractor acknowledges to the best of its knowledge, information and belief, there are no past or pending investigations, legal actions, or matters subject to arbitration involving Independent Contractor or any of its employees, contractors, Governing Body members, Downstream Entities, or any major shareholders (5% or more) on matters relating to payments from governmental entities, both federal and state, for health care and/or prescription drug services. 2. Independent Contractor acknowledges to the best of its knowledge, information, and belief that neither Independent Contractor nor any of its employees, contractors, Governing Body members, Downstream Entities, or any major shareholders (5% or more) have been criminally convicted nor has a civil judgment been entered against them for fraudulent activities nor are they sanctioned under any Federal program involving the provision of health care and/or prescription drug services. 3. Independent Contractor acknowledges to the best of its knowledge, information and belief, that neither Independent Contractor nor any of its employees, contractors, Governing Body members, Downstream Entities, or any major shareholders (5% or more) appear in the list of excluded individuals/entities as published by the Department of Health and Human Services (DHHS) Office of the Inspector General (OIG List), nor in the list of debarred contractors as published in the System for Award Management by the General Services Administration (GSA List). 4. Independent Contractor agrees that it shall review the OIG List and the GSA List prior to the hiring of any new employees, contractors, or Governing Body members. Independent Contractor also agrees that it shall, on a monthly basis, for all employees, contractors, Governing Body members, Downstream Entities, and major shareholders (5% or more) review the OIG and GSA Lists to ensure that none of these persons or entities are excluded or become excluded from participation in Federal programs. 5. Independent Contractor is obligated to notify BCBSM immediately to the best of its knowledge, information, and belief of any change in circumstances occurring after the Effective Date of this Medicare Advantage Addendum which would require Independent Contractor to then respond affirmatively to any of the questions posed in paragraphs 1, 2 and 3 of this Medicare Advantage Addendum. 6. Independent Contractor shall, and shall require its Downstream Entities to, annually attest to compliance with Sections 1 through 4 above. BCBSM reserves the right to audit Independent Contractor or its Downstream Entities for compliance and/or to request verification that employees, contractors, Governing Body members, Downstream Entities, and major shareholders have been checked against the OIG and GSA Lists on a monthly basis. Independent Contractor agrees to provide BCBSM with any information necessary for BCBSM to conduct checks of the OIG and GSA Lists for Independent Contractor’s employees, contractors, Governing Body members, Downstream Entities, and major shareholders (5% or more); or otherwise assist BCBSM in documenting compliance with this provision, including but not limited to, supplying attestations as required in this Section. 7. Independent Contractor shall require its subcontractors, agents or other Downstream Entities to provide reasonable assurance as evidenced by written contract that such subcontractor, agent or other Downstream Entity shall comply with the same Medicare Advantage program requirements and obligations that are applicable to Independent Contractor under this Medicare Advantage Addendum. Page 1 of 7 8. Notwithstanding any relationships that BCBSM may have with first tier, downstream, and related entities, BCBSM maintains ultimate responsibility for adhering to and otherwise fully complying with all terms and conditions of its contract with CMS. Independent Contractor shall participate in and comply with BCBSM’s oversight program, including but not limited to, attending meetings; providing attestations; responding to document, policy, and procedure review requests; implementing corrective action plans suggested by BCBSM or CMS; participating in monitoring and reviews; and providing BCBSM with similar information about Independent Contractor’s Downstream Entities. 9. Independent Contractor shall give any authorized local, state, or federal government agency, including without limitation BCBSM, the U.S. Department of Health and Human Services (“HHS”), U.S. General Accounting Office (“GAO”), the Comptroller General, Centers for Medicare and Medicaid Services (“CMS”), and their authorized designees, the right to audit, evaluate, collect directly from, and inspect any books; contracts; computer or other electronic systems; records, including medical records and documentation; patient care documentation; and other records of the first tier, downstream and related entities involving transactions related to CMS’ contract with BCBSM. This right will exist through ten (10) years from the final date of the contract period or from the date of completion of any audit, whichever is later. Independent Contractor also agrees to maintain such records for a period of ten (10) years following termination or expiration of this Medicare Advantage Addendum, or until completion of an audit, whichever is later. Independent Contractor shall produce such records directly to the requesting entity. Independent Contractor shall document and take appropriate corrective actions in response to any potential noncompliance or potential Fraud, Waste and Abuse (FWA) identified via audit, monitoring or otherwise, by BCBSM, HHS, GAO, or CMS. Independent Contractor shall allow BCBSM, HHS, GAO and/or CMS to oversee its documentation and implementation of corrective actions. 10. Independent Contractor is prohibited from holding an enrollee liable for payment of any fees that are the obligation of BCBSM. 11. To the extent Independent Contractor performs any of the following functions, it will do so in accordance with 42 CFR Parts 422 and 423 and BCBSM’s policies and procedures, which shall be consistent with and comply with BCBSM’s contractual obligations to CMS. a. Provision of benefits / health care services delivery b. Bid preparation c. Enrollment / disenrollment / applications processing / outbound enrollment verification / coordination with other benefit programs like Medicaid, state pharmaceutical assistance programs or other coordination of benefits d. Coverage determinations, grievance and appeals e. Claims processing / claims adjudication / determination of payment amounts f. Reconciliation of benefit liabilities g. Quality review / quality improvement h. Marketing & sales i. Data reporting j. Member servicing k. Disease / case / care management l. Network contracting / credentialing / licensing / network management m. Pharmacy benefit management n. Oversight, negotiation and/or management of prescription drug rebates, discounts and price concessions o. Administration and tracking of drug benefits, including TrOOP (True Out of Pocket) balance processing p. Compliance Program functions, including hotline operations q. Utilization management / retrospective claim audits / claim reviews Page 2 of 7 12. BCBSM retains the right to revoke the activities and reporting requirements delegated to Independent Contractor and/or its Downstream Entities, or to terminate this Medicare Advantage Addendum, in instances where BCBSM or CMS determine that either Independent Contractor or its Downstream Entities have not performed satisfactorily. 13. If Independent Contractor generates data to determine payment on behalf of BCBSM, then Independent Contractor must certify (based on best knowledge, information and belief) the accuracy, completeness, and truthfulness of the data. 14. BCBSM may only delegate activities or functions to Independent Contractor in a manner consistent with the requirements set forth in 42 CFR 422.504(i)(4). 15. BCBSM has delegated to Independent Contractor the activities and reporting responsibilities set forth in the applicable active and legally binding master agreement(s) and schedules and/or other contracts, including statements of work. 16. Consistent with the terms of any Master Agreement or Health Insurance Portability and Accountability Act of 1996 (HIPAA) Business Associate Agreement, Independent Contractor agrees to: a. Abide by all federal and state laws regarding confidentiality and disclosure of medical records, or other health and enrollment information. Independent Contractor must safeguard the privacy of any information that identifies a particular enrollee and have procedures that specify: i. For what purposes the information will be used within the organization; and ii. To whom and for what purposes it will disclose the information outside the organization. b. Ensure that medical information is released only in accordance with applicable federal or state law, or pursuant to court orders or subpoenas. c. Maintain the records and information in an accurate and timely manner. d. Ensure timely access by enrollees to the records and information that pertain to them. 17. Independent Contractor agrees to incorporate into this Medicare Advantage Addendum such other terms and conditions as CMS may find necessary and appropriate, including amendments to CMS rules, regulations and guidance. Independent Contractor also agrees to incorporate into its Downstream Entity contracts all terms and conditions contained herein. 18. Independent Contractor shall have a compliance plan that consists of (1) measures to detect, correct, and prevent fraud, waste, and abuse; (2) written policies, procedures, and standards of conduct articulating Independent Contractor’s commitment to comply with all applicable Federal and State standards; (3) the designation of a compliance officer and compliance committee accountable to senior management and responsible for high level oversight of Independent Contractor’s compliance plan; (4) effective training and education for Independent Contractor’s compliance officer and Independent Contractor’s employees, Governing Body members, and Downstream Entities, including training on fraud, waste and abuse; (5) effective lines of communication between the compliance officer and BCBSM, and the compliance officer and Independent Contractor’s employees, Governing Body members, and Downstream Entities; Page 3 of 7 (6) enforcement of standards through well-publicized disciplinary actions; (7) procedures for effective and routine internal monitoring and auditing; and (8) procedures for ensuring prompt responses to detected offenses and development of corrective action initiatives related to any evidence of fraud or misconduct. 19. Independent Contractor agrees to complete the Fraud, Waste, and Abuse (FWA) and general compliance training modules, available at the Medicare Learning Network, and provide to BCBSM, upon request, certificates of completion validating its compliance with the requirements set forth at 42 CFR 422.503(b)(4)(vi). 20. Independent Contractor shall allow BCBSM to maintain appropriate oversight of Independent Contractor’s training efforts under its compliance plan as BCBSM maintains ultimate responsibility for compliance training. Independent Contractor shall attest to BCBSM annually that it meets the requirements identified in this Section and has conducted compliance training in accordance with its compliance plan. Independent Contractor shall maintain training records for a period of ten (10) years. Such records shall include attendance, topic, certificates of completion (if applicable), and test scores of any tests administered. Independent Contractor shall provide BCBSM and/or CMS with training logs and other materials related to training upon request by BCBSM and/or CMS. 21. Independent Contractor shall, and shall require its Downstream Entities to, within five (5) business days of becoming aware of an actual, suspected or potential compliance concern or actual, suspected or potential fraud, waste and abuse by Independent Contractor, its Governing Body members, employees, contractors, agents, or Downstream Entities, report such compliance and FWA concerns to BCBSM. These reports may be made to the BCBSM Contract Administrator or by contacting the BCBSM Medicare Anti-Fraud Hotline at (888) 650-8136 or TTY (800) 588-2711. Reports may also be submitted to: Fraud Investigations Unit, Blue Cross and Blue Shield of Michigan, 600 E. Lafayette Blvd., Detroit, MI 48226. 22. Independent Contractor shall protect against retaliation for reporting of such compliance and fraud, waste, and abuse concerns. Independent Contractor shall ensure that these reporting requirements and its non-retaliation policy are well publicized. 23. Independent Contractor shall coordinate with BCBSM to (a) timely investigate the compliance or FWA concern, (b) mitigate the compliance or FWA concern, and (c) implement appropriate corrective actions. 24. Independent Contractor shall monitor and audit its Downstream Entities to ensure that they are in compliance with all applicable laws, regulations, and contractual requirements, including compliance with these Medicare Advantage provisions. If Independent Contractor determines its Downstream Entity requires corrective action(s), Independent Contractor shall ensure that such corrective action(s) are taken by its Downstream Entity. Independent Contractor shall provide information about its Downstream Entity oversight, including any corrective action plans, to BCBSM upon request. 25. Payments from BCBSM to Independent Contractor are made, in whole or in part, from Federal funds, and subject Independent Contractor to all laws applicable to the individuals or entities who receive Federal funds, including the False Claims Act (32 USC 3729, et. seq.), the Anti- Page 4 of 7 Kickback Statute (section 1128B (b) of the Social Security Act), Title VI of the Civil Rights Act of 1964, the Age Discrimination Act of 1975, the Americans with Disabilities Act, the HIPAA administrative simplification rules at 45 CFR Part 160, 162, and 164, and the Rehabilitation Act of 1973. 26. Independent Contractor will comply with all applicable Medicare laws, regulations, and CMS instructions. Independent Contractor acknowledges that BCBSM shall oversee and monitor Independent Contractor’s performance on an ongoing basis. 27. In the event Independent Contractor performs work under this Medicare Advantage Addendum at an Offshore (Non-United States) location (referred to as “Offshore Subcontract Arrangement/Agreement”), including but not limited to work at an Offshore location by Independent Contractor’s employees or entering into an agreement with a subcontractor to perform work at an Offshore location, Independent Contractor will provide BCBSM the name, address and narrative description of Offshore functions and state the proposed or actual effective date for the Offshore Subcontract Arrangement/Agreement and further agrees to and will provide an attestation of the following: a. b. c. d. e. f. 28. The Offshore Subcontracting Arrangement/Agreement ensures that the Offshore subcontractor receives only the minimum amount of Protected Health Information (PHI) necessary to perform the services contemplated, and that policies and procedures are in place to ensure that PHI remains secure. The Offshore Subcontracting Arrangement/Agreement grants BCBSM (or, in the alternative, Independent Contractor at BCBSM’s request) the right to terminate the Subcontracting Arrangement/Agreement immediately without cause. The Offshore Subcontracting Arrangement /Agreement includes minimum necessary access provisions and prohibits access to BCBSM/BCN data by offshore resource not associated with providing services or functions to BCBSM/BCN; The Offshore Subcontracting Arrangement/Agreement contains the applicable required Medicare provisions contained in BCBSM’s Medicare Part C and D contracts (i.e. record retention requirements, compliance with all Medicare Part C and D requirements, etc). The Offshore Subcontracting Arrangement/Agreement grants Independent Contractor the right to conduct an annual audit of the Offshore subcontractor to evaluate the practices and procedures, including but not limited to PHI privacy and security controls, of the subcontractor and the audit results will be used to evaluate the continuation of the Offshore relationship. Independent Contractor agrees it shall conduct such an annual audit of Offshore activities and subcontractor, and that Independent Contractor shall share the results of the annual audit with both BCBSM and, if requested, CMS. To the extent Independent Contractor performs services or functions that are governed by the CMS Manual System, Pub. 100-16 Medicare Managed Care, Chapter 3, Medicare Marketing Guidelines for the Department of Health & Human Services Centers for Medicare & Medicaid Services, as amended, Independent Contractor agrees to comply with such guidelines. CMS’ authority for marketing oversight extends to include a range of different marketing materials and activities as noted in the guidelines. While not exhaustive, the following summaries are the responsibility of the Independent Contractor. Page 5 of 7 a. b. c. d. e. f. Communications going to Medicare Advantage members or prospects must comply with current CMS marketing guidelines. Communications are subject to BCBSM and BCN brand standards. Must prepare and provide compliant draft documents in an editable format. Provide a list of all member documents with details for how and when they will be distributed and to whom. No communications to members will be distributed without BCBSM approval and if required, CMS approval. Acknowledges that all communications going to Medicare beneficiaries are subject to the BCBSM’s review process. The definition of marketing materials includes any informational materials targeted to Medicare beneficiaries pursuant to 42 CFR 422.2260 and 42 CFR 423.2260. ADDITIONAL PROVISIONS FOR PROVIDER / HEALTH CARE DELIVERY AGREEMENTS 29. If Independent Contractor is a Provider, Independent Contractor is also prohibited from holding an Enrollee liable for Medicare Parts A and B cost sharing that is the legal obligation of the State or BCBSM. 30. If Independent Contractor is a Provider, BCBSM must provide for continuation of Enrollee health care benefits 1) for all Enrollees, for the duration of the contract period for which CMS payments have been made; and 2) for Enrollees who are hospitalized on the date its contract with CMS terminates, or in the event of BCBSM’s insolvency, through the date of discharge. 31. If BCBSM has delegated to Independent Contractor the selection of Providers, BCBSM shall retain the right to approve, suspend, or terminate such arrangement. 32. If BCBSM delegates to Independent Contractor the credentialing of Providers, BCBSM shall review and approve the credentialing process and will audit the credentialing process on an ongoing basis. 33. If Independent Contractor performs network contracting or otherwise is responsible for provider agreements, Independent Contractor shall ensure that the Provider Agreement specifies a prompt payment requirement, the terms and conditions of which are developed and agreed to by BCBSM and the contracted providers and suppliers. 34. If Independent Contractor is a Provider, Provider will include supporting documentation in a Member’s medical record for all diagnosis codes submitted by Provider to BCBSM for payment consistent with CMS guidelines. In the event of a CMS Risk Adjustment Data Validation (RADV) audit, Independent Contractor will be required to submit medical records for the validation of risk adjustment data. Provider acknowledges their obligation to cooperate with BCBSM and/or CMS during such audits and to timely produce requested medical records in accordance with 422.310(e). 35. Independent Contractor shall not discriminate against members in the delivery of health care services based on race, ethnicity, national origin, religion, sex, age, mental or physical disability or medical condition, health status, sexual orientation, claim experience, medical history, Page 6 of 7 evidence of insurability (including conditions arising out of acts of domestic violence), genetic information or source of payment. Page 7 of 7